LAMOTRIGINE EXTENDED RELEASE tablet
Lamotrigine Extended Release by
Drug Labeling and Warnings
Lamotrigine Extended Release by is a Prescription medication manufactured, distributed, or labeled by Bryant Ranch Prepack. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use LAMOTRIGINE EXTENDED-RELEASE TABLETS safely and effectively. See full prescribing information for LAMOTRIGINE EXTENDED-RELEASE TABLETS.
LAMOTRIGINE EXTENDED-RELEASE TABLETS, for oral use.
Initial U.S. Approval: 1994WARNING: SERIOUS SKIN RASHES
See full prescribing information for complete boxed warning.
Cases of life-threatening serious rashes, including Stevens-Johnson syndrome, and toxic-epidermal necrolysis, and/or rash-related death, have been caused by lamotrigine. The rate of serious rash is greater in pediatric patients than in adults. Additional factors that may increase the risk of rash include:
- coadministration with valproate
- exceeding recommended initial dose of lamotrigine extended-release
- exceeding recommended dose escalation of lamotrigine extended-release (5.1)
Benign rashes are also caused by lamotrigine; however, it is not possible to predict which rashes will prove to be serious or life-threatening. Lamotrigine extended-release should be discontinued at the first sign of rash, unless the rash is clearly not drug-related. ( 5.1)
RECENT MAJOR CHANGES
INDICATIONS AND USAGE
Lamotrigine extended-release is indicated for:
- Adjunctive therapy for primary generalized tonic-clonic seizures and partial-onset seizures with or without secondary generalization in patients aged 13 years and older. (1.1)
- Conversion to monotherapy in patients aged 13 years and older with partial-onset seizures who are receiving treatment with a single AED. (1.2)
Limitation of use: Safety and effectiveness in patients younger than 13 years have not been established. (1.3)
DOSAGE AND ADMINISTRATION
- Do not exceed the recommended initial dosage and subsequent dose escalation. (2.1)
- Initiation of adjunctive therapy and conversion to monotherapy requires slow titration dependent on concomitant AEDs; the prescriber must refer to the appropriate algorithm in Dosage and Administration. (2.2, 2.3)
- Conversion from immediate-release lamotrigine to lamotrigine extended-release: The initial dose of lamotrigine extended-release should match the total daily dose of the immediate-release lamotrigine. Patients should be closely monitored for seizure control after conversion. (2.4)
- Do not restart lamotrigine extended-release in patients who discontinued due to rash unless the potential benefits clearly outweigh the risks. (2.1, 5.1)
- Adjustments to maintenance doses will be necessary in most patients starting or stopping estrogen-containing oral contraceptives. (2.1, 5.7)
- Discontinuation: Taper over a period of at least two weeks (approximately 50% dose reduction per week). (2.1, 5.8)
DOSAGE FORMS AND STRENGTHS
CONTRAINDICATIONS
Hypersensitivity to the drug or its ingredients. (Boxed Warning, 4)
WARNINGS AND PRECAUTIONS
- Life-threatening serious rash and/or rash-related death: Discontinue at the first sign of rash, unless the rash is clearly not drug related. (Boxed Warning, 5.1)
- Fatal or life-threatening hypersensitivity reaction: Multiorgan hypersensitivity reactions, also known as drug reaction with eosinophilia and systemic symptoms (DRESS), may be fatal or life threatening. Early signs may include rash, fever, and lymphadenopathy. These reactions may be associated with other organ involvement, such as hepatitis, hepatic failure, blood dyscrasias, or acute multiorgan failure. Lamotrigine extended-release should be discontinued if alternate etiology for this reaction is not found.(5.2)
- Blood dyscrasias (e.g., neutropenia, thrombocytopenia, pancytopenia): May occur, either with or without an associated hypersensitivity syndrome. Monitor for signs of anemia, unexpected infection, or bleeding. (5.3)
- Suicidal behavior and ideation: Monitor for suicidal thoughts or behaviors. (5.4)
- Aseptic meningitis: Monitor for signs of meningitis. (5.5)
- Medication errors due to product name confusion: Strongly advise patients to visually inspect tablets to verify the received drug is correct. (5.6, 16, 17)
ADVERSE REACTIONS
- Most common adverse reactions with use as adjunctive therapy (treatment difference between lamotrigine extended-release and placebo ≥4%) are dizziness, tremor/intention tremor, vomiting, and diplopia. (6.1)
- Most common adverse reactions with use as monotherapy were similar to those seen with previous trials conducted with immediate-release lamotrigine and lamotrigine extended-release. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Par Pharmaceutical, Inc. at 1-800-828-9393 and/or www.parpharm.com or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
- Valproate increases lamotrigine concentrations more than 2-fold. (7, 12.3)
- Carbamazepine, phenytoin, phenobarbital, primidone, and rifampin decrease lamotrigine concentrations by approximately 40%. (7, 12.3)
- Estrogen-containing oral contraceptives decrease lamotrigine concentrations by approximately 50%. (7, 12.3)
- Protease inhibitors lopinavir/ritonavir and atazanavir/lopinavir decrease lamotrigine exposure by approximately 50% and 32%, respectively. (7,12.3)
- Coadministration with organic cationic transporter 2 substrates with narrow therapeutic index is not recommended (7, 12.3).
USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 5/2017
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
BOXED WARNING
1 INDICATIONS AND USAGE
1.1 Adjunctive Therapy
1.2 Monotherapy
1.3 Limitation of Use
2 DOSAGE AND ADMINISTRATION
2.1 General Dosing Considerations
2.2 Adjunctive Therapy for Primary Generalized Tonic-Clonic and Partial-Onset Seizures
2.3 Conversion From Adjunctive Therapy to Monotherapy
2.4 Conversion From Immediate-Release Lamotrigine Tablets to Lamotrigine Extended-Release
3 DOSAGE FORMS AND STRENGTHS
3.1 Extended-Release Tablets
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Serious Skin Rashes (see Boxed Warning)
5.2 Multiorgan Hypersensitivity Reactions and Organ Failure
5.3 Blood Dyscrasias
5.4 Suicidal Behavior and Ideation
5.5 Aseptic Meningitis
5.6 Potential Medication Errors
5.7 Concomitant Use With Oral Contraceptives
5.8 Withdrawal Seizures
5.9 Status Epilepticus
5.10 Sudden Unexplained Death in Epilepsy (SUDEP)
5.11 Addition of Lamotrigine Extended-Release to a Multidrug Regimen That Includes Valproate
5.12 Binding in the Eye and Other Melanin-Containing Tissues
5.13 Laboratory Tests
6 ADVERSE REACTIONS
6.1 Clinical Trial Experience with Lamotrigine Extended-Release for Treatment of Primary Generalized Tonic-Clonic and Partial-Onset Seizures
6.2 Other Adverse Reactions Observed During the Clinical Development of Immediate-Release Lamotrigine
6.3 Postmarketing Experience with the Immediate-Release Lamotrigine
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Labor and Delivery
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Hepatic Impairment
8.7 Renal Impairment
10 OVERDOSAGE
10.1 Human Overdose Experience
10.2 Management of Overdose
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis and Mutagenesis and Impairment of Fertility
14 CLINICAL STUDIES
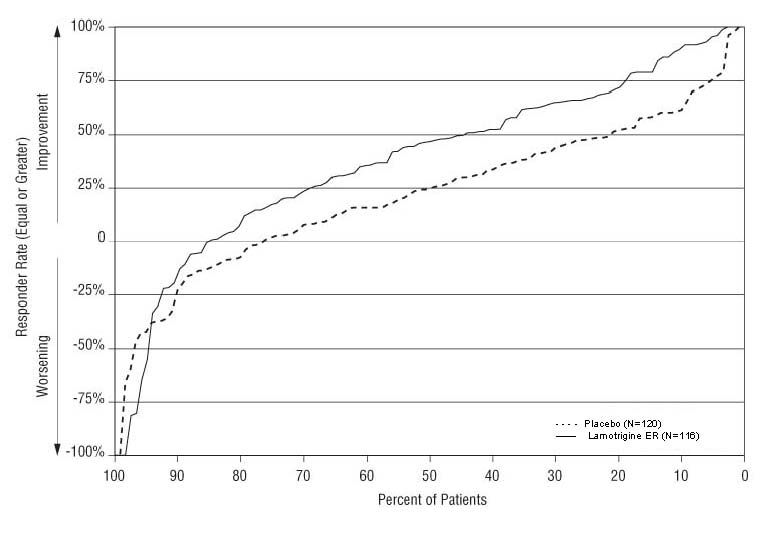
14.1 Adjunctive Therapy for Primary Generalized Tonic-Clonic Seizures
14.2 Adjunctive Therapy for Partial-Onset Seizures
14.3 Conversion to Monotherapy for Partial-Onset Seizures
15. References
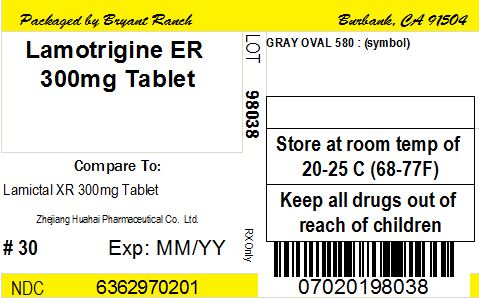
16 HOW SUPPLIED
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
BOXED WARNING
WARNING: SERIOUS SKIN RASHES
Lamotrigine extended-release can cause serious rashes requiring hospitalization and discontinuation of treatment. The incidence of these rashes, which have included Stevens-Johnson syndrome, is approximately 0.8% (8 per 1,000) in pediatric patients (aged 2 to 16 years) receiving immediate-release lamotrigine as adjunctive therapy for epilepsy and 0.3% (3 per 1,000) in adults on adjunctive therapy for epilepsy. In a prospectively followed cohort of 1,983 pediatric patients (aged 2 to 16 years) with epilepsy taking adjunctive immediate-release lamotrigine, there was 1 rash-related death. Lamotrigine extended-release is not approved for patients younger than 13 years. In worldwide postmarketing experience, rare cases of toxic epidermal necrolysis and/or rash-related death have been reported in adult and pediatric patients, but their numbers are too few to permit a precise estimate of the rate.
The risk of serious rash caused by treatment with lamotrigine extended-release is not expected to differ from that with immediate-release lamotrigine. However, the relatively limited treatment experience with lamotrigine extended-release makes it difficult to characterize the frequency and risk of serious rashes caused by treatment with lamotrigine extended-release.
Other than age, there are as yet no factors identified that are known to predict the risk of occurrence or the severity of rash caused by lamotrigine extended-release. There are suggestions, yet to be proven, that the risk of rash may also be increased by (1) coadministration of lamotrigine extended-release with valproate (includes valproic acid and divalproex sodium), (2) exceeding the recommended initial dose of lamotrigine extended-release, or (3) exceeding the recommended dose escalation for lamotrigine extended-release. However, cases have occurred in the absence of these factors.
Nearly all cases of life-threatening rashes caused by immediate-release lamotrigine have occurred within 2 to 8 weeks of treatment initiation. However, isolated cases have occurred after prolonged treatment (e.g., 6 months). Accordingly, duration of therapy cannot be relied upon as means to predict the potential risk heralded by the first appearance of a rash.
Although benign rashes are also caused by lamotrigine extended-release, it is not possible to predict reliably which rashes will prove to be serious or life-threatening. Accordingly, lamotrigine extended-release should ordinarily be discontinued at the first sign of rash, unless the rash is clearly not drug-related. Discontinuation of treatment may not prevent a rash from becoming life-threatening or permanently disabling or disfiguring [see Warnings and Precautions
( 5.1)].
-
1 INDICATIONS AND USAGE
1.1 Adjunctive Therapy
Lamotrigine extended-release is indicated as adjunctive therapy for primary generalized tonic-clonic (PGTC) seizures and partial-onset seizures with or without secondary generalization in patients aged 13 years and older.
1.2 Monotherapy
Lamotrigine extended-release is indicated for conversion to monotherapy in patients aged 13 years and older with partial-onset seizures who are receiving treatment with a single antiepileptic drug (AED).
Safety and effectiveness of lamotrigine extended-release have not been established (1) as initial monotherapy or (2) for simultaneous conversion to monotherapy from two or more concomitant AEDs.
-
2 DOSAGE AND ADMINISTRATION
Lamotrigine Extended-Release Tablets are taken once daily, with or without food. Tablets must be swallowed whole and must not be chewed, crushed, or divided.
2.1 General Dosing Considerations
Rash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine extended-release with valproate, (2) exceeding the recommended initial dose of lamotrigine extended-release, or (3) exceeding the recommended dose escalation for lamotrigine extended-release. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine extended-release is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine extended-release not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine extended-release, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Extended-Release Added to Drugs Known to Induce or Inhibit Glucuronidation: Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine. Drugs that induce glucuronidation include carbamazepine, phenytoin, phenobarbital, primidone, rifampin, estrogen-containing oral contraceptives, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Valproate inhibits glucuronidation. For dosing considerations for lamotrigine extended-release in patients on estrogen-containing contraceptives and atazanavir/ritonavir, see below and Table 5. For dosing considerations for lamotrigine extended-release in patients on other drugs known to induce or inhibit glucuronidation, see Table 1 and Table 5.
Target Plasma Levels: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine extended-release should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine Extended-Release in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine extended-release should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine extended-release based on the concomitant AED or other concomitant medications (see Table 1). See below for adjustments to maintenance doses of lamotrigine extended-release in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine Extended-Release in Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: In women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions, (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine extended-release will in most cases need to be increased by as much as 2-fold over the recommended target maintenance dose in order to maintain a consistent lamotrigine plasma level.
