Rasagiline by Alvogen, Inc. RASAGILINE tablet
Rasagiline by
Drug Labeling and Warnings
Rasagiline by is a Prescription medication manufactured, distributed, or labeled by Alvogen, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use RASAGILINE TABLETS safely and effectively. See full prescribing information for RASAGILINE TABLETS.
RASAGILINE tablets, for oral use
Initial U.S. Approval: 2006INDICATIONS AND USAGE
Rasagiline tablets, a monoamine oxidase (MAO)-B inhibitor (MAOI), is indicated for the treatment of Parkinson’s disease (1)
DOSAGE AND ADMINISTRATION
- Monotherapy: Rasagiline tablets 1 mg once daily (2.1)
- As adjunct without levodopa: Rasagiline tablets 1 mg once daily (2.1)
- As adjunct to levodopa: Rasagiline tablets 0.5 mg once daily. Increase dose to 1 mg daily as needed for sufficient clinical response (2.1)
- Patients taking ciprofloxacin or other CYP1A2 inhibitors: Rasagiline tablets 0.5 mg once daily (2.2, 5.4)
- Patients with mild hepatic impairment: Rasagiline tablets 0.5 mg once daily. Rasagiline tablets should not be used in patients with moderate or severe hepatic impairment (2.3, 5.5)
DOSAGE FORMS AND STRENGTHS
- Rasagiline tablets 0.5 mg (3)
- Rasagiline tablets 1 mg (3)
CONTRAINDICATIONS
Concomitant use of meperidine, tramadol, methadone, propoxyphene dextromethorphan, St. John’s wort, cyclobenzaprine, or another (selective or non-selective) MAO inhibitor (4)
WARNINGS AND PRECAUTIONS
- May cause hypertension (including severe hypertensive syndromes) at recommended doses (5.1)
- May cause serotonin syndrome when used with antidepressants (5.2)
- May cause falling asleep during activities of daily living, daytime drowsiness, and somnolence (5.3)
- May cause hypotension, especially orthostatic (5.6)
- May cause or exacerbate dyskinesia. Decreasing the levodopa dose may lessen or eliminate this side effect (5.7)
- May cause hallucinations and psychotic-like behavior (5.8)
- May cause impulse control/compulsive behaviors (5.9)
- May cause withdrawal-emergent hyperpyrexia and confusion (5.10)
ADVERSE REACTIONS
Most common adverse reactions (incidence 3% or greater than placebo):
- Rasagiline monotherapy: flu syndrome, arthralgia, depression, dyspepsia (6.1)
- Rasagiline used as adjunct without levodopa: peripheral edema, fall, arthralgia, cough, and insomnia (6.1)
- Rasagiline used as adjunct to levodopa: dyskinesia, accidental injury, weight loss, postural hypotension, vomiting, anorexia, arthralgia, abdominal pain, nausea, constipation, dry mouth, rash, abnormal dreams, fall, and tenosynovitis (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Alvogen, Inc. at 1-866-770-3024 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
USE IN SPECIFIC POPULATIONS
- Pregnancy: Based on animal data, may cause fetal harm. (8.1)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 3/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 General Dosing Recommendations
2.2 Patients Taking Ciprofloxacin or Other CYP1A2 Inhibitors
2.3 Patients with Hepatic Impairment
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Hypertension
5.2 Serotonin Syndrome
5.3 Falling Asleep During Activities of Daily Living and Somnolence
5.4 Ciprofloxacin or Other CYP1A2 Inhibitors
5.5 Hepatic Impairment
5.6 Hypotension / Orthostatic Hypotension
5.7 Dyskinesia
5.8 Hallucinations / Psychotic-Like Behavior
5.9 Impulse Control / Compulsive Behaviors
5.10 Withdrawal-Emergent Hyperpyrexia and Confusion
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
7 DRUG INTERACTIONS
7.1 Meperidine
7.2 Dextromethorphan
7.3 MAO Inhibitors
7.4 Sympathomimetic Medications
7.5 Antidepressants
7.6 Ciprofloxacin or Other CYP1A2 Inhibitors
7.7 Tyramine/Rasagiline Interaction
7.8 Dopaminergic Antagonists
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Hepatic Impairment
8.7 Renal Impairment
9 DRUG ABUSE AND DEPENDENCE
9.1 Controlled Substance
9.2 Abuse
9.3 Dependence
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Monotherapy Use of Rasagiline
14.2 Adjunct Use of Rasagiline
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 General Dosing Recommendations
When rasagiline tablets are prescribed as monotherapy or as adjunct therapy in patients not taking levodopa, patients may start rasagiline tablets at the recommended dose of 1 mg administered orally once daily.
In patients taking levodopa, with or without other PD drugs (e.g., dopamine agonist, amantadine, anticholinergics), the recommended initial dose of rasagiline tablets is 0.5 mg once daily. If the patient tolerates the daily 0.5 mg dose, but a sufficient clinical response is not achieved, the dose may be increased to 1 mg once daily. When rasagiline tablets are used in combination with levodopa, a reduction of the levodopa dose may be considered, based upon individual response.
The recommended doses of rasagiline tablets should not be exceeded because of risk of hypertension [see Warnings and Precautions (5.1)].
2.2 Patients Taking Ciprofloxacin or Other CYP1A2 Inhibitors
Patients taking concomitant ciprofloxacin or other CYP1A2 inhibitors should not exceed a dose of rasagiline tablets 0.5 mg once daily [see Warnings and Precautions (5.4), Drug Interactions (7.6), and Clinical Pharmacology (12.3)].
2.3 Patients with Hepatic Impairment
Patients with mild hepatic impairment should not exceed a dose of rasagiline tablets 0.5 mg once daily. Rasagiline tablets should not be used in patients with moderate or severe hepatic impairment [see Warnings and Precautions (5.5), Use in Specific Populations (8.6), and Clinical Pharmacology (12.3)].
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
Rasagiline is contraindicated for use with meperidine, tramadol, methadone, propoxyphene, and MAO inhibitors (MAOIs), including other selective MAO-B inhibitors, because of risk of serotonin syndrome [see Warnings and Precautions (5.2)]. At least 14 days should elapse between discontinuation of rasagiline and initiation of treatment with these medications.
Rasagiline is contraindicated for use with St. John’s wort and with cyclobenzaprine.
Rasagiline is contraindicated for use with dextromethorphan because of risk of episode of psychosis or bizarre behavior.
-
5 WARNINGS AND PRECAUTIONS
5.1 Hypertension
Exacerbation of hypertension may occur during treatment with rasagiline. Medication adjustment may be necessary if elevation of blood pressure is sustained. Monitor patients for new onset hypertension or hypertension that is not adequately controlled after starting rasagiline.
In Study 3, rasagiline (1 mg/day) given in conjunction with levodopa, produced an increased incidence of significant blood pressure elevation (systolic > 180 or diastolic > 100 mm Hg) of 4% compared to 3% for placebo [see Adverse Reactions (6.1)].
When used as an adjunct to levodopa (Studies 3 and 4), the risk for developing post-treatment high blood pressure (e.g., systolic > 180 or diastolic >100 mm Hg) combined with a significant increase from baseline (e.g., systolic > 30 or diastolic > 20 mm Hg) was higher for rasagiline (2%) compared to placebo (1%).
Dietary tyramine restriction is not required during treatment with recommended doses of rasagiline. However, certain foods that may contain very high amounts (i.e., more than 150 mg) of tyramine that could potentially cause severe hypertension because of tyramine interaction (including various clinical syndromes referred to as hypertensive urgency, crisis, or emergency) in patients taking rasagiline, even at the recommended doses, due to increased sensitivity to tyramine. Patients should be advised to avoid foods containing a very large amount of tyramine while taking recommended doses of rasagiline because of the potential for large increases in blood pressure including clinical syndromes referred to as hypertensive urgency, crisis, or emergency. Rasagiline is a selective inhibitor of MAO-B at the recommended doses of 0.5 or 1 mg daily. Selectivity for inhibiting MAO-B diminishes in a dose-related manner as the dose is progressively increased above the recommended daily doses.
5.2 Serotonin Syndrome
Serotonin syndrome has been reported with concomitant use of an antidepressant (e.g., selective serotonin reuptake inhibitors-SSRIs, serotonin-norepinephrine reuptake inhibitors-SNRIs, tricyclic antidepressants, tetracyclic antidepressants, triazolopyridine antidepressants) and a nonselective MAOI (e.g., phenelzine, tranylcypromine) or selective MAO-B inhibitors, such as selegiline (Eldepryl) and rasagiline. Serotonin syndrome has also been reported with concomitant use of rasagiline with meperidine, tramadol, methadone, or propoxyphene. Rasagiline is contraindicated for use with meperidine, tramadol, methadone, propoxyphene, and MAO inhibitors (MAOIs), including other selective MAO-B inhibitors [see Contraindications (4) and Drug Interactions (7.1, 7.2, 7.3)].
