LOPRESSOR- metoprolol tartrate tablet
LOPRESSOR by
Drug Labeling and Warnings
LOPRESSOR by is a Prescription medication manufactured, distributed, or labeled by VALIDUS PHARMACEUTICALS LLC, Rubicon Research Limited. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use LOPRESSOR ®safely and effectively. See full prescribing information for LOPRESSOR ®TABLETS.
LOPRESSOR ®(metoprolol tartrate) tablets, for oral use
Initial U.S. Approval: 1992INDICATIONS AND USAGE
LOPRESSOR is a beta-adrenergic blocker indicated in the treatment of hemodynamically stable adult patients with myocardial infarction, to reduce the risk of cardiovascular mortality. ( 1.1)
DOSAGE AND ADMINISTRATION
Myocardial Infarction: The recommended starting dosage is 50 mg orally every 6 hours. Maintenance dosage depends upon hemodynamic tolerance, see full prescribing information. ( 2.1)
DOSAGE FORMS AND STRENGTHS
Tablets: 12.5 mg. of metoprolol tartrate ( 3)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- Abrupt cessation may exacerbate myocardial ischemia. ( 5.1)
- Heart Failure: Worsening cardiac failure may occur. ( 5.2)
- Bronchospastic Disease: Avoid beta-blockers. ( 5.3)
- Pheochromocytoma: Initiate therapy with an alpha blocker. ( 5.4)
- Major Surgery: Avoid initiation of high-dose metoprolol in patients undergoing non- cardiac surgery. Do not routinely withdraw chronic beta-blocker therapy prior to surgery. ( 5.5, 6.1)
- Diabetes: May mask symptoms of hypoglycemia. ( 5.6)
- Thyrotoxicosis: Abrupt withdrawal in patients with thyrotoxicosis might precipitate a thyroid storm. ( 5.7)
- Peripheral Vascular Disease: Can aggravate symptoms of arterial insufficiency. ( 5.9)
ADVERSE REACTIONS
- Most common adverse reactions in the setting of treatment of myocardial infarction are hypotension and bradycardia. ( 6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Validus Pharmaceuticals LLC at 1-866-982-5438 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
- Catecholamine-depleting drugs may have an additive effect when given with beta-blocking agents. ( 7.1)
- Patients may be unresponsive to the usual doses of epinephrine used to treat allergic reaction. ( 7.2)
- CYP2D6 Inhibitors are likely to increase metoprolol concentration. ( 7.3)
- Concomitant use of glycosides, clonidine, and diltiazem and verapamil with beta-blockers can increase the risk of bradycardia. ( 7.4)
- Beta-blockers including metoprolol, may exacerbate the rebound hypertension that can follow the withdrawal of clonidine. ( 7.4)
USE IN SPECIFIC POPULATIONS
- Hepatic Impairment: Consider initiating LOPRESSOR therapy at low doses and gradually increase dosage to optimize therapy, while monitoring closely for adverse events. ( 8.6)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 11/2025
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
1.1 Myocardial Infarction
2 DOSAGE AND ADMINISTRATION
2.1 Myocardial Infarction
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Abrupt Cessation of Therapy
5.2 Heart Failure
5.3 Bronchospastic Disease
5.4 Pheochromocytoma
5.5 Major Surgery
5.6 Hypoglycemia
5.7 Thyrotoxicosis
5.8 Risk of Anaphylactic Reactions
5.9 Peripheral Vascular Disease
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Post-Marketing Experience
7 DRUG INTERACTIONS
7.1 Catecholamine Depleting Drugs
7.2 Epinephrine
7.3 CYP2D6 Inhibitors
7.4 Negative Chronotropes
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Hepatic Impairment
8.7 Renal Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
12.5 Pharmacogenomics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Myocardial Infarction
16 HOW SUPPLIED/ STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 Myocardial Infarction
The recommended starting dose in hemodynamically stable patients is 50 mg orally every 6 hours. In case of intolerance, reduce the starting dose to 25 mg orally every 6 hours and administer for 48 hours. Titrate dosage based on tolerability and hemodynamic parameters (i.e., heart rate, blood pressure). LOPRESSOR should preferably be administered with or following meals. The maximum daily maintenance dosage is 100 mg orally twice daily.
