These highlights do not include all the information needed to use METOPROLOL SUCCINATE EXTENDED-RELEASE TABLETS safely and effectively. See full prescribing information for METOPROLOL SUCCINATE EXTENDED-RELEASE TABLETS. METOPROLOL SUCCINATE extended-release tablets for oral use. Initial U.S. Approval: 1992
Metoprolol Succinate by
Drug Labeling and Warnings
Metoprolol Succinate by is a Prescription medication manufactured, distributed, or labeled by Wockhardt USA LLC., Pharmadax Inc., CorePharma, LLC, Pharmadax (Foshan) Co.,Ltd. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
METOPROLOL SUCCINATE- metoprolol succinate tablet, extended release
Wockhardt USA LLC.
----------
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use METOPROLOL SUCCINATE EXTENDED-RELEASE TABLETS safely and effectively. See full prescribing information for METOPROLOL SUCCINATE EXTENDED-RELEASE TABLETS.
METOPROLOL SUCCINATE extended-release tablets for oral use. Initial U.S. Approval: 1992 WARNING: ISCHEMIC HEART DISEASE(See Full Prescribing Information for complete boxed warning)Following abrupt cessation of therapy with beta-blocking agents, exacerbations of angina pectoris and myocardial infarction have occurred. Warn patients against interruption or discontinuation of therapy without the physician’s advice. ( 5.1)
INDICATIONS AND USAGEMetoprolol Succinate Extended-Release Tablets, metoprolol succinate, is a beta 1-selective adrenoceptor blocking agent. Metoprolol Succinate Extended-Release Tablets are indicated for the treatment of:
DOSAGE AND ADMINISTRATION
DOSAGE FORMS AND STRENGTHS
CONTRAINDICATIONSWARNINGS AND PRECAUTIONS
ADVERSE REACTIONS
To report SUSPECTED ADVERSE REACTIONS, contact Wockhardt USA LLC. at 1-800-346-6854 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch . DRUG INTERACTIONS
USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION. See 17 for PATIENT COUNSELING INFORMATION. Revised: 4/2021 |
FULL PRESCRIBING INFORMATION
WARNING: ISCHEMIC HEART DISEASE:
Following abrupt cessation of therapy with certain beta-blocking agents, exacerbations of angina pectoris and, in some cases, myocardial infarction have occurred. When discontinuing chronically administered Metoprolol Succinate Extended-Release Tablets, particularly in patients with ischemic heart disease, the dosage should be gradually reduced over a period of 1 to 2 weeks and the patient should be carefully monitored. If angina markedly worsens or acute coronary insufficiency develops, Metoprolol Succinate Extended-Release Tablets administration should be reinstated promptly, at least temporarily, and other measures appropriate for the management of unstable angina should be taken. Warn patients against interruption or discontinuation of therapy without the physician’s advice. Because coronary artery disease is common and may be unrecognized, it may be prudent not to discontinue Metoprolol Succinate Extended-Release Tablets therapy abruptly even in patients treated only for hypertension (5.1).
1 INDICATIONS & USAGE
1.1 Hypertension
Metoprolol Succinate Extended-Release Tablets USP are indicated for the treatment of hypertension, to lower blood pressure. Lowering blood pressure lowers the risk of fatal and non-fatal cardiovascular events, primarily strokes and myocardial infarctions. These benefits have been seen in controlled trials of antihypertensive drugs from a wide variety of pharmacologic classes including metoprolol.
Control of high blood pressure should be part of comprehensive cardiovascular risk management, including, as appropriate, lipid control, diabetes management, antithrombotic therapy, smoking cessation, exercise, and limited sodium intake. Many patients will require more than 1 drug to achieve blood pressure goals. For specific advice on goals and management, see published guidelines, such as those of the National High Blood Pressure Education Program’s Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC).
Numerous antihypertensive drugs, from a variety of pharmacologic classes and with different mechanisms of action, have been shown in randomized controlled trials to reduce cardiovascular morbidity and mortality, and it can be concluded that it is blood pressure reduction, and not some other pharmacologic property of the drugs, that is largely responsible for those benefits. The largest and most consistent cardiovascular outcome benefit has been a reduction in the risk of stroke, but reductions in myocardial infarction and cardiovascular mortality also have been seen regularly.
Elevated systolic or diastolic pressure causes increased cardiovascular risk, and the absolute risk increase per mmHg is greater at higher blood pressures, so that even modest reductions of severe hypertension can provide substantial benefit. Relative risk reduction from blood pressure reduction is similar across populations with varying absolute risk, so the absolute benefit is greater in patients who are at higher risk independent of their hypertension (for example, patients with diabetes or hyperlipidemia), and such patients would be expected to benefit from more aggressive treatment to a lower blood pressure goal.
Some antihypertensive drugs have smaller blood pressure effects (as monotherapy) in black patients, and many antihypertensive drugs have additional approved indications and effects (e.g., on angina, heart failure, or diabetic kidney disease). These considerations may guide selection of therapy.
Metoprolol Succinate Extended-Release Tablets USP may be administered with other antihypertensive agents.
1.2 Angina Pectoris
Metoprolol Succinate Extended-Release Tablets USP are indicated in the long-term treatment of angina pectoris, to reduce angina attacks and to improve exercise tolerance.
1.3 Heart Failure
Metoprolol Succinate Extended-Release Tablets USP are indicated for the treatment of stable, symptomatic (NYHA Class II or III) heart failure of ischemic, hypertensive, or cardiomyopathic origin. It was studied in patients already receiving ACE inhibitors, diuretics, and, in the majority of cases, digitalis. In this population, Metoprolol Succinate Extended-Release Tablets USP decreased the rate of mortality plus hospitalization, largely through a reduction in cardiovascular mortality and hospitalizations for heart failure.
