HYPERRHO S/D MINI-DOSE (rho(d) immune globulin- human solution
HYPERRHO by
Drug Labeling and Warnings
HYPERRHO by is a Other medication manufactured, distributed, or labeled by GRIFOLS USA, LLC, GRIFOLS THERAPEUTICS LLC. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
DESCRIPTION
Rho(D) Immune Globulin (Human) — HyperRHO® S/D Mini-Dose treated with solvent/ detergent is a colorless to pale yellow or pink sterile solution of immune globulin containing antibodies to Rho(D) for intramuscular administration; it is preservative-free, in a latex-free delivery system. HyperRHO S/D Mini-Dose is prepared by cold ethanol fractionation from human plasma. The immune globulin is isolated from solubilized Cohn Fraction II. The Fraction II solution is adjusted to a final concentration of 0.3% tri-n-butyl phosphate (TNBP) and 0.2% sodium cholate. After the addition of solvent (TNBP) and detergent (sodium cholate), the solution is heated to 30°C and maintained at that temperature for not less than 6 hours. After the viral inactivation step, the reactants are removed by precipitation, filtration and finally ultrafiltration and diafiltration. HyperRHO S/D Mini-Dose is then incubated in the final container for 21–28 days at 20–27°C. HyperRHO S/D Mini-Dose is formulated as a 15–18% protein solution at a pH of 6.4–7.2 in 0.21–0.32 M glycine. One dose of HyperRHO S/D Mini-Dose contains not less than one-sixth the quantity of Rho(D) antibody contained in one standard dose of Rho(D) Immune Globulin (Human), and it will suppress the immunizing potential of 2.5 mL of Rho(D) positive packed red blood cells or the equivalent of whole blood (5 mL). The quantity of Rho(D) antibody in HyperRHO S/D Mini-Dose is not less than 250 IU (50 mcg).
The removal and inactivation of spiked model enveloped and non-enveloped viruses during the manufacturing process for HyperRHO S/D Mini-Dose has been validated in laboratory studies. Human Immunodeficiency Virus, Type 1 (HIV-1), was chosen as the relevant virus for blood products; Bovine Viral Diarrhea Virus (BVDV) was chosen to model Hepatitis C virus; Pseudorabies virus (PRV) was chosen to model Human Herpes viruses and other large enveloped DNA viruses; and Reo virus type 3 (Reo) was chosen to model non-enveloped viruses and for its resistance to physical and chemical inactivation. Significant removal of model enveloped and non-enveloped viruses is achieved at two steps in the Cohn fractionation process leading to the collection of Cohn Fraction II: the precipitation and removal of Fraction III in the processing of Fraction II + IIIW suspension to Effluent III and the filtration step in the processing of Effluent III to Filtrate III. Significant inactivation of enveloped viruses is achieved at the time of treatment of solubilized Cohn Fraction II with TNBP/sodium cholate.
Additionally, the manufacturing process was investigated for its capacity to decrease the infectivity of an experimental agent of transmissible spongiform encephalopathy (TSE), considered as a model for the vCJD and CJD agents. [11-14]
Studies of the HyperRHO S/D manufacturing process demonstrate that TSE clearance is achieved during the Pooled Plasma to Effluent III Fractionation Process (6.7 log10). These studies provide reasonable assurance that low levels of CJD/vCJD agent infectivity, if present in the starting material, would be removed.
-
CLINICAL PHARMACOLOGY
Rh sensitization may occur in nonsensitized Rho(D) negative women following transplacental hemorrhage resulting from spontaneous or induced abortions. [1-2] The risk of sensitization is higher in women undergoing induced abortions than in those aborting spontaneously. [1-3]
HyperRHO S/D Mini-Dose is used to prevent the formation of anti-Rho(D) antibody in Rho(D) negative women who are exposed to the Rho(D) antigen at the time of spontaneous or induced abortion (up to 12 weeks’ gestation). [3-5] HyperRHO S/D Mini-Dose suppresses the stimulation of active immunity by Rho(D) positive fetal erythrocytes that may enter the maternal circulation at the time of termination of the pregnancy.
The amount of anti-Rho(D) in HyperRHO S/D Mini-Dose has been shown to effectively prevent maternal isosensitization to the Rho(D) antigens following spontaneous or induced abortion occurring up to the 12th week of gestation. [6-8] After the 12th week of gestation, a standard dose of HyperRHO S/D Full Dose is indicated.
