ZIMHI TM (naloxone hydrochloride injection) for intramuscular or subcutaneous use These highlights do not include all the information needed to use ZIMHI TM safely and effectively. See full prescribing information for ZIMHI TM ZIMHI TM (naloxone hydrochloride injection) for intramuscular or subcutaneous use Initial U.S. Approval: 1971
ZIMHI by
Drug Labeling and Warnings
ZIMHI by is a Prescription medication manufactured, distributed, or labeled by Adamis Pharmaceuticals. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
ZIMHI- naloxone hydrochloride injection, solution
Adamis Pharmaceuticals
----------
HIGHLIGHTS OF PRESCRIBING INFORMATION
ZIMHI
TM (naloxone hydrochloride injection) for intramuscular or subcutaneous use
These highlights do not include all the information needed to use ZIMHITM safely and effectively. See full prescribing information for ZIMHITM ZIMHITM (naloxone hydrochloride injection) for intramuscular or subcutaneous use Initial U.S. Approval: 1971 INDICATIONS AND USAGEZIMHI is an opioid antagonist indicated in adult and pediatric patients for the emergency treatment of known or suspected opioid overdose, as manifested by respiratory and/or central nervous system depression. ( 1) ZIMHI is intended for immediate administration as emergency therapy in settings where opioids may be present. ( 1) ZIMHI is not a substitute for emergency medical care. ( 1) DOSAGE AND ADMINISTRATION
DOSAGE FORMS AND STRENGTHSInjection: 5 mg/0.5 mL naloxone hydrochloride solution in a single-dose, prefilled syringe. ( 3) CONTRAINDICATIONSHypersensitivity to naloxone hydrochloride or to any of the other ingredients in ZIMHI. ( 4) WARNINGS AND PRECAUTIONS
ADVERSE REACTIONSThe following adverse reactions were most commonly observed in ZIMHI clinical studies: nausea, dizziness, lightheadedness, and elevated bilirubin. ( 6)
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling. Revised: 10/2021 |
FULL PRESCRIBING INFORMATION
1. INDICATIONS AND USAGE
ZIMHI TM is indicated in adults and pediatric patients for:
- the emergency treatment of known or suspected opioid overdose, as manifested by respiratory and/or central nervous system depression.
ZIMHI is intended for immediate administration as emergency therapy in settings where opioids may be present.
ZIMHI is not a substitute for emergency medical care.
2. DOSAGE AND ADMINISTRATION
2.1 Important Administration Instructions
ZIMHI is for intramuscular and subcutaneous use only.
Because treatment of known or suspected opioid overdose must be performed by someone other than the patient, instruct the prescription recipient to inform those around them about the presence of ZIMHI and the Instructions for Use.
ZIMHI is intended to be administered by individuals 12 years of age or older. Younger individuals or those with limited hand strength may find the device difficult to use.
ZIMHI is light sensitive. Store ZIMHI in the outer case provided to protect it from light.
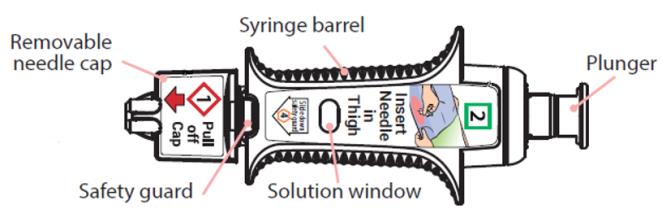
Prior to a medical emergency (during storage), periodically visually inspect ZIMHI TM through the viewing window on the device. If the solution is discolored yellow or brown color, cloudy, or contains particles, replace ZIMHI TM with a new one [ see How Supplied/Storage and Handling (16.2)].
Do not attempt to reuse ZIMHI. Each ZIMHI contains a single dose of naloxone hydrochloride for single-dose injection.
Instruct the patient or caregiver to read the Instructions for Use at the time they receive a prescription for ZIMHI TM. Emphasize the following instructions to the patient or caregiver:
-
Seek emergency medical care immediately after use. Because the duration of action of most opioids exceeds that of naloxone hydrochloride and the suspected opioid overdose may occur outside of supervised medical settings, seek immediate emergency medical assistance, keep the patient under continued surveillance until emergency personnel arrive, and administer repeated doses of ZIMHI as necessary. Always seek emergency medical assistance in the event of a suspected potentially life-threatening opioid emergency after administration of the first dose of ZIMHI.
- Additional doses of ZIMHI may be required until emergency medical assistance becomes available [
see Dosage and Administration (2.2)].