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine extended-release and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation (pill-free week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine extended-release consistently occur during the pill-free week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the pill-free week are not recommended. For women taking lamotrigine extended-release in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine extended-release should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: In women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine extended-release will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine extended-release should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine extended-release in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine extended-release should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine extended-release in the presence of progestogens alone will likely not be needed.
Patients Taking Atazanavir/Ritonavir: While atazanavir/ritonavir does reduce the lamotrigine plasma concentration, no adjustments to the recommended dose-escalation guidelines for lamotrigine extended-release should be necessary solely based on the use of atazanavir/ritonavir. Dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine extended-release based on concomitant AED or other concomitant medications (see Table 1 and Table 5). In patients already taking maintenance doses of lamotrigine extended-release and not taking glucuronidation inducers, the dose of lamotrigine extended-release may need to be increased if atazanavir/ritonavir is added, or decreased if atazanavir/ritonavir is discontinued [see Clinical Pharmacology (12.3)].
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 subjects with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine extended-release should be based on patients’ concomitant medications (see Table 1); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with immediate-release lamotrigine. Because there is inadequate experience in this population, lamotrigine extended-release should be used with caution in these patients.
Discontinuation Strategy: For patients receiving lamotrigine extended-release in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine extended-release, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.8)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
2.2 Adjunctive Therapy for Primary Generalized Tonic-Clonic and Partial-Onset Seizures
This section provides specific dosing recommendations for patients aged 13 years and older. Specific dosing recommendations are provided depending upon concomitant AEDs or other concomitant medications.
Table 1. Escalation Regimen for Lamotrigine Extended-Release Tablets in Patients Aged 13 Years and Older a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see DRUG INTERACTIONS (7), Clinical Pharmacology (12.3)] In Patients TAKING Valproatea
In Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primodone,b or Valproatea
In Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb and NOT TAKING Valproatea
Weeks 1 and 2
25 mg every other day
25 mg every day
50 mg every day
Weeks 3 and 4
25 mg every day
50 mg every day
100 mg every day
Week 5
50 mg every day
100 mg every day
200 mg every day
Week 6
100 mg every day
150 mg every day
300 mg every day
Week 7
150 mg every day
200 mg every day
400 mg every day
Maintenance range (week 8 and onward)
200 to 250 mg every dayc
300 to 400 mg every dayc
400 to 600 mg every dayc
bDrugs that induce lamotrigine glucuronidation and increase clearance, other than the specified antiepileptic drugs, include estrogen-containing oral contraceptives, rifampin, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Dosing recommendations for oral contraceptives and the protease inhibitor atazanavir/ritonavir can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin and the protease inhibitor lopinavir/ritonavir should follow the same dosing titration/maintenance regimen used with antiepileptic drugs that induce glucuronidation and increase clearance [see DOSAGE AND ADMINISTRATION (2.1), DRUG INTERACTIONS (7), Clinical Pharmacology (12.3)].
cDose increases at week 8 or later should not exceed 100 mg daily at weekly intervals.
2.3 Conversion From Adjunctive Therapy to Monotherapy
The goal of the transition regimen is to attempt to maintain seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine extended-release.
To avoid an increased risk of rash, the recommended maintenance dosage range of lamotrigine extended-release as monotherapy is 250 to 300 mg given once daily.
The recommended initial dose and subsequent dose escalations for lamotrigine extended-release should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy with Lamotrigine Extended-Release: After achieving a dose of 500 mg/day of lamotrigine extended-release using the guidelines in Table 1, the concomitant enzyme-inducing AED should be withdrawn by 20% decrements each week over a 4 week period. Two weeks after completion of withdrawal of the enzyme-inducing AED, the dosage of lamotrigine extended-release may be decreased no faster than 100 mg/day each week to achieve the monotherapy maintenance dosage range of 250 to 300 mg/day.
The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial using immediate-release lamotrigine.
Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Extended-Release: The conversion regimen involves the 4 steps outlined in Table 2.
Table 2. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Extended-Release in Patients Aged 13 Years and Older With Epilepsy
Lamotrigine Extended-Release
Valproate
Step 1
Achieve a dose of 150 mg/day according to guidelines in Table 1.
Maintain established stable dose.
Step 2
Maintain at 150 mg/day.
Decrease dose by decrements no greater than 500 mg/day/week to 500 mg/day and then maintain for 1 week.
Step 3
Increase to 200 mg/day.
Simultaneously decrease to 250 mg/day and maintain for 1 week.
Step 4
Increase to 250 or 300 mg/day.
Discontinue.
Conversion From Adjunctive Therapy With Antiepileptic Drugs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy with Lamotrigine Extended-Release: After achieving a dosage of 250 to 300 mg/day of lamotrigine extended-release using the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4 week period. No adjustment to the monotherapy dose of lamotrigine extended-release is needed.
2.4 Conversion From Immediate-Release Lamotrigine Tablets to Lamotrigine Extended-Release
Patients may be converted directly from immediate-release lamotrigine to lamotrigine extended-release tablets. The initial dose of lamotrigine extended-release should match the total daily dose of immediate-release lamotrigine. However, some subjects on concomitant enzyme-inducing agents may have lower plasma levels of lamotrigine on conversion and should be monitored [see Clinical Pharmacology (12.3)].
Following conversion to lamotrigine extended-release, all patients (but especially those on drugs that induce lamotrigine glucuronidation) should be closely monitored for seizure control [see Drug Interactions (7)]. Depending on the therapeutic response after conversion, the total daily dose may need to be adjusted within the recommended dosing instructions (Table 1).
-
3 DOSAGE FORMS AND STRENGTHS
3.1 Extended-Release Tablets
25 mg, round, beige, biconvex, film-coated tablet debossed with “561” on one side and “Par” on the other
50 mg, round, white, biconvex, film-coated tablet debossed with “562” on one side and “Par” on the other
100 mg, round, brown, biconvex, film-coated tablet debossed with “563” on one side and “Par” on the other
200 mg, round, yellow, biconvex, film-coated tablet debossed with “564” on one side and “Par” on the other
250 mg, round, white, biconvex, film-coated tablet debossed with “604” on one side and “Par” on the other
300 mg, round, grey, biconvex, film-coated tablet debossed with “605” on one side and “Par” on the other
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Serious Skin Rashes (see Boxed Warning)
The risk of serious rash caused by treatment with lamotrigine extended-release is not expected to differ from that with the immediate-release lamotrigine [see Boxed Warning]. However, the relatively limited treatment experience with lamotrigine extended-release makes it difficult to characterize the frequency and risk of serious rashes caused by treatment with lamotrigine extended-release.
Pediatric Population: The incidence of serious rash associated with hospitalization and discontinuation of the immediate-release lamotrigine in a prospectively followed cohort of pediatric patients (aged 2 to 16 years) with epilepsy receiving adjunctive therapy with immediate-release lamotrigine was approximately 0.8% (16 of 1,983). When 14 of these cases were reviewed by 3 expert dermatologists, there was considerable disagreement as to their proper classification. To illustrate, one dermatologist considered none of the cases to be Stevens-Johnson syndrome; another assigned 7 of the 14 to this diagnosis. There was 1 rash-related death in this 1,983-patient cohort. Additionally, there have been rare cases of toxic epidermal necrolysis with and without permanent sequelae and/or death in U.S. and foreign postmarketing experience.
There is evidence that the inclusion of valproate in a multidrug regimen increases the risk of serious, potentially life-threatening rash in pediatric patients. In pediatric patients who used valproate concomitantly, 1.2% (6 of 482) experienced a serious rash compared with 0.6% (6 of 952) patients not taking valproate.
Lamotrigine extended-release is not approved in patients younger than 13 years.
Adult Population: Serious rash associated with hospitalization and discontinuation of the immediate-release lamotrigine occurred in 0.3% (11 of 3,348) of adult patients who received immediate-release lamotrigine in premarketing clinical trials of epilepsy. In worldwide postmarketing experience, rare cases of rash-related death have been reported, but their numbers are too few to permit a precise estimate of the rate.
Among the rashes leading to hospitalization were Stevens-Johnson syndrome, toxic epidermal necrolysis, angioedema, and those associated with multiorgan hypersensitivity [see Warnings and Precautions (5.2)].
There is evidence that the inclusion of valproate in a multidrug regimen increases the risk of serious, potentially life-threatening rash in adults. Specifically, of 584 patients administered immediate-release formulation of lamotrigine with valproate in epilepsy clinical trials, 6 (1%) were hospitalized in association with rash; in contrast, 4 (0.16%) of 2,398 clinical trial patients and volunteers administered the immediate-release formulation of lamotrigine in the absence of valproate were hospitalized.
Patients With History of Allergy or Rash to Other Antiepileptic Drugs: The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine extended-release is exceeded and in patients with a history of allergy or rash to other AEDs.
5.2 Multiorgan Hypersensitivity Reactions and Organ Failure
Multiorgan hypersensitivity reactions, also known as drug reaction with eosinophilia and systemic symptoms (DRESS), have occurred with lamotrigine. Some have been fatal or life threatening. DRESS typically, although not exclusively, presents with fever, rash and/or lymphadenopathy in association with other organ system involvement, such as hepatitis, nephritis, hematologic abnormalities, myocarditis, or myositis, sometimes resembling an acute viral infection. Eosinophilia is often present. This disorder is variable in its expression and other organ systems not noted here may be involved.
Fatalities associated with acute multiorgan failure and various degrees of hepatic failure have been reported in 2 of 3,796 adult patients and 4 of 2,435 pediatric patients who received lamotrigine in epilepsy clinical trials. Rare fatalities from multiorgan failure have also been reported in postmarketing use.
Isolated liver failure without rash or involvement of other organs has also been reported with lamotrigine.
It is important to note that early manifestations of hypersensitivity (e.g., fever, lymphadenopathy) may be present even though a rash is not evident. If such signs or symptoms are present, the patient should be evaluated immediately. Lamotrigine extended-release should be discontinued if an alternative etiology for the signs or symptoms cannot be established.
Prior to initiation of treatment with lamotrigine extended-release, the patient should be instructed that a rash or other signs or symptoms of hypersensitivity (e.g., fever, lymphadenopathy) may herald a serious medical event and that the patient should report any such occurrence to a physician immediately.
5.3 Blood Dyscrasias
There have been reports of blood dyscrasias with the immediate-release lamotrigine that may or may not be associated with multiorgan hypersensitivity (also known as DRESS) [see Warnings and Precautions (5.2)]. These have included neutropenia, leukopenia, anemia, thrombocytopenia, pancytopenia, and, rarely, aplastic anemia and pure red cell aplasia.
5.4 Suicidal Behavior and Ideation
AEDs, including lamotrigine extended-release, increase the risk of suicidal thoughts or behavior in patients taking these drugs for any indication. Patients treated with any AED for any indication should be monitored for the emergence or worsening of depression, suicidal thoughts or behavior, and/or any unusual changes in mood or behavior.
Pooled analyses of 199 placebo-controlled clinical trials (monotherapy and adjunctive therapy) of 11 different AEDs showed that patients randomized to one of the AEDs had approximately twice the risk (adjusted Relative Risk 1.8, 95% CI:1.2, 2.7) of suicidal thinking or behavior compared to patients randomized to placebo. In these trials, which had a median treatment duration of 12 weeks, the estimated incidence of suicidal behavior or ideation among 27,863 AED-treated patients was 0.43%, compared to 0.24% among 16,029 placebo-treated patients, representing an increase of approximately 1 case of suicidal thinking or behavior for every 530 patients treated. There were 4 suicides in drug-treated patients in the trials and none in placebo-treated patients, but the number of events is too small to allow any conclusion about drug effect on suicide.
The increased risk of suicidal thoughts or behavior with AEDs was observed as early as 1 week after starting treatment with AEDs and persisted for the duration of treatment assessed. Because most trials included in the analysis did not extend beyond 24 weeks, the risk of suicidal thoughts or behavior beyond 24 weeks could not be assessed.
The risk of suicidal thoughts or behavior was generally consistent among drugs in the data analyzed. The finding of increased risk with AEDs of varying mechanism of action and across a range of indications suggests that the risk applies to all AEDs used for any indication. The risk did not vary substantially by age (5 to 100 years) in the clinical trials analyzed.
Table 3 shows absolute and relative risk by indication for all evaluated AEDs.
Table 3. Risk by Indication for Antiepileptic Drugs in the Pooled Analysis Indication
Placebo Patients With Events Per 1,000 Patients
Drug Patients With Events Per 1,000 Patients
Relative Risk: Incidence of Events in Drug Patients/Incidence in Placebo Patients
Risk Difference: Additional Drug Patients With Events Per 1,000 Patients
Epilepsy
1.0
3.4
3.5
2.4
Psychiatric
5.7
8.5
1.5
2.9
Other
1.0
1.8
1.9
0.9
Total
2.4
4.3
1.8
1.9
The relative risk for suicidal thoughts or behavior was higher in clinical trials for epilepsy than in clinical trials for psychiatric or other conditions, but the absolute risk differences were similar for the epilepsy and psychiatric indications.
Anyone considering prescribing lamotrigine extended-release or any other AED must balance the risk of suicidal thoughts or behavior with the risk of untreated illness. Epilepsy and many other illnesses for which AEDs are prescribed are themselves associated with morbidity and mortality and an increased risk of suicidal thoughts and behavior. Should suicidal thoughts and behavior emerge during treatment, the prescriber needs to consider whether the emergence of these symptoms in any given patient may be related to the illness being treated.