In a clinical study in eight healthy human adults receiving another hyperimmune immune globulin product treated with solvent/detergent, Rabies Immune Globulin (Human), HyperRAB® S/D, prepared by the same manufacturing process, detectable passive antibody titers were observed in the serum of all subjects by 24 hours post injection and persisted through the 21 day study period. These results suggest that passive immunization with immune globulin products is not affected by the solvent/detergent treatment.
-
INDICATIONS AND USAGE
HyperRHO S/D Mini-Dose is recommended to prevent the isoimmunization of Rho(D) negative women at the time of spontaneous or induced abortion of up to 12 weeks’ gestation provided the following criteria are met:
-
The mother must be Rho(D) negative and must not already be sensitized to the Rho(D) antigen.
-
The father is not known to be Rho(D) negative.
-
Gestation is not more than 12 weeks at termination.
Note: Rho(D) Immune Globulin (Human) prophylaxis is not indicated if the fetus or father can be determined to be Rh negative. If the Rh status of the fetus is unknown, the fetus must be assumed to be Rho(D) positive, and HyperRHO S/D Mini-Dose should be administered to the mother.
FOR ABORTIONS OR MISCARRIAGES OCCURRING AFTER 12 WEEKS’ GESTATION, A STANDARD DOSE OF Rho(D) IMMUNE GLOBULIN (HUMAN) IS INDICATED.
HyperRHO S/D Mini-Dose should be administered within 3 hours or as soon as possible after spontaneous passage or surgical removal of the products of conception. However, if HyperRHO S/D Mini-Dose is not given within this time period, consideration should still be given to its administration since clinical studies in male volunteers have demonstrated the effectiveness of Rho(D) Immune Globulin (Human) in preventing isoimmunization as long as 72 hours after infusion of Rho(D) positive red cells. [9]
-
- CONTRAINDICATIONS
-
WARNINGS
HyperRHO S/D Mini-Dose is made from human plasma. Products made from human plasma may contain infectious agents, such as viruses, and, theoretically, the Creutzfeldt-Jakob Disease (CJD) agent that can cause disease. The risk that such products will transmit an infectious agent has been reduced by screening plasma donors for prior exposure to certain viruses, by testing for the presence of certain current virus infections, and by inactivating and/or removing certain viruses. Despite these measures, such products can still potentially transmit disease. There is also the possibility that unknown infectious agents may be present in such products. Individuals who receive infusions of blood or plasma products may develop signs and/or symptoms of some viral infections, particularly hepatitis C. ALL infections thought by a physician possibly to have been transmitted by this product should be reported by the physician or other healthcare provider to Grifols Therapeutics LLC [1-800-520-2807].
The physician should discuss the risks and benefits of this product with the patient, before prescribing or administering it to the patient.
NEVER ADMINISTER HYPERRHO S/D MINI-DOSE INTRAVENOUSLY. INJECT ONLY INTRAMUSCULARLY. ADMINISTER ONLY TO WOMEN POSTABORTION OR POSTMISCARRIAGE OF UP TO 12 WEEKS’ GESTATION. NEVER ADMINISTER TO THE NEONATE.
HyperRHO S/D Mini-Dose should be given with caution to patients with a history of prior systemic allergic reactions following the administration of human immune globulin preparations.
The attending physician who wishes to administer HyperRHO S/D Mini-Dose to persons with isolated immunoglobulin A (IgA) deficiency must weigh the benefits of immunization against the potential risks of hypersensitivity reactions. Such persons have increased potential for developing antibodies to IgA and could have anaphylactic reactions to subsequent administration of blood products that contain IgA.
As with all preparations administered by the intramuscular route, bleeding complications may be encountered in patients with thrombocytopenia or other bleeding disorders.
-
PRECAUTIONS
General
Although systemic reactions to immunoglobulin preparations are rare, epinephrine should be available for treatment of acute anaphylactic symptoms.
Drug Interactions
Other antibodies in the HyperRHO S/D Mini-Dose preparation may interfere with the response to live vaccines such as measles, mumps, polio or rubella. Therefore, immunization with live vaccines should not be given within 3 months after HyperRHO S/D Mini-Dose administration.
Pregnancy
Animal reproduction studies have not been conducted with HyperRHO S/D Mini-Dose. It is also not known whether HyperRHO S/D Mini-Dose can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity.
