HYCAMTIN- topotecan capsule
HYCAMTIN by
Drug Labeling and Warnings
HYCAMTIN by is a Prescription medication manufactured, distributed, or labeled by Novartis Pharmaceuticals Corporation. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use HYCAMTIN CAPSULES safely and effectively. See full prescribing information for HYCAMTIN CAPSULES.
HYCAMTIN® (topotecan) capsules, for oral use
Initial U.S. Approval: 1996WARNING: MYELOSUPPRESSION
See full prescribing information for complete boxed warning.
HYCAMTIN can cause severe myelosuppression. Administer first cycle only to patients with baseline neutrophil counts of greater than or equal to 1,500/mm3 and platelet counts of greater than or equal to 100,000/mm3. Monitor blood cell counts (2.2, 5.1).
INDICATIONS AND USAGE
HYCAMTIN capsules is a topoisomerase inhibitor indicated for treatment of patients with relapsed small cell lung cancer (SCLC). (1)
DOSAGE AND ADMINISTRATION
DOSAGE FORMS AND STRENGTHS
Capsules: 0.25 mg or 1 mg (3)
CONTRAINDICATIONS
- History of severe hypersensitivity reactions to topotecan (4)
WARNINGS AND PRECAUTIONS
- Diarrhea: Severe diarrhea can occur. Withhold and reduce dose as recommended. (2.2, 5.2)
- Interstitial Lung Disease (ILD): Fatal cases have occurred. Permanently discontinue if confirmed ILD. (5.3)
- Embryo-Fetal Toxicity: Can cause fetal harm. Advise patients of potential risk to the fetus and to use effective contraception. (5.4, 8.1, 8.3)
ADVERSE REACTIONS
- The most common Grade 3 or 4 hematologic adverse reactions (incidence > 20%) were neutropenia, anemia, and thrombocytopenia.
- The most common (incidence > 10%) non-hematologic adverse reactions (all Grades) were nausea, diarrhea, vomiting, alopecia, fatigue, and anorexia. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Novartis Pharmaceuticals Corporation at 1-888-669-6682 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
USE IN SPECIFIC POPULATIONS
- Lactation: Advise not to breastfeed. (8.2)
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 9/2018
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: MYELOSUPPRESSION
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage
2.2 Dosage Modifications for Adverse Reactions
2.3 Dosage Modifications for Renal Impairment
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Myelosuppression
5.2 Diarrhea
5.3 Interstitial Lung Disease
5.4 Embryo-Fetal Toxicity
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Effect of Other Drugs on HYCAMTIN
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Small Cell Lung Cancer (SCLC)
15 REFERENCES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: MYELOSUPPRESSION
HYCAMTIN can cause severe myelosuppression. Administer first cycle only to patients with baseline neutrophil counts of greater than or equal to 1,500/mm3 and platelet counts greater than or equal to 100,000/mm3. Monitor blood cell counts [see Warnings and Precautions (5.1)].
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage
The recommended dosage of HYCAMTIN capsules is 2.3 mg/m2/day orally once daily, with or without food, for 5 consecutive days, starting on Day 1 of a 21-day cycle. Round the dose to the nearest 0.25 mg and prescribe the minimum number of 1 mg and 0.25 mg capsules. Prescribe the same number of capsules for each of the 5 dosing days.
Swallow capsules whole. Do not chew, crush, or divide the capsules.
If a dose of HYCAMTIN capsules is missed or vomiting occurs after taking a dose, do not administer an additional dose and take the next dose at the scheduled time.
2.2 Dosage Modifications for Adverse Reactions
Diarrhea
Do not administer HYCAMTIN capsules to patients with Grade 3 or 4 diarrhea. After recovery to Grade 1 or less, reduce the dose by 0.4 mg/m2/day for subsequent courses [see Warnings and Precautions (5.2)].
Hematologic
Do not administer subsequent cycles of HYCAMTIN capsules until neutrophils recover to greater than 1,000/mm3, platelets recover to greater than 100,000/mm3, and hemoglobin levels recover to greater than or equal to 9 g/dL (with transfusion if necessary) [see Warnings and Precautions (5.1)].
Reduce dose by 0.4 mg/m2/day for:
- neutrophil counts of less than 500/mm3 associated with fever or infection or lasting for 7 days or more;
- neutrophil counts of 500 to 1,000/mm3 lasting beyond day 21 of the treatment course; or
- platelet counts less than 25,000/mm3.
2.3 Dosage Modifications for Renal Impairment
Reduce the dose of HYCAMTIN capsules in patients with the following creatinine clearance (CLcr), calculated with the Cockcroft-Gault method using ideal body weight.
- CLcr 30 to 49 mL/min: Administer 1.5 mg/m2/day.
- CLcr less than 30 mL/min: Administer 0.6 mg/m2/day.
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Myelosuppression
HYCAMTIN can cause severe myelosuppression. The following safety data are based on an integrated safety database from four trials in patients with lung cancer (N = 682) who received HYCAMTIN capsules at a dose of 2.3 mg/m2 orally once daily for 5 consecutive days, starting on Day 1 of a 21-day cycle.
