Adenosine by Hikma Pharmaceuticals USA Inc. / BAXTER PHARMACEUTICAL SOLUTIONS, LLC ADENOSINE injection
Adenosine by
Drug Labeling and Warnings
Adenosine by is a Prescription medication manufactured, distributed, or labeled by Hikma Pharmaceuticals USA Inc., BAXTER PHARMACEUTICAL SOLUTIONS, LLC. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
- SPL UNCLASSIFIED SECTION
-
DESCRIPTION
Adenosine is an endogenous nucleoside occurring in all cells of the body. It is chemically 6-amino-9-ß-D-ribofuranosyl-9-H-purine and has the following structural formula:
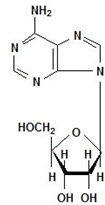
C10H13N5O4 267.24
Adenosine is a white crystalline powder. It is soluble in water and practically insoluble in alcohol. Solubility increases by warming and lowering the pH. Adenosine is not chemically related to other antiarrhythmic drugs. Adenosine injection is a sterile, nonpyrogenic solution for rapid bolus intravenous injection. Each mL contains 3 mg adenosine and 9 mg sodium chloride in Water for Injection. The pH of the solution is between 4.5 and 7.5.
-
CLINICAL PHARMACOLOGY
Mechanism of Action
Adenosine slows conduction time through the A-V node, can interrupt the reentry pathways through the A-V node, and can restore normal sinus rhythm in patients with paroxysmal supraventricular tachycardia (PSVT), including PSVT associated with Wolff-Parkinson-White Syndrome.
Adenosine is antagonized competitively by methylxanthines such as caffeine and theophylline, and potentiated by blockers of nucleoside transport such as dipyridamole. Adenosine is not blocked by atropine.
Hemodynamics
The intravenous bolus dose of 6 or 12 mg adenosine usually has no systemic hemodynamic effects. When larger doses are given by infusion, adenosine decreases blood pressure by decreasing peripheral resistance.
Pharmacokinetics
Intravenously administered adenosine is rapidly cleared from the circulation via cellular uptake, primarily by erythrocytes and vascular endothelial cells. This process involves a specific transmembrane nucleoside carrier system that is reversible, nonconcentrative, and bidirectionally symmetrical. Intracellular adenosine is rapidly metabolized either via phosphorylation to adenosine monophosphate by adenosine kinase, or via deamination to inosine by adenosine deaminase in the cytosol. Since adenosine kinase has a lower Km and Vmax than adenosine deaminase, deamination plays a significant role only when cytosolic adenosine saturates the phosphorylation pathway. Inosine formed by deamination of adenosine can leave the cell intact or can be degraded to hypoxanthine, xanthine, and ultimately uric acid. Adenosine monophosphate formed by phosphorylation of adenosine is incorporated into the high-energy phosphate pool. While extracellular adenosine is primarily cleared by cellular uptake with a half-life of less than 10 seconds in whole blood, excessive amounts may be deaminated by an ecto-form of adenosine deaminase. As adenosine requires no hepatic or renal function for its activation or inactivation, hepatic and renal failure would not be expected to alter its effectiveness or tolerability.
Clinical Trial Results
In controlled studies in the United States, bolus doses of 3, 6, 9, and 12 mg were studied. A cumulative 60% of patients with paroxysmal supraventricular tachycardia had converted to normal sinus rhythm within one minute after an intravenous bolus dose of 6 mg Adenosine (some converted on 3 mg and failures were given 6 mg), and a cumulative 92% converted after a bolus dose of 12 mg. Seven to sixteen percent of patients converted after 1-4 placebo bolus injections. Similar responses were seen in a variety of patient subsets, including those using or not using digoxin, those with Wolff-Parkinson-White Syndrome, males, females, blacks, Caucasians, and Hispanics.
Adenosine is not effective in converting rhythms other than PSVT, such as atrial flutter, atrial fibrillation, or ventricular tachycardia, to normal sinus rhythm.
