Torsemide by Bryant Ranch Prepack TORSEMIDE tablet
Torsemide by
Drug Labeling and Warnings
Torsemide by is a Prescription medication manufactured, distributed, or labeled by Bryant Ranch Prepack. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
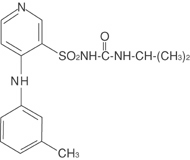
DESCRIPTION
Torsemide is a diuretic of the pyridine-sulfonylurea class. Its chemical name is 1-isopropyl-3-[(4-m-toluidino-3-pyridyl) sulfonyl]urea and its structural formula is:
Its molecular formula is C H N O S, its pKa is 6.42, and its molecular weight is 348.43. Torsemide is a white to off-white crystalline powder. The tablets for oral administration also contain lactose anhydrous, lactose monohydrate NF, microcrystalline cellulose NF, crospovidone NF, povidone USP and magnesium stearate NF. 162043
-
CLINICAL PHARMACOLOGY
Mechanism of Action
Micropuncture studies in animals have shown that torsemide acts from within the lumen of the thick ascending portion of the loop of Henle, where it inhibits the Na+/K+/2Cl-carrier system. Clinical pharmacology studies have confirmed this site of action in humans, and effects in other segments of the nephron have not been demonstrated. Diuretic activity thus correlates better with the rate of drug excretion in the urine than with the concentration in the blood.
Torsemide increases the urinary excretion of sodium, chloride, and water, but it does not significantly alter glomerular filtration rate, renal plasma flow, or acid-base balance.
Pharmacokinetics and Metabolism
The bioavailability of torsemide tablets is approximately 80%, with little inter subject variation; the 90% confidence interval is 75% to 89%. The drug is absorbed with little first-pass metabolism, and the serum concentration reaches its peak (C ) within 1 hour after oral administration. C and area under the serum concentration-time curve (AUC) after oral administration are proportional to dose over the range of 2.5 mg to 200 mg. Simultaneous food intake delays the time to C by about 30 minutes, but overall bioavailability (AUC) and diuretic activity are unchanged. Absorption is essentially unaffected by renal or hepatic dysfunction. maxmaxmax
The volume of distribution of torsemide is 12 liters to 15 liters in normal adults or in patients with mild to moderate renal failure or congestive heart failure. In patients with hepatic cirrhosis, the volume of distribution is approximately doubled.
In normal subjects the elimination half-life of torsemide is approximately 3.5 hours. Torsemide is cleared from the circulation by both hepatic metabolism (approximately 80% of total clearance) and excretion into the urine (approximately 20% of total clearance in patients with normal renal function). The major metabolite in humans is the carboxylic acid derivative, which is biologically inactive. Two of the lesser metabolites possess some diuretic activity, but for practical purposes metabolism terminates the action of the drug.
Because torsemide is extensively bound to plasma protein (>99%), very little enters tubular urine via glomerular filtration. Most renal clearance of torsemide occurs via active secretion of the drug by the proximal tubules into tubular urine.
In patients with decompensated congestive heart failure, hepatic and renal clearance are both reduced, probably because of hepatic congestion and decreased renal plasma flow, respectively. The total clearance of torsemide is approximately 50% of that seen in healthy volunteers, and the plasma half-life and AUC are correspondingly increased. Because of reduced renal clearance, a smaller fraction of any given dose is delivered to the intraluminal site of action, so at any given dose there is less natriuresis in patients with congestive heart failure than in normal subjects.
In patients with renal failure, renal clearance of torsemide is markedly decreased but total plasma clearance is not significantly altered. A smaller fraction of the administered dose is delivered to the intraluminal site of action, and the natriuretic action of any given dose of diuretic is reduced. A diuretic response in renal failure may still be achieved if patients are given higher doses. The total plasma clearance and elimination half-life of torsemide remain normal under the conditions of impaired renal function because metabolic elimination by the liver remains intact.
In patients with hepatic cirrhosis, the volume of distribution, plasma half-life, and renal clearance are all increased, but total clearance is unchanged.
