OZEMPIC- semaglutide injection, solution
Ozempic by
Drug Labeling and Warnings
Ozempic by is a Prescription medication manufactured, distributed, or labeled by REMEDYREPACK INC.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use OZEMPIC ® safely and effectively. See full prescribing information for OZEMPIC.
OZEMPIC (semaglutide) injection, for subcutaneous use
Initial U.S. Approval: 2017WARNING: RISK OF THYROID C-CELL TUMORS
See full prescribing information for complete boxed warning.
- In rodents, semaglutide causes thyroid C-cell tumors. It is unknown whether OZEMPIC causes thyroid C-cell tumors, including medullary thyroid carcinoma (MTC), in humans as the human relevance of semaglutide-induced rodent thyroid C-cell tumors has not been determined ( 5.1, 13.1).
- OZEMPIC is contraindicated in patients with a personal or family history of MTC or in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN 2). Counsel patients regarding the potential risk of MTC and symptoms of thyroid tumors ( 4, 5.1).
INDICATIONS AND USAGE
OZEMPIC is a glucagon-like peptide 1 (GLP-1) receptor agonist indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus ( 1).
Limitations of Use:
- Not recommended as first-line therapy for patients inadequately controlled on diet and exercise ( 1, 5.1).
- Has not been studied in patients with a history of pancreatitis. Consider another antidiabetic therapy ( 1, 5.2).
- Not indicated for use in type 1 diabetes mellitus or treatment of diabetic ketoacidosis ( 1).
DOSAGE AND ADMINISTRATION
- Start at 0.25 mg once weekly. After 4 weeks, increase the dose to 0.5 mg once weekly. If after at least 4 weeks additional glycemic control is needed, increase to 1 mg once weekly ( 2.1).
- Administer once weekly at any time of day, with or without meals ( 2.1).
- If a dose is missed administer within 5 days of missed dose ( 2.1).
- Inject subcutaneously in the abdomen, thigh, or upper arm ( 2.2).
DOSAGE FORMS AND STRENGTHS
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- Pancreatitis: Has been reported in clinical trials. Discontinue promptly if pancreatitis is suspected. Do not restart if pancreatitis is confirmed ( 5.2).
- Diabetic Retinopathy Complications: Has been reported in a clinical trial. Patients with a history of diabetic retinopathy should be monitored ( 5.3).
- Never share an OZEMPIC pen between patients, even if the needle is changed ( 5.4).
- Hypoglycemia: When OZEMPIC is used with an insulin secretagogue or insulin, consider lowering the dose of the secretagogue or insulin to reduce the risk of hypoglycemia ( 5.5).
- Acute Kidney Injury: Monitor renal function in patients with renal impairment reporting severe adverse gastrointestinal reactions ( 5.6).
- Hypersensitivity Reactions: Discontinue OZEMPIC if suspected and promptly seek medical advice ( 5.7).
- Macrovascular outcomes: There have been no clinical studies establishing conclusive evidence of macrovascular risk reduction with semaglutide ( 5.8).
ADVERSE REACTIONS
The most common adverse reactions, reported in ≥5% of patients treated with OZEMPIC are: nausea, vomiting, diarrhea, abdominal pain and constipation ( 6.1).
To report SUSPECTED ADVERSE REACTIONS, contact Novo Nordisk Inc., at 1-888-693-6742 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
Oral Medications: OZEMPIC delays gastric emptying. May impact absorption of concomitantly administered oral medications ( 7.2).
USE IN SPECIFIC POPULATIONS
Females and Males of Reproductive Potential: Discontinue OZEMPIC in women at least 2 months before a planned pregnancy due to the long washout period for semaglutide ( 8.3).
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 7/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: RISK OF THYROID C-CELL TUMORS
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage
2.2 Important Administration Instructions
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Risk of Thyroid C-Cell Tumors
5.2 Pancreatitis
5.3 Diabetic Retinopathy Complications
5.4 Never Share an OZEMPIC Pen Between Patients
5.5 Hypoglycemia with Concomitant Use of Insulin Secretagogues or Insulin
5.6 Acute Kidney Injury
5.7 Hypersensitivity
5.8 Macrovascular Outcomes
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Immunogenicity
7 DRUG INTERACTIONS
7.1 Concomitant Use with an Insulin Secretagogue (e.g., Sulfonylurea) or with Insulin
7.2 Oral Medications
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Overview of Clinical Studies
14.2 Monotherapy Use of OZEMPIC in Patients with Type 2 Diabetes Mellitus
14.3 Combination Therapy Use of OZEMPIC in Patients with Type 2 Diabetes Mellitus
14.4 Cardiovascular Outcomes Trial of OZEMPIC in Patients with Type 2 Diabetes Mellitus
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: RISK OF THYROID C-CELL TUMORS
- In rodents, semaglutide causes dose-dependent and treatment-duration-dependent thyroid C-cell tumors at clinically relevant exposures. It is unknown whether OZEMPIC causes thyroid C-cell tumors, including medullary thyroid carcinoma (MTC), in humans as human relevance of semaglutide-induced rodent thyroid C-cell tumors has not been determined [see Warnings and Precautions ( 5.1) and Nonclinical Toxicology ( 13.1)] .
- OZEMPIC is contraindicated in patients with a personal or family history of MTC or in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN 2) [see Contraindications ( 4)] . Counsel patients regarding the potential risk for MTC with the use of OZEMPIC and inform them of symptoms of thyroid tumors (e.g. a mass in the neck, dysphagia, dyspnea, persistent hoarseness). Routine monitoring of serum calcitonin or using thyroid ultrasound is of uncertain value for early detection of MTC in patients treated with OZEMPIC [see Contraindications ( 4) and Warnings and Precautions ( 5.1)] .
-
1 INDICATIONS AND USAGE
OZEMPIC is indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus [see Clinical Studies ( 14.1)] .
Limitations of Use
- OZEMPIC is not recommended as a first-line therapy for patients who have inadequate glycemic control on diet and exercise because of the uncertain relevance of rodent C-cell tumor findings to humans [see Warnings and Precautions ( 5.1)] .
- OZEMPIC has not been studied in patients with a history of pancreatitis. Consider other antidiabetic therapies in patients with a history of pancreatitis [see Warnings and Precautions (5.2)] .
- OZEMPIC is not a substitute for insulin. OZEMPIC is not indicated for use in patients with type 1 diabetes mellitus or for the treatment of patients with diabetic ketoacidosis, as it would not be effective in these settings.
-
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage
- Start OZEMPIC with a 0.25 mg subcutaneous injection once weekly for 4 weeks. The 0.25 mg dose is intended for treatment initiation and is not effective for glycemic control.
- After 4 weeks on the 0.25 mg dose, increase the dosage to 0.5 mg once weekly.
- If additional glycemic control is needed after at least 4 weeks on the 0.5 mg dose, the dosage may be increased to 1 mg once weekly. The maximum recommended dosage is 1 mg once weekly.
- Administer OZEMPIC once weekly, on the same day each week, at any time of the day, with or without meals.
- The day of weekly administration can be changed if necessary as long as the time between two doses is at least 2 days (>48 hours).
- If a dose is missed, administer OZEMPIC as soon as possible within 5 days after the missed dose. If more than 5 days have passed, skip the missed dose and administer the next dose on the regularly scheduled day. In each case, patients can then resume their regular once weekly dosing schedule.
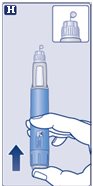
2.2 Important Administration Instructions
- Administer OZEMPIC subcutaneously to the abdomen, thigh, or upper arm. Instruct patients to use a different injection site each week when injecting in the same body region.
- Inspect OZEMPIC visually before use. It should appear clear and colorless. Do not use OZEMPIC if particulate matter and coloration is seen.
- When using OZEMPIC with insulin, instruct patients to administer as separate injections and to never mix the products. It is acceptable to inject OZEMPIC and insulin in the same body region but the injections should not be adjacent to each other.
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Risk of Thyroid C-Cell Tumors
In mice and rats, semaglutide caused a dose-dependent and treatment-duration-dependent increase in the incidence of thyroid C-cell tumors (adenomas and carcinomas) after lifetime exposure at clinically relevant plasma exposures [see Nonclinical Toxicology ( 13.1)] . It is unknown whether OZEMPIC causes thyroid C-cell tumors, including medullary thyroid carcinoma (MTC), in humans as human relevance of semaglutide-induced rodent thyroid C-cell tumors has not been determined.
Cases of MTC in patients treated with liraglutide, another GLP-1 receptor agonist, have been reported in the postmarketing period; the data in these reports are insufficient to establish or exclude a causal relationship between MTC and GLP-1 receptor agonist use in humans.
OZEMPIC is contraindicated in patients with a personal or family history of MTC or in patients with MEN 2. Counsel patients regarding the potential risk for MTC with the use of OZEMPIC and inform them of symptoms of thyroid tumors (e.g. a mass in the neck, dysphagia, dyspnea, persistent hoarseness).
Routine monitoring of serum calcitonin or using thyroid ultrasound is of uncertain value for early detection of MTC in patients treated with OZEMPIC. Such monitoring may increase the risk of unnecessary procedures, due to the low test specificity for serum calcitonin and a high background incidence of thyroid disease. Significantly elevated serum calcitonin value may indicate MTC and patients with MTC usually have calcitonin values >50 ng/L. If serum calcitonin is measured and found to be elevated, the patient should be further evaluated. Patients with thyroid nodules noted on physical examination or neck imaging should also be further evaluated.
