OCREVUS ZUNOVO- ocrelizumab and hyaluronidase injection, solution
Ocrevus Zunovo by
Drug Labeling and Warnings
Ocrevus Zunovo by is a Prescription medication manufactured, distributed, or labeled by Genentech, Inc., Roche Diagnostics GmbH, F. Hoffmann-La Roche Ltd., Roche Singapore Technical Operations Pte. Ltd. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use OCREVUS ZUNOVO safely and effectively. See full prescribing information for OCREVUS ZUNOVO.
OCREVUS ZUNOVO® (ocrelizumab and hyaluronidase-ocsq) injection, for subcutaneous use
Initial U.S. Approval: 2024INDICATIONS AND USAGE
DOSAGE AND ADMINISTRATION
- OCREVUS ZUNOVO should be administered by a healthcare professional (2.1)
- For subcutaneous use in the abdomen only (2.1)
- OCREVUS ZUNOVO has different dosage and administration instructions than intravenous ocrelizumab (2.1)
- Before initiating OCREVUS ZUNOVO, screen for Hepatitis B virus and obtain serum quantitative immunoglobulins, aminotransferases, alkaline phosphatase, and bilirubin (2.2)
- Pre-medicate orally with dexamethasone (or an equivalent corticosteroid) and an antihistamine (e.g., desloratadine) at least 30 minutes prior to each injection (2.3)
- Administer 23 mL of OCREVUS ZUNOVO (920 mg ocrelizumab and 23,000 units hyaluronidase) subcutaneously in the abdomen over approximately 10 minutes every 6 months (2.4)
- Monitor patients closely during all injections, for at least one hour after the initial injection, and for at least 15 minutes after subsequent injections (2.4)
DOSAGE FORMS AND STRENGTHS
- Injection: 920 mg ocrelizumab and 23,000 units hyaluronidase per 23 mL (40 mg and 1,000 units per mL) solution in a single-dose vial (3)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- Injection Reactions: Management recommendations for injection reactions depend on the type and severity of the reaction. Permanently discontinue OCREVUS ZUNOVO if a life-threatening injection reaction occurs (4, 5.1)
- Infections: Serious, including life-threatening and fatal, infections have occurred in patients treated with ocrelizumab. Delay OCREVUS ZUNOVO administration in patients with an active infection until the infection is resolved. Vaccination with live-attenuated or live vaccines is not recommended during treatment with OCREVUS ZUNOVO and after discontinuation, until B-cell repletion (5.2)
- Progressive Multifocal Leukoencephalopathy (PML): Withhold OCREVUS ZUNOVO at the first sign or symptom suggestive of PML (5.3)
- Reduction in Immunoglobulins: Monitor the level of immunoglobulins at the beginning of treatment. Monitor during and after discontinuation of treatment with OCREVUS ZUNOVO, until B-cell repletion, and especially when recurrent serious infections are suspected. Consider discontinuing OCREVUS ZUNOVO in patients with serious opportunistic or recurrent serious infections, and if prolonged hypogammaglobulinemia requires treatment with intravenous immunoglobulins (2.1, 5.4)
- Malignancies: An increased risk of malignancy, including breast cancer, may exist with OCREVUS ZUNOVO (5.5)
- Immune-Mediated Colitis: Immune-mediated colitis has been reported in the postmarketing setting. Monitor patients for new or persistent diarrhea or other gastrointestinal symptoms, and evaluate promptly if colitis is suspected (5.6)
- Liver Injury: Clinically significant liver injury has occurred. Obtain serum aminotransferases, alkaline phosphatase, and bilirubin levels before initiating OCREVUS ZUNOVO, and during treatment as clinically indicated. Discontinue OCREVUS ZUNOVO in patients with evidence of liver injury in the absence of an alternative etiology (5.7)
ADVERSE REACTIONS
The most common adverse reactions in patients treated with intravenous ocrelizumab were:
- RMS (incidence ≥10% and > REBIF®): upper respiratory tract infections and infusion reactions (6.1)
- PPMS (incidence ≥10% and > placebo): upper respiratory tract infections, infusion reactions, skin infections, and lower respiratory tract infections (6.1)
The most common adverse reaction observed with OCREVUS ZUNOVO in patients with RMS and PPMS was injection reactions (incidence of 49%) (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Genentech at 1-888-835-2555 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 8/2025
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Important Administration Information
2.2 Assessments Prior to First Dose of OCREVUS ZUNOVO
2.3 Assessments and Premedication Prior to Every Dose
2.4 Recommended Dosage
2.5 Delayed or Missed Doses
2.6 Preparation and Administration
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Injection Reactions
5.2 Infections
5.3 Progressive Multifocal Leukoencephalopathy
5.4 Reduction in Immunoglobulins
5.5 Malignancies
5.6 Immune-Mediated Colitis
5.7 Liver Injury
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Immunosuppressive or Immune-Modulating Therapies
7.2 Vaccinations
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
12.6 Immunogenicity
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Intravenous Ocrelizumab in Patients With Relapsing Forms of Multiple Sclerosis
14.2 Intravenous Ocrelizumab in Patients With Primary Progressive Multiple Sclerosis
14.3 OCREVUS ZUNOVO in Patients With RMS or PPMS
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 Important Administration Information
OCREVUS ZUNOVO is for subcutaneous use in the abdomen only.
OCREVUS ZUNOVO has different dosage and administration instructions than intravenous ocrelizumab.
OCREVUS ZUNOVO should be administered via subcutaneous injection by a healthcare professional.
2.2 Assessments Prior to First Dose of OCREVUS ZUNOVO
Hepatitis B Virus Screening
Prior to initiating ocrelizumab treatment, perform Hepatitis B virus (HBV) screening. OCREVUS ZUNOVO is contraindicated in patients with active HBV confirmed by positive results for HBsAg and anti-HBV tests. For patients who are negative for surface antigen [HBsAg] and positive for HB core antibody [HBcAb+] or are carriers of HBV [HBsAg+], consult liver disease experts before starting and during treatment [see Warnings and Precautions (5.2)].
Serum Immunoglobulins
Prior to initiating ocrelizumab treatment, perform testing for quantitative serum immunoglobulins [see Warnings and Precautions (5.4)]. For patients with low serum immunoglobulins, consult immunology experts before initiating treatment with ocrelizumab.
Vaccinations
Because vaccination with live-attenuated or live vaccines is not recommended during treatment and after discontinuation until B-cell repletion, administer all immunizations according to immunization guidelines at least 4 weeks prior to initiation of ocrelizumab treatment for live or live-attenuated vaccines and, whenever possible, at least 2 weeks prior to initiation of ocrelizumab treatment for non-live vaccines [see Warnings and Precautions (5.2) and Clinical Pharmacology (12.2)].
Liver Function Tests
Prior to initiating OCREVUS ZUNOVO, obtain serum aminotransferases (alanine aminotransferase [ALT] and aspartate aminotransferase [AST]), alkaline phosphatase, and bilirubin levels [see Warnings and Precautions (5.7)].
2.3 Assessments and Premedication Prior to Every Dose
Infection Assessment
Prior to every dose of OCREVUS ZUNOVO, determine whether there is an active infection. In case of active infection, delay administration of OCREVUS ZUNOVO until the infection resolves [see Warnings and Precautions (5.2)].
Recommended Premedication
Pre-medicate orally with 20 mg of dexamethasone (or an equivalent corticosteroid) and an antihistamine (e.g., desloratadine) administered at least 30 minutes prior to each OCREVUS ZUNOVO administration to reduce the risk of local and systemic injection reactions [see Warnings and Precautions (5.1)].
The addition of an antipyretic (e.g., acetaminophen) may also be considered.
2.4 Recommended Dosage
The recommended dosage of OCREVUS ZUNOVO is 920 mg/23,000 units (920 mg ocrelizumab and 23,000 units of hyaluronidase) administered as a single 23 mL subcutaneous injection in the abdomen over approximately 10 minutes every 6 months.
Monitor the patient closely during injections, with access to appropriate medical support to manage severe injection reactions. For the initial dose, monitor the patient for at least one hour post-injection. For subsequent doses, monitor the patient for at least 15 minutes post-injection [see Warnings and Precautions (5.1)].
2.5 Delayed or Missed Doses
If a planned injection of OCREVUS ZUNOVO is missed, administer OCREVUS ZUNOVO as soon as possible; do not wait until the next scheduled dose. Reset the dose schedule to administer the next sequential dose 6 months after the missed dose is administered. Doses of OCREVUS ZUNOVO must be separated by at least 5 months [see Dosage and Administration (2.4)].
2.6 Preparation and Administration
To prevent medication errors, check the vial labels to ensure that the drug being prepared and administered is OCREVUS ZUNOVO and not intravenous ocrelizumab.
Visually inspect the vial for particulate matter and discoloration prior to administration, whenever solution and container permit. Do not use the vial if particulates or discoloration are present. Do not shake. Discard any unused portion remaining in the vial.
OCREVUS ZUNOVO is compatible with polypropylene (PP), polycarbonate (PC), polyethylene (PE), stainless steel (SS), polyvinylchloride (PVC), and polyurethane (PUR).
Preparation of the Syringe
OCREVUS ZUNOVO should be prepared by a healthcare professional.
- Immediate use is recommended, as OCREVUS ZUNOVO does not contain any antimicrobial preservative. If the dose is not administered immediately, refer to "Storage of the Syringe" below.
