piroxicam by DIRECT RX PIROXICAM capsule
piroxicam by
Drug Labeling and Warnings
piroxicam by is a Prescription medication manufactured, distributed, or labeled by DIRECT RX. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
BOXED WARNING
(What is this?)
BOXED WARNING SECTION
Cardiovascular Risk
- NSAIDs may cause an increased risk of serious cardiovascular thrombotic events, myocardial infarction, and stroke, which can be fatal. This risk may increase with duration of use. Patient's with cardiovascular disease or risk factors for cardiovascular disease may be at greater risk (see WARNINGS).
- Piroxicam Capsules USP is contraindicated for the treatment of peri-operative pain in the setting of coronary artery bypass graft (CABG) surgery (see WARNINGS).
Gastrointestinal Risk
- NSAID's cause an increased risk of serious gastrointestinal adverse events including bleeding, ulceration, and perforation of the stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Elderly patients are at greater risk for serious gastrointestinal events (see WARNINGS).
-
DESCRIPTION SECTION
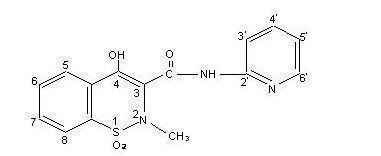
Piroxicam Capsules USP contains piroxicam which is a member of the oxicam group of nonsteroidal anti-inflammatory drugs (NSAIDs). Each ivory opaque/Swedish orange opaque capsule contains 10 mg piroxicam; each Swedish orange opaque/Swedish orange opaque capsule contains 20 mg piroxicam for oral administration. The chemical name for piroxicam is 4-hydroxyl-2-methyl-N-2-pyridinyl-2H-1,2,-benzothiazine-3-carboxamide 1,1-dioxide. Piroxicam occurs as a white crystalline solid, sparingly soluble in water, dilute acid and most organic solvents. It is slightly soluble in alcohol and in aqueous solutions. It exhibits a weakly acidic 4-hydroxy proton (pKa 5.1) and a weakly basic pyridyl nitrogen (pKa 1.8). The molecular weight of piroxicam is 331.35. Its molecular formula is C15H13N3O4S and it has the following structural formula:
The inactive ingredients in Piroxicam Capsules USP include: hard gelatin capsules (which may contain FD&C Blue1, FD&C Red 40, D&C Yellow 10, titanium dioxide and gelatin inactive ingredients), corn starch, lactose, magnesium stearate and sodium lauryl sulfate.
-
CLINICAL PHARMACOLOGY SECTION
Pharmacodynamics
Piroxicam Capsules USP is a nonsteroidal anti-inflammatory drug (NSAID) that exhibits anti-inflammatory, analgesic, and antipyretic activities in animal models. The mechanism of action of piroxicam, like that of other NSAIDs, is not completely understood but may be related to prostaglandin synthetase inhibition.
PharmacokineticsAbsorption
Piroxicam is well absorbed following oral administration. Drug plasma concentrations are proportional for 10 and 20 mg doses and generally peak within three to five hours after medication. The prolonged half-life (50 hours) results in the maintenance of relatively stable plasma concentrations throughout the day on once daily doses and to significant accumulation upon multiple dosing. A single 20-mg dose generally produces peak piroxicam plasma levels of 1.5 to 2 mcg/mL, while maximum drug plasma concentrations, after repeated daily ingestion of 20 mg Piroxicam Capsules USP, usually stabilize at 3–8 mcg/mL. Most patients approximate steady state plasma levels within 7–12 days. Higher levels, which approximate steady state at two to three weeks, have been observed in patients in whom longer plasma half-lives of piroxicam occurred.
With food there is a slight delay in the rate but not the extent of absorption following oral administration. The concomitant administration of antacids (aluminum hydroxide or aluminum hydroxide with magnesium hydroxide) have been shown to have no effect on the plasma levels of orally administered piroxicam.
Distribution
The apparent volume of distribution of piroxicam is approximately 0.14 L/kg. Ninety-nine percent of plasma piroxicam is bound to plasma proteins. Piroxicam is excreted into human milk. The presence in breast milk has been determined during initial and long-term conditions (52 days). Piroxicam appeared in breast milk at about 1% to 3% of the maternal concentration. No accumulation of piroxicam occurred in milk relative to that in plasma during treatment.