In the postmarketing period, potentially life-threatening serotonin syndrome has been reported in patients treated with antidepressants concomitantly with rasagiline. Concomitant use of rasagiline with one of many classes of antidepressants (e.g., SSRIs, SNRIs, triazolopyridine, tricyclic or tetracyclic antidepressants) is not recommended [see Drug Interactions (7.5)].
The symptoms of serotonin syndrome have included behavioral and cognitive/mental status changes (e.g., confusion, hypomania, hallucinations, agitation, delirium, headache, and coma), autonomic effects (e.g., syncope, shivering, sweating, high fever/hyperthermia, hypertension, tachycardia, nausea, diarrhea), and somatic effects (e.g., muscular rigidity, myoclonus, muscle twitching, hyperreflexia manifested by clonus, and tremor). Serotonin syndrome can result in death.
Rasagiline clinical trials did not allow concomitant use of fluoxetine or fluvoxamine with rasagiline, and the potential drug interaction between rasagiline and antidepressants has not been studied systematically. Although a small number of rasagiline-treated patients were concomitantly exposed to antidepressants (tricyclics n=115; SSRIs n=141), the exposure, both in dose and number of subjects, was not adequate to rule out the possibility of an untoward reaction from combining these agents. At least 14 days should elapse between discontinuation of rasagiline and initiation of treatment with a SSRI, SNRI, tricyclic, tetracyclic, or triazolopyridine antidepressant. Because of the long half-lives of certain antidepressants (e.g., fluoxetine and its active metabolite), at least five weeks (perhaps longer, especially if fluoxetine has been prescribed chronically and/or at higher doses) should elapse between discontinuation of fluoxetine and initiation of rasagiline [see Drug Interactions (7.5)].
5.3 Falling Asleep During Activities of Daily Living and Somnolence
It has been reported that falling asleep while engaged in activities of daily living always occurs in a setting of preexisting somnolence, although patients may not give such a history. For this reason, prescribers should monitor patients for drowsiness or sleepiness, because some of the events occur well after initiation of treatment with dopaminergic medication. Prescribers should also be aware that patients may not acknowledge drowsiness or sleepiness until directly questioned about drowsiness or sleepiness during specific activities.
Cases of patients treated with rasagiline and other dopaminergic medications have reported falling asleep while engaged in activities of daily living including the operation of motor vehicles, which sometimes resulted in accidents. Although many of these patients reported somnolence while on rasagiline with other dopaminergic medications, some perceived that they had no warning signs, such as excessive drowsiness, and believed that they were alert immediately prior to the event. Some of these events have been reported more than 1 year after initiation of treatment.
In Study 3, somnolence was a common occurrence in patients receiving rasagiline and was more frequent in patients with Parkinson’s disease receiving rasagiline than in respective patients receiving placebo (6% rasagiline compared to 4% Placebo) [see Adverse Reactions (6.1)].
Before initiating treatment with rasagiline, patients should be advised of the potential to develop drowsiness and specifically asked about factors that may increase the risk with rasagiline such as concomitant sedating medications, the presence of sleep disorders, and concomitant medications that increase rasagiline plasma levels (e.g., ciprofloxacin) [see Drug Interactions (7.6)]. If a patient develops significant daytime sleepiness or episodes of falling asleep during activities that require active participation (e.g., driving a motor vehicle, conversations, eating), rasagiline should ordinarily be discontinued. If a decision is made to continue these patients on rasagiline, advise them to avoid driving and other potentially dangerous activities. There is insufficient information to establish that dose reduction will eliminate episodes of falling asleep while engaged in activities of daily living.
5.4 Ciprofloxacin or Other CYP1A2 Inhibitors
Rasagiline plasma concentrations may increase up to 2 fold in patients using concomitant ciprofloxacin and other CYP1A2 inhibitors. Patients taking concomitant ciprofloxacin or other CYP1A2 inhibitors should not exceed a dose of rasagiline 0.5 mg once daily [see Dosage and Administration (2.2), Drug Interactions (7.6), and Clinical Pharmacology (12.3)].
5.5 Hepatic Impairment
Rasagiline plasma concentration may increase in patients with hepatic impairment. Patients with mild hepatic impairment should be given the dose of rasagiline 0.5 mg once daily. Rasagiline should not be used in patients with moderate or severe hepatic impairment [see Dosage and Administration (2.3) and Clinical Pharmacology (12.3)].
5.6 Hypotension / Orthostatic Hypotension
In Study 3, the incidence of orthostatic hypotension consisting of a systolic blood pressure decrease (≥30 mm Hg) or a diastolic blood pressure decrease (≥ 20 mm Hg) after standing was 13% with rasagiline (1 mg/day) compared to 9% with placebo [see Adverse Reactions (6.1)].
At the 1 mg dose, the frequency of orthostatic hypotension (at any time during the study) was approximately 44% for rasagiline vs 33% for placebo for mild to moderate systolic blood pressure decrements (≥ 20 mm Hg), 40% for rasagiline vs 33% for placebo for mild to moderate diastolic blood pressure decrements (≥ 10 mm Hg), 7% for rasagiline vs 3% for placebo for severe systolic blood pressure decrements (≥ 40 mm Hg), and 9% for rasagiline vs 6% for placebo for severe diastolic blood pressure decrements (≥ 20 mm Hg). There was also an increased risk for some of these abnormalities at the lower 0.5 mg daily dose and for an individual patient having mild to moderate or severe orthostatic hypotension for both systolic and diastolic blood pressure.
In Study 2 where rasagiline was given as an adjunct therapy in patients not taking concomitant levodopa, there were 5 reports of orthostatic hypotension in patients taking rasagiline 1 mg (3.1%) and 1 report in patients taking placebo (0.6%) [see Adverse Reactions (6.1)].
Clinical trial data further suggest that orthostatic hypotension occurs most frequently in the first two months of rasagiline treatment and tends to decrease over time.
Some patients treated with rasagiline experienced a mildly increased risk for significant decreases in blood pressure unrelated to standing but while supine.
The risk for post-treatment hypotension (e.g., systolic < 90 or diastolic < 50 mm Hg) combined with a significant decrease from baseline (e.g., systolic > 30 or diastolic > 20 mm Hg) was higher for rasagiline 1 mg (3.2%) compared to placebo (1.3%).
There was no clear increased risk for lowering of blood pressure or postural hypotension associated with rasagiline 1 mg/day as monotherapy.
When used as an adjunct to levodopa, postural hypotension was also reported as an adverse reaction in approximately 6% of patients treated with rasagiline 0.5 mg, 9% of patients treated with rasagiline 1 mg and 3% of patients treated with placebo. Postural hypotension led to drug discontinuation and premature withdrawal from clinical trials in one (0.7%) patient treated with rasagiline 1 mg/day, no patients treated with rasagiline 0.5 mg/day and no placebo-treated patients.
5.7 Dyskinesia
When used as an adjunct to levodopa, rasagiline may cause dyskinesia or potentiate dopaminergic side effects and exacerbate preexisting dyskinesia. In Study 3, the incidence of dyskinesia was 18% for patients treated with 0.5 mg or 1 mg rasagiline as an adjunct to levodopa and 10% for patients treated with placebo as an adjunct to levodopa. Decreasing the dose of levodopa may mitigate this side effect [see Adverse Reactions (6.1)].
5.8 Hallucinations / Psychotic-Like Behavior
In the monotherapy study (Study 1), the incidence of hallucinations reported as an adverse event was 1.3% in patients treated with rasagiline 1 mg and 0.7% in patients treated with placebo. In Study 1, the incidence of hallucinations reported as an adverse reaction and leading to drug discontinuation and premature withdrawal was 1.3% in patients treated with rasagiline 1 mg and 0% in placebo-treated patients.
When studied as an adjunct therapy without levodopa (Study 2), hallucinations were reported as an adverse reaction in 1.2% of patients treated with 1 mg/day rasagiline and 1.8% of patients treated with placebo. Hallucinations led to drug discontinuation and premature withdrawal from the clinical trial in 0.6% of patients treated with rasagiline 1 mg/day and in none of the placebo-treated patients.
