ESMOLOL HYDROCHLORIDE injection
Esmolol Hydrochloride by
Drug Labeling and Warnings
Esmolol Hydrochloride by is a Prescription medication manufactured, distributed, or labeled by West Ward Pharmaceutical Corporation, West Ward Pharmaceutical Corporation, Cherry Hill New Jersey, Lancaster Laboratories. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
- SPL UNCLASSIFIED SECTION
-
DESCRIPTION
Esmolol hydrochloride is a beta1-selective (cardioselective) adrenergic receptor blocking agent with a very short duration of action (elimination half-life is approximately 9 minutes). Esmolol Hydrochloride is:
(±)-Methyl p- [2-hydroxy-3- (isopropylamino) propoxy] hydrocinnamate hydrochloride and has the following structure:
![Image of the Esmolol Hydrochloride structure: (±)-Methyl p- [2-hydroxy-3- (isopropylamino) propoxy] hydrocinnamate hydrochloride](https://fda.report/DailyMed/a70baf53-e38a-4b23-8905-ee284170236d/9adad150-da57-4281-bfab-7780c25f26a6-01.jpg)
Esmolol hydrochloride has the empirical formula C16H26NO4Cl and a molecular weight of 331.8. It has one asymmetric center and exists as an enantiomeric pair.
Esmolol hydrochloride is a white to off-white crystalline powder. It is a relatively hydrophilic compound which is very soluble in water and freely soluble in alcohol. Its partition coefficient (octanol/water) at pH 7.0 is 0.42 compared to 17.0 for propranolol.
Esmolol Hydrochloride Injection
Esmolol Hydrochloride Injection is a clear, colorless to light yellow, sterile, nonpyrogenic, iso-osmotic solution of esmolol hydrochloride in sodium chloride.
100 mg, 10 mL Single Dose Vial– Each mL contains 10 mg Esmolol Hydrochloride, 5.9 mg Sodium Chloride, USP and Water for Injection, USP; buffered with 2.8 mg Sodium Acetate Trihydrate, USP and 0.546 mg Glacial Acetic Acid, USP. Sodium Hydroxide and/or Hydrochloric Acid added, as necessary to adjust pH to 5.0 (4.5-5.5).
-
CLINICAL PHARMACOLOGY
Esmolol hydrochloride is a beta1-selective (cardioselective) adrenergic receptor blocking agent with rapid onset, a very short duration of action, and no significant intrinsic sympathomimetic or membrane stabilizing activity at therapeutic dosages. Its elimination half-life after intravenous infusion is approximately 9 minutes. Esmolol hydrochloride inhibits the beta1 receptors located chiefly in cardiac muscle, but this preferential effect is not absolute and at higher doses it begins to inhibit beta2 receptors located chiefly in the bronchial and vascular musculature.
Pharmacokinetics and Metabolism
Esmolol hydrochloride is rapidly metabolized by hydrolysis of the ester linkage, chiefly by the esterases in the cytosol of red blood cells and not by plasma cholinesterases or red cell membrane acetylcholinesterase. Total body clearance in man was found to be about 20 L/kg/hr, which is greater than cardiac output; thus the metabolism of esmolol hydrochloride is not limited by the rate of blood flow to metabolizing tissues such as the liver or affected by hepatic or renal blood flow. Esmolol hydrochloride has a rapid distribution half-life of about 2 minutes and an elimination half-life of about 9 minutes.
Using an appropriate loading dose, steady-state blood levels of esmolol hydrochloride for dosages from 50-300 mcg/kg/min (0.05-0.3 mg/kg/min) are obtained within five minutes. (Steady-state is reached in about 30 minutes without the loading dose.) Steady-state blood levels of esmolol hydrochloride increase linearly over this dosage range and elimination kinetics are dose-independent over this range. Steady-state blood levels are maintained during infusion but decrease rapidly after termination of the infusion. Because of its short half-life, blood levels of esmolol hydrochloride can be rapidly altered by increasing or decreasing the infusion rate and rapidly eliminated by discontinuing the infusion.
Consistent with the high rate of blood-based metabolism of esmolol hydrochloride, less than 2% of the drug is excreted unchanged in the urine. Within 24 hours of the end of infusion, approximately 73-88% of the dosage has been accounted for in the urine as the acid metabolite of esmolol hydrochloride.
