CEFPROZIL tablet, film coated
Cefprozil by
Drug Labeling and Warnings
Cefprozil by is a Prescription medication manufactured, distributed, or labeled by Rising Pharma Holdings, Inc., Aurobindo Pharma Limited. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
- SPL UNCLASSIFIED SECTION
-
DESCRIPTION
Cefprozil is a semi-synthetic broad-spectrum cephalosporin antibiotic.
Cefprozil is a cis and trans isomeric mixture (≥90% cis). The chemical name for the monohydrate is (6R,7R)-7-[(R)-2-Amino-2-(p-hydroxyphenyl)acetamido]-8-oxo-3-propenyl-5-thia-1-azabicyclo[4.2.0]oct-2-ene-2-carboxylic acid monohydrate, and the structural formula is:
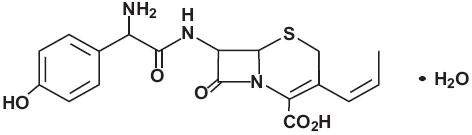
Cefprozil USP is a white to yellowish powder with a molecular formula for the monohydrate of C18H19N3O5SH2O and a molecular weight of 407.45.
Cefprozil tablets USP are intended for oral administration.
Cefprozil tablets USP contain cefprozil USP equivalent to 250 mg or 500 mg of anhydrous cefprozil. In addition, each tablet contains the following inactive ingredients: microcrystalline cellulose, sodium starch glycolate, magnesium stearate, hypromellose, polyethylene glycol, polysorbate 80, and titanium dioxide. The 250 mg tablets also contain FD&C Yellow #6 aluminum lake. The tablets are imprinted with edible ink containing shellac glaze, black iron oxide, propylene glycol and ammonium hydroxide. -
CLINICAL PHARMACOLOGY
The pharmacokinetic data were derived from the capsule formulation; however, bioequivalence has been demonstrated for the oral solution, capsule, tablet, and suspension formulations under fasting conditions.
Following oral administration of cefprozil to fasting subjects, approximately 95% of the dose was absorbed. The average plasma half-life in normal subjects was 1.3 hours, while the steady-state volume of distribution was estimated to be 0.23 L/kg. The total body clearance and renal clearance rates were approximately 3 mL/min/kg and 2.3 mL/min/kg, respectively.
Average peak plasma concentrations after administration of 250 mg, 500 mg, or 1 g doses of cefprozil to fasting subjects were approximately 6.1, 10.5, and 18.3 mcg/mL, respectively, and were obtained within 1.5 hours after dosing. Urinary recovery accounted for approximately 60% of the administered dose. (See Table.)
*Data represent mean values of 12 healthy volunteers. Dosage
(mg)
Mean Plasma Cefprozil Concentrations (mcg/mL)*
8-hour Urinary Excretion (%)
Peak appx.1.5h
4h
8h
250 mg
6.1
1.7
0.2
60%
500 mg
10.5
3.2
0.4
62%
1000 mg
18.3
8.4
1.0
54%
During the first 4-hour period after drug administration, the average urine concentrations following 250 mg, 500 mg, and 1 g doses were approximately 700 mcg/mL, 1000 mcg/mL, and 2900 mcg/mL, respectively.
Administration of cefprozil with food did not affect the extent of absorption (AUC) or the peak plasma concentration (Cmax) of cefprozil. However, there was an increase of 0.25 to 0.75 hours in the time to maximum plasma concentration of cefprozil (Tmax).
The bioavailability of the capsule formulation of cefprozil was not affected when administered 5 minutes following an antacid.
Plasma protein binding is approximately 36% and is independent of concentration in the range of 2 mcg/mL to 20 mcg/mL.
There was no evidence of accumulation of cefprozil in the plasma in individuals with normal renal function following multiple oral doses of up to 1000 mg every 8 hours for 10 days.
In patients with reduced renal function, the plasma half-life may be prolonged up to 5.2 hours depending on the degree of the renal dysfunction. In patients with complete absence of renal function, the plasma half-life of cefprozil has been shown to be as long as 5.9 hours. The half-life is shortened during hemodialysis. Excretion pathways in patients with markedly impaired renal function have not been determined. (See PRECAUTIONS and DOSAGE AND ADMINISTRATION.)
In patients with impaired hepatic function, the half-life increases to approximately 2 hours. The magnitude of the changes does not warrant a dosage adjustment for patients with impaired hepatic function.
