These highlights do not include all the information needed to use PREGABALIN EXTENDED-RELEASE TABLETS safely and effectively. See full prescribing information for PREGABALIN EXTENDED-RELEASE TABLETS. PREGABALIN extended-release tablets, for oral use, CV Initial U.S. Approval: 2004
Pregabalin Extended Release by
Drug Labeling and Warnings
Pregabalin Extended Release by is a Prescription medication manufactured, distributed, or labeled by Alvogen Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
PREGABALIN EXTENDED RELEASE- pregabalin tablet, film coated, extended release
Alvogen Inc.
----------
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use PREGABALIN EXTENDED-RELEASE TABLETS safely and effectively. See full prescribing information for PREGABALIN EXTENDED-RELEASE TABLETS.
PREGABALIN extended-release tablets, for oral use, CV Initial U.S. Approval: 2004 INDICATIONS AND USAGEPregabalin extended-release tablets are indicated for the management of:
Efficacy of pregabalin extended-release tablets has not been established for the management of fibromyalgia or as adjunctive therapy for adult patients with partial onset seizures. DOSAGE AND ADMINISTRATION
DOSAGE FORMS AND STRENGTHSExtended-release tablets: 82.5 mg, 165 mg, and 330 mg. (3) CONTRAINDICATIONSKnown hypersensitivity to pregabalin or any of its components. (4) WARNINGS AND PRECAUTIONS
ADVERSE REACTIONSMost common adverse reactions reported in greater than or equal to 4% of patients treated with pregabalin extended-release tablets are dizziness, somnolence, headache, fatigue, peripheral edema, nausea, blurred vision, dry mouth, and weight gain. (6.1) To report SUSPECTED ADVERSE REACTIONS, contact Alvogen, Inc. at 1-866-770-3024 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide. Revised: 8/2024 |
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
Pregabalin extended-release tablets are indicated for the management of:
- Neuropathic pain associated with diabetic peripheral neuropathy
- Postherpetic neuralgia
Efficacy of pregabalin extended-release tablets has not been established for the management of fibromyalgia or as adjunctive therapy for adult patients with partial onset seizures.
2 DOSAGE AND ADMINISTRATION
2.1 Important Dosage and Administration Instructions
Pregabalin extended-release tablets should be administered once daily after an evening meal.
Pregabalin extended-release tablets should be swallowed whole and should not be split, crushed, or chewed.
When discontinuing pregabalin extended-release tablets, taper gradually over a minimum of 1 week.
Instruct patients that if they miss taking their dose of pregabalin extended-release tablets after an evening meal, then they should take their usual dose of pregabalin extended-release tablets prior to bedtime following a snack. If they miss taking the dose of pregabalin extended-release tablets prior to bedtime, then they should take their usual dose of pregabalin extended-release tablets following a morning meal. If they miss taking the dose of pregabalin extended-release tablets following the morning meal, then they should take their usual dose of pregabalin extended-release tablets at the usual time that evening following an evening meal [see Patient Counseling Information (17)].
2.2 Neuropathic Pain Associated with Diabetic Peripheral Neuropathy
Begin dosing at 165 mg once daily and increase to 330 mg once daily within 1 week based on individual patient response and tolerability. The maximum recommended dose of pregabalin extended-release tablets is 330 mg once daily.
Although pregabalin was studied at 600 mg/day, there was no evidence that this dose conferred additional significant benefit and this dose was less well tolerated. In view of the dose-dependent adverse reactions with pregabalin, treatment with doses above 330 mg/day is not recommended for pregabalin extended-release tablets.
2.3 Postherpetic Neuralgia
Begin dosing at 165 mg once daily and increase to 330 mg once daily within 1 week based on individual patient response and tolerability.
Patients who do not experience sufficient pain relief following 2 to 4 weeks of treatment with 330 mg once daily and who are able to tolerate pregabalin extended-release tablets, may be treated with up to 660 mg once daily. In view of the dose-dependent adverse reactions and the higher rate of treatment discontinuation due to adverse reactions, dosing above 330 mg/day should be reserved only for those patients who have on-going pain and are tolerating 330 mg daily. The maximum recommended dose of pregabalin extended-release tablets is 660 mg once daily.
2.4 Conversion from Pregabalin Capsules or Oral Solution to Pregabalin Extended-Release Tablets
When switching from pregabalin to pregabalin extended-release tablets on the day of the switch, instruct patients to take their morning dose of pregabalin as prescribed and initiate pregabalin extended-release tablets therapy after an evening meal.
| Pregabalin Total Daily Dose (dosed 2 or 3 times daily) | Pregabalin Extended-Release Tablets Dose (dosed once a day) |
|---|---|
|
|
|
| 75 mg/daily | 82.5 mg/day |
| 150 mg/daily | 165 mg/day |
| 225 mg/daily | 247.5 mg/day* |
| 300 mg/daily | 330 mg/day |
| 450 mg/daily | 495 mg/day† |
| 600 mg/daily | 660 mg/day‡ |
2.5 Patients with Renal Impairment
Use of pregabalin extended-release tablets is not recommended for patients with creatinine clearance (CLcr) less than 30 mL/min or who are undergoing hemodialysis. Those patients should receive pregabalin.
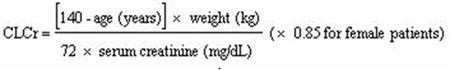
In view of dose-dependent adverse reactions and because pregabalin is eliminated primarily by renal excretion, adjust the dose in patients with reduced renal function. Base the dose adjustment in patients with renal impairment on CLcr, as indicated in Table 2. To use the dosing tables, an estimate of the patient's CLcr in mL/min is needed. CLcr in mL/min may be estimated from serum creatinine (mg/dL) determination using the Cockcroft and Gault equation:
Next, refer to the Dosage and Administration section to determine the recommended total daily dose based on indication, for a patient with normal renal function (CLcr greater than or equal to 60 mL/min). Then refer to Table 2 to determine the corresponding renal adjusted dose.
(For example: A patient initiating pregabalin extended-release tablets therapy for postherpetic neuralgia with normal renal function [CLcr greater than or equal to 60 mL/min], receives a single daily dose of 165 mg/day pregabalin. Therefore, a renal impaired patient with a CLcr of 50 mL/min would receive a single daily dose of 82.5 mg.)
| Creatinine Clearance (CLcr) (mL/min) | Total Pregabalin Extended-Release Tablets Daily Dose (mg/day) | Dose Regimen | |||
|---|---|---|---|---|---|
|
|
|||||
| greater than or equal to 60 | 165 | 330 | 495* | 660† | Once a day |
| 30–60 | 82.5 | 165 | 247.5‡ | 330 | Once a day |
| less than 30/hemodialysis | Dose with Pregabalin | ||||
3 DOSAGE FORMS AND STRENGTHS
Extended-release tablets: 82.5 mg, 165 mg, and 330 mg [see Description (11) and How Supplied/Storage and Handling (16)].
| Pregabalin Extended-Release Tablets | |
|---|---|
| Tablet Strength (mg) | Tablet Description |
| 82.5 mg | White, oval-shaped, film-coated tablets, “ALV 379” imprinted in black ink on one side, blank on the other side. |
| 165 mg | Yellow, oval-shaped, film-coated tablets, “ALV 380” imprinted in black ink on one side, blank on the other side. |
| 330 mg | Pink, oval-shaped, film-coated tablets, “ALV 381” imprinted in black ink on one side, blank on the other side. |
4 CONTRAINDICATIONS
Pregabalin extended-release tablets are contraindicated in patients with known hypersensitivity to pregabalin or any of its components. Angioedema and hypersensitivity reactions have occurred in patients receiving pregabalin therapy [see Warnings and Precautions (5.1, 5.2), Adverse Reactions (6)].
5 WARNINGS AND PRECAUTIONS
5.1 Angioedema
There have been postmarketing reports of angioedema in patients during initial and chronic treatment with pregabalin. Specific symptoms included swelling of the face, mouth (tongue, lips, and gums), and neck (throat and larynx). There were reports of life-threatening angioedema with respiratory compromise requiring emergency treatment. Discontinue pregabalin extended-release tablets immediately in patients with these symptoms.
Exercise caution when prescribing pregabalin extended-release tablets to patients who have had a previous episode of angioedema. In addition, patients who are taking other drugs associated with angioedema (e.g., angiotensin converting enzyme inhibitors [ACE-inhibitors]) may be at increased risk of developing angioedema.
5.2 Hypersensitivity Reactions
There have been postmarketing reports of hypersensitivity reactions in patients shortly after initiation of treatment with pregabalin. Adverse reactions included skin redness, blisters, hives, rash, dyspnea, and wheezing. Discontinue pregabalin extended-release tablets immediately in patients with these symptoms.
5.3 Suicidal Behavior and Ideation
Antiepileptic drugs (AEDs), including pregabalin, the active ingredient in pregabalin extended-release tablets, increase the risk of suicidal thoughts or behavior in patients taking these drugs for any indication. Monitor patients treated with any AED for any indication for the emergence or worsening of depression, suicidal thoughts or behavior, and/or any unusual changes in mood or behavior.
