AMLODIPINE AND VALSARTAN tablet, film coated
AMLODIPINE AND VALSARTAN by
Drug Labeling and Warnings
AMLODIPINE AND VALSARTAN by is a Prescription medication manufactured, distributed, or labeled by Mylan Pharmaceuticals Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use AMLODIPINE AND VALSARTAN TABLETS safely and effectively. See full prescribing information for AMLODIPINE AND VALSARTAN TABLETS.
AMLODIPINE and VALSARTAN tablets, for oral use
Initial U.S. Approval: 2007INDICATIONS AND USAGE
Amlodipine and valsartan is the combination tablet of amlodipine, a dihydropyridine calcium channel blocker (DHP CCB), and valsartan, an angiotensin II receptor blocker (ARB). Amlodipine and valsartan tablets are indicated for the treatment of hypertension, to lower blood pressure:
- In patients not adequately controlled on monotherapy (1)
- As initial therapy in patients likely to need multiple drugs to achieve their blood pressure goals (1)
Lowering blood pressure reduces the risk of fatal and nonfatal cardiovascular events, primarily strokes and myocardial infarctions.
DOSAGE AND ADMINISTRATION
General Considerations:
- Majority of effect attained within 2 weeks (2.1)
- May be administered with other antihypertensive agents (2.1)
Hypertension:
- May be used as add-on therapy for patients not controlled on monotherapy (2.2)
- Patients who experience dose-limiting adverse reactions on monotherapy may be switched to amlodipine and valsartan tablets containing a lower dose of that component (2.2)
- May be substituted for titrated components (2.3)
- When used as initial therapy: Initiate with 5/160 mg, then titrate upwards as necessary to a maximum of 10/320 mg once daily (2.4)
DOSAGE FORMS AND STRENGTHS
Tablets (amlodipine/valsartan mg): 5/160, 10/160, 5/320, 10/320 (3)
CONTRAINDICATIONS
Known hypersensitivity to any component;
Do not coadminister aliskiren with amlodipine and valsartan tablets in patients with diabetes (4)
WARNINGS AND PRECAUTIONS
ADVERSE REACTIONS
In placebo-controlled clinical trials, discontinuation due to side effects occurred in 1.8% of patients in the amlodipine and valsartan tablet-treated patients and 2.1% in the placebo-treated group. The most common reasons for discontinuation of therapy with amlodipine and valsartan tablets were peripheral edema and vertigo. The adverse experiences that occurred in clinical trials (≥ 2% of patients) at a higher incidence than placebo included peripheral edema, nasopharyngitis, upper respiratory tract infection, and dizziness. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Mylan at 1-877-446-3679 (1-877-4-INFO-RX) or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
- If simvastatin is coadministered with amlodipine, do not exceed doses greater than 20 mg daily of simvastatin (7)
- NSAID use may lead to increased risk of renal impairment and loss of antihypertensive effect (7)
- Dual inhibition of the renin-angiotensin system: Increased risk of renal impairment, hypotension, and hyperkalemia (7)
- Lithium: Increases in serum lithium level and lithium toxicity (7)
USE IN SPECIFIC POPULATIONS
Lactation: Breastfeeding is not recommended (8.2)
Geriatric Patients: Not recommended for initial therapy (8.5)
Hepatic Impairment: Not recommended for initial therapy (8.7)See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 7/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: FETAL TOXICITY
1 INDICATIONS AND USAGE
1.1 Hypertension
2 DOSAGE AND ADMINISTRATION
2.1 General Considerations
2.2 Add-on Therapy
2.3 Replacement Therapy
2.4 Initial Therapy
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Fetal Toxicity
5.2 Hypotension
5.3 Risk of Myocardial Infarction or Increased Angina
5.4 Impaired Renal Function
5.5 Hyperkalemia
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
- BOXED WARNING (What is this?)
-
1 INDICATIONS AND USAGE
1.1 Hypertension
Amlodipine and valsartan tablets are indicated for the treatment of hypertension, to lower blood pressure. Lowering blood pressure reduces the risk of fatal and nonfatal cardiovascular events, primarily strokes and myocardial infarctions. These benefits have been seen in controlled trials of antihypertensive drugs from a wide variety of pharmacologic classes, including amlodipine and the ARB class to which valsartan principally belongs. There are no controlled trials demonstrating risk reduction with amlodipine and valsartan tablets.
Control of high blood pressure should be part of comprehensive cardiovascular risk management, including, as appropriate, lipid control, diabetes management, antithrombotic therapy, smoking cessation, exercise, and limited sodium intake. Many patients will require more than 1 drug to achieve blood pressure goals. For specific advice on goals and management, see published guidelines, such as those of the National High Blood Pressure Education Program’s Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC).
Numerous antihypertensive drugs, from a variety of pharmacologic classes and with different mechanisms of action, have been shown in randomized controlled trials to reduce cardiovascular morbidity and mortality, and it can be concluded that it is blood pressure reduction, and not some other pharmacologic property of the drugs, that is largely responsible for those benefits. The largest and most consistent cardiovascular outcome benefit has been a reduction in the risk of stroke, but reductions in myocardial infarction and cardiovascular mortality also have been seen regularly.
Elevated systolic or diastolic pressure causes increased cardiovascular risk, and the absolute risk increase per mmHg is greater at higher blood pressures, so that even modest reductions of severe hypertension can provide substantial benefit. Relative risk reduction from blood pressure reduction is similar across populations with varying absolute risk, so the absolute benefit is greater in patients who are at higher risk independent of their hypertension (for example, patients with diabetes or hyperlipidemia), and such patients would be expected to benefit from more aggressive treatment to a lower blood pressure goal.
Some antihypertensive drugs have smaller blood pressure effects (as monotherapy) in black patients, and many antihypertensive drugs have additional approved indications and effects (e.g., on angina, heart failure, or diabetic kidney disease). These considerations may guide selection of therapy. Amlodipine and valsartan tablets are indicated for the treatment of hypertension.
Amlodipine and valsartan tablets may be used in patients whose blood pressure is not adequately controlled on either monotherapy.
Amlodipine and valsartan tablets may also be used as initial therapy in patients who are likely to need multiple drugs to achieve their blood pressure goals.
The choice of amlodipine and valsartan tablets as initial therapy for hypertension should be based on an assessment of potential benefits and risks including whether the patient is likely to tolerate the lowest dose of amlodipine and valsartan tablets.
Patients with stage 2 hypertension (moderate or severe) are at a relatively higher risk for cardiovascular events (such as strokes, heart attacks, and heart failure), kidney failure and vision problems, so prompt treatment is clinically relevant. The decision to use a combination as initial therapy should be individualized and should be shaped by considerations such as baseline blood pressure, the target goal and the incremental likelihood of achieving goal with a combination compared to monotherapy. Individual blood pressure goals may vary based upon the patient’s risk.
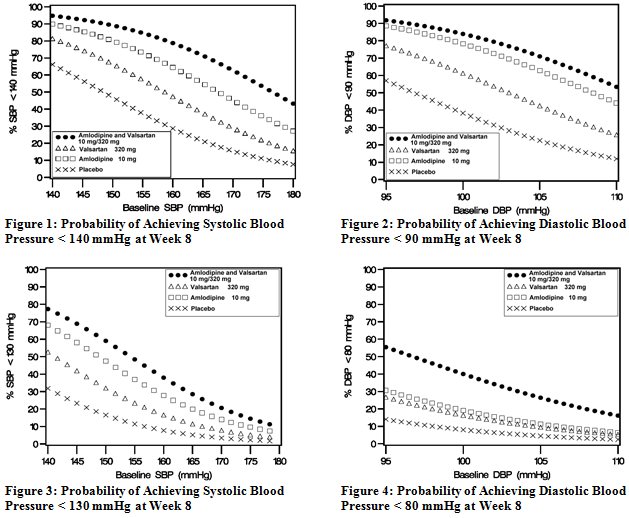
Data from the high-dose multifactorial study [see Clinical Studies (14)] provide estimates of the probability of reaching a blood pressure goal with amlodipine and valsartan tablets compared to amlodipine or valsartan monotherapy. The figures below provide estimates of the likelihood of achieving systolic or diastolic blood pressure control with amlodipine and valsartan tablets 10/320 mg, based upon baseline systolic or diastolic blood pressure. The curve of each treatment group was estimated by logistic regression modeling. The estimated likelihood at the right tail of each curve is less reliable due to small numbers of subjects with high baseline blood pressures.
For example, a patient with a baseline blood pressure of 160/100 mmHg has about a 67% likelihood of achieving a goal of < 140 mmHg (systolic) and 80% likelihood of achieving < 90 mmHg (diastolic) on amlodipine alone, and the likelihood of achieving these goals on valsartan alone is about 47% (systolic) or 62% (diastolic). The likelihood of achieving these goals on amlodipine and valsartan tablets rises to about 80% (systolic) or 85% (diastolic). The likelihood of achieving these goals on placebo is about 28% (systolic) or 37% (diastolic).
-
2 DOSAGE AND ADMINISTRATION
2.1 General Considerations
Dose once daily. The dosage can be increased after 1 to 2 weeks of therapy to a maximum of one 10/320 mg tablet once daily as needed to control blood pressure. The majority of the antihypertensive effect is attained within 2 weeks after initiation of therapy or a change in dose.
Amlodipine and valsartan tablets may be administered with other antihypertensive agents.
2.2 Add-on Therapy
A patient whose blood pressure is not adequately controlled with amlodipine (or another dihydropyridine calcium-channel blocker) alone or with valsartan (or another angiotensin II receptor blocker) alone may be switched to combination therapy with amlodipine and valsartan tablets.
