SULFAMETHOXAZOLE AND TRIMETHOPRIM injection, solution, concentrate
Sulfamethoxazole and Trimethoprim by
Drug Labeling and Warnings
Sulfamethoxazole and Trimethoprim by is a Prescription medication manufactured, distributed, or labeled by Teva Parenteral Medicines, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
SPL UNCLASSIFIED SECTION
Rx only
To reduce the development of drug-resistant bacteria and maintain the effectiveness of sulfamethoxazole and trimethoprim injection and other antibacterial drugs, sulfamethoxazole and trimethoprim injection should be used only to treat or prevent infections that are proven or strongly suspected to be caused by bacteria.
-
DESCRIPTION
Sulfamethoxazole and Trimethoprim Injection USP, a sterile solution for intravenous infusion only, is a synthetic antibacterial combination product. Each mL contains: sulfamethoxazole, USP 80 mg; trimethoprim, USP 16 mg; benzyl alcohol 10 mg (1.0% v/v and 1.0% w/v) as a preservative; diethanolamine 3 mg (0.3% v/v and 0.3% w/v); ethyl alcohol 100 mg (12.3% v/v and 10.0% w/v); propylene glycol 400 mg (38.6% v/v and 40.0% w/v); sodium metabisulfite 1 mg as an antioxidant; water for injection q.s.; air replaced with nitrogen; pH adjusted with sodium hydroxide and/or hydrochloric acid if necessary. pH: 9.5 to 10.5.
Sulfamethoxazole, USP is N1-(5-methyl-3-isoxazolyl)sulfanilamide. It is an almost white, odorless, tasteless compound with the following structural formula:
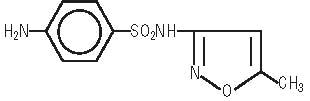
C10H11N3O3S M.W. 253.28
Trimethoprim, USP is 2,4-diamino-5-(3,4,5-trimethoxybenzyl)pyrimidine. It is a white to light yellow, odorless, bitter compound with the following structural formula:
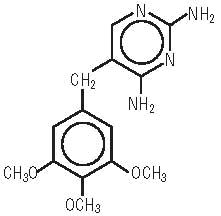
C14H18N4O3 M.W. 290.3
-
CLINICAL PHARMACOLOGY
Following a 1 hour intravenous infusion of a single dose of 800 mg sulfamethoxazole and 160 mg trimethoprim to 11 patients whose weight ranged from 105 lbs to 165 lbs (mean, 143 lbs) the peak plasma concentrations of sulfamethoxazole and trimethoprim were 46.3 ± 2.7 mcg/mL and 3.4 ± 0.3 mcg/mL, respectively. Following repeated intravenous administration of the same dose at 8 hour intervals, the mean plasma concentrations just prior to and immediately after each infusion at steady state were 70.6 ± 7.3 mcg/mL and 105.6 ± 10.9 mcg/mL for sulfamethoxazole and 5.6 ± 0.6 mcg/mL and 8.8 ± 0.9 mcg/mL for trimethoprim. The mean plasma half-life was 12.8 ± 1.8 hours for sulfamethoxazole and 11.3 ± 0.7 hours for trimethoprim. All of these 11 patients had normal renal function, and their ages ranged from 17 to 78 years (median, 60 years).1
Pharmacokinetic studies in children and adults suggest an age-dependent half-life of trimethoprim, as indicated in the following table.2
Age
(years)
No. of
Patients
Mean TMP
Half-life (hours)
< 1
2
7.67
1 to 10
9
5.49
10 to 20
5
8.19
20 to 63
6
12.82
Patients with severely impaired renal function exhibit an increase in the half-lives of both components, requiring dosage regimen adjustment (see DOSAGE AND ADMINISTRATION section).
Both sulfamethoxazole and trimethoprim exist in the blood as unbound, protein-bound and metabolized forms; sulfamethoxazole also exists as the conjugated form. The metabolism of sulfamethoxazole occurs predominately by N4-acetylation, although the glucuronide conjugate has been identified. The principal metabolites of trimethoprim are the 1- and 3-oxides and the 3’- and 4’-hydroxy derivatives. The free forms of sulfamethoxazole and trimethoprim are considered to be the therapeutically active forms. Approximately 70% of sulfamethoxazole and 44% of trimethoprim are bound to plasma proteins. The presence of 10 mg percent sulfamethoxazole in plasma decreases the protein binding of trimethoprim by an insignificant degree; trimethoprim does not influence the protein binding of sulfamethoxazole.
Excretion of sulfamethoxazole and trimethoprim is primarily by the kidneys through both glomerular filtration and tubular secretion. Urine concentrations of both sulfamethoxazole and trimethoprim are considerably higher than are the concentrations in the blood. The percent of dose excreted in urine over a 12 hour period following the intravenous administration of the first dose of 1200 mg of sulfamethoxazole and 240 mg of trimethoprim on day 1 ranged from 7% to 12.7% as free sulfamethoxazole and 17% to 42.4% as free trimethoprim; and 36.7% to 56% as total (free plus the N4-acetylated metabolite) sulfamethoxazole. When administered together, neither sulfamethoxazole nor trimethoprim affects the urinary excretion pattern of the other. Both sulfamethoxazole and trimethoprim distribute to sputum and vaginal fluid; trimethoprim also distributes to bronchial secretions, and both pass the placental barrier and are excreted in breast milk.
Microbiology
Sulfamethoxazole inhibits bacterial synthesis of dihydrofolic acid by competing with para-aminobenzoic acid (PABA). Trimethoprim blocks the production of tetrahydrofolic acid from dihydrofolic acid by binding to and reversibly inhibiting the required enzyme, dihydrofolate reductase. Thus, sulfamethoxazole and trimethoprim blocks two consecutive steps in the biosynthesis of nucleic acids and proteins essential to many bacteria.
In vitro studies have shown that bacterial resistance develops more slowly with both sulfamethoxazole and trimethoprim in combination than with either sulfamethoxazole or trimethoprim alone.
Sulfamethoxazole and trimethoprim have been shown to be active against most strains of the following microorganisms, both in vitro and in clinical infections as described in the INDICATIONS AND USAGE section.
