SANCUSO- granisetron patch
SANCUSO by
Drug Labeling and Warnings
SANCUSO by is a Prescription medication manufactured, distributed, or labeled by Kyowa Kirin, Inc., 3M Drug Delivery Systems. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use SANCUSO safely and effectively. See full prescribing information for SANCUSO.
SANCUSO (Granisetron Transdermal System)
Initial U.S. Approval: 2008INDICATIONS AND USAGE
Sancuso is a serotonin -3 (5-HT3) receptor antagonist indicated for the prevention of nausea and vomiting in patients receiving moderately and/or highly emetogenic chemotherapy for up to 5 consecutive days. (1)
DOSAGE AND ADMINISTRATION
Apply a single transdermal system (patch) to the upper outer arm a minimum of 24 hours before chemotherapy. The patch may be applied up to a maximum of 48 hours before chemotherapy as appropriate. Remove the patch a minimum of 24 hours after completion of chemotherapy. The patch can be worn for up to 7 days depending on the duration of the chemotherapy regimen. (2)
DOSAGE FORMS AND STRENGTHS
Transdermal System: 52 cm2 patch containing 34.3 mg of granisetron delivering 3.1 mg per 24 hours (3)
CONTRAINDICATIONS
Known hypersensitivity to granisetron or to any of the components of the patch (4)
WARNINGS AND PRECAUTIONS
- Granisetron may mask a progressive ileus and/or gastric distention caused by the underlying condition. (5.1)
- Serotonin syndrome has been reported with 5-HT3 receptor antagonists alone but particularly with concomitant use of serotonergic drugs. (5.2)
- Mild application site reactions have occurred; remove patch if severe reactions or a generalized skin reaction occur. (5.3)
- Avoid exposing the granisetron patch and surrounding area to direct external heat sources, such as heating pads (5.4).
- Avoid direct exposure of application site to natural or artificial sunlight by covering with clothing while wearing the patch and for 10 days after removing it. (5.5)
ADVERSE REACTIONS
The most common adverse reaction (incidence ≥ 3%) is constipation. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Kyowa Kirin, Inc. at 1-800-SANCUSO (1-800-726-2876) or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
No clinically relevant drug interactions have been reported in clinical studies with Sancuso. (7)
USE IN SPECIFIC POPULATIONS
- Pregnancy: Use only if clearly needed. (8.1)
- Nursing women: Caution should be exercised when administered to a nursing woman. (8.3)
- Pediatric use: Safety and effectiveness have not been established in pediatric patients. (8.4)
- Geriatric use: Clinical studies of Sancuso did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger patients (8.5)
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 1/2017
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Adults
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Gastrointestinal
5.2 Serotonin Syndrome
5.3 Skin Reactions
5.4 External Heat Sources
5.5 Exposure to Sunlight
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment or Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
13.3 Phototoxicity
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
17.1 Gastrointestinal
17.2 Skin Reactions
17.3 Exposure to Sunlight
17.4 Serotonin Syndrome
17.5 External Heat Sources
- * Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
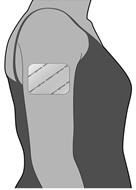
The transdermal system (patch) should be applied to clean, dry, intact healthy skin on the upper outer arm. Sancuso should not be placed on skin that is red, irritated, or damaged.
Each patch is packed in a pouch and should be applied directly after the pouch has been opened.
The patch should not be cut into pieces.
2.1 Adults
Apply a single patch to the upper outer arm a minimum of 24 hours before chemotherapy. The patch may be applied up to a maximum of 48 hours before chemotherapy as appropriate. Remove the patch a minimum of 24 hours after completion of chemotherapy. The patch can be worn for up to 7 days depending on the duration of the chemotherapy regimen.
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Gastrointestinal
The use of granisetron in patients may mask a progressive ileus and/or gastric distention caused by the underlying condition.
5.2 Serotonin Syndrome
The development of serotonin syndrome has been reported with 5-HT3 receptor antagonists. Most reports have been associated with concomitant use of serotonergic drugs (e.g., selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors (SNRIs), monoamine oxidase inhibitors, mirtazapine, fentanyl, lithium, tramadol, and intravenous methylene blue). Some of the reported cases were fatal. Serotonin syndrome occurring with overdose of another 5-HT3 receptor antagonist alone has also been reported. The majority of reports of serotonin syndrome related to 5-HT3 receptor antagonist use occurred in a post-anesthesia care unit or an infusion center.
Symptoms associated with serotonin syndrome may include the following combination of signs and symptoms: mental status changes (e.g., agitation, hallucinations, delirium, and coma), autonomic instability (e.g., tachycardia, labile blood pressure, dizziness, diaphoresis, flushing, hyperthermia), neuromuscular symptoms (e.g., tremor, rigidity, myoclonus, hyperreflexia, incoordination), seizures, with or without gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea). Patients should be monitored for the emergence of serotonin syndrome, especially with concomitant use of Sancuso and other serotonergic drugs. If symptoms of serotonin syndrome occur, discontinue Sancuso and initiate supportive treatment. Patients should be informed of the increased risk of serotonin syndrome, especially if Sancuso is used concomitantly with other serotonergic drugs. [see Drug Interactions (7), Patient Counseling Information (17.4)].