The median day for neutrophil and platelet nadirs occurred on Day 15. Grade 4 neutropenia occurred in 32% of the 682 patients, with a median duration of 7 days. Grade 4 neutropenia most commonly occurred during cycle 1 (20% of patients). Clinical sequelae of neutropenia included infection (17%), febrile neutropenia (4%), sepsis (2%), and septic death (1%). Grade 4 thrombocytopenia occurred in 6%, with a median duration of 3 days. Grade 3 or 4 anemia occurred in 25%.
HYCAMTIN can cause fatal typhlitis (neutropenic enterocolitis). Consider the possibility of typhlitis in patients presenting with fever, neutropenia, and abdominal pain.
Administer the first cycle of HYCAMTIN capsules only to patients with a baseline neutrophil count greater than or equal to 1,500/mm3 and a platelet count greater than or equal to 100,000/mm3. Monitor blood cell counts frequently during treatment. Withhold and reduce dose of HYCAMTIN capsules based on neutrophil counts, platelet counts and hemoglobin levels [see Dosage and Administration (2.2)].
5.2 Diarrhea
Diarrhea, including severe and life-threatening diarrhea requiring hospitalization, can occur with HYCAMTIN capsules. Diarrhea can occur at the same time as drug-induced neutropenia and its sequelae. In the 682 patients who received HYCAMTIN capsules in the four lung cancer trials, the incidence of diarrhea caused by HYCAMTIN capsules was 22%, including Grade 3 (4%) and Grade 4 (0.4%). The incidence of Grade 3 or 4 diarrhea proximate (within 5 days) to Grade 3 or 4 neutropenia was 5%. The median time to onset of Grade 2 to 4 diarrhea was 9 days in the group receiving HYCAMTIN capsules.
Monitor patients for diarrhea and treat with antidiarrheals at the first sign of diarrhea. Withhold and dose reduce as recommended based on severity [see Dosage and Administration (2.2)].
5.3 Interstitial Lung Disease
Interstitial lung disease (ILD), including fatalities, can occur with HYCAMTIN. Underlying risk factors include history of ILD, pulmonary fibrosis, lung cancer, thoracic radiation, and use of pneumotoxic drugs or colony stimulating factors.
Monitor for pulmonary symptoms indicative of ILD. Permanently discontinue HYCAMTIN capsules if ILD is confirmed.
5.4 Embryo-Fetal Toxicity
Based on animal data, HYCAMTIN can cause fetal harm when administered to a pregnant woman. Topotecan caused embryolethality, fetotoxicity, and teratogenicity in rats and rabbits when administered during organogenesis. Advise women of the potential risk to fetus. Advise females of reproductive potential to use effective contraception during treatment and for at least 6 months after the last dose of HYCAMTIN capsules. Advise males with a female partner of reproductive potential to use effective contraception during treatment with HYCAMTIN capsules and for 3 months after the last dose [see Use in Specific Populations (8.1, 8.3), Nonclincial Toxicology (13.1)].
-
6 ADVERSE REACTIONS
The following serious adverse reactions are described elsewhere in the labeling:
- Myelosuppression [see Warnings and Precautions (5.1)]
- Diarrhea [see Warnings and Precautions (5.2)]
- Interstitial Lung Disease (ILD) [see Warnings and Precautions (5.3)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared with rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The data in the Warnings and Precautions and below reflects exposure to HYCAMTIN capsules in 682 patients with recurrent lung cancer enrolled in four randomized, open label trials, including 275 patients with small lung cell lung cancer (SCLC) (Studies 478, 065 and 396), and 407 patients with non-small cell lung cancer (NSCLC) (Study 387), who received at least one dose of HYCAMTIN capsules. Patients in these trials had advanced lung cancer and received prior chemotherapy in the first-line setting. Patients received HYCAMTIN capsules 2.3 mg/m2 orally once daily for 5 consecutive days, starting on Day 1 of a 21-day cycle. The median number of cycles was 3 (range: 1 to 20).
The safety of HYCAMTIN capsules was evaluated in a randomized trial (Study 478) conducted in 70 patients with recurrent SCLC [see Clinical Studies (14)].
In the 682 patients who received HYCAMTIN capsules in the four lung cancer trials, 39 deaths (6%) occurred within 30 days after the last dose for a reason other than progressive disease: 13 due to hematologic toxicity, 5 due to non-hematologic toxicity (2 from diarrhea), and 21 due to other causes.
Table 1 describes the hematologic and non-hematologic adverse reactions that occurred in greater than 5% of patients treated with HYCAMTIN capsules in these trials.
