ULTOMIRIS- ravulizumab solution, concentrate
ULTOMIRIS by
Drug Labeling and Warnings
ULTOMIRIS by is a Prescription medication manufactured, distributed, or labeled by Alexion Pharmaceuticals Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use ULTOMIRIS safely and effectively. See full prescribing information for ULTOMIRIS.
ULTOMIRIS® (ravulizumab-cwvz) injection, for intravenous use
Initial U.S. Approval: 2018WARNING: SERIOUS MENINGOCOCCAL INFECTIONS
See full prescribing information for complete boxed warning
Life-threatening meningococcal infections/sepsis have occurred in patients treated with ULTOMIRIS and may become rapidly life-threatening or fatal if not recognized and treated early (5.1).
- Comply with the most current Advisory Committee on Immunization Practices (ACIP) recommendations for meningococcal vaccination in patients with complement deficiencies (5.1).
- Immunize patients with meningococcal vaccines at least 2 weeks prior to administering the first dose of ULTOMIRIS, unless the risks of delaying ULTOMIRIS therapy outweigh the risks of developing a meningococcal infection. See Warnings and Precautions (5.1) for additional guidance on the management of the risk of meningococcal infection.
- Vaccination reduces, but does not eliminate, the risk of meningococcal infection. Monitor patients for early signs of meningococcal infections, and evaluate immediately if infection is suspected.
ULTOMIRIS is available only through a restricted program under a Risk Evaluation and Mitigation Strategy (REMS). Under the ULTOMIRIS REMS, prescribers must enroll in the program (5.1).
RECENT MAJOR CHANGES
Indications and Usage 10/2019 Dosing and Administration (2.3, 2.4) 10/2019 Contraindications 10/2019 Warnings and Precautions (5.3) 10/2019 INDICATIONS AND USAGE
ULTOMIRIS is a complement inhibitor indicated for:
- the treatment of adult patients with paroxysmal nocturnal hemoglobinuria (PNH) (1).
- the treatment of adults and pediatric patients one month of age and older with atypical hemolytic uremic syndrome (aHUS) to inhibit complement-mediated thrombotic microangiopathy (TMA) (1).
Limitations of Use:
ULTOMIRIS is not indicated for the treatment of patients with Shiga toxin E. coli related hemolytic uremic syndrome (STEC-HUS).
DOSAGE AND ADMINISTRATION
See Full Prescribing Information for instructions on dosage, preparation, and administration (2.2, 2.3, 2.4, 2.5).
DOSAGE FORMS AND STRENGTHS
Injection: 300 mg/30 mL (10 mg/mL) in a single-dose vial (3).
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
Other Infections: Use caution when administering ULTOMIRIS to patients with any other systemic infection (5.2).
ADVERSE REACTIONS
Most common adverse reactions in patients with PNH (incidence ≥10%) were upper respiratory tract infection and headache (6.1).
Most common adverse reactions in patients with aHUS (incidence ≥20%) were upper respiratory tract infection, diarrhea, nausea, vomiting, headache, hypertension and pyrexia (6.1).
To report SUSPECTED ADVERSE REACTIONS, contact Alexion Pharmaceuticals, Inc. at 1-844-259-6783 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 10/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: SERIOUS MENINGOCOCCAL INFECTIONS
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Vaccination and Prophylaxis
2.2 Recommended Weight-Based Dosage Regimen - PNH
2.3 Recommended Weight-Based Dosage Regimen - aHUS
2.4 Dosing Considerations
2.5 Preparation and Administration
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Serious Meningococcal Infections
5.2 Other Infections
5.3 Monitoring Disease Manifestations after ULTOMIRIS Discontinuation
5.4 Thromboembolic Event Management
5.5 Infusion Reactions
6 ADVERSE REACTIONS
6.1 Clinical Trial Experience
6.2 Immunogenicity
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Paroxysmal Nocturnal Hemoglobinuria (PNH)
14.2 Atypical Hemolytic Uremic Syndrome (aHUS)
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: SERIOUS MENINGOCOCCAL INFECTIONS
Life-threatening meningococcal infections/sepsis have occurred in patients treated with ULTOMIRIS. Meningococcal infection may become rapidly life-threatening or fatal if not recognized and treated early [see Warnings and Precautions (5.1)].
- Comply with the most current Advisory Committee on Immunization Practices (ACIP) recommendations for meningococcal vaccination in patients with complement deficiencies.
- Immunize patients with meningococcal vaccines at least 2 weeks prior to administering the first dose of ULTOMIRIS, unless the risks of delaying ULTOMIRIS therapy outweigh the risk of developing a meningococcal infection. See Warnings and Precautions (5.1) for additional guidance on the management of the risk of meningococcal infection.
- Vaccination reduces, but does not eliminate, the risk of meningococcal infections. Monitor patients for early signs of meningococcal infections and evaluate immediately if infection is suspected.
ULTOMIRIS is available only through a restricted program under a Risk Evaluation and Mitigation Strategy (REMS). Under the ULTOMIRIS REMS, prescribers must enroll in the program [see Warnings and Precautions (5.1)]. Enrollment in the ULTOMIRIS REMS program and additional information are available by telephone: 1-888-765-4747 or at www.ultomirisrems.com.
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Vaccination and Prophylaxis
Vaccinate patients for meningococcal disease according to current ACIP guidelines to reduce the risk of serious infection [see Warnings and Precautions (5.1, 5.2)].
Provide 2 weeks of antibacterial drug prophylaxis to patients if ULTOMIRIS must be initiated immediately and vaccines are administered less than 2 weeks before starting ULTOMIRIS therapy.
Healthcare professionals who prescribe ULTOMIRIS must enroll in the ULTOMIRIS REMS [see Warnings and Precautions (5.1)].
2.2 Recommended Weight-Based Dosage Regimen - PNH
The recommended dosing regimen in adult patients with PNH weighing 40 kg or greater, consists of a loading dose followed by maintenance dosing, administered by intravenous infusion. Administer the doses based on the patient's body weight, as shown in Table 1. Starting 2 weeks after the loading dose administration, begin maintenance doses at a once every 8-week interval.
The dosing schedule is allowed to occasionally vary within 7 days of the scheduled infusion day (except for the first maintenance dose of ULTOMIRIS); but the subsequent doses should be administered according to the original schedule.
Table 1: ULTOMIRIS Weight-Based Dosing Regimen - PNH Body Weight Range (kg) Loading Dose (mg) Maintenance Dose (mg) and Dosing Interval greater than or equal to 40 to less than 60 2,400 3,000 Every 8 weeks greater than or equal to 60 to less than 100 2,700 3,300 greater than or equal to 100 3,000 3,600 2.3 Recommended Weight-Based Dosage Regimen - aHUS
The recommended dosing regimen in adult and pediatric patients one month of age and older with aHUS weighing 5 kg or greater, consists of a loading dose followed by maintenance dosing, administered by intravenous infusion. Administer the doses based on the patient's body weight, as shown in Table 2. Starting 2 weeks after the loading dose administration, begin maintenance doses once every 8 weeks or every 4 weeks (depending on body weight).
The dosing schedule is allowed to occasionally vary within 7 days of the scheduled infusion day (except for the first maintenance dose of ULTOMIRIS); but the subsequent doses should be administered according to the original schedule.
Table 2: ULTOMIRIS Weight-Based Dosing Regimen - aHUS Body Weight Range (kg) Loading Dose (mg) Maintenance Dose (mg) and Dosing Interval greater than or equal to 5 to less than 10 600 300 Every 4 weeks greater than or equal to 10 to less than 20 600 600 greater than or equal to 20 to less than 30 900 2,100 Every 8 weeks greater than or equal to 30 to less than 40 1,200 2,700 greater than or equal to 40 to less than 60 2,400 3,000 greater than or equal to 60 to less than 100 2,700 3,300 greater than or equal to 100 3,000 3,600 2.4 Dosing Considerations
For patients switching from eculizumab to ULTOMIRIS, administer the loading dose of ULTOMIRIS 2 weeks after the last eculizumab infusion, and then administer maintenance doses once every 8 weeks or every 4 weeks (depending on body weight), starting 2 weeks after loading dose administration.
Administration of PE/PI (plasmapheresis or plasma exchange, or fresh frozen plasma infusion) may reduce ULTOMIRIS serum levels. There is no experience with administration of supplemental doses of ULTOMIRIS.
2.5 Preparation and Administration
Preparation of ULTOMIRIS
Each vial of ULTOMIRIS is intended for single-dose only.
ULTOMIRIS requires dilution to a final concentration of 5 mg/mL.
Use aseptic technique to prepare ULTOMIRIS as follows:
- The number of vials to be diluted is determined based on the individual patient's weight and the prescribed dose [see Dosage and Administration (2.2, 2.3)].
- Prior to dilution, visually inspect the solution in the vials; the solution should be free of any particulate matter or precipitation. Do not use if there is evidence of particulate matter or precipitation.
- Withdraw the calculated volume of ULTOMIRIS from the appropriate number of vials and dilute in an infusion bag using 0.9% Sodium Chloride Injection, USP to a final concentration of 5 mg/mL. Refer to the administration reference tables below. The product should be mixed gently. Do not shake. Protect from light. Do not freeze.