5.3 Skin Reactions
In clinical trials with Sancuso, application site reactions were reported that were generally mild in intensity and did not lead to discontinuation of use. The incidence of reactions was comparable with placebo.
If severe reactions, or a generalized skin reaction occur (e.g., allergic rash, including erythematous, macular, papular rash or pruritus), the patch must be removed.
5.4 External Heat Sources
A heat pad should not be applied over or in vicinity of Sancuso patch. Patients should avoid prolonged exposure to heat as plasma concentration continues increasing during the period of heat exposure [see Clinical Pharmacology (12.3)].
5.5 Exposure to Sunlight
Granisetron may be affected by direct natural or artificial sunlight. Patients must be advised to cover the patch application site, e.g. with clothing, if there is a risk of exposure to sunlight throughout the period of wear and for 10 days following its removal because of a potential skin reaction [see Nonclinical Toxicology (13.3)].
-
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
The safety of Sancuso was evaluated in a total of 404 patients undergoing chemotherapy who participated in two double-blind, comparator studies with patch treatment durations of up to 7 days. The control groups included a total of 406 patients who received a daily dose of 2 mg oral granisetron, for 1 to 5 days.
Adverse reactions occurred in 8.7% (35/404) of patients receiving Sancuso and 7.1% (29/406) of patients receiving oral granisetron. The most common adverse reaction was constipation that occurred in 5.4% of patients in the Sancuso group and 3.0% of patients in the oral granisetron group.
Table 1 lists the adverse reactions that occurred in at least 3% of patients treated with Sancuso or oral granisetron.
Table 1: Incidence of Adverse Reactions in Double-Blind, Active Comparator Controlled Studies in Cancer Patients Receiving Chemotherapy (Events ≥ 3% in either group) Body System
Preferred TermSancuso TDS
N=404
(%)Oral granisetron
N=406
(%)Gastrointestinal disorders Constipation 5.4 3.0 Nervous system disorders Headache 0.7 3.0 5-HT3 receptor antagonists, such as granisetron, may be associated with arrhythmias or ECG abnormalities. Three ECGs were performed on 588 patients in a randomized, parallel group, double-blind, double-dummy study: at baseline before treatment, the first day of chemotherapy, and 5 to 7 days after starting chemotherapy. QTcF prolongation greater than 450 milliseconds was seen in a total of 11 (1.9%) patients after receiving granisetron, 8 (2.7%) on oral granisetron, and 3 (1.1%) on the patch. No new QTcF prolongation greater than 480 milliseconds was observed in any patient in this study. No arrhythmias were detected in this study.
Adverse reactions reported in clinical trials with other formulations of granisetron include the following:
Gastrointestinal: abdominal pain, diarrhea, constipation, elevation of ALT and AST levels, nausea and vomiting
Cardiovascular: hypertension, hypotension, angina pectoris, atrial fibrillation and syncope have been observed rarely
Central Nervous System: dizziness, insomnia, headache, anxiety, somnolence and asthenia
Hypersensitivity: rare cases of hypersensitivity reactions, sometimes severe (e.g. anaphylaxis, shortness of breath, hypotension, urticaria) have been reported
Other: fever; events often associated with chemotherapy have also been reported: leucopenia, decreased appetite, anemia, alopecia, thrombocytopenia.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post approval use of Sancuso. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
General Disorders and Administration Site Conditions: Application site reactions (pain, pruritus, erythema, rash, irritation, vesicles, burn, discoloration, urticaria); patch non-adhesion.
Cardiac Disorders: bradycardia, chest pain, palpitations, sick sinus syndrome
-
7 DRUG INTERACTIONS
Granisetron does not induce or inhibit the cytochrome P-450 drug-metabolizing enzyme system in vitro. There have been no definitive drug-drug interaction studies to examine pharmacokinetic or pharmacodynamic interaction with other drugs. However, in humans, granisetron hydrochloride injection has been safely administered with drugs representing benzodiazepines, neuroleptics and anti-ulcer medications commonly prescribed with antiemetic treatments. Granisetron hydrochloride injection also does not appear to interact with emetogenic cancer therapies. In agreement with these data, no clinically relevant drug interactions have been reported in clinical studies with Sancuso.
Because granisetron is metabolized by hepatic cytochrome P-450 drug-metabolizing enzymes (CYP1A1 and CYP3A4), inducers or inhibitors of these enzymes may change the clearance and hence, the half-life of granisetron. In addition, the activity of the cytochrome P-450 subfamily 3A4 (involved in the metabolism of some of the main narcotic analgesic agents) is not modified by granisetron hydrochloride in vitro. In in vitro human microsomal studies, ketoconazole inhibited ring oxidation of granisetron hydrochloride. However, the clinical significance of in vivo pharmacokinetic interactions with ketoconazole is not known. In a human pharmacokinetic study, hepatic enzyme induction with phenobarbital resulted in a 25% increase in total plasma clearance of intravenous granisetron hydrochloride. The clinical significance of this change is not known.