A patient who experiences dose-limiting adverse reactions on either component alone may be switched to amlodipine and valsartan tablets containing a lower dose of that component in combination with the other to achieve similar blood pressure reductions. The clinical response to amlodipine and valsartan tablets should be subsequently evaluated and if blood pressure remains uncontrolled after 3 to 4 weeks of therapy, the dose may be titrated up to a maximum of 10/320 mg.
-
3 DOSAGE FORMS AND STRENGTHS
Amlodipine and Valsartan Tablets, USP are available containing 6.94 mg or 13.88 mg of amlodipine besylate, USP equivalent to 5 mg or 10 mg of amlodipine free base, respectively, with 160 mg or 320 mg of valsartan, USP providing for the following available combinations: 5 mg/160 mg, 10 mg/160 mg, 5 mg/320 mg or 10 mg/320 mg.
- The 5 mg/160 mg tablets are light orange, film-coated, oval, unscored tablets debossed with MX1 on one side of the tablet and blank on the other side.
- The 10 mg/160 mg tablets are tan, film-coated, oval, unscored tablets debossed with MX2 on one side of the tablet and blank on the other side.
- The 5 mg/320 mg tablets are orange, film-coated, capsule-shaped, unscored tablets debossed with MX43 on one side of the tablet and blank on the other side.
- The 10 mg/320 mg tablets are light orange, film-coated, capsule-shaped, unscored tablets debossed with MX44 on one side of the tablet and blank on the other side.
-
4 CONTRAINDICATIONS
Do not use in patients with known hypersensitivity to any component.
Do not coadminister aliskiren with amlodipine and valsartan tablets in patients with diabetes [see Drug Interactions (7)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Fetal Toxicity
Amlodipine and valsartan tablets can cause fetal harm when administered to a pregnant woman. Use of drugs that act on the renin-angiotensin system during the second and third trimesters of pregnancy reduces fetal renal function and increases fetal and neonatal morbidity and death. Resulting oligohydramnios can be associated with fetal lung hypoplasia and skeletal deformations. Potential neonatal adverse effects include skull hypoplasia, anuria, hypotension, renal failure, and death. When pregnancy is detected, discontinue amlodipine and valsartan tablets as soon as possible [see Use in Specific Populations (8.1)].
5.2 Hypotension
Excessive hypotension was seen in 0.4% of patients with uncomplicated hypertension treated with amlodipine and valsartan tablets in placebo-controlled studies. In patients with an activated renin-angiotensin system, such as volume- and/or salt-depleted patients receiving high doses of diuretics, symptomatic hypotension may occur in patients receiving angiotensin receptor blockers. Volume depletion should be corrected prior to administration of amlodipine and valsartan tablets. Treatment with amlodipine and valsartan tablets should start under close medical supervision.
Initiate therapy cautiously in patients with heart failure or recent myocardial infarction and in patients undergoing surgery or dialysis. Patients with heart failure or post-myocardial infarction patients given valsartan commonly have some reduction in blood pressure, but discontinuation of therapy because of continuing symptomatic hypotension usually is not necessary when dosing instructions are followed. In controlled trials in heart failure patients, the incidence of hypotension in valsartan-treated patients was 5.5% compared to 1.8% in placebo-treated patients. In the Valsartan in Acute Myocardial Infarction Trial (VALIANT), hypotension in post-myocardial infarction patients led to permanent discontinuation of therapy in 1.4% of valsartan-treated patients and 0.8% of captopril-treated patients.
Since the vasodilation induced by amlodipine is gradual in onset, acute hypotension has rarely been reported after oral administration. Nonetheless, caution, as with any other peripheral vasodilator, should be exercised when administering amlodipine, particularly in patients with severe aortic stenosis.
If excessive hypotension occurs with amlodipine and valsartan tablets, place the patient in a supine position and, if necessary, give intravenous normal saline. A transient hypotensive response is not a contraindication to further treatment, which usually can be continued without difficulty once the blood pressure has stabilized.
5.3 Risk of Myocardial Infarction or Increased Angina
Worsening angina and acute myocardial infarction can develop after starting or increasing the dose of amlodipine, particularly in patients with severe obstructive coronary artery disease.
5.4 Impaired Renal Function
Changes in renal function including acute renal failure can be caused by drugs that inhibit the renin-angiotensin system and by diuretics. Patients whose renal function may depend in part on the activity of the renin-angiotensin system (e.g., patients with renal artery stenosis, chronic kidney disease, severe congestive heart failure, or volume depletion) may be at particular risk of developing acute renal failure on amlodipine and valsartan tablets. Monitor renal function periodically in these patients. Consider withholding or discontinuing therapy in patients who develop a clinically significant decrease in renal function on amlodipine and valsartan tablets [see Drug Interactions (7)].
5.5 Hyperkalemia
Drugs that inhibit the renin-angiotensin system can cause hyperkalemia. Monitor serum electrolytes periodically.
Some patients with heart failure have developed increases in potassium with valsartan therapy. These effects are usually minor and transient, and they are more likely to occur in patients with pre-existing renal impairment. Dosage reduction and/or discontinuation of amlodipine and valsartan tablets may be required [see Adverse Reactions (6.1)].
-
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. The adverse reaction information from clinical trials does, however, provide a basis for identifying the adverse events that appear to be related to drug use and for approximating rates.
Studies with Amlodipine and Valsartan Tablets
Amlodipine and valsartan tablets have been evaluated for safety in over 2600 patients with hypertension; over 1440 of these patients were treated for at least 6 months and over 540 of these patients were treated for at least 1 year. Adverse reactions have generally been mild and transient in nature and have only infrequently required discontinuation of therapy.
The hazards [see Warnings and Precautions (5)] of valsartan are generally independent of dose; those of amlodipine are a mixture of dose-dependent phenomena (primarily peripheral edema) and dose-independent phenomena, the former much more common than the latter.
The overall frequency of adverse reactions was neither dose-related nor related to gender, age, or race. In placebo-controlled clinical trials, discontinuation due to side effects occurred in 1.8% of patients in the amlodipine and valsartan tablet-treated patients and 2.1% in the placebo-treated group. The most common reasons for discontinuation of therapy with amlodipine and valsartan tablets were peripheral edema (0.4%), and vertigo (0.2%).
The adverse reactions that occurred in placebo-controlled clinical trials in at least 2% of patients treated with amlodipine and valsartan tablets but at a higher incidence in amlodipine/valsartan patients (n = 1437) than placebo (n = 337) included peripheral edema (5.4% vs 3.0%), nasopharyngitis (4.3% vs 1.8%), upper respiratory tract infection (2.9% vs 2.1%) and dizziness (2.1% vs 0.9%).
Orthostatic events (orthostatic hypotension and postural dizziness) were seen in less than 1% of patients.
Studies with Valsartan
Diovan® has been evaluated for safety in more than 4000 hypertensive patients in clinical trials. In trials in which valsartan was compared to an ACE inhibitor with or without placebo, the incidence of dry cough was significantly greater in the ACE inhibitor group (7.9%) than in the groups who received valsartan (2.6%) or placebo (1.5%). In a 129-patient trial limited to patients who had had dry cough when they had previously received ACE inhibitors, the incidences of cough in patients who received valsartan, HCTZ, or lisinopril were 20%, 19%, and 69% respectively (p < 0.001).
Clinical Lab Test Findings
Creatinine
In heart failure patients, greater than 50% increases in creatinine were observed in 3.9% of valsartan-treated patients compared to 0.9% of placebo-treated patients. In post-myocardial infarction patients, doubling of serum creatinine was observed in 4.2% of valsartan-treated patients and 3.4% of captopril-treated patients.
Blood Urea Nitrogen (BUN)
In hypertensive patients, greater than 50% increases in BUN were observed in 5.5% of amlodipine and valsartan tablet-treated patients compared to 4.7% of placebo-treated patients. In heart failure patients, greater than 50% increases in BUN were observed in 16.6% of valsartan-treated patients compared to 6.3% of placebo-treated patients [see Warnings and Precautions (5.4)].
6.2 Postmarketing Experience
The following additional adverse reactions have been reported in postmarketing experience. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Amlodipine
Gynecomastia has been reported infrequently and a causal relationship is uncertain. Jaundice and hepatic enzyme elevations (mostly consistent with cholestasis or hepatitis), in some cases severe enough to require hospitalization, have been reported in association with use of amlodipine.
Valsartan
The following additional adverse reactions have been reported in postmarketing experience with valsartan:
Hypersensitivity: Angioedema has been reported. Some of these patients previously experienced angioedema with other drugs including ACE inhibitors. Diovan should not be re-administered to patients who have had angioedema.
Digestive: Elevated liver enzymes and reports of hepatitis
Musculoskeletal: Rhabdomyolysis
Renal: Impaired renal function, renal failure
Dermatologic: Alopecia, bullous dermatitis
Blood and Lymphatic: Thrombocytopenia
Vascular: Vasculitis
-
7 DRUG INTERACTIONS
No drug interaction studies have been conducted with amlodipine and valsartan tablets and other drugs, although studies have been conducted with the individual amlodipine and valsartan components.
Amlodipine: Impact of Other Drugs on Amlodipine: CYP3A Inhibitors: Coadministration with CYP3A inhibitors (moderate and strong) results in increased systemic exposure to amlodipine and may require dose reduction. Monitor for symptoms of hypotension and edema when amlodipine is coadministered with CYP3A inhibitors to determine the need for dose adjustment [see Clinical Pharmacology (12.3)].
