ELIGARD- leuprolide acetate kit
ELIGARD by
Drug Labeling and Warnings
ELIGARD by is a Prescription medication manufactured, distributed, or labeled by TOLMAR PHARMACEUTICALS INC., Bachem AG, Isomedix Operations Inc, TOLMAR 1201 Cornerstone LLC, TOLMAR Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use ELIGARD® safely and effectively. See full prescribing information for ELIGARD®.
ELIGARD® (leuprolide acetate) for injectable suspension, for subcutaneous use
Initial U.S. Approval: 2002RECENT MAJOR CHANGES
INDICATIONS AND USAGE
ELIGARD® is a gonadotropin releasing hormone (GnRH) agonist indicated for the palliative treatment of advanced prostate cancer (1)
DOSAGE AND ADMINISTRATION
DOSAGE FORMS AND STRENGTHS
CONTRAINDICATIONS
- Known hypersensitivity to GnRH, GnRH agonist analogs or any of the components of ELIGARD® (4.1)
WARNINGS AND PRECAUTIONS
- Tumor Flare: Transient increase in serum levels of testosterone during treatment may result in worsening of symptoms or onset of new signs and symptoms during the first few weeks of treatment, including bone pain, neuropathy, hematuria, bladder outlet obstruction, ureteral obstruction, or spinal cord compression. Monitor patients at risk closely and manage as appropriate. (5.1, 5.2)
- Hyperglycemia and diabetes: Hyperglycemia and an increased risk of developing diabetes have been reported in men receiving GnRH analogs. Monitor blood glucose level and manage according to current clinical practice. (5.3)
- Cardiovascular diseases: Increased risk of myocardial infarction, sudden cardiac death and stroke has been reported in men. Monitor for cardiovascular disease and manage according to current clinical practice. (5.4)
- Effect on QT/QTc Interval: Androgen deprivation therapy may prolong the QT interval. Consider risks and benefits. (5.5)
- Embryo-Fetal Toxicity: May cause fetal harm. (5.6, 8.1)
- Convulsions have been observed in patients with or without a history of predisposing factors. Manage convulsions according to the current clinical practice. (5.7)
ADVERSE REACTIONS
- Most common adverse reactions in clinical studies (incidence ≥ 5%): Malaise, fatigue, hot flashes/sweats, and testicular atrophy. (6.1)
- As with other GnRH agonists, other adverse reactions, including decreased bone density and rare cases of pituitary apoplexy have been reported. (6.1, 6.2)
To report SUSPECTED ADVERSE REACTIONS, contact Tolmar Pharmaceuticals, Inc. at 1-888-354-4273 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 4/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
RECENT MAJOR CHANGES
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Mixing Procedure
2.2 Administration Procedure
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Tumor Flare
5.2 Laboratory Tests
5.3 Hyperglycemia and Diabetes
5.4 Cardiovascular Diseases
5.5 Effect on QT/QTc Interval
5.6 Embryo-Fetal Toxicity
5.7 Convulsions
6 ADVERSE REACTIONS
6.1 Clinical Trial Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
15 REFERENCES
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
16.2 Storage
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
ELIGARD® is administered subcutaneously and provides continuous release of leuprolide acetate over a one-, three-, four-, or six-month treatment period (Table 1). The injection delivers the dose of leuprolide acetate incorporated in a polymer formulation.
Table 1. ELIGARD® Recommended Dosing
Dosage
7.5 mg
22.5 mg
30 mg
45 mg
Recommended dose
1 injection every
month1 injection every
3 months1 injection every
4 months1 injection every
6 monthsAs with other drugs administered by subcutaneous injection, the injection site should vary periodically. The specific injection location should be an area with sufficient soft or loose subcutaneous tissue. In clinical trials, the injections were administered in the upper- or mid-abdominal area. Avoid areas with brawny or fibrous subcutaneous tissue or locations that could be rubbed or compressed (i.e., with a belt or clothing waistband).
2.1 Mixing Procedure
Use aseptic technique throughout the procedure. As with other similar agents, the use of gloves is recommended during mixing and administration.1 Allow the product to reach room temperature before mixing. Once mixed, the product must be administered within 30 minutes or it should be discarded.
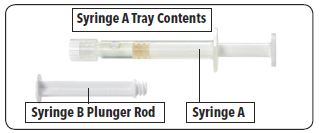
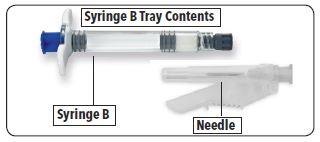
- ELIGARD® is packaged in a carton containing two thermoformed trays and this package insert:
Table 2: Contents of the Two Trays in the ELIGARD® Carton
Syringe A Tray
Syringe B Tray
Syringe A pre-filled with the ATRIGEL® Delivery System
Syringe B pre-filled with the leuprolide acetate powder
Long white plunger rod
Safety needle
Desiccant pack
Desiccant pack
Follow the detailed instructions below to ensure correct preparation of ELIGARD® prior to administration:
1. On a clean field, open both trays by tearing off the foil from the corners and removing the contents. Discard the desiccant pack(s). Open the safety needle package by peeling back the paper tab. 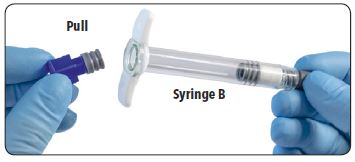
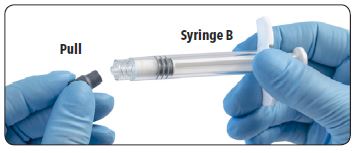
2. Pull out (do not unscrew) the short blue plunger rod with attached gray stopper from Syringe B and discard.
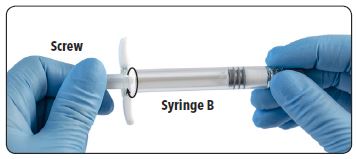
3. Gently screw the white plunger rod into the remaining gray stopper in Syringe B.
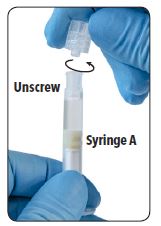
4. Unscrew and discard the clear cap from Syringe A.
5. Remove and discard the gray rubber cap from Syringe B.
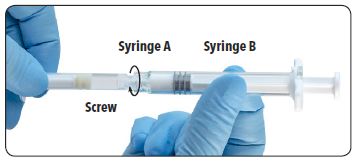
6. Join the two syringes together by pushing and gently screwing until secure.
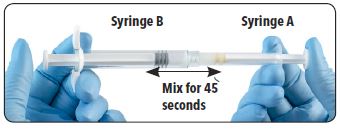
7. Inject the liquid contents of Syringe A into the leuprolide acetate powder contained in Syringe B. Thoroughly mix the product for approximately 45 seconds by pushing the contents back and forth between both syringes to obtain a uniform suspension. When thoroughly mixed, the suspension will appear light tan to tan (ELIGARD® 7.5 mg) or colorless to pale yellow (ELIGARD® 22.5 mg, 30 mg and 45 mg). Note: Product must be mixed as described; shaking will NOT provide adequate mixing.
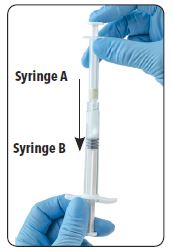
8. After mixing, hold the syringes vertically (upright) with Syringe B (short, wide syringe) on the bottom. The syringes should remain securely coupled. Draw all of the mixed product into Syringe B by depressing the Syringe A plunger and slightly withdrawing the Syringe B plunger.

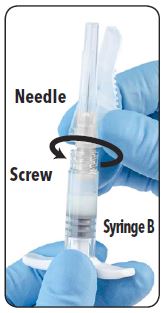
9. Unscrew Syringe A to decouple the syringes while continuing to push down on the Syringe A plunger. Note: Small air bubbles will remain in the formulation – this is acceptable.