Metabolism
Metabolism of piroxicam occurs by hydroxylation at the 5 position of the pyridyl side chain and conjugation of this product; by cyclodehydration; and by a sequence of reactions involving hydrolysis of the amide linkage, decarboxylation, ring contraction and N-demethylation. In vitro studies indicate cytochrome P4502C9 (CYP2C9) as the main enzyme involved in the formation to the 5'-hydroxy-piroxicam, the major metabolite (see Pharmacogenetics, and Special Populations, Poor Metabolizers of CYP2C9 Substrates). The biotransformation products of piroxicam metabolism are reported to not have any anti-inflammatory activity.
Higher systemic exposure of piroxicam has been noted in subjects with CYP2C9 polymorphisms compared to normal metabolizer type subjects (see Pharmacogenetics, and Special Populations, Poor Metabolizers of CYP2C9 Substrates).
Excretion
Piroxicam and its biotransformation products are excreted in urine and feces, with about twice as much appearing in the urine as in the feces. Approximately 5% of a piroxicam dose is excreted unchanged. The plasma half-life (T½) for piroxicam is approximately 50 hours.
Pharmacogenetics
CYP2C9 activity is reduced in individuals with genetic polymorphisms, such as the CYP2C9*2 and CYP2C9*3 polymorphisms. Limited data from one published report that included nine subjects each with heterozygous CYP2C9*1/*2 and CYP2C9*1/*3 genotypes and one subject with the homozygous CYP2C9*3/*3 genotype showed piroxicam systemic levels that were 1.7-, 1.7- and 5.3-fold, respectively, higher compared to the 17 subjects with CYP2C9*1/*1 or normal metabolizer genotype. The pharmacokinetics of piroxicam have not been evaluated in subjects with other CYP2C9 polymorphisms, such as *5, *6, *9 and *11. It is estimated that the frequency of the homozygous *3/*3 genotype is 0.3% to 1.0% in various ethnic groups.
Special PopulationsPediatric
Piroxicam Capsules USP has not been investigated in pediatric patients.
Race
Pharmacokinetic differences due to race have not been identified.
Hepatic Insufficiency
The effects of hepatic disease on piroxicam pharmacokinetics have not been established. However, a substantial portion of piroxicam elimination occurs by hepatic metabolism. Consequently, patients with hepatic disease may require reduced doses of piroxicam as compared to patients with normal hepatic function.
Poor Metabolizers of CYP2C9 Substrates
Patients who are known or suspected to be poor CYP2C9 metabolizers based on genotype or previous history/experience with other CYP2C9 substrates (such as warfarin and phenytoin) should be administered piroxicam with caution as they may have abnormally high plasma levels due to reduced metabolic clearance.
Renal Insufficiency
Piroxicam pharmacokinetics have been investigated in patients with renal insufficiency. Studies indicate patients with mild to moderate renal impairment may not require dosing adjustments. However, the pharmacokinetic properties of Piroxicam in patients with severe renal insufficiency or those receiving hemodialysis are not known.
Other Information
In controlled clinical trials, the effectiveness of piroxicam has been established for both acute exacerbations and long-term management of rheumatoid arthritis and osteoarthritis.
The therapeutic effects of piroxicam are evident early in the treatment of both diseases with a progressive increase in response over several (8–12) weeks. Efficacy is seen in terms of pain relief and, when present, subsidence of inflammation.
Doses of 20 mg/day piroxicam display a therapeutic effect comparable to therapeutic doses of aspirin, with a lower incidence of minor gastrointestinal effects and tinnitus.
Piroxicam has been administered concomitantly with fixed doses of gold and corticosteroids. The existence of a "steroid-sparing" effect has not been adequately studied to date.
-
INDICATIONS & USAGE SECTION
Carefully consider the potential benefits and risks of Piroxicam Capsules USP and other treatment options before deciding to use Piroxicam Capsules USP. Use the lowest effective dose for the shortest duration consistent with individual patient treatment goals (see WARNINGS).
