CTC-310- crotalus durissus terrificus venom and cardiotoxin iii injection, solution
CTC-310 by
Drug Labeling and Warnings
CTC-310 by is a Homeopathic medication manufactured, distributed, or labeled by Celtic Biotech Iowa, Inc., Complete Pharmacy and Medical Solutions, LLC. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
DESCRIPTION
CTC-310 is a liquid for injection formula comprising a 1:1 combination of Crotoxin and Cardiotoxin
Crotoxin preparations are made from the venom of the South American rattlesnake, Crotalus durissus.
Cardiotoxin preparations are made from the venom of the Asian cobra Naja naja.
They are homeopathic formulations that include sterile injectables for intravenous and subcutaneous use.
-
INDICATIONS
According to the FDA reference text “Clarkes’ Materia Medica 1900”;
Crotalus venom preparations are indicated as homeopathic medications for numerous conditions but especially; Cancers. Tongue, inflammation of ; cancer of. Clinical experience shows that Crotoxin also provide relief from some forms of pain.
Cobra venom preparations are indicated as homeopathic medications for several conditions but especially for; angina faucium, angina pectoris, asthma, dysmenia (painful menses), grief (depression), headache (migraine), pain in ovaries (ovarian cysts), spinal irritation (back pain) and sore throat. Cardiotoxin is the principal active analgesic component.
- PHARMACOLOGIC CATEGORY
-
PHARMACOLOGY
The principal active components in both venoms are cytotoxins. Crotoxin (CT) is a pre-synaptic bi-partite beta-neurotoxin with phospholipase A2 (PLA2) activity. Evaluation by the Developmental Therapeutics Program of the National Cancer Institute (NSC 624244) for cytotoxicity in vitro against a panel of human tumour cell lines showed enhanced cytotoxicity towards melanoma, CNS and non-small cell lung cancer lines. Toxin-phospholipid interaction and subsequent accumulation of products of phospholipid hydrolysis in the membrane may alter membrane packing, disrupt lipid domains and affect protein conformation resulting in effects like inhibition of type II Ca2+ channels or alteration of transmembrane signaling pathways. Current thought suggests that CT binds to the upregulated Crocalbin that is upregulated in malignant cells. The Nicotinic Acetylcholine receptor is also upregulated in tumor cell lines and have been clearly identified as having a role in proliferation especially in lung cancer and CNS tumors – tumor populations with high sensitivity to CT. The released PLA2 produces arachidonic acid at the membrane surface that activates protein kinase C (PKC) and possibly other tyrosine kinases. PKC in turn phosphorylates endogenous caspases and the activated caspases initiate the process of programmed cell death.
The main pharmacological target for Cardiotoxin has not been clearly identified though it has been shown to target heparin sulphate-glyco proteins. Cardiotoxins (CD) have a number of pharmacological properties in intact tissues including hemolysis, cytolysis, contractures of muscle, membrane depolarization and activation of tissue phospholipase C and, to a far lesser extent, an arachidonic acid-associated phospholipase A2. The toxins have also been demonstrated to open the Ca2+ release channel (ryanodine receptor) and alter the activity of the Ca2++Mg2+-ATPase in isolated sarcoplasmic reticulum preparations derived from cardiac or skeletal muscle. However, a relationship of these actions in isolated organelles to contracture induction has not yet been established. The toxins also bind to and, in some cases, alter the function of a number of other proteins in disrupted tissues. The most difficult tasks in understanding the mechanism of action of these toxins have been dissociating the primary from secondary effects and distinguishing between effects that only occur in disrupted tissues and those that occur in intact tissue.
-
PHARMACODYNAMICS
Both actives exert potent cytolytic activities in-vitro. Tissue culture studies were performed using murine and human tumour cell lines. The responses are summarized in Table 1.
Table 1: Comparison of cytotoxicity of CT, CD, and VRCTC-310 Panel LC50 mg/ml Theoretical Additive LC50 Potent. (factor) CT CD CTC-310 Leukemia 43.6 6.3 7.2 11.0 (1.5) Non Small Cell Lung 12.7 3.9 5.0 6.0 (1.2) Small Cell Lung 30.1 1.15 3.9 2.2 Colon 74.9 22.4 36.4 34.5 Central Nervous System 7.5 2.2 2.1 3.4 (1.6) Melanoma 7.6 1.86 2.8 3.0 Ovaria 21.0 5.4 7.3 8.6 (1.2) Renal 10.1 3.2 5.4 4.9 Prior data showed that CT-induced cytotoxic effects appeared to be highly selective toward cell lines expressing an upregulated density of Epidermal-like Growth Factor receptors, though CT appeared to unexpectedly promote EGFR phosphorylation. Enhanced EGFR activity in cancer cells and tumors is associated with increased growth, survival and angiogenesis of tumors. CT stimulated phosphorylation of the EGFR is a cellular response to the induction of apoptosis.