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
LOPRESSOR is contraindicated in severe bradycardia, second or third degree heart block, cardiogenic shock, systolic blood pressure <100, decompensated heart failure, sick sinus syndrome (unless a permanent pacemaker is in place), and in patients who are hypersensitive to any component of this product.
-
5 WARNINGS AND PRECAUTIONS
5.1 Abrupt Cessation of Therapy
Following abrupt cessation of therapy with certain beta-blocking agents, exacerbations of angina pectoris and, in some cases, myocardial infarction have occurred. When discontinuing chronically administered LOPRESSOR, gradually reduce the dosage over a period of 1 to 2 weeks and monitor the patient. Warn patients not to interrupt therapy without their physician’s advice.
5.2 Heart Failure
Worsening cardiac failure may occur during up-titration of LOPRESSOR. If such symptoms occur, increase diuretics and restore clinical stability before advancing the dose of LOPRESSOR [see Dosage and Administration (2)]. It may be necessary to lower the dose of LOPRESSOR or temporarily discontinue it. Such episodes do not preclude subsequent successful titration of LOPRESSOR.
5.3 Bronchospastic Disease
Patients with bronchospastic disease, should in general, not receive beta-blockers, including LOPRESSOR. Because of its relative beta 1cardio-selectivity, however, LOPRESSOR may be used in patients with bronchospastic disease who do not respond to, or cannot tolerate, other antihypertensive treatment. Because beta1-selectivity is not absolute, use the lowest possible dose of LOPRESSOR. Bronchodilators, including beta 2-agonists, should be readily available or administered concomitantly [see Dosage and Administration (2)].
5.4 Pheochromocytoma
If LOPRESSOR is used in the setting of pheochromocytoma, it should be given in combination with an alpha blocker, and only after the alpha blocker has been initiated. Administration of beta-blockers alone in the setting of pheochromocytoma has been associated with a paradoxical increase in blood pressure due to the attenuation of beta-mediated vasodilatation in skeletal muscle.
5.5 Major Surgery
Avoid initiation of a high-dose regimen of beta blocker therapy in patients undergoing non-cardiac surgery, since such use in patients with cardiovascular risk factors has been associated with bradycardia, hypotension, stroke and death.
Chronically administered beta-blocking therapy should not be routinely withdrawn prior to major surgery, however, the impaired ability of the heart to respond to reflex adrenergic stimuli may augment the risks of general anesthesia and surgical procedures.
5.6 Hypoglycemia
Beta-blockers may prevent early warning signs of hypoglycemia, such as tachycardia, and increase the risk for severe or prolonged hypoglycemia at any time during treatment, especially in patients with diabetes mellitus or children and patients who are fasting (i.e., surgery, not eating regularly, or are vomiting). If severe hypoglycemia occurs, patients should be instructed to seek emergency treatment.
5.7 Thyrotoxicosis
Beta-adrenergic blockade may mask certain clinical signs of hyperthyroidism, such as tachycardia. Abrupt withdrawal of beta-blockade may precipitate a thyroid storm.
5.8 Risk of Anaphylactic Reactions
While taking beta-blockers, patients with a history of severe anaphylactic reaction to a variety of allergens may be more reactive to repeated challenge, either accidental, diagnostic, or therapeutic. Such patients may be unresponsive to the usual doses of epinephrine used to treat allergic reaction.
-
6 ADVERSE REACTIONS
The following adverse reactions are described elsewhere in labeling:
- Worsening Ischemia with Abrupt Discontinuation [see Warnings and Precautions (5)]
- Worsening heart failure [see Warnings and Precautions (5)].
- Worsening atrioventricular (AV) block [see Contraindications (4)].