Table 1. Adverse Reactions Occurring in Greater than or Equal to 5% of Patients With Lung Cancer aAdverse reactions were graded using National Cancer Institute (NCI) Common Toxicity Criteria (CTC) Version 2.0. Adverse Reactionsa
HYCAMTIN Capsules With Best
Supportive Care
(Study 478)HYCAMTIN Capsules
Lung Cancer Population
(Studies 478, 065, 396 and 387)N = 70
N = 682
All Grades
(%)
Grade 3
(%)
Grade 4
(%)
All Grades
(%)
Grade 3
(%)
Grade 4
(%)
Hematologic
Anemia
94
15
10
98
18
7
Neutropenia
91
28
33
83
24
32
Thrombocytopenia
81
30
7
81
29
6
Non-hematologic
Nausea
27
1
0
33
3
0
Vomiting
19
1
0
21
3
0.4
Diarrhea
14
4
1
22
4
0.4
Fatigue
11
0
0
19
4
0.1
Alopecia
10
0
0
20
0.1
0
Pyrexia
7
1
0
5
1
1
Anorexia
7
0
0
14
2
0
Asthenia
3
0
0
7
2
0
6.2 Postmarketing Experience
The following reactions have been identified during post approval use of HYCAMTIN. Because these reactions are reported voluntarily from a population of unknown size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Gastrointestinal: Gastrointestinal perforation
General and Administration Site Conditions: Mucosal inflammation
Hypersensitivity: Allergic manifestations, anaphylactoid reactions, angioedema
-
7 DRUG INTERACTIONS
7.1 Effect of Other Drugs on HYCAMTIN
P-glycoprotein or Breast Cancer Resistance Protein Inhibitor
Concomitant use of a P-glycoprotein (P-gp) or breast cancer resistance protein (BCRP) inhibitor increases topotecan AUC [see Clinical Pharmacology (12.3)], which may increase the risk of adverse reactions. Avoid concomitant use HYCAMTIN capsules with P-gp inhibitors or BCRP inhibitors.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Based on animal data and its mechanism of action, HYCAMTIN can cause fetal harm when administered to a pregnant woman. There are no available clinical data on the use of HYCAMTIN in pregnancy. Topotecan caused embryolethality, fetotoxicity, and teratogenicity in rats and rabbits when administered during organogenesis at doses similar to the clinical dose (see Data). Advise pregnant women of the potential risk to a fetus.
In the U.S. general population, the background risk of major birth defects is 2% to 4% and of miscarriage is 15% to 20% of clinically recognized pregnancies.
Data
Animal Data
In rabbits, an intravenous dose of 0.10 mg/kg/day [about equal to the 1.5 mg/m2 clinical intravenous dose based on body surface area (BSA)] given on days 6 through 20 of gestation caused maternal toxicity, embryolethality, and reduced fetal body weight. In the rat, an intravenous dose of 0.23 mg/kg/day (about equal to the 1.5 mg/m2 clinical intravenous dose based on BSA) given for 14 days before mating through gestation day 6 caused fetal resorption, microphthalmia, pre-implant loss, and mild maternal toxicity. Administration of an intravenous dose of 0.10 mg/kg/day (about half the 1.5 mg/m2 clinical intravenous dose based on BSA) to rats on days 6 through 17 of gestation caused an increase in post-implantation mortality. This dose also caused an increase in total fetal malformations. The most frequent malformations were of the eye (microphthalmia, anophthalmia, rosette formation of the retina, coloboma of the retina, ectopic orbit), brain (dilated lateral and third ventricles), skull, and vertebrae.
8.2 Lactation
Risk Summary
There are no data on the presence of topotecan or its metabolites in human milk, or their effects on the breastfed infant or milk production. Lactating rats excrete high concentrations of topotecan into milk (see Data). Because of the potential for serious adverse reactions in breastfed infants, advise women not to breastfeed during treatment with HYCAMTIN and for 1 week after the last dose.
Data
Following intravenous administration of topotecan to lactating rats at a dose of 4.72 mg/m2 (about twice the 1.5 mg/m2 clinical intravenous dose based on BSA), topotecan was excreted into milk at concentrations up to 48-fold higher than those in plasma.
8.3 Females and Males of Reproductive Potential
Pregnancy Testing
Verify pregnancy status of females of reproductive potential prior to initiating HYCAMTIN capsules [see Use in Specific Populations (8.1)].
Contraception
HYCAMTIN can cause fetal harm when administered to a pregnant woman [see Use in Specific Populations (8.1)].
Females
Advise female patients of reproductive potential to use effective contraception during treatment with HYCAMTIN capsules and for 6 months after the last dose.
Males
HYCAMTIN capsules may damage spermatozoa, resulting in possible genetic and fetal abnormalities. Advise males with a female partner of reproductive potential to use effective contraception during treatment with HYCAMTIN capsules and for 3 months after the last dose [see Nonclinical Toxicology (13.1)].
Infertility
Females
HYCAMTIN can have both acute and long-term effects on fertility [see Nonclinical Toxicology (13.1)].
Males
Effects on spermatogenesis have occurred in animals administered topotecan [see Nonclinical Toxicology (13.1)].
8.5 Geriatric Use
Of the 682 patients with lung cancer who received HYCAMTIN capsules in the four clinical trials, 33% were aged 65 years and older, while 4.8% were aged 75 years and older. Treatment-related diarrhea was more frequent in patients aged greater than or equal to 65 years (28%) compared with those younger than 65 years (19%) [see Warnings and Precautions (5.2), Adverse Reactions (6.1)]. No overall differences in effectiveness were observed between patients 65 years and older and younger patients.