Serotonin syndrome (including altered mental status, autonomic instability, and neuromuscular symptoms) has been described following the concomitant use of 5-HT3 receptor antagonists and other serotonergic drugs, including selective serotonin reuptake inhibitors (SSRIs) and serotonin and noradrenaline reuptake inhibitors (SNRIs) [see Warnings and Precautions (5.4)].
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category B
Reproduction studies with granisetron hydrochloride have been performed in pregnant rats at intravenous doses up to 9 mg/kg/day (54 mg/m2/day, about 24 times the recommended human dose delivered by the Sancuso patch, based on body surface area) and oral doses up to 125 mg/kg/day (750 mg/m2/day, about 326 times the recommended human dose with Sancuso based on body surface area). Reproduction studies have been performed in pregnant rabbits at intravenous doses up to 3 mg/kg/day (36 mg/m2/day, about 16 times the human dose with Sancuso based on body surface area) and at oral doses up to 32 mg/kg/day (384 mg/m2/day, about 167 times the human dose with Sancuso based on body surface area). These studies did not reveal any evidence of impaired fertility or harm to the fetus due to granisetron. There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, Sancuso should be used during pregnancy only if clearly needed.
8.3 Nursing Mothers
It is not known whether granisetron is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when Sancuso is administered to a nursing woman.
8.4 Pediatric Use
Safety and effectiveness of Sancuso have not been established in pediatric patients.
8.5 Geriatric Use
Clinical studies of Sancuso did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, cautious treatment selection for an elderly patient is prudent because of the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
8.6 Renal Impairment or Hepatic Impairment
Although no studies have been performed to investigate the pharmacokinetics of Sancuso in patients with renal or hepatic impairment, pharmacokinetic information is available for intravenous granisetron [see Clinical Pharmacology (12.3)].
-
10 OVERDOSAGE
There is no specific antidote for granisetron overdosage. In the case of overdosage, symptomatic treatment should be given.
Overdosage of up to 38.5 mg of granisetron hydrochloride, as a single intravenous injection, has been reported without symptoms or only the occurrence of a slight headache.
In clinical trials there were no reported cases of overdosage with Sancuso.
-
11 DESCRIPTION
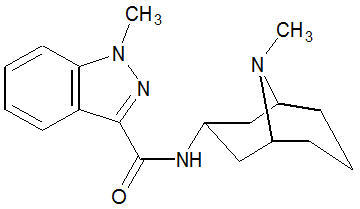
Sancuso contains granisetron, which is a serotonin-3 (5-HT3) receptor antagonist. Chemically it is 1-methyl-N-[(1R,3r,5S)-9-methyl-9-azabicyclo[3.3.1]non-3-yl]-1H-indazole-3-carboxamide with a molecular weight of 312.4. Its empirical formula is C18H24N4O, while its chemical structure is:
Granisetron Granisetron is a white to off-white solid that is insoluble in water. Sancuso is a thin, translucent, matrix-type transdermal patch that is rectangular-shaped with rounded corners, consisting of a backing, the drug matrix and a release liner.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Granisetron is a selective 5-hydroxytryptamine3 (5-HT3) receptor antagonist with little or no affinity for other serotonin receptors, including 5-HT1, 5-HT1A, 5-HT1B/C, 5-HT2; for alpha1-, alpha2-, or beta-adrenoreceptors; for dopamine-D2; or for histamine-H1; benzodiazepine; picrotoxin or opioid receptors.
Serotonin receptors of the 5-HT3 type are located peripherally on vagal nerve terminals and centrally in the chemoreceptor trigger zone of the area postrema. During chemotherapy that induces vomiting, mucosal enterochromaffin cells release serotonin, which stimulates 5-HT3 receptors. This evokes vagal afferent discharge, inducing vomiting. Animal studies demonstrate that, in binding to 5-HT3 receptors, granisetron blocks serotonin stimulation and subsequent vomiting after emetogenic stimuli such as cisplatin. In the ferret animal model, a single granisetron injection prevented vomiting due to high-dose cisplatin or arrested vomiting within 5 to 30 seconds.
12.2 Pharmacodynamics
The effect of granisetron on QTc prolongation was evaluated in a randomized, single-blind, positive (moxifloxacin 400 mg) - and placebo controlled parallel study in healthy subjects. A total of 120 subjects were administered Sancuso patch (n=60) or intravenous granisetron (10 mcg/kg over 30 seconds; n=60). In a study with demonstrated ability to detect small effects, the upper bound of the 90% confidence interval for the largest placebo adjusted, baseline corrected QTc based on Fridericia correction method (QTcF) for Sancuso was below 10 ms. This study suggests that Sancuso does not have significant effects on QT prolongation.