Pooled analyses of 199 placebo-controlled clinical trials (mono- and adjunctive therapy) of 11 different AEDs showed that patients randomized to one of the AEDs had approximately twice the risk (adjusted Relative Risk 1.8, 95% CI:1.2, 2.7) of suicidal thinking or behavior compared to patients randomized to placebo. In these trials, which had a median treatment duration of 12 weeks, the estimated incidence rate of suicidal behavior or ideation among 27,863 AED-treated patients was 0.43%, compared to 0.24% among 16,029 placebo-treated patients, representing an increase of approximately one case of suicidal thinking or behavior for every 530 patients treated. There were four suicides in drug-treated patients in the trials and none in placebo-treated patients, but the number is too small to allow any conclusion about drug effect on suicide.
The increased risk of suicidal thoughts or behavior with AEDs was observed as early as one week after starting drug treatment with AEDs and persisted for the duration of treatment assessed. Because most trials included in the analysis did not extend beyond 24 weeks, the risk of suicidal thoughts or behavior beyond 24 weeks could not be assessed.
The risk of suicidal thoughts or behavior was generally consistent among drugs in the data analyzed. The finding of increased risk with AEDs of varying mechanisms of action and across a range of indications suggests that the risk applies to all AEDs used for any indication. The risk did not vary substantially by age (5 to 100 years) in the clinical trials analyzed.
Table 3 shows absolute and relative risk by indication for all evaluated AEDs.
| Indication | Placebo Patients With Events per 1000 Patients | Drug Patients With Events per 1000 Patients | Relative Risk: Incidence of Events in Drug Patients/Incidence in Placebo Patients | Risk Difference: Additional Drug Patients With Events per 1000 Patients |
|---|---|---|---|---|
| Epilepsy | 1.0 | 3.4 | 3.5 | 2.4 |
| Psychiatric | 5.7 | 8.5 | 1.5 | 2.9 |
| Other | 1.0 | 1.8 | 1.9 | 0.9 |
| Total | 2.4 | 4.3 | 1.8 | 1.9 |
The relative risk for suicidal thoughts or behavior was higher in clinical trials for epilepsy than in clinical trials for psychiatric or other conditions, but the absolute risk differences were similar for the epilepsy and psychiatric indications.
Anyone considering prescribing pregabalin extended-release tablets must balance the risk of suicidal thoughts or behavior with the risk of untreated illness. Many other illnesses for which AEDs are prescribed are themselves associated with morbidity and mortality and an increased risk of suicidal thoughts and behavior. Should suicidal thoughts and behavior emerge during treatment, the prescriber needs to consider whether the emergence of these symptoms in any given patient may be related to the illness being treated.
Inform patients, their caregivers, and families that pregabalin extended-release tablets can increase the risk of suicidal thoughts and behavior and advise them of the need to be alert for the emergence or worsening of the signs and symptoms of depression, any unusual changes in mood or behavior, or the emergence of suicidal thoughts, behavior, or thoughts about self-harm. Report behaviors of concern immediately to healthcare providers.
5.4 Respiratory Depression
There is evidence from case reports, human studies, and animal studies associating pregabalin with serious, life-threatening, or fatal respiratory depression when co-administered with central nervous system (CNS) depressants, including opioids, or in the setting of underlying respiratory impairment. When the decision is made to co-prescribe pregabalin extended-release tablets with another CNS depressant, particularly an opioid, or to prescribe pregabalin extended-release tablets to patients with underlying respiratory impairment, monitor patients for symptoms of respiratory depression and sedation, and consider initiating pregabalin extended-release tablets at a low dose. The management of respiratory depression may include close observation, supportive measures, and reduction or withdrawal of CNS depressants (including pregabalin extended-release tablets).
There is more limited evidence from case reports, animal studies, and human studies associating pregabalin with serious respiratory depression, without co-administered CNS depressants or without underlying respiratory impairment.
5.5 Dizziness and Somnolence
Pregabalin extended-release tablets may cause dizziness and somnolence. Inform patients that Pregabalin extended-release tablets-related dizziness and somnolence may impair their ability to perform tasks such as driving or operating machinery. Concomitant use of pregabalin extended-release tablets with other central nervous system (CNS) depressants may exacerbate these effects [see Drug Interactions (7)].
In the pregabalin extended-release tablets controlled trials for pain indications, dizziness was experienced by 24% of pregabalin extended-release tablets-treated patients during the single-blind phase; somnolence was experienced by 15.8% of pregabalin extended-release tablets-treated patients. Dizziness and somnolence generally began shortly after the initiation of pregabalin extended-release tablets therapy and occurred more frequently at higher doses. Dizziness and somnolence were the adverse reactions most frequently leading to withdrawal (2.4%, 1.2% each) during the single-blind phase of the controlled studies. In pregabalin-treated patients reporting these adverse reactions in short-term, controlled studies, dizziness persisted until the last dose in 30% and somnolence persisted until the last dose in 42% of patients.
5.6 Risks Associated with Abrupt or Rapid Discontinuation
Following abrupt or rapid discontinuation of pregabalin extended-release tablets, some patients reported symptoms including, insomnia, nausea, headache, anxiety, and diarrhea. Increased seizure frequency may occur in patients with seizure disorders taking pregabalin extended-release tablets for pain if pregabalin extended-release tablets are rapidly discontinued. Taper pregabalin extended-release tablets gradually over a minimum of 1 week rather than discontinuing the drug abruptly. The efficacy of pregabalin extended-release tablets as adjunctive therapy for adult patients with partial onset seizures has not been established.
5.7 Peripheral Edema
Pregabalin extended-release tablets treatment may cause peripheral edema. In short-term trials of patients without clinically significant heart or peripheral vascular disease, there was no apparent association between peripheral edema and cardiovascular complications such as hypertension or congestive heart failure. Peripheral edema was not associated with laboratory changes suggestive of deterioration in renal or hepatic function.
In controlled clinical trials for pain indications, the incidence of peripheral edema for patients receiving pregabalin extended-release tablets in the single-blind phase was 5.3% of patients. In controlled clinical trials for pain indications, 0.8% of pregabalin extended-release tablets patients withdrew due to peripheral edema during the single-blind phase.
Higher frequencies of weight gain and peripheral edema were observed in patients taking both pregabalin and a thiazolidinedione antidiabetic agent compared to patients taking either drug alone. The majority of patients using thiazolidinedione antidiabetic agents in the overall safety database were participants in studies of pain associated with diabetic peripheral neuropathy. In this population, peripheral edema was reported in 3% (2/60) of patients who were using thiazolidinedione antidiabetic agents only, 8% (69/859) of patients who were treated with pregabalin only, and 19% (23/120) of patients who were on both pregabalin and thiazolidinedione antidiabetic agents. Similarly, weight gain was reported in 0% (0/60) of patients on thiazolidinediones only; 4% (35/859) of patients on pregabalin only; and 7.5% (9/120) of patients on both drugs.
As the thiazolidinedione class of antidiabetic drugs can cause weight gain and/or fluid retention, possibly exacerbating or leading to heart failure, monitor patients for the development of edema when co-administering pregabalin extended-release tablets and these agents.
Because there are limited data on congestive heart failure patients with New York Heart Association (NYHA) Class III or IV cardiac status, monitor these patients for possible exacerbation of congestive heart failure symptoms when using pregabalin extended-release tablets.
5.8 Weight Gain
Pregabalin extended-release tablets treatment may cause weight gain. In pregabalin extended-release tablets controlled trials for pain indications, weight gain was experienced by 4% of pregabalin extended-release tablets- treated patients during the single-blind phase. Adverse events of weight gain were observed in 3.7% of pregabalin extended-release tablets-treated patients and 1% of placebo-treated patients during the double-blind phase.
In pregabalin controlled clinical trials of up to 14 weeks a gain of 7% or more over baseline weight was observed in 9% of pregabalin-treated patients and 2% of placebo-treated patients. Few patients treated with pregabalin (0.3%) withdrew from controlled trials due to weight gain. In studies with pregabalin, associated weight gain was related to pregabalin dose and duration of exposure but did not appear to be associated with baseline BMI, gender, or age. Weight gain was not limited to patients with edema [see Warnings and Precautions (5.7)].
Although weight gain was not associated with clinically important changes in blood pressure in short-term controlled studies with pregabalin, the long-term cardiovascular effects of pregabalin-associated weight gain are unknown.
Among diabetic patients, pregabalin-treated patients gained an average of 1.6 kg (range: -16 to 16 kg), compared to an average 0.3 kg (range: -10 to 9 kg) weight gain in placebo patients. In a cohort of 333 diabetic patients who received pregabalin for at least 2 years, the average weight gain was 5.2 kg.
While the effects of pregabalin-associated weight gain on glycemic control have not been systematically assessed, in controlled and longer-term open-label clinical trials with diabetic patients, pregabalin treatment did not appear to be associated with loss of glycemic control (as measured by HbA1C).
5.9 Tumorigenic Potential
In standard preclinical in vivo lifetime carcinogenicity studies of pregabalin, an unexpectedly high incidence of hemangiosarcoma was identified in 2 different strains of mice [see Nonclinical Toxicology (13.1)]. The clinical significance of this finding is unknown. Clinical experience during premarketing development of pregabalin provides no direct means to assess its potential for inducing tumors in humans.