Patients, their caregivers, and families should be informed that AEDs increase the risk of suicidal thoughts and behavior and should be advised of the need to be alert for the emergence or worsening of the signs and symptoms of depression, any unusual changes in mood or behavior, or the emergence of suicidal thoughts or suicidal behavior, or thoughts about self-harm. Behaviors of concern should be reported immediately to healthcare providers.
5.5 Aseptic Meningitis
Therapy with lamotrigine increases the risk of developing aseptic meningitis. Because of the potential for serious outcomes of untreated meningitis due to other causes, patients should also be evaluated for other causes of meningitis and treated as appropriate.
Postmarketing cases of aseptic meningitis have been reported in pediatric and adult patients taking lamotrigine for various indications. Symptoms upon presentation have included headache, fever, nausea, vomiting, and nuchal rigidity. Rash, photophobia, myalgia, chills, altered consciousness, and somnolence were also noted in some cases. Symptoms have been reported to occur within 1 day to one and a half months following the initiation of treatment. In most cases, symptoms were reported to resolve after discontinuation of lamotrigine. Re-exposure resulted in a rapid return of symptoms (from within 30 minutes to 1 day following re-initiation of treatment) that were frequently more severe. Some of the patients treated with lamotrigine who developed aseptic meningitis had underlying diagnoses of systemic lupus erythematosus or other autoimmune diseases.
Cerebrospinal fluid (CSF) analyzed at the time of clinical presentation in reported cases was characterized by a mild to moderate pleocytosis, normal glucose levels, and mild to moderate increase in protein. CSF white blood cell count differentials showed a predominance of neutrophils in a majority of the cases, although a predominance of lymphocytes was reported in approximately one third of the cases. Some patients also had new onset of signs and symptoms of involvement of other organs (predominantly hepatic and renal involvement), which may suggest that in these cases the aseptic meningitis observed was part of a hypersensitivity reaction [see Warnings and Precautions (5.2.)].
5.6 Potential Medication Errors
Medication errors involving lamotrigine have occurred. In particular, the name lamotrigine can be confused with the names of other commonly used medications. Medication errors may also occur between the different formulations of lamotrigine. To reduce the potential of medication errors, write and say lamotrigine extended-release clearly. Depictions of the lamotrigine extended-release tablets can be found in the Medication Guide. Each lamotrigine extended-release tablet has a distinct color and is printed with Par and 561, 562, 563, 564, 604 or 605. These distinctive features serve to identify the different presentations of the drug and thus may help reduce the risk of medication errors. Lamotrigine extended-release is supplied in round, unit-of-use bottles containing 30 tablets. Lamotrigine extended-release is also available in bottles of 100 and 500 tablets. The label on the bottle includes a depiction of the tablets that further communicates to patients and pharmacists that the medication is lamotrigine extended-release and the specific tablet strength included in the bottle. The unit-of-use-bottle with a distinctive bottle label feature serves to identify the different presentations of the drug and thus may help to reduce the risk of medication errors. To avoid the medication error of using the wrong drug or formulation, patients should be strongly advised to visually inspect their tablets to verify that they are lamotrigine extended-release each time they fill their prescription.
5.7 Concomitant Use With Oral Contraceptives
Some estrogen-containing oral contraceptives have been shown to decrease serum concentrations of lamotrigine [see Clinical Pharmacology (12.3)]. Dosage adjustments will be necessary in most patients who start or stop estrogen-containing oral contraceptives while taking lamotrigine extended-release [see Dosage and Administration (2.1)]. During the week of inactive hormone preparation (pill-free week) of oral contraceptive therapy, plasma lamotrigine levels are expected to rise, as much as doubling at the end of the week. Adverse reactions consistent with elevated levels of lamotrigine, such as dizziness, ataxia, and diplopia, could occur.
5.8 Withdrawal Seizures
As with other AEDs, lamotrigine extended-release should not be abruptly discontinued. In patients with epilepsy there is a possibility of increasing seizure frequency. Unless safety concerns require a more rapid withdrawal, the dose of lamotrigine extended-release should be tapered over a period of at least 2 weeks (approximately 50% reduction per week) [see Dosage and Administration (2.1)].
5.9 Status Epilepticus
Valid estimates of the incidence of treatment-emergent status epilepticus among patients treated with immediate-release lamotrigine are difficult to obtain because reporters participating in clinical trials did not all employ identical rules for identifying cases. At a minimum, 7 of 2,343 adult patients had episodes that could unequivocally be described as status epilepticus. In addition, a number of reports of variably defined episodes of seizure exacerbation (e.g., seizure clusters, seizure flurries) were made.
5.10 Sudden Unexplained Death in Epilepsy (SUDEP)
During the premarketing development of the immediate-release lamotrigine, 20 sudden and unexplained deaths were recorded among a cohort of 4,700 patients with epilepsy (5,747 patient-years of exposure).
Some of these could represent seizure-related deaths in which the seizure was not observed, e.g., at night. This represents an incidence of 0.0035 deaths per patient-year. Although this rate exceeds that expected in a healthy population matched for age and sex, it is within the range of estimates for the incidence of sudden unexplained death in epilepsy (SUDEP) in patients not receiving lamotrigine (ranging from 0.0005 for the general population of patients with epilepsy, to 0.004 for a recently studied clinical trial population similar to that in the clinical development program for immediate-release lamotrigine, to 0.005 for patients with refractory epilepsy). Consequently, whether these figures are reassuring or suggest concern depends on the comparability of the populations reported upon with the cohort receiving immediate-release lamotrigine and the accuracy of the estimates provided. Probably most reassuring is the similarity of estimated SUDEP rates in patients receiving immediate-release lamotrigine and those receiving other AEDs, chemically unrelated to each other, that underwent clinical testing in similar populations. Importantly, that drug is chemically unrelated to lamotrigine. This evidence suggests, although it certainly does not prove, that the high SUDEP rates reflect population rates, not a drug effect.
5.11 Addition of Lamotrigine Extended-Release to a Multidrug Regimen That Includes Valproate
Because valproate reduces the clearance of lamotrigine, the dosage of lamotrigine in the presence of valproate is less than half of that required in its absence. [see Dosage and Administration (2.1, 2.2), Drug Interactions (7)]
5.12 Binding in the Eye and Other Melanin-Containing Tissues
Because lamotrigine binds to melanin, it could accumulate in melanin-rich tissues over time. This raises the possibility that lamotrigine may cause toxicity in these tissues after extended use. Although ophthalmological testing was performed in one controlled clinical trial, the testing was inadequate to exclude subtle effects or injury occurring after long-term exposure. Moreover, the capacity of available tests to detect potentially adverse consequences, if any, of lamotrigine binding to melanin is unknown.
Accordingly, although there are no specific recommendations for periodic ophthalmological monitoring, prescribers should be aware of the possibility of long-term ophthalmologic effects.
5.13 Laboratory Tests
False-Positive Drug Test Results - Lamotrigine has been reported to interfere with the assay used in some rapid urine drug screens, which can result in false-positive readings, particularly for phencyclidine (PCP). A more specific analytical method should be used to confirm a positive result.
Plasma Concentrations of Lamotrigine: The value of monitoring plasma concentrations of lamotrigine in patients treated with lamotrigine extended-release has not been established. Because of the possible pharmacokinetic interactions between lamotrigine and other drugs including AEDs (see Table 6), monitoring of the plasma levels of lamotrigine and concomitant drugs may be indicated, particularly during dosage adjustments. In general, clinical judgment should be exercised regarding monitoring of plasma levels of lamotrigine and other drugs and whether or not dosage adjustments are necessary.
Effect on Leukocytes: Treatment with lamotrigine extended-release caused an increased incidence of subnormal (below the reference range) values in some hematology analytes (e.g., total white blood cells, monocytes). The treatment effect (lamotrigine extended-release % - Placebo %) incidence of subnormal counts was 3% for total white blood cells and 4% for monocytes.
-
6 ADVERSE REACTIONS
The following adverse reactions are described in more detail in the Warnings and Precautions section of the label:
- Serious skin rashes [see Warnings and Precautions (5.1)]
- Multiorgan hypersensitivity reactions and organ failure [see Warnings and Precautions (5.2)]
- Blood dyscrasias [see Warnings and Precautions (5.3)]
- Suicidal behavior and ideation [see Warnings and Precautions (5.4)]
- Aseptic meningitis (see Warnings and Precautions (5.5)]
- Withdrawal seizures [see Warnings and Precautions (5.8)]
- Status epilepticus [see Warnings and Precautions (5.9)]
- Sudden unexplained death in epilepsy [see Warnings and Precautions (5.10]
6.1 Clinical Trial Experience with Lamotrigine Extended-Release for Treatment of Primary Generalized Tonic-Clonic and Partial-Onset Seizures
Most Common Adverse Reactions in Clinical Trials: Adjunctive Therapy in Patients With Epilepsy: Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared with rates in the clinical trials of another drug and may not reflect the rates observed in practice.
In these 2 trials, adverse reactions led to withdrawal of 4 (2%) patients in the group receiving placebo and 10 (5%) patients in the group receiving lamotrigine extended-release. Dizziness was the most common reason for withdrawal in the group receiving lamotrigine extended-release (5 patients [3%]). The next most common adverse reactions leading to withdrawal in 2 patients each (1%) were rash, headache, nausea, and nystagmus.
Table 4 displays the incidence of adverse reactions in these two 19-week, double-blind, placebo-controlled trials of patients with PGTC and partial-onset seizures.
Table 4. Adverse Reactions in Pooled, Placebo-Controlled, Adjunctive Trials in Patients with Epilepsya Body System/Adverse Reaction
Percent of Patients Receiving Adjunctive
Lamotrigine Extended-Release
(n = 190) %
Percent of Patients Receiving Adjunctive
Placebo
(n = 195) %
Ear and Labyrinth Disorders
Vertigo
3
<1
Eye Disorders
Diplopia
Vision blurred
5
3
<1
2
Gastrointestinal Disorders
Nausea
Vomiting
Diarrhea
Constipation
Dry mouth
7
6
5
2
2
4
3
3
<1
1
General Disorders and Administration Site Conditions
Asthenia and fatigue
6
4
Infections and Infestations
Sinusitis
2
1
Metabolic and Nutritional Disorders
Anorexia
3
2
Musculoskeletal and Connective Tissue Disorder
Myalgia
2
0
Nervous System
Dizziness
Tremor and intention tremor
Somnolence
Cerebellar coordination and balance disorder
Nystagmus
14
6
5
3
2
6
1
3
0
<1
Psychiatric Disorders
Depression
Anxiety
3
3
<1
0
Respiratory, Thoracic, and Mediastinal Disorders
Pharyngolaryngeal pain
3
2
Vascular Disorder
Hot flush
2
0
a Adverse reactions that occurred in at least 2% of patients treated with lamotrigine extended-release and at a greater incidence than placebo.
Note: In these trials the incidence of nonserious rash was 2% for lamotrigine extended-release and 3% for placebo. In clinical trials evaluating the immediate-release lamotrigine, the rate of serious rash was 0.3% in adults on adjunctive therapy for epilepsy [see Boxed Warning].
Adverse reactions were also analyzed to assess the incidence of the onset of an event in the titration period, and in the maintenance period, and if adverse reactions occurring in the titration phase persisted in the maintenance phase.
The incidence for many adverse reactions caused by treatment with lamotrigine extended-release was increased relative to placebo (i.e., treatment difference between lamotrigine extended-release and placebo ≥2%) in either the titration or maintenance phases of the trial. During the titration phase, an increased incidence (shown in descending order of % treatment difference) was observed for diarrhea, nausea, vomiting, somnolence, vertigo, myalgia, hot flush, and anxiety. During the maintenance phase, an increased incidence was observed for dizziness, tremor, and diplopia. Some adverse reactions developing in the titration phase were notable for persisting (>7 days) into the maintenance phase. These persistent adverse reactions included somnolence and dizziness.
There were inadequate data to evaluate the effect of dose and/or concentration on the incidence of adverse reactions because although patients were randomized to different target doses based upon concomitant AEDs, the plasma exposure was expected to be generally similar among all patients receiving different doses. However, in a randomized, parallel trial comparing placebo with 300 and 500 mg/day of immediate-release lamotrigine, the incidence of the most common adverse reactions ( >5%) such as ataxia, blurred vision, diplopia, and dizziness were dose-related. Less common adverse reactions (<5%) were not assessed for dose-response relationships.
Monotherapy in Patients With Epilepsy: Adverse reactions observed in this trial were generally similar to those observed and attributed to drug in adjunctive and monotherapy immediate-release lamotrigine and adjunctive lamotrigine extended-release placebo controlled trials. Only 2 adverse events, nasopharyngitis and upper respiratory tract infection, were observed at a rate of ≥3% and not reported at a similar rate in previous trials. Because this trial did not include a placebo control group, causality could not be established [see Clinical Studies (14.3)].
6.2 Other Adverse Reactions Observed During the Clinical Development of Immediate-Release Lamotrigine
All reported reactions are included except those already listed in the previous tables or elsewhere in the labeling, those too general to be informative, and those not reasonably associated with the use of the drug.
Adjunctive Therapy in Adults With Epilepsy: In addition to the adverse reactions reported above from the development of lamotrigine extended-release, the following adverse reactions with an uncertain relationship to lamotrigine were reported during the clinical development of immediate-release lamotrigine for treatment of epilepsy in adults. These reactions occurred in ≥2% of patients receiving immediate-release lamotrigine and more frequently than in the placebo group.
Body as a Whole: Headache, flu syndrome, fever, neck pain.
Musculoskeletal: Arthralgia.
Nervous: Insomnia, convulsion, irritability, speech disorder, concentration disturbance.
Respiratory: Pharyngitis, cough increased.
Skin and Appendages: Rash, pruritus.
Urogenital: (female patients only) Vaginitis, amenorrhea, dysmenorrhea.