No evidence of an effect on plasma prolactin or aldosterone concentrations has been found in studies using granisetron.
The effect on oro-cecal transit time following application of Sancuso has not been studied. Granisetron hydrochloride injection exhibited no effect on oro-cecal transit time in healthy subjects given a single intravenous infusion of 50 mcg/kg or 200 mcg/kg. Single and multiple oral doses of granisetron hydrochloride slowed colonic transit in healthy subjects.
12.3 Pharmacokinetics
Absorption
Granisetron crosses intact skin into the systemic circulation by a passive diffusion process.
Following a 7-day application of Sancuso in 24 healthy subjects, high inter-subject variability in systemic exposure was observed. Maximal concentration was reached at approximately 48 hours (range: 24-168 hours) following patch application. Mean Cmax was 5.0 ng/mL (CV: 170%) and mean AUC0-168hr was 527 ng-hr/mL (CV: 173%).
Mean Plasma Concentration of Granisetron (mean ± SD) 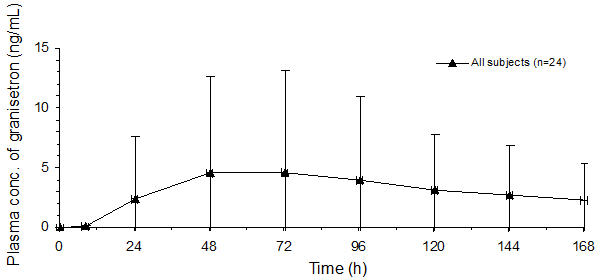
Based on the measure of residual content of the patch after removal, approximately 66% (SD: ± 10.9) of granisetron is delivered following patch application for 7 days.
Following consecutive application of two Sancuso patches, each for seven days, granisetron levels were maintained over the study period with evidence of minimal accumulation. The mean plasma concentration at 24 hours after the second patch application was 1.5-fold higher due to residual granisetron from the first patch. As the plasma concentration increased after the second patch application, the difference decreased and the mean plasma concentration at 48 hours was 1.3-fold higher after the second patch compared to that after the first patch.
In a study designed to assess the effect of heat on the transdermal delivery of granisetron from Sancuso in healthy subjects, a heat pad generating an average temperature of 42°C (107.6°F) was applied over the patch for 4 hours each day over the 5 day period of wear. The application of the heat pad was associated with an increase in plasma granisetron concentrations during the period of heat pad application. The elevated plasma concentration declined after removal of the heat pad. Mean Cmax with intermittent heat exposure was 6% higher than without heat. Mean partial AUCs over 6 hours with 4 hour of heat application (AUC0-6, AUC24-30, and AUC48-54) were 4.9, 1.4, and 1.1 folds higher, respectively, with heat pad than without heat pad. A heat pad should not be applied over or in the near vicinity of the Sancuso patch.
Distribution
Plasma protein binding is approximately 65%. Granisetron distributes freely between plasma and red blood cells.
Metabolism
Granisetron metabolism involves N-demethylation and aromatic ring oxidation followed by conjugation. In vitro liver microsomal studies show that granisetron's major route of metabolism is inhibited by ketoconazole, suggestive of metabolism mediated by the cytochrome P-450 3A subfamily. Animal studies suggest that some of the metabolites may also have 5-HT3 receptor antagonist activity.
Elimination
Clearance is predominantly by hepatic metabolism. Based on a study with intravenous injection, approximately 12% of the dose is excreted unchanged in the urine of healthy subjects in 48 hours. The remainder of the dose is excreted as metabolites, 49% in the urine, and 34% in the feces.
Subpopulations
Gender
There is evidence to suggest that female subjects had higher granisetron concentrations than males following patch application. However, no statistically significant difference in clinical efficacy outcome was observed between genders.
Pediatrics
No studies have been performed to investigate the pharmacokinetics of Sancuso in pediatrics.
Elderly
Following application of Sancuso patch in healthy subjects, mean AUC0-z, Cmax, and Cavg were 17%, 15%, and 16% higher, respectively in male and female elderly subjects (≥ 65 years) compared to younger subjects (aged 18-45 years inclusive). These pharmacokinetic parameters were largely overlapped between the two age groups with high variability (CV: >50%).
Following a single 40 mcg/kg intravenous dose of granisetron hydrochloride in elderly volunteers (mean age 71 years), lower clearance and longer half-life were observed compared to younger healthy volunteers.
Renal Impairment
Total clearance of granisetron was not affected in patients with severe renal failure who received a single 40 mcg/kg intravenous dose of granisetron hydrochloride.
Hepatic Impairment
In patients with hepatic impairment due to neoplastic liver involvement, total plasma clearance following a single 40 mcg/kg intravenous dose of granisetron hydrochloride was approximately halved compared to patients without hepatic impairment. Given the wide variability in pharmacokinetic parameters of granisetron and the good tolerance of doses well above the recommended dose, dose adjustment in patients with hepatic functional impairment is not necessary.