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Myocardial Infarction
In a randomized comparison of LOPRESSOR and placebo in the setting of acute MI [see Clinical studies 14.1] the following adverse reactions were reported:
Adverse Reaction LOPRESSOR
N=698
%Placebo
N=697
%Hypotension (systolic BP < 90 mm Hg) 27.4% 23.2% Bradycardia (heart rate < 40 beats/min) 15.9% 6.7% Second- or third-degree heart block 4.7% 4.7% First-degree heart block (P-R ≥ 0.26 sec) 5.3% 1.9% Heart failure 27.5% 29.6% 6.2 Post-Marketing Experience
The following adverse reactions have been reported during post-approval use of LOPRESSOR. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Central Nervous System:Reversible mental depression progressing to catatonia; an acute reversible syndrome characterized by disorientation for time and place, short-term memory loss, emotional lability, slightly clouded sensorium, and decreased cognitive performance.
Cardiovascular: Worsening AV block [see Contraindications (4)].
Hematologic:Agranulocytosis, nonthrombocytopenic purpura and thrombocytopenic purpura.
Hypersensitive Reactions:Fever combined with aching and sore throat, laryngospasm and respiratory distress.
Laboratory Findings:
Increase in blood triglycerides, elevated transaminase and decrease in high-density lipoprotein (HDL)
-
7 DRUG INTERACTIONS
7.1 Catecholamine Depleting Drugs
Observe patients treated with LOPRESSOR plus a catecholamine depletor for evidence of hypotension or marked bradycardia, which may produce vertigo, syncope, or postural hypotension. Catecholamine depleting drugs (e.g., reserpine, monoamine oxidase (MAO) inhibitors) may have an additive effect when given with beta-blocking agents.
7.2 Epinephrine
The cardiostimulating and bronchodilating effects of epinephrine are antagonized by beta-adrenergic blocking drugs, such as metoprolol. Higher doses of epinephrine might be necessary for patients taking metoprolol.
7.3 CYP2D6 Inhibitors
Monitor patients closely when the combination use of CYP2D6 inhibitor and metoprolol cannot be avoided. Drugs that are strong inhibitors of CYP2D6 such as quinidine, fluoxetine, paroxetine, and propafenone were shown to double metoprolol concentrations. While there is no information about moderate or weak inhibitors, these may also increase metoprolol concentration. Increases in plasma concentration decrease the beta 1cardioselectivity of metoprolol [see Clinical Pharmacology (12.3)] .
7.4 Negative Chronotropes
If clonidine and metoprolol are coadministered, withdraw the beta-blocker several days before the gradual withdrawal of clonidine because metoprolol may exacerbate the rebound hypertension that can follow the withdrawal of clonidine. If replacing clonidine with metoprolol, delay the introduction of metoprolol for several days after clonidine discontinuation.
Digitalis glycosides, clonidine, diltiazem, and verapamil slow atrioventricular conduction and decrease heart rate. Concomitant use with beta blockers can increase the risk of bradycardia.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Available data from published observational studies have not demonstrated an association of adverse developmental outcomes with maternal use of metoprolol during pregnancy (see Data) . Untreated myocardial infarction during pregnancy can lead to adverse outcomes for the mother and the fetus (see Clinical Considerations) . In animal reproduction studies, metoprolol has been shown to increase post- implantation loss and decrease neonatal survival in rats at oral dosages of 500 mg/kg/day, approximately 11 times the daily dose of 450 mg in a 60-kg patient on a mg/m 2basis.
All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Fetal/Neonatal adverse reactions
Metoprolol crosses the placenta. Neonates born to mothers who are receiving metoprolol during pregnancy, may be at risk for hypotension, hypoglycemia, bradycardia, and respiratory depression. Observe neonates and manage accordingly.
Human Data
Data from published observational studies did not demonstrate an association of major congenital malformations and use of metoprolol in pregnancy. The published literature has reported inconsistent findings of intrauterine growth retardation, preterm birth and perinatal mortality with maternal use of metoprolol during pregnancy; however, these studies have methodological limitations hindering interpretation. Methodological limitations include retrospective design, concomitant use of other medications, and other unadjusted confounders that may account for the study findings including the underlying disease in the mother. These observational studies cannot definitively establish or exclude any drug-associated risk during pregnancy.