Healthy geriatric volunteers (≥65 years old) who received a single 1 g dose of cefprozil had 35% to 60% higher AUC and 40% lower renal clearance values compared with healthy adult volunteers 20 to 40 years of age. The average AUC in young and elderly female subjects was approximately 15% to 20% higher than in young and elderly male subjects. The magnitude of these age- and gender-related changes in the pharmacokinetics of cefprozil is not sufficient to necessitate dosage adjustments.
Adequate data on CSF levels of cefprozil are not available.
Comparable pharmacokinetic parameters of cefprozil are observed between pediatric patients (6 months to 12 years) and adults following oral administration of selected matched doses. The maximum concentrations are achieved at 1 to 2 hours after dosing.
The plasma elimination half-life is approximately 1.5 hours. In general, the observed plasma concentrations of cefprozil in pediatric patients at the 7.5, 15, and 30 mg/kg doses are similar to those observed within the same time frame in normal adult subjects at the 250, 500, and 1000 mg doses, respectively. The comparative plasma concentrations of cefprozil in pediatric patients and adult subjects at the equivalent dose level are presented in the table below.an=11; bn=5; cn=9; dn=11.
Mean (SD) Plasma Cefprozil Concentrations (mcg/mL)
Population
Dose
1 h
2 h
4 h
6 h
TT1/2 (h)
children (n=18)
7.5 mg/kg
4.70 (1.57)
3.99 (1.24)
0.91 (0.30)
0.23a (0.13)
0.94 (0.32)
adults (n=12)
250 mg
4.82 (2.13)
4.92 (1.13)
1.70b (0.53)
0.53 (0.17)
1.28 (0.34)
children (n=19)
15 mg/kg
10.86 (2.55)
8.47 (2.03)
2.75 (1.07)
0.61c (0.27)
1.24 (0.43)
adults (n=12)
500 mg
8.39 (1.95)
9.42 (0.98)
3.18d (0.76)
1.00d (0.24)
1.29 (0.14)
children (n=10)
30 mg/kg
16.69 (4.26)
17.61 (6.39)
8.66 (2.70)
—
2.06 (0.21)
adults (n=12)
1000 mg
11.99 (4.67)
16.95 (4.07)
8.36 (4.13)
2.79 (1.77)
1.27 (0.12)
Microbiology
Cefprozil has in vitro activity against a broad range of gram-positive and gram-negative bacteria. The bactericidal action of cefprozil results from inhibition of cell-wall synthesis. Cefprozil has been shown to be active against most strains of the following microorganisms both in vitro and in clinical infections as described in the INDICATIONS AND USAGE section.
Aerobic gram-positive microorganisms: Aerobic gram-negative microorganisms:
Staphylococcus aureus (including Haemophilus influenzae (including β-
β-lactamase-producing strains) lactamase-producing strains)
NOTE: Cefprozil is inactive against Moraxella (Branhamella) catarrhalis
methicillin-resistant staphylococci. (including β-lactamase-producing strains)
Streptococcus pneumoniae
Streptococcus pyogenes
The following in vitro data are available; however, their clinical significance is unknown. Cefprozil exhibits in vitro minimum inhibitory concentrations (MICs) of 8 mcg/mL or less against most (≥90%) strains of the following microorganisms; however, the safety and effectiveness of cefprozil in treating clinical infections due to these microorganisms have not been established in adequate and well-controlled clinical trials.
Aerobic gram-positive microorganisms:
Enterococcus durans Staphylococcus warneri
Enterococcus faecalis Streptococcus agalactiae
Listeria monocytogenes Streptococci (Groups C,D,F, and G)
Staphylococcus epidermidis viridans group Streptococci
Staphylococcus saprophyticus
NOTE: Cefprozil is inactive against Enterococcus faecium.
Aerobic gram-negative microorganisms:
Citrobacter diversus Proteus mirabilis
Escherichia coli Salmonella spp.
Klebsiella pneumoniae Shigella spp.
Neisseria gonorrhoeae Vibrio spp.
(including β-lactamase-producing strains)
NOTE: Cefprozil is inactive against most strains of Acinetobacter, Enterobacter, Morganella morganii, Proteus vulgaris, Providencia, Pseudomonas, and Serratia.
Anaerobic microorganisms:
Prevotella (Bacteroides) melaninogenicus Fusobacterium spp.
Clostridium difficile Peptostreptococcus spp.
Clostridium perfringens Propionibacterium acnes
NOTE: Most strains of the Bacteroides fragilis group are resistant to cefprozil.