The pharmacokinetic profile of torsemide in healthy elderly subjects is similar to that in young subjects except for a decrease in renal clearance related to the decline in renal function that commonly occurs with aging. However, total plasma clearance and elimination half-life remain unchanged.
-
INDICATIONS AND USAGE
Torsemide tablets are indicated for the treatment of edema associated with congestive heart failure, renal disease, or hepatic disease. Use of torsemide has been found to be effective for the treatment of edema associated with chronic renal failure. Chronic use of any diuretic in hepatic disease has not been studied in adequate and well-controlled trials.
Torsemide tablets are indicated for the treatment of hypertension alone or in combination with other antihypertensive agents.
- CONTRAINDICATIONS
- WARNINGS
-
PRECAUTIONS
Drug Interactions
In patients with essential hypertension, torsemide has been administered together with beta-blockers, ACE inhibitors and calcium-channel blockers. In patients with congestive heart failure, torsemide has been administered together with digitalis glycosides, ACE inhibitors, and organic nitrates. None of these combined uses was associated with new or unexpected adverse events.
Torsemide does not affect the protein binding of glyburide or warfarin, the anticoagulant effect of phenprocoumon (a related coumarin derivative), or the pharmacokinetics of digoxin or carvedilol (a vasodilator/beta-blocker). In healthy subjects, coadministration of torsemide was associated with significant reduction in the renal clearance of spironolactone, with corresponding increases in the AUC. However, clinical experience indicates that dosage adjustment of either agent is not required.
Because torsemide and salicylates compete for secretion by renal tubules, patients receiving high doses of salicylates may experience salicylate toxicity when torsemide is concomitantly administered. Also, although possible interactions between torsemide and nonsteroidal anti-inflammatory agents (including aspirin) have not been studied, coadministration of these agents with another loop diuretic (furosemide) has occasionally been associated with renal dysfunction.
The natriuretic effect of torsemide (like that of many other diuretics) is partially inhibited by the concomitant administration of indomethacin. This effect has been demonstrated for torsemide under conditions of dietary sodium restriction (50 mEq/day) but not in the presence of normal sodium intake (150 mEq/day).
The pharmacokinetic profile and diuretic activity of torsemide are not altered by cimetidine or spironolactone. Coadministration of digoxin is reported to increase the area under the curve for torsemide by 50%, but dose adjustment of torsemide is not necessary.
Concomitant use of torsemide and cholestyramine has not been studied in humans but, in a study in animals, coadministration of cholestyramine decreased the absorption of orally administered torsemide. If torsemide and cholestyramine are used concomitantly, simultaneous administration is not recommended.
Coadministration of probenecid reduces secretion of torsemide into the proximal tubule and thereby decreases the diuretic activity of torsemide.
Other diuretics are known to reduce the renal clearance of lithium, inducing a high risk of lithium toxicity, so coadministration of lithium and diuretics should be undertaken with great caution, if at all. Coadministration of lithium and torsemide has not been studied.
Other diuretics have been reported to increase the ototoxic potential of aminoglycoside antibiotics and of ethacrynic acid, especially in the presence of impaired renal function. These potential interactions with torsemide have not been studied.
Carcinogenesis and Mutagenesis and Impairment of Fertility
No overall increase in tumor incidence was found when torsemide was given to rats and mice throughout their lives at doses up to 9 mg/kg/day (rats) and 32 mg/kg/day (mice). On a body-weight basis, these doses are 27 to 96 times a human dose of 20 mg; on a body-surface-area basis, they are 5 to 8 times this dose. In the rat study, the high-dose female group demonstrated renal tubular injury, interstitial inflammation, and a statistically significant increase in renal adenomas and carcinomas. The tumor incidence in this group was, however, not much higher than the incidence sometimes seen in historical controls. Similar signs of chronic non-neoplastic renal injury have been reported in high-dose animal studies of other diuretics such as furosemide and hydrochlorothiazide.
