GEMCITABINE injection, powder, lyophilized, for solution
gemcitabine by
Drug Labeling and Warnings
gemcitabine by is a Prescription medication manufactured, distributed, or labeled by Bedford Laboratories, Dr. Reddy's Laboratories Limited , Dr. Reddy's Laboratories Limited-FTO7. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use gemcitabine for injection safely and effectively. See full prescribing information for gemcitabine for injection.
Gemcitabine For Injection, Powder, Lyophilized, For Solution For Intravenous Use
Initial U.S. Approval: 1996RECENT MAJOR CHANGES
INDICATIONS AND USAGE
Gemcitabine for injection is a nucleoside metabolic inhibitor indicated:
- in combination with carboplatin, for the treatment of advanced ovarian cancer that has relapsed at least 6 months after completion of platinum-based therapy (1.1)
- in combination with paclitaxel, for first-line treatment of metastatic breast cancer after failure of prior anthracycline-containing adjuvant chemotherapy, unless anthracyclines were clinically contraindicated (1.2)
- in combination with cisplatin for the treatment of non-small cell lung cancer (1.3)
- as a single agent for the treatment of pancreatic cancer (1.4)
DOSAGE AND ADMINISTRATION
Gemcitabine for injection is for intravenous use only.
- Ovarian Cancer: 1000 mg/m2 over 30 minutes on Days 1 and 8 of each 21-day cycle (2.1)
- Breast Cancer: 1250 mg/m2 over 30 minutes on Days 1 and 8 of each 21-day cycle (2.2)
- Non-Small Cell Lung Cancer: 1000 mg/m2 over 30 minutes on Days 1, 8, and 15 of each 28-day cycle or 1250 mg/m2 over 30 minutes on Days 1 and 8 of each 21-day cycle (2.3)
- Pancreatic Cancer: 1000 mg/m2 over 30 minutes once weekly for the first 7 weeks, then one week rest, then once weekly for 3 weeks of each 28-day cycle (2.4)
CONTRAINDICATIONS
Patients with a known hypersensitivity to Gemcitabine (4)
WARNINGS AND PRECAUTIONS
- Schedule-dependent toxicity: Increased toxicity with infusion time greater than 60 minutes or dosing more frequently than once weekly. (5.1)
- Myelosuppression: Monitor for myelosuppression prior to each cycle and reduce or withhold dose for severe myelosuppression. (5.2, 5.7)
- Pulmonary Toxicity and Respiratory Failure: Discontinue gemcitabine for injection immediately for unexplained new or worsening dyspnea or evidence of severe pulmonary toxicity. (5.3)
- Hemolytic-Uremic Syndrome (HUS): Monitor renal function prior to initiation and during therapy. Discontinue gemcitabine for injection for HUS or severe renal impairment. (5.4)
- Hepatic Toxicity: Monitor hepatic function prior to initiation and during therapy. Discontinue gemcitabine for injection for severe hepatic toxicity. (5.5)
- Embryofetal Toxicity: Can cause fetal harm. Advise women of potential risk to the fetus. (5.6, 8.1)
- Exacerbation of Radiation Therapy Toxicity: May cause severe and life-threatening toxicity when administered during or within 7 days of radiation therapy. (5.7)
- Capillary Leak Syndrome: Discontinue gemcitabine for injection. (5.8)
- Posterior reversible encephalopathy syndrome (PRES): Discontinue gemcitabine for injection. (5.9)
ADVERSE REACTIONS
The most common adverse reactions for the single agent (≥20%) are nausea/vomiting, anemia, hepatic transaminitis, neutropenia, increased alkaline phosphatase, proteinuria, fever, hematuria, rash, thrombocytopenia, dyspnea, and peripheral edema (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Dr. Reddy’s Laboratories Inc., at 1-888-375-3784 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 6/2013
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
1.1 Ovarian Cancer
1.2 Breast Cancer
1.3 Non-Small Cell Lung Cancer
1.4 Pancreatic Cancer
2 DOSAGE AND ADMINISTRATION
2.1 Ovarian Cancer
2.2 Breast Cancer
2.3 Non-Small Cell Lung Cancer
2.4 Pancreatic Cancer
2.5 Dose Modifications for Non-Hematologic Adverse Reactions
2.6 Preparation and Administration Precautions
2.7 Preparation for Intravenous Infusion Administration
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Schedule-dependent Toxicity
5.2 Myelosuppression
5.3 Pulmonary Toxicity and Respiratory Failure
5.4 Hemolytic Uremic Syndrome
5.5 Hepatic Toxicity
5.6 Embryofetal Toxicity
5.7 Exacerbation of Radiation Therapy Toxicity
5.8 Capillary Leak Syndrome
5.9 Posterior Reversible Encephalopathy Syndrome
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Post-Marketing Experience
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
8.8 Gender
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment Of Fertility
14 CLINICAL STUDIES
14.1 Ovarian Cancer
14.2 Breast Cancer
14.3 Non-Small Cell Lung Cancer (NSCLC)
14.4 Pancreatic Cancer
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
16.2 Storage and Handling
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
1.1 Ovarian Cancer
Gemcitabine for injection in combination with carboplatin is indicated for the treatment of patients with advanced ovarian cancer that has relapsed at least 6 months after completion of platinum-based therapy.
1.2 Breast Cancer
Gemcitabine for injection in combination with paclitaxel is indicated for the first-line treatment of patients with metastatic breast cancer after failure of prior anthracycline-containing adjuvant chemotherapy, unless anthracyclines were clinically contraindicated.
-
2 DOSAGE AND ADMINISTRATION
Gemcitabine for injection is for intravenous use only. Gemcitabine for injection may be administered on an outpatient basis.
2.1 Ovarian Cancer
Recommended Dose and Schedule
The recommended dose of gemcitabine for injection is 1000 mg/m2 as an intravenous infusion over 30 minutes on Days 1 and 8 of each 21-day cycle, in combination with carboplatin AUC 4 intravenously after gemcitabine for injection administration on Day 1 of each 21-day cycle. Refer to carboplatin prescribing information for additional information.
Dose Modifications
Recommended gemcitabine for injection dose modifications for myelosuppression are described Table 1 and Table 2 [see Warnings and Precautions (5.2)]. Refer to Dosage and Administration (2.5) for recommendations for non-hematologic adverse reactions.
Table 1: Dosage Reduction Guidelines for Gemcitabine For Injection for Myelosuppression on Day of Treatment in Ovarian Cancer
Treatment Day Absolute granulocyte count (x 106/L) Platelet count (x 106/L) % of full dose Day 1 ≥1500 and ≥100,000 100% <1500 or <100,000 Delay Treatment Cycle Day 8 ≥1500 and ≥100,000 100 1000 to 1499 or 75,000 to 99,999 50 <1000 or <75,000 Hold Table 2: Gemcitabine For Injection Dose Modification for Myelosuppression in Previous Cycle In Ovarian Cancer
Occurrence Myelosuppression During Treatment Cycle Dose Modification Initial Occurrence Absolute granulocyte count less than 500 x 106/L for more than 5 days
Absolute granulocyte count less than 100 x 106/L for more than 3 days
Febrile neutropenia Platelets less than 25,000x106/L
Cycle delay of more than one week due to toxicityPermanently reduce gemcitabine for injection to 800 mg/m2 on Days 1 and 8 Subsequent Occurrence If any of the above toxicities occur after the initial dose reduction Permanently reduce gemcitabine for injection dose to 800 mg/m2on Day 1 only 2.2 Breast Cancer
Recommended Dose and Schedule
The recommended dose of gemcitabine for injection is 1250 mg/m2 intravenously over 30 minutes on Days 1 and 8 of each 21-day cycle that includes paclitaxel. Paclitaxel should be administered at 175 mg/m2 on Day 1 as a 3 hour intravenous infusion before gemcitabine for injection administration.
Dose Modifications Recommended dose modifications for gemcitabine for injection for myelosuppression are described in Table 3 [see Warnings and Precautions (5.2)]. Refer to Dosage and Administration (2.5) for recommendations for non-hematologic adverse reactions.
Table 3: Recommended Dose Reductions for Gemcitabine For Injection for Myelosuppression on Day of Treatment in Breast Cancer
Treatment Day Absolute granulocyte count (x 106/L) Platelet count(x 106/L) % of full dose Day 1 ≥1500 and ≥ 100,000 100% less than1500 or less than 100,000 Hold Day 8 ≥ 1200 and > 75,000 100% 1000 to 1199 or 50,000 to 75,000 75% 700 to 999 and ≥ 50,000 50% < 700 or < 50,000 Hold 2.3 Non-Small Cell Lung Cancer
Recommended Dose and Schedule
Every 4-week schedule The recommended dose of gemcitabine for injection is 1000 mg/m2 intravenously over 30 minutes on Days 1, 8, and 15 in combination with cisplatin therapy. Administer cisplatin intravenously at 100 mg/m2 on Day 1 after the infusion of gemcitabine for injection.