- Administer ZIMHI according to the Instructions for Use and the printed instructions on the device label:
- Place the patient in the supine position.
- Inject ZIMHI intramuscularly or subcutaneously into the anterolateral aspect of the thigh with the needle facing downwards. Inject through clothing if necessary [ see Instructions for Use].
- Embed the needle completely before transferring the thumb to the syringe plunger.

- Immediately after injection, using one hand with fingers behind the needle, slide the safety guard over the needle. Do not use two hands to activate the safety guard.

- Never put thumb, fingers, or hand over the exposed needle. Failure to follow these instructions may result in a needlestick injury. If an accidental needlestick occurs, get medical help immediately [ see Warnings and Precautions (5.4)].
- Do NOT attempt to re-cap the needle with the needle cap once it has been removed [ see Warnings and Precautions (5.4)].
- Place the patient in the lateral recumbent position (recovery position).
- ZIMHI must be used and/or properly disposed of as described below once the protective cap covering the needle is removed.
- Put the used syringe into the blue case, close the case, and give your used ZIMHI syringe to the healthcare provider for inspection and proper disposal.
- Tell the healthcare provider that you have received or administered an injection of naloxone HCL. Show the healthcare provider where the injection was administered.
2.2 Dosing Information
Initial Dosing
Administer the initial dose of ZIMHI TM to adult or pediatric patients intramuscularly or subcutaneously into the anterolateral aspect of the thigh, through clothing if necessary, and seek emergency medical assistance. Administer ZIMHI TM as quickly as possible because prolonged respiratory depression may result in damage to the central nervous system or death.
Repeat Dosing
The requirement for repeat doses of ZIMHI depends upon the amount, type, and route of administration of the opioid being antagonized.
If the desired response is not obtained after 2 or 3 minutes, an additional dose of ZIMHI may be administered. If there is still no response and additional doses are available, additional doses of ZIMHI may be administered every 2 to 3 minutes until emergency medical assistance arrives.
Additional supportive and/or resuscitative measures may be helpful while awaiting emergency medical assistance.
If the patient responds to ZIMHI and relapses back into respiratory depression before emergency assistance arrives, administer an additional dose of ZIMHI and continue surveillance of the patient after administering an additional dose.
Reversal of respiratory depression by partial agonists or mixed agonist/antagonists, such as buprenorphine and pentazocine, may be incomplete and may require higher doses of naloxone hydrochloride or repeated administration of ZIMHI.
Dosing in Adults and Pediatric Patients
Instruct patients or their caregivers to administer ZIMHI according to the Instructions for Use, intramuscularly or subcutaneously.
Dosing in Pediatric Patients under Age One Year
In pediatric patients under the age of one year, the caregiver should pinch the thigh muscle while administering ZIMHI. Carefully observe the administration site for signs of infection following resolution of the opioid emergency.
3. DOSAGE FORMS AND STRENGTHS
Injection: 5 mg/0.5 mL naloxone hydrochloride is a clear, colorless to slightly yellow, sterile solution in a single-dose, prefilled syringe. Each ZIMHI 5 mg delivers 5 mg naloxone hydrochloride (equivalent to 4.5 mg naloxone) injection, USP (0.5 mL).
4. CONTRAINDICATIONS
ZIMHI is contraindicated in patients known to be hypersensitive to naloxone hydrochloride or to any of the other ingredients.
5. WARNINGS AND PRECAUTIONS
5.1 Risk of Recurrent Respiratory and Central Nervous System Depression
The duration of action of most opioids may exceed that of ZIMHI resulting in a return of respiratory and/or central nervous system depression after an initial improvement in symptoms. Therefore, it is necessary to seek emergency medical assistance immediately after delivering the first dose of ZIMHI. Keep the patient under continued surveillance and administer additional doses of ZIMHI if the patient is not adequately responding or responds and then relapses back into respiratory depression, as necessary [ see Dosage and Administration (2.2)]. Additional supportive and/or resuscitative measures may be helpful while awaiting emergency medical assistance.
5.2 Risk of Limited Efficacy with Partial Agonists or Mixed Agonist/Antagonists
Reversal of respiratory depression by partial agonists or mixed agonist/antagonists such as buprenorphine and pentazocine, may be incomplete. Larger or repeat doses of naloxone hydrochloride may be required to antagonize buprenorphine because the latter has a long duration of action due to its slow rate of binding and subsequent slow dissociation from the opioid receptor [ see Dosage and Administration (2)]. Buprenorphine antagonism is characterized by a gradual onset of the reversal effects and a decreased duration of action of the normally prolonged respiratory depression.