- Administer the prepared solution immediately following preparation. Refer to the administration reference tables below for minimum infusion duration. Infusion must be administered through a 0.2 or 0.22 micron filter.
- If the diluted ULTOMIRIS infusion solution is not used immediately, storage under refrigeration at 2°C - 8°C (36°F - 46°F) must not exceed 24 hours taking into account the expected infusion time. Once removed from refrigeration, administer the diluted ULTOMIRIS infusion solution within 6 hours.
Administration of ULTOMIRIS
Only administer as an intravenous infusion.
Dilute ULTOMIRIS to a final concentration of 5 mg/mL.
Administer ULTOMIRIS only through a 0.2 or 0.22 micron filter.
Table 3: Loading Dose Administration Reference Table Body Weight Range
(kg)*Loading Dose (mg) ULTOMIRIS Volume (mL) Volume of NaCl Diluent†
(mL)Total Volume
(mL)Minimum Infusion Time
(hr)Maximum Infusion Rate
(mL/hr)- * Body weight at time of treatment.
- † Dilute ULTOMIRIS only using 0.9% Sodium Chloride Injection, USP.
greater than or equal to 5 to less than 10 600 60 60 120 3.8 31 greater than or equal to 10 to less than 20 600 60 60 120 1.9 63 greater than or equal to 20 to less than 30 900 90 90 180 1.5 120 greater than or equal to 30 to less than 40 1,200 120 120 240 1.3 184 greater than or equal to 40 to less than 60 2,400 240 240 480 1.9 252 greater than or equal to 60 to less than 100 2,700 270 270 540 1.7 317 greater than or equal to 100 3,000 300 300 600 1.8 333 Table 4: Maintenance Dose Administration Reference Table Body Weight Range
(kg)*Maintenance Dose (mg) ULTOMIRIS Volume (mL) Volume of NaCl Diluent†
(mL)Total Volume
(mL)Minimum Infusion Time
(hr)Maximum Infusion Rate
(mL/hr)- * Body weight at time of treatment.
- † Dilute ULTOMIRIS only using 0.9% Sodium Chloride Injection, USP.
greater than or equal to 5 to less than 10 300 30 30 60 1.9 31 greater than or equal to 10 to less than 20 600 60 60 120 1.9 63 greater than or equal to 20 to less than 30 2,100 210 210 420 3.3 127 greater than or equal to 30 to less than 40 2,700 270 270 540 2.8 192 greater than or equal to 40 to less than 60 3,000 300 300 600 2.3 257 greater than or equal to 60 to less than 100 3,300 330 330 660 2 330 greater than or equal to 100 3,600 360 360 720 2.2 327 Prior to administration, allow the admixture to adjust to room temperature (18°C-25°C, 64°F-77°F). Do not heat the admixture in a microwave or with any heat source other than ambient air temperature.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
If an adverse reaction occurs during the administration of ULTOMIRIS, the infusion may be slowed or stopped at the discretion of the physician. Monitor the patient for at least one hour following completion of the infusion for signs or symptoms of an infusion reaction.
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
ULTOMIRIS is contraindicated in:
- Patients with unresolved Neisseria meningitidis infection [see Warnings and Precautions (5.1)].
- Patients who are not currently vaccinated against Neisseria meningitidis, unless the risks of delaying ULTOMIRIS treatment outweigh the risks of developing a meningococcal infection [see Warnings and Precautions (5.1)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Serious Meningococcal Infections
Risk and Prevention
Life-threatening meningococcal infections have occurred in patients treated with ULTOMIRIS. The use of ULTOMIRIS increases a patient's susceptibility to serious meningococcal infections (septicemia and/or meningitis). Meningococcal disease due to any serogroup may occur.
Vaccinate for meningococcal disease according to the most current Advisory Committee on Immunization Practices (ACIP) recommendations for patients with complement deficiencies. Revaccinate patients in accordance with ACIP recommendations considering the duration of ULTOMIRIS therapy.
Immunize patients without a history of meningococcal vaccination at least 2 weeks prior to receiving the first dose of ULTOMIRIS. If urgent ULTOMIRIS therapy is indicated in an unvaccinated patient, administer meningococcal vaccine(s) as soon as possible and provide patients with 2 weeks of antibacterial drug prophylaxis.
In clinical studies, 59 patients with PNH were treated with ULTOMIRIS less than 2 weeks after meningococcal vaccination. All of these patients received antibiotics for prophylaxis of meningococcal infection until at least 2 weeks after meningococcal vaccination. The benefits and risks of antibiotic prophylaxis for prevention of meningococcal infections in patients receiving ULTOMIRIS have not been established.
Vaccination reduces, but does not eliminate, the risk of meningococcal infections. In PNH clinical studies, 3 out of 261 PNH patients developed serious meningococcal infections/sepsis while receiving treatment with ULTOMIRIS; all 3 had been vaccinated. These 3 patients recovered while continuing treatment with ULTOMIRIS.
Closely monitor patients for early signs and symptoms of meningococcal infection and evaluate patients immediately if infection is suspected. Inform patients of these signs and symptoms and steps to be taken to seek immediate medical care. Meningococcal infection may become rapidly life-threatening or fatal if not recognized and treated early. Consider discontinuation of ULTOMIRIS in patients who are undergoing treatment for serious meningococcal infection.
REMS
Due to the risk of meningococcal infections, ULTOMIRIS is available only through a restricted program under a Risk Evaluation and Mitigation Strategy (REMS). Under the ULTOMIRIS REMS, prescribers must enroll in the program.
Prescribers must counsel patients about the risk of meningococcal infection/sepsis, provide the patients with the REMS educational materials, and ensure patients are vaccinated with meningococcal vaccines.
Enrollment in the ULTOMIRIS REMS and additional information are available by telephone: 1-888-765-4747 or at www.ultomirisrems.com.
5.2 Other Infections
ULTOMIRIS blocks terminal complement activation; therefore, patients may have increased susceptibility to encapsulated bacteria infections, especially infections caused by Neisseria meningitidis but also Streptococcus pneumoniae, Haemophilus influenzae, and to a lesser extent, Neisseria gonorrhoeae. Children treated with ULTOMIRIS may be at increased risk of developing serious infections due to Streptococcus pneumoniae and Haemophilus influenzae type b (Hib). Administer vaccinations for the prevention of Streptococcus pneumoniae and Haemophilus influenzae type b (Hib) infections according to ACIP guidelines. If ULTOMIRIS therapy is administered to patients with active systemic infections, monitor closely for signs and symptoms of worsening infection.
5.3 Monitoring Disease Manifestations after ULTOMIRIS Discontinuation
Treatment Discontinuation for PNH
After discontinuing treatment with ULTOMIRIS, closely monitor for signs and symptoms of hemolysis, identified by elevated LDH along with sudden decrease in PNH clone size or hemoglobin, or re-appearance of symptoms such as fatigue, hemoglobinuria, abdominal pain, shortness of breath (dyspnea), major adverse vascular event (including thrombosis), dysphagia, or erectile dysfunction. Monitor any patient who discontinues ULTOMIRIS for at least 16 weeks to detect hemolysis and other reactions. If signs and symptoms of hemolysis occur after discontinuation, including elevated LDH, consider restarting treatment with ULTOMIRIS.
Treatment Discontinuation for aHUS
ULTOMIRIS treatment of aHUS should be a minimum duration of 6 months. Due to heterogeneous nature of aHUS events and patient-specific risk factors, treatment duration beyond the initial 6 months should be individualized.
There are no specific data on ULTOMIRIS discontinuation.
After discontinuing treatment with ULTOMIRIS, patients should be monitored for clinical symptoms and laboratory signs of TMA complications for at least 12 months.
TMA complications post-discontinuation can be identified if any of the following is observed:
- Clinical symptoms of TMA include changes in mental status, seizures, angina, dyspnea, thrombosis or increasing blood pressure.
-
In addition, at least two of the following laboratory signs observed concurrently and results should be confirmed by a second measurement 28 days apart with no interruption
- a decrease in platelet count of 25% or more as compared to either baseline or to peak platelet count during ULTOMIRIS treatment;
- an increase in serum creatinine of 25% or more as compared to baseline or to nadir during ULTOMIRIS treatment;
- an increase in serum LDH of 25% or more as compared to baseline or to nadir during ULTOMIRIS treatment.
If TMA complications occur after ULTOMIRIS discontinuation, consider reinitiation of ULTOMIRIS treatment or appropriate organ-specific supportive measures.
5.4 Thromboembolic Event Management
The effect of withdrawal of anticoagulant therapy during ULTOMIRIS treatment has not been established. Therefore, treatment with ULTOMIRIS should not alter anticoagulant management.
5.5 Infusion Reactions
Administration of ULTOMIRIS may result in infusion reactions. In clinical trials, 5 out of 296 patients treated with ULTOMIRIS experienced infusion reactions (lower back pain, drop in blood pressure, infusion-related pain, elevation in blood pressure and limb discomfort) during ULTOMIRIS administration. These reactions did not require discontinuation of ULTOMIRIS. Interrupt ULTOMIRIS infusion and institute appropriate supportive measures if signs of cardiovascular instability or respiratory compromise occur.