Every 3-week schedule
The recommended dose of gemcitabine for injection is 1250 mg/m2 intravenously over 30 minutes on Days 1 and 8 in combination with cisplatin therapy. Administer cisplatin intravenously at 100 mg/m2 on Day 1 after the infusion of gemcitabine for injection.
Dose Modifications
Recommended dose modifications for gemcitabine for injection myelosuppression are described in Table 4 [see Warnings and Precautions (5.2)]. Refer to Dosage and Administration (2.5) for gemcitabine for injection recommendations for non-hematologic adverse reactions.
2.4 Pancreatic Cancer
Recommended Dose and Schedule
The recommended dose of gemcitabine for injection is 1000 mg/m2 over 30 minutes intravenously. The recommended treatment schedule
Weeks 1 to 8: weekly dosing for the first 7 weeks followed by one week rest.
After week 8: weekly dosing on Days 1, 8, and 15 of 28-day cycles.
Dose Modifications
Recommended dose modifications for gemcitabine for injection for myelosuppression are described in Table 4 [see Warnings and Precautions (5.2)]. Refer to Dosage and Administration (2.5) for recommendations for non-hematologic adverse reactions.
Patients receiving gemcitabine for injection should be monitored prior to each dose with a complete blood count (CBC), including differential and platelet count. If marrow suppression is detected, therapy should be modified or suspended according to the guidelines in Table 4.
Table 4: Recommended Dose Reductions for Gemcitabine For Injection for Myelosuppression in Pancreatic Cancer and Non-Small Cell Lung Cancer
Absolute granulocyte count (x 106/L) Platelet count(x 106/L) % of full dose ≥1000 And ≥100,000 100 500 to 999 Or 50,000 to 99,999 75 <500 Or <50,000 Hold 2.5 Dose Modifications for Non-Hematologic Adverse Reactions
Permanently discontinue gemcitabine for injection for any of the following
- Unexplained dyspnea or other evidence of severe pulmonary toxicity
- Severe hepatic toxicity
- Hemolytic-Uremic Syndrome
- Capillary Leak Syndrome
- Posterior reversible encephalopathy syndrome
Withhold gemcitabine for injection or reduce dose by 50% for other severe (Grade 3 or 4) non-hematological toxicity until resolved. No dose modifications are recommended for alopecia, nausea, or vomiting.
2.6 Preparation and Administration Precautions
Exercise caution and wear gloves when preparing gemcitabine for injection solutions. Immediately wash the skin thoroughly or rinse the mucosa with copious amounts of water if gemcitabine for injection contacts the skin or mucus membranes. Death has occurred in animal studies due to dermal absorption. For further guidance on handling gemcitabine for injection go to “OSHA Hazardous Drugs” (refer to antineoplastic weblinks including OSHA Technical Manual) at OSHA. http://www.osha.gov/SLTC/hazardousdrugs/index.html
2.7 Preparation for Intravenous Infusion Administration
Reconstitute the vials with 0.9% Sodium Chloride Injection without preservatives. Add 5 mL to the 200 mg vial or 25 mL to the 1 g vial. These dilutions each yield a gemcitabine for injection concentration of 38 mg/mL. Complete withdrawal of the vial contents will provide 200 mg or 1 g of gemcitabine for injection. Prior to administration the appropriate amount of drug must be diluted with 0.9% Sodium Chloride Injection. Final concentrations may be as low as 0.1 mg/mL.
Reconstituted gemcitabine for injection is a clear, colorless to light straw-colored solution. Inspect visually prior to administration and discard for particulate matter or discoloration. Gemcitabine for injection solutions are stable for 24 hours at controlled room temperature of 20° to 25°C (68° to 77°F). Do not refrigerate as crystallization can occur.
No incompatibilities have been observed with infusion bottles or polyvinyl chloride bags and administration sets.
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
Patients receiving therapy with gemcitabine for injection should be monitored closely by a physician experienced in the use of cancer chemotherapeutic agents.
5.1 Schedule-dependent Toxicity
In clinical trials evaluating the maximum tolerated dose of gemcitabine for injection, prolongation of the infusion time beyond 60 minutes or more frequent than weekly dosing resulted in an increased incidence of clinically significant hypotension, severe flu-like symptoms, myelosuppression, and asthenia. The half-life of gemcitabine for injection is influenced by the length of the infusion [see Clinical Pharmacology (12.3)].
5.2 Myelosuppression
Myelosuppression manifested by neutropenia, thrombocytopenia, and anemia occurs with gemcitabine for injection as a single agent and the risks are increased when gemcitabine for injection is combined with other cytotoxic drugs. In clinical trials, Grade 3-4 neutropenia, anemia, and thrombocytopenia occurred in 25%, 8%, and 5%, respectively of patients receiving single-agent. The frequencies of Grade 3-4 neutropenia, anemia, and thrombocytopenia varied from 48% to 71%, 8 to 28%, and 5 to 55%, respectively, in patients receiving gemcitabine for injection in combination with another drug.
5.3 Pulmonary Toxicity and Respiratory Failure
Pulmonary toxicity, including interstitial pneumonitis, pulmonary fibrosis, pulmonary edema, and adult respiratory distress syndrome (ARDS), has been reported. In some cases, these pulmonary events can lead to fatal respiratory failure despite discontinuation of therapy. The onset of pulmonary symptoms may occur up to 2 weeks after the last dose of gemcitabine for injection. Discontinue gemcitabine for injection in patients who develop unexplained dyspnea, with or without bronchospasm, or have any evidence of pulmonary toxicity [see Adverse Reactions (6.1 and 6.2)].
5.4 Hemolytic Uremic Syndrome
Hemolytic Uremic Syndrome to include fatalities from renal failure or the requirement for dialysis can occur in patients treated with gemcitabine for injection. In clinical trials, HUS was reported in 6 of 2429 patients (0.25%). Most fatal cases of renal failure were due to HUS [see Adverse Reactions (6.1 and 6.2)]. Assess renal function prior to initiation of gemcitabine for injection and periodically during treatment. Consider the diagnosis of HUS in patients who develops anemia with evidence of microangiopathic hemolysis, elevation of bilirubin or LDH, or reticulocytosis; severe thrombocytopenia; or evidence of renal failure (elevation of serum creatinine or BUN) [see Dosage and Administration (2.5) and Use In Specific Populations (8.6)]. Permanently discontinue gemcitabine for injection in patients with HUS or severe renal impairment. Renal failure may not be reversible even with discontinuation of therapy. Renal failure may not be reversible even with discontinuation of therapy.
5.5 Hepatic Toxicity
Drug-induced liver injury, including liver failure and death, has been reported in patients receiving gemcitabine for injection alone or in combination with other potentially hepatotoxic drugs [see Adverse Reactions (6.1 and 6.2)]. Administration of gemcitabine for injection in patients with concurrent liver metastases or a pre-existing medical history or hepatitis, alcoholism, or liver cirrhosis can lead to exacerbation of the underlying hepatic insufficiency [see Use in Specific Populations (8.7)]. Assess hepatic function prior to initiation of gemcitabine for injection and periodically during treatment. Discontinue gemcitabine for injection in patients that develop severe liver injury.
5.6 Embryofetal Toxicity
Gemcitabine for injection can cause fetal harm when administered to a pregnant woman, based on its mechanism of action. Gemcitabine was teratogenic, embryotoxic, and fetotoxic in mice and rabbits. If this drug is used during pregnancy, or if a woman becomes pregnant while taking gemcitabine for injection, the patient should be apprised of the potential hazard to a fetus. [see Use In Specific Populations (8.1)]
5.7 Exacerbation of Radiation Therapy Toxicity
Gemcitabine for injection is not indicated for use in combination with radiation therapy.
Concurrent (given together or ≤7 days apart) — Life-threatening mucositis, especially esophagitis and pneumonitis occurred in a trial in which gemcitabine for injection was administered at a dose of 1000 mg/m2 to patients with non-small cell lung cancer for up to 6 consecutive weeks concurrently with thoracic radiation.
Non-concurrent (given >7 days apart) — Excessive toxicity has not been observed when gemcitabine for injection is administered more than 7 days before or after radiation. Radiation recall has been reported in patients who receive gemcitabine for injection after prior radiation.
