IMOVAX RABIES (rabies virus strain pm-1503-3m antigen- propiolactone inactivated and water kit
IMOVAX RABIES by
Drug Labeling and Warnings
IMOVAX RABIES by is a Other medication manufactured, distributed, or labeled by Sanofi Pasteur Inc., Sanofi Pasteur, Sanofi Winthrop Industrie. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
- SPL UNCLASSIFIED SECTION
-
DESCRIPTION
The Imovax® Rabies Vaccine produced by Sanofi Pasteur SA is a sterile, stable, freeze-dried suspension of rabies virus prepared from strain PM-1503-3M obtained from the Wistar Institute, Philadelphia, PA.
The virus is harvested from infected human diploid cells, MRC-5 strain, concentrated by ultrafiltration and is inactivated by beta-propiolactone. One dose of reconstituted vaccine contains less than 100 mg human albumin, less than 150 mcg neomycin sulfate and 20 mcg of phenol red indicator. Beta-propiolactone, a residual component of the manufacturing process, is present in less than 50 parts per million.
The finished, freeze-dried vaccine is provided for intramuscular administration in a single dose vial containing no preservative. After reconstitution, immediately administer the full 1.0 mL amount of vaccine. If it cannot be administered promptly, discard.
The potency of one dose (1.0 mL) of Imovax Rabies vaccine is equal to or greater than 2.5 international units of rabies antigen.
-
CLINICAL PHARMACOLOGY
Pre-exposure immunization
High titer antibody responses to the Imovax Rabies vaccine made in human diploid cells have been demonstrated in trials conducted in England (1), Germany (2) (3), France (4) and Belgium. (5) Seroconversion was often obtained with only one dose. With two doses one month apart, 100% of the recipients developed specific antibody, and the geometric mean titer of the group was approximately 10 international units. In the US, Imovax Rabies vaccine resulted in geometric mean titers (GMT) of 12.9 IU/mL at Day 49 and 5.1 IU/mL at Day 90 when three doses were given intramuscularly during the course of one month. The range of antibody responses was 2.8 to 55.0 IU/mL at Day 49 and 1.8 to 12.4 IU at Day 90. (6) The definition of a minimally accepted antibody titer varies among laboratories and is influenced by the type of test conducted. CDC currently specifies a 1:5 titer (complete inhibition) by the rapid fluorescent focus inhibition test (RFFIT) as acceptable. The World Health Organization (WHO) specifies a titer of 0.5 IU.
Post-exposure immunization
Post-exposure efficacy of Imovax Rabies vaccine was successfully proven during clinical experience in Iran in which six 1.0 mL doses were given on days 0, 3, 7, 14, 30, and 90, in conjunction with antirabies serum. Forty-five persons severely bitten by rabid dogs and wolves received Imovax Rabies vaccine within hours of and up to 14 days after the bites. All individuals were fully protected against rabies. (7)
Studies conducted by the United States Centers for Disease Control and Prevention (CDC) have shown that a regimen of 1 dose of Rabies Immune Globulin (RIG) and 5 doses of HDCV induced an excellent antibody response in all recipients. Of 511 persons bitten by proven rabid animals and so treated, none developed rabies. (8)
Do not inject Imovax Rabies vaccine in the gluteal area as there have been reports of possible vaccine failure when the vaccine has been administered in this area. Presumably, subcutaneous fat in the gluteal area may interfere with the immune response to human diploid cell rabies vaccine (HDCV). (9) (10)
For adults and older children, Imovax Rabies vaccine should be administered in the deltoid muscle. For infants and younger children, the anterolateral aspect of the thigh is also acceptable, depending on age and body mass (see DOSAGE AND ADMINISTRATION).
-
INDICATIONS AND USAGE
Imovax Rabies is a vaccine indicated for pre-exposure and post-exposure prophylaxis against rabies. Imovax Rabies vaccine is approved for use in all age groups.
1. Rationale of treatment
Physicians must evaluate each possible rabies exposure. Local or state public health officials should be consulted if questions arise about the need for prophylaxis. (11)
The following factors should be considered before antirabies prophylaxis is initiated.
Species of biting animal
Bats
Rabid bats have been documented in the 49 continental states, and bats are increasingly implicated as important wildlife reservoirs for variants of rabies virus transmitted to humans. Transmission of rabies virus can occur from minor, seemingly underappreciated or unrecognized bites from bats (see Table 2). (11)
Wild Terrestrial Carnivores
Raccoons, skunks, and foxes are the terrestrial carnivores most often infected with rabies in the United States. Suggestive clinical signs of rabies among wildlife cannot be interpreted reliably. All bites by such wildlife should be considered possible exposures to rabies virus. Post-exposure prophylaxis should be initiated as soon as possible following exposure to such wildlife, unless the animal is available for diagnosis and public health authorities are facilitating expeditious laboratory testing, or if the brain tissue from the animal has already tested negative (see Table 2). (11)
Other Wild Animals
Small rodents (eg, squirrels, chipmunks, rats, mice, hamsters, guinea pigs, and gerbils) and lagomorphs (including rabbits and hares) are rarely infected with rabies and have not been known to transmit rabies to humans. In all cases involving rodents, the state or local health department should be consulted before a decision is made to initiate post-exposure prophylaxis (see Table 2). (11)
Domestic Dogs, Cats, and Ferrets
The likelihood of rabies in a domestic animal varies regionally, and the need for post-exposure prophylaxis also varies on the basis of regional epidemiology (see Table 2). (11)
Circumstances of biting incident
An unprovoked attack might be more likely than a provoked attack to indicate the animal is rabid. Bites inflicted on a person attempting to feed or handle an apparently healthy animal should generally be regarded as provoked. Consult the local or state health department following a provoked or unprovoked exposure to determine the best course of action based on current public health recommendations.