Aerobic gram-positive microorganisms
Streptococcus pneumoniae
Aerobic gram-negative microorganisms
Escherichia coli (including susceptible enterotoxigenic strains implicated in traveler’s diarrhea)
Klebsiella species
Enterobacter species
Haemophilus influenzae
Morganella morganii
Proteus mirabilis
Proteus vulgaris
Shigella flexneri
Shigella sonneiOther Organisms
Pneumocystis jiroveci
Susceptibility Testing
For specific information regarding susceptibility test interpretive criteria and associated test methods and quality control standards recognized by FDA for this drug, please see: https://www.fda.gov/STIC.
-
INDICATIONS AND USAGE
To reduce the development of drug-resistant bacteria and maintain the effectiveness of sulfamethoxazole and trimethoprim injection and other antibacterial drugs, sulfamethoxazole and trimethoprim injection should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to empiric selection of therapy.
Pneumocystis Jiroveci Pneumonia
Sulfamethoxazole and trimethoprim injection is indicated in the treatment of Pneumocystis jiroveci pneumonia in children and adults.
Shigellosis
Sulfamethoxazole and trimethoprim injection is indicated in the treatment of enteritis caused by susceptible strains of Shigella flexneri and Shigella sonnei in children and adults.
Urinary Tract Infections
Sulfamethoxazole and trimethoprim injection is indicated in the treatment of severe or complicated urinary tract infections due to susceptible strains of Escherichia coli, Klebsiella species, Enterobacter species, Morganella morganii and Proteus species when oral administration of sulfamethoxazole and trimethoprim is not feasible and when the organism is not susceptible to single-agent antibacterials effective in the urinary tract.
Although appropriate culture and susceptibility studies should be performed, therapy may be started while awaiting the results of these studies.
-
CONTRAINDICATIONS
Sulfamethoxazole and trimethoprim are contraindicated in patients with a known hypersensitivity to trimethoprim or sulfonamides, in patients with a history of drug-induced immune thrombocytopenia with use of trimethoprim and/or sulfonamides, and in patients with documented megaloblastic anemia due to folate deficiency. Sulfamethoxazole and trimethoprim are also contraindicated in pregnant patients and nursing mothers, because sulfonamides pass the placenta and are excreted in the milk and may cause kernicterus. Sulfamethoxazole and trimethoprim are contraindicated in pediatric patients less than 2 months of age.
-
WARNINGS
Hypersensitivity and Other Fatal Reactions
FATALITIES ASSOCIATED WITH THE ADMINISTRATION OF SULFONAMIDES, ALTHOUGH RARE, HAVE OCCURRED DUE TO SEVERE REACTIONS, INCLUDING STEVENS-JOHNSON SYNDROME, TOXIC EPIDERMAL NECROLYSIS, FULMINANT HEPATIC NECROSIS, AGRANULOCYTOSIS, APLASTIC ANEMIA, AND OTHER BLOOD DYSCRASIAS.
SULFONAMIDES, INCLUDING SULFONAMIDE-CONTAINING PRODUCTS SUCH AS SULFAMETHOXAZOLE AND TRIMETHOPRIM INJECTION, SHOULD BE DISCONTINUED AT THE FIRST APPEARANCE OF SKIN RASH OR ANY SIGN OF ADVERSE REACTION. In rare instances, a skin rash may be followed by a more severe reaction, such as Stevens-Johnson syndrome, toxic epidermal necrolysis, hepatic necrosis, and serious blood disorders (see PRECAUTIONS). Clinical signs, such as rash, sore throat, fever, arthralgia, pallor, purpura, or jaundice may be early indications of serious reactions.
Cough, shortness of breath, and pulmonary infiltrates are hypersensitivity reactions of the respiratory tract that have been reported in association with sulfonamide treatment.
Thrombocytopenia
Sulfamethoxazole and trimethoprim-induced thrombocytopenia may be an immune-mediated disorder. Severe cases of thrombocytopenia that are fatal or life threatening have been reported. Thrombocytopenia usually resolves within a week upon discontinuation of sulfamethoxazole and trimethoprim.
Streptococcal Infections and Rheumatic Fever
The sulfonamides should not be used for the treatment of group A beta-hemolytic streptococcal infections. In an established infection, they will not eradicate the streptococcus and, therefore, will not prevent sequelae such as rheumatic fever.
Clostridium Difficile Associated Diarrhea
Clostridium difficile associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents, including sulfamethoxazole and trimethoprim, and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon leading to overgrowth of C. difficile.
C. difficile produces toxins A and B which contribute to the development of CDAD. Hypertoxin producing strains of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibiotic use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents.
If CDAD is suspected or confirmed, ongoing antibiotic use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibiotic treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated.
Sulfite Sensitivity
Sulfamethoxazole and trimethoprim injection contains sodium metabisulfite, a sulfite that may cause allergic-type reactions, including anaphylactic symptoms and life-threatening or less severe asthmatic episodes in certain susceptible people. The overall prevalence of sulfite sensitivity in the general population is unknown and probably low. Sulfite sensitivity is seen more frequently in asthmatic than in nonasthmatic people.
Benzyl Alcohol
Contains benzyl alcohol. In newborn infants, benzyl alcohol has been associated with an increased incidence of neurological and other complications which are sometimes fatal.
Adjunctive Treatment With Leucovorin for Pneumocystis Jiroveci Pneumonia
Treatment failure and excess mortality were observed when trimethoprim and sulfamethoxazole was used concomitantly with leucovorin for the treatment of HIV positive patients with Pneumocystis jiroveci pneumonia in a randomized placebo controlled trial.3 Coadministration of trimethoprim and sulfamethoxazole and leucovorin during treatment of Pneumocystis jiroveci pneumonia should be avoided.
-
PRECAUTIONS
Development of Drug Resistant Bacteria
Prescribing sulfamethoxazole and trimethoprim injection in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
General
Folate Deficiency
Sulfamethoxazole and trimethoprim injection should be given with caution to patients with impaired renal or hepatic function, to those with possible folate deficiency (e.g., the elderly, chronic alcoholics, patients receiving anticonvulsant therapy, patients with malabsorption syndrome, and patients in malnutrition states) and to those with severe allergies or bronchial asthma.
Hematological changes indicative of folic acid deficiency may occur in elderly patients or in patients with preexisting folic acid deficiency or kidney failure. These effects are reversible by folinic acid therapy.
Hemolysis
In glucose-6-phosphate dehydrogenase deficient individuals, hemolysis may occur. This reaction is frequently dose-related (see CLINICAL PHARMACOLOGY and DOSAGE AND ADMINISTRATION).