In clinical studies across various patient populations, comprising 6,396 patient-years of exposure in patients greater than 12 years of age, new or worsening-preexisting tumors were reported in 57 patients. Without knowledge of the background incidence and recurrence in similar populations not treated with pregabalin, it is impossible to know whether the incidence seen in these cohorts is or is not affected by treatment.
5.10 Ophthalmological Effects
In controlled studies for pain indications, 4.8% of patients treated with pregabalin extended-release tablets in the single-blind phase reported blurred vision, which resolved in a majority of cases with continued dosing. Less than 1% of patients discontinued pregabalin extended-release tablets treatment due to vision-related events (primarily blurred vision). Additionally, 0.7% of pregabalin extended-release tablets-treated patients as compared to no placebo-treated patients experienced blurred vision in the double-blind phase.
Prospectively planned ophthalmologic testing during the premarketing development of pregabalin, including visual acuity testing, formal visual field testing and dilated funduscopic examination, was performed in over 3600 patients. In these patients, visual acuity was reduced in 7% of pregabalin-treated patients and 5% of placebo-treated patients. Visual field changes were detected in 13% of pregabalin-treated and 12% of placebo-treated patients. Funduscopic changes were observed in 2% of pregabalin-treated and 2% of placebo-treated patients.
Although the clinical significance of the ophthalmologic findings is unknown, inform patients to notify their physician if changes in vision occur. If visual disturbance persists, consider further assessment. Consider more frequent assessment for patients who are already routinely monitored for ocular conditions.
5.11 Creatine Kinase Elevations
Pregabalin treatment was associated with creatine kinase elevations. Mean changes in creatine kinase from baseline to the maximum value were 60 U/L for pregabalin-treated patients and 28 U/L for the placebo patients. In all controlled trials across multiple patient populations, 1.5% of patients on pregabalin and 0.7% of placebo patients had a value of creatine kinase at least 3 times the upper limit of normal. Three pregabalin-treated subjects had events reported as rhabdomyolysis in premarketing clinical trials. The relationship between these myopathy events and pregabalin is not completely understood because the cases had documented factors that may have caused or contributed to these events. Instruct patients to promptly report unexplained muscle pain, tenderness, or weakness, particularly if these muscle symptoms are accompanied by malaise or fever. Discontinue treatment with pregabalin extended-release tablets if myopathy is diagnosed or suspected or if markedly elevated creatine kinase levels occur.
5.12 Decreased Platelet Count
Both pregabalin extended-release tablets and pregabalin treatment were associated with a decrease in platelet count. In the double-blind phase of controlled studies for pain indication, pregabalin extended-release tablets-treated patients experienced a median change from baseline in platelet count of 11 × 103/mm3 (for the PHN population) and 14 × 103/mm3 (for the FM population) as compared to 1 × 103/mm3 in placebo-treated patients (for both populations). Pregabalin-treated patients experienced a mean maximal decrease in platelet count of 20 × 103/µL, compared to 11 × 103/µL in placebo patients. In the overall database of controlled trials, 2% of placebo patients and 3% of pregabalin patients experienced a potentially clinically significant decrease in platelets, defined as 20% below baseline value and less than 150 × 103/µL. A single pregabalin-treated subject developed severe thrombocytopenia with a platelet count less than 20 × 103/µL. In randomized controlled trials, pregabalin or pregabalin extended-release tablets were not associated with an increase in bleeding-related adverse reactions.
5.13 PR Interval Prolongation
Pregabalin treatment was associated with PR interval prolongation. In analyses of clinical trial ECG data, the mean PR interval increase was 3 to 6 msec at pregabalin doses greater than or equal to 300 mg/day. This mean change difference was not associated with an increased risk of PR increase greater than or equal to 25% from baseline, an increased percentage of subjects with on-treatment PR greater than 200 msec, or an increased risk of adverse reactions of second or third degree AV block.
Subgroup analyses did not identify an increased risk of PR prolongation in patients with baseline PR prolongation or in patients taking other PR prolonging medications. However, these analyses cannot be considered definitive because of the limited number of patients in these categories.
6 ADVERSE REACTIONS
The following adverse reactions are described elsewhere in the labeling:
- Angioedema [see Warnings and Precautions (5.1)]
- Hypersensitivity Reactions [see Warnings and Precautions (5.2)]
- Suicidal Behavior and Ideation [see Warnings and Precautions (5.3)]
- Respiratory Depression [see Warnings and Precautions (5.4)]
- Dizziness and Somnolence [see Warnings and Precautions (5.5)]
- Risks Associated with Abrupt or Rapid Discontinuation [see Warnings and Precautions (5.6)]
- Peripheral Edema [see Warnings and Precautions (5.7)]
- Weight Gain [see Warnings and Precautions (5.8)]
- Ophthalmological Effects [see Warnings and Precautions (5.10)]
- Creatine Kinase Elevations [see Warnings and Precautions (5.11)]
- Decreased Platelet Count [see Warnings and Precautions (5.12)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Two randomized placebo-controlled clinical trials were conducted in patients with postherpetic neuralgia and fibromyalgia in which a total of 1,242 patients received pregabalin extended-release tablets. Both studies were randomized withdrawal design where a 6-week single-blind, dose optimization phase was followed by a 13-week double-blind phase. The most common adverse events leading to discontinuation from the single-blind phase of the study occurring in greater than or equal to 0.3% of patients were dizziness, somnolence, peripheral edema, fatigue, blurred vision, and increased weight. Sixty-four percent of patients experienced adverse events during the single-blind phase, with the most common adverse events occurring in greater than or equal to 4% of patients being dizziness, somnolence, headache, fatigue, peripheral edema, nausea, blurred vision, dry mouth, and weight gain.
Controlled Study in Postherpetic Neuralgia
Adverse Reactions Leading to Discontinuation
In a clinical trial in patients with postherpetic neuralgia, 8.9% of patients treated with pregabalin extended-release tablets discontinued prematurely during the single-blind phase due to adverse reactions. The most common reasons for discontinuation due to adverse reactions were dizziness (2.1%), somnolence (0.87%), and peripheral edema (0.50%).
Most Common Adverse Reactions
Table 4 lists all adverse reactions, regardless of causality, occurring in greater than or equal to 1% of patients with postherpetic neuralgia who received pregabalin extended-release tablets, regardless of the phase of the study.
| System Organ Class Preferred Term | Single-Blind Phase | Double-Blind Phase | |
|---|---|---|---|
| Pregabalin Extended-Release Tablets [N=801] n (%) | Pregabalin Extended-Release Tablets [N=208] n (%) | Placebo [N=205] n (%) |
|
|
|
|||
| Ear and labyrinth disorders | |||
| Vertigo | 31 (3.9) | 2 (1.0) | 1 (0.5) |
| Eye disorders | |||
| Vision blurred | 30 (3.7) | 1 (0.5) | 0 |
| Diplopia | 8 (1.0) | 1 (0.5) | 0 |
| Gastrointestinal disorders | |||
| Dry mouth | 30 (3.7) | 1 (0.5) | 0 |
| Nausea | 24 (3.0) | 7 (3.4) | 0 |
| Constipation | 22 (2.7) | 0 | 0 |
| Diarrhea | 11 (1.4) | 2 (1.0) | 1 (0.5) |
| Vomiting | 9 (1.1) | 3 (1.4) | 1 (0.5) |
| General disorders and administration site conditions | |||
| Edema peripheral | 39 (4.9) | 8 (3.8) | 1 (0.5) |
| Fatigue | 31 (3.9) | 3 (1.4) | 2 (1.0) |
| Edema | 3 (0.4) | 3 (1.4) | 0 |
| Infections and infestations | |||
| Nasopharyngitis | 12 (1.5) | 3 (1.4) | 0 |
| Urinary tract infection | 11 (1.4) | 3 (1.4) | 1 (0.5) |
| Bronchitis | 4 (0.5) | 3 (1.4) | 2 (1.0) |
| Respiratory tract infection viral | 3 (0.4) | 3 (1.4) | 1 (0.5) |
| Sinusitis | 3 (0.4) | 2 (1.0) | 0 |
| Gastroenteritis viral | 2 (0.2) | 2 (1.0) | 0 |
| Investigations | |||
| Weight increased | 20 (2.5) | 8 (3.8) | 2 (1.0) |
| Alanine aminotransferase increased | 2 (0.2) | 3 (1.4) | 0 |
| Aspartate aminotransferase increased | 2 (0.2) | 2 (1.0) | 0 |
| Musculoskeletal and connective tissue disorders | |||
| Arthralgia | 6 (0.7) | 2 (1.0) | 1 (0.5) |
| Joint swelling | 0 | 4 (1.9) | 0 |
| Nervous system disorders | |||
| Dizziness | 137 (17.1) | 7 (3.4) | 1 (0.5) |
| Somnolence | 91 (11.4) | 1 (0.5) | 0 |
| Headache | 31 (3.9) | 4 (1.9) | 1 (0.5) |
| Balance disorder | 21 (2.6) | 1 (0.5) | 0 |
| Reproductive system and breast disorders | |||
| Erectile dysfunction | 2 (0.6) | 1 (1.4) | 0 |
| Respiratory, thoracic, and mediastinal disorders | |||
| Cough | 2 (0.2) | 2 (1.0) | 1 (0.5) |
| Skin and subcutaneous tissue disorders | |||
| Dermatitis contact | 0 | 2 (1.0) | 0 |
Other Adverse Reactions Observed During Clinical Studies with Pregabalin and Pregabalin Extended-Release Tablets
In addition to the adverse reactions reported during the controlled studies with pregabalin extended-release tablets in postherpetic neuralgia, the following adverse reactions have been reported in patients treated with pregabalin and pregabalin extended-release tablets during all clinical studies. This listing does not include those adverse reactions already listed above. The adverse reactions are categorized by system organ class and listed in order of decreasing frequency according to the following definitions: frequent adverse reactions are those occurring on 1 or more occasions in at least 1/100 patients; infrequent adverse reactions are those occurring in 1/100 to 1/1000 patients; rare reactions are those occurring in fewer than 1/1000 patients. Adverse reactions of major clinical importance are described in the Warnings and Precautions section (5).