Susceptibility Testing
For specific information regarding susceptibility test interpretive criteria and associated test methods and quality control standards recognized by FDA for this drug, please see: https://www.fda.gov/STIC. -
INDICATIONS AND USAGE
To reduce the development of drug-resistant bacteria and maintain the effectiveness of cefprozil and other antibacterial drugs, cefprozil should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
Cefprozil tablets are indicated for the treatment of patients with mild to moderate infections caused by susceptible strains of the designated microorganisms in the conditions listed below:
UPPER RESPIRATORY TRACT
Pharyngitis/tonsillitis caused by Streptococcus pyogenes.
NOTE: The usual drug of choice in the treatment and prevention of streptococcal infections, including the prophylaxis of rheumatic fever, is penicillin given by the intramuscular route. Cefprozil is generally effective in the eradication of Streptococcus pyogenes from the nasopharynx; however, substantial data establishing the efficacy of cefprozil in the subsequent prevention of rheumatic fever are not available at present.
Otitis Media caused by Streptococcus pneumoniae, Haemophilus influenzae (including β-lactamase-producing strains), and Moraxella (Branhamella) catarrhalis (including β-lactamase-producing strains). (See CLINICAL STUDIES.)
NOTE: In the treatment of otitis media due to β-lactamase producing organisms, cefprozil had bacteriologic eradication rates somewhat lower than those observed with a product containing a specific β-lactamase inhibitor. In considering the use of cefprozil, lower overall eradication rates should be balanced against the susceptibility patterns of the common microbes in a given geographic area and the increased potential for toxicity with products containing β-lactamase inhibitors.
Acute Sinusitis caused by Streptococcus pneumoniae, Haemophilus influenzae (including β-lactamase-producing strains), and Moraxella (Branhamella) catarrhalis (including β-lactamase-producing strains).
LOWER RESPIRATORY TRACT
Acute Bacterial Exacerbation of Chronic Bronchitis caused by Streptococcus pneumoniae, Haemophilus influenzae (including β-lactamase-producing strains), and Moraxella (Branhamella) catarrhalis (including β-lactamase-producing strains).
SKIN AND SKIN STRUCTURE
Uncomplicated Skin and Skin-Structure Infections caused by Staphylococcus aureus (including penicillinase-producing strains) and Streptococcus pyogenes. Abscesses usually require surgical drainage. - CONTRAINDICATIONS
-
WARNINGS
BEFORE THERAPY WITH CEFPROZIL IS INSTITUTED, CAREFUL INQUIRY SHOULD BE MADE TO DETERMINE WHETHER THE PATIENT HAS HAD PREVIOUS HYPERSENSITIVITY REACTIONS TO CEFPROZIL, CEPHALOSPORINS, PENICILLINS, OR OTHER DRUGS. IF THIS PRODUCT IS TO BE GIVEN TO PENICILLIN-SENSITIVE PATIENTS, CAUTION SHOULD BE EXERCISED BECAUSE CROSS-SENSITIVITY AMONG β-LACTAM ANTIBIOTICS HAS BEEN CLEARLY DOCUMENTED AND MAY OCCUR IN UP TO 10% OF PATIENTS WITH A HISTORY OF PENICILLIN ALLERGY. IF AN ALLERGIC REACTION TO CEFPROZIL OCCURS, DISCONTINUE THE DRUG. SERIOUS ACUTE HYPERSENSITIVITY REACTIONS MAY REQUIRE TREATMENT WITH EPINEPHRINE AND OTHER EMERGENCY MEASURES, INCLUDING OXYGEN, INTRAVENOUS FLUIDS, INTRAVENOUS ANTIHISTAMINES, CORTICOSTEROIDS, PRESSOR AMINES, AND AIRWAY MANAGEMENT, AS CLINICALLY INDICATED.
Clostridium difficile associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents, including cefprozil, and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon leading to overgrowth of C. difficile.
C. difficile produces toxins A and B which contribute to the development of CDAD. Hypertoxin-producing strains of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibiotic use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents.
If CDAD is suspected or confirmed, ongoing antibiotic use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibiotic treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated. -
PRECAUTIONS
General
Prescribing cefprozil tablets in the absence of proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
In patients with known or suspected renal impairment (see DOSAGE AND ADMINISTRATION), careful clinical observation and appropriate laboratory studies should be done prior to and during therapy. The total daily dose of cefprozil tablets should be reduced in these patients because high and/or prolonged plasma antibiotic concentrations can occur in such individuals from usual doses. Cephalosporins, including cefprozil tablets, should be given with caution to patients receiving concurrent treatment with potent diuretics since these agents are suspected of adversely affecting renal function.