Type of exposure
Rabies is transmitted by introducing the virus into open cuts or wounds in skin or via mucous membranes. The likelihood of rabies infection varies with the nature and extent of exposure. Two categories of exposure should be considered, bite and nonbite.
Nonbite
Scratches, abrasions, open wounds, or mucous membranes contaminated with saliva or other potentially infectious material, such as brain tissue, from a rabid animal. Casual contact, such as petting a rabid animal, (without a bite or nonbite exposure as described above), does not constitute an exposure and is not an indication for prophylaxis. Rare reports of airborne rabies have been received from laboratory and bat-infested cave settings. (11)
Rare cases of rabies from human-to-human transmission have occurred in patients in the US and overseas who received organs transplanted from persons who died of rabies undiagnosed at the time of death. No documented laboratory-diagnosed cases of human-to-human rabies transmission have been documented from a bite or nonbite exposure other than the transplant cases. At least two cases of human-to-human rabies transmission in Ethiopia have been suggested, but rabies as the cause of death was not confirmed by laboratory testing. The reported route of exposure in both cases was direct salivary contact from another human (ie, a bite and a kiss). Routine delivery of health care to a patient with rabies is not an indication for post-exposure prophylaxis unless the healthcare worker is reasonably certain that he or she was bitten by the patient or that his or her mucous membranes or nonintact skin was exposed directly to potentially infectious saliva or neural tissue. (11)
2. Pre- and post-exposure prophylaxis of rabies
A. Pre-exposure
Pre-exposure immunization should be offered to rabies researchers, certain laboratory workers and other persons in high-risk groups, such as veterinarians and their staff, and animal handlers. Pre-exposure vaccination also should be considered for persons whose activities bring them into frequent contact with rabies virus or potentially rabid bats, raccoons, skunks, cats, dogs, or other species at risk for having rabies. In addition, some international travelers might be candidates for pre-exposure vaccination if they are likely to come in contact with animals in areas where dog or other animal rabies is enzootic and immediate access to appropriate medical care, including rabies vaccine and immune globulin, might be limited. (11)
Vaccination is recommended for children living in or visiting countries where exposure to rabid animals is a constant threat. Worldwide statistics indicate children are more at risk than adults.
Pre-exposure prophylaxis is administered for several reasons. First, although pre-exposure vaccination does not eliminate the need for additional medical evaluation after a rabies exposure, it simplifies management by eliminating the need for Rabies Immune Globulin (RIG) and decreases the number of doses of vaccine needed. This is particularly important for persons at high risk for being exposed to rabies in areas where modern immunizing products might not be available or where cruder, less safe biologics might be used, placing the exposed person at increased risk for adverse events. Second, pre-exposure prophylaxis might offer partial immunity to persons whose post-exposure prophylaxis is delayed. Finally, pre-exposure prophylaxis might provide some protection to persons at risk for unrecognized exposures to rabies. (11)
PRE-EXPOSURE RABIES PROPHYLAXIS GUIDE
Pre-exposure prophylaxis consists of three 1.0 mL doses of Imovax Rabies vaccine administered intramuscularly, using a sterile needle and syringe, one injection per day on Days 0, 7, and 21 or 28. In adults and older children, the vaccine should be administered in the deltoid muscle. In infants and small children, the anterolateral aspect of the thigh may be preferable, depending on age and body mass.
Administration of booster doses of vaccine depends on exposure risk category and serologic testing as noted in Table 1.
Immunosuppressed persons should postpone pre-exposure vaccinations and consider avoiding activities for which rabies pre-exposure prophylaxis is indicated. When this course is not possible, immunosuppressed persons who are at risk for rabies should have their viral neutralizing antibody titers checked after completing the pre-exposure series. If no acceptable antibody response is detected, the patient should be managed in consultation with their physician and appropriate public health officials. (11)
Table 1: Rabies Pre-exposure Prophylaxis Guide (11) Risk category Nature of risk Typical populations Pre-exposure recommendations - * Minimum acceptable antibody level is complete virus neutralization at a 1:5 serum dilution by the rapid fluorescent focus inhibition test. A booster dose should be administered if the titer falls below this level.
Continuous Virus present continuously and often in high concentrations. Specific exposures likely to go unrecognized. Bite, nonbite, or aerosol exposure. Rabies research laboratory workers; rabies biologics production workers. Primary course.
Serologic testing every 6 months; booster vaccination if antibody titer is below acceptable level.*Frequent Exposure usually episodic, with source recognized, but exposure also might be unrecognized. Bite, nonbite, or aerosol exposure. Rabies diagnostic laboratory workers, cavers, veterinarians and staff, and animal-control and wildlife workers in areas where rabies is enzootic. All persons who frequently handle bats. Primary course.
Serologic testing every 2 years; booster vaccination if antibody titer is below acceptable level.*Infrequent (greater than population at large) Exposure nearly always episodic with source recognized. Bite or nonbite exposure. Veterinarians and animal-control staff working with terrestrial animals in areas where rabies is uncommon to rare. Veterinary students. Travelers visiting areas where rabies is enzootic and immediate access to appropriate medical care including biologics is limited. Primary course.
No serologic testing or booster vaccination.Rare (population at large) Exposure always episodic with source recognized. Bite or nonbite exposure. US population at large, including persons in areas where rabies is epizootic. No vaccination necessary. B. Post-exposure
The essential components of rabies post-exposure prophylaxis are wound treatment and, for previously unvaccinated persons, the administration of both human rabies immune globulin (RIG) and vaccine. (11)
1. Local treatment of wounds
Thorough washing and flushing (for about 15 minutes, if possible) with soap or a cleansing agent and copious amounts of water of all bite wounds and scratches should be done immediately or as early as possible. Where available, an iodine-containing, or similarly viricidal, topical preparation should be applied to the wound. (12)
Tetanus prophylaxis and measures to control bacterial infection should be given as indicated.