It should be again noted, however, that HyperRHO S/D Mini-Dose is not indicated for use during pregnancy and it should be administered only postabortion or postmiscarriage.
- ADVERSE REACTIONS
-
DOSAGE AND ADMINISTRATION
NEVER ADMINISTER HYPERRHO S/D MINI-DOSE INTRAVENOUSLY. INJECT ONLY INTRAMUSCULARLY. ADMINISTER ONLY TO WOMEN POSTABORTION OR POSTMISCARRIAGE OF UP TO 12 WEEKS’ GESTATION. NEVER ADMINISTER TO THE NEONATE.
One syringe of HyperRHO S/D Mini-Dose provides sufficient antibody to prevent Rh sensitization to 2.5 mL Rho(D) positive packed red cells or the equivalent (5 mL) of whole blood. This dose is sufficient to provide protection against maternal Rh sensitization for women undergoing spontaneous or induced abortion of up to 12 weeks’ gestation.
Rho(D) Immune Globulin (Human) — HyperRHO® S/D Mini-Dose (250 IU; 50 mcg) should be administered within 3 hours or as soon as possible following spontaneous or induced abortion. If prompt administration is not possible, HyperRHO S/D Mini-Dose should be given within 72 hours following termination of the pregnancy.
HyperRHO S/D Mini-Dose is administered intramuscularly, preferably in the deltoid muscle of the upper arm or lateral thigh muscle. The gluteal region should not be used as an injection site because of the risk of injury to the sciatic nerve. [10]
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
HyperRHO S/D Mini-Dose is supplied with a syringe and an attached UltraSafe® Needle Guard for your protection and convenience. Please follow instructions below for proper use of syringe and UltraSafe® Needle Guard.
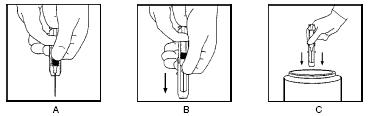
Directions for Syringe Usage
-
Remove the prefilled syringe from the package. Lift syringe by barrel, not by plunger.
-
Twist the plunger rod clockwise until the threads are seated.
-
With the rubber needle shield secured on the syringe tip, push the plunger rod forward a few millimeters to break any friction seal between the rubber stopper and the glass syringe barrel.
-
Remove the needle shield and expel air bubbles. [Do not remove the rubber needle shield to prepare the product for administration until immediately prior to the anticipated injection time.]
- Proceed with hypodermic needle puncture.
- Aspirate prior to injection to confirm that the needle is not in a vein or artery.
- Inject the medication.
-
Keeping your hands behind the needle, grasp the guard with free hand and slide forward toward needle until it is completely covered and guard clicks into place. If audible click is not heard, guard may not be completely activated. (See Diagrams A and B)
-
Place entire prefilled glass syringe with guard activated into an approved sharps container for proper disposal. (See Diagram C)
A number of factors could reduce the efficacy of this product or even result in an ill effect following its use. These include improper storage and handling of the product after it leaves our hands, diagnosis, dosage, method of administration, and biological differences in individual patients. Because of these factors, it is important that this product be stored properly and that the directions be followed carefully during use.
-
- HOW SUPPLIED
- STORAGE
- CAUTION
-
REFERENCES
-
Queenan JT, Shah S, Kubarych SF, et al: Role of induced abortion in rhesus immunisation. Lancet 1(7704):815-7, 1971.
-
Goldman JA, Eckerling B: Prevention of Rh immunization after abortion with anti-Rho(D)-immuno globulin. Obstet Gynecol 40(3):366-70, 1972.
-
The selective use of Rho(D) immune globulin (RhIG). ACOG Tech Bull 61,1981.
-
Prevention of Rh sensitization. WHO Tech Rep Ser 468, 1971.
-
Recommendation of the Public Health Service Advisory Committee on Immunization Practices: Rh immune globulin. MMWR 21(15):126-7, 1972.
-
Stewart FH, Burnhill MS, Bozorgi N: Reduced dose of Rh immunoglobulin following first trimester pregnancy termination. Obstet Gynecol 51(3):318-22, 1978.
-
McMaster conference on prevention of Rh immunization. 28-30 September, 1977. Vox Sang 36(1):50-64, 1979.
-
Simonovits I: Efficiency of anti-D IgG prevention after induced abortion. Vox Sang 26(4):361-7, 1974.