2 DOSAGE & ADMINISTRATION
Metoprolol Succinate Extended-Release Tablets are an extended-release tablet intended for once daily administration. For treatment of hypertension and angina, when switching from immediate-release metoprolol to Metoprolol Succinate Extended-Release Tablets, use the same total daily dose of Metoprolol Succinate Extended-Release Tablets. Individualize the dosage of Metoprolol Succinate Extended-Release Tablets. Titration may be needed in some patients.
Metoprolol Succinate Extended-Release Tablets are scored and can be divided; however, do not crush or chew the whole or half tablet.
2.1 Hypertension
Adults: The usual initial dosage is 25 to 100 mg daily in a single dose. The dosage may be increased at weekly (or longer) intervals until optimum blood pressure reduction is achieved. In general, the maximum effect of any given dosage level will be apparent after 1 week of therapy. Dosages above 400 mg per day have not been studied.
Pediatric Hypertensive Patients ≥ 6 Years of age: A pediatric clinical hypertension study in patients 6 to 16 years of age did not meet its primary endpoint (dose response for reduction in SBP); however some other endpoints demonstrated effectiveness [see Use in Specific Populations (8.4)]. If selected for treatment, the recommended starting dose of Metoprolol Succinate Extended-Release Tablets is 1 mg/kg once daily, but the maximum initial dose should not exceed 50 mg once daily. Dosage should be adjusted according to blood pressure response. Doses above 2 mg/kg (or in excess of 200 mg) once daily have not been studied in pediatric patients [see Clinical Pharmacology (12.3)].
Metoprolol Succinate Extended-Release Tablets are not recommended in pediatric patients < 6 years of age [see Use in Specific Populations (8.4)].
2.2 Angina Pectoris
Individualize the dosage of Metoprolol Succinate Extended-Release Tablets. The usual initial dosage is 100 mg daily, given in a single dose. Gradually increase the dosage at weekly intervals until optimum clinical response has been obtained or there is a pronounced slowing of the heart rate. Dosages above 400 mg per day have not been studied. If treatment is to be discontinued, reduce the dosage gradually over a period of 1 to 2 weeks [see Warnings and Precautions (5)].
2.3 Heart Failure
Dosage must be individualized and closely monitored during up-titration. Prior to initiation of Metoprolol Succinate Extended-Release Tablets, stabilize the dose of other heart failure drug therapy. The recommended starting dose of Metoprolol Succinate Extended-Release Tablets is 25 mg once daily for two weeks in patients with NYHA Class II heart failure and 12.5 mg once daily in patients with more severe heart failure. Double the dose every two weeks to the highest dosage level tolerated by the patient or up to 200 mg of Metoprolol Succinate Extended-Release Tablets. Initial difficulty with titration should not preclude later attempts to introduce Metoprolol Succinate Extended-Release Tablets. If patients experience symptomatic bradycardia, reduce the dose of Metoprolol Succinate Extended-Release Tablets. If transient worsening of heart failure occurs, consider treating with increased doses of diuretics, lowering the dose of Metoprolol Succinate Extended-Release Tablets or temporarily discontinuing it. The dose of Metoprolol Succinate Extended-Release Tablets should not be increased until symptoms of worsening heart failure have been stabilized.
3 DOSAGE FORMS AND STRENGTHS
100 mg tablets: White to off-white capsule-shaped film coated tablets with a score on one side and engraved with “P03” on the other side.
200 mg tablets: White to off-white oval film coated tablets with a score on one side and engraved with “P04” on the other side.
4 CONTRAINDICATIONS
Metoprolol Succinate Extended-Release Tablets are contraindicated in severe bradycardia, second or third degree heart block, cardiogenic shock, decompensated cardiac failure, sick sinus syndrome (unless a permanent pacemaker is in place), and in patients who are hypersensitive to any component of this product.
5 WARNINGS AND PRECAUTIONS
5.1 Ischemic Heart Disease
Following abrupt cessation of therapy with certain beta-blocking agents, exacerbations of angina pectoris and, in some cases, myocardial infarction have occurred. When discontinuing chronically administered Metoprolol Succinate Extended-Release Tablets, particularly in patients with ischemic heart disease, gradually reduce the dosage over a period of 1 to 2 weeks and monitor the patient. If angina markedly worsens or acute coronary ischemia develops, promptly reinstate Metoprolol Succinate Extended-Release Tablets, and take measures appropriate for the management of unstable angina. Warn patients not to interrupt therapy without their physician’s advice. Because coronary artery disease is common and may be unrecognized, avoid abruptly discontinuing Metoprolol Succinate Extended-Release Tablets in patients treated only for hypertension.
5.2 Heart Failure
Worsening cardiac failure may occur during up-titration of Metoprolol Succinate Extended-Release Tablets. If such symptoms occur, increase diuretics and restore clinical stability before advancing the dose of Metoprolol Succinate Extended-Release Tablets [see Dosage and Administration (2)]. It may be necessary to lower the dose of Metoprolol Succinate Extended-Release Tablets or temporarily discontinue it. Such episodes do not preclude subsequent successful titration of Metoprolol Succinate Extended-Release Tablets.
5.3 Bronchospastic Disease
PATIENTS WITH BRONCHOSPASTIC DISEASES SHOULD, IN GENERAL, NOT RECEIVE BETA-BLOCKERS. Because of its relative beta 1 cardio-selectivity, however, Metoprolol Succinate Extended-Release Tablets may be used in patients with bronchospastic disease who do not respond to, or cannot tolerate, other antihypertensive treatment. Because beta 1-selectivity is not absolute, use the lowest possible dose of Metoprolol Succinate Extended-Release Tablets. Bronchodilators, including beta 2-agonists, should be readily available or administered concomitantly [see Dosage and Administration (2)].