10. Continue to hold Syringe B upright with the open end at the top. Hold back the white plunger on Syringe B to prevent loss of the product and attach the safety needle cartridge. Gently screw clockwise with approximately a three-quarter turn until the needle is secure. Do not overtighten, as the hub may become damaged resulting in leakage of the product during injection. The safety sheath may also be damaged if the needle is screwed with too much force.
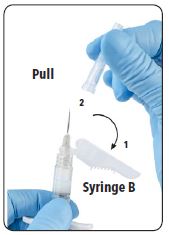
11. (1) Move the safety sheath away from the needle and towards the syringe and (2) pull off the clear needle cartridge cover immediately prior to administration.
Note: Should the needle hub appear to be damaged, or leak, the product should NOT be used. The damaged needle should NOT be replaced and the product should NOT be injected. In the event of damage to the needle hub, use a new replacement ELIGARD® carton.
2.2 Administration Procedure
1. Select an injection site on the abdomen, upper buttocks, or another location with adequate amounts of subcutaneous tissue that does not have excessive pigment, nodules, lesions, or hair and hasn’t recently been used.
2. Cleanse the injection-site area with an alcohol swab (not enclosed).
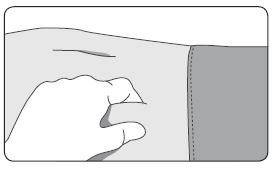
3. Using the thumb and forefinger, grab and bunch the area of skin around the injection site.
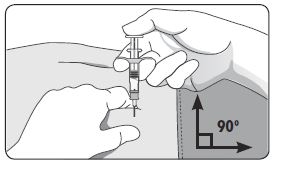
4. Using your dominant hand, insert the needle quickly at a 90° angle to the skin surface. The depth of penetration will depend on the amount and fullness of the subcutaneous tissue and the length of the needle. After the needle is inserted, release the skin.
5. Inject the drug using a slow, steady push and press down on the plunger until the syringe is empty.
6. Withdraw the needle quickly at the same 90° angle used for insertion.


7. Immediately following the withdrawal of the needle, activate the safety shield using a finger/thumb or flat surface and push until it completely covers the needle tip and locks into place.


8. An audible and tactile “click” verifies a locked position.
9. Check to confirm the safety sheath is fully engaged. Discard all components safely in an appropriate biohazard container.
-
3 DOSAGE FORMS AND STRENGTHS
ELIGARD® is an injectable suspension of leuprolide acetate available in a single-dose kit. The kit consists of a two-syringe mixing system, a sterile safety needle (Table 3), a desiccant, and a package insert for reconstitution and administration procedures. The syringes are packaged separately: Syringe A contains the ATRIGEL® Delivery System and the Syringe B contains leuprolide acetate powder. When reconstituted, ELIGARD® is administered as a single dose.
Table 3. Specifications for ELIGARD® Sterile Safety Needle
ELIGARD® strength
Gauge
Length 7.5 mg
20-gauge
5/8-inch 22.5 mg
20-gauge
5/8-inch 30 mg
20-gauge
5/8-inch 45 mg 18-gauge 5/8-inch - 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Tumor Flare
ELIGARD® 7.5 mg 22.5 mg 30 mg, like other GnRH agonists, causes a transient increase in serum concentrations of testosterone during the first week of treatment. ELIGARD® 45 mg causes a transient increase in serum concentrations of testosterone during the first two weeks of treatment. Patients may experience worsening of symptoms or onset of new signs and symptoms during the first few weeks of treatment, including bone pain, neuropathy, hematuria, or bladder outlet obstruction.
Cases of ureteral obstruction and/or spinal cord compression, which may contribute to paralysis with or without fatal complications, have been observed in the palliative treatment of advanced prostate cancer using GnRH agonists.
Patients with metastatic vertebral lesions and/or with urinary tract obstruction should be closely observed during the first few weeks of therapy. If spinal cord compression or ureteral obstruction develops, standard treatment of these complications should be instituted.
5.2 Laboratory Tests
Response to ELIGARD® should be monitored by periodic measurement of serum concentrations of testosterone and prostate specific antigen.
In the majority of patients, testosterone levels increased above Baseline during the first week, declining thereafter to Baseline levels or below by the end of the second or third week. Castrate levels were generally reached within two to four weeks.
Castrate testosterone levels were maintained for the duration of the treatment with ELIGARD® 7.5 mg. No increases to above the castrate level occurred in any of the patients.
Castrate levels were generally maintained for the duration of treatment with ELIGARD® 22.5 mg.
Once castrate levels were achieved with ELIGARD® 30 mg, most (86/89) patients remained suppressed throughout the study.
Once castrate levels were achieved with ELIGARD® 45 mg, only one patient (< 1%) experienced a breakthrough, with testosterone levels > 50 ng/dL.
Results of testosterone determinations are dependent on assay methodology. It is advisable to be aware of the type and precision of the assay methodology to make appropriate clinical and therapeutic decisions.
Drug/Laboratory Test Interactions: Therapy with leuprolide acetate results in suppression of the pituitary-gonadal system. Results of diagnostic tests of pituitary gonadotropic and gonadal functions conducted during and after leuprolide therapy may be affected.
5.3 Hyperglycemia and Diabetes
Hyperglycemia and an increased risk of developing diabetes have been reported in men receiving GnRH agonists. Hyperglycemia may represent development of diabetes mellitus or worsening of glycemic control in patients with diabetes. Monitor blood glucose and/or glycosylated hemoglobin (HbA1c) periodically in patients receiving a GnRH agonist and manage with current practice for treatment of hyperglycemia or diabetes.
5.4 Cardiovascular Diseases
Increased risk of developing myocardial infarction, sudden cardiac death and stroke has been reported in association with use of GnRH agonists in men. The risk appears low based on the reported odds ratios, and should be evaluated carefully along with cardiovascular risk factors when determining a treatment for patients with prostate cancer. Patients receiving a GnRH agonist should be monitored for symptoms and signs suggestive of development of cardiovascular disease and be managed according to current clinical practice.
5.5 Effect on QT/QTc Interval
Androgen deprivation therapy may prolong the QT/QTc interval. Providers should consider whether the benefits of androgen deprivation therapy outweigh the potential risks in patients with congenital long QT syndrome, congestive heart failure, frequent electrolyte abnormalities, and in patients taking drugs known to prolong the QT interval. Electrolyte abnormalities should be corrected. Consider periodic monitoring of electrocardiograms and electrolytes.
5.6 Embryo-Fetal Toxicity
Based on findings in animal studies and mechanism of action, leuprolide acetate may cause fetal harm when administered to a pregnant woman. In animal developmental and reproductive studies, major fetal abnormalities were observed after administration of leuprolide acetate throughout gestation in rats. Advise pregnant patients and females of reproductive potential of the potential risk to the fetus [see Use in Specific Populations (8.1), Clinical Pharmacology (12.1)].
5.7 Convulsions
Postmarketing reports of convulsions have been observed in patients on leuprolide acetate therapy. These included patients with a history of seizures, epilepsy, cerebrovascular disorders, central nervous system anomalies or tumors, and in patients on concomitant medications that have been associated with convulsions such as bupropion and SSRIs. Convulsions have also been reported in patients in the absence of any of the conditions mentioned above. Patients receiving a GnRH agonist who experience convulsion should be managed according to current clinical practice.
-
6 ADVERSE REACTIONS
6.1 Clinical Trial Experience
The safety of all ELIGARD® formulations was evaluated in clinical trials involving patients with advanced prostate cancer. In addition, the safety of ELIGARD® 7.5 mg was evaluated in 8 surgically castrated males (Table 5). ELIGARD®, like other GnRH analogs, caused a transient increase in serum testosterone concentrations during the first one to two weeks of treatment. Therefore, potential exacerbations of signs and symptoms of the disease during the first weeks of treatment are of concern in patients with vertebral metastases and/or urinary obstruction or hematuria. If these conditions are aggravated, it may lead to neurological problems such as weakness and/or paresthesia of the lower limbs or worsening of urinary symptoms [see WARNINGS AND PRECAUTIONS (5.2)].