When studied as an adjunct to levodopa (Study 3), the incidence of hallucinations was approximately 5% in patients treated with rasagiline 0.5 mg/day, 4% in patients treated with rasagiline 1 mg/day, and 3% in patients treated with placebo. The incidence of hallucinations leading to drug discontinuation and premature withdrawal was about 1% in patients treated with 0.5 mg rasagiline and 1 mg rasagiline per day, and 0% in placebo-treated patients [see Adverse Reactions (6.1)].
Postmarketing reports indicate that patients may experience new or worsening mental status and behavioral changes, which may be severe, including psychotic-like behavior during treatment with rasagiline or after starting or increasing the dose of rasagiline. Other drugs prescribed to improve the symptoms of Parkinson’s disease can have similar effects on thinking and behavior. This abnormal thinking and behavior can consist of one or more of a variety of manifestations including paranoid ideation, delusions, hallucinations, confusion, psychotic-like behavior, disorientation, aggressive behavior, agitation, and delirium.
Patients should be informed of the possibility of developing hallucinations and instructed to report them to their healthcare provider promptly should they develop.
Patients with a major psychotic disorder should ordinarily not be treated with rasagiline because of the risk of exacerbating the psychosis with an increase in central dopaminergic tone. In addition, many treatments for psychosis that decrease central dopaminergic tone may decrease the effectiveness of rasagiline [see Drug Interactions (7.8)].
Consider dose reduction or stopping the medication if a patient develops hallucinations or psychotic like behaviors while taking rasagiline.
5.9 Impulse Control / Compulsive Behaviors
Case reports suggest that patients can experience intense urges to gamble, increased sexual urges, intense urges to spend money, binge eating, and/or other intense urges, and the inability to control these urges while taking one or more of the medications, including rasagiline, that increase central dopaminergic tone and that are generally used for the treatment of Parkinson’s disease. In some cases, although not all, these urges were reported to have stopped when the dose was reduced or the medication was discontinued. Because patients may not recognize these behaviors as abnormal, it is important for prescribers to specifically ask patients or their caregivers about the development of new or increased gambling urges, sexual urges, uncontrolled spending, or other urges while being treated with rasagiline. Consider dose reduction or stopping the medication if a patient develops such urges while taking rasagiline.
5.10 Withdrawal-Emergent Hyperpyrexia and Confusion
A symptom complex resembling neuroleptic malignant syndrome (characterized by elevated temperature, muscular rigidity, altered consciousness, and autonomic instability), with no other obvious etiology, has been reported in association with rapid dose reduction, withdrawal of, or changes in drugs that increase central dopaminergic tone.
-
6 ADVERSE REACTIONS
The following adverse reactions are described in more detail in the Warnings and Precautions section of the label:
- Hypertension [see Warnings and Precautions (5.1)]
- Serotonin Syndrome [see Warnings and Precautions (5.2)]
- Falling Asleep During Activities of Daily Living and Somnolence [see Warnings and Precautions (5.3)]
- Hypotension / Orthostatic Hypotension [see Warnings and Precautions (5.6)]
- Dyskinesia [see Warnings and Precautions (5.7)]
- Hallucinations / Psychotic-Like Behavior [see Warnings and Precautions (5.8)]
- Impulse Control /Compulsive Behaviors [see Warnings and Precautions (5.9)]
- Withdrawal-Emergent Hyperpyrexia and Confusion [see Warnings and Precautions (5.10)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to the incidence of adverse reactions in the clinical trials of another drug and may not reflect the rates of adverse reactions observed in practice.
During the clinical development of rasagiline, Parkinson’s disease patients received rasagiline as initial monotherapy (Study 1) and as adjunct therapy (Study 2, Study 3, Study 4). As the populations in these studies differ, not only in the adjunct use of dopamine agonists or levodopa during rasagiline treatment, but also in the severity and duration of their disease, the adverse reactions are presented separately for each study.
Monotherapy Use of Rasagiline
In Study 1, approximately 5% of the 149 patients treated with rasagiline discontinued treatment due to adverse reactions compared to 2% of the 151 patients who received placebo.The only adverse reaction that led to the discontinuation of more than one patient was hallucinations.
The most commonly observed adverse reactions in Study 1 (incidence in rasagiline-treated patients 3% or greater than the incidence in placebo-treated patients) included flu syndrome, arthralgia, depression, and dyspepsia. Table 1 lists adverse reactions that occurred in 2% or greater of patients receiving rasagiline as monotherapy and were numerically more frequent than in the placebo group in Study 1.
Table 1: Adverse Reactions* in Study 1 Rasagiline 1 mg (N=149) Placebo
(N=151)% of Patients % of Patients Headache 14 12 Arthralgia 7 4 Dyspepsia 7 4 Depression 5 2 Fall 5 3 Flu syndrome 5 1 Conjunctivitis 3 1 Fever 3 1 Gastroenteritis 3 1 Rhinitis 3 1 Arthritis 2 1 Ecchymosis 2 0 Malaise 2 0 Neck Pain 2 0 Paresthesia 2 1 Vertigo 2 1 *Incidence 2% or greater in rasagiline 1 mg group and numerically more frequent than in placebo group
There were no significant differences in the safety profile based on age or gender.
Adjunct Use of Rasagiline
Rasagiline was studied as an adjunct therapy without levodopa (Study 2), or as an adjunct therapy to levodopa, with some patients also taking dopamine agonists, COMT inhibitors, anticholinergics, or amantadine (Study 3 and Study 4).
In Study 2, approximately 8% of the 162 patients treated with rasagiline discontinued treatment due to adverse reactions compared to 4% of the 164 patients who received placebo.
Adverse reactions that led to the discontinuation of more than one patient were nausea and dizziness.
The most commonly observed adverse reactions in Study 2 (incidence in rasagiline-treated patients 3% or greater than incidence in placebo-treated patients) included peripheral edema, fall, arthralgia, cough, and insomnia. Table 2 lists adverse reactions that occurred in 2% or greater in patients receiving rasagiline as adjunct therapy without levodopa and numerically more frequent than in the placebo group in Study 2.
Table 2: Adverse Reactions* in Study 2 Rasagiline 1 mg
(N=162)Placebo
(N=164)% of Patients % of Patients Dizziness 7 6 Peripheral edema 7 4 Headache 6 4 Nausea 6 4 Fall 6 1 Arthralgia 5 2 Back pain 4 3 Cough 4 1 Insomnia 4 1 Upper respiratory tract infection 4 2 Orthostatic hypotension 3 1 * Incidence 2% or greater in rasagiline 1 mg group and numerically more frequent than in placebo group
There were no significant differences in the safety profile based on age or gender.
In Study 3, adverse event reporting was considered more reliable than Study 4; therefore, only the adverse event data from Study 3 are presented below.
In Study 3, approximately 9% of the 164 patients treated with rasagiline 0.5 mg/day and 7% of the 149 patients treated with rasagiline 1 mg/day discontinued treatment due to adverse reactions, compared to 6% of the 159 patients who received placebo. The adverse reactions that led to discontinuation of more than one rasagiline-treated patient were diarrhea, weight loss, hallucination, and rash.
The most commonly observed adverse reactions in Study 3 (incidence in rasagiline-treated patients 3% or greater than the incidence in placebo-treated patients) included dyskinesia, accidental injury, weight loss, postural hypotension, vomiting, anorexia, arthralgia, abdominal pain, nausea, constipation, dry mouth, rash, abnormal dreams, fall, and tenosynovitis.
Table 3 lists adverse reactions that occurred in 2% or greater of patients treated with rasagiline 1 mg/day and that were numerically more frequent than the placebo group in Study 3.
Table 3: Adverse Reactions* in Study 3 Rasagiline 1 mg
(N=149)Rasagiline 0.5 mg
(N=164)Placebo (N=159) % of Patients % of Patients % of Patients Dyskinesia 18 18 10 Accidental injury 12 8 5 Nausea 12 10 8 Headache 11 8 10 Fall 11 12 8 Weight loss 9 2 3 Constipation 9 4 5 Postural hypotension 9 6 3 Arthralgia 8 6 4 Vomiting 7 4 1 Dry mouth 6 2 3 Rash 6 3 3 Somnolence 6 4 4 Abdominal pain 5 2 1 Anorexia 5 2 1 Diarrhea 5 7 4 Ecchymosis 5 2 3 Dyspepsia 5 4 4 Paresthesia 5 2 3 Abnormal dreams 4 1 1 Hallucinations 4 5 3 Ataxia 3 6 1 Dyspnea 3 5 2 Infection 3 2 2 Neck pain 3 1 1 Sweating 3 2 1 Tenosynovitis 3 1 0 Dystonia 3 2 1 Gingivitis 2 1 1 Hemorrhage 2 1 1 Hernia 2 1 1 Myasthenia 2 2 1 *Incidence 2% or greater in rasagiline 1 mg group and numerically more frequent than in placebo group
Several of the more common adverse reactions seemed dose-related, including weight loss, postural hypotension, and dry mouth.