-
6 ADVERSE REACTIONS
The following clinically significant adverse reactions are discussed in greater detail in other sections of the labeling:
- Serious Meningococcal Infections [see Warnings and Precautions (5.1)]
- Other Infections [see Warnings and Precautions (5.2)]
- Monitoring Disease Manifestations after ULTOMIRIS Discontinuation [see Warnings and Precautions (5.3)]
- Infusion Reactions [see Warnings and Precautions (5.5)]
6.1 Clinical Trial Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Paroxysmal Nocturnal Hemoglobinuria (PNH)
The data described below reflect exposure of 441 adult patients with PNH in Phase 3 studies who received ULTOMIRIS (n = 222) or eculizumab (n = 219) at the recommended dosing regimens with median treatment duration of 6 months for ULTOMIRIS and 6 months for eculizumab. The most frequent adverse reactions (≥10%) with ULTOMIRIS were upper respiratory tract infection and headache. Table 5 describes adverse reactions that occurred at a rate of 5% or more among patients treated with ULTOMIRIS in PNH studies.
Serious adverse reactions were reported in 15 (6.8%) patients with PNH receiving ULTOMIRIS. The serious adverse reactions in patients treated with ULTOMIRIS included hyperthermia and pyrexia. No serious adverse reaction was reported in more than 1 patient treated with ULTOMIRIS.
One fatal case of sepsis was identified in a patient treated with ULTOMIRIS.
Table 5: Adverse Reactions Reported in 5% or More of ULTOMIRIS-Treated Patients in Complement Inhibitor Naïve and Eculizumab-Experienced Patients with PNH Body System
Adverse ReactionNumber of Patients ULTOMIRIS
(N=222)
n (%)Eculizumab
(N=219)
n (%)- * Grouped term includes: Nasopharyngitis, Upper respiratory tract infection, Oropharyngeal pain, Viral upper respiratory tract infection, Rhinitis, Respiratory tract infection, Rhinorrhea, Pharyngitis, and Upper respiratory tract inflammation
Gastrointestinal disorders Diarrhea 19 (9) 12 (5) Nausea 19 (9) 19 (9) Abdominal pain 13 (6) 16 (7) General Disorders and Administration Site Conditions Pyrexia 15 (7) 18 (8) Infections and Infestations Upper respiratory tract infection* 86 (39) 86 (39) Musculoskeletal and Connective Tissue Disorders Pain in extremity 14 (6) 11 (5) Arthralgia 11 (5) 12 (5) Nervous System Disorders Headache 71 (32) 57 (26) Dizziness 12 (5) 14 (6) Atypical Hemolytic Uremic Syndrome (aHUS)
The data described below reflect exposure of 58 adult and 16 pediatric patients with aHUS in single-arm trials who received ULTOMIRIS at the recommended dose and schedule. The most frequent adverse reactions reported in ≥20% of patients treated with ULTOMIRIS were upper respiratory tract infection, diarrhea, nausea, vomiting, headache, hypertension and pyrexia. Tables 6, 7 and 8 describes adverse reactions that occurred at a rate of 10% or more among patients treated with ULTOMIRIS in aHUS studies. Serious adverse reactions were reported in 42 (57%) patients with aHUS receiving ULTOMIRIS. The most frequent serious adverse reactions reported in more than 2 patients (2.7%) treated with ULTOMIRIS were hypertension, pneumonia and abdominal pain. Four patients died during the ALXN1210-aHUS-311 study. The cause of death was sepsis in two patients and intracranial hemorrhage in one patient. The fourth patient, who was excluded from the trial after a diagnosis of STEC-HUS, died due to pretreatment cerebral arterial thrombosis.
Table 6: Adverse Reactions Reported in ≥10% of ULTOMIRIS-Treated Patients with aHUS in Study ALXN1210-aHUS-311 Body System
Adverse ReactionALXN1210-aHUS-311
(N=58)All Grades*
(n=53)
n (%)≥ Grade 3
(n=14)
n (%)- * Graded per CTCAE v5.0.
- † Grouped term includes Nasopharyngitis, Pharyngitis, Upper respiratory tract infection, Rhinitis, Viral upper respiratory tract infection, Rhinovirus infection, Viral pharyngitis, Rhinorrhea, and Oropharyngeal pain.
- ‡ Grouped term includes Gastroenteritis, Gastrointestinal infection, Enterocolitis infectious, Infectious colitis, and Enterocolitis.
Blood and lymphatic system disorders Anemia 8 (14) 0 (0) Gastrointestinal disorders Diarrhea 18 (31) 2 (3) Nausea 15 (26) 2 (3) Vomiting 15 (26) 2 (3) Constipation 8 (14) 1 (2) Abdominal pain 7 (12) 1 (2) General disorders and administration site conditions Pyrexia 11 (19) 1 (2) Edema peripheral 10 (17) 0 (0) Fatigue 8 (14) 0 (0) Infections and infestations Upper respiratory tract infection† 15 (26) 0 (0) Urinary tract infection 10 (17) 5 (9) Gastrointestinal infection‡ 8 (14) 2 (3) Metabolism and nutrition disorders Hypokalemia 6 (10) 1 (2) Musculoskeletal and connective tissue disorders Arthralgia 13 (22) 0 (0) Back pain 7 (12) 1 (2) Muscle spasms 6 (10) 0 (0) Pain in extremity 6 (10) 0 (0) Nervous system disorders Headache 23 (40) 1 (2) Psychiatric disorders Anxiety 8 (14) 1 (2) Respiratory, thoracic and mediastinal disorders Cough 10 (17) 0 (0) Dyspnea 10 (17) 1 (2) Skin and subcutaneous tissue disorders Alopecia 6 (10) 0 (0) Dry skin 6 (10) 0 (0) Vascular disorders Hypertension 14 (24) 7 (12) Clinically relevant adverse reactions in <10% of patients include viral tonsillitis.
Table 7: Adverse Reactions Reported in ≥10% of ULTOMIRIS-Treated Patients with aHUS in Study ALXN1210-aHUS-312 Body System
Adverse ReactionALXN1210-aHUS-312
(N=16)All Grades*
(n=16)
n (%)≥ Grade 3
(n=6)
n (%)- * Graded per CTCAE v5.0.
- † Grouped term includes Nasopharyngitis, Pharyngitis, Upper respiratory tract infection, Rhinitis, Viral upper respiratory tract infection, Rhinovirus infection, Viral pharyngitis, Rhinorrhea, and Oropharyngeal pain.
Blood and lymphatic system disorders Anemia 2 (13) 1 (6) Lymphadenopathy 2 (13) 0 (0) Gastrointestinal disorders Diarrhea 6 (38) 0 (0) Constipation 4 (25) 0 (0) Vomiting 4 (25) 1 (6) Abdominal pain 3 (19) 0 (0) Nausea 2 (13) 0 (0) General disorders and administration site conditions Pyrexia 8 (50) 0 (0) Infections and infestations Upper respiratory tract infection† 7 (44) 1 (6) Gastroenteritis viral 2 (13) 2 (13) Pneumonia 2 (13) 1 (6) Tonsillitis 2 (13) 0 (0) Injury, poisoning and procedural complications Contusion 3 (19) 0 (0) Investigations Vitamin D decreased 3 (19) 0 (0) Metabolism and nutrition disorders Decreased appetite 2 (13) 0 (0) Iron deficiency 2 (13) 0 (0) Musculoskeletal and connective tissue disorders Myalgia 3 (19) 0 (0) Pain in extremity 2 (13) 0 (0) Nervous system disorders Headache 5 (31) 0 (0) Respiratory, thoracic and mediastinal disorders Cough 3 (19) 0 (0) Dyspnea 2 (13) 0 (0) Skin and subcutaneous tissue disorders Rash 3 (19) 0 (0) Vascular disorders Hypertension 4 (25) 1 (6) Hypotension 2 (13) 0 (0) Clinically relevant adverse reactions in <10% of patients include viral infection.