2. Specific treatment
The sooner treatment is begun after exposure, the better. Post-exposure antirabies vaccination should always include administration of both passive antibody and vaccine, with the exception of persons who have ever previously received complete vaccination regimens (pre-exposure or post-exposure) with a cell culture vaccine or persons who have been vaccinated with other types of vaccines and have previously had a documented rabies virus neutralizing antibody titer. These persons should receive only vaccine (ie, post-exposure for a person previously vaccinated). The combination of RIG and vaccine is recommended for both bite and nonbite exposures reported by persons who have never been previously vaccinated for rabies, regardless of the interval between exposure and initiation of prophylaxis. If post-exposure prophylaxis has been initiated and appropriate laboratory diagnostic testing (ie, the direct fluorescent antibody test) indicates that the exposing animal was not rabid, post-exposure prophylaxis can be discontinued. (11)
3. Treatment outside the United States
If post-exposure is begun outside the United States with locally produced biologics, it may be desirable to provide additional treatment when the patient reaches the US. State or local health departments should be contacted for specific advice in such cases. (11)
POST-EXPOSURE RABIES PROPHYLAXIS GUIDE
The following recommendations are only a guide. In applying them, take into account the animal species involved, the circumstances of the bite or other exposure, the vaccination status of the animal, the availability of the exposing animal for observation or rabies testing, and the presence of rabies in the region (see Table 2). Local or state public health officials should be consulted if questions arise about the need for rabies prophylaxis. (11)
Table 2: Post-exposure Treatments Guide (11) Animal type Evaluation and disposition of animal Post-exposure prophylaxis recommendations - * During the 10-day observation period, begin post-exposure prophylaxis at the first sign of rabies in a dog, cat, or ferret that has bitten someone. If the animal exhibits clinical signs of rabies, it should be euthanized immediately and tested.
- † Post-exposure prophylaxis should be initiated as soon as possible following exposure to such wildlife unless the animal is available for testing and public health authorities are facilitating expeditous laboratory testing or it is already known that brain material from the animal has tested negative. Other factors that might influence the urgency of decision-making regarding initiation of post-exposure prophylaxis before diagnostic results are known include the species of the animal, the general appearance and behavior of the animal, whether the encounter was provoked by the presence of a human, and the severity and location of bites. Discontinue vaccine if appropriate laboratory diagnostic test (ie, the direct fluorescent antibody test) is negative.
- ‡ The animal should be euthanized and tested as soon as possible. Holding for observation is not recommended.
Dogs, cats, and ferrets Healthy and available for 10 days observation. Persons should not begin prophylaxis unless animal develops clinical signs of rabies.* Rabid or suspected rabid. Immediately begin prophylaxis. Unknown (eg, escaped). Consult public health officials. Skunks, raccoons, foxes, and most other carnivores; bats† Regard as rabid unless animal proven negative by laboratory tests.‡ Consider immediate prophylaxis. Livestock, small rodents (rabbits and hares), large rodents (woodchucks and beavers), and other mammals Consider individually. Consult public health officials. Bites from squirrels, hamsters, guinea pigs, gerbils, chipmunks, rats, mice, other small rodents, rabbits, and hares almost never require anti-rabies post-exposure prophylaxis. -
CONTRAINDICATIONS
Pre-exposure Prophylaxis
Do not administer to anyone with a known life-threatening systemic hypersensitivity reaction to any component of the vaccine (see WARNINGS, PRECAUTIONS, and DESCRIPTION sections).
-
WARNINGS
- Do not inject the vaccine into the gluteal area as administration in this area may result in lower neutralizing antibody titers. (11)
- The product is provided in a single dose vial. Because the single dose vial contains no preservative, it is not to be used as a multidose vial for intradermal injection.
- In both pre-exposure and post-exposure immunization, the full 1.0 mL dose should be given intramuscularly.
- Serum sickness type reactions have been reported in persons receiving booster doses of rabies vaccine for pre-exposure prophylaxis. The reaction is characterized by onset approximately 2 to 21 days post-booster, presents with a generalized urticaria, and may also include arthralgia, arthritis, angioedema, nausea, vomiting, fever, and malaise. None of the reported reactions were life-threatening. This has been reported in up to 7% of persons receiving booster vaccination. (13)
- Rare cases of neurologic illness resembling Guillain-Barré syndrome, (14) (15) a transient neuroparalytic illness, that resolved without sequelae in 12 weeks and a focal subacute central nervous system disorder temporally associated with HDCV, have been reported. (16)
- This product contains albumin, a derivative of human blood. Based on effective donor screening and product manufacturing processes, it carries an extremely remote risk for transmission of viral diseases and variant Creutzfeldt-Jakob disease (vCJD). There is a theoretical risk for transmission of Creutzfeldt-Jakob disease (CJD), but if that risk actually exists, the risk of transmission would also be considered extremely remote. No cases of transmission of viral diseases, CJD, or vCJD have ever been identified for licensed albumin or albumin contained in other licensed products.
All serious systemic neuroparalytic or anaphylactic reactions to a rabies vaccine should be immediately reported to VAERS at 1-800-822-7967 (http://vaers.hhs.gov) or Sanofi Pasteur Inc., 1-800-VACCINE (1-800-822-2463).
- Vaccination with Imovax Rabies vaccine may not protect 100% of vaccinated individuals.