Cardiac Disorders – Infrequent: Palpitations, Deep thrombophlebitis, Heart failure, Hypotension, Postural hypotension, Retinal vascular disorder, Syncope; Rare: Cardiac failure, Tachycardia
Eye Disorders – Infrequent: Periorbital edema
Gastrointestinal Disorders – Frequent: Increased appetite; Infrequent: Abdominal distension, Abdominal pain, Dysphagia, Pancreatitis, Tongue edema
General Disorders – Frequent: Fever; Infrequent: Chest pain, Face edema; Rare: Facial pain, Mucosal dryness
Hemic and Lymphatic System Disorders – Frequent: Ecchymosis; Infrequent: Anemia, Eosinophilia, Hypochromic anemia, Leukocytosis, Leukopenia, Lymphadenopathy, Thrombocytopenia; Rare: Myelofibrosis, Polycythemia, Prothrombin decreased, Purpura, Thrombocythemia
Infections and Infestations – Infrequent: Otitis media, Pneumonia
Investigations – Rare: Glucose urine present, Lipase increased, Neutrophil count increased, Proteinuria
Metabolic and Nutritional Disorders – Rare: Glucose Tolerance Decreased, Urate Crystalluria
Musculoskeletal and Connective Tissue Disorders – Frequent: Leg cramps, Myalgia, Myasthenia; Infrequent: Joint stiffness; Rare: Coccydynia, Myokymia
Nervous System Disorders – Frequent: Anxiety, Depersonalization, Hypertonia, Hypoesthesia, Libido decreased, Nystagmus, Paresthesia, Sedation, Stupor, Twitching; Infrequent: Coordination abnormal, Abnormal dreams, Agitation, Amnesia, Apathy, Aphasia, Circumoral paresthesia, Cognitive disorder, Dysarthria, Dysgeusia, Hallucinations, Hostility, Hyperalgesia, Hyperesthesia, Hyperkinesia, Hypokinesia, Hypotonia, Libido increased, Myoclonus, Neuralgia, Sciatica, Sleep phase rhythm disturbance; Rare: Addiction, Altered state of consciousness, Bradykinesia, Cerebellar syndrome, Cogwheel rigidity, Coma, Delirium, Delusions, Depressed level of consciousness, Dysautonomia, Dyskinesia, Dystonia, Encephalopathy, Extrapyramidal syndrome, Psychomotor hyperactivity, Psychomotor skills impaired
Psychiatric Disorders – Infrequent: Irritability
Respiratory System Disorders – Rare: Lung edema
Skin Disorders – Frequent: Pruritus; Rare: Stevens-Johnson syndrome
Special Senses – Frequent: Conjunctivitis, Tinnitus
Urogenital System Disorders – Frequent: Anorgasmia, Impotence, Urinary frequency, Urinary incontinence; Infrequent: Abnormal ejaculation, Albuminuria, Dysuria, Hematuria, Kidney calculus, Leukorrhea, Nephritis, Oliguria, Urinary retention
6.2 Postmarketing Experience with Pregabalin
The following adverse reactions have been identified during post-approval use of pregabalin. These adverse reactions have not been listed above and data are insufficient to support an estimate of their incidence or to establish causation. The listing is alphabetized: breast enlargement, bullous pemphigoid, gynecomastia.
There are postmarketing reports of life-threatening or fatal respiratory depression in patients taking pregabalin with opioids or other CNS depressants, or in the setting of underlying respiratory impairment.
In addition, there are postmarketing reports of events related to reduced lower gastrointestinal tract function (e.g., intestinal obstruction, paralytic ileus, constipation) when pregabalin was co-administered with medications that have the potential to produce constipation, such as opioid analgesics.
7 DRUG INTERACTIONS
Since pregabalin is predominantly excreted unchanged in the urine, undergoes negligible metabolism in humans (less than 2% of a dose recovered in urine as metabolites), and does not bind to plasma proteins, its pharmacokinetics are unlikely to be affected by other agents through metabolic interactions or protein binding displacement. In vitro studies showed that pregabalin is unlikely to be involved in significant pharmacokinetic drug interactions [see Clinical Pharmacology (12)].
The interactions of pregabalin extended-release tablets with co-administration of other drugs have not been systematically evaluated. Co-administration of the prokinetic drug erythromycin with pregabalin extended-release tablets did not result in any clinically important changes in the pharmacokinetics of pregabalin extended-release tablets [see Clinical Pharmacology (12)].
Additional studies have been performed with pregabalin. No pharmacokinetic interactions were observed between pregabalin and carbamazepine, gabapentin, lamotrigine, oral contraceptive, phenobarbital, phenytoin, topiramate, and valproic acid. A similar lack of pharmacokinetic interactions would be expected to occur with pregabalin extended-release tablets.
Pharmacodynamics
Although no pharmacokinetic interactions were seen with pregabalin and ethanol, lorazepam, or oxycodone, additive effects on cognitive and gross motor functioning were seen when pregabalin was co-administered with these drugs. No clinically important effects on respiration were seen in studies of pregabalin.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to pregabalin during pregnancy. To provide information regarding the effects of in utero exposure to pregabalin extended-release tablets, physicians are advised to recommend that pregnant patients taking pregabalin extended-release tablets enroll in the North American Antiepileptic Drug (NAAED) Pregnancy Registry. This can be done by calling the toll free number 1-888-233-2334, and must be done by patients themselves. Information on the registry can also be found at the website http://www.aedpregnancyregistry.org/.
Risk Summary
Observational studies on the use of pregabalin during pregnancy suggest a possible small increase in the rate of overall major birth defects, but there was no consistent or specific pattern of major birth defects identified (see Data). Available postmarketing data on miscarriage and other maternal, fetal, and long term developmental adverse effects were insufficient to identify risk associated with pregabalin.
In animal reproduction studies, increased incidences of fetal structural abnormalities and other manifestations of developmental toxicity, including skeletal malformations, retarded ossification, and decreased fetal body weight were observed in the offspring of rats and rabbits given pregabalin orally during organogenesis, at doses that produced plasma pregabalin exposures (AUC) greater than or equal to 18 times human exposure at the maximum recommended dose (MRD) of 660 mg/day (see Data). In an animal development study, lethality, growth retardation, and nervous and reproductive system functional impairment were observed in the offspring of rats given pregabalin during gestation and lactation. The no-effect dose for developmental toxicity was approximately twice the human exposure at MRD. The background risk of major birth defects and miscarriage for the indicated populations are unknown. However, the background risk in the U.S. general population of major birth defects is 2% to 4% and of miscarriage is 15% to 20% of clinically recognized pregnancies.
Data
Human Data
One database study, which included over 2,700 pregnancies exposed to pregabalin (monotherapy) during the first trimester compared to 3,063,251 pregnancies unexposed to antiepileptics demonstrated prevalence ratios for major malformations overall of 1.14 (CI 95% 0.96 to 1.35) for pregabalin, 1.29 (CI 95% 1.01 to 1.65) for lamotrigine, 1.39 (CI 95% 1.07 to 1.82) for duloxetine, and 1.24 (CI 95% 1.00 to 1.54) for exposure to either lamotrigine or duloxetine. Important study limitations include uncertainty of whether women who filled a prescription took the medication and inability to adequately control for the underlying disease and other potential confounders.
A published study included results from two separate databases. One database, which included 353 pregnancies exposed to pregabalin (monotherapy) during the first trimester compared to 368,489 pregnancies unexposed to antiepileptics, showed no increase in risk of major birth defects; adjusted relative risk 0.87 (CI 95% 0.53 to 1.42). The second database, which included 118 pregnancies exposed to pregabalin (monotherapy) during the first trimester compared to 380,347 pregnancies unexposed to antiepileptics, suggested a small increase in risk of major birth defects; adjusted relative risk 1.26 (CI 95% 0.64 to 2.49). The risk estimates crossed the null, and the study had limitations similar to the prior study.
Other published epidemiologic studies reported inconsistent findings. No specific pattern of birth defects was identified across studies. All of the studies had limitations due to their retrospective design.