5.8 Capillary Leak Syndrome
Capillary leak syndrome (CLS) with severe consequences has been reported in patients receiving gemcitabine for injection as a single agent or in combination with other chemotherapeutic agents. Discontinue gemcitabine for injection if CLS develops during therapy.
5.9 Posterior Reversible Encephalopathy Syndrome
Posterior reversible encephalopathy syndrome (PRES) has been reported in patients receiving gemcitabine for injection as a single agent or in combination with other chemotherapeutic agents. PRES can present with headache, seizure, lethargy, hypertension, confusion, blindness, and other visual and neurologic disturbances. Confirm the diagnosis of PRES with magnetic resonance imaging (MRI) and discontinue gemcitabine for injection if PRES develops during therapy.
-
6 ADVERSE REACTIONS
The following serious adverse reactions are discussed in greater detail in another section of the label
- Schedule-Dependent Toxicity [see Warnings and Precautions (5.1) ]
- Myelosuppression [see Warnings and Precautions (5.2)]
- Pulmonary Toxicity and Respiratory Failure [see Warnings and Precautions (5.3)]
- Hemolytic Uremic Syndrome [see Warnings and Precautions (5.4)]
- Hepatic Toxicity [see Warnings and Precautions (5.5)]
- Embryo-fetal Toxicity [ see Warnings and Precautions (5.6), Use in Specific Populations (8.1), and Nonclinical Toxicology (13.1)].
- Posterior Reversible Encephalopathy Syndrome [see Warnings and Precautions (5.9)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
Single-Agent Use:
The data described below reflect exposure to gemcitabine for injection as a single agent administered at doses between 800 mg/m2 to 1250 mg/m2 over 30 minutes intravenously, once weekly, in 979 patients with a variety of malignancies. The most common (≥20%) adverse reactions of single-agent gemcitabine for injection are nausea/vomiting, anemia, increased ALT, increased AST, neutropenia, increased alkaline phosphatase, proteinuria, fever, hematuria, rash, thrombocytopenia, dyspnea, and edema. The most common (≥5%) Grade 3 or 4 adverse reactions were neutropenia, nausea/vomiting; increased ALT, increase alkaline phosphatase, anemia, increased AST, and thrombocytopenia. Approximately 10% of the 979 patients discontinued gemcitabine for injection due to adverse reactions. Adverse reactions resulting in discontinuation of gemcitabine for injection in 2% of 979 patients were cardiovascular adverse events (myocardial infarction, cerebrovascular accident, arrhythmia, and hypertension) and adverse reactions resulting in discontinuation of gemcitabine for injection in less than 1% of the 979 patients were anemia, thrombocytopenia, hepatic dysfunction, renal dysfunction, nausea/vomiting, fever, rash, dyspnea, hemorrhage, infection, stomatitis, somnolence, flu-like syndrome, and edema.
Table 5 presents the incidence of adverse reactions reported in 979 patients with various malignancies receiving single-agent gemcitabine for injection across 5 clinical trials. Table 5 includes all clinical adverse reactions, reported in at least 10% of patients. A listing of clinically significant adverse reactions is provided following the table.
Table 5: Selected Per-Patient Incidence of Adverse Events in Patients Receiving Single-Agent Gemcitabine For Injectiona
All Patients b All Grades Grade 3 Grade 4 Laboratoryc Hematologic Anemia 68 7 1 Neutropenia 63 19 6 Thrombocytopenia 24 4 1 Hepatic Increased ALT 68 8 2 Increased AST 67 6 2 Increased Alkaline Phosphatase 55 7 2 Hyperbilirubinemia 13 2 <1 Renal Proteinuria 45 <1 0 Hematuria 35 <1 0 Increased BUN 16 0 0 Increased Creatinine 8 <1 0 Non– laboratoryd Nausea and Vomiting 69 13 1 Fever 41 2 0 Rash 30 <1 0 Dyspnea 23 3 <1 Diarrhea 19 1 0 Hemorrhage 17 <1 <1 Infection 16 1 <1 Alopecia 15 <1 0 Stomatitis 11 <1 0 Somnolence 11 <1 <1 Paresthesias 10 <1 0 a Grade based on criteria from the World Health Organization (WHO).
b N=699-974; all patients with laboratory or non-laboratory data.
c Regardless of causality.
d For approximately 60% of patients, non-laboratory adverse events were graded only if assessed to be possibly drug-related.
- Transfusion requirements — Red blood cell transfusions (19%); platelet transfusions (<1%)
- Fever — Fever occurred in the absence of clinical infection and frequently in combination with other flu-like symptoms.
- Pulmonary — Dyspnea unrelated to underlying disease and sometimes accompanied by bronchospasm.
- Edema — Edema (13%), peripheral edema (20%), and generalized edema (<1%); <1% of patients. discontinued gemcitabine for injection due to edema.
- Flu-like Symptoms — Characterized by fever, asthenia, anorexia, headache, cough, chills, myalgia, asthenia insomnia, rhinitis, sweating, and/or malaise (19%); <1% of patients discontinued gemcitabine for injection due to flu-like symptoms
- Infection — Sepsis (<1%)
- Extravasation — Injection-site reactions (4%)
- Allergic — Bronchospasm (<2%); anaphylactoid reactions [see Contraindications (4)].
Non-Small Cell Lung Cancer:
Table 6 presents the incidence of selected adverse reactions, occurring in ≥10% of gemcitabine for injection-treated patients and at a higher incidence in the gemcitabine for injection plus cisplatin arm, reported in a randomized trial of gemcitabine for injection plus cisplatin (n=262) administered in 28-day cycles as compared to cisplatin alone (n=260) in patients receiving first-line treatment for locally advanced or metastatic non-small cell lung cancer (NSCLC) [see Clinical Studies (14.3)].
Patients randomized to gemcitabine for injection plus cisplatin received a median of 4 cycles of treatment and those randomized to cisplatin received a median of 2 cycles of treatment. In this trial, the requirement for dose adjustments (>90% versus 16%), discontinuation of treatment for adverse reactions (15% versus 8%), and the proportion of patients hospitalized (36% versus 23%) were all higher for patients receiving gemcitabine for injection plus cisplatin arm compared to those receiving cisplatin alone. The incidence of febrile neutropenia (9/262 versus 2/260), sepsis (4% versus 1%), Grade 3 cardiac dysrhythmias (3% versus <1%) were all higher in the gemcitabine for injection plus cisplatin arm compared to the cisplatin alone arm. The two-drug combination was more myelosuppressive with 4 (1.5%) possibly treatment-related deaths, including 3 resulting from myelosuppression with infection and one case of renal failure associated with pancytopenia and infection. No deaths due to treatment were reported on the cisplatin arm.
Table 6: Per-Patient Incidence of Selected Adverse Reactions from Randomized Trial of Gemcitabine For Injection plus Cisplatin versus Single-Agent Cisplatin in Patients with NSCLC Occurring at Higher Incidence in Gemcitabine For Injection-Treated Patients [Between Arm Difference of ≥5% (All Grades) or ≥2% (Grades 3 - 4)]a
Gemcitabine For Injection plus Cisplatin b Cisplatin c All Grades Grade 3 Grade 4 All Grades Grade 3 Grade 4 Laboratoryd Hematologic Anemia 89 22 3 67 6 1 RBC Transfusion e 39 13 Neutropenia 79 22 35 20 3 1 Thrombocytopenia 85 25 25 13 3 1 Platelet Transfusion e 21 <1 Lymphopenia 75 25 18 51 12 5 Hepatic Increased Transaminases 22 2 1 10 1 0 Increased Alkaline Phosphatase 19 1 0 13 0 0 Renal Proteinuria 23 0 0 18 0 0 Hematuria 15 0 0 13 0 0 Elevated creatinine 38 4 <1 31 2 <1 Other Laboratory Hyperglycemia 30 4 0 23 3 0 Hypomagnesemia 30 4 3 17 2 0 Hypocalcemia 18 2 0 7 0 <1 Non-laboratoryf Nausea 93 25 2 87 20 <1 Vomiting 78 11 12 71 10 9 Alopecia 53 1 0 33 0 0 Neuro Motor 35 12 0 15 3 0 Diarrhea 24 2 2 13 0 0 Neuro Sensory 23 1 0 18 1 0 Infection 18 3 2 12 1 0 Fever 16 0 0 5 0 0 Neuro Cortical 16 3 1 9 1 0 Neuro Mood 16 1 0 10 1 0 Local 15 0 0 6 0 0 Neuro Headache 14 0 0 7 0 0 Stomatitis 14 1 0 5 0 0 Hemorrhage 14 1 0 4 0 0 Hypotension 12 1 0 7 1 0 Rash 11 0 0 3 0 0 a National Cancer Institute Common Toxicity Criteria (CTC) for severity grading.
b N=217–253; all gemcitabine for injection plus cisplatin patients with laboratory or non–laboratory data gemcitabine for injection at 1000 mg/m2 on Days 1, 8, and 15 and cisplatin at 100 mg/m2 on Day 1 every 28 days.
c N=213–248; all cisplatin patients with laboratory or non–laboratory data. Cisplatin at 100 mg/m2 on Day 1 every 28 days.
d Regardless of causality.
e Percent of patients receiving transfusions. Percent transfusions are not CTC–graded events.
f Non–laboratory events were graded only if assessed to be possibly drug–related.