Metabolism of esmolol hydrochloride results in the formation of the corresponding free acid and methanol. The acid metabolite has been shown in animals to have about 1/1500th the activity of esmolol and in normal volunteers its blood levels do not correspond to the level of beta blockade. The acid metabolite has an elimination half-life of about 3.7 hours and is excreted in the urine with a clearance approximately equivalent to the glomerular filtration rate. Excretion of the acid metabolite is significantly decreased in patients with renal disease, with the elimination half-life increased to about ten-fold that of normals, and plasma levels considerably elevated.
Methanol blood levels, monitored in subjects receiving esmolol hydrochloride for up to 6 hours at 300 mcg/kg/min (0.3 mg/kg/min) and 24 hours at 150 mcg/kg/min (0.15 mg/kg/min), approximated endogenous levels and were less than 2% of levels usually associated with methanol toxicity.
Esmolol hydrochloride has been shown to be 55% bound to human plasma protein, while the acid metabolite is only 10% bound.
Pharmacodynamics
Clinical pharmacology studies in normal volunteers have confirmed the beta blocking activity of esmolol hydrochloride, showing reduction in heart rate at rest and during exercise, and attenuation of isoproterenol-induced increases in heart rate. Blood levels of esmolol hydrochloride have been shown to correlate with extent of beta blockade. After termination of infusion, substantial recovery from beta blockade is observed in 10-20 minutes.
In human electrophysiology studies, esmolol hydrochloride produced effects typical of a beta blocker; a decrease in the heart rate, increase in sinus cycle length, prolongation of the sinus node recovery time, prolongation of the AH interval during normal sinus rhythm and during atrial pacing, and an increase in antegrade Wenckebach cycle length.
In patients undergoing radionuclide angiography, esmolol hydrochloride, at dosages of 200 mcg/kg/min (0.2 mg/kg/min), produced reductions in heart rate, systolic blood pressure, rate pressure product, left and right ventricular ejection fraction and cardiac index at rest, which were similar in magnitude to those produced by intravenous propranolol (4 mg). During exercise, esmolol hydrochloride produced reductions in heart rate, rate pressure product and cardiac index which were also similar to those produced by propranolol, but produced a significantly larger fall in systolic blood pressure. In patients undergoing cardiac catheterization, the maximum therapeutic dose of 300 mcg/kg/min (0.3 mg/kg/min) of esmolol hydrochloride produced similar effects and, in addition, there were small, clinically insignificant increases in the left ventricular end diastolic pressure and pulmonary capillary wedge pressure. At thirty minutes after the discontinuation of esmolol hydrochloride infusion, all of the hemodynamic parameters had returned to pretreatment levels.
The relative cardioselectivity of esmolol hydrochloride was demonstrated in 10 mildly asthmatic patients. Infusions of esmolol hydrochloride [100, 200 and 300 mcg/kg/min (0.1, 0.2 and 0.3 mg/kg/min)] produced no significant increases in specific airway resistance compared to placebo. At 300 mcg/kg/min (0.3 mg/kg/min), esmolol hydrochloride produced slightly enhanced bronchomotor sensitivity to dry air stimulus. These effects were not clinically significant, and esmolol hydrochloride was well tolerated by all patients. Six of the patients also received intravenous propranolol, and at a dosage of 1 mg, two experienced significant, symptomatic bronchospasm requiring bronchodilator treatment. One other propranolol-treated patient also experienced dry air-induced bronchospasm. No adverse pulmonary effects were observed in patients with COPD who received therapeutic dosages of esmolol hydrochloride for treatment of supraventricular tachycardia (51 patients) or in perioperative settings (32 patients).
Supraventricular Tachycardia
In two multicenter, randomized, double-blind, controlled comparisons of esmolol hydrochloride with placebo and propranolol, maintenance doses of 50 to 300 mcg/kg/min (0.05 to 0.3 mg/kg/min) of esmolol hydrochloride were found to be more effective than placebo and about as effective as propranolol, 3-6 mg given by bolus injections, in the treatment of supraventricular tachycardia, principally atrial fibrillation and atrial flutter. The majority of these patients developed their arrhythmias postoperatively. About 60-70% of the patients treated with esmolol hydrochloride had a desired therapeutic effect (either a 20% reduction in heart rate, a decrease in heart rate to less than 100 bpm, or, rarely, conversion to NSR) and about 95% of those who responded did so at a dosage of 200 mcg/kg/min (0.2 mg/kg/min) or less. The average effective dosage of esmolol hydrochloride was approximately 100-115 mcg/kg/min (0.1-0.115 mg/kg/min) in the two studies. Other multicenter baseline-controlled studies gave essentially similar results. In the comparison with propranolol, about 50% of patients in both the esmolol hydrochloride and propranolol groups were on concomitant digoxin. Response rates were slightly higher with both beta blockers in the digoxin-treated patients.