Body Mass Index
In a clinical study designed to assess granisetron exposure from Sancuso in subjects with differing levels of body fat, using body mass index (BMI) as a surrogate measure for subcutaneous fat, no significant differences were seen in the plasma pharmacokinetics of Sancuso in male and female subjects with low BMI [<19.5 kg/m2 (males), <18.5 kg/m2 (females)] and high BMI (30.0 to 39.9 kg/m2 inclusive) compared to a control group (BMI 20.0 to 24.9 kg/m2 inclusive).
Race
The pharmacokinetic profile of granisetron from Sancuso was assessed in healthy Japanese males. Following the application of a single 6-day Sancuso 52 cm2, in healthy male Japanese subjects, mean Cmax, AUC(0-144), and AUC(0-∞) values were 5.02 ng/mL (CV: 66%), 492 ng.hr/mL (CV: 72%), and 562 ng.hr/mL (CV: 60%), respectively, and a median tmax value was 48 hours.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
In a 24-month carcinogenicity study, rats were treated orally with granisetron 1, 5 or 50 mg/kg/day (6, 30 or 300 mg/m2/day). The 50 mg/kg/day dose was reduced to 25 mg/kg/day (150 mg/m2/day) during week 59 due to toxicity. For a 50 kg person of average height (1.46 m2 body surface area), these doses represent about 2.6, 13, and 65 times the recommended clinical dose (3.1 mg/day, 2.3 mg/m2/day, delivered by the Sancuso patch, on a body surface area basis). There was a statistically significant increase in the incidence of hepatocellular carcinomas and adenomas in males treated with 5 mg/kg/day (30 mg/m2/day, about 13 times the recommended human dose with Sancuso, on a body surface area basis) and above, and in females treated with 25 mg/kg/day (150 mg/m2/day, about 65 times the recommended human dose with Sancuso, on a body surface area basis). No increase in liver tumors was observed at a dose of 1 mg/kg/day (6 mg/m2/day, about 2.6 times the recommended human dose with Sancuso, on a body surface area basis) in males and 5 mg/kg/day (30 mg/m2/day, about 13 times the recommended human dose with Sancuso, on a body surface area basis) in females.
In a 12-month oral toxicity study, treatment with granisetron 100 mg/kg/day (600 mg/m2/day, about 261 times the recommended human dose with Sancuso, on a body surface area basis) produced hepatocellular adenomas in male and female rats while no such tumors were found in the control rats. A 24-month mouse carcinogenicity study of granisetron did not show a statistically significant increase in tumor incidence, but the study was not conclusive.
Because of the tumor findings in rat studies, Sancuso should be prescribed only at the dose and for the indication recommended [see Indications and Usage (1) and Dosage and Administration (2)].
Granisetron was not mutagenic in an in vitro Ames test and mouse lymphoma cell forward mutation assay, and in vivo mouse micronucleus test and in vitro and ex vivo rat hepatocyte UDS assays. It, however, produced a significant increase in UDS in HeLa cells in vitro and a significant increased incidence of cells with polyploidy in an in vitro human lymphocyte chromosomal aberration test.
Granisetron at subcutaneous doses up to 6 mg/kg/day (36 mg/m2/day, about 16 times the recommended human dose of Sancuso, on a body surface area basis), and oral doses up to 100 mg/kg/day (600 mg/m2/day, about 261 times the recommended human dose of Sancuso, on a body surface area basis) was found to have no effect on fertility and reproductive performance of male and female rats.
13.3 Phototoxicity
When tested for potential photogenotoxicity in vitro in a Chinese hamster ovary (CHO) cell line, at 200 and 300 mcg/mL, granisetron increased the percentage of cells with chromosomal aberration following photoirradiation.
Granisetron was not phototoxic when tested in vitro in a mouse fibroblast cell line. When tested in vivo in guinea-pigs, Sancuso patches did not show any potential for photoirritation or photosensitivity. No phototoxicity studies have been performed in humans.
-
14 CLINICAL STUDIES
The effectiveness of Sancuso in the prevention of chemotherapy-induced nausea and vomiting (CINV) was evaluated in a randomized, parallel group, double-blind, double-dummy study conducted in the U.S. and abroad. The study compared the efficacy, tolerability and safety of Sancuso with that of 2 mg oral granisetron once daily in the prevention of nausea and vomiting in a total of 641 patients receiving multi-day chemotherapy.
The population randomized into the trial included 48% males and 52% females aged 16 to 86 years receiving moderately emetogenic (ME) or highly emetogenic (HE) multi-day chemotherapy. Seventy-eight (78%) of patients were White, 12% Asian, 10% Hispanic/Latino and 0% Black.
The granisetron patch was applied 24 to 48 hours before the first dose of chemotherapy, and kept in place for 7 days. Oral granisetron was administered daily for the duration of the chemotherapy regimen, 1 hour before each dose of chemotherapy. Efficacy was assessed from the first administration until 24 hours after the start of the last day's administration of the chemotherapy regimen.