Table 8: Adverse Reactions Reported in ≥10% of ULTOMIRIS Treated Patients from Birth to 16 Years of Age with aHUS in Study ALXN1210-aHUS-312 Body System
Adverse ReactionALXN1210-aHUS-312 Age 0 to <2
(N=2)Age 2 to <12
(N=12)Age 12 to 16
(N=1)Total
(N=15)n (%) n (%) n (%) n (%) - * Grouped term includes Nasopharyngitis, Pharyngitis, Upper respiratory tract infection, Rhinitis, Viral upper respiratory tract infection, Rhinovirus infection, Viral pharyngitis, Rhinorrhea, and Oropharyngeal pain
Blood and lymphatic system disorders Lymphadenopathy 0 (0) 2 (17) 0 (0) 2 (13) Gastrointestinal disorders Diarrhea 1 (50) 3 (25) 1 (100) 5 (33) Constipation 0 (0) 4 (33) 0 (0) 4 (27) Vomiting 0 (0) 3 (25) 0 (0) 3 (20) Abdominal pain 0 (0) 2 (17) 0 (0) 2 (13) General disorders and administration site conditions Pyrexia 1 (50) 5 (42) 1 (100) 7 (47) Infections and infestations Upper respiratory tract infection* 1 (50) 6 (50) 0 (0) 7 (47) Gastroenteritis viral 0 (0) 2 (17) 0 (0) 2 (13) Tonsillitis 1 (50) 1 (8) 0 (0) 2 (13) Injury, poisoning and procedural complications Contusion 0 (0) 2 (17) 0 (0) 2 (13) Investigations Vitamin D decreased 0 (0) 2 (17) 1 (100) 3 (20) Metabolism and nutrition disorders Decreased appetite 1 (50) 1 (8) 0 (0) 2 (13) Iron deficiency 0 (0) 2 (17) 0 (0) 2 (13) Musculoskeletal and connective tissue disorders Myalgia 1 (50) 1 (8) 0 (0) 2 (13) Pain in extremity 0 (0) 2 (17) 0 (0) 2 (13) Nervous system disorders Headache 0 (0) 4 (33) 0 (0) 4 (27) Respiratory, thoracic and mediastinal disorders Cough 0 (0) 3 (25) 0 (0) 3 (20) Dyspnea 1 (50) 1 (8) 0 (0) 2 (13) Skin and subcutaneous tissue disorders Rash 1 (50) 2 (17) 0 (0) 3 (20) Vascular disorders Hypertension 1 (50) 3 (25) 0 (0) 4 (27) Hypotension 0 (0) 2 (17) 0 (0) 2 (13) Clinically relevant adverse reactions in <10% of patients include viral infection.
6.2 Immunogenicity
As with all therapeutic proteins, there is potential for immunogenicity. The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibodies) positivity in an assay may be influenced by several factors including assay methodology, sample handling, timing of sample collection, concomitant medications and underlying disease. For these reasons, comparison of the incidence of antibodies in the studies described below with the incidence of antibodies in other studies or to other ravulizumab products may be misleading.
The immunogenicity of ravulizumab-cwvz has been evaluated using an enzyme-linked immunosorbent assay (ELISA) for the detection of binding anti-ravulizumab-cwvz antibodies. For patients whose sera tested positive in the screening immunoassay, an in vitro biological assay was performed to detect neutralizing antibodies.
In clinical studies, treatment-emergent antibodies to ravulizumab-cwvz were detected in 1 of 206 (0.5%) patients with PNH and 1 of 71 (1.4%) patients with aHUS. No apparent correlation of antibody development to altered pharmacokinetic profile, clinical response, or adverse events was observed.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There are no available data on ULTOMIRIS use in pregnant women to inform a drug-associated risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes. There are risks to the mother and fetus associated with untreated PNH and aHUS in pregnancy (see Clinical Considerations). Animal studies using a mouse analogue of the ravulizumab-cwvz molecule (murine anti-C5 antibody) showed increased rates of developmental abnormalities and an increased rate of dead and moribund offspring at doses 0.8-2.2 times the human dose (see Data).
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively.
Clinical Considerations
Disease-associated maternal and/or fetal/neonatal risk
PNH in pregnancy is associated with adverse maternal outcomes, including worsening cytopenias, thrombotic events, infections, bleeding, miscarriages, and increased maternal mortality, and adverse fetal outcomes, including fetal death and premature delivery.
In pregnancy, aHUS is associated with adverse maternal outcomes, including preeclampsia and preterm delivery, and adverse fetal/neonatal outcomes, including intrauterine growth restriction (IUGR), fetal death and low birth weight.
Data
Animal Data
Animal reproduction studies were conducted in mice using doses of a murine anti-C5 antibody that approximated 1-2.2 times (loading dose) and 0.8-1.8 times (maintenance dose) the recommended human ULTOMIRIS dose, based on a body weight comparison. When animal exposure to the antibody occurred in the time period from before mating until early gestation, no decrease in fertility or reproductive performance was observed. When maternal exposure to the antibody occurred during organogenesis, two cases of retinal dysplasia and one case of umbilical hernia were observed among 230 offspring born to mothers exposed to the higher antibody dose; however, the exposure did not increase fetal loss or neonatal death. When maternal exposure to the antibody occurred in the time period from implantation through weaning, a higher number of male offspring became moribund or died (1/25 controls, 2/25 low dose group, 5/25 high dose group). Surviving offspring had normal development and reproductive function. Human IgG are known to cross the human placental barrier, and thus ULTOMIRIS may potentially cause terminal complement inhibition in the fetal circulation.
8.2 Lactation
Risk summary
There are no data on the presence of ravulizumab-cwvz in human milk, the effect on the breastfed child, or the effect on milk production. Since many medicinal products and immunoglobulins are secreted into human milk, and because of the potential for serious adverse reactions in a nursing child, breastfeeding should be discontinued during treatment and for 8 months after the final dose.
8.4 Pediatric Use
The safety and efficacy of ULTOMIRIS for the treatment of PNH in pediatric patients have not been established.
The safety and effectiveness of ULTOMIRIS for the treatment of aHUS have been established in pediatric patients aged one month and older. Use of ULTOMIRIS for this indication is supported by evidence from adequate and well-controlled studies in adults with additional pharmacokinetic, safety, and efficacy data in pediatric patients aged 10 months to <17 years. The safety and efficacy of ULTOMIRIS for the treatment of aHUS appear similar in pediatric and adult patients [see Adverse Reactions (6.1), and Clinical Studies (14.2)].
8.5 Geriatric Use
Clinical studies of ULTOMIRIS did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients.
-
11 DESCRIPTION
Ravulizumab-cwvz, a complement inhibitor, is a humanized monoclonal antibody (mAb) produced in Chinese hamster ovary (CHO) cells. Ravulizumab-cwvz consists of 2 identical 448 amino acid heavy chains and 2 identical 214 amino acid light chains and has a molecular weight of approximately 148 kDa. The constant regions of ravulizumab-cwvz include the human kappa light chain constant region, and the protein engineered "IgG2/4" heavy chain constant region.
The heavy chain CH1 domain, hinge region, and the first 5 amino acids of the CH2 domain match the human IgG2 amino acid sequence, residues 6 to 36 in the CH2 region (common to both human IgG2 and IgG4 amino acid sequences), while the remainder of the CH2 domain and the CH3 domain match the human IgG4 amino acid sequence. The heavy and light chain variable regions that form the human C5 binding site consist of human framework regions grafted to murine complementarity-determining regions.
ULTOMIRIS (ravulizumab-cwvz) injection is a sterile, clear to translucent, slight whitish color, preservative-free solution for intravenous use. Each single-dose vial contains 300 mg ravulizumab-cwvz at a concentration of 10 mg/mL with a pH of 7.0. Each mL also contains polysorbate 80 (0.2 mg) (vegetable origin), sodium chloride (8.77 mg), sodium phosphate dibasic (1.78 mg), sodium phosphate monobasic (0.46 mg), and Water for Injection, USP.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Ravulizumab-cwvz is a terminal complement inhibitor that specifically binds to the complement protein C5 with high affinity, thereby inhibiting its cleavage to C5a (the proinflammatory anaphylatoxin) and C5b (the initiating subunit of the terminal complement complex [C5b-9]) and preventing the generation of the terminal complement complex C5b9. ULTOMIRIS inhibits terminal complement-mediated intravascular hemolysis in patients with PNH and complement-mediated thrombotic microangiopathy (TMA) in patients with aHUS.
12.2 Pharmacodynamics
Complete inhibition of serum free C5 (concentration of less than 0.5 mcg/mL) was observed by the end of the first ULTOMIRIS infusion and sustained throughout the entire 26-week treatment period in all adult patients with PNH and in the majority (93%) of adult and pediatric patients with aHUS.
The extent and duration of the pharmacodynamic response in patients with PNH and aHUS were exposure-dependent for ULTOMIRIS. Free C5 levels of <0.5 mcg/mL were correlated with maximal intravascular hemolysis control and complete terminal complement inhibition in patients with PNH.
Complete terminal complement inhibition following initiation of ULTOMIRIS treatment led to normalization of serum LDH by week 4 in complement-inhibitor naïve patients with PNH, and maintained LDH normalization in patients previously treated with eculizumab with PNH [see Clinical Studies (14)].
12.3 Pharmacokinetics
Ravulizumab-cwvz pharmacokinetics increase proportionally over a dose range of 200 to 5400 mg. Ravulizumab-cwvz Cmax and Ctrough parameters are presented in Table 9 and Table 10.