In all studies significant decreases of blood pressure occurred in 20-50% of patients, identified either as adverse reaction reports by investigators, or by observation of systolic pressure less than 90 mmHg or diastolic pressure less than 50 mmHg. The hypotension was symptomatic (mainly diaphoresis or dizziness) in about 12% of patients, and therapy was discontinued in about 11% of patients, about half of whom were symptomatic. In comparison to propranolol, hypotension was about three times as frequent with esmolol hydrochloride, 53% vs. 17%. The hypotension was rapidly reversible with decreased infusion rate or after discontinuation of therapy with esmolol hydrochloride. For both esmolol hydrochloride and propranolol, hypotension was reported less frequently in patients receiving concomitant digoxin.
-
INDICATIONS AND USAGE
Supraventricular Tachycardia
Esmolol hydrochloride is indicated for the rapid control of ventricular rate in patients with atrial fibrillation or atrial flutter in perioperative, postoperative, or other emergent circumstances where short term control of ventricular rate with a short-acting agent is desirable. Esmolol hydrochloride is also indicated in noncompensatory sinus tachycardia where, in the physician’s judgment, the rapid heart rate requires specific intervention. Esmolol hydrochloride is not intended for use in chronic settings where transfer to another agent is anticipated.
Intraoperative and Postoperative Tachycardia and/or Hypertension
Esmolol hydrochloride is indicated for the treatment of tachycardia and hypertension that occur during induction and tracheal intubation, during surgery, on emergence from anesthesia, and in the postoperative period, when in the physician’s judgment such specific intervention is considered indicated.
Use of esmolol hydrochloride to prevent such events is not recommended.
-
CONTRAINDICATIONS
Esmolol hydrochloride is contraindicated in patients with sinus bradycardia, heart block greater than first degree, cardiogenic shock or overt heart failure (see WARNINGS).
-
WARNINGS
Hypotension
In clinical trials 20-50% of patients treated with esmolol hydrochloride have experienced hypotension, generally defined as systolic pressure less than 90 mmHg and/or diastolic pressure less than 50 mmHg. About 12% of the patients have been symptomatic (mainly diaphoresis or dizziness). Hypotension can occur at any dose but is dose-related so that doses beyond 200 mcg/kg/min (0.2 mg/kg/min) are not recommended. Patients should be closely monitored, especially if pretreatment blood pressure is low. Decrease of dose or termination of infusion reverses hypotension, usually within 30 minutes.
Cardiac Failure
Sympathetic stimulation is necessary in supporting circulatory function in congestive heart failure, and beta blockade carries the potential hazard of further depressing myocardial contractility and precipitating more severe failure. Continued depression of the myocardium with beta blocking agents over a period of time can, in some cases, lead to cardiac failure. At the first sign or symptom of impending cardiac failure, esmolol hydrochloride should be withdrawn. Although withdrawal may be sufficient because of the short elimination half-life of esmolol hydrochloride, specific treatment may also be considered (see OVERDOSAGE). The use of esmolol hydrochloride for control of ventricular response in patients with supraventricular arrhythmias should be undertaken with caution when the patient is compromised hemodynamically or is taking other drugs that decrease any or all of the following: peripheral resistance, myocardial filling, myocardial contractility, or electrical impulse propagation in the myocardium. Despite the rapid onset and offset of the effects of esmolol hydrochloride, several cases of death have been reported in complex clinical states where esmolol hydrochloride was presumably being used to control ventricular rate.
Intraoperative and Postoperative Tachycardia and/or Hypertension
Esmolol hydrochloride should not be used as the treatment for hypertension in patients in whom the increased blood pressure is primarily due to the vasoconstriction associated with hypothermia.