Piroxicam Capsules USP is indicated:
- For relief of the signs and symptoms of osteoarthritis.
- For relief of the signs and symptoms of rheumatoid arthritis.
-
CONTRAINDICATIONS SECTION
Piroxicam Capsules USP is contraindicated in patients with known hypersensitivity to piroxicam.
Piroxicam Capsules USP should not be given to patients who have experienced asthma, urticaria or allergic-type reactions after taking aspirin or other NSAIDs. Severe, rarely fatal, anaphylactic-like reactions to NSAIDs have been reported in such patients (see WARNINGS: Anaphylactoid Reactions and PRECAUTIONS: Preexisting Asthma).
Piroxicam Capsules USP is contraindicated for the treatment of peri-operative pain in the setting of coronary artery bypass graft (CABG) surgery (see WARNINGS).
-
WARNINGS SECTION
CARDIOVASCULAR EFFECTSCardiovascular Thrombotic Events
Clinical trials of several COX-2 selective and nonselective NSAIDs of up to three years duration have shown an increased risk of serious cardiovascular (CV) thrombotic events, myocardial infarction, and stroke, which can be fatal. All NSAIDs, both COX-2 selective and nonselective, may have a similar risk. Patients with known CV disease or risk factors for CV disease may be at greater risk. To minimize the potential risk for an adverse CV event in patients treated with an NSAID, the lowest effective dose should be used for the shortest duration possible. Physicians and patients should remain alert for the development of such events, even in the absence of previous CV symptoms. Patients should be informed about the signs and/or symptoms of serious CV events and the steps to take if they occur.
There is no consistent evidence that concurrent use of aspirin mitigates the increased risk of serious CV thrombotic events associated with NSAID use. The concurrent use of aspirin and an NSAID does increase the risk of serious GI events (see GI WARNINGS).
Two large, controlled clinical trials of a COX-2 selective NSAID for the treatment of pain in the first 10–14 days following CABG surgery found an increased incidence of myocardial infarction and stroke (see CONTRAINDICATIONS).
Hypertension
NSAIDs, including Piroxicam Capsules USP, can lead to onset of new hypertension or worsening of pre-existing hypertension, either of which may contribute to the increased incidence of CV events. Patients taking thiazides or loop diuretics may have impaired response to these therapies when taking NSAIDs. NSAIDs, including Piroxicam Capsules USP, should be used with caution in patients with hypertension. Blood pressure (BP) should be monitored closely during the initiation of NSAID treatment and throughout the course of therapy.
Congestive Heart Failure and Edema
Fluid retention and edema have been observed in some patients taking NSAIDs. Piroxicam Capsules USP should be used with caution in patients with fluid retention or heart failure.
Gastrointestinal Effects - Risk of Ulceration, Bleeding and Perforation
NSAIDs, including Piroxicam Capsules USP, can cause serious gastrointestinal (GI) adverse events including inflammation, bleeding, ulceration, and perforation of the stomach, small intestine, or large intestine, which can be fatal. These serious adverse events can occur at any time, with or without warning symptoms, in patients treated with NSAIDs. Only one in five patients, who develop a serious upper GI adverse event on NSAID therapy, is symptomatic. Upper GI ulcers, gross bleeding, or perforation caused by NSAIDs occur in approximately 1% of patients treated for 3–6 months, and in about 2–4% of patients treated for one year. These trends continue with longer duration of use, increasing the likelihood of developing a serious GI event at some time during the course of therapy. However, even short-term therapy is not without risk.
NSAIDs should be prescribed with extreme caution in those with a prior history of ulcer disease or gastrointestinal bleeding. Patients with a prior history of peptic ulcer disease and/or gastrointestinal bleeding who use NSAIDs have a greater than 10-fold increased risk for developing a GI bleed compared to patients with neither of these risk factors. Other factors that increase the risk of GI bleeding in patients treated with NSAIDs include concomitant use of oral corticosteroids or anticoagulants, longer duration of NSAID therapy, smoking, use of alcohol, older age, and poor general health status. Most spontaneous reports of fatal GI events are in elderly or debilitated patients and therefore, special care should be taken in treating this population.