- Remove the vial from refrigerated storage and allow the solution to acclimate to room temperature at or below 25°C (77°F).
- Withdraw the entire contents of OCREVUS ZUNOVO solution from the vial with a syringe and transfer needle (21G needle recommended).
- Do not dilute.
- Remove the transfer needle from the syringe and replace with a subcutaneous infusion set (e.g., winged/butterfly) containing a 24G-26G needle for injection. Use a subcutaneous infusion set with a priming volume NOT to exceed 0.8 mL for administration.
- Prime the subcutaneous infusion line with the drug product solution to eliminate the air in the infusion line and stop before the fluid reaches the needle.
- Ensure the syringe contains exactly 23 mL of drug product solution after priming and expelling any excess volume from the syringe.
- Administer immediately to avoid needle clogging. DO NOT store the prepared syringe that has been attached to the already primed subcutaneous infusion set.
Administration
- Administer 23 mL of OCREVUS ZUNOVO subcutaneously in the abdomen over approximately 10 minutes. DO NOT administer the remaining priming volume in the subcutaneous infusion set to the patient.
- The recommended injection site is the abdomen, except for 2 inches (5 cm) around the navel. Do not administer OCREVUS ZUNOVO injections into areas where the skin is red, bruised, tender, or hard, or areas where there are moles or scars.
Storage of the Syringe
- If the dose is not to be administered immediately, use aseptic technique to withdraw the entire OCREVUS ZUNOVO contents from the vial into the syringe to account for the dose volume (23 mL) plus the priming volume for the subcutaneous infusion set. Replace the transfer needle with a syringe closing cap. DO NOT attach a subcutaneous infusion set.
- If not used immediately, the closed syringe can be refrigerated (2°C to 8°C [36°F to 46°F]) for up to 72 hours followed by 8 hours at ambient temperatures at or below 25°C (77°F) in diffuse daylight.
- If the prepared syringe was stored at 2°C to 8°C (36°F to 46°F), allow the syringe to acclimate to room temperature prior to administration.
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
OCREVUS ZUNOVO is contraindicated in patients with:
- Active HBV infection [see Dosage and Administration (2.2) and Warnings and Precautions (5.2)]
- A history of life-threatening administration reaction to ocrelizumab [see Warnings and Precautions (5.1)]
- A history of hypersensitivity to ocrelizumab, hyaluronidase, or any component of OCREVUS ZUNOVO [see Warnings and Precautions (5.1)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Injection Reactions
OCREVUS ZUNOVO can cause injection reactions, which can be local or systemic. Common symptoms of local injection reactions reported by patients treated with OCREVUS ZUNOVO in multiple sclerosis (MS) clinical trials included erythema, pain, swelling, and pruritus. Common symptoms of systemic injection reactions reported by patients included headache and nausea. In an open-label, active-controlled trial, injection reactions were more frequently reported with the first injection; 49% of patients experienced an injection reaction with the first injection [see Adverse Reactions (6.1)].
In MS clinical trials where ocrelizumab was administered intravenously, the incidence of infusion reactions in patients [who received methylprednisolone (or an equivalent steroid) and possibly other premedication to reduce the risk of infusion reactions prior to infusion] was 34% to 40%, with the highest incidence with the first infusion. There were no fatal infusion reactions, but 0.3% of intravenous ocrelizumab-treated MS patients experienced infusion reactions that were serious, some requiring hospitalization. Symptoms of infusion reactions can include pruritus, rash, urticaria, erythema, bronchospasm, throat irritation, oropharyngeal pain, dyspnea, pharyngeal or laryngeal edema, flushing, hypotension, pyrexia, fatigue, headache, dizziness, nausea, tachycardia, and anaphylaxis.
Monitor patients during and after injections [see Dosage and Administration (2.4)]. Inform patients that injection reactions can occur during or within 24 hours of the injection.
Reducing the Risk of Injection Reactions and Managing Injection Reactions
Administer oral premedication (e.g., dexamethasone or an equivalent corticosteroid, and an antihistamine) at least 30 minutes prior to each OCREVUS ZUNOVO injection to reduce the risk of injection reactions. The addition of an antipyretic (e.g., acetaminophen) may also be considered [see Dosage and Administration (2.3)].
Management recommendations for injection reactions depend on the type and severity of the reaction. For life-threatening injection reactions, immediately and permanently stop OCREVUS ZUNOVO and administer appropriate supportive treatment. For less severe injection reactions, the injection should be interrupted immediately, and the patient should receive symptomatic treatment. The injection should be completed at the healthcare provider's discretion and only after all symptoms have resolved.
5.2 Infections
Serious, including life-threatening or fatal, bacterial, viral, parasitic, and fungal infections have been reported in patients receiving ocrelizumab. An increased risk of infections (including serious and fatal bacterial, fungal, and new or reactivated viral infections) has been observed in patients during and following completion of treatment with anti-CD20 B-cell depleting therapies.
A higher proportion of intravenous ocrelizumab-treated patients experienced infections compared to patients taking REBIF or placebo. In RMS trials, 58% of intravenous ocrelizumab-treated patients experienced one or more infections compared to 52% of REBIF-treated patients. In the PPMS trial, 70% of intravenous ocrelizumab-treated patients experienced one or more infections compared to 68% of patients on placebo.
Intravenous ocrelizumab was not associated with an increased risk of serious infections in MS patients in controlled trials.
Ocrelizumab increases the risk for upper respiratory tract infections, lower respiratory tract infections, skin infections, and herpes-related infections [see Adverse Reactions (6.1)].
Delay OCREVUS ZUNOVO administration in patients with an active infection until the infection is resolved.
Respiratory Tract Infections
A higher proportion of intravenous ocrelizumab-treated patients experienced respiratory tract infections compared to patients taking REBIF or placebo. In RMS trials, 40% of patients treated with intravenous ocrelizumab experienced upper respiratory tract infections compared to 33% of REBIF-treated patients, and 8% of patients treated with intravenous ocrelizumab experienced lower respiratory tract infections compared to 5% of REBIF-treated patients. In the PPMS trial, 49% of patients treated with intravenous ocrelizumab experienced upper respiratory tract infections compared to 43% of patients on placebo, and 10% of patients treated with intravenous ocrelizumab experienced lower respiratory tract infections compared to 9% of patients on placebo. The infections were predominantly mild to moderate and consisted mostly of upper respiratory tract infections and bronchitis.
Herpes
In active-controlled (RMS) clinical trials, herpes infections were reported more frequently in patients treated with intravenous ocrelizumab than in REBIF-treated patients, including herpes zoster (2.1% vs. 1.0%), herpes simplex (0.7% vs. 0.1%), oral herpes (3.0% vs. 2.2%), genital herpes (0.1% vs. 0%), and herpes virus infection (0.1% vs. 0%). Infections were predominantly mild to moderate in severity.
In the placebo-controlled (PPMS) clinical trial, oral herpes was reported more frequently in the patients treated with intravenous ocrelizumab than in the patients on placebo (2.7% vs. 0.8%).
Serious cases of infections caused by herpes simplex virus and varicella zoster virus, including central nervous system infections (encephalitis and meningitis), intraocular infections, and disseminated skin and soft tissue infections, have been reported in the postmarketing setting in multiple sclerosis patients receiving ocrelizumab. Some cases were life-threatening. Serious herpes virus infections may occur at any time during treatment with OCREVUS ZUNOVO.
If serious herpes infections occur, OCREVUS ZUNOVO should be discontinued or withheld until the infection has resolved, and appropriate treatment should be administered [see Patient Counseling Information (17)].
Hepatitis B Virus Reactivation
Hepatitis B virus (HBV) reactivation has been reported in MS patients treated with ocrelizumab in the postmarketing setting. Fulminant hepatitis, hepatic failure, and death caused by HBV reactivation have occurred in patients treated with anti-CD20 antibodies. Perform HBV screening in all patients before initiation of treatment with ocrelizumab. Do not administer OCREVUS ZUNOVO to patients with active HBV confirmed by positive results for HBsAg and anti-HB tests. For patients who are negative for surface antigen [HBsAg] and positive for HB core antibody [HBcAb+] or are carriers of HBV [HBsAg+], consult liver disease experts before starting and during treatment.
Possible Increased Risk of Immunosuppressant Effects With Other Immunosuppressants
When initiating OCREVUS ZUNOVO after an immunosuppressive therapy or initiating an immunosuppressive therapy after OCREVUS ZUNOVO, consider the potential for increased immunosuppressive effects [see Drug Interactions (7.1) and Clinical Pharmacology (12.1, 12.2)]. OCREVUS ZUNOVO has not been studied in combination with other MS therapies.
Vaccinations
Administer all immunizations according to immunization guidelines at least 4 weeks prior to initiation of ocrelizumab treatment for live or live-attenuated vaccines and, whenever possible, at least 2 weeks prior to initiation of ocrelizumab for non-live vaccines.
OCREVUS ZUNOVO may interfere with the effectiveness of non-live vaccines [see Drug Interactions (7.2)].
The safety of immunization with live or live-attenuated vaccines following OCREVUS ZUNOVO therapy has not been studied, and vaccination with live-attenuated or live vaccines is not recommended during treatment and until B-cell repletion [see Clinical Pharmacology (12.2)].
Vaccination of Infants Born to Mothers Treated with OCREVUS ZUNOVO During Pregnancy
In infants of mothers exposed to OCREVUS ZUNOVO during pregnancy, do not administer live or live-attenuated vaccines before confirming the recovery of B-cell counts as measured by CD19+ B-cells. Depletion of B-cells in these infants may increase the risks from live or live-attenuated vaccines.