Table 9: Mean (%CV) Pharmacokinetic Parameters of ULTOMIRIS in Patients with PNH who are Complement Inhibitor-Naïve and Patients Previously Treated with Eculizumab N Complement Inhibitor-Naïve
(ALXN1210-PNH-301)N Previously Treated with Eculizumab
(ALXN1210-PNH-302)LD = Loading Dose; MD = Maintenance Dose Cmax
(mcg/mL)LD 125 771 (21.5) 95 843 (24.1) MD 124 1,379 (20.0) 95 1,386 (19.4) Ctrough
(mcg/mL)LD 125 391 (35.0) 96 405 (29.9) MD 124 473 (33.4) 95 501 (28.6) Table 10: Mean (%CV) Pharmacokinetic Parameters of ULTOMIRIS in Patients with aHUS Pediatric Patients
(ALXN1210-aHUS-312)Adult Patients
(ALXN1210-aHUS-311)N < 20 kg
MD Q4WN ≥ 20 to < 40 kg
MD Q8WN ≥ 40 kg
MD Q8WLD = Loading Dose; MD = Maintenance Dose; Q4W = Every 4 Weeks; Q8W = Every 8 Weeks Cmax
(mcg/mL)LD 8 656 (38.1) 4 600 (17.3) 52 754 (35.2) MD 7 1,467 (37.8) 6 1,863 (15.3) 46 1,458 (17.6) Ctrough
(mcg/mL)LD 9 241 (52.1) 5 186 (16.5) 55 313 (33.9) MD 7 683 (46.1) 6 549 (34.1) 46 507 (42.5) Distribution
The mean (%CV) volume of distribution at steady state was 5.34 (17.2) L and 5.22 (35.4) L in patients with PNH and aHUS, respectively.
Elimination
The mean (%CV) terminal elimination half-life of ravulizumab-cwvz in patients with PNH and aHUS are 49.7 (18.0) days and 51.8 (31.3) days, respectively. The mean (%CV) clearance of ravulizumab-cwvz in patients with PNH and aHUS are 0.08 (29.5) L/day and 0.08 (53.3) L/day, respectively.
Specific Populations
No clinically significant differences in the pharmacokinetics of ravulizumab-cwvz were observed based on sex, age (10 months to 83 years), race, hepatic impairment, or any degree of renal impairment, including patients with proteinuria or receiving dialysis.
Body weight was a clinically significant covariate on the pharmacokinetics of ravulizumab-cwvz.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term animal carcinogenicity studies of ravulizumab-cwvz have not been conducted.
Genotoxicity studies have not been conducted with ravulizumab-cwvz.
Effects of ravulizumab-cwvz upon fertility have not been studied in animals. Intravenous injections of male and female mice with a murine anti-C5 antibody at up to 0.8-2.2 times the equivalent of the clinical dose of ULTOMIRIS had no adverse effects on mating or fertility.
-
14 CLINICAL STUDIES
14.1 Paroxysmal Nocturnal Hemoglobinuria (PNH)
The safety and efficacy of ULTOMIRIS in patients with PNH was assessed in two open-label, randomized, active-controlled, non-inferiority Phase 3 studies: PNH Study 301 and PNH Study 302. Study 301 enrolled patients with PNH who were complement inhibitor naïve and had active hemolysis. Study 302 enrolled patients with PNH who were clinically stable after having been treated with eculizumab for at least the past 6 months.
In both studies, ULTOMIRIS was dosed intravenously in accordance with the weight-based dosing described in Section 2.2 (4 infusions of ULTOMIRIS over 26 weeks) above. Eculizumab was administered on Days 1, 8, 15, and 22, followed by maintenance treatment with 900 mg of eculizumab on Day 29 and every 2 weeks (q2w) thereafter for a total of 26 weeks of treatment, according to the approved dosing regimen of eculizumab which was the standard-of-care for PNH at the time of studies.
Patients were vaccinated against meningococcal infection prior to or at the time of initiating treatment with ULTOMIRIS or eculizumab, or received prophylactic treatment with appropriate antibiotics until 2 weeks after vaccination. Prophylactic treatment with appropriate antibiotics beyond 2 weeks after vaccination was at the discretion of the provider.
Study in Complement-Inhibitor Naïve Patients with PNH
The Complement-Inhibitor Naïve Study [ALXN1210-PNH-301; NCT02946463] was a 26-week, multicenter, open-label, randomized, active-controlled, non-inferiority Phase 3 study conducted in 246 patients naïve to complement inhibitor treatment prior to study entry.
Patients with PNH with flow cytometric confirmation of at least 5% PNH cells were randomized 1:1 to either ULTOMIRIS or eculizumab. The mean total PNH granulocyte clone size was 85%, the mean total PNH monocyte clone size was 88%, and the mean total PNH RBC clone size was 39%. Ninety-eight percent of patients had a documented PNH-associated condition diagnosed prior to enrollment on the trial: anemia (85%), hemoglobinuria (63%), history of aplastic anemia (32%), history of renal failure (12%), myelodysplastic syndrome (5%), pregnancy complications (3%), and other (16%). Major baseline characteristics were balanced between treatment groups.
Table 11: Baseline Characteristics in the Complement-Inhibitor Naïve Study Parameter Statistics ULTOMIRIS
(N=125)Eculizumab
(N=121)- * MAVE = major adverse vascular event
Age (years) at first infusion in study Mean (SD) 44.8 (15.2) 46.2 (16.2) Min, max 18, 83 18, 86 Sex Male n (%) 65 (52.0) 69 (57.0) Race n (%) Asian 72 (57.6) 57 (47.1) White 43 (34.4) 51 (42.1) Black or African American 2 ( 1.6) 4 ( 3.3) American Indian or Alaska Native 1 ( 0.8) 1 ( 0.8) Other 4 ( 3.2) 4 ( 3.3) Not reported 3 ( 2.4) 4 ( 3.3) Pre-treatment LDH levels (U/L) Median 1513.5 1445.0 Min, max (378.0, 3759.5) (423.5, 3139.5) Units of pRBC/whole blood transfused within 12 months prior to first dose Median
Min, max6.0
(1, 44)6.0
(1, 32)Antithrombotic agents used within 28 days prior to first dose n (%) 22 (17.6) 22 (18.2) Patients with a history of MAVE * n (%) 17 (13.6) 25 (20.7) Patients with a history of thrombosis n (%) 17 (13.6) 20 (16.5) Patients with concomitant anticoagulant treatment n (%) 23 (18.4) 28 (23.1) Efficacy was established based upon transfusion avoidance and hemolysis as directly measured by normalization of LDH levels. Transfusion avoidance was defined as patients who did not receive a transfusion and not meet the protocol specified guidelines for transfusion from baseline up to Day 183. Supportive efficacy data included the percent change from baseline in LDH levels, the proportion of patients with breakthrough hemolysis defined as at least one new or worsening symptom or sign of intravascular hemolysis in the presence of elevated LDH ≥ 2 × ULN, after prior LDH reduction to < 1.5 × ULN on therapy and the proportion of patients with stabilized hemoglobin.
Non-inferiority of ULTOMIRIS to eculizumab was demonstrated across endpoints in the complement inhibitor naïve treatment population described in the table below.
Table 12: Efficacy Results in the Complement-Inhibitor Naïve Study ULTOMIRIS
(N=125)Eculizumab
(N=121)Statistic for Comparison Treatment Effect
(95% CI)Note: LDH = lactate dehydrogenase; CI = confidence interval For the transfusion avoidance endpoint, treatment differences (95% CIs) are based on estimated differences in percent with 95% CI. For the lactate dehydrogenase normalization endpoint, the adjusted prevalence within each treatment is displayed. Transfusion avoidance rate 73.6% 66.1% Difference in rate 6.8
(-4.66, 18.14)LDH normalization 53.6% 49.4% Odds ratio 1.19
(0.80, 1.77)LDH percent change -76.84% -76.02% Difference in % change from baseline -0.83
(-5.21, 3.56)Breakthrough hemolysis 4.0% 10.7% Difference in rate -6.7
(-14.21, 0.18)Hemoglobin stabilization 68.0% 64.5% Difference in rate 2.9
(-8.80, 14.64)There was no observable difference in fatigue between ULTOMIRIS and eculizumab after 26 weeks of treatment compared to baseline as measured by the FACIT-fatigue instrument. Patient-reported fatigue may be an under-or over-estimation, because patients were not blinded to treatment assignment.
Study in Eculizumab-Experienced Patients with PNH
The study in eculizumab-experienced patients [ALXN1210-PNH-302; NCT03056040] was a 26-week, multicenter, open-label, randomized, active-controlled, non-inferiority Phase 3 study conducted in 195 patients with PNH who were clinically stable after having been treated with eculizumab for at least the past 6 months.
Patients who demonstrated clinically stable disease after being treated with eculizumab for at least the prior 6 months were randomized 1:1 to either continue eculizumab or to switch to ULTOMIRIS. The mean total PNH granulocyte clone size was 83%, the mean total PNH monocyte clone size was 86%, and the mean total PNH RBC clone size was 60%. Ninety five percent of patients had a documented PNH-associated condition diagnosed prior to enrollment on the trial: anemia (67%), hematuria or hemoglobinuria (49%), history of aplastic anemia (37%), history of renal failure (9%), myelodysplastic syndrome (5%), pregnancy complication (7%), and other (14%). Major baseline characteristics were balanced between the two treatment groups.