5.2 Pancreatitis
In glycemic control trials, acute pancreatitis was confirmed by adjudication in 7 OZEMPIC-treated patients (0.3 cases per 100 patient years) versus 3 in comparator-treated patients (0.2 cases per 100 patient years). One case of chronic pancreatitis was confirmed in an OZEMPIC-treated patient. In a 2-year trial, acute pancreatitis was confirmed by adjudication in 8 OZEMPIC-treated patients (0.27 cases per 100 patient years) and 10 placebo-treated patients (0.33 cases per 100 patient years), both on a background of standard of care.
After initiation of OZEMPIC, observe patients carefully for signs and symptoms of pancreatitis (including persistent severe abdominal pain, sometimes radiating to the back and which may or may not be accompanied by vomiting). If pancreatitis is suspected, OZEMPIC should be discontinued and appropriate management initiated; if confirmed, OZEMPIC should not be restarted.
5.3 Diabetic Retinopathy Complications
In a 2-year trial involving patients with type 2 diabetes and high cardiovascular risk, more events of diabetic retinopathy complications occurred in patients treated with OZEMPIC (3.0%) compared to placebo (1.8%). The absolute risk increase for diabetic retinopathy complications was larger among patients with a history of diabetic retinopathy at baseline (OZEMPIC 8.2%, placebo 5.2%) than among patients without a known history of diabetic retinopathy (OZEMPIC 0.7%, placebo 0.4%).
Rapid improvement in glucose control has been associated with a temporary worsening of diabetic retinopathy. The effect of long-term glycemic control with semaglutide on diabetic retinopathy complications has not been studied. Patients with a history of diabetic retinopathy should be monitored for progression of diabetic retinopathy.
5.4 Never Share an OZEMPIC Pen Between Patients
OZEMPIC pens must never be shared between patients, even if the needle is changed. Pen-sharing poses a risk for transmission of blood-borne pathogens.
5.5 Hypoglycemia with Concomitant Use of Insulin Secretagogues or Insulin
The risk of hypoglycemia is increased when OZEMPIC is used in combination with insulin secretagogues (e.g., sulfonylureas) or insulin. Patients may require a lower dose of the secretagogue or insulin to reduce the risk of hypoglycemia in this setting [see Adverse Reactions ( 6.1), Drug Interactions ( 7.1)] .
5.6 Acute Kidney Injury
There have been postmarketing reports of acute kidney injury and worsening of chronic renal failure, which may sometimes require hemodialysis, in patients treated with GLP-1 receptor agonists. Some of these events have been reported in patients without known underlying renal disease. A majority of the reported events occurred in patients who had experienced nausea, vomiting, diarrhea, or dehydration. Monitor renal function when initiating or escalating doses of OZEMPIC in patients reporting severe adverse gastrointestinal reactions.
5.7 Hypersensitivity
Serious hypersensitivity reactions (e.g., anaphylaxis, angioedema) have been reported with GLP-1 receptor agonists. If hypersensitivity reactions occur, discontinue use of OZEMPIC; treat promptly per standard of care, and monitor until signs and symptoms resolve. Do not use in patients with a previous hypersensitivity to OZEMPIC [see Contraindications ( 4)] .
Anaphylaxis and angioedema have been reported with other GLP-1 receptor agonists. Use caution in a patient with a history of angioedema or anaphylaxis with another GLP-1 receptor agonist because it is unknown whether such patients will be predisposed to anaphylaxis with OZEMPIC.
-
6 ADVERSE REACTIONS
The following serious adverse reactions are described below or elsewhere in the prescribing information:
Risk of Thyroid C-cell Tumors [see Warnings and Precautions ( 5.1)]
Pancreatitis [see Warnings and Precautions ( 5.2)]
Diabetic Retinopathy Complications [see Warnings and Precautions ( 5.3)]
Hypoglycemia with Concomitant Use of Insulin Secretagogues or Insulin [see Warnings and Precautions ( 5.5)]
Acute Kidney Injury [see Warnings and Precautions ( 5.6)]
Hypersensitivity [see Warnings and Precautions ( 5.7)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Pool of Placebo-Controlled Trials
The data in Table 1 are derived from 2 placebo-controlled trials (1 monotherapy trial and 1 trial in combination with basal insulin) in patients with type 2 diabetes [see Clinical Studies ( 14)] . These data reflect exposure of 521 patients to OZEMPIC and a mean duration of exposure to OZEMPIC of 32.9 weeks. Across the treatment arms, the mean age of patients was 56 years, 3.4% were 75 years or older and 55% were male. In these trials 71% were White, 7% were Black or African American, and 19% were Asian; 21% identified as Hispanic or Latino ethnicity. At baseline, patients had type 2 diabetes for an average of 8.8 years and had a mean HbA 1c of 8.2%. At baseline, 8.9% of the population reported retinopathy. Baseline estimated renal function was normal (eGFR ≥90 mL/min/1.73m 2) in 57.2%, mildly impaired (eGFR 60 to 90 mL/min/1.73m 2) in 35.9% and moderately impaired (eGFR 30 to 60 mL/min/1.73m 2) in 6.9% of patients.
Pool of Placebo- and Active-Controlled Trials
The occurrence of adverse reactions was also evaluated in a larger pool of patients with type 2 diabetes
participating in 7 placebo- and active-controlled glycemic control trials [see Clinical Studies ( 14)] including two trials in Japanese patients evaluating the use of OZEMPIC as monotherapy and add-on therapy to oral medications or insulin. In this pool, a total of 3150 patients with type 2 diabetes were treated with OZEMPIC for a mean duration of 44.9 weeks. Across the treatment arms, the mean age of patients was 57 years, 3.2% were 75 years or older and 57% were male. In these trials, 60% were White, 6% were Black or African American, and 31% were Asian; 16% identified as Hispanic or Latino ethnicity. At baseline, patients had type 2 diabetes for an average of 8.2 years and had a mean HbA 1c of 8.2%. At baseline, 7.8% of the population reported retinopathy. Baseline estimated renal function was normal (eGFR ≥90 mL/min/1.73m 2) in 63.1%, mildly impaired (eGFR 60 to 90 mL/min/1.73m 2) in 34.3%, and moderately impaired (eGFR 30 to 60 mL/min/1.73m 2) in 2.5% of the patients.
Common Adverse Reactions
Table 1 shows common adverse reactions, excluding hypoglycemia, associated with the use of OZEMPIC in the pool of placebo-controlled trials. These adverse reactions occurred more commonly on OZEMPIC than on placebo, and occurred in at least 5% of patients treated with OZEMPIC.
Table 1. Adverse Reactions in Placebo-Controlled Trials Reported in ≥5% of OZEMPIC-Treated Patients with Type 2 Diabetes Mellitus
Adverse Reaction
Placebo
(N=262)
%
OZEMPIC 0.5 mg
(N=260)
%
OZEMPIC 1 mg
(N=261)
%
Nausea
6.1
15.8
20.3
Vomiting
2.3
5.0
9.2
Diarrhea
1.9
8.5
8.8
Abdominal pain
4.6
7.3
5.7
Constipation
1.5
5.0
3.1
In the pool of placebo- and active-controlled trials and in the 2-year cardiovascular outcomes trial, the types and frequency of common adverse reactions, excluding hypoglycemia, were similar to those listed in Table 1.
Gastrointestinal Adverse Reactions
In the pool of placebo-controlled trials, gastrointestinal adverse reactions occurred more frequently among patients receiving OZEMPIC than placebo (placebo 15.3%, OZEMPIC 0.5 mg 32.7%, OZEMPIC 1 mg 36.4%). The majority of reports of nausea, vomiting, and/or diarrhea occurred during dose escalation. More patients receiving OZEMPIC 0.5 mg (3.1%) and OZEMPIC 1 mg (3.8%) discontinued treatment due to gastrointestinal adverse reactions than patients receiving placebo (0.4%).
- In addition to the reactions in Table 1, the following gastrointestinal adverse reactions with a frequency of <5% were associated with OZEMPIC (frequencies listed, respectively, as: placebo; 0.5 mg; 1 mg): dyspepsia (1.9%, 3.5%, 2.7%), eructation (0%, 2.7%, 1.1%), flatulence (0.8%, 0.4%, 1.5%), gastroesophageal reflux disease (0%, 1.9%, 1.5%), and gastritis (0.8%, 0.8%, 0.4%).
Other Adverse Reactions
Hypoglycemia
Table 2 summarizes the incidence of events related to hypoglycemia by various definitions in the placebo-controlled trials.
Table 2. Hypoglycemia Adverse Reactions in Placebo-Controlled Trials In Patients with Type 2 Diabetes Mellitus
Placebo
OZEMPIC 0.5 mg
OZEMPIC 1 mg
Monotherapy
(30 weeks)
N=129
N=127
N=130
Severe †
0%
0%
0%
- Documented symptomatic (≤70 mg/dL glucose threshold)
0%
1.6%
3.8%
- Severe † or Blood Glucose Confirmed Symptomatic (≤56 mg/dL glucose threshold)
1.6%
0%
0%
Add-on to Basal Insulin with or without Metformin
(30 weeks)
N=132
N=132
N=131
Severe †
0%
0%
1.5%
- Documented symptomatic (≤70 mg/dL glucose threshold)
15.2%
16.7%
29.8%
- Severe † or Blood Glucose Confirmed Symptomatic (≤56 mg/dL glucose threshold)
5.3%
8.3%
10.7%
† “Severe” hypoglycemia adverse reactions are episodes requiring the assistance of another person.