5.4 Pheochromocytoma
If Metoprolol Succinate Extended-Release Tablets are used in the setting of pheochromocytoma, it should be given in combination with an alpha blocker, and only after the alpha blocker has been initiated. Administration of beta-blockers alone in the setting of pheochromocytoma has been associated with a paradoxical increase in blood pressure due to the attenuation of beta-mediated vasodilatation in skeletal muscle.
5.5 Major Surgery
Avoid initiation of a high-dose regimen of extended-release metoprolol in patients undergoing non-cardiac surgery, since such use in patients with cardiovascular risk factors has been associated with bradycardia, hypotension, stroke and death.
Chronically administered beta-blocking therapy should not be routinely withdrawn prior to major surgery, however, the impaired ability of the heart to respond to reflex adrenergic stimuli may augment the risks of general anesthesia and surgical procedures.
5.6 Diabetes and Hypoglycemia
Beta-blockers may mask tachycardia occurring with hypoglycemia, but other manifestations such as dizziness and sweating may not be significantly affected.
5.7 Hepatic Impairment
Consider initiating Metoprolol Succinate Extended-Release Tablets therapy at doses lower than those recommended for a given indication; gradually increase dosage to optimize therapy, while monitoring closely for adverse events.
5.8 Thyrotoxicosis
Beta-adrenergic blockade may mask certain clinical signs of hyperthyroidism, such as tachycardia. Abrupt withdrawal of beta-blockade may precipitate a thyroid storm.
5.9 Anaphylactic Reaction
While taking beta-blockers, patients with a history of severe anaphylactic reactions to a variety of allergens may be more reactive to repeated challenge and may be unresponsive to the usual doses of epinephrine used to treat an allergic reaction.
6 ADVERSE REACTIONS
The following adverse reactions are described elsewhere in labeling:
- Worsening angina or myocardial infarction. [see Warnings and Precautions (5)]
- Worsening heart failure. [see Warnings and Precautions (5)]
- Worsening AV block. [see Contraindications (4)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. The adverse reaction information from clinical trials does, however, provide a basis for identifying the adverse events that appear to be related to drug use and for approximating rates.
Hypertension and Angina: Most adverse reactions have been mild and transient. The most common (>2%) adverse reactions are tiredness, dizziness, depression, diarrhea, shortness of breath, bradycardia, and rash.
Heart Failure: In the MERIT-HF study comparing Metoprolol Succinate Extended-Release Tablets in daily doses up to 200 mg (mean dose 159 mg once-daily; n=1990) to placebo (n=2001), 10.3% of Metoprolol Succinate Extended-Release Tablets patients discontinued for adverse reactions vs.12.2% of placebo patients.
The table below lists adverse reactions in the MERIT-HF study that occurred at an incidence of ≥ 1% in the Metoprolol Succinate Extended-Release Tablets group and greater than placebo by more than 0.5%, regardless of the assessment of causality.
| Metoprolol Succinate Extended-Release Tablets
n=1990 % of patients | Placebo
n=2001 % of patients |
|
| Dizziness/vertigo | 1.8 | 1.0 |
| Bradycardia | 1.5 | 0.4 |
| Accident and/or injury | 1.4 | 0.8 |
Post-operative Adverse Events: In a randomized, double-blind, placebo-controlled trial of 8351 patients with or at risk for atherosclerotic disease undergoing non-vascular surgery and who were not taking beta–blocker therapy, Metoprolol Succinate Extended-Release Tablets 100 mg was started 2 to 4 hours prior to surgery then continued for 30 days at 200 mg per day. Metoprolol Succinate Extended-Release Tablets use was associated with a higher incidence of bradycardia (6.6% vs. 2.4%; HR 2.74; 95% CI 2.19, 3.43), hypotension (15% vs. 9.7%; HR 1.55; 95% CI 1.37, 1.74), stroke (1.0% vs. 0.5%; HR 2.17; 95% CI 1.26, 3.74) and death (3.1% vs. 2.3%; HR 1.33; 95% CI 1.03, 1.74) compared to placebo.
6.2 Post-Marketing Experience
The following adverse reactions have been identified during post-approval use of Metoprolol Succinate Extended-Release Tablets or immediate-release metoprolol. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Cardiovascular: Cold extremities, arterial insufficiency (usually of the Raynaud type), palpitations, peripheral edema, syncope, chest pain and hypotension.
Respiratory: Wheezing (bronchospasm), dyspnea.
Central Nervous System: Confusion, short-term memory loss, headache, somnolence, nightmares, insomnia, anxiety/nervousness, hallucinations, paresthesia.
Gastrointestinal: Nausea, dry mouth, constipation, flatulence, heartburn, hepatitis, vomiting.
Hypersensitive Reactions: Pruritus.
Miscellaneous: Musculoskeletal pain, arthralgia, blurred vision, decreased libido, male impotence, tinnitus, reversible alopecia, agranulocytosis, dry eyes, worsening of psoriasis, Peyronie’s disease, sweating, photosensitivity, taste disturbance.
Potential Adverse Reactions: In addition, there are adverse reactions not listed above that have been reported with other beta-adrenergic blocking agents and should be considered potential adverse reactions to Metoprolol Succinate Extended-Release Tablets.
Central Nervous System: Reversible mental depression progressing to catatonia; an acute reversible syndrome characterized by disorientation for time and place, short-term memory loss, emotional lability, clouded sensorium, and decreased performance on neuropsychometrics.
Hematologic: Agranulocytosis, nonthrombocytopenic purpura, thrombocytopenic purpura.
Hypersensitive Reactions: Laryngospasm, respiratory distress.
7 DRUG INTERACTIONS
7.1 Catecholamine Depleting Drugs
Catecholamine depleting drugs (e.g., reserpine, monoamine oxidase (MAO) inhibitors) may have an additive effect when given with beta-blocking agents. Observe patients treated with Metoprolol Succinate Extended-Release Tablets plus a catecholamine depletor for evidence of hypotension or marked bradycardia, which may produce vertigo, syncope, or postural hypotension.