Table 13: Baseline Characteristics in Eculizumab-Experienced Patients with PNH Parameter Statistics ULTOMIRIS
(N=97)Eculizumab
(N=98)- * MAVE = major adverse vascular event
Age (years) at first infusion in study Mean (SD) 46.6 (14.41) 48.8 (13.97) Min, max 18, 79 23, 77 Race n (%) White 50 (51.5) 61 (62.2) Asian 23 (23.7) 19 (19.4) Black or African American 5 (5.2) 3 (3.1) Other 2 (2.1) 1 (1.0) Not reported 13 (13.4) 13 (13.3) Unknown 3 (3.1) 1 (1.0) Multiple 1 (1.0) 0 Sex n (%) Male 50 (51.5) 48 (49.0) Pre-treatment LDH levels (U/L) Median 224.0 234.0 Min, max 135.0, 383.5 100.0, 365.5 Units of pRBC/whole blood transfused within 12 months prior to first dose Median 4.0 2.5 Min, max (1, 32) (2, 15) Antithrombotic agents used within 28 days prior to first dose n (%) 20 (20.6) 13 (13.3) Patients with a history of MAVE* n (%) 28 (28.9) 22 (22.4) Patients with a history of thrombosis n (%) 27 (27.8) 21 (21.4) Patients with concomitant anticoagulant treatment n (%) 22 (22.7) 16 (16.3) Efficacy was established based on hemolysis as measured by LDH percent change from baseline to Day 183 and supportive efficacy data was transfusion avoidance, proportion of patients with stabilized hemoglobin, and the proportion of patients with breakthrough hemolysis through Day 183.
Non-inferiority of ULTOMIRIS to eculizumab was demonstrated across endpoints in the patients with PNH previously treated with eculizumab described in the table below.
Table 14: Efficacy Results in the Eculizumab-Experienced Patients with PNH Eculizumab-Experienced Study ULTOMIRIS
N = 97Eculizumab
N = 98Statistic for Comparison Treatment Effect
(95% CI)Note: CI = confidence interval LDH Percent change -0.82% 8.4% Difference in % change from baseline 9.2
(-0.42, 18.8)Breakthrough hemolysis 0% 5.1% Difference in rate 5.1
(-8.9, 19.0)Transfusion avoidance 87.6 % 82.7% Difference in rate 5.5
(-4.3, 15.7)Hemoglobin stabilization 76.3% 75.5% Difference in rate 1.4
(-10.4, 13.3)There was no observable difference in fatigue between ULTOMIRIS and eculizumab after 26 weeks of treatment compared to baseline as measured by the FACIT-fatigue instrument. Patient-reported fatigue may be an under-or over-estimation, because patients were not blinded to treatment assignment.
14.2 Atypical Hemolytic Uremic Syndrome (aHUS)
The efficacy of ULTOMIRIS in patients with aHUS was assessed in 2 open-label, single-arm studies. Study ALXN1210-aHUS-311 enrolled adult patients who displayed signs of TMA. In order to qualify for enrollment, patients were required to have a platelet count ≤150 × 109/L, evidence of hemolysis such as an elevation in serum LDH, and serum creatinine above the upper limits of normal or required dialysis.
Study ALXN1210-aHUS-312 enrolled pediatric patients who displayed signs of TMA. In order to qualify for enrollment, patients were required to have a platelet count ≤150 × 109/L, evidence of hemolysis such as an elevation in serum LDH, and serum creatinine level ≥97.5% percentile at screening or required dialysis. In both studies, enrollment criteria excluded patients presenting with TMA due to a disintegrin and metalloproteinase with a thrombospondin type 1 motif, member 13 (ADAMTS13) deficiency, Shiga toxin Escherichia coli related hemolytic uremic syndrome (STEC-HUS) and genetic defect in cobalamin C metabolism. Patients with confirmed diagnosis of STEC-HUS after enrollment were excluded from the efficacy evaluation.
Study in Adult Patients with aHUS
The adult study [ALXN1210-aHUS-311; NCT02949128] was conducted in patients who were naïve to complement inhibitor treatment prior to study entry. The study consisted of a 26-week Initial Evaluation Period and patients were allowed to enter an extension period for up to 4.5 years.
A total of 56 patients with aHUS were evaluated for efficacy. Ninety-three percent of patients had extra-renal signs (cardiovascular, pulmonary, central nervous system, gastrointestinal, skin, skeletal muscle) or symptoms of aHUS at baseline. At baseline, 71.4% (n = 40) of patients had Stage 5 chronic kidney disease (CKD). Fourteen percent had a medical history of kidney transplant and 51.8% were on dialysis at study entry. Eight patients entered the study with evidence of TMA for > 3 days after childbirth (ie, postpartum).
Table 15 presents the demographics and baseline characteristics of the 56 adult patients enrolled in Study ALXN1210-aHUS-311 that constituted the Full Analysis Set.
Table 15: Demographics and Baseline Characteristics in Study ALXN1210-aHUS-311 Parameter Statistics ULTOMIRIS
(N=56)Note: Percentages are based on the total number of patients. Abbreviations: eGFR = estimated glomerular filtration rate; LDH = lactate dehydrogenase; max = maximum; min = minimum. - * Patients can have multiple races selected.
Age at time of first infusion (years) Mean (SD) 42.2 (14.98) Min, max 19.5, 76.6 Sex Female n (%) 37 (66.1) Race * n (%) White 29 (51.8) Asian 15 (26.8) Unknown 8 (14.3) Other 4 (7.1) Platelets (109/L) blood n 56 [normal range 130 to 400 × 109/L] Median (min,max) 95.25 (18, 473) Hemoglobin (g/L) blood n 56 [normal range 115 to 160 g/L (female), 130 to 175 g/L (male)] Median (min,max) 85.00 (60.5, 140) LDH (U/L) serum n 56 [normal range 120 to 246 U/L] Median (min,max) 508.00 (229.5, 3249) eGFR (mL/min/1.73 m2) n (%) 55 [normal range ≥ 60 mL/min/1.73 m2] Mean (SD) 15.86 (14.815) Median (min,max) 10.00 (4, 80) The efficacy evaluation was based on Complete TMA Response during the 26-week Initial Evaluation Period, as evidenced by normalization of hematological parameters (platelet count and LDH) and ≥ 25% improvement in serum creatinine from baseline. Patients had to meet each Complete TMA Response criteria at 2 separate assessments obtained at least 4 weeks (28 days) apart, and any measurement in between.
Complete TMA Response was observed in 30 of the 56 patients (54%) during the 26-week Initial Evaluation Period as shown in Table 16.
Table 16: Efficacy Results in aHUS during the 26-Week Initial Evaluation Period (ALXN1210-aHUS-311) Total Responder n Proportion (95% CI)* Abbreviations: CI = confidence interval; LDH = lactate dehydrogenase; TMA = thrombotic microangiopathy. - * 95% CIs for the proportion were based on exact confidence limits using the Clopper-Pearson method.
Complete TMA Response 56 30 0.54 (0.40, 0.67) Components of Complete TMA Response Platelet count normalization 56 47 0.84 (0.72, 0.92) LDH normalization 56 43 0.77 (0.64, 0.87) ≥25% improvement in serum creatinine from baseline 56 33 0.59 (0.45, 0.72) Hematologic normalization 56 41 0.73 (0.60, 0.84) One additional patient had a Complete TMA Response that was confirmed after the 26-week Initial Evaluation Period. Complete TMA Response was achieved at a median time of 86 days (range: 7 to 169 days). The median duration of Complete TMA Response was 7.97 months (range: 2.52 to 16.69 months). All responses were maintained through all available follow-up.
Other endpoints included platelet count change from baseline, dialysis requirement, and renal function as evaluated by estimated glomerular filtration rate (eGFR).
An increase in mean platelet count was observed after commencement of ULTOMIRIS, increasing from 118.52 × 109/L at baseline to 240.34 ×109/L at Day 8 and remaining above 227 × 109/L at all subsequent visits in the Initial Evaluation Period (26 weeks).
Renal function, as measured by eGFR, was improved or maintained during ULTOMIRIS therapy. The mean eGFR (+/- SD) increased from 15.86 (14.82) at baseline to 51.83 (39.16) by 26 weeks. In patients with Complete TMA Response, renal function continued to improve after the Complete TMA Response was achieved .
Seventeen of the 29 patients (59%) who required dialysis at study entry discontinued dialysis by the end of the available follow-up and 6 of 27 (22%) patients were off dialysis at baseline were on dialysis at last available follow-up.
Study in Pediatric Patients with aHUS
The Pediatric Study [ALXN1210-aHUS-312; NCT03131219] is a 26-week ongoing, multicenter, single-arm, study conducted in 16 pediatric patients.
A total of 14 eculizumab-naïve patients with documented diagnosis of aHUS were enrolled and included in this interim analysis. The median age at the time of first infusion was 5.2 years (range 0.9, 17.3 years). The overall mean weight at Baseline was 19.8 kg; half of the patients were in the baseline weight category ≥ 10 to < 20 kg. The majority of patients (71%) had pretreatment extra-renal signs (cardiovascular, pulmonary, central nervous system, gastrointestinal, skin, skeletal muscle) or symptoms of aHUS at baseline.
At baseline, 35.7% (n = 5) of patients had a CKD Stage 5. Seven percent had history of prior kidney transplant and 35.7% were on dialysis at study entry.