Bronchospastic Diseases
PATIENTS WITH BRONCHOSPASTIC DISEASES SHOULD, IN GENERAL, NOT RECEIVE BETA BLOCKERS. Because of its relative beta1 selectivity and titratability, esmolol hydrochloride may be used with caution in patients with bronchospastic diseases. However, since beta1 selectivity is not absolute, esmolol hydrochloride should be carefully titrated to obtain the lowest possible effective dose. In the event of bronchospasm, the infusion should be terminated immediately; a beta2 stimulating agent may be administered if conditions warrant but should be used with particular caution as patients already have rapid ventricular rates.
-
PRECAUTIONS
General
Because the acid metabolite of esmolol hydrochloride is primarily excreted unchanged by the kidney, esmolol hydrochloride should be administered with caution to patients with impaired renal function. The elimination half-life of the acid metabolite was prolonged ten-fold and the plasma level was considerably elevated in patients with end-stage renal disease.
Drug Interactions
Catecholamine-depleting drugs, e.g., reserpine, may have an additive effect when given with beta blocking agents. Patients treated concurrently with esmolol hydrochloride and a catecholamine depletor should therefore be closely observed for evidence of hypotension or marked bradycardia, which may result in vertigo, syncope, or postural hypotension.
A study of interaction between esmolol hydrochloride and warfarin showed that concomitant administration of esmolol hydrochloride and warfarin does not alter warfarin plasma levels. Esmolol hydrochloride concentrations were equivocally higher when given with warfarin, but this is not likely to be clinically important.
When digoxin and esmolol hydrochloride were concomitantly administered intravenously to normal volunteers, there was a 10-20% increase in digoxin blood levels at some time points. Digoxin did not affect esmolol hydrochloride pharmacokinetics. When intravenous morphine and esmolol hydrochloride were concomitantly administered in normal subjects, no effect on morphine blood levels was seen, but esmolol hydrochloride steady-state blood levels were increased by 46% in the presence of morphine. No other pharmacokinetic parameters were changed.
The effect of esmolol hydrochloride on the duration of succinylcholine-induced neuromuscular blockade was studied in patients undergoing surgery. The onset of neuromuscular blockade by succinylcholine was unaffected by esmolol hydrochloride, but the duration of neuromuscular blockade was prolonged from 5 minutes to 8 minutes.
Although the interactions observed in these studies do not appear to be of major clinical importance, esmolol hydrochloride should be titrated with caution in patients being treated concurrently with digoxin, morphine, succinylcholine or warfarin.
While taking beta blockers, patients with a history of severe anaphylactic reaction to a variety of allergens may be more reactive to repeated challenge, either accidental, diagnostic, or therapeutic. Such patients may be unresponsive to the usual doses of epinephrine used to treat allergic reaction.
Caution should be exercised when considering the use of esmolol hydrochloride and verapamil in patients with depressed myocardial function. Fatal cardiac arrests have occurred in patients receiving both drugs. Additionally, esmolol hydrochloride should not be used to control supraventricular tachycardia in the presence of agents which are vasoconstrictive and inotropic such as dopamine, epinephrine, and norepinephrine because of the danger of blocking cardiac contractility when systemic vascular resistance is high.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Because of its short term usage no carcinogenicity, mutagenicity or reproductive performance studies have been conducted with esmolol hydrochloride.
Pregnancy Category C
Teratogenicity studies in rats at intravenous dosages of esmolol hydrochloride up to 3000 mcg/kg/min (3 mg/kg/min) (ten times the maximum human maintenance dosage) for 30 minutes daily produced no evidence of maternal toxicity, embryotoxicity or teratogenicity, while a dosage of 10,000 mcg/kg/min (10 mg/kg/min) produced maternal toxicity and lethality. In rabbits, intravenous dosages up to 1000 mcg/kg/min (1 mg/kg/min) for 30 minutes daily produced no evidence of maternal toxicity, embryotoxicity or teratogenicity, while 2500 mcg/kg/min (2.5 mg/kg/min) produced minimal maternal toxicity and increased fetal resorptions.
Although there are no adequate and well-controlled studies in pregnant women, use of esmolol in the last trimester of pregnancy or during labor or delivery has been reported to cause fetal bradycardia, which continued after termination of drug infusion. Esmolol hydrochloride should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
-
ADVERSE REACTIONS
The following adverse reaction rates are based on use of esmolol hydrochloride in clinical trials involving 369 patients with supraventricular tachycardia and over 600 intraoperative and postoperative patients enrolled in clinical trials. Most adverse effects observed in controlled clinical trial settings have been mild and transient.