7.2 CYP2D6 Inhibitors
Drugs that inhibit CYP2D6 such as quinidine, fluoxetine, paroxetine, and propafenone are likely to increase metoprolol concentration. In healthy subjects with CYP2D6 extensive metabolizer phenotype, coadministration of quinidine 100 mg and immediate-release metoprolol 200 mg tripled the concentration of S-metoprolol and doubled the metoprolol elimination half-life. In four patients with cardiovascular disease, coadministration of propafenone 150 mg t.i.d. with immediate-release metoprolol 50 mg t.i.d. resulted in two- to five-fold increases in the steady-state concentration of metoprolol. These increases in plasma concentration would decrease the cardioselectivity of metoprolol.
7.3 Digitalis, Clonidine, and Calcium Channel Blockers
Digitalis glycosides, clonidine, diltiazem and verapamil slow atrioventricular conduction and decrease heart rate. Concomitant use with beta blockers can increase the risk of bradycardia.
If clonidine and a beta blocker, such as metoprolol are coadministered, withdraw the beta-blocker several days before the gradual withdrawal of clonidine because beta-blockers may exacerbate the rebound hypertension that can follow the withdrawal of clonidine. If replacing clonidine by beta-blocker therapy, delay the introduction of beta-blockers for several days after clonidine administration has stopped [see Warnings and Precautions (5.11)].
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category C
Metoprolol tartrate has been shown to increase post-implantation loss and decrease neonatal survival in rats at doses up to 22 times, on a mg/m 2 basis, the daily dose of 200 mg in a 60-kg patient. Distribution studies in mice confirm exposure of the fetus when metoprolol tartrate is administered to the pregnant animal. These studies have revealed no evidence of impaired fertility or teratogenicity. There are no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, use this drug during pregnancy only if clearly needed.
8.3 Nursing Mothers
Metoprolol is excreted in breast milk in very small quantities. An infant consuming 1 liter of breast milk daily would receive a dose of less than 1 mg of the drug. Consider possible infant exposure when Metoprolol Succinate Extended-Release Tablets are administered to a nursing woman.
8.4 Pediatric Use
One hundred forty-four hypertensive pediatric patients aged 6 to 16 years were randomized to placebo or to one of three dose levels of Metoprolol Succinate Extended-Release Tablets (0.2, 1.0 or 2.0 mg/kg once daily) and followed for 4 weeks. The study did not meet its primary endpoint (dose response for reduction in SBP). Some pre-specified secondary endpoints demonstrated effectiveness including:
- Dose-response for reduction in DBP,
- 1.0 mg/kg vs. placebo for change in SBP, and
- 2.0 mg/kg vs. placebo for change in SBP and DBP.
The mean placebo corrected reductions in SBP ranged from 3 to 6 mmHg, and DBP from 1 to 5 mmHg. Mean reduction in heart rate ranged from 5 to 7 bpm but considerably greater reductions were seen in some individuals [see Dosage and Administration (2.1)].
No clinically relevant differences in the adverse event profile were observed for pediatric patients aged 6 to 16 years as compared with adult patients.
Safety and effectiveness of Metoprolol Succinate Extended-Release Tablets have not been established in patients < 6 years of age.
8.5 Geriatric Use
Clinical studies of Metoprolol Succinate Extended-Release Tablets in hypertension did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience in hypertensive patients has not identified differences in responses between elderly and younger patients.
Of the 1,990 patients with heart failure randomized to Metoprolol Succinate Extended-Release Tablets in the MERIT-HF trial, 50% (990) were 65 years of age and older and 12% (238) were 75 years of age and older. There were no notable differences in efficacy or the rate of adverse reactions between older and younger patients.
In general, use a low initial starting dose in elderly patients given their greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
8.6 Hepatic Impairment
No studies have been performed with Metoprolol Succinate Extended-Release Tablets in patients with hepatic impairment. Because Metoprolol Succinate Extended-Release Tablets are metabolized by the liver, metoprolol blood levels are likely to increase substantially with poor hepatic function. Therefore, initiate therapy at doses lower than those recommended for a given indication; and increase doses gradually in patients with impaired hepatic function.
8.7 Renal Impairment
The systemic availability and half-life of metoprolol in patients with renal failure do not differ to a clinically significant degree from those in normal subjects. No reduction in dosage is needed in patients with chronic renal failure [see Clinical Pharmacology (12.3)].
10 OVERDOSAGE
Signs and Symptoms - Overdosage of Metoprolol Succinate Extended-Release Tablets may lead to severe bradycardia, hypotension, and cardiogenic shock. Clinical presentation can also include: atrioventricular block, heart failure, bronchospasm, hypoxia, impairment of consciousness/coma, nausea and vomiting.
Treatment – Consider treating the patient with intensive care. Patients with myocardial infarction or heart failure may be prone to significant hemodynamic instability. Seek consultation with a regional poison control center and a medical toxicologist as needed. Beta-blocker overdose may result in significant resistance to resuscitation with adrenergic agents, including beta-agonists. On the basis of the pharmacologic actions of metoprolol, employ the following measures.
There is very limited experience with the use of hemodialysis to remove metoprolol, however metoprolol is not highly protein bound.
Bradycardia: Evaluate the need for atropine, adrenergic-stimulating drugs or pacemaker to treat bradycardia and conduction disorders.
Hypotension: Treat underlying bradycardia. Consider intravenous vasopressor infusion, such as dopamine or norepinephrine.
Heart failure and shock: May be treated when appropriate with suitable volume expansion, injection of glucagon (if necessary, followed by an intravenous infusion of glucagon), intravenous administration of adrenergic drugs such as dobutamine, with α 1 receptor agonistic drugs added in presence of vasodilation.
