These highlights do not include all the information needed to use AEMCOLO safely and effectively. See full prescribing information for AEMCOLO. AEMCOLO (rifamycin) delayed-release tablets, for oral use. Initial U.S. Approval: 2018
Aemcolo by
Drug Labeling and Warnings
Aemcolo by is a Prescription medication manufactured, distributed, or labeled by RedHill Biopharma Ltd. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
AEMCOLO- rifamycin tablet, delayed release
RedHill Biopharma Ltd
----------
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use AEMCOLO safely and effectively. See full prescribing information for AEMCOLO.
AEMCOLO (rifamycin) delayed-release tablets, for oral use. Initial U.S. Approval: 2018 INDICATIONS AND USAGEAEMCOLO is a rifamycin antibacterial indicated for the treatment of travelers' diarrhea caused by noninvasive strains of Escherichia coliin adults. ( 1.1) Limitations of Use: AEMCOLO is not recommended for use in patients with diarrhea complicated by fever and/or bloody stool or due to pathogens other than noninvasive strains of E. coli.( 1, 5.1, 14) To reduce the development of drug-resistant bacteria and maintain the effectiveness of AEMCOLO and other antibacterial drugs, AEMCOLO should be used only to treat or prevent infections that are proven or strongly suspected to be caused by bacteria ( 1.2). DOSAGE AND ADMINISTRATION
DOSAGE FORMS AND STRENGTHSDelayed-Release Tablets: 194 mg rifamycin. ( 3) CONTRAINDICATIONSAEMCOLO is contraindicated in patients with a known hypersensitivity to rifamycin, any of the other rifamycin class antimicrobial agents (e.g. rifaximin), or any of the components in AEMCOLO ( 4) WARNINGS AND PRECAUTIONS
ADVERSE REACTIONSMost common adverse reactions (incidence > 2%) are headache and constipation. ( 6.1) To report SUSPECTED ADVERSE REACTIONS, contact RedHill Biopharma Inc. at 833-ADR-HILL (833-237-4455) or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. See 17 for PATIENT COUNSELING INFORMATION. Revised: 2/2021 |
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
1.1 Travelers' Diarrhea
AEMCOLO is indicated for the treatment of travelers' diarrhea (TD) caused by non-invasive strains of Escherichia coliin adults.
Limitations of Use
AEMCOLO is not indicated in patients with diarrhea complicated by fever or bloody stool or due to pathogens other than noninvasive strains of Escherichia coli [see Warnings and Precautions (5), Clinical Studies (14)] .
1.2 Usage
To reduce the development of drug-resistant bacteria and maintain the effectiveness of AEMCOLO and other antibacterial drugs, AEMCOLO should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
2 DOSAGE AND ADMINISTRATION
3 DOSAGE FORMS AND STRENGTHS
AEMCOLO is a yellow-brown, ellipsoidal, film-coated, delayed-release tablet debossed on one side with "SV2". Each delayed-release tablet contains 194 mg of rifamycin.
4 CONTRAINDICATIONS
AEMCOLO is contraindicated in patients with a known hypersensitivity to rifamycin, any of the other rifamycin class antimicrobial agents (e.g. rifaximin), or any of the components in AEMCOLO.
5 WARNINGS AND PRECAUTIONS
5.1 Risk of Persistent or Worsening of Diarrhea Complicated by Fever and/or Bloody Stool
AEMCOLO was not shown to be effective in patients with diarrhea complicated by fever and/or bloody stool. Patients with these conditions treated with AEMCOLO had prolonged time to last unformed stool (TLUS). The effectiveness of AEMCOLO in travelers' diarrhea caused by pathogens other than E. colihas not been demonstrated. AEMCOLO is not recommended for use in patients with diarrhea accompanied by fever or bloody stools or due to pathogens other than noninvasive strains of E. coli [see Indications and Usage (1), Clinical Studies (14)].