During the clinical trials, injection sites were closely monitored. Refer to Table 4 for a summary of reported injection site events.
Table 4. Reported Injection Site Adverse Events
ELIGARD®
7.5 mg
22.5 mg
30 mg
45 mg
Study number
AGL9904
AGL9909
AGL0001
AGL0205
Number of patients
120
117
90
111
Treatment
1 injection every month up to 6 months
1 injection every 3 months up to 6 months
1 injection every 4 months up to 8 months
1 injection every 6 months up to 12 months
Number of injections
716
230
175
217
Transient burning/
stinging248 (34.6%) injections; 84% reported as mild
50 (21.7%) injections; 86% reported as mild
35 (20%) injections; 100% reported as mild
35 (16%) injections; 91.4% reported as mild3
Pain (generally brief and mild)
4.3% of injections (18.3% of patients)
3.5% of injections
(6.0% of patients)2.3% of injections2
(3.3% of patients)4.6% of injections4
Erythema (generally brief and mild) 2.6% of injections (12.5% of patients) 0.9% of injections1
(1.7% of patients)1.1% of injections
(2.2% of patients)- Bruising (mild) 2.5% of injections (11.7% of patients) 1.7% of injections
(3.4% of patients)- 2.3% of injections5 Pruritus 1.4% of injections (9.2% of patients) 0.4% of injections
(0.9% of patients)- - Induration 0.4% of injections (2.5% of patients) - - - Ulceration 0.1% of injections
(> 0.8% of patients)- - - - Erythema was reported following 2 injections of ELIGARD® 22.5 mg. One report characterized the erythema as mild and it resolved within 7 days. The other report characterized the erythema as moderate and it resolved within 15 days. Neither patient experienced erythema at multiple injection times.
- A single event reported as moderate pain resolved within two minutes and all 3 mild pain events resolved within several days following injection of ELIGARD® 30 mg.
- Following injection of ELIGARD® 30 mg, three of the 35 burning/stinging events were reported as moderate.
- Transient pain was reported as mild in intensity in nine of ten (90%) events and moderate in intensity in one of ten (10%) events following injection of ELIGARD® 45 mg.
- Mild bruising was reported following 5 (2.3%) study injections and moderate bruising was reported following 2 (<1%) study injections of ELIGARD® 45 mg.
These localized adverse events were non-recurrent over time. No patient discontinued therapy due to an injection site adverse event.
The following possibly or probably related systemic adverse events occurred during clinical trials with ELIGARD®, and were reported in > 2% of patients (Table 5). Often, causality is difficult to assess in patients with metastatic prostate cancer. Reactions considered not drug-related are excluded.
Table 5. Summary of Possible or Probably Related Systemic Adverse Events Reported by > 2% of Patients Treated with ELIGARD®
ELIGARD®
7.5 mg
7.5 mg
22.5 mg
30 mg
45 mg
Study number
AGL9904
AGL9802
AGL9909
AGL0001
AGL0205
Number of patients
120
8
117
90
111
Treatment
1 injection
every month
up to 6 months1 injection
(surgically castrated
patients)1 injection every 3 months up to 6 months
1 injection
every 4 months up
to 8
months1 injection
every 6 months up to
12 monthsBody system Adverse event Number (percent) Body as a whole Malaise and fatigue 21 (17.5%) - 7 (6.0%) 12 (13.3%) 13 (11.7%) Weakness - - - - 4 (3.6%) Nervous system Dizziness 4 (3.3%) - - 4 (4.4%) - Vascular Hot flashes/sweats 68 (56.7%)* 2 (25.0%)* 66 (56.4%)* 66 (73.3%)*
64 (57.7%)* Renal/urinary
Urinary frequency - - 3 (2.6%) 2 (2.2%) - Nocturia - - - 2 (2.2%) - Gastrointestinal Nausea - - 4 (3.4%) 2 (2.2%) - Gastroenteritis/colitis 3 (2.5%) - - - - Skin Pruritus - - 3 (2.6%) - - Clamminess - - - 4 (4.4%)* - Night sweats - - - 3 (3.3%)* 3 (2.7%)* Alopecia - - - 2 (2.2%) - Musculoskeletal Arthralgia - - 4 (3.4%) - - Myalgia - - - 2 (2.2%) 5 (4.5%) Pain in limb - - - - 3 (2.7%) Reproductive Testicular atrophy 6 (5.0%) - - 4 (4.4%)* 8 (7.2%)* Gynecomastia - - - 2 (2.2%)* 4 (3.6%)* Testicular pain - - - 2 (2.2%) - Psychiatric Decreased libido - - - 3 (3.3%)* - *Expected pharmacological consequences of testosterone suppression.
In the patient populations studied with ELIGARD® 7.5 mg, a total of 86 hot flashes/sweats adverse events were reported in 70 patients. Of these, 71 events (83%) were mild; 14 (16%) were moderate; 1 (1%) was severe.
In the patient population studied with ELIGARD® 22.5 mg, a total of 84 hot flashes/sweats adverse events were reported in 66 patients. Of these, 73 events (87%) were mild; 11 (13%) were moderate; none were severe.
In the patient population studied with ELIGARD® 30 mg, a total of 75 hot flash adverse events were reported in 66 patients. Of these, 57 events (76%) were mild; 16 (21%) were moderate; 2 (3%) were severe.
In the patient population studied with ELIGARD® 45 mg, a total of 89 hot flash adverse events were reported in 64 patients. Of these, 62 events (70%) were mild; 27 (30%) were moderate; none were severe.In addition, the following possibly or probably related systemic adverse events were reported by < 2% of the patients treated with ELIGARD® in these clinical studies.
Body system
Adverse event
General
Sweating, insomnia, syncope, rigors, weakness, lethargy
Gastrointestinal
Flatulence, constipation, dyspepsia
Hematologic
Decreased red blood cell count, hematocrit and hemoglobin
Metabolic
Weight gain
Musculoskeletal
Tremor, backache, joint pain, muscle atrophy, limb pain
Nervous
Disturbance of smell and taste, depression, vertigo
Psychiatric
Insomnia, depression, loss of libido*
Renal/urinary
Difficulties with urination, pain on urination, scanty urination, bladder spasm, blood in urine, urinary retention, urinary urgency, incontinence, nocturia, nocturia aggravated
Reproductive/
UrogenitalTesticular soreness/pain, impotence*, decreased libido*, gynecomastia*, breast soreness/tenderness*, testicular atrophy*, erectile dysfunction, penile disorder*, reduced penis size
Skin
Alopecia, clamminess, night sweats*, sweating increased*
Vascular
Hypertension, hypotension
* Expected pharmacological consequences of testosterone suppression.
Changes in Bone Density: Decreased bone density has been reported in the medical literature in men who have had orchiectomy or who have been treated with a GnRH agonist analog. It can be anticipated that long periods of medical castration in men will have effects on bone density.
6.2 Postmarketing Experience
Pituitary apoplexy-During post-marketing surveillance, rare cases of pituitary apoplexy (a clinical syndrome secondary to infarction of the pituitary gland) have been reported after the administration of gonadotropin-releasing hormone agonists. In a majority of these cases, a pituitary adenoma was diagnosed with a majority of pituitary apoplexy cases occurring within 2 weeks of the first dose, and some within the first hour. In these cases, pituitary apoplexy has presented as sudden headache, vomiting, visual changes, ophthalmoplegia, altered mental status, and sometimes cardiovascular collapse. Immediate medical attention has been required.