-
Freda VJ, Gorman JG, Pollack W: Prevention of Rh-hemolytic disease with Rh-immune globulin. Am J Obstet Gynecol 128(4):456-60, 1977.
-
Recommendations of the Advisory Committee on Immunization Practices (ACIP) and the AmericanAcademy of Family Physicians (AAFP): General recommendations on immunization. MMWR 2002: 51(RR02), 1-36.
-
Stenland CJ, Lee DC, Brown P, et al. Partitioning of human and sheep forms of the pathogenic prion protein during the purification of therapeutic proteins from human plasma. Transfusion 2002. 42(11):1497-500.
-
Lee DC, Stenland CJ, Miller JL, et al. A direct relationship between the partitioning of the pathogenic prion protein and transmissible spongiform encephalopathy infectivity during the purification of plasma proteins. Transfusion 2001. 41(4):449-55.
-
Lee DC, Stenland CJ, Hartwell RC, et al. Monitoring plasma processing steps with a sensitive Western blot assay for the detection of the prion protein. J Virol Methods 2000. 84(1):77-89.
-
Cai K, Miller JL, Stenland CJ, et al. Solvent-dependent precipitation of prion protein. Biochim Biophys Acta 2002. 1597(1):28-35.
(Rev. 6/2018)
Grifols Therapeutics LLC
Research Triangle Park NC 27709 USA
U.S. License No. 1871
3047913 -
-
The Rh Factor and Your Pregnancy

Information About Pregnancy Protection
The Rh Factor and When It Is Important
The Rh factor is one of many blood group antigens found on the surface of red blood cells. If you have this antigen you are considered Rh positive. If you don’t, then you are considered Rh negative. Everyone is either Rh positive or Rh negative. One type is neither better nor worse than the other, only different.
Your Rh factor is important if you are an Rh negative woman and you become pregnant, or if you receive a blood transfusion.
How the Rh Factor Can Affect Your Future
If you have Rh negative blood, there are two situations that can affect you:
- 1. If the father of your baby is Rh positive, the baby will probably be Rh positive too. An Rh negative woman carrying an Rh positive baby may have an immune reaction if some of the baby’s Rh positive blood cells enter her bloodstream.
-
This immune reaction, called isoimmunization, means your body’s defense system recognizes Rh positive blood as foreign from your own and produces “antibodies” to destroy the invading Rh positive blood cells. -
The passage of blood from the baby to the mother’s bloodstream happens most often at delivery, but can also occur during miscarriage, the termination of pregnancy, amniocentesis (test performed to determine fetal health), or due to an injury or trauma. It is important to note that a small number of women develop antibodies to Rh positive blood cells during pregnancy for no apparent reason. -
Antibodies to Rh positive blood may not be a problem in first pregnancies; however, the antibodies stay in your bloodstream, ready to attack invading Rh positive blood cells, for many years to come. This can lead to problems in future pregnancies by causing miscarriage or a disease known as hemolytic disease of the newborn. -
Babies born to Rh positive mothers, regardless of the father’s blood type, will usually be free of the dangers of hemolytic disease.
- 2. Someday it may become necessary for you to receive a blood transfusion. If Rh positive antibodies already reside in your bloodstream due to isoimmunization and the blood you receive is Rh positive due to error or lifesaving reasons, your Rh positive antibodies will become mobilized and destroy the donor Rh positive cells. As a result, the transfusion could be unsuccessful and possibly harmful to you.
Hemolytic Disease of the Newborn: A Threat to Your Baby
When an Rh negative woman has Rh positive antibodies in her blood and the baby she is carrying is Rh positive, the antibodies could possibly enter the baby’s bloodstream, attack the baby’s red blood cells and cause hemolytic disease of the newborn. At birth, the infant suffering from hemolytic disease may be jaundiced and anemic or suffer permanent damage of the brain and central nervous system which may result in mental retardation, hearing loss, or cerebral palsy. Extensive medical care can be required, including an exchange transfusion, in which all of the baby’s blood is replaced. This usually stops the destruction of the baby’s red blood cells and gives the infant a chance to survive.
The risk of hemolytic disease of the newborn is slight with the first baby, but increases with each successive pregnancy.
Preventing Hemolytic Disease
HyperRHO® S/D, Rho(D) Immune Globulin (Human) can prevent hemolytic disease of the newborn, provided Rh positive antibodies do not already reside in your bloodstream.