Discontinue AEMCOLO if diarrhea gets worse or persists more than 48 hours and consider alternative antibacterial therapy.
5.2 Clostridium difficile-Associated Diarrhea
Clostridium difficile-associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents, and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon which may lead to overgrowth of C. difficile.
C. difficileproduces toxins A and B which contribute to the development of CDAD. Hypertoxin producing strains of C. difficilemay cause increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibacterial drug use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents.
If CDAD is suspected or confirmed, antibacterial drug use not directed against C. difficilemay need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, specific antibacterial treatment of C. difficile, and/or surgical evaluation should be instituted as clinically indicated.
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The safety of oral AEMCOLO 388 mg twice daily was assessed in 619 adults with travelers' diarrhea in two controlled clinical trials (Trial 1 and Trial 2) with 96% of patients receiving three or four days of treatment. These patients had a mean age of 36.2 years (range 18 to 87 years) with 7% ≥ 65 years old; 49% were male, 84% were White, and 4% were Hispanic.
Discontinuation of AEMCOLO due to adverse reactions occurred in 1% of patients. The most frequent adverse reactions leading to discontinuation of AEMCOLO were abdominal pain (0.5%) and pyrexia (0.3%).
In Trial 1 (placebo-controlled), the adverse reaction that occurred in at least 2% of AEMCOLO-treated patients (n = 199) and with an incidence higher than in the placebo group was constipation (3.5% AEMCOLO, 1.5% placebo)
In Trial 2 (active comparator), the adverse reaction that occurred in at least 2% of AEMCOLO-treated patients (n = 420) and with an incidence higher than in the ciprofloxacin group was headache (3.3% AEMCOLO, 1.9% ciprofloxacin)
Adverse reactions reported in <2% of patients receiving AEMCOLO 388 mg twice daily with a higher incidence than the comparator group was dyspepsia.
7 DRUG INTERACTIONS
No clinical Drug-Drug Interactions (DDIs) have been studied. Based on the minimal systemic rifamycin concentrations observed after the recommended dose of AEMCOLO, clinically relevant DDIs are not expected [see Clinical Pharmacology (12.3)]
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There are no available data on AEMCOLO use in pregnant women to inform any drug associated risks for major birth defects, miscarriage, or adverse maternal or fetal outcomes. Systemic absorption of AEMCOLO in humans is negligible following oral administration of the recommended dose of AEMCOLO [see Clinical Pharmacology (12.3)] . Due to the negligible systemic exposure, it is not expected that maternal use of AEMCOLO will result in fetal exposure to the drug.
In animal reproduction studies, no malformations were observed in pregnant rats or rabbits at exposures 25,000 and 500 times (based on AUC), respectively, the human exposure achieved with the recommended clinical dose of AEMCOLO. Treatment of pregnant rats with AEMCOLO at more than 1,000 times the maximum plasma concentration (C max) and 25,000 times the systemic exposure (based on AUC) during the period of organogenesis resulted in maternal toxicity, decreased fetal weight, and variations in diaphragm formation. Similarly, treatment of pregnant rabbits with AEMCOLO at more than 10 times the maximum human plasma concentration (C max), resulted in maternal toxicity, decreased fetal weight, and slightly delayed fetal ossifications [See Data].
All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively. Advise pregnant women of the potential risk to a fetus.
Animal Data
Embryofetal toxicity studies in rats and rabbits did not show malformations up to the maximum tested doses of 855 and 85.5 mg/kg, (25,000 and 500 times greater plasma exposure based on AUC), respectively, of rifamycin given orally during the period of organogenesis (gestational days 6-17/18). In rats, the high dose of 855 mg/kg/day caused reduction in maternal food consumption, reduced fetal weight and a higher number of fetuses with thin tendinous diaphragm. In rabbits, the high dose of 85.5 mg/kg/day caused a reduction in food consumption and bodyweight gain in pregnant dams, as well as reduced fetal weights and slight delay in ossification, including slightly higher incidences of fetuses with skull suture bone variations, enlarged skull fontanelle and incompletely ossified digit 5 medial phalanx of both forelimbs. No adverse fetal effects were observed in rats and rabbits administered lower doses of oral rifamycin.