-
PRECAUTIONS
- IN ADULTS AND CHILDREN THE VACCINE SHOULD BE INJECTED INTO THE DELTOID MUSCLE. IN INFANTS AND SMALL CHILDREN, THE ANTEROLATERAL ASPECT OF THE THIGH MAY BE PREFERABLE.
- When a person with a history of hypersensitivity must be given rabies vaccine, antihistamines may be given. Epinephrine (1:1000) and other appropriate agents should be readily available to counteract anaphylactic reactions, and the person should be carefully observed after immunization.
- While the concentration of antibiotics in each dose of vaccine is extremely small, persons with known hypersensitivity to any of these agents, or any other component of the vaccine, could manifest an allergic reaction. While the risk is small, it should be weighed in light of the potential risk of contracting rabies.
DRUG INTERACTIONS
Corticosteroids, other immunosuppressive agents or treatments, and immunosuppressive illnesses can interfere with the development of active immunity and predispose the patient to developing rabies. Immunosuppressive agents should not be administered during post-exposure therapy, unless essential for the treatment of other conditions. When rabies post-exposure prophylaxis is administered to persons receiving steroids or other immunosuppressive therapy, it is especially important that serum be tested for rabies antibody to ensure that an adequate response has developed. (11)
USAGE IN PREGNANCY
Pre-exposure
Animal reproduction studies have not been conducted with Imovax Rabies vaccine. It is also not known whether Imovax Rabies vaccine can cause fetal harm when administered to a pregnant woman or can affect reproductive capacity. Imovax Rabies vaccine should be given to a pregnant woman only if potential benefits outweigh potential risks. If there is substantial risk of exposure to rabies, pre-exposure prophylaxis may also be indicated during pregnancy. (11)
-
ADVERSE REACTIONS
- Once initiated, rabies prophylaxis should not be interrupted or discontinued because of local or mild systemic adverse reactions to rabies vaccine. Usually such reactions can be successfully managed with anti-inflammatory, antihistaminic, and antipyretic agents. (11)
- Reactions after vaccination with HDCV have been observed. (13) In a study using five doses of HDCV, local reactions such as pain, erythema, swelling or itching at the injection site were reported in about 25% of recipients of HDCV, and mild systemic reactions such as headache, nausea, abdominal pain, muscle aches, and dizziness were reported in about 20% of recipients. (8)
- Serious systemic anaphylactic or neuroparalytic reactions occurring during the administration of rabies vaccines pose a dilemma for the attending physician. A patient's risk of developing rabies must be carefully considered before deciding to discontinue vaccination. Moreover, the use of corticosteroids to treat life-threatening neuroparalytic reactions carries the risk of inhibiting the development of active immunity to rabies. It is especially important in these cases that the serum of the patient be tested for rabies antibodies. Advice and assistance on the management of serious adverse reactions in persons receiving rabies vaccines may be sought from the local or state health department. (8)
- SEE WARNINGS AND CONTRAINDICATIONS SECTIONS FOR ADDITIONAL STATEMENTS.
Data from post-marketing experience
The following additional adverse events have been identified during postapproval use of Imovax Rabies vaccine. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to Imovax Rabies vaccine exposure.
Blood and Lymphatic System Disorders
- Lymphadenopathy
Immune System Disorders
- Anaphylactic reaction, serum sickness type reaction, dermatitis allergic, pruritus (itching), edema
Nervous System Disorders
- Paresthesia, neuropathy, convulsion, encephalitis
Gastrointestinal Disorders
- Vomiting, diarrhea
Musculoskeletal and Connective Tissue Disorders
- Arthralgia
General Disorders and Administration Site Conditions
- Asthenia, malaise, fever and chills (shivering), injection site hematoma
Respiratory, Thoracic, and Mediastinal Disorders
- Wheezing, dyspnea
-
DOSAGE AND ADMINISTRATION
The package contains a vial of freeze-dried vaccine, a Luer-Lok™ syringe containing 1.0 mL of diluent with a plunger rod either inserted into the syringe or provided separately, and a sterile reconstitution needle. The syringe and its package should be inspected prior to use for evidence of leakage, premature activation of the plunger rod, or a faulty tip seal. If evidence of such defects is observed, the product should not be used.
Instructions for vaccine reconstitution
Luer-Lok™ syringe components (with plunger rod inserted)
Step 1: Remove plastic cover from the vial. Cleanse the vial stopper with a suitable germicide. Do not remove the stopper or the metal seal holding it in place.
Step 2: Screw the plunger rod into the syringe, if it is provided separately.
Step 3: Hold the syringe cap in one hand (avoid holding the plunger rod or syringe barrel), and unscrew the tip cap by twisting it counterclockwise. 