5.3 Precipitation of Severe Opioid Withdrawal
The use of ZIMHI in patients who are opioid dependent results in opioid withdrawal characterized by rapid onset of severe body aches, vomiting, diarrhea, tachycardia, fever, runny nose, sneezing, piloerection, sweating, yawning, nausea, nervousness, restlessness or irritability, shivering or trembling, abdominal cramps, weakness, and increased blood pressure. In neonates, opioid withdrawal may be life-threatening if not recognized and properly treated and may include the following signs and symptoms: convulsions, excessive crying, and hyperactive reflexes. Monitor patients for the development of the signs and symptoms of opioid withdrawal.
Abrupt postoperative reversal of opioid depression after using naloxone hydrochloride may result in nausea, vomiting, sweating, tremulousness, tachycardia, hypotension, hypertension, seizures, ventricular tachycardia and fibrillation, pulmonary edema, and cardiac arrest. Death, coma, and encephalopathy have been reported as sequelae of these events. These events have primarily occurred in patients who had pre-existing cardiovascular disorders or received other drugs that may have similar adverse cardiovascular effects. Although a direct cause and effect relationship has not been established, after use of naloxone hydrochloride, monitor patients with pre-existing cardiac disease or patients who have received medications with potential adverse cardiovascular effects for hypotension, ventricular tachycardia or fibrillation, and pulmonary edema in an appropriate healthcare setting. It has been suggested that the pathogenesis of pulmonary edema associated with the use of naloxone hydrochloride is similar to neurogenic pulmonary edema, i.e., a centrally mediated massive catecholamine response leading to a dramatic shift of blood volume into the pulmonary vascular bed resulting in increased hydrostatic pressures.
There may be clinical settings, particularly the postpartum period in neonates with known or suspected exposure to maternal opioid use, where it is preferable to avoid the abrupt precipitation of opioid withdrawal symptoms. In these settings, consider use of an alternative naloxone product which can be titrated to effect and, where applicable, dosed according to weight [ see Use in Specific Populations (8.4)].
5.4 Risk of Accidental Needlestick Injury
After use, the ZIMHI needle is exposed until the safety guard is deployed. A needlestick injury could occur during use in emergency situations. In the event that an accidental needlestick occurs, medical attention should be sought. Potential exposure to blood borne pathogens including HIV, HBV, and HCV requires immediate evaluation by a medical professional. Stress to patients the importance of familiarizing themselves with the device and its operation prior to experiencing an emergency situation, so they are familiar with the safety guard and its deployment.
6. ADVERSE REACTIONS
The following serious adverse reactions are discussed elsewhere in the labeling:
- Precipitation of Severe Opioid Withdrawal [ see Warnings and Precautions (5.3)]
Because clinical studies are conducted under widely varying conditions, adverse reaction rates observed in the clinical studies of a drug cannot be directly compared to the rates in the clinical studies of another drug and may not reflect the rates observed in practice.
The following adverse reactions were observed in ZIMHI TM clinical studies in healthy volunteers without opioid dependence: nausea, dizziness, lightheadedness, and elevated bilirubin.
The following adverse reactions have been identified during post-approval use of naloxone hydrochloride in the post-operative setting. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure: Hypotension, hypertension, ventricular tachycardia and fibrillation, dyspnea, pulmonary edema, and cardiac arrest. Death, coma, and encephalopathy have been reported as sequelae of these events. Excessive doses of naloxone hydrochloride in post-operative patients have resulted in significant reversal of analgesia and have caused agitation [ see Warnings and Precautions (5.3)].
Other events that have been reported in post-marketing use of naloxone hydrochloride include agitation, disorientation, confusion, and anger.
Abrupt reversal of opioid effects in persons who were opioid dependent resulted in opioid withdrawal characterized by rapid onset of severe body aches, vomiting, diarrhea, tachycardia, fever, runny nose, sneezing, piloerection, sweating, yawning, nausea, nervousness, restlessness or irritability, shivering or trembling, abdominal cramps, weakness, and increased blood pressure. In some patients, aggressive behavior has occurred in the context of abrupt reversal of an opioid overdose. In the neonate, opioid withdrawal signs and symptoms also included: convulsions, excessive crying, and hyperactive reflexes [ see Warnings and Precautions (5.3)].
8. USE IN SPECIFIC POPULATIONS
8.l Pregnancy
Risk Summary
Life-sustaining therapy for opioid overdose should not be withheld ( see Clinical Considerations). Available data from retrospective cohort studies on naloxone use in pregnant women have not identified a drug-associated risk of major birth defects or miscarriage. In animal reproduction studies, no embryotoxic or teratogenic effects were observed in mice and rats treated with naloxone hydrochloride during the period of organogenesis at doses equivalent to 4-times and 8-times, respectively, a human dose of 10 mg/day.