CD has poor anti-tumor effect in-vivo but it has recently been discovered the CD can block this rescue mechanism thereby enhancing the cytocidal activity. CD induces apoptosis in adeno-carcinoma A549 cells, as indicated by an increase in the sub-G(1) population, phosphatidyl-serine externalization, loss of mitochondrial membrane potential (Psi(m)) with cytochrome c release and activation of caspases 9 and 3. The signal transduction pathways involved in the effects of CD in A549 cells were evaluated and the results indicated that CD suppresses phosphorylation of EGFR and activation of phosphatidylinositol 3-kinase (PI3-K)/Akt and Janus tyrosine kinase (JAK) 2/signal transducer and activator of transcription (STAT) 3, all of which are downstream molecules in the EGFR signaling pathway. Additional testing suggested that PI3-K is an upstream activator of JAK2/STAT3. Together, the results of the study indicated that CD induces apoptosis in A549 cells by inactivating the EGFR, PI3-K/Akt and JAK2/STAT3 signaling pathways. Similar data was observed for MDA-MB-231 breast cancer cells, a highly metastatic human breast carcinoma cell line in addition to the inhibition of metastasis.
In wound-healing assay, the cell migration of oral squamous cells (Ca9-22 cells) was attenuated by CD in a dose- and time-responsive manner. After CD treatment, the MMP-2 and MMP-9 protein expressions were downregulated, and the phosphorylation of JNK and p38-MAPK was increased independent of ERK phosphorylation. It was determined that CD also has antiproliferative and -migrating effects on oral cancer cells involving the p38-MAPK and MMP-2/-9 pathways.
Secondary Pharmacology
CT can produce flaccid paralysis and death due to paralysis of respiratory muscles. Artificial respiration can keep the animals alive and, provided that the dose is not higher than 1.5 LD50, is followed by recovery. CD is a basic amphipathic peptide of relatively weak lethal toxicity when administered by the i.m. route (LD50 i.m. in mice 52 mg/kg; in rats 65 mg/kg). Strangely, when CT and CD are combined the toxic effects of CT are significantly reduces through an unknown mechanism. Additionally, CT has been reported to exert anti-viral activity which is thought to use a mechanism similar to the anti-tumor pathways.
Animal studies showed that CT administered by parenteral injection exhibited a dose-dependent analgesic action in mice using hot plate test and acetic acid-writhing test. The peak effect of CT analgesia was seen 3 h after its’ administration (in contrast to its pharmacokinetics). CT had significant analgesic action in rat tail-flick test. In the mouse acetic acid-writhing test, intra-cerebral ventricle administration of CT also produced marked analgesic effects. Atropine at 0.5 mg/kg (im) or 10 mg/kg (ip) or Naloxone at 3 mg/kg (ip) failed to block the analgesic effects of Crotoxin. In animal models of neuropathic pain induced by rat sciatic nerve transaction, it was revealed that CT has prolonged activity persisting for up to 64 days. It was found that the analgesia was mediated by activation of central muscarinic receptors and partially, by activation of alpha-adrenoceptors and 5-HT receptors.
CD’s antiproliferative activity is exerted through mechanisms associated with inflammatory activity so it is consistent that CD exhibits analgesic and anti-inflammatory activity. CD has been shown to be effective in animal models of acute, chronic and neuropathic pain including rheumatoid arthritis. It has also be found be orally bioavailable. It is reported to ameliorate kidney injury in several CKD animal models and potentiates the release of insulin from pancreatic cells.
- CONTRAINDICATIONS
-
PRECAUTIONS
Pregnancy: No significant data has been collected on the use of Crotoxin during pregnancy. No animal reproduction studies have been conducted to assess the effects of Crotoxin on the developing fetus.
- INTERACTIONS
- ADVERSE REACTIONS
- SERIOUS ADVERSE REACTIONS
-
FORMATS
CTC-310 is supplied in a solution of 0.9% saline for injection, at a concentration of 0.4mg/ml of each active with 0.01% benzalkonium chloride as a preservative. Dilution of this solution with saline for injection (SFI) can be useful for the initiation of therapy by subcutaneous injection in addition to tolerising the patient and their immune system to the drug. Always follow your health practitioner’s instructions.