The most important adverse effect has been hypotension (see WARNINGS). Deaths have been reported in post-marketing experience occurring during complex clinical states where esmolol hydrochloride was presumably being used simply to control ventricular rate (see WARNINGS, Cardiac Failure).
Cardiovascular
Symptomatic hypotension (diaphoresis, dizziness) occurred in 12% of patients, and therapy was discontinued in about 11%, about half of whom were symptomatic. Asymptomatic hypotension occurred in about 25% of patients. Hypotension resolved during esmolol hydrochloride infusion in 63% of these patients and within 30 minutes after discontinuation of infusion in 80% of the remaining patients. Diaphoresis accompanied hypotension in 10% of patients. Peripheral ischemia occurred in approximately 1% of patients. Pallor, flushing, bradycardia (heart rate less than 50 beats per minute), chest pain, syncope, pulmonary edema and heart block have each been reported in less than 1% of patients. In two patients without supraventricular tachycardia but with serious coronary artery disease (post inferior myocardial infarction or unstable angina), severe bradycardia/sinus pause/asystole has developed, reversible in both cases with discontinuation of treatment.
Central Nervous System
Dizziness has occurred in 3% of patients; somnolence in 3%; confusion, headache, and agitation in about 2%; and fatigue in about 1% of patients. Paresthesia, asthenia, depression, abnormal thinking, anxiety, anorexia, and lightheadedness were reported in less than 1% of patients. Seizures were also reported in less than 1% of patients, with one death.
Respiratory
Bronchospasm, wheezing, dyspnea, nasal congestion, rhonchi, and rales have each been reported in less than 1% of patients.
Gastrointestinal
Nausea was reported in 7% of patients. Vomiting has occurred in about 1% of patients. Dyspepsia, constipation, dry mouth, and abdominal discomfort have each occurred in less than 1% of patients. Taste perversion has also been reported.
-
OVERDOSAGE
Acute Toxicity
Overdoses of esmolol hydrochloride can cause cardiac arrest. In addition, overdoses can produce bradycardia, hypotension, electromechanical dissociation and loss of consciousness. Cases of massive accidental overdoses of esmolol hydrochloride have occurred due to dilution errors. Some of these overdoses have been fatal while others resulted in permanent disability. Bolus doses in the range of 625 mg to 2.5 g (12.5-50 mg/kg) have been fatal. Patients have recovered completely from overdoses as high as 1.75 g given over one minute or doses of 7.5 g given over one hour for cardiovascular surgery. The patients who survived appear to be those whose circulation could be supported until the effects of esmolol hydrochloride resolved.
Because of its approximately 9-minute elimination half-life, the first step in the management of toxicity should be to discontinue the esmolol hydrochloride infusion. Then, based on the observed clinical effects, the following general measures should also be considered.
Bradycardia: Intravenous administration of atropine or another anticholinergic drug.
Bronchospasm: Intravenous administration of a beta2 stimulating agent and/or a theophylline derivative.
Cardiac Failure: Intravenous administration of a diuretic and/or digitalis glycoside. In shock resulting from inadequate cardiac contractility, intravenous administration of dopamine, dobutamine, isoproterenol, or amrinone may be considered.
Symptomatic Hypotension: Intravenous administration of fluids and/or pressor agents.
-
DOSAGE AND ADMINISTRATION
Dosing Information:
SUPRAVENTRICULAR TACHYCARDIA
Dosage needs to be titrated, using ventricular rate as the guide.
An initial loading dose of 0.5 milligrams/kg (500 micrograms/kg) infused over a minute duration followed by a maintenance infusion of 0.05 milligrams/kg/min (50 micrograms/kg/min) for the next 4 minutes is recommended. This should give a rough guide with respect to the responsiveness of ventricular rate.
After the 4 minutes of initial maintenance infusion (total treatment duration being 5 minutes), depending upon the desired ventricular response, the maintenance infusion may be continued at 0.05 mg/kg/min or increased step-wise (e.g. 0.1 mg/kg/min, 0.15 mg/kg/min to a maximum of 0.2 mg/kg/min) with each step being maintained for 4 or more minutes.