Nervous System-Convulsions
Respiratory System-Interstitial lung disease
- 7 DRUG INTERACTIONS
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Based on findings in animal studies and mechanism of action, ELIGARD® may cause fetal harm when administered to a pregnant woman [see Clinical Pharmacology (12.1)]. There are no available data in pregnant women to inform the drug-associated risk. Expected hormonal changes that occur with ELIGARD® treatment increase the risk for pregnancy loss. In animal developmental and reproductive studies, major fetal abnormalities were observed after administration of leuprolide acetate throughout gestation in rats. Advise pregnant patients and females of reproductive potential of the potential risk to the fetus (see Data).Animal Data
In animal developmental and reproductive studies, major fetal abnormalities were observed after administration of leuprolide acetate throughout gestation. There were increased fetal mortality and decreased fetal weights in rats and rabbits. The effects of fetal mortality are expected consequences of the alterations in hormonal levels brought about by this drug.8.2 Lactation
The safety and efficacy of ELIGARD® have not been established in females. There is no information regarding the presence of ELIGARD® in human milk, the effects on the breastfed child, or the effects on milk production. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in a breastfed child from ELIGARD®, a decision should be made to discontinue breastfeeding or discontinue the drug, taking into account the importance of the drug to the mother.
8.3 Females and Males of Reproductive Potential
Infertility
Males
Based on mechanism of action, ELIGARD® may impair fertility in males of reproductive potential [see Clinical Pharmacology (12.1)]. - 10 OVERDOSAGE
-
11 DESCRIPTION
ELIGARD® is a sterile polymeric matrix formulation of leuprolide acetate, a GnRH agonist, for subcutaneous injection. It is designed to deliver leuprolide acetate at a controlled rate over a one-, three-, four- or six-month therapeutic period.
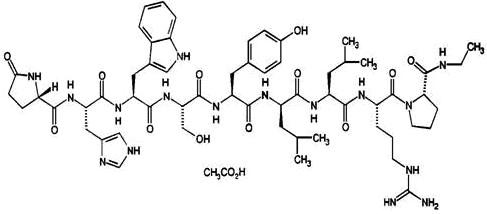
Leuprolide acetate is a synthetic nonapeptide analog of naturally occurring gonadotropin releasing hormone (GnRH) that, when given continuously, inhibits pituitary gonadotropin secretion and suppresses testicular and ovarian steroidogenesis. The analog possesses greater potency than the natural hormone. The chemical name is 5-oxo-L-prolyl-L-histidyl-L-tryptophyl-L-seryl-L-tyrosyl-D-leucyl-L-leucyl-L-arginyl-N-ethyl-L-prolinamide acetate (salt) with the following structural formula:
ELIGARD® is prefilled and supplied in two separate, sterile syringes whose contents are mixed immediately prior to administration. The two syringes are joined and the single dose product is mixed until it is homogenous. ELIGARD® is administered subcutaneously, where it forms a solid drug delivery depot.
One syringe contains the ATRIGEL® Delivery System and the other contains leuprolide acetate. ATRIGEL® is a polymeric (non-gelatin containing) delivery system consisting of a biodegradable poly (DL-lactide-co-glycolide) (PLGH or PLG) polymer formulation dissolved in a biocompatible solvent, N-methyl-2-pyrrolidone (NMP).
Refer to Table 6 for the delivery system composition and reconstituted product formulation for each ELIGARD® product.
Table 6. ELIGARD® Delivery System Composition and Reconstituted Product Formulation
ELIGARD®
7.5 mg
22.5 mg
30 mg
45 mg
ATRIGEL® Delivery System syringe
Polymer
PLGH
PLG
PLG
PLG
Polymer description
Copolymer containing carboxyl endgroups
Copolymer with hexanediol
Copolymer with hexanediol
Copolymer with hexanediol
Polymer DL-lactide to glycolide
molar ratio50:50
75:25
75:25
85:15
Reconstituted product
Polymer delivered
82.5 mg
158.6 mg
211.5 mg
165 mg
NMP delivered
160.0 mg
193.9 mg
258.5 mg
165 mg
Leuprolide acetate delivered
7.5 mg
22.5 mg
30 mg
45 mg
Approximate Leuprolide free
base equivalent7.0 mg
21 mg
28 mg
42 mg
Approximate administered formulation weight
250 mg
375 mg
500 mg
375 mg
Approximate injection volume
0.25 mL
0.375 mL
0.5 mL
0.375 mL -
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Leuprolide acetate, a gonadotropin releasing hormone (GnRH) agonist, acts as a potent inhibitor of gonadotropin secretion when given continuously in therapeutic doses. Animal and human studies indicate that after an initial stimulation, chronic administration of leuprolide acetate results in suppression of testicular and ovarian steroidogenesis. This effect is reversible upon discontinuation of drug therapy.
In humans, administration of leuprolide acetate results in an initial increase in circulating levels of luteinizing hormone (LH) and follicle stimulating hormone (FSH), leading to a transient increase in levels of the gonadal steroids (testosterone and dihydrotestosterone in males, and estrone and estradiol in premenopausal females). However, continuous administration of leuprolide acetate results in decreased levels of LH and FSH. In males, testosterone is reduced to below castrate threshold (≤50 ng/dL). These decreases occur within two to four weeks after initiation of treatment. Long-term studies have shown that continuation of therapy with leuprolide acetate maintains testosterone below the castrate level for up to seven years.
12.2 Pharmacodynamics
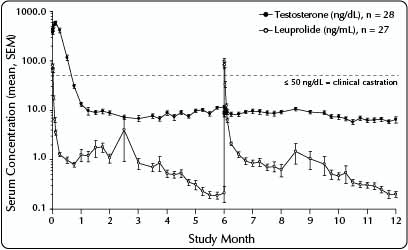
Following the first dose of ELIGARD®, mean serum testosterone concentrations transiently increased, then fell to below castrate threshold (≤ 50 ng/dL) within three weeks for all ELIGARD® concentrations.
Continued monthly treatment with ELIGARD® 7.5 mg maintained castrate testosterone suppression throughout the study. No breakthrough of testosterone concentrations above castrate threshold (> 50 ng/dL) occurred at any time during the study once castrate suppression was achieved (Figure 1).
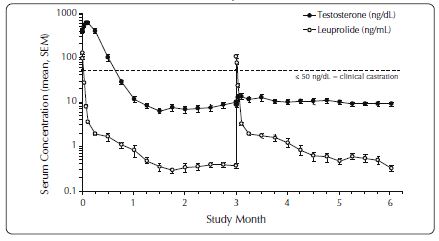
One patient received less than a full dose of ELIGARD® 22.5 mg at baseline, never suppressed and withdrew from the study at Day 73. Of the 116 patients remaining in the study, 115 (99%) had serum testosterone levels below the castrate threshold by Month 1 (Day 28). By Day 35, 116 (100%) had serum testosterone levels below the castrate threshold. Once testosterone suppression was achieved, one patient (< 1%) demonstrated breakthrough (concentrations > 50 ng/dL after achieving castrate levels) following the initial injection; that patient remained below the castrate threshold following the second injection (Figure 2).
One patient withdrew from the ELIGARD® 30 mg study at Day 14. Of the 89 patients remaining in the study, 85 (96%) had serum testosterone levels below the castrate threshold by Month 1 (Day 28). By Day 42, 89 (100%) of patients attained castrate testosterone suppression. Once castrate testosterone suppression was achieved, three patients (3%) demonstrated breakthrough (concentrations > 50 ng/dL after achieving castrate levels) (Figure 3).