You may administer non-live vaccines, as indicated, prior to recovery from B-cell depletion, but should consider assessing vaccine immune responses, including consultation with a qualified specialist, to assess whether a protective immune response was mounted [see Use in Specific Populations (8.1)].
5.3 Progressive Multifocal Leukoencephalopathy
Cases of progressive multifocal leukoencephalopathy (PML) have been reported in patients with MS treated with ocrelizumab in the postmarketing setting. PML is an opportunistic viral infection of the brain caused by the JC virus (JCV) that typically only occurs in patients who are immunocompromised, and that usually leads to death or severe disability. PML has occurred in ocrelizumab-treated patients who had not been treated previously with natalizumab (which has a known association with PML), were not taking any immunosuppressive or immunomodulatory medications associated with the risk of PML prior to or concomitantly with ocrelizumab, and did not have any known ongoing systemic medical conditions resulting in compromised immune system function.
JCV infection resulting in PML has also been observed in patients treated with other anti-CD20 antibodies and other MS therapies.
At the first sign or symptom suggestive of PML, withhold OCREVUS ZUNOVO and perform an appropriate diagnostic evaluation. Typical symptoms associated with PML are diverse, progress over days to weeks, and include progressive weakness on one side of the body or clumsiness of limbs, disturbance of vision, and changes in thinking, memory, and orientation leading to confusion and personality changes.
MRI findings may be apparent before clinical signs or symptoms. Cases of PML, diagnosed based on MRI findings and the detection of JCV DNA in the cerebrospinal fluid in the absence of clinical signs or symptoms specific to PML, have been reported in patients treated with other MS medications associated with PML. Many of these patients subsequently became symptomatic with PML. Therefore, monitoring with MRI for signs that may be consistent with PML may be useful, and any suspicious findings should lead to further investigation to allow for an early diagnosis of PML, if present. Following discontinuation of another MS medication associated with PML, lower PML-related mortality and morbidity have been reported in patients who were initially asymptomatic at diagnosis compared to patients who had characteristic clinical signs and symptoms at diagnosis.
It is not known whether these differences are due to early detection and discontinuation of MS treatment or due to differences in disease in these patients.
If PML is confirmed, treatment with OCREVUS ZUNOVO should be discontinued.
5.4 Reduction in Immunoglobulins
As expected with any B-cell depleting therapy, decreased immunoglobulin levels are observed with ocrelizumab treatment. The pooled data of intravenous ocrelizumab clinical studies (RMS and PPMS) and their open-label extensions (up to approximately 7 years of exposure) have shown an association between decreased levels of immunoglobulin G (IgG<LLN) and increased rates of serious infections. Monitor the levels of quantitative serum immunoglobulins during OCREVUS ZUNOVO treatment and after discontinuation of treatment, until B-cell repletion, and especially in the setting of recurrent serious infections. Consider discontinuing OCREVUS ZUNOVO therapy in patients with serious opportunistic or recurrent serious infections, and if prolonged hypogammaglobulinemia requires treatment with intravenous immunoglobulins [see Adverse Reactions (6.1)].
5.5 Malignancies
An increased risk of malignancy with OCREVUS ZUNOVO may exist. In controlled trials, malignancies, including breast cancer, occurred more frequently in patients treated with intravenous ocrelizumab. Breast cancer occurred in 6 of 781 females treated with intravenous ocrelizumab and none of 668 females treated with REBIF or placebo. Patients should follow standard breast cancer screening guidelines.
5.6 Immune-Mediated Colitis
Immune-mediated colitis, which can present as a severe and acute-onset form of colitis, has been reported in patients receiving ocrelizumab in the postmarketing setting. Some cases of colitis were serious, requiring hospitalization, with a few patients requiring surgical intervention. Systemic corticosteroids were required in many of these patients. The time from treatment initiation to onset of symptoms in these cases ranged from a few weeks to years. Monitor patients for immune-mediated colitis during OCREVUS ZUNOVO treatment, and evaluate promptly if signs and symptoms that may indicate immune-mediated colitis, such as new or persistent diarrhea or other gastrointestinal signs and symptoms, occur.
5.7 Liver Injury
Clinically significant liver injury, without findings of viral hepatitis, has been reported in the postmarketing setting in patients treated with anti-CD20 B-cell depleting therapies approved for the treatment of MS, including ocrelizumab. Signs of liver injury, including markedly elevated serum hepatic enzymes with elevated total bilirubin, have occurred from weeks to months after administration.
Patients treated with OCREVUS ZUNOVO found to have an alanine aminotransferase (ALT) or aspartate aminotransferase (AST) greater than 3× the upper limit of normal (ULN) with serum total bilirubin greater than 2× ULN are potentially at risk for severe drug-induced liver injury.
Obtain liver function tests prior to initiating treatment with OCREVUS ZUNOVO [see Dosage and Administration (2.2)], and monitor for signs and symptoms of any hepatic injury during treatment. Measure serum aminotransferases, alkaline phosphatase, and bilirubin levels promptly in patients who report symptoms that may indicate liver injury, including new or worsening fatigue, anorexia, nausea, vomiting, right upper abdominal discomfort, dark urine, or jaundice. If liver injury is present and an alternative etiology is not identified, discontinue OCREVUS ZUNOVO.
-
6 ADVERSE REACTIONS
The following serious adverse reactions are discussed in greater detail in other sections of the labeling:
- Injection Reactions [see Warnings and Precautions (5.1)]
- Infections [see Warnings and Precautions (5.2)]
- Progressive Multifocal Leukoencephalopathy [see Warnings and Precautions (5.3)]
- Reduction in Immunoglobulins [see Warnings and Precautions (5.4)]
- Malignancies [see Warnings and Precautions (5.5)]
- Immune-Mediated Colitis [see Warnings and Precautions (5.6)]
- Liver Injury [see Warnings and Precautions (5.7)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
The safety of ocrelizumab has been evaluated in active-controlled clinical trials of ocrelizumab administered intravenously in patients with relapsing forms of MS (RMS) (Study 1 and Study 2) [see Clinical Studies (14.1)] and primary progressive MS (PPMS) (Study 3) [see Clinical Studies (14.2)], and in an open-label, active-controlled trial of OCREVUS ZUNOVO administered subcutaneously in patients with RMS and PPMS (Study 4) [see Clinical Studies (14.3)].
Adverse Reactions With Ocrelizumab Intravenous in Patients With RMS and PPMS
The safety of intravenous ocrelizumab has been evaluated in 1311 patients across the MS clinical studies, which included 825 patients in active-controlled clinical trials in patients with RMS and 486 patients in a placebo-controlled study in patients with PPMS.
RMS
In active-controlled intravenous ocrelizumab clinical trials (Study 1 and Study 2), 825 patients with RMS received ocrelizumab 600 mg intravenously every 24 weeks (initial treatment was given as two separate 300 mg infusions at Weeks 0 and 2) [see Clinical Studies (14.1)]. The overall exposure in the 96-week controlled treatment periods was 1448 patient-years.
The most common adverse reactions in RMS trials (incidence ≥ 10%) were upper respiratory tract infections and infusion reactions. Table 1 summarizes the adverse reactions that occurred in active-controlled intravenous ocrelizumab RMS trials (Study 1 and Study 2).
Table 1 Adverse Reactions in Adult Patients With RMS With an Incidence of at least 5% for Intravenous Ocrelizumab and Higher than REBIF Adverse Reactions Studies 1 and 2 Ocrelizumab
600 mg IV
Every 24 Weeks*
(n=825)
%REBIF
44 mcg SQ
3 Times per Week
(n=826)
%- * The first dose was given as two separate 300 mg infusions at Weeks 0 and 2.
Upper respiratory tract infections 40 33 Infusion reactions 34 10 Depression 8 7 Lower respiratory tract infections 8 5 Back pain 6 5 Herpes virus- associated infections 6 4 Pain in extremity 5 4 PPMS
In a placebo-controlled intravenous ocrelizumab clinical trial (Study 3), a total of 486 patients with PPMS received one course of ocrelizumab (600 mg of ocrelizumab administered as two 300 mg infusions two weeks apart) given intravenously every 24 weeks and 239 patients received placebo intravenously [see Clinical Studies (14.2)]. The overall exposure in the controlled treatment period was 1416 patient-years, with median treatment duration of 3 years.
The most common adverse reactions in the PPMS trial (incidence ≥ 10%) were upper respiratory tract infections, infusion reactions, skin infections, and lower respiratory tract infections. Table 2 summarizes the adverse reactions that occurred in the placebo-controlled intravenous ocrelizumab PPMS trial (Study 3).
Table 2 Adverse Reactions in Adult Patients With PPMS With an Incidence of at Least 5% for Intravenous Ocrelizumab and Higher Than Placebo Adverse Reactions Study 3 Ocrelizumab 600 mg IV Every 24 Weeks* Placebo (n=486)
%(n=239)
%- * One dose of intravenous ocrelizumab (600 mg administered as two 300 mg infusions two weeks apart)
Upper respiratory tract infections 49 43 Infusion reactions 40 26 Skin infections 14 11 Lower respiratory tract infections 10 9 Cough 7 3 Diarrhea 6 5 Edema peripheral 6 5 Herpes virus associated infections 5 4 Laboratory Abnormalities
Decreased Immunoglobulins
Ocrelizumab decreased total immunoglobulins, with the greatest decline seen in IgM levels; however, a decrease in IgG levels was associated with an increased rate of serious infections.