-
DOSAGE AND ADMINISTRATION
The maximum reported tolerable dose of CTC-310 by intramuscular bolus injection is 0.017 mg/Kg. Injection site reactions are common though will subside in 2-3 weeks with continued use. With dose escalation procedures doses of 0.023 mg/Kg have been attained. Subcutaneous administration may be easier and more comfortable that intramuscular without any likely loss in activity.
- STORAGE
-
STABILITY
For maximum shelf life, the product should be stored at 4°C when not in use though shipping at transient ambient temperatures (10-30 °C) is not expected to significantly affect the product. CTC-310 is potent for a period in excess of 60 months when stored as directed.
Do not store at room temperature or strong sources of lights. Do not freeze or expose to high heat.
-
SAFETY INFORMATION
The toxic effects of CTC-310 are associated with CT. Paradoxically, CD reduces CT’s over toxicity.
Neurological: CT exerts analgesic activity presumed to be in the CNS despite the suggestion in pharmacokinetics studies that CT does not accumulate in the brain. Intracerebroventricular administration of CT to mice and rats yielded analgesic responses and was not toxic to the exposed nerve cells at the doses tested. In other studies CT appeared to increase the anxiety level in rodents. It is assumed that CT exerts these effects through peripheral pathways.
Cardiovascular: CT has no direct effects on the heart in-vivo. Rat hearts showed no response to the presence of CT though it is the most resistant species to this neurotoxin. In Guinea pigs, which have a high sensitivity to CT, no effect was noted in the heart unless protein was removed from the perfusion solution. At this point the contractile force of the heart was reduced by approximately 25%, reported to be a consequence of non-specific binding that occurred in the absence of albumin. No impact (NOEL) on heartbeat was noted at doses of 0.25mg/kg. Studies on the cardiovascular effects in anaesthetized dogs demonstrated that CT induced a transient and minor reduction (20%) in blood pressure on administration. With the administration of sequential doses of CT, the animal became resistant to the vascular effects of CT.
Respiration: CT is characterized by its ability to induce respiratory paralysis at high doses through blockade at the neuromuscular junction of the phrenic nerve. However, no respiratory effects were observed with the use of CT at 0.25 mg/Kg in dogs (maximum human dose is <0.015 mg/Kg). This would demonstrate a clear dose relationship between a NOEL and overt respiratory failure. In cases where respiratory paralysis was induced, the animal’s survival could be assured with the use of artificial ventilation. Crotoxin’s direct effects on the phrenic diaphragm has been well-established and provided the mechanism by which crotoxin interferes with respiration. Furthermore, it has been established that resistance to the toxic effects of Crotoxin are located at this site and resistance can be induced using low doses of Crotoxin.
Renal: The effects of Crotalus durissus terrificus venom and CT were studied on glomerular filtration rate (GFR), urinary flow (UF), perfusion pressure (PP) and percentage sodium tubular transport (%TNa+). The infusion of Crotalus durissus terrificus venom (10 microg/ml) and CT (10 microg/ml) increased GFR (control = 0.78 +/- 0.07, venom = 1.1 +/- 0.07, CT = 2.0 +/- 0.05 ml g(-1) min(-1), P<0.05) and UF (control = 0.20 +/- 0.02, venom = 0.32 +/- 0.03, CT = 0.70 +/- 0.05 ml g(-1) min(-1), P<0.05), and decreased %TNa+ (control = 75.0 +/- 2.3, venom = 62.9 +/- 1.0, CT = 69.0 +/- 1.0 ml g(-1) min(-1), P<0.05). The infusion of crude venom tended to reduce PP, although the effect was not significant, whereas with CT PP remained stable during the 100 min of perfusion. The kidneys perfused with crude venom and CT showed abundant protein material in the urinary space and tubules. It was concluded that Crotalus durissus terrificus venom and CT, its major component, caused acute nephrotoxicity in the isolated rat kidney. The current experiments demonstrated a direct effect of venom and CT on the perfused isolated kidney.
All in-vivo pharmacological studies have shown the toxic effects of CT to be reversible.
Chronic rodent toxicity studies with CTC-310
The LD50 of CTC-310 in mice after a single i.p. injection is approximately 0.45 mg/kg; the LD50 for i.m. administration is 0.93 mg/kg. When compared with the i.p. values for CT (0.095 mg/kg) and CD (1.7 mg/kg), the combined CTC-310 results in a 2.5-fold decrease specifically in CT-mediated neurotoxicity. Thus, the addition of the non-neurotoxic CD provides protection against the neurotoxic effects of CT. Different ratios were tested in vivo, and the optimal molar ratio was CD 3:1 CT (with a 1:1 mass ratio).