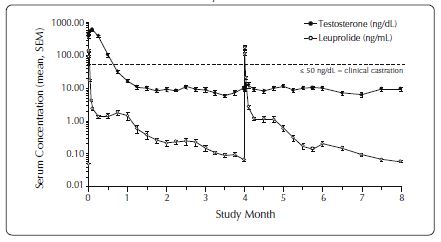
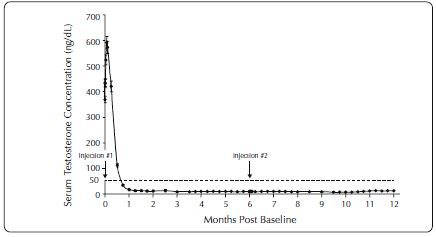
One patient at Day 1 and another patient at Day 29 were withdrawn from the ELIGARD® 45 mg study. Of the 109 patients remaining in the study, 108 (99.1%) had serum testosterone levels below the castrate threshold by Month 1 (Day 28). One patient did not achieve castrate suppression and was withdrawn from the study at Day 85. Once castrate testosterone suppression was achieved, one patient (< 1%) demonstrated breakthrough (concentrations > 50 ng/dL after achieving castrate levels) (Figure 4).
Leuprolide acetate is not active when given orally.
12.3 Pharmacokinetics
Absorption
ELIGARD® 7.5 mg
The pharmacokinetics/pharmacodynamics observed during three once-monthly injections in 20 patients with advanced prostate cancer is shown in Figure 1. Mean serum leuprolide concentrations following the initial injection rose to 25.3 ng/mL (Cmax) at approximately 5 hours after injection. After the initial increase following each injection, serum concentrations remained relatively constant (0.28 – 2.00 ng/mL).Figure 1. Pharmacokinetic/Pharmacodynamic Response (N=20) to ELIGARD® 7.5 mg – Patients Dosed Initially and at Months 1 and 2
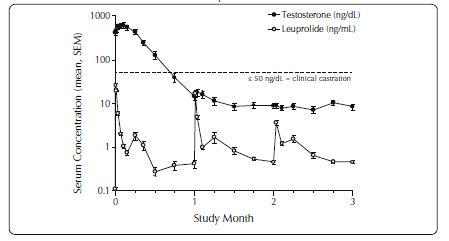
A reduced number of sampling time points resulted in the apparent decrease in Cmax values with the second and third doses of ELIGARD® 7.5 mg (Figure 1).
ELIGARD® 22.5 mg
The pharmacokinetics/pharmacodynamics observed during two injections every three months (ELIGARD® 22.5 mg) in 22 patients with advanced prostate cancer is shown in Figure 2. Mean serum leuprolide concentrations rose to 127 ng/mL and 107 ng/mL at approximately 5 hours following the initial and second injections, respectively. After the initial increase following each injection, serum concentrations remained relatively constant (0.2 – 2.0 ng/mL).Figure 2. Pharmacokinetic/Pharmacodynamic Response (N=22) to ELIGARD® 22.5 mg – Patients Dosed Initially and at Month 3
ELIGARD® 30 mg
The pharmacokinetics/pharmacodynamics observed during injections administered initially and at four months (ELIGARD® 30 mg) in 24 patients with advanced prostate cancer is shown in Figure 3. Mean serum leuprolide concentrations following the initial injection rose rapidly to 150 ng/mL (Cmax) at approximately 3.3 hours after injection. After the initial increase following each injection, mean serum concentrations remained relatively constant (0.1 – 1.0 ng/mL).Figure 3. Pharmacokinetic/Pharmacodynamic Response (N=24) to ELIGARD® 30 mg - Patients Dosed Initially and at Month 4
ELIGARD® 45 mg
The pharmacokinetics/pharmacodynamics observed during injections administered initially and at six months (ELIGARD® 45 mg) in 27 patients with advanced prostate cancer is shown in Figure 4. Mean serum leuprolide concentrations rose to 82 ng/mL and 102 ng/mL (Cmax) at approximately 4.5 hours following the initial and second injections, respectively. After the initial increase following each injection, mean serum concentrations remained relatively constant (0.2 – 2.0 ng/mL).Figure 4. Pharmacokinetic/Pharmacodynamic Response (N=27) to ELIGARD® 45 mg - Patients Dosed Initially and at Month 6
There was no evidence of significant accumulation during repeated dosing. Non-detectable leuprolide plasma concentrations have been occasionally observed during ELIGARD® administration, but testosterone levels were maintained at castrate levels.
Distribution. The mean steady-state volume of distribution of leuprolide following intravenous bolus administration to healthy male volunteers was 27 L. In vitro binding to human plasma proteins ranged from 43% to 49%.
Metabolism. In healthy male volunteers, a 1-mg bolus of leuprolide administered intravenously revealed that the mean systemic clearance was 8.34 L/h, with a terminal elimination half-life of approximately 3 hours based on a two compartment model.
No drug metabolism study was conducted with ELIGARD®. Upon administration with different leuprolide acetate formulations, the major metabolite of leuprolide acetate is a pentapeptide (M-1) metabolite.
Excretion. No drug excretion study was conducted with ELIGARD®.
Geriatrics. [see USE IN SPECIAL POPULATIONS (8.5)]
Race. In patients studied, mean serum leuprolide concentrations were similar regardless of race. Refer to Table 7 for distribution of study patients by race.
Table 7. Race Characterization of ELIGARD® Study Patients
Race
ELIGARD®
7.5 mgELIGARD®
22.5 mgELIGARD®
30 mgELIGARD®
45 mgWhite
26
19
18
17
Black
-
4
4
7
Hispanic
2
2
2
3
Renal and Hepatic Insufficiency. The pharmacokinetics of ELIGARD® in hepatically and renally impaired patients have not been determined.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Two-year carcinogenicity studies were conducted with leuprolide acetate in rats and mice. In rats, a dose-related increase of benign pituitary hyperplasia and benign pituitary adenomas was noted at 24 months when the drug was administered subcutaneously at high daily doses (0.6 to 4 mg/kg). There was a significant but not dose-related increase of pancreatic islet-cell adenomas in females and of testicular interstitial cell adenomas in males (highest incidence in the low dose group). In mice, no leuprolide acetate-induced tumors or pituitary abnormalities were observed at a dose as high as 60 mg/kg for two years. Patients have been treated with leuprolide acetate for up to three years with doses as high as 10 mg/day and for two years with doses as high as 20 mg/day without demonstrable pituitary abnormalities. No carcinogenicity studies have been conducted with ELIGARD®.
Mutagenicity studies have been performed with leuprolide acetate using bacterial and mammalian systems and with ELIGARD® 7.5 mg in bacterial systems. These studies provided no evidence of a mutagenic potential.
-
14 CLINICAL STUDIES
One open-label, multicenter study was conducted with each ELIGARD® formulation (7.5 mg, 22.5 mg, 30 mg, and 45 mg) in patients with Jewett stage A though D prostate cancer who were treated with at least a single injection of study drug (Table 8). These studies evaluated the achievement and maintenance of castrate serum testosterone suppression over the duration of therapy (Figures 5-8).
During the AGL9904 study using ELIGARD® 7.5 mg, once testosterone suppression was achieved, no patients (0%) demonstrated breakthrough (concentration > 50 ng/dL) at any time in the study.
During the AGL9909 study using ELIGARD® 22.5 mg, once testosterone suppression was achieved, only one patient (< 1%) demonstrated breakthrough following the initial injection; that patient remained below the castrate threshold following the second injection.
During the AGL0001 study using ELIGARD® 30 mg, once testosterone suppression was achieved, three patients (3%) demonstrated breakthrough. In the first of these patients, a single serum testosterone concentration of 53 ng/dL was reported on the day after the second injection. In this patient, castrate suppression was reported for all other time points. In the second patient, a serum testosterone concentration of 66 ng/dL was reported immediately prior to the second injection. This rose to a maximum concentration of 147 ng/dL on the second day after the second injection. In this patient, castrate suppression was again reached on the seventh day after the second injection and was maintained thereafter. In the final patient, serum testosterone concentrations > 50 ng/dL were reported at 2 and at 8 hours after the second injection. Serum testosterone concentration rose to a maximum of 110 ng/dL on the third day after the second injection. In this patient, castrate suppression was again reached eighteen days after the second injection and was maintained until the final day of the study, when a single serum testosterone concentration of 55 ng/dL was reported.