Step 4: Attach the reconstitution needle to the syringe, by gently twisting the needle clockwise into the syringe until slight resistance is felt. 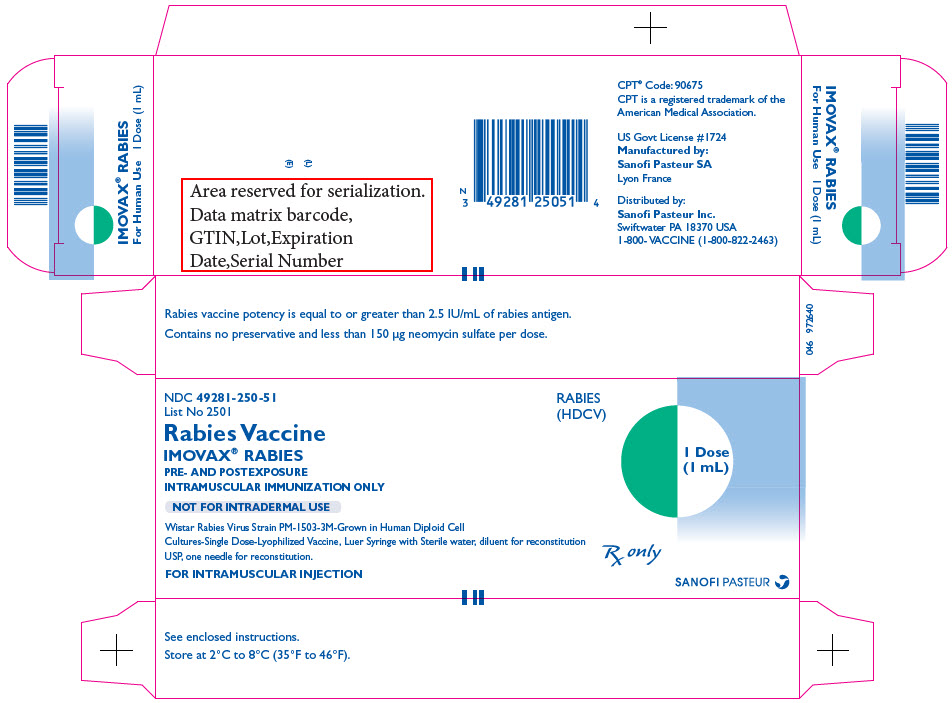
Step 5: Reconstitute the freeze-dried vaccine by injecting the diluent from the syringe into the vial. While the syringe and reconstitution needle are still attached, gently swirl the contents of the vial until completely dissolved and proceed to Step 6.
Step 6: Prior to withdrawing vial contents and without removing the reconstitution needle from the vial, unscrew the syringe to eliminate negative pressure (as the vial is sealed under vacuum). Reattach the syringe to the reconstitution needle which has remained in the vial.
Step 7: Withdraw the total contents of the vial into the syringe. Remove the reconstitution needle and discard it.
Step 8: Attach a new sterile needle (as per step 4) of a proper length and gauge suitable for intramuscular injection.
The supplied syringe is intended for single use only, must not be reused, and must be disposed of properly and promptly following its use.
To help avoid transmission of infectious diseases due to accidental needle sticks, needles should not be recapped but disposed of according to recommended guidelines.
The reconstituted vaccine should not be mixed with any other vaccine and should be used immediately.
Vaccine administration
Parenteral drug products should be inspected for particulate matter and discoloration prior to administration, whenever solution and container permit. If evidence of such defects is observed, the product should not be used.
After preparation of the injection site with an appropriate germicide, immediately inject the vaccine intramuscularly. For adults and older children, the vaccine should be injected into the deltoid muscle. (10) (18) (19) In infants and small children, the anterolateral aspect of the thigh may be preferable, depending on age and body mass. Care should be taken to avoid injection into or near blood vessels and nerves. If blood or any suspicious discoloration appears in the syringe, do not inject but discard contents and repeat procedure using a new dose of vaccine at a different site.
The gluteal area should not be used for administration of the vaccine as administration in this area may result in lower neutralizing antibody titers. (11)
NOTE: The freeze-dried vaccine is creamy white to orange. After reconstitution, it is pink to red.
Dosage schedules
A. Pre-exposure dosage
1. Primary vaccination
In the United States, the Advisory Committee on Immunization Practices (ACIP) recommends three injections of 1.0 mL each, one injection on Day 0, one on Day 7, and one either on Day 21 or 28. (11)
2. Booster dose
A booster dose consists of one injection of 1.0 mL of Imovax Rabies vaccine. To ensure the presence of a primed immune response over time among persons at higher than normal risk for exposure, titers should be checked periodically, with booster doses administered only as needed. Persons working with live rabies virus in research laboratories and in vaccine production facilities (continuous risk category) should have rabies antibody titers checked every six months and boosters given as needed to maintain an adequate titer defined as virus neutralization at a 1:5 dilution by a RFFIT. Other laboratory workers (eg, those performing rabies diagnostic testing), cavers, veterinarians and staff, animal-control and wildlife officers in areas where rabies is enzootic, and bat handlers regardless of location, (frequent risk category), should have their serum tested for rabies antibody every 2 years. If their titer is inadequate, they should receive a single booster dose of vaccine. Veterinarians, veterinary students, and terrestrial animal-control and wildlife officers, working in areas of low rabies endemicity (infrequent risk category) and certain at-risk international travelers who have completed a full pre-exposure vaccination series with licensed vaccines and according to schedule do not require routine booster serologic verification of detectable antibody titers or routine pre-exposure booster doses of vaccine (see Table 1). (11)
Persons who have experienced "immune complex-like" hypersensitivity reactions should receive no further doses of Imovax Rabies vaccine unless they are exposed to rabies or they are truly likely to be inapparently and/or unavoidably exposed to rabies virus and have unsatisfactory antibody titers.
B. Post-exposure dosage
1. Post-exposure dosage for previously unimmunized persons
Dose
Previously unvaccinated persons should receive 5 intramuscular doses (1 mL each) of Imovax Rabies vaccine, one dose immediately after exposure (Day 0) and one dose 3, 7, 14, and 28 days later.
RIG
Rabies immune globulin (RIG) 20 IU/kg on Day 0 in conjunction with the first vaccine dose. If possible, the full calculated dose of RIG should be used to infiltrate the wound(s). If it is not possible to do so, any remaining portion of the dose should be administered intramuscularly at a site different from the site used to administer the vaccine.