To evaluate the toxicity of CTC-310, 10 Sprague-Dawley rats were implanted with intraperitoneal slow-release devices and subjected to treatment with 0.5 microgram/g body weight/d for 14 days. Biochemical evidence at days 7 and 14 showed blood, muscular, renal and metabolic disturbance, mostly reversed by day 28. No significant changes were found in necropsy.
To assess i.v. administration of CTC-310 in rabbits, ten animals were subjected to surgical implant of fixed jugular catheter, by which they received daily IV doses of 0.03 mg/kg body weight of CTC-310 for 30 days (n = 8) or saline (n = 2). The procedure was well tolerated in all rabbits. One of the animals died after the sixth dose of VRCTC-310 with CNS involvement; two additional rabbits required dose-reduction. All other rabbits achieved 30 days of treatment and were sacrificed. All rabbits (even controls) developed lymphocytosis and mild anaemia, without changes in blood neutrophils. No changes were found in serum transaminases (GOT and GPT), cholesterol, triglycerides, and y-glutamyl transpeptidase. At necropsy, chronic granulation tissue was found surrounding the implant in all rabbits. CTC-310-treated rabbits presented generalised and marked swelling of hepatocytes, with areas of cytoplasmic vacuolisation. No abnormalities were found in kidney, heart, lung, spleen, adrenal gland, uterus, testes and ovary.
Acute and subchronic toxicities of CTC-310 have been studied in Beagle dogs. Single i.m. doses of 0.25, 0.5 and 1.0 mg/kg resulted in dose-dependent local muscular toxicity consisting of myofiber atrophy, interstitial edema and macrophage infiltration. AST, ALT and LDH levels also increased on day 2, returning to normal values on days 6-8. Local lesions were absent after recovery on day 45. At 2.0 mg/kg, signs of neurotoxicity (ataxia) appeared, in addition to vomitus, salivation, hematuria and myotoxicity in tongue and diaphragm on day 8. Local lesions healed with fibrosis at the site of injection on day 45. Administration of fixed (0.025 and 0.05 mg/kg) or escalating (0.025-0.1 mg/kg) daily doses for 30 days also produced local muscular damage, which was absent at day 75. The increases in AST, ALT and LDH serum activities on days 2-4 were independent of dosing schedule and sharply decreased on day 8, despite continuation of treatment. An escalating dose schedule of 0.025-2.0 mg/kg showed local muscle damage at the site of injection on day 31, however, there were no lesions of myotoxicity in the tongue or diaphragm and no clinical signs of neurotoxicity were observed. Animals tolerated the subchronic treatment better than the acute. The resolution of serum enzymes to normal values during treatment may be attributed to a decrease of sensitivity to CTC-310-mediated myotoxic effects.
There is no explanation for the unexpected reduction in overt toxicity when CT was combined with CD. Within the outlined toxicity studies the manifestation of toxic effects in animals (rabbits, cats, dogs and monkeys) using CT or CTC-310 were consistent implying that the majority of effects were contributed specifically by CT. CD served only to permit higher doses of CT be administered – thereby suggesting CD did not mask CT’s neurotoxic effects in-vivo. However, this is clearly a positive effect when it comes to the use of the product in humans. There is no evidence that CD masks other symptoms as the outcomes from toxicity studies for both products appear identical. Human experience does not reveal any subtle differences between the two products in the side-effect profile.
Pharmacokinetics
Studies on organ distribution of 125I-CT show that 1h after the intravenous injection into mice only 5% remains in plasma, while major amounts are found in liver (16%), kidneys (8.26%) and the carcass (48%). About 9% is excreted with the urine in three hours. Two hours after injection the liver contain 12% of the amount injected, kidney 3% and the carcass 22%. After 26 h only 12% of the radioactivity injected remains, mainly in liver.
Disposition of CT administered i.v. at the doses of 0.045 and 0.06 mg/kg was also followed by double-sandwich ELISA amplified by avidin-peroxidase. Plasma concentrations of CT fell rapidly in the first hour and then slowly up to a level below the detection limit of the assay 18h after injection. Disposition was consistent with a two-compartment open model with half-lives of 6.4 ± 0.4 min for the α-phase and 4.8-5.2 h for the β-phase. The AUC was 12 ± 1.9 µg.min.ml-1.