Prolonged use of cefprozil tablets may result in the overgrowth of nonsusceptible organisms. Careful observation of the patient is essential. If superinfection occurs during therapy, appropriate measures should be taken.
Cefprozil should be prescribed with caution in individuals with a history of gastrointestinal disease particularly colitis.
Positive direct Coombs’ tests have been reported during treatment with cephalosporin antibiotics.Information for Patients
Patients should be counseled that antibacterial drugs including cefprozil tablets should only be used to treat bacterial infections. They do not treat viral infections (e.g., the common cold). When cefprozil tablets are prescribed to treat a bacterial infection, patients should be told that although it is common to feel better early in the course of therapy, the medication should be taken exactly as directed. Skipping doses or not completing the full course of therapy may (1) decrease the effectiveness of the immediate treatment and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by cefprozil tablets or other antibacterial drugs in the future.
Diarrhea is a common problem caused by antibiotics which usually ends when the antibiotic is discontinued. Sometimes after starting treatment with antibiotics, patients can develop watery and bloody stools (with or without stomach cramps and fever) even as late as two or more months after having taken the last dose of the antibiotic. If this occurs, patients should contact their physician as soon as possible.Drug Interactions
Nephrotoxicity has been reported following concomitant administration of aminoglycoside antibiotics and cephalosporin antibiotics. Concomitant administration of probenecid doubled the AUC for cefprozil.
The bioavailability of the capsule formulation of cefprozil was not affected when administered 5 minutes following an antacid.Drug/laboratory Test Interactions
Cephalosporin antibiotics may produce a false positive reaction for glucose in the urine with copper reduction tests (Benedict’s or Fehling’s solution or with Clinitest® tablets1), but not with enzyme-based tests for glycosuria (e,g., Clinistix®). A false negative reaction may occur in the ferricyanide test for blood glucose. The presence of cefprozil in the blood does not interfere with the assay of plasma or urine creatinine by the alkaline picrate method.
1 Clinitest® and Clinistix® are registered trademarks of Bayer Healthcare LLC.Carcinogenesis, Mutagenesis, Impairment of Fertility
Long term in vivo studies have not been performed to evaluate the carcinogenic potential of cefprozil.
Cefprozil was not found to be mutagenic in either the Ames Salmonella or E. coli WP2 urvA reversion assays or the Chinese hamster ovary cell HGPRT forward gene mutation assay and it did not induce chromosomal abnormalities in Chinese hamster ovary cells or unscheduled DNA synthesis in rat hepatocytes in vitro. Chromosomal aberrations were not observed in bone marrow cells from rats dosed orally with over 30 times the highest recommended human dose based upon mg/m2.
Impairment of fertility was not observed in male or female rats given oral doses of cefprozil up to 18.5 times the highest recommended human dose based upon mg/m2.Pregnancy
Teratogenic Effects: Pregnancy Category B
Reproduction studies have been performed in rabbits, mice, and rats using oral doses of cefprozil of 0.8, 8.5, and 18.5 times the maximum daily human dose (1000 mg) based upon mg/m2, and have revealed no harm to the fetus. There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed.
Labor and Delivery
Cefprozil has not been studied for use during labor and delivery. Treatment should only be given if clearly needed.
Nursing Mothers
Small amounts of cefprozil (<0.3% of dose) have been detected in human milk following administration of a single 1 gram dose to lactating women. The average levels over 24 hours ranged from 0.25 to 3.3 mcg/mL. Caution should be exercised when cefprozil tablets are administered to a nursing woman, since the effect of cefprozil on nursing infants is unknown.
Pediatric Use
(See INDICATIONS AND USAGE and DOSAGE AND ADMINISTRATION.)
The safety and effectiveness of cefprozil in the treatment of otitis media have been established in the age groups 6 months to 12 years. Use of cefprozil tablets for the treatment of otitis media is supported by evidence from adequate and well-controlled studies of cefprozil in pediatric patients. (See CLINICAL STUDIES.)
The safety and effectiveness of cefprozil in the treatment of pharyngitis/tonsillitis or uncomplicated skin and skin-structure infections have been established in the age groups 2 to 12 years. Use of cefprozil for the treatment of these infections is supported by evidence from adequate and well-controlled studies of cefprozil in pediatric patients.
The safety and effectiveness of cefprozil in the treatment of acute sinusitis have been established in the age groups 6 months to 12 years. Use of cefprozil in these age groups is supported by evidence from adequate and well-controlled studies of cefprozil in adults.