Animal Data
When pregnant rats were given pregabalin (500, 1250, or 2500 mg/kg) orally throughout the period of organogenesis, incidences of specific skull alterations attributed to abnormally advanced ossification (premature fusion of the jugal and nasal sutures) were increased at greater than or equal to 1250 mg/kg, and incidences of skeletal variations and retarded ossification were increased at all doses. Fetal body weights were decreased at the highest dose. The low dose in this study was associated with a plasma exposure (AUC) approximately 18 times human exposure at the MRD of 660 mg/day. A no-effect dose for rat embryo-fetal developmental toxicity was not established.
When pregnant rabbits were given pregabalin (250, 500, or 1250 mg/kg) orally throughout the period of organogenesis, decreased fetal body weight and increased incidences of skeletal malformations, visceral variations, and retarded ossification were observed at the highest dose. The no-effect dose for developmental toxicity in rabbits (500 mg/kg) was associated with a plasma exposure approximately 17 times human exposure at the MRD.
In a study in which female rats were dosed with pregabalin (50, 100, 250, 1250, or 2500 mg/kg) throughout gestation and lactation, offspring growth was reduced at greater than or equal to 100 mg/kg and offspring survival was decreased at greater than or equal to 250 mg/kg. The effect on offspring survival was pronounced at doses greater than or equal to 1250 mg/kg, with 100% mortality in high-dose litters. When offspring were tested as adults, neurobehavioral abnormalities (decreased auditory startle responding) were observed at greater than or equal to 250 mg/kg and reproductive impairment (decreased fertility and litter size) was seen at 1250 mg/kg. The no-effect dose for pre- and postnatal developmental toxicity in rats (50 mg/kg) produced a plasma exposure approximately 2 times human exposure at the MRD.
In the prenatal-postnatal study in rats, pregabalin prolonged gestation and induced dystocia at exposures greater than or equal to 50 times the mean human exposure (AUC (0–24) of 123 μg∙hr/mL) at the MRD.
8.2 Lactation
Risk Summary
Small amounts of pregabalin have been detected in the milk of lactating women. A pharmacokinetic study in lactating women detected pregabalin in breast milk at average steady state concentrations approximately 76% of those in maternal plasma. The estimated average daily infant dose of pregabalin from breast milk (assuming mean milk consumption of 150 mL/kg/day) was 0.31 mg/kg/day, which on a mg/kg basis would be approximately 7% of the maternal dose (see Data). The study did not evaluate the effects of pregabalin on milk production or the effects of pregabalin on the breastfed infant.
Based on animal studies, there is a potential risk of tumorigenicity with pregabalin exposure via breast milk to the breastfed infant [see Nonclinical Toxicology (13.1)]. Available clinical study data in patients greater than 12 years of age do not provide a clear conclusion about the potential risk of tumorigenicity with pregabalin [see Warnings and Precautions (5.9)]. Because of the potential risk of tumorigenicity, breastfeeding is not recommended during treatment with pregabalin extended-release tablets.
Data
A pharmacokinetic study in ten lactating women, who were at least 12 weeks postpartum, evaluated the concentrations of pregabalin in plasma and breast milk. Pregabalin 150 mg oral capsule was given every 12 hours (300 mg daily dose) for a total of 4 doses. Pregabalin was detected in breast milk at average steady-state concentrations approximately 76% of those in maternal plasma. The estimated average daily infant dose of pregabalin from breast milk (assuming mean milk consumption of 150 mL/kg/day) was 0.31 mg/kg/day, which on a mg/kg basis would be approximately 7% of the maternal dose. The study did not evaluate the effects of pregabalin on milk production. Infants did not receive breast milk obtained during the dosing period, therefore, the effects of pregabalin on the breastfed infant were not evaluated.
8.3 Females and Males of Reproductive Potential
Infertility
Males
Effects on Spermatogenesis
In a randomized, double-blind, placebo-controlled non-inferiority study to assess the effect of pregabalin on sperm characteristics, healthy male subjects received pregabalin at a daily dose up to 600 mg (n=111) or placebo (n=109) for 13 weeks (1 complete sperm cycle) followed by a 13-week washout period (off-drug). A total of 65 subjects in the pregabalin group (59%) and 62 subjects in the placebo group (57%) were included in the per protocol (PP) population. These subjects took study drug for at least 8 weeks, had appropriate timing of semen collections and did not have any significant protocol violations. Among these subjects, approximately 9% of the pregabalin group (6/65) vs. 3% in the placebo group (2/62) had greater than or equal to 50% reduction in mean sperm concentrations from baseline at Week 26 (the primary endpoint). The difference between pregabalin and placebo was within the pre-specified non-inferiority margin of 20%. There were no adverse effects of pregabalin on sperm morphology, sperm motility, serum FSH or serum testosterone levels as compared to placebo. In subjects in the PP population with greater than or equal to 50% reduction in sperm concentration from baseline, sperm concentrations were no longer reduced by greater than or equal to 50% in any affected subject after an additional 3 months off-drug. In 1 subject, however, subsequent semen analyses demonstrated reductions from baseline of greater than or equal to 50% at 9 and 12 months off-drug. The clinical relevance of these data is unknown.
In the animal fertility study with pregabalin in male rats, adverse reproductive and developmental effects were observed [see Nonclinical Toxicology (13.1)].
8.4 Pediatric Use
The safety and effectiveness of pregabalin extended-release tablets in pediatric patients have not been established.
Juvenile Animal Toxicity Data
In studies in which pregabalin (50 to 500 mg/kg) was orally administered to young rats from early in the postnatal period (Postnatal Day 7) through sexual maturity, neurobehavioral abnormalities (deficits in learning and memory, altered locomotor activity, decreased auditory startle responding and habituation) and reproductive impairment (delayed sexual maturation and decreased fertility in males and females) were observed at doses greater than or equal to 50 mg/kg. The neurobehavioral changes of acoustic startle persisted at greater than or equal to 250 mg/kg and locomotor activity and water maze performance at greater than or equal to 500 mg/kg in animals tested after cessation of dosing and, thus, were considered to represent long-term effects. The low effect dose for developmental neurotoxicity and reproductive impairment in juvenile rats (50 mg/kg) was associated with a plasma pregabalin exposure (AUC) approximately equal to human exposure at the maximum recommended dose of 660 mg/day. A no-effect dose was not established.
8.5 Geriatric Use
In controlled clinical studies of pregabalin in neuropathic pain associated with diabetic peripheral neuropathy, 246 patients were 65 to 74 years of age, and 73 patients were 75 years of age or older.
In controlled clinical studies of pregabalin in neuropathic pain associated with postherpetic neuralgia, 282 patients were 65 to 74 years of age, and 379 patients were 75 years of age or older.
In the pregabalin extended-release tablets neuropathic pain associated with postherpetic neuralgia study, 422 patients 65 years of age and older received pregabalin.
No overall differences in safety and effectiveness were observed between these patients and younger patients, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
Pregabalin is known to be substantially excreted by the kidney, and the risk of adverse reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function. See Dosage and Administration (2.5) for recommendations for dosing in patients with renal impairment.
9 DRUG ABUSE AND DEPENDENCE
9.1 Controlled Substance
Pregabalin extended-release tablets contains pregabalin, a Schedule V controlled substance.
9.2 Abuse
In a study of recreational users (N=15) of sedative/hypnotic drugs, including alcohol, pregabalin (450 mg, single dose) received subjective ratings of "good drug effect," "high" and "liking" to a degree that was similar to diazepam (30 mg, single dose). In controlled clinical studies in over 5,500 patients, 4% of pregabalin-treated patients and 1% of placebo-treated patients overall reported euphoria as an adverse reaction, though in some patient populations studied, this reporting rate was higher and ranged from 1% to 12%.
Carefully evaluate all patients treated with pregabalin extended-release tablets for history of drug abuse and observe them for signs of pregabalin extended-release tablets misuse or abuse (e.g., development of tolerance, dose escalation, drug-seeking behavior).
9.3 Dependence
In clinical studies, following abrupt or rapid discontinuation of pregabalin extended-release tablets, some patients reported symptoms including insomnia, nausea, headache diarrhea, or anxiety [see Warnings and Precautions (5.6)], consistent with physical dependence. In the postmarketing experience with pregabalin, in addition to these reported symptoms there have also been reported cases of hyperhidrosis.
10 OVERDOSAGE
Signs, Symptoms and Laboratory Findings of Acute Overdosage in Humans
In the postmarketing experience, the most commonly reported adverse events observed with pregabalin when taken in overdose include reduced consciousness, depression/anxiety, confusional state, agitation, and restlessness. Seizures and heart block have also been reported. Deaths have been reported in the setting of lone pregabalin overdose and in combination with other CNS depressants.
Treatment or Management of Overdose
There is no specific antidote for overdose with pregabalin. If indicated, elimination of unabsorbed drug may be attempted by emesis or gastric lavage; observe usual precautions to maintain the airway. General supportive care of the patient is indicated including monitoring of vital signs and observation of the clinical status of the patient. Contact a Certified Poison Control Center for up-to-date information on the management of overdose with pregabalin.
Pregabalin can be removed by hemodialysis. Standard hemodialysis procedures result in significant clearance of pregabalin (approximately 50% in 4 hours).