There were no significant differences in the safety profile based on age or gender.
During all Parkinson's disease phase 2/3 clinical trials, the long-term safety profile was similar to that observed with shorter duration exposure.
-
7 DRUG INTERACTIONS
7.1 Meperidine
Serious, sometimes fatal reactions have been precipitated with concomitant use of meperidine (e.g., Demerol and other tradenames) and MAO inhibitors including selective MAO-B inhibitors [see Contraindications (4)].
7.2 Dextromethorphan
The concomitant use of rasagiline and dextromethorphan was not allowed in clinical studies. The combination of MAO inhibitors and dextromethorphan has been reported to cause brief episodes of psychosis or bizarre behavior. Therefore, in view of rasagiline’s MAO inhibitory activity, dextromethorphan is contraindicated for use with rasagiline [see Contraindications (4)].
7.3 MAO Inhibitors
Rasagiline is contraindicated for use with other MAO inhibitors because of the increased risk of nonselective MAO inhibition that may lead to a hypertensive crisis [see Contraindications (4)].
7.4 Sympathomimetic Medications
The concomitant use of rasagiline and sympathomimetic medications was not allowed in clinical studies. Severe hypertensive reactions have followed the administration of sympathomimetics and nonselective MAO inhibitors. Hypertensive crisis has been reported in patients taking the recommended dose of rasagiline and sympathomimetic medications. Severe hypertension has been reported in patients taking the recommended dose of rasagiline and ophthalmic drops containing sympathomimetic medications.
Because rasagiline is a selective MAOI, hypertensive reactions are not ordinarily expected with the concomitant use of sympathomimetic medications. Nevertheless, caution should be exercised when concomitantly using recommended doses of rasagiline with any sympathomimetic medications including nasal, oral, and ophthalmic decongestants and cold remedies.
7.5 Antidepressants
Concomitant use of rasagiline with one of many classes of antidepressants (e.g., SSRIs, SNRIs, triazolopyridine, tricyclic, or tetracyclic antidepressants) is not recommended [see Warnings and Precautions (5.2) and Clinical Pharmacology (12.3)]. Concomitant use of rasagiline and MAO inhibitors is contraindicated [see Contraindications (4)].
7.6 Ciprofloxacin or Other CYP1A2 Inhibitors
Rasagiline plasma concentrations may increase up to 2 fold in patients using concomitant ciprofloxacin and other CYP1A2 inhibitors. This could result in increased adverse events. Patients taking concomitant ciprofloxacin or other CYP1A2 inhibitors should not exceed a dose of rasagiline 0.5 mg once daily [see Warnings and Precautions (5.4) and Clinical Pharmacology (12.3)].
7.7 Tyramine/Rasagiline Interaction
MAO in the gastrointestinal tract and liver (primarily type A) provides protection from exogenous amines (e.g., tyramine) that have the capacity, if absorbed intact, to cause a tyramine reaction with hypertension including clinical syndromes referred to as hypertensive urgency, crisis, or emergency. Foods and medications containing large amounts of exogenous amines (e.g., from fermented cheese, herring, over-the-counter cough/cold medications) may cause release of norepinephrine resulting in a rise in systemic blood pressure.
Results of a special tyramine challenge study indicate that rasagiline is selective for MAO-B at recommended doses and can be used without dietary tyramine restriction. However, certain foods may contain very high amounts (i.e., 150 mg or greater) of tyramine and could potentially cause a hypertensive reaction in individual patients taking rasagiline due to increased sensitivity to tyramine. Selectivity for inhibiting MAO-B diminishes in a dose-related manner as the dose is progressively increased above the recommended daily doses.
There were no cases of hypertensive crisis in the clinical development program associated with 1 mg daily rasagiline treatment, in which most patients did not follow dietary tyramine restriction.
There have been postmarketing reports of patients who experienced significantly elevated blood pressure (including rare cases of hypertensive crisis) after ingestion of unknown amounts of tyramine-rich foods while taking recommended doses of rasagiline. Patients should be advised to avoid foods containing a very large amount of tyramine while taking recommended doses of rasagiline [see Warnings and Precautions (5.1)].
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There are no adequate data on the developmental risks associated with the use of rasagiline in pregnant women. In animal studies, oral administration of rasagiline to rats during gestation and lactation resulted in decreased survival and reduced body weight in the offspring at doses similar to those used clinically. When administered to pregnant animals in combination with levodopa/carbidopa, there were increased incidences of fetal skeletal variations in rats and increases in embryofetal death and cardiovascular abnormalities in rabbits [see Data].In the US general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively. The background risks of major birth defects and miscarriage for the indicated population is unknown.
Data
Animal Data
In a combined mating/fertility and embryofetal development study in pregnant rats, no effect on embryofetal development was observed at oral doses up to 3 mg/kg/day (approximately 30 times the plasma exposure (AUC) in humans at the maximum recommended human dose [MRHD, 1 mg/day]).In pregnant rabbits administered rasagiline throughout the period of organogenesis at oral doses of up to 36 mg/kg/day, no developmental toxicity was observed. At the highest dose tested, the plasma AUC was approximately 800 times that in humans at the MRHD.
In pregnant rats administered rasagiline (0, 0.1, 0.3, 1 mg/kg/day) orally during gestation and lactation, offspring survival was decreased and offspring body weight was reduced at 0.3 mg/kg/day and 1 mg/kg/day (10 and 16 times the plasma AUC in humans at the MRHD). The no-effect dose (0.1 mg/kg) for adverse developmental effects is similar to the MRHD on a body surface area (mg/m2) basis. The effect of rasagiline on physical and behavioral development was not adequately assessed in this study.
Rasagiline may be given as an adjunct therapy to levodopa/carbidopa treatment. In pregnant rats administered rasagiline (0, 0.1, 0.3, 1 mg/kg/day) and levodopa/carbidopa (80/20 mg/kg/day) (alone and in combination) orally throughout the period of organogenesis, there was an increased incidence of fetal skeletal variations in fetuses from rats treated with rasagiline in combination with levodopa/carbidopa at 1/80/20 mg/kg/day (approximately 8 times the rasagiline plasma AUC in humans at the MRHD and similar to the MRHD of levodopa/carbidopa [800/200 mg/day] on a mg/m2 basis). In pregnant rabbits dosed orally throughout the period of organogenesis with rasagiline alone (3 mg/kg) or in combination with levodopa/carbidopa (rasagiline: 0.1, 0.6, 1.2 mg/kg, levodopa/carbidopa: 80/20 mg/kg/day), an increase in embryofetal death was noted at rasagiline doses of 0.6 and 1.2 mg/kg/day when administered in combination with levodopa/carbidopa (approximately 7 and 13 times, respectively, the rasagiline plasma AUC in humans at the MRHD). There was an increase in cardiovascular abnormalities with levodopa/carbidopa alone (similar to the MRHD on a mg/m2 basis) and to a greater extent when rasagiline (at all doses; 1 to 13 times the rasagiline plasma AUC in humans at the MRHD) was administered in combination with levodopa/carbidopa.
8.2 Lactation
Risk Summary
There are no data on the presence of rasagiline in human milk or the effects on the breastfed infant. In rats, rasagiline was shown to inhibit prolactin secretion. The clinical relevance in humans is unknown, and there are no data on the effects of rasagiline on prolactin secretion or milk production in humans.The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for rasagiline and any potential adverse effects on the breastfed infant from rasagiline or from the underlying maternal condition.
8.5 Geriatric Use
Approximately half of patients in clinical trials were 65 years and over. There were no significant differences in the safety profile of the geriatric and nongeriatric patients.
8.6 Hepatic Impairment
Rasagiline plasma concentration may be increased in patients with mild (up to 2 fold, Child-Pugh score 5 to 6), moderate (up to 7 fold, Child-Pugh score 7 to 9), and severe (Child-Pugh score 10 to 15) hepatic impairment. Patients with mild hepatic impairment should not exceed a dose of 0.5 mg/day. Rasagiline should not be used in patients with moderate or severe hepatic impairment [see Dosage and Administration (2.3), Warnings and Precautions (5.5) and Clinical Pharmacology (12.3)].