In the active-controlled (RMS) trials (Study 1 and Study 2), the proportion of patients at baseline reporting IgG, IgA, and IgM below the lower limit of normal (LLN) in patients treated with intravenous ocrelizumab was 0.5%, 1.5%, and 0.1%, respectively. Following treatment, the proportion of patients treated with intravenous ocrelizumab reporting IgG, IgA, and IgM below the LLN at 96 weeks was 1.5%, 2.4%, and 16.5%, respectively.
In the placebo-controlled (PPMS) trial (Study 3), the proportion of patients at baseline reporting IgG, IgA, and IgM below the LLN in patients treated with intravenous ocrelizumab was 0.0%, 0.2%, and 0.2%, respectively. Following treatment, the proportion of patients treated with intravenous ocrelizumab reporting IgG, IgA, and IgM below the LLN at 120 weeks was 1.1%, 0.5%, and 15.5%, respectively.
The pooled data of intravenous ocrelizumab clinical studies (RMS and PPMS) and their open-label extensions (up to approximately 7 years of exposure) have shown an association between decreased levels of IgG and increased rates of serious infections. The type, severity, latency, duration, and outcome of serious infections observed during episodes of immunoglobulins below LLN were consistent with the overall serious infections observed in patients treated with intravenous ocrelizumab.
Decreased Neutrophil Levels
In the PPMS clinical trial (Study 3), decreased neutrophil counts occurred in 13% of patients treated with intravenous ocrelizumab compared to 10% in placebo patients. The majority of the decreased neutrophil counts were only observed once for a given patient treated with intravenous ocrelizumab and were between the LLN and 1.0 × 109/L. Overall, 1% of the patients in the intravenous ocrelizumab group had neutrophil counts less than 1.0 × 109/L and these were not associated with an infection.
Adverse Reactions With OCREVUS ZUNOVO in Patients With RMS and PPMS
The safety of OCREVUS ZUNOVO was evaluated in Study 4, an active-controlled, open-label, randomized study in ocrelizumab-naïve patients with RMS or PPMS [see Clinical Studies (14.3)]. One hundred eighteen patients received OCREVUS ZUNOVO as their first dose and 118 patients received intravenous ocrelizumab for their first dose (two separate 300 mg infusions at Weeks 0 and 2).
The most common adverse reactions (reported in at least 10% of OCREVUS ZUNOVO-treated patients) were injection reactions.
In Study 4, injection reactions occurred in 49% (58/118) of patients after the first injection of OCREVUS ZUNOVO. Of these 118 patients, 47% and 11% experienced at least one local injection reaction and one systemic injection reaction, respectively. The most common symptoms reported by patients with local and systemic injection reactions included: injection site erythema, injection site pain, injection site swelling, injection site pruritus, headache, and nausea. Among the patients experiencing an injection reaction, the majority of patients (83%) had injection reactions occur within 24 hours after the end of the injection, as opposed to during the injection (19%). All injection reactions were of mild (73%) or moderate (27%) severity. The median duration of symptoms was 3 days for systemic injection reactions and 3.5 days for local injection reactions. All patients recovered from injection reactions, of which 26% required symptomatic treatment.
For subsequent injections, among the 118 patients who received OCREVUS ZUNOVO only throughout the study, the frequency of local injection reactions ranged from 31% to 43% and the frequency of systemic injection reactions ranged from 3% to 7% from Injection 2 to Injection 4. All injection reactions were of mild or moderate severity.
6.2 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of ocrelizumab. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Gastrointestinal Disorders: Immune-mediated colitis [see Warnings and Precautions (5.6)]
Hepatobiliary Disorders: Liver injury [see Warnings and Precautions (5.7)]
Infections and Infestations: Serious herpes infections [see Warnings and Precautions (5.2)], progressive multifocal leukoencephalopathy [see Warnings and Precautions (5.3)], and babesiosis
Skin: Pyoderma gangrenosum
-
7 DRUG INTERACTIONS
7.1 Immunosuppressive or Immune-Modulating Therapies
The concomitant use of OCREVUS ZUNOVO and other immune-modulating or immunosuppressive therapies, including immunosuppressant doses of corticosteroids, is expected to increase the risk of immunosuppression. Consider the risk of additive immune system effects when coadministering immunosuppressive therapies with OCREVUS ZUNOVO. When switching from drugs with prolonged immune effects, such as daclizumab, fingolimod, natalizumab, teriflunomide, or mitoxantrone, consider the duration and mode of action of these drugs because of additive immunosuppressive effects when initiating OCREVUS ZUNOVO [see Warnings and Precautions (5.2)].
7.2 Vaccinations
A Phase 3b randomized, open-label study examined the concomitant use of intravenous ocrelizumab and several non-live vaccines in adults 18-55 years of age with relapsing forms of MS (68 subjects undergoing treatment with intravenous ocrelizumab at the time of vaccination and 34 subjects not undergoing treatment with intravenous ocrelizumab at the time of vaccination). Concomitant exposure to intravenous ocrelizumab attenuated antibody responses to tetanus toxoid-containing vaccine, pneumococcal polysaccharide, pneumococcal conjugate vaccines, and seasonal inactivated influenza vaccines. The impact of the observed attenuation on vaccine effectiveness in this patient population is unknown. The safety and effectiveness of live or live-attenuated vaccines administered concomitantly with ocrelizumab have not been assessed [see Warnings and Precautions (5.2)].
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
OCREVUS ZUNOVO is a humanized monoclonal antibody of an immunoglobulin G1 subtype and immunoglobulins are known to cross the placental barrier. There are no adequate data on the developmental risk associated with use of OCREVUS ZUNOVO or ocrelizumab-containing products in pregnant women. However, transient peripheral B-cell depletion and lymphocytopenia have been reported in infants born to mothers exposed to other anti-CD20 antibodies during pregnancy. B-cell levels in infants following maternal exposure to OCREVUS ZUNOVO or ocrelizumab-containing products have not been studied in clinical trials. The potential duration of B-cell depletion in such infants, and the impact of B-cell depletion on vaccine safety and effectiveness, is unknown [see Warnings and Precautions (5.2)].
Following administration of ocrelizumab to pregnant monkeys at doses similar to or greater than those used clinically, increased perinatal mortality, depletion of B-cell populations, and renal, bone marrow, and testicular toxicity were observed in the offspring in the absence of maternal toxicity [see Data].
In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively. The background risk of major birth defects and miscarriage for the indicated population is unknown.
Data
Animal Data
OCREVUS ZUNOVO for subcutaneous injection contains ocrelizumab and hyaluronidase [see Description (11)].
Ocrelizumab:
- - Following intravenous administration of ocrelizumab to monkeys during organogenesis (loading doses of 15 or 75 mg/kg on gestation days 20, 21, and 22, followed by weekly doses of 20 or 100 mg/kg), depletion of B-lymphocytes in lymphoid tissue (spleen and lymph nodes) was observed in fetuses at both doses.
- - Intravenous administration of ocrelizumab (three daily loading doses of 15 or 75 mg/kg, followed by weekly doses of 20 or 100 mg/kg) to pregnant monkeys throughout the period of organogenesis and continuing through the neonatal period resulted in perinatal deaths (some associated with bacterial infections), renal toxicity (glomerulopathy and inflammation), lymphoid follicle formation in the bone marrow, and severe decreases in circulating B-lymphocytes in neonates. The cause of the neonatal deaths is uncertain; however, both affected neonates were found to have bacterial infections. Reduced testicular weight was observed in neonates at the high dose.
- - A no-effect dose for adverse developmental effects was not identified; the doses tested in monkey are 2 and 10 times the recommended human dose of 600 mg intravenous ocrelizumab, on a mg/kg basis.
Hyaluronidase:
- - In an embryo-fetal study, mice were dosed daily by subcutaneous injection during the period of organogenesis with hyaluronidase (human recombinant) at dose levels up to 2,200,000 U/kg, which is > 5,700 times higher than the human dose. The study found no evidence of teratogenicity. Reduced fetal weight and increased numbers of fetal resorptions were observed, with no effects found at a daily dose of 360,000 U/kg, which is > 940 times higher than the human dose.
- - In a pre-and postnatal development study, mice have been dosed daily by subcutaneous injection, with hyaluronidase (human recombinant) from implantation through lactation and weaning at dose levels up to 1,100,000 U/kg, which is > 2,800 times higher than the human dose. The study found no adverse effects on sexual maturation, learning and memory, or fertility of the offspring.
8.2 Lactation
Risk Summary
There are no data on the presence of ocrelizumab or hyaluronidase, from administration of OCREVUS ZUNOVO, in human milk, the effects on the breastfed infant, or the effects of the drug on milk production. Ocrelizumab was excreted in the milk of ocrelizumab-treated monkeys. Human IgG is excreted in human milk, and the potential for absorption of ocrelizumab to lead to B-cell depletion in the infant is unknown. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for OCREVUS ZUNOVO and any potential adverse effects on the breastfed infant from OCREVUS ZUNOVO or from the underlying maternal condition.
8.3 Females and Males of Reproductive Potential
Contraception
Women of childbearing potential should use effective contraception while receiving OCREVUS ZUNOVO and for 6 months after the last dose of OCREVUS ZUNOVO [see Clinical Pharmacology (12.3)].