Infusion Reactions
Local irritation and inflammation due to extravascular infiltration of the infusion have been observed with sulfamethoxazole and trimethoprim. If these occur the infusion should be discontinued and restarted at another site.
Hypoglycemia
Cases of hypoglycemia in non-diabetic patients treated with sulfamethoxazole and trimethoprim are seen rarely, usually occurring after a few days of therapy. Patients with renal dysfunction, liver disease, malnutrition or those receiving high doses of sulfamethoxazole and trimethoprim are particularly at risk.
Use in the Treatment of Pneumocystis Jiroveci Pneumonia in Patients with Acquired Immunodeficiency Syndrome (AIDS)
AIDS patients may not tolerate or respond to sulfamethoxazole and trimethoprim in the same manner as non-AIDS patients. The incidence of side effects, particularly rash, fever, leukopenia and elevated aminotransferase (transaminase) values, with sulfamethoxazole and trimethoprim therapy in AIDS patients who are being treated for Pneumocystis jiroveci pneumonia has been reported to be greatly increased compared with the incidence normally associated with the use of sulfamethoxazole and trimethoprim in non-AIDS patients. The incidence of hyperkalemia appears to be increased in AIDS patients receiving sulfamethoxazole and trimethoprim. Adverse effects are generally less severe in patients receiving sulfamethoxazole and trimethoprim for prophylaxis. A history of mild intolerance to sulfamethoxazole and trimethoprim in AIDS patients does not appear to predict intolerance of subsequent secondary prophylaxis.4 However, if a patient develops skin rash or any sign of adverse reaction, therapy with sulfamethoxazole and trimethoprim should be reevaluated (see WARNINGS).
Coadministration of sulfamethoxazole and trimethoprim and leucovorin should be avoided with Pneumocystis jiroveci pneumonia (see WARNINGS).
High dosage of trimethoprim, as used in patients with Pneumocystis jiroveci pneumonia, induces a progressive but reversible increase of serum potassium concentrations in a substantial number of patients. Even treatment with recommended doses may cause hyperkalemia when trimethoprim is administered to patients with underlying disorders of potassium metabolism, with renal insufficiency, or if drugs known to induce hyperkalemia are given concomitantly. Close monitoring of serum potassium is warranted in these patients.
During treatment, adequate fluid intake and urinary output should be ensured to prevent crystalluria. Patients who are “slow acetylators” may be more prone to idiosyncratic reactions to sulfonamides.
Information for Patients
Patients should be counseled that antibacterial drugs including sulfamethoxazole and trimethoprim injection should only be used to treat bacterial infections. It does not treat viral infections (e.g., the common cold).
Patients should be instructed to maintain an adequate fluid intake in order to prevent crystalluria and stone formation.
Diarrhea is a common problem caused by antibiotics which usually ends when the antibiotic is discontinued. Sometimes after starting treatment with antibiotics, patients can develop watery and bloody stools (with or without stomach cramps and fever) even as late as two or more months after having taken the last dose of the antibiotic. If this occurs, patients should contact their physician as soon as possible.
Laboratory Tests
Complete blood counts should be done frequently in patients receiving sulfamethoxazole and trimethoprim; if a significant reduction in the count of any formed blood element is noted, sulfamethoxazole and trimethoprim should be discontinued. Urinalyses with careful microscopic examination and renal function tests should be performed during therapy, particularly for those patients with impaired renal function.
Drug Interactions
In elderly patients concurrently receiving certain diuretics, primarily thiazides, an increased incidence of thrombocytopenia with purpura has been reported.
It has been reported that sulfamethoxazole and trimethoprim may prolong the prothrombin time in patients who are receiving the anticoagulant warfarin. This interaction should be kept in mind when sulfamethoxazole and trimethoprim is given to patients already on anticoagulant therapy, and the coagulation time should be reassessed. Sulfamethoxazole and trimethoprim may inhibit the hepatic metabolism of phenytoin. Sulfamethoxazole and trimethoprim, given at a common clinical dosage, increased the phenytoin half-life by 39% and decreased the phenytoin metabolic clearance rate by 27%. When administering these drugs concurrently, one should be alert for possible excessive phenytoin effect.
Sulfonamides can also displace methotrexate from plasma protein binding sites and can compete with the renal transport of methotrexate, thus increasing free methotrexate concentrations.
There have been reports of marked but reversible nephrotoxicity with coadministration of sulfamethoxazole and trimethoprim and cyclosporine in renal transplant recipients.
Increased digoxin blood levels can occur with concomitant sulfamethoxazole and trimethoprim therapy, especially in elderly patients. Serum digoxin levels should be monitored.
Increased sulfamethoxazole blood levels may occur in patients who are also receiving indomethacin.
Occasional reports suggest that patients receiving pyrimethamine as malaria prophylaxis in doses exceeding 25 mg weekly may develop megaloblastic anemia if sulfamethoxazole and trimethoprim is prescribed.
The efficacy of tricyclic antidepressants can decrease when coadministered with sulfamethoxazole and trimethoprim.
Like other sulfonamide-containing drugs, sulfamethoxazole and trimethoprim potentiates the effect of oral hypoglycemics.
In the literature, a single case of toxic delirium has been reported after concomitant intake of sulfamethoxazole and trimethoprim and amantadine.
In the literature, three cases of hyperkalemia in elderly patients have been reported after concomitant intake of sulfamethoxazole and trimethoprim and an angiotensin converting enzyme inhibitor.5, 6
Drug/Laboratory Test Interactions
Sulfamethoxazole and trimethoprim, specifically the trimethoprim component, can interfere with a serum methotrexate assay as determined by the competitive binding protein technique (CBPA) when a bacterial dihydrofolate reductase is used as the binding protein. No interference occurs, however, if methotrexate is measured by a radioimmunoassay (RIA).
The presence of sulfamethoxazole and trimethoprim may also interfere with the Jaffé alkaline picrate reaction assay for creatinine, resulting in overestimations of about 10% in the range of normal values.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Long-term studies in animals to evaluate carcinogenic potential have not been conducted with sulfamethoxazole and trimethoprim.