To minimize the potential risk for an adverse GI event in patients treated with an NSAID, the lowest effective dose should be used for the shortest possible duration. Patients and physicians should remain alert for signs and symptoms of GI ulcerations and bleeding during NSAID therapy and promptly initiate additional evaluation and treatment if a serious GI event is suspected. This should include discontinuation of the NSAID until a serious GI adverse event is ruled out. For high-risk patients, alternate therapies that do not involve NSAIDs should be considered.
Renal Effects
Long-term administration of NSAIDs has resulted in renal papillary necrosis and other renal injury. Renal toxicity has also been seen in patients in whom renal prostaglandins have a compensatory role in the maintenance of renal perfusion. In these patients, administration of a nonsteroidal anti-inflammatory drug may cause a dose-dependent reduction in prostaglandin formation and, secondarily, in renal blood flow, which may precipitate overt renal decompensation. Patients at greatest risk of this reaction are those with impaired renal function, heart failure, liver dysfunction, those taking diuretics and ACE inhibitors, and the elderly. Discontinuation of NSAID therapy is usually followed by recovery to the pretreatment state.
Advanced Renal Disease
No information is available from controlled clinical studies regarding the use of Piroxicam Capsules USP in patients with advanced renal disease. Therefore, treatment with Piroxicam Capsules USP is not recommended in these patients with advanced renal disease. If Piroxicam Capsules USP therapy must be initiated, close monitoring of the patient's renal function is advisable.
Anaphylactoid Reactions
As with other NSAIDs, anaphylactoid reactions may occur in patients without known prior exposure to Piroxicam Capsules USP. Piroxicam Capsules USP should not be given to patients with the aspirin triad. This symptom complex typically occurs in asthmatic patients who experience rhinitis with or without nasal polyps, or who exhibit severe, potentially fatal bronchospasm after taking aspirin or other NSAIDs (see CONTRAINDICATIONS and PRECAUTIONS: Preexisting Asthma). Emergency help should be sought in cases where an anaphylactoid reaction occurs.
Skin Reactions
NSAIDs, including Piroxicam Capsules USP, can cause serious skin adverse events such as exfoliative dermatitis, Stevens-Johnson Syndrome (SJS), and toxic epidermal necrolysis (TEN), which can be fatal. These serious events may occur without warning. Patients should be informed about the signs and symptoms of serious skin manifestations and use of the drug should be discontinued at the first appearance of skin rash or any other sign of hypersensitivity.
Other Hypersensitivity Reactions
A combination of dermatological and/or allergic signs and symptoms suggestive of serum sickness have occasionally occurred in conjunction with the use of piroxicam. These include arthralgias, pruritus, fever, fatigue, and rash including vesiculobullous reactions and exfoliative dermatitis.
Pregnancy
In late pregnancy, as with other NSAIDs, Piroxicam Capsules USP should be avoided because it may cause premature closure of the ductus arteriosus.
-
PRECAUTIONS SECTION
General
Piroxicam Capsules USP cannot be expected to substitute for corticosteroids or to treat corticosteroid insufficiency. Abrupt discontinuation of corticosteroids may lead to disease exacerbation. Patients on prolonged corticosteroid therapy should have their therapy tapered slowly if a decision is made to discontinue corticosteroids.
The pharmacological activity of Piroxicam Capsules USP in reducing fever and inflammation may diminish the utility of these diagnostic signs in detecting complications of presumed noninfectious, painful conditions.
Hepatic Effects
Borderline elevations of one or more liver tests may occur in up to 15% of patients taking NSAIDs including Piroxicam Capsules USP. These laboratory abnormalities may progress, may remain unchanged, or may be transient with continuing therapy. Notable elevations of ALT or AST (approximately three or more times the upper limit of normal) have been reported in approximately 1% of patients in clinical trials with NSAIDs. In addition, rare cases of severe hepatic reactions, including jaundice and fatal fulminant hepatitis, liver necrosis and hepatic failure, some of them with fatal outcomes have been reported.