During the AGL0205 study using ELIGARD® 45 mg, once testosterone suppression was achieved, one patient (<1%) demonstrated breakthrough. This patient reached castrate suppression at Day 21 and remained suppressed until Day 308 when his testosterone level rose to 112 ng/dL. At Month 12 (Day 336), his testosterone was 210 ng/dL.
Table 8. Summary of ELIGARD® Clinical Studies
ELIGARD®
7.5 mg
22.5 mg
30 mg
45 mg
Study number
AGL9904
AGL9909
AGL0001
AGL0205
Total number of patients
120 (117 completed)
1172 (111 completed3)
90 (82 completed4)
111 (103 completed5)
Jewett stages
Stage A
‑
2
2
5
Stage B
‑
19
38
43
Stage C
89
60
16
19
Stage D
31
36
34
44
Treatment
6 monthly injections
1 injection (4 patients)
1 injection (5 patients)
1 injection
(5 patients)2 injections, one every three months (113 patients)
2 injections, one every four months (85 patients)
2 injections, one every six months (106 patients)
Duration of therapy
6 months
6 months
8 months
12 months
Mean testosterone concentration (ng/dL)
Baseline
361.3
367.1
385.5
367.7
Day 2
574.6 (Day 3)
588.0
610.0
588.6
Day 14
Below Baseline (Day 10)
Below Baseline
Below Baseline
Below Baseline
Day 28
21.8
27.7 (Day 21)
17.2
16.7
Conclusion
6.1
10.1
12.4
12.6
Number of patients below castrate threshold
(≤ 50 ng/dL)Day 28
112 of 119 (94.1%)
115 of 116 (99%)
85 of 89 (96%)
108 of 109 (99.1%)
Day 35
‑
116 (100%)
‑
‑
Day 42
119 (100%)
‑
89 (100%)
‑
Conclusion
1171 (100%)
111 (100%)
81 (99%)
102 (99%)
- Two patients withdrew for reasons unrelated to drug.
- One patient received less than a full dose at Baseline, never suppressed, and was withdrawn at Day 73 and given an alternate treatment.
- All non-evaluable patients who attained castration by Day 28 maintained castration at each time point up to and including the time of withdrawal.
- One patient withdrew on Day 14. All 7 non-evaluable patients who had achieved castration by Day 28 maintained castration at each time point, up to and including the time of withdrawal.
- Two patients were withdrawn prior to the Month 1 blood draw. One patient did not achieve castration and was withdrawn on Day 85. All 5 non-evaluable patients who attained castration by Day 28, maintained castration at each time point up to and including the time of withdrawal.
Figure 5. ELIGARD® 7.5 mg Mean Serum Testosterone Concentrations (n=117)
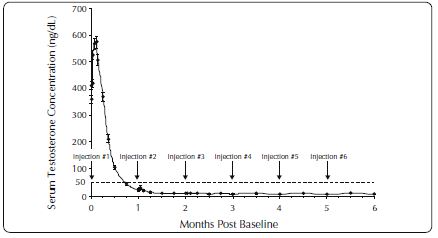
Figure 6. ELIGARD® 22.5 mg Mean Serum Testosterone Concentrations (n=111)
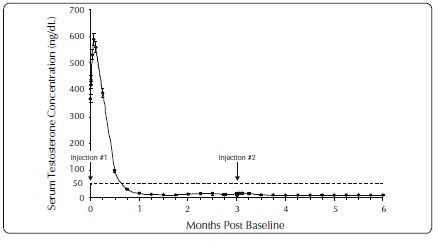
Figure 7. ELIGARD® 30 mg Mean Serum Testosterone Concentrations (n=90)
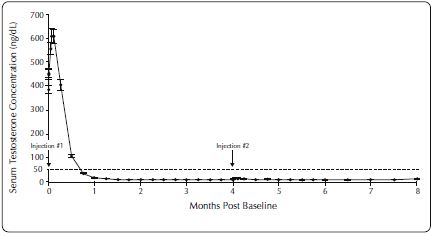
Figure 8. ELIGARD® 45 mg Mean Serum Testosterone Concentrations (n=103)
Serum PSA decreased in all patients in all studies whose Baseline values were elevated above the normal limit. Refer to Table 9 for a summary of the effectiveness of ELIGARD® in reducing serum PSA values.
Table 9. Effect of ELIGARD® on Patient Serum PSA Values
ELIGARD®
7.5 mg 22.5 mg 30 mg 45 mg Mean PSA reduction at study conclusion
94% 98% 86% 97% Patients with normal PSA at study conclusion*
94% 91% 93% 95% *Among patients who presented with elevated levels at Baseline
Other secondary efficacy endpoints evaluated included WHO performance status, bone pain, urinary pain and urinary signs and symptoms. Refer to Table 10 for a summary of these endpoints.
Table 10. Secondary Efficacy Endpoints
ELIGARD® 7.5 mg 22.5 mg 30 mg 45 mg Baseline
WHO Status = 01
88%
94%
90%
90%
WHO Status = 12 11%
6% 10% 7% WHO Status = 23 - - - 3% Mean bone pain4
(range)1.22 (1-9)
1.20 (1-9)
1.20 (1-7)
1.38 (1-7)
Mean urinary pain (range)
1.12 (1-5)
1.02 (1-2)
1.01 (1-2)
1.22 (1-8)
Mean urinary signs and symptoms (range)
Low
1.09 (1-4)
Low
Low
Number of patients with prostate abnormalities
102 (85%)
96 (82%)
66 (73%)
89 (80%)
Month 6
Month 6
Month 8
Month 12
Follow-up
WHO status = 0
Unchanged
96%
87%
94%
WHO status = 1
Unchanged
4%
12%
5%
WHO status = 2
- - 1% 1%
Mean bone pain (range)
1.26 (1-7)
1.22 (1-5)
1.19 (1-8)
1.31 (1-8)
Mean urinary pain (range)
1.07 (1-8)
1.10 (1-8)
1.00 (1-1)
1.07 (1-5)
Mean urinary signs and symptoms (range)
Modestly decreased
1.18 (1-7)
Modestly decreased
Modestly decreased
Number of patients with prostate abnormalities
77 (64%)
76 (65%)
54 (60%)
60 (58%)
-
WHO status = 0 classified as “fully active.”
-
WHO status = 1 classified as “restricted in strenuous activity but ambulatory and able to carry out work of a light or sedentary nature.”
-
WHO status = 2 classified as “ambulatory but unable to carry out work activities.”
-
Pain score scale: 1 (no pain) to 10 (worst pain possible).