Mutagenesis
Bacterial mutagenic studies have not been performed with sulfamethoxazole and trimethoprim in combination. Trimethoprim was demonstrated to be nonmutagenic in the Ames assay. No chromosomal damage was observed in human leukocytes cultured in vitro with sulfamethoxazole and trimethoprim alone or in combination; the concentrations used exceeded blood levels of these compounds following therapy with sulfamethoxazole and trimethoprim. Observations of leukocytes obtained from patients treated with sulfamethoxazole and trimethoprim revealed no chromosomal abnormalities.
Pregnancy
Teratogenic Effects
Pregnancy Category C
In rats, oral doses of 533 mg/kg or 200 mg/kg produced teratologic effects manifested mainly as cleft palates.
The highest dose which did not cause cleft palates in rats was 512 mg/kg sulfamethoxazole or 192 mg/kg trimethoprim when administered separately. In two studies in rats, no teratology was observed when 512 mg/kg of sulfamethoxazole was used in combination with 128 mg/kg of trimethoprim. In one study, however, cleft palates were observed in one litter out of 9 when 355 mg/kg of sulfamethoxazole was used in combination with 88 mg/kg of trimethoprim.
In some rabbit studies, an overall increase in fetal loss (dead and resorbed and malformed conceptuses) was associated with doses of trimethoprim six times the human therapeutic dose.
While there are no large, well-controlled studies on the use of sulfamethoxazole and trimethoprim in pregnant women, Brumfitt and Pursell,7 in a retrospective study, reported the outcome of 186 pregnancies during which the mother received either placebo or sulfamethoxazole and trimethoprim. The incidence of congenital abnormalities was 4.5% (3 of 66) in those who received placebo and 3.3% (4 of 120) in those receiving sulfamethoxazole and trimethoprim. There were no abnormalities in the 10 children whose mothers received the drug during the first trimester. In a separate survey, Brumfitt and Pursell also found no congenital abnormalities in 35 children whose mothers had received oral sulfamethoxazole and trimethoprim at the time of conception or shortly thereafter.
Because sulfamethoxazole and trimethoprim may interfere with folic acid metabolism, sulfamethoxazole and trimethoprim injection should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Pediatric Use
Sulfamethoxazole and trimethoprim is contraindicated for infants younger than 2 months of age (see CONTRAINDICATIONS section).
Geriatric Use
Clinical studies of sulfamethoxazole and trimethoprim did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects.
There may be an increased risk of severe adverse reactions in elderly patients, particularly when complicating conditions exist, e.g., impaired kidney and/or liver function, possible folate deficiency, or concomitant use of other drugs. Severe skin reactions, generalized bone marrow suppression (see WARNINGS and ADVERSE REACTIONS sections), a specific decrease in platelets (with or without purpura), and hyperkalemia are the most frequently reported severe adverse reactions in elderly patients. In those concurrently receiving certain diuretics, primarily thiazides, an increased incidence of thrombocytopenia with purpura has been reported. Increased digoxin blood levels can occur with concomitant sulfamethoxazole and trimethoprim therapy, especially in elderly patients. Serum digoxin levels should be monitored. Hematological changes indicative of folic acid deficiency may occur in elderly patients. These effects are reversible by folinic acid therapy. Appropriate dosage adjustments should be made for patients with impaired kidney function and duration of use should be as short as possible to minimize risks of undesired reactions (see DOSAGE AND ADMINISTRATION section). The trimethoprim component of sulfamethoxazole and trimethoprim may cause hyperkalemia when administered to patients with underlying disorders of potassium metabolism, with renal insufficiency or when given concomitantly with drugs known to induce hyperkalemia, such as angiotensin converting enzyme inhibitors. Close monitoring of serum potassium is warranted in these patients. Discontinuation of sulfamethoxazole and trimethoprim treatment is recommended to help lower potassium serum levels.
Pharmacokinetics parameters for sulfamethoxazole were similar for geriatric subjects and younger adult subjects. The mean maximum serum trimethoprim concentration was higher and mean renal clearance of trimethoprim was lower in geriatric subjects compared with younger subjects (see CLINICAL PHARMACOLOGY).
-
ADVERSE REACTIONS
The most common adverse effects are gastrointestinal disturbances (nausea, vomiting, anorexia) and allergic skin reactions (such as rash and urticaria). FATALITIES ASSOCIATED WITH THE ADMINISTRATION OF SULFONAMIDES, ALTHOUGH RARE, HAVE OCCURRED DUE TO SEVERE REACTIONS, INCLUDING STEVENS-JOHNSON SYNDROME, TOXIC EPIDERMAL NECROLYSIS, FULMINANT HEPATIC NECROSIS, AGRANULOCYTOSIS, APLASTIC ANEMIA AND OTHER BLOOD DYSCRASIAS (SEE WARNINGS SECTION). Local reaction, pain and slight irritation on IV administration are infrequent. Thrombophlebitis has rarely been observed.
Hematologic
Agranulocytosis, aplastic anemia, thrombocytopenia, leukopenia, neutropenia, hemolytic anemia, megaloblastic anemia, hypoprothrombinemia, methemoglobinemia, eosinophilia.
Allergic Reactions
Stevens-Johnson syndrome, toxic epidermal necrolysis, anaphylaxis, allergic myocarditis, erythema multiforme, exfoliative dermatitis, angioedema, drug fever, chills, Henoch-Schoenlein purpura, serum sickness-like syndrome, generalized allergic reactions, generalized skin eruptions, conjunctival and scleral injection, photosensitivity, pruritus, urticaria and rash. In addition, periarteritis nodosa and systemic lupus erythematosus have been reported.
Gastrointestinal
Hepatitis (including cholestatic jaundice and hepatic necrosis), elevation of serum transaminase and bilirubin, pseudomembranous enterocolitis, pancreatitis, stomatitis, glossitis, nausea, emesis, abdominal pain, diarrhea, anorexia.
Genitourinary
Renal failure, interstitial nephritis, BUN and serum creatinine elevation, toxic nephrosis with oliguria and anuria, and crystalluria.
Metabolic and Nutritional
Hyperkalemia
See PRECAUTIONS, Use in the Treatment of Pneumocystis Jiroveci Pneumonia in Patients with Acquired Immunodeficiency Syndrome (AIDS).
Neurologic
Aseptic meningitis, convulsions, peripheral neuritis, ataxia, vertigo, tinnitus, headache.