CYP3A Inducers: No information is available on the quantitative effects of CYP3A inducers on amlodipine. Blood pressure should be closely monitored when amlodipine is coadministered with CYP3A inducers (e.g., rifampicin, St. Johns Wort).
Sildenafil: Monitor for hypotension when sildenafil is coadministered with amlodipine [see Clinical Pharmacology (12.2)].
Impact of Amlodipine on Other Drugs: Simvastatin: Coadministration of simvastatin with amlodipine increases the systemic exposure of simvastatin. Limit the dose of simvastatin in patients on amlodipine to 20 mg daily [see Clinical Pharmacology (12.3)].
Immunosuppressants: Amlodipine may increase the systemic exposure of cyclosporine or tacrolimus when coadministered. Frequent monitoring of trough blood levels of cyclosporine and tacrolimus is recommended and adjust the dose when appropriate [see Clinical Pharmacology (12.3)].
Valsartan:Agents Increasing Serum Potassium: Concomitant use of valsartan with other agents that block the renin-angiotensin system, potassium-sparing diuretics (e.g., spironolactone, triamterene, amiloride), potassium supplements, salt substitutes containing potassium or other drugs that may increase potassium levels (e.g., heparin) may lead to increases in serum potassium and in heart failure patients to increases in serum creatinine. If co-medication is considered necessary, monitoring of serum potassium is advisable.
Non-Steroidal Anti-Inflammatory Agents Including Selective Cyclooxygenase-2 Inhibitors (COX-2 Inhibitors):In patients who are elderly, volume-depleted (including those on diuretic therapy), or with compromised renal function, coadministration of NSAIDs, including selective COX-2 inhibitors, with angiotensin II receptor antagonists, including valsartan, may result in deterioration of renal function, including possible acute renal failure. These effects are usually reversible. Monitor renal function periodically in patients receiving valsartan and NSAID therapy.
The antihypertensive effect of angiotensin II receptor antagonists, including valsartan, may be attenuated by NSAIDs including selective COX-2 inhibitors.
Dual Blockade of the Renin-Angiotensin System (RAS): Dual blockade of the RAS with angiotensin receptor blockers, ACE inhibitors, or aliskiren is associated with increased risks of hypotension, hyperkalemia, and changes in renal function (including acute renal failure) compared to monotherapy. Most patients receiving the combination of two RAS inhibitors do not obtain any additional benefit compared to monotherapy. In general, avoid combined use of RAS inhibitors. Closely monitor blood pressure, renal function and electrolytes in patients on valsartan and other agents that affect the RAS.
Do not coadminister aliskiren with amlodipine and valsartan in patients with diabetes. Avoid use of aliskiren with amlodipine and valsartan in patients with renal impairment (GFR < 60 mL/min).
Lithium: Increases in serum lithium concentrations and lithium toxicity have been reported during concomitant administration of lithium with angiotensin II receptor antagonists. Monitor serum lithium levels during concomitant use.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Amlodipine and valsartan tablets can cause fetal harm when administered to a pregnant woman. Use of drugs that act on the renin-angiotensin system during the second and third trimesters of pregnancy reduces fetal renal function and increases fetal and neonatal morbidity and death. Most epidemiologic studies examining fetal abnormalities after exposure to antihypertensive use in the first trimester have not distinguished drugs affecting the renin-angiotensin system from other antihypertensive agents. Published reports include cases of anhydramnios and oligohydramnios in pregnant women treated with valsartan (see Clinical Considerations).
When pregnancy is detected, discontinue amlodipine and valsartan tablets as soon as possible.
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively.
Clinical Considerations
Disease-associated Maternal and/or Embryo/Fetal Risk:Hypertension in pregnancy increases the maternal risk for pre-eclampsia, gestational diabetes, premature delivery, and delivery complications (e.g., need for cesarean section, and post-partum hemorrhage). Hypertension increases the fetal risk for intrauterine growth restriction and intrauterine death. Pregnant women with hypertension should be carefully monitored and managed accordingly.
Fetal/Neonatal Adverse Reactions: Oligohydramnios in pregnant women who use drugs affecting the renin-angiotensin system in the second and third trimesters of pregnancy can result in the following: reduced fetal renal function leading to anuria and renal failure, fetal lung hypoplasia, skeletal deformations, including skull hypoplasia, hypotension and death.
Perform serial ultrasound examinations to assess the intra-amniotic environment. Fetal testing may be appropriate, based on the week of gestation. Patients and physicians should be aware, however, that oligohydramnios may not appear until after the fetus has sustained irreversible injury. If oligohydramnios is observed, consider alternative drug treatment. Closely observe neonates with histories of in utero exposure to amlodipine and valsartan for hypotension, oliguria, and hyperkalemia. In neonates with a history of in utero exposure to amlodipine and valsartan, if oliguria or hypotension occurs, support blood pressure and renal perfusion. Exchange transfusions or dialysis may be required as a means of reversing hypotension and replacing renal function.
Data
Animal Data
In rats, administered 20 mg/kg/day amlodipine plus 320 mg/kg/day valsartan, treatment-related maternal and fetal effects (developmental delays and alterations noted in the presence of significant maternal toxicity) were noted with the high dose combination. This corresponds to dose multiples of 9 and 19.5 times, respectively, the maximum recommended human dose (MRHD) of 10 mg/day for amlodipine and 320 mg/day for valsartan (based on body surface area and considering a 60 kg patient).
8.2 Lactation
Risk Summary
There is limited information regarding the presence of amlodipine and valsartan in human milk, the effects on the breastfed infant, or the effects on milk production. Valsartan is present in rat milk. Limited published studies report that amlodipine is present in human milk. Because of the potential for serious adverse reactions in breastfed infants, advise a nursing woman that breastfeeding is not recommended during treatment with amlodipine and valsartan tablets.
8.4 Pediatric Use
Safety and effectiveness of amlodipine and valsartan tablets in pediatric patients have not been established.
8.5 Geriatric Use
In controlled clinical trials, 323 (22.5%) hypertensive patients treated with amlodipine and valsartan tablets were ≥ 65 years and 79 (5.5%) were ≥ 75 years. No overall differences in the efficacy or safety of amlodipine and valsartan tablets were observed in this patient population, but greater sensitivity of some older individuals cannot be ruled out.
Amlodipine
The recommended starting dose of amlodipine 2.5 mg is not an available strength with amlodipine and valsartan tablets.
Clinical studies of amlodipine besylate tablets did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal or cardiac function, and of concomitant disease or other drug therapy. Elderly patients have decreased clearance of amlodipine with a resulting increase of AUC of approximately 40% to 60%.
Valsartan
In the controlled clinical trials of valsartan, 1214 (36.2%) of hypertensive patients treated with valsartan were ≥ 65 years and 265 (7.9%) were ≥ 75 years. No overall difference in the efficacy or safety of valsartan was observed in this patient population, but greater sensitivity of some older individuals cannot be ruled out.
8.6 Renal Impairment
Safety and effectiveness of amlodipine and valsartan tablets in patients with severe renal impairment (CrCl < 30 mL/min) have not been established. No dose adjustment is required in patients with mild (CrCl 60 to 90 mL/min) or moderate (CrCl 30 to 60 mL/min) renal impairment.
8.7 Hepatic Impairment
Amlodipine
Exposure to amlodipine is increased in patients with hepatic insufficiency [see Clinical Pharmacology (12.3)]. The recommended initial dose of amlodipine in patients with hepatic impairment is 2.5 mg, which is not an available strength with amlodipine and valsartan tablets.
-
10 OVERDOSAGE
Amlodipine: Single oral doses of amlodipine maleate equivalent to 40 mg/kg and 100 mg/kg amlodipine in mice and rats, respectively, caused deaths. Single oral doses equivalent to 4 or more mg/kg amlodipine in dogs (11 or more times the maximum recommended human dose on a mg/m2 basis) caused a marked peripheral vasodilation and hypotension.
Overdosage might be expected to cause excessive peripheral vasodilation with marked hypotension. In humans, experience with intentional overdosage of amlodipine is limited. Marked and potentially prolonged systemic hypotension up to and including shock with fatal outcome have been reported.
If massive overdose should occur, initiate active cardiac and respiratory monitoring. Frequent blood pressure measurements are essential. Should hypotension occur, cardiovascular support including elevation of the extremities and the judicious administration of fluids should be initiated. If hypotension remains unresponsive to these conservative measures, consider administration of vasopressors (such as phenylephrine) with attention to circulating volume and urine output. As amlodipine is highly protein bound, hemodialysis is not likely to be of benefit. Administration of activated charcoal to healthy volunteers immediately or up to two hours after ingestion of amlodipine has been shown to significantly decrease amlodipine absorption.
Valsartan: Limited data are available related to overdosage in humans. The most likely effect of overdose with valsartan would be peripheral vasodilation, hypotension, and tachycardia; bradycardia could occur from parasympathetic (vagal) stimulation. Depressed level of consciousness, circulatory collapse, and shock have been reported. If symptomatic hypotension should occur institute supportive treatment.
Valsartan is not removed from the plasma by hemodialysis.
Valsartan was without grossly observable adverse effects at single oral doses up to 2000 mg/kg in rats and up to 1000 mg/kg in marmosets, except for the salivation and diarrhea in the rat and vomiting in the marmoset at the highest dose (60 and 37 times, respectively, the MRHD on a mg/m2 basis). (Calculations assume an oral dose of 320 mg/day and a 60 kg patient.)
-
11 DESCRIPTION
Amlodipine and valsartan tablets, USP are a fixed combination of amlodipine and valsartan.