-
10 OVERDOSAGE
Overdoses (up to 5-fold of the prescribed dose) have occurred in patients receiving HYCAMTIN capsules. The primary complication of overdosage is myelosuppression. Mucositis have occurred with overdosages. If an overdose is suspected, monitor the patient closely for myelosuppression and institute supportive-care measures as appropriate.
-
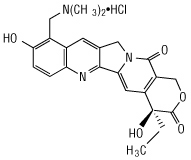
11 DESCRIPTION
Topotecan is a topoisomerase inhibitor. The chemical name for topotecan hydrochloride is (S)-10-[(dimethylamino)methyl]-4-ethyl-4,9-dihydroxy-1H-pyrano[3',4':6,7] indolizino [1,2-b]quinoline-3,14-(4H,12H)-dione monohydrochloride. The molecular formula is C23H23N3O5HCl and the molecular weight is 457.9 g/mol. It is soluble in water and melts with decomposition at 213°C to 218°C.
Topotecan hydrochloride has the following structural formula:
HYCAMTIN capsules, contain topotecan hydrochloride, the content of which is expressed as topotecan free base. Each 0.25 mg and 1 mg capsule contain topotecan hydrochloride equivalent to 0.25 mg and 1 mg topotecan free-base, respectively. The excipients are gelatin, glyceryl monostearate, hydrogenated vegetable oil, and titanium dioxide. The capsules are imprinted with edible black ink. The 1 mg capsules also contain red iron oxide.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Topoisomerase I relieves torsional strain in DNA by inducing reversible single-strand breaks. Topotecan binds to the topoisomerase I-DNA complex and prevents re-ligation of these single-strand breaks. The cytotoxicity of topotecan is thought to be due to double-strand DNA damage produced during DNA synthesis, when replication enzymes interact with the ternary complex formed by topotecan, topoisomerase I, and DNA. Mammalian cells cannot efficiently repair these double-strand breaks.
12.3 Pharmacokinetics
Following administration of HYCAMTIN capsules at doses of 1.2 to 3.1 mg/m2 (0.52 to 1.35 times the recommended dose) administered daily for 5 days, the area under the curve (AUC) increased proportionally with dose.
Absorption
The time to the peak plasma concentrations is between 1 to 2 hours following oral administration. The oral bioavailability of topotecan is approximately 40%.
Food Effect
Following a high-fat meal, the AUC was similar in the fed and fasted states, while Tmax was delayed from 1.5 to 3 hours for topotecan lactone and from 3 to 4 hours for total topotecan.
Distribution
Protein binding of topotecan is approximately 35%.
Elimination
The mean terminal half-life (t½) of topotecan is 3 to 6 hours following oral administration.
Metabolism
Topotecan undergoes a reversible pH-dependent hydrolysis of a pharmacologically active lactone moiety. At pH less than or equal to 4, the lactone is exclusively present, whereas the ring-opened hydroxy-acid form predominates at physiologic pH. The mean metabolite: parent AUC ratio was less than 10% for total topotecan and topotecan lactone.
Excretion
The overall recovery of drug-related material following 5 daily doses of topotecan was 57% of the administered oral dose. In the urine, 20% of the orally administered dose was excreted as total topotecan and 2% was excreted as N-desmethyl topotecan. Fecal elimination of total topotecan accounted for 33%, while fecal elimination of the active metabolite N-desmethyl topotecan accounted for 1.5%. Overall, the N-desmethyl metabolite contributed a mean of less than 6% (range: 4% to 8%) of the total drug-related material accounted for in the urine and feces.
Specific Populations
No clinically significant differences in the pharmacokinetics of topotecan were observed based on age, sex, or hepatic impairment following oral administration.
Racial and Ethnic Groups
In patients with creatinine clearance (CLcr) greater than 80 mL/min, the dose-normalized AUCinf to topotecan lactone and total topotecan each were approximately 30% higher in Asians compared to Whites
Patients with Renal Impairment
The mean dose-normalized for total topotecan and topotecan lactone AUCinf increased in advanced cancer patients with renal impairment compared to patients with CLcr greater than 80 mL/min as presented in Table 2 [see Dosage and Administration (2.3)]. Prior platinum-based chemotherapy had no effect on the systemic exposure to both total topotecan and topotecan lactone in patients with CLcr greater than 80 mL/min.
Table 2. AUCinf Increases Compared to Normal Renal Function Renal Impairment
Geometric Mean Dose-Normalized AUCinf
Total Topotecan
Topotecan Lactone
Whites
CLcr 50-79 mL/min
CLcr 30-49 mL/min
< 30 mL/min70%
108%
227%34%
80%
114%Asians
CLcr 50-79 mL/min
CLcr 30-49 mL/min
< 30 mL/min26%
153%
331%34%
121%
247%Drug Interaction Studies
Clinical Studies
Effect of P-glycoprotein (P-gp) and Breast Cancer Resistance Protein (BCRP) Inhibitors
Following coadministration of escalating doses of a dual inhibitor of BCRP and P-gp, the AUCinf of topotecan lactone and total topotecan increased approximately 2.5-fold compared to topotecan alone [see Drug Interactions (7.1)].