Endocrine
The sulfonamides bear certain chemical similarities to some goitrogens, diuretics (acetazolamide and the thiazides) and oral hypoglycemic agents. Cross-sensitivity may exist with these agents. Diuresis and hypoglycemia have occurred rarely in patients receiving sulfonamides.
Musculoskeletal
Arthralgia and myalgia. Isolated cases of rhabdomyolysis have been reported with sulfamethoxazole and trimethoprim, mainly in AIDS patients.
Postmarketing Experience
The following adverse reactions have been identified during post-approval use of trimethoprim and sulfamethoxazole. Because these reactions were reported voluntarily from a population of uncertain size, it is not possible to reliably estimate their frequency or establish a causal relationship to drug exposure:
- Thrombotic thrombocytopenia purpura
- Idiopathic thrombocytopenic purpura
-
OVERDOSAGE
Acute
Since there has been no extensive experience in humans with single doses of sulfamethoxazole and trimethoprim injection in excess of 25 mL (2000 mg sulfamethoxazole and 400 mg trimethoprim), the maximum tolerated dose in humans is unknown. Signs and symptoms of overdosage reported with sulfonamides include anorexia, colic, nausea, vomiting, dizziness, headache, drowsiness and unconsciousness. Pyrexia, hematuria and crystalluria may be noted. Blood dyscrasias and jaundice are potential late manifestations of overdosage.
Signs of acute overdosage with trimethoprim include nausea, vomiting, dizziness, headache, mental depression, confusion and bone marrow depression.
General principles of treatment include the administration of intravenous fluids if urine output is low and renal function is normal. Acidification of the urine will increase renal elimination of trimethoprim. The patient should be monitored with blood counts and appropriate blood chemistries, including electrolytes. If a significant blood dyscrasia or jaundice occurs, specific therapy should be instituted for these complications. Peritoneal dialysis is not effective and hemodialysis is only moderately effective in eliminating trimethoprim and sulfamethoxazole.
Chronic
Use of sulfamethoxazole and trimethoprim injection at high doses and/or for extended periods of time may cause bone marrow depression manifested as thrombocytopenia, leukopenia and/or megaloblastic anemia. If signs of bone marrow depression occur, the patient should be given leucovorin 5 to 15 mg daily until normal hematopoiesis is restored.
Animal Toxicity
The LD50 of sulfamethoxazole and trimethoprim injection in mice is 700 mg/kg or 7.3 mL/kg; in rats and rabbits the LD50 is > 500 mg/kg or > 5.2 mL/kg. The vehicle produced the same LD50 in each of these species as the active drug.
The signs and symptoms noted in mice, rats and rabbits with sulfamethoxazole and trimethoprim or its vehicle at the high IV doses used in acute toxicity studies included ataxia, decreased motor activity, loss of righting reflex, tremors or convulsions, and/or respiratory depression.
-
DOSAGE AND ADMINISTRATION
SULFAMETHOXAZOLE AND TRIMETHOPRIM INJECTION IS CONTRAINDICATED IN PEDIATRIC PATIENTS LESS THAN 2 MONTHS OF AGE. CAUTION—SULFAMETHOXAZOLE AND TRIMETHOPRIM INJECTION MUST BE DILUTED IN 5% DEXTROSE IN WATER SOLUTION PRIOR TO ADMINISTRATION. DO NOT MIX SULFAMETHOXAZOLE AND TRIMETHOPRIM INJECTION WITH OTHER DRUGS OR SOLUTIONS. RAPID INFUSION OR BOLUS INJECTION MUST BE AVOIDED.
Dosage
Children and Adults
Pneumocystis Jiroveci Pneumonia
Total daily dose is 15 to 20 mg/kg (based on the trimethoprim component) given in 3 or 4 equally divided doses every 6 to 8 hours for up to 14 days. One investigator noted that a total daily dose of 10 to 15 mg/kg was sufficient in 10 adult patients with normal renal function.8
Severe Urinary Tract Infections and Shigellosis
Total daily dose is 8 to 10 mg/kg (based on the trimethoprim component) given in 2 or 4 equally divided doses every 6, 8 or 12 hours for up to 14 days for severe urinary tract infections and 5 days for shigellosis. The maximum recommended daily dose is 60 mL per day.
For Patients With Impaired Renal Function
When renal function is impaired, a reduced dosage should be employed using the following table:
Creatinine
Clearance (mL/min)
Recommended
Dosage Regimen
Above 30
Usual standard regimen
15 to 30
1⁄2 the usual regimen
Below 15
Use not recommended
Method of Preparation
Sulfamethoxazole and trimethoprim injection must be diluted. EACH 5 ML SHOULD BE ADDED TO 125 ML OF 5% DEXTROSE IN WATER. After diluting with 5% dextrose in water the solution should not be refrigerated and should be used within 6 hours. If a dilution of 5 mL per 100 mL of 5% dextrose in water is desired, it should be used within 4 hours. If upon visual inspection there is cloudiness or evidence of crystallization after mixing, the solution should be discarded and a fresh solution prepared.
Multidose Vials
After initial entry into the vial, the remaining contents must be used within 48 hours.
The following infusion systems have been tested and found satisfactory: unit-dose glass containers; unit-dose polyvinyl chloride and polyolefin containers. No other systems have been tested and therefore no others can be recommended.
Dilution
EACH 5 ML OF SULFAMETHOXAZOLE AND TRIMETHOPRIM INJECTION SHOULD BE ADDED TO 125 ML OF 5% DEXTROSE IN WATER.
Note: In those instances where fluid restriction is desirable, each 5 mL may be added to 75 mL of 5% dextrose in water. Under these circumstances the solution should be mixed just prior to use and should be administered within 2 hours. If upon visual inspection there is cloudiness or evidence of crystallization after mixing, the solution should be discarded and a fresh solution prepared.
DO NOT MIX SULFAMETHOXAZOLE AND TRIMETHOPRIM INJECTION 5% DEXTROSE IN WATER WITH DRUGS OR SOLUTIONS IN THE SAME CONTAINER.
Administration
The solution should be given by intravenous infusion over a period of 60 to 90 minutes. Rapid infusion or bolus injection must be avoided. Sulfamethoxazole and trimethoprim injection should not be given intramuscularly.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever the solution and container permit.