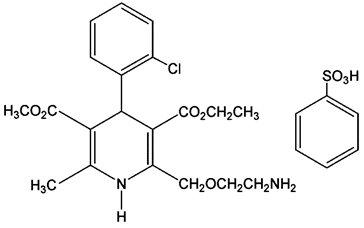
Amlodipine and valsartan tablets contain the besylate salt of amlodipine, a dihydropyridine calcium-channel blocker (CCB). Amlodipine besylate, USP is a white or almost white powder, slightly soluble in water and sparingly soluble in ethanol. Amlodipine besylate’s chemical name is 3-ethyl-5-methyl (4RS)-2-[(2-aminoethoxy)methyl]-4-(2-chlorophenyl)-6-methyl-1,4-dihydropyridine-3,5-dicarboxylate benzenesulfonate; its structural formula is:
Its molecular formula is C20H25ClN2O5C6H6O3S and its molecular weight is 567.1.
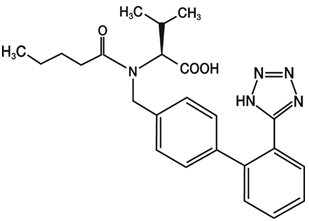
Valsartan is a nonpeptide, orally active, and specific angiotensin II antagonist acting on the AT1 receptor subtype. Valsartan, USP is a white to almost white amorphous powder, soluble in ethanol and methanol and slightly soluble in water. Valsartan’s chemical name is N-[p-(o-1H-Tetrazol-5-ylphenyl)benzyl]-N-valeryl-L-valine; its structural formula is:
Its molecular formula is C24H29N5O3 and its molecular weight is 435.52.
Amlodipine and valsartan tablets are formulated in 4 strengths for oral administration with a combination of amlodipine besylate, equivalent to 5 mg or 10 mg of amlodipine free base, with 160 mg, or 320 mg of valsartan providing for the following available combinations: 5/160 mg, 10/160 mg, 5/320 mg, and 10/320 mg.
The inactive ingredients for all strengths of the tablets are colloidal silicon dioxide, crospovidone, hypromellose, magnesium stearate, microcrystalline cellulose, polyethylene glycol, red iron oxide, sodium starch glycolate (potato), talc, titanium dioxide and yellow iron oxide.
Meets USP Dissolution Test 3.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Amlodipine
Amlodipine is a dihydropyridine calcium channel blocker that inhibits the transmembrane influx of calcium ions into vascular smooth muscle and cardiac muscle. Experimental data suggest that amlodipine binds to both dihydropyridine and nondihydropyridine binding sites. The contractile processes of cardiac muscle and vascular smooth muscle are dependent upon the movement of extracellular calcium ions into these cells through specific ion channels. Amlodipine inhibits calcium ion influx across cell membranes selectively, with a greater effect on vascular smooth muscle cells than on cardiac muscle cells. Negative inotropic effects can be detected in vitro but such effects have not been seen in intact animals at therapeutic doses. Serum calcium concentration is not affected by amlodipine. Within the physiologic pH range, amlodipine is an ionized compound (pKa = 8.6), and its kinetic interaction with the calcium channel receptor is characterized by a gradual rate of association and dissociation with the receptor binding site, resulting in a gradual onset of effect.
Amlodipine is a peripheral arterial vasodilator that acts directly on vascular smooth muscle to cause a reduction in peripheral vascular resistance and reduction in blood pressure.
Valsartan
Angiotensin II is formed from angiotensin I in a reaction catalyzed by angiotensin-converting enzyme (ACE, kininase II). Angiotensin II is the principal pressor agent of the renin-angiotensin system, with effects that include vasoconstriction, stimulation of synthesis and release of aldosterone, cardiac stimulation, and renal reabsorption of sodium. Valsartan blocks the vasoconstrictor and aldosterone-secreting effects of angiotensin II by selectively blocking the binding of angiotensin II to the AT1 receptor in many tissues, such as vascular smooth muscle and the adrenal gland. Its action is therefore independent of the pathways for angiotensin II synthesis.
There is also an AT2 receptor found in many tissues, but AT2 is not known to be associated with cardiovascular homeostasis. Valsartan has much greater affinity (about 20,000-fold) for the AT1 receptor than for the AT2 receptor. The increased plasma levels of angiotensin following AT1 receptor blockade with valsartan may stimulate the unblocked AT2 receptor. The primary metabolite of valsartan is essentially inactive with an affinity for the AT1 receptor about one-200th that of valsartan itself.
Blockade of the renin-angiotensin system with ACE inhibitors, which inhibit the biosynthesis of angiotensin II from angiotensin I, is widely used in the treatment of hypertension. ACE inhibitors also inhibit the degradation of bradykinin, a reaction also catalyzed by ACE. Because valsartan does not inhibit ACE (kininase II), it does not affect the response to bradykinin. Whether this difference has clinical relevance is not yet known. Valsartan does not bind to or block other hormone receptors or ion channels known to be important in cardiovascular regulation.
Blockade of the angiotensin II receptor inhibits the negative regulatory feedback of angiotensin II on renin secretion, but the resulting increased plasma renin activity and angiotensin II circulating levels do not overcome the effect of valsartan on blood pressure.
12.2 Pharmacodynamics
Amlodipine
Following administration of therapeutic doses to patients with hypertension, amlodipine produces vasodilation resulting in a reduction of supine and standing blood pressures. These decreases in blood pressure are not accompanied by a significant change in heart rate or plasma catecholamine levels with chronic dosing. Although the acute intravenous administration of amlodipine decreases arterial blood pressure and increases heart rate in hemodynamic studies of patients with chronic stable angina, chronic oral administration of amlodipine in clinical trials did not lead to clinically significant changes in heart rate or blood pressures in normotensive patients with angina.
With chronic, once-daily administration, antihypertensive effectiveness is maintained for at least 24 hours. Plasma concentrations correlate with effect in both young and elderly patients. The magnitude of reduction in blood pressure with amlodipine is also correlated with the height of pretreatment elevation; thus, individuals with moderate hypertension (diastolic pressure 105-114 mmHg) had about a 50% greater response than patients with mild hypertension (diastolic pressure 90-104 mmHg). Normotensive subjects experienced no clinically significant change in blood pressure (+1/-2 mmHg).
In hypertensive patients with normal renal function, therapeutic doses of amlodipine resulted in a decrease in renal vascular resistance and an increase in glomerular filtration rate and effective renal plasma flow without change in filtration fraction or proteinuria.
As with other calcium channel blockers, hemodynamic measurements of cardiac function at rest and during exercise (or pacing) in patients with normal ventricular function treated with amlodipine have generally demonstrated a small increase in cardiac index without significant influence on dP/dt or on left ventricular end diastolic pressure or volume. In hemodynamic studies, amlodipine has not been associated with a negative inotropic effect when administered in the therapeutic dose range to intact animals and man, even when coadministered with beta-blockers to man. Similar findings, however, have been observed in normal or well-compensated patients with heart failure with agents possessing significant negative inotropic effects.
Amlodipine does not change sinoatrial nodal function or atrioventricular (AV) conduction in intact animals or man. In patients with chronic stable angina, intravenous administration of 10 mg did not significantly alter A-H and H-V conduction and sinus node recovery time after pacing. Similar results were obtained in patients receiving amlodipine and concomitant beta-blockers. In clinical studies in which amlodipine was administered in combination with beta-blockers to patients with either hypertension or angina, no adverse effects of electrocardiographic (ECG) parameters were observed. In clinical trials with angina patients alone, amlodipine therapy did not alter electrocardiographic intervals or produce higher degrees of AV blocks.
Amlodipine has indications other than hypertension which can be found in the Norvasc® package insert.
Drug Interactions
Sildenafil
When amlodipine and sildenafil were used in combination, each agent independently exerted its own blood pressure lowering effect [see Drug Interactions (7)].
Valsartan
Valsartan inhibits the pressor effect of angiotensin II infusions. An oral dose of 80 mg inhibits the pressor effect by about 80% at peak with approximately 30% inhibition persisting for 24 hours. No information on the effect of larger doses is available.
Removal of the negative feedback of angiotensin II causes a 2- to 3-fold rise in plasma renin and consequent rise in angiotensin II plasma concentration in hypertensive patients. Minimal decreases in plasma aldosterone were observed after administration of valsartan; very little effect on serum potassium was observed.
In multiple dose studies in hypertensive patients with stable renal insufficiency and patients with renovascular hypertension, valsartan had no clinically significant effects on glomerular filtration rate, filtration fraction, creatinine clearance, or renal plasma flow.
Administration of valsartan to patients with essential hypertension results in a significant reduction of sitting, supine, and standing systolic blood pressure, usually with little or no orthostatic change. Valsartan has indications other than hypertension which can be found in the Diovan package insert.
Amlodipine and Valsartan Tablets
Amlodipine and valsartan tablets have been shown to be effective in lowering blood pressure. Both amlodipine and valsartan lower blood pressure by reducing peripheral resistance, but calcium influx blockade and reduction of angiotensin II vasoconstriction are complementary mechanisms.
12.3 Pharmacokinetics
Amlodipine
Peak plasma concentrations of amlodipine are reached 6 to 12 hours after administration of amlodipine alone. Absolute bioavailability has been estimated to be between 64% and 90%. The bioavailability of amlodipine is not altered by the presence of food.
The apparent volume of distribution of amlodipine is 21 L/kg. Approximately 93% of circulating amlodipine is bound to plasma proteins in hypertensive patients.
Amlodipine is extensively (about 90%) converted to inactive metabolites via hepatic metabolism with 10% of the parent compound and 60% of the metabolites excreted in the urine.