HyperRHO S/D is a specially prepared gamma globulin with a high level of preformed antibodies against Rh positive blood cells. The injection of HyperRHO S/D destroys any Rh positive blood cells that may have entered the mother’s bloodstream and prevents the mother’s immune system from producing Rh positive antibodies; thus protecting the baby from developing hemolytic disease.
HyperRHO S/D Full Dose — When Prescribed
Pregnancy and Other Obstetric Conditions Pertaining to Rh Negative Women
HyperRHO S/D Full Dose (1,500 IU; 300 mcg) is administered during pregnancy if you fall into a high-risk category. For example, you are at risk of producing Rh positive antibodies if you have an amniocentesis procedure performed, or if you have a miscarriage or other termination of pregnancy at or beyond 13 weeks' gestation.
Laboratory findings have shown that some Rh negative women develop Rh positive antibodies during the last weeks of pregnancy even without an antibody-stimulating event. As a preventive measure, your physician will probably recommend the first injection of HyperRHO S/D Full Dose at the 28th week of pregnancy.
In both of the above situations, if the blood type of the father or baby can be determined to be Rh negative, an injection of HyperRHO S/D is not required.
Another injection of HyperRHO S/D Full Dose is administered within 72 hours of delivery of an Rh positive baby.
Blood Transfusion
HyperRHO S/D Full Dose (1,500 IU; 300 mcg) may be used to prevent isoimmunization in Rh negative individuals who have been transfused with Rh positive red blood cells or blood components containing red blood cells.
HyperRHO S/D Mini-Dose — When Prescribed
A single dose of HyperRHO S/D Mini-Dose (250 IU; 50 mcg) may be prescribed for an Rh negative woman instead of HyperRHO S/D Full Dose (1,500 IU; 300 mcg) in the event of miscarriage or other termination of pregnancy occurring prior to 13 weeks' gestation. HyperRHO S/D Mini-Dose is not required if the blood type of the father or fetus can be determined to be Rh negative..
Will You Need HyperRHO S/D Again?
HyperRHO S/D provides protection only if you have not already produced Rh positive antibodies. Women who have developed antibodies through previous pregnancy, miscarriage, other termination of pregnancy, or blood transfusion cannot be protected by HyperRHO S/D. This is why with each pregnancy it is important to have HyperRHO S/D injections within the prescribed time period.
Reactions to HyperRHO S/D
You may feel a temporary soreness at the site of the injection. You may also have a slight and temporary change in body temperature. In very rare instances, an allergic type of reaction can occur, for which your physician will take appropriate measures.
Delivering a Sound, Healthy Baby
Your physician can answer any questions you may have about receiving a HyperRHO S/D injection to prevent hemolytic disease of the newborn. If you know that you are Rh negative and you are pregnant, you should discuss your situation with your physician. Today, with HyperRHO S/D, hemolytic disease of the newborn can be reduced to its lowest possible rate of incidence.
GRIFOLS
Grifols Therapeutics LLC
Research Triangle Park, NC 27709 USA
U.S. License No. 1871
(Rev.6/2018)Development of Hemolytic Disease
1
Rh positive (+) father.
Rh negative (–) mother.
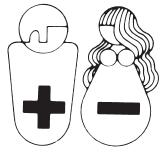
2
Pregnancy: Rh– mother is carrying Rh+ baby.

3
The passage of Rh+ blood from the baby to the mother’s bloodstream happens most often at delivery, but can also occur during miscarriage, other termination of pregnancy, amniocentesis, or due to injury or trauma.
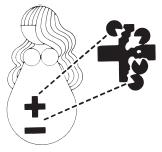
4
Rh+ antibodies stay in your bloodstream, ready to attack invading Rh+ blood cells, for many years to come.

5
Next pregnancy, mother’s Rh+ antibodies enter baby’s Rh+ bloodstream,
attacking baby’s blood cells and causing hemolytic disease of the newborn.

How HyperRHO S/D Immune Globulin Can Prevent Hemolytic Disease
1
You will probably be given two injections of HyperRHO S/D Full Dose, one at the 28th week of your pregnancy and another within 72 hours of delivery, miscarriage or other termination of pregnancy. A single injection of HyperRHO S/D Mini-Dose may be prescribed instead of HyperRHO S/D Full Dose in the event of miscarriage or other termination of pregnancy occurring prior to 13 weeks' gestation.