Hypoglycemia was more frequent when OZEMPIC was used in combination with a sulfonylurea [see Warnings and Precautions ( 5.5) and Clinical Studies ( 14)]. Severe hypoglycemia occurred in 0.8% and 1.2% of patients when OZEMPIC 0.5 mg and 1 mg, respectively, was co-administered with a sulfonylurea. Documented symptomatic hypoglycemia occurred in 17.3% and 24.4% of patients when OZEMPIC 0.5 mg and 1 mg, respectively, was co-administered with a sulfonylurea. Severe or blood glucose confirmed symptomatic hypoglycemia occurred in 6.5% and 10.4% of patients when OZEMPIC 0.5 mg and 1 mg, respectively, was co-administered with a sulfonylurea.
Injection Site Reactions
In placebo-controlled trials, injection site reactions (e.g., injection-site discomfort, erythema) were reported in 0.2% of OZEMPIC-treated patients.
Increases in Amylase and Lipase
In placebo-controlled trials, patients exposed to OZEMPIC had a mean increase from baseline in amylase of 13% and lipase of 22%. These changes were not observed in placebo-treated patients.
Cholelithiasis
In placebo-controlled trials, cholelithiasis was reported in 1.5% and 0.4% of patients-treated with OZEMPIC 0.5 mg and 1 mg, respectively. Cholelithiasis was not reported in placebo-treated patients.
Increases in Heart Rate
In placebo-controlled trials, OZEMPIC 0.5 mg and 1 mg resulted in a mean increase in heart rate of 2 to 3 beats per minute. There was a mean decrease in heart rate of 0.3 beats per minute in placebo-treated patients.
Fatigue, Dysgeusia and Dizziness
Other adverse reactions with a frequency of >0.4% were associated with OZEMPIC include fatigue, dysgeusia and dizziness.
6.2 Immunogenicity
Consistent with the potentially immunogenic properties of protein and peptide pharmaceuticals, patients treated with OZEMPIC may develop anti-semaglutide antibodies. The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, the incidence of antibodies to semaglutide in the studies described below cannot be directly compared with the incidence of antibodies in other studies or to other products.
Across the placebo- and active-controlled glycemic control trials, 32 (1.0%) OZEMPIC-treated patients developed anti-drug antibodies (ADAs) to the active ingredient in OZEMPIC (i.e., semaglutide). Of the 32 semaglutide-treated patients that developed semaglutide ADAs, 19 patients (0.6% of the overall population) developed antibodies cross-reacting with native GLP-1. The in vitro neutralizing activity of the antibodies is uncertain at this time.
-
7 DRUG INTERACTIONS
7.1 Concomitant Use with an Insulin Secretagogue (e.g., Sulfonylurea) or with Insulin
The risk of hypoglycemia is increased when OZEMPIC is used in combination with insulin secretagogues (e.g., sulfonylureas) or insulin. The risk of hypoglycemia may be lowered by a reduction in the dose of sulfonylurea (or other concomitantly administered insulin secretagogues) or insulin [see Warnings and Precautions ( 5.5)] .
7.2 Oral Medications
OZEMPIC causes a delay of gastric emptying, and thereby has the potential to impact the absorption of concomitantly administered oral medications. In clinical pharmacology trials, semaglutide did not affect the absorption of orally administered medications to any clinically relevant degree [see Clinical Pharmacology ( 12.3)] . Nonetheless, caution should be exercised when oral medications are concomitantly administered with OZEMPIC.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There are limited data with semaglutide use in pregnant women to inform a drug-associated risk for adverse developmental outcomes. There are clinical considerations regarding the risks of poorly controlled diabetes in pregnancy (see Clinical Considerations). Based on animal reproduction studies, there may be potential risks to the fetus from exposure to semaglutide during pregnancy. OZEMPIC should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
In pregnant rats administered semaglutide during organogenesis, embryofetal mortality, structural abnormalities and alterations to growth occurred at maternal exposures below the maximum recommended human dose (MRHD) based on AUC. In rabbits and cynomolgus monkeys administered semaglutide during organogenesis, early pregnancy losses and structural abnormalities were observed at below the MRHD (rabbit) and ≥5-fold the MRHD (monkey). These findings coincided with a marked maternal body weight loss in both animal species (see Data).
The estimated background risk of major birth defects is 6–10% in women with pre-gestational diabetes with an HbA 1c >7 and has been reported to be as high as 20–25% in women with a HbA 1c >10. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively.
Clinical Considerations
Disease associated maternal and fetal risk
Poorly controlled diabetes during pregnancy increases the maternal risk for diabetic ketoacidosis, pre- eclampsia, spontaneous abortions, preterm delivery, stillbirth and delivery complications. Poorly controlled diabetes increases the fetal risk for major birth defects, stillbirth, and macrosomia related morbidity.
Data
Animal Data
In a combined fertility and embryofetal development study in rats, subcutaneous doses of 0.01, 0.03 and 0.09 mg/kg/day (0.1-, 0.4-, and 1.1-fold the MRHD) were administered to males for 4 weeks prior to and throughout mating and to females for 2 weeks prior to mating, and throughout organogenesis to Gestation Day 17. In parental animals, pharmacologically mediated reductions in body weight gain and food consumption were observed at all dose levels. In the offspring, reduced growth and fetuses with visceral (heart blood vessels) and skeletal (cranial bones, vertebra, ribs) abnormalities were observed at the human exposure.
In an embryofetal development study in pregnant rabbits, subcutaneous doses of 0.0010, 0.0025 or 0.0075 mg/kg/day (0.03-, 0.3-, and 2.3-fold the MRHD) were administered throughout organogenesis from Gestation Day 6 to 19. Pharmacologically mediated reductions in maternal body weight gain and food consumption were observed at all dose levels. Early pregnancy losses and increased incidences of minor visceral (kidney, liver) and skeletal (sternebra) fetal abnormalities were observed at ≥0.0025 mg/kg/day, at clinically relevant exposures.
In an embryofetal development study in pregnant cynomolgus monkeys, subcutaneous doses of 0.015, 0.075, and 0.15 mg/kg twice weekly (1.0-, 5.2-, and 14.9-fold the MRHD) were administered throughout organogenesis, from Gestation Day 16 to 50. Pharmacologically mediated, marked initial maternal body weight loss and reductions in body weight gain and food consumption coincided with the occurrence of sporadic abnormalities (vertebra, sternebra, ribs) at ≥0.075 mg/kg twice weekly ( >5X human exposure).
In a pre- and postnatal development study in pregnant cynomolgus monkeys, subcutaneous doses of 0.015, 0.075, and 0.15 mg/kg twice weekly (0.7-, 3.3-, and 7.2-fold the MRHD) were administered from Gestation Day 16 to 140. Pharmacologically mediated marked initial maternal body weight loss and reductions in body weight gain and food consumption coincided with an increase in early pregnancy losses and led to delivery of slightly smaller offspring at ≥0.075 mg/kg twice weekly ( >3X human exposure).
8.2 Lactation
Risk Summary
There are no data on the presence of semaglutide in human milk, the effects on the breastfed infant, or the effects on milk production. Semaglutide was present in the milk of lactating rats, however, due to species-specific differences in lactation physiology, the clinical relevance of these data are not clear (see Data). The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for OZEMPIC and any potential adverse effects on the breastfed infant from OZEMPIC or from the underlying maternal condition.
Data
In lactating rats, semaglutide was detected in milk at levels 3-12 fold lower than in maternal plasma.
8.3 Females and Males of Reproductive Potential
Discontinue OZEMPIC in women at least 2 months before a planned pregnancy due to the long washout period for semaglutide [see Use in Specific Populations ( 8.1)] .
8.4 Pediatric Use
Safety and efficacy of OZEMPIC have not been established in pediatric patients (younger than 18 years).
8.5 Geriatric Use
In the pool of placebo- and active-controlled glycemic control trials, 744 (23.6%) OZEMPIC-treated patients were 65 years of age and over and 102 OZEMPIC-treated patients (3.2%) patients were 75 years of age and over. In SUSTAIN 6, the cardiovascular outcome trial, 788 (48.0%) OZEMPIC-treated patients were 65 years of age and over and 157 OZEMPIC-treated patients (9.6%) patients were 75 years of age and over.
No overall differences in safety or efficacy were detected between these patients and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
8.6 Renal Impairment
No dose adjustment of OZEMPIC is recommended for patients with renal impairment. In subjects with renal impairment including end-stage renal disease (ESRD), no clinically relevant change in semaglutide pharmacokinetics (PK) was observed [see Clinical Pharmacology ( 12.3)] .
8.7 Hepatic Impairment
No dose adjustment of OZEMPIC is recommended for patients with hepatic impairment. In a study in subjects with different degrees of hepatic impairment, no clinically relevant change in semaglutide pharmacokinetics (PK) was observed [see Clinical Pharmacology ( 12.3)] .