Monotherapy in Adults With Epilepsy: In addition to the adverse reactions reported above from the development of lamotrigine extended-release, the following adverse reactions with an uncertain relationship to lamotrigine were reported during the clinical development of immediate-release lamotrigine for treatment of epilepsy in adults. These reactions occurred in >2% of patients receiving immediate-release lamotrigine and more frequently than in the placebo group.
- Body as a Whole: Chest pain.
- Digestive: Rectal hemorrhage, peptic ulcer.
- Metabolic and Nutritional: Weight decrease, peripheral edema.
- Nervous: Hypesthesia, libido increase, decreased reflexes.
- Respiratory: Epistaxis, dyspnea.
- Skin and Appendages: Contact dermatitis, dry skin, sweating.
- Special Senses: Vision abnormality.
Urogenital: (female patients only) Dysmenorrhea.
Other Clinical Trial Experience: Immediate-release lamotrigine has been administered to 6,694 individuals for whom complete adverse reaction data was captured during all clinical trials, only some of which were placebo controlled.
Adverse reactions are further classified within body system categories and enumerated in order of decreasing frequency using the following definitions: frequent adverse reactions are defined as those occurring in at least 1/100 patients; infrequent adverse reactions are those occurring in 1/100 to 1/1,000 patients; rare adverse reactions are those occurring in fewer than 1/1,000 patients.
Cardiovascular System: Infrequent: Hypertension, palpitations, postural hypotension, syncope, tachycardia, and vasodilation.
Dermatological: Infrequent: Acne, alopecia, hirsutism, maculopapular rash, urticaria. Rare: Leukoderma, multiforme erythema, petechial rash, pustular rash.
Digestive System: Infrequent: Dysphagia, liver function tests abnormal, mouth ulceration. Rare: Gastrointestinal hemorrhage, hemorrhagic colitis, hepatitis, melena and stomach ulcer.
Endocrine System: Rare: Goiter and hypothyroidism.
Hematologic and Lymphatic System: Infrequent: Ecchymosis and leukopenia. Rare: Anemia, eosinophilia, fibrin decrease, fibrinogen decrease, iron deficiency anemia, leukocytosis, lymphocytosis, macrocytic anemia, petechia, and thrombocytopenia.
Metabolic and Nutritional Disorders: Infrequent: Aspartate transaminase increased. Rare: Alcohol intolerance, alkaline phosphatase increase, alanine transaminase increase, bilirubinemia, gamma glutamyl transpeptidase increase, hyperglycemia.
Musculoskeletal System: Rare: Muscle atrophy, pathological fracture, and tendinous contracture.
Nervous System: Frequent: Confusion. Infrequent: Akathisia, apathy, aphasia, depersonalization, dysarthria, dyskinesia, euphoria, hallucinations, hostility, hyperkinesia, hypertonia, libido decreased, memory decrease, mind racing, movement disorder, myoclonus, panic attack, paranoid reaction, personality disorder, psychosis, stupor. Rare: Choreoathetosis, delirium, delusions, dysphoria, dystonia, extrapyramidal syndrome, hemiplegia, hyperalgesia, hyperesthesia, hypokinesia, hypotonia, manic depression reaction, neuralgia, paralysis, and peripheral neuritis.
Respiratory System: Rare: Hiccup and hyperventilation.
Special Senses: Frequent: Amblyopia. Infrequent: Abnormality of accommodation, conjunctivitis, dry eyes, ear pain, photophobia, taste perversion, and tinnitus. Rare: Deafness, lacrimation disorder, oscillopsia, parosmia, ptosis, strabismus, taste loss, uveitis, and visual field defect.
Urogenital System: Infrequent: Abnormal ejaculation, hematuria, impotence, menorrhagia, polyuria, urinary incontinence. Rare: Acute kidney failure, breast neoplasm, creatinine increase, female lactation, kidney failure, kidney pain, nocturia, urinary retention, urinary urgency.
6.3 Postmarketing Experience with the Immediate-Release Lamotrigine
The following adverse events (not listed above in clinical trials or other sections of the prescribing information) have been identified during postapproval use of the immediate-release lamotrigine. Because these events are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Blood and Lymphatic: Agranulocytosis, hemolytic anemia, lymphadenopathy not associated with hypersensitivity disorder.
Gastrointestinal: Esophagitis.
Hepatobiliary Tract and Pancreas: Pancreatitis.
Immunologic: Lupus-like reaction, vasculitis.
Lower Respiratory: Apnea.
Musculoskeletal: Rhabdomyolysis has been observed in patients experiencing hypersensitivity reactions.
Nervous System: Aggression, exacerbation of Parkinsonian symptoms in patients with pre-existing Parkinson’s disease, tics.
Non-site Specific: Progressive immunosuppression.
-
7 DRUG INTERACTIONS
Significant drug interactions with Lamotrigine are summarized in this section. Additional details of these drug interaction studies, which were conducted using the immediate-release lamotrigine, are provided in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)].
Table 5. Established and Other Potentially Significant Drug Interactions ↓= Decreased (induces lamotrigine glucuronidation). ↑= Increased (inhibits lamotrigine glucuronidation). ? = Conflicting data. Concomitant Drug
Effect on Concentration of Lamotrigine or Concomitant Drug
Clinical Comment
Estrogen-containing oral contraceptive preparations containing 30 mcg ethinylestradiol and 150 mcg levonorgestrel
↓ lamotrigine
↓levonorgestrel
Decreased lamotrigine concentrations approximately 50%.
Decrease in levonorgestrel component by 19%.
Carbamazepine and Carbamazepine epoxide
↓ lamotrigine
? carbamazepine epoxide
Addition of carbamazepine decreases lamotrigine concentration approximately 40%. May increase carbamazepine epoxide levels.
Lopinavir/ritonavir
↓ lamotrigine
Decreased lamotrigine concentration approximately 50%.
Atazanavir/ritonavir
↓ lamotrigine
Decreased lamotrigine AUC approximately 32%.
Phenobarbital/primidone
↓ lamotrigine
Decreased lamotrigine concentration approximately 40%.
Phenytoin
↓ lamotrigine
Decreased lamotrigine concentration approximately 40%.
Rifampin
↓ lamotrigine
Decreased lamotrigine AUC approximately 40%.
Valproate
↑ lamotrigine
? valproate
Increased lamotrigine concentrations slightly more than 2-fold.
There are conflicting study results regarding effect of lamotrigine on valproate concentrations: 1) a mean 25% decrease in valproate concentrations in healthy volunteers, 2) no change in valproate concentrations in controlled clinical trials in patients with epilepsy.
Effect of Lamotrigine Extended-Release on Organic Cationic Transporter 2 Substrates
Lamotrigine is an inhibitor of renal tubular secretion via organic cationic transporter 2 (OCT2) proteins [see Clinical Pharmacology (12.3)]. This may result in increased plasma levels of certain drugs that are substantially excreted via this route. Coadministration of lamotrigine extended-release with OCT2 substrates with a narrow therapeutic index (e.g., dofetilide) is not recommended.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
As with other AEDs, physiological changes during pregnancy may affect lamotrigine concentrations and/or therapeutic effect. There have been reports of decreased lamotrigine concentrations during pregnancy and restoration of pre-partum concentrations after delivery. Dosage adjustments may be necessary to maintain clinical response.
Pregnancy Category C
There are no adequate and well-controlled studies in pregnant women. In animal studies, lamotrigine was developmentally toxic at doses lower than those administered clinically.
Lamotrigine extended-release should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
When lamotrigine was administered to pregnant mice, rats, or rabbits during the period of organogenesis (oral doses of up to 125, 25, and 30 mg/kg, respectively), reduced fetal body weight and increased incidences of fetal skeletal variations were seen in mice and rats at doses that were also maternally toxic. The no-effect doses for embryo-fetal developmental toxicity in mice, rats, and rabbits (75, 6.25, and 30 mg/kg, respectively) are similar to (mice and rabbits) or less than (rats) the human dose of 400 mg/day on a body surface area (mg/m2) basis.
In a study in which pregnant rats were administered lamotrigine (oral doses of 5 or 25 mg/kg) during the period of organogenesis and offspring were evaluated postnatally, behavioral abnormalities were observed in exposed offspring at both doses. The lowest effect dose for developmental neurotoxicity in rats is less than the human dose of 400 mg/day on a mg/m2 basis. Maternal toxicity was observed at the higher dose tested.
When pregnant rats were administered lamotrigine (oral doses of 5, 10, or 20 mg/kg) during the latter part of gestation, increased offspring mortality (including stillbirths) was seen at all doses. The lowest effect dose for peri/postnatal developmental toxicity in rats is less than the human dose of 400 mg/day on a mg/m2 basis. Maternal toxicity was observed at the two highest doses tested.
Lamotrigine decreases fetal folate concentrations in rat, an effect known to be associated with adverse pregnancy outcomes in animals and humans.
Pregnancy Registry: To provide information regarding the effects of in utero exposure to lamotrigine extended-release, physicians are advised to recommend that pregnant patients taking lamotrigine extended-release enroll in the North American Antiepileptic Drug (NAAED) Pregnancy Registry. This can be done by calling the toll-free number 1-888-233-2334, and must be done by patients themselves. Information on the registry can also be found at the website http://www.aedpregnancyregistry.org/.
8.2 Labor and Delivery
The effect of lamotrigine extended-release on labor and delivery in humans is unknown.
8.3 Nursing Mothers
Lamotrigine is present in milk from lactating women taking lamotrigine extended-release. Data from multiple small studies indicate that lamotrigine plasma levels in human milk-fed infants have been reported to be as high as 50% of the maternal serum levels. Neonates and young infants are at risk for high serum levels because maternal serum and milk levels can rise to high levels postpartum if lamotrigine dosage has been increased during pregnancy but not later reduced to the pre-pregnancy dosage. Lamotrigine exposure is further increased due to the immaturity of the infant glucuronidation capacity needed for drug clearance. Events including apnea, drowsiness, and poor sucking have been reported in infants who have been human milk-fed by mothers using lamotrigine; whether or not these events were caused by lamotrigine is unknown. Human milk-fed infants should be closely monitored for adverse events resulting from lamotrigine. Measurement of infant serum levels should be performed to rule out toxicity if concerns arise. Human milk-feeding should be discontinued in infants with lamotrigine toxicity. Caution should be exercised when lamotrigine extended-release is administered to a nursing woman.
8.4 Pediatric Use
Lamotrigine extended-release is indicated as adjunctive therapy for PGTC and partial-onset seizures with or without secondary generalization in patients aged 13 years and older. Safety and effectiveness of lamotrigine extended-release for any use in patients younger than 13 years have not been established.
Immediate-release lamotrigine is indicated for adjunctive therapy in patients aged 2 years and older for partial-onset seizures, the generalized seizures of Lennox-Gastaut syndrome, and PGTC seizures.
Safety and efficacy of the immediate-release lamotrigine, used as adjunctive treatment for partial-onset seizures, were not demonstrated in a small, randomized, double-blind, placebo-controlled, withdrawal trial in very young pediatric patients (aged 1 to 24 months). Immediate-release lamotrigine was associated with an increased risk for infectious adverse reactions (lamotrigine 37%, placebo 5%), and respiratory adverse reactions (lamotrigine 26%, placebo 5%). Infectious adverse reactions included: bronchiolitis, bronchitis, ear infection, eye infection, otitis externa, pharyngitis, urinary tract infection, and viral infection. Respiratory adverse reactions included nasal congestion, cough, and apnea.
In a juvenile animal study in which lamotrigine (oral doses of 5, 15, or 30 mg/kg) was administered to young rats (postnatal days 7 to 62), decreased viability and growth were seen at the highest dose tested and long-term behavioral abnormalities (decreased locomotor activity, increased reactivity, and learning deficits in animals tested as adults) were observed at the two highest doses. The no-effect dose for adverse effects on neurobehavioral development is less than the human dose of 400 mg/day on a mg/m2 basis.
8.5 Geriatric Use
Clinical trials of lamotrigine extended-release for epilepsy did not include sufficient numbers of patients aged 65 years and older to determine whether they respond differently from younger patients or exhibit a different safety profile than that of younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
8.6 Hepatic Impairment
Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study with the immediate-release lamotrigine in 24 subjects with mild, moderate, and severe liver impairment [see Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response [see Dosage and Administration (2.1)].
8.7 Renal Impairment
Lamotrigine is metabolized mainly by glucuronic acid conjugation, with the majority of the metabolites being recovered in the urine. In a small study comparing a single dose of immediate-release lamotrigine in subjects with varying degrees of renal impairment with healthy volunteers, the plasma half-life of lamotrigine was approximately twice as long in the subjects with chronic renal impairment [see Clinical Pharmacology (12.3)].
Initial doses of lamotrigine extended-release should be based on patients' AED regimens; reduced maintenance doses may be effective for patients with significant renal impairment. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine. Because there is inadequate experience in this population, lamotrigine extended-release should be used with caution in these patients [see Dosage and Administration (2.1)].
-
10 OVERDOSAGE
10.1 Human Overdose Experience
Overdoses involving quantities up to 15 g have been reported for immediate-release lamotrigine, some of which have been fatal. Overdose has resulted in ataxia, nystagmus, seizures (including tonic-clonic seizures), decreased level of consciousness, coma, and intraventricular conduction delay.
10.2 Management of Overdose
There are no specific antidotes for lamotrigine. Following a suspected overdose, hospitalization of the patient is advised. General supportive care is indicated, including frequent monitoring of vital signs and close observation of the patient. If indicated, emesis should be induced; usual precautions should be taken to protect the airway. It is uncertain whether hemodialysis is an effective means of removing lamotrigine from the blood. In 6 renal failure patients, about 20% of the amount of lamotrigine in the body was removed by hemodialysis during a 4-hour session. A Poison Control Center should be contacted for information on the management of overdosage of lamotrigine extended-release.
