LEVONORGESTREL AND ETHINYL ESTRADIOL kit
Tyblume by
Drug Labeling and Warnings
Tyblume by is a Prescription medication manufactured, distributed, or labeled by Exeltis USA, Inc., Laboratorios Leon Farma S.A.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use LEVONORGESTREL AND ETHINYL ESTRADIOL TABLETS safely and effectively. See full prescribing information for LEVONORGESTREL AND ETHINYL ESTRADIOL TABLETS.
LEVONORGESTREL AND ETHINYL ESTRADIOL tablets, for oral use
Initial U.S. Approval: 1968 (norgestrel and ethinyl estradiol)WARNING: CIGARETTE SMOKING AND SERIOUS CARDIOVASCULAR EVENTS
See full prescribing information for complete boxed warning.
INDICATIONS AND USAGE
Levonorgestrel and Ethinyl Estradiol Tablets (LNG/EE Tablets) is a combination of levonorgestrel, a progestin, and ethinyl estradiol, an estrogen, indicated for use by females of reproductive potential to prevent pregnancy. (1)
DOSAGE AND ADMINISTRATION
- Take LNG/EE Tablets in one of two ways: (1) swallow whole on an empty stomach or (2) chew and then immediately swallow with a full glass of 240 mL water on an empty stomach. (2.1)
- Take one tablet daily for 28 consecutive days: one white active tablet daily during the first 21 consecutive days, followed by one peach inactive tablet daily during the 7 following days. (2)
DOSAGE FORMS AND STRENGTHS
A LNG/EE Tablets pack consists of 28 tablets: (3)
- 21 white tablets (active), each containing levonorgestrel 0.1 mg and ethinyl estradiol 0.02 mg.
- 7 peach-colored tablets (inactive placebo).
CONTRAINDICATIONS
- High risk of arterial or venous thrombotic diseases. (4)
- Breast cancer or other estrogen- or progestin-sensitive cancer. (4)
- Liver tumors, acute viral hepatitis or decompensated cirrhosis. (4)
- Undiagnosed abnormal uterine bleeding. (4)
- Use of Hepatitis C drug combinations containing ombitasvir/paritaprevir/ritonavir, with or without dasabuvir. (4)
WARNINGS AND PRECAUTIONS
- Vascular risks: Stop if a thrombotic or thromboembolic event occurs. Stop LNG/EE Tablets at least 4 weeks before and through 2 weeks after major surgery. Start no earlier than 4 weeks after delivery, in females who are not breast-feeding. Consider cardiovascular risk factors before initiating in all females, particularly those over 35 years. (5.1, 5.4)
- Liver disease: Discontinue LNG/EE Tablets if jaundice occurs. (5.2)
- Hypertension: If used in females with well-controlled hypertension, monitor blood pressure. Stop use of Levonorgestrel and Ethinyl Estradiol Tablets if blood pressure rises significantly. (5.3)
- Gallbladder disease: May cause or worsen gallbladder disease. (5.5)
- Adverse carbohydrate and lipid effect: Monitor glucose in prediabetic and diabetic females using LNG/EE Tablets. Consider an alternate contraceptive method for females with uncontrolled dyslipidemia. (5.6)
- Headache: Evaluate significant change in headaches and discontinue LNG/EE Tablets if indicated. (5.7)
- Uterine bleeding: May cause irregular bleeding or amenorrhea. Evaluate for other causes if symptoms persist. (5.8)
ADVERSE REACTIONS
Common adverse reactions are: headache, abdominal pain, nausea, metrorrhagia, vaginal moniliasis and pain, acne, and vaginitis. (6)
To report SUSPECTED ADVERSE REACTIONS, contact Exeltis USA, Inc. at 1-877-324-9349 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
Enzyme inducers (e.g., CYP3A4): May decrease the effectiveness of LNG/EE Tablets or increase breakthrough bleeding. Counsel patients to use a back-up or alternative method of contraception when enzyme inducers are used with LNG/EE Tablets. (7.1, 7.2)
USE IN SPECIFIC POPULATIONS
- Lactation: Advise use of another method; LNG/EE Tablets can decrease milk production. (8.2)
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 3/2020
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: CIGARETTE SMOKING AND SERIOUS CARDIOVASCULAR EVENTS
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Important Administration Instructions
2.2 Additional Administration Information
2.3 Missed Doses
2.4 Administration Recommendations after Vomiting or Acute Diarrhea
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Thromboembolic Disorders and Other Vascular Problems
5.2 Liver Disease
5.3 Hypertension
5.4 Age-related Considerations
5.5 Gallbladder Disease
5.6 Adverse Carbohydrate and Lipid Metabolic Effects
5.7 Headache
5.8 Bleeding Irregularities and Amenorrhea
5.9 Depression
5.10 Cervical Cancer
5.11 Effect on Binding Globulins
5.12 Hereditary Angioedema
5.13 Chloasma
5.14 Risk of Liver Enzyme Elevations with Concomitant Hepatitis C Treatment
6 ADVERSE REACTIONS
7 DRUG INTERACTIONS
7.1 Effects of Other Drugs on Combined Hormonal Contraceptives
7.2 Effects of Combined Hormonal Contraceptives on Other Drugs
7.3 Effect on Laboratory Tests
7.4 Concomitant Use with HCV Combination Therapy – Liver Enzyme Elevation
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Hepatic Impairment
8.7 Body Mass Indexes
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
16.2 Storage and Handling
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: CIGARETTE SMOKING AND SERIOUS CARDIOVASCULAR EVENTS
Cigarette smoking increases the risk of serious cardiovascular events from combined hormonal contraceptive (CHC) use. This risk increases with age, particularly in women over 35 years of age, and with the number of cigarettes smoked. For this reason, CHCs, including Levonorgestrel and Ethinyl Estradiol Tablets, are contraindicated in women who are over 35 years of age and smoke [see Contraindications (4) and Warnings and Precautions (5.1)].
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 Important Administration Instructions
Take Levonorgestrel and Ethinyl Estradiol Tablets (LNG/EE Tablets) in one of two ways: (1) swallow whole on an empty stomach or (2) chew and then immediately swallow with a full glass of 240 mL of water on an empty stomach [see Dosage and Administration (2.2)].
2.2 Additional Administration Information
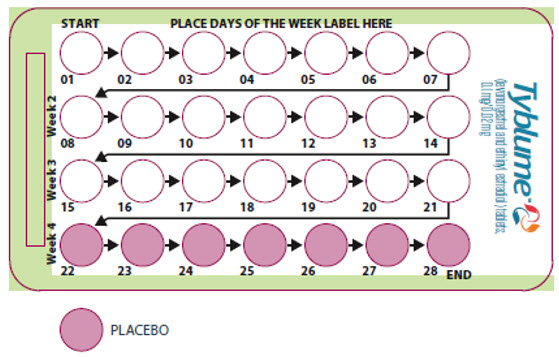
To achieve maximum contraceptive effectiveness, take LNG/EE Tablets exactly as directed (one tablet orally at the same time every day) and at intervals not exceeding 24 hours. The failure rate may increase when tablets are missed or taken incorrectly. The recommended dosage of LNG/EE Tablets is one tablet daily for 28 consecutive days: one white active tablet daily during the first 21 consecutive days, followed by one peach inactive tablet daily during the 7 following days (see Table 1).
Table 1 Instructions for Administration of LNG/EE Tablets Starting LNG/EE Tablets in females with no current use of hormonal contraception (start on Day 1 or Sunday) Day 1 start - Take first tablet without food (i.e. empty stomach) on the first day of menses
- Take subsequent tablets once daily at the same time each day
- Begin each subsequent 28-day pack on the same day of the week as the first cycle pack (i.e., on the day after taking the last tablet)
Sunday start - Take first tablet without food (i.e. empty stomach) on the first Sunday after the onset of menstrual period
- Take subsequent tablets once daily at the same time each day
- Use additional nonhormonal contraception for the first seven days of LNG/EE Tablets use
- Begin each subsequent 28-day pack on the same day of the week as the first cycle pack (i.e., on the day after taking the last tablet)
Switching to LNG/EE Tablets from another contraceptive method Start LNG/EE Tablets: - A combined oral contraceptive (COC)
- On the day when the new pack of the previous COC would have been started
- Transdermal system
- On the day when next application would have been scheduled
- Vaginal ring
- On the day when next insertion would have been scheduled
- Injection
- On the day when next injection would have been scheduled
- Intrauterine system
- On the day of removal
- Implant
- On the day of removal
Complete instructions to facilitate patient counseling on proper tablet usage are located in the FDA-Approved Patient Labeling (Instructions for Use). 2.3 Missed Doses
Instruct patients about the handling of missed doses (e.g., to take a missed tablet as soon as possible) and to follow the dosing instructions provided in the FDA-approved patient labeling (Instructions for Use).