If more rapid slowing of ventricular response is imperative, the 0.5 mg/kg loading dose infused over a 1 minute period may be repeated, followed by a maintenance infusion of 0.1 mg/kg/min for 4 minutes. Then, depending upon ventricular rate, another (and final) loading dose of 0.5 mg/kg/min infused over a 1 minute period may be administered followed by a maintenance infusion of 0.15 mg/kg/min. If needed, after 4 minutes of the 0.15 mg/kg/min maintenance infusion, the maintenance infusion may be increased to a maximum of 0.2 mg/kg/min.
In the absence of loading doses, constant infusion of a single concentration of esmolol reaches pharmacokinetic and pharmacodynamic steady-state in about 30 minutes. Maintenance infusions (with or without loading doses) may be continued for as long as 24 hours.
The following table summarizes the above and assumes that 3 loading doses (the maximum recommended) are infused over 1 minute and incremental maintenance doses are required after each loading dose. There should be no 4th loading dose, but the maintenance dose may be incremented one more time.
- * As the desired heart rate or endpoint is approached, the loading infusion may be omitted and the maintenance infusion titrated to 300 mcg/kg/min (0.3 mg/kg/min) or downward as appropriate. Maintenance dosages above 200 mcg/kg/min (0.2 mg/kg/min) have not been shown to have significantly increased benefits. The interval between titration steps may be increased.
Elapsed Time Loading Dose
(over 1 minute)Maintenance Dose
(over 4 minutes)(minutes) micrograms/kg/min milligrams/kg/min micrograms/kg/min milligrams/kg/min 0 – 1 500 0.5 1 – 5 50 0.05 5 – 6 500 0.5 6 – 10 100 0.1 10 – 11 500 0.5 11 – 15 150 0.15 15 – 16 · · 16 - 20 *200 *0.2 > 20 Maintenance dose titrated to heart rate or other clinical endpoint. In the treatment of supraventricular tachycardia, responses to esmolol hydrochloride usually (over 95%) occur within the range of 50 to 200 micrograms/kg/min (0.05 to 0.2 milligrams/kg/min). The average effective dosage is approximately 100 micrograms/kg/min (0.1 milligrams/kg/min) although dosages as low as 25 micrograms/kg/min (0.025 milligrams/kg/min) have been adequate in some patients. Dosages as high as 300 micrograms/kg/min (0.3 milligrams/kg/min) have been used, but these provide little added effect and increase the rate of adverse effects, so doses greater than 200 micrograms/kg/min are not recommended. Dosage of esmolol hydrochloride in supraventricular tachycardia must be individualized by titration in which each step consists of a loading dosage followed by a maintenance dosage.
This specific dosage regimen has not been studied intraoperatively and, because of the time required for titration, may not be optimal for intraoperative use.
The safety of dosages above 300 mcg/kg/min (0.3 mg/kg/min) has not been studied.
In the event of an adverse reaction, the dosage of esmolol hydrochloride may be reduced or discontinued. If a local infusion site reaction develops, an alternate infusion site should be used and caution should be taken to prevent extravasation. The use of butterfly needles should be avoided.
Abrupt cessation of esmolol hydrochloride in patients has not been reported to produce the withdrawal effects which may occur with abrupt withdrawal of beta blockers following chronic use in coronary artery disease (CAD) patients. However, caution should still be used in abruptly discontinuing infusions of esmolol hydrochloride in CAD patients.
After achieving an adequate control of the heart rate and a stable clinical status in patients with supraventricular tachycardia, transition to alternative antiarrhythmic agents such as propranolol, digoxin, or verapamil, may be accomplished.
A recommended guideline for such a transition is given below but the physician should carefully consider the labeling instructions for the alternative agent selected.
Alternative Agent Dosage Propranolol hydrochloride 10-20 mg q 4-6 hrs Digoxin 0.125-0.5 mg q 6 hrs (p.o. or i.v.) Verapamil 80 mg q 6 hrs The dosage of esmolol hydrochloride should be reduced as follows:
- Thirty minutes following the first dose of the alternative agent, reduce the infusion rate of esmolol hydrochloride by one-half (50%).
- Following the second dose of the alternative agent, monitor the patient’s response and if satisfactory control is maintained for the first hour, discontinue esmolol hydrochloride.