8.2 Lactation
Risk Summary
There is no information regarding the presence of AEMCOLO in human milk, the effects on the breastfed infant, or the effects on milk production. Systemic absorption of AEMCOLO in humans is negligible following oral administration of the recommended dose of AEMCOLO; therefore, exposure to a breastfed infant through breastmilk is expected to be negligible [see Clinical Pharmacology (12.3)] . There are no animal lactation data following oral rifamycin administration. Following single intravenous injection of rifamycin to lactating ewes, rifamycin has been shown to pass into milk. 1
The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for AEMCOLO and any potential adverse effects on the breast-fed infant from AEMCOLO or from the underlying maternal condition.
8.4 Pediatric Use
The safety and effectiveness of AEMCOLO has not been established in pediatric patients less than 18 years of age with travelers' diarrhea.
8.5 Geriatric Use
Clinical studies with AEMCOLO for travelers' diarrhea did not include sufficient numbers of patients aged 65 and older to determine whether they respond differently than younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients.
8.6 Renal Impairment
The pharmacokinetics of AEMCOLO in patients with impaired renal function has not been studied. Given the minimal systemic exposure of rifamycin (taken as AEMCOLO) and minor role of renal excretion in elimination of rifamycin, renal impairment is not expected to have a clinically meaningful effect on rifamycin systemic exposure necessitating a dose adjustment.
8.7 Hepatic Impairment
The pharmacokinetics of AEMCOLO in patients with impaired hepatic function has not been studied. Given the minimal systemic exposure of rifamycin (taken as AEMCOLO) hepatic impairment is not expected to have a clinically meaningful effect on rifamycin systemic exposure necessitating a dose adjustment.
10 OVERDOSAGE
No specific information is available on the treatment of overdose with AEMCOLO. In the case of overdose, discontinue AEMCOLO, treat symptomatically, and institute supportive measures as required.
11 DESCRIPTION
AEMCOLO, delayed-release tablet, for oral administration, contains 194 mg of rifamycin equivalent to 200 mg of rifamycin sodium.
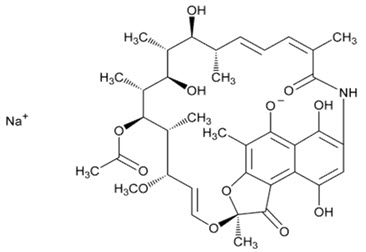
Rifamycin sodium is a rifamycin antibacterial. It is designated chemically as: Sodium (2S,12Z,14E,16S,17S,18R,19R,20R,21S,22R,23S,24E)-21-(acetyloxy)-6,9,17,19-tetrahydroxy-23-methoxy-2,4,12,16,18,20,22-heptamethyl-1,11-dioxo-1,2-dihydro-2,7-(epoxypentadeca[1,11,13]trienimino)naphtho[2,1- b]furan-5-olate. Its empirical formula is C 37H 46NNaO 12. The molecular weight is 720 g/mol.
Its structural formula is:
Rifamycin sodium is a fine or slightly granular powder, soluble in water, and freely soluble in anhydrous ethanol.
AEMCOLO, delayed-release tablets are enteric coated with a pH-resistant polymer film which breaks down above pH 7. The tablet core contains rifamycin. The tablets are yellow brown and ellipsoidal.
Each tablet contains the following inactive ingredients: ammonio methacrylate copolymer (Type B), ascorbic acid, glyceryl distearate, lecithin, magnesium stearate, mannitol, methacrylic acid and methyl methacrylate copolymer (1:2), polyethylene glycol 6000, colloidal silicon dioxide, talc, titanium dioxide, triethylcitrate, yellow ferric oxide.