A patient with symptoms and/or signs suggesting liver dysfunction, or in whom an abnormal liver test has occurred, should be evaluated for evidence of the development of more severe hepatic reaction while on therapy with Piroxicam Capsules USP. If clinical signs and symptoms consistent with liver disease develop, or if systemic manifestations occur (e.g., eosinophilia, rash, etc.), Piroxicam Capsules USP should be discontinued (see ADVERSE REACTIONS).
Hematological Effects
Anemia is sometimes seen in patients receiving NSAIDs, including Piroxicam Capsules USP. This may be due to fluid retention, occult or gross GI blood loss, or an incompletely described effect upon erythropoiesis. Patients on long-term treatment with NSAIDs, including Piroxicam Capsules USP, should have their hemoglobin or hematocrit checked if they exhibit any signs or symptoms of anemia.
NSAIDs inhibit platelet aggregation and have been shown to prolong bleeding time in some patients. Unlike aspirin, their effect on platelet function is quantitatively less, of shorter duration, and reversible. Patients receiving Piroxicam Capsules USP who may be adversely affected by alterations in platelet function, such as those with coagulation disorders or patients receiving anticoagulants, should be carefully monitored.
Ophthalmologic Effects
Because of reports of adverse eye findings with nonsteroidal anti-inflammatory agents, it is recommended that patients who develop visual complaints during treatment with Piroxicam Capsules USP have ophthalmic evaluations.
Preexisting Asthma
Patients with asthma may have aspirin-sensitive asthma. The use of aspirin in patients with aspirin-sensitive asthma has been associated with severe bronchospasm which can be fatal. Since crossreactivity, including bronchospasm, between aspirin and other nonsteroidal anti-inflammatory drugs has been reported in such aspirin-sensitive patients, Piroxicam Capsules USP should not be administered to patients with this form of aspirin sensitivity and should be used with caution in patients with preexisting asthma.
Information for Patients
Patients should be informed of the following information before initiating therapy with an NSAID and periodically during the course of ongoing therapy. Patients should also be encouraged to read the NSAID Medication Guide that accompanies each prescription dispensed.
- Piroxicam Capsules USP, like other NSAIDs, may cause CV side effects, such as MI or stroke, which may result in hospitalization and even death. Although serious CV events can occur without warning symptoms, patients should be alert for the signs and symptoms of chest pain, shortness of breath, weakness, slurring of speech, and should ask for medical advice when observing any indicative sign or symptoms. Patients should be apprised of the importance of this follow-up (see WARNINGS, Cardiovascular Effects).
- Piroxicam Capsules USP, like other NSAIDs, can cause GI discomfort and, rarely, serious GI side effects, such as ulcers and bleeding, which may result in hospitalization and even death. Although serious GI tract ulcerations and bleeding can occur without warning symptoms, patients should be alert for the signs and symptoms of ulcerations and bleeding, and should ask for medical advice when observing any indicative sign or symptoms including epigastric pain, dyspepsia, melena, and hematemesis. Patients should be apprised of the importance of this follow-up (see WARNINGS: Gastrointestinal Effects: Risk of Ulceration, Bleeding and Perforation).
- Piroxicam Capsules USP, like other NSAIDs, can cause serious skin side effects such as exfoliative dermatitis, SJS and TEN, which may result in hospitalizations and even death. Although serious skin reactions may occur without warning, patients should be alert for the signs and symptoms of skin rash and blisters, fever, or other signs hypersensitivity such as itching, and should ask for medical advice when observing any indicative signs or symptoms. Patients should be advised to stop the drug immediately if they develop any type of rash and contact their physicians as soon as possible.
- Patients should promptly report signs or symptoms of unexplained weight gain, or edema to their physicians.
- Patients should be informed of the warning signs and symptoms of hepatotoxicity (e.g., nausea, fatigue, lethargy, pruritus, jaundice, right upper quadrant tenderness and "flu-like" symptoms). If these occur, patients should be instructed to stop therapy and seek immediate medical therapy.
- Patients should be informed of the signs of an anaphylactoid reaction (e.g. difficulty breathing, swelling of the face or throat). If these occur, patients should be instructed to seek immediate emergency help (see WARNINGS).
- In late pregnancy, as with other NSAIDs, Piroxicam Capsules USP should be avoided because it may cause premature closure of the ductus arteriosus.