Safety and effectiveness in pediatric patients below the age of 6 months have not been established for the treatment of otitis media or acute sinusitis, or below the age of 2 years for the treatment of pharyngitis/tonsillitis or uncomplicated skin and skin-structure infections. However, accumulation of other cephalosporin antibiotics in newborn infants (resulting from prolonged drug half-life in this age group) has been reported.Geriatric Use
Of the more than 4500 adults treated with cefprozil tablets in clinical studies, 14% were 65 years and older, while 5% were 75 years and older. When geriatric patients received the usual recommended adult doses, their clinical efficacy and safety were comparable to clinical efficacy and safety in nongeriatric adult patients. Other reported clinical experience has not identified differences in responses between elderly and younger patients, but greater sensitivity of some older individuals to the effects of cefprozil tablets cannot be excluded (see CLINICAL PHARMACOLOGY).
Cefprozil is known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection and it may be useful to monitor renal function. See DOSAGE AND ADMINISTRATION for dosing recommendations for patients with impaired renal function. -
ADVERSE REACTIONS
The adverse reactions to cefprozil are similar to those observed with other orally administered cephalosporins. Cefprozil was usually well tolerated in controlled clinical trials. Approximately 2% of patients discontinued cefprozil therapy due to adverse events.
The most common adverse effects observed in patients treated with cefprozil are:
Gastrointestinal: Diarrhea (2.9%), nausea (3.5%), vomiting (1%), and abdominal pain (1%).
Hepatobiliary: Elevations of AST (SGOT) (2%), ALT (SGPT) (2%), alkaline phosphatase (0.2%), and bilirubin values (<0.1%). As with some penicillins and some other cephalosporin antibiotics, cholestatic jaundice has been reported rarely.
Hypersensitivity: Rash (0.9%), urticaria (0.1%). Such reactions have been reported more frequently in children than in adults. Signs and symptoms usually occur a few days after initiation of therapy and subside within a few days after cessation of therapy.
CNS: Dizziness (1%), hyperactivity, headache, nervousness, insomnia, confusion, and somnolence have been reported rarely (<1%). All were reversible.
Hematopoietic: Decreased leukocyte count (0.2%), eosinophilia (2.3%).
Renal: Elevated BUN (0.1%), serum creatinine (0.1%).
Other: Diaper rash and superinfection (1.5%), genital pruritus and vaginitis (1.6%).
The following adverse events, regardless of established causal relationship to cefprozil tablets, have been rarely reported during postmarketing surveillance: anaphylaxis, angioedema, colitis (including pseudomembranous colitis), erythema multiforme, fever, serum-sickness like reactions, Stevens-Johnson syndrome, and thrombocytopenia.Cephalosporin class paragraph
In addition to the adverse reactions listed above which have been observed in patients treated with cefprozil, the following adverse reactions and altered laboratory tests have been reported for cephalosporin-class antibiotics:
Aplastic anemia, hemolytic anemia, hemorrhage, renal dysfunction, toxic epidermal necrolysis, toxic nephropathy, prolonged prothrombin time, positive Coombs’ test, elevated LDH, pancytopenia, neutropenia, agranulocytosis.
Several cephalosporins have been implicated in triggering seizures, particularly in patients with renal impairment, when the dosage was not reduced. (See DOSAGE AND ADMINISTRATION and OVERDOSAGE.) If seizures associated with drug therapy occur, the drug should be discontinued. Anticonvulsant therapy can be given if clinically indicated. -
OVERDOSAGE
Single 5000 mg/kg oral doses of cefprozil caused no mortality or signs of toxicity in adult, weanling, or neonatal rats, or adult mice. A single oral dose of 3000 mg/kg caused diarrhea and loss of appetite in cynomolgus monkeys, but no mortality.
Cefprozil is eliminated primarily by the kidneys. In case of severe overdosage, especially in patients with compromised renal function, hemodialysis will aid in the removal of cefprozil from the body. -
DOSAGE AND ADMINISTRATION
Cefprozil tablets are administered orally.
Population/Infection Dosage
(mg)Duration
(days)a In the treatment of infections due to Streptococcus pyogenes, cefprozil should be administered for at least 10 days.
b Not to exceed recommended adult doses.