Because the antibody response following the recommended vaccination regimen with HDCV has been satisfactory, routine post-vaccination serologic testing is not recommended. Serologic testing is indicated in unusual circumstances, as when the patient is known to be immunosuppressed. Contact local or state health department or CDC for recommendations. (11)
2. Post-exposure dosage for previously immunized persons
When an immunized person who was vaccinated using the recommended pre-exposure regimen or a prior post-exposure regimen with a cell culture vaccine or who had previously demonstrated rabies antibody is exposed to rabies, that person should receive two intramuscular doses (1.0 mL each) of Imovax Rabies vaccine, one dose immediately after the exposure and one dose 3 days later. RIG should not be given in these cases.
If the immune status of a previously vaccinated person who did not receive the recommended HDCV regimen is not known, full primary post-exposure antirabies treatment (RIG plus 5 doses of HDCV) may be necessary. In such cases, if antibody levels of greater than 1:5 dilution by a RFFIT can be demonstrated in a serum sample collected before vaccine is given, treatment can be discontinued after at least two doses of HDCV. (20)
-
HOW SUPPLIED
Imovax Rabies vaccine is supplied in a tamper evident unit dose box with:
- - One vial of freeze-dried vaccine containing a single dose (NDC: 49281-248-58 or 49281-246-58).
- - One sterile syringe containing diluent (NDC: 49281-249-01 or 49281-263-58). If not already inserted into the syringe, a separate plunger rod is provided.
- - One sterile disposable needle for reconstitution.
Packaged as NDC: 49281-250-51 or 49281-252-51.
-
REFERENCES
- 1 Aoki FY, Tyrell DAJ, Hill LE. Immunogenicity and acceptability of a human diploid cell culture rabies vaccine in volunteers. The Lancet. 1975 Mar 22;1(7908):660-2.
- 2 Cox JH, Schneider LG. Prophylactic immunization of humans against rabies by intradermal inoculation of human diploid cell culture vaccine. J Clin Microbiol. 1976 Feb;3(2):96-101.
- 3 Kuwert EK, Marcus I, Werner J, Iwand A, Thraenhart O. Some experiences with human diploid cell strain—(HDCS) rabies vaccine in pre- and postexposure vaccinated humans. Dev Biol Stand. 1978;40:79-88.
- 4 Ajjan N, Soulebot J-P, Stellmann C, Biron G, Charbonnier C, Triau R, Mérieux C. Résultats de la vaccination antirabique préventive par le vaccin inactivé concentré souche rabies PM/W138-1503-3M cultivés sur cellules diploïdes humaines. Dev Biol Stand. 1978;40:89-100.
- 5 Costy-Berger F. Vaccination antirabique préventive par du vaccin préparé sur cellules diploïdes humaines. Dev Biol Stand. 1978;40:101-4.
- 6 Bernard KW, Roberts MA, Sumner J, Winkler WG, Mallonee J, Baer GM, Chaney R. Human diploid cell rabies vaccine. JAMA. 1982 Feb 26;247(8):1138-42.
- 7 Bahmanyar M, Fayaz A, Nour-Salehi S, Mohammadi M, Koprowski H. Successful protection of humans exposed to rabies infection. JAMA. 1976 Dec 13;236(24):2751-4.
- 8 CDC. Recommendations of the Advisory Committee on Immunization Practices (ACIP). Rabies Prevention--United States, 1984. MMWR. 1984 Jul 20;33(28):393-402, 407-8.
- 9 Shill M, Baynes RD, Miller SD. Fatal rabies encephalitis despite appropriate postexposure prophylaxis. N Engl J Med. 1987 May 14;316(20):1257-58.
- 10 CDC. Human rabies despite treatment with rabies immune globulin and human diploid cell rabies vaccine - Thailand. MMWR. 1987 Nov 27;36(46):759-60, 765.
- 11 Manning SE, Rupprecht CE, Fishbein D, Hanlon CA, Lumlertdacha B, Guerra M, et al. Human rabies prevention - United States 2008: recommendations of the Advisory Committee on Immunization Practices. MMWR. 2008 May 23;57(RR-3):1-28.
- 12 Rabies vaccines: WHO position paper. Weekly epidemiological record. 2010 Aug 6;85(32):309-320. Available from: http://www.who.int/wer.
- 13 CDC. Systemic allergic reactions following immunization with human diploid cell rabies vaccine. MMWR. 1984 Apr 13;33(14):185-7.
- 14 Boe E, Nyland H. Guillain-Barré syndrome after vaccination with human diploid cell rabies vaccine. Scand J Infect Dis. 1980;12(3):231-2.
- 15 CDC. Adverse reactions to human diploid cell rabies vaccine. MMWR. 1980;29:609-10.
- 16 Bernard KW, Smith PW, Kader FJ, Moran MJ. Neuroparalytic illness and human diploid cell rabies vaccine. JAMA. 1982 Dec 17;248(23):3136-8.
- 17 Varner MW, McGuinness GA, Galask RP. Rabies vaccination in pregnancy. Am J of Obstet Gynecol. 1982 Jul 15;143(6):717-8.
- 18 Cockshott WP, Thompson GT, Howlett LJ, Seely ET. Intramuscular or intralipomatous injections? N Eng J Med. 1982 Aug 5;307(6):356-8.
- 19 Baer GM, Fishbein DB. Rabies postexposure prophylaxis. N Engl J Med. 1987;316:1270-72.
- 20 CDC. Recommendations of the Advisory Committee on Immunization Practices. Human rabies prevention-United States, 1999. MMWR. 1999;48(RR-1):1-21.