Animal Data
Metoprolol has been shown to increase post-implantation loss and decrease neonatal survival in rats at oral dosages of 500 mg/kg/day, i.e. 11 times, on a mg/m 2basis, the daily dose of 450 mg in a 60-kg patient.
No fetal abnormalities were observed when pregnant rats received metoprolol orally up to a dose of 200 mg/kg/day, i.e. 4 times, the daily dose of 400mg in a 60-kg patient.
8.2 Lactation
Risk Summary
Limited available data from published literature report that metoprolol is present in human milk. The estimated daily infant dose of metoprolol received from breastmilk ranges from 0.05 mg to less than 1 mg. The estimated relative infant dosage was 0.5% to 2% of the mother's weight-adjusted dosage (see Data). No adverse reactions of metoprolol on the breastfed infant have been identified. There is no information regarding the effects of metoprolol on milk production.
Clinical consideration
Monitoring for adverse reactions
For a lactating woman who is a slow metabolizer of metoprolol, monitor the breastfed infant for bradycardia and other symptoms of beta blockade such as dry mouth, skin or eyes, diarrhea or constipation. In a report of 6 mothers taking metoprolol, none reported adverse effects in her breastfed infant.
Limited published cases estimate the infant daily dose of metoprolol received from breast milk range from 0.05 mg to less than 1 mg.
In 2 women who were taking unspecified amount of metoprolol, milk samples were taken after one dose of metoprolol. The estimated amount of metoprolol and alpha-hydroxymetoprolol in breast milk is reported to be less than 2% of the mother's weight-adjusted dosage.
In a small study, breast milk was collected every 2 to 3 hours over one dosage interval, in three mothers (at least 3 months postpartum) who took metoprolol of unspecified amount. The average amount of metoprolol present in breast milk was 71.5 mcg/day (range 17.0 mcg to 158.7 mcg). The average relative infant dosage was 0.5% of the mother's weight-adjusted dosage.
8.3 Females and Males of Reproductive Potential
Risk Summary
Based on the published literature, beta blockers (including metoprolol) may cause erectile dysfunction and inhibit sperm motility. In animal fertility studies, metoprolol has been associated with reversible adverse effects on spermatogenesis starting at oral dose level of 3.5 mg/kg in rats, which would correspond to a dose of 34 mg/day in humans in mg/m 2 equivalent, although other studies have shown no effect of metoprolol on reproductive performance in male rats.
No evidence of impaired fertility due to metoprolol was observed in rats [see Nonclinical Toxicology (13.1)].
8.4 Pediatric Use
Safety and effectiveness of LOPRESSOR have not been established in pediatric patients.
8.5 Geriatric Use
In worldwide clinical trials of LOPRESSOR in myocardial infarction, where approximately 478 patients were over 65 years of age (0 over 75 years of age), no age-related differences in safety and effectiveness were found. Other reported clinical experience in myocardial infarction has not identified differences in response between the elderly and younger patients.
In general, use a low initial starting dose in elderly patients given their greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
8.6 Hepatic Impairment
No studies have been performed with LOPRESSOR in patients with hepatic impairment. LOPRESSOR is metabolized by the liver, metoprolol blood levels are likely to increase substantially with poor hepatic function. Therefore, initiate therapy at doses lower than those recommended; and increase doses gradually in patients with impaired hepatic function.
8.7 Renal Impairment
The systemic availability and half-life of metoprolol in patients with renal failure do not differ to a clinically significant degree from those in normal subjects. No reduction in dosage is needed in patients with renal failure [see Clinical Pharmacology (12.3)] .
-
10 OVERDOSAGE
Signs and Symptoms - Overdosage of LOPRESSOR may lead to severe bradycardia, hypotension, and cardiogenic shock. Clinical presentation can also include AV block, heart failure, bronchospasm, hypoxia, impairment of consciousness/coma, nausea, and vomiting.
Treatment – Consider treating the patient with intensive care. Patients with myocardial infarction or heart failure may be prone to significant hemodynamic instability. Beta-blocker overdose may result in significant resistance to resuscitation with adrenergic agents, including beta-agonists. On the basis of the pharmacologic actions of metoprolol, employ the following measures.