Table 17 presents the baseline characteristics of the pediatric patients enrolled in Study ALXN1210-aHUS-312.
Table 17: Demographics and Baseline Characteristics in Study ALXN1210-aHUS-312 Parameter Statistics ULTOMIRIS
(N = 14)Note: Percentages are based on the total number of patients. Abbreviations: eGFR = estimated glomerular filtration rate; LDH = lactate dehydrogenase; max = maximum; min = minimum. - * Patients can have multiple races selected.
Age at time of first infusion (years) category n (%) Birth to < 2 years 2 (14.3) 2 to < 6 years 7 (50.0) 6 to < 12 years 4 (28.6) 12 to < 18 years 1 (7.1) Sex n (%) Female 9 (64.3) Race* n (%) White 7 (50.0) Asian 4 (28.6) Black or African American 2 (14.3) American Indian or Alaskan Native 1 (7.1) Unknown 1 (7.1) Platelets (109/L) blood [normal range 229 to 533 × 109/L] Median (min, max) 64.00 (14, 125) Hemoglobin (g/L) blood [normal range 107 to 131 g/L] Median (min, max) 74.25 (32, 106) LDH (U/L) serum [normal range 165 to 395 U/L] Median (min, max) 2077.00 (772, 4985) eGFR (mL/min/1.73 m2) [normal range ≥ 60 mL/min/1.73 m2] Mean (SD) 28.4 (23.11) Median (min, max) 22.0 (10, 84) Efficacy evaluation was based upon Complete TMA Response during the 26-week Initial Evaluation Period, as evidenced by normalization of hematological parameters (platelet count and LDH) and ≥ 25% improvement in serum creatinine from baseline. Patients had to meet all Complete TMA Response criteria at 2 separate assessments obtained at least 4 weeks (28 days) apart, and any measurement in between.
Complete TMA Response was observed in 10 of the 14 patients (71%) during the 26-week Initial Evaluation Period as shown in Table 18.
Table 18: Efficacy Results in aHUS during the 26-Week Initial Evaluation Period (ALXN1210-aHUS-312) Total Responder n Proportion (95% CI)* Note: 1 patient withdrew from study after receiving 2 doses of ravulizumab. Abbreviations: CI = confidence interval; LDH = lactate dehydrogenase; TMA = thrombotic microangiopathy. - * 95% CIs for the proportion were based on on exact confidence limits using the Clopper-Pearson method.
Complete TMA Response 14 10 0.71 (0.42, 0.92) Components of Complete TMA Response Platelet count normalization 14 13 0.93 (0.66, 0.99) LDH normalization 14 12 0.86 (0.57, 0.98) ≥25% improvement in serum creatinine from baseline 14 11 0.79 (0.49, 0.95) Hematologic normalization 14 12 0.86 (0.57, 0.98) Complete TMA Response during the Initial Evaluation Period was achieved at a median time of 30 days (range:15 to 88 days). The median duration of Complete TMA Response was 5.08 months (range: 3.08 to 5.54 months). All responses were maintained through all available follow-up.
Other endpoints included platelet count change from baseline, dialysis requirement, and renal function as evaluated by eGFR.
An increase in mean platelet count was observed after commencement of ULTOMIRIS, increasing from 60.50 × 109/L at baseline to 296.67 × 109/L at Day 8 and remained above 296 × 109/L at all subsequent visits in the Initial Evaluation Period (26 weeks). The mean eGFR (+/- SD) increased from 28.4 (23.11) at baseline to 108.0 (63.21) by 26 weeks.
Four of the 5 patients who required dialysis at study entry were able to discontinue dialysis after the first month in study and for the duration of ULTOMIRIS treatment. No patient started dialysis during the study.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
ULTOMIRIS (ravulizumab-cwvz) injection is a clear to translucent, slight whitish color preservative-free, solution supplied as one 300 mg/30 mL (10 mg/mL) single-dose vial per carton. NDC: 25682-022-01.
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read FDA-approved patient labeling (Medication Guide).
Meningococcal Infection
Advise patients of the risk of meningococcal infection/sepsis. Inform patients that they are required to receive meningococcal vaccination at least 2 weeks prior to receiving the first dose of ULTOMIRIS, if they have not previously been vaccinated. They are required to be revaccinated according to current medical guidelines for meningococcal vaccines use while on ULTOMIRIS therapy. Inform patients that vaccination may not prevent meningococcal infection. Inform patients about the signs and symptoms of meningococcal infection/sepsis, and strongly advise patients to seek immediate medical attention if these signs or symptoms occur. These signs and symptoms are as follows:
- headache with nausea or vomiting
- headache and a fever
- headache with a stiff neck or stiff back
- fever
- fever and a rash
- confusion
- muscle aches with flu-like symptoms
- eyes sensitive to light
Inform patients that they will be given an ULTOMIRIS Patient Safety Card that they should carry with them at all times. This card describes symptoms which, if experienced, should prompt the patient to immediately seek medical evaluation.
Other Infections
Counsel patients of the increased risk of infections, particularly those due to encapsulated bacteria, especially Neisseria species. Advise patients of the need for vaccination against meningococcal infections according to current medical guidelines. Counsel patients about gonorrhea prevention and advise regular testing for patients at risk. Advise patients to report any new signs and symptoms of infection.
Discontinuation
Inform patients with PNH or aHUS that they may develop hemolysis or TMA, respectively, when ULTOMIRIS is discontinued and that they will be monitored by their healthcare professional for at least 16 weeks for PNH or at least 12 months for aHUS following ULTOMIRIS discontinuation.
Inform patients who discontinue ULTOMIRIS to keep the ULTOMIRIS Patient Safety Card with them for eight months after the last ULTOMIRIS dose, because the increased risk of meningococcal infection persists for several weeks following discontinuation of ULTOMIRIS.
-
SPL UNCLASSIFIED SECTION
Manufactured by:
Alexion Pharmaceuticals, Inc.
121 Seaport Boulevard
Boston, MA 02210 USAUS License Number 1743
This product, or its use, may be covered by one or more US patents, including US Patent No. 9,079,949; 9,107,861; 9,206,251; 9,371,377; 9,663,574; 9,803,007; and 10,227,400 in addition to others including patents pending.
ULTOMIRIS is a trademark of Alexion Pharmaceuticals, Inc.
© 2019 Alexion Pharmaceuticals, Inc.
-
MEDICATION GUIDE
This Medication Guide has been approved by the U.S. Food and Drug Administration. Revised: 10/2019 MEDICATION GUIDE
ULTOMIRIS® (ul-toe-meer-is)
(ravulizumab-cwvz)
injection, for intravenous useWhat is the most important information I should know about ULTOMIRIS? ULTOMIRIS is a medicine that affects your immune system. ULTOMIRIS can lower the ability of your immune system to fight infections. - ULTOMIRIS increases your chance of getting serious and life-threatening meningococcal infections. Meningococcal infections may quickly become life-threatening and cause death if not recognized and treated early.
- You must receive meningococcal vaccines at least 2 weeks before your first dose of ULTOMIRIS if you have not already had this vaccine.
- If your doctor decided that urgent treatment with ULTOMIRIS is needed, you should receive meningococcal vaccination as soon as possible.
- If you have not been vaccinated and ULTOMIRIS therapy must be initiated immediately, you should also receive 2 weeks of antibiotics with your vaccinations.
- If you had a meningococcal vaccine in the past, you might need additional vaccination before starting ULTOMIRIS. Your doctor will decide if you need additional meningococcal vaccination.
- Meningococcal vaccines reduce the risk of meningococcal infection but do not prevent all meningococcal infections. Call your doctor or get emergency medical care right away if you get any of these signs and symptoms of a meningococcal infection:
- headache with nausea or vomiting
- headache with a stiff neck or stiff back
- fever and a rash
- muscle aches with flu-like symptoms
- headache and fever
- fever
- confusion
- eyes sensitive to light
Your doctor will give you a Patient Safety Card about the risk of meningococcal infection. Carry it with you at all times during treatment and for 8 months after your last ULTOMIRIS dose. Your risk of meningococcal infection may continue for several months after your last dose of ULTOMIRIS. It is important to show this card to any doctor or nurse who treats you. This will help them diagnose and treat you quickly. ULTOMIRIS is only available through a program called the ULTOMIRIS REMS. Before you can receive ULTOMIRIS, your doctor must: - enroll in the ULTOMIRIS REMS program
- counsel you about the risk of meningococcal infection
- give you information about the symptoms of meningococcal infection
- give you a Patient Safety Card about your risk of meningococcal infection, as discussed above
- make sure that you are vaccinated with a meningococcal vaccine
ULTOMIRIS may also increase the risk of other types of serious infections. - People who take ULTOMIRIS may have an increased risk of getting infections caused by Streptococcus pneumoniae and Haemophilus influenzae.
- Certain people may also have an increased risk of gonorrhea infection. Talk to your doctor to find out if you are at risk for gonorrhea infection, about gonorrhea prevention, and regular testing.
Call your doctor right away if you have any new signs or symptoms of infection. What is ULTOMIRIS? ULTOMIRIS is a prescription medicine called a monoclonal antibody. ULTOMIRIS is used to treat: - adults with a disease called Paroxysmal Nocturnal Hemoglobinuria (PNH).