-
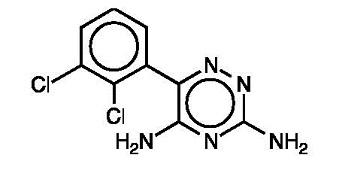
11 DESCRIPTION
Lamotrigine extended-release, an AED of the phenyltriazine class, is chemically unrelated to existing AEDs. Its chemical name is 3,5-diamino-6-(2,3-dichlorophenyl)-as-triazine, its molecular formula is C9H7N5Cl2, and its molecular weight is 256.09. Lamotrigine is a white to pale cream-colored powder and has a pKa of 5.7. Lamotrigine is very slightly soluble in water (0.17 mg/mL at 25°C) and slightly soluble in 0.1 M HCl (4.1 mg/mL at 25°C). The structural formula is:
Lamotrigine Extended-Release Tablets are supplied for oral administration as 25 mg (round beige biconvex film-coated), 50 mg (round white biconvex film-coated), 100 mg (round brown biconvex film-coated), 200 mg (round yellow biconvex film-coated), 250 mg (round white biconvex film coated) and 300 mg (round grey biconvex film-coated) tablets. Each tablet contains the labeled amount of lamotrigine and the following inactive ingredients: hypromellose, lactose monohydrate, magnesium stearate, colloidal anhydrous silica (25 mg, 50 mg, 200 mg, 250 mg and 300 mg tablets only), methacrylic acid copolymer, talc, titanium dioxide, triethyl citrate, sodium bicarbonate, sodium laurel sulfate, iron oxide yellow (25 mg and 100 mg tablets only), iron oxide red (25 mg and 100 mg tablets only), D&C Yellow # 10 (200 mg tablet only), FD&C Yellow # 6 (200 mg tablet only) and black iron oxide (300 mg tablet only).
Lamotrigine extended-release tablet contains a modified-release eroding formulation as the core. The tablets are coated with an enteric coat and have pore forming ingredient in the coat to enable a controlled release of the drug in the acidic environment of the stomach. The combinations of the modified-release core and the enteric coat are designed to control the dissolution rate of lamotrigine over a period of approximately 12 to 15 hours, leading to a gradual increase in blood lamotrigine levels.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The precise mechanism(s) by which lamotrigine exerts its anticonvulsant action are unknown. In animal models designed to detect anticonvulsant activity, lamotrigine was effective in preventing seizure spread in the maximum electroshock (MES) and pentylenetetrazol (scMet) tests, and prevented seizures in the visually and electrically evoked after-discharge (EEAD) tests for antiepileptic activity. Lamotrigine also displayed inhibitory properties in a kindling model in rats both during kindling development and in the fully kindled state. The relevance of these models to human epilepsy, however, is not known.
One proposed mechanism of action of lamotrigine, the relevance of which remains to be established in humans, involves an effect on sodium channels. In vitro pharmacological studies suggest that lamotrigine inhibits voltage-sensitive sodium channels, thereby stabilizing neuronal membranes and consequently modulating presynaptic transmitter release of excitatory amino acids (e.g., glutamate and aspartate).
Effect of Lamotrigine on N-Methyl d-Aspartate-Receptor Mediated Activity: Lamotrigine did not inhibit N-methyl d-aspartate (NMDA)-induced depolarizations in rat cortical slices or NMDA-induced cyclic GMP formation in immature rat cerebellum, nor did lamotrigine displace compounds that are either competitive or noncompetitive ligands at this glutamate receptor complex (CNQX, CGS, TCHP). The IC50 for lamotrigine effects on NMDA-induced currents (in the presence of 3 µM of glycine) in cultured hippocampal neurons exceeded 100 µM.
12.2 Pharmacodynamics
Folate Metabolism: In vitro, lamotrigine inhibited dihydrofolate reductase, the enzyme that catalyzes the reduction of dihydrofolate to tetrahydrofolate. Inhibition of this enzyme may interfere with the biosynthesis of nucleic acids and proteins. When oral daily doses of lamotrigine were given to pregnant rats during organogenesis, fetal, placental, and maternal folate concentrations were reduced. Significantly reduced concentrations of folate are associated with teratogenesis [see Use in Specific Populations (8.1)]. Folate concentrations were also reduced in male rats given repeated oral doses of lamotrigine. Reduced concentrations were partially returned to normal when supplemented with folinic acid.
Cardiovascular: In dogs, lamotrigine is extensively metabolized to a 2-N-methyl metabolite. This metabolite causes dose-dependent prolongation of the PR interval, widening of the QRS complex, and, at higher doses, complete AV conduction block. Similar cardiovascular effects are not anticipated in humans because only trace amounts of the 2-N-methyl metabolite (<0.6% of lamotrigine dose) have been found in human urine [see Clinical Pharmacology (12.3)]. However, it is conceivable that plasma concentrations of this metabolite could be increased in patients with a reduced capacity to glucuronidate lamotrigine (e.g., in patients with liver disease, patients taking concomitant medications that inhibit glucuronidation).
12.3 Pharmacokinetics
In comparison to immediate-release lamotrigine, the plasma lamotrigine levels following administration of lamotrigine extended-release are not associated with any significant changes in trough plasma concentrations, and are characterized by lower peaks, longer time to peaks, and lower peak-to-trough fluctuation, as described in detail below.
Absorption: Lamotrigine is absorbed after oral administration with negligible first-pass metabolism. The bioavailability of lamotrigine is not affected by food.
In an open-label, crossover study of 44 subjects with epilepsy receiving concomitant AEDs, the steady-state pharmacokinetics of lamotrigine were compared following administration of equivalent total doses of lamotrigine extended-release given once daily with those of lamotrigine immediate-release given twice daily. In this study, the median time to peak concentration (Tmax) following administration of lamotrigine extended-release was 4 to 6 hours in subjects taking carbamazepine, phenytoin, phenobarbital, or primidone; 9 to 11 hours in subjects taking valproate; and 6 to 10 hours in subjects taking AEDs other than carbamazepine, phenytoin, phenobarbital, primidone, or valproate. In comparison, the median Tmax following administration of immediate-release lamotrigine was between 1 and 1.5 hours.
The steady-state trough concentrations for extended-release lamotrigine were similar to or higher than those of immediate-release lamotrigine depending on concomitant AED (Table 6). A mean reduction in the lamotrigine C max by 11% to 29% was observed for lamotrigine extended-release compared with immediate-release lamotrigine resulting in a decrease in the peak-to-trough fluctuation in serum lamotrigine concentrations. However, in some subjects receiving enzyme-inducing AEDs, a reduction in Cmax of 44% to 77% was observed. The degree of fluctuation was reduced by 17% in subjects taking enzyme-inducing AEDs, 34% in subjects taking valproate, and 37% in subjects taking AEDs other than carbamazepine, phenytoin, phenobarbital, primidone, or valproate. Lamotrigine extended-release and immediate-release lamotrigine regimens were similar with respect to area under the curve (AUC, a measure of the extent of bioavailability) for subjects receiving AEDs other than those known to induce the metabolism of lamotrigine. The relative bioavailability of extended-release lamotrigine was approximately 21% lower than immediate-release lamotrigine in subjects receiving enzyme-inducing AEDs. However, a reduction in exposure of up to 70% was observed in some subjects in this group when they switched to lamotrigine extended-release tablets. Therefore, doses may need to be adjusted in some patients based on therapeutic response.
Table 6. Steady-State Bioavailability of Lamotrigine Extended-Release Relative to Immediate-Release Lamotrigine at Equivalent Daily Doses (Ratio of Extended-Release to Immediate-Release 90% CI) a Enzyme-inducing antiepileptic drugs include carbamazepine, phenytoin, phenobarbital, and primidone. Concomitant Antiepileptic Drug
AUC(0-24ss)
Cmax
Cmin
Enzyme-inducing antiepileptic drugsa
0.79 (0.69, 0.90)
0.71 (0.61, 0.82)
0.99 (0.89, 1.09)
Valproate
0.94 (0.81, 1.08)
0.88 (0.75, 1.03)
0.99 (0.88, 1.10)
Antiepileptic drugs other than enzyme-inducing antiepileptic drugsa or valproate
1.00 (0.88, 1.14)
0.89 (0.78, 1.03)
1.14 (1.03, 1.25)
Dose Proportionality: In healthy volunteers not receiving any other medications and given lamotrigine extended-release once daily, the systemic exposure to lamotrigine increased in direct proportion to the dose administered over the range of 50 to 200 mg. At doses between 25 and 50 mg, the increase was less than dose proportional, with a 2-fold increase in dose resulting in an approximately 1.6-fold increase in systemic exposure.
Distribution: Estimates of the mean apparent volume of distribution (Vd/F) of lamotrigine following oral administration ranged from 0.9 to 1.3 L/kg. Vd/F is independent of dose and is similar following single and multiple doses in both patients with epilepsy and in healthy volunteers.
Protein Binding: Data from in vitro studies indicate that lamotrigine is approximately 55% bound to human plasma proteins at plasma lamotrigine concentrations from 1 to 10 mcg/mL (10 mcg/mL is 4 to 6 times the trough plasma concentration observed in the controlled efficacy trials). Because lamotrigine is not highly bound to plasma proteins, clinically significant interactions with other drugs through competition for protein binding sites are unlikely. The binding of lamotrigine to plasma proteins did not change in the presence of therapeutic concentrations of phenytoin, phenobarbital, or valproate. Lamotrigine did not displace other AEDs (carbamazepine, phenytoin, phenobarbital) from protein binding sites.
Metabolism: Lamotrigine is metabolized predominantly by glucuronic acid conjugation; the major metabolite is an inactive 2-N-glucuronide conjugate. After oral administration of 240 mg of 14C-lamotrigine (15 μCi) to 6 healthy volunteers, 94% was recovered in the urine and 2% was recovered in the feces. The radioactivity in the urine consisted of unchanged lamotrigine (10%), the 2-N-glucuronide (76%), a 5-N-glucuronide (10%), a 2-N-methyl metabolite (0.14%), and other unidentified minor metabolites (4%).
Enzyme Induction: The effects of lamotrigine on the induction of specific families of mixed-function oxidase isozymes have not been systematically evaluated.
Following multiple administrations (150 mg twice daily) to normal volunteers taking no other medications, lamotrigine induced its own metabolism, resulting in a 25% decrease in t ½ and a 37% increase in CL/F at steady state compared with values obtained in the same volunteers following a single dose. Evidence gathered from other sources suggests that self-induction by lamotrigine may not occur when lamotrigine is given as adjunctive therapy in patients receiving enzyme-inducing drugs such as carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7)].
Elimination: The elimination half-life and apparent clearance of lamotrigine following oral administration of immediate-release lamotrigine to adult subjects with epilepsy and healthy volunteers is summarized in Table 7. Half-life and apparent oral clearance vary depending on concomitant AEDs.
Since the half-life of lamotrigine following administration of single doses of immediate-release lamotrigine is comparable to that observed following administration of lamotrigine extended-release, similar changes in the half-life of lamotrigine would be expected for lamotrigine extended-release.
Table 7. Mean Pharmacokinetic Parametersa of Immediate-Release Lamotrigine in Healthy Volunteers and Adult Subjects With Epilepsy a The majority of parameter means determined in each study had coefficients of variation between 20% and 40% for half-life and CL/F and between 30% and 70% for Tmax. The overall mean values were calculated from individual study means that were weighted based on the number of volunteers/subjects in each study. The numbers in parentheses below each parameter mean represent the range of individual volunteer/subjects values across studies. b Carbamazepine, phenytoin, phenobarbital, and primidone have been shown to increase the apparent clearance of lamotrigine. Estrogen-containing oral contraceptives and other drugs, such as rifampin and protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation have also been shown to increase the apparent clearance of lamotrigine [see Drug Interactions (7)]. Adult Study Population
Number of Subjects
t½: Elimination Half-life (h)
CL/F: Apparent Plasma Clearance (mL/min/kg)
Healthy volunteers taking no other medications:
Single-dose lamotrigine
Multiple-dose lamotrigine
179
36
32.8
(14.0-103.0)
25.4
(11.6-61.6)
0.44
(0.12-1.10)
0.58
(0.24-1.15)
Healthy volunteers taking valproate:
Single-dose lamotrigine
Multiple-dose lamotrigine
6
18
48.3
(31.5-88.6)
70.3
(41.9-113.5)
0.30
(0.14-0.42)
0.18
(0.12-0.33)
Subjects with epilepsy taking valproate only:
Single-dose lamotrigine
4
58.8
(30.5-88.8)
0.28
(0.16-0.40)
Subjects with epilepsy taking carbamazepine, phenytoin, phenobarbital, or primidoneb plus valproate:
Single-dose lamotrigine
25
27.2
(11.2-51.6)
0.53
(0.27-1.04)
Subjects with epilepsy taking carbamazepine, phenytoin, phenobarbital, or primidone:b
Single-dose lamotrigine
Multiple-dose lamotrigine
24
17
14.4
(6.4-30.4)
12.6
(7.5-23.1)
1.10
(0.51-2.22)
1.21
(0.66-1.82)
Drug Interactions: The apparent clearance of lamotrigine is affected by the coadministration of certain medications [see Warnings and Precautions (5.7, 5.11), Drug Interactions (7)].
The net effects of drug interactions with lamotrigine, based on drug interaction studies using immediate-release lamotrigine, are summarized in Tables 5 and 8, followed by details of the drug interaction studies below.