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Clinical Considerations
Disease-associated maternal and/or embryo/fetal risk
An opioid overdose is a medical emergency and can be fatal for the pregnant woman and fetus if left untreated. Treatment with ZIMHI for opioid overdose should not be withheld because of potential concerns regarding the effects of ZIMHI on the fetus.
Data
Animal Data
Naloxone hydrochloride was administered during organogenesis to mice and rats at doses 4-times and 8-times, respectively, the dose of 10 mg/day given to a 50 kg human (when based on body surface area or mg/m 2). These studies demonstrated no embryotoxic or teratogenic effects due to naloxone hydrochloride.
8.2 Lactation
Risk Summary
Naloxone is minimally orally available and is unlikely to affect the breastfed infant. There is no information regarding the presence of naloxone in human milk, the effects of naloxone on the breastfed infant, or on milk production. Studies in nursing mothers have shown that naloxone does not affect prolactin or oxytocin hormone levels.
8.4 Pediatric Use
The safety and effectiveness of ZIMHI TM (for intramuscular and subcutaneous use) have been established in pediatric patients of all ages for the emergency treatment of known or suspected opioid overdose as manifested by respiratory and/or central nervous system depression. Use of naloxone hydrochloride in all pediatric patients is supported by adult bioequivalence studies coupled with evidence from the safe and effective use of another naloxone hydrochloride injectable product. No pediatric studies were conducted for ZIMHI.
Absorption of naloxone hydrochloride following subcutaneous or intramuscular administration in pediatric patients may be erratic or delayed. Even when the opiate-intoxicated pediatric patient responds appropriately to naloxone hydrochloride injection, he/she must be carefully monitored for at least 24 hours as a relapse may occur as naloxone is metabolized.
In opioid-dependent pediatric patients, (including neonates), administration of naloxone hydrochloride may result in an abrupt and complete reversal of opioid effects, precipitating an acute opioid withdrawal syndrome. There may be clinical settings, particularly the postpartum period in neonates with known or suspected exposure to maternal opioid use, where it is preferable to avoid the abrupt precipitation of opioid withdrawal symptoms. Unlike acute opioid withdrawal in adults, acute opioid withdrawal in neonates manifesting as seizures may be life-threatening if not recognized and properly treated. Other signs and symptoms in neonates may include excessive crying and hyperactive reflexes. In these settings where it may be preferable to avoid the abrupt precipitation of acute opioid withdrawal symptoms, consider use of an alternative, naloxone hydrochloride product that can be dosed according to weight and titrated to effect. [ see Warnings and Precautions (5.3)].
In pediatric patients under the age of one year, the caregiver should pinch the thigh muscle while administering ZIMHI. Carefully observe the administration site for evidence of residual needle parts, signs of infection, or both. [ see Dosing Information (2.2)].
8.5 Geriatric Use
Geriatric patients have a greater frequency of decreased hepatic, renal, or cardiac function and of concomitant disease or other drug therapy. Therefore, the systemic exposure of naloxone can be higher in these patients.
Clinical studies of naloxone hydrochloride did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients.
11. DESCRIPTION
ZIMHI (naloxone hydrochloride injection, USP) is an opioid antagonist supplied in a single-dose prefilled syringe. ZIMHI is not made with natural rubber latex. Chemically, naloxone hydrochloride is the hydrochloride salt of 17-Allyl-4,5α-epoxy-3,14-dihydroxymorphinan-6-one hydrochloride with the following structure:
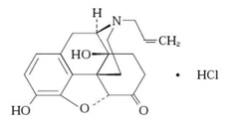
C 19H 21NO 4 HCl
363.8 g/mol
Naloxone hydrochloride occurs as a white to slightly off-white powder, and is soluble in water, in dilute acids, and in strong alkali; slightly soluble in alcohol; practically insoluble in ether and in chloroform.
Each 0.5 mL contains 5 mg naloxone hydrochloride (equivalent to 4.5 mg naloxone), 4.17 mg sodium chloride, hydrochloric acid to adjust pH, and water for injection.
12. CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Naloxone hydrochloride is an opioid antagonist that antagonizes opioid effects by competing for the same receptor sites.
Naloxone hydrochloride reverses the effects of opioids, including respiratory depression, sedation, and hypotension. Also, it can reverse the psychotomimetic and dysphoric effects of agonist-antagonists such as pentazocine.