Hemodialysis is unlikely to make a useful contribution to metoprolol elimination [see Clinical Pharmacology (12.3)] .
Bradycardia: Evaluate the need for atropine, adrenergic-stimulating drugs or pacemaker to treat bradycardia and conduction disorders.
Hypotension: Treat underlying bradycardia. Consider intravenous vasopressor infusion, such as dopamine or norepinephrine.
Heart failure and shock: May be treated when appropriate with suitable volume expansion, injection of glucagon (if necessary, followed by an intravenous infusion of glucagon), intravenous administration of adrenergic drugs such as dobutamine, with α 1receptor agonistic drugs added in presence of vasodilation.
Bronchospasm: Can usually be reversed by bronchodilators
-
11 DESCRIPTION
LOPRESSOR tablets contain metoprolol tartrate, a beta-adrenergic blocker. Metoprolol tartrate is (±)-1- (Isopropylamino)-3-[p-(2-methoxyethyl) phenoxy]-2-propanol L-(+)-tartrate (2:1) salt, and its structural formula is
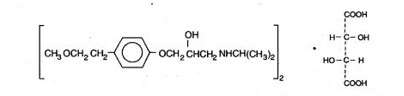
Metoprolol tartrate USP is a white, practically odorless, crystalline powder with a molecular weight of 684.82 g/mol. It is very soluble in water; freely soluble in methylene chloride, in chloroform, and in alcohol; slightly soluble in acetone; and insoluble in ether.
LOPRESSOR is available as 12.5 mg tablets for oral administration containing 12.5 mg metoprolol tartrate (equivalent to 9.76 mg of metoprolol).
Inactive Ingredients: Tablets contain colloidal silicon dioxide, lactose monohydrate, magnesium stearate, microcrystalline cellulose, sodium starch glycolate. Film coating contains D&C Red 30, hypromellose, polyethylene glycol, talc, and titanium dioxide.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Metoprolol is a beta 1-selective (cardioselective) adrenergic receptor blocking agent. This preferential effect is not absolute, however, and at higher plasma concentrations, metoprolol also inhibits beta 2-adrenoreceptors, chiefly located in the bronchial and vascular musculature.
Metoprolol has no intrinsic sympathomimetic activity, and membrane-stabilizing activity is detectable only at plasma concentrations much greater than required for beta-blockade. Animal and human experiments indicate that metoprolol slows the sinus rate and decreases AV nodal conduction.
The relative beta 1-selectivity of metoprolol has been confirmed by the following: (1) In normal subjects, metoprolol is unable to reverse the beta 2-mediated vasodilating effects of epinephrine. This contrasts with the effect of nonselective beta-blockers, which completely reverse the vasodilating effects of epinephrine. (2) In asthmatic patients, metoprolol reduces FEV 1and FVC significantly less than a nonselective beta-blocker, propranolol, at equivalent beta 1-receptor blocking doses.
12.2 Pharmacodynamics
Clinical pharmacology studies have confirmed the beta-blocking activity of metoprolol in humans, as shown by (1) reduction in heart rate and cardiac output at rest and upon exercise, (2) reduction of systolic blood pressure upon exercise, (3) inhibition of isoproterenol-induced tachycardia, and (4) reduction of reflex orthostatic tachycardia.
The relationship between plasma metoprolol levels and reduction in exercise heart rate is independent of the pharmaceutical formulation. Beta 1-blocking effects in the range of 30-80% of the maximal effect (approximately 8 to 23% reduction in exercise heart rate) correspond to metoprolol plasma concentrations from 30 to 540 nmol/L. The relative beta 1-selectivity of metoprolol diminishes, and blockade of beta 2-adrenoceptors increases at plasma concentration above 300 nmol/L.
12.3 Pharmacokinetics
Absorption:The estimated oral bioavailability of immediate release metoprolol is about 50% because of pre- systemic metabolism which is saturable leading to non-proportionate increase in the exposure with increased dose.