Table 8. Summary of Drug Interactions With Lamotrigine Drug
Drug Plasma Concentration With Adjunctive Lamotriginea
Lamotrigine Plasma Concentration With Adjunctive Drugsb
Oral contraceptives (e.g., ethinylestradiol/levonorgestrelc)
↔d
↓
Aripiprazole
Not assessed
↔e
Atazanavir/ritonavir
↔f
↓
Bupropion
Not assessed
↔
Carbamazepine
↔
↓
Carbamazepine epoxideg
?
Felbamate
Not assessed
↔
Gabapentin
Not assessed
↔
Levetiracetam
↔
↔
Lithium
↔
Not assessed
Lopinavir/ritonavir
↔e
↓
Olanzapine
↔
↔e
Oxcarbazepine
↔
↔
10-monohydroxy oxcarbazepine metaboliteh
↔
Phenobarbital/primidone
↔
↓
Phenytoin
↔
↓
Pregabalin
↔
↔
Rifampin
Not assessed
↓
Risperidone
↔
Not assessed
9-hydroxyrisperidonei
↔
Topiramate
↔j
↔
Valproate
↓
↑
Valproate + phenytoin and/or carbamazepine
Not assessed
↔
Zonisamide
Not assessed
↔
- a From adjunctive clinical trials and volunteer trials.
- b Net effects were estimated by comparing the mean clearance values obtained in adjunctive clinical trials and volunteer trials.
- c The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated in clinical trials, although the effect may be similar to that seen with the ethinylestradiol/levonorgestrel combinations.
- d Modest decrease in levonorgestrel.
- e Slight decrease, not expected to be clinically meaningful.
- f Compared to historical controls.
- g Not administered, but an active metabolite of carbamazepine.
- h Not administered, but an active metabolite of oxcarbazepine.
- i Not administered, but an active metabolite of risperidone.
- j Slight increase, not expected to be clinically meaningful.
- ↔= No significant effect.
- ? = Conflicting data.
Estrogen-Containing Oral Contraceptives: In 16 female volunteers, an oral contraceptive preparation containing 30 mcg ethinylestradiol and 150 mcg levonorgestrel increased the apparent clearance of lamotrigine (300 mg/day) by approximately 2-fold with mean decreases in AUC of 52% and in Cmax of 39%. In this study, trough serum lamotrigine concentrations gradually increased and were approximately 2-fold higher on average at the end of the week of the inactive hormone preparation compared with trough lamotrigine concentrations at the end of the active hormone cycle.
Gradual transient increases in lamotrigine plasma levels (approximate 2-fold increase) occurred during the week of inactive hormone preparation (pill-free week) for women not also taking a drug that increased the clearance of lamotrigine (carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7)]. The increase in lamotrigine plasma levels will be greater if the dose of lamotrigine extended-release is increased in the few days before or during the pill-free week. Increases in lamotrigine plasma levels could result in dose-dependent adverse reactions.
In the same study, coadministration of lamotrigine (300 mg/day) in 16 female volunteers did not affect the pharmacokinetics of the ethinylestradiol component of the oral contraceptive preparation. There were mean decreases in the AUC and Cmax of the levonorgestrel component of 19% and 12%, respectively. Measurement of serum progesterone indicated that there was no hormonal evidence of ovulation in any of the 16 volunteers, although measurement of serum FSH, LH, and estradiol indicated that there was some loss of suppression of the hypothalamic-pituitary-ovarian axis.
The effects of doses of lamotrigine other than 300 mg/day have not been systematically evaluated in controlled clinical trials.
The clinical significance of the observed hormonal changes on ovulatory activity is unknown. However, the possibility of decreased contraceptive efficacy in some patients cannot be excluded. Therefore, patients should be instructed to promptly report changes in their menstrual pattern (e.g., break-through bleeding).
Dosage adjustments may be necessary for women receiving estrogen-containing oral contraceptive preparations [see Dosage and Administration (2.1)].
Other Hormonal Contraceptives or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine extended-release in the presence of progestogens alone will likely not be needed.
Aripiprazole: In 18 patients with bipolar disorder on a stable regimen of 100 to 400 mg/day of lamotrigine, the lamotrigine AUC and Cmax were reduced by approximately 10% in patients who received aripiprazole 10 to 30 mg/day for 7 days, followed by 30 mg/day for an additional 7 days. This reduction in lamotrigine exposure is not considered clinically meaningful.
Atazanavir/Ritonavir: In a study in healthy volunteers, daily doses of atazanavir/ritonavir (300 mg/100 mg) reduced the plasma AUC and Cmax of lamotrigine (single 100 mg dose) by an average of 32% and 6%, respectively, and shortened the elimination half-lives by 27%. In the presence of atazanavir/ritonavir (300 mg/100 mg), the metabolite to lamotrigine ratio was increased from 0.45 to 0.71 consistent with induction of glucuronidation. The pharmacokinetics of atazanavir/ritonavir were similar in the presence of concomitant lamotrigine to the historical data of the pharmacokinetics in the absence of lamotrigine.
Bupropion: The pharmacokinetics of a 100-mg single dose of lamotrigine in healthy volunteers (n = 12) were not changed by coadministration of bupropion sustained-release formulation (150 mg twice daily) starting 11 days before lamotrigine.
Carbamazepine: Lamotrigine has no appreciable effect on steady-state carbamazepine plasma concentration. Limited clinical data suggest there is a higher incidence of dizziness, diplopia, ataxia, and blurred vision in patients receiving carbamazepine with lamotrigine than in patients receiving other AEDs with lamotrigine [see Adverse Reactions (6.1)]. The mechanism of this interaction is unclear. The effect of lamotrigine on plasma concentrations of carbamazepine-epoxide is unclear. In a small subset of patients (n = 7) studied in a placebo-controlled trial, lamotrigine had no effect on carbamazepine-epoxide plasma concentrations, but in a small, uncontrolled study (n = 9), carbamazepine-epoxide levels increased. The addition of carbamazepine decreases lamotrigine steady-state concentrations by approximately 40%.
Esomeprazole: In a study of 30 subjects, coadministration of lamotrigine extended-release with esomeprazole resulted in no significant change in lamotrigine levels and a small decrease in Tmax. The levels of gastric pH were not altered compared with pre-lamotrigine dosing.
Felbamate: In a trial of 21 healthy volunteers, coadministration of felbamate (1,200 mg twice daily) with lamotrigine (100 mg twice daily for 10 days) appeared to have no clinically relevant effects on the pharmacokinetics of lamotrigine.
Folate Inhibitors: Lamotrigine is a weak inhibitor of dihydrofolate reductase. Prescribers should be aware of this action when prescribing other medications that inhibit folate metabolism.
Gabapentin: Based on a retrospective analysis of plasma levels in 34 subjects who received lamotrigine both with and without gabapentin, gabapentin does not appear to change the apparent clearance of lamotrigine.
Levetiracetam: Potential drug interactions between levetiracetam and lamotrigine were assessed by evaluating serum concentrations of both agents during placebo-controlled clinical trials. These data indicate that lamotrigine does not influence the pharmacokinetics of levetiracetam and that levetiracetam does not influence the pharmacokinetics of lamotrigine.
Lithium: The pharmacokinetics of lithium were not altered in healthy subjects (n = 20) by coadministration of lamotrigine (100 mg/day) for 6 days.
Lopinavir/Ritonavir: The addition of lopinavir (400 mg twice daily)/ritonavir (100 mg twice daily) decreased the AUC, Cmax, and elimination half-life of lamotrigine by approximately 50% to 55.4% in 18 healthy subjects. The pharmacokinetics of lopinavir/ritonavir were similar with concomitant lamotrigine, compared to that in historical controls.
Olanzapine: The AUC and Cmax of olanzapine were similar following the addition of olanzapine (15 mg once daily) to lamotrigine (200 mg once daily) in healthy male volunteers (n = 16) compared with the AUC and Cmax in healthy male volunteers receiving olanzapine alone (n = 16).
In the same trial, the AUC and Cmax of lamotrigine were reduced on average by 24% and 20%, respectively, following the addition of olanzapine to lamotrigine in healthy male volunteers compared with those receiving lamotrigine alone. This reduction in lamotrigine plasma concentrations is not expected to be clinically relevant.
Oxcarbazepine: The AUC and Cmax of oxcarbazepine and its active 10-monohydroxy oxcarbazepine metabolite were not significantly different following the addition of oxcarbazepine (600 mg twice daily) to lamotrigine (200 mg once daily) in healthy male volunteers (n = 13) compared with healthy male volunteers receiving oxcarbazepine alone (n = 13).
In the same trial, the AUC and Cmax of lamotrigine were similar following the addition of oxcarbazepine (600 mg twice daily) to lamotrigine in healthy male volunteers compared with those receiving lamotrigine alone. Limited clinical data suggest a higher incidence of headache, dizziness, nausea, and somnolence with coadministration of lamotrigine and oxcarbazepine compared with lamotrigine alone or oxcarbazepine alone.
Phenobarbital, Primidone: The addition of phenobarbital or primidone decreases lamotrigine steady-state concentrations by approximately 40%.
Phenytoin: Lamotrigine has no appreciable effect on steady-state phenytoin plasma concentrations in patients with epilepsy. The addition of phenytoin decreases lamotrigine steady-state concentrations by approximately 40%.
Pregabalin: Steady-state trough plasma concentrations of lamotrigine were not affected by concomitant pregabalin (200 mg 3 times daily) administration. There are no pharmacokinetic interactions between lamotrigine and pregabalin.
Rifampin: In 10 male volunteers, rifampin (600 mg/day for 5 days) significantly increased the apparent clearance of a single 25-mg dose of lamotrigine by approximately 2-fold (AUC decreased by approximately 40%).
Risperidone: In a 14 healthy volunteers study, multiple oral doses of lamotrigine 400 mg daily had no clinically significant effect on the single-dose pharmacokinetics of risperidone 2mg and its active metabolite 9-OH risperidone. Following the coadministration of risperidone 2 mg with lamotrigine, 12 of the 14 volunteers reported somnolence compared with 1 out of 20 when risperidone was given alone, and none when lamotrigine was administered alone.
Topiramate: Topiramate resulted in no change in plasma concentrations of lamotrigine. Administration of lamotrigine resulted in a 15% increase in topiramate concentrations.
Valproate: When lamotrigine was administered to healthy volunteers (n = 18) receiving valproate, the trough steady-state valproate plasma concentrations decreased by an average of 25% over a 3-week period, and then stabilized. However, adding lamotrigine to the existing therapy did not cause a change in valproate plasma concentrations in either adult or pediatric patients in controlled clinical trials.
The addition of valproate increased lamotrigine steady-state concentrations in normal volunteers by slightly more than 2-fold. In one trial, maximal inhibition of lamotrigine clearance was reached at valproate doses between 250 and 500 mg/day and did not increase as the valproate dose was further increased.
Zonisamide: In a study of 18 patients with epilepsy, coadministration of zonisamide (200 to 400 mg/day) with lamotrigine (150 to 500 mg/day for 35 days) had no significant effect on the pharmacokinetics of lamotrigine.
Known Inducers or Inhibitors of Glucuronidation: Drugs other than those listed above have not been systematically evaluated in combination with lamotrigine. Since lamotrigine is metabolized predominately by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine, and doses of lamotrigine extended-release may require adjustment based on clinical response.
Other: In vitro assessments of inhibitory effect of lamotrigine at OCT2 demonstrate that lamotrigine, but not the N(2)-glucuronide metabolite, is an inhibitor of OCT2 at potentially clinically relevant concentrations, with IC50 value of 53.8 uM [see Drug Interactions (7)].
Results of in vitro experiments suggest that clearance of lamotrigine is unlikely to be reduced by concomitant administration of amitriptyline, clonazepam, clozapine, fluoxetine, haloperidol, lorazepam, phenelzine, sertraline, or trazodone.
Results of in vitro experiments suggest that lamotrigine does not reduce the clearance of drugs eliminated predominantly by CYP2D6.
Specific Populations: Renal Impairment: Twelve volunteers with chronic renal failure (mean creatinine clearance: 13 mL/min; range: 6 to 23) and another 6 individuals undergoing hemodialysis were each given a single 100 mg dose of immediate-release lamotrigine. The mean plasma half-lives determined in the study were 42.9 hours (chronic renal failure), 13.0 hours (during hemodialysis), and 57.4 hours (between hemodialysis) compared with 26.2 hours in healthy volunteers. On average, approximately 20% (range: 5.6 to 35.1) of the amount of lamotrigine present in the body was eliminated by hemodialysis during a 4-hour session [see Dosage and Administration (2.1)].
Hepatic Disease: The pharmacokinetics of lamotrigine following a single 100 mg dose of immediate-release lamotrigine were evaluated in 24 subjects with mild, moderate, and severe hepatic impairment (Child-Pugh Classification system) and compared with 12 subjects without hepatic impairment. The subjects with severe hepatic impairment were without ascites (n = 2) or with ascites (n = 5). The mean apparent clearances of lamotrigine in subjects with mild (n = 12), moderate (n = 5), severe without ascites (n = 2), and severe with ascites (n = 5) liver impairment were 0.30 ± 0.09, 0.24 ± 0.1, 0.21 ± 0.04, and 0.15 ± 0.09 mL/min/kg, respectively, as compared with 0.37 ± 0.1 mL/min/kg in the healthy controls. Mean half-lives of lamotrigine in subjects with mild, moderate, severe without ascites, and severe with ascites hepatic impairment were 46 ± 20, 72 ± 44, 67 ± 11, and 100 ± 48 hours, respectively, as compared with 33 ± 7 hours in healthy controls [see Dosage and Administration (2.1)].