-
HOW SUPPLIED
Sulfamethoxazole and Trimethoprim Injection USP, 80 mg and 16 mg are supplied as follows:
NDC Numbers Sulfamethoxazole, USP Trimethoprim, USP Size 0703-9503-03 80 mg/mL 16 mg/mL 5 mL
Single
dose vial0703-9514-03 80 mg/mL 16 mg/mL 10 mL
Multiple
dose vial0703-9526-01 80 mg/mL 16 mg/mL 30 mL
Multiple
dose vial5 mL single dose amber vials packaged 10 per carton.
10 mL multiple dose amber vials packaged 10 per carton.
30 mL multiple dose amber vials packaged individually.
Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
DO NOT REFRIGERATE.
-
REFERENCES
- Grose WE, Bodey GP, Loo TL. Clinical Pharmacology of Intravenously Administered Trimethoprim-Sulfamethoxazole. Antimicrob Agents Chemother. Mar 1979;15:447-451.
- Siber GR, Gorham C, Durbin W, Lesko L, Levin MJ. Pharmacology of Intravenous Trimethoprim-Sulfamethoxazole in Children and Adults. Current Chemotherapy and Infectious Diseases, American Society for Microbiology, Washington, D.C., 1980, Vol. 1, pp. 691-692.
- Safrin S, Lee BL, Sande MA. Adjunctive folinic acid with trimethoprim-sulfamethoxazole for Pneumocystis carinii pneumonia in AIDS patients is associated with an increased risk of therapeutic failure and death. J Infect Dis. 1994 Oct;170(4):912-7.
- Hardy DW, et al. A controlled trial of trimethoprim-sulfamethoxazole or aerosolized pentamidine for secondary prophylaxis of Pneumocystis carinii pneumonia in patients with the acquired immunodeficiency syndrome. N Engl J Med. 1992; 327: 1842–1848.
- Marinella Mark A. 1999. Trimethoprim-induced hyperkalemia: An analysis of reported cases. Gerontol. 45:209–212.
- Margassery, S. and B. Bastani. 2002. Life threatening hyperkalemia and acidosis secondary to trimethoprim-sulfamethoxazole treatment. J. Nephrol. 14:410–414.
- Brumfitt W, Pursell R. Trimethoprim/Sulfamethoxazole in the Treatment of Bacteriuria in Women. J Infect Dis. Nov 1973;128 (Suppl):S657-S663.
- Winston DJ, Lau WK, Gale RP, Young LS. Trimethoprim- Sulfamethoxazole for the Treatment of Pneumocystis carinii pneumonia. Ann Intern Med. June 1980;92:762-769.
Rev. L 4/2019
Manufactured In Israel By:
Teva Pharmaceutical Ind. Ltd.
Kfar Saba, 44102, Israel
Manufactured For:
Teva Pharmaceuticals USA, Inc.
North Wales, PA 19454
-
Package/Label Display Panel
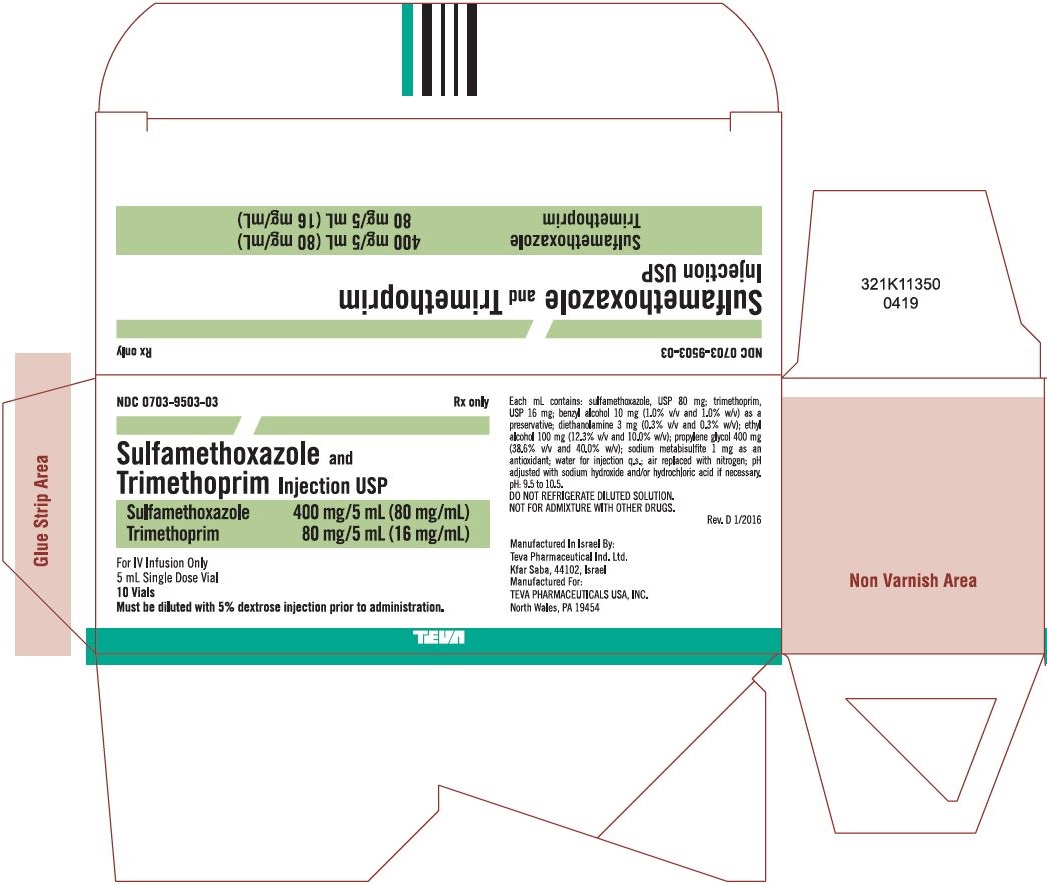
Sulfamethoxazole 80 mg/mL and Trimethoprim 16 mg/mL Injection USP, 10 x 5 mL Single Dose Vial Carton Text
NDC: 0703-9503-03 Rx only
Sulfamethoxazole and Trimethoprim
Injection USPSulfamethoxazole 400 mg/5 mL (80 mg/mL)
Trimethoprim 80 mg/5 mL (16 mg/mL)For IV Infusion Only
5 mL Single Dose Vial
10 Vials
Must be diluted with 5% dextrose injection prior to administration.TEVA
-
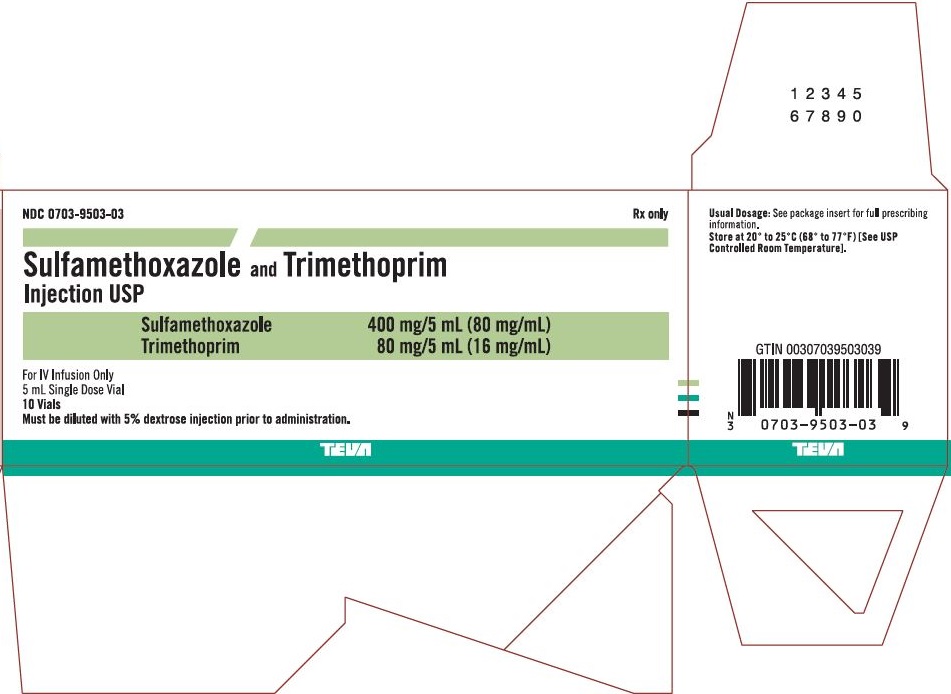
Package/Label Display Panel
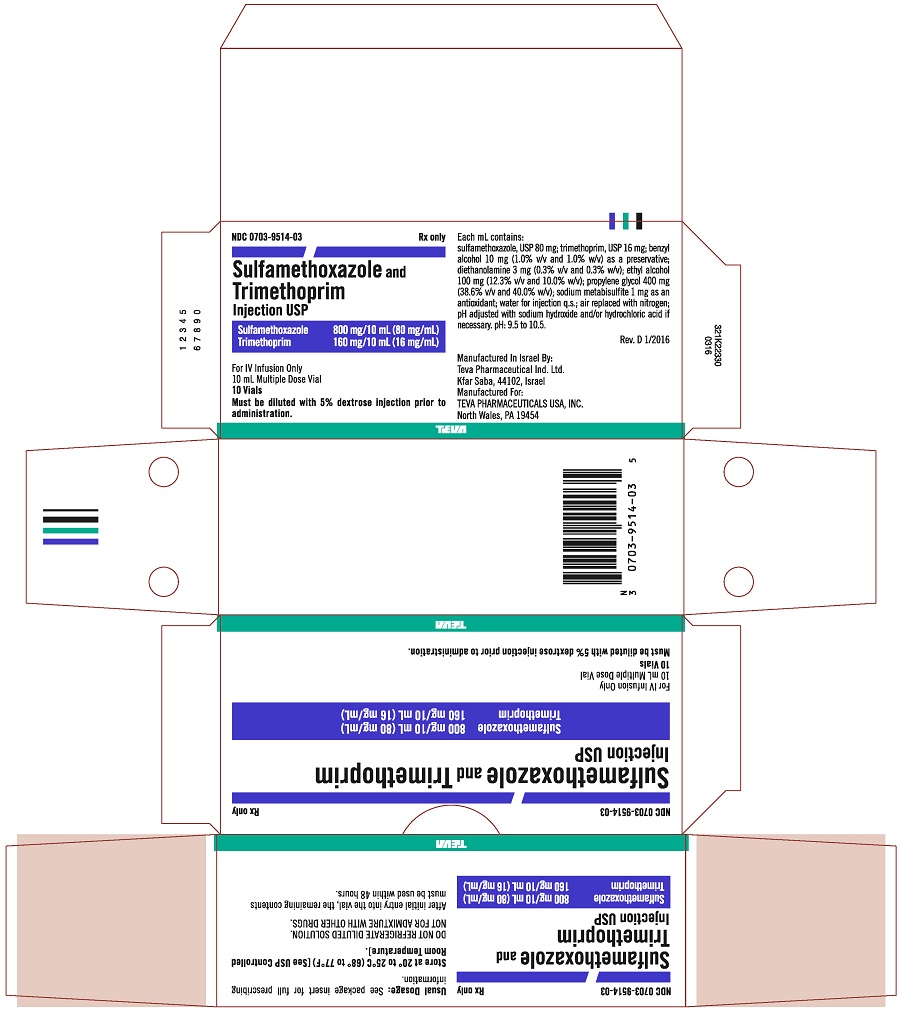
Sulfamethoxazole 80 mg/mL and Trimethoprim 16 mg/mL Injection USP, 10 x 10 mL Multiple Dose Vial Carton Text
NDC: 0703-9514-03 Rx only
Sulfamethoxazole and Trimethoprim
Injection USPSulfamethoxazole 800 mg/10 mL (80 mg/mL)
Trimethoprim 160 mg/10 mL (16 mg/mL)For IV Infusion Only
10 mL Multiple Dose Vial
10 Vials
Must be diluted with 5% dextrose injection prior to administration.TEVA
-
Package/Label Display Panel
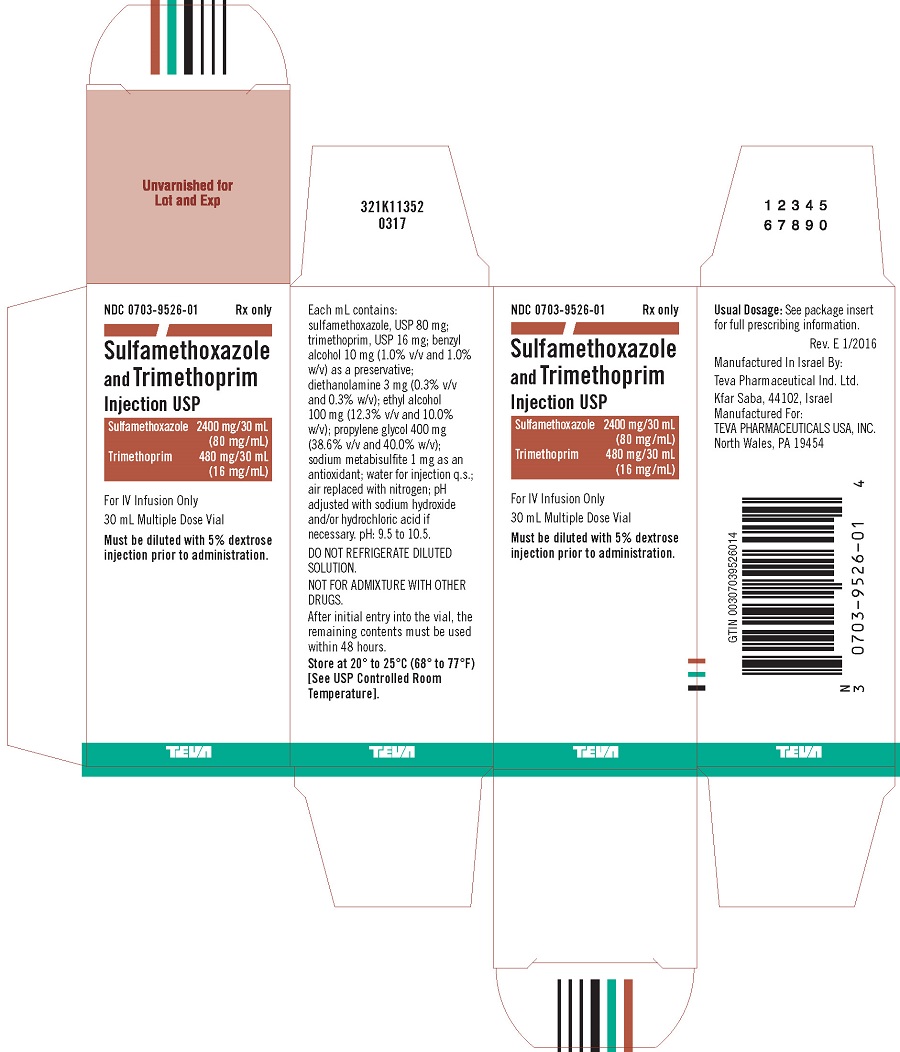
Sulfamethoxazole 80 mg/mL and Trimethoprim 16 mg/mL Injection USP, 30 mL Multiple Dose Vial Carton Text
NDC: 0703-9526-01 Rx only
Sulfamethoxazole
and Trimethoprim
Injection USPSulfamethoxazole 2400 mg/30 mL
(80 mg/mL)
Trimethoprim 480 mg/30 mL
(16 mg/mL)For IV Infusion Only
30 mL Multiple Dose Vial
Must be diluted with 5% dextrose
injection prior to administration.TEVA
-
INGREDIENTS AND APPEARANCE
SULFAMETHOXAZOLE AND TRIMETHOPRIM
sulfamethoxazole and trimethoprim injection, solution, concentrateProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0703-9503 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength SULFAMETHOXAZOLE (UNII: JE42381TNV) (SULFAMETHOXAZOLE - UNII:JE42381TNV) SULFAMETHOXAZOLE 80 mg in 1 mL TRIMETHOPRIM (UNII: AN164J8Y0X) (TRIMETHOPRIM - UNII:AN164J8Y0X) TRIMETHOPRIM 16 mg in 1 mL Inactive Ingredients Ingredient Name Strength BENZYL ALCOHOL (UNII: LKG8494WBH) DIETHANOLAMINE (UNII: AZE05TDV2V) ALCOHOL (UNII: 