Bronchospasm: Can usually be reversed by bronchodilators.
11 DESCRIPTION
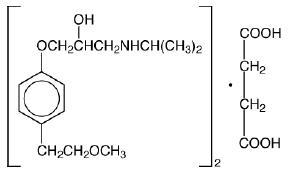
Metoprolol succinate is a beta 1-selective (cardioselective) adrenoceptor blocking agent, for oral administration, available as extended-release tablets. Metoprolol Succinate Extended-Release Tablets USP have been formulated to provide a controlled and predictable release of metoprolol for once-daily administration. The tablets comprise a multiple unit system containing metoprolol succinate in a multitude of controlled release granules. Each granule acts as a separate drug delivery unit and is designed to deliver metoprolol continuously over the dosage interval. The tablets contain 95 and 190 mg of metoprolol succinate equivalent to 100 and 200 mg of metoprolol tartrate, USP, respectively. Its chemical name is (±)1-(isopropylamino)-3-[p-(2-methoxyethyl) phenoxy]-2-propanol succinate (2:1) (salt). Its structural formula is:
Metoprolol succinate is a white crystalline powder with a molecular weight of 652.8. It is freely soluble in water; soluble in methanol; sparingly soluble in ethanol; slightly soluble in dichloromethane and 2-propanol; practically insoluble in ethyl-acetate, acetone, diethylether and heptane. Inactive ingredients: colloidal silicon dioxide, crospovidone, ethylcellulose, ethylene glycol and vinyl alcohol graft copolymer, glycerol monocaprylocaprate, magnesium stearate, microcrystalline cellulose, polyethylene glycol, polyvinyl alcohol, povidone, talc, titanium dioxide, triethyl citrate. Contains no ingredient made from a gluten-containing grain (wheat, barley, or rye).
Meets USP Dissolution Test 7.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Hypertension: The mechanism of the antihypertensive effects of beta-blocking agents has not been elucidated. However, several possible mechanisms have been proposed: (1) competitive antagonism of catecholamines at peripheral (especially cardiac) adrenergic neuron sites, leading to decreased cardiac output; (2) a central effect leading to reduced sympathetic outflow to the periphery; and (3) suppression of renin activity.
Heart Failure: The precise mechanism for the beneficial effects of beta-blockers in heart failure has not been elucidated.
12.2 Pharmacodynamics
Clinical pharmacology studies have confirmed the beta-blocking activity of metoprolol in man, as shown by (1) reduction in heart rate and cardiac output at rest and upon exercise, (2) reduction of systolic blood pressure upon exercise, (3) inhibition of isoproterenol-induced tachycardia, and (4) reduction of reflex orthostatic tachycardia.
Metoprolol is a beta 1-selective (cardioselective) adrenergic receptor blocking agent. This preferential effect is not absolute, however, and at higher plasma concentrations, metoprolol also inhibits beta 2-adrenoreceptors, chiefly located in the bronchial and vascular musculature. Metoprolol has no intrinsic sympathomimetic activity, and membrane-stabilizing activity is detectable only at plasma concentrations much greater than required for beta-blockade. Animal and human experiments indicate that metoprolol slows the sinus rate and decreases AV nodal conduction.
The relative beta 1-selectivity of metoprolol has been confirmed by the following: (1) In normal subjects, metoprolol is unable to reverse the beta 2-mediated vasodilating effects of epinephrine. This contrasts with the effect of nonselective beta-blockers, which completely reverse the vasodilating effects of epinephrine. (2) In asthmatic patients, metoprolol reduces FEV 1 and FVC significantly less than a nonselective beta-blocker, propranolol, at equivalent beta 1-receptor blocking doses.
The relationship between plasma metoprolol levels and reduction in exercise heart rate is independent of the pharmaceutical formulation. Using an E max model, the maximum effect is a 30% reduction in exercise heart rate, which is attributed to beta 1-blockade. Beta 1-blocking effects in the range of 30 to 80% of the maximal effect (approximately 8 to 23% reduction in exercise heart rate) correspond to metoprolol plasma concentrations from 30 to 540 nmol/L. The relative beta 1-selectivity of metoprolol diminishes and blockade of beta 2-adrenoceptors increases at plasma concentration above 300 nmol/L.
Although beta-adrenergic receptor blockade is useful in the treatment of angina, hypertension, and heart failure there are situations in which sympathetic stimulation is vital. In patients with severely damaged hearts, adequate ventricular function may depend on sympathetic drive. In the presence of AV block, beta-blockade may prevent the necessary facilitating effect of sympathetic activity on conduction. Beta 2-adrenergic blockade results in passive bronchial constriction by interfering with endogenous adrenergic bronchodilator activity in patients subject to bronchospasm and may also interfere with exogenous bronchodilators in such patients.
In other studies, treatment with Metoprolol Succinate Extended-Release Tablets produced an improvement in left ventricular ejection fraction. Metoprolol Succinate Extended-Release Tablets were also shown to delay the increase in left ventricular end-systolic and end-diastolic volumes after 6 months of treatment.
12.3 Pharmacokinetics
Adults: In man, absorption of metoprolol is rapid and complete. Plasma levels following oral administration of conventional metoprolol tablets, however, approximate 50% of levels following intravenous administration, indicating about 50% first-pass metabolism. Metoprolol crosses the blood-brain barrier and has been reported in the CSF in a concentration 78% of the simultaneous plasma concentration.
Plasma levels achieved are highly variable after oral administration. Only a small fraction of the drug (about 12%) is bound to human serum albumin. Metoprolol is a racemic mixture of R- and S- enantiomers, and is primarily metabolized by CYP2D6. When administered orally, it exhibits stereoselective metabolism that is dependent on oxidation phenotype. Elimination is mainly by biotransformation in the liver, and the plasma half-life ranges from approximately 3 to 7 hours. Less than 5% of an oral dose of metoprolol is recovered unchanged in the urine; the rest is excreted by the kidneys as metabolites that appear to have no beta-blocking activity.