Table 7 presents the incidence of selected adverse reactions, occurring in ≥10% of gemcitabine for injection-treated patients and at a higher incidence in the gemcitabine for injection plus cisplatin arm, reported in a randomized trial of gemcitabine for injection plus cisplatin (n=69) administered in 21-day cycles as compared to etoposide plus cisplatin alone (n=66) in patients receiving first-line treatment for locally advanced or metastatic non-small cell lung cancer (NSCLC) [see Clinical Studies (14.3)]. A listing of clinically significant adverse reactions is provided following the table.
Patients in the gemcitabine for injection cisplatin (GC) arm received a median of 5 cycles and those in the etoposide/cisplatin (EC) arm received a median of 4 cycles. The majority of patients receiving more than one cycle of treatment required dose adjustments; 81% in the (GC) arm and 68% in the (EC) arm. The incidence of hospitalizations for treatment-related adverse events was 22% (GC) and 27% in the (EC) arm. The proportion of discontinuation of treatment for treatment-related adverse reactions was higher for patients in the (GC) arm (14% versus 8%). The proportion of patients hospitalized for febrile neutropenia was lower in the (GC) arm (7% versus 12%). There was one death attributed to treatment, a patient with febrile neutropenia and renal failure, which occurred in the gemcitabine for injection /cisplatin arm.
Table 7: Per-Patient Incidence of Selected Adverse Reactions in Randomized Trial of Gemcitabine For Injection plus Cisplatin versus Etoposide plus Cisplatin in Patients with NSCLCa
Gemcitabine For Injection plus Cisplatinb Etoposide plus Cisplatinc All Grades Grade 3 Grade 4 All Grades Grade 3 Grade 4 Laboratoryd Hematologic Anemia 88 22 0 77 13 2 RBC Transfusionse 29 - - 21 - - Neutropenia 88 36 28 87 20 56 Thrombocytopenia 81 39 16 45 8 5 Platelet Transfusionse 3 - - 8 - - Hepatic Increased ALT 6 0 0 12 0 0 Increased AST 3 0 0 11 0 0 Increased Alkaline 16 0 0 11 0 0 Phosphatase Bilirubin 0 0 0 0 0 0 Renal Proteinuria 12 0 0 5 0 0 Hematuria 22 0 0 10 0 0 BUN 6 0 0 4 0 0 Creatinine 2 0 0 2 0 0 Non– laboratoryf,g Nausea and Vomiting 96 35 4 86 19 7 Fever 6 0 0 3 0 0 Rash 10 0 0 3 0 0 Dyspnea 1 0 1 3 0 0 Diarrhea 14 1 1 13 0 2 Hemorrhage 9 0 3 3 0 3 Infection 28 3 1 21 8 0 Alopecia 77 13 0 92 51 0 Stomatitis 20 4 0 18 2 0 Somnolence 3 0 0 3 2 0 Paresthesias 38 0 0 16 2 0 a Grade based on criteria from the World Health Organization (WHO).
b N=67–69; all gemcitabine for injection plus cisplatin patients with laboratory or non–laboratory data. Gemcitabine for injection at 1250 mg/m2 on Days 1 and 8 and cisplatin at 100 mg/m2 on Day 1 every 21 days.
c N=57–63; all cisplatin plus etoposide patients with laboratory or non–laboratory data. Cisplatin at 100 mg/m2 on Day 1 and intravenous etoposide at 100 mg/m2 on Days 1, 2, and 3 every 21 days.
dRegardless of causality.
e WHO grading scale not applicable to proportion of patients with transfusions
fNon–laboratory events were graded only if assessed to be possibly drug–related.
g Pain data were not collected.
-
Flu-like syndrome: 3% in the gemcitabine for injection/cisplatin arm versus none in the etoposide/cisplatin arm.
-
Edema: 12% in the gemcitabine for injection/cisplatin arm versus 2% in the etoposide/cisplaarm.tin
Breast CancerTable 8 presents the incidence of selected adverse reactions, occurring in ≥10% of gemcitabine for injection-treated patients and at a higher incidence in the gemcitabine for injection plus paclitaxel arm, reported in a randomized trial of gemcitabine for injection plus paclitaxel (n=262) compared to paclitaxel alone (n=259) for the first-line treatment of metastatic breast cancer (MBC) in women who received anthracycline-containing chemotherapy in the adjuvant/neo-adjuvant setting or for whom anthracyclines were contraindicated. [see Clinical Studies (14.2)].
The requirement for dose reduction of paclitaxel were higher for patients in the gemcitabine for injection/paclitaxel arm (5% versus 2%). The number of paclitaxel doses omitted (<1%), the proportion of patients discontinuing treatment for treatment-related adverse reactions (7% versus 5%), and the number of treatment-related deaths (1 patient in each arm) were similar between the two arms.
Table 8: Per-Patient Incidence of Selected Adverse Reactions from Comparative Trial of Gemcitabine For Injection plus Paclitaxel versus Single-Agent Paclitaxel in Breast Cancera Occurring at Higher Incidence in Gemcitabine For Injection-Treated Patients [Between Arm Difference of ≥5% (All Grades) or ≥2% (Grades 3 - 4)]
Gemcitabine For Injection plus Paclitaxel (N=262) Paclitaxel(N=259) All Grades Grade 3 Grade 4 All Grades Grade 3 Grade 4 Laboratoryb Hematologic Anemia 69 6 1 51 3 <1 Neutropenia 69 31 17 31 4 7 Thrombocytopenia 26 5 <1 7 <1 <1 Hepatobiliary Increased ALT 18 5 <1 6 <1 0 Increased AST 16 2 0 5 <1 0 Non– laboratoryc Alopecia 90 14 4 92 19 3 Neuropathy– sensory 64 5 <1 58 3 0 Nausea 50 1 0 31 2 0 Fatigue 40 6 <1 28 1 <1 Vomiting 29 2 0 15 2 0 Diarrhea 20 3 0 13 2 0 Anorexia 17 0 0 12 <1 0 Neuropathy– motor 15 2 <1 10 <1 0 Stomatitis/ pharyngitis 13 1 <1 8 <1 0 Fever 13 <1 0 3 0 0 Rash/ desquamation 11 <1 <1 5 0 0 a Severity grade based on National Cancer Institute Common Toxicity Criteria (CTC) Version 2.0
b Regardless of causality.
c Non–laboratory events were graded only if assessed to be possibly drug–relate
The following clinically relevant, Grade 3 or 4 adverse reactions occurred with a higher incidence in the gemcitabine for injection plus paclitaxel arm compared with paclitaxel arm: febrile neutropenia (5% versus 1.2%) and dyspnea (1.9%versus 0)
Ovarian Cancer
Table 9 presents the incidence of selected adverse reactions, occurring in ≥10% of gemcitabine-treated patients and at a higher incidence in the gemcitabine for injection plus carboplatin arm, reported in a randomized trial of gemcitabine for injection plus carboplatin (n=175) compared to carboplatin alone (n=174) for the second-line treatment of ovarian cancer in women with disease that had relapsed more than 6 months following first-line platinum-based chemotherapy. [see Clinical Studies (14.1)]. Additional clinically significant adverse reactions, occurring in less than 10% of patients, are provided following Table 9.
The proportion of patients with dose adjustments for carboplatin (1.8% versus 3.8%), doses of carboplatin omitted (0.2% versus 0), and discontinuing treatment for treatment-related adverse reactions (10.9% versus 9.8%), were similar between arms. Dose adjustment for gemcitabine for injection occurred in 10.4% of patients and gemcitabine for injection dose was omitted in 13.7% of patients in the gemcitabine for injection /carboplatin arm.