8.7 Renal Impairment
Dose adjustment of rasagiline is not required for patients with mild or moderate renal impairment because rasagiline plasma concentrations are not increased in patients with moderate renal impairment. Rasagiline has not been studied in patients with severe renal impairment [see Clinical Pharmacology (12.3)].
-
9 DRUG ABUSE AND DEPENDENCE
9.2 Abuse
Studies conducted in mice and rats did not reveal any potential for drug abuse and dependence. Clinical trials have not revealed any evidence of the potential for abuse, tolerance, or physical dependence; however, systematic studies in humans designed to evaluate these effects have not been performed.
9.3 Dependence
Studies conducted in mice and rats did not reveal any potential for drug abuse and dependence. Clinical trials have not revealed any evidence of the potential for abuse, tolerance, or physical dependence; however, systematic studies in humans designed to evaluate these effects have not been performed.
-
10 OVERDOSAGE
In a dose escalation study in patients on chronic levodopa therapy treated with 10 mg of rasagiline there were three reports of cardiovascular side effects (including hypertension and postural hypotension) which resolved following treatment discontinuation. Although no cases of overdose have been observed with rasagiline during the clinical development program, the following description of presenting symptoms and clinical course is based upon overdose descriptions of nonselective MAO inhibitors.
The signs and symptoms of nonselective MAOI overdose may not appear immediately. Delays of up to 12 hours after ingestion of drug and the appearance of signs may occur. The peak intensity of the syndrome may not be reached until for a day following the overdose. Death has been reported following overdose; therefore, immediate hospitalization, with continuous patient observation and monitoring for at least two days following the ingestion of such drugs in overdose, is strongly recommended.
The severity of the clinical signs and symptoms of MAOI overdose varies and may be related to the amount of drug consumed. The central nervous and cardiovascular systems are prominently involved.
Signs and symptoms of MAOI overdose may include: drowsiness, dizziness, faintness, irritability, hyperactivity, agitation, severe headache, hallucinations, trismus, opisthotonos, convulsions, and coma; rapid and irregular pulse, hypertension, hypotension and vascular collapse; precordial pain, respiratory depression and failure, hyperpyrexia, diaphoresis, and cool, clammy skin.
There is no specific antidote for rasagiline overdose. The following suggestions are offered based upon the assumption that rasagiline overdose may be modeled after nonselective MAO inhibitor poisoning. Treatment of overdose with nonselective MAO inhibitors is symptomatic and supportive. Respiration should be supported by appropriate measures, including management of the airway, use of supplemental oxygen, and mechanical ventilatory assistance, as required. Body temperature should be monitored closely. Intensive management of hyperpyrexia may be required. Maintenance of fluid and electrolyte balance is essential. For this reason, in cases of overdose with rasagiline, dietary tyramine restriction should be observed for several weeks to reduce the risk of hypertensive tyramine reaction.
A poison control center should be called for the most current treatment guidelines.
A postmarketing report described a single patient who developed a nonfatal serotonin syndrome after ingesting 100 mg of rasagiline in a suicide attempt. Another patient who was treated in error with 4 mg rasagiline daily and tramadol also developed a serotonin syndrome. One patient who was treated in error with 3 mg rasagiline daily experienced alternating episodes of vascular fluctuations consisting of hypertension and orthostatic hypotension.
-
11 DESCRIPTION
Rasagiline tablets contain rasagiline (as the mesylate), a propargylamine-based drug indicated for the treatment of idiopathic Parkinson’s disease. Rasagiline mesylate is designated chemically as: 1H-Inden-1-amine,2,3-dihydro-N-2-propynyl-,(1R)-,
methanesulfonate. The molecular formula of rasagiline mesylate is C12H13NCH4SO3 and its molecular weight is 267.34.Its structural formula is:
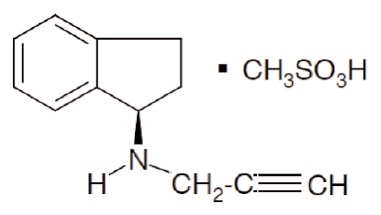
Rasagiline mesylate is a white to off-white powder, freely soluble in water or ethanol and sparingly soluble in isopropanol. Each rasagiline tablet for oral administration contains 0.5 mg or 1 mg of rasagiline (equivalent to 0.78 mg or 1.56 mg of rasagiline mesylate).
Each rasagiline tablet also contains the following inactive ingredients: lactose monohydrate, pregelatinized starch, corn starch, talc, stearic acid, and citric acid monohydrate.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Rasagiline is a selective, irreversible MAO-B inhibitor indicated for the treatment of idiopathic Parkinson’s disease. The results of a clinical trial designed to examine the effects of rasagiline on blood pressure when it is administered with increasing doses of tyramine indicates the functional selectivity can be incomplete when healthy subjects ingest large amounts of tyramine while receiving recommended doses of rasagiline. The selectivity for inhibiting MAO-B diminishes in a dose-related manner.
MAO, a flavin-containing enzyme, is classified into two major molecular species, A and B, and is localized in mitochondrial membranes throughout the body in nerve terminals, brain, liver and intestinal mucosa. MAO regulates the metabolic degradation of catecholamines and serotonin in the CNS and peripheral tissues. MAO-B is the major form in the human brain. In ex vivo animal studies in brain, liver, and intestinal tissues, rasagiline was shown to be a potent, irreversible monoamine oxidase type B (MAO-B) selective inhibitor. Rasagiline at the recommended therapeutic dose was also shown to be a potent and irreversible inhibitor of MAO-B in platelets. The precise mechanisms of action of rasagiline are unknown. One mechanism is believed to be related to its MAO-B inhibitory activity, which causes an increase in extracellular levels of dopamine in the striatum. The elevated dopamine level and subsequent increased dopaminergic activity are likely to mediate rasagiline’s beneficial effects seen in models of dopaminergic motor dysfunction.
12.2 Pharmacodynamics
Tyramine Challenge Test
Results of a tyramine challenge study indicate that rasagiline at recommended doses is relatively selective for inhibiting MAO-B and can be used without dietary tyramine restriction. However, certain foods (e.g., aged cheeses, such as Stilton cheese) may contain very high amounts of tyramine (i.e., 150 mg or greater) and could potentially cause severe hypertension caused by tyramine interaction in patients taking rasagiline due to mild increased sensitivity to tyramine at recommended doses. Relative selectivity of rasagiline for inhibiting MAO-B diminished in a dose-related manner as the dose progressively increased above the highest recommended daily dose (1 mg) [see Warnings and Precautions (5.1) and Drug Interactions (7.7)].
Platelet MAO Activity in Clinical Studies
Studies in healthy subjects and in Parkinson’s disease patients have shown that rasagiline inhibits platelet MAO-B irreversibly. The inhibition lasts at least 1 week after last dose. Almost 25 to 35% MAO-B inhibition was achieved after a single rasagiline dose of 1 mg/day and more than 55% of MAO-B inhibition was achieved after a single rasagiline dose of 2 mg/day. Over 90% inhibition was achieved 3 days after rasagiline daily dosing at 2 mg/day and this inhibition level was maintained 3 days postdose. Multiple doses of rasagiline of 0.5, 1, and 2 mg per day resulted in complete MAO-B inhibition.
12.3 Pharmacokinetics
Rasagiline in the range of 1 to 6 mg demonstrated a more than proportional increase in AUC, while Cmax was dose proportional. Rasagiline mean steady-state half life is 3 hours but there is no correlation of pharmacokinetics with its pharmacological effect because of its irreversible inhibition of MAO-B.
Absorption
Rasagiline is rapidly absorbed, reaching peak plasma concentration (Cmax) in approximately 1 hour. The absolute bioavailability of rasagiline is about 36%.Food does not affect the Tmax of rasagiline, although Cmax and exposure (AUC) are decreased by approximately 60% and 20%, respectively, when the drug is taken with a high fat meal. Because AUC is not significantly affected, rasagiline can be administered with or without food.