12 CLINICAL PHARMACOLOGY
12.2 Pharmacodynamics
AEMCOLO exposure-response relationships and time course of pharmacodynamic response are unknown.
12.3 Pharmacokinetics
Plasma Concentrations
In healthy adults receiving the recommended dose of 388 mg rifamycin (taken as AEMCOLO) twice daily for 3 days, the maximum observed rifamycin concentration in plasma was 8.72 ng/mL (6 hours after the last dose). A majority (67%) of rifamycin concentrations in plasma were below the limit of quantification (< 2 ng/mL) at this time point.
Absorption
Rifamycin (taken as AEMCOLO) has limited systemic exposure after oral administration of the recommended dosage. Based on total urinary excretion data, bioavailability was < 0.1% under fasting conditions.
Food Effect
A food-effect study involving administration of AEMCOLO to healthy volunteers under a fasted state and with a meal (approximately 1,000 kcal including 500 kcal from fat) indicated that food decreased systemic exposure of rifamycin. The decrease in systemic exposure of rifamycin is not expected to be clinically relevant [see Dosage and Administration (2.2)].
Distribution
Plasma protein binding was approximately 80% in vitro. Binding was primarily to albumin and was inversely proportional to concentration.
Elimination
The apparent half-life of orally administered rifamycin (taken as AEMCOLO) in plasma is unknown.
Specific Populations
The pharmacokinetics of rifamycin (taken as AEMCOLO) in patients with impaired renal or hepatic function have not been studied.
Drug Interaction Studies
Clinical drug-drug interaction studies of rifamycin (taken as AEMCOLO) have not been conducted.
In Vitro Transporter Studies where Drug Interaction Potential Was Not Further Evaluated Clinically
Rifamycin is a substrate of P-glycoprotein (P-gp) and anticipated to be an inhibitor of P-gp and breast cancer resistant protein (BCRP) in the gut.
Rifamycin is an inhibitor of renal transporters organic anion transporter (OAT) 3, multidrug and toxin extrusion (MATE) 1, and MATE2-K transporters in vitro, however, based on systemic concentrations of rifamycin observed after administration of the recommended dose, clinically relevant inhibition of these transporters in vivo is unlikely.
In Vitro Cytochrome P450 (CYP) Studies where Drug Interaction Potential Was Not Further Evaluated Clinically
Rifamycin is an inhibitor of CYP1A2, 2B6, 2C8, 2C9, 2C19, 2D6 and 3A4/5 in vitro, however, based on systemic concentrations of rifamycin observed after administration of the recommended dose clinically relevant inhibition of these enzymes in vivo is unlikely.
Rifamycin is an inducer of CYP3A4 and CYP2B6 but not CYP1A2 in vitro, however, based on systemic concentrations of rifamycin observed after administration of the recommended dose, clinically relevant induction of these enzymes in vivo is unlikely.
Rifamycin is not a substrate of CYPs 1A2, 2B6, 2C9, 2C19, 2D6, 2E1, and 3A4/5.
12.4 Microbiology
Mechanism of Action
Rifamycin belongs to the ansamycin class of antibacterial drugs and acts by inhibiting the beta-subunit of the bacterial DNA-dependent RNA polymerase, blocking one of the steps in DNA transcription. This results in inhibition of bacterial synthesis and consequently growth of bacteria.
Resistance
Resistance to rifamycin is associated with mutations in the RNA polymerase beta subunit. Among E. colistrains, the spontaneous mutation frequency rate of rifamycin ranged from 10 -6to 10 -10at 4× – 16× MIC; the mutation frequency was independent of rifamycin concentration. Increases in the minimum inhibitory concentrations were observed both in vitro and while on treatment following exposure to rifamycin. Cross-resistance between rifamycin and other ansamycins have been observed.