Table 2 Instructions for Missed LNG/EE Tablets - If one white active tablet is missed in Weeks 1, 2, or 3
Take the missed active tablet as soon as possible, even if two active tablets are taken in one day. Continue taking one tablet a day until the pack is finished. - If two white active tablets are missed in Week 1 or Week 2
Take two active tablets as soon as possible. Then, take two active tablets the next day. This means taking 4 tablets in 2 days. Continue taking one tablet a day until the pack is finished. Additional nonhormonal contraception (such as condoms and spermicide) should be used as back-up if the patient has sex within 7 days after missing tablets. - If two white active tablets are missed in the third week or three or more active tablets are missed in a row in Weeks 1, 2, or 3
Day 1 start: Throw out the rest of the 28-day pack and start a new pack that same day.
Sunday start: Continue taking one tablet a day until Sunday, then throw out the rest of the pack and start a new pack that same day. Additional nonhormonal contraception (such as condoms and spermicide) should be used as back-up if the patient has sex within 7 days after missing tablets.- If one or more peach (inactive) tablets are missed in the fourth week
Throw away the missed inactive tablets. Keep taking one tablet each day until the pack is empty. Back-up nonhormonal birth-control method is not needed but take the next pack on time. 2.4 Administration Recommendations after Vomiting or Acute Diarrhea
If vomiting or acute diarrhea occurs within 3 to 4 hours after taking an active tablet, take the new active tablet (scheduled for the next day) as soon as possible. If more than two active tablets are missed, see the recommendations in Table 2 [see Dosage and Administration (2.3)].
-
3 DOSAGE FORMS AND STRENGTHS
One pack of Levonorgestrel and Ethinyl Estradiol Tablets consists of 28 tablets:
- 21 active tablets are white, round, and debossed with 30 on one side and L2 on the other side. Each active tablet contains levonorgestrel 0.1 mg and ethinyl estradiol 0.02 mg.
- 7 inactive tablets (placebo) are peach-colored, round, and debossed with 1 on one side and L2 on the other side.
-
4 CONTRAINDICATIONS
Levonorgestrel and Ethinyl Estradiol Tablets (LNG/EE Tablets) is contraindicated in females who are known to have the following conditions:
- A high risk of arterial or venous thrombotic diseases. Examples include females who are known to:
- – Smoke, if over age 35 [see Boxed Warning and Warnings and Precautions (5.1)]
- – Have current or history of deep vein thrombosis or pulmonary embolism [see Warnings and Precautions (5.1)]
- – Have cerebrovascular disease [see Warnings and Precautions (5.1)]
- – Have coronary artery disease [see Warnings and Precautions (5.1)]
- – Have thrombogenic valvular or thrombogenic rhythm diseases of the heart (for example, subacute bacterial endocarditis with valvular disease, or atrial fibrillation) [see Warnings and Precautions (5.1)]
- – Have inherited or acquired hypercoagulopathies [see Warnings and Precautions (5.1)]
- – Have uncontrolled hypertension or hypertension with vascular disease [see Warnings and Precautions (5.3)]
- – Have diabetes mellitus and are over age 35, diabetes mellitus with hypertension or vascular disease or other end-organ damage, or diabetes mellitus of > 20 years duration [see Warnings and Precautions (5.6)]
- – Have headaches with focal neurological symptoms, migraine headaches with aura, or over age 35 with any migraine headaches [see Warnings and Precautions (5.7)]
- Current or history of breast cancer or other estrogen- or progestin-sensitive cancer
- Liver tumors, acute viral hepatitis, or severe (decompensated) cirrhosis [see Warnings and Precautions (5.2)]
- Undiagnosed abnormal uterine bleeding [see Warnings and Precautions (5.8)]
- Use of hepatitis C drug combinations containing ombitasvir/paritaprevir/ritonavir, with or without dasabuvir, due to the potential for ALT elevations [see Warnings and Precautions (5.14)]
- A high risk of arterial or venous thrombotic diseases. Examples include females who are known to:
-
5 WARNINGS AND PRECAUTIONS
5.1 Thromboembolic Disorders and Other Vascular Problems
Before starting Levonorgestrel and Ethinyl Estradiol Tablets (LNG/EE Tablets) evaluate any past medical history or family history of thrombotic or thromboembolic disorders and consider whether the history suggests an inherited or acquired hypercoagulopathy. LNG/EE Tablets is contraindicated in females with a high risk of arterial or venous thrombotic/thromboembolic diseases [see Contraindications (4)].
- Stop Levonorgestrel and Ethinyl Estradiol Tablets (LNG/EE Tablets) if an arterial or venous thrombotic/thromboembolic event occurs.
- Stop LNG/EE Tablets if there is unexplained loss of vision, proptosis, diplopia, papilledema, or retinal vascular lesions and evaluate for retinal vein thrombosis immediately.
- Discontinue LNG/EE Tablets during prolonged immobilization. If feasible, stop LNG/EE Tablets at least four weeks before and through two weeks after major surgery, or other surgeries known to have an elevated risk of thromboembolism.
- Start LNG/EE Tablets no earlier than four weeks after delivery in females who are not breastfeeding. The risk of postpartum thromboembolism decreases after the third postpartum week, whereas the likelihood of ovulation increases after the third postpartum week.
Arterial Events
CHCs increase the risk of cardiovascular events and cerebrovascular events, such as myocardial infarction and stroke. The risk is greater among older women (> 35 years of age), smokers, and females with hypertension, dyslipidemia, diabetes, or obesity.
LNG/EE Tablets is contraindicated in women over 35 years of age who smoke [see Contraindications (4)]. Cigarette smoking increases the risk of serious cardiovascular events from CHC use. This risk increases with age, particularly in women over 35 years of age, and with the number of cigarettes smoked.
Venous Events
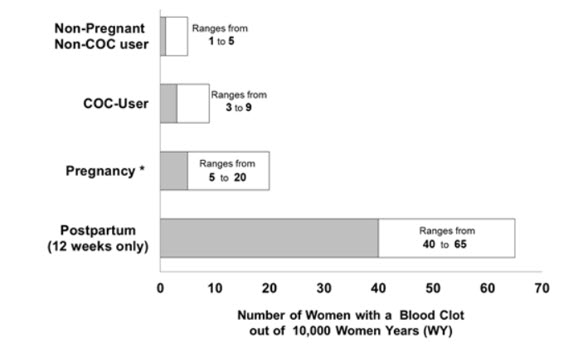
Use of CHCs increases the risk of venous thromboembolic events (VTEs), such as deep vein thrombosis and pulmonary embolism. Risk factors for VTEs include smoking, obesity, and family history of VTE, in addition to other factors that contraindicate use of CHCs [see Contraindications (4)]. While the increased risk of VTE associated with use of CHCs is well-established, the rates of VTE are even greater during pregnancy, and especially during the postpartum period (see Figure 1). The rate of VTE in females using COCs has been estimated to be 3 to 9 cases per 10,000 woman-years.
The risk of VTE is highest during the first year of use of a CHC and when restarting hormonal contraception after a break of four weeks or longer. Based on results from a few studies, there is some evidence that this is true for non-oral products as well. The risk of thromboembolic disease due to CHCs gradually disappears after CHC use is discontinued.
Figure 1 shows the risk of developing a VTE for females who are not pregnant and do not use oral contraceptives, for females who use oral contraceptives, for pregnant females, and for females in the postpartum period. To put the risk of developing a VTE into perspective: If 10,000 females who are not pregnant and do not use oral contraceptives are followed for one year, between 1 and 5 of these females will develop a VTE.
5.2 Liver Disease
Elevated Liver Enzymes
LNG/EE Tablets is contraindicated in females with acute viral hepatitis or severe (decompensated) cirrhosis of the liver [see Contraindications (4)]. Discontinue LNG/EE Tablets if jaundice develops. Acute liver test abnormalities may necessitate the discontinuation of CHC use until the liver tests return to normal and CHC causation has been excluded.