Coadministration of single oral dose of cyclosporine A (15 mg/kg), an inhibitor of P-gp, multidrug-resistance-associated protein (MRP-1) and CYP3A4, within 4 hours of oral topotecan increased the dose-normalized AUC0-24h of topotecan lactone and total topotecan 2- to 3-fold compared to topotecan alone [see Drug Interactions (7.1)].
Effect of Gastric Acid Reducing Agents
No clinically significant changes in the pharmacokinetics of oral topotecan were observed when coadministered with ranitidine, a histamine-2 receptor antagonist.
In Vitro Studies
Topotecan does not inhibit CYP1A2, CYP2A6, CYP2C8/9, CYP2C19, CYP2D6, CYP2E, CYP3A, CYP4A, or dihydropyrimidine dehydrogenase.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenicity testing of topotecan has not been done. Nevertheless, topotecan is known to be genotoxic to mammalian cells and is a probable carcinogen. Topotecan was mutagenic to L5178Y mouse lymphoma cells and clastogenic to cultured human lymphocytes with and without metabolic activation. It was also clastogenic to mouse bone marrow. Topotecan did not cause mutations in bacterial cells.
Topotecan given to female rats prior to mating at an intravenous dose of 1.4 mg/m2 [(about 0.6 times the 2.3 mg/m2 oral clinical dose based on body surface area (BSA)] caused superovulation possibly related to inhibition of follicular atresia. This dose given to pregnant female rats also caused increased pre-implantation loss. Studies in dogs given an intravenous dose of 0.4 mg/m2 (about 0.2 times the 2.3 mg/m2 oral clinical dose based on BSA) of topotecan daily for a month suggest that treatment may cause an increase in the incidence of multinucleated spermatogonial giant cells in the testes.
-
14 CLINICAL STUDIES
14.1 Small Cell Lung Cancer (SCLC)
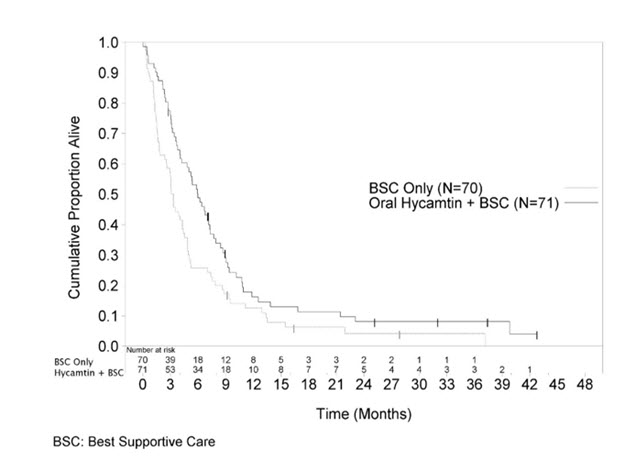
The efficacy of HYCAMTIN capsules was studied in 141 patients with relapsed SCLC in a randomized, controlled, open-label trial (Study 478). The patients were prior responders (complete or partial) to first-line chemotherapy, were not considered candidates for standard intravenous chemotherapy and had relapsed at least 45 days from the end of first-line chemotherapy. Patients were randomized 1:1 to HYCAMTIN capsules (2.3 mg/m2 orally once daily for 5 consecutive days, starting on Day 1 of a 21-day cycle) with best supportive care (BSC) or BSC alone. The major efficacy outcome measure was overall survival (OS).
Patients randomized to HYCAMTIN capsules with BSC received a median of 4 courses (range: 1 to 10) and maintained a median dose intensity of 3.77 mg/m2/week. The median patient age in patients receiving HYCAMTIN capsules with BSC and BSC alone was 60 years and 58 years, while the percentage of patients aged greater than or equal to 65 years was 34% and 29%, respectively. The majority of patients were White (99%) and male (73%). In the HYCAMTIN capsules with BSC arm, 68% of patients had extensive disease and 28% had liver metastasis. In the BSC alone arm, 61% had extensive disease and 20% had liver metastases. Eighty percent of patients receiving HYCAMTIN capsules with BSC previously received carboplatin or cisplatin and 77% of patients in the BSC alone arm received prior carboplatin or cisplatin. In the arm receiving HYCAMTIN capsules with BSC, 18% of patients had prior carboplatin and 62% had prior cisplatin. In the BSC-alone arm, 26% of patients had prior carboplatin and 51% had prior cisplatin.
The arm receiving HYCAMTIN capsules with BSC showed a statistically significant improvement in OS compared with the BSC-alone arm (Log-rank P = 0.0104). Efficacy results are shown in Table 3 and Figure 1.