13 NONCLINICAL TOXICOLOGY
14 CLINICAL STUDIES
14.1 Travelers' Diarrhea
The efficacy of AEMCOLO given as 388 mg orally, taken two times a day, for 3 days was evaluated in one multi-center, randomized, double-blind, placebo-controlled trial in adults with travelers' diarrhea. Trial 1 (NCT01142089) was conducted at clinical sites in Guatemala and Mexico, and provides the primary evidence for the efficacy of AEMCOLO. A second active-controlled trial (Trial 2 – NCT01208922) conducted in India, Guatemala and Ecuador, provided supportive evidence for the efficacy of AEMCOLO. Although patients with fever and/or bloody stool at baseline were to be excluded from both trials, 18 subjects treated with AEMCOLO had fever and bloody diarrhea at enrollment in Trial 2. Stool specimens were collected before treatment and 1 to 2 days following the end of treatment to identify enteric pathogens. The predominant pathogen in both trials was E. coli.
The clinical efficacy of AEMCOLO was assessed using an endpoint of time to last unformed (watery or soft) stool (TLUS) before achieving clinical cure. The endpoint of clinical cure was defined as two or fewer soft stools and minimal enteric symptoms at the beginning of a 24-hour period or no unformed stools at the beginning of a 48-hour period. Kaplan-Meier estimates of TLUS for the intent-to-treat (ITT) Population, which includes all randomized subjects, in Trial 1 (Figure 1) show that AEMCOLO significantly reduced the TLUS compared to placebo (p=0.0008).
Figure 1: Kaplan-Meier Estimates of Time to Last Unformed Stool (TLUS) in Trial 1 (ITT Population)
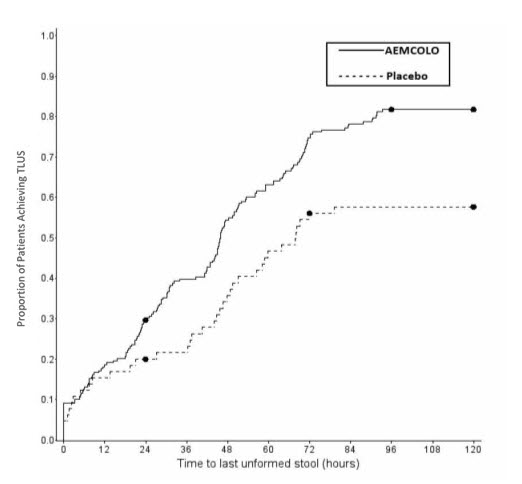
Table 1 displays the median TLUS and the number of patients who achieved clinical cure for the ITT population in Trial 1. The median duration of diarrhea was significantly shorter in patients treated with AEMCOLO than in the placebo group. More patients treated with AEMCOLO were classified as clinical cures than were those in the placebo group.
| AEMCOLO
(N=199) | Placebo
(N=65) | Difference | P value | |
|---|---|---|---|---|
| ITT = Intent-to-Treat; TLUS = time to last unformed stool (in hours) | ||||
|
|
||||
| Median TLUS (hrs) | 46.0 | 68.0 | -22.0 | p = 0.0008 * |
| Clinical cure, n (%) | 162 (81.4%) | 37 (56.9%) | 24.5% | p =0.0001 † |
The results of Trial 2 supported the results presented for Trial 1. In addition, this trial provided evidence that AEMCOLO-treated subjects with fever and/or bloody diarrhea at baseline had prolonged TLUS. [see Warnings and Precautions (5.1)]
15 REFERENCES
- Ziv G, Sulman FG. Evaluation of rifamycin SV and rifampin kinetics in lactating ewes. Antimicrob Agents Chemother.1974;5(2):139-142.