- 10 OVERDOSAGE
-
11 DESCRIPTION
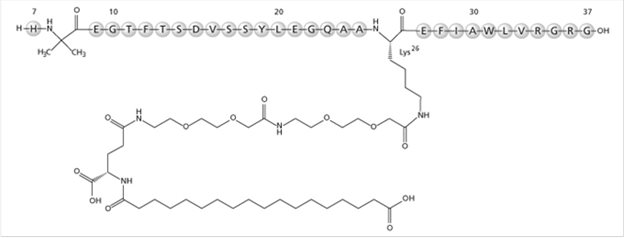
OZEMPIC (semaglutide) injection, for subcutaneous use, contains semaglutide, a human GLP-1 receptor agonist (or GLP-1 analog). The peptide backbone is produced by yeast fermentation. The main protraction mechanism of semaglutide is albumin binding, facilitated by modification of position 26 lysine with a hydrophilic spacer and a C18 fatty di-acid. Furthermore, semaglutide is modified in position 8 to provide stabilization against degradation by the enzyme dipeptidyl-peptidase 4 (DPP-4). A minor modification was made in position 34 to ensure the attachment of only one fatty di-acid. The molecular formula is C 187H 291N 45O 59 and the molecular weight is 4113.58 g/mol.
Structural formula:
OZEMPIC is a sterile, aqueous, clear, colorless solution. Each pre-filled pen contains a 1.5 mL solution of OZEMPIC equivalent to 2 mg semaglutide. Each 1 mL of OZEMPIC solution contains 1.34 mg of semaglutide and the following inactive ingredients: disodium phosphate dihydrate, 1.42 mg; propylene glycol, 14.0 mg; phenol, 5.50 mg; and water for injections. OZEMPIC has a pH of approximately 7.4. Hydrochloric acid or sodium hydroxide may be added to adjust pH.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Semaglutide is a GLP-1 analogue with 94% sequence homology to human GLP-1. Semaglutide acts as a GLP-1 receptor agonist that selectively binds to and activates the GLP-1 receptor, the target for native GLP-1.
GLP-1 is a physiological hormone that has multiple actions on glucose, mediated by the GLP-1 receptors.
The principal mechanism of protraction resulting in the long half-life of semaglutide is albumin binding, which results in decreased renal clearance and protection from metabolic degradation. Furthermore, semaglutide is stabilized against degradation by the DPP-4 enzyme.
Semaglutide reduces blood glucose through a mechanism where it stimulates insulin secretion and lowers glucagon secretion, both in a glucose-dependent manner. Thus, when blood glucose is high, insulin secretion is stimulated and glucagon secretion is inhibited. The mechanism of blood glucose lowering also involves a minor delay in gastric emptying in the early postprandial phase.
12.2 Pharmacodynamics
Semaglutide lowers fasting and postprandial blood glucose and reduces body weight. All pharmacodynamic evaluations were performed after 12 weeks of treatment (including dose escalation) at steady state with semaglutide 1 mg.
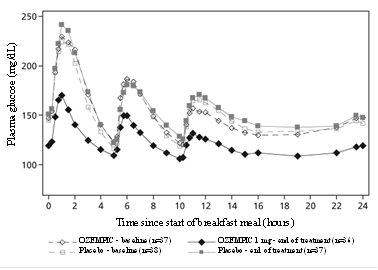
Fasting and Postprandial Glucose
Semaglutide reduces fasting and postprandial glucose concentrations. In patients with type 2 diabetes, treatment with semaglutide 1 mg resulted in reductions in glucose in terms of absolute change from baseline and relative reduction compared to placebo of 29 mg/dL (22%) for fasting glucose, 74 mg/dL (36%) for 2 hour postprandial glucose, and 30 mg/dL (22%) for mean 24 hour glucose concentration (see Figure 1).
Figure 1. Mean 24 hour plasma glucose profiles (standardized meals) in patients with type 2 diabetes before (baseline) and after 12 weeks of treatment with semaglutide or placebo
Insulin Secretion
Both first-and second-phase insulin secretion are increased in patients with type 2 diabetes treated with OZEMPIC compared with placebo.
Glucagon Secretion
Semaglutide lowers the fasting and postprandial glucagon concentrations. In patients with type 2 diabetes, treatment with semaglutide resulted in the following relative reductions in glucagon compared to placebo, fasting glucagon (8%), postprandial glucagon response (14-15%), and mean 24 hour glucagon concentration (12%).
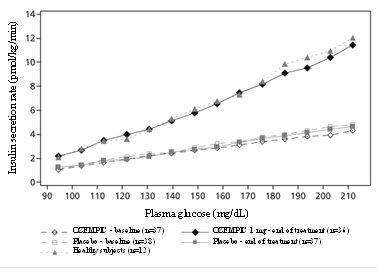
Glucose dependent insulin and glucagon secretion
Semaglutide lowers high blood glucose concentrations by stimulating insulin secretion and lowering glucagon secretion in a glucose-dependent manner. With semaglutide, the insulin secretion rate in patients with type 2 diabetes was similar to that of healthy subjects (see Figure 2).
Figure 2. Mean insulin secretion rate versus glucose concentration in patients with type 2 diabetes during graded glucose infusion before (baseline) and after 12 weeks of treatment with semaglutide or placebo and in untreated healthy subjects
During induced hypoglycemia, semaglutide did not alter the counter regulatory responses of increased glucagon compared to placebo, and did not impair the decrease of C-peptide in patients with type 2 diabetes.
Gastric emptying
Semaglutide causes a delay of early postprandial gastric emptying, thereby reducing the rate at which glucose appears in the circulation postprandially.
Cardiac electrophysiology (QTc)
The effect of semaglutide on cardiac repolarization was tested in a thorough QTc trial. At a dose 1.5 times the maximum recommended dose, semaglutide does not prolong QTc intervals to any clinically relevant extent.
12.3 Pharmacokinetics
Absorption
Absolute bioavailability of semaglutide is 89%. Maximum concentration of semaglutide is reached 1 to 3 days post dose.
Similar exposure is achieved with subcutaneous administration of semaglutide in the abdomen, thigh, or upper arm.
In patients with type 2 diabetes, semaglutide exposure increases in a dose-proportional manner for once-weekly doses of 0.5 mg and 1 mg. Steady-state exposure is achieved following 4-5 weeks of once-weekly administration. In patients with type 2 diabetes, the mean population-PK estimated steady-state concentrations following once weekly subcutaneous administration of 0.5 mg and 1 mg semaglutide were approximately 65.0 ng/mL and 123.0 ng/mL, respectively.
Distribution
The mean apparent volume of distribution of semaglutide following subcutaneous administration in patients with type 2 diabetes is approximately 12.5 L. Semaglutide is extensively bound to plasma albumin (>99%).
Elimination
The apparent clearance of semaglutide in patients with type 2 diabetes is approximately 0.05 L/h. With an elimination half-life of approximately 1 week, semaglutide will be present in the circulation for about 5 weeks after the last dose.
Metabolism
The primary route of elimination for semaglutide is metabolism following proteolytic cleavage of the peptide backbone and sequential beta-oxidation of the fatty acid sidechain.
Excretion
The primary excretion routes of semaglutide-related material is via the urine and feces. Approximately 3% of the dose is excreted in the urine as intact semaglutide.
Specific Populations
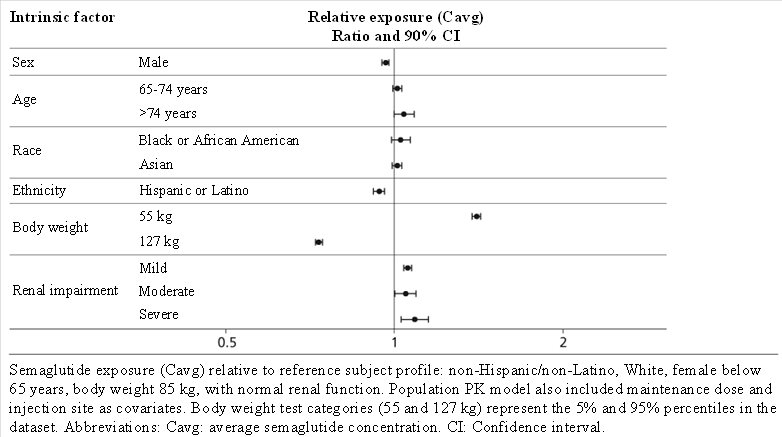
Based on a population pharmacokinetic analysis, age, sex, race, and ethnicity, and renal impairment do not have a clinically meaningful effect on the pharmacokinetics of semaglutide. The exposure of semaglutide decreases with an increase in body weight. However, semaglutide doses of 0.5 mg and 1 mg provide adequate systemic exposure over the body weight range of 40-198 kg evaluated in the clinical trials. The effects of intrinsic factors on the pharmacokinetics of semaglutide are shown in Figure 3.
Figure 3. Impact of intrinsic factors on semaglutide exposure
Patients with Renal impairment - Renal impairment does not impact the pharmacokinetics of semaglutide in a clinically relevant manner. This was shown in a study with a single dose of 0.5 mg semaglutide in patients with different degrees of renal impairment (mild, moderate, severe, ESRD) compared with subjects with normal renal function. This was also shown for subjects with both type 2 diabetes and renal impairment based on data from clinical studies (Figure 3).
Patients with Hepatic impairment - Hepatic impairment does not have any impact on the exposure of semaglutide. The pharmacokinetics of semaglutide were evaluated in patients with different degrees of hepatic impairment (mild, moderate, severe) compared with subjects with normal hepatic function in a study with a single-dose of 0.5 mg semaglutide.
Pediatric Patients- Semaglutide has not been studied in pediatric patients.
Drug Interaction Studies
In vitro studies have shown very low potential for semaglutide to inhibit or induce CYP enzymes, and to inhibit drug transporters.