Table 3. Efficacy Results in Small Cell Lung Cancer in Study 478 Abbreviations: BSC, Best Supportive Care; N, Total number of patients randomized; CI, Confidence Interval. Parameters
Treatment Group
HYCAMTIN Capsules with BSC
BSC
(N = 71)
(N = 70)
Median Overall Survival (months) (95% CI)
6.0 (4.2, 7.3)
3.2 (2.6, 4.3)
Hazard ratio (95% CI)
0.64 (0.45, 0.90)
Log-rank P-value
0.0104
Figure 1. Kaplan-Meier Curves for Overall Survival in Small Cell Lung Cancer in Study 478
- 15 REFERENCES
-
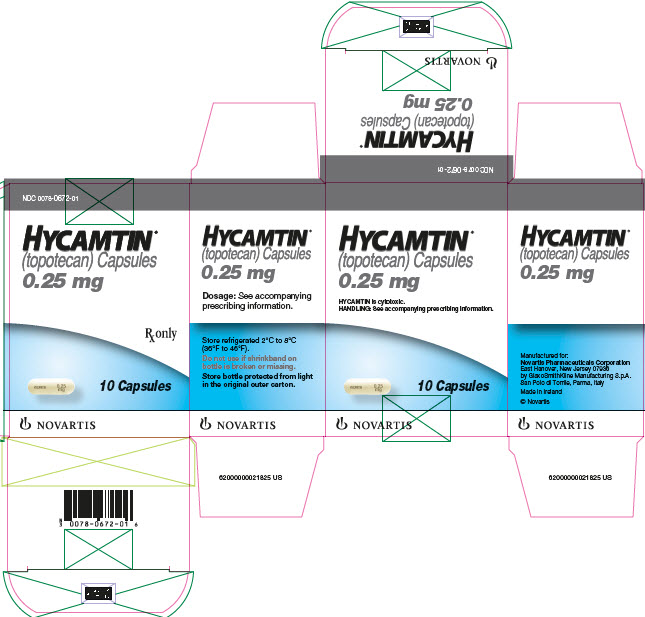
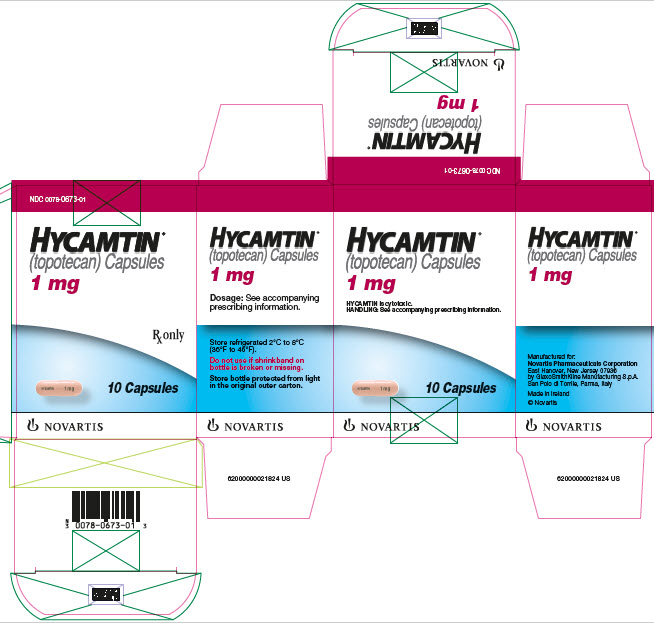
16 HOW SUPPLIED/STORAGE AND HANDLING
The 0.25 mg HYCAMTIN capsules are opaque white to yellowish-white imprinted with HYCAMTIN and 0.25 mg and are available in bottles of 10: NDC: 0078-0672-01.
The 1 mg HYCAMTIN capsules are opaque pink imprinted with HYCAMTIN and 1 mg and are available in bottles of 10: NDC: 0078-0673-01.
Store refrigerated 2ºC to 8ºC (36ºF to 46ºF) protected from light in the original carton.
HYCAMTIN is a cytotoxic drug. Follow applicable special handling and disposable procedures.1
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information).
Myelosuppression
Inform patients that HYCAMTIN decreases blood cell counts, such as white blood cells, platelets, and red blood cells. Instruct patients to notify their healthcare provider promptly for fever or other signs of infection [see Warnings and Precautions (5.1)].
Diarrhea
Inform patients that HYCAMTIN capsules can cause diarrhea which may be severe and life-threatening. Instruct patients how to manage and/or prevent diarrhea and to inform their physician if severe diarrhea occurs during treatment with HYCAMTIN capsules [see Warnings and Precautions (5.2)].
Interstitial Lung Disease (ILD)
Inform patients of the risks of severe ILD. Advise patients to contact their healthcare provider immediately to report new or worsening respiratory symptoms [see Warnings and Precautions (5.3)].
Embryo-Fetal Toxicity
Advise females of reproductive potential and males with female partners of reproductive potential of the potential risk to a fetus. Advise women to contact their healthcare provider if they become pregnant, or if pregnancy is suspected during treatment with HYCAMTIN capsules [see Warnings and Precautions (5.4), Use in Specific Populations (8.1, 8.3)].
Advise females of reproductive potential to use effective contraception during treatment and for 6 months after the last dose of HYCAMTIN capsules [see Use in Specific Populations (8.1, 8.3)].
Advise males with a female partner of reproductive potential to use effective contraception during treatment and for 3 months after the last dose of HYCAMTIN capsules [see Use in Specific Populations (8.1, 8.3), Nonclinical Toxicology (13.1)].
Lactation
Advise women to discontinue breastfeeding during treatment and for 1 week after the last dose of HYCAMTIN capsules [see Use in Specific Populations (8.2)].