ADULTS (13 years and older)
UPPER RESPIRATORY TRACT
Pharyngitis/Tonsillitis
500 q24h
10a
Acute Sinusitis
(For moderate to severe infections, the higher dose should be used)
250 q12h or
500 q12h
10
LOWER RESPIRATORY TRACT
Acute Bacterial Exacerbation of Chronic Bronchitis
500 q12h
10
SKIN AND SKIN STRUCTURE
Uncomplicated Skin and Skin Structure Infections
250 q12h or
500 q24h or
500 q12h
10
CHILDREN (2 years to 12 years)
UPPER RESPIRATORY TRACTb
Pharyngitis/Tonsillitis
7.5 mg/kg q12h
10a
SKIN AND SKIN STRUCTURE
Uncomplicated Skin and Skin Structure Infections
20 mg/kg q24h
10
INFANTS & CHILDREN (6 months to 12 years)
UPPER RESPIRATORY TRACTb
Otitis Media
(See INDICATIONS AND USAGE and CLINICAL STUDIES)
15 mg/kg q12h
10
Acute Sinusitis
(For moderate to severe infections, the higher dose should be used)
7.5 mg/kg q12h or
15 mg/kg q12h
10
Renal Impairment
Cefprozil may be administered to patients with impaired renal function. The following dosage schedule should be used.
Creatinine Clearance
(mL/min)Dosage
(mg)Dosing Interval * Cefprozil is in part removed by hemodialysis; therefore, cefprozil should be administered after the completion of hemodialysis.
30 to 120
0 to 29*
standard
50% of standard
standard
standard
-
HOW SUPPLIED
Cefprozil Tablets, USP 250 mg are orange colored, biconvex, film-coated capsule-shaped tablets, imprinted “C16” with black ink on one side.
Bottles of 100 NDC: 57237-036-01
Cefprozil Tablets, USP 500 mg are white, biconvex, film-coated capsule-shaped tablets, imprinted “C17” with black ink on one side.
Bottles of 50 NDC: 57237-037-50
Bottles of 100 NDC: 57237-037-01
Store at 20° to 25°C (68° to 77°F); excursions permitted to 15° to 30°C (59° to 86°F) [see USP Controlled Room Temperature]. -
CLINICAL STUDIES
Study One:
In a controlled clinical study of acute otitis media performed in the United States where significant rates of β-lactamase-producing organisms were found, cefprozil was compared to an oral antimicrobial agent that contained a specific β-lactamase inhibitor. In this study, using very strict evaluability criteria and microbiologic and clinical response criteria at the 10 to 16 days post-therapy follow-up, the following presumptive bacterial eradication/clinical cure outcomes i.e., clinical success) and safety results were obtained:
U.S. Acute Otitis Media Study Cefprozil vs β-lactamase inhibitor-containing control drug EFFICACY:
Pathogen
% of Cases with Pathogen
(n=155)
Outcome
S. pneumoniae
48.4%
cefprozil success rate 5% better than control
H. influenzae
35.5%
cefprozil success rate 17% less than control
M. catarrhalis
13.5%
cefprozil success rate 12% less than control
S. pyogenes
2.6%
cefprozil equivalent to control
Overall
100.0%
cefprozil success rate 5% less than control
SAFETY:
The incidences of adverse events, primarily diarrhea and rash*, were clinically and statistically significantly higher in the control arm versus the cefprozil arm.
Age Group Cefprozil Control *The majority of these involved the diaper area in young children.
6 months to 2 years
21%
41%
3 to 12 years
10%
19%
Study Two:
In a controlled clinical study of acute otitis media performed in Europe, cefprozil was compared to an oral antimicrobial agent that contained a specific β-lactamase inhibitor. As expected in a European population, this study population had a lower incidence of β-lactamase-producing organisms than usually seen in U.S. trials. In this study, using very strict evaluability criteria and microbiologic and clinical response criteria at the 10 to 16 days post-therapy follow-up, the following presumptive bacterial eradication/clinical cure outcomes (i.e., clinical success) were obtained:
European Acute Otitis Media Study Cefprozil vs β-lactamase inhibitor-containing control drug EFFICACY:
Pathogen
% of Cases with Pathogen (n=47)
Outcome
S. pneumoniae
51.0%
cefprozil equivalent to control
H. influenzae
29.8%
cefprozil equivalent to control
M. catarrhalis
6.4%
cefprozil equivalent to control
S. pyogenes
12.8%
cefprozil equivalent to control
Overall
100.0%
cefprozil equivalent to control
SAFETY:
The incidence of adverse events in the cefprozil arm was comparable to the incidence of adverse events in the control arm (agent that contained a specific β-lactamase inhibitor).