Following the intramuscular injection of CT at 0.1 mg/kg, there is a rapid absorption of toxin from the injection site, reaching a peak (50-60 ng/ml) 10-15 min after injection. The half-lives of the α and β phases were 23 ± 4 min and 4.7 ± 0.3 h, respectively. However, the AUC was 7.0 ±1.0 µg min.ml-1, i.e., smaller than that obtained for i.v. injection of a smaller dose. This may indicate that absorption from the injection site is rapid but incomplete, the toxin bound to muscular tissue being slowly released.
-
CLINICAL EXPERIENCE
Pure CT and CT/Cardiotoxin (CTC-310) formulations have been through 6 clinical investigations. The results of five of these studies have been published in scientific journals. The results from each condensed into table 1 and briefly summarized below. While CT is the principle active agent of interest the drug has been employed alone and in combination with CD, CD may allow the patient avoid the longer dose escalation phase of CT alone, and be more useful in subjects with advanced disease.. With that said, both products have been employed in human Phase I studies as listed in Table 2 & 3.
Table 2: Human Clinical Oncology Studies. i.m.; intramuscular, i.t.: intratumour, p.t.; peri-tumour, i.v.; intravenous
Product Indication No. of patients Duration Route Drug ADR CTC-310 Cancer 15 30 days i.m. 2 anaphylactic reactions CTC-310 Cancer 5 8 weeks i.t. & p.t. Not available CT Cancer 23 30 days, longest 117 days i.m. 1 anaphylactic reaction CT Cancer 6 Longest 75 days i.v. None reported CT Cancer 6 54 days i.v. grade 1 to 2 drug-related events of anorexia, diplopia and nystagmus. CT Cancer 6 35 days i.v. None reported A phase I study was performed to evaluate the maximum tolerated dose (MTD), safety profile and pharmacokinetic data with CTC-310 (Costa et al., 1997). Fifteen patients with refractory malignancies were entered after providing written informed consent. CTC-310 was administered as an intramuscular injection daily for 30 consecutive days. Doses were escalated from 0.0025 to 0.023 mg/kg. Toxicities included local pain at the injection site, eosinophilia, reversible diplopia and palpebral ptosis. Dose escalation was stopped at 0.023 mg/kg, when two patients had developed anaphylactoid reactions. Both cases had high drug-specific IgG by EIA. MTD was 0.017 mg/kg and the recommended dose for phase II studies is 0.017 mg/kg. Stabilization was found in six patients.
From December 1996 to August 1997, five patients with histologic confirmed local advanced cancer (breast cancer 3, squamous cell cancer of the hand 1, chordoma 1) were treated at Bernardo Houssay Hospital, Oncology Unit with CTC-310, at the full dose of 0.014 mg/kg once a week, inoculated peritumorally and distributed into four different injections around the tumor, for no less than eight courses. All patients gave written informed consent according to local ethics committee requirements (Costa et al., 1998).
Table 3: Cancer types observed in treated Subjects and disease response. Reference Product Dose Cancer types involved Plata et al.
9 patientsCT 0.3mg/ m2 (0.009mg/Kg)
i.m & i.t DailyBreast (2 CR), Pancreas (2 PR), liposarcoma (1 PR), Mesothelioma (1 PR), Fusocellular sarcoma (1 PR), Glioma (1 PR), Orbital adenocarcinoma (1 PR) Costa et al. 1997
15 patientsCTC-310 0.0025-0.023 mg/Kg
i.m. DailyNSCLC (1 PR, 1 PD), Breast (2 SD, 1PD), Laryngeal (1 SD), Cervical (1 SD, 1 PD), Ovarian (1 SD), Stomach ( PD), Pancreas (1 PD), Gall bladder (1 PD), Colon (1 PD), Rectum (1 SD), Maxilla (1 PD) Costa et al. 1998
5 patientsCTC-310 0.014mg/Kg
i.m. WeeklyBreast (2 CR, 1PR), Squamous cell (1 CR), Chordoma (1 PR) Hawkins
6 patientsCT 0.03mg/m2 (0.0009mg/Kg)
i.m. WeeklyColon cancer (4 PD), Pancreatic (2 PD) Cura et al.