No mutagenic activity was detected in any of a variety of and tests of torsemide and its major human metabolite. The tests included the Ames test in bacteria (with and without metabolic activation), tests for chromosome aberrations and sister-chromatid exchanges in human lymphocytes, tests for various nuclear anomalies in cells found in hamster and murine bone marrow, tests for unscheduled DNA synthesis in mice and rats, and others. in vivoin vitro
In doses up to 25 mg/kg/day (75 times a human dose of 20 mg on a body-weight basis; 13 times this dose on a body-surface-area basis), torsemide had no adverse effect on the reproductive performance of male or female rats.
Pregnancy
There was no fetotoxicity or teratogenicity in rats treated with up to 5 mg/ kg/day of torsemide (on a mg/kg basis, this is 15 times a human dose of 20 mg/day; on a mg/m basis, the animal dose is 10 times the human dose), or in rabbits, treated with 1.6 mg/kg/day (on a mg/kg basis, 5 times the human dose of 20 mg/kg/day; on a mg/m basis, 1.7 times this dose). Fetal and maternal toxicity (decrease in average body weight, increase in fetal resorption and delayed fetal ossification) occurred in rabbits and rats given doses 4 (rabbits) and 5 (rats) times larger. Adequate and well-controlled studies have not been carried out in pregnant women. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed. 22
Nursing Mothers
It is not known whether torsemide is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when torsemide is administered to a nursing woman.
Pediatric Use
Safety and effectiveness in pediatric patients have not been established.
Administration of another loop diuretic to severely premature infants with edema due to patent ductus arteriosus and hyaline membrane disease has occasionally been associated with renal calcifications, sometimes barely visible on X-ray but sometimes in staghorn form, filling the renal pelves. Some of these calculi have been dissolved, and hypercalciuria has been reported to have decreased, when chlorothiazide has been coadministered along with the loop diuretic. In other premature neonates with hyaline membrane disease, another loop diuretic has been reported to increase the risk of persistent patent ductus arteriosus, possibly through a prostaglandin-E-mediated process. The use of torsemide in such patients has not been studied.
-
ADVERSE REACTIONS
At the time of approval, torsemide had been evaluated for safety in approximately 4000 subjects: over 800 of these subjects received torsemide for at least 6 months, and over 380 were treated for more than 1 year. Among these subjects were 564 who received torsemide during United States-based trials in which 274 other subjects received placebo.
The reported side effects of torsemide were generally transient, and there was no relationship between side effects and age, sex, race, or duration of therapy. Discontinuation of therapy due to side effects occurred in 3.5% of United States patients treated with torsemide and in 4.4% of patients treated with placebo. In studies conducted in the United States and Europe, discontinuation rates due to side effects were 3.0% (38/1250) with torsemide and 3.4% (13/380) with furosemide in patients with congestive heart failure, 2.0% (8/409) with torsemide and 4.8% (11/230) with furosemide in patients with renal insufficiency, and 7.6% (13/170) with torsemide and 0% (0/33) with furosemide in patients with cirrhosis.
The most common reasons for discontinuation of therapy with torsemide were (in descending order of frequency) dizziness, headache, nausea, weakness, vomiting, hyperglycemia, excessive urination, hyperuricemia, hypokalemia, excessive thirst, hypovolemia, impotence, esophageal hemorrhage, and dyspepsia. Dropout rates for these adverse events ranged from 0.1% to 0.5%.
The side effects considered possibly or probably related to study drug that occurred in United States placebo-controlled trials in more than 1% of patients treated with torsemide are shown in Table 1.
Table 1 - Reactions Possibly or Probably Drug-Related United States Placebo-Controlled Studies Incidence (Percentages of Patients) Torsemide Placebo (N=564) (N=274) Headache 7.3 9.1 Excessive Urination 6.7 2.2 Dizziness 3.2 4.0 Rhinitis 2.8 2.2 Asthenia 2.0 1.5 Diarrhea 2.0 1.1 ECG Abnormality 2.0 0.4 Cough Increase 2.0 1.5 Constipation 1.8 0.7 Nausea 1.8 0.4 Arthralgia 1.8 0.7 Dyspepsia 1.6 0.7 Sore Throat 1.6 0.7 Myalgia 1.6 1.5 Chest Pain 1.2 0.4 Insomnia 1.2 1.8 Edema 1.1 1.1 Nervousness 1.1 0.4 The daily doses of torsemide used in these trials ranged from 1.25 mg to 20 mg, with most patients receiving 5 mg to 10 mg; the duration of treatment ranged from 1 to 52 days, with a median of 41 days. Of the side effects listed in the table, only “excessive urination” occurred significantly more frequently in patients treated with torsemide than in patients treated with placebo. In the placebo-controlled hypertension studies whose design allowed side-effect rates to be attributed to dose, excessive urination was reported by 1% of patients receiving placebo, 4% of those treated with 5 mg of daily torsemide, and 15% of those treated with 10 mg. The complaint of excessive urination was generally not reported as an adverse event among patients who received torsemide for cardiac, renal, or hepatic failure.