Liver Tumors
LNG/EE Tablets is contraindicated in females with benign or malignant liver tumors [see Contraindications (4)]. CHCs increase the risk of hepatic adenomas. An estimate of the attributable risk is 3.3 cases/100,000 CHC users. Rupture of hepatic adenomas may cause death from abdominal hemorrhage.
Studies have shown an increased risk of developing hepatocellular carcinoma in long-term (> 8 years) CHC users. The attributable risk of liver cancers in CHC users is less than one case per million users.
5.3 Hypertension
LNG/EE Tablets is contraindicated in females with uncontrolled hypertension or hypertension with vascular disease [see Contraindications (4)]. For all females, including those with well-controlled hypertension, monitor blood pressure at routine visits and stop LNG/EE Tablets if blood pressure rises significantly.
An increase in blood pressure has been reported in females using CHCs, and this increase is more likely in older women with extended duration of use. The effect of CHCs on blood pressure may vary according to the progestin in the CHC.
5.4 Age-related Considerations
The risk for cardiovascular disease and prevalence of risk factors for cardiovascular disease increase with age. Certain conditions, such as smoking and migraine headache without aura, that do not contraindicate CHC use in younger females, are contraindications to use in women over 35 years of age [see Contraindications (4) and Warnings and Precautions (5.1)]. Consider the presence of underlying risk factors that may increase the risk of cardiovascular disease or VTE, particularly before initiating a CHC for women over 35 years, such as:
- Hypertension
- Diabetes
- Dyslipidemia
- Obesity
5.5 Gallbladder Disease
Studies suggest an increased risk of developing gallbladder disease among CHC users. Use of CHCs may also worsen existing gallbladder disease.
A past history of CHC-related cholestasis predicts an increased risk with subsequent CHC use. Females with a history of pregnancy-related cholestasis may be at an increased risk for CHC related cholestasis.
5.6 Adverse Carbohydrate and Lipid Metabolic Effects
Hyperglycemia
LNG/EE Tablets is contraindicated in diabetic women over age 35, or females who have diabetes with hypertension, nephropathy, retinopathy, neuropathy, other vascular disease, or females with diabetes of > 20 years duration [see Contraindications (4)]. LNG/EE Tablets may decrease glucose tolerance. Carefully monitor prediabetic and diabetic females who are using LNG/EE Tablets.
Dyslipidemia
Consider alternative contraception for females with uncontrolled dyslipidemia. LNG/EE Tablets may cause adverse lipid changes.
Females with hypertriglyceridemia, or a family history thereof, may have an increase in serum triglyceride concentrations when using LNG/EE Tablets, which may increase the risk of pancreatitis.
5.7 Headache
LNG/EE Tablets is contraindicated in females who have headaches with focal neurological symptoms or have migraine headaches with aura, and in women over age 35 years who have migraine headaches with or without aura [see Contraindications (4)].
If a woman using LNG/EE Tablets develops new headaches that are recurrent, persistent, or severe, evaluate the cause and discontinue LNG/EE Tablets if indicated. Consider discontinuation of LNG/EE Tablets if there is an increased frequency or severity of migraines during CHC use (which may be prodromal of a cerebrovascular event).
5.8 Bleeding Irregularities and Amenorrhea
Unscheduled Bleeding and Spotting
Females using LNG/EE Tablets may experience unscheduled (breakthrough or intracyclic) bleeding and spotting, especially during the first three months of use. Bleeding irregularities may resolve over time or by changing to a different contraceptive product. If bleeding persists or occurs after previously regular cycles, evaluate for causes such as pregnancy or malignancy.
Amenorrhea and Oligomenorrhea
Females who use LNG/EE Tablets may experience absence of scheduled (withdrawal) bleeding, even if they are not pregnant.
If scheduled bleeding does not occur, consider the possibility of pregnancy. If the patient has not adhered to the prescribed dosing schedule (missed one or two active tablets or started taking them on a day later than she should have), consider the possibility of pregnancy at the time of the first missed period and perform appropriate diagnostic measures. If the patient has adhered to the prescribed dosing schedule and misses two consecutive periods, rule out pregnancy.
After discontinuation of a CHC, amenorrhea or oligomenorrhea may occur, especially if these conditions were pre-existent.
5.9 Depression
Carefully observe females with a history of depression and discontinue LNG/EE Tablets if depression recurs to a serious degree. Data on the association of CHCs with onset of depression or exacerbation of existing depression are limited.
5.10 Cervical Cancer
Some studies suggest that CHCs are associated with an increase in the risk of cervical cancer or intraepithelial neoplasia. There is controversy about the extent to which these findings are due to differences in sexual behavior and other factors.
5.11 Effect on Binding Globulins
The estrogen component of LNG/EE Tablets may raise the serum concentrations of thyroxine-binding globulin, sex hormone-binding globulin, and cortisol-binding globulin. The dose of replacement thyroid hormone or cortisol therapy may need to be increased.
5.12 Hereditary Angioedema
In females with hereditary angioedema, exogenous estrogens may induce or exacerbate symptoms of angioedema.
5.13 Chloasma
Chloasma may occur with LNG/EE Tablets use, especially in females with a history of chloasma gravidarum. Advise females with a history of chloasma to avoid exposure to the sun or ultraviolet radiation while using LNG/EE Tablets.
5.14 Risk of Liver Enzyme Elevations with Concomitant Hepatitis C Treatment
During clinical trials with the Hepatitis C combination drug regimen that contains ombitasvir/paritaprevir/ritonavir, with or without dasabuvir, ALT elevations greater than 5 times the upper limit of normal (ULN), including some cases greater than 20 times the ULN, were significantly more frequent in women using ethinyl estradiol-containing medications, such as COCs. COCs are contraindicated for use with Hepatitis C drug combinations containing ombitasvir/paritaprevir/ritonavir, with or without dasabuvir [see Contraindications (4)]. Discontinue LNG/EE Tablets prior to starting therapy with the combination drug regimen ombitasvir/paritaprevir/ritonavir, with or without dasabuvir.
LNG/EE Tablets can be restarted approximately 2 weeks following completion of treatment with the Hepatitis C combination drug regimen.
-
6 ADVERSE REACTIONS
The following serious adverse reactions with the use of CHCs are discussed elsewhere in labeling:
- Serious cardiovascular events [see Boxed Warning and Warnings and Precautions (5.1 and 5.4)]
- Vascular events [see Warnings and Precautions (5.1)]
- Liver disease [see Warnings and Precautions (5.2)]
- Hypertension [see Warnings and Precautions (5.3)]
- Gallbladder disease [see Warnings and Precautions (5.5)]
- Adverse carbohydrate and lipid metabolic effects [see Warnings and Precautions (5.6)]
- Headache [see Warnings and Precautions (5.7)]
- Bleeding irregularities and amenorrhea [see Warnings and Precautions (5.8)]
- Depression [see Warnings and Precautions (5.9)]
- Cervical cancer [see Warnings and Precautions (5.10)]
- Effect on binding globulins [see Warnings and Precautions (5.11)]
- Hereditary angioedema [see Warnings and Precautions (5.12)]
- Chloasma [see Warnings and Precautions (5.13)]
- Risk of liver enzyme elevations with concomitant hepatitis C treatment [see Warnings and Precautions (5.14)]
The following adverse reactions associated with the use of oral CHCs were identified in clinical studies or postmarketing reports. Because some of these reactions were reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Common adverse reactions associated with oral CHCs are headache, abdominal pain, nausea, metrorrhagia, vaginal moniliasis and pain, acne, and vaginitis.
Additional adverse reactions that have been reported include the following:
Eye disorder: intolerance to contact lenses, steepening of corneal curvature
Gastrointestinal disorders: Abdominal bloating, vomiting
General disorders and administration site condition: Edema, fluid retention
Hepatobiliary disorders: Cholestatic jaundice
Psychiatric disorders: Change in libido, mood changes
Reproductive system and breast disorders: Amenorrhea, breast tenderness, breast pain, breast enlargement, increased cervical mucous, change in menstrual flow, unscheduled bleeding
Skin and subcutaneous tissue disorders: Acne, melasma [see Warnings and Precautions (5.13)]
Vascular disorders: Budd-Chiari syndrome, aggravation of varicose veins
-
7 DRUG INTERACTIONS
The sections below provide information on substances for which data on drug interactions with CHCs are available. There is little information available about the clinical effect of most drug interactions that may affect CHCs. However, based on the known pharmacokinetic effects of these drugs, clinical strategies to minimize any potential adverse effect on contraceptive effectiveness or safety are suggested.