Table 9: Per-Patient Incidence of Adverse Reactions in Randomized Trial of Gencitabine For Injection plus Carboplatin versus Carboplatin in Ovarian Cancer Occurring at Higher Incidence in Gemcitabine For Injection-Treated Patients [Between Arm Difference of ≥ 5% (All Grades) or ≥2% (Grades 3-4)]
Gemcitabine For Injection plus Carboplatin (N=175) Carboplatin (N=174) All Grades Grade 3 Grade 4 All Grades Grade 3 Grade 4 Laboratoryb Hematologic Neutropenia 90 42 29 58 11 1 Anemia 86 22 6 75 9 2 Thrombocytopenia 78 30 5 57 10 1 RBC Transfusionsc 38 15 Platelet Transfusionsc 9 3 Non–laboratoryb Nausea 69 6 0 61 3 0 Alopecia 49 0 0 17 0 0 Vomiting 46 6 0 36 2 <1 Constipation 42 6 1 37 3 0 Fatigue 40 3 <1 32 5 0 Diarrhea 25 3 0 14 <1 0 Stomatitis/ pharyngitis 22 <1 0 13 0 0 a Grade based on Common Toxicity Criteria (CTC) Version 2.0.
b Regardless of causality.
c Percent of patients receiving transfusions. Transfusions are not CTC–graded events. Blood transfusions included both packed red blood cells and whole blood.
Hematopoietic growth factors were administered more frequently in the gemcitabine for injection-containing arm: granulocyte growth factors (23.6% and 10.1%) and erythropoietic agents (7.3% and 3.9%).
The following clinically relevant, Grade 3 and 4 adverse reactions occurred more frequently in the gemcitabine for injection plus carboplatin arm: dyspnea (3.4% versus 2.9%), febrile neutropenia (1.1% versus 0), hemorrhagic event (2.3% versus 1.1 %), motor neuropathy (1.1% versus 0.6%), and rash/desquamation (0.6% versus 0).
6.2 Post-Marketing Experience
The following adverse reactions have been identified during post-approval use of gemcitabine for injection. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Cardiovascular — Congestive heart failure, myocardial infarction, Arrhythmias, supraventricular arrhythmias.
Vascular Disorders — Peripheral vasculitis, gangrene, and capillary leak syndrome [see Warnings and Precautions (5.9)]
Skin — Cellulitis, severe skin reactions, including desquamation and bullous skin eruptions
Hepatic — Hepatic failure, hepatic veno-occlusive disease
Pulmonary — Interstitial pneumonitis, pulmonary fibrosis, pulmonary edema, and adult respiratory distress syndrome (ARDS)
Nervous System — Posterior reversible encephalopathy syndrome (PRES) [see Warnings and Precautions (5.9)]
- 7 DRUG INTERACTIONS
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category D. [see Warnings and Precautions (5.6)].
Risk Summary
Gemcitabine for injection can cause fetal harm when administered to a pregnant woman. Based on its mechanism of action, gemcitabine for injection is expected to result in adverse reproductive effects. Gemcitabine was teratogenic, embryotoxic, and fetotoxic in mice and rabbits. If gemcitabine for injection is used during pregnancy, or if the patient becomes pregnant while taking gemcitabine for injection, the patient should be apprised of the potential hazard to a fetus.
Animal Data
Gemcitabine is embryotoxic causing fetal malformations (cleft palate, incomplete ossification) at doses of 1.5 mg/kg/day in mice (approximately 0.005 times the recommended human dose on a mg/m2 basis). Gemcitabine is fetotoxic causing fetal malformations (fused pulmonary artery, absence of gall bladder) at doses of 0.1 mg/kg/day in rabbits (about 0.002 times the recommended human dose on a mg/m2 basis). Embryotoxicity was characterized by decreased fetal viability, reduced live litter sizes, and developmental delays. [see Warnings and Precautions (5.6)]
8.3 Nursing Mothers
It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from Gemcitabine for injection, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
8.4 Pediatric Use
The safety and effectiveness of gemcitabine for injection have not been established in pediatric patients. The safety and pharmacokinetics of gemcitabine were evaluated in a trial in pediatric patients with refractory leukemia. The maximum tolerated dose was 10 mg/m2/min for 360 minutes three times weekly followed by a one-week rest period. The safety and activity of gemcitabine for injection were evaluated in a trial of pediatric patients with relapsed acute lymphoblastic leukemia (22 patients) and acute myelogenous leukemia (10 patients) at a dose of 10 mg/m2/min administered over 360 minutes three times weekly followed by a one-week rest period. Toxicities observed included bone marrow suppression, febrile neutropenia, elevation of serum transaminases, nausea, and rash/desquamation. No meaningful clinical activity was observed in this trial.
8.5 Geriatric Use
In clinical studies of gemcitabine for injection, enrolling 979 patients with various cancers who received gemcitabine for injection as a single agent, no overall differences in safety were observed between patients aged 65 and older and younger patients, with the exception of a higher rate of Grade 3-4 thrombocytopenia in older patients as compared to younger patients. In a randomized trial in women with ovarian cancer, 175 women received gemcitabine for injection plus carboplatin, of which 29% were age 65 years or older. Similar effectiveness was observed between older and younger women. There was significantly higher Grade 3/4 neutropenia in women 65 years of age or older.
Gemcitabine for injection clearance is affected by age, however there are no recommended dose adjustments based on patients’ age [see Clinical Pharmacology (12.3)].
8.6 Renal Impairment
No clinical studies have been conducted with gemcitabine in patients with decreased renal function.
8.7 Hepatic Impairment
No clinical studies have been conducted with gemcitabine in patients with decreased hepatic function.
8.8 Gender
Gemcitabine for injection clearance is affected by gender. [see Clinical Pharmacology (12.3)]. In single-agent studies of gemcitabine for injection women, especially older women, were more likely not to proceed to a subsequent cycle and to experience Grade 3/4 neutropenia and thrombocytopenia.
- 10 OVERDOSAGE
-
11 DESCRIPTION
Gemcitabine for injection, USP is a nucleoside metabolic inhibitor that exhibits antitumor activity. Gemcitabine HCl USP is 2´-deoxy-2´,2´-difluorocytidine monohydrochloride (β-isomer).
The structural formula is as follows:
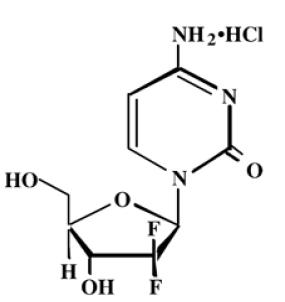
The molecular formula for gemcitabine HCl is C9H11F2N3O4 HCl. It has a molecular weight of 299.66.
Gemcitabine HCl USP is a white to off-white solid. It is soluble in water, slightly soluble in methanol, and practically insoluble in ethanol and polar organic solvents.
Gemcitabine for Injection is supplied in a sterile form for intravenous use only. Vials of gemcitabine for injection, USP contain either 200 mg or 1 g of gemcitabine HCl USP (expressed as free base) formulated with mannitol (200 mg or 1 g, respectively) and sodium acetate trihydrate (20.73 mg or 103.5 mg), or sodium acetate (12.5 mg or 62.5 mg), respectively as a sterile lyophilized powder. Hydrochloric acid and/or sodium hydroxide may have been added for pH adjustment.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Gemcitabine kills cells undergoing DNA synthesis and blocks the progression of cells through the G1/S-phase boundary. Gemcitabine is metabolized by nucleoside kinases to diphosphate (dFdCDP) and triphosphate (dFdCTP) nucleosides. Gemcitabine diphosphate inhibits ribonucleotide reductase, an enzyme responsible for catalyzing the reactions that generate deoxynucleoside triphosphates for DNA synthesis, resulting in reductions in deoxynucleotide concentrations, including dCTP. Gemcitabine triphosphate competes with dCTP for incorporation into DNA. The reduction in the intracellular concentration of dCTP by the action of the diphosphate enhances the incorporation of gemcitabine triphosphate into DNA (self-potentiation). After the gemcitabine nucleotide is incorporated into DNA, only one additional nucleotide is added to the growing DNA strands, which eventually results in the initiation of apoptotic cell death.
12.3 Pharmacokinetics
Absorption and Distribution
The pharmacokinetics of gemcitabine were examined in 353 patients, with various solid tumors. Pharmacokinetic parameters were derived using data from patients treated for varying durations of therapy given weekly with periodic rest weeks and using both short infusions (<70 minutes) and long infusions (70 to 285 minutes). The total gemcitabine for injection dose varied from 500 to 3600 mg/m2.
The volume of distribution was increased with infusion length. Volume of distribution of gemcitabine was 50 L/m2 following infusions lasting <70 minutes. For long infusions, the volume of distribution rose to 370 L/m2.