Elimination of amlodipine from the plasma is biphasic with a terminal elimination half-life of about 30 to 50 hours. Steady state plasma levels of amlodipine are reached after 7 to 8 days of consecutive daily dosing.
Valsartan
Following oral administration of valsartan alone peak plasma concentrations of valsartan are reached in 2 to 4 hours. Absolute bioavailability is about 25% (range 10% to 35%). Food decreases the exposure (as measured by AUC) to valsartan by about 40% and peak plasma concentration (Cmax) by about 50%.
The steady state volume of distribution of valsartan after intravenous administration is 17 L indicating that valsartan does not distribute into tissues extensively. Valsartan is highly bound to serum proteins (95%), mainly serum albumin.
Valsartan shows biexponential decay kinetics following intravenous administration with an average elimination half-life of about 6 hours. The recovery is mainly as unchanged drug, with only about 20% of dose recovered as metabolites. The primary metabolite, accounting for about 9% of dose, is valeryl 4-hydroxy valsartan. In vitro metabolism studies involving recombinant CYP 450 enzymes indicated that the CYP 2C9 isoenzyme is responsible for the formation of valeryl-4-hydroxy valsartan. Valsartan does not inhibit CYP 450 isozymes at clinically relevant concentrations. CYP 450 mediated drug interaction between valsartan and coadministered drugs are unlikely because of the low extent of metabolism.
Valsartan, when administered as an oral solution, is primarily recovered in feces (about 83% of dose) and urine (about 13% of dose). Following intravenous administration, plasma clearance of valsartan is about 2 L/h and its renal clearance is 0.62 L/h (about 30% of total clearance).
Amlodipine and Valsartan Tablets
Following oral administration of amlodipine and valsartan tablets in normal healthy adults, peak plasma concentrations of valsartan and amlodipine are reached in 3 and 6 to 8 hours, respectively. The rate and extent of absorption of valsartan and amlodipine from amlodipine and valsartan tablets are the same as when administered as individual tablets. The bioavailabilities of amlodipine and valsartan are not altered by the coadministration of food. Amlodipine and valsartan tablets may be administered with or without food.
Specific Populations
Geriatric
Renal Insufficiency
Valsartan
There is no apparent correlation between renal function (measured by creatinine clearance) and exposure (measured by AUC) to valsartan in patients with different degrees of renal impairment. Consequently, dose adjustment is not required in patients with mild-to-moderate renal dysfunction. No studies have been performed in patients with severe impairment of renal function (creatinine clearance < 10 mL/min). Valsartan is not removed from the plasma by hemodialysis. In the case of severe renal disease, exercise care with dosing of valsartan.
Hepatic Insufficiency
Amlodipine
Patients with hepatic insufficiency have decreased clearance of amlodipine with resulting increase in AUC of approximately 40% to 60%.
Valsartan
On average, patients with mild-to-moderate chronic liver disease have twice the exposure (measured by AUC values) to valsartan of healthy volunteers (matched by age, sex and weight). In general, no dosage adjustment is needed in patients with mild-to-moderate liver disease. Care should be exercised in patients with liver disease.
Drug Interactions
Amlodipine
In vitro data in human plasma indicate that amlodipine has no effect on the protein binding of digoxin, phenytoin, warfarin and indomethacin.
Impact of Other Drugs on Amlodipine
Coadministered cimetidine, magnesium- and aluminum hydroxide antacids, sildenafil, and grapefruit juice have no impact on the exposure to amlodipine.
CYP3A Inhibitors
Coadministration of a 180 mg daily dose of diltiazem with 5 mg amlodipine in elderly hypertensive patients resulted in a 60% increase in amlodipine systemic exposure. Erythromycin coadministration in healthy volunteers did not significantly change amlodipine systemic exposure. However, strong inhibitors of CYP3A (e.g., itraconazole, clarithromycin) may increase the plasma concentrations of amlodipine to a greater extent [see Drug Interactions (7)].
Impact of Amlodipine on Other Drugs
Coadministered amlodipine does not affect the exposure to atorvastatin, digoxin, ethanol and the warfarin prothrombin response time.
Simvastatin
Coadministration of multiple doses of 10 mg of amlodipine with 80 mg simvastatin resulted in a 77% increase in exposure to simvastatin compared to simvastatin alone [see Drug Interactions (7)].
Cyclosporine
A prospective study in renal transplant patients (N = 11) showed on an average of 40% increase in trough cyclosporine levels when concomitantly treated with amlodipine [see Drug Interactions (7)].
Tacrolimus
A prospective study in healthy Chinese volunteers (N = 9) with CYP3A5 expressers showed a 2.5- to 4-fold increase in tacrolimus exposure when concomitantly administered with amlodipine compared to tacrolimus alone. This finding was not observed in CYP3A5 non-expressers (N = 6). However, a 3-fold increase in plasma exposure to tacrolimus in a renal transplant patient (CYP3A5 non-expresser) upon initiation of amlodipine for the treatment of post-transplant hypertension resulting in reduction of tacrolimus dose has been reported. Irrespective of the CYP3A5 genotype status, the possibility of an interaction cannot be excluded with these drugs [see Drug Interactions (7)].
Valsartan
No clinically significant pharmacokinetic interactions were observed when valsartan was coadministered with amlodipine, atenolol, cimetidine, digoxin, furosemide, glyburide, hydrochlorothiazide, or indomethacin. The valsartan-atenolol combination was more antihypertensive than either component, but it did not lower the heart rate more than atenolol alone.
Coadministration of valsartan and warfarin did not change the pharmacokinetics of valsartan or the time-course of the anticoagulant properties of warfarin.
Transporters
The results from an in vitro study with human liver tissue indicate that valsartan is a substrate of the hepatic uptake transporter OATP1B1 and the hepatic efflux transporter MRP2. Coadministration of inhibitors of the uptake transporter (rifampin, cyclosporine) or efflux transporter (ritonavir) may increase the systemic exposure to valsartan.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Amlodipine
Rats and mice treated with amlodipine maleate in the diet for up to 2 years, at concentrations calculated to provide daily dosage levels of 0.5, 1.25, and 2.5 mg amlodipine/kg/day, showed no evidence of a carcinogenic effect of the drug. For the mouse, the highest dose was, on mg/m2 basis, similar to the MRHD of 10 mg amlodipine/day. For the rat, the highest dose was, on a mg/m2 basis, about 2.5 the MRHD. (Calculations based on a 60 kg patient.)
Mutagenicity studies conducted with amlodipine maleate revealed no drug-related effects at either the gene or chromosome level.
There was no effect on the fertility of rats treated orally with amlodipine maleate (males for 64 days and females for 14 days prior to mating) at doses of up to 10 mg amlodipine/kg/day (about 10 times the MRHD of 10 mg/day on a mg/m2 basis).
Valsartan
There was no evidence of carcinogenicity when valsartan was administered in the diet to mice and rats for up to 2 years at concentrations calculated to provide doses of up to 160 and 200 mg/kg/day, respectively. These doses in mice and rats are about 2.4 and 6 times, respectively, the MRHD of 320 mg/day on a mg/m2 basis. (Calculations based on a 60 kg patient.)
Mutagenicity assays did not reveal any valsartan-related effects at either the gene or chromosome level. These assays included bacterial mutagenicity tests with Salmonella and E. coli, a gene mutation test with Chinese hamster V79 cells, a cytogenetic test with Chinese hamster ovary cells, and a rat micronucleus test.
Valsartan had no adverse effects on the reproductive performance of male or female rats at oral doses of up to 200 mg/kg/day. This dose is about 6 times the MRHD on a mg/m2 basis.
-
14 CLINICAL STUDIES
Amlodipine and valsartan tablets were studied in 2 placebo-controlled and 4 active-controlled trials in hypertensive patients. In a double-blind, placebo-controlled study, a total of 1012 patients with mild-to-moderate hypertension received treatments of 3 combinations of amlodipine and valsartan (5/80, 5/160, 5/320 mg) or amlodipine alone (5 mg), valsartan alone (80, 160, or 320 mg) or placebo. All doses with the exception of the 5/320 mg dose were initiated at the randomized dose. The high dose was titrated to that dose after a week at a dose of 5/160 mg. At week 8, the combination treatments were statistically significantly superior to their monotherapy components in reduction of diastolic and systolic blood pressures.
Table 1: Effect of Amlodipine and Valsartan Tablets on Sitting Diastolic Blood Pressure - * Mean Change and Placebo-Subtracted Mean Change from Baseline (mmHg) at Week 8 in Sitting Diastolic Blood Pressure. Mean baseline diastolic BP was 99.3 mmHg.
Amlodipine Dosage
Valsartan Dosage
0 mg
80 mg
160 mg
320 mg
Mean Change*
Placebo-Subtracted
Mean Change*
Placebo- Subtracted
Mean Change*
Placebo- Subtracted
Mean Change*
Placebo- Subtracted
0 mg
-6.4
---
-9.5
-3.1
-10.9
-4.5
-13.2
-6.7
5 mg
-11.1
-4.7
-14.2
-7.8
-14.0
-7.6
-15.7
-9.3
Table 2: Effect of Amlodipine and Valsartan Tablets on Sitting Systolic Blood Pressure - * Mean Change and Placebo-Subtracted Mean Change from Baseline (mmHg) at Week 8 in Sitting Systolic Blood Pressure. Mean baseline systolic BP was 152.8 mmHg.