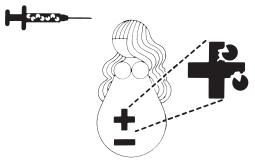
2
HyperRHO S/D immunization prevents formation of mother’s own Rh+ antibodies. Mother’s bloodstream remains free of Rh+ antibodies.

3
Next pregnancy, baby develops normally. HyperRHO S/D should be administered following delivery, miscarriage, or other termination of pregnancy to continue protection if baby is Rh+.

-
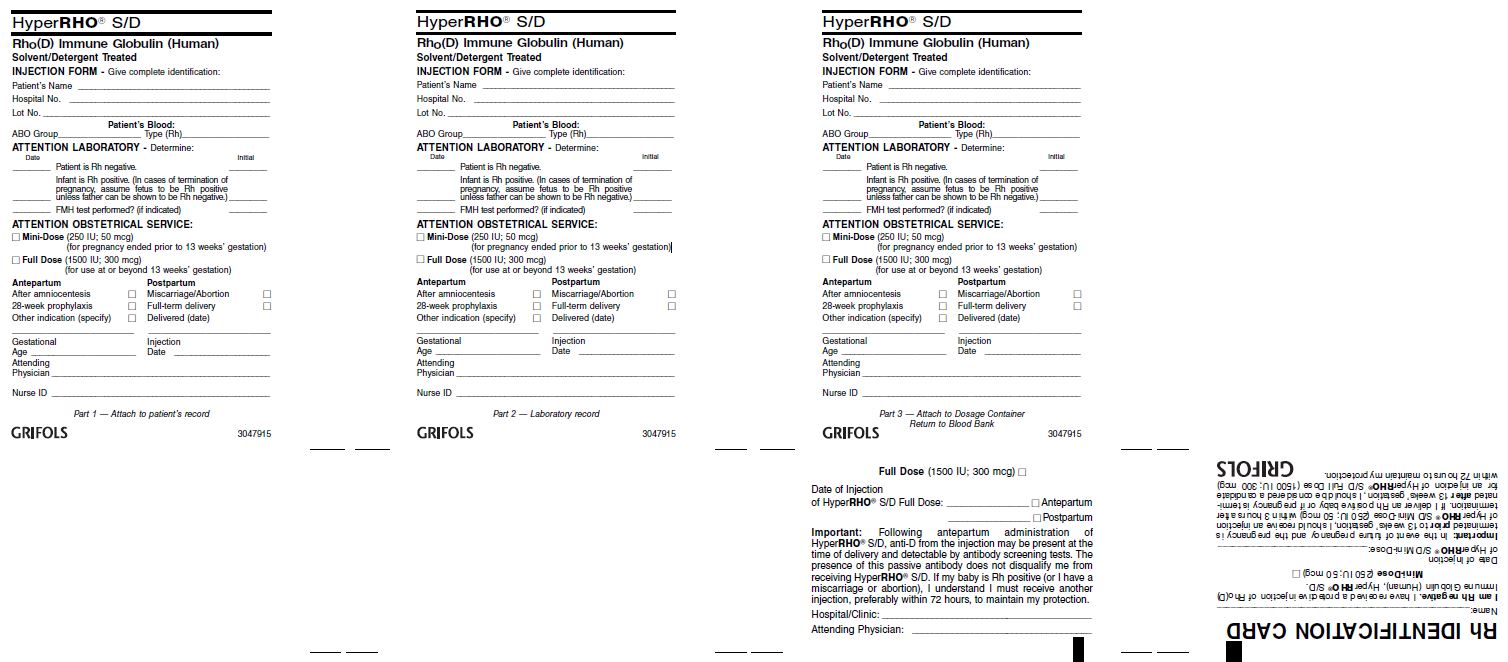
PACKAGE LABEL
Rho(D)Immune Globulin (Human)
HyperRHO®S/D Mini-Dose
250 IU (50 mcg)
Solvent/Detergent Treated
Preservative-free, latex-free delivery system
Contents: 10 single dose disposable syringes with attached needles
The patient and physician should discuss the risks and benefits of this product.
Rho(D) Immune Globulin (Human) — HyperRHO® S/D Mini-Dose is a sterile solution of immunoglobulin containing 15%–18% protein stabilized with 0.21–0.32 M glycine. The pH is adjusted with sodium carbonate.