Metabolism
Gemcitabine disposition was studied in 5 patients who received a single 1000 mg/m2/30 minute infusion of radiolabeled drug. Within one (1) week, 92% to 98% of the dose was recovered, almost entirely in the urine. Gemcitabine (<10%) and the inactive uracil metabolite, 2´-deoxy-2´,2´-difluorouridine (dFdU), accounted for 99% of the excreted dose. The metabolite dFdU is also found in plasma.
The active metabolite, gemcitabine triphosphate, can be extracted from peripheral blood mononuclear cells. The half-life of the terminal phase for gemcitabine triphosphate from mononuclear cells ranges from 1.7 to 19.4 hours.
Elimination
Clearance of gemcitabine was affected by age and gender. The lower clearance in women and the elderly results in higher concentrations of gemcitabine for any given dose. Differences in either clearance or volume of distribution based on patient characteristics or the duration of infusion result in changes in half-life and plasma concentrations. Table 10 shows plasma clearance and half-life of gemcitabine following short infusions for typical patients by age and gender.
Table 10: Gemcitabine Clearance and Half–Life for the “Typical” Patient
Age Clearance Men
(L/hr/m2)Clearance Women
(L/hr/m2)Half–Lifea
Men (min)Half–Lifea
Women (min)29 92.2 69.4 42 49 45 75.7 57 48 57 65 55.1 41.5 61 73 79 40.7 30.7 79 94 aHalf–life for patients receiving < 70 minute infusion.
Gemcitabine half-life for short infusions ranged from 42 to 94 minutes, and the value for long infusions varied from 245 to 638 minutes, depending on age and gender, reflecting a greatly increased volume of distribution with longer infusions.
Drug Interactions
When gemcitabine for injection (1250 mg/m2 on Days 1 and 8) and cisplatin (75 mg/m2 on Day 1) were administered in NSCLC patients, the clearance of gemcitabine on Day 1 was 128 L/hr/m2 and on Day 8 was 107 L/hr/m2. Analysis of data from metastatic breast cancer patients shows that, on average, gemcitabine for injection has little or no effect on the pharmacokinetics (clearance and half-life) of paclitaxel and paclitaxel has little or no effect on the pharmacokinetics of gemcitabine. Data from NSCLC patients demonstrate that gemcitabine for injection and carboplatin given in combination does not alter the pharmacokinetics of gemcitabine or carboplatin compared to administration of either single-agent. However, due to wide confidence intervals and small sample size, interpatient variability may be observed.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment Of Fertility
Long-term animal studies to evaluate the carcinogenic potential of gemcitabine for injection have not been conducted. Gemcitabine was mutagenic in an in vitro mouse lymphoma (L5178Y) assay and was clastogenic in an in vivo mouse micronucleus assay. Gemcitabine IP doses of 0.5 mg/kg/day (about 1/700 the human dose on a mg/m2 basis) in male mice had an effect on fertility with moderate to severe hypospermatogenesis, decreased fertility, and decreased implantations. In female mice, fertility was not affected but maternal toxicities were observed at 1.5 mg/kg/day administered intravenously (about 1/200 the human dose on a mg/m2 basis) and fetotoxicity or embryolethality was observed at 0.25 mg/kg/day administered intravenously (about 1/1300 the human dose on a mg/m2 basis).
-
14 CLINICAL STUDIES
14.1 Ovarian Cancer
The safety and efficacy of gemcitabine for injection was studied in a randomized trial of 356 women with advanced ovarian cancer that had relapsed at least 6 months after first-line platinum-based therapy. Patients were randomized to receive either gemcitabine for injection 1000 mg/m2 on Days 1 and 8 of a 21-day cycle and carboplatin AUC 4 administered after gemcitabine for injection infusion on Day 1 of each cycle (n=178) or to carboplatin AUC 5 administered on Day 1 of each 21-day cycle (n=178). The primary efficacy outcome measure was progression free survival (PFS).
Patient characteristics are shown in Table 11. The addition of gemcitabine for injection to carboplatin resulted in statistically significant improvements in PFS and overall response rate as shown in Table 12 and Figure 1. Approximately 75% of patients in each arm received additional chemotherapy for disease progression; 13 of 120 patients in the carboplatin alone arm received gemcitabine for injection for treatment of disease progression. There was no significant difference in overall survival between the treatment arms.
Table 11: Randomized Trial of Gemcitabine For Injection plus Carboplatin versus Carboplatin in Ovarian Cancer - Baseline Demographics and Clinical Characteristics
Gemcitabine For Injection/Carboplatin Carboplatin Number of randomized patients 178 178 Median age, years 59 58 Range 36 to 78 21 to 81 Baseline ECOG performance status 0 to 1a 94% 95% Disease Status Evaluable 8% 3% Bidimensionally measurable 92% 96% Platinum–free intervalb 6 to 12 months 40% 40% >12 months 59% 60% First–line therapy Platinum–taxane combination 70% 71% Platinum–non–taxane combination 29% 28% Platinum monotherapy 1% 1% a 5 patients on gemcitabine for injection plus carboplatin arm and 4 patients on carboplatin arm with no baseline Eastern Cooperative Oncology Group (ECOG) performance status.
b 2 on gemcitabine for injection plus carboplatin arm and 1 on carboplatin arm had platinum-free interval <6 months.
Table 12: Randomized Trial of Gemcitabine For Injection plus Carboplatin versus Carboplatin in Ovarian Cancer - Efficacy Outcomes
Gemcitabine For Injection/Carboplatin(N=178) Carboplatin(N=178) Progression-free Survival
Median (95% CIa) months
8.6 (8, 9.7) 5.8 (5.2, 7.1) Hazard Ratio (95%, C.I.) 0.72 (0.57, 0.90) p-valueb p=0.0038 Overall Survival
Median (95% CI) months
18 (16.2, 20.3) 17.3 (15.2, 19.3) Hazard Ratio (95% CI) 0.98 (0.78, 1.24) p-valueb p=0.8977 Investigator Reviewed
Overall Response Rate47.2% 30.9% p-valuee p=0.0016 CRd
PR plus PRNMe14.6%
32.6%6.2%
24.7%Independently Reviewed Overall Response Ratef 46.3% 35.6% p-valuee p=0.11 CRd
PR plus PRNMe9.1%
37.2%4%
31.7%a CI=confidence interval
b Complete response
c Partial response plus partial response, non-measurable disease
d log Rank, unadjusted
e chi Square
f Independently reviewed cohort –gemcitabine for injection/carboplatin (n=121), carboplatin (n=101); independent reviewers unable to measure disease detected by sonography or physical exam
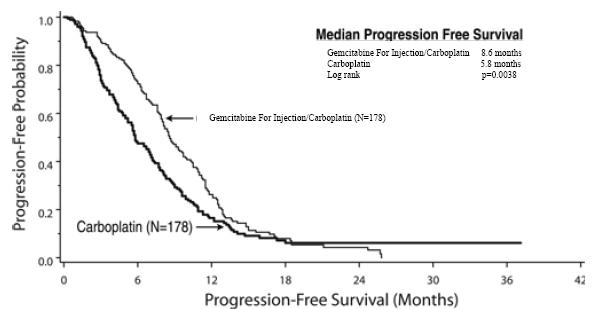
Figure 1: Kaplan–Meier Curve of Progression Free Survival in Gemcitabine For Injection Plus Carboplatin Versus Carboplatin in Ovarian Cancer (N=356)
14.2 Breast Cancer
The safety and efficacy of gemcitabine for injection were evaluated in a multi-national, randomized, open-label trial conducted in women receiving initial treatment for metastatic breast cancer in women who have received prior adjuvant/neoadjuvant anthracycline chemotherapy unless clinically contraindicated. Patients were randomized to receive gemcitabine for injection 1250 mg/m2 on Days 1 and 8 of a 21-day cycle and paclitaxel 175 mg/m2 administered prior to gemcitabine for injection on Day 1 of each cycle (n=267) or to receive paclitaxel 175 mg/m2 was administered on Day 1 of each 21-day cycle (n=262). The primary efficacy outcome measure was time to documented disease progression.