The primary endpoint of the trial was the proportion of patients achieving no vomiting and/or retching, no more than mild nausea and no rescue medication from the first administration until 24 hours after the start of the last day's administration of multi-day chemotherapy. Using this definition, the effect of Sancuso was established in 60.2% of patients in the Sancuso arm and 64.8% of patients receiving oral granisetron (difference -4.89%; 95% confidence interval –12.91% to +3.13%).
An assessment of patch adhesion in 621 patients receiving either active or placebo patches showed that less than 1% of patches became detached over the course of the 7 day period of patch application.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
Sancuso (Granisetron Transdermal System) is supplied as a 52 cm2 patch containing 34.3 mg of granisetron. Each patch is printed on one side with the words "Granisetron 3.1 mg/24 hours". Each patch is packaged in a separate sealed foil-lined plastic pouch.
Sancuso is available in packages of 1 (NDC: 42747-726-01) patch.
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information)
17.1 Gastrointestinal
Because the use of granisetron may mask a progressive ileus and/or gastric distention caused by the underlying condition, patients should be instructed to tell their physician if they have pain or swelling in their abdomen.
17.2 Skin Reactions
Patients should be instructed to remove the patch if they have a severe skin reaction, or a generalized skin reaction (e.g. allergic rash, including erythematous, macular, papular rash or pruritus).
When patients remove the patch, they should be instructed to peel it off gently.
17.3 Exposure to Sunlight
Granisetron may be degraded by direct sunlight or exposure to sunlamps. In addition, an in vitro study using Chinese hamster ovary cells suggests that granisetron has the potential for photogenotoxicity [see Nonclinical Toxicology (13.3)].
Patients must be advised to cover the patch application site, e.g. with clothing, if there is a risk of exposure to sunlight or sunlamps throughout the period of wear and for 10 days following its removal.
17.4 Serotonin Syndrome
Advise patients of the possibility of serotonin syndrome with concomitant use of Sancuso and another serotonergic agent such as medications to treat depression and migraines. Advise patients to seek immediate medical attention if the following symptoms occur: changes in mental status, autonomic instability, neuromuscular symptoms, with or without gastrointestinal symptoms.
- SPL UNCLASSIFIED SECTION
-
Patient Information
Sancuso® [san-KOO-so]
(granisetron transdermal system)IMPORTANT: For skin use only Read the Patient Information that comes with Sancuso before you start using it and each time you get a refill. There may be new information. This information does not take the place of talking to your healthcare provider about your medical condition or your treatment. If you have any questions about Sancuso, ask your healthcare provider.
What is Sancuso?
Sancuso is a prescription medicine used to prevent nausea and vomiting in people receiving some types of chemotherapy treatment. Sancuso is a skin patch that slowly releases the medicine contained in the adhesive (glue), through clean and intact skin areas into your bloodstream while you wear the patch.
Important: Sancuso contains granisetron, the same medicine in Kytril. Do not take Kytril at the same time you use Sancuso unless your healthcare provider tells you it is alright. 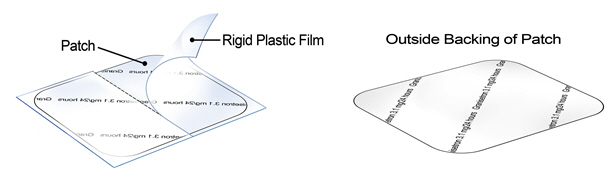
Who should not use Sancuso?
Do not use Sancuso if you are allergic to any of the ingredients in Sancuso. See the end of this leaflet for a list of ingredients in Sancuso.
What should I tell my healthcare provider before using Sancuso?
Tell your healthcare provider about all your medical conditions, including if you:
- are allergic to medical adhesive tape, adhesive dressings or other skin patches
- have pain or swelling in your stomach area (abdomen).
- are pregnant. It is not known if Sancuso will harm your unborn baby. Talk to your healthcare provider if you are pregnant or plan to become pregnant.
- are breast-feeding or plan to breast-feed. It is not known if Sancuso passes into your breast milk.
Tell your healthcare provider about all the medicines you take, including prescription and non-prescription medicines, vitamins and herbal supplements. Other medicines may affect how Sancuso works. Sancuso may also affect how other medicines work.
How should Sancuso be used?
Use Sancuso exactly as prescribed. See the detailed Patient Instructions for Applying Sancuso at the end of this Patient Information leaflet.
What should I avoid while using Sancuso?
Do not apply any heat source over or near the Sancuso patch. For example,
- A heating pad or heat lamp should not be used where the patch is applied.
- You should avoid extended exposure to heat as it may increase your blood levels during the time of heat exposure.
Avoid sunlight. The medicine in Sancuso (granisetron) may not work as well and/or may affect your skin if exposed to direct sunlight or the light from sunlamps or tanning beds. It is important to do the following:
- While you wear the patch, keep it covered with clothing if you will be in sunlight or near a sunlamp, including tanning beds.