Consult the approved product labeling of all concurrently used drugs to obtain further information about interactions with CHCs or the potential for metabolic enzyme or transporter system alterations.
No drug-drug interaction studies were conducted with LNG/EE Tablets.
7.1 Effects of Other Drugs on Combined Hormonal Contraceptives
Substances decreasing the Plasma Concentration of CHCs and Potentially Diminishing the Efficacy of CHCs
Table 3 Significant Drug Interactions Involving Substances That Affect CHCs a Induction potency of St. John's wort may vary widely based on preparation. Metabolic Enzyme Inducers Clinical effect - Concomitant use of CHCs with metabolic enzyme inducers may decrease the plasma concentrations of the estrogen and/or progestin component of CHCs [see Clinical Pharmacology (12.3)].
- Decreased exposure of the estrogen and/or progestin component of CHCs may potentially diminish the effectiveness of CHCs and may lead to contraceptive failure or an increase in breakthrough bleeding.
Prevention or management - Counsel females to use an alternative method of contraception or a backup method when enzyme inducers are used with CHCs.
- Continue backup contraception for 28 days after discontinuing the enzyme inducer to maintain contraceptive reliability.
Examples Aprepitant, barbiturates, bosentan, carbamazepine, efavirenz, felbamate, griseofulvin, oxcarbazepine, phenytoin, rifampin, primidone, phenylbutazone, rifabutin, rufinamide, topiramate, products containing St. John's wort, and certain protease inhibitors (see separate section on protease inhibitors below). Colesevelam Clinical effect - Concomitant use of CHCs with colesevelam significantly decreases systemic exposure of ethinyl estradiol [see Clinical Pharmacology (12.3)].
- Decreased exposure of the estrogen component of CHCs may potentially reduce contraceptive efficacy or result in an increase in breakthrough bleeding, depending on the strength of ethinyl estradiol in the CHC.
Prevention or management Administer 4 or more hours apart to attenuate this drug interaction. Substances increasing the systemic exposure of CHCs:
Co-administration of atorvastatin or rosuvastatin and CHCs containing ethinyl estradiol increase systemic exposure of ethinyl estradiol by approximately 20 to 25 percent. Ascorbic acid and acetaminophen may increase systemic exposure of ethinyl estradiol, possibly by inhibition of conjugation. CYP3A inhibitors such as itraconazole, voriconazole, fluconazole, grapefruit juice1, or ketoconazole may increase systemic exposure of the estrogen and/or progestin component of CHCs.
- 1 The effect of grapefruit juice on CYP3A4 enzymes (e.g., strong vs. moderate inhibition) depends on its brand, concentration, and preparation.
Human immunodeficiency virus (HIV)/hepatitis C virus (HCV) protease inhibitors and non-nucleoside reverse transcriptase inhibitors:
Significant decreases in systemic exposure of the estrogen and/or progestin have been noted when CHCs are co-administered with some HIV protease inhibitors (e.g., nelfinavir, ritonavir, darunavir/ritonavir, (fos)amprenavir/ritonavir, lopinavir/ritonavir, and tipranavir/ritonavir), some HCV protease inhibitors (e.g., boceprevir and telaprevir), and some non-nucleoside reverse transcriptase inhibitors (e.g., nevirapine).
In contrast, significant increases in systemic exposure of the estrogen and/or progestin have been noted when CHCs are co-administered with certain other HIV protease inhibitors (e.g., indinavir and atazanavir/ritonavir) and with other non-nucleoside reverse transcriptase inhibitors (e.g., etravirine).
7.2 Effects of Combined Hormonal Contraceptives on Other Drugs
Table 4 provides significant drug interaction information for drugs co-administered with LNG/EE Tablets.
Table 4 Significant Drug Interaction Information for Drugs Co-Administered with CHCs Lamotrigine Clinical effect - Concomitant use of CHCs with lamotrigine may significantly decrease systemic exposure of lamotrigine due to induction of lamotrigine glucuronidation [see Clinical Pharmacology (12.3)].
- Decreased systemic exposure of lamotrigine may reduce seizure control.
Prevention or management Dose adjustment may be necessary. Consult the approved product labeling for lamotrigine. Thyroid Hormone Replacement Therapy or Corticosteroid Replacement Therapy Clinical effect Concomitant use of CHCs with thyroid hormone replacement therapy or corticosteroid replacement therapy may increase systemic exposure of thyroid-binding and cortisol-binding globulin [see Warnings and Precautions (5.11)]. Prevention or management The dose of replacement thyroid hormone or cortisol therapy may need to be increased. Consult the approved product labeling for the therapy in use. [See Warnings and Precautions (5.11)]. Other Drugs Clinical effect Concomitant use of CHCs may decrease systemic exposure of acetaminophen, morphine, salicylic acid, and temazepam. Concomitant use with ethinyl estradiol-containing CHCs may increase systemic exposure of other drugs (e.g., cyclosporine, prednisolone, theophylline, tizanidine, and voriconazole). Prevention or management The dosage of drugs that can be affected by this interaction may need to be increased. Consult the approved product labeling for the concomitantly used drug. 7.3 Effect on Laboratory Tests
The use of CHCs may influence the results of certain laboratory tests, such as coagulation factors, lipids, glucose tolerance, and binding proteins.
7.4 Concomitant Use with HCV Combination Therapy – Liver Enzyme Elevation
CHCs are contraindicated for use with Hepatitis C drug combinations containing ombitasvir/paritaprevir/ritonavir, with or without dasabuvir [see Contraindications (4)]. Discontinue LNG/EE Tablets prior to starting therapy with the combination drug regimen ombitasvir/paritaprevir/ritonavir, with or without dasabuvir. LNG/EE Tablets can be restarted approximately 2 weeks following completion of treatment with the Hepatitis C combination drug regimen.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There is no use for contraception in pregnancy; therefore, LNG/EE Tablets should be discontinued during pregnancy. Epidemiologic studies and meta-analyses have not found an increased risk of genital or nongenital birth defects (including cardiac anomalies and limb-reduction defects) following exposure to CHCs before conception or during early pregnancy.
In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4 percent and 15 to 20 percent, respectively.
8.2 Lactation
Risk Summary
Contraceptive hormones and/or metabolites are present in human milk. CHCs can reduce milk production in breast-feeding females. This reduction can occur at any time but is less likely to occur once breast-feeding is well established. When possible, advise the nursing female to use other methods of contraception until she discontinues breast-feeding [see Dosage and Administration (2.2)]. The developmental and health benefits of breast-feeding should be considered along with the mother's clinical need for LNG/EE Tablets and any potential adverse effects on the breast-fed child from LNG/EE Tablets or from the underlying maternal condition.
Data
Small amounts of oral-contraceptive steroids and/or metabolites have been identified in the milk of nursing mothers, and a few adverse effects on the child have been reported, including jaundice and breast enlargement. In addition, combination oral contraceptives given in the postpartum period may interfere with lactation by decreasing the quantity and quality of breast milk.
8.4 Pediatric Use
The safety and effectiveness of LNG/EE Tablets have been established in females of reproductive potential. Efficacy is expected to be the same for post-menarchal females under the age of 17 as for users 17 years and older. The use of LNG/EE Tablets before menarche is not indicated.
8.5 Geriatric Use
LNG/EE Tablets has not been studied in postmenopausal women and is not indicated in this population.
8.6 Hepatic Impairment
The pharmacokinetics of LNG/EE Tablets have not been studied in women with hepatic impairment. However, steroid hormones may be poorly metabolized in patients with hepatic impairment. Acute or chronic disturbances of liver function may necessitate the discontinuation of COC use until markers of liver function return to normal and COC causation has been excluded [see Contraindications (4) and Warnings and Precautions (5.2)].
- 10 OVERDOSAGE
-
11 DESCRIPTION
Levonorgestrel and Ethinyl Estradiol Tablets is an oral contraceptive product. A LNG/EE Tablets pack consists of 21 white active tablets and 7 peach-colored inactive tablets.
The twenty-one white active tablets each contain 0.1 mg of levonorgestrel, a progestin, and 0.02 mg of ethinyl estradiol, an estrogen. Each tablet also contains the following inactive ingredients: corn starch, crospovidone, lactose monohydrate, magnesium stearate, povidone, and pregelatinized starch.
Seven peach-colored inactive tablets, each contains anhydrous lactose, corn starch, crospovidone, D&C yellow No. 10 aluminum lake, FD&C Red No. 40 aluminum lake, magnesium stearate, and povidone.