- SPL UNCLASSIFIED SECTION
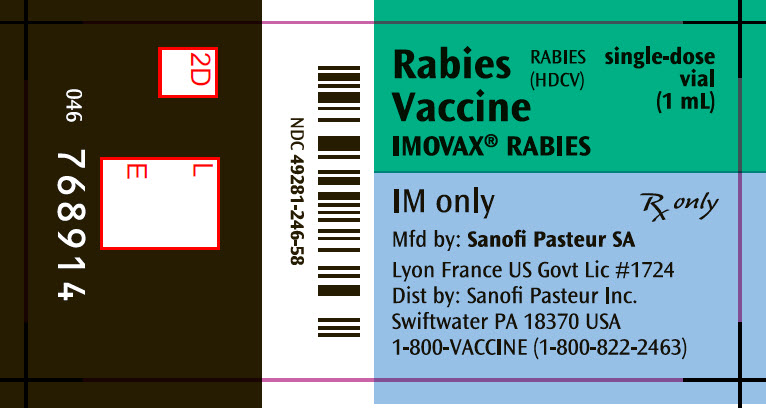
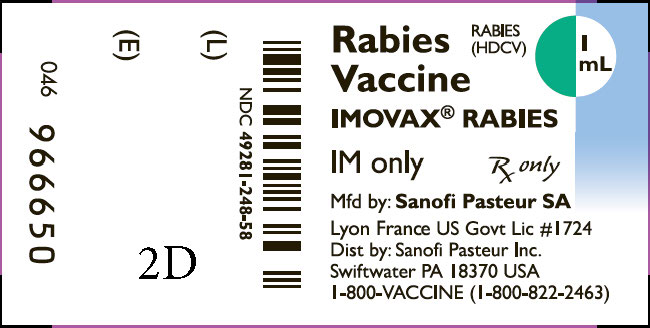
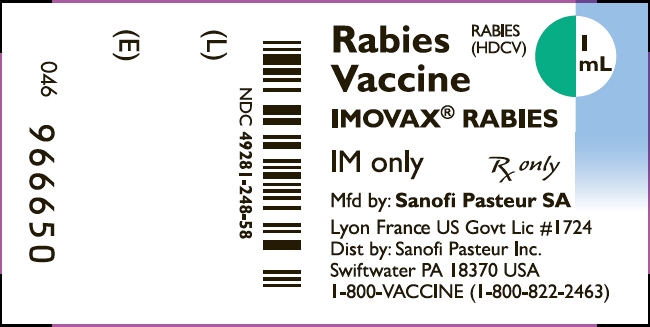
- PRINCIPAL DISPLAY PANEL - 1 mL Vial Label
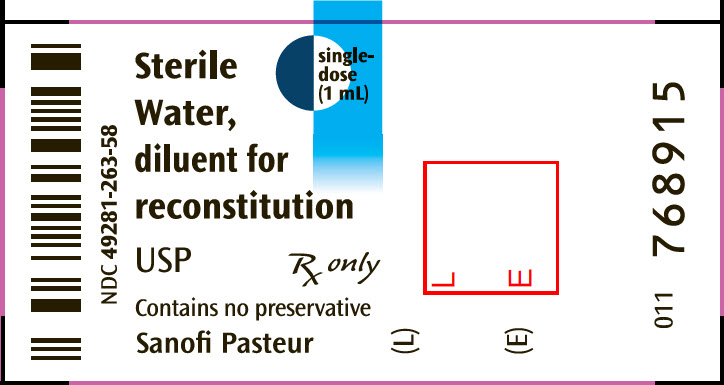
- PRINCIPAL DISPLAY PANEL - 1 mL Syringe Label
-
PRINCIPAL DISPLAY PANEL - Kit Carton
NDC: 49281-252-51
List No 2501RABIES
(HDCV)Rabies Vaccine
IMOVAX® RABIES
PRE- AND POSTEXPOSURE
INTRAMUSCULAR IMMUNIZATION ONLYsingle-dose
(1 mL)NOT FOR INTRADERMAL USE
Wistar Rabies Virus Strain PM-1503-3M-Grown in Human Diploid Cell
Cultures-Single Dose-Lyophilized Vaccine, Luer Syringe with Sterile water, diluent for reconstitution
USP, one needle for reconstitution.Rx only
FOR INTRAMUSCULAR INJECTION
SANOFI PASTEUR
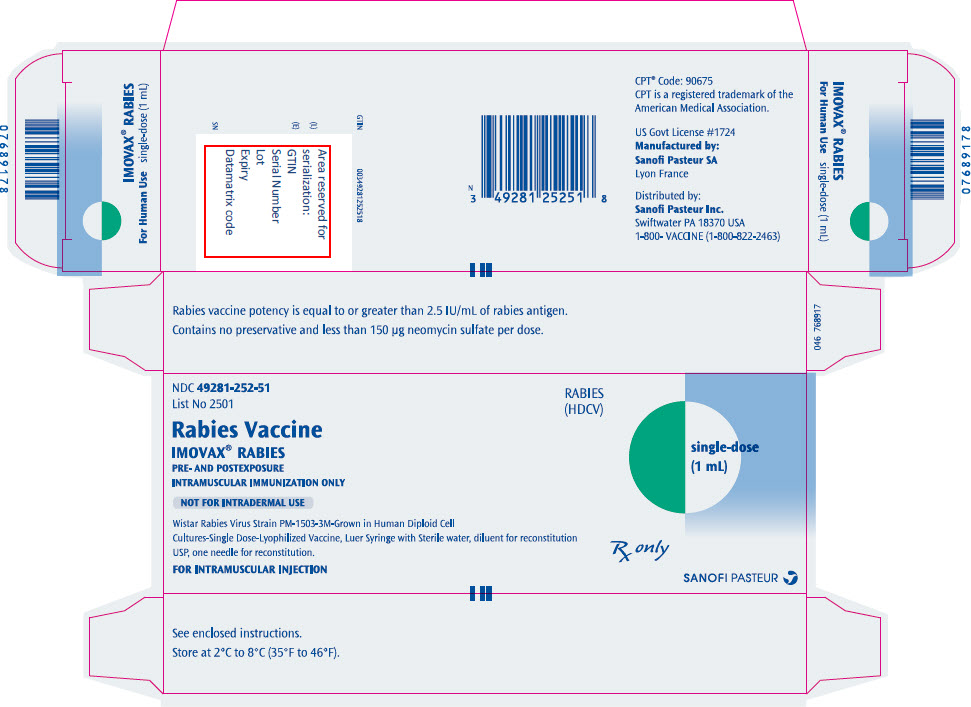
- PRINCIPAL DISPLAY PANEL - 1 mL Vial Label
- PRINCIPAL DISPLAY PANEL - 1 mL Syringe Label
-
PRINCIPAL DISPLAY PANEL - Kit Carton
NDC 49281-250-51
List No 2501Rabies Vaccine
IMOVAX®RABIES
PRE- AND POSTEXPOSURE
INTRAMUSCULAR IMMUNIZATION ONLYNOT FOR INTRADERMAL USE
Wistar Rabies Virus Strain PM-1503-3M-Grown in Human Diploid Cell
Cultures-Single Dose-Lyophilized Vaccine, Luer Syringe with Sterile water, diluent for reconstitution
USP, one needle for reconstitution.FOR INTRAMUSCULAR INJECTION
RABIES
(HDCV)1 Dose
(1 mL)Rx only
SANOFI PASTEUR
-
INGREDIENTS AND APPEARANCE
IMOVAX RABIES
rabies virus strain pm-1503-3m antigen (propiolactone inactivated) and water kitProduct Information Product Type VACCINE Item Code (Source) NDC: 49281-250 Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 49281-250-51 1 in 1 PACKAGE Quantity of Parts Part # Package Quantity Total Product Quantity Part 1 1 VIAL, SINGLE-USE 1 mL Part 2 1 SYRINGE 1 mL Part 1 of 2 IMOVAX RABIES
rabies virus strain pm-1503-3m antigen (propiolactone inactivated) injection, powder, lyophilized, for suspensionProduct Information Item Code (Source) NDC: 49281-248 Route of Administration INTRAMUSCULAR Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength RABIES VIRUS STRAIN PM-1503-3M ANTIGEN (PROPIOLACTONE INACTIVATED) (UNII: C4HQF74XMW) (RABIES VIRUS STRAIN PM-1503-3M ANTIGEN (PROPIOLACTONE INACTIVATED) - UNII:C4HQF74XMW) RABIES VIRUS STRAIN PM-1503-3M ANTIGEN (PROPIOLACTONE INACTIVATED) 2.5 [iU] in 1 mL Inactive Ingredients Ingredient Name Strength ALBUMIN HUMAN (UNII: ZIF514RVZR) 100 mg in 1 mL NEOMYCIN SULFATE (UNII: 057Y626693) 150 ug in 1 mL PHENOLSULFONPHTHALEIN (UNII: I6G9Y0J1OJ) 20 ug in 1 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 49281-248-58 1 mL in 1 VIAL, SINGLE-USE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA103931 06/09/1980 Part 2 of 2 WATER