Distribution:Metoprolol is extensively distributed with a reported volume of distribution of 3.2 to 5.6 L/kg. About 10% of metoprolol in plasma is bound to serum albumin. Metoprolol is known to cross the placenta and is found in breast milk. Metoprolol is also known to cross the blood brain barrier following oral administration and cerebrospinal fluid (CSF) concentrations close to that observed in plasma have been reported. Metoprolol is not a significant P-glycoprotein substrate.
Elimination:
Elimination of LOPRESSOR is mainly by biotransformation in the liver. The mean elimination half-life of metoprolol is 3 to 4 hours; in poor CYP2D6 metabolizers the half-life may be 7 to 9 hours.
Metabolism:LOPRESSOR is primarily metabolized by CYP2D6. Metoprolol is a racemic mixture of R- and S- enantiomers, and when administered orally, it exhibits stereoselective metabolism that is dependent on oxidation phenotype. CYP2D6 is absent (poor metabolizers) in about 8% of Caucasians and about 2% of most other populations. Poor CYP2D6 metabolizers exhibit several-fold higher plasma concentrations of Metoprolol tartrate than extensive metabolizers with normal CYP2D6 activity thereby decreasing Metoprolol tartrate’s cardioselectivity.
Excretion: Approximately 95% of the dose can be recovered in urine. In most subjects (extensive metabolizers), less than 5% of an oral dose and the rest is excreted by the kidneys as metabolites that appear to have no beta-blocking activity. The renal clearance of the stereoisomers does not exhibit stereo-selectivity in renal excretion.
Specific populations
Geriatric patients:The geriatric population may show slightly higher plasma concentrations of metoprolol as a combined result of a decreased metabolism of the drug in elderly population and a decreased hepatic blood flow. However, this increase is not clinically significant or therapeutically relevant.
Patients with Renal impairment:The systemic availability and half-life of LOPRESSOR in patients with renal failure do not differ to a clinically significant degree from those in normal subjects.
Patients with Hepatic Impairment: Since the drug is primarily eliminated by hepatic metabolism, hepatic impairment may impact the pharmacokinetics of metoprolol.
Drug Interactions:
Metoprolol is metabolized predominantly by CYP2D6. In healthy subjects with CYP2D6 extensive metabolizer phenotype, coadministration of quinidine 100 mg, a potent CYP2D6 inhibitor, and immediate-release metoprolol 200 mg tripled the concentration of S-metoprolol and doubled the metoprolol elimination half-life. In four patients with cardiovascular disease, coadministration of propafenone 150 mg t.i.d. with immediate-release metoprolol 50 mg t.i.d. increased the steady-state metoprolol concentration 2- to 5-fold compared to metoprolol alone. Extensive metabolizers who concomitantly use CYP2D6 inhibiting drugs will have increased (several-fold) metoprolol blood levels, decreasing metoprolol's cardioselectivity [see Drug Interactions (7.2)].
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term studies in animals have been conducted to evaluate the carcinogenic potential of metoprolol tartrate. In 2-year studies in rats at three oral dosage levels of up to 800 mg/kg/day (19 times, on a mg/m 2basis, the daily dose of 400 mg for a 60-kg patient), there was no increase in the development of spontaneously occurring benign or malignant neoplasms of any type. The only histologic changes that appeared to be drug related were an increased incidence of generally mild focal accumulation of foamy macrophages in pulmonary alveoli and a slight increase in biliary hyperplasia. In a 21-month study in Swiss albino mice at three oral dosage levels of up to 750 mg/kg/day (9 times, on a mg/m 2basis, the daily dose of 400 mg for a 60-kg patient), benign lung tumors (small adenomas) occurred more frequently in female mice receiving the highest dose than in untreated control animals. There was no increase in malignant or total (benign plus malignant) lung tumors, nor in the overall incidence of tumors or malignant tumors. This 21-month study was repeated in CD-1 mice, and no statistically or biologically significant differences were observed between treated and control mice of either sex for any type of tumor.