11 DESCRIPTION
Pregabalin extended-release tablets are for oral use and contain pregabalin. Pregabalin is described chemically as (S)-3-(aminomethyl)-5-methylhexanoic acid. The molecular formula is C8H17NO2 and the molecular weight is 159.23. The chemical structure of pregabalin is:
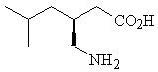
Pregabalin is a white to off-white, crystalline solid with a pKa1 of 4.2 and a pKa2 of 10.6. It is freely soluble in water and both basic and acidic aqueous solutions. The log of the partition coefficient (n-octanol/0.05M phosphate buffer) at pH 7.4 is – 1.35.
Pregabalin extended-release tablets are administered orally and contain 82.5 mg, 165 mg, or 330 mg of pregabalin, along with amino methacrylate copolymer, colloidal silicon dioxide, crospovidone, hydroxypropyl cellulose, hypromellose, and magnesium stearate.
The monogramming ink is comprised of ammonium hydroxide, black iron oxide, isopropyl alcohol, N-butyl alcohol, propylene glycol and shellac glaze.
The 82.5 mg tablets also contain macrogol, polyvinyl alcohol, talc, and titanium dioxide. The 165 mg tablets also contain iron oxide yellow, iron oxide red, macrogol, polyvinyl alcohol, talc, and titanium dioxide. The 330 mg tablets also contain ferrosoferric oxide, iron oxide red, macrogol, polyvinyl alcohol, talc, and titanium dioxide.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Pregabalin binds with high affinity to the alpha2-delta site (an auxiliary subunit of voltage-gated calcium channels) in central nervous system tissues. Although the mechanism of action of pregabalin has not been fully elucidated, results with genetically modified mice and with compounds structurally related to pregabalin (such as gabapentin) suggest that binding to the alpha2-delta subunit may be involved in pregabalin’s anti-nociceptive and antiseizure effects in animals. In animal models of nerve damage, pregabalin has been shown to reduce calcium-dependent release of pro-nociceptive neurotransmitters in the spinal cord, possibly by disrupting alpha2-delta containing-calcium channel trafficking and/or reducing calcium currents. Evidence from other animal models of nerve damage and persistent pain suggest the anti-nociceptive activities of pregabalin may also be mediated through interactions with descending noradrenergic and serotonergic pathways originating from the brainstem that modulate pain transmission in the spinal cord.
While pregabalin is a structural derivative of the inhibitory neurotransmitter gamma-aminobutyric acid (GABA), it does not bind directly to GABAA, GABAB, or benzodiazepine receptors, does not augment GABAA responses in cultured neurons, does not alter rat brain GABA concentration or have acute effects on GABA uptake or degradation. However, in cultured neurons prolonged application of pregabalin increases the density of GABA transporter protein and increases the rate of functional GABA transport. Pregabalin does not block sodium channels, is not active at opiate receptors, and does not alter cyclooxygenase enzyme activity. It is inactive at serotonin and dopamine receptors and does not inhibit dopamine, serotonin, or noradrenaline reuptake.
12.3 Pharmacokinetics
Pregabalin extended-release tablets has linear pharmacokinetics with dose-proportional increases in maximum plasma concentration (Cmax) and area under the plasma concentration-time curve (AUC) from 82.5 to 660 mg/day. Following repeated administration, steady state is achieved within approximately 48 to 72 hours.
Pregabalin extended-release tablets administered once daily following an evening meal has equivalent AUC and lower Cmax relative to a comparative dose of pregabalin administered without food twice daily (Table 5). Variability in Cmax and AUC for pregabalin extended-release tablets is less than or equal to 25%.
| Pregabalin Extended-Release Tablets Once Daily | Pregabalin BID |
|
|---|---|---|
| Note: Geometric mean (%CV) for AUC24, Cmax, Cmin; median (range) for Tmax. Abbreviations: AUC24=area under the curve over 24 hours; BID=every 12 hours; Cmax=peak concentrations; Cmin=minimum concentrations; N=Number of subjects; Tmax=time to peak concentrations. |
||
| N | 24 | 24 |
| Cmax (µg/mL) | 2.0 (17) | 3.2 (21) |
| Tmax (h) | 8.0 (5.0 – 12.0) | 0.7 (0.7 – 1.5) |
| AUC24 (µg∙h/mL) | 29.4 (17) | 31.5 (18) |
| Cmin (µg/mL) | 0.44 (24) | 0.59 (25) |
Absorption
Pregabalin is absorbed from the small intestine and proximal colon. Pregabalin extended-release tablets absorption is linear and dose proportional.
The bioavailability of pregabalin extended-release tablets is reduced if taken on an empty stomach. The AUC is approximately 30% lower when pregabalin extended-release tablets are administered fasted relative to following an evening meal.
When pregabalin extended-release tablets are administered following a 600 to 750 calorie (50% carbohydrates, 20% protein, 30% fat) evening meal, peak plasma concentrations occur within approximately 8 to 10 hours and AUC is approximately 93% to 97% relative to a comparative dose of pregabalin. The rate and extent of pregabalin extended-release tablets absorption is similar when administered following a 400 to 500 calorie, 30% fat or an 800 to 1000 calorie, 15%, 30%, or 50% fat evening meal.
When pregabalin extended-release tablets are administered following an 800 to 1000 calorie (50% carbohydrates, 20% protein, 30% fat) morning meal, peak plasma concentrations occur within approximately 12 hours and AUC is 99% relative to a comparative dose of pregabalin. AUC decreases approximately 13% to 25% when pregabalin extended-release tablets are administered following a 400 to 500 calorie or 600 to 750 calorie (50% carbohydrates, 20% protein, 30% fat) morning meal relative to the 800 to 1000 calorie meal, while Cmax remains the same.
Distribution
Pregabalin does not bind to plasma proteins. The apparent volume of distribution of pregabalin following oral administration is approximately 0.5 L/kg. Pregabalin is a substrate for system L transporter which is responsible for the transport of large amino acids across the blood brain barrier. Although there are no data in humans, pregabalin has been shown to cross the blood brain barrier in mice, rats, and monkeys. In addition, pregabalin has been shown to cross the placenta in rats and is present in the milk of lactating rats.
Elimination
Metabolism
Pregabalin undergoes negligible metabolism in humans. Following a dose of radiolabeled pregabalin, approximately 90% of the administered dose was recovered in the urine as unchanged pregabalin. The N-methylated derivative of pregabalin, the major metabolite of pregabalin found in urine, accounted for 0.9% of the dose. In preclinical studies, pregabalin (S-enantiomer) did not undergo racemization to the R-enantiomer in mice, rats, rabbits, or monkeys.
Excretion
Pregabalin is eliminated from the systemic circulation primarily by renal excretion as unchanged drug with a mean elimination half-life of 6.3 hours in subjects with normal renal function. Mean renal clearance was estimated to be 67.0 to 80.9 mL/min in young healthy subjects. Because pregabalin is not bound to plasma proteins this clearance rate indicates that renal tubular reabsorption is involved. Pregabalin elimination is nearly proportional to CLcr [see Dosage and Administration (2.5)].
Specific Populations
Age: Geriatric Patients
Pregabalin oral clearance tended to decrease with increasing age. This decrease in pregabalin oral clearance is consistent with age-related decreases in CLcr. Reduction of pregabalin dose may be required in patients who have age-related compromised renal function [see Dosage and Administration (2.5)].
Sex
Population pharmacokinetic analyses of the clinical studies showed that the relationship between daily dose and pregabalin extended-release tablets drug exposure is similar between genders.
Race/Ethnicity
In population pharmacokinetic analyses of the clinical studies of pregabalin and pregabalin extended-release tablets, the pharmacokinetics of pregabalin were not significantly affected by race (Caucasians, Blacks, and Hispanics).
Renal Impairment
Pregabalin clearance is nearly proportional to CLcr. Dosage reduction in patients with reduced renal function is necessary. Pregabalin is effectively removed from plasma by hemodialysis. Following a 4-hour hemodialysis treatment, plasma pregabalin concentrations are reduced by approximately 50%. For patients on hemodialysis, treatment with pregabalin extended-release tablets is not recommended [see Dosage and Administration (2.5)].
Drug Interaction Studies
In Vitro Studies
In vitro studies showed that pregabalin is unlikely to be involved in significant pharmacokinetic drug interactions. Pregabalin, at concentrations that were, in general, 10-times those attained in clinical trials, does not inhibit human CYP1A2, CYP2A6, CYP2C9, CYP2C19, CYP2D6, CYP2E1, and CYP3A4 enzyme systems. In vitro drug interaction studies demonstrate that pregabalin does not induce CYP1A2 or CYP3A4 activity. Therefore, an increase in the metabolism of co-administered CYP1A2 substrates (e.g., theophylline, caffeine) or CYP3A4 substrates (e.g., midazolam, testosterone) is not anticipated.
In Vivo Studies
With the exception of erythromycin, the interactions of pregabalin extended-release tablets with co-administration of other drugs have not been systematically evaluated.
Additional studies have been performed with pregabalin [see Drug Interactions (7)]. No pharmacokinetic interactions were observed between pregabalin and carbamazepine, ethanol, gabapentin, lamotrigine, lorazepam, oral contraceptive, oxycodone, phenobarbital, phenytoin, topiramate, and valproic acid. A similar lack of pharmacokinetic interactions would be expected to occur with pregabalin extended-release tablets.