Distribution
The mean volume of distribution at steady-state is 87 L, indicating that the tissue binding of rasagiline is in excess of plasma protein binding. Plasma protein binding ranges from 88 to 94% with mean extent of binding of 61 to 63% to human albumin over the concentration range of 1 to 100 ng/mL.Metabolism and Elimination
Rasagiline undergoes almost complete biotransformation in the liver prior to excretion. The metabolism of rasagiline proceeds through two main pathways: N-dealkylation and/or hydroxylation to yield 1-aminoindan (AI), 3-hydroxy-N-propargyl-1-aminoindan (3-OH-PAI) and 3-hydroxy-1-aminoindan (3-OH-AI). In vitro experiments indicate that both routes of rasagiline metabolism are dependent on the cytochrome P450 (CYP) system, with CYP1A2 being the major isoenzyme involved in rasagiline metabolism. Glucuronide conjugation of rasagiline and its metabolites, with subsequent urinary excretion, is the major elimination pathway.After oral administration of 14C-labeled rasagiline, elimination occurred primarily via urine and secondarily via feces (62% of total dose in urine and 7% of total dose in feces over 7 days), with a total calculated recovery of 84% of the dose over a period of 38 days. Less than 1% of rasagiline was excreted as unchanged drug in urine.
Specific Populations
Hepatic Impairment
Following repeat dose administration (7 days) of rasagiline (1 mg/day) in subjects with mild hepatic impairment (Child-Pugh score 5 to 6), AUC and Cmax were increased by 2 fold and 1.4 fold, respectively, compared to healthy subjects. In subjects with moderate hepatic impairment (Child-Pugh score 7 to 9), AUC and Cmax were increased by 7 fold and 2 fold, respectively, compared to healthy subjects [see Dosage and Administration (2.3) and Warnings and Precautions (5.5)].Renal Impairment
Following repeat dose administration (8 days) of rasagiline (1 mg/day) in subjects with moderate renal impairment, rasagiline exposure (AUC) was similar to rasagiline exposure in healthy subjects, while the major metabolite 1-AI exposure (AUC) was increased 1.5 fold in subjects with moderate renal impairment, compared to healthy subjects. Because 1-AI is not an MAO inhibitor, no dose adjustment is needed for patients with mild and moderate renal impairment. Data are not available for patients with severe renal impairment.Elderly
Since age has little influence on rasagiline pharmacokinetics, it can be administered at the recommended dose in the elderly (≥ 65 years).Pediatric
Rasagiline has not been investigated in patients below 18 years of age.Gender
The pharmacokinetic profile of rasagiline is similar in men and women.Drug-Drug Interactions
Levodopa
A study in Parkinson’s disease patients, in which the effect of levodopa/carbidopa (LD/CD) on rasagiline pharmacokinetics at steady state was investigated, showed that the pharmacokinetics of rasagiline were not affected by concomitant administration of LD/CD.Effect of Other Drugs on the Metabolism of Rasagiline
In vitro metabolism studies showed that CYP1A2 was the major enzyme responsible for the metabolism of rasagiline. There is the potential for inhibitors of this enzyme to alter rasagiline clearance when coadministered [see Dosage and Administration (2.2) and Warnings and Precautions (5.4)].Ciprofloxacin: When ciprofloxacin, an inhibitor of CYP1A2, was administered to healthy volunteers (n=12) at 500 mg (BID) with rasagiline at 2 mg/day, the AUC of rasagiline increased by 83% and there was no change in the elimination half life [see Dosage and Administration (2.2) and Warnings and Precautions (5.4)].
Theophylline: Coadministration of rasagiline 1 mg/day and theophylline, a substrate of CYP1A2, up to 500 mg twice daily to healthy subjects (n=24) did not affect the pharmacokinetics of either drug.
Antidepressants: Severe CNS toxicity (occasionally fatal) associated with hyperpyrexia as part of a serotonin syndrome, has been reported with combined treatment of an antidepressant (e.g., from one of many classes including tricyclic or tetracyclic antidepressants, SSRIs, SNRIs, triazolopyridine antidepressants) and nonselective MAOI or a selective MAO-B inhibitor [see Warnings and Precautions (5.2)].
Effect of Rasagiline on Other Drugs
No additional in vivo trials have investigated the effect of rasagiline on other drugs metabolized by the cytochrome P450 enzyme system. In vitro studies showed that rasagiline at a concentration of 1 mcg/mL (equivalent to a level that is 160 times the average Cmax ~ 5.9 to 8.5 ng/mL in Parkinson’s disease patients after 1 mg rasagiline multiple dosing) did not inhibit cytochrome P450 isoenzymes, CYP1A2, CYP2A6, CYP2C9, CYP2C19, CYP2D6, CYP2E1, CYP3A4 and CYP4A. These results indicate that rasagiline is unlikely to cause any clinically significant interference with substrates of these enzymes. -
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Two-year carcinogenicity studies were conducted in mice at oral doses of 0, 1, 15, and 45 mg/kg/day and in rats at oral doses of 0.3, 1, and 3 mg/kg/day (males) or 0, 0.5, 2, 5, and 17 mg/kg/day (females). In rats, there was no increase in tumors at any dose tested. Plasma exposures (AUC) at the highest dose tested were approximately 33 and 260 times, in male and female rats, respectively, that in humans at the maximum recommended human dose (MRHD) of 1 mg/day.
In mice, there was an increase in lung tumors (combined adenomas/carcinomas) at 15 and 45 mg/kg in males and females. At the lowest dose tested, plasma AUCs were approximately 5 times those expected in humans at the MRHD.
The carcinogenic potential of rasagiline administered in combination with levodopa/carbidopa has not been examined.
Mutagenesis
Rasagiline was reproducibly clastogenic in in vitro chromosomal aberration assays in human lymphocytes in the presence of metabolic activation and was mutagenic and clastogenic in the in vitro mouse lymphoma tk assay in the absence and presence of metabolic activation. Rasagiline was negative in the in vitro bacterial reverse mutation (Ames) assay and in the in vivo micronucleus assay in mice. Rasagiline was also negative in the in vivo micronucleus assay in mice when administered in combination with levodopa/carbidopa.Impairment of Fertility
Rasagiline had no effect on mating performance or fertility in rats treated prior to and throughout the mating period and continuing in females through gestation day 17 at oral doses of up to 3 mg/kg/day (approximately 30 times the plasma AUC in humans at the MRHD). The effect of rasagiline administered in combination with levodopa/carbidopa on mating and fertility has not been examined. -
14 CLINICAL STUDIES
The effectiveness of rasagiline for the treatment of Parkinson’s disease was established in four 18 to 26 week, randomized, placebo-controlled trials, as initial monotherapy or adjunct therapy.
14.1 Monotherapy Use of Rasagiline
Study 1 was a double-blind, randomized, fixed-dose parallel group, 26 week study in early Parkinson’s disease patients not receiving any concomitant dopaminergic therapy at the start of the study. The majority of the patients were not treated with medications for Parkinson’s disease before receiving rasagiline.
In Study 1, 404 patients were randomly assigned to receive placebo (138 patients), rasagiline 1 mg/day (134 patients) or rasagiline 2 mg/day (132 patients). Patients were not allowed to take levodopa, dopamine agonists, selegiline, or amantadine, but could take stable doses of anticholinergic medication, if necessary. The average Parkinson’s disease duration was approximately 1 year (range 0 to 11 years).
The primary measure of effectiveness was the change from baseline in the total score of the Unified Parkinson’s Disease Rating Scale (UPDRS), [mentation (Part I) + activities of daily living (ADL) (Part II) + motor function (Part III)]. The UPDRS is a multi-item rating scale that measures the ability of a patient to perform mental and motor tasks as well as activities of daily living. A reduction in the score represents improvement and a beneficial change from baseline appears as a negative number.
Rasagiline (1 or 2 mg once daily) was superior to placebo on the primary measure of effectiveness in patients receiving six months of treatment and not on dopaminergic therapy. The effectiveness of rasagiline 1 mg and 2 mg was comparable. Table 4 shows the results of Study 1. There were no differences in effectiveness based on age or gender between rasagiline 1 mg/day and placebo.
Table 4: Change in Total UPDRS Score in Study 1 Baseline score Change from baseline to termination score p-value vs.
placeboPlacebo 24.5 3.9 --- Rasagiline 1 mg 24.7 0.1 0.0001 Rasagiline 2 mg 25.9 0.7 0.0001 14.2 Adjunct Use of Rasagiline
Study 2 was a double-blind, randomized, placebo-controlled, parallel group, 18-week study, investigating rasagiline 1 mg as adjunct therapy to dopamine agonists without levodopa. Patients were on a stable dose of dopamine agonist (ropinirole, mean 8 mg/day or pramipexole, mean 1.5 mg/day) therapy for ≥ 30 days, but at doses not sufficient to control Parkinson’s disease symptoms.