Table 13: Randomized Trial of Gemcitabine For Injection plus Paclitaxel versus Paclitaxel in Breast Cancer
Gemcitabine For Injection/Paclitaxel Paclitaxel Number of patients 267 262 Demographic/Entry Characteristics
Median age (years)
Range53
26 to 8352
26 to 75Metastatic disease 97% 97% Baseline KPSa ≥90 70% 74% Number of tumor sites
1 to 2
≥ 357%
43%59%
41%Visceral disease 73% 73% Prior anthracycline 97% 96% Efficacy Outcomes Time to Documented Disease Progressionb Median in months (95% CI) 5.2 (4.2, 5.6) 2.9 (2.6, 3.7) Hazard Ratio (95% CI) 0.650 (0.524, 0.805) p-value p<0.0001 Overall Survivalc Median Survival in months (95% CI) 18.6 (16.5, 20.7) 15.8 (14.1, 17.3) Hazard Ratio (95% CI) 0.86 (0.71, 1.04) p-value Not Significant Overall Response Rate (95% CI) 40.8% (34.9, 46.7) 22.1% (17.1, 27.2) p-value p<0.0001 a Karnofsky Performance Status.
b These represent reconciliation of investigator and Independent Review Committee assessments according to a predefined algorithm. c Based on the ITT population
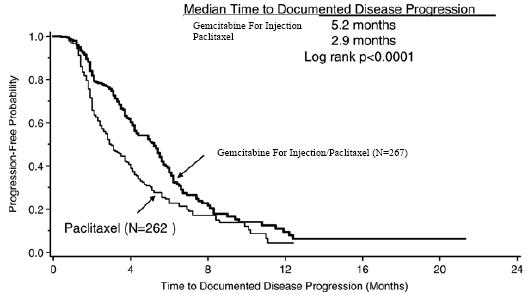
Figure 2: Kaplan–Meier Curve of Time to Documented Disease Progression in Gemcitabine For Injection Plus Paclitaxel versus Paclitaxel Breast Cancer Study (N=529)
14.3 Non-Small Cell Lung Cancer (NSCLC)
The safety and efficacy of gemcitabine for injection was evaluated in two randomized, multicenter trials.
28-Day Schedule
A multinational, randomized trial compared gemcitabine for injection plus cisplatin to cisplatin alone in the treatment of patients with inoperable Stage IIIA, IIIB, or IV NSCLC who had not received prior chemotherapy. Patients were randomized to receive gemcitabine for injection 1000 mg/m2 on Days 1, 8, and 15 of a 28-day cycle with cisplatin 100 mg/m2 administered on Day 1 of each cycle or to receive cisplatin 100 mg/m2 on Day 1 of each 28-day cycle. The primary efficacy outcome measure was overall survival. A total of 522 patients were enrolled at clinical centers in Europe, the US, and Canada. Patient demographics and baseline characteristics (shown in Table 13) were similar between arms with the exception of histologic subtype of NSCLC, with 48% of patients on the cisplatin arm and 37% of patients on the gemcitabine for injection plus cisplatin arm having adenocarcinoma. Efficacy results are presented in Table 13 and Figure 3 for overall survival.
21-Day Schedule
A randomized (1:1), multicenter trial was conducted in 135 patients with Stage IIIB or IV NSCLC. Patients were randomized to receive gemcitabine for injection 1250 mg/m2 on Days 1 and 8, and cisplatin 100 mg/m2 on Day 1 of a 21-day cycle or to receive etoposide 100 mg/m2 intravenously on Days 1, 2, and 3 and cisplatin 100 mg/m2 on Day 1 of a 21 -day cycle.
There was no significant difference in survival between the two treatment arms (Log rank p=0.18, two-sided). The median survival was 8.7 months for the gemcitabine for injection plus cisplatin arm versus 7 months for the etoposide plus cisplatin arm. Median time to disease progression for the gemcitabine for injection plus cisplatin arm was 5 months compared to 4.1 months on the etoposide plus cisplatin arm (Log rank p=0.015, two-sided). The objective response rate for the gemcitabine for injection plus cisplatin arm was 33% compared to 14% on the etoposide plus cisplatin arm (Fisher’s Exact p=0.01, two-sided).
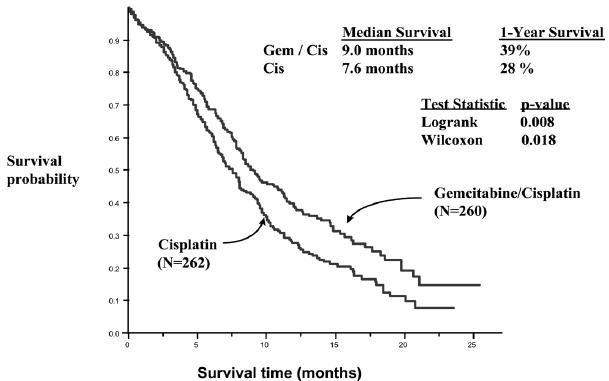
Figure 3: Kaplan-Meier Survival Curve in Gemcitabine for injection Plus Cisplatin versus Cisplatin in patients with NSCLC Study (N=522)
Table 14: Randomized Trials of Gemcitabine For Injection plus Cisplatin in Patients with NSCLC
a 28–day schedule — Gemcitabine for injection plus cisplatin: Gemcitabine for injection 1000 mg/m2 on Days 1, 8, and 15 and cisplatin 100 mg/m2 on Day 1 every 28 days; Single–agent cisplatin: cisplatin 100 mg/m2 on Day 1 every 28 days.
b 21–day schedule — Gemcitabine for injection plus cisplatin: Gemcitabine for injection 1250 mg/m2 on Days 1 and 8 and cisplatin 100 mg/m2 on Day 1 every 21 days; Etoposide plus Cisplatin: cisplatin 100 mg/m2 on Day 1 and intravenous etoposide 100 mg/m2 on Days 1, 2, and 3 every 21 days.
c N/A Not applicable
d Karnofsky Performance Status.
e CI=confidence intervals
f p-value two-sided Fisher’s Exact test for difference in binomial proportions; log rank test for time-to-event analyses.
14.4 Pancreatic Cancer
The safety and efficacy of gemcitabine for injection was evaluated in two trials, a randomized, single-blind, two-arm, active-controlled trial conducted in patients with locally advanced or metastatic pancreatic cancer who had received no prior chemotherapy and in a single-arm, open-label, multicenter trial conducted in patients with locally advanced or metastatic pancreatic cancer previously treated with 5-FU or a 5-FU-containing regimen. The first trial randomized patients to receive gemcitabine for injection 1000 mg/m2 intravenously over 30 minutes once weekly for 7 weeks followed by a one-week rest, then once weekly dosing for 3 consecutive weeks every 28-days in subsequent cycles (n=63) or to 5-fluorouracil (5-FU) 600 mg/m2 intravenously over 30 minutes once weekly (n=63). In the second trial, all patients received gemcitabine for injection 1000 mg/m2 intravenously over 30 minutes once weekly for 7 weeks followed by a one-week rest, then once weekly dosing for 3 consecutive weeks every 28-days in subsequent cycles.
The primary efficacy outcome measure in both trials was "clinical benefit response". A patient was considered to have had a clinical benefit response if either occurred:
The patient achieved a ≥50% reduction in pain intensity (Memorial Pain Assessment Card) or analgesic consumption, or a 20-point or greater improvement in performance status (Karnofsky Performance Status) for a period of at least 4 consecutive weeks, without showing any sustained worsening in any of the other parameters. Sustained worsening was defined as 4 consecutive weeks with either any increase in pain intensity or analgesic consumption or a 20-point decrease in performance status occurring during the first 12 weeks of therapy.
OR
The patient was stable on all of the aforementioned parameters, and showed a marked, sustained weight gain (≥7% increase maintained for ≥4 weeks) not due to fluid accumulation.
The randomized trial enrolled 126 patients across 17 sites in the US and Canada. The demographic and entry characteristics were similar between the arms (Table 15). The efficacy outcome results are shown in Table 15 and for overall survival in Figure 4. Patients treated with gemcitabine for injection had statistically significant increases in clinical benefit response, survival, and time to disease progression compared to those randomized to receive 5-FU. No confirmed objective tumor responses were observed in either treatment arm.
Table 15: Randomized Trial of Gemcitabine For Injection versus 5-Fluorouracil in Pancreatic Cancer
Gemcitabine For Injection 5–FU Number of patients 63 63 Demographic/Entry Characteristics Male 54% 54% Median age 62 years 61 years Range 37 to 79 36 to 77 Stage IV disease 71% 76% Baseline KPSa ≤ 70 70% 68% Efficacy Outcomes Clinical benefit response 22.2% 4.8% p-valueb p=0.004 Survival Median 5.7 months 4.2 months (95% CI) (4.7, 6.9) (3.1, 5.1) p-valueb p=0.0009 Time Disease Progression Median 2.1 months 0.9 months (95% CI) (1.9, 3.4) (0.9, 1.1) p-value b p=0.0013 a Karnofsky Performance Status.
b p-value for clinical benefit response calculated using the two-sided test for difference in binomial proportions. All other p-values are calculated using log rank test.