- Keep the skin where Sancuso was applied covered for another 10 days after the patch is taken off to protect from exposure to direct sunlight.
What are the possible side effects of Sancuso?
Sancuso can cause serious side effects:
- Using Sancuso may make it harder to identify certain stomach and bowel problems that are from other causes. Tell your healthcare provider if you have any stomach area (abdominal) pain or swelling while using Sancuso.
- Skin reactions. Skin reactions can happen just at the patch application site or outside the patch application site. Tell your healthcare provider if you get any redness, rashes, bumps, blisters or itching at the patch application site, and especially if they spread outside the place where the patch was or if they appear outside the patch application site. You may need to stop using Sancuso.
Common side effects of Sancuso are:
- constipation
- headache.
Tell your healthcare provider if you have any side effect that bothers you or that does not go away. These are not all the possible side effects of Sancuso. For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store Sancuso?
- Keep Sancuso in the package it comes in.
- Store Sancuso at 20-25°C (68-77°F).
Keep Sancuso out of the reach of children.
General information about Sancuso
Medicines are sometimes prescribed for conditions that are not mentioned in Patient Information leaflets. Do not use Sancuso for a condition for which it is not prescribed. Do not give Sancuso to other people, even if they have the same symptoms you have. It may harm them.
This Patient Information leaflet summarizes the most important information about Sancuso. If you would like more information, talk to your healthcare provider. You can ask your pharmacist or healthcare provider for information about Sancuso that is written for health professionals.
For more information, go to www.sancuso.com or call 1-800-SANCUSO.
Patient Instructions for Applying Sancuso
When do I apply the Sancuso patch?
- Apply Sancuso at least 1 day (24 hours) before your scheduled chemotherapy treatment.
- You may apply Sancuso up to 2 days (48 hours) before your scheduled chemotherapy.
- Wear the patch all the time during your chemotherapy.
- Sancuso may be worn for up to 7 days, depending on how long your chemotherapy treatment lasts (up to 5 days).
- Remove the patch at least 1 day (24 hours) after your chemotherapy is finished.
- Keep the patch covered, such as under clothing, while you are wearing it to avoid a skin reaction to sunlight or sunlamps. Keep the skin where Sancuso was applied (application site) covered up for another 10 days after the patch is taken off to prevent a skin reaction. See "What should I avoid while using Sancuso?"
Where do I apply the Sancuso patch?
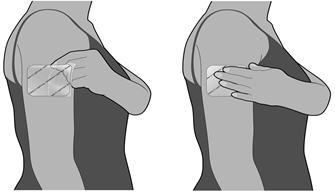
- Apply Sancuso to a clean, dry, healthy area of skin on the outside part of your upper arm.
- The area you choose should not be oily, recently shaved or have any skin problems such as being damaged (cut or scraped) or irritated (redness or a rash).
- Do not apply Sancuso to areas that have been treated with creams, oils, lotions, powders or other skin products that could keep the patch from sticking well to your skin.
How do I apply the Sancuso patch?
The Sancuso patch comes inside a pouch which is inside the carton.
- 1. Do not remove the patch from the pouch until you are ready to use it.
- 2. Do not cut the Sancuso patch into pieces.
- 3.
Remove the pouch from the carton.
- 4.
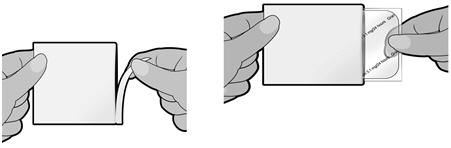
Tear the pouch open using the slit provided, and remove the patch. Each pouch contains one Sancuso patch stuck onto a rigid plastic film.
- 5.
The unprinted, sticky side of the patch is covered by a two-piece rigid plastic film. Bend the patch in the middle and remove one half of the rigid plastic film. Be careful not to stick the patch to itself and avoid touching the sticky side of the patch.

- 6.
While holding the remaining half of the rigid plastic film, apply the patch to your skin. Remove the second half of the rigid plastic film and press the whole patch firmly in place with your fingers and smooth down. Press firmly making sure it sticks well to the skin, especially around the edges.
- 7. Wash your hands right away after applying the patch to remove any medicine that may have stuck to your fingers.
- 8. Keep the patch in place for the whole time you are having chemotherapy. Remove the patch at least 1 day (24 hours) after your chemotherapy is finished. The patch can be worn for up to 7 days, depending on the number of days your chemotherapy treatment lasts.
- 9. Do not re-use the patch after you remove it. See below for instructions on the right way to remove and throw away the patch.
What to do if the Sancuso patch does not stick well?
If the patch does not stick well, you may use surgical bandages or medical adhesive tape to keep the patch in place. Place tape or bandages on the edges of the patch. Do not completely cover the patch with bandages or tape and do not wrap completely around your arm. If the patch comes more than half off or it becomes damaged see your healthcare provider.
Can I bathe or shower while wearing Sancuso?