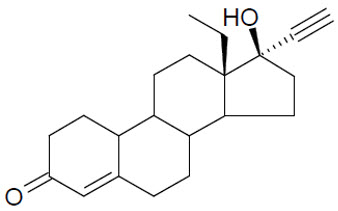
The chemical name for levonorgestrel is [18,19-Dinorpregn-4-en-20-yn-3-one, 13-ethyl-17-hydroxy-, (17α)-(-)-]. It has the molecular formula of C21H28O2, the molecular weight of 312.5, and the structural formula is provided below:
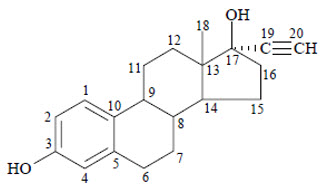
The chemical name for ethinyl estradiol is [19-norpregna-1,3,5(10)-trien-20-yne-3,17-diol, (17α)-]. It has the molecular formula of C20H24O2, the molecular weight of 296.4, and the structural formula is provided below:
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
CHCs lower the risk of becoming pregnant primarily by suppressing ovulation.
12.3 Pharmacokinetics
Absorption
No specific investigation of the absolute bioavailability of LNG/EE Tablets in humans has been conducted. However, literature indicates that levonorgestrel is rapidly and completely absorbed after oral administration (bioavailability about 100%) and is not subject to first-pass metabolism. Ethinyl estradiol is rapidly and almost completely absorbed from the gastrointestinal tract but, due to first-pass metabolism in gut mucosa and liver, the bioavailability of ethinyl estradiol is between 38% and 48%.
The kinetics of total levonorgestrel are non-linear due to an increase in binding of levonorgestrel to sex hormone binding globulin (SHBG), which is attributed to increased SHBG levels that are induced by the daily administration of ethinyl estradiol.
Table 5 provides a summary of pharmacokinetics of levonorgestrel and ethinyl estradiol after a single dose of LNG/EE Tablets in 32 female subjects only under fasting condition.
Table 5 Summary Mean (CV%) Pharmacokinetic Parameters from Single Dose Administration of LNG/EE Tablets Analyte Sample Size Cmax
(pg/mL)Tmax
(h)*AUC0-T
(pg*h/mL)AUC0-∞
(pg*h/mL)T1/2
(h)- * Median (min – max)
- † n = 30 for AUC0-∞ and T1/2
EE n = 32 53.22 (33.9) 1.50 (1.00-2.25) 477.75 (32.5) 515.51 (31.0) 16.42 (25.0) LNG n = 32† 3225.0 (33.1) 0.75 (0.50-1.00) 27586.0 (39.0) 34099.0 (36.8) 33.67 (31.8) Distribution
Levonorgestrel in serum is primarily bound to SHBG. Ethinyl estradiol is about 97% bound to plasma albumin. Ethinyl estradiol does not bind to SHBG, but induces SHBG synthesis.
Elimination
Metabolism
Levonorgestrel: The most important metabolic pathway occurs in the reduction of the Δ4-3-oxo group and hydroxylation at positions 2α, 1β, and 16β, followed by conjugation. Most of the metabolites that circulate in the blood are sulfates of 3α,5β-tetrahydro-levonorgestrel, while excretion occurs predominantly in the form of glucuronides. Some of the parent levonorgestrel also circulates as 17β-sulfate. Metabolic clearance rates may differ among individuals by several-fold, and this may account in part for the wide variation observed in levonorgestrel concentrations among users.
Ethinyl estradiol: Cytochrome P450 enzymes (CYP3A4) in the liver are responsible for the 2-hydroxylation that is the major oxidative reaction. The 2-hydroxy metabolite is further transformed by methylation and glucuronidation prior to urinary and fecal excretion. Levels of Cytochrome P450 (CYP3A) vary widely among individuals and can explain the variation in rates of ethinyl estradiol 2-hydroxylation. Ethinyl estradiol is excreted in the urine and feces as glucuronide and sulfate conjugates, and undergoes enterohepatic circulation.
Excretion
The elimination half-life for levonorgestrel is approximately 36 ± 13 hours at steady state. Levonorgestrel and its metabolites are primarily excreted in the urine (40% to 68%) and about 16% to 48% are excreted in feces. The elimination half-life of ethinyl estradiol is 18 ± 4.7 hours at steady state.
- 13 NONCLINICAL TOXICOLOGY
-
14 CLINICAL STUDIES
In a clinical trial with Levonorgestrel and Ethinyl Estradiol Tablets (LNG/EE Tablets) (0.1 mg and 0.02 mg, respectively), 1,477 subjects had 7,720 cycles of use and a total of 5 pregnancies were reported. This represented an overall pregnancy rate of 0.84 per 100 woman-years. These data included patients who did not take LNG/EE Tablets correctly. One or more tablets were missed during 1,479 (19%) of the 7,870 cycles; thus all tablets were taken during 6,391 (81%) of the 7,870 cycles. Of the total 7,870 cycles, a total of 150 cycles were excluded from the calculation of the Pearl Index due to the use of backup contraception and/or missing 3 or more consecutive tablets.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
Levonorgestrel and Ethinyl Estradiol Tablets are available as follows:
Each blister card contains 28 tablets in the following order: 21 active tablets and 7 inactive tablets. The 21 active tablets are white, round, and debossed with 30 on one side and L2 on the other side; each contains levonorgestrel 0.1 mg and ethinyl estradiol 0.02 mg. The 7 inactive tablets (placebo) are peach-colored, round, and debossed with 1 on one side and L2 on the other side.
- NDC: 0642-7471-01, one carton containing 1 individual blister card
- NDC: 0642-7471-03, one carton containing 3 individual blister cards
- NDC: 0642-7471-06, one carton containing 6 individual blister cards
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information and Instructions for Use).
Cigarette Smoking
Advise women that cigarette smoking increases the risk of serious cardiovascular events from CHC use, and that women who are over 35 years old and smoke should not use LNG/EE Tablets [see Boxed Warning and Warning and Precautions (5.1)].
Venous Thromboembolism
Advise women that the increased risk of VTE compared to non-users of CHCs is greatest after initially starting a CHC or restarting (following a 4-week or greater tablet-free interval) the same or a different CHC [see Warnings and Precautions (5.1)].
Use During Pregnancy
Advise women that there is no reason to use LNG/EE Tablets during pregnancy. Instruct the woman to stop LNG/EE Tablets if pregnancy is confirmed during treatment [see Use in Specific Populations (8.1)].
Sexually Transmitted Infections
Advise women that LNG/EE Tablets does not protect against HIV-infection (AIDS) and other sexually transmitted infections.
Dosing, Administration and Missed Dose Instructions
Advise women to take LNG/EE Tablets in one of two ways: (1) swallow whole on an empty stomach or (2) chew and then immediately swallow with a full glass of 240 mL water on an empty stomach. Advise women to take one tablet daily by mouth at the same time every day [see Dosage and Administration (2.1)].
Advise women about what to do in the event tablets are missed. See "What should I do if I miss any LNG/EE Tablets" section in FDA-approved patient labeling [see Dosage and Administration (2.3)].
Need for Additional Contraception
- Advise women to use a back-up or alternative method of contraception when enzyme inducers are used with LNG/EE Tablets [see Drug Interactions (7.1)].
- Advise a woman who starts CHCs postpartum and has not yet had a period that she should use an additional method of contraception until she has taken a white tablet for 7 consecutive days.
Lactation
CHCs may reduce breast milk production; this is less likely to occur if breastfeeding is well established [see Use in Specific Populations (8.2)].
Amenorrhea and Possible Symptoms of Pregnancy
Advise women that amenorrhea may occur. Advise women to contact their health care provider in the event of amenorrhea in two or more consecutive cycles or in case of symptoms of pregnancy such as morning sickness or unusual breast tenderness [see Warnings and Precautions (5.8)].
Bleeding Irregularities
Advise women that irregular bleeding and/or spotting may occur. Bleeding irregularities typically resolve after the first few months of use. Advise women to consult their healthcare provider if bleeding irregularities persist for more than three to four months [see Warnings and Precautions (5.8)].
- SPL UNCLASSIFIED SECTION
-
PATIENT PACKAGE INSERT
This Patient Information has been approved by the U.S. Food and Drug Administration. Revised: March 2020 PATIENT INFORMATION
TYBLUME [tye bloom]
(levonorgestrel and ethinyl estradiol tablets) for oral useWhat is the most important information I should know about TYBLUME (a type of birth control pill)?