Amlodipine Dosage
Valsartan Dosage
0 mg
80 mg
160 mg
320 mg
Mean Change*
Placebo-Subtracted
Mean Change*
Placebo- Subtracted
Mean Change*
Placebo- Subtracted
Mean Change*
Placebo- Subtracted
0 mg
-6.2
---
-12.9
-6.8
-14.3
-8.2
-16.3
-10.1
5 mg
-14.8
-8.6
-20.7
-14.5
-19.4
-13.2
-22.4
-16.2
In a double-blind, placebo-controlled study, a total of 1246 patients with mild-to-moderate hypertension received treatments of 2 combinations of amlodipine and valsartan (10/160, 10/320 mg), or amlodipine alone (10 mg), valsartan alone (160 or 320 mg) or placebo. With the exception of the 10/320 mg dose, treatment was initiated at the randomized dose. The high dose was initiated at a dose of 5/160 mg and titrated to the randomized dose after 1 week. At week 8, the combination treatments were statistically significantly superior to their monotherapy components in reduction of diastolic and systolic blood pressures.
Table 3: Effect of Amlodipine and Valsartan Tablets on Sitting Diastolic Blood Pressure - * Mean Change and Placebo-Subtracted Mean Change from Baseline (mmHg) at Week 8 in Sitting Diastolic Blood Pressure. Mean baseline diastolic BP was 99.1 mmHg.
Amlodipine Dosage
Valsartan Dosage
0 mg
160 mg
320 mg
Mean Change*
Placebo-Subtracted
Mean Change*
Placebo- Subtracted
Mean Change*
Placebo- Subtracted
0 mg
-8.2
---
-12.8
- 4.5
-12.8
-4.5
10 mg
-15.0
-6.7
- 17.2
- 9.0
-18.1
-9.9
Table 4: Effect of Amlodipine and Valsartan Tablets on Sitting Systolic Blood Pressure - * Mean Change and Placebo-Subtracted Mean Change from Baseline (mmHg) at Week 8 in Sitting Systolic Blood Pressure. Mean baseline systolic BP was 156.7 mmHg.
Amlodipine Dosage
Valsartan Dosage
0 mg
160 mg
320 mg
Mean Change*
Placebo-Subtracted
Mean Change*
Placebo- Subtracted
Mean Change*
Placebo- Subtracted
0 mg
-11.0
---
-18.1
-7.0
-18.5
-7.5
10 mg
-22.2
-11.2
-26.6
-15.5
-26.9
-15.9
In a double-blind, active-controlled study, a total of 947 patients with mild-to-moderate hypertension who were not adequately controlled on valsartan 160 mg received treatments of 2 combinations of amlodipine and valsartan (10/160, 5/160 mg) or valsartan alone (160 mg). At week 8, the combination treatments were statistically significantly superior to the monotherapy component in reduction of diastolic and systolic blood pressures.
Table 5: Effect of Amlodipine and Valsartan Tablets on Sitting Diastolic/Systolic Blood Pressure - * Mean Change from Baseline at Week 8 in Sitting Diastolic/Systolic Blood Pressure. Mean baseline BP was 149.5/ 96.5 (systolic/diastolic) mmHg.
- † Treatment Difference = difference in mean BP reduction between amlodipine and valsartan tablets and the control group (valsartan 160 mg).
Treatment Group
Diastolic BP
Systolic BP
Mean Change*
Treatment Difference†
Mean Change*
Treatment Difference†
Amlodipine and Valsartan Tablets
10/160 mg-11.4
-4.8
-13.9
-5.7
Amlodipine and Valsartan Tablets
5/160 mg-9.6
-3.1
-12.0
-3.9
Valsartan 160 mg
-6.6
---
-8.2
---
In a double-blind, active-controlled study, a total of 944 patients with mild-to-moderate hypertension who were not adequately controlled on amlodipine 10 mg received a combination of amlodipine and valsartan (10/160 mg) or amlodipine alone (10 mg). At week 8, the combination treatment was statistically significantly superior to the monotherapy component in reduction of diastolic and systolic blood pressures.
Table 6: Effect of Amlodipine and Valsartan Tablets on Sitting Diastolic/Systolic Blood Pressure - * Mean Change from Baseline at Week 8 in Sitting Diastolic/Systolic Blood Pressure. Mean baseline BP was 147.0/95.1 (systolic/diastolic) mmHg.
- † Treatment Difference = difference in mean BP reduction between amlodipine and valsartan tablets and the control group (amlodipine 10 mg).
Treatment Group
Diastolic BP
Systolic BP
Mean Change*
Treatment Difference†
Mean Change*
Treatment Difference†
Amlodipine and Valsartan Tablets
10/160 mg-11.8
-1.8
-12.7
-1.9
Amlodipine 10 mg
-10.0
---
-10.8
---
Amlodipine and valsartan tablets were also evaluated for safety in a 6-week, double-blind, active-controlled trial of 130 hypertensive patients with severe hypertension (mean baseline BP of 171/113 mmHg). Adverse events were similar in patients with severe hypertension and mild/moderate hypertension treated with amlodipine and valsartan tablets.
A wide age range of the adult population, including the elderly was studied (range 19 to 92 years, mean 54.7 years). Women comprised almost half of the studied population (47.3%). Of the patients in the studied amlodipine and valsartan tablets group, 87.6% were Caucasian. Black and Asian patients each represented approximately 4% of the population in the studied amlodipine and valsartan tablets group.
Two additional double-blind, active-controlled studies were conducted in which amlodipine and valsartan tablets were administered as initial therapy. In 1 study, a total of 572 black patients with moderate to severe hypertension were randomized to receive either combination amlodipine/valsartan or amlodipine monotherapy for 12 weeks. The initial dose of amlodipine/valsartan was 5/160 mg for 2 weeks with forced titration to 10/160 mg for 2 weeks, followed by optional titration to 10/320 mg for 4 weeks and optional addition of HCTZ 12.5 mg for 4 weeks. The initial dose of amlodipine was 5 mg for 2 weeks with forced titration to 10 mg for 2 weeks, followed by optional titration to 10 mg for 4 weeks and optional addition of HCTZ 12.5 mg for 4 weeks. At the primary endpoint of 8 weeks, the treatment difference between amlodipine/valsartan and amlodipine was 6.7/2.8 mmHg.
In the other study of similar design, a total of 646 patients with moderate to severe hypertension (MSSBP of ≥ 160 mmHg and < 200 mmHg) were randomized to receive either combination amlodipine/valsartan or amlodipine monotherapy for 8 weeks. The initial dose of amlodipine/valsartan was 5/160 mg for 2 weeks with forced titration to 10/160 mg for 2 weeks, followed by the optional addition of HCTZ 12.5 mg for 4 weeks. The initial dose of amlodipine was 5 mg for 2 weeks with forced titration to 10 mg for 2 weeks, followed by the optional addition of HCTZ 12.5 mg for 4 weeks. At the primary endpoint of 4 weeks, the treatment difference between amlodipine/valsartan and amlodipine was 6.6/3.9 mmHg.
There are no trials of the amlodipine and valsartan combination tablet demonstrating reductions in cardiovascular risk in patients with hypertension, but the amlodipine component and several ARBs, which are the same pharmacological class as the valsartan component, have demonstrated such benefits.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
Amlodipine and Valsartan Tablets, USP are available containing 6.94 mg or 13.88 mg of amlodipine besylate, USP equivalent to 5 mg or 10 mg of amlodipine free base, respectively, with 160 mg or 320 mg of valsartan, USP providing for the following available combinations: 5 mg/160 mg, 10 mg/160 mg, 5 mg/320 mg or 10 mg/320 mg.
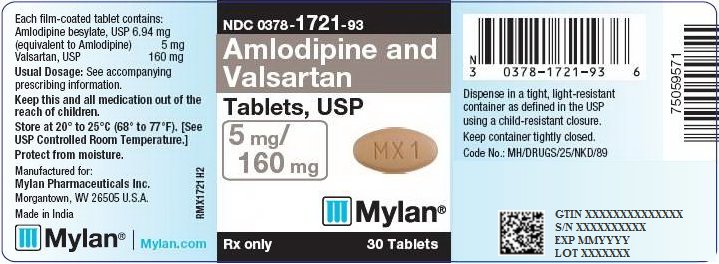
The 5 mg/160 mg tablets are light orange, film-coated, oval, unscored tablets debossed with MX1 on one side of the tablet and blank on the other side. They are available as follows:
NDC: 0378-1721-93
bottles of 30 tabletsThe 10 mg/160 mg tablets are tan, film-coated, oval, unscored tablets debossed with MX2 on one side of the tablet and blank on the other side. They are available as follows:
NDC: 0378-1722-93
bottles of 30 tabletsThe 5 mg/320 mg tablets are orange, film-coated, capsule-shaped, unscored tablets debossed with MX43 on one side of the tablet and blank on the other side. They are available as follows:
NDC: 0378-1723-93
bottles of 30 tabletsThe 10 mg/320 mg tablets are light orange, film-coated, capsule-shaped, unscored tablets debossed with MX44 on one side of the tablet and blank on the other side. They are available as follows:
NDC: 0378-1724-93
bottles of 30 tabletsStore at 20° to 25°C (68° to 77°F). [See USP Controlled Room Temperature.]
Protect from moisture.
Dispense in a tight, light-resistant container as defined in the USP using a child-resistant closure.
-
17 PATIENT COUNSELING INFORMATION
Information for Patients: Advise the patient to read the FDA-approved patient labeling (Patient Information).
Pregnancy: Advise female patients of childbearing age about the consequences of exposure to amlodipine and valsartan tablets during pregnancy. Discuss treatment options with women planning to become pregnant. Ask patients to report pregnancies to their physicians as soon as possible [see Warnings and Precautions (5.1) and Use in Specific Populations (8.1)].