Laboratory Tests
Because serious GI tract ulcerations and bleeding can occur without warning symptoms, physicians should monitor for signs of symptoms of GI bleeding. Patients on long-term treatment with NSAIDs should have their CBC and a chemistry profile checked periodically. If clinical signs and symptoms consistent with liver or renal disease develop, systemic manifestations occur (e.g., eosinophilia, rash, etc.) or if abnormal liver tests persist or worsen, Piroxicam Capsules USP should be discontinued.
Drug InteractionsHighly Protein Bound Drugs
Piroxicam is highly protein bound and, therefore, might be expected to displace other protein bound drugs. Physicians should closely monitor patients for a change in dosage requirements when administering Piroxicam Capsules USP to patients on other highly protein bound drugs.
Aspirin
When piroxicam is administered with aspirin, its protein binding is reduced, although the clearance of free piroxicam is not altered. Plasma levels of piroxicam are depressed to approximately 80% of their normal values when piroxicam is administered (20 mg/day) in conjunction with aspirin (3900 mg/day). The clinical significance of this interaction is not known; however, as with other NSAIDs, concomitant administration of piroxicam and aspirin is not generally recommended because of the potential for increased adverse effects.
Methotrexate
NSAIDs have been reported to competitively inhibit methotrexate accumulation in rabbit kidney slices. This may indicate that they could enhance the toxicity of methotrexate. Caution should be used when NSAIDs are administered concomitantly with methotrexate.
ACE-Inhibitors
Reports suggest that NSAIDs may diminish the antihypertensive effect of ACE-inhibitors. This interaction should be given consideration in patients taking NSAIDs concomitantly with ACE-inhibitors.
Diuretics
Clinical studies, as well as postmarketing observations, have shown that Piroxicam Capsules USP can reduce the natriuretic effect of furosemide and thiazides in some patients. This response has been attributed to inhibition of renal prostaglandin synthesis. During concomitant therapy with NSAIDs, the patient should be observed closely for signs of renal failure (see WARNINGS: Renal Effects), as well as to assure diuretic efficacy.
Lithium
NSAIDs have produced an elevation of plasma lithium levels and a reduction in renal lithium clearance. The mean minimum lithium concentration increased 15% and the renal clearance was decreased by approximately 20%. These effects have been attributed to inhibition of renal prostaglandin synthesis by the NSAID. Thus, when NSAIDs and lithium are administered concurrently, subjects should be observed carefully for signs of lithium toxicity.
Warfarin
The effects of warfarin and NSAIDs on GI bleeding are synergistic, such that users of both drugs together have a risk of serious GI bleeding higher than users of either drug alone.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Subacute, acute and chronic toxicity studies have been carried out in rats, mice, dogs and monkeys. The pathology most often seen was that characteristically associated with the animal toxicology of anti-inflammatory agents: renal papillary necrosis (see PRECAUTIONS) and gastrointestinal lesions.
Reproductive studies revealed no impairment of fertility in animals.
PregnancyTeratogenic EffectsPregnancy Category C
Reproductive studies conducted in rats and rabbits have not demonstrated evidence of developmental abnormalities. However, animal reproduction studies are not always predictive of human response. There are no adequate and well-controlled studies in pregnant women. Piroxicam Capsules USP is not recommended for use in pregnant women since safety has not been established in humans. Piroxicam Capsules USP should be used in pregnancy only if the potential benefit justifies the potential risk to the fetus.
Nonteratogenic Effects
Because of the known effects of nonsteroidal anti-inflammatory drugs on the fetal cardiovascular system (closure of ductus arteriosus), use during pregnancy (particularly late pregnancy) should be avoided. In animal studies of piroxicam, gastrointestinal tract toxicity was increased in pregnant females in the last trimester of pregnancy compared to nonpregnant females or females in earlier trimesters of pregnancy.
Labor and Delivery
In rat studies with NSAIDs, as with other drugs known to inhibit prostaglandin synthesis, an increased incidence of dystocia, delayed parturition, and decreased pup survival occurred. The effects of piroxicam on labor and delivery in pregnant women are unknown.