Elderly: The pharmacokinetics of lamotrigine following a single 150 mg dose of immediate-release lamotrigine were evaluated in 12 elderly volunteers between the ages of 65 and 76 years (mean creatinine clearance: 61 mL/min, range: 33 to 108 mL/min). The mean half-life of lamotrigine in these subjects was 31.2 hours (range: 24.5 to 43.4 hours), and the mean clearance was 0.40 mL/min/kg (range: 0.26 to 0.48 mL/min/kg).
Gender: The clearance of lamotrigine is not affected by gender. However, during dose escalation of immediate-release lamotrigine in one clinical trial in patients with epilepsy on a stable dose of valproate (n = 77), mean trough lamotrigine concentrations, unadjusted for weight, were 24% to 45% higher (0.3 to 1.7 mcg/mL) in females than in males.
Race: The apparent oral clearance of lamotrigine was 25% lower in non-Caucasians than Caucasians.
Pediatric Patients: Safety and effectiveness of lamotrigine extended-release for use in patients younger than 13 years have not been established.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis and Mutagenesis and Impairment of Fertility
No evidence of carcinogenicity was seen in mouse or rat following oral administration of lamotrigine for up to 2 years at doses up to 30 mg/kg/day and 10 to 15 mg/kg/day in mouse and rat, respectively. The highest doses tested are less than the human dose of 400 mg/day on a body surface area (mg/m2) basis.
Lamotrigine was negative in in vitro gene mutation (Ames and mouse lymphoma tk) assays and in clastogenicity (in vitro human lymphocyte and in vivo rat bone marrow) assays.
No evidence of impairment of fertility was detected in rats given oral doses of lamotrigine up to 20 mg/kg/day. The highest dose tested is less than the human dose of 400 mg/day on a mg/m2 basis.
-
14 CLINICAL STUDIES
14.1 Adjunctive Therapy for Primary Generalized Tonic-Clonic Seizures
The effectiveness of Lamotrigine extended-release as adjunctive therapy in subjects with PGTC seizures was established in a 19-week, international, multicenter, double-blind, randomized, placebo-controlled trial in 143 patients aged 13 years and older (n=70 on lamotrigine extended-release and n=73 on placebo). Patients with at least 3 PGTC seizures during an 8-week baseline phase were randomized to 19 weeks of treatment with lamotrigine extended-release or placebo added to their current AED regimen of up to 2 drugs. Patients were dosed on a fixed-dose regimen, with target doses ranging from 200 to 500 mg/day of lamotrigine extended-release based on concomitant AEDs (target dose =200 mg for valproate, 300 mg for AEDs not altering plasma lamotrigine levels, and 500 mg for enzyme-inducing AEDs).
The primary efficacy endpoint was percent change from baseline in PGTC seizure frequency during the double-blind treatment phase. For the intent-to-treat population, the median percent reduction in PGTC seizure frequency was 75% in patients treated with lamotrigine extended-release and 32% in patients treated with placebo, a difference that was statistically significant, defined as a 2-sided P value ≤0.05.
Figure 1 presents the percentage of patients (X-axis) with a percent reduction in PGTC seizure frequency (responder rate) from baseline through the entire treatment period at least as great as that represented on the Y-axis. A positive value on the Y-axis indicates an improvement from baseline (i.e., a decrease in seizure frequency), while a negative value indicates a worsening from baseline (i.e., an increase in seizure frequency). Thus, in a display of this type, a curve for an effective treatment is shifted to the left of the curve for placebo. The proportion of patients achieving any particular level of reduction in PGTC seizure frequency was consistently higher for the group treated with lamotrigine extended-release compared with the placebo group. For example, 70% of patients randomized to lamotrigine extended-release experienced a 50% or greater reduction in PGTC seizure frequency, compared with 32% of patients randomized to placebo. Patients with an increase in seizure frequency >100% are represented on the Y-axis as equal or greater than -100%. Figure 1. Proportion of Patients by Responder Rate for Lamotrigine Extended-Release and Placebo Group (Primary Generalized Tonic-Clonic Seizures Study)
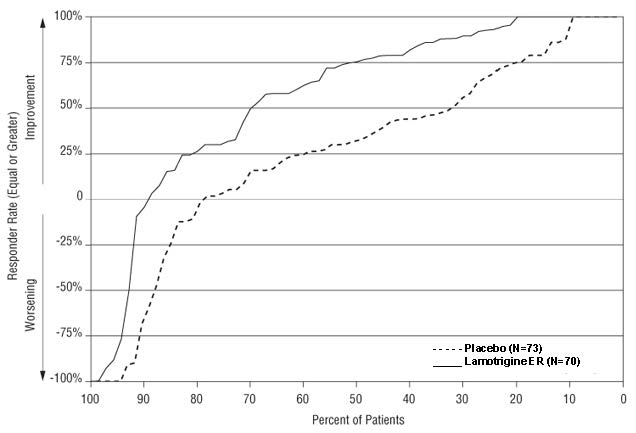
14.2 Adjunctive Therapy for Partial-Onset Seizures
The effectiveness of immediate-release lamotrigine as adjunctive therapy was initially established in 3 pivotal multicenter, placebo-controlled, double-blind clinical trials in 355 adults with refractory partial-onset seizures.
The effectiveness of lamotrigine extended-release as adjunctive therapy in partial-onset seizures, with or without secondary generalization, was established in a 19-week, multicenter, double-blind, placebo-controlled trial in 236 patients aged 13 years and older (approximately 93% of patients were 16 to 65 years old). Approximately 36% were from the U.S. and approximately 64% were from other countries including Argentina, Brazil, Chile, Germany, India, Korea, Russian Federation, and Ukraine. Patients with at least 8 partial-onset seizures during an 8-week prospective baseline phase (or 4-week prospective baseline coupled with a 4-week historical baseline documented with seizure diary data) were randomized to treatment with lamotrigine extended-release (n = 116) or placebo (n = 120) added to their current regimen of 1 or 2 AEDs. Approximately half of the patients were taking 2 concomitant AEDs at baseline. Target doses ranged from 200 to 500 mg/day of lamotrigine extended-release based on concomitant AED (target dose = 200 mg for valproate, 300 mg for AEDs not altering plasma lamotrigine, and 500 mg for enzyme-inducing AEDs). The median partial seizure frequency per week at baseline was 2.3 for lamotrigine extended-release and 2.1 for placebo.
The primary endpoint was the median percent change from baseline in partial-onset seizure frequency during the entire double-blind treatment phase. The median percent reductions in weekly partial-onset seizures were 47% in patients treated with lamotrigine extended-release and 25% on placebo, a difference that was statistically significant, defined as a 2-sided P value <0.05.
Figure 2 presents the percentage of patients (X-axis) with a percent reduction in partial-onset seizure frequency (responder rate) from baseline through the entire treatment period at least as great as that represented on the Y-axis. The proportion of patients achieving any particular level of reduction in partial-onset seizure frequency was consistently higher for the group treated with lamotrigine extended-release compared with the placebo group. For example, 44% of patients randomized to lamotrigine extended-release experienced a 50% or greater reduction in partial-onset seizure frequency, compared with 21% of patients randomized to placebo.
Figure 2. Proportion of Patients by Responder Rate for Lamotrigine Extended-Release and Placebo Group (Partial-Onset Seizure Study)
14.3 Conversion to Monotherapy for Partial-Onset Seizures
The effectiveness of lamotrigine extended-release as monotherapy for partial-onset seizures was established in a historical control trial in 223 adults with partial-onset seizures. The historical control methodology is described in a publication by French, et al. [see References 15)]. Briefly, in this study, patients were randomized to ultimately receive either lamotrigine extended-release 300 mg or 250 mg once a day, and their responses were compared to those of a historical control group. This historical control consisted of a pooled analysis of the control groups from 8 studies of similar design, which utilized a subtherapeutic dose of an AED as a comparator. Statistical superiority to the historical control was considered to be demonstrated if the upper 95% confidence interval for the proportion of patients meeting escape criteria in patients receiving lamotrigine extended-release remained below the lower 95% prediction interval of 65.3% derived from the historical control data.
In this study, patients aged 13 years and older experienced at least 4 partial-onset seizures during an 8 week baseline period with at least 1 seizure occurring during each of 2 consecutive 4 week periods while receiving valproate or a non-enzyme inducing AED. Lamotrigine extended-release was added to either valproate or a non-enzyme inducing AED over a 6 to 7 week period followed by the gradual withdrawal of the background AED. Patients were then continued on monotherapy with lamotrigine extended-release for 12 weeks. The escape criteria were one or more of the following: (1) doubling of average monthly seizure count during any 28 consecutive days, (2) doubling of highest consecutive 2 day seizure frequency during the entire treatment phase, (3) emergence of a new seizure type compared to baseline (4) clinically significant prolongation of generalized tonic-clonic seizures or worsening of seizure considered by the investigator to require intervention. These criteria were similar to those in the 8 controlled trials from which the historical control group was constituted.
The upper 95% confidence limits of the proportion of subjects meeting escape criteria (40.2% at 300 mg/day and 44.5% at 250 mg/day) were below the threshold of 65.3% derived from the historical control data.
Although the study population was not fully comparable to the historical controlled population and the study was not fully blinded, numerous sensitivity analyses supported the primary results. Efficacy was further supported by the established effectiveness of the immediate-release formulation as monotherapy.
- 15. References
- 16 HOW SUPPLIED
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
Rash
Prior to initiation of treatment with lamotrigine extended-release, inform patients that a rash or other signs or symptoms of hypersensitivity (e.g., fever, lymphadenopathy) may herald a serious medical event and instruct them to report any such occurrence to their physician immediately.
Multiorgan Hypersensitivity Reactions, Blood Dyscrasias and Organ Failure
Inform patients that multiorgan hypersensitivity reactions and acute multiorgan failure may occur with lamotrigine. Isolated organ failure or isolated blood dyscrasias without evidence of multiorgan hypersensitivity may also occur. Instruct patients to contact their physician immediately if they experience any signs or symptoms of these conditions [see Warnings and Precautions (5.2, 5.3)].
Suicidal Thinking and Behavior
Inform patients, their caregivers, and families that AEDs, including lamotrigine extended-release, may increase the risk of suicidal thoughts and behavior. Instruct them to be alert for the emergence or worsening of symptoms of depression, any unusual changes in mood or behavior, or the emergence of suicidal thoughts or behavior or thoughts about self-harm. Instruct them to immediately report behaviors of concern to their physician.
Worsening of Seizures
Advise patients to notify their physician if worsening of seizure control occurs.
Central Nervous System Adverse Effects
Inform patients that lamotrigine extended-release may cause dizziness, somnolence, and other symptoms and signs of central nervous system depression. Accordingly, instruct them neither to drive a car nor to operate other complex machinery until they have gained sufficient experience on lamotrigine extended-release to gauge whether or not it adversely affects their mental and/or motor performance.
Pregnancy and Nursing
Instruct patients to notify their physicians if they become pregnant or intend to become pregnant during therapy and if they intend to breastfeed or are breastfeeding an infant.
Encourage patients to enroll in the NAAED Pregnancy Registry if they become pregnant. This registry is collecting information about the safety of antiepileptic drugs during pregnancy. To enroll, patients can call the toll-free number 1-888-233-2334 [see Use in Specific Populations (8.1)].
Inform patients who intend to breastfeed that lamotrigine extended-release is present in breast milk and advise them to monitor their child for potential adverse effects of this drug. Discuss the benefits and risks of continuing breastfeeding.
Oral Contraceptive Use
Instruct women to notify their physician if they plan to start or stop use of oral contraceptives or other female hormonal preparations. Starting estrogen-containing oral contraceptives may significantly decrease lamotrigine plasma levels and stopping estrogen-containing oral contraceptives (including the pill-free week) may significantly increase lamotrigine plasma levels [see Warnings and Precautions (5.7), Clinical Pharmacology (12.3)]. Also instruct women to promptly notify their physician if they experience adverse reactions or changes in menstrual pattern (e.g., break-through bleeding) while receiving lamotrigine extended-release in combination with these medications.
Discontinuing Lamotrigine Extended-Release
Instruct patients to notify their physician if they stop taking lamotrigine extended-release for any reason and not to resume lamotrigine extended-release without consulting their physician.
Aseptic Meningitis
Inform patients that lamotrigine extended-release may cause aseptic meningitis. Instruct them to notify their physician immediately if they develop signs and symptoms of meningitis such as headache, fever, nausea, vomiting, stiff neck, rash, abnormal sensitivity to light, myalgia, chills, confusion, or drowsiness while taking lamotrigine extended-release.
Potential Medication Errors
Medication errors involving lamotrigine have occurred. In particular the name lamotrigine can be confused with the names of other commonly used medications. Medication errors may also occur between the different formulations of lamotrigine. To reduce the potential of medication errors, write and say lamotrigine extended-release clearly. Depictions of the lamotrigine extended-release tablets can be found in the Medication Guide. Each lamotrigine extended-release tablet has a distinct color and is printed with Par and 561, 562, 563, 564, 604 or 605. These distinctive features serve to identify the different presentations of the drug and thus may help reduce the risk of medication errors. Lamotrigine extended-release is supplied in round, unit-of-use bottles containing 30 tablets. Lamotrigine extended-release is also supplied in bottles of 100 and 500 tablets. The label on the bottle includes a depiction of the tablets which further communicates to patients and pharmacists that the medication is lamotrigine extended-release and the specific tablet strength included in the bottle. The unit-of-use bottle with a distinctive bottle label feature serves to identify the different presentations of the drug and this may help reduce the risk of medication errors. To avoid a medication error of using the wrong drug or formulation, patients should be strongly advised to visually inspect their tablets to verify that they are lamotrigine each time they fill their prescription. [see Dosage Forms and Strengths (3), How Supplied/Storage and Handling (16)].