23 patientsCT 0.03-0.22 mg/m2 (0.0009-0.007mg/Kg)
i.m. DailyBreast (1 CR, 2 PD), Rectal (1 PR), larynx (1 PR), Thyroid (1 PR), Fibrosarcoma (1 SD), Bladder (1 PD), Cervix (2 PD), Gastrointestinal (6 PD), NSCLC (3 PD), Head & Neck (1 PD), Fallopian (x1), Ewing sarcoma (1 PD), Liposarcoma (1 PD) Medioni et al
6 patientsCT 0.04-0.32 mg/m2
i.v. over 2 hr, 5 of 7 days per week.Colorectal Lieberkuhnian adenocarcinoma (PD), epithelioid mesothelioma (PD), non-small-cell lung cancer (PD), carcinoma of the unknown primary site (PD), invasive ductal carcinoma (PD) and ovarian papillary adenocarcinoma (PD). Delgado et al
6 patientsCT 0.04-0.32 mg/m2
i.v. pump, 7 days per week.Nasal squamous cell carcinoma (SD), glioblastomas (PD), endometrial adenocarcinoma (PD), NSCLC (PD) and prostatic carcinoma (SD) TOTAL 70 subjects 7 SD, 13 PR, 8 CR A complete response was observed in 3 pts (breast cancer 2, skin carcinoma of the hand 1), and a partial response was registered for the other two pts. The patient with local-advanced breast cancer (carcinoma en cuirasse) who was inoculated intra-and-peritumoral with CTC-310 for 6 weekly courses (0.014 mg/kg/week) with the drug had a >80% reduction in tumor. A 133 days follow-up demonstrated not only an objective complete response of the primary tumor mass, but the disappearance of supraclavicular tumor mass as well a significant reduction in lymphangitis. No toxicities were observed, except for a mild local pain at the site of the injection. It was concluded that weekly CTC-310 given by subcutaneous, peritumoral route is an active treatment for advanced skin metastatic tumors that is well tolerated and safe.
Phase I clinical trials of CT (Cura et al., 2002) was performed at the Hospital “General San Martìn” (Universidad Nacional de Rosario), Paranà, Entre Rìos. According to the protocol approved by the National Administration of Foods, Medicines and Medical Technology (A.N.M.A.T, Argentina), twenty six patients with solid tumours refractory to conventional therapy were admitted after signing a written informed consent. Twenty three patients were evaluated after the administration of CT as a daily intramuscular injection for 30 consecutive days (1-3 cycles) at doses from 0.03 to 0.22 mg.m-2. No drug-related deaths occurred in this study. Reversible (non-limiting) neuromuscular toxicity (Grades I to II) with diplopia and palpebral ptosis resulting from self-limited paresis of the external ocular muscles due to neuromuscular toxicity was the most characteristic side effect observed starting at the dose of 0.18 mg/m2.
Strabysmus and/or nystagmus appeared at 0.22 mg/m2. Patients complained by the discomfort during nystagmus episodes and no further increase in dose were considered. At the doses employed, neuromuscular toxicity did not impair the function of intrinsic ocular musculature and never extended to other muscular groups. No impairment of pharyngeal or laryngeal muscles was observed. Dysphonia, dysphagia, disartria or changes in FVC, suggesting drug related involvement of respiratory muscles were consistently absent (Cura et al., 2002). Neuromuscular toxicity did not require any dose adjustment and disappeared after one to three weeks even continuing the treatment. Except for transient increases (Grades I-III) in the levels of aminotransferases and creatinine kinase attributable to CT myotoxicity (Table III.1.3.1.5.2d), no other drug-related limiting toxicities were observed.
A Phase I clinical study with CT was completed at the George Pompidou Hospital (Paris, France). Titled as an “Open Label Phase I Clinical Trial of Crotoxin in Patients with Advanced Cancer using an Intravenous Route of Administration,– designed to be conducted in two cohorts, cohort 1 was conducted with six patients (one male and five females) with advanced solid tumors and no further therapeutic options (Medioni et al, 2017). The primary objectives of the cohort 1 study was to; 1. Confirm that human subjects can be made tolerant to i.v. CT; 2. Assess the safety and tolerability of CT administered i.v. to Stage IV cancer patients using intra-patient dose escalation procedure; 3.Define Maximum Tolerated Dose (MTD) associated with intra-patient dose escalation. The secondary objectives of the study were to determine the frequency and titer of anti-CT antibodies, document any objective anti-tumour responses and assess if CT could affect analgesic activity: evaluated using questionnaire filled by patients during daily infusions.