The use of infusions of esmolol hydrochloride up to 24 hours has been well documented; in addition, limited data from 24-48 hrs (N=48) indicate that esmolol hydrochloride is well tolerated up to 48 hours.
INTRAOPERATIVE AND POSTOPERATIVE TACHYCARDIA AND/OR HYPERTENSION
In the intraoperative and postoperative settings it is not always advisable to slowly titrate the dose of esmolol hydrochloride to a therapeutic effect. Therefore, two dosing options are presented: immediate control dosing and a gradual control when the physician has time to titrate.
-
Immediate Control
For intraoperative treatment of tachycardia and/or hypertension give an 80 mg (approximately 1 mg/kg) bolus dose over 30 seconds followed by a 150 mcg/kg/min infusion, if necessary. Adjust the infusion rate as required up to 300 mcg/kg/min to maintain desired heart rate and/or blood pressure. -
Gradual Control
For postoperative tachycardia and hypertension, the dosing schedule is the same as that used in supraventricular tachycardia. To initiate treatment, administer a loading dosage infusion of 500 mcg/kg/min of esmolol hydrochloride for one minute followed by a four-minute maintenance infusion of 50 mcg/kg/min. If an adequate therapeutic effect is not observed within five minutes, repeat the same loading dosage and follow with a maintenance infusion increased to 100 mcg/kg/min (see above SUPRAVENTRICULAR TACHYCARDIA).
Notes:
1. Higher dosages (250-300 mcg/kg/min) may be required for adequate control of blood pressure than those required for the treatment of atrial fibrillation, flutter and sinus tachycardia. One third of the postoperative hypertensive patients required these higher doses.
2. Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
Directions for Use of the 10 mL Ready-to-use Vial (10 milligrams/mL)
This dosage form is prediluted to provide a ready-to-use, iso-osmotic solution of 10 mg/mL esmolol hydrochloride in sodium chloride recommended for esmolol hydrochloride intravenous administration. It may be used to administer the appropriate esmolol hydrochloride loading dosage infusions by hand-held syringe while the maintenance infusion is being prepared.
The 10 mL Ready-to-use Vial esmolol hydrochloride at a concentration of 10 milligrams/mL. When using a 10 milligrams/mL concentration, a loading dose of 0.5 mg/kg infused over 1 minute period of time, for a 70 kg patient is 3.5 mL.
Compatibility with Commonly Used Intravenous Fluids
Esmolol hydrochloride was tested for compatibility with ten commonly used intravenous fluids at a final concentration of 10 mg Esmolol Hydrochloride per mL. Esmolol hydrochloride was found to be compatible with the following solutions and was stable for at least 24 hours at controlled room temperature or under refrigeration:
- Dextrose (5%) Injection, USP
- Dextrose (5%) in Lactated Ringer’s Injection
- Dextrose (5%) in Ringer’s Injection
- Dextrose (5%) and Sodium Chloride (0.45%) Injection, USP
- Dextrose (5%) and Sodium Chloride (0.9%) Injection, USP
- Lactated Ringer’s Injection, USP
- Potassium Chloride (40 mEq/liter) in Dextrose (5%) Injection, USP
- Sodium Chloride (0.45%) Injection, USP
- Sodium Chloride (0.9%) Injection, USP
Esmolol hydrochloride is NOT compatible with Sodium Bicarbonate (5%) Injection, USP.
-
HOW SUPPLIED
Esmolol Hydrochloride Injection
NDC: 0641-2965-45, 100 mg - 10 mL Ready-to-use Vials, Package of 25
Store at 25˚C (77˚F). Excursions permitted to 15˚-30˚C (59˚-86˚F). [See USP Controlled Room Temperature.] PROTECT FROM FREEZING. Avoid excessive heat.
Manufactured for
Baxter Healthcare Corporation
Deerfield, IL 60015 USA
Baxter is a registered trademark of Baxter International Inc.
U.S. Patent Nos. 6,310,094 and 6,528,540.