All genotoxicity tests performed on metoprolol tartrate (a dominant lethal study in mice, chromosome studies in somatic cells, a Salmonella/mammalian-microsome mutagenicity test, and a nucleus anomaly test in somatic interphase nuclei) and metoprolol succinate (a Salmonella/mammalian-microsome mutagenicity test) were negative.
No evidence of impaired fertility due to metoprolol tartrate was observed in a study performed in rats at doses up to 55.5 times, on a mg/m 2basis, the daily dose of 450 mg in a 60-kg patient.
-
14 CLINICAL STUDIES
14.1 Myocardial Infarction
The study supporting the approval of metoprolol post-myocardial infarction to reduce cardiovascular mortality was conducted before the reperfusion era. In this double-blind, placebo-controlled study, 1395 patients with suspected acute myocardial infarction were randomized to LOPRESSOR or placebo. LOPRESSOR reduced 3-month cardiovascular mortality by 36%.
Patients were randomized and treated as soon as possible after arrival in the hospital, once their clinical condition had stabilized and their hemodynamic status had been carefully evaluated. Subjects were ineligible if they had hypotension, bradycardia, peripheral signs of shock, and/or more than minimal basal rales as signs of congestive heart failure. Initial treatment consisted of intravenous followed by oral administration of LOPRESSOR or placebo, given in a coronary care or comparable unit. Oral maintenance therapy with LOPRESSOR or placebo was continued for 3 months. The median delay from the onset of symptoms to the initiation of therapy was 8 hours in both the LOPRESSOR - and placebo-treatment groups. Among patients treated with LOPRESSOR, there were comparable reductions in 3- month cardiovascular mortality for those treated early (≤ 8 hours) and those in whom treatment was started later. Significant reductions in the incidence of ventricular fibrillation and in chest pain following initial intravenous therapy were also observed with LOPRESSOR and were independent of the interval between onset of symptoms and initiation of therapy.
-
16 HOW SUPPLIED/ STORAGE AND HANDLING
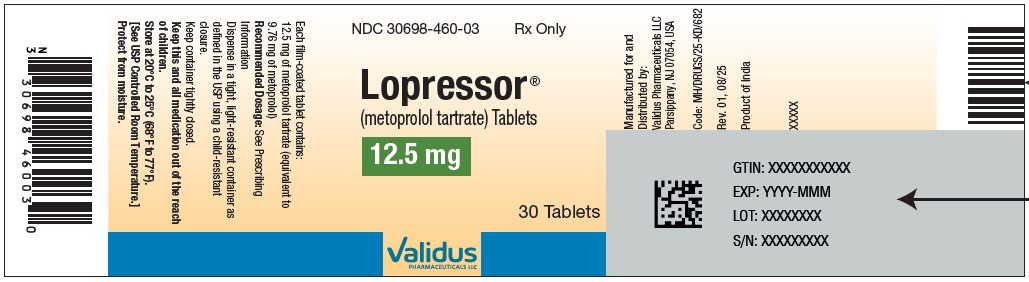
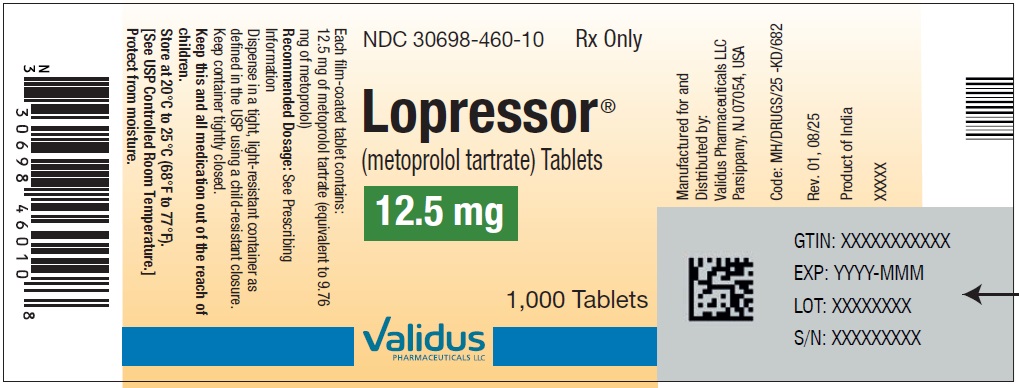
LOPRESSOR (metoprolol tartrate) tablets
Tablets 12.5 mg- pink colored film coated, round, biconvex tablets debossed with “˄E” on one side and plain on the other side. They are available as follows:
Bottles of 30 ………………………………………..NDC: 30698-460-03
Bottles of 60 ………………………………………..NDC: 30698-460-01
Bottles of 1,000 …………………………………….NDC: 30698-460-10
Storage:
Store at 20°C to 25°C (68°F to 77°F). [See USP Controlled Room Temperature.]