-
INDICATIONS AND USAGE
Intravenous adenosine injection is indicated for the following:
Conversion to sinus rhythm of paroxysmal supraventricular tachycardia (PSVT), including that associated with accessory bypass tracts (Wolff-Parkinson-White Syndrome). When clinically advisable, appropriate vagal maneuvers (e.g., Valsalva maneuver), should be attempted prior to adenosine administration.
It is important to be sure the adenosine solution actually reaches the systemic circulation (see DOSAGE AND ADMINISTRATION).
Adenosine does not convert atrial flutter, atrial fibrillation, or ventricular tachycardia to normal sinus rhythm. In the presence of atrial flutter or atrial fibrillation, a transient modest slowing of ventricular response may occur immediately following adenosine administration.
-
CONTRAINDICATIONS
Intravenous adenosine injection is contraindicated in:
- Second- or third-degree A-V block (except in patients with a functioning artificial pacemaker).
- Sinus node disease, such as sick sinus syndrome or symptomatic bradycardia (except in patients with a functioning artificial pacemaker).
- Known hypersensitivity to adenosine.
-
WARNINGS
Heart Block
Adenosine injection exerts its effect by decreasing conduction through the A-V node and may produce a short lasting first-, second- or third-degree heart block. Appropriate therapy should be instituted as needed. Patients who develop high-level block on one dose of adenosine should not be given additional doses. Because of the very short half-life of adenosine, these effects are generally self-limiting. Appropriate resuscitative measures should be available.
Transient or prolonged episodes of asystole have been reported with fatal outcomes in some cases. Rarely, ventricular fibrillation has been reported following adenosine administration, including both resuscitated and fatal events. In most instances, these cases were associated with the concomitant use of digoxin and, less frequently with digoxin and verapamil. Although no causal relationship or drug-drug interaction has been established, adenosine should be used with caution in patients receiving digoxin or digoxin and verapamil in combination.
Arrhythmias at Time of Conversion
At the time of conversion to normal sinus rhythm, a variety of new rhythms may appear on the electrocardiogram. They generally last only a few seconds without intervention, and may take the form of premature ventricular contractions, atrial premature contractions, atrial fibrillation, sinus bradycardia, sinus tachycardia, skipped beats, and varying degrees of A-V nodal block. Such findings were seen in 55% of patients.
Bronchoconstriction
Adenosine is a respiratory stimulant (probably through activation of carotid body chemoreceptors) and intravenous administration in man has been shown to increase minute ventilation (Ve) and reduce arterial PCO2 causing respiratory alkalosis.
Adenosine administered by inhalation has been reported to cause bronchoconstriction in asthmatic patients, presumably due to mast cell degranulation and histamine release. These effects have not been observed in normal subjects. Adenosine has been administered to a limited number of patients with asthma and mild to moderate exacerbation of their symptoms has been reported. Respiratory compromise has occurred during adenosine infusion in patients with obstructive pulmonary disease. Adenosine should be used with caution in patients with obstructive lung disease not associated with bronchoconstriction (e.g., emphysema, bronchitis, etc.) and should be avoided in patients with bronchoconstriction or bronchospasm (e.g., asthma). Adenosine should be discontinued in any patient who develops severe respiratory difficulties.
-
PRECAUTIONS
Drug Interactions
Intravenous adenosine has been effectively administered in the presence of other cardioactive drugs, such as quinidine, beta-adrenergic blocking agents, calcium channel blocking agents, and angiotensin converting enzyme inhibitors, without any change in the adverse reaction profile. Digoxin and verapamil use may be rarely associated with ventricular fibrillation when combined with adenosine (see WARNINGS). Because of the potential for additive or synergistic depressant effects on the SA and AV nodes, however, adenosine should be used with caution in the presence of these agents. The use of adenosine in patients receiving digitalis may be rarely associated with ventricular fibrillation (see WARNINGS).
The effects of adenosine are antagonized by methylxanthines such as caffeine and theophylline. In the presence of these methylxanthines, larger doses of adenosine may be required or adenosine may not be effective. Adenosine effects are potentiated by dipyridamole. Thus, smaller doses of adenosine may be effective in the presence of dipyridamole. Carbamazepine has been reported to increase the degree of heart block produced by other agents. As the primary effect of adenosine is to decrease conduction through the A-V node, higher degrees of heart block may be produced in the presence of carbamazepine.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Studies in animals have not been performed to evaluate the carcinogenic potential of adenosine. Adenosine was negative for genotoxic potential in the Salmonella (Ames Test) and Mammalian Microsome Assay.
Adenosine, however, like other nucleosides at millimolar concentrations present for several doubling times of cells in culture, is known to produce a variety of chromosomal alterations. Fertility studies in animals have not been conducted with adenosine.
Pregnancy Category C
Animal reproduction studies have not been conducted with adenosine; nor have studies been performed in pregnant women. As adenosine is a naturally occurring material, widely dispersed throughout the body, no fetal effects would be anticipated. However, since it is not known whether adenosine can cause fetal harm when administered to pregnant women, adenosine should be used during pregnancy only if clearly needed.
Pediatric Use
No controlled studies have been conducted in pediatric patients to establish the safety and efficacy of adenosine for the conversion of paroxysmal supraventricular tachycardia (PSVT). However, intravenous adenosine has been used for the treatment of PSVT in neonates, infants, children and adolescents (see DOSAGE AND ADMINISTRATION).1
Geriatric Use
Clinical studies of adenosine did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between elderly and younger patients. In general, adenosine in geriatric patients should be used with caution since this population may have a diminished cardiac function, nodal dysfunction, concomitant diseases or drug therapy that may alter hemodynamic function and produce severe bradycardia or AV block.
-
ADVERSE REACTIONS
The following reactions were reported with intravenous adenosine used in controlled U.S. clinical trials. The placebo group had a less than 1% rate of all of these reactions.
Cardiovascular
Facial flushing (18%), headache (2%), sweating, palpitations, chest pain, hypotension (less than 1%).
Respiratory
Shortness of breath/dyspnea (12%), chest pressure (7%), hyperventilation, head pressure (less than 1%).
Central Nervous
SystemLightheadedness (2%), dizziness, tingling in arms, numbness (1%), apprehension, blurred vision, burning sensation, heaviness in arms, neck and back pain (less than 1%).
Gastrointestinal
Nausea (3%), metallic taste, tightness in throat, pressure in groin (less than 1%).
Post Marketing Experience
(see WARNINGS)
The following adverse events have been reported from marketing experience with adenosine. Because these events are reported voluntarily from a population of uncertain size, are associated with concomitant diseases and multiple drug therapies and surgical procedures, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. Decisions to include these events in labeling are typically based on one or more of the following factors: (1) seriousness of the event, (2) frequency of the reporting, (3) strength of causal connection to the drug, or a combination of these factors.
-
OVERDOSAGE
The half-life of adenosine injection is less than 10 seconds. Thus, adverse effects are generally rapidly self-limiting. Treatment of any prolonged adverse effects should be individualized and be directed toward the specific effect. Methylxanthines, such as caffeine and theophylline, are competitive antagonists of adenosine.
-
DOSAGE AND ADMINISTRATION
For rapid bolus intravenous use only.
Adenosine injection should be given as a rapid bolus by the peripheral intravenous route. To be certain the solution reaches the systemic circulation, it should be administered either directly into a vein or, if given into an IV line, it should be given as close to the patient as possible and followed by a rapid saline flush.
Adult Patients
The dose recommendation is based on clinical studies with peripheral venous bolus dosing. Central venous (CVP or other) administration of adenosine has not been systematically studied.
The recommended intravenous doses for adults are as follows:
Initial dose: 6 mg given as a rapid intravenous bolus (administered over a 1 to 2 second period).
Repeat administration: If the first dose does not result in elimination of the supraventricular tachycardia within 1 to 2 minutes, 12 mg should be given as a rapid intravenous bolus. This 12 mg dose may be repeated a second time if required.
Pediatric Patients
The dosages used in neonates, infants, children and adolescents were equivalent to those administered to adults on a weight basis.
Pediatric Patients with a Body Weight < 50 kg:
Initial dose: Give 0.05 to 0.1 mg/kg as a rapid IV bolus given either centrally or peripherally. A saline flush should follow.
Repeat administration: If conversion of PSVT does not occur within 1 to 2 minutes, additional bolus injections of adenosine can be administered at incrementally higher doses, increasing the amount given by 0.05 to 0.1 mg/kg. Follow each bolus with a saline flush. This process should continue until sinus rhythm is established or a maximum single dose of 0.3 mg/kg is used.
Pediatric Patients with a Body Weight > 50 kg:
Administer the adult dose.
Doses greater than 12 mg are not recommended for adult and pediatric patients.
NOTE: Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration.
-
HOW SUPPLIED
Adenosine Injection, USP is supplied as a sterile, nonpyrogenic solution in normal saline.
NDC: 0641-6113-10 6 mg/2 mL (3 mg/mL) in 2 mL flip-top vials, packaged in shelf packs of ten.
Storage
Store at 20°-25°C (68°-77°F), excursions permitted to 15°-30°C (59°-86°F). [See USP Controlled Room Temperature.]
DO NOT REFRIGERATE as crystallization may occur. If crystallization has occurred, dissolve crystals by warming to room temperature. The solution must be clear at the time of use.
Contains no preservatives. Discard unused portion.
To report SUSPECTED ADVERSE REACTIONS, contact West-Ward Pharmaceutical Corp. at 1-877-845-0689, or the FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
For Product Inquiry call 1-877-845-0689.
- REFERENCE
- SPL UNCLASSIFIED SECTION
-
PRINCIPAL DISPLAY PANEL
Adenosine Injection, USP
6 mg/2 mL
(3 mg/mL)
2 mL Single Dose Vial
NDC: 0641-6113-01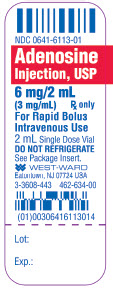
Adenosine Injection, USP
6 mg/2 mL
(3 mg/mL)
10 x 2 mL Single Dose Vials
NDC: 0641-6113-10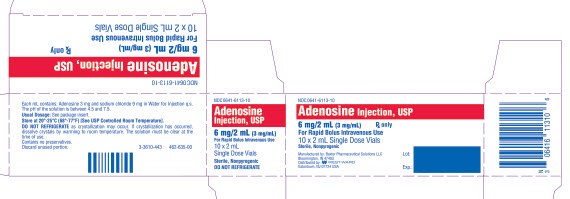
-
INGREDIENTS AND APPEARANCE
ADENOSINE
adenosine injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0641-6113 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ADENOSINE (UNII: K72T3FS567) (ADENOSINE - UNII:K72T3FS567) ADENOSINE 3 mg in 1 mL Inactive Ingredients Ingredient Name Strength SODIUM CHLORIDE (UNII: 451W47IQ8X) 9 mg in 1 mL WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0641-6113-10 10 in 1 CARTON 06/16/2004 1 NDC: 0641-6113-01 2 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA076500 06/16/2004 Labeler - Hikma Pharmaceuticals USA Inc. (946499746) Establishment Name Address ID/FEI Business Operations BAXTER PHARMACEUTICAL SOLUTIONS, LLC 604719430 ANALYSIS(0641-6113) , LABEL(0641-6113) , MANUFACTURE(0641-6113) , PACK(0641-6113) , STERILIZE(0641-6113)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.