- adults and children 1 month of age and older with a disease called atypical hemolytic uremic syndrome (aHUS).
ULTOMIRIS is not used in treating people with Shiga toxin E. coli related hemolytic uremic syndrome (STEC-HUS).
It is not known if ULTOMIRIS is safe and effective in children with PNH. It is not known if ULTOMIRIS is safe and effective in children younger than 1 month of age. Who should not receive ULTOMIRIS? Do not receive ULTOMIRIS if you: - have a meningococcal infection
- have not been vaccinated against meningococcal infection unless your doctor decides that urgent treatment with ULTOMIRIS is needed. See "What is the most important information I should know about ULTOMIRIS."
Before you receive ULTOMIRIS, tell your doctor about all of your medical conditions, including if you: - have an infection or fever
- are pregnant or plan to become pregnant. It is not known if ULTOMIRIS will harm your unborn baby.
- are breastfeeding or plan to breastfeed. It is not known if ULTOMIRIS passes into your breast milk. You should not breastfeed during treatment and for 8 months after your final dose of ULTOMIRIS.
Tell your doctor about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. ULTOMIRIS and other medicines can affect each other causing side effects. Know the medicines you take and the vaccines you receive. Keep a list of them to show your doctor and pharmacist when you get a new medicine. How should I receive ULTOMIRIS? - ULTOMIRIS is given through a vein by intravenous (I.V.) infusion usually over about 2 hours in adults and up to 4 hours in children.
If you are an adult with PNH or aHUS, you will usually receive: - a starting dose of ULTOMIRIS as an infusion by your doctor, and then
- 2 weeks later, you will start to receive an infusion of ULTOMIRIS every 8 weeks.
Children 1 month of age and older with aHUS will usually receive: - a starting dose of ULTOMIRIS as an infusion by your doctor, and then
- your doctor will decide how often your child will receive ULTOMIRIS, either every 4 weeks or every 8 weeks, depending on their weight, starting 2 weeks after the starting dose.
Your doctor will decide how long you need to take ULTOMIRIS for your aHUS. - If you are changing treatment from SOLIRIS to ULTOMIRIS, you should receive your starting dose of ULTOMIRIS 2 weeks after your last dose of SOLIRIS.
- After each infusion, you should be monitored for at least 1 hour for infusion reactions. See "What are the possible side effects of ULTOMIRIS?"
-
If you have PNH and you stop receiving ULTOMIRIS, your doctor will need to monitor you closely for at least 16 weeks after you stop ULTOMIRIS. Stopping ULTOMIRIS may cause breakdown of your red blood cells due to PNH.
Symptoms or problems that can happen due to red blood cell breakdown include:
- drop in your red blood cell count
- tiredness
- blood in your urine
- stomach-area (abdomen) pain
- shortness of breath
- blood clots
- trouble swallowing
- erectile dysfunction (ED) in males
-
If you have aHUS, your doctor will need to monitor you closely for at least 12 months after stopping treatment for signs of worsening aHUS or problems related to a type of abnormal clotting and breakdown of your red blood cells called thrombotic microangiopathy (TMA).
Symptoms or problems that can happen with TMA may include:
- confusion or loss of consciousness
- seizures
- chest pain (angina)
- difficulty breathing
- blood clots or stroke
If you miss an ULTOMIRIS infusion, call your doctor right away. What are the possible side effects of ULTOMIRIS? ULTOMIRIS can cause serious side effects including: - See "What is the most important information I should know about ULTOMIRIS?"
-
Infusion reactions. Infusion reactions may happen during your ULTOMIRIS infusion. Symptoms of an infusion reaction with ULTOMIRIS may include lower back pain, pain with the infusion, feeling faint or discomfort in your arms or legs. Tell your doctor or nurse right away if you develop these symptoms, or any other symptoms during your ULTOMIRIS infusion that may mean you are having a serious infusion reaction, including:
- chest pain
- trouble breathing or shortness of breath
- swelling of your face, tongue, or throat
- feel faint or pass out
Your doctor will treat your symptoms as needed. The most common side effects of ULTOMIRIS in people treated for PNH are upper respiratory infection and headache. The most common side effects of ULTOMIRIS in people with aHUS are: - upper respiratory infections
- diarrhea
- nausea
- vomiting
- headache
- high blood pressure
- fever
Tell your doctor about any side effect that bothers you or that does not go away. These are not all the possible side effects of ULTOMIRIS. For more information, ask your doctor or pharmacist. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. General information about the safe and effective use of ULTOMIRIS. Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. You can ask your pharmacist or doctor for information about ULTOMIRIS that is written for health professionals. What are the ingredients in ULTOMIRIS? Active ingredient: ravulizumab-cwvz Inactive ingredients: polysorbate 80 (vegetable origin), sodium chloride, sodium phosphate dibasic, sodium phosphate monobasic, and Water for Injection Manufactured by Alexion Pharmaceuticals, Inc., 121 Seaport Boulevard, Boston, MA 02210 USA. U.S. License Number 1743 For more information, go to www.ULTOMIRIS.com or call: 1-888-765-4747 -
PRINCIPAL DISPLAY PANEL - 30 mL Vial Carton
NDC: 25682-022-01
ULTOMIRIS®
(ravulizumab-cwvz)
injection300 mg/30 mL
(10 mg/mL)For Intravenous Infusion
Dilute with 0.9% Sodium Chloride
Injection prior to use.Rx only
30 mL Single-dose vial
Discard Unused PortionAttention: Dispense the enclosed
Medication Guide to each patient.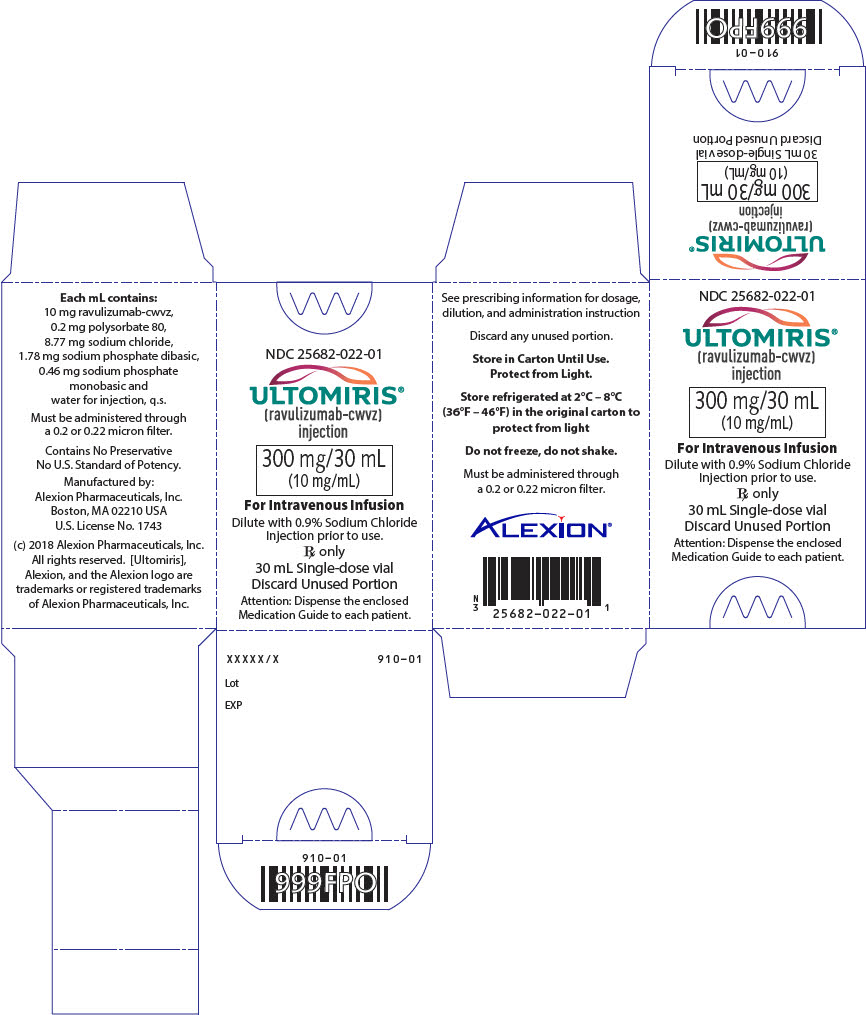
-
INGREDIENTS AND APPEARANCE
ULTOMIRIS
ravulizumab solution, concentrateProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 25682-022 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ravulizumab (UNII: C3VX249T6L) (ravulizumab - UNII:C3VX249T6L) ravulizumab 300 mg in 30 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 25682-022-01 1 in 1 CARTON 12/21/2018 1 30 mL in 1 VIAL, GLASS; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA761108 12/21/2018 Labeler - Alexion Pharmaceuticals Inc. (789359510)
Trademark Results [ULTOMIRIS]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 ULTOMIRIS 87713118 5716901 Live/Registered |
Alexion Pharmaceuticals, Inc. 2017-12-08 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.