KABIVEN- dextrose, soybean oil, electrolytes, lysine, phenylalanine, leucine, valine, threonine, methionine, isoleucine, tryptophan, alanine, arginine, glycine, proline, histidine, glutamic acid, serine, aspartic acid and tyrosine injection, emulsion
Kabiven by
Drug Labeling and Warnings
Kabiven by is a Prescription medication manufactured, distributed, or labeled by Fresenius Kabi USA, LLC, Fresenius Kabi AB. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use KABIVEN® safely and effectively. See full prescribing information for KABIVEN®.
KABIVEN® (amino acids, electrolytes, dextrose and lipid injectable emulsion), for intravenous use
Initial U.S. Approval: 2014
WARNING: DEATH IN PRETERM INFANTS
See full prescribing information for complete boxed warning
- Deaths in preterm infants have been reported in literature. ( 5.1, 8.4)
- Autopsy findings included intravascular fat accumulation in the lungs. ( 5.1, 8.4)
- Preterm and low birth weight infants have poor clearance of intravenous lipid emulsion and increased free fatty acid plasma levels following lipid emulsion infusion. ( 5.1, 8.4)
INDICATIONS AND USAGE
KABIVEN ® is indicated as a source of calories, protein, electrolytes and essential fatty acids for adult patients requiring parenteral nutrition when oral or enteral nutrition is not possible, insufficient, or contraindicated. KABIVEN ® may be used to prevent essential fatty acid deficiency or treat negative nitrogen balance in adult patients. ( 1)
Limitations of Use:Not recommended for use in pediatric patients < 2 years including preterm infants because the fixed content of the formulation does not meet nutritional requirements in this age group. ( 1, 5.1, 8.4)
DOSAGE AND ADMINISTRATION
- For intravenous infusion only into a central vein. ( 2.1, 5.8)
- Recommended dosage depends on clinical status, body weight and nutritional requirements. ( 2.4)
- Adult dosage: 19 to 38 mL/kg/day (0.63 to 1.26 g/kg/day of protein, 1.85 to 3.71 g/kg/day of dextrose, 0.74 to 1.48 g/kg/day of lipid) ( 2.4)
- The maximum infusion rate is 2.6 mL/kg/hour (corresponding to 0.09 g/kg/hour of amino acids, 0.25 g/kg/hour of dextrose, the limiting factor, and 0.1 g/kg/hour of lipid). The recommended infusion period is 12 to 24 hours. ( 2.4)
DOSAGE FORMS AND STRENGTHS
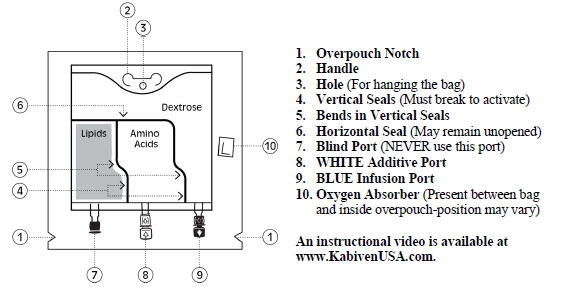
- KABIVEN ® is a sterile, hypertonic emulsion in a three chamber container. The individual chambers contain one of the following: amino acids and electrolytes, dextrose, or lipid injectable emulsion, respectively. ( 3)
- KABIVEN ® is available in four sizes 2,566 mL, 2,053 mL, 1,540 mL and 1,026 mL. ( 3)
CONTRAINDICATIONS
- Known hypersensitivity to egg, soybean proteins, peanut proteins, corn or corn products, or to any of the active substances or excipients. ( 4)
- Severe hyperlipidemia or severe disorders of lipid metabolism with serum triglycerides >1,000 mg/dL. ( 4, 5.12)
- Inborn errors of amino acid metabolism. ( 4)
- Cardiopulmonary instability. ( 4)
- Hemophagocytic syndrome. ( 4)
WARNINGS AND PRECAUTIONS
ADVERSE REACTIONS
The most common adverse reactions (≥3%) are nausea, pyrexia, hypertension, vomiting, decreased hemoglobin, decreased total protein, hypokalemia, decreased potassium, and increased gamma glutamyltransferase. ( 6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Fresenius Kabi USA, LLC at 1-800-551-7176 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
Coumarin and coumarin derivatives, including warfarin: Anticoagulant activity may be counteracted; monitor laboratory parameters. ( 7.1)
USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 10/2016
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: DEATH IN PRETERM INFANTS
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Administration
2.2 Important Preparation Instructions
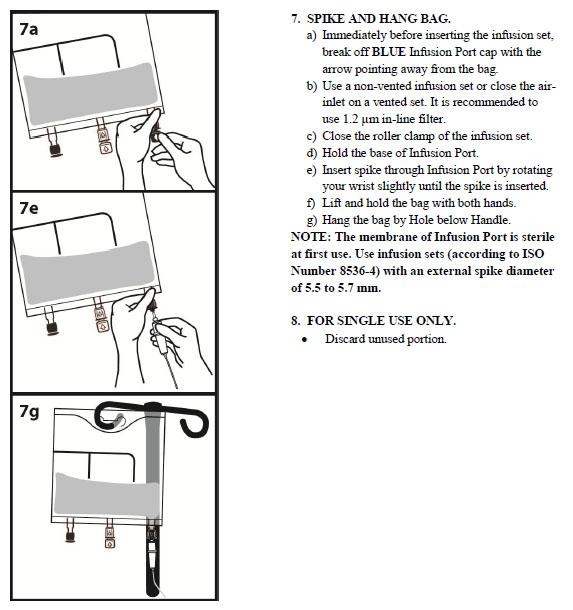
2.3 Instructions for Use
2.4 Dosing Considerations
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Death in Preterm Infants
5.2 Hypersensitivity Reactions
5.3 Infections
5.4 Fat Overload Syndrome
5.5 Refeeding Syndrome
5.6 Diabetes/Hyperglycemia
5.7 Monitoring/Laboratory Tests
5.8 Vein Damage and Thrombosis
5.9 Precipitation with Ceftriaxone
5.10 Hepatobiliary Disorders
5.11 Electrolyte Imbalance and Fluid Overload in Renal Impairment
5.12 Hypertriglyceridemia
5.13 Aluminum Toxicity
5.14 Interference with Laboratory Tests
5.15 Risk of Parenteral Nutrition Associated Liver Disease
6 ADVERSE REACTIONS
6.1 Clinical Trial Experience
6.2 Post-Marketing Experience
7 DRUG INTERACTIONS
7.1 Coumarin and Coumarin Derivatives
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Hepatic Impairment
8.7 Renal Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
15 REFERENCES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: DEATH IN PRETERM INFANTS
- Deaths in preterm infants after infusion of intravenous lipid emulsions have been reported in the medical literature.
- Autopsy findings included intravascular fat accumulation in the lungs.
- Preterm infants and low birth weight infants have poor clearance of intravenous lipid emulsion and increased free fatty acid plasma levels following lipid emulsion infusion.
[See Warnings and Precautions (5.1) and Use in Specific Populations (8.4)]
-
1 INDICATIONS AND USAGE
KABIVEN ® is indicated as a source of calories, protein, electrolytes and essential fatty acids for adult patients requiring parenteral nutrition when oral or enteral nutrition is not possible, insufficient, or contraindicated. KABIVEN ® may be used to prevent essential fatty acid deficiency or treat negative nitrogen balance in adult patients.
Limitations of Use:
KABIVEN ® is not recommended for use in pediatric patients under the age of 2 years, including preterm infants because the fixed content of the formulation does not meet the nutritional requirements of this age group [see Warnings and Precautions (5.1) and Use in Specific Populations (8.4)].
-
2 DOSAGE AND ADMINISTRATION
2.1 Administration
- KABIVEN ® is for intravenous infusion only into a central vein [see Warnings and Precautions (5.8)].
- Use a 1.2 micron in-line filter.
- Use of a vented intravenous administration set with the vent in the open position could result in air embolism.
- Use a dedicated line without any connections. Multiple connections could result in air embolism due to residual air being drawn from the primary container before administration of the fluid from the secondary container is completed.
- Ceftriaxone must not be administered simultaneously with calcium-containing intravenous solutions such as KABIVEN ® via a Y-site due to precipitation. However, ceftriaxone and KABIVEN ® may be administered sequentially if the infusion lines are thoroughly flushed between infusions with a compatible fluid [see Warnings and Precautions (5.9)] .
- Do not use administration sets and lines that contain di-2-ethylhexyl phthalate (DEHP). Administration sets that contain polyvinyl chloride (PVC) components have DEHP as a plasticizer.
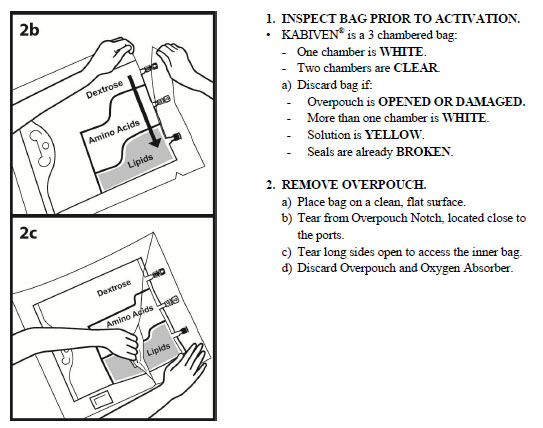
2.2 Important Preparation Instructions
- Inspect the bag prior to activation. Discard the bag in the following situations:
- Evidence of damage to the bag
- More than one chamber is white
- Solution is yellow
- Any seal is already broken
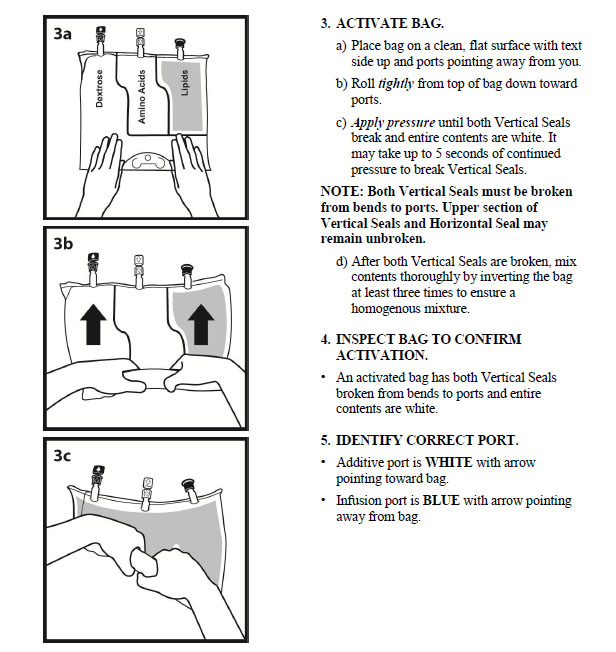
- Activate the bag [see Dosage and Administration (2.3)] .
- Once the bag is activated, ensure the vertical seals between chambers are broken at least from the bend in the seals and down to the ports. The upper sections of the vertical seals above the bend and the horizontal seal may remain closed.
- It is recommended to mix the contents thoroughly by inverting the bag upside down to ensure a homogenous admixture.
- Ensure the vertical seals between chambers are broken and the contents of all three chambers are mixed together prior to infusion [see Dosage and Administration (2.3)] .
- Use KABIVEN ® immediately after the introduction of additives. If not used immediately, the storage time and conditions prior to use should not be longer than 24 hours at 2° to 8°C (36° to 46°F). After removal from storage at 2° to 8°C (36° to 46°F), the admixture should be infused within 24 hours. Any mixture remaining must be discarded.
- In the absence of additives, once activated, KABIVEN ® remains stable for 48 hours at 25°C (77°F). If not used immediately, the activated bag can be stored for up to 7 days under refrigeration [2° to 8°C (36º to 46°F)]. After removal from refrigeration, the activated bag should be used within 48 hours.
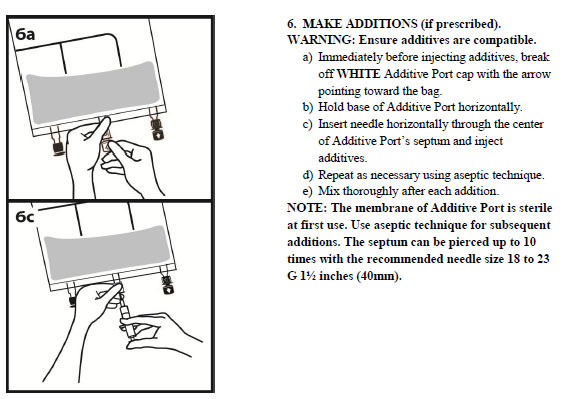
- For total parenteral nutrition add multivitamins and trace elements via the additive port. Any other additions to the bag should be evaluated by a pharmacist for compatibility. Questions about compatibility may be directed to Fresenius Kabi USA, LLC.
- When introducing additives, it is recommended to use 18 to 23 gauge needles with a maximum length of 1.5 inches (40 mm) and to mix thoroughly after each addition, use aseptic technique and add after the vertical seals have been broken (i.e. bag has been activated) and the three components are mixed [see Dosage and Administration (2.3)].
- Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. Inspect KABIVEN
® to ensure:
- Precipitates have not formed during the mixing or addition of additives.
- The emulsion has not separated. Separation of the emulsion can be visibly identified by a yellowish streaking or the accumulation of yellowish droplets in the mixed emulsion.
Discard the admixture if any of the above are observed.
2.4 Dosing Considerations
The dosage of KABIVEN ® should be individualized based on the patient’s clinical condition (ability to adequately metabolize amino acids, dextrose and lipids), body weight and nutritional/fluid requirements, as well as additional energy given orally/enterally to the patient.
KABIVEN ® is a combination of amino acids, electrolytes, dextrose, and lipids in a fixed volume and concentration. The dosage selection is based upon fluid requirements which can be used in conjunction with the nutritional requirements to determine final dosage [see Table 1]. KABIVEN ® meets the total nutritional requirements for protein, dextrose and lipids in stable patients, and can be individualized to meet specific needs with the addition of nutrients. The maximum infusion rate is based upon the dextrose component.
Prior to administration of KABIVEN ®, correct severe fluid, electrolyte and acid-base disorders. Before starting the infusion, obtain serum triglyceride levels to establish the baseline value.
Recommended Adult Dosage
The recommended dosage of KABIVEN ® in adults is 19 to 38 mL/kg/day. The recommended daily nutritional requirements for protein, dextrose and lipids compared to the amount of nutrition provided by KABIVEN ® are shown in Table 1.
The maximum daily dosage of KABIVEN ® in adults should not exceed 40 mL/kg/day.
In patients with serum triglyceride concentrations above 400 mg/dL, stop the KABIVEN ® infusion and monitor serum triglyceride levels. Once the triglycerides are <400 mg/dL, restart KABIVEN ® at a lower infusion rate and advance rate in smaller increments towards target dosage, checking the triglyceride levels prior to each adjustment [see Contraindications (4) and Warnings and Precautions (5.12)].
Table 1: Nutritional Comparison
Nutrition Provided
by KABIVEN ®
recommended dosage
Recommended Nutritional Requirements 1
Stable Patients
Critically Ill Patients*
Fluid mL/kg/day
19 to 38
30 to 40
Minimum needed to deliver adequate macronutrients
Protein** g/kg/day
Nitrogen g/kg/day
0.6 to 1.3
0.1 to 0.2
0.8 to 1.0
0.13 to 0.16
1.5 to 2
0.24 to 0.3
Dextrose g/kg/day
1.9 to 3.7
≤10
≤5.8
Lipids g/kg/day
0.7 to 1.5
1
≤1
Total Energy Requirement kcal/kg/day
16 to 32
20 to 30
25 to 30
* Do not use in patients with conditions that are contraindicated [see Contraindications (4)].
** Protein is provided as amino acids. When infused intravenously amino acids are metabolized and utilized as the building blocks of protein.
Treatment with KABIVEN ® may be continued for as long as is required by the patient’s condition.
Dosing in Renal Impairment
In patients with renal impairment, the dosage of KABIVEN ® should be the recommended adult dosage (see above). Prior to administration, correct severe fluid or electrolyte imbalances. Closely monitor serum electrolyte levels and adjust the volume of KABIVEN ® administered as required [see Warnings and Precautions (5.11)] .
Renal patients not needing dialysis require 0.6 to 0.8 g of protein/kg/day. Patients on dialysis or continuous renal replacement therapy should receive 1.2 to 1.8 g of protein/kg/day up to a maximum of 2.5 g of protein/kg/day based on nutritional status and estimated protein losses 2. The KABIVEN ® dosage can be adjusted based on the treatment for the renal impairment, supplementing protein as indicated. If required, additional amino acids may be added to the KABIVEN ® bag or infused separately. Compatibility of additions should be evaluated by a pharmacist and questions may be directed to Fresenius Kabi USA, LLC.
Infusion Duration and Rate
The recommended duration of infusion for KABIVEN ® is between 12 and 24 hours, depending on the clinical situation.
The maximum infusion rate of KABIVEN ® is 2.6 mL/kg/hour. This corresponds to 0.09 g/kg/hour of amino acids, 0.25 g/kg/hour of dextrose (the rate limiting factor) and 0.1 g/kg/hour of lipids.
Dosing Instructions
- Determine the fluid requirements (19 to 38 mL/kg/day) and the patient’s nutritional requirements (see Table 1) to be delivered, and then select the corresponding KABIVEN ® bag.
- Determine the preferred duration of infusion (12 to 24 hours).
- Ensure that the rate of infusion (KABIVEN ® dosage in mL/kg/day divided by the preferred duration of infusion (hours)) does not exceed the maximum infusion rate for the patient (i.e., 2.6 mL/kg/hour). The infusion rate may need to be reduced and duration of infusion increased in order not to exceed the maximum infusion rate.
- Once the infusion rate in mL/kg/hour has been selected, calculate the infusion rate (mL/hour) using the patient’s weight.
- Compare the patient’s nutrient requirements with the amount supplied by KABIVEN ®. Discuss with a pharmacist any additions that may be required.
-
3 DOSAGE FORMS AND STRENGTHS
KABIVEN ® is a sterile, hypertonic emulsion in a three chamber container. The individual chambers contain one of the following respectively: amino acids and electrolytes, dextrose, or lipid injectable emulsion. Table 2 describes the individual components of KABIVEN ®.
Table 2: Contents of KABIVEN ® when mixed
How Supplied
2,566
mL
2,053
mL
1,540 mL
1,026 mL
Composition of KABIVEN ®
Soybean Oil, USP (g/100 mL)
3.9
Dextrose Anhydrous, USP (g/100 mL)
9.8
Amino Acids, USP (g/100 mL)
3.31
Total Nitrogen (mg/100 mL)
526
Essential amino acids
(mg/100 mL)
Lysine, USP (added as the hydrochloride salt)
263
Phenylalanine, USP
231
Leucine, USP
231
Valine, USP
213
Threonine, USP
164
Methionine, USP
164
Isoleucine, USP
164
Tryptophan, USP
55
Nonessential amino acids
(mg/100 mL)
Alanine, USP
467
Arginine, USP
330
Glycine, USP
231
Proline, USP
199
Histidine, USP
199
Glutamic Acid
164
Serine, USP
131
Aspartic Acid, USP
99
Tyrosine, USP
6.7
Electrolytes
(mg/100 mL)
Sodium Acetate Trihydrate, USP
239
Potassium Chloride, USP
174
Sodium Glycerophosphate Anhydrous
147
Magnesium Sulfate Heptahydrate, USP
96
Calcium Chloride Dihydrate, USP
29
Electrolyte Profile 1
(mEq/L)
Sodium 2
31 (31 mmol/L)
Potassium
23 (23 mmol/L)
Magnesium
7.8 (3.9 mmol/L)
Calcium
3.8 (1.9 mmol/L)
Phosphorous 3
N.A. (9.7 mmol/L)
Acetate 4
38 (38 mmol/L)
Chloride 5
45 (45 mmol/L)
Sulfate 6
7.8 (3.9 mmol/L)
Calorie Content (kcal/L)
From Dextrose
330
From Lipid
390 7
From Amino Acids
130
Total
850
pH 8
5.6
Osmolarity (mOsm/L)
1060
- Balanced by ions from amino acids
- Contributed by sodium glycerophosphate and sodium acetate
- Contributed by sodium glycerophosphate and phospholipids
- Derived from sodium acetate and glacial acetic acid (for pH adjustment)
- Contributed by calcium chloride, lysine hydrochloride, and potassium chloride
- Derived from magnesium sulfate
- Total caloric value including lipid, phospholipid and glycerin
- pH of amino acid with electrolyte solution was adjusted with glacial acetic acid, USP and pH of lipid emulsion was adjusted with sodium hydroxide, USP
-
4 CONTRAINDICATIONS
The use of KABIVEN ® is contraindicated in patients with the following:
- Known hypersensitivity to egg, soybean proteins, peanut proteins, corn or corn products or to any of the active substances or excipients:
- Severe hyperlipidemia or severe disorders of lipid metabolism characterized by hypertriglyceridemia (serum triglyceride concentration >1,000 g/dL) [see Warnings and Precautions (5.12)] .
- Inborn error of amino acid metabolism
- Cardiopulmonary instability (including pulmonary edema, cardiac insufficiency, myocardial infarction, acidosis and hemodynamic instability requiring significant vasopressor support)
- Hemophagocytic syndrome
-
5 WARNINGS AND PRECAUTIONS
5.1 Death in Preterm Infants
Deaths in preterm infants after infusion of intravenous lipid emulsions have been reported. Autopsy findings included intravascular lipid accumulation in the lungs.
Preterm and small for gestational age infants have poor clearance of intravenous lipid emulsion and increased free fatty acid plasma levels following lipid emulsion infusion.
The safe and effective use of KABIVEN ® injection in pediatric patients, including preterm infants, has not been established. KABIVEN ® is not recommended for use in pediatric patients under the age of 2 years including preterm infants.
5.2 Hypersensitivity Reactions
Stop infusion immediately and treat patient accordingly if signs or symptoms of a hypersensitivity or allergic reaction develop. Signs or symptoms may include: tachypnea, dyspnea, hypoxia, bronchospasm, tachycardia, hypotension, cyanosis, vomiting, nausea, headache, sweating, dizziness, altered mentation, flushing, rash, urticaria, erythema, pyrexia and chills.
5.3 Infections
Patients who require parenteral nutrition are at high risk of infections due to malnutrition and their underlying disease state. Infection and sepsis may occur as a result of the use of intravenous catheters to administer parenteral nutrition, poor maintenance of catheters, or immunosuppressive effects of illness, drugs, and parenteral formulations.
Decrease the risk of septic complications with heightened emphasis on aseptic technique in catheter placement and maintenance, as well as aseptic technique in the preparation of the nutritional formula.
Monitor for signs and symptoms (including fever and chills) of early infections, including laboratory test results (including leukocytosis and hyperglycemia) and frequent checks of the parenteral access device.
5.4 Fat Overload Syndrome
Fat overload syndrome is a rare condition that has been reported with intravenous lipid formulations. A reduced or limited ability to metabolize the lipid contained in KABIVEN ® accompanied by prolonged plasma clearance may result in a syndrome characterized by a sudden deterioration in the patient's condition accompanied by fever, anemia, leukopenia, thrombocytopenia, coagulation disorders, hyperlipidemia, liver fatty infiltration (hepatomegaly), deteriorating liver function, and central nervous system manifestations (e.g., coma). The cause of the fat overload syndrome is unclear. The syndrome is usually reversible when the infusion of the lipid emulsion is stopped. Although it has been most frequently observed when the recommended lipid dosage was exceeded, cases have also been described where the lipid formulation was administered according to instructions.
5.5 Refeeding Syndrome
Refeeding severely undernourished patients with parenteral nutrition may result in the refeeding syndrome, characterized by the intracellular shift of potassium, phosphorus, and magnesium as the patient becomes anabolic. Thiamine deficiency and fluid retention may also develop. Carefully monitor severely undernourished patients and slowly increase their nutrient intakes, while avoiding overfeeding, to prevent these complications.
5.6 Diabetes/Hyperglycemia
KABIVEN ® should be used with caution in patients with diabetes mellitus or hyperglycemia. With the administration of KABIVEN ®, hyperglycemia and hyperosmolar syndrome may result. Administration of dextrose at a rate exceeding the patient's utilization rate may lead to hyperglycemia, coma and death. Monitor blood glucose levels and treat hyperglycemia to maintain optimum levels while infusing KABIVEN ®. Insulin may be administered or adjusted to maintain optimal blood glucose levels during KABIVEN ® administration.
5.7 Monitoring/Laboratory Tests
Routine Monitoring
- Frequent clinical evaluation and laboratory determinations are necessary for proper monitoring during administration.
- Monitor fluid status closely in patients with heart failure or pulmonary edema.
- Monitor serum triglycerides, fluid and electrolyte status, serum osmolarity, blood glucose, liver and kidney function, and blood count, including platelet and coagulation parameters, throughout treatment. In situations of severely elevated electrolyte levels stop KABIVEN ® until levels have been corrected.
Essential Fatty Acids
Monitoring patients for signs and symptoms of essential fatty acid deficiency (EFAD) is recommended. Laboratory tests are available to determine serum fatty acids levels. Reference values should be consulted to help determine adequacy of essential fatty acid status. Increasing essential fatty acid intake (enterally or parenterally) is effective in treating and preventing EFAD.
In KABIVEN ®, the mean composition of linoleic acid (an omega-6 essential fatty acid) is 21 mg/mL (range 19 to 23 mg/mL) and alpha-linolenic acid (an omega-3 essential fatty acid) is 2.6 mg/mL (range 2.0 to 4.3 mg/mL). There are insufficient long-term data to determine whether KABIVEN ® can supply essential fatty acids in adequate amounts in patients who may have increased requirements.
5.8 Vein Damage and Thrombosis
KABIVEN ® is indicated for administration into a central vein only, such as the superior vena cava. The infusion of hypertonic nutrient injections into a peripheral vein may result in vein irritation, vein damage, and/or thrombosis.
5.9 Precipitation with Ceftriaxone
Precipitation of ceftriaxone-calcium can occur when ceftriaxone is mixed with calcium-containing parenteral nutrition solutions, such as KABIVEN ® in the same intravenous administration line. Ceftriaxone must not be administered simultaneously with KABIVEN ® via a Y-site. However, ceftriaxone and KABIVEN ® may be administered sequentially if the infusion lines are thoroughly flushed between infusions with a compatible fluid [s ee Dosage and Administration (2.1)] .
5.10 Hepatobiliary Disorders
Hepatobiliary disorders are known to develop in some patients without preexisting liver disease who receive parenteral nutrition, including cholecystitis, cholelithiasis, cholestasis, hepatic steatosis, fibrosis and cirrhosis, possibly leading to hepatic failure. The etiology of these disorders is thought to be multifactorial and may differ between patients.
Increase of blood ammonia levels and hyperammonemia may occur in patients receiving amino acid solutions. In some patients this may indicate hepatic insufficiency or the presence of an inborn error of amino acid metabolism [see Contraindications (4)] or hepatic insufficiency.
Monitor liver function parameters and ammonia. Patients developing signs of hepatobiliary disorders should be assessed early by a clinician knowledgeable in liver diseases in order to identify causative and contributory factors, and possible therapeutic and prophylactic interventions.
5.11 Electrolyte Imbalance and Fluid Overload in Renal Impairment
Patients with renal impairment, such as pre-renal azotemia, renal obstruction and protein-losing nephropathy may be at increased risk of electrolyte and fluid volume imbalance. KABIVEN ® should be used with caution in patients with renal impairment. KABIVEN ® dosage may require adjustment with specific attention to fluid, protein and electrolyte content in these patients.
Monitor renal function parameters. Patients developing signs of renal impairment should be assessed early by a clinician knowledgeable in renal disease in order to determine the appropriate KABIVEN ® dosage and other treatment options.
5.12 Hypertriglyceridemia
To evaluate the patient’s capacity to eliminate and metabolize the infused lipid emulsion, measure serum triglycerides before the start of infusion (baseline value), with each increase in dosage, and regularly throughout treatment.
Reduce dose of KABIVEN ® and monitor serum triglyceride levels in patients with serum triglyceride concentrations above 400 mg/dL to avoid the clinical consequences associated with hypertriglyceridemia. Serum triglyceride levels above 1,000 mg/dL have been associated with an increased risk of pancreatitis.
Impaired lipid metabolism with hypertriglyceridemia may occur in conditions such as inherited lipid disorders, obesity, diabetes mellitus, and metabolic syndrome. In these cases, increased triglycerides can also be increased by dextrose and/or overfeeding. Monitor overall energy intake and other sources of lipid and dextrose, as well as drugs that may interfere with lipid and dextrose metabolism.
5.13 Aluminum Toxicity
KABIVEN ® contains no more than 25 mcg/L of aluminum.
The aluminum contained in KABIVEN ® may reach toxic levels with prolonged parenteral administration in patients with impaired kidney function. Preterm infants are at greater risk because their kidneys are immature, and they require large amounts of calcium and phosphate solutions that contain aluminum. Patients with impaired kidney function, including preterm infants, who receive parenteral levels of aluminum at greater than 4 to 5 mcg/kg/day, accumulate aluminum at levels associated with central nervous system and bone toxicity. Tissue loading may occur at even lower rates of administration of total parenteral nutrition products.
5.14 Interference with Laboratory Tests
High levels of lipids in plasma may interfere with some laboratory blood tests such as hemoglobin, triglycerides, bilirubin, LDH, and oxygen saturation, if blood is sampled before lipid has been cleared from the bloodstream. Lipids are normally cleared after a lipid-free interval of 5 to 6 hours in most patients.
KABIVEN ® contains Vitamin K 1 which may interfere with anticoagulant activity [see Drug Interactions (7.1)] .
5.15 Risk of Parenteral Nutrition Associated Liver Disease
Parenteral Nutrition Associated Liver Disease (PNALD) has been reported in patients who receive parenteral nutrition for extended periods of time, especially preterm infants, and can present as cholestasis or steatohepatitis. The exact etiology is unknown and is likely multifactorial. Intravenously administered phytosterols (plant sterols) contained in plant-derived lipid formulations have been associated with development of PNALD although a causal relationship has not been established. If KABIVEN ® treated patients develop liver test abnormalities consider discontinuation or dosage reduction.
-
6 ADVERSE REACTIONS
The following serious adverse reactions are discussed in greater detail in other sections of the prescribing information.
- Hypersensitivity Reactions [see Warnings and Precautions (5.2)]
- Infections [see Warnings and Precautions (5.3)]
- Fat Overload Syndrome [see Warnings and Precautions (5.4)]
- Refeeding Syndrome [see Warnings and Precautions (5.5)]
- Diabetes/Hyperglycemia [see Warnings and Precautions (5.6)]
- Vein Damage and Thrombosis [see Warnings and Precautions (5.8)]
- Hepatobiliary Disorders [see Warnings and Precautions (5.10, 5.15)]
- Electrolyte Imbalance and Fluid Overload in Renal Impairment [see Warnings and Precautions (5.11)]
- Hypertriglyceridemia [see Warnings and Precautions (5.12)]
- Aluminum Toxicity [see Warnings and Precautions (5.13)]
6.1 Clinical Trial Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The clinical data described for KABIVEN ® reflects exposure in 145 patients exposed for 7 days to 4 weeks in 7 active-controlled trials. The pooled population exposed to KABIVEN ® was 25 to 87 years old, 35% female, 99% Caucasian. The enrolled patients had varied underlying conditions such as gastrointestinal disorders (41%) neoplasms (48%), vascular disorders (35%) and other surgical procedures (21%). Most patients received central intravenous infusion doses of ≥80% of their target mean daily exposure.
Adverse reactions occurring in at least 1% of patients who received KABIVEN ® are shown in Table 3.
Table 3: Adverse Reactions in >1% of Patients Treated with KABIVEN ®
Adverse reaction
KABIVEN ®
N=145 (%)
Nausea
22 (15)
Pyrexia
13 (9)
Hypertension
12 (8)
Vomiting
8 (6)
Hemoglobin decreased
8 (6)
Protein total decreased
6 (4)
Hypokalemia
6 (4)
Blood potassium decreased
6 (4)
Gamma-glutamyltransferase increased
6 (4)
Hyperglycemia
3 (2)
Blood alkaline phosphatase increased
2 (1)
Blood calcium decreased
2 (1)
Prothrombin time prolonged
2 (1)
Pruritus
2 (1)
Tachycardia
2 (1)
* Terms as reported in clinical studies
Less common adverse reactions in ≤1% of patients who received KABIVEN ® were hyperkalemia, hypertriglyceridemia, headache, dizziness, dysgeusia, rash, eczema, blood glucose increased, and increase in blood triglycerides.
6.2 Post-Marketing Experience
The following additional adverse reactions have been identified during post-approval use of KABIVEN ® in countries where it is registered. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to product exposure.
- Hepatobiliary disorders: cholestasis
- Infections and infestations: infection
- Nervous system disorders: subependymal hemorrhage
-
7 DRUG INTERACTIONS
7.1 Coumarin and Coumarin Derivatives
The soybean oil present in KABIVEN ® has vitamin K 1. Vitamin K 1 can reverse the anticoagulant activity of coumarin and coumarin derivatives, including warfarin, which work by blocking recycling of vitamin K 1. Monitor laboratory parameters for anticoagulant activity in patients who are on both KABIVEN ® and coumarin or coumarin derivatives.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
The limited available data on the use of KABIVEN ® in pregnant women are not sufficient to inform a drug-associated risk. However, there are clinical considerations if KABIVEN ® is used in pregnant women [see Clinical Considerations]. Animal reproduction studies have not been conducted with KABIVEN ®.
The estimated background risk of major birth defects and miscarriage for the indicated population are unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Clinical Considerations
Disease-Associated Maternal and/or Embryofetal Risk
Severe malnutrition in a pregnant woman is associated with preterm delivery, low birth weight, intrauterine growth restriction, congenital malformations and perinatal mortality. Parenteral nutrition should be considered if a pregnant woman’s nutritional requirements cannot be fulfilled by oral or enteral intake.
8.2 Lactation
Risk Summary
There are no data available to assess the presence of KABIVEN ® and/or its active metabolite(s) in human milk, the effects on the breastfed child or the effects on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for KABIVEN ®, and any potential adverse effects of KABIVEN ® on the breastfed child or from the underlying maternal condition.8.4 Pediatric Use
The safety and effectiveness of KABIVEN ® in pediatric patients has not been established.
Deaths in preterm infants after infusion of intravenous lipid emulsion have been reported [see Warnings and Precautions (5.1)]. Patients, particularly preterm infants, are at risk for aluminum toxicity [see Warnings and Precautions (5.13)] .
KABIVEN ® is not recommended for use in pediatric patients under the age of two years, including preterm infants, as the fixed content of the formulation does not meet the nutritional requirements of this age group due to the following reasons:
- Calcium and dextrose needs are not met and lipids, protein and magnesium exceed requirements.
- The product does not contain the amino acids cysteine and taurine, considered conditionally essential for neonates and infants.
Patients, including pediatric patients, may be at risk for PNALD [see Warnings and Precautions (5.15)] .
Newborns – especially those born premature and with low birth weight – are at increased risk of developing hypo – or hyperglycemia and therefore need close monitoring during treatment with intravenous dextrose solutions to ensure adequate glycemic control in order to avoid potential long term adverse effects. Hypoglycemia in the newborn can cause prolonged seizures, coma and brain damage. Hyperglycemia has been associated with intraventricular hemorrhage, late onset bacterial and fungal infection, retinopathy of prematurity, necrotizing enterocolitis, bronchopulmonary dysplasia, prolonged length of hospital stay, and death.
8.5 Geriatric Use
Clinical studies of KABIVEN ® did not include sufficient numbers of patients aged 65 and over to determine whether they respond differently from other younger patients. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or drug therapy.
8.6 Hepatic Impairment
In patients with impaired liver function KABIVEN ® should be administered with caution. Frequent clinical evaluation and laboratory tests to monitor liver function such as bilirubin and liver function parameters should be conducted [s ee Warnings and Precautions (5.10)] .
8.7 Renal Impairment
In patients with impaired renal function, KABIVEN ® should be administered with caution. Frequent clinical evaluation and laboratory tests to monitor renal function such as serum electrolytes (especially phosphate and potassium) and fluid balance should be conducted [see Dosage and Administration (2.4) and Warnings and Precautions (5.11)] .
-
10 OVERDOSAGE
In the event of overdose, fat overload syndrome may result [see Warnings and Precautions (5.4)] . Stop the infusion of KABIVEN ® to allow lipids to clear from serum. The effects are usually reversible after the lipid infusion is stopped. If medically appropriate, further intervention may be indicated. The lipid administered and fatty acids produced are not dialyzable.
-
11 DESCRIPTION
KABIVEN ® is a sterile, hypertonic emulsion, for central venous administration, in a Three Chamber Bag. The product contains no added sulfites.
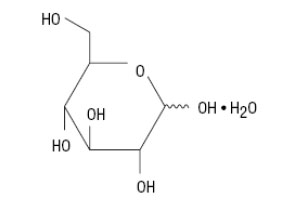
Chamber 1 contains Dextrose solution for fluid replenishment and caloric supply.
Chamber 2 contains the Amino Acid solution with Electrolytes, which comprises essential and nonessential amino acids provided with electrolytes.
Chamber 3 contains Intralipid ® 20% (a 20% Lipid Injectable Emulsion), prepared for intravenous administration as a source of calories and essential fatty acids.
See below for formulations of each chamber and Table 2 for strength, pH, osmolarity, ionic concentration and caloric content of KABIVEN ® when all the chambers are mixed together.
Chamber 1: Contains sterile, hypertonic solution of Dextrose, USP in water for injection with a pH range of 3.5 to 5.5. Dextrose, USP is chemically designated D-glucose, monohydrate (C 6H 12O 6 H 2O) and has the following structure:
Chamber 2: Contains a sterile solution of amino acids and electrolytes in water for injection. In addition, glacial acetic acid has been added to adjust the pH so that the final solution pH is 5.4 to 5.8. The formulas for the individual electrolytes and amino acids are as follows:
Electrolytes
Sodium Acetate Trihydrate, USP
CH 3COONax3H 2O
Potassium Chloride, USP
KCl
Sodium Glycerophosphate
C 3H 5(OH) 2PO 4Na 2xH 2O
Magnesium Sulfate Heptahydrate, USP
MgSO 4x7H 2O
Calcium Chloride Dihydrate, USP
CaCl 2x2H 2O
Essential Amino Acids
Lysine (added as the hydrochloride salt)
H 2N(CH 2) 4CH(NH 2)COOH.HCl
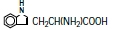
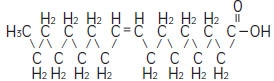
Phenylalanine
Leucine
(CH 3) 2CHCH 2CH(NH 2)COOH
Valine
(CH 3) 2CHCH(NH 2)COOH
Threonine
CH 3CH(OH)CH(NH 2)COOH
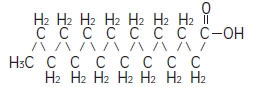
Methionine
CH 3S(CH 2) 2CH(NH 2)COOH
Isoleucine
CH 3CH 2CH(CH 3)CH(NH 2)COOH
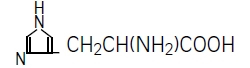
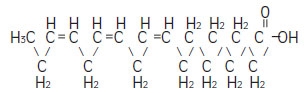
Tryptophan
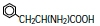
Nonessential Amino Acids
Alanine
CH 3CH(NH 2)COOH
Arginine
H 2NC(NH)NH(CH 2) 3CH(NH 2)COOH
Glycine
H 2NCH 2COOH
Proline

Histidine
Glutamic Acid
HOOC(CH 2) 2CH(NH 2)COOH
Serine
HOCH 2CH(NH 2)COOH
Aspartic Acid
HOOCCH 2CH(NH 2)COOH
Tyrosine

Chamber 3: Contains a 20% Lipid Injectable Emulsion (Intralipid ® 20%) which is made up of 20% Soybean Oil, 1.2% Egg Yolk Phospholipids, 2.25% Glycerin, and water for injection. In addition, sodium hydroxide has been added to adjust the pH. The final product pH range is 6 to 9.
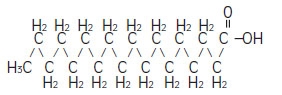
The soybean oil is a refined natural product consisting of a mixture of neutral triglycerides of predominantly unsaturated fatty acids with the following structure:

where
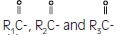 are saturated and unsaturated fatty acid residues. The major component fatty acids are linoleic (48 to 58 %), oleic (17 to 30%), palmitic (9 to 13%), linolenic (5 to 11%) and stearic acid (2.5 to 5%).
are saturated and unsaturated fatty acid residues. The major component fatty acids are linoleic (48 to 58 %), oleic (17 to 30%), palmitic (9 to 13%), linolenic (5 to 11%) and stearic acid (2.5 to 5%).
These fatty acids have the following chemical and structural formulas:
Linoleic acid
C 18H 32O 2
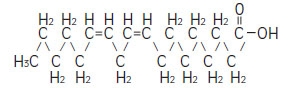
Oleic acid
C 18H 34O 2
Palmitic acid
C 16H 32O 2
Linolenic acid
C 18H 30O 2
Stearic acid
C 18H 36O 2
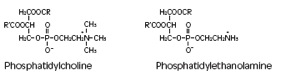
Purified egg phosphatides are a mixture of naturally occurring phospholipids which are isolated from the egg yolk. These phospholipids have the following general structure:

 contain saturated and unsaturated fatty acids that abound in neutral fats. R3 is primarily either the choline or ethanolamine ester of phosphoric acid.
contain saturated and unsaturated fatty acids that abound in neutral fats. R3 is primarily either the choline or ethanolamine ester of phosphoric acid.
Glycerin is chemically designated C 3H 8O 3 and is a clear colorless, hygroscopic syrupy liquid. It has the following structural formula:

The container-solution unit is a closed system and is not dependent upon entry of external air during administration. The container is overwrapped to provide protection from the physical environment and to provide an additional oxygen and moisture barrier when necessary. An oxygen absorber is placed between the inner bag and the overpouch.
The container is not made with natural rubber latex or polyvinyl chloride (PVC).
KABIVEN ® contains no more than 25 mcg/L of aluminum.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
KABIVEN ® is used as a supplement or as the sole source of nutrition in patients, providing macronutrients (amino acids, dextrose and lipids) and micronutrients (electrolytes) parenterally.
The amino acids provide the structural units that make up proteins and are used to synthesize proteins and other biomolecules or are oxidized to urea and carbon dioxide as a source of energy.
The administered dextrose is oxidized to carbon dioxide and water, yielding energy.
Intravenously administered lipids provide a biologically utilizable source of calories and essential fatty acids. Fatty acids serve as an important substrate for energy production. The most common mechanism of action for energy derived from fatty acid metabolism is beta- oxidation. Fatty acids are important for membrane structure and function, precursors for bioactive molecules (such as prostaglandins), and as regulators of gene expression.
12.3 Pharmacokinetics
The infused lipid particles provided by KABIVEN ® are expected to be cleared from the blood stream in a manner thought to be comparable to the clearing of chylomicrons. In healthy volunteers, the maximum clearance rate of the triglycerides after fasting overnight has been found to be 3.8 ± 1.5 g/kg per 24 hours.
Both elimination and oxidation rates are dependent on the patient's clinical condition; elimination is faster and utilization is increased in postoperative patients, in sepsis, burns and trauma, while patients with renal impairment and hypertriglyceridemia may show lower utilization of exogenous lipid emulsions. Due to differences in elimination, patients with these conditions should be closely monitored during KABIVEN ® administration [see Warnings and Precautions (5.3, 5.11)] .The disposition of infused amino acids, dextrose and electrolytes are essentially the same as those supplied by ordinary food.
A clinical study in healthy volunteers employing high intravenous doses (80 mmol) of either sodium glycerophosphate used in KABIVEN ® or reference, inorganic sodium phosphate demonstrated that both compounds resulted in comparable serum inorganic phosphate concentrations after a single intravenous dose. Changes from baseline in the serum levels of sodium, potassium and total calcium were comparable across the two phosphate sources in this study.
- 13 NONCLINICAL TOXICOLOGY
- 15 REFERENCES
-
16 HOW SUPPLIED/STORAGE AND HANDLING
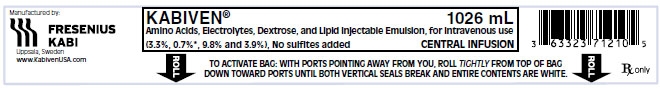
KABIVEN ® is a sterile emulsion available in the following 4 sizes:
NDC Volume
63323-712-25 2,566 mL
63323-712-20 2,053 mL
63323-712-15 1,540 mL
63323-712-10 1,026 mL
Exposure of pharmaceutical products to heat should be minimized. Avoid excessive heat. Protect from freezing. If accidentally frozen, discard the bag. It is recommended that the product be stored at 20º to 25°C (68º to 77°F) [see USP Controlled Room Temperature].
Do not remove container from overpouch until intended for use.
After breaking the vertical seals, chemical and physical in-use stability of the mixed three chamber bag has been demonstrated for 48 hours at 25°C (77°F). If not used immediately, the activated bag can be stored for up to 7 days under refrigeration [2° to 8°C (36º to 46°F)]. After removal from refrigeration, the activated bag should be used within 48 hours.
The product should be used immediately after the introduction of additives. If not used immediately, the storage time and conditions prior to use should not be longer than 24 hours at 2° to 8°C (36° to 46°F). After removal from storage at 2° to 8°C (36° to 46°F), the admixture should be infused within 24 hours. Any mixture remaining must be discarded.
-
17 PATIENT COUNSELING INFORMATION
To ensure the safe and effective use of KABIVEN ®, this information should be discussed with the patient.
Inform patients of the following:
- KABIVEN ® is given by infusion through a central vein catheter only.
- Allergic reactions to KABIVEN ® may occur.
- There is a risk of infection and sepsis associated with formulations administered intravenously.
- KABIVEN ® may cause adverse reactions such as nausea and vomiting, excess fat (lipids) in the blood, high blood sugar, abnormally increased transaminase and bilirubin, or abnormally high or low blood electrolyte levels.
- Contact their healthcare provider if they develop symptoms of an allergic reaction, infection, high blood sugar, low blood sugar, nausea, vomiting, or fluid retention occurs.
- Have periodic laboratory tests and routinely follow-up with their healthcare provider.
- Inform their healthcare provider about any changes in prescription or over the counter medications and supplements to avoid potential drug interactions and side effects.
When patients self-administer KABIVEN® injection at home, inform patients of the following:
- Patients and/or caregiver must be trained in how to inspect, activate and administer KABIVEN ®.
- Follow the KABIVEN ® inspection, activation and administration instructions provided by their home care provider, and Prescribing Information [see Dosage and Administration (2.1, 2.2 and 2.3)].
- Do not deviate from the administration instructions given by the healthcare provider.
- Inspect KABIVEN ® before using for evidence of damage, particulate matter, and/or discoloration.
- Discard the bag in the following situations:
- Evidence of damage to the bag
- More than one chamber is white
- Solution is yellow
- Any seal is already broken
- Prior to activation, store KABIVEN ® between 20° to 25°C (68° to 77°F).
- Activate bag just prior to use or refrigerate activated bag at 2° to 8°C (36° to 46°F) for up to 7 days. After removal from storage at 2° to 8°C (36° to 46°F), the activated bag should be used within 48 hours. Discard any unused portion.
- After activation and prior to administration carefully inspect bag for separation of the lipid emulsion, which can be visibly identified by a yellowish streaking or the accumulation of yellowish droplets in the mixed emulsion. Discard the bag if this occurs.
Additional information is available at www.KabivenUSA.com.
- SPL UNCLASSIFIED SECTION
- PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
KABIVEN
dextrose, soybean oil, electrolytes, lysine, phenylalanine, leucine, valine, threonine, methionine, isoleucine, tryptophan, alanine, arginine, glycine, proline, histidine, glutamic acid, serine, aspartic acid and tyrosine injection, emulsionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 63323-712 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength DEXTROSE MONOHYDRATE (UNII: LX22YL083G) (ANHYDROUS DEXTROSE - UNII:5SL0G7R0OK) DEXTROSE MONOHYDRATE 9.8 g in 100 mL SOYBEAN OIL (UNII: 241ATL177A) (SOYBEAN OIL - UNII:241ATL177A) SOYBEAN OIL 3.9 g in 100 mL SODIUM ACETATE (UNII: 4550K0SC9B) (SODIUM CATION - UNII:LYR4M0NH37, ACETATE ION - UNII:569DQM74SC) SODIUM ACETATE ANHYDROUS 239 mg in 100 mL POTASSIUM CHLORIDE (UNII: 660YQ98I10) (POTASSIUM CATION - UNII:295O53K152, CHLORIDE ION - UNII:Q32ZN48698) POTASSIUM CHLORIDE 174 mg in 100 mL SODIUM GLYCEROPHOSPHATE ANHYDROUS (UNII: YP1H63LJ2K) (SODIUM CATION - UNII:LYR4M0NH37, PHOSPHATE ION - UNII:NK08V8K8HR) SODIUM GLYCEROPHOSPHATE ANHYDROUS 147 mg in 100 mL MAGNESIUM SULFATE HEPTAHYDRATE (UNII: SK47B8698T) (MAGNESIUM CATION - UNII:T6V3LHY838) MAGNESIUM SULFATE HEPTAHYDRATE 96 mg in 100 mL CALCIUM CHLORIDE (UNII: M4I0D6VV5M) (CALCIUM CATION - UNII:2M83C4R6ZB, CHLORIDE ION - UNII:Q32ZN48698) CALCIUM CHLORIDE 29 mg in 100 mL LYSINE HYDROCHLORIDE (UNII: JNJ23Q2COM) (LYSINE - UNII:K3Z4F929H6) LYSINE 263 mg in 100 mL PHENYLALANINE (UNII: 47E5O17Y3R) (PHENYLALANINE - UNII:47E5O17Y3R) PHENYLALANINE 231 mg in 100 mL LEUCINE (UNII: GMW67QNF9C) (LEUCINE - UNII:GMW67QNF9C) LEUCINE 231 mg in 100 mL VALINE (UNII: HG18B9YRS7) (VALINE - UNII:HG18B9YRS7) VALINE 213 mg in 100 mL THREONINE (UNII: 2ZD004190S) (THREONINE - UNII:2ZD004190S) THREONINE 164 mg in 100 mL METHIONINE (UNII: AE28F7PNPL) (METHIONINE - UNII:AE28F7PNPL) METHIONINE 164 mg in 100 mL ISOLEUCINE (UNII: 04Y7590D77) (ISOLEUCINE - UNII:04Y7590D77) ISOLEUCINE 164 mg in 100 mL TRYPTOPHAN (UNII: 8DUH1N11BX) (TRYPTOPHAN - UNII:8DUH1N11BX) TRYPTOPHAN 55 mg in 100 mL ALANINE (UNII: OF5P57N2ZX) (ALANINE - UNII:OF5P57N2ZX) ALANINE 467 mg in 100 mL ARGININE (UNII: 94ZLA3W45F) (ARGININE - UNII:94ZLA3W45F) ARGININE 330 mg in 100 mL GLYCINE (UNII: TE7660XO1C) (GLYCINE - UNII:TE7660XO1C) GLYCINE 231 mg in 100 mL PROLINE (UNII: 9DLQ4CIU6V) (PROLINE - UNII:9DLQ4CIU6V) PROLINE 199 mg in 100 mL HISTIDINE (UNII: 4QD397987E) (HISTIDINE - UNII:4QD397987E) HISTIDINE 199 mg in 100 mL GLUTAMIC ACID (UNII: 3KX376GY7L) (GLUTAMIC ACID - UNII:3KX376GY7L) GLUTAMIC ACID 164 mg in 100 mL SERINE (UNII: 452VLY9402) (SERINE - UNII:452VLY9402) SERINE 131 mg in 100 mL ASPARTIC ACID (UNII: 30KYC7MIAI) (ASPARTIC ACID - UNII:30KYC7MIAI) ASPARTIC ACID 99 mg in 100 mL TYROSINE (UNII: 42HK56048U) (TYROSINE - UNII:42HK56048U) TYROSINE 6.7 mg in 100 mL Inactive Ingredients Ingredient Name Strength EGG PHOSPHOLIPIDS (UNII: 1Z74184RGV) GLYCERIN (UNII: PDC6A3C0OX) WATER (UNII: 059QF0KO0R) SODIUM HYDROXIDE (UNII: 55X04QC32I) ACETIC ACID (UNII: Q40Q9N063P) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 63323-712-10 1026 mL in 1 BAG; Type 0: Not a Combination Product 08/25/2014 2 NDC: 63323-712-15 1540 mL in 1 BAG; Type 0: Not a Combination Product 08/25/2014 3 NDC: 63323-712-20 2053 mL in 1 BAG; Type 0: Not a Combination Product 08/25/2014 4 NDC: 63323-712-25 2566 mL in 1 BAG; Type 0: Not a Combination Product 08/25/2014 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA200656 08/25/2014 Labeler - Fresenius Kabi USA, LLC (608775388) Establishment Name Address ID/FEI Business Operations Fresenius Kabi AB Uppsala 559785113 analysis(63323-712) , manufacture(63323-712)
Trademark Results [Kabiven]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 KABIVEN 85191861 4601728 Live/Registered |
Fresenius Kabi AG 2010-12-07 |
 KABIVEN 78196149 2908219 Dead/Cancelled |
FRESENIUS SE 2002-12-19 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.