Following intravenous administration of metoprolol, the urinary recovery of unchanged drug is approximately 10%. The systemic availability and half-life of metoprolol in patients with renal failure do not differ to a clinically significant degree from those in normal subjects. Consequently, no reduction in metoprolol succinate dosage is usually needed in patients with chronic renal failure.
Metoprolol is metabolized predominantly by CYP2D6, an enzyme that is absent in about 8% of Caucasians (poor metabolizers) and about 2% of most other populations. CYP2D6 can be inhibited by a number of drugs. Poor metabolizers and extensive metabolizers who concomitantly use CYP2D6 inhibiting drugs will have increased (several-fold) metoprolol blood levels, decreasing metoprolol's cardioselectivity [see Drug Interactions (7.2)].
In comparison to conventional metoprolol, the plasma metoprolol levels following administration of Metoprolol Succinate Extended-Release Tablets are characterized by lower peaks, longer time to peak and significantly lower peak to trough variation. The peak plasma levels following once-daily administration of Metoprolol Succinate Extended-Release Tablets average one-fourth to one-half the peak plasma levels obtained following a corresponding dose of conventional metoprolol, administered once daily or in divided doses. At steady state the average bioavailability of metoprolol following administration of Metoprolol Succinate Extended-Release Tablets, across the dosage range of 50 to 400 mg once daily, was 77% relative to the corresponding single or divided doses of conventional metoprolol. Nevertheless, over the 24-hour dosing interval, β 1-blockade is comparable and dose-related [see Clinical Pharmacology (12)]. The bioavailability of metoprolol shows a dose-related, although not directly proportional, increase with dose and is not significantly affected by food following Metoprolol Succinate Extended-Release Tablets administration.
Pediatrics: The pharmacokinetic profile of Metoprolol Succinate Extended-Release Tablets was studied in 120 pediatric hypertensive patients (6 to 17 years of age) receiving doses ranging from 12.5 to 200 mg once daily. The pharmacokinetics of metoprolol were similar to those described previously in adults. Age, gender, race, and ideal body weight had no significant effects on metoprolol pharmacokinetics. Metoprolol apparent oral clearance (CL/F) increased linearly with body weight. Metoprolol pharmacokinetics have not been investigated in patients < 6 years of age.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term studies in animals have been conducted to evaluate the carcinogenic potential of metoprolol tartrate. In 2-year studies in rats at three oral dosage levels of up to 800 mg/kg/day (41 times, on a mg/m 2 basis, the daily dose of 200 mg for a 60-kg patient), there was no increase in the development of spontaneously occurring benign or malignant neoplasms of any type. The only histologic changes that appeared to be drug related were an increased incidence of generally mild focal accumulation of foamy macrophages in pulmonary alveoli and a slight increase in biliary hyperplasia. In a 21-month study in Swiss albino mice at three oral dosage levels of up to 750 mg/kg/day (18 times, on a mg/m 2 basis, the daily dose of 200 mg for a 60-kg patient), benign lung tumors (small adenomas) occurred more frequently in female mice receiving the highest dose than in untreated control animals. There was no increase in malignant or total (benign plus malignant) lung tumors, nor in the overall incidence of tumors or malignant tumors. This 21-month study was repeated in CD-1 mice, and no statistically or biologically significant differences were observed between treated and control mice of either sex for any type of tumor.
All genotoxicity tests performed on metoprolol tartrate (a dominant lethal study in mice, chromosome studies in somatic cells, a Salmonella/mammalian-microsome mutagenicity test, and a nucleus anomaly test in somatic interphase nuclei) and metoprolol succinate (a Salmonella/mammalian-microsome mutagenicity test) were negative.
No evidence of impaired fertility due to metoprolol tartrate was observed in a study performed in rats at doses up to 22 times, on a mg/m 2 basis, the daily dose of 200 mg in a 60 kg patient.
14 CLINICAL STUDIES
In five controlled studies in normal healthy subjects, the same daily doses of Metoprolol Succinate Extended-Release Tablets and immediate-release metoprolol were compared in terms of the extent and duration of beta 1-blockade produced. Both formulations were given in a dose range equivalent to 100 to 400 mg of immediate-release metoprolol per day. In these studies, Metoprolol Succinate Extended-Release Tablets was administered once a day and immediate-release metoprolol was administered once to four times a day. A sixth controlled study compared the beta 1-blocking effects of a 50 mg daily dose of the two formulations. In each study, beta 1-blockade was expressed as the percent change from baseline in exercise heart rate following standardized submaximal exercise tolerance tests at steady state. Metoprolol Succinate Extended-Release Tablets administered once a day, and immediate-release metoprolol administered once to four times a day, provided comparable total beta 1-blockade over 24 hours (area under the beta 1-blockade versus time curve) in the dose range 100 to 400 mg. At a dosage of 50 mg once daily, Metoprolol Succinate Extended-Release Tablets produced significantly higher total beta 1-blockade over 24 hours than immediate-release metoprolol. For Metoprolol Succinate Extended-Release Tablets, the percent reduction in exercise heart rate was relatively stable throughout the entire dosage interval and the level of beta1-blockade increased with increasing doses from 50 to 300 mg daily. The effects at peak/trough (i.e., at 24-hours post-dosing) were: 14/9, 16/10, 24/14, 27/22 and 27/20% reduction in exercise heart rate for doses of 50, 100, 200, 300 and 400 mg Metoprolol Succinate Extended-Release Tablets once a day, respectively. In contrast to Metoprolol Succinate Extended-Release Tablets, immediate-release metoprolol given at a dose of 50 to100 mg once a day produced a significantly larger peak effect on exercise tachycardia, but the effect was not evident at 24 hours. To match the peak to trough ratio obtained with Metoprolol Succinate Extended-Release Tablets over the dosing range of 200 to 400 mg, a t.i.d. to q.i.d. divided dosing regimen was required for immediate-release metoprolol. A controlled cross-over study in heart failure patients compared the plasma concentrations and beta 1-blocking effects of 50 mg immediate-release metoprolol administered t.i.d., 100 mg and 200 mg Metoprolol Succinate Extended-Release Tablets once daily. A 50 mg dose of immediate-release metoprolol t.i.d. produced a peak plasma level of metoprolol similar to the peak level observed with 200 mg of Metoprolol Succinate Extended-Release Tablets. A 200 mg dose of Metoprolol Succinate Extended-Release Tablets produced a larger effect on suppression of exercise-induced and Holter-monitored heart rate over 24 hours compared to 50 mg t.i.d. of immediate-release metoprolol.