Infertility
Advise male and female patients of the potential risk for impaired fertility [see Use in Specific Populations (8.3), Nonclinical Toxicology (13.1)].
Distributed by:
Novartis Pharmaceuticals Corporation
East Hanover, New Jersey 07936© Novartis
T2018-112
-
PATIENT PACKAGE INSERT
This Patient Information has been approved by the U.S. Food and Drug Administration. Revised: 9/2018 PATIENT INFORMATION
HYCAMTIN® (hi-CAM-tin)
(topotecan)
capsulesWhat is the most important information I should know about HYCAMTIN?
HYCAMTIN may cause serious side effects, including:-
Bone marrow problems. HYCAMTIN can affect your bone marrow and can cause a severe decrease in your white blood cell, red blood cell, and platelet counts. Decreased blood cell counts can make you more likely to develop bleeding, bruising, anemia, or infections which may be life-threatening. Your healthcare provider will do blood tests regularly to check your blood cell counts during treatment with HYCAMTIN. Tell your healthcare provider right away if you have any signs of infection, including:
- fever (temperature of 100.5°F or greater)
- chills
- cough
- burning or pain on urination
-
Diarrhea. HYCAMTIN can cause severe and life-threatening diarrhea that may need to be treated in a hospital. Tell your healthcare provider right away if you develop:
- diarrhea with fever
- diarrhea 3 or more times a day
- diarrhea with stomach-area pain or cramps
See “What are the possible side effects of HYCAMTIN?” for more information about side effects.
What is HYCAMTIN?
HYCAMTIN is a prescription medicine used to treat small cell lung cancer (SCLC) that has come back (relapsed) and:- the cancer responded to your first chemotherapy, and
- it has been at least 45 days from the last dose of chemotherapy
It is not known if HYCAMTIN is safe and effective in children.
Do not take HYCAMTIN if you are allergic to topotecan or any of the ingreidents in HYCAMTIN. See the end of this leaflet for a complete list of ingredients in HYCAMTIN. Before taking HYCAMTIN, tell your healthcare provider about all of your medical conditions, including if you:
- have diarrhea or watery stools
- have or have had lung problems
- have kidney problems
- are pregnant or plan to become pregnant. HYCAMTIN can harm your unborn baby.
- Females who are able to become pregnant should use effective birth control (contraception) during treatment with HYCAMTIN and for 6 months after the last dose of HYCAMTIN.
- Males who have female partners who are able to become pregnant, should use effective birth control during treatment with HYCAMTIN and for 3 months after the last dose of HYCAMTIN.
- Talk to your healthcare provider about birth control methods that may be right for you during treatment with HYCAMTIN.
- Your healthcare provider will do a pregnancy test before you start taking HYCAMTIN. Tell your healthcare provider right away if you become pregnant, think you might be pregnant, or your female partner becomes pregnant during treatment with HYCAMTIN.
- are breastfeeding or plan to breastfeed. It is not known if HYCAMTIN passes into your breast milk. Do not breastfeed during treatment with HYCAMTIN and for 1 week after the last dose. Talk to your healthcare provider about the best way to feed your baby during this time.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
Taking HYCAMTIN with certain other medicines can affect how HYCAMTIN works causing side effects.
Know the medicines you take. Keep a list of them to show your healthcare provider and pharmacist when you get a new medicine.
How should I take HYCAMTIN?
- Take HYCAMTIN exactly as your healthcare provider tells you to take it.
- Your healthcare provider will tell you how many HYCAMTIN capsules to take and when to take them. Your healthcare provider may change your dose if needed.
- Your healthcare provider may want you to take both 1 mg and 0.25 mg HYCAMTIN capsules for your prescribed dose. It is important for you to be able to tell the difference between the capsules. The 1-mg capsule is a pink color and the 0.25 mg capsule is a white to yellowish-white color.
- Take HYCAMTIN one time a day for 5 days in a row. This treatment will normally be repeated every 3 weeks (a treatment cycle). Your healthcare provider will decide how long you will take HYCAMTIN.
- Take HYCAMTIN with or without food.
- Swallow HYCAMTIN whole. Do not open, chew, crush, or divide HYCAMTIN.
- If any of the HYCAMTIN capsules are broken or leaking, do not touch them with your bare hands. Carefully throw away (dispose of) the capsules, and then wash your hands well with soap and water.
- If you get any of the contents of HYCAMTIN capsules on your skin or in your eyes, do the following:
- Wash the area of skin well with soap and water right away.
- Wash your eyes right away with gently flowing water for at least 15 minutes.
- Call your healthcare provider if you get a skin reaction or get HYCAMTIN in your eyes.
- If you take too much HYCAMTIN, call your healthcare provider right away.
- If you miss a dose of HYCAMTIN, or if you vomit after taking your HYCAMTIN, take your next dose at the next scheduled time. Do not take another dose on the same day.
What are the possible side effects of HYCAMTIN?
HYCAMTIN may cause serious side effects, including:- See “What is the most important information I should know about HYCAMTIN?”