Cohort dose escalation was planned once per week, with weekends off. Crotoxin was administered to subjects as out-patients daily by i.v. administration at the hospital over a 2-hour period by saline drip. Patients received Polaramine 10 mg i.v. (antihistamine) before CT administration and Ranitidine 50mg (anti-emetic) intravenously prior to treatment to minimize the potential for anaphylaxis. The escalation schedule extended over 54 days, with dose increased from 0.04 to 0.32 mg/m2. The patients were monitored daily at the clinic for the duration of the infusion (2 hours) and observed for 30 min following the infusion for adverse reactions. A total of 15 patients were screened and 6 were enrolled. Patients were treated with 8 cycles of Crotoxin administered i.v. over 2h daily, 5 days out of 7, with weekly intra-patient dose escalation. Dose escalation started at 0.04 mg/m2/day and the last dose was 0.32 mg/m2/day. Dose escalation extended over a period of 54 days (8 weeks).
For Serious Adverse Events (SAEs) unrelated to the study drug there were none in Patient 001, Patient 003 & Patient 004 (Medioni et al., 2018). Patient 002 experienced Anemia at dose level 6 (0.24 mg/m2/day) at day 37, grade 3, unrelated, reported as SAE, not reported as (Sudden Unexpected Serious Adverse Reaction (SUSAR), study drug was interrupted for 1 day. Patient 005 experience Hypoxia at dose level 5 (0.20 mg/m2/day) at day 29, grade 3, unrelated, reported as SAE, not reported as SUSAR. The study drug dose was not changed though treatment and hospitalization was required. Also, sepsis grade 4 and confusion grade 2 at dose level 5 (0.20 mg/m2/day) at day 35, unrelated, reported as SAE, not reported as SUSAR, patient died 2 days after stopping the study. Patient 006 also experienced Hypoxia at dose level at dose level 3 (0.12 mg/m2/day) at day 17, grade 2, unrelated, reported as SAE, not reported as SUSAR study drug dose not changed though treatment and hospitalization was required. Fever was reported at dose level 6 (0.24 mg/m2/day) at day 43, grade 1, unrelated, reported as SAE, not reported as SUSAR, study drug dose was interrupted for 1 day requiring treatment and hospitalization.
Table 3. Summary of Cohort 1 Adverse Event during Study Subject no Unrelated to study drug Related to study drug Total AE SAE AE SAE 001 9 0 4 0 13 002 11 1 0 0 12 003 8 0 0 0 8 004 25 0 1 0 26 005 22 3 0 0 25 006 15 2 1 0 18 There were no reported SAEs or SUSARs related to the study drug. Adverse Events (AEs) related to the study drug were not reported in Subjects 002, 003 & 005. Diplopia and nystagmus were the most common. For those patients for whom pain was reported appeared to experience relief when CT was administered. The analgesic effect in all subjects appeared to dissipate during the weekends when no drug was being administered. The reported analgesic activity of Crotoxin in the Cura et al study (2002) was confirmed. All six patients presented Progressive Disease potentially due to the slow dose escalation protocol. It was established that intra-patient dose escalation of Crotoxin was safer than simple bolus administration.
Part 2 of the Phase I study was recently completed at the University Hospital Pitié-Salpêtrière (Paris, France). It followed design of Medioni et al (2017) in intra-patient dose escalation study to treat six patients (5 males and 1 female) with advanced solid tumours and no further treatment options: 1 nasal squamous cell carcinoma, 2 glioblastomas, 1 endometrial adenocarcinoma, 1 NSCLC and 1 prostatic carcinoma (Gil-Delgado et al., 2018). Lightweight Rythmic™ pump capable of continuous delivery (no weekend breaks) allowed patients to stay at home. Dose escalation from 0.08 to 0.64 mg/m2/day over 35 days and was carried on Mondays, Wednesdays and Fridays, followed by 2h observation at the clinic. Two of 6 patients developed possibly drug-related G1 diplopia and 1/6 pts increased ASAT/ALAT. One patient recruited with pre-existent diarrhoea syndrome with uncontrolled G2 hypomagnesaemia, G3 hypokalaemia and G2 anaemia, developed complete arrhythmia with asymptomatic atrial fibrillation that resolved with amiodarone. Patient was hospitalised for observation and the event was classified as a possible study drug-related SAE as well as related to the digestive syndrome and tubulopathy resulting from previous chemotherapy (nivolumab and platinum salts). It was concluded CT dose escalation is safe but too slow, doses achieved too low and too late for advanced pts. However, stable disease was observed in 2/6 patients and no DLT or MTD were reached.
Overall, of the 70 subjects recorded as having been treated with CT or CTC-310, 8 have had complete remissions, 13 had partial responses and 8 had stable disease. These outcomes were achieved in the absence of optimized treatment programs.