The quantity of Rho(D) antibody in each single dose syringe of HyperRHO® S/D Mini-Dose is not less than 250 IU (50 mcg). One dose will suppress the immunizing potential of 2.5 mL Rho(D) positive packed red cells or the
equivalent of whole blood (5.0 mL).
FOR INTRAMUSCULAR INJECTION ONLY. DO NOT GIVE INTRAVENOUSLY. NEVER ADMINISTER
TO NEONATES.
Store at 2–8°C (36–46°F). Do not freeze.
For complete dosage and administration information, read enclosed package insert.
For directions for syringe usage, see enclosed package insert.
Do not use if the syringe is prematurely engaged.
Not returnable for credit or exchange.
Rx only
CAUTION: U.S. federal law prohibits dispensing without prescription.
GRIFOLS
Grifols Therapeutics LLC
Research Triangle Park, NC 27709 USA
U.S. License No. 1871
NDC 13533-661-06
Carton: 3048955
GTIN XXXXXXXXXXXXXX
LOT XXXXXXXXXX
EXP DDMMMYYYY
SN XXXXXXXXXXXXXXXX
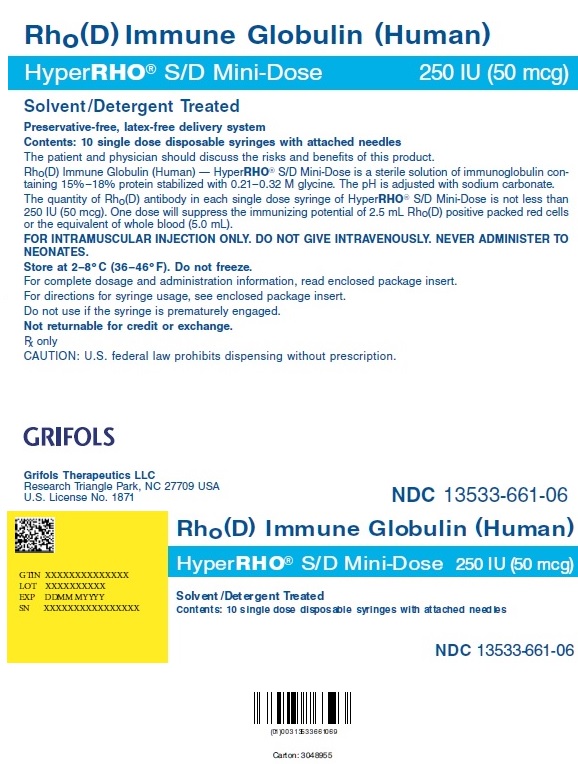
Rho(D) Immune Globulin (Human)
HyperRHO® S/D Mini-Dose
Solvent/Detergent Treated
Grifols Therapeutics LLC
RTP, NC 27709 USA
U.S. License No. 1871
The patient and physician should discuss the risks and benefits of this product.
3048430
Lot
Exp.
-
INGREDIENTS AND APPEARANCE
HYPERRHO S/D MINI-DOSE
rho(d) immune globulin (human) solutionProduct Information Product Type PLASMA DERIVATIVE Item Code (Source) NDC: 13533-661 Route of Administration INTRAMUSCULAR Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength Human Rho(d) Immune Globulin (UNII: 48W7181FLP) (Human Rho(d) Immune Globulin - UNII:48W7181FLP) Human Rho(d) Immune Globulin 250 [iU] Inactive Ingredients Ingredient Name Strength Glycine (UNII: TE7660XO1C) Water (UNII: 059QF0KO0R) Product Characteristics Color YELLOW (YELLOW (clear liquid, colorless to pale yellow or pink)) Score Shape Size Flavor Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 13533-661-06 10 in 1 CARTON 1 NDC: 13533-661-60 1 in 1 SYRINGE; Type 3: Prefilled Biologic Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA101141 08/14/1996 Labeler - GRIFOLS USA, LLC (048987452) Establishment Name Address ID/FEI Business Operations GRIFOLS THERAPEUTICS LLC 611019113 manufacture(13533-661)
Trademark Results [HYPERRHO]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 HYPERRHO 78622902 3206858 Live/Registered |
GRIFOLS THERAPEUTICS LLC 2005-05-04 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.