- Lung problems that can cause death. Tell your healthcare provider right away if you have new or worse symptoms of coughing, fever, shortness of breath, or problems breathing. Your healthcare provider may tell you to stop taking HYCAMTIN capsules.
The most common side effects of HYCAMTIN include: decreased blood cell counts
diarrhea
hair lossnausea
vomiting
fatigue
Your healthcare provider may tell you to decrease your dose, temporarily stop, or completely stop taking HYCAMTIN if you develop certain serious side effects during treatment with HYCAMTIN.HYCAMTIN may cause short-term and long-term fertility problems in females. This could affect your ability to become pregnant.
HYCAMTIN may cause lower sperm count problems in men. This could affect your ability to father a child and cause birth defects. Talk to your healthcare provider about family planning options that might be right for you.
These are not all the possible side effects of HYCAMTIN.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store HYCAMTIN? - Store HYCAMTIN in a refrigerator between 36°F to 46°F (2°C to 8°C).
- Keep the bottle of HYCAMTIN in the carton that it comes in to protect it from light.
- Ask your healthcare provider or pharmacist how to safely throw away any unused or expired HYCAMTIN.
Keep HYCAMTIN and all medicines out of the reach of children.
General information about the safe and effective use of HYCAMTIN
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use HYCAMTIN for a condition for which it was not prescribed. Do not give HYCAMTIN to other people, even if they have the same symptoms that you have. It may harm them. You can ask your pharmacist or healthcare provider for information about HYCAMTIN that is written for health professionals.What are the ingredients in HYCAMTIN?
Active ingredient: topotecan hydrochloride
Inactive ingredients: gelatin, glyceryl monostearate, hydrogenated vegetable oil, and titanium dioxide. The 1-mg capsules also contain red iron oxide. The capsules are imprinted with edible black ink.
Distributed by:
Novartis Pharmaceuticals Corporation, East Hanover, New Jersey 07936
© Novartis
T2018-113
For more information go to www.pharma.us.novartis.com or call 1-888-669-6682. -
Bone marrow problems. HYCAMTIN can affect your bone marrow and can cause a severe decrease in your white blood cell, red blood cell, and platelet counts. Decreased blood cell counts can make you more likely to develop bleeding, bruising, anemia, or infections which may be life-threatening. Your healthcare provider will do blood tests regularly to check your blood cell counts during treatment with HYCAMTIN. Tell your healthcare provider right away if you have any signs of infection, including:
-
PRINCIPAL DISPLAY PANEL
Principal Display Panel
NDC: 0078-0672-01
HYCAMTIN®
(topotecan) Capsules
0.25 mg
Rx only
10 Capsules
Novartis
-
PRINCIPAL DISPLAY PANEL
Principal Display Panel
NDC: 0078-0673-01
HYCAMTIN®
(topotecan) Capsules
1 mg
Rx only
10 Capsules
Novartis
-
INGREDIENTS AND APPEARANCE
HYCAMTIN
topotecan capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0078-0672 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength TOPOTECAN HYDROCHLORIDE (UNII: 956S425ZCY) (TOPOTECAN - UNII:7M7YKX2N15) TOPOTECAN .25 mg Inactive Ingredients Ingredient Name Strength GLYCERYL MONOSTEARATE (UNII: 230OU9XXE4) GELATIN (UNII: 2G86QN327L) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) FERRIC OXIDE RED (UNII: 1K09F3G675) Product Characteristics Color WHITE (opaque white to yellowish-white) Score no score Shape CAPSULE Size 18mm Flavor Imprint Code HYCAMTIN;0;25;mg Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0078-0672-01 10 in 1 BOTTLE; Type 0: Not a Combination Product 07/07/2017 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA020981 07/07/2017 HYCAMTIN
topotecan capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0078-0673 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength TOPOTECAN HYDROCHLORIDE (UNII: 956S425ZCY) (TOPOTECAN - UNII:7M7YKX2N15) TOPOTECAN 1 mg Inactive Ingredients Ingredient Name Strength GLYCERYL MONOSTEARATE (UNII: 230OU9XXE4) GELATIN (UNII: 2G86QN327L) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) FERRIC OXIDE RED (UNII: 1K09F3G675) Product Characteristics Color PINK (opaque pink) Score no score Shape CAPSULE Size 18mm Flavor Imprint Code HYCAMTIN;1mg Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0078-0673-01 10 in 1 BOTTLE; Type 0: Not a Combination Product 02/24/2017 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA020981 02/24/2017 Labeler - Novartis Pharmaceuticals Corporation (002147023)
Trademark Results [HYCAMTIN]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 HYCAMTIN 75906637 2598707 Live/Registered |
NOVARTIS PHARMA AG 2000-02-01 |
 HYCAMTIN 75448624 2275693 Live/Registered |
NOVARTIS PHARMA AG 1998-03-11 |
 HYCAMTIN 75130999 not registered Dead/Abandoned |
SmithKline Beecham PLC 1996-06-04 |
 HYCAMTIN 75104975 not registered Dead/Abandoned |
SmithKline Beecham P.L.C. 1996-05-16 |
 HYCAMTIN 74366306 2030440 Live/Registered |
NOVARTIS PHARMA AG 1993-03-09 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.