In a double-blind study, 1092 patients with mild-to-moderate hypertension were randomized to once daily Metoprolol Succinate Extended-Release Tablets (25, 100, or 400 mg), PLENDIL ® (felodipine extended-release tablets), the combination, or placebo. After 9 weeks, Metoprolol Succinate Extended-Release Tablets alone decreased sitting blood pressure by 6 to 8/4 to 7 mmHg (placebo-corrected change from baseline) at 24 hours post-dose. The combination of Metoprolol Succinate Extended-Release Tablets with PLENDIL has greater effects on blood pressure.
In controlled clinical studies, an immediate-release dosage form of metoprolol was an effective antihypertensive agent when used alone or as concomitant therapy with thiazidetype diuretics at dosages of 100 to 450 mg daily. Metoprolol Succinate Extended-Release Tablets, in dosages of 100 to 400 mg once daily, produces similar β 1-blockade as conventional metoprolol tablets administered two to four times daily. In addition, Metoprolol Succinate Extended-Release Tablets administered at a dose of 50 mg once daily lowered blood pressure 24-hours post-dosing in placebo-controlled studies. In controlled, comparative, clinical studies, immediate-release metoprolol appeared comparable as an antihypertensive agent to propranolol, methyldopa, and thiazide-type diuretics, and affected both supine and standing blood pressure. Because of variable plasma levels attained with a given dose and lack of a consistent relationship of antihypertensive activity to drug plasma concentration, selection of proper dosage requires individual titration.
14.1 Angina Pectoris
By blocking catecholamine-induced increases in heart rate, in velocity and extent of myocardial contraction, and in blood pressure, metoprolol reduces the oxygen requirements of the heart at any given level of effort, thus making it useful in the long-term management of angina pectoris.
In controlled clinical trials, an immediate-release formulation of metoprolol has been shown to be an effective antianginal agent, reducing the number of angina attacks and increasing exercise tolerance. The dosage used in these studies ranged from 100 to 400 mg daily. Metoprolol Succinate Extended-Release Tablets, in dosages of 100 to 400 mg once daily, have been shown to possess beta-blockade similar to conventional metoprolol tablets administered two to four times daily.
14.2 Heart Failure
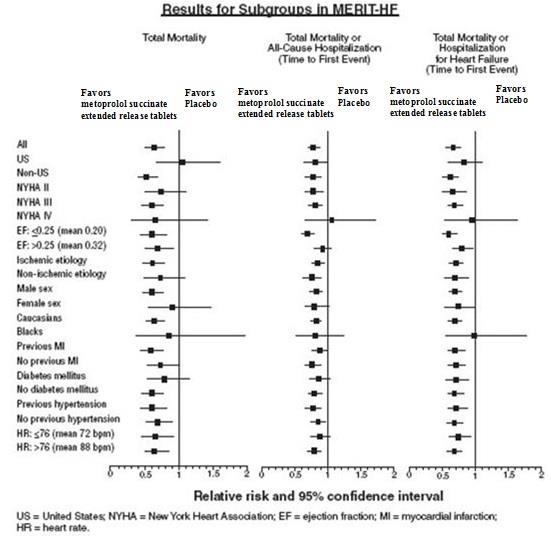
MERIT-HF was a double-blind, placebo-controlled study of Metoprolol Succinate Extended-Release Tablets conducted in 14 countries including the US. It randomized 3991 patients (1990 to Metoprolol Succinate Extended-Release Tablets) with ejection fraction ≤ 0.40 and NYHA Class II-IV heart failure attributable to ischemia, hypertension, or cardiomyopathy. The protocol excluded patients with contraindications to beta-blocker use, those expected to undergo heart surgery, and those within 28 days of myocardial infarction or unstable angina. The primary endpoints of the trial were (1) all-cause mortality plus all-cause hospitalization (time to first event) and (2) all-cause mortality. Patients were stabilized on optimal concomitant therapy for heart failure, including diuretics, ACE inhibitors, cardiac glycosides, and nitrates. At randomization, 41% of patients were NYHA Class II; 55% NYHA Class III; 65% of patients had heart failure attributed to ischemic heart disease; 44% had a history of hypertension; 25% had diabetes mellitus; 48% had a history of myocardial infarction. Among patients in the trial, 90% were on diuretics, 89% were on ACE inhibitors, 64% were on digitalis, 27% were on a lipid-lowering agent, 37% were on an oral anticoagulant, and the mean ejection fraction was 0.28. The mean duration of follow-up was one year. At the end of the study, the mean daily dose of Metoprolol Succinate Extended-Release Tablets was 159 mg.
The trial was terminated early for a statistically significant reduction in all-cause mortality (34%, nominal p= 0.00009). The risk of all-cause mortality plus all-cause hospitalization was reduced by 19% (p= 0.00012). The trial also showed improvements in heart failure-related mortality and heart failure-related hospitalizations, and NYHA functional class.