12.2 Pharmacodynamics
When naloxone hydrochloride is administered intravenously, the onset of action is generally apparent within two minutes. The time to onset of action is shorter for intravenous compared to subcutaneous or intramuscular routes of administration.
The duration of action is dependent upon the dose and route of administration of naloxone hydrochloride.
12.3 Pharmacokinetics
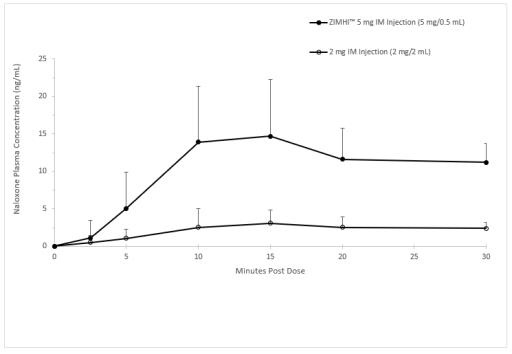
In a pharmacokinetic study of 14 healthy adults, a single intramuscular injection of 5 mg ZIMHI in a single-dose prefilled syringe in a delivery device provides significantly higher C max and AUC compared to a single intramuscular injection of 2 mg naloxone hydrochloride (1mg /1mL). Naloxone plasma concentration versus time profiles are shown in Figure 1.
The pharmacokinetic parameters of naloxone in plasma are shown in Table 1.
| Parameter | Intramuscular Injection of 5 mg ZIMHI
(N = 14) | Intramuscular Injection of 2 mg Naloxone HCl
(N = 14) |
| T max (h)* | 0.25 (0.17, 0.52) | 0.25 (0.05, 3.00) |
| C max (ng/mL) | 17.2 (44) | 3.58 (58.1) |
| AUC 0-t (ng.h/mL) | 26.2 (21.5) | 9.43 (23.8) |
| AUC 0-inf (ng.h/mL) | 26.6 (21.2) | 9.97 (22.6) |
| AUC 0-0.04h (ng.h/mL) | 0.02 (208) | 0.01 (164) |
| AUC 0-0.08h (ng.h/mL) | 0.15 (117) | 0.04 (128) |
| T 1/2 (h) | 1.50 (15.2) | 1.86 (28.9) |
*t max reported as median (minimum, maximum)
Figure 1 Mean ± SD Plasma Concentration of Naloxone, (a) 0-30 min and (b) 0-12 h Following a Single Intramuscular Administration of 5 mg ZIMHI and a Single Intramuscular Administration of 2 mg Naloxone HCl
a)
b)
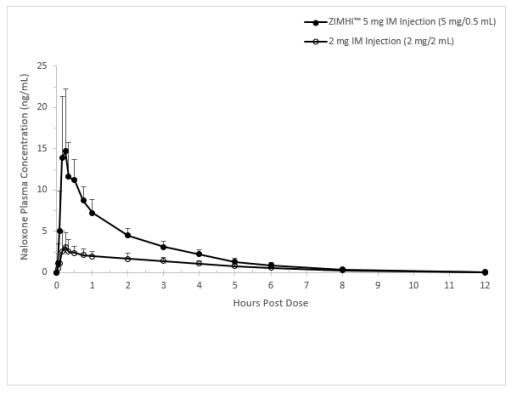
Distribution
Following parenteral administration, naloxone is distributed in the body and readily crosses the placenta. Plasma protein binding occurs but is relatively weak. Plasma albumin is the major binding constituent, but significant binding of naloxone also occurs to plasma constituents other than albumin. It is not known whether naloxone is excreted into human milk.
Elimination
Following a single intramuscular injection of 5 mg ZIMHI, the mean plasma half-life of naloxone in healthy adults was 1.50 (15.2% CV) hours with values for individual subjects ranging from 1.18 to 1.87 hours. In a neonatal study of naloxone injection, the mean (± SD) plasma half-life was observed to be 3.1 (± 0.5) hours.
Metabolism
Naloxone hydrochloride is metabolized in the liver, primarily by glucuronide conjugation with naloxone-3-glucoronide as the major metabolite.
Excretion
After an oral or intravenous dose, about 25-40% of naloxone is excreted as metabolites in urine within 6 hours, about 50% in 24 hours, and 60-70% in 72 hours.
13. NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Long-term animal studies to evaluate the carcinogenic potential of naloxone have not been completed.
Mutagenesis
Naloxone was weakly positive in the Ames mutagenicity and in the in vitro human lymphocyte chromosome aberration test but was negative in the in vitro Chinese hamster V79 cell HGPRT mutagenicity assay and in the in vivo rat bone marrow chromosome aberration study.