-
11 DESCRIPTION
Ocrelizumab is a recombinant humanized monoclonal antibody directed against CD20-expressing B-cells. Ocrelizumab is a glycosylated immunoglobulin G1 (IgG1) with a molecular mass of approximately 145 kDa.
Hyaluronidase (human recombinant) is an endoglycosidase used to increase the dispersion and absorption of co-administered drugs when administered subcutaneously. It is a glycosylated single-chain protein produced by mammalian (Chinese Hamster Ovary) cells containing a DNA plasmid encoding for a soluble fragment of human hyaluronidase (PH20). Hyaluronidase (human recombinant) has a molecular weight of approximately 61 kDa.
OCREVUS ZUNOVO (ocrelizumab and hyaluronidase-ocsq) injection for subcutaneous use is a sterile, preservative-free, clear to slightly opalescent, and colorless to pale brown solution supplied in single-dose vials. Each 23 mL of solution contains 920 mg ocrelizumab, 23,000 units of hyaluronidase (human recombinant), glacial acetic acid (5.5 mg), methionine (34.3 mg), polysorbate 20 (13.8 mg), sodium acetate (30.2 mg), trehalose (1889.5 mg), and water for injection at pH 5.3.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The precise mechanism by which ocrelizumab exerts its therapeutic effects in multiple sclerosis is unknown, but is presumed to involve binding to CD20, a cell surface antigen present on pre-B and mature B lymphocytes. Following cell surface binding to B lymphocytes, ocrelizumab results in antibody-dependent cellular cytolysis and complement-mediated lysis.
Hyaluronan is a polysaccharide found in the extracellular matrix of the subcutaneous tissue. It is depolymerized by the naturally occurring enzyme hyaluronidase. Unlike the stable structural components of the interstitial matrix, hyaluronan has a half-life of approximately 0.5 days. Hyaluronidase increases permeability of the subcutaneous tissue by depolymerizing hyaluronan. In the doses administered, hyaluronidase in OCREVUS ZUNOVO acts transiently and locally. The effects of hyaluronidase are reversible and permeability of the subcutaneous tissue is restored within 24 to 48 hours.
12.2 Pharmacodynamics
For B-cell counts, assays for CD19+ B-cells are used because the presence of ocrelizumab interferes with the CD20 assay. In clinical studies with OCREVUS ZUNOVO and intravenous ocrelizumab, CD19+ B-cell counts in blood were reduced by 14 days after administration. In clinical studies with intravenous ocrelizumab, B-cell counts rose to above the lower limit of normal (LLN) or above baseline counts between infusions of ocrelizumab at least one time in 0.3% to 4.1% of patients. In a clinical study of 51 patients treated with intravenous ocrelizumab, the median time for B-cell counts to return to either baseline or LLN was 72 weeks (range 27-175 weeks) after the last ocrelizumab infusion. Within 2.5 years after the last infusion, B-cell counts rose to either baseline or LLN in 90% of patients.
12.3 Pharmacokinetics
After subcutaneous administration of 920 mg ocrelizumab, the estimated mean exposure (AUC over the 24-week dosing interval) was 3730 µg/mL∙day. The mean Cmax was 132 µg/mL and tmax was reached after approximately 4 days (range 2 – 13 days). The estimated absolute bioavailability following subcutaneous administration was 81%.
In Study 4, the differences in pharmacokinetic exposures following the administration of OCREVUS ZUNOVO subcutaneously at 920 mg/23,000 units and ocrelizumab intravenously at 600 mg in MS patients were not clinically significant.
Pharmacokinetics (PK) of ocrelizumab in MS clinical studies fit a two-compartment model with time-dependent clearance.
Distribution
The population PK estimate of the central volume of distribution was 2.78 L. Peripheral volume and inter-compartment clearance were estimated at 2.68 L and 0.55 L/day, respectively.
Elimination
Constant clearance was estimated at 0.17 L/day, and initial time-dependent clearance at 0.05 L/day, which declined with a half-life of 33 weeks. The terminal elimination half-life was 20 days.
Metabolism
The metabolism of OCREVUS ZUNOVO has not been directly studied because antibodies are cleared principally by catabolism.
12.6 Immunogenicity
As with all therapeutic proteins, there is potential for immunogenicity. Immunogenicity data are highly dependent on the sensitivity and specificity of the test methods used. Additionally, the observed incidence of a positive result in a test method may be influenced by several factors, including sample handling, timing of sample collection, drug interference, concomitant medication, and the underlying disease. Therefore, comparison of the incidence of antibodies to OCREVUS ZUNOVO with the incidence of antibodies to other products may be misleading.
In Study 4, no patients tested positive for ocrelizumab anti-drug antibodies (ADAs) or anti-rHuPH20 (hyaluronidase [human recombinant]) antibodies.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
OCREVUS ZUNOVO contains ocrelizumab and hyaluronidase.
No carcinogenicity studies have been performed to assess the carcinogenic potential of ocrelizumab.
No studies have been performed to assess the mutagenic potential of ocrelizumab. As an antibody, ocrelizumab is not expected to interact directly with DNA.
No effects on reproductive organs were observed in male monkeys administered ocrelizumab by intravenous injection (three loading doses of 15 or 75 mg/kg, followed by weekly doses of 20 or 100 mg/kg) for 8 weeks. There were also no effects on estrus cycle in female monkeys administered ocrelizumab over three menstrual cycles using the same dosing regimen. The doses tested in monkey are 2 and 10 times the recommended human dose of 600 mg intravenous ocrelizumab, on a mg/kg basis.
Hyaluronidases are found in most tissues of the body. Long-term animal studies have not been performed to assess the carcinogenic or mutagenic potential of hyaluronidase. In addition, when subcutaneous hyaluronidase (recombinant human) was administered to cynomolgus monkeys for 39 weeks at dose levels up to 220,000 U/kg, which is > 570 times higher than the human dose, no evidence of toxicity to the male or female reproductive system was found through periodic monitoring of in-life parameters, e.g., semen analyses, hormone levels, menstrual cycles, and also from gross pathology, histopathology and organ weight data.
-
14 CLINICAL STUDIES
Studies 1-3 (described below), which established the effectiveness of ocrelizumab for the treatment of RMS and PPMS in adults, were conducted with intravenously-administered ocrelizumab. Study 4 demonstrated comparable exposure of OCREVUS ZUNOVO relative to the ocrelizumab intravenous formulation, which established the efficacy of OCREVUS ZUNOVO [see Clinical Pharmacology (12.3)].
14.1 Intravenous Ocrelizumab in Patients With Relapsing Forms of Multiple Sclerosis
The efficacy of intravenous ocrelizumab was demonstrated in two randomized, double-blind, double-dummy, active comparator-controlled clinical trials of identical design, in patients with relapsing forms of multiple sclerosis (RMS) treated for 96 weeks (Study 1; NCT01247324 and Study 2; NCT01412333). The dose of intravenous ocrelizumab was 600 mg every 24 weeks (initial treatment was given as two 300 mg IV infusions administered 2 weeks apart, and subsequent doses were administered as a single 600 mg IV infusion) and placebo subcutaneous injections were given 3 times per week. The dose of REBIF, the active comparator, was 44 mcg given as subcutaneous injections 3 times per week and placebo IV infusions were given every 24 weeks. Both studies included patients who had experienced at least one relapse within the prior year, or two relapses within the prior two years, and had an Expanded Disability Status Scale (EDSS) score from 0 to 5.5. Patients with primary progressive forms of multiple sclerosis (MS) were excluded. Neurological evaluations were performed every 12 weeks and at the time of a suspected relapse. Brain MRIs were performed at baseline and at Weeks 24, 48, and 96.
The primary outcome of both Study 1 and Study 2 was the annualized relapse rate (ARR). Additional outcome measures included the proportion of patients with confirmed disability progression, the mean number of MRI T1 gadolinium (Gd)-enhancing lesions at Weeks 24, 48, and 96, and new or enlarging MRI T2 hyperintense lesions. Progression of disability was defined as an increase of 1 point or more from the baseline EDSS score attributable to MS when the baseline EDSS score was 5.5 or less, or 0.5 points or more when the baseline EDSS score was above 5.5. Disability progression was considered confirmed when the increase in the EDSS was confirmed at a regularly scheduled visit 12 weeks after the initial documentation of neurological worsening. The primary population for analysis of confirmed disability progression was the pooled population from Studies 1 and 2.
In Study 1, 410 patients were randomized to intravenous ocrelizumab and 411 to REBIF; 11% of intravenous ocrelizumab-treated patients and 17% of REBIF-treated patients did not complete the 96-week double-blind treatment period. The baseline demographic and disease characteristics were balanced between the two treatment groups. At baseline, the mean age of patients was 37 years; 66% were female. The mean time from MS diagnosis to randomization was 3.8 years, the mean number of relapses in the previous year was 1.3, and the mean EDSS score was 2.8; 74% of patients had not been treated with a non-steroid therapy for MS in the 2 years prior to the study. At baseline, 40% of patients had one or more T1 Gd-enhancing lesions (mean 1.8).
In Study 2, 417 patients were randomized to intravenous ocrelizumab and 418 to REBIF; 14% of intravenous ocrelizumab-treated patients and 23% of REBIF-treated patients did not complete the 96-week double-blind treatment period. The baseline demographic and disease characteristics were balanced between the two treatment groups. At baseline, the mean age of patients was 37 years; 66% were female. The mean time from MS diagnosis to randomization was 4.1 years, the mean number of relapses in the previous year was 1.3, and the mean EDSS score was 2.8; 74% of patients had not been treated with a non-steroid therapy for MS in the 2 years prior to the study. At baseline, 40% of intravenous ocrelizumab-treated patients had one or more T1 Gd-enhancing lesions (mean 1.9).