Protect from moisture.
Dispense in a tight, light-resistant container as defined in the USP using a child-resistant closure.
-
17 PATIENT COUNSELING INFORMATION
Advise patients to take LOPRESSOR regularly and continuously, as directed, preferably with or immediately following meals. If a dose is missed, the patient should take only the next scheduled dose (without doubling it). Patients should not interrupt or discontinue LOPRESSOR without consulting the physician.
Advise patients (1) to avoid operating automobiles and machinery or engaging in other tasks requiring alertness until the patient’s response to therapy with LOPRESSOR has been determined; (2) to contact the physician if any difficulty in breathing occurs; (3) to inform the physician or dentist before any type of surgery that he or she is taking LOPRESSOR.
Inform patients or caregivers that there is a risk of hypoglycemia when LOPRESSOR is given to patients who are fasting or who are vomiting. Instruct patients or caregivers how to monitor for signs of hypoglycemia [see Warnings and Precautions (5.6)].
Manufactured for and Distributed by:
Validus Pharmaceuticals LLC
Parsippany, NJ 07054, USA
info@validuspharma.com
www.validuspharma.comRevised: 01, 11/2025
-
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
Lopressor ®(metoprolol tartrate) Tablets, USP 12.5 mg - NDC: 30698-460-03 - 30s Bottle Label
Lopressor ®(metoprolol tartrate) Tablets, USP 12.5 mg - NDC: 30698-460-01 - 60s Bottle Label

Lopressor ®(metoprolol tartrate) Tablets, USP 12.5 mg - NDC: 30698-460-10 - 1,000s Bottle Label
-
INGREDIENTS AND APPEARANCE
LOPRESSOR
metoprolol tartrate tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 30698-460 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength METOPROLOL TARTRATE (UNII: W5S57Y3A5L) (METOPROLOL - UNII:GEB06NHM23) METOPROLOL TARTRATE 12.5 mg Inactive Ingredients Ingredient Name Strength SILICON DIOXIDE (UNII: ETJ7Z6XBU4) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MAGNESIUM STEARATE (UNII: 70097M6I30) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) SODIUM STARCH GLYCOLATE TYPE A POTATO (UNII: 5856J3G2A2) D&C RED NO. 30 (UNII: 2S42T2808B) HYPROMELLOSE, UNSPECIFIED (UNII: 3NXW29V3WO) POLYETHYLENE GLYCOL, UNSPECIFIED (UNII: 3WJQ0SDW1A) TALC (UNII: 7SEV7J4R1U) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) Product Characteristics Color pink Score no score Shape ROUND Size 5mm Flavor Imprint Code UpArrowheadE Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 30698-460-03 30 in 1 BOTTLE; Type 0: Not a Combination Product 08/11/2025 2 NDC: 30698-460-01 60 in 1 BOTTLE; Type 0: Not a Combination Product 01/25/2026 3 NDC: 30698-460-10 1000 in 1 BOTTLE; Type 0: Not a Combination Product 08/11/2025 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA218698 08/11/2025 Labeler - VALIDUS PHARMACEUTICALS LLC (801194619) Establishment Name Address ID/FEI Business Operations Rubicon Research Limited 677604197 manufacture(30698-460) , analysis(30698-460) , label(30698-460) , pack(30698-460)
Trademark Results [LOPRESSOR]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 LOPRESSOR 73098196 1105414 Live/Registered |
CIBA-GEIGY CORPORATION 1976-08-30 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.