The drug interaction studies described in this section were conducted in healthy adults, and across various patient populations.
Erythromycin
Multiple-dose administration of erythromycin (500 mg every 6 hours for 18 hours) in healthy subjects resulted in a 17% decrease in AUC of pregabalin extended-release tablets (330 mg single dose).
Ethanol
Multiple-dose administration of pregabalin (300 mg twice a day) in healthy subjects had no effect on the rate and extent of ethanol single-dose pharmacokinetics and single-dose administration of ethanol (0.7 g/kg) had no effect on the steady-state pharmacokinetics of pregabalin. Additive effects on cognitive and gross motor functioning were seen when pregabalin was co-administered with ethanol. No clinically important effects on respiration were seen [see Drug Interactions (7)].
Gabapentin
The pharmacokinetic interactions of pregabalin and gabapentin were investigated in 12 healthy subjects following concomitant single-dose administration of 100-mg pregabalin and 300-mg gabapentin and in 18 healthy subjects following concomitant multiple-dose administration of 200-mg pregabalin every 8 hours and 400-mg gabapentin every 8 hours. Gabapentin pharmacokinetics following single- and multiple-dose administration were unaltered by pregabalin co-administration. The extent of pregabalin absorption was unaffected by gabapentin co-administration, although there was a small reduction in rate of absorption.
Lorazepam
Multiple-dose administration of pregabalin (300 mg twice a day) in healthy subjects had no effect on the rate and extent of lorazepam single-dose pharmacokinetics and single-dose administration of lorazepam (1 mg) had no effect on the steady-state pharmacokinetics of pregabalin. Additive effects on cognitive and gross motor functioning were seen when pregabalin was co-administered with lorazepam. No clinically important effects on respiration were seen [see Drug Interactions (7)].
Oral Contraceptive
Pregabalin co-administration (200 mg 3 times a day) had no effect on the steady-state pharmacokinetics of norethindrone and ethinyl estradiol (1 mg/35 μg, respectively) in healthy subjects.
Oxycodone
Multiple-dose administration of pregabalin (300 mg twice a day) in healthy subjects had no effect on the rate and extent of oxycodone single-dose pharmacokinetics. Single-dose administration of oxycodone (10 mg) had no effect on the steady-state pharmacokinetics of pregabalin. Additive effects on cognitive and gross motor functioning were seen when pregabalin was co-administered with oxycodone. No clinically important effects on respiration were seen [see Drug Interactions (7)].
Carbamazepine, Lamotrigine, Phenobarbital, Phenytoin, Topiramate and Valproic Acid
Steady-state trough plasma concentrations of phenytoin, carbamazepine, and carbamazepine 10,11 epoxide, valproic acid, and lamotrigine were not affected by concomitant pregabalin (200 mg 3 times a day) administration.
Population pharmacokinetic analyses in patients treated with pregabalin and various concomitant medications suggest the following:
| Therapeutic class | Specific concomitant drug studied |
|---|---|
| Concomitant drug has no effect on the pharmacokinetics of pregabalin | |
| Hypoglycemics | Glyburide, insulin, metformin |
| Diuretics | Furosemide |
| Antiepileptic Drugs | Tiagabine |
| Concomitant drug has no effect on the pharmacokinetics of pregabalin and pregabalin has no effect on the pharmacokinetics of concomitant drug | |
| Antiepileptic Drugs | Carbamazepine, lamotrigine, phenobarbital, phenytoin, topiramate, valproic acid |
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
A dose-dependent increase in the incidence of malignant vascular tumors (hemangiosarcomas) was observed in 2 strains of mice (B6C3F1 and CD-1) given pregabalin (200, 1000, or 5000 mg/kg) in the diet for 2 years. Plasma pregabalin exposure (AUC) in mice receiving the lowest dose that increased hemangiosarcomas was approximately equal to the human exposure at the maximum recommended human dose (MRD) of 660 mg/day. A no-effect dose for induction of hemangiosarcomas in mice was not established. No evidence of carcinogenicity was seen in 2 studies in Wistar rats following dietary administration of pregabalin for 2 years at doses (50, 150, or 450 mg/kg in males and 100, 300, or 900 mg/kg in females) that were associated with plasma exposures in males and females up to approximately 15 and 26 times, respectively, human exposure at the MRD.
Mutagenesis
Pregabalin was not mutagenic in bacteria or in mammalian cells in vitro, was not clastogenic in mammalian systems in vitro and in vivo, and did not induce unscheduled DNA synthesis in mouse or rat hepatocytes.
Impairment of Fertility
In fertility studies in which male rats were orally administered pregabalin (50 to 2500 mg/kg) prior to and during mating with untreated females, a number of adverse reproductive and developmental effects were observed. These included decreased sperm counts and sperm motility, increased sperm abnormalities, reduced fertility, increased preimplantation embryo loss, decreased litter size, decreased fetal body weights, and an increased incidence of fetal abnormalities. Effects on sperm and fertility parameters were reversible in studies of this duration (3 to 4 months). The no-effect dose for male reproductive toxicity in these studies (100 mg/kg) was associated with a plasma pregabalin exposure (AUC) approximately 4 times human exposure at the MRD of 660 mg/day.
In addition, adverse reactions on reproductive organ (testes, epididymides) histopathology were observed in male rats exposed to pregabalin (500 to 1250 mg/kg) in general toxicology studies of 4 weeks or greater duration. The no-effect dose for male reproductive organ histopathology in rats (250 mg/kg) was associated with a plasma exposure approximately 10 times human exposure at the MRD.
In a fertility study in which female rats were given pregabalin (500, 1250, or 2500 mg/kg) orally prior to and during mating and early gestation, disrupted estrous cyclicity and an increased number of days to mating were seen at all doses, and embryolethality occurred at the highest dose. The low dose in this study produced a plasma exposure approximately 10 times that in humans receiving the MRD. A no-effect dose for female reproductive toxicity in rats was not established.
13.2 Animal Toxicology and/or Pharmacology
Dermatopathy
Skin lesions ranging from erythema to necrosis were seen in repeated-dose toxicology studies in both rats and monkeys. The etiology of these skin lesions is unknown. At the MRD of 660 mg/day, there is a 2-fold safety margin for the dermatological lesions. The more severe dermatopathies involving necrosis were associated with pregabalin exposures (as expressed by plasma AUCs) of approximately 3 to 8 times those achieved in humans given the MRD. No increase in incidence of skin lesions was observed in clinical studies.
Ocular Lesions
Ocular lesions (characterized by retinal atrophy [including loss of photoreceptor cells] and/or corneal inflammation/mineralization) were observed in 2 lifetime carcinogenicity studies in Wistar rats. These findings were observed at plasma pregabalin exposures (AUC) greater than or equal to 2 times those achieved in humans given the maximum recommended dose of 660 mg/day. A no-effect dose for ocular lesions was not established. Similar lesions were not observed in lifetime carcinogenicity studies in 2 strains of mice or in monkeys treated for 1 year.
14 CLINICAL STUDIES
14.1 Management of Postherpetic Neuralgia (Study PHN CR)
Support for efficacy of pregabalin extended-release tablets for the management of PHN and diabetic peripheral neuropathy (DPN) was based on the efficacy of pregabalin for these indications along with an adequate and well-controlled study in adults with PHN. This 19-week randomized withdrawal study compared daily doses of pregabalin extended-release tablets 82.5 mg, 165 mg, 247.5 mg, 330 mg, 495 mg, or 660 mg with placebo. Those enrolled were required to have pain present for more than 3 months after healing of the herpes zoster skin rash and a baseline pain score of greater than or equal to 4 on the numeric rating scale (NRS)-Pain (assessed over a 1 week recall period). The baseline mean pain scores were 6.83 for pregabalin extended-release tablets-treated patients vs. 6.85 for placebo-treated patients. A total of 82.4% of patients completed the single-blind phase of the study. Patients were considered responders if they had at least a 50% reduction in pain in the single-blind phase. Those who responded to treatment were then randomized in the double-blind phase to treatment with either the pregabalin extended-release tablets dose achieved in the single-blind phase or placebo. Patients were treated for up to 3 months following randomization. A total of 87.5% of pregabalin extended-release tablets-treated patients and 78% of placebo-treated patients completed the double-blind phase of the study.
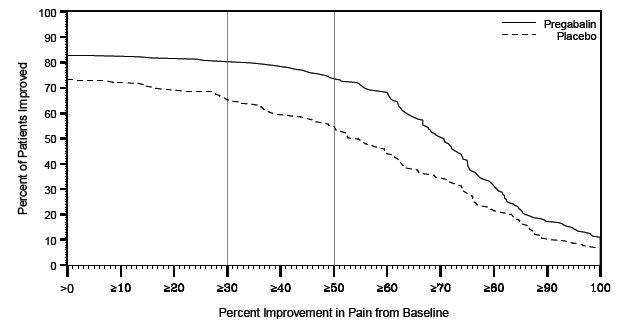
Pregabalin extended-release tablets treatment demonstrated statistically significant improvement in the endpoint change in mean pain score from baseline compared to placebo. For a range of levels of improvement in pain intensity from baseline to study endpoint, Figure 1 shows the fraction of patients achieving that degree of improvement. The figure is cumulative, so that patients whose change from baseline is, for example, 50%, are also included at every level of improvement below 50%. Patients who did not complete the study were assigned 0% improvement. In the pregabalin extended-release tablets group, 79.8% of subjects achieved at least a 30% improvement and 73.6% at least 50% improvement in pain intensity. In the placebo group, 64.9% of subjects achieved at least a 30% improvement and 54.6% at least a 50% improvement in pain intensity.