- 15 REFERENCES
-
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
ELIGARD® is available in a single-dose kit of a two syringe-mixing system with a sterile safety needle in the following strengths:
ELIGARD® 7.5 mg – NDC: 62935-753-75
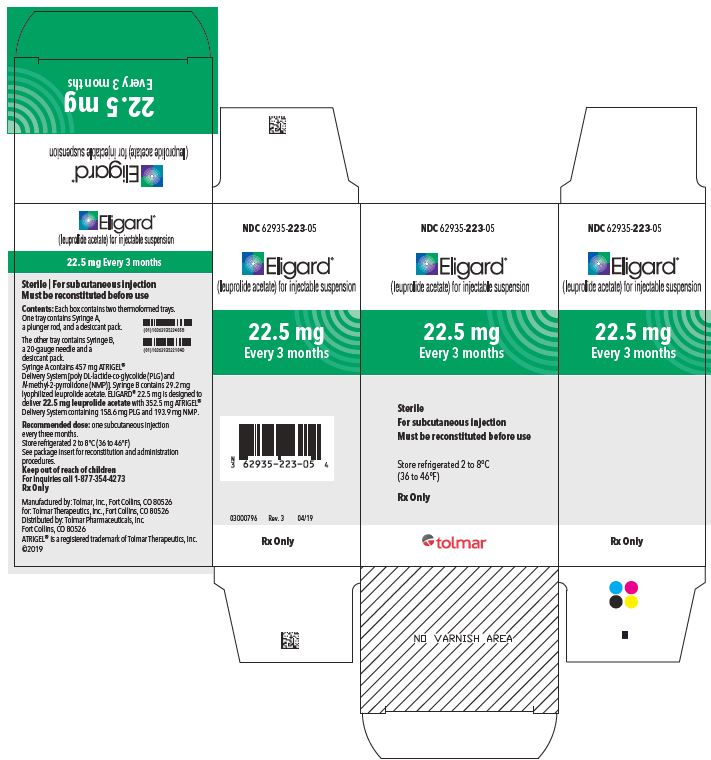
ELIGARD® 22.5 mg – NDC: 62935-223-05
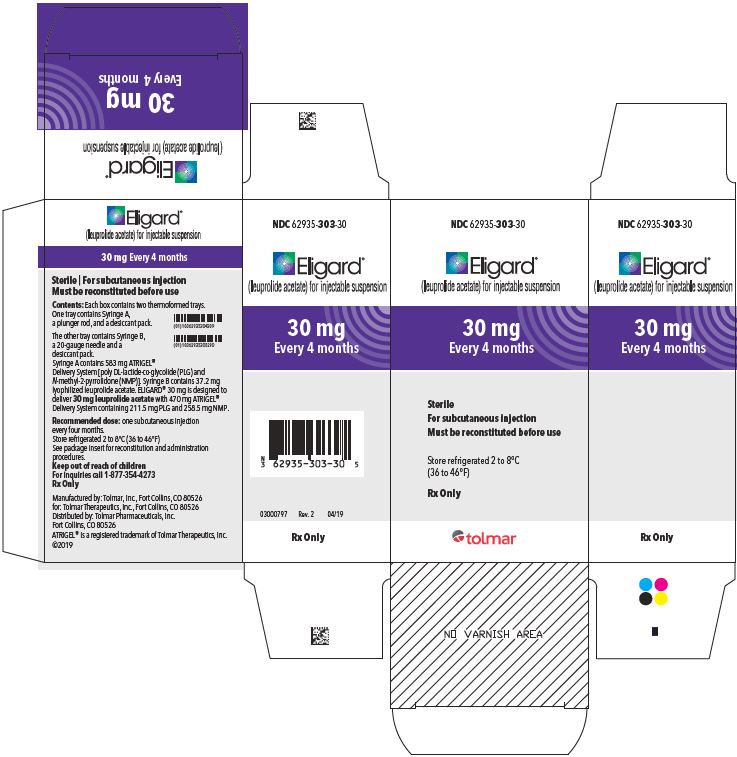
ELIGARD® 30 mg – NDC: 62935-303-30
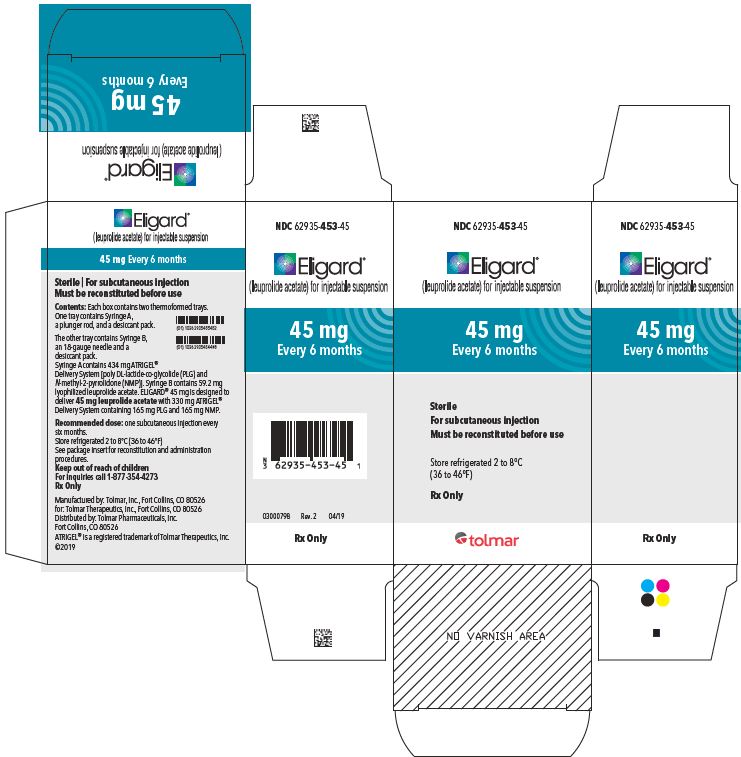
ELIGARD® 45 mg – NDC: 62935-453-45 -
17 PATIENT COUNSELING INFORMATION
Hypersensitivity
- Inform patients that if they have experienced hypersensitivity with other GnRH agonist drugs like ELIGARD®, ELIGARD® is contraindicated [see Contraindications (4)].
Tumor Flare
- Inform patients that ELIGARD® can cause tumor flare during the first weeks of treatment. Inform patients that the increase in testosterone can cause an increase in urinary symptoms or pain. Advise patients to contact their healthcare provider if uretral obstruction, spinal cord compression, paralysis, or new or worsened symptoms occur after beginning ELIGARD® treatment [see Warnings and Precautions (5.1)].
Hyperglycemia and Diabetes
- Advise patients that there is an increased risk of hyperglycemia and diabetes with ELIGARD® therapy. Inform patients that periodic monitoring for hyperglycemia and diabetes is required when being treated with ELIGARD® [see Warnings and Precautions (5.3)].
Cardiovascular Disease
- Inform patients that there is an increased risk of myocardial infarction, sudden cardiac death, and stroke with ELIGARD® treatment. Advise patients to immediately report signs and symptoms associated with these events to their healthcare provider for evaluation [see Warnings and Precautions (5.4)].
Injection Site Reactions
- Inform patients that injection site related adverse reactions may occur such as transient burning/stinging, pain, bruising, and redness. Advise patients to contact their healthcare provider if they experience rash or severe injection site reactions [see Adverse Reactions (6.1)].
Urogenital Disorders
- Advise patients that ELIGARD® may cause impotence.
Infertility
- Inform patients that ELIGARD® may cause infertility [see Use In Specific Populations (8.3)].
Rx only
Revised 04/2019
Manufactured by: Tolmar, Inc.
Fort Collins, CO 80526
for: Tolmar Therapeutics, Inc.
Fort Collins, CO 80526Distributed by: Tolmar Pharmaceuticals, Inc.
Fort Collins, CO 80526©2019 Tolmar Pharmaceuticals, Inc.