Lactation: Advise women not to breastfeed during treatment with amlodipine and valsartan tablets [see Use in Specific Populations (8.2)].
Symptomatic Hypotension: Advise patients that lightheadedness can occur, especially during the first days of therapy, and that it should be reported to their healthcare provider. Tell patients that if syncope occurs to discontinue amlodipine and valsartan tablets until the physician has been consulted. Caution all patients that inadequate fluid intake, excessive perspiration, diarrhea, or vomiting can lead to an excessive fall in blood pressure, with the same consequences of lightheadedness and possible syncope [see Warnings and Precautions (5.2)].
Hyperkalemia: Advise patients not to use salt substitutes without consulting their healthcare provider [see Drug Interactions (7)].
FDA-APPROVED PATIENT LABELING
-
Patient Information
Amlodipine and Valsartan Tablets, USP
(am loe′ di peen val sar′ tan)Read the Patient Information that comes with amlodipine and valsartan tablets before you start taking them and each time you get a refill. There may be new information. This leaflet does not take the place of talking with your doctor about your medical condition or treatment. If you have any questions about amlodipine and valsartan tablets, ask your doctor or pharmacist.
What is the most important information I should know about amlodipine and valsartan tablets?
- Amlodipine and valsartan tablets can cause harm or death to an unborn baby.
- Talk to your doctor about other ways to lower your blood pressure if you plan to become pregnant.
- If you get pregnant while taking amlodipine and valsartan tablets, tell your doctor right away.
What are amlodipine and valsartan tablets?
Amlodipine and valsartan tablets contain 2 prescription medicines:
- amlodipine, a calcium channel blocker
- valsartan, an angiotensin receptor blocker (ARB).
Amlodipine and valsartan tablets may be used to lower high blood pressure (hypertension) in adults
- when 1 medicine to lower your high blood pressure is not enough
- as the first medicine to lower high blood pressure if your doctor decides you are likely to need more than 1 medicine.
Amlodipine and valsartan tablets have not been studied in children under 18 years of age.
What should I tell my doctor before taking amlodipine and valsartan tablets?
Tell your doctor about all of your medical conditions, including if you:
- are pregnant or plan to become pregnant. See “What is the most important information I should know about amlodipine and valsartan tablets?”
- are breastfeeding or plan to breastfeed. Amlodipine and valsartan are present in human milk. It is not known whether amlodipine and valsartan tablets affect your breastfed baby or milk production. Do not breastfeed while you are taking amlodipine and valsartan tablets.
- have heart problems
- have liver problems
- have kidney problems
- are vomiting or having a lot of diarrhea
- have ever had a reaction called angioedema, to another blood pressure medicine. Angioedema causes swelling of the face, lips, tongue, throat, and may cause difficulty breathing.
Tell your doctor about all the medicines you take, including prescription and nonprescription medicines, vitamins, and herbal supplements. Some of your other medicines and amlodipine and valsartan tablets could affect each other, causing serious side effects.
Especially tell your doctor if you take:
- simvastatin or other cholesterol-lowering medicine
- other medicines for high blood pressure or a heart problem
- water pills (diuretics)
- potassium supplements. Your doctor may check the amount of potassium in your blood periodically.
- a salt substitute. Your doctor may check the amount of potassium in your blood periodically.
- nonsteroidal anti-inflammatory drugs (like ibuprofen or naproxen)
- medicines used to prevent and treat fungal skin infections (such as ketoconazole, itraconazole)
- medicines used to treat bacterial infections (such as clarithromycin, telithromycin)
- certain antibiotics (rifamycin group), a drug used to protect against transplant rejection (cyclosporine) or an antiretroviral drug used to treat HIV/AIDS infection (ritonavir). These drugs may increase the effect of valsartan.
- lithium, a medicine used in some types of depression
Know the medicines you take. Keep a list of your medicines and show it to your doctor or pharmacist when you get a new medicine. Talk to your doctor or pharmacist before you start taking any new medicine. Your doctor or pharmacist will know what medicines are safe to take together.
How should I take amlodipine and valsartan tablets?
- Take amlodipine and valsartan tablets exactly as your doctor tells you.
- Take amlodipine and valsartan tablets once each day.
- Amlodipine and valsartan tablets can be taken with or without food.
- If you miss a dose, take it as soon as you remember. If it is close to your next dose, do not take the missed dose. Just take the next dose at your regular time.
- If you take too many amlodipine and valsartan tablets, call your doctor or Poison Control Center, or go to the emergency room.
-
Tell all your doctors or dentist you are taking amlodipine and valsartan tablets if you:
- are going to have surgery
- go for kidney dialysis
What should I avoid while taking amlodipine and valsartan tablets?
You should not take amlodipine and valsartan tablets during pregnancy. See “What is the most important information I should know about amlodipine and valsartan tablets?”
What are the possible side effects of amlodipine and valsartan tablets?
Amlodipine and valsartan tablets may cause serious side effects including:
- harm to an unborn baby causing injury and even death. See “What is the most important information I should know about amlodipine and valsartan tablets?”
-
low blood pressure (hypotension). Low blood pressure is most likely to happen if you:
- take water pills
- are on a low-salt diet
- get dialysis treatments
- have heart problems
- get sick with vomiting or diarrhea
-
drink alcohol
- Lie down if you feel faint or dizzy. Call your doctor right away.
- more heart attacks and chest pain (angina) in people that already have severe heart problems. This may happen when you start amlodipine and valsartan tablets or when there is an increase in your dose of amlodipine and valsartan tablets. Get emergency help if you get worse chest pain or chest pain that does not go away.
- kidney problems. Kidney problems may become worse in people that already have kidney disease. Some people will have changes in blood tests for kidney function and may need a lower dose of amlodipine and valsartan tablets. Call your doctor if you have swelling in your feet, ankles, or hands or unexplained weight gain. If you have heart failure, your doctor should check your kidney function before prescribing amlodipine and valsartan tablets.
- laboratory blood test changes in people with heart failure. Some people with heart failure who take valsartan, 1 of the medicines in amlodipine and valsartan tablets, have changes in blood tests including increased potassium and decreased kidney function.
The most common side effects of amlodipine and valsartan tablets include:
- swelling (edema) of the hands, ankles, or feet
- nasal congestion, sore throat, and discomfort when swallowing
- upper respiratory tract infection (head or chest cold)
- dizziness
Tell your doctor if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of amlodipine and valsartan tablets. For more information, ask your doctor or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store amlodipine and valsartan tablets?
- Store amlodipine and valsartan tablets at room temperature between 20° to 25°C (68° to 77°F).
- Keep amlodipine and valsartan tablets dry (protect them from moisture).
Keep amlodipine and valsartan tablets and all medicines out of the reach of children.
General information about amlodipine and valsartan tablets
Medicines are sometimes prescribed for conditions that are not mentioned in the patient information leaflet. Do not use amlodipine and valsartan tablets for a condition for which they were not prescribed. Do not give amlodipine and valsartan tablets to other people, even if they have the same symptoms that you have. They may harm them.
This patient information leaflet summarizes the most important information about amlodipine and valsartan tablets. If you would like more information about amlodipine and valsartan tablets, talk with your doctor. You can ask your doctor or pharmacist for information about amlodipine and valsartan tablets that is written for health professionals. For more information, call Mylan at 1-877-446-3679 (1-877-4-INFO-RX).
What are the ingredients in amlodipine and valsartan tablets?
Active ingredients: amlodipine besylate and valsartan
The inactive ingredients of all strengths of the tablets are colloidal silicon dioxide, crospovidone, hypromellose, magnesium stearate, microcrystalline cellulose, polyethylene glycol, red iron oxide, sodium starch glycolate (potato), talc, titanium dioxide and yellow iron oxide.
What is high blood pressure (hypertension)?
Blood pressure is the force of blood in your blood vessels when your heart beats and when your heart rests. You have high blood pressure when the force is too much. Amlodipine and valsartan tablets can help your blood vessels relax so your blood pressure is lower. Medicines that lower blood pressure lower your chance of having a stroke or heart attack.
High blood pressure makes the heart work harder to pump blood throughout the body and causes damage to blood vessels. If high blood pressure is not treated, it can lead to stroke, heart attack, heart failure, kidney failure, and vision problems.
The brands listed are trademarks of their respective owners.
Manufactured for:
Mylan Pharmaceuticals Inc.
Morgantown, WV 26505 U.S.A.Manufactured by:
Mylan Laboratories Limited
Hyderabad — 500 096, India
75068926
Revised: 7/2019
MX:AMLOVALT:R4 -
PRINCIPAL DISPLAY PANEL – 5 mg/160 mg
NDC: 0378-1721-93
Amlodipine and
Valsartan
Tablets, USP
5 mg/
160 mgRx only 30 Tablets
Each film-coated tablet contains:
Amlodipine besylate, USP 6.94 mg
(equivalent to Amlodipine) 5 mg
Valsartan, USP 160 mgUsual Dosage: See accompanying
prescribing information.Keep this and all medication out of the
reach of children.Store at 20° to 25°C (68° to 77°F). [See
USP Controlled Room Temperature.]Protect from moisture.
Manufactured for:
Mylan Pharmaceuticals Inc.
Morgantown, WV 26505 U.S.A.Made in India
Mylan.com
RMX1721H2
Dispense in a tight, light-resistant
container as defined in the USP
using a child-resistant closure.Keep container tightly closed.