You can continue to shower and wash normally while wearing the Sancuso patch. It is not known how other activities, for example swimming, strenuous exercise or using a sauna or whirlpool, may affect Sancuso. Avoid these activities while wearing Sancuso.
How do I remove and dispose of Sancuso?
- When you remove the patch, peel it off gently.
- The used patch will still contain some of the medicine. After removing the used Sancuso patch, fold it in half so that the sticky side sticks to itself. Throw away the Sancuso patch in the garbage, out of the reach of children and pets. Do not re-use the patch.
- After removing the patch you may find some adhesive is left on your skin. Gently wash the area with soap and water to remove it. Do not use alcohol or other dissolving liquids, such as nail polish remover. These may cause skin irritation.
- Wash your hands after handling the patch.
- You may see mild redness on the skin where the patch is removed. This redness should go away within three days. If redness continues, tell your healthcare provider.
What are the ingredients in Sancuso?
Active ingredient: granisetron.
Inactive ingredients: acrylate-vinylacetate copolymer, polyester, titanium dioxide, polyamide resin and polyethylene wax.Manufactured by:
3M Drug Delivery Systems, St. Paul, MN 55107Manufactured for:
Kyowa Kirin, Inc., Bedminster, NJ 07921Copyright © 2017 Kyowa Kirin, Inc. All rights reserved.
Sancuso and Kyowa Kirin are trademarks owned by the Kyowa Kirin group of companies
Revised: 09/2017
-
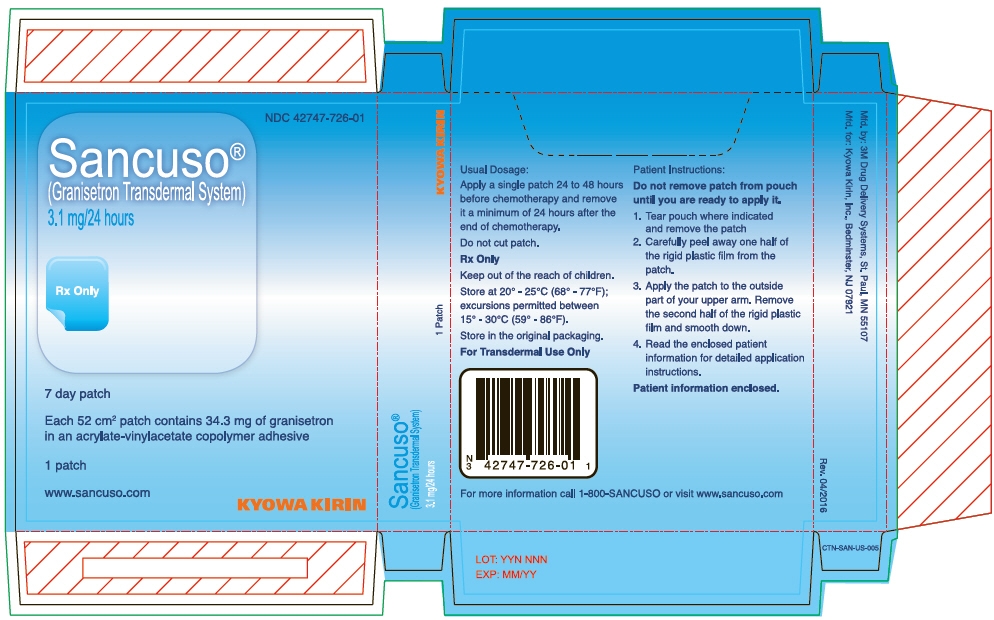
PRINCIPAL DISPLAY PANEL - 3.1 mg Patch Pouch Carton
NDC: 42747-726-01
Sancuso®
(Granisetron Transdermal System)
3.1 mg/24 hoursRx Only
7 day patch
Each 52 cm2 patch contains 34.3 mg of granisetron
in an acrylate-vinylacetate copolymer adhesive1 patch
www.sancuso.com
KYOWA KIRIN
-
INGREDIENTS AND APPEARANCE
SANCUSO
granisetron patchProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 42747-726 Route of Administration TRANSDERMAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength GRANISETRON (UNII: WZG3J2MCOL) (GRANISETRON - UNII:WZG3J2MCOL) GRANISETRON 3.1 mg in 24 h Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 42747-726-01 1 in 1 CARTON 09/12/2008 1 1 in 1 POUCH 1 168 h in 1 PATCH; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA022198 09/12/2008 Labeler - Kyowa Kirin, Inc. (014778321) Establishment Name Address ID/FEI Business Operations 3M Delivery Systems 830016361 MANUFACTURE(42747-726) , PACK(42747-726) , ANALYSIS(42747-726)
Trademark Results [SANCUSO]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 SANCUSO 79064017 3744866 Live/Registered |
Kyowa Kirin, Inc. 2008-12-19 |
 SANCUSO 76460343 2814630 Live/Registered |
STRAKAN INTERNATIONAL S.A. 2002-10-17 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.