Figure 1. Percent of Patients Achieving Various Levels of Improvement in Pain Intensity (N=413)
16 HOW SUPPLIED/STORAGE AND HANDLING
Pregabalin extended-release tablets are supplied in the following strengths and package configurations:
| Package Configuration | Tablet Strength (mg) | NDC | Tablet Description |
|---|---|---|---|
| Bottles of 30 tablets | 82.5 mg | NDC: 47781-379-30 | White, oval-shaped, film-coated tablets, “ALV 379” imprinted in black ink on one side, blank on the other side. |
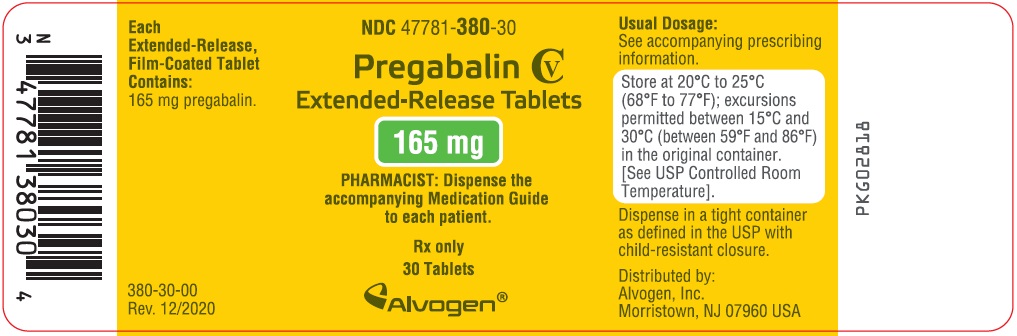
| Bottles of 30 tablets | 165 mg | NDC: 47781-380-30 | Yellow, oval-shaped, film-coated tablets, “ALV 380” imprinted in black ink on one side, blank on the other side. |
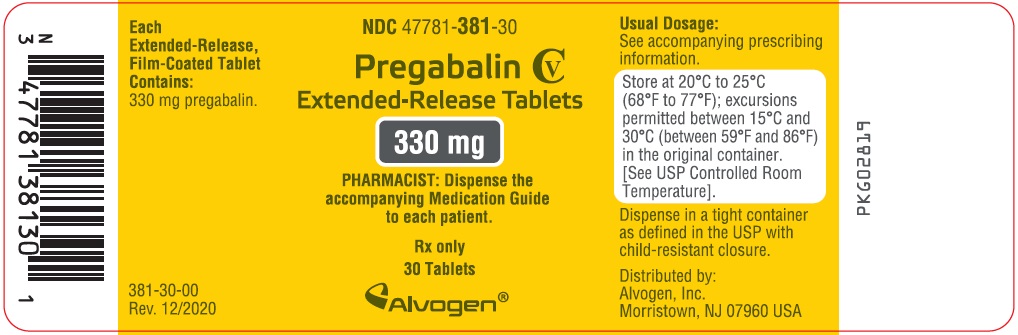
| Bottles of 30 tablets | 330 mg | NDC: 47781-381-30 | Pink, oval-shaped, film-coated tablets, “ALV 381” imprinted in black ink on one side, blank on the other side. |
Store at 20°C to 25°C (68°F to 77°F), excursions permitted between 15°C and 30°C (between 59°F and 86°F) in the original container. (See USP Controlled Room Temperature)
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
Angioedema
Advise patients that pregabalin may cause angioedema, with swelling of the face, mouth (lip, gum, tongue) and neck (larynx and pharynx) that can lead to life-threatening respiratory compromise. Instruct patients to discontinue pregabalin extended-release tablets and immediately seek medical care if they experience these symptoms [see Warnings and Precautions (5.1)].
Hypersensitivity
Advise patients that pregabalin extended-release tablets has been associated with hypersensitivity reactions such as skin redness, blisters, hives, rash, dyspnea, and wheezing. Instruct patients to discontinue pregabalin extended-release tablets and immediately seek medical care if they experience these symptoms [see Warnings and Precautions (5.2)].
Suicidal Thinking and Behavior
Counsel patients, their caregivers, and families that AEDs, including pregabalin, the active ingredient in pregabalin extended-release tablets, may increase the risk of suicidal thoughts and behavior and should be advised of the need to be alert for the emergence or worsening of symptoms of depression, any unusual changes in mood or behavior, or the emergence of suicidal thoughts, behavior, or thoughts about self-harm. Instruct patients, caregivers, and families to report behaviors of concern immediately to a healthcare provider [see Warnings and Precautions (5.3)].
Respiratory Depression
Inform patients about the risk of respiratory depression. Include information that the risk is greatest for those using concomitant central nervous system (CNS) depressants (such as opioid analgesics) or in those with underlying respiratory impairment. Teach patients how to recognize respiratory depression and advise them to seek medical attention immediately if it occurs [see Warnings and Precautions (5.4)].
Dizziness and Somnolence
Inform patients that pregabalin extended-release tablets may cause dizziness, somnolence, blurred vision, and other CNS signs and symptoms. Accordingly, advise patients not to drive, operate complex machinery, or engage in other hazardous activities until they have gained sufficient experience on pregabalin extended-release tablets to gauge whether or not it affects their mental, visual, and/or motor performance adversely [see Warnings and Precautions (5.5)].
CNS Depressants
Inform patients who require concomitant treatment with central nervous system depressants such as opiates or benzodiazepines that they may experience additive CNS side effects, such as respiratory depression, somnolence, and dizziness [see Warnings and Precautions (5.4, 5.5) and Drug Interactions (7)]. Advise patients to avoid consuming alcohol while taking pregabalin extended-release tablets, as pregabalin extended-release tablets may potentiate the impairment of motor skills and sedating effects of alcohol [see Drug Interactions (7)].
Abrupt or Rapid Discontinuation
Advise patients to take pregabalin extended-release tablets as prescribed. Abrupt or rapid discontinuation may result in insomnia, nausea, headache, anxiety, or diarrhea. Advise patients with seizure disorders that abrupt or rapid discontinuation may increase seizure frequency [see Warnings and Precautions (5.6)].
Missed Dose
Instruct patients that if they miss taking their dose of pregabalin extended-release tablets after an evening meal, then they should take their usual dose of pregabalin extended-release tablets prior to bedtime following a snack. If they miss taking the dose of pregabalin extended-release tablets prior to bedtime, then they should take their usual dose of pregabalin extended-release tablets following a morning meal. If they miss taking the dose of pregabalin extended-release tablets following the morning meal, then they should take their usual dose of pregabalin extended-release tablets at the usual time that evening following an evening meal.
Weight Gain and Edema
Inform patients that pregabalin extended-release tablets may cause edema and weight gain. Advise patients that concomitant treatment with pregabalin extended-release tablets and a thiazolidinedione antidiabetic agent may lead to an additive effect on edema and weight gain. Advise patients with preexisting cardiac conditions that this may increase the risk of heart failure [see Warnings and Precautions (5.7, 5.8)].
Ophthalmological Effects
Counsel patients that pregabalin extended-release tablets may cause visual disturbances. Inform patients that if changes in vision occur, they should notify their physician [see Warnings and Precautions (5.10)].
Creatine Kinase Elevations
Instruct patients to promptly report unexplained muscle pain, tenderness, or weakness, particularly if accompanied by malaise or fever [see Warnings and Precautions (5.11)].
Use in Pregnancy
Advise pregnant patients to enroll in the North American Antiepileptic Drug (NAAED) Pregnancy Registry [see Use in Specific Populations (8.1)].
Lactation
Advise nursing mothers that breastfeeding is not recommended during treatment with pregabalin extended-release tablets [see Use in Specific Populations (8.2)].
Male Fertility
Inform men being treated with pregabalin extended-release tablets who plan to father a child of the potential risk of male-mediated teratogenicity [see Nonclinical Toxicology (13.1) and Use in Specific Populations (8.3)].
Dermatopathy
Instruct diabetic patients to pay particular attention to skin integrity while being treated with pregabalin extended-release tablets [see Nonclinical Toxicology (13.2)].
PRINCIPAL DISPLAY PANEL - 82.5 mg Bottle Label
NDC 47781-379-30
Pregabalin CV
Extended-Release Tablets
82.5 mg
PHARMACIST: Dispense the accompanying Medication Guide to each patient.
Rx only
30 Tablets
| PREGABALIN EXTENDED RELEASE
pregabalin tablet, film coated, extended release |
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
| PREGABALIN EXTENDED RELEASE
pregabalin tablet, film coated, extended release |
||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||
| PREGABALIN EXTENDED RELEASE
pregabalin tablet, film coated, extended release |
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
| Labeler - Alvogen Inc. (008057330) |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.