The table below shows the principal results for the overall study population. The figure below illustrates principal results for a wide variety of subgroup comparisons, including US vs. non-US populations (the latter of which was not pre-specified). The combined endpoints of all-cause mortality plus all-cause hospitalization and of mortality plus heart failure hospitalization showed consistent effects in the overall study population and the subgroups, including women and the US population. However, in the US subgroup (n=1071) and women (n=898), overall mortality and cardiovascular mortality appeared less affected. Analyses of female and US patients were carried out because they each represented about 25% of the overall population. Nonetheless, subgroup analyses can be difficult to interpret and it is not known whether these represent true differences or chance effects.
| Clinical Endpoint | Number of Patients | Relative Risk (95% Cl) | Risk Reduction With Metoprolol Succinate Extended-Release Tablets | Nominal P-value | |
| *Time to first event
†Comparison of treatment groups examines the number of hospitalizations (Wilcoxon test); relative risk and risk reduction are not applicable. |
|||||
| Placebo n=2001 | Metoprolol Succinate Extended-Release Tabletsn=1990 | ||||
| All-cause mortality plus all-caused hospitalization* | 767 | 641 | 0.81 (0.73 to 0.90) | 19% | 0.00012 |
| All-cause mortality | 217 | 145 | 0.66 (0.53 to 0.81) | 34% | 0.00009 |
| All-cause mortality plus heart failure hospitalization* | 439 | 311 | 0.69 (0.60 to 0.80) | 31% | 0.0000008 |
| Cardiovascular mortality | 203 | 128 | 0.62 (0.50 to 0.78) | 38% | 0.000022 |
| Sudden death | 132 | 79 | 0.59 (0.45 to 0.78) | 41% | 0.0002 |
| Death due to worsening heart failure | 58 | 30 | 0.51 (0.33 to 0.79) | 49% | 0.0023 |
| Hospitalizations due to worsening heart failure† | 451 | 317 | N/A | N/A | 0.0000076 |
| Cardiovascular hospitalization† | 773 | 649 | N/A | N/A | 0.00028 |
15 REFERENCES
1. Devereaux PJ, Yang H, Yusuf S, Guyatt G, Leslie K, Villar JC et al. Effects of extended-release metoprolol succinate in patients undergoing non-cardiac surgery (POISE trial): a randomised controlled trial. Lancet. 2008; 371:1839-47.
16 HOW SUPPLIED/STORAGE AND HANDLING
Tablets containing metoprolol succinate equivalent to the indicated weight of metoprolol tartrate, USP, are white, film-coated, and scored.
Metoprolol Succinate Extended-Release Tablets USP are supplied as follows:
100 mg tablets: White to off-white capsule-shaped film coated tablets with a score on one side and engraved with “P03” on the other side.
Bottle of 100: NDC# 64679-848-02
Bottle of 500: NDC# 64679-848-03
Bottle of 1000: NDC# 64679-848-10
200 mg tablets: White to off-white oval film coated tablets with a score on one side and engraved with “P04” on the other side.
Bottle of 100: NDC# 64679-849-02
Bottle of 500: NDC# 64679-849-03
Store at 20° to 25°C (68° to 77°F); excursions permitted to 15° to 30°C (59° to 86°F). [see USP Controlled Room Temperature]
17 PATIENTS COUNSELING INFORMATION INFORMATION FOR PATIENTS
Advise patients to take Metoprolol Succinate Extended-Release Tablets regularly and continuously, as directed, preferably with or immediately following meals. If a dose is missed, the patient should take only the next scheduled dose (without doubling it). Patients should not interrupt or discontinue Metoprolol Succinate Extended-Release Tablets without consulting the physician.
Advise patients (1) to avoid operating automobiles and machinery or engaging in other tasks requiring alertness until the patient’s response to therapy with Metoprolol Succinate Extended-Release Tablets has been determined; (2) to contact the physician if any difficulty in breathing occurs; (3) to inform the physician or dentist before any type of surgery that he or she is taking Metoprolol Succinate Extended-Release Tablets.
Heart failure patients should be advised to consult their physician if they experience signs or symptoms of worsening heart failure such as weight gain or increasing shortness of breath.
PLENDIL is a trademark of the AstraZeneca group of companies.
Manufactured by:

Pharmadax Inc.
Guangdong Province, P.R. China 528244
Distributed by:
Wockhardt USA LLC.
20 Waterview Blvd.,
Parsippany NJ 07054 USA
Revised: 04/2021
Metoprolol Succinate Extended-Release Tablets USP, 100 mg
NDC: 64679-848-02
100 tablets
Metoprolol Succinate Extended-Release Tablets USP, 100 mg
Rx only

NDC: 64679-848-03
500 tablets
Metoprolol Succinate Extended-Release Tablets USP, 100 mg
Rx only

NDC: 64679-848-10
1000 tablets
Metoprolol Succinate Extended-Release Tablets USP, 100 mg
Rx only

Metoprolol Succinate Extended-Release Tablets USP, 200 mg
NDC: 64679-849-02
100 tablets
Metoprolol Succinate Extended-Release Tablets USP, 200 mg
Rx only

NDC: 64679-849-03
500 tablets
Metoprolol Succinate Extended-Release Tablets USP, 200 mg
Rx only

| METOPROLOL SUCCINATE
metoprolol succinate tablet, extended release |
||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||
| METOPROLOL SUCCINATE
metoprolol succinate tablet, extended release |
||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||
| Labeler - Wockhardt USA LLC. (170508365) |
| Registrant - Pharmadax Inc. (656535874) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| CorePharma, LLC | 031192276 | pack(64679-848, 64679-849) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Pharmadax (Foshan) Co.,Ltd | 421295980 | manufacture(64679-848, 64679-849) | |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.