Do not use TYBLUME if you smoke cigarettes and are over 35 years old. Smoking increases your risk of serious cardiovascular side effects (heart and blood vessel problems) from birth control, including death from heart attack, blood clots or stroke. This risk increases with age and the number of cigarettes you smoke.What is TYBLUME? - TYBLUME is a birth control pill (oral contraceptive) used by women to prevent pregnancy.
- TYBLUME does not protect against HIV infections (AIDS) and other sexually transmitted infections.
How does TYBLUME work for contraception?
Your chance of getting pregnant depends on how well you follow the directions for taking your birth control pills. The better you follow the directions, the less chance you have of getting pregnant.
Based on the results of one clinical study of a 28-day regimen of levonorgestrel 0.1mg/ethinyl estradiol 0.02 mg tablets, about 1 out of 100 women may get pregnant within the first year they use TYBLUME.
The following chart shows the chance of getting pregnant for women who use different methods of birth control. Each box on the chart contains a list of birth control methods that are similar in effectiveness. The most effective methods are at the top of the chart. The box on the bottom of the chart shows the chance of getting pregnant for women who do not use birth control and are trying to get pregnant.
Do not take TYBLUME if you: - smoke and are over 35 years of age.
- have or have had blood clots in your arms, legs, lungs, or eyes.
- have a problem with your blood that makes it clot more than normal.
- have certain heart valve problems or an irregular heartbeat that increases your risk of having blood clots.
- had a stroke.
- had a heart attack.
- have high blood pressure that cannot be controlled by medicine or have high blood pressure with blood vessel problems.
- have diabetes and are over 35 years of age; have diabetes with high blood pressure, blood vessel problems, or kidney, eye, nerve, or blood vessel damage; or have had diabetes for more than 20 years.
- have certain kinds of severe migraine headaches with aura, numbness, weakness or changes in vision, or any migraine headaches if you are over 35 years of age.
- have liver problems, including liver tumors.
- have any unexplained vaginal bleeding.
- have or have had breast cancer or any cancer that is sensitive to female hormones.
- take any Hepatitis C drug combination containing ombitasvir/paritaprevir/ritonavir, with or without dasabuvir. This may increase levels of the liver enzyme "alanine aminotransferase" (ALT) in the blood.
Before you take TYBLUME, tell your healthcare provider about all of your medical conditions, including if you: - are scheduled for surgery. TYBLUME may increase your risk of blood clots after surgery. You should stop taking TYBLUME at least 4 weeks before you have surgery and not restart TYBLUME until at least 2 weeks after your surgery.
- are pregnant or think you may be pregnant.
- are depressed now or have been depressed in the past.
- had yellowing of your skin or eyes (jaundice) caused by pregnancy (cholestasis of pregnancy).
- are breastfeeding or plan to breastfeed. TYBLUME may decrease the amount of breast milk you make. A small amount of the hormones in TYBLUME may pass into your breast milk. Talk to your healthcare provider about the best birth control method for you while breastfeeding.
TYBLUME may affect the way other medicines work, and other medicines may affect how well TYBLUME works.
Women on thyroid replacement therapy or steroid therapy may need increased doses of thyroid hormone or steroid medicines.
Know the medicines you take. Keep a list of them to show your healthcare provider and pharmacist when you get a new medicine.How should I take TYBLUME? - Read the detailed Instructions for Use at the end of this Patient Information leaflet about the right way to take TYBLUME.
- Take TYBLUME exactly as your healthcare provider tells you to take it.
- You may take TYBLUME 1 of 2 ways:
- Chew TYBLUME and then swallow TYBLUME with a full 8 oz (240 mL) glass of water right away, or
- Swallow TYBLUME whole.
- Take TYBLUME on an empty stomach.
What are the possible side effects of TYBLUME?
TYBLUME may cause serious side effects, including:-
blood clots in your lungs, heart attack, or a stroke that may lead to death. Some other examples of serious blood clots include blood clots in the legs or eyes. Serious blood clots can happen especially if you smoke, are obese, or are older than 35 years of age. Serious blood clots are more likely to happen when you:
- first start taking birth control pills.
- restart the same or different birth control pills after not using them for a month or more.
- leg pain that will not go away.
- sudden severe shortness of breath.
- sudden change in vision or blindness.
- chest pain.
- a sudden, severe headache unlike our usual headaches.
- weakness or numbness in your arm or leg.
- trouble speaking.
-
liver problems, including:
- jaundice. Call your healthcare provider if you have yellowing of your skin or eyes.
- rare liver tumors.
- high blood pressure. You should see your healthcare provider to check your blood pressure regularly.
- gallbladder problems (cholestasis), especially if you previously had cholestasis of pregnancy.
- changes in the sugar and fat (cholesterol and triglycerides) levels in your blood.
- new or worsening headaches including migraine headaches.
- irregular or unusual vaginal bleeding and spotting between your menstrual periods, especially during the first 3 months of taking TYBLUME or the absence of menstrual periods (amenorrhea).
- depression.
- possible cancer in your cervix.
- swelling of your skin especially around your mouth, eyes, and in your throat (angioedema). Call your healthcare provider right away if you have a swollen face, lips, mouth, tongue or throat, which may lead to difficulty swallowing or breathing. Your chance of having angioedema is higher if you have a history of angioedema.
- dark patches of skin around your forehead, nose, cheeks and around your mouth, especially during pregnancy (chloasma). Women who tend to get chloasma should avoid spending a long time in sunlight, tanning booths, and under sun lamps while taking TYBLUME. Use sunscreen if you have to be in the sunlight.
- headache
- stomach (abdominal) pain
- nausea
- vaginal bleeding in between your periods
- vaginal yeast infection and pain
- acne
- infection or swelling of the vagina that can cause discharge, itching, and pain
These are not all the possible side effects of TYBLUME. For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.What else should I know about taking TYBLUME? - If you are scheduled for any lab tests, tell your healthcare provider you are taking TYBLUME. Certain blood tests may be affected by TYBLUME.
How should I store TYBLUME? - Store the blister card that TYBLUME comes in at room temperature between 68°F to 77°F (20°C to 25°C).
- Protect TYBLUME from light.
- Protect TYBLUME from high heat.
General information about the safe and effective use of TYBLUME.
Medicines are sometimes prescribed for purposes other than those listed in Patient Information. Do not use TYBLUME for a condition for which it was not prescribed. Do not give TYBLUME to other people, even if they have the same symptoms that you have. It may harm them.
You can ask your pharmacist or healthcare provider for information about TYBLUME that is written for health professionals.
Manufactured for: Exeltis USA, Inc., Florham Park, NJ 07932
Manufactured by: Laboratorios León Farma, S.A., León, Spain -
INSTRUCTIONS FOR USETYBLUME [tye bloom] (levonorgestrel and ethinyl estradiol tablets) for oral use
Important information about taking TYBLUME (a type of birth control pill):
- Take 1 pill every day at the same time. Take the pills in the order directed on your blister pack.
- You may either chew 1 pill and then swallow it with a full 8oz (240mL) glass of water right away, or swallow the pill whole. Take the pill without food (on an empty stomach). Take the white pills and the peach pills the same way.
- Do not skip your pills, even if you do not have sex often. If you miss pills (including starting the pack late) you could get pregnant. The more pills you miss, the more likely you are to get pregnant.
- If you have trouble remembering to take TYBLUME, talk to your healthcare provider. When you first start taking TYBLUME, spotting or light bleeding in between your periods may occur. Contact your healthcare provider if this does not go away after a few months.
- You may feel sick to your stomach (nauseous), especially in the first few months after starting TYBLUME. If you feel sick to your stomach, do not stop taking TYBLUME. The nausea will usually go away. If your nausea does not go away, call your healthcare provider.
- Missing pills can also cause spotting or light bleeding in between your menstrual periods, even when you take the missed pills later. On the days you take 2 pills to make up for missed pills (see "What should I do if I miss any TYBLUME tablets?"), you could also feel sick to your stomach.
- Some women miss periods on hormonal birth control, even when they are not pregnant. However, if you miss a period and have not taken TYBLUME according to the directions, or miss 2 or more periods in a row, or feel like you may be pregnant, call your healthcare provider. If you have a positive pregnancy test, you should stop taking TYBLUME.
- If you have vomiting or diarrhea within 3 to 4 hours of taking your pill, take another pill of the same color (that was originally scheduled for you to take the next day) from your blister pack. If you miss more than 2 pills, see "What should I do if I miss any TYBLUME tablets?"