The delay of gastric emptying with semaglutide may influence the absorption of concomitantly administered oral medicinal products. The potential effect of semaglutide on the absorption of co-administered oral medications was studied in trials at semaglutide 1 mg steady-state exposure.
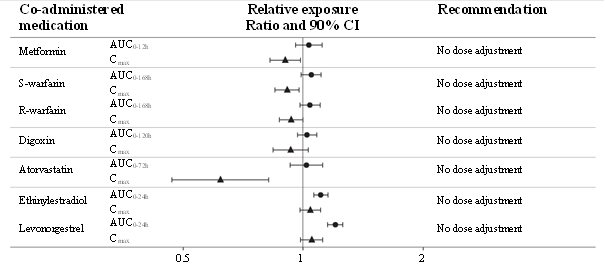
No clinically relevant drug-drug interaction with semaglutide (Figure 4) was observed based on the evaluated medications; therefore, no dose adjustment is required when co-administered with semaglutide.
Figure 4. Impact of semaglutide on the exposure of co-administered oral medications
Relative exposure in terms of AUC and C max for each medication when given with semaglutide compared to without semaglutide. Metformin and oral contraceptive drug (ethinylestradiol/levonorgestrel) were assessed at steady state. Warfarin (S-warfarin/R-warfarin), digoxin and atorvastatin were assessed after a single dose.
Abbreviations: AUC: area under the curve. C max: maximum concentration. CI: confidence interval.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
In a 2-year carcinogenicity study in CD-1 mice, subcutaneous doses of 0.3, 1 and 3 mg/kg/day [5-, 17-, and 59-fold the maximum recommended human dose (MRHD) of 1 mg/week, based on AUC] were administered to the males, and 0.1, 0.3 and 1 mg/kg/day (2-, 5-, and 17-fold MRHD) were administered to the females. A statistically significant increase in thyroid C-cell adenomas and a numerical increase in C-cell carcinomas were observed in males and females at all dose levels ( >2X human exposure).
- In a 2-year carcinogenicity study in Sprague Dawley rats, subcutaneous doses of 0.0025, 0.01, 0.025 and 0.1 mg/kg/day were administered (below quantification, 0.4-, 1-, and 6-fold the exposure at the MRHD). A statistically significant increase in thyroid C-cell adenomas was observed in males and females at all dose levels, and a statistically significant increase in thyroid C-cell carcinomas was observed in males at ≥0.01 mg/kg/day, at clinically relevant exposures.
Human relevance of thyroid C-cell tumors in rats is unknown and could not be determined by clinical studies or nonclinical studies [see Boxed Warning and Warnings and Precautions ( 5.1)] .
Semaglutide was not mutagenic or clastogenic in a standard battery of genotoxicity tests (bacterial mutagenicity (Ames), human lymphocyte chromosome aberration, rat bone marrow micronucleus).
In a combined fertility and embryo-fetal development study in rats, subcutaneous doses of 0.01, 0.03 and 0.09 mg/kg/day (0.1-, 0.4-, and 1.1-fold the MRHD) were administered to male and female rats. Males were dosed for 4 weeks prior to mating, and females were dosed for 2 weeks prior to mating and throughout organogenesis until Gestation Day 17. No effects were observed on male fertility. In females, an increase in oestrus cycle length was observed at all dose levels, together with a small reduction in numbers of corpora lutea at ≥0.03 mg/kg/day. These effects were likely an adaptive response secondary to the pharmacological effect of semaglutide on food consumption and body weight.
-
14 CLINICAL STUDIES
14.1 Overview of Clinical Studies
OZEMPIC has been studied as monotherapy and in combination with metformin, metformin and sulfonylureas, metformin and/or thiazolidinedione, and basal insulin in patients with type 2 diabetes mellitus. The efficacy of OZEMPIC was compared with placebo, sitagliptin, exenatide extended-release (ER), and insulin glargine.
Most trials evaluated the use of OZEMPIC 0.5 mg, and 1 mg, with the exception of the trial comparing OZEMPIC and exenatide ER where only the 1 mg dose was studied.
In patients with type 2 diabetes mellitus, OZEMPIC produced clinically relevant reduction from baseline in HbA 1c compared with placebo.
The efficacy of OZEMPIC was not impacted by age, gender, race, ethnicity, BMI at baseline, body weight (kg) at baseline, diabetes duration and level of renal function impairment.
14.2 Monotherapy Use of OZEMPIC in Patients with Type 2 Diabetes Mellitus
In a 30-week double-blind trial (NCT02054897), 388 patients with type 2 diabetes mellitus inadequately controlled with diet and exercise were randomized to OZEMPIC 0.5 mg or OZEMPIC 1 mg once weekly or placebo. Patients had a mean age of 54 years and 54% were men. The mean duration of type 2 diabetes was 4.2 years, and the mean BMI was 33 kg/m 2. Overall, 64% were White, 8% were Black or African American, and 21% were Asian; 30% identified as Hispanic or Latino ethnicity.
Monotherapy with OZEMPIC 0.5 mg and 1 mg once weekly for 30 weeks resulted in a statistically significant reduction in HbA 1c compared with placebo (see Table 3).
Table 3. Results at Week 30 in a Trial of OZEMPIC as Monotherapy in Adult Patients with Type 2 Diabetes Mellitus Inadequately Controlled with Diet and Exercise
Placebo
OZEMPIC
0.5 mg
OZEMPIC
1 mg
Intent-to-Treat (ITT) Population (N) a
129
128
130
HbA 1c (%)
- Baseline (mean)
8.0
8.1
8.1
- Change at week 30 b
-0.1
-1.4
-1.6
- Difference from placebo b [95% CI]
-1.2 [-1.5, -0.9] c
-1.4 [-1.7, -1.1] c
Patients (%) achieving HbA 1c <7%
28
73
70
FPG (mg/dL)
- Baseline (mean)
174
174
179
- Change at week 30 b
-15
-41
-44
aThe intent-to-treat population includes all randomized and exposed patients. At week 30 the primary HbA 1c endpoint was missing for 10%, 7% and 7% of patients and during the trial rescue medication was initiated by 20%, 5% and 4% of patients randomized to placebo, OZEMPIC 0.5 mg and OZEMPIC 1 mg, respectively. Missing data were imputed using multiple imputation based on retrieved dropouts.
bIntent-to-treat analysis using ANCOVA adjusted for baseline value and country.
cp<0.0001 (2-sided) for superiority, adjusted for multiplicity.
The mean baseline body weight was 89.1 kg, 89.8 kg, 96.9 kg in the placebo, OZEMPIC 0.5 mg, and OZEMPIC 1 mg arms, respectively. The mean changes from baseline to week 30 were -1.2 kg, -3.8 kg and -4.7 kg in the placebo, OZEMPIC 0.5 mg, and OZEMPIC 1 mg arms, respectively. The difference from placebo (95% CI) for OZEMPIC 0.5 mg was -2.6 kg (-3.8, -1.5), and for OZEMPIC 1 mg was -3.5 kg (-4.8, -2.2).
14.3 Combination Therapy Use of OZEMPIC in Patients with Type 2 Diabetes Mellitus
Combination with metformin and/or thiazolidinediones
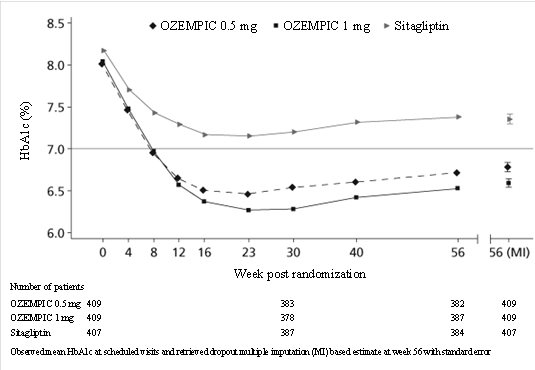
In a 56-week, double-blind trial (NCT01930188), 1231 patients with type 2 diabetes mellitus were randomized to OZEMPIC 0.5 mg once weekly, OZEMPIC 1 mg once weekly, or sitagliptin 100 mg once daily, all in combination with metformin (94%) and/or thiazolidinediones (6%). Patients had a mean age of 55 years and 51% were men. The mean duration of type 2 diabetes was 6.6 years, and the mean BMI was 32 kg/m 2. Overall, 68% were White, 5% were Black or African American, and 25% were Asian; 17% identified as Hispanic or Latino ethnicity.
Treatment with OZEMPIC 0.5 mg and 1 mg once weekly for 56 weeks resulted in a statistically significant reduction in HbA 1c compared to sitagliptin (see Table 4 and Figure 5).
Table 4. Results at Week 56 in a Trial of OZEMPIC Compared to Sitagliptin in Adult Patients with Type 2 Diabetes Mellitus In Combination with Metformin and/or Thiazolidinediones
OZEMPIC
0.5 mg
OZEMPIC
1 mg
Sitagliptin
Intent-to-Treat (ITT) Population (N) a
409
409
407
HbA 1c (%)
- Baseline (mean)
8.0
8.0
8.2
- Change at week 56 b
-1.3
-1.5
-0.7
- Difference from sitagliptin b
- [95% CI]
-0.6
[-0.7, -0.4] c
-0.8
[-0.9, -0.6] c
Patients (%) achieving HbA 1c <7%
66
73
40
FPG (mg/dL)
- Baseline (mean)
168
167
173
- Change at week 56 b
-35
-43
-23
aThe intent-to-treat population includes all randomized and exposed patients. At week 56 the primary HbA 1c endpoint was missing for 7%, 5% and 6% of patients and during the trial rescue medication was initiated by 5%, 2% and 19% of patients randomized to OZEMPIC 0.5 mg, OZEMPIC 1 mg and sitagliptin, respectively. Missing data were imputed using multiple imputation based on retrieved dropouts.
bIntent-to-treat analysis using ANCOVA adjusted for baseline value and country.
cp<0.0001 (2-sided) for superiority, adjusted for multiplicity.