-
MEDICATION GUIDE
Lamotrigine (la-MO-tri-jen) Extended-Release Tablets
Read this Medication Guide before you start taking lamotrigine extended-release tablets and each time you get a refill. There may be new information. This information does not take the place of talking with your healthcare provider about your medical condition or treatment. If you have questions about lamotrigine extended-release tablets, ask your healthcare provider or pharmacist.
What is the most important information I should know about lamotrigine extended-release tablets?
1. Lamotrigine extended-release tablets may cause a serious skin rash that may cause you to be hospitalized or even cause death.
There is no way to tell if a mild rash will become more serious. A serious skin rash can happen at any time during your treatment with lamotrigine extended-release tablets, but is more likely to happen within the first 2 to 8 weeks of treatment. Children aged between 2 and 16 years have a higher chance of getting this serious skin rash while taking lamotrigine extended-release tablets. Lamotrigine extended-release tablets is not approved for use in children younger than 13 years.
The risk of getting a serious skin rash is higher if you:
- take lamotrigine extended-release tablets while taking valproate (DEPAKENE® (valproic acid) or DEPAKOTE® (divalproex sodium)).
- take a higher starting dose of lamotrigine extended-release tablet than your healthcare provider prescribed.
- increase your dose of lamotrigine extended-release tablet faster than prescribed.
Call your healthcare provider right away if you have any of the following:
- a skin rash
- blistering or peeling of your skin
- hives
- painful sores in your mouth or around your eyes
These symptoms may be the first signs of a serious skin reaction. A healthcare provider should examine you to decide if you should continue taking lamotrigine extended-release tablets.
2. Other serious reactions, including serious blood problems or liver problems. Lamotrigine extended-release tablets can also cause other types of allergic reactions or serious problems that may affect organs and other parts of your body like your liver or blood cells. You may or may not have a rash with these types of reactions. Call your healthcare provider right away if you have any of these symptoms:
● fever
● frequent infections
● severe muscle pain
● swelling of your face, eyes, lips or tongue
● swollen lymph glands
● unusual bruising or bleeding
● weakness, fatigue
● yellowing of your skin or the white part of your eyes
3. Like other antiepileptic drugs, Lamotrigine extended-release tablets may cause suicidal thoughts or actions in a very small number of people, about 1 in 500.
Call a healthcare provider right away if you have any of these symptoms, especially if they are new, worse, or worry you:
- thoughts about suicide or dying
- attempt to commit suicide
- new or worse depression
- new or worse anxiety
- feeling agitated or restless
- panic attacks
- trouble sleeping (insomnia)
- new or worse irritability
- acting aggressive, being angry, or violent
- acting on dangerous impulses
- an extreme increase in activity and talking (mania)
- other unusual changes in behavior or mood
Do not stop lamotrigine extended-release tablets without first talking to a healthcare provider.
-
- Stopping lamotrigine extended-release tablets suddenly can cause serious problems.
- Suicidal thoughts or actions can be caused by things other than medicines. If you have suicidal thoughts or actions, your healthcare provider may check for other causes.
How can I watch for early symptoms of suicidal thoughts and actions?
- Pay attention to any changes, especially sudden changes, in mood, behaviors, thoughts, or feelings.
- Keep all follow-up visits with your healthcare provider as scheduled.
- Call your healthcare provider between visits as needed, especially if you are worried about symptoms.
4. Lamotrigine extended-release tablets may rarely cause aseptic meningitis, a serious inflammation of the protective membrane that covers the brain and spinal cord.
Call your healthcare provider right away if you have any of the following symptoms:
- headache
- fever
- nausea
- vomiting
- stiff neck
- rash
- unusual sensitivity to light
- muscle pains
- chills
- confusion
- drowsiness
Meningitis has many causes other than lamotrigine extended-release tablets, which your doctor would check for if you developed meningitis while taking lamotrigine extended-release tablets.
Lamotrigine extended-release tablets can have other serious side effects. For more information ask your healthcare provider or pharmacist. Tell your healthcare provider if you have any side effect that bothers you. Be sure to read the section below entitled “What are the possible side effects of lamotrigine extended-release tablets?”
5. Patients prescribed Lamotrigine extended-release tablets have sometimes been given the wrong medicine because many medicines have names similar to Lamotrigine extended-release tablets, so always check that you receive Lamotrigine extended-release tablets.
Taking the wrong medication can cause serious health problems. When your healthcare provider gives you a prescription for lamotrigine extended-release tablets:
- Make sure you can read it clearly.
- Talk to your pharmacist to check that you are given the correct medicine.
- Each time you fill your prescription, check the tablets you receive against the pictures of the tablets below.
These pictures show the distinct wording, colors, and shapes of the tablets that help identify the right strength of lamotrigine extended-release tablet. Immediately call your pharmacist if you receive a lamotrigine extended-release tablet that does not look like one of the tablets shown below, as you may have received the wrong medication.
25 mg: round, beige, biconvex, film-coated tablet debossed with “561” on one side and “Par” on the other
50 mg: round, white, biconvex, film-coated tablet debossed with “562” on one side and “Par” on the other
100 mg: round, brown, biconvex, film-coated tablet debossed with “563” on one side and “Par” on the other
200 mg: round, yellow, biconvex, film-coated tablet debossed with “564” on one side and “Par” on the other
250 mg: round white, biconvex, film-coated tablet debossed with “604” on one side and “Par” on the other
300 mg: round, grey, biconvex, film-coated tablet debossed with “605” on one side and “Par” on the other
What is Lamotrigine Extended-Release Tablets?
Lamotrigine extended-release tablet is a prescription medicine used:
- together with other medicines to treat primary generalized tonic-clonic seizures and partial-onset seizures in people aged 13 years and older.
- alone when changing from 1 other medicine used to treat partial-onset seizures in people aged 13 years and older.
It is not known if lamotrigine extended-release tablets are safe or effective in children younger than 13 years. Other forms of lamotrigine can be used in children aged 2 to 12 years.
It is not known if lamotrigine extended-release tablets is safe or effective when used alone as the first treatment of seizures.
Who should not take Lamotrigine Extended-Release Tablets?
You should not take lamotrigine extended-release tablets if you have had an allergic reaction to lamotrigine or to any of the inactive ingredients in lamotrigine extended-release tablets. See the end of this leaflet for a complete list of ingredients in lamotrigine extended-release tablets.
What should I tell my healthcare provider before taking Lamotrigine Extended-Release Tablets?
Before taking lamotrigine extended-release tablets, tell your healthcare provider about all of your medical conditions, including if you:
- have had a rash or allergic reaction to another antiseizure medicine.
- have or have had depression, mood problems or suicidal thoughts or behavior.
- have had aseptic meningitis after taking lamotrigine extended-release tablets.
- are taking oral contraceptives (birth control pills) or other female hormonal medicines. Do not start or stop taking birth control pills or other female hormonal medicine until you have talked with your healthcare provider. Tell your healthcare provider if you have any changes in your menstrual pattern such as breakthrough bleeding. Stopping these medicines may cause side effects (such as dizziness, lack of coordination, or double vision). Starting these medicines may lessen how well lamotrigine extended-release tablet works.
- are pregnant or plan to become pregnant. It is not known if lamotrigine extended-release tablets will harm your unborn baby. If you become pregnant while taking lamotrigine extended-release tablets, talk to your healthcare provider about registering with the North American Antiepileptic Drug Pregnancy Registry. You can enroll in this registry by calling 1-888-233-2334. The purpose of this registry is to collect information about the safety of antiepileptic drugs during pregnancy.
- are breastfeeding. Lamotrigine extended-release passes into breast milk and may cause side effects in a breastfed baby. If you breastfeed while taking lamotrigine extended-release tablets, watch your baby closely for trouble breathing, episodes of temporarily stopping breathing, sleepiness, or poor sucking. Call your baby’s healthcare provider right away if you see any of these problems. Talk to your healthcare provider about the best way to feed your baby if you take lamotrigine extended-release tablets.
Tell your healthcare provider about all the medicines you take or if you are planning to take a new medicine, including prescription and non-prescription medicines, vitamins, and herbal supplements. If you use lamotrigine extended-release tablets with certain other medicines, they can affect each other, causing side effects.
How should I take Lamotrigine Extended-Release Tablets?
- Take lamotrigine extended-release tablets exactly as prescribed.
- Your healthcare provider may change your dose. Do not change your dose without talking to your healthcare provider.
- Do not stop taking lamotrigine extended-release tablets without talking to your healthcare provider. Stopping lamotrigine extended-release tablets suddenly may cause serious problems. For example, if you have epilepsy and you stop taking lamotrigine extended-release tablets suddenly, you may have seizures that do not stop. Talk with your healthcare provider about how to stop lamotrigine extended-release tablets slowly.
- If you miss a dose of lamotrigine extended-release tablets, take it as soon as you remember. If it is almost time for your next dose, just skip the missed dose. Take the next dose at your regular time. Do not take two doses at the same time.
- If you take too much lamotrigine extended-release tablets, call your healthcare provider or your local Poison Control Center or go to the nearest hospital emergency room right away.
- You may not feel the full effect of lamotrigine extended-release tablets for several weeks.
- If you have epilepsy, tell your healthcare provider if your seizures get worse or if you have any new types of seizures.
- Lamotrigine extended-release tablets can be taken with or without food.
- Do not chew, crush, or divide lamotrigine extended-release tablets.
- Swallow lamotrigine extended-release tablets whole.
- If you have trouble swallowing lamotrigine extended-release tablets, tell your healthcare provider because there may be another form of lamotrigine you can take.
What should I avoid while taking Lamotrigine Extended-Release Tablets?
- Do not drive a car or operate complex, hazardous machinery until you know how lamotrigine extended-release tablets affects you.
What are possible side effects of Lamotrigine Extended-Release Tablets?
See “What is the most important information I should know about lamotrigine extended-release tablets?” Common side effects of lamotrigine extended-release tablets include:
- dizziness
- tremor
- double vision
- nausea
- vomiting
- trouble with balance and coordination
- anxiety
Other common side effects that have been reported with another form of lamotrigine include headache, sleepiness, blurred vision, runny nose, and rash.
Tell your healthcare provider about any side effect that bothers you or that does not go away. These are not all the possible side effects of lamotrigine extended-release tablets.
For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1‑800-FDA-1088.
How should I store Lamotrigine Extended-Release Tablets?
- Store lamotrigine extended-release tablets at room temperature between 20° to 25°C (68° to 77°F); excursions permitted to 15° to 30ºC (59° to 86°F) [see USP Controlled Room Temperature].
- Keep lamotrigine extended-release tablets and all medicines out of the reach of children.
General information about Lamotrigine Extended-Release Tablets
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use lamotrigine extended-release tablets for a condition for which it was not prescribed. Do not give lamotrigine extended-release tablets to other people, even if they have the same symptoms you have. It may harm them.
If you take a urine drug screening test, Lamotrigine Extended-Release Tablets may make the test result positive for another drug. If you require a urine drug screening test, tell the healthcare professional administering the test that you are taking Lamotrigine Extended-Release Tablets.
This Medication Guide summarizes the most important information about lamotrigine extended-release tablets. If you would like more information, talk with your healthcare provider. You can ask your healthcare provider or pharmacist for information about lamotrigine extended-release tablets that is written for healthcare professionals.
For more information, go to www.parpharm.com or call 1-800-828-9393.
What are the ingredients in Lamotrigine Extended-Release Tablets?
Active ingredient: Lamotrigine.
Inactive ingredients: hypromellose, lactose monohydrate; magnesium stearate; colloidal anhydrous silica (25 mg, 50 mg, 200 mg, 250 mg and 300 mg tablets only), methacrylic acid copolymer, talc, titanium dioxide, triethyl citrate, sodium bicarbonate, sodium laurel sulfate, iron oxide yellow (25 mg and 100 mg tablets only), iron oxide red (25 mg and 100 mg tablets only), D&C Yellow # 10 (200 mg tablet only), FD&C Yellow # 6 (200 mg tablet only) and black iron oxide (300 mg tablet only).
This Medication Guide has been approved by the U.S. Food and Drug Administration.
Manufactured by:
Zhejiang Huahai Pharmaceutical Co., Ltd.
Zhejiang 317024 China
For:
Par Pharmaceutical Companies, Inc.
Chestnut Ridge, NY 10977 U.S.A.
MADE IN CHINA
DEPAKENE® and DEPAKOTE® are registered trademarks of Abbott Laboratories.
Revised: 01/2016
- Lamotrigine ER 300mg Tablet
-
INGREDIENTS AND APPEARANCE
LAMOTRIGINE EXTENDED RELEASE
lamotrigine extended release tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 63629-7020(NDC:49884-605) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LAMOTRIGINE (UNII: U3H27498KS) (LAMOTRIGINE - UNII:U3H27498KS) LAMOTRIGINE 300 mg Inactive Ingredients Ingredient Name Strength FERROSOFERRIC OXIDE (UNII: XM0M87F357) METHACRYLIC ACID (UNII: 1CS02G8656) HYPROMELLOSE, UNSPECIFIED (UNII: 3NXW29V3WO) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) Product Characteristics Color gray Score no score Shape ROUND Size 10mm Flavor Imprint Code Par;605 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 63629-7020-1 30 in 1 BOTTLE; Type 0: Not a Combination Product 06/07/2016 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA201791 01/18/2013 Labeler - Bryant Ranch Prepack (171714327) Establishment Name Address ID/FEI Business Operations Bryant Ranch Prepack 171714327 REPACK(63629-7020) , RELABEL(63629-7020)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.