In Study 1 and Study 2, intravenous ocrelizumab significantly lowered the annualized relapse rate and the proportion of patients with disability progression confirmed at 12 weeks after onset compared to REBIF. Results for Study 1 and Study 2 are presented in Table 3 and Figure 1.
Table 3 Key Clinical and MRI Endpoints in RMS Patients From Study 1 and Study 2 Endpoints Study 1 Study 2 Intravenous Ocrelizumab 600 mg REBIF 44 mcg three times a week Intravenous Ocrelizumab 600 mg REBIF 44 mcg three times a week every 24 weeks
N=410N=411 every 24 weeks
N=417N=418 - * Defined as an increase of 1.0 point or more from the baseline Expanded Disability Status Scale (EDSS) score for patients with baseline score of 5.5 or less, or 0.5 or more when the baseline score is greater than 5.5, Kaplan-Meier estimates at Week 96.
- † Data prospectively pooled from Study 1 and Study 2.
Clinical Endpoints Annualized Relapse Rate (Primary Endpoint) 0.156 0.292 0.155 0.290 Relative Reduction 46% (p<0.0001) 47% (p<0.0001) Proportion Relapse-free 83% 71% 82% 72% Proportion of Patients with 12-week Confirmed Disability Progression* 9.8% Intravenous Ocrelizumab vs 15.2% REBIF Risk Reduction (Pooled Analysis†) 40%; p=0.0006 MRI Endpoints Mean number of T1 Gd-enhancing lesions per MRI scan 0.016 0.286 0.021 0.416 Relative Reduction 94% (p<0.0001) 95% (p<0.0001) Mean number of new and/or enlarging T2 hyperintense lesions per MRI 0.323 1.413 0.325 1.904 Relative Reduction 77% (p<0.0001) 83% (p<0.0001) - * Pre-specified pooled analysis of Study 1 and 2
Figure 1 Kaplan-Meier Plot* of Time to Onset of Confirmed Disability Progression Sustained for at Least 12 Weeks With the Initial Event of Neurological Worsening Occurring During the Double-Blind Treatment Period in Pooled Studies 1 and 2 in Patients With RMS (Pooled ITT Population) 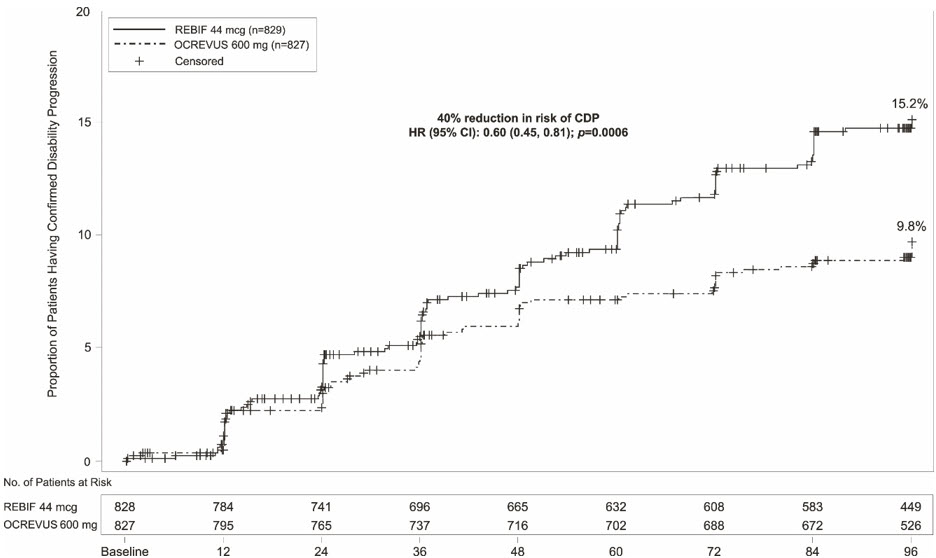
In exploratory subgroup analyses of Study 1 and Study 2, the effect of intravenous ocrelizumab on annualized relapse rate and disability progression was similar in male and female patients.
14.2 Intravenous Ocrelizumab in Patients With Primary Progressive Multiple Sclerosis
Study 3 was a randomized, double-blind, placebo-controlled clinical trial in patients with primary progressive multiple sclerosis (PPMS) (NCT01194570). Patients were randomized 2:1 to receive either intravenous ocrelizumab 600 mg or placebo as two 300 mg intravenous infusions 2 weeks apart every 24 weeks for at least 120 weeks. Selection criteria required a baseline EDSS of 3 to 6.5 and a score of 2 or greater for the EDSS pyramidal functional system due to lower extremity findings. Neurological assessments were conducted every 12 weeks. An MRI scan was obtained at baseline and at Weeks 24, 48, and 120.
In Study 3, the primary outcome was the time to onset of disability progression attributable to MS confirmed to be present at the next neurological assessment at least 12 weeks later. Disability progression occurred when the EDSS score increased by 1 point or more from the baseline EDSS if the baseline EDSS was 5.5 points or less, or by 0.5 points or more if the baseline EDSS was more than 5.5 points. In Study 3, confirmed disability progression also was deemed to have occurred if patients who had onset of disability progression discontinued participation in the study before the next assessment. Additional outcome measures included timed 25-foot walk, and percentage change in T2 hyperintense lesion volume.
Study 3 randomized 488 patients to intravenous ocrelizumab and 244 to placebo; 21% of intravenous ocrelizumab-treated patients and 34% of placebo-treated patients did not complete the trial. The baseline demographic and disease characteristics were balanced between the two treatment groups. At baseline, the mean age of patients was 45; 49% were female. The mean time since symptom onset was 6.7 years, the mean EDSS score was 4.7, and 26% had one or more T1 Gd-enhancing lesions at baseline; 88% of patients had not been treated previously with a non-steroid treatment for MS. The time to onset of disability progression confirmed at 12 weeks after onset was significantly longer for intravenous ocrelizumab-treated patients than for placebo-treated patients (see Figure 2). Results for Study 3 are presented in Table 4 and Figure 2.
Table 4 Key Clinical and MRI Endpoints in PPMS Patients for Study 3 Endpoints Study 3 Intravenous Ocrelizumab 600 mg
(two 300 mg infusions two weeks apart every 24 weeks)Placebo N=488 N=244 - * Defined as an increase of 1.0 point or more from the baseline EDSS score for patients with baseline score of 5.5 or less, or an increase of 0.5 or more when the baseline score is more than 5.5.
Clinical Outcomes Proportion of patients with 12-week Confirmed Disability Progression* 32.9% 39.3% Risk reduction 24%; p=0.0321 MRI Endpoints Mean change in volume of T2 lesions, from baseline to Week 120 (cm3) -0.39 0.79 p<0.0001 - * All patients in this analysis had a minimum of 120 weeks of follow-up. The primary analysis is based on all disability progression events accrued including 21 without confirmatory EDSS at 12 weeks.
Figure 2 Kaplan-Meier Plot of Time to Onset of Confirmed Disability Progression Sustained for at Least 12 Weeks With the Initial Event of Neurological Worsening Occurring During the Double-Blind Treatment Period in Study 3* 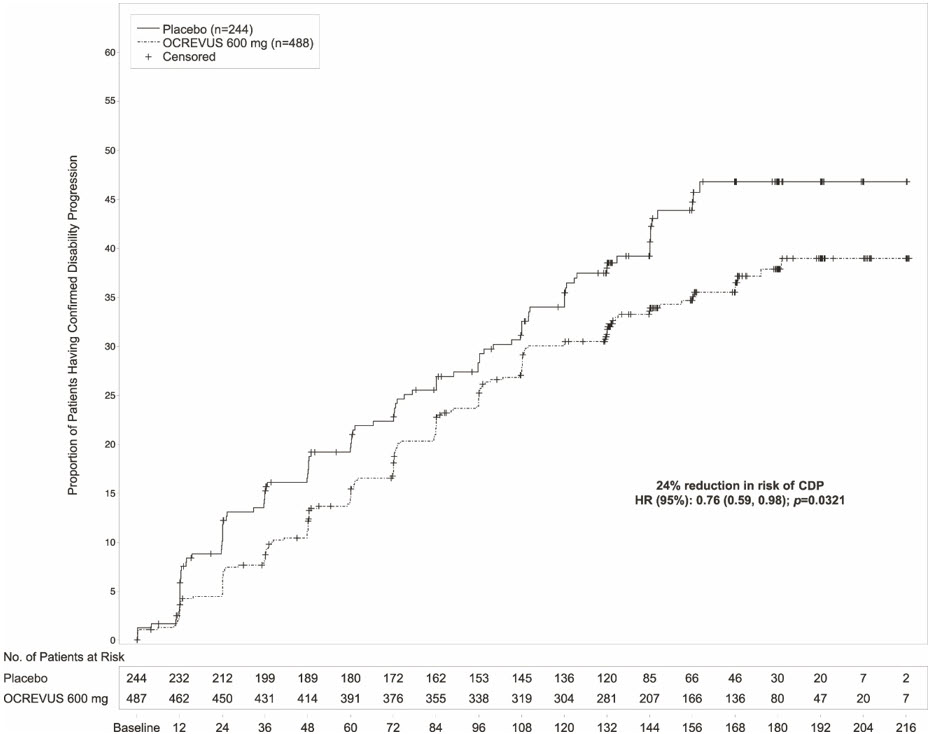
In the overall population in Study 3, the proportion of patients with 20 percent worsening of the timed 25-foot walk confirmed at 12 weeks was 49% in intravenous ocrelizumab-treated patients compared to 59% in placebo-treated patients (25% risk reduction).