water injection, solutionProduct Information Item Code (Source) NDC: 49281-249 Route of Administration INTRAMUSCULAR Inactive Ingredients Ingredient Name Strength WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 49281-249-01 1 mL in 1 SYRINGE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA103931 06/09/1980 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA103931 06/09/1980 IMOVAX RABIES
rabies virus strain pm-1503-3m antigen (propiolactone inactivated) and water kitProduct Information Product Type VACCINE Item Code (Source) NDC: 49281-252 Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 49281-252-51 1 in 1 PACKAGE Quantity of Parts Part # Package Quantity Total Product Quantity Part 1 1 VIAL, SINGLE-USE 1 mL Part 2 1 SYRINGE 1 mL Part 1 of 2 IMOVAX RABIES
rabies virus strain pm-1503-3m antigen (propiolactone inactivated) injection, powder, lyophilized, for suspensionProduct Information Item Code (Source) NDC: 49281-246 Route of Administration INTRAMUSCULAR Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength RABIES VIRUS STRAIN PM-1503-3M ANTIGEN (PROPIOLACTONE INACTIVATED) (UNII: C4HQF74XMW) (RABIES VIRUS STRAIN PM-1503-3M ANTIGEN (PROPIOLACTONE INACTIVATED) - UNII:C4HQF74XMW) RABIES VIRUS STRAIN PM-1503-3M ANTIGEN (PROPIOLACTONE INACTIVATED) 2.5 [iU] in 1 mL Inactive Ingredients Ingredient Name Strength ALBUMIN HUMAN (UNII: ZIF514RVZR) 100 mg in 1 mL NEOMYCIN SULFATE (UNII: 057Y626693) 150 ug in 1 mL PHENOLSULFONPHTHALEIN (UNII: I6G9Y0J1OJ) 20 ug in 1 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 49281-246-58 1 mL in 1 VIAL, SINGLE-USE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA103931 10/25/2019 Part 2 of 2 WATER
water injection, solutionProduct Information Item Code (Source) NDC: 49281-263 Route of Administration INTRAMUSCULAR Inactive Ingredients Ingredient Name Strength WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 49281-263-58 1 mL in 1 SYRINGE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA103931 10/25/2019 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA103931 10/25/2019 Labeler - Sanofi Pasteur Inc. (086723285) Establishment Name Address ID/FEI Business Operations Sanofi Pasteur 578763542 MANUFACTURE(49281-250, 49281-252)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.