In Study 2, 321 patients randomly received placebo (162 patients) or rasagiline 1 mg/day (159 patients) and had a post-baseline assessment. The average Parkinson’s disease duration was approximately 2 years (range 0.1 to 14.5 years).
The primary measure of effectiveness was the change from baseline in the total score of the Unified Parkinson’s Disease Rating Scale (UPDRS) [mentation (Part I) + activities of daily living (ADL) (Part II) + motor function (Part III)].
In Study 2, rasagiline 1 mg was superior to placebo on the primary measure of effectiveness (see Table 5).
Table 5: Change in Total UPDRS Score in Study 2 Baseline score Change from baseline to termination score* p-value vs. placebo Placebo 29.8 -1.2 --- Rasagiline 1 mg 32.1 -3.6 0.012 * A negative change from baseline indicates improvement in the UPDRS
Secondary outcome assessment of the individual subscales of the UPDRS indicates that the UPDRS Part III motor subscale was primarily responsible for the overall rasagiline effect on the UPDRS score (see Table 6).
Table 6: Secondary Measures of Effectiveness in Study 2 Baseline (score) Change from baseline to termination score UPDRS Part II ADL (Activities of Daily Living) subscale score Placebo 7.9 0.4 Rasagiline 1 mg 8.6 -0.3 UPDRS Part III Motor subscale score Placebo 20.4 -1.2 Rasagiline 1 mg 22.2 -3.7 Study 3 and Study 4 were randomized, multinational trials conducted in more advanced Parkinson’s disease patients treated chronically with levodopa and experiencing motor fluctuations (including but not limited to, end of dose “wearing off,” sudden or random “off,” etc.). Study 3 was conducted in North America (U.S. and Canada) and compared rasagiline 0.5 mg and 1 mg daily to placebo. Study 4 was conducted outside of North America in Europe, Argentina, and Israel, and compared rasagiline 1 mg daily to placebo.
Patients had Parkinson’s disease for an average of 9 years (range 5 months to 33 years), had taken levodopa for an average of 8 years (range 5 months to 32 years), and had motor fluctuations for approximately 3 to 4 years (range 1 month to 23 years). Patients kept home Parkinson’s disease diaries just prior to baseline and at specified intervals during the trial. Diaries recorded one of the following four conditions for each half-hour interval over a 24 hour period: “ON” (period of relatively good function and mobility) as either “ON” with no dyskinesia or without troublesome dyskinesia, or “ON” with troublesome dyskinesia, “OFF” (period of relatively poor function and mobility) or asleep. “Troublesome” dyskinesia is defined as dyskinesia that interferes with the patient’s daily activity. All patients had inadequate control of their motor symptoms with motor fluctuations typical of advanced stage disease despite receiving levodopa/decarboxylase inhibitor. The average dose of levodopa taken with a decarboxylase inhibitor was approximately 700 to 800 mg (range 150 to 3000 mg/day). Patients continued their stable doses of additional anti-PD medications at entry into the trials. Approximately 65% of patients in both studies were also taking a dopamine agonist. In the North American study (Study 3), approximately 35% of patients took entacapone with levodopa/decarboxylase inhibitor. The majority of patients taking entacapone were also taking a dopamine agonist.
In Study 3 and Study 4, the primary measure of effectiveness was the change in the mean number of hours spent in the “OFF” state at baseline compared to the mean number of hours spent in the “OFF” state during the treatment period.
In Study 3, patients were randomly assigned to receive placebo (159 patients), rasagiline 0.5 mg/day (164 patients), or rasagiline 1 mg/day (149 patients) for 26 weeks. Patients averaged 6 hours daily in the “OFF” state at baseline as confirmed by home diaries.
In Study 4, patients were randomly assigned to receive placebo (229 patients), rasagiline 1 mg/day (231 patients) or a COMT inhibitor (active comparator), taken along with scheduled doses of levodopa/decarboxylase inhibitor (227 patients) for 18 weeks. Patients averaged 5.6 hours daily in the “OFF” state at baseline as confirmed by home diaries.
In Study 3 and Study 4, rasagiline 1 mg once daily reduced “OFF” time compared to placebo when added to levodopa in patients experiencing motor fluctuations (Tables 7 and 8). The lower dose (0.5 mg) of rasagiline also significantly reduced “OFF” time (Table 7), but had a numerically smaller effect than the 1 mg dose of rasagiline. In Study 4, the active comparator also reduced “OFF” time when compared to placebo.
Table 7: Change in mean total daily "OFF" time in Study 3 Baseline (hours) Change from baseline to treatment period (hours) p-value vs. placebo Placebo 6 -0.9 --- Rasagiline 0.5 mg 6 -1.4 0.0199 Rasagiline 1 mg 6.3 -1.9 <0.0001 Table 8: Change in mean total daily "OFF" time in Study 4 Baseline (hours) Change from baseline to treatment period (hours) p-value vs. placebo Placebo 5.5 -0.4 --- Rasagiline 1 mg 5.6 -1.2 0.0001 In Study 3 and Study 4, dose reduction of levodopa was allowed within the first 6 weeks, if dopaminergic side effects developed including dyskinesia or hallucinations. In Study 3, the levodopa dose was reduced in 8% of patients in the placebo group and in 16% and 17% of patients in the 0.5 mg/day and 1 mg/day rasagiline groups, respectively. When levodopa was reduced, the dose was reduced by 7%, 9%, and 13% in the placebo, 0.5 mg/day, and 1 mg/day groups, respectively. In Study 4, levodopa dose reduction occurred in 6% of patients in the placebo group and in 9% in the rasagiline 1 mg/day groups, respectively. When levodopa was reduced, it was reduced by 13% and 11% in the placebo and the rasagiline groups, respectively.
There were no differences in effectiveness based on age or gender between rasagiline 1 mg per day and placebo.
Several secondary outcome assessments in the two studies showed statistically significant improvements with rasagiline. These included effects on the activities of daily living (ADL) subscale of the UPDRS performed during an “OFF” period and the motor subscale of the UPDRS performed during an “ON” period. In both scales, a negative response represents improvement. Tables 9 and 10 show these results for Studies 3 and 4.
Table 9: Secondary Measures of Effectiveness in Study 3 Baseline (score) Change from baseline to last value UPDRS ADL (Activities of Daily Living) subscale score while "OFF" Placebo 15.5 0.68 Rasagiline 0.5 mg 15.8 -0.6 Rasagiline 1 mg 15.5 -0.68 UPDRS Motor subscale score while "ON" Placebo 20.8 1.21 Rasagiline 0.5 mg 21.5 -1.43 Rasagiline 1 mg 20.9 -1.30 Table 10: Secondary Measures of Effectiveness in Study 4 Baseline (score) Change from baseline to last value UPDRS ADL (Activities of Daily Living) subscale score while "OFF" Placebo 18.7 -0.89 Rasagiline 1 mg 19 -2.61 UPDRS Motor subscale score while "ON" Placebo 23.5 -0.82 Rasagiline 1 mg 23.8 -3.87 -
16 HOW SUPPLIED/STORAGE AND HANDLING
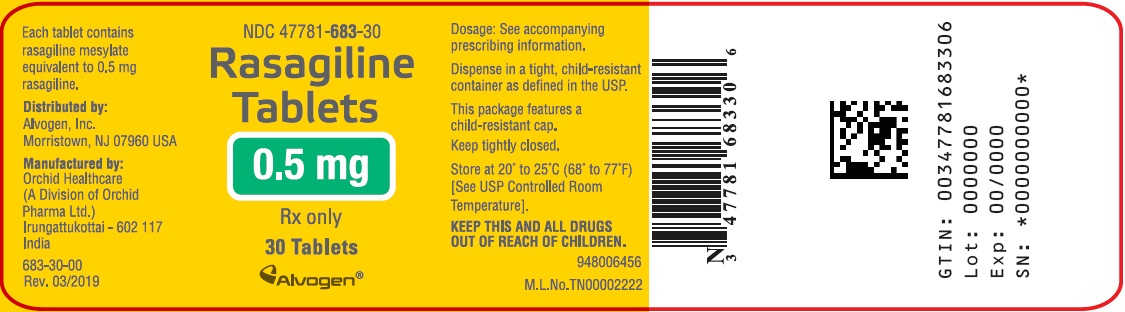
Rasagiline Tablets 0.5 mg:
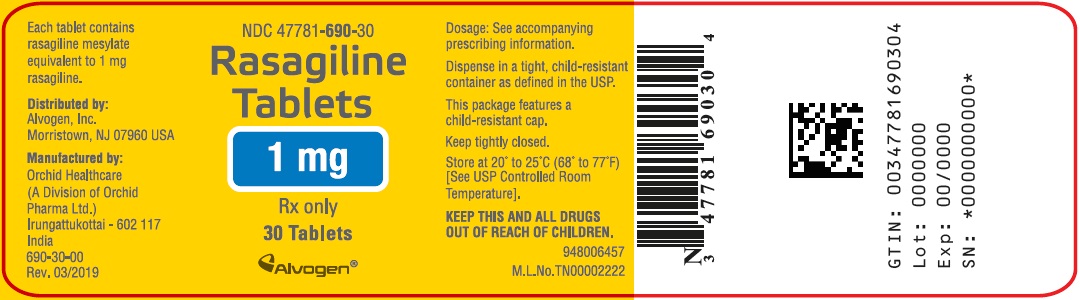
White to off-white, round, flat, beveled tablets, debossed with “R1” on one side and plain on the other side. Supplied as bottles of 30 tablets (NDC: 47781-683-30)Rasagiline Tablets 1 mg:
White to off-white, round, flat, beveled tablets, debossed with “R2” on one side and plain on the other side. Supplied as bottles of 30 tablets (NDC: 47781-690-30)Storage:
Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature]. -
17 PATIENT COUNSELING INFORMATION
Hypertension
Advise patients that treatment with recommended doses of rasagiline tablets may be associated with elevations of blood pressure. Tell patients who experience elevation of blood pressure while taking rasagiline tablets to contact their healthcare provider.The risk of using higher than recommended daily doses of rasagiline tablets should be explained, and a brief description of the tyramine associated hypertensive reaction provided.