Impairment of Fertility
Reproduction studies conducted in mice and rats at doses 4-times and 8-times, respectively, the dose of 10 mg/day given to a 50 kg human (when based on surface area or mg/m 2), demonstrated no adverse effect of naloxone hydrochloride on fertility.
16. HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
ZIMHI (naloxone hydrochloride injection, USP) 5 mg/0.5 mL is a clear, colorless to slightly yellow, sterile solution provided as follows:
NDC38739-600-01: Case containing one 5 mg/0.5 mL single-dose, prefilled syringe
NDC38739-600-02: Carton containing two cases, each of which contain one 5 mg/0.5 mL single-dose, prefilled syringe per case
16.2 Storage and Handling
Store ZIMHI in the outer case provided.
Store at controlled room temperature 20°C to 25°C (68°F to 77°F), excursions between 15° and 30° (59° and 86° F) are allowed. Do not refrigerate. Protect from light, extreme heat, and freezing.
Prior to a medical emergency (during storage), periodically visually inspect ZIMHI through the viewing window on the device. If the solution is discolored yellow or brown color, cloudy, or contains particles, replace ZIMHI with a new one.
17. PATIENT COUNSELING INFORMATION
Advise the patient and family members or caregivers to read the FDA-approved patient labeling (Patient Information and Instructions for Use).
Instruct patients and their family members or caregivers to become familiar with all information contained in the case and carton as soon as they receive ZIMHI.
Inform patients of the following:
- ZIMHI is for the emergency treatment of known or suspected overdose.
- It is administered by a caregiver according to the Instructions for Use.
- After administration, the caregiver should get emergency help immediately.
Recognition of Opioid Overdose
Instruct the patients and their family members or caregivers how to recognize the signs and symptoms of an opioid overdose requiring the use of ZIMHI TM such as the following:
- Extreme somnolence - inability to awaken a patient verbally or upon a firm sternal rub.
- Respiratory depression - this can range from slow or shallow respiration to no respiration in a patient who is unarousable.
- Other signs and symptoms that may accompany somnolence and respiratory depression include the following:
- Miosis.
- Bradycardia and/or hypotension.
- Miosis.
Risk of Recurrent Respiratory and Central Nervous System Depression
Instruct patients and their family members or caregivers that, because the duration of action of most opioids may exceed that of ZIMHI, they must seek immediate emergency medical assistance after the first dose of ZIMHI and keep the patient under continued surveillance [ see Dosage and Administration (2.2), Warnings and Precautions (5.3)].
Limited Efficacy for/with Partial Agonists or Mixed Agonist/Antagonists
Instruct patients and their family members or caregivers that the reversal of respiratory depression caused by partial agonists or mixed agonist/antagonists such as buprenorphine and pentazocine, may be incomplete and may require higher doses of naloxone hydrochloride or repeated administration of ZIMHI [ see Dosage and Administration (2.2), Warnings and Precautions (5.3)].
Precipitation of Severe Opioid Withdrawal
Instruct patients and their family members or caregivers that the use of ZIMHI in patients who are opioid dependent may precipitate an acute abstinence syndrome characterized by the following signs and symptoms: body aches, diarrhea, tachycardia, fever, runny nose, sneezing, piloerection, sweating, yawning, nausea or vomiting, nervousness, restlessness or irritability, shivering or trembling, abdominal cramps, weakness, and increased blood pressure. In neonates, opioid withdrawal may be life threatening if not recognized and properly treated and may include the following signs and symptoms: convulsions, excessive crying, and hyperactive reflexes [ see Warnings and Precautions (5.3), Adverse Reactions (6)].
Administration Instructions
Instruct patients and their family members or caregivers to carefully read the Instructions for Use before an emergency arises. Emphasize the following important information:
-
ZIMHI is intended to be administered by individuals 12 years of age or older. Younger individuals or those with limited hand strength may find the device difficult to use.
- Each syringe is for a single-dose injection.
- Make sure ZIMHI is present whenever persons may be intentionally or accidentally exposed to an opioid to treat serious opioid overdose (i.e., opioid emergencies).
- Administer ZIMHI as quickly as possible if a patient is unresponsive and an opioid overdose is suspected, even when in doubt, because prolonged respiratory depression may result in damage to the central nervous system or death. ZIMHI is not a substitute for emergency medical care [
see Dosage and Administration (2.1)].
- Place the patient in the supine position.
- Inject ZIMHI into the anterolateral aspect of the thigh (through clothing, if necessary). Instruct patients to the correct location for injection.
