EVOMELA- melphalan injection, powder, lyophilized, for solution
EVOMELA by
Drug Labeling and Warnings
EVOMELA by is a Prescription medication manufactured, distributed, or labeled by Acrotech Biopharma LLC, Spectrum Pharmaceuticals, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use EVOMELA® safely and effectively. See full prescribing information for EVOMELA.
EVOMELA (melphalan) for injection, for intravenous use.
Initial U.S. Approval: 1964WARNING: SEVERE BONE MARROW SUPPRESSION, HYPERSENSITIVITY, AND LEUKEMOGENICITY
See full prescribing information for complete boxed warning.
- Severe bone marrow suppression with resulting infection or bleeding may occur. Controlled trials comparing intravenous (IV) melphalan to oral melphalan have shown more myelosuppression with the IV formulation. Monitor hematologic laboratory parameters. (5.1)
- Hypersensitivity reactions, including anaphylaxis, have occurred in approximately 2% of patients who received the IV formulation of melphalan. Discontinue treatment with Evomela for serious hypersensitivity reactions. (5.4)
- Melphalan produces chromosomal aberrations in vitro and in vivo. Evomela should be considered potentially leukemogenic in humans. (5.5)
RECENT MAJOR CHANGES
Dosage and Administration (2.4) 09/2017
INDICATIONS AND USAGE
DOSAGE AND ADMINISTRATION
- For Conditioning Treatment, the recommended dose of Evomela is 100 mg/m2/day administered over 30 minutes by intravenous infusion for 2 consecutive days (Day -3 and Day -2) prior to autologous stem cell transplantation (ASCT, Day 0). (2.1)
- For Palliative Treatment