Distributed by:
Rising Health, LLC
Saddle Brook, NJ 07663
Made in India
Code: TS/DRUGS/78/1996
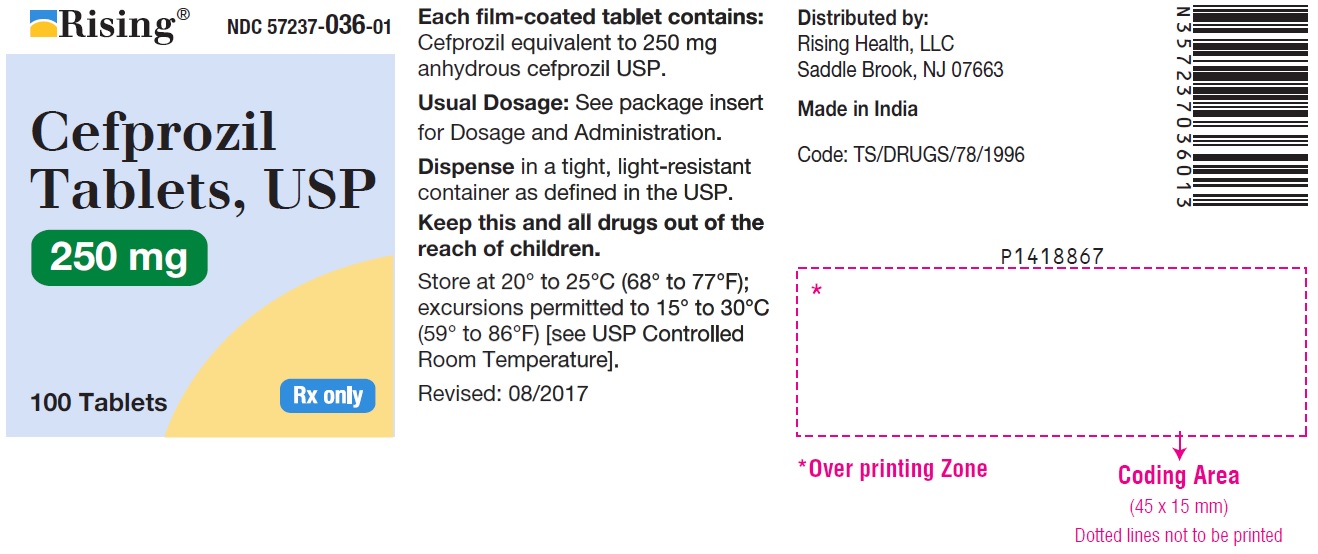
Revised: 11/2018 - PACKAGE LABEL-PRINCIPAL DISPLAY PANEL - 250 mg (100 Tablets Bottle)
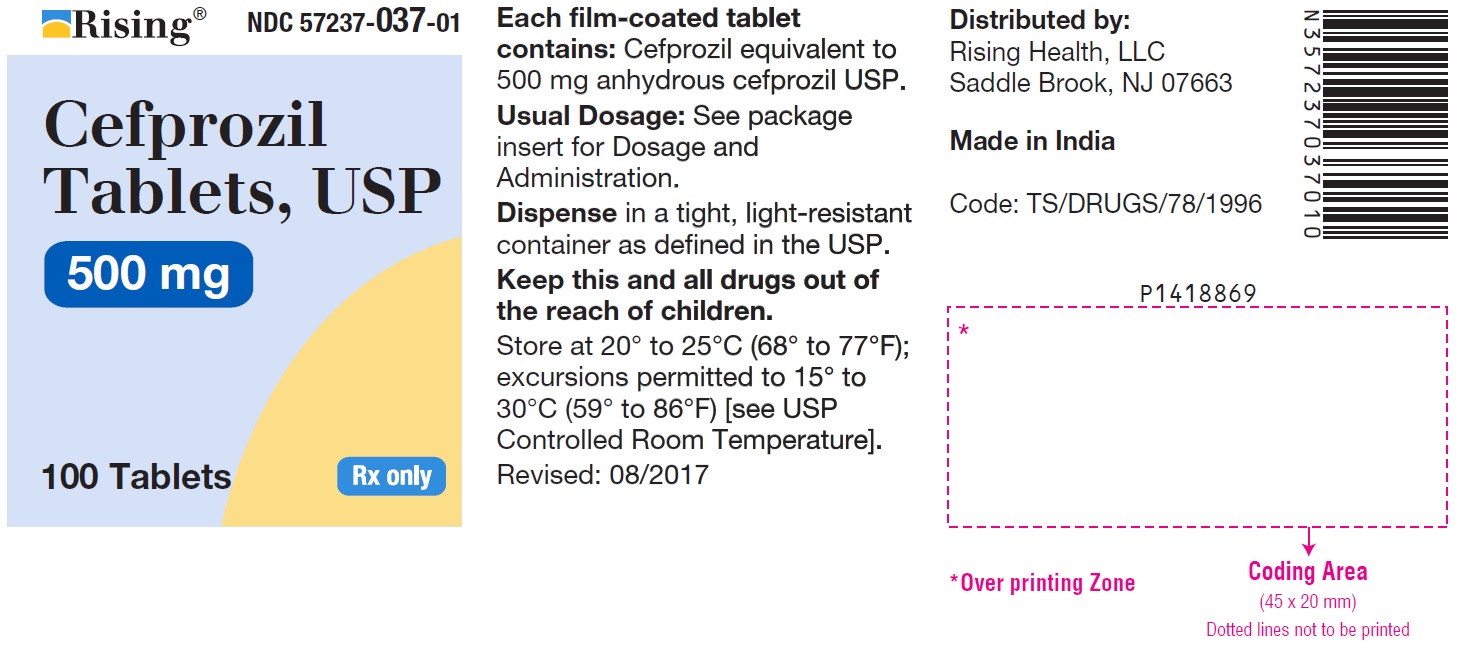
- PACKAGE LABEL-PRINCIPAL DISPLAY PANEL - 500 mg (100 Tablets Bottle)
-
INGREDIENTS AND APPEARANCE
CEFPROZIL
cefprozil tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 57237-036 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CEFPROZIL (UNII: 4W0459ZA4V) (CEFPROZIL ANHYDROUS - UNII:1M698F4H4E) CEFPROZIL ANHYDROUS 250 mg Inactive Ingredients Ingredient Name Strength MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) SODIUM STARCH GLYCOLATE TYPE A POTATO (UNII: 5856J3G2A2) MAGNESIUM STEARATE (UNII: 70097M6I30) HYPROMELLOSE 2910 (3 MPA.S) (UNII: 0VUT3PMY82) HYPROMELLOSE 2910 (6 MPA.S) (UNII: 0WZ8WG20P6) POLYETHYLENE GLYCOL 400 (UNII: B697894SGQ) POLYSORBATE 80 (UNII: 6OZP39ZG8H) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) FD&C YELLOW NO. 6 (UNII: H77VEI93A8) SHELLAC (UNII: 46N107B71O) FERROSOFERRIC OXIDE (UNII: XM0M87F357) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) AMMONIA (UNII: 5138Q19F1X) Product Characteristics Color ORANGE Score no score Shape CAPSULE (Biconvex) Size 14mm Flavor Imprint Code C16 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 57237-036-01 100 in 1 BOTTLE; Type 0: Not a Combination Product 05/24/2007 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA065340 05/24/2007 CEFPROZIL