04005921 Rev. 4 04/19
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
- 7.5 mg carton
- 22.5 mg carton
- 30 mg carton
- 45 mg carton
-
INGREDIENTS AND APPEARANCE
ELIGARD
leuprolide acetate kitProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 62935-753 Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 62935-753-75 1 in 1 CARTON; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) 05/15/2002 Quantity of Parts Part # Package Quantity Total Product Quantity Part 1 1 SYRINGE 0.25 mL Part 2 1 SYRINGE 0.25 mL Part 1 of 2 LEUPROLIDE ACETATE
leuprolide acetate injection, suspension, extended releaseProduct Information Item Code (Source) NDC: 62935-754 Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LEUPROLIDE ACETATE (UNII: 37JNS02E7V) (LEUPROLIDE - UNII:EFY6W0M8TG) LEUPROLIDE ACETATE 7.5 mg in 0.25 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 62935-754-74 0.25 mL in 1 SYRINGE; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA021343 Part 2 of 2 ATRIGEL
atrigel suspension, extended releaseProduct Information Item Code (Source) NDC: 62935-755 Route of Administration SUBCUTANEOUS Inactive Ingredients Ingredient Name Strength METHYL PYRROLIDONE (UNII: JR9CE63FPM) 160 mg in 0.25 mL POLY(DL-LACTIC-CO-GLYCOLIC ACID), (50:50; 46000 MW) (UNII: LQ35R50VR1) 82.5 mg in 0.25 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 62935-755-75 0.25 mL in 1 SYRINGE; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA021343 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA021343 05/15/2002 ELIGARD
leuprolide acetate kitProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 62935-223 Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 62935-223-05 1 in 1 CARTON; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) 08/26/2002 Quantity of Parts Part # Package Quantity Total Product Quantity Part 1 1 SYRINGE 0.375 mL Part 2 1 SYRINGE 0.375 mL Part 1 of 2 LEUPROLIDE ACETATE
leuprolide acetate injection, suspension, extended releaseProduct Information Item Code (Source) NDC: 62935-221 Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LEUPROLIDE ACETATE (UNII: 37JNS02E7V) (LEUPROLIDE - UNII:EFY6W0M8TG) LEUPROLIDE ACETATE 22.5 mg in 0.375 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 62935-221-04 0.375 mL in 1 SYRINGE; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA021379 Part 2 of 2 ATRIGEL
atrigel suspension, extended releaseProduct Information Item Code (Source) NDC: 62935-224 Route of Administration SUBCUTANEOUS Inactive Ingredients Ingredient Name Strength METHYL PYRROLIDONE (UNII: JR9CE63FPM) 193.9 mg in 0.375 mL POLY(DL-LACTIC-CO-GLYCOLIC ACID), (75:25; 20000 MW) (UNII: 58X445TH30) 158.6 mg in 0.375 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 62935-224-05 0.375 mL in 1 SYRINGE; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA021379 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA021379 08/26/2002 ELIGARD
leuprolide acetate kitProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 62935-303 Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 62935-303-30 1 in 1 CARTON; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) 02/26/2003 Quantity of Parts Part # Package Quantity Total Product Quantity Part 1 1 SYRINGE 0.5 mL Part 2 1 SYRINGE 0.5 mL Part 1 of 2 LEUPROLIDE ACETATE
leuprolide acetate injection, suspension, extended releaseProduct Information Item Code (Source) NDC: 62935-305 Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LEUPROLIDE ACETATE (UNII: 37JNS02E7V) (LEUPROLIDE - UNII:EFY6W0M8TG) LEUPROLIDE ACETATE 30 mg in 0.5 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 62935-305-29 0.5 mL in 1 SYRINGE; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA021488 Part 2 of 2 ATRIGEL
atrigel suspension, extended releaseProduct Information Item Code (Source) NDC: 62935-304 Route of Administration SUBCUTANEOUS Inactive Ingredients Ingredient Name Strength METHYL PYRROLIDONE (UNII: JR9CE63FPM) 258.5 mg in 0.5 mL POLY(DL-LACTIC-CO-GLYCOLIC ACID), (75:25; 20000 MW) (UNII: 58X445TH30) 211.5 mg in 0.5 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 62935-304-30 0.5 mL in 1 SYRINGE; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA021488 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA021488 02/26/2003 ELIGARD
leuprolide acetate kitProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 62935-453 Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 62935-453-45 1 in 1 CARTON; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) 01/07/2005 Quantity of Parts Part # Package Quantity Total Product Quantity Part 1 1 SYRINGE 0.375 mL Part 2 1 SYRINGE 0.375 mL Part 1 of 2 LEUPROLIDE ACETATE
leuprolide acetate injection, suspension, extended releaseProduct Information Item Code (Source) NDC: 62935-454 Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LEUPROLIDE ACETATE (UNII: 37JNS02E7V) (LEUPROLIDE - UNII:EFY6W0M8TG) LEUPROLIDE ACETATE 45 mg in 0.375 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 62935-454-44 0.375 mL in 1 SYRINGE; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA021731 Part 2 of 2 ATRIGEL
atrigel suspension, extended releaseProduct Information Item Code (Source) NDC: 62935-455 Route of Administration SUBCUTANEOUS Inactive Ingredients Ingredient Name Strength METHYL PYRROLIDONE (UNII: JR9CE63FPM) 165 mg in 0.375 mL POLY(DL-LACTIC-CO-GLYCOLIC ACID), (85:15; 23000 MW) (UNII: 93PPD1S477) 165 mg in 0.375 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 62935-455-45 0.375 mL in 1 SYRINGE; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA021731 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA021731 01/07/2005 Labeler - TOLMAR PHARMACEUTICALS INC. (079303122) Establishment Name Address ID/FEI Business Operations Bachem AG 482220311 API MANUFACTURE(62935-754, 62935-221, 62935-305, 62935-454) Establishment Name Address ID/FEI Business Operations Cangene BioPharma, LLC 050783398 ANALYSIS(62935-754, 62935-221, 62935-305, 62935-454) , MANUFACTURE(62935-754, 62935-221, 62935-305, 62935-454) Establishment Name Address ID/FEI Business Operations Isomedix Operations Inc 144785870 STERILIZE(62935-755, 62935-224, 62935-304, 62935-455) Establishment Name Address ID/FEI Business Operations TOLMAR 1201 Cornerstone LLC 079112310 ANALYSIS(62935-223, 62935-221, 62935-224, 62935-303, 62935-305, 62935-304, 62935-453, 62935-454, 62935-455) , LABEL(62935-221, 62935-305, 62935-454) , MANUFACTURE(62935-221, 62935-305, 62935-454) Establishment Name Address ID/FEI Business Operations TOLMAR 1413 ACQUISITION, LLC 832366970 LABEL(62935-753, 62935-754, 62935-755, 62935-223, 62935-221, 62935-224, 62935-303, 62935-305, 62935-304, 62935-453, 62935-454, 62935-455) , MANUFACTURE(62935-755, 62935-224, 62935-304, 62935-455) , PACK(62935-753, 62935-754, 62935-755, 62935-223, 62935-221, 62935-224, 62935-303, 62935-305, 62935-304, 62935-453, 62935-454, 62935-455) Establishment Name Address ID/FEI Business Operations TOLMAR Inc. 791156578 ANALYSIS(62935-753, 62935-754, 62935-755, 62935-223, 62935-221, 62935-224, 62935-303, 62935-305, 62935-304, 62935-453, 62935-454, 62935-455) , LABEL(62935-753, 62935-754, 62935-755, 62935-223, 62935-221, 62935-224, 62935-303, 62935-305, 62935-304, 62935-453, 62935-454, 62935-455) , MANUFACTURE(62935-753, 62935-754, 62935-755, 62935-223, 62935-221, 62935-224, 62935-303, 62935-305, 62935-304, 62935-453, 62935-454, 62935-455) , PACK(62935-753, 62935-754, 62935-755, 62935-223, 62935-221, 62935-224, 62935-303, 62935-305, 62935-304, 62935-453, 62935-454, 62935-455)
Trademark Results [ELIGARD]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 ELIGARD 90593589 not registered Live/Pending |
Tolmar Therapeutics, Inc. 2021-03-22 |
 ELIGARD 76331615 2645629 Live/Registered |
TOLMAR THERAPEUTICS, INC. 2001-10-30 |
 ELIGARD 75128282 2115522 Dead/Cancelled |
Synthelabo 1996-07-01 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.