- Immediately after injection, using one hand with fingers behind the needle, slide the safety guard over the needle. Do not use two hands to activate the Safety guard. Put the used syringe into the blue case and close the case.
-
Seek emergency medical care immediately following administration of ZIMHI.
- Place the patient in the lateral recumbent position (recovery position) as shown in the Instructions for Use.
- Additional supportive and/or resuscitative measures may be helpful while awaiting emergency medical assistance.
- Administer additional doses of ZIMHI every two to three minutes if the patient does not respond or relapses back into respiratory depression before emergency assistance arrives.
- If an accidental needlestick occurs seek medical attention immediately. Potential exposure to blood borne pathogens including HIV, HBV, and HCV requires immediate evaluation by a medical professional at an emergency room, urgent care, or your primary care provider. In addition, report accidental needle injury or device malfunction to Adamis Pharmacovigilance at (800) 230-3935.
- Complete patient information, including dosage, directions for proper administration, and precautions can be found inside each ZIMHI case or carton. A printed label on the surface of the ZIMHI case or carton shows instructions for use.
- During storage, periodically visually inspect the naloxone solution through the viewing window. If the solution is discolored yellow or brown color, cloudy or contains particles, replace ZIMHI with a new one.
- Replace ZIMHI before its expiration date.
Manufactured for Adamis Pharmaceuticals Corporation. San Diego, CA:
Alliance Medical Products, Inc.
Siegfried Irvine
9342 Jeronimo Road
Irvine, CA 92618
U.S.A.
Phillips Medisize LLC
428 Technology Drive East
Menomonie, Wisconsin 54751
U.S.A.
| PATIENT INFORMATION
ZIMHI TM (ZIM-hye) (naloxone hydrochloride injection) |
||
| You and your caregivers should read this Patient Information leaflet before an opioid emergency happens. This
information does not take the place of talking with your healthcare provider about your medical condition or your treatment. |
||
| What is the most important information I should know about ZIMHI?
ZIMHI is used to temporarily reverse the effects of opioid medicines. The medicine in ZIMHI has no effect in people who are not taking opioid medicines. Always carry ZIMHI with you in case of an opioid emergency.
|
||
What is ZIMHI?
|
||
| Who should not use ZIMHI?
Do not use ZIMHI if you are allergic to naloxone hydrochloride or any of the ingredients in ZIMHI. See the end of this leaflet for a complete list of ingredients in ZIMHI. |
||
| What should I tell my healthcare provider before using ZIMHI?
Before using ZIMHI, tell your healthcare provider about all of your medical conditions, including if you:
|
||
| How should I use ZIMHI?
Read the “Instructions for Use” at the end of this Patient Information leaflet for detailed information about the right way to use ZIMHI.
|
||
What are the possible side effects of ZIMHI? ZIMHI may cause serious side effects, including:
|
||
| ◦ body aches
◦ runny nose ◦ yawning ◦ nervousness ◦ nausea or vomiting ◦ increased heart rate | ◦ fever
◦ sneezing ◦ weakness ◦ restlessness or irritability ◦ stomach cramping | ◦ sweating
◦ goose bumps ◦ shivering or trembling ◦ diarrhea ◦ increased blood pressure |
| The most common side effects of ZIMHI include: nausea, dizziness, lightheadedness, and increased amounts of red blood cell breakdown products (bilirubin) in your blood.
In infants under 4 weeks old who have been receiving opioids regularly, sudden opioid withdrawal may be life-threatening if not treated the right way. Signs and symptoms include: seizures, crying more than usual and increased reflexes. These are not all of the possible side effects of ZIMHI. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. |
||
How should I store ZIMHI?
|
||
| General information about the safe and effective use of ZIMHI.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use ZIMHI for a condition for which it was not prescribed. You can ask your pharmacist or healthcare provider for information about ZIMHI that is written for health professionals. |
||
| What are the ingredients in ZIMHI? Active ingredient: naloxone hydrochloride
Inactive ingredients: sodium chloride, hydrochloric acid to adjust pH, and water for injection. ZIMHI is not made with natural rubber latex. ZIMHI is a registered trademark of Adamis Pharmaceuticals Corporation. Manufactured for Adamis Pharmaceuticals, San Diego, CA 92130, USA. For more information about ZIMHI prefilled syringe and proper use of the ZIMHI, call 1-800-230-3935 or visit www.ZIMHI.com. |
||
INSTRUCTIONS FOR USE
ZIMHITM (ZIM-hye)
(naloxone hydrochloride injection)
Prefilled syringe
Use ZIMHI for known or suspected opioid overdose in adults and children.