cefprozil tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 57237-037 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CEFPROZIL (UNII: 4W0459ZA4V) (CEFPROZIL ANHYDROUS - UNII:1M698F4H4E) CEFPROZIL ANHYDROUS 500 mg Inactive Ingredients Ingredient Name Strength MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) SODIUM STARCH GLYCOLATE TYPE A POTATO (UNII: 5856J3G2A2) MAGNESIUM STEARATE (UNII: 70097M6I30) HYPROMELLOSE 2910 (5 MPA.S) (UNII: R75537T0T4) POLYETHYLENE GLYCOL 400 (UNII: B697894SGQ) POLYSORBATE 80 (UNII: 6OZP39ZG8H) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) SHELLAC (UNII: 46N107B71O) FERROSOFERRIC OXIDE (UNII: XM0M87F357) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) AMMONIA (UNII: 5138Q19F1X) Product Characteristics Color WHITE Score no score Shape CAPSULE (Biconvex) Size 18mm Flavor Imprint Code C17 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 57237-037-50 50 in 1 BOTTLE; Type 0: Not a Combination Product 05/24/2007 2 NDC: 57237-037-01 100 in 1 BOTTLE; Type 0: Not a Combination Product 05/24/2007 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA065340 05/24/2007 Labeler - Rising Health, LLC (080500961) Registrant - Aurobindo Pharma Limited (650082092) Establishment Name Address ID/FEI Business Operations Aurobindo Pharma Limited 918917639 ANALYSIS(57237-036, 57237-037) , MANUFACTURE(57237-036, 57237-037)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.