Advise patients to avoid certain foods (e.g., aged cheese) containing a very large amount of tyramine while taking recommended doses of rasagiline tablets because of the potential for large increases in blood pressure. If patients eat foods very rich in tyramine and do not feel well soon after eating, they should contact their healthcare provider [see Warnings and Precautions (5.1)].
Serotonin Syndrome
Tell patients to inform their physician if they are taking, or planning to take, any prescription or over-the-counter drugs, especially antidepressants and over-the-counter cold medications, since there is a potential for interaction with rasagiline tablets. Because patients should not use meperidine or certain other analgesics with rasagiline tablets, they should contact their healthcare provider before taking analgesics [see Contraindications (4) and Warnings and Precautions (5.2)].Falling Asleep During Activities of Daily Living and Somnolence
Advise and alert patients about the potential for sedating effects associated with rasagiline tablets and other dopaminergic medications, including somnolence and particularly to the possibility of falling asleep while engaged in activities of daily living. Because somnolence can be a frequent adverse reaction with potentially serious consequences, patients should neither drive a car nor engage in other potentially dangerous activities until they have gained sufficient experience with rasagiline tablets and other dopaminergic medications to gauge whether or not it affects their mental and/or motor performance adversely. Advise patients that if increased somnolence or new episodes of falling asleep during activities of daily living (e.g., watching television, passenger in a car, etc.) are experienced at any time during treatment, they should not drive or participate in potentially dangerous activities until they have contacted their physician. Patients should not drive, operate machinery, or work at heights during treatment if they have previously experienced somnolence and/or have fallen asleep without warning prior to use of rasagiline tablets.Because of possible additive effects, advise patients to exercise caution when patients are taking other sedating medications, alcohol, or other central nervous system depressants (e.g., benzodiazepines, antipsychotics, antidepressants) in combination with rasagiline tablets or when taking concomitant medications that increase plasma levels of rasagiline (e.g., ciprofloxacin) [see Warnings and Precautions (5.3)].
Ciprofloxacin or Other CYP1A2 Inhibitors
Inform patients that they should contact their healthcare provider of rasagiline tablets if they take ciprofloxacin or a similar drug that could increase blood levels of rasagiline because of the need to adjust the dose of rasagiline tablets [see Dosage and Administration (2.2) and Warnings and Precautions (5.4)].Hepatic Impairment
Tell patients who have hepatic problems to contact their healthcare provider regarding possible changes in rasagiline tablets dosing [see Warnings and Precautions (5.5)].Hypotension / Orthostatic Hypotension
Patients should be advised that they may develop orthostatic hypotension with or without symptoms such as dizziness, nausea, syncope, and sometimes sweating. Hypotension and/or orthostatic symptoms may occur more frequently during initial therapy or with an increase in dose at any time (cases have been seen after weeks of treatment). Accordingly, patients should be cautioned against standing up rapidly after sitting or lying down, especially if they have been doing so for prolonged periods, and especially, at the initiation of treatment with rasagiline tablets [see Warnings and Precautions (5.6)].Dyskinesia
Advise patients taking rasagiline tablets as adjunct to levodopa that there is a possibility of dyskinesia or increased dyskinesia [see Warnings and Precautions (5.7)].Hallucinations / Psychotic-Like Behavior
Inform patients that hallucinations or other manifestations of psychotic-like behavior can occur when taking rasagiline tablets. Advise patients that, if they have a major psychotic disorder, that rasagiline tablets should not ordinarily be used because of the risk of exacerbating the psychosis. Patients with a major psychotic disorder should also be aware that many treatments for psychosis may decrease the effectiveness of rasagiline tablets [see Warnings and Precautions (5.8)].Impulse Control/Compulsive Behaviors
Advise patients that they may experience intense urges to gamble, increased sexual urges, other intense urges, and the inability to control these urges while taking one or more of the medications that increase central dopaminergic tone and that are generally used for the treatment of Parkinson’s disease (including rasagiline tablets). Although it is not proven that the medications caused these events, these urges were reported to have stopped in some cases when the dose was reduced or the medication was stopped. Prescribers should ask patients about the development of new or increased gambling urges, sexual urges, or other urges while being treated with rasagiline tablets. Patients should inform their physician if they experience new or increased gambling urges, increased sexual urges, or other intense urges while taking rasagiline tablets. Physicians should consider dose reduction or stopping the medication if a patient develops such urges while taking rasagiline tablets [see Warnings and Precautions (5.9)].Withdrawal-Emergent Hyperpyrexia and Confusion
Tell patients to contact their healthcare provider if they wish to discontinue rasagiline tablets [see Warnings and Precautions (5.10)].Missing Dose
Instruct patients to take rasagiline tablets as prescribed. If a dose is missed, the patient should not double-up the dose of rasagiline tablets. The next dose should be taken at the usual time on the following day.Pregnancy
Advise patients to notify their healthcare provider if they are pregnant or plan to become pregnant [see Use in Specific Populations (8.1)].Trademarks are the property of their respective owners.
Distributed by :Alvogen, Inc.
Morristown, NJ 07960 USAManufactured by : Orchid Healthcare
(A Division of Orchid Pharma Ltd.)
Irungattukottai - 602 117, India948026683
PI683-00
Rev. 3/2019 - PRINCIPAL DISPLAY PANEL
- PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
RASAGILINE
rasagiline tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 47781-683 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength Rasagiline Mesylate (UNII: LH8C2JI290) (Rasagiline - UNII:003N66TS6T) Rasagiline 0.5 mg Inactive Ingredients Ingredient Name Strength LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) STARCH, CORN (UNII: O8232NY3SJ) TALC (UNII: 7SEV7J4R1U) STEARIC ACID (UNII: 4ELV7Z65AP) CITRIC ACID MONOHYDRATE (UNII: 2968PHW8QP) Product Characteristics Color white (white to off-white) Score no score Shape ROUND (flat, beveled) Size 7mm Flavor Imprint Code R1 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 47781-683-30 30 in 1 BOTTLE, PLASTIC; Type 0: Not a Combination Product 03/01/2019 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA201970 03/01/2019 RASAGILINE
rasagiline tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 47781-690 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength Rasagiline Mesylate (UNII: LH8C2JI290) (Rasagiline - UNII:003N66TS6T) Rasagiline 1 mg Inactive Ingredients Ingredient Name Strength LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) STARCH, CORN (UNII: O8232NY3SJ) TALC (UNII: 7SEV7J4R1U) STEARIC ACID (UNII: 4ELV7Z65AP) CITRIC ACID MONOHYDRATE (UNII: 2968PHW8QP) Product Characteristics Color white (white to off-white) Score no score Shape ROUND (flat, beveled) Size 8mm Flavor Imprint Code R2 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 47781-690-30 30 in 1 BOTTLE, PLASTIC; Type 0: Not a Combination Product 03/01/2019 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA201970 03/01/2019 Labeler - Alvogen, Inc. (008057330)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.