- Continue to take all of your remaining pills in order. Start the first pill of your next blister pack the day after you finish your current blister pack. This will be 1 day earlier than originally scheduled. Continue on your new schedule.
Before you start taking TYBLUME:
- Decide what time of day you want to take your pill. It is important to take it at the same time every day and in the order as directed on your blister pack.
- Have non-hormonal backup birth control (such as condoms or spermicide) available and an extra full pack of pills as needed.
When should I start taking TYBLUME?
If you start taking TYBLUME and you have not used a hormonal birth control method before:
- There are 2 ways to start taking your birth control pills.
- You can either start on a Sunday (Sunday Start) after you period starts, or
- You can start on the first day (Day 1) of your natural menstrual period (Day 1 Start).
Your healthcare provider should tell you when to start taking your birth control pill.
If you use the Sunday Start, use a non-hormonal back-up birth control method such as condoms or spermicide for the first 7 days that you take TYBLUME. You do not need a back-up birth control method if you use the Day 1 Start.
If you start taking TYBLUME and you are switching from another birth control pill:
- Start your new TYBLUME pack on the same day that you would start the next pack of your previous birth control method.
- Do not continue taking the pills from your previous birth control pack.
If you start taking TYBLUME and previously used a vaginal ring or transdermal patch:
- Start using TYBLUME on the day you would have reapplied the next vaginal ring or transdermal patch.
If you start taking TYBLUME and you are switching from a progestin-only method such as an implant or injection:
- Start taking TYBLUME on the day of removal of your implant or on the day when you would have had your next injection.
If you start taking TYBLUME and you are switching from an intrauterine device or system (IUD or IUS):
- Start taking TYBLUME on the day of removal of your IUD or IUS.
- You do not need a back-up birth control method if your IUD or IUS is removed on the first day (Day 1) of your period. If your IUD or IUS is removed on any other day, use a non-hormonal back-up birth control method such as condoms or spermicide for the first 7 days that you take TYBLUME.
If you start taking TYBLUME after you have given birth (postpartum) and have not yet had a menstrual period, use an additional method of birth control (such as condoms or spermicide) for the first 7 days that you take TYBLUME.
Keep a calendar to track your menstrual period:
If this is the first time you are taking birth control pills, read, "When should I start taking TYBLUME?" above. Follow these instructions for either a Sunday Start or a Day 1 Start.
Sunday Start:
You will use a Sunday Start if your healthcare provider told you to take your first pill on a Sunday. Use a non-hormonal back-up birth control method (such as condoms or spermicide) for the first 7 days of the first cycle that you take TYBLUME.
Instructions for using your pill pack:
- Look at your TYBLUME pack. See Figure A.
- Take pill 1 on the Sunday after your period starts.
- If your period starts on a Sunday, take pill "1" that day and see "Day 1 Start" instructions below.
- Take 1 pill every day in the order on the blister pack at the same time each day for 28 days.
- After taking the last pill on Day 28 from the blister pack, start taking the first pill from a new pack, on the same day of the week as the first pack (Sunday). Take the first pill in the new pack whether or not you are having your period.
You will use a Day 1 Start if your healthcare provider told you to take your first pill (Day 1) on the first day of your period.
- Take 1 pill every day in the order of the blister pack, at the same time each day, for 28 days.
- After taking the last pill on Day 28 from the blister pack, start taking the first pill from a new pack, on the same day of the week as the first pack. Take the first pill in the new pack whether or not you are having your period.
Instructions for using your pill pack:
Step 1.
Look at your TYBLUME pack. See Figure A.
The TYBLUME pack has:
- 21 white (active) tablets (pills) with hormones for Week 1 through Week 3
- 7 peach (inactive) tablets (pills) without hormones for Week 4
Step 2.
Find what day of the week you are to start taking your pills. If your period begins on a day other than Sunday, place the day label strip that starts with the first day of your period. For example, if your period begins on Monday, place the day label strip with Monday as the first day. See Figure B.
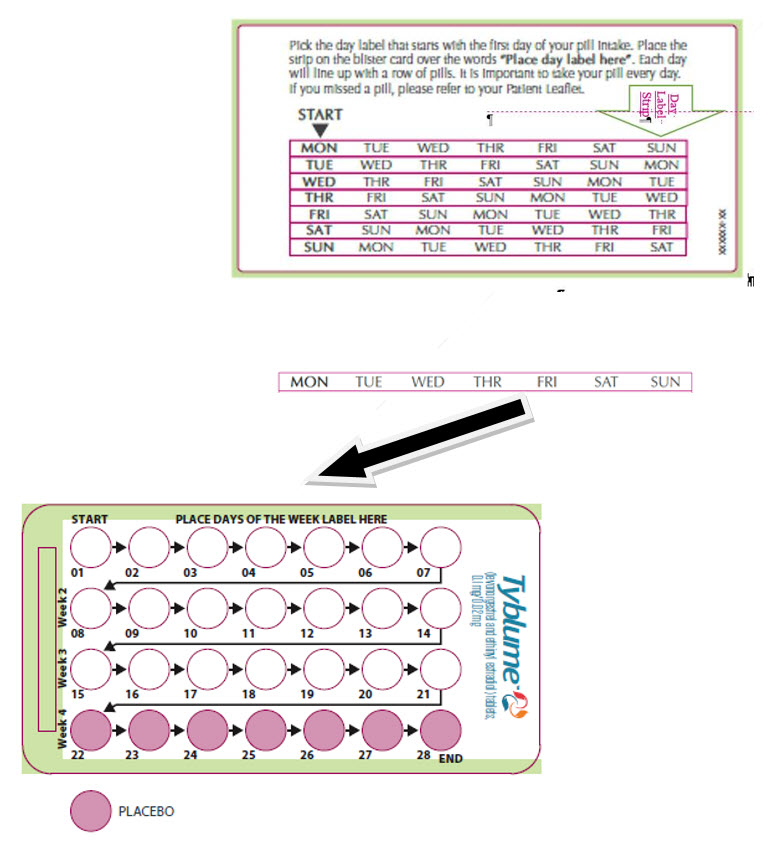
Step 3.
Remove the white pill by pressing the pill through the foil in the bottom of the pill pack. Continue taking the white pills every day for 21 days.
Step 4.
On the first day of Week 4 start taking the peach pills. Take 1 peach pill every day for 7 days. Your period should start during this time.
Step 5.
When you have taken all of the peach pills in your pill pack, get a new pill pack and start taking the white pills.
- For a Day 1 start:
Begin your next pill pack on the same day of the week as your first cycle pill pack. - For a Sunday Start:
Begin your next pill pack on Sunday.
What should I do if I miss any TYBLUME tablets?
If you miss 1 white pill in Weeks 1, 2, or 3 of your pill pack, follow these steps:
- Take it as soon as you remember. Take the next pill at your regular time. This means you may take 2 pills in 1 day.
- Then continue taking 1 pill every day until you finish the pack.
- You do not need to use a non-hormonal back-up birth control method if you have sex.
If you miss 2 white pills in Week 1 or Week 2 of your pill pack, follow these steps:
- Take 2 pills as soon as possible. Then, take 2 pills the next day. This means you will take 4 pills in 2 days.
- Then continue to take 1 pill every day until you finish the pack.
- Use a non-hormonal back-up birth control method (such as a condom or spermicide) if you have sex during the first 7 days after missing your pills.
If you miss 2 white pills in a row in Week 3, or you miss 3 or more white pills in a row during Weeks 1, 2, or 3 of your pill pack, follow these steps:
-
If you are a Day 1 Starter:
- Throw away the rest of the pill pack and start a new pack that same day.
-
If you are a Sunday Starter:
- Keep taking 1 white pill every day until Sunday. On Sunday, throw away the rest of the pack and start a new pack of pills that same day.
- You may not have your period this month, but this is expected. However, if you miss your period 2 months in a row, call your healthcare provider because you might be pregnant.
- You could become pregnant if you have sex during the first 7 days after you restart your pills. You should use a non-hormonal birth control method (such as a condom or spermicide) as a back-up if you have sex during the first 7 days after you restart your pills.
If you miss 1 or more peach pills in Week 4
- Throw away the missed pills.
- Keep taking 1 pill every day until you finish the pack.
- You do not need to use a non-hormonal back-up birth control method (such as condoms or spermicide).
- Make sure you start your next pack on time.