Nursing Mothers
Piroxicam is excreted into human milk. The presence in breast milk has been determined during initial and long-term conditions (52 days). Piroxicam appeared in breast milk at about 1% to 3% of the maternal concentration. No accumulation of piroxicam occurred in milk relative to that in plasma during treatment. Piroxicam Capsules USP is not recommended for use in nursing mothers.
Pediatric Use
Safety and effectiveness in pediatric patients have not been established.
Geriatric Use
As with any NSAID, caution should be exercised in treating the elderly (65 years and older). Most spontaneous reports of fatal GI events with NSAIDs are in the elderly or debilitated patients and, therefore, care should be taken in treating this population. In addition to a past history of ulcer disease, older age and poor general health status (among other factors) may increase the risk for GI bleeding. To minimize the potential risk of an adverse GI event, the lowest effective dose should be used for the shortest possible duration (see WARNINGS: Gastrointestinal (GI) Effects – Risk of GI Ulceration, Bleeding and Perforation).
As with all other NSAIDs, there is a risk of developing renal toxicity in patients in which renal prostaglandins have a compensatory role in maintenance of renal perfusion. Discontinuation of nonsteroidal anti-inflammatory drug therapy is usually followed by recovery to the pretreatment state (see Warnings: Renal Effects).
In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting a greater frequency of impaired drug elimination and of concomitant disease or other drug therapy.
-
ADVERSE REACTIONS SECTION
In patients taking Piroxicam Capsules USP or other NSAIDs, the most frequently reported adverse experiences occurring in approximately 1–10% of patients are:
Cardiovascular System: Edema. Digestive System: Anorexia, abdominal pain, constipation, diarrhea, dyspepsia, elevated liver enzymes, flatulence, gross bleeding/perforation, heartburn, nausea, ulcers (gastric/duodenal), vomiting. Hemic and Lymphatic System: Anemia, increased bleeding time. Nervous System: Dizziness, headache. Skin and Appendages: Pruritus, rash. Special Senses: Tinnitus. Urogenital System: Abnormal renal function.
Additional adverse experiences reported occasionally include:
Body As a Whole: Fever, infection, sepsis. Cardiovascular System: Congestive heart failure, hypertension, tachycardia, syncope. Digestive System: Dry mouth, esophagitis, gastritis, glossitis, hematemesis, hepatitis, jaundice, melena, rectal bleeding, stomatitis. Hemic and Lymphatic System: Ecchymosis, eosinophilia, epistaxis, leukopenia, purpura, petechial rash, thrombocytopenia. Metabolic and Nutritional: Weight changes. Nervous System: Anxiety, asthenia, confusion, depression, dream abnormalities, drowsiness, insomnia, malaise, nervousness, paresthesia, somnolence, tremors, vertigo. Respiratory System: Asthma, dyspnea. Skin and Appendages: Alopecia, bruising, desquamation, erythema, photosensitivity, sweat. Special Senses: Blurred vision. Urogenital System: Cystitis, dysuria, hematuria, hyperkalemia, interstitial nephritis, nephrotic syndrome, oliguria/polyuria, proteinuria, renal failure.
Other adverse reactions which occur rarely are:
Body As a Whole: Anaphylactic reactions, appetite changes, death, flu-like syndrome, pain (colic), serum sickness. Cardiovascular System: Arrhythmia, exacerbation of angina, hypotension, myocardial infarction, palpitations, vasculitis. Digestive System: Eructation, liver failure, pancreatitis. Hemic and Lymphatic System: Agranulocytosis, hemolytic anemia, aplastic anemia, lymphadenopathy, pancytopenia. Hypersensitivity: Positive ANA. Metabolic and Nutritional: Hyperglycemia, hypoglycemia. Nervous System: Akathisia, convulsions, coma, hallucinations, meningitis, mood alterations. Respiratory: Respiratory depression, pneumonia. Skin and Appendages: Angioedema, toxic epidermal necrosis, erythema multiforme, exfoliative dermatitis, onycholysis, Stevens-Johnson syndrome, urticaria, vesiculobullous reaction. Special Senses: Conjunctivitis, hearing impairment, swollen eyes.