16 HOW SUPPLIED/STORAGE AND HANDLING
AEMCOLO delayed-release tablets contain 194 mg of rifamycin (equivalent to 200 mg of rifamycin sodium), and are yellow brown, ellipsoidal and film coated. These are packaged in blister cards of 6 tablets contained in a cardboard carton. They are supplied as follows:
NDC (57841-1200-1) : carton of 12 tablets (2 blister cards of 6 tablets)
NDC (57841-1200-2) : carton of 36 tablets (6 blister cards of 6 tablets)
17 PATIENT COUNSELING INFORMATION
Persistent Diarrhea
Inform the patient being treated for travelers' diarrhea to discontinue AEMCOLO if diarrhea persists more than 48 hours or worsens. Advise the patient to seek medical care for fever and/or blood in the stool [see Warnings and Precautions (5.1)].
Fever and/or Bloody Stool
Inform the patient that AEMCOLO is not recommended for use if they have fever and/or bloody stool [see Warnings and Precautions (5.1)] .
Clostridium difficile-Associated Diarrhea
Advise patients that diarrhea is a common problem caused by antibacterial drugs, which usually ends when the antibacterial drugs is discontinued. Sometimes after starting treatment with antibacterial drugs, patients can develop watery or bloody stools (with or without stomach cramps and fever) even as late as two or more months after having taken the last dose of AEMCOLO. Inform the patient that if diarrhea occurs after therapy or does not improve or worsens during therapy, patients should contact their physician as soon as possible [see Warnings and Precautions (5.2)].
Important Administration Instructions
Instruct the patients that:
- AEMCOLO tablets should be swallowed whole with a full glass of liquid (6-8 ounces).
- AEMCOLO must not be taken concomitantly with alcohol.
- AEMCOLO tablets must not be chewed, crushed or broken.
- AEMCOLO may be taken with or without food.
Antibacterial Resistance
Patients should be counseled that antibacterial drugs including AEMCOLO should only be used to treat bacterial infections. They do not treat viral infections (e.g., the common cold). When AEMCOLO is prescribed to treat a bacterial infection, patients should be told that although it is common to feel better early in the course of therapy, the medication should be taken exactly as directed. Skipping doses or not completing the full course of therapy may (1) decrease the effectiveness of the immediate treatment and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by AEMCOLO or other antibacterial drugs in the future.
Manufactured for:
RedHill Biopharma Inc.
Raleigh, NC 27617
833-ADR-HILL (833-237-4455)
Manufactured by:
Cosmo S.p.A.
Lainate, Milan, Italy
Made in Italy
U.S. Patents:
http://www.cosmopharma.com/activities/patents
ARTW-0008-000
PRINCIPAL DISPLAY PANEL - 194 mg Tablet Blister Pack Carton
Rx only
NDC 57841-1200-1
194 mg tablets*
Swallow tablet whole.
Do not chew or break.
Aemcolo
®
(rifamycin)
delayed
release tablets
*Each tablet contains:
Rifamycin 194 mg
(equivalent to 200 mg Rifamycin Sodium Salt)
aemcolo.com
12 tablets
(2 cards x
6 tablets each)

PRINCIPAL DISPLAY PANEL - 194 mg Tablet Blister Pack Carton
Rx only
NDC 57841-1201-1
194 mg tablets*
Swallow tablet whole.
Do not chew or break.
Aemcolo
®
(rifamycin)
delayed
release tablets
Sample/Not for Sale
*Each tablet contains:
Rifamycin 194 mg
(equivalent to 200 mg Rifamycin Sodium Salt)
aemcolo.com
4 tablets
(1 card x
4 tablets)

| AEMCOLO
rifamycin tablet, delayed release |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| AEMCOLO
rifamycin tablet, delayed release |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| Labeler - RedHill Biopharma Ltd (533278342) |
Trademark Results [Aemcolo]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 AEMCOLO 87774308 not registered Live/Pending |
Cosmo Technologies Ltd 2018-01-29 |
 AEMCOLO 87593590 not registered Live/Pending |
Cosmo Technologies Ltd 2017-09-01 |
 AEMCOLO 87119637 5885718 Live/Registered |
Cosmo Technologies Ltd 2016-07-28 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.