In exploratory subgroup analyses of Study 3, the proportion of female patients with disability progression confirmed at 12 weeks after onset was similar in intravenous ocrelizumab-treated patients and placebo-treated patients (approximately 36% in each group). In male patients, the proportion of patients with disability progression confirmed at 12 weeks after onset was approximately 30% in intravenous ocrelizumab-treated patients and 43% in placebo-treated patients. Clinical and MRI endpoints that generally favored intravenous ocrelizumab numerically in the overall population, and that showed similar trends in both male and female patients, included annualized relapse rate, change in T2 lesion volume, and number of new or enlarging T2 lesions.
14.3 OCREVUS ZUNOVO in Patients With RMS or PPMS
Study 4 was a multicenter, randomized, open-label, parallel arm trial conducted to evaluate the comparative bioavailability, pharmacokinetics, pharmacodynamics, safety, and immunogenicity of OCREVUS ZUNOVO compared with intravenous ocrelizumab in patients with either RMS or PPMS (NCT05232825).
Study 4 enrolled 236 patients (213 with RMS, 23 with PPMS), 18-65 years of age with an EDSS between 0 to 6.5 at screening. The demographics were similar and baseline characteristics were balanced across the two treatment groups. The mean age was 40 years in both groups. In the OCREVUS ZUNOVO group, 35% of patients were male and the mean/median duration since MS diagnosis was 5.7/3.1 years, compared to 41% male and 4.8/2.4 years in the ocrelizumab IV group.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
OCREVUS ZUNOVO (ocrelizumab and hyaluronidase-ocsq) injection for subcutaneous use is a sterile, preservative-free, clear to slightly opalescent, and colorless to pale brown solution supplied as a carton containing one 920 mg and 23,000 units/23 mL (40 mg and 1,000 units/mL) single-dose vial (NDC: 50242-554-01).
Store OCREVUS ZUNOVO vials refrigerated at 2°C to 8°C (36°F to 46°F) in the original carton to protect from light. Do not freeze or shake.
If necessary, OCREVUS ZUNOVO can be removed and placed back into the refrigerator. Unopened OCREVUS ZUNOVO vials may be stored in the original carton for a cumulative time of up to 12 hours without refrigeration at a temperature up to 25°C (77°F).
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
Injection Reactions
Inform patients that the signs and symptoms of injection reactions can be local or systemic, and that injection reactions can occur up to 24 hours after injection. Advise patients to contact their healthcare provider immediately for signs or symptoms of injection reactions [see Warnings and Precautions (5.1)].
Infection
Advise patients to contact their healthcare provider for any signs of infection during treatment or after the last dose [see Clinical Pharmacology (12.2)]. Signs include fever, chills, constant cough, dysuria, or signs of herpes such as cold sores, shingles, or genital sores [see Warnings and Precautions (5.2)].
Advise patients that OCREVUS ZUNOVO may cause reactivation of hepatitis B infection and that monitoring will be required if they are at risk [see Warnings and Precautions (5.2)].
Advise patients that herpes infections, including serious herpes infections affecting the central nervous system, skin, and eyes, have occurred during treatment with ocrelizumab. Advise patients to promptly contact their healthcare provider if they experience any signs or symptoms of herpes infections including oral or genital symptoms, fever, skin rash, pain, itching, decreased visual acuity, eye redness, eye pain, headache, neck stiffness, or change in mental status [see Warnings and Precautions (5.2)].
Vaccination
Advise patients to complete any required live or live-attenuated vaccinations at least 4 weeks and, whenever possible, non-live vaccinations at least 2 weeks prior to initiation of ocrelizumab treatment. Administration of live-attenuated or live vaccines is not recommended during OCREVUS ZUNOVO treatment and until B-cell recovery [see Warnings and Precautions (5.2)].
Progressive Multifocal Leukoencephalopathy
Inform patients that PML has occurred in patients who received ocrelizumab, and may happen with OCREVUS ZUNOVO. Inform the patient that PML is characterized by a progression of deficits and usually leads to death or severe disability over weeks or months. Instruct the patient of the importance of contacting their healthcare provider if they develop any symptoms suggestive of PML. Inform the patient that typical symptoms associated with PML are diverse, progress over days to weeks, and include progressive weakness on one side of the body or clumsiness of limbs, disturbance of vision, and changes in thinking, memory, and orientation leading to confusion and personality changes [see Warnings and Precautions (5.3)].
Malignancies
Advise patients that an increased risk of malignancy, including breast cancer, may exist with OCREVUS ZUNOVO. Advise patients that they should follow standard breast cancer screening guidelines [see Warnings and Precautions (5.5)].
Immune-Mediated Colitis
Advise patients to promptly contact their healthcare provider if they experience any signs and symptoms of colitis, including diarrhea, abdominal pain, and blood in stool [see Warnings and Precautions (5.6)].
Liver Injury
Inform patients that liver injury has been reported with anti-CD20 B-cell depleting therapies, including ocrelizumab. Instruct patients treated with OCREVUS ZUNOVO to promptly report any symptoms that may indicate liver injury, including fatigue, anorexia, nausea, vomiting, right upper abdominal discomfort, dark urine, or jaundice. A blood test should be obtained before patients start therapy, and during treatment as clinically indicated [see Warnings and Precautions (5.7)].
Contraception
Females of childbearing potential should use effective contraception while receiving OCREVUS ZUNOVO and for 6 months after the last injection of OCREVUS ZUNOVO [see Clinical Pharmacology (12.3)]. Instruct patients that if they are pregnant or plan to become pregnant while taking OCREVUS ZUNOVO, they should inform their healthcare provider [see Use in Specific Populations (8.1)].
- SPL UNCLASSIFIED SECTION
-
MEDICATION GUIDE
This Medication Guide has been approved by the U.S. Food and Drug Administration Issued: 8/2025 MEDICATION GUIDE
OCREVUS ZUNOVO® (OH-creh-vus zoo-NOH-voh)
(ocrelizumab and hyaluronidase-ocsq)
injection, for subcutaneous useWhat is the most important information I should know about OCREVUS ZUNOVO?
OCREVUS ZUNOVO can cause serious side effects, including:- Injection reactions: Injection reactions are a common side effect of OCREVUS ZUNOVO, which can be serious and may require you to be hospitalized. You will be monitored for signs and symptoms of an injection reaction when you receive OCREVUS ZUNOVO. This will happen during all injections, for at least 1 hour after your first injection, and for at least 15 minutes after all injections following the first injection. Tell your healthcare provider or nurse if you get any of these symptoms:
- itchy skin
- rash
- hives
- tiredness
- coughing or wheezing
- trouble breathing
- throat irritation or pain
- feeling faint
- fever
- redness on your face (flushing)
- nausea
- headache
- swelling of the throat
- dizziness
- injection site pain, swelling or redness
- shortness of breath
- fatigue
- fast heart beat
These injection reactions can happen during or up to 24 hours after your injection. It is important that you call your healthcare provider right away if you get any of the signs or symptoms listed above after each injection. - Infection:
- Infections are a common side effect. OCREVUS ZUNOVO increases your risk of getting upper respiratory tract infections, lower respiratory tract infections, skin infections, and herpes infections. Serious infections can happen with OCREVUS ZUNOVO, which can be life-threatening or cause death. Tell your healthcare provider if you have an infection or have any of the following signs of infection including fever, chills, or a cough that does not go away, or painful urination. Signs of herpes infection include:
- cold sores
- shingles
- genital sores
- skin rash
- pain
- itching
Signs of a more serious herpes infection include: - changes in vision
- eye redness or eye pain
- severe or persistent headache
- stiff neck
- confusion
Signs of infection can happen during treatment or after you have received your last dose of OCREVUS ZUNOVO. Tell your healthcare provider right away if you have an infection. Your healthcare provider should delay your treatment with OCREVUS ZUNOVO until your infection is gone. - Hepatitis B virus (HBV) reactivation: Before starting treatment with ocrelizumab, your healthcare provider will do blood tests to check for hepatitis B viral infection. If you have ever had hepatitis B virus infection, the hepatitis B virus may become active again during or after treatment with OCREVUS ZUNOVO. Hepatitis B virus becoming active again (called reactivation) may cause serious liver problems including liver failure or death. Your healthcare provider will monitor you if you are at risk for hepatitis B virus reactivation during treatment and after you stop receiving OCREVUS ZUNOVO.
- Weakened immune system: OCREVUS ZUNOVO taken before or after other medicines that weaken the immune system could increase your risk of getting infections.
- Progressive Multifocal Leukoencephalopathy (PML): PML is a rare brain infection that usually leads to death or severe disability, and has been reported with ocrelizumab. Symptoms of PML get worse over days to weeks. It is important that you call your healthcare provider right away if you have any new or worsening neurologic signs or symptoms that have lasted several days, including problems with:
- thinking
- eyesight
- strength
- balance
- weakness on 1 side of your body
- using your arms or legs
- Decreased immunoglobulins: OCREVUS ZUNOVO may cause a decrease in some types of antibodies. Your healthcare provider will do blood tests to check your blood immunoglobulin levels.