If you have any questions or are unsure about the information in this Instructions for Use, call your healthcare provider. You may also read the Patient Information.
Manufactured for: Exeltis USA, Inc., Florham Park, NJ 07932
Manufactured by: Laboratorios León Farma, S.A., León, SpainThis Instructions for Use has been approved by the U.S. Food and Drug Administration.
Revised Date: March 2020
-
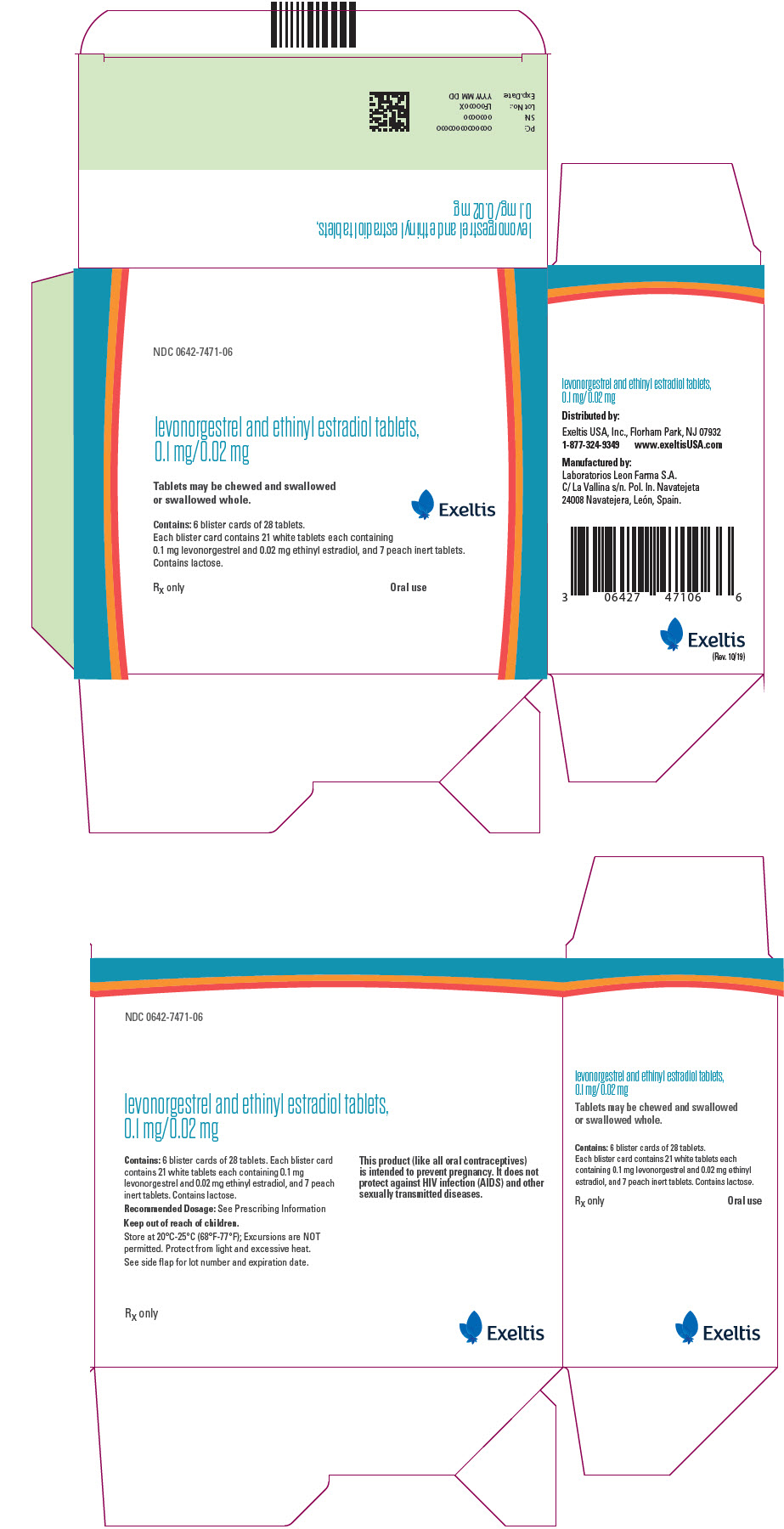
PRINCIPAL DISPLAY PANEL - Kit Carton
NDC: 0642-7471-06
levonorgestrel and ethinyl estradiol tablets,
0.1 mg/0.02 mgTablets may be chewed and swallowed
or swallowed whole.Exeltis
Contains: 6 blister cards of 28 tablets.
Each blister card contains 21 white tablets each containing
0.1 mg levonorgestrel and 0.02 mg ethinyl estradiol, and 7 peach inert tablets.
Contains lactose.Rx only
Oral use
-
INGREDIENTS AND APPEARANCE
LEVONORGESTREL AND ETHINYL ESTRADIOL
levonorgestrel and ethinyl estradiol kitProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0642-7471 Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0642-7471-01 1 in 1 BOX 03/30/2020 1 1 in 1 BLISTER PACK 2 NDC: 0642-7471-03 3 in 1 BOX 03/30/2020 2 1 in 1 BLISTER PACK 3 NDC: 0642-7471-06 6 in 1 BOX 03/30/2020 3 1 in 1 BLISTER PACK Quantity of Parts Part # Package Quantity Total Product Quantity Part 1 21 Part 2 7 Part 1 of 2 LEVONORGESTREL AND ETHINYL ESTRADIOL
levonorgestrel and ethinyl estradiol tabletProduct Information Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LEVONORGESTREL (UNII: 5W7SIA7YZW) (LEVONORGESTREL - UNII:5W7SIA7YZW) LEVONORGESTREL 0.1 mg ETHINYL ESTRADIOL (UNII: 423D2T571U) (ETHINYL ESTRADIOL - UNII:423D2T571U) ETHINYL ESTRADIOL 0.02 mg Inactive Ingredients Ingredient Name Strength Lactose Monohydrate (UNII: EWQ57Q8I5X) 63.58 mg STARCH, CORN (UNII: O8232NY3SJ) 15.5 mg POVIDONE K30 (UNII: U725QWY32X) 3.4 mg CROSPOVIDONE, UNSPECIFIED (UNII: 2S7830E561) 3.5 mg Magnesium Stearate (UNII: 70097M6I30) 0.5 mg Product Characteristics Color WHITE Score no score Shape ROUND Size 6mm Flavor Imprint Code 30;L2 Contains Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA209405 03/30/2020 Part 2 of 2 LEVONORGESTREL AND ETHINYL ESTRADIOL
inactive placebo tabletProduct Information Route of Administration ORAL Inactive Ingredients Ingredient Name Strength ANHYDROUS LACTOSE (UNII: 3SY5LH9PMK) 81.35 mg STARCH, CORN (UNII: O8232NY3SJ) 12.5 mg POVIDONE K30 (UNII: U725QWY32X) 3 mg CROSPOVIDONE, UNSPECIFIED (UNII: 2S7830E561) 2.5 mg Magnesium Stearate (UNII: 70097M6I30) 0.5 mg Product Characteristics Color PINK (PEACH COLORED) Score no score Shape ROUND Size 6mm Flavor Imprint Code 1;L2 Contains Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA209405 03/30/2020 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA209405 03/30/2020 Labeler - Exeltis USA, Inc. (071170534) Establishment Name Address ID/FEI Business Operations ASPEN OSS B. V. 491017488 API MANUFACTURE(0642-7471) Establishment Name Address ID/FEI Business Operations ASPEN OSS B. V. 491013870 API MANUFACTURE(0642-7471) Establishment Name Address ID/FEI Business Operations Industriale Chimica s.r.l. 436796809 API MANUFACTURE(0642-7471) Establishment Name Address ID/FEI Business Operations Lab-Service S.A. 269257291 PARTICLE SIZE REDUCTION(0642-7471) Establishment Name Address ID/FEI Business Operations Laboratorios Leon Farma S.A. 467782459 MANUFACTURE(0642-7471) , ANALYSIS(0642-7471) , PACK(0642-7471) Establishment Name Address ID/FEI Business Operations Laboratorio DR. F. Echevarne Análisis S. A. 460391733 ANALYSIS(0642-7471) Establishment Name Address ID/FEI Business Operations Eurofins Biolab s.r.l. 429117112 ANALYSIS(0642-7471)
Trademark Results [Tyblume]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 TYBLUME 88849932 not registered Live/Pending |
Exeltis Healthcare, S.L. 2020-03-27 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.