-
OVERDOSAGE SECTION
Symptoms following acute NSAID overdoses are usually limited to lethargy, drowsiness, nausea, vomiting, and epigastric pain, which are generally reversible with supportive care. Gastrointestinal bleeding can occur. Hypertension, acute renal failure, respiratory depression and coma may occur, but are rare. Anaphylactoid reactions have been reported with therapeutic ingestion of NSAIDs, and may occur following an overdose.
Patients should be managed by symptomatic and supportive care following an NSAID overdose. There are no specific antidotes. Emesis and/or activated charcoal (60–100 g in adults, 1–2 g/kg in children) and/or osmotic cathartic may be indicated. The long plasma half-life of piroxicam should be considered when treating an overdose with piroxicam. Experiments in dogs have demonstrated that the use of multiple-dose treatments with activated charcoal could reduce the half-life of piroxicam by more than 50% and systemic bioavailability by as much as 37% when activated charcoal is given as late as 6 hours after ingestion of piroxicam. Forced diuresis, alkalinization of urine, hemodialysis, or hemoperfusion may not be useful due to high protein binding.
-
DOSAGE & ADMINISTRATION SECTION
Carefully consider the potential benefits and risks of Piroxicam Capsules USP and other treatment options before deciding to use Piroxicam Capsules USP. Use the lowest effective dose for the shortest duration consistent with individual patient treatment goals (see WARNINGS).
After observing the response to initial therapy with Piroxicam Capsules USP, the dose and frequency should be adjusted to suit an individual patient's needs.
For the relief of rheumatoid arthritis and osteoarthritis, the recommended dose is 20 mg given orally once per day. If desired, the daily dose may be divided. Because of the long half-life of Piroxicam Capsules USP, steady-state blood levels are not reached for 7–12 days. Therefore, although the therapeutic effects of piroxicam are evident early in treatment, there is a progressive increase in response over several weeks and the effect of therapy should not be assessed for two weeks.
-
HOW SUPPLIED SECTION
Piroxicam Capsules USP for oral administration:
Bottles of 100's: 10 mg Capsule, (NDC#29033-012-01) Swedish Orange Opaque cap is imprinted with "NP" above "10" in black with a lvory opaque body.
Bottles of 100's: 20 mg Capsule, (NDC#29033-013-01) Swedish Orange Opaque cap is imprinted with "NP" above "20" in black with a Swedish Orange Opaque body.
Bottles of 500's: 20 mg Capsule, (NDC#29033-013-05) Swedish Orange Opaque Cap is imprinted with "NP" above "20" in black with a Swedish Orange Opaque body.
Store at 20°-25°C (68°-77°F); excursions permitted to 15°-30°C (59°-86°F) [see USP Controlled Room Temperature]
Dispense in a tight,light-resistant container as defined in the USP.
- MEDICATION GUIDE
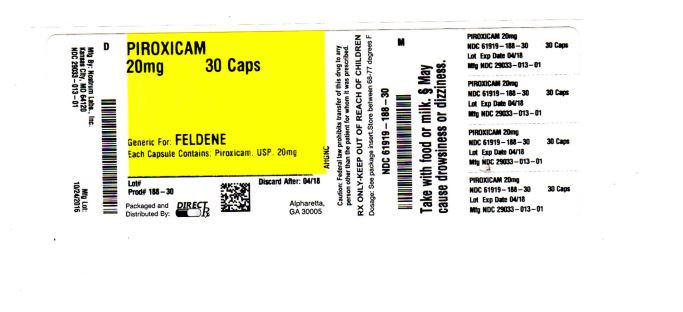
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
PIROXICAM
piroxicam capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 61919-188(NDC:29033-013) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength PIROXICAM (UNII: 13T4O6VMAM) (PIROXICAM - UNII:13T4O6VMAM) PIROXICAM 20 mg Product Characteristics Color orange Score no score Shape CAPSULE Size 17mm Flavor Imprint Code NP;20 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 61919-188-30 30 in 1 BOTTLE; Type 0: Not a Combination Product 01/01/2015 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA074116 01/01/2014 Labeler - DIRECT RX (079254320) Establishment Name Address ID/FEI Business Operations DIRECT RX 079254320 relabel(61919-188) , repack(61919-188)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.