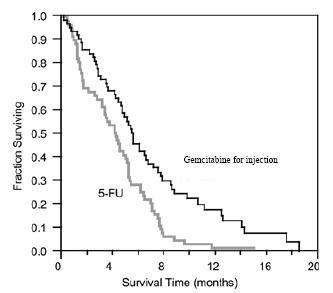
Figure 4: Kaplan-Meier Survival Curve
-
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
Gemcitabine for Injection, USP is available in sterile single-use vials individually packaged in a carton containing:
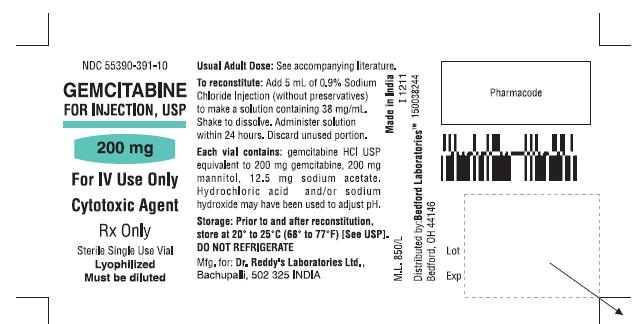
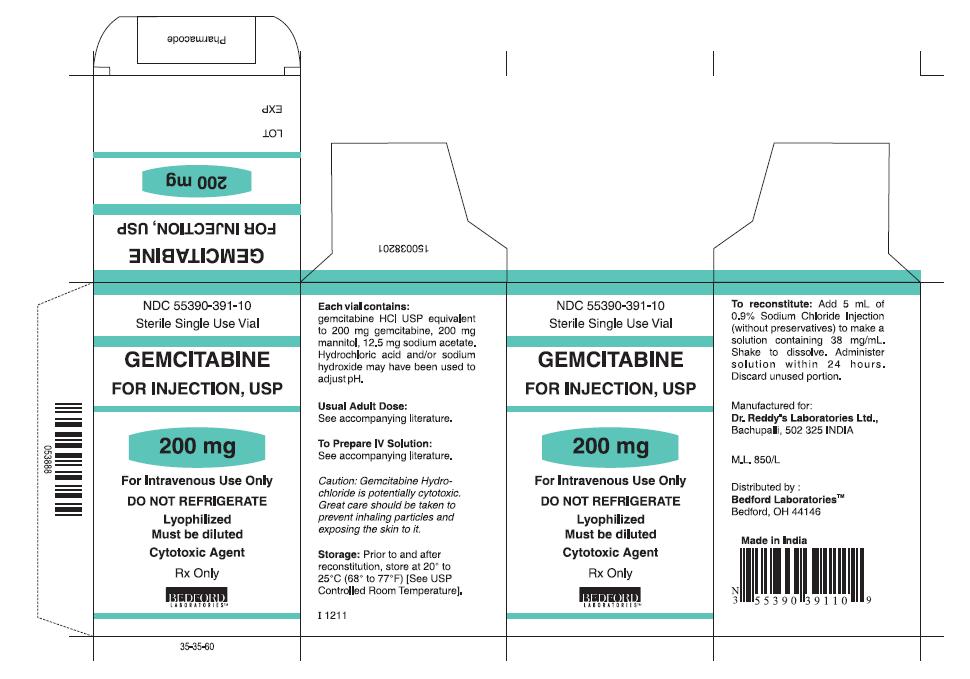
200 mg white, lyophilized powder in a sterile single-use vial - NDC: 55390-391-10.
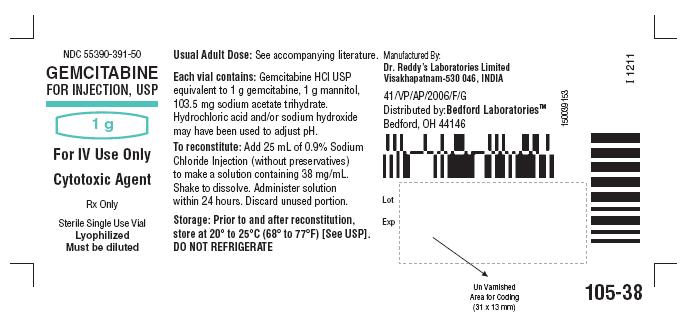
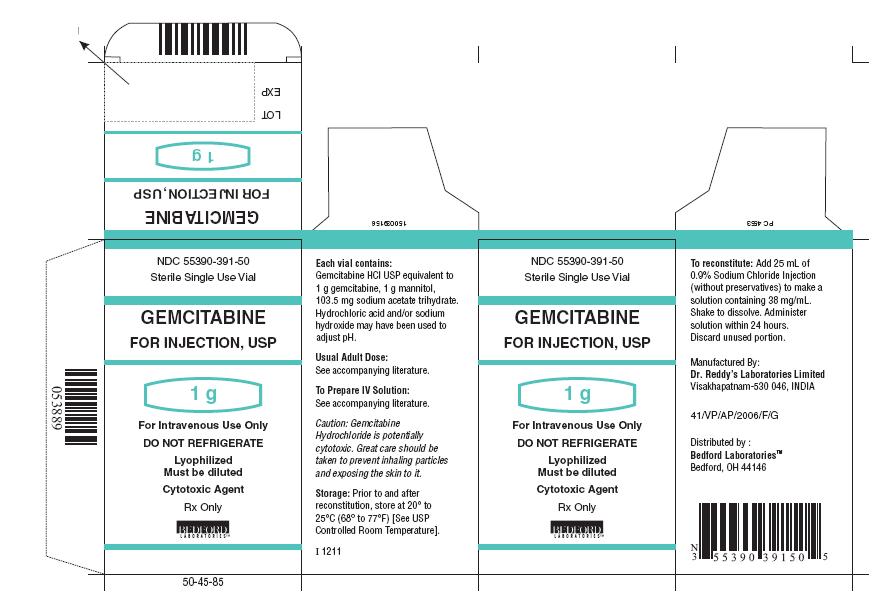
1 g white, lyophilized powder in a sterile single-use vial – 55390-391-50.
-
17 PATIENT COUNSELING INFORMATION
- Advise patients of the risks of low blood cell counts and the potential need for blood transfusions and increased susceptibility to infections. Instruct patients to immediately contact their healthcare provided for development of signs or symptoms of infection, fever, prolonged or unexpected bleeding, bruising, or shortness of breath [see Warnings and Precautions (5.2)]
- Advise patients of the risks of pulmonary toxicity including respiratory failure and death. Instruct patients to immediately contact their healthcare provider for development of shortness of breath, wheezing, or cough [see Warnings and Precautions (5.3)]
- Advise patients of the risks of hemolytic-uremic syndrome and associated renal failure. Instruct patients to immediately contact their healthcare provider for changes in the color or volume of urine output or for increased bruising or bleeding [see Warnings and Precautions (5.4)]
- Advise patients of the risks of hepatic toxicity including liver failure and death. Instruct patients to immediately contact their healthcare provider for signs of jaundice or for pain/tenderness in the right upper abdominal quadrant [see Warnings and Precautions (5.5)]
-
SPL UNCLASSIFIED SECTION
Rx Only
Manufactured by:
Dr. Reddy’s Laboratories Limited
Visakhapatnam - 530 046 INDIA
Distributed by:
Bedford Laboratories
TM Bedford, OH 44146
or
Manufactured for:
Dr. Reddy’s Laboratories Limited
BachupallY – 500 090 INDIA
Distributed by:
Bedford LaboratoriesTM
Bedford, OH 44146
Made in India
Revised: 0514
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL SECTION
- PRINCIPAL DISPLAY PANEL
- PRINCIPAL DISPLAY PANEL
- PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
GEMCITABINE
gemcitabine injection, powder, lyophilized, for solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 55390-391 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength gemcitabine hydrochloride (UNII: U347PV74IL) (gemcitabine - UNII:B76N6SBZ8R) gemcitabine 40 mg in 1 mL Inactive Ingredients Ingredient Name Strength mannitol (UNII: 3OWL53L36A) sodium acetate (UNII: 4550K0SC9B) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 55390-391-10 1 in 1 CARTON 1 5 mL in 1 VIAL, SINGLE-USE 2 NDC: 55390-391-50 1 in 1 CARTON 2 25 mL in 1 VIAL, SINGLE-USE Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA091365 03/19/2012 Labeler - Bedford Laboratories (884528407) Registrant - Dr. Reddy's Laboratories Limited (650562841) Establishment Name Address ID/FEI Business Operations Dr. Reddy's Laboratories Limited-FTO7 650446243 manufacture(55390-391) , analysis(55390-391)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.