The mean baseline body weight was 89.9 kg, 89.2 kg, 89.3 kg in the OZEMPIC 0.5 mg, OZEMPIC 1 mg, and sitagliptin arms, respectively. The mean changes from baseline to week 56 were -4.2 kg, -5.5 kg, and -1.7 kg for the OZEMPIC 0.5 mg, OZEMPIC 1 mg, and sitagliptin arms, respectively. The difference from sitagliptin (95% CI) for OZEMPIC 0.5 mg was -2.5 kg (-3.2, -1.8), and for OZEMPIC 1 mg was -3.8 kg (-4.5, -3.1).
- Figure 5. Mean HbA 1c (%) over time - baseline to week 56
Combination with metformin or metformin with sulfonylurea
In a 56-week, open-label trial (NCT01885208), 813 patients with type 2 diabetes mellitus on metformin alone (49%), metformin with sulfonylurea (45%), or other (6%) were randomized to OZEMPIC 1 mg once weekly or exenatide 2 mg once weekly. Patients had a mean age of 57 years and 55% were men. The mean duration of type 2 diabetes was 9 years, and the mean BMI was 34 kg/m 2. Overall, 84% were White, 7% were Black or African American, and 2% were Asian; 24% identified as Hispanic or Latino ethnicity.
Treatment with OZEMPIC 1 mg once weekly for 56 weeks resulted in a statistically significant reduction in HbA 1c compared to exenatide 2 mg once weekly (see Table 5).
Table 5. Results at Week 56 in a Trial of OZEMPIC Compared to Exenatide 2 mg Once Weekly in Adult Patients with Type 2 Diabetes Mellitus In Combination with Metformin or Metformin with Sulfonylurea
OZEMPIC
1 mg
Exenatide ER
2 mg
Intent-to-Treat (ITT) Population (N) a
404
405
HbA 1c (%)
- Baseline (mean)
8.4
8.3
- Change at week 56 b
-1.4
-0.9
- Difference from exenatide b
- [95% CI]
-0.5
[-0.7, -0.3] c
Patients (%) achieving HbA 1c <7%
62
40
FPG (mg/dL)
- Baseline (mean)
191
188
- Change at week 56 b
-44
-34
aThe intent-to-treat population includes all randomized and exposed patients. At week 56 the primary HbA 1c endpoint was missing for 9% and 11% of patients and during the trial rescue medication was initiated by 5% and 10% of patients randomized to OZEMPIC 1 mg and exenatide ER 2 mg, respectively. Missing data were imputed using multiple imputation based on retrieved dropouts.
bIntent-to-treat analysis using ANCOVA adjusted for baseline value and country.
cp<0.0001 (2-sided) for superiority, adjusted for multiplicity.
The mean baseline body weight was 96.2 kg and 95.4 kg in the OZEMPIC 1 mg and exenatide ER arms, respectively. The mean changes from baseline to week 56 were -4.8 kg and -2.0 kg in the OZEMPIC 1 mg and exenatide ER arms, respectively. The difference from exenatide ER (95% CI) for OZEMPIC 1 mg was -2.9 kg (-3.6, -2.1).
Combination with metformin or metformin with sulfonylurea
In a 30-week, open-label trial (NCT02128932), 1089 patients with type 2 diabetes mellitus were randomized to OZEMPIC 0.5 mg once weekly, OZEMPIC 1 mg once weekly, or insulin glargine once daily on a background of metformin (48%) or metformin and sulfonylurea (51%). Patients had a mean age of 57 years and 53% were men. The mean duration of type 2 diabetes was 8.6 years, and the mean BMI was 33 kg/m 2. Overall, 77% were White, 9% were Black or African American, and 11% were Asian; 20% identified as Hispanic or Latino ethnicity.
Patients assigned to insulin glargine had a baseline mean HbA 1c of 8.1% and were started on a dose of 10 U once daily. Insulin glargine dose adjustments occurred throughout the trial period based on self-measured fasting plasma glucose before breakfast, targeting 71 to <100 mg/dL. In addition, investigators could titrate insulin glargine at their discretion between study visits. Only 26% of patients had been titrated to goal by the primary endpoint at week 30, at which time the mean daily insulin dose was 29 U per day.
Treatment with OZEMPIC 0.5 mg and 1 mg once weekly for 30 weeks resulted in a statistically significant reduction in HbA 1c compared with the insulin glargine titration implemented in this study protocol (see Table 6).
Table 6. Results at Week 30 in a Trial of OZEMPIC Compared to Insulin Glargine in Adult Patients with Type 2 Diabetes Mellitus In Combination with Metformin or Metformin with Sulfonylurea
OZEMPIC
0.5 mg
OZEMPIC
1 mg
Insulin Glargine
Intent-to-Treat (ITT) Population (N) a
362
360
360
HbA 1c (%)
- Baseline (mean)
8.1
8.2
8.1
- Change at week 30 b
-1.2
-1.5
-0.9
- Difference from insulin glargine b
- [95% CI]
-0.3
[-0.5, -0.1] c
-0.6
[-0.8, -0.4] c
Patients (%) achieving HbA 1c <7%
55
66
40
FPG (mg/dL)
- Baseline (mean)
172
179
174
- Change at week 30 b
-35
-46
-37
aThe intent-to-treat population includes all randomized and exposed patients. At week 30 the primary HbA 1c endpoint was missing for 8%, 6% and 6% of patients and during the trial rescue medication was initiated by 4%, 3% and 1% of patients randomized to OZEMPIC 0.5 mg, OZEMPIC 1 mg and insulin glargine, respectively. Missing data were imputed using multiple imputation based on retrieved dropouts.
bIntent-to-treat analysis using ANCOVA adjusted for baseline value, country and stratification factors.
cp<0.0001 (2-sided) for superiority, adjusted for multiplicity .
The mean baseline body weight was 93.7 kg, 94.0 kg, 92.6 kg in the OZEMPIC 0.5 mg, OZEMPIC 1 mg, and insulin glargine arms, respectively. The mean changes from baseline to week 30 were -3.2 kg, -4.7 kg and 0.9 kg in the OZEMPIC 0.5 mg, OZEMPIC 1 mg, and insulin glargine arms, respectively. The difference from insulin glargine (95% CI) for OZEMPIC 0.5 mg was -4.1 kg (-4.9, -3.3) and for OZEMPIC 1 mg was -5.6 kg (-6.4, -4.8).
Combination with basal insulin
In a 30-week, double-blind trial (NCT02305381), 397 patients with type 2 diabetes mellitus inadequately controlled with basal insulin, with or without metformin, were randomized to OZEMPIC 0.5 mg once weekly, OZEMPIC 1 mg once weekly, or placebo. Patients with HbA 1c ≤ 8.0% at screening reduced their insulin dose by 20% at start of the trial to reduce the risk of hypoglycemia. Patients had a mean age of 59 years and 56% were men. The mean duration of type 2 diabetes was 13 years, and the mean BMI was 32 kg/m 2. Overall, 78% were White, 5% were Black or African American, and 17% were Asian; 12% identified as Hispanic or Latino ethnicity.
Treatment with OZEMPIC resulted in a statistically significant reduction in HbA 1c after 30 weeks of treatment compared to placebo (see Table 7).
Table 7. Results at Week 30 in a Trial of OZEMPIC in Adult Patients with Type 2 Diabetes Mellitus In Combination with Basal Insulin With or Without Metformin
Placebo
OZEMPIC
0.5 mg
OZEMPIC
1 mg
Intent-to-Treat (ITT) Population (N) a
133
132
131
HbA 1c (%)
- Baseline (mean)
8.4
8.4
8.3
- Change at week 30 b
-0.2
-1.3
-1.7
- Difference from placebo b
- [95% CI]
-1.1
[-1.4, -0.8] c
-1.6
[-1.8, -1.3] c
Patients (%) achieving HbA 1c <7%
13
56
73
FPG (mg/dL)
- Baseline (mean)
154
161
153
- Change at week 30 b
-8
-28
-39
aThe intent-to-treat population includes all randomized and exposed patients. At week 30 the primary HbA 1c endpoint was missing for 7%, 5% and 5% of patients and during the trial rescue medication was initiated by 14%, 2% and 1% of patients randomized to placebo, OZEMPIC 0.5 mg and OZEMPIC 1 mg, respectively. Missing data were imputed using multiple imputation based on retrieved dropouts.
bIntent-to-treat analysis using ANCOVA adjusted for baseline value, country and stratification factors.
cp<0.0001 (2-sided) for superiority, adjusted for multiplicity.
The mean baseline body weight was 89.9 kg, 92.7 kg, and 92.5 kg in the placebo, OZEMPIC 0.5 mg, and OZEMPIC 1 mg arms, respectively. The mean changes from baseline to week 30 were -1.2 kg, -3.5 kg, and ‑6.0 kg in the placebo, OZEMPIC 0.5 mg, and OZEMPIC 1 mg arms, respectively. The difference from placebo (95% CI) for OZEMPIC 0.5 mg was -2.2 kg (-3.4, -1.1), and for OZEMPIC 1 mg was -4.7 kg (-5.8, -3.6).