3K9958V90M) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) SODIUM METABISULFITE (UNII: 4VON5FNS3C) WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0703-9503-03 10 in 1 CARTON 11/01/1991 1 NDC: 0703-9503-01 5 mL in 1 VIAL, SINGLE-DOSE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA073303 11/01/1991 SULFAMETHOXAZOLE AND TRIMETHOPRIM
sulfamethoxazole and trimethoprim injection, solution, concentrateProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0703-9514 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength SULFAMETHOXAZOLE (UNII: JE42381TNV) (SULFAMETHOXAZOLE - UNII:JE42381TNV) SULFAMETHOXAZOLE 80 mg in 1 mL TRIMETHOPRIM (UNII: AN164J8Y0X) (TRIMETHOPRIM - UNII:AN164J8Y0X) TRIMETHOPRIM 16 mg in 1 mL Inactive Ingredients Ingredient Name Strength BENZYL ALCOHOL (UNII: LKG8494WBH) DIETHANOLAMINE (UNII: AZE05TDV2V) ALCOHOL (UNII: 3K9958V90M) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) SODIUM METABISULFITE (UNII: 4VON5FNS3C) WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0703-9514-03 10 in 1 CARTON 11/01/1991 1 NDC: 0703-9514-01 10 mL in 1 VIAL, MULTI-DOSE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA073303 11/01/1991 SULFAMETHOXAZOLE AND TRIMETHOPRIM
sulfamethoxazole and trimethoprim injection, solution, concentrateProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0703-9526 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength SULFAMETHOXAZOLE (UNII: JE42381TNV) (SULFAMETHOXAZOLE - UNII:JE42381TNV) SULFAMETHOXAZOLE 80 mg in 1 mL TRIMETHOPRIM (UNII: AN164J8Y0X) (TRIMETHOPRIM - UNII:AN164J8Y0X) TRIMETHOPRIM 16 mg in 1 mL Inactive Ingredients Ingredient Name Strength BENZYL ALCOHOL (UNII: LKG8494WBH) DIETHANOLAMINE (UNII: AZE05TDV2V) ALCOHOL (UNII: 3K9958V90M) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) SODIUM METABISULFITE (UNII: 4VON5FNS3C) WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0703-9526-01 1 in 1 CARTON 11/01/1991 1 30 mL in 1 VIAL, MULTI-DOSE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA073303 11/01/1991 Labeler - Teva Parenteral Medicines, Inc. (794362533)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.