Serious adverse events reported in the clinical studies for which a drug relationship could not be excluded were atrial fibrillation, chest pain, diarrhea, digitalis intoxication, gastrointestinal hemorrhage, hyperglycemia, hyperuricemia, hypokalemia, hypotension, hypovolemia, shunt thrombosis, rash, rectal bleeding, syncope, and ventricular tachycardia.
Angioedema has been reported in a patient exposed to torsemide who was later found to be allergic to sulfa drugs.
Of the adverse reactions during placebo-controlled trials listed without taking into account assessment of relatedness to drug therapy, arthritis and various other nonspecific musculoskeletal problems were more frequently reported in association with torsemide than with placebo, even though gout was somewhat more frequently associated with placebo. These reactions did not increase in frequency or severity with the dose of torsemide. One patient in the group treated with torsemide withdrew due to myalgia, and one in the placebo group withdrew due to gout.
-
OVERDOSAGE
There is no human experience with overdoses of torsemide, but the signs and symptoms of overdosage can be anticipated to be those of excessive pharmacologic effect: dehydration, hypovolemia, hypotension, hyponatremia, hypokalemia, hypochloremic alkalosis, and hemoconcentration. Treatment of overdosage should consist of fluid and electrolyte replacement.
Laboratory determinations of serum levels of torsemide and its metabolites are not widely available.
No data are available to suggest physiological maneuvers (e.g., maneuvers to change the pH of the urine) that might accelerate elimination of torsemide and its metabolites. Torsemide is not dialyzable, so hemodialysis will not accelerate elimination.
- DOSAGE AND ADMINISTRATION
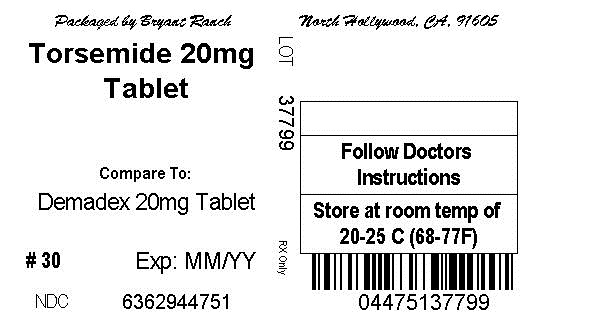
- Torsemide 20mg Tablet
-
INGREDIENTS AND APPEARANCE
TORSEMIDE
torsemide tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 63629-4475(NDC: 49884-108) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength TORSEMIDE (UNII: W31X2H97FB) (TORSEMIDE - UNII:W31X2H97FB) TORSEMIDE 20 mg Inactive Ingredients Ingredient Name Strength ANHYDROUS LACTOSE (UNII: 3SY5LH9PMK) CROSPOVIDONE (UNII: 68401960MK) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MAGNESIUM STEARATE (UNII: 70097M6I30) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) POVIDONES (UNII: FZ989GH94E) Product Characteristics Color WHITE Score 2 pieces Shape OVAL Size 11mm Flavor Imprint Code 59;H Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 63629-4475-1 30 in 1 BOTTLE Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA079234 01/27/2009 Labeler - Bryant Ranch Prepack (171714327) Registrant - Bryant Ranch Prepack (171714327) Establishment Name Address ID/FEI Business Operations Bryant Ranch Prepack 171714327 REPACK(63629-4475) , RELABEL(63629-4475)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.