14.4 Cardiovascular Outcomes Trial of OZEMPIC in Patients with Type 2 Diabetes Mellitus
SUSTAIN 6 (NCT01720446) was a 104-week, double-blind trial in which 3,297 patients with type 2 diabetes and high risk of cardiovascular events were randomized to OZEMPIC 0.5 mg once weekly, OZEMPIC 1 mg once weekly, or placebo in addition to standard-of-care. In total, 2,735 (83%) of the patients had a history of cardiovascular disease and 562 (17%) were at high risk but without known cardiovascular disease. The mean age at baseline was 65 years, and 61% were men. The mean duration of diabetes was 13.9 years, and mean BMI was 33 kg/m 2. Overall, 83% were White, 7% were Black or African American, and 8% were Asian; 16% identified as Hispanic or Latino ethnicity. Concomitant diseases of patients in this trial included, but were not limited to, heart failure (24%), hypertension (93%), history of ischemic stroke (12%) and history of a myocardial infarction (33%).
In total, 98.0% of the patients completed the trial and the vital status was known at the end of the trial for 99.6%. The primary composite endpoint was the time from randomization to first occurrence of a major adverse cardiovascular event (MACE): cardiovascular death, non-fatal myocardial infarction or non-fatal stroke. The secondary endpoint was time from randomization to first occurrence of an expanded composite cardiovascular outcome, defined as MACE, revascularization (coronary and peripheral), unstable angina requiring hospitalization or hospitalization for heart failure. The total number of primary component MACE endpoints was 254 (108 [6.6%] with OZEMPIC and 146 [8.9%] with placebo). No increased risk for MACE was observed with OZEMPIC.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
How Supplied
Injection: clear, colorless solution of 1.34 mg/mL of semaglutide available in pre-filled, disposable, single-patient-use pens in the following packaging configurations:
Dose per Injection
Use For
Total Strength per Total Volume
Doses per Pen
Carton Contents
NDC
0.25 mg
0.5 mg
Initiation
Maintenance
2 mg / 1.5 mL
4 doses of 0.25 mg and
2 doses of 0.5 mg
or
4 doses of 0.5 mg
1 pen
6 NovoFine ® Plus needles
0169-4132-12
1 mg
Maintenance
2 mg / 1.5 mL
2 doses of 1 mg
2 pens
4 NovoFine ® Plus needles
0169-4136-02
Each OZEMPIC pen is for use by a single patient. An OZEMPIC pen must never be shared between patients, even if the needle is changed [see Warnings and Precautions ( 5.4)] .
Recommended Storage
Prior to first use, OZEMPIC should be stored in a refrigerator between 36ºF to 46ºF (2ºC to 8ºC) (Table 8). Do not store in the freezer or directly adjacent to the refrigerator cooling element. Do not freeze OZEMPIC and do not use OZEMPIC if it has been frozen.
After first use of the OZEMPIC pen, the pen can be stored for 56 days at controlled room temperature (59°F to 86°F; 15°C to 30°C) or in a refrigerator (36°F to 46°F; 2°C to 8°C). Do not freeze. Keep the pen cap on when not in use. OZEMPIC should be protected from excessive heat and sunlight.
Always remove and safely discard the needle after each injection and store the OZEMPIC pen without an injection needle attached. Always use a new needle for each injection.
The storage conditions are summarized in Table 8:
- Table 8. Recommended Storage Conditions for the OZEMPIC Pen
Prior to first use
After first use
Refrigerated
36°F to 46°F
(2°C to 8°C)
Room Temperature
59°F to 86°F
(15°C to 30°C)
Refrigerated
36°F to 46°F
(2°C to 8°C)
Until expiration date
56 days
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide and Instructions for Use).
Risk of Thyroid C-cell Tumors
Inform patients that semaglutide causes thyroid C-cell tumors in rodents and that the human relevance of this finding has not been determined. Counsel patients to report symptoms of thyroid tumors (e.g., a lump in the neck, hoarseness, dysphagia, or dyspnea) to their physician [see Boxed Warning and Warnings and Precautions ( 5.1)] .
Pancreatitis
Inform patients of the potential risk for pancreatitis. Instruct patients to discontinue OZEMPIC promptly and contact their physician if pancreatitis is suspected (severe abdominal pain that may radiate to the back, and which may or may not be accompanied by vomiting) [see Warnings and Precautions ( 5.2)].
Diabetic Retinopathy Complications
Inform patients to contact their physician if changes in vision are experienced during treatment with OZEMPIC [see Warnings and Precautions ( 5.3)].
Never Share an OZEMPIC Pen Between Patients
Advise patients that they must never share an OZEMPIC pen with another person, even if the needle is changed, because doing so carries a risk for transmission of blood-borne pathogens [see Warnings and Precautions ( 5.4)] .
Dehydration and Renal Failure
Advise patients treated with OZEMPIC of the potential risk of dehydration due to gastrointestinal adverse reactions and take precautions to avoid fluid depletion. Inform patients of the potential risk for worsening renal function and explain the associated signs and symptoms of renal impairment, as well as the possibility of dialysis as a medical intervention if renal failure occurs [see Warnings and Precautions ( 5.6)] .
Hypersensitivity Reactions
Inform patients to stop taking OZEMPIC and seek medical advice promptly if symptoms of hypersensitivity reactions occur [see Warnings and Precautions ( 5.7)] .
Pregnancy
Advise a pregnant woman of the potential risk to a fetus. Advise women to inform their healthcare provider if they are pregnant or intend to become pregnant [see Use in SpecificPopulations ( 8.1), ( 8.3)].
Instructions
Inform patients of the potential risks and benefits of OZEMPIC and of alternative modes of therapy. Inform patients about the importance of adherence to dietary instructions, regular physical activity, periodic blood glucose monitoring and A1c testing, recognition and management of hypoglycemia and hyperglycemia, and assessment for diabetes complications. Advise patients to seek medical advice promptly during periods of stress such as fever, trauma, infection, or surgery as medication requirements may change.
Advise patients that the most common side effects of OZEMPIC are nausea, vomiting, diarrhea, abdominal pain and constipation. Inform patients that nausea, vomiting and diarrhea are most common when first starting OZEMPIC, but decreases over time in the majority of patients.
Instruct patients to reread the Medication Guide each time the prescription is renewed.
Inform patients if a dose is missed, it should be administered as soon as possible within 5 days after the missed dose. If more than 5 days have passed, the missed dose should be skipped and the next dose should be administered on the regularly scheduled day. In each case, inform patients to resume their regular once weekly dosing schedule [see Dosage and Administration ( 2.1)] .
Manufactured by:
Novo Nordisk A/SDK-2880 Bagsvaerd
Denmark
For information about OZEMPIC contact:
Novo Nordisk Inc.
800 Scudders Mill Road
Plainsboro, NJ 08536
1-888-693-6742
Date of Issue: April 2019
Version: 3
OZEMPIC® and NovoFine® are registered trademarks of Novo Nordisk A/S.
PATENT INFORMATION: http://novonordisk-us.com/patients/products/product-patents.html
© 2019 Novo Nordisk
-
Medication Guide
OZEMPIC ® (oh-ZEM-pick)
(semaglutide)
injection, for subcutaneous use
Do not share your OZEMPIC pen with other people, even if the needle has been changed. You may give other people a serious infection, or get a serious infection from them.
Read this Medication Guide before you start using OZEMPIC and each time you get a refill. There may be new information. This information does not take the place of talking to your healthcare provider about your medical condition or your treatment.
What is the most important information I should know about OZEMPIC?
OZEMPIC may cause serious side effects, including:
- Possible thyroid tumors, including cancer. Tell your healthcare provider if you get a lump or swelling in your neck, hoarseness, trouble swallowing, or shortness of breath. These may be symptoms of thyroid cancer. In studies with rodents, OZEMPIC and medicines that work like OZEMPIC caused thyroid tumors, including thyroid cancer. It is not known if OZEMPIC will cause thyroid tumors or a type of thyroid cancer called medullary thyroid carcinoma (MTC) in people.
- Do not use OZEMPIC if you or any of your family have ever had a type of thyroid cancer called medullary thyroid carcinoma (MTC), or if you have an endocrine system condition called Multiple Endocrine Neoplasia syndrome type 2 (MEN 2).
What is OZEMPIC?
OZEMPIC is an injectable prescription medicine for adults with type 2 diabetes mellitus that:
- along with diet and exercise may improve blood sugar (glucose).
- OZEMPIC is not recommended as the first choice of medicine for treating diabetes.
- It is not known if OZEMPIC can be used in people who have had pancreatitis.
- OZEMPIC is not a substitute for insulin and is not for use in people with type 1 diabetes or people with diabetic ketoacidosis.
- It is not known if OZEMPIC is safe and effective for use in children under 18 years of age.
Do not use OZEMPIC if:
- you or any of your family have ever had a type of thyroid cancer called medullary thyroid carcinoma (MTC) or if you have an endocrine system condition called Multiple Endocrine Neoplasia syndrome type 2 (MEN 2).
- you are allergic to semaglutide or any of the ingredients in OZEMPIC. See the end of this Medication Guide for a complete list of ingredients in OZEMPIC.
Before using OZEMPIC, tell your healthcare provider if you have any other medical conditions, including if you:
- have or have had problems with your pancreas or kidneys.
- have a history of diabetic retinopathy.