-
CLINICAL REFERENCES
- Costa LA, Miles F, Diez RA, Araujo CE, Coni Molina CM and Cervellino JC; Phase I study of VRCTC310, a purified phospholipase A2 purified from snake venom, in patients with refractory cancer: safety and pharmacokinetic data, Anticancer Drugs 8 (9), 829-34 (1997)
- Costa LA, Miles F, Araujo CE, and Villaruba VG. Intratumoral therapy with VRCTC-310 for refractory skin metastatic breast cancer. Preliminary report. Euro J. Cancer, 34, suppl 5, pg S22 (1998)
- Costa LA, Fornari MC, Berardi VE, Miloes HA and Diez RA; In vivo effect of snake phospholipase A2 (CT + Cardiotoxin) on serum Il-1alpha, TNF-alpha and IL-1ra level in humans, Immunol Lett, Jan 1, 75(2), 137-41 (2001).
- Cura, JE, Blanzaco DP, Brisson CB, Cura MA, Cabrol R, Larrateguy L, Mendez C, Sechi JC, Silveira JS, Theiller E, deRoodt AR, Vidal JC. Phase I and Pharmocokinetic study of Crotoxin (Cytotoxic PLA2, NSC-624244) in Patients with Advanced Cancer. Clinical Cancer Research, Vol. 8, 1033-1041 (2002).
- Gil Delgado M, Bray DH, Delgado FM, Spano JP, Gougis P, Brentano C, Idbaih A, Reid P, Benlhassan K, Diaw K, Khayat D.. Continuous i.v. CROTOXIN in advanced cancer: intra-patient dose escalation, AACR abstract, 2018 accepted
- Medioni J, Brizard M, Elaidi R, Reid PF, Benlhassan K, Bray D. Innovative design for a phase 1 trial with intra-patient dose escalation: The Crotoxin study. Contemp Clin Trials Comm 7 (2017): 186-168
- Medioni J, Brizard M, Elaidi R, Reid PF, Benlhassan K, Bray D. Innovative design for a Phase 1 trial with intra-patient dose escalation: the Crotoxin study. AACR abstract, 2018 accepted
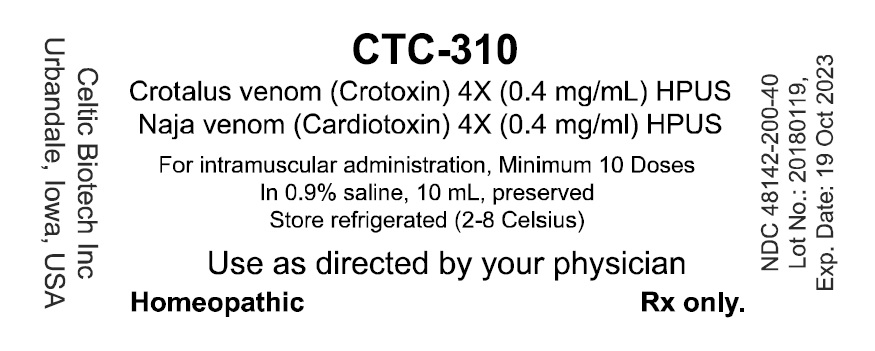
- PRINCIPAL DISPLAY PANEL - NDC: 48142-200-40 - 10 mL Vial Label
-
INGREDIENTS AND APPEARANCE
CTC-310
crotalus durissus terrificus venom and cardiotoxin iii injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 48142-200 Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CROTALUS DURISSUS TERRIFICUS VENOM (UNII: 2XF6I0446G) (CROTALUS DURISSUS TERRIFICUS VENOM - UNII:2XF6I0446G) CROTALUS DURISSUS TERRIFICUS VENOM 4 [hp_X] in 1 mL CARDIOTOXIN III (UNII: 0QBH3Y8M6J) (CARDIOTOXIN III - UNII:0QBH3Y8M6J) CARDIOTOXIN III 4 [hp_X] in 1 mL Inactive Ingredients Ingredient Name Strength SODIUM CHLORIDE (UNII: 451W47IQ8X) 9 mg in 1 mL BENZALKONIUM CHLORIDE (UNII: F5UM2KM3W7) 0.1 mg in 1 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 48142-200-40 10 mL in 1 VIAL, MULTI-DOSE; Type 0: Not a Combination Product 04/30/2018 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date Unapproved homeopathic 04/30/2018 Labeler - Celtic Biotech Iowa, Inc. (079574151) Establishment Name Address ID/FEI Business Operations Complete Pharmacy and Medical Solutions, LLC 004417520 API MANUFACTURE(48142-200) , HUMAN DRUG COMPOUNDING OUTSOURCING FACILITY(48142-200) , MANUFACTURE(48142-200)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.