Code No.: MH/DRUGS/25/NKD/89
-
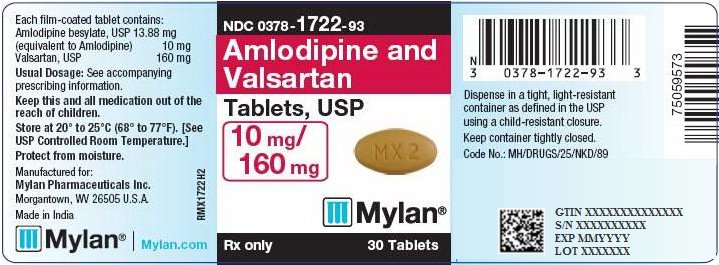
PRINCIPAL DISPLAY PANEL – 10 mg/160 mg
NDC: 0378-1722-93
Amlodipine and
Valsartan
Tablets, USP
10 mg/
160 mgRx only 30 Tablets
Each film-coated tablet contains:
Amlodipine besylate, USP 13.88 mg
(equivalent to Amlodipine) 10 mg
Valsartan, USP 160 mgUsual Dosage: See accompanying
prescribing information.Keep this and all medication out of the
reach of children.Store at 20° to 25°C (68° to 77°F). [See
USP Controlled Room Temperature.]Protect from moisture.
Manufactured for:
Mylan Pharmaceuticals Inc.
Morgantown, WV 26505 U.S.A.Made in India
Mylan.com
RMX1722H2
Dispense in a tight, light-resistant
container as defined in the USP
using a child-resistant closure.Keep container tightly closed.
Code No.: MH/DRUGS/25/NKD/89
-
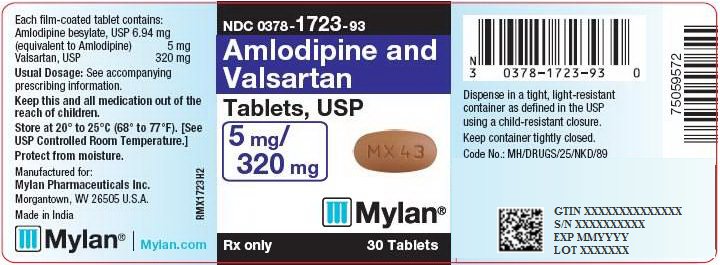
PRINCIPAL DISPLAY PANEL – 5 mg/320 mg
NDC: 0378-1723-93
Amlodipine and
Valsartan
Tablets, USP
5 mg/
320 mgRx only 30 Tablets
Each film-coated tablet contains:
Amlodipine besylate, USP 6.94 mg
(equivalent to Amlodipine) 5 mg
Valsartan, USP 320 mgUsual Dosage: See accompanying
prescribing information.Keep this and all medication out of the
reach of children.Store at 20° to 25°C (68° to 77°F). [See
USP Controlled Room Temperature.]Protect from moisture.
Manufactured for:
Mylan Pharmaceuticals Inc.
Morgantown, WV 26505 U.S.A.Made in India
Mylan.com
RMX1723H2
Dispense in a tight, light-resistant
container as defined in the USP
using a child-resistant closure.Keep container tightly closed.
Code No.: MH/DRUGS/25/NKD/89
-
PRINCIPAL DISPLAY PANEL – 10 mg/320 mg
NDC: 0378-1724-93
Amlodipine and
Valsartan
Tablets, USP
10 mg/
320 mgRx only 30 Tablets
Each film-coated tablet contains:
Amlodipine besylate, USP 13.88 mg
(equivalent to Amlodipine) 10 mg
Valsartan, USP 320 mgUsual Dosage: See accompanying
prescribing information.Keep this and all medication out of the
reach of children.Store at 20° to 25°C (68° to 77°F). [See
USP Controlled Room Temperature.]Protect from moisture.
Manufactured for:
Mylan Pharmaceuticals Inc.
Morgantown, WV 26505 U.S.A.Made in India
Mylan.com
RMX1724H2
Dispense in a tight, light-resistant
container as defined in the USP
using a child-resistant closure.Keep container tightly closed.
Code No.: MH/DRUGS/25/NKD/89
-
INGREDIENTS AND APPEARANCE
AMLODIPINE AND VALSARTAN
amlodipine and valsartan tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0378-1721 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength AMLODIPINE BESYLATE (UNII: 864V2Q084H) (AMLODIPINE - UNII:1J444QC288) AMLODIPINE 5 mg VALSARTAN (UNII: 80M03YXJ7I) (VALSARTAN - UNII:80M03YXJ7I) VALSARTAN 160 mg Inactive Ingredients Ingredient Name Strength SILICON DIOXIDE (UNII: ETJ7Z6XBU4) CROSPOVIDONE (15 MPA.S AT 5%) (UNII: 68401960MK) HYPROMELLOSE, UNSPECIFIED (UNII: 3NXW29V3WO) MAGNESIUM STEARATE (UNII: 70097M6I30) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) POLYETHYLENE GLYCOL, UNSPECIFIED (UNII: 3WJQ0SDW1A) FERRIC OXIDE RED (UNII: 1K09F3G675) SODIUM STARCH GLYCOLATE TYPE B POTATO (UNII: 27NA468985) TALC (UNII: 7SEV7J4R1U) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) Product Characteristics Color ORANGE (light orange) Score no score Shape OVAL Size 16mm Flavor Imprint Code MX1 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0378-1721-93 30 in 1 BOTTLE, PLASTIC; Type 0: Not a Combination Product 03/30/2015 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA090483 03/30/2015 AMLODIPINE AND VALSARTAN
amlodipine and valsartan tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0378-1722 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength AMLODIPINE BESYLATE (UNII: 864V2Q084H) (AMLODIPINE - UNII:1J444QC288) AMLODIPINE 10 mg VALSARTAN (UNII: 80M03YXJ7I) (VALSARTAN - UNII:80M03YXJ7I) VALSARTAN 160 mg Inactive Ingredients Ingredient Name Strength SILICON DIOXIDE (UNII: ETJ7Z6XBU4) CROSPOVIDONE (15 MPA.S AT 5%) (UNII: 68401960MK) HYPROMELLOSE, UNSPECIFIED (UNII: 3NXW29V3WO) MAGNESIUM STEARATE (UNII: 70097M6I30) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) POLYETHYLENE GLYCOL, UNSPECIFIED (UNII: 3WJQ0SDW1A) FERRIC OXIDE RED (UNII: 1K09F3G675) SODIUM STARCH GLYCOLATE TYPE B POTATO (UNII: 27NA468985) TALC (UNII: 7SEV7J4R1U) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) Product Characteristics Color BROWN (tan) Score no score Shape OVAL Size 16mm Flavor Imprint Code MX2 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0378-1722-93 30 in 1 BOTTLE, PLASTIC; Type 0: Not a Combination Product 03/30/2015 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA090483 03/30/2015 AMLODIPINE AND VALSARTAN
amlodipine and valsartan tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0378-1723 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength AMLODIPINE BESYLATE (UNII: 864V2Q084H) (AMLODIPINE - UNII:1J444QC288) AMLODIPINE 5 mg VALSARTAN (UNII: 80M03YXJ7I) (VALSARTAN - UNII:80M03YXJ7I) VALSARTAN 320 mg Inactive Ingredients Ingredient Name Strength SILICON DIOXIDE (UNII: ETJ7Z6XBU4) CROSPOVIDONE (15 MPA.S AT 5%) (UNII: 68401960MK) HYPROMELLOSE, UNSPECIFIED (UNII: 3NXW29V3WO) MAGNESIUM STEARATE (UNII: 70097M6I30) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) POLYETHYLENE GLYCOL, UNSPECIFIED (UNII: 3WJQ0SDW1A) FERRIC OXIDE RED (UNII: 1K09F3G675) SODIUM STARCH GLYCOLATE TYPE B POTATO (UNII: 27NA468985) TALC (UNII: 7SEV7J4R1U) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) Product Characteristics Color ORANGE Score no score Shape OVAL (capsule-shaped) Size 21mm Flavor Imprint Code MX43 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0378-1723-93 30 in 1 BOTTLE, PLASTIC; Type 0: Not a Combination Product 03/30/2015 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA090483 03/30/2015 AMLODIPINE AND VALSARTAN
amlodipine and valsartan tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0378-1724 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength AMLODIPINE BESYLATE (UNII: 864V2Q084H) (AMLODIPINE - UNII:1J444QC288) AMLODIPINE 10 mg VALSARTAN (UNII: 80M03YXJ7I) (VALSARTAN - UNII:80M03YXJ7I) VALSARTAN 320 mg Inactive Ingredients Ingredient Name Strength SILICON DIOXIDE (UNII: ETJ7Z6XBU4) CROSPOVIDONE (15 MPA.S AT 5%) (UNII: 68401960MK) HYPROMELLOSE, UNSPECIFIED (UNII: 3NXW29V3WO) MAGNESIUM STEARATE (UNII: 70097M6I30) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) FERRIC OXIDE RED (UNII: 1K09F3G675) SODIUM STARCH GLYCOLATE TYPE B POTATO (UNII: 27NA468985) TALC (UNII: 7SEV7J4R1U) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) POLYETHYLENE GLYCOL, UNSPECIFIED (UNII: 3WJQ0SDW1A) Product Characteristics Color ORANGE (light orange) Score no score Shape OVAL (capsule-shaped) Size 21mm Flavor Imprint Code MX44 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0378-1724-93 30 in 1 BOTTLE, PLASTIC; Type 0: Not a Combination Product 03/30/2015 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA090483 03/30/2015 Labeler - Mylan Pharmaceuticals Inc. (059295980)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.