For Product Inquiry 1 800 ANA DRUG (1-800-262-3784)
MLT-01608/4.0
-
PRINCIPLE DISPLAY PANEL - PACKAGING LABELING
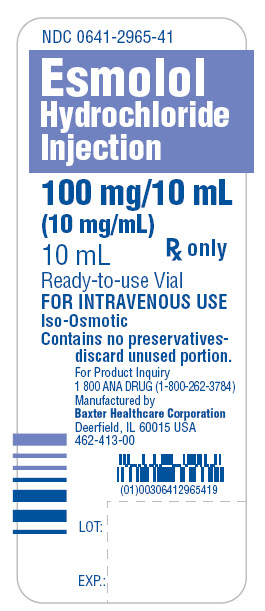
NDC: 0641-2965-41
Esmolol
Hydrochloride
Injection100 mg/10 mL
(10 mg/mL)
10 mLRx only
Ready-to-use Vial
FOR INTRAVENOUS USE
Iso-Osmotic
Contains no preservatives-
discardunused portion.For Product Inquiry
1 800 ANA DRUG (1-800-262-3784)
Manufactured by
Baxter Healthcare Corporation
Deerfield, IL 60015 USA
462-413-00(01)00306412965419
LOT:
EXP.:
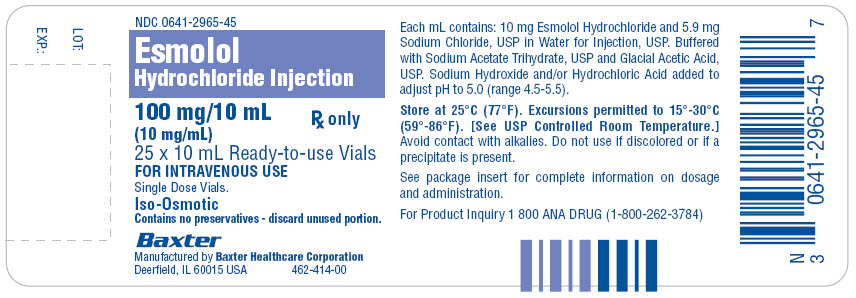
NDC: 0641-2965-45
Esmolol
Hydrochloride Injection
100 mg/10 mL Rx only
(10 mg/mL)
25 x 10 mL Ready-to-use Vials
FOR INTRAVENOUS USE
Single Dose Vials.
Iso-Osmotic
Contains no preservatives - discard unused portion.
Baxter
Manufactured by Baxter Healthcare Corporation
Deerfield, IL 60015 USA 462-414-00
Each mL contains: 10 mg Esmolol Hydrochloride and 5.9 mg
Sodium Chloride, USP in Water for Injection, USP. Buffered
with Sodium Acetate Trihydrate, USP and Glacial Acetic Acid,
USP. Sodium Hydroxide and/or Hydrochloric Acid added to
adjust pH to 5.0 (range 4.5-5.5).
Store at 25°C (77°F). Excursions permitted to 15°-30°C
(59°-86°F). [See USP Controlled Room Temperature.]
Avoid contact with alkalies. Do not use if discolored or if a
precipitate is present.
See package insert for complete information on dosage
and administration.
For Product Inquiry 1 800 ANA DRUG (1-800-262-3784)
N 3 0641-2965-45 7
LOT:
EXP.:
-
INGREDIENTS AND APPEARANCE
ESMOLOL HYDROCHLORIDE
esmolol hydrochloride injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0641-2965 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ESMOLOL HYDROCHLORIDE (UNII: V05260LC8D) (ESMOLOL - UNII:MDY902UXSR) ESMOLOL HYDROCHLORIDE 10 mg in 1 mL Inactive Ingredients Ingredient Name Strength SODIUM CHLORIDE (UNII: 451W47IQ8X) 5.9 mg in 1 mL SODIUM ACETATE (UNII: 4550K0SC9B) ACETIC ACID (UNII: Q40Q9N063P) SODIUM HYDROXIDE (UNII: 55X04QC32I) HYDROCHLORIC ACID (UNII: QTT17582CB) WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0641-2965-45 25 in 1 BOX 1 NDC: 0641-2965-41 10 mL in 1 VIAL Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA019386 12/31/1986 Labeler - West Ward Pharmaceutical Corporation (946499746) Establishment Name Address ID/FEI Business Operations West Ward Pharmaceutical Corporation, Cherry Hill New Jersey 946499746 MANUFACTURE(0641-2965) , LABEL(0641-2965) , PACK(0641-2965) , STERILIZE(0641-2965) , ANALYSIS(0641-2965) Establishment Name Address ID/FEI Business Operations Lancaster Laboratories 069777290 ANALYSIS(0641-2965)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.