- are pregnant or plan to become pregnant. It is not known if OZEMPIC will harm your unborn baby. You should stop using OZEMPIC 2 months before you plan to become pregnant. Talk to your healthcare provider about the best way to control your blood sugar if you plan to become pregnant or while you are pregnant.
- are breastfeeding or plan to breastfeed. It is not known if OZEMPIC passes into your breast milk. You should talk with your healthcare provider about the best way to feed your baby while using OZEMPIC.
- Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. OZEMPIC may affect the way some medicines work and some medicines may affect the way OZEMPIC works.
- Before using OZEMPIC, talk to your healthcare provider about low blood sugar and how to manage it. Tell your healthcare provider if you are taking other medicines to treat diabetes, including insulin or sulfonylureas.
Know the medicines you take. Keep a list of them to show your healthcare provider and pharmacist when you get a new medicine.
How should I use OZEMPIC?
- Read the Instructions for Use that comes with OZEMPIC.
- Use OZEMPIC exactly as your healthcare provider tells you to.
- Your healthcare provider should show you how to use OZEMPIC before you use it for the first time.
- OZEMPIC is injected under the skin (subcutaneously) of your stomach (abdomen), thigh, or upper arm. Do not inject OZEMPIC into a muscle (intramuscularly) or vein (intravenously).
- Use OZEMPIC 1 time each week, on the same day each week, at any time of the day.
- You may change the day of the week you use OZEMPIC as long as your last dose was given 2 or more days before.
- If you miss a dose of OZEMPIC, take the missed dose as soon as possible within 5 days after the missed dose. If more than 5 days have passed, skip the missed dose and take your next dose on the regularly scheduled day.
- OZEMPIC may be taken with or without food.
- Do not mix insulin and OZEMPIC together in the same injection.
- You may give an injection of OZEMPIC and insulin in the same body area (such as your stomach area), but not right next to each other.
- Change (rotate) your injection site with each injection. Do not use the same site for each injection.
- Check your blood sugar as your healthcare provider tells you to.
- Stay on your prescribed diet and exercise program while using OZEMPIC.
- Talk to your healthcare provider about how to prevent, recognize and manage low blood sugar (hypoglycemia), high blood sugar (hyperglycemia), and problems you have because of your diabetes.
- Your healthcare provider will check your diabetes with regular blood tests, including your blood sugar levels and your hemoglobin A1C.
- Do not share your OZEMPIC pen with other people, even if the needle has been changed. You may give other people a serious infection, or get a serious infection from them.
Your dose of OZEMPIC and other diabetes medicines may need to change because of:
- change in level of physical activity or exercise, weight gain or loss, increased stress, illness, change in diet, fever, trauma, infection, surgery or because of other medicines you take.
What are the possible side effects of OZEMPIC?
OZEMPIC may cause serious side effects, including:
- See “What is the most important information I should know about OZEMPIC?”
- inflammation of your pancreas(pancreatitis). Stop using OZEMPIC and call your healthcare provider right away if you have severe pain in your stomach area (abdomen) that will not go away, with or without vomiting. You may feel the pain from your abdomen to your back.
- changes in vision. Tell your healthcare provider if you have changes in vision during treatment with OZEMPIC.
-
low blood sugar (hypoglycemia). Your risk for getting low blood sugar may be higher if you use OZEMPIC with another medicine that can cause low blood sugar, such as a sulfonylurea or insulin.
Signs and symptoms of low blood sugar may include:
- dizziness or light-headedness
- blurred vision
- anxiety, irritability, or mood changes
- sweating
- slurred speech
- hunger
- confusion or drowsiness
- shakiness
- weakness
- headache
- fast heartbeat
- feeling jittery
- kidney problems (kidney failure). In people who have kidney problems, diarrhea, nausea, and vomiting may cause a loss of fluids (dehydration) which may cause kidney problems to get worse. It is important for you to drink fluids to help reduce your chance of dehydration.
- seriousallergic reactions. Stop using OZEMPIC and get medical help right away, if you have any symptoms of a serious allergic reaction including itching, rash, or difficulty breathing.
The most common side effects of OZEMPIC may include nausea, vomiting, diarrhea, stomach (abdominal) pain and constipation.
Talk to your healthcare provider about any side effect that bothers you or does not go away. These are not all the possible side effects of OZEMPIC.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1‑800‑FDA‑1088.
General information about the safe and effective use of OZEMPIC.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use OZEMPIC for a condition for which it was not prescribed. Do not give OZEMPIC to other people, even if they have the same symptoms that you have. It may harm them.
You can ask your pharmacist or healthcare provider for information about OZEMPIC that is written for health professionals.
For more information, go to OZEMPIC.com or call 1-888-693-6742.
What are the ingredients in OZEMPIC?
Active Ingredient: semaglutide
Inactive Ingredients: disodium phosphate dihydrate, propylene glycol, phenol and water for injection
Manufactured by: Novo Nordisk A/S, DK-2880 Bagsvaerd, Denmark
OZEMPIC ® is a registered trademark of Novo Nordisk A/S.
PATENT Information: http://novonordisk-us.com/patients/products/product-patents.html
© 2017 Novo Nordisk
Revised: December 2017
This Medication Guide has been approved by the U.S. Food and Drug Administration.
-
Instructions for Use – 1 mg
-
Instructions for Use – 0.25 mg or 0.5 doses
-
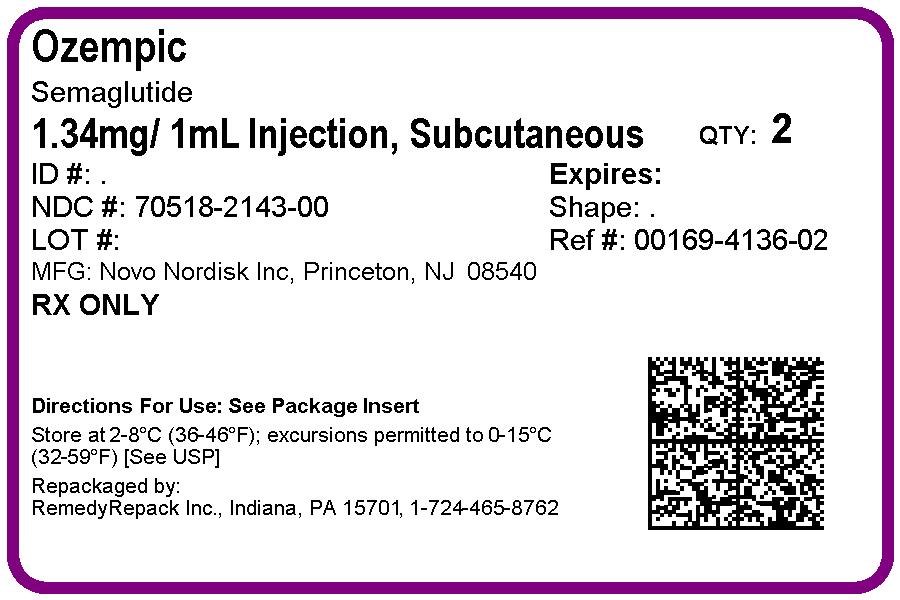
PRINCIPAL DISPLAY PANEL
DRUG: Ozempic
GENERIC: semaglutide
DOSAGE: INJECTION, SOLUTION
ADMINSTRATION: SUBCUTANEOUS
NDC: 70518-2143-0
PACKAGING: 1.5 mL in 1 SYRINGE, PLASTIC
OUTER PACKAGING: 2 in 1 CARTON
ACTIVE INGREDIENT(S):
- SEMAGLUTIDE 1.34mg in 1mL
INACTIVE INGREDIENT(S):
- PHENOL
- PROPYLENE GLYCOL
- SODIUM PHOSPHATE, DIBASIC, DIHYDRATE
- WATER
-
INGREDIENTS AND APPEARANCE
OZEMPIC
semaglutide injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 70518-2143(NDC:0169-4136) Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength SEMAGLUTIDE (UNII: 53AXN4NNHX) (SEMAGLUTIDE - UNII:53AXN4NNHX) SEMAGLUTIDE 1.34 mg in 1 mL Inactive Ingredients Ingredient Name Strength SODIUM PHOSPHATE, DIBASIC, DIHYDRATE (UNII: 94255I6E2T) 1.42 mg in 1 mL PROPYLENE GLYCOL (UNII: 6DC9Q167V3) 14 mg in 1 mL PHENOL (UNII: 339NCG44TV) 5.5 mg in 1 mL WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 70518-2143-0 2 in 1 CARTON 06/11/2019 1 1.5 mL in 1 SYRINGE, PLASTIC; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA209637 06/11/2019 Labeler - REMEDYREPACK INC. (829572556)
Trademark Results [Ozempic]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 OZEMPIC 79159431 4774881 Live/Registered |
Novo Nordisk A/S 2014-12-03 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.

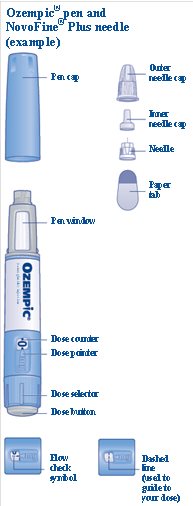











 ) will guide you to 1 mg.
) will guide you to 1 mg.





























 ) will guide you to your dose.
) will guide you to your dose.
