ZIMHI is intended to be administered by people 12 years of age or older. Younger children or those with limited hand strength may find the device difficult to use.
Read this Instructions for Use carefully before you use this product.
Before you need to use your ZIMHI syringe make sure your healthcare provider shows you the right way to use it. Parents, caregivers, and others who may be in a position to administer ZIMHI should also understand how to use it. If you have questions, ask your healthcare provider.
Get Ready to Use ZIMHI
ZIMHI works like a standard prefilled syringe.

ZIMHI is injected downwards, into the middle of the outer thigh, (as shown), through clothing if needed.

Ready to Use ZIMHI

Place the patient on their back.
When ready to inject, pull off cap to expose needle.

Do not put finger on top of the device.
In children under the age of 1 year old, pinch the thigh muscle while administering the dose.
Hold ZIMHI by finger grips only and slowly insert the needle into the thigh.
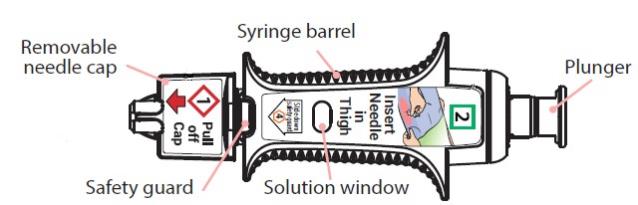

After needle is in thigh: Push the plunger all the way down until it clicks and hold for 2 seconds.


After Use
Right after the injection, using one hand with fingers behind the needle, slide the safety guard over the needle. Do not use two hands to activate the safety guard. Put the used syringe into the blue case and close the case.


Get Help
Get emergency medical help now

Tell healthcare provider that you gave an injection of naloxone hydrochloride. Turn the patient on their side (recovery position) after giving ZIMHI.

Use second syringe if needed

You may need a second ZIMHI syringe if symptoms continue or return.
If symptoms return after an injection with ZIMHI, an additional injection using another ZIMHI prefilled syringe may be needed. Give additional injections using a new ZIMHI prefilled syringe every 2 to 3 minutes and continue to closely watch the person until emergency help is received. Using ZIMHI does not take the place of emergency medical care.
After Use and Disposal
- ZIMHI is a single-dose prefilled syringe that delivers a fixed dose of naloxone hydrochloride. The prefilled syringe cannot be reused. It is normal for most of the medicine to remain in the syringe after the dose has been injected.
- The correct dose has been injected if the plunger has been pushed all the way down and the solution window is at least partially blocked.
- Tell the healthcare provider that you have received or administered an injection of naloxone hydrochloride. Show the healthcare provider where the injection was administered.
- Give your used ZIMHI syringe, contained in the blue case, to the healthcare provider for inspection and proper disposal.
For more information see Patient Information sheet or ask your healthcare provider.
How to Store — Keep ZIMHI in its plastic case nearby and ready for use at all times.
- Store at controlled room temperature, between 68°F to 77°F (20°C to 25°C). Do not expose to extreme cold or heat. For example,
do not store in your vehicle's glove box and
do not store in the refrigerator or freezer.
- Store the ZIMHI syringe in its closed plastic case to protect from light.
Check Your Stored ZIMHI Often - The solution should be clear when viewed through the window on the device. If the solution is discolored (yellowish or brown color), cloudy or contains particles, replace the ZIMHI with a new one.
Your ZIMHI Has an Expiration Date — Example YYYY-MM. Replace ZIMHI before the last day of expiration month. Dispose of expired ZIMHI properly by taking the ZIMHI in its case to a healthcare provider or hospital emergency room.
For more information about ZIMHI prefilled syringe and proper use of the ZIMHI, call 1-800-230-3935 or visit www.ZIMHI.com.
ZIMHI is a registered trademark of Adamis Pharmaceuticals Corporation. Manufactured for Adamis Pharmaceuticals, San Diego, CA 92130, USA.
This Instructions for Use has been approved by the U.S. Food and Drug Administration. Issued: October 2021
PRINCIPAL DISPLAY PANEL
NDC: 38739-600-02
Rx Only
ZIMHI
TM
(naloxone HCL Injection, USP)
5 mg/ 0.5 mL

| ZIMHI
naloxone hydrochloride injection, solution |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| Labeler - Adamis Pharmaceuticals (618661680) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Noramco | 157990263 | api manufacture(38739-600) | |
Trademark Results [ZIMHI]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 ZIMHI 88281598 not registered Live/Pending |
Adamis Pharmaceuticals Corporation 2019-01-29 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.