See "What are the possible side effects of OCREVUS ZUNOVO?" for more information about side effects. What is OCREVUS ZUNOVO?
OCREVUS ZUNOVO is a prescription medicine used to treat:- relapsing forms of multiple sclerosis (MS), to include clinically isolated syndrome, relapsing-remitting disease, and active secondary progressive disease, in adults.
- primary progressive MS, in adults.
Who should not receive OCREVUS ZUNOVO?
Do not receive OCREVUS ZUNOVO if you:- have an active hepatitis B virus (HBV) infection.
- have had a life-threatening administration reaction to ocrelizumab.
- have had a life-threatening allergic reaction to ocrelizumab, hyaluronidase, or any of the ingredients of OCREVUS ZUNOVO. Tell your healthcare provider if you have had an allergic reaction to OCREVUS ZUNOVO or any of its ingredients in the past. See "What are the ingredients in OCREVUS ZUNOVO?" for a complete list of ingredients in OCREVUS ZUNOVO.
Before receiving OCREVUS ZUNOVO, tell your healthcare provider about all of your medical conditions, including if you: - have or think you have an infection. See "What is the most important information I should know about OCREVUS ZUNOVO?"
- have ever taken, take, or plan to take medicines that affect your immune system, or other treatments for MS. These medicines could increase your risk of getting an infection.
- have ever had hepatitis B or are a carrier of the hepatitis B virus.
- have a history of inflammatory bowel disease or colitis.
- have a history of liver problems.
- have had a recent vaccination or are scheduled to receive any vaccinations.
- You should receive any required 'live' or 'live-attenuated' vaccines at least 4 weeks before you start treatment with OCREVUS ZUNOVO. You should not receive 'live' or 'live-attenuated' vaccines while you are being treated with OCREVUS ZUNOVO and until your healthcare provider tells you that your immune system is no longer weakened.
- When possible, you should receive any 'non-live' vaccines at least 2 weeks before you start treatment with OCREVUS ZUNOVO. If you would like to receive any non-live (inactivated) vaccines, including the seasonal flu vaccine, while you are being treated with OCREVUS ZUNOVO, talk to your healthcare provider.
- If you have a baby and you received OCREVUS ZUNOVO during your pregnancy, it is important to tell your baby's healthcare provider about receiving OCREVUS ZUNOVO so they can decide when your baby should be vaccinated.
- are pregnant, think that you might be pregnant, or plan to become pregnant. It is not known if OCREVUS ZUNOVO will harm your unborn baby. You should use birth control (contraception) during treatment with OCREVUS ZUNOVO and for 6 months after your last injection of OCREVUS ZUNOVO. Talk with your healthcare provider about what birth control method is right for you during this time. Tell your healthcare provider if you become pregnant while receiving OCREVUS ZUNOVO.
- are breastfeeding or plan to breastfeed. It is not known if OCREVUS ZUNOVO passes into your breast milk. Talk to your healthcare provider about the best way to feed your baby if you take OCREVUS ZUNOVO.
How will I receive OCREVUS ZUNOVO? - OCREVUS ZUNOVO should be administered by a healthcare professional.
- OCREVUS ZUNOVO is given through an injection (subcutaneous injection) in your stomach.
- Before treatment with OCREVUS ZUNOVO, your healthcare provider will give you a corticosteroid medicine and an antihistamine to help reduce injection reactions (make them less frequent and less severe). You may also receive other medicines to help reduce injection reactions. See "What is the most important information I should know about OCREVUS ZUNOVO?"
- Each injection will last about 10 minutes and will be given every 6 months.
What are the possible side effects of OCREVUS ZUNOVO?
OCREVUS ZUNOVO may cause serious side effects, including:- see "What is the most important information I should know about OCREVUS ZUNOVO?"
- Risk of cancers (malignancies) including breast cancer: Follow your healthcare provider's instructions about standard screening guidelines for breast cancer.
-
Inflammation of the colon, or colitis: Tell your healthcare provider if you have any symptoms of colitis, such as:
- Diarrhea (loose stools) or more frequent bowel movements than usual
- Stools that are black, tarry, sticky or have blood or mucus
- Severe stomach-area (abdomen) pain or tenderness
-
Liver damage: OCREVUS ZUNOVO may cause liver damage. Your healthcare provider will do blood tests to check your liver before you start OCREVUS ZUNOVO and while you take OCREVUS ZUNOVO if needed. Tell your healthcare provider right away if you have any symptoms of liver damage, such as:
- yellowing of the skin and eyes (jaundice)
- nausea
- vomiting
- unusual darkening of the urine
- feeling tired or weak
- injection reactions
- respiratory tract infections
- skin infections
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.General information about the safe and effective use of OCREVUS ZUNOVO.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. You can ask your pharmacist or healthcare provider for information about OCREVUS ZUNOVO that is written for health professionals.What are the ingredients in OCREVUS ZUNOVO?
Active ingredient: ocrelizumab and hyaluronidase-ocsq.
Inactive ingredients: glacial acetic acid, methionine, polysorbate 20, sodium acetate, trehalose, and water for injection.
Manufactured by: Genentech, Inc., A Member of the Roche Group, 1 DNA Way, South San Francisco, CA 94080-4990
U.S. License No. 1048
For more information, go to www.OCREVUS.com or call 1-844-627-3887. -
PRINCIPAL DISPLAY PANEL - 23 mL Vial Carton
NDC: 50242-554-01
Ocrevus Zunovo®
(ocrelizumab and
hyaluronidase-ocsq)
Injection920 mg and
23,000 units/23 mL
(40 mg and 1,000 units/mL)For Subcutaneous Use Only.
For subcutaneous injection in the
abdomen over approximately 10 minutes.Single-Dose Vial.
Discard Unused Portion.Attention Pharmacist: Dispense the
accompanying Medication Guide to
each patient.1 vial
Rx only
Genentech11038285
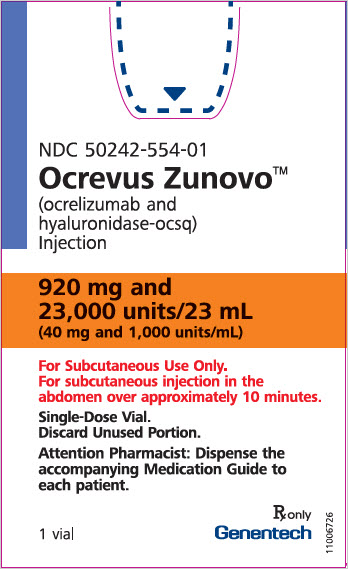
-
INGREDIENTS AND APPEARANCE
OCREVUS ZUNOVO
ocrelizumab and hyaluronidase injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 50242-554 Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength OCRELIZUMAB (UNII: A10SJL62JY) (OCRELIZUMAB - UNII:A10SJL62JY) OCRELIZUMAB 920 mg in 23 mL HYALURONIDASE (HUMAN RECOMBINANT) (UNII: 743QUY4VD8) (HYALURONIDASE (HUMAN RECOMBINANT) - UNII:743QUY4VD8) HYALURONIDASE (HUMAN RECOMBINANT) 23000 U in 23 mL Inactive Ingredients Ingredient Name Strength TREHALOSE DIHYDRATE (UNII: 7YIN7J07X4) 1889.5 mg in 23 mL ACETIC ACID (UNII: Q40Q9N063P) 5.5 mg in 23 mL METHIONINE (UNII: AE28F7PNPL) 34.3 mg in 23 mL POLYSORBATE 20 (UNII: 7T1F30V5YH) 13.8 mg in 23 mL SODIUM ACETATE (UNII: 4550K0SC9B) 30.2 mg in 23 mL WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 50242-554-01 1 in 1 CARTON 09/13/2024 1 23 mL in 1 VIAL, SINGLE-USE; Type 0: Not a Combination Product 2 NDC: 50242-554-86 1 in 1 CARTON 09/13/2024 2 23 mL in 1 VIAL, SINGLE-USE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA761371 09/13/2024 Labeler - Genentech, Inc. (080129000) Registrant - Genentech, Inc. (080129000) Establishment Name Address ID/FEI Business Operations Roche Diagnostics GmbH 315028860 ANALYSIS(50242-554) , MANUFACTURE(50242-554) , PACK(50242-554) Establishment Name Address ID/FEI Business Operations F. Hoffmann-La Roche AG 485244961 ANALYSIS(50242-554) , PACK(50242-554) , LABEL(50242-554) Establishment Name Address ID/FEI Business Operations Roche Singapore Technical Operations Pte. Ltd. 937189173 ANALYSIS(50242-554) , API MANUFACTURE(50242-554) Establishment Name Address ID/FEI Business Operations Genentech, Inc. (Oceanside) 146373191 ANALYSIS(50242-554) Establishment Name Address ID/FEI Business Operations Genentech, Inc. 080129000 ANALYSIS(50242-554) Establishment Name Address ID/FEI Business Operations Roche Diagnostics GmbH 323105205 ANALYSIS(50242-554)
Trademark Results [Ocrevus Zunovo]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 OCREVUS ZUNOVO 98182263 not registered Live/Pending |
Genentech, Inc. 2023-09-15 |
 OCREVUS ZUNOVO 97906638 not registered Live/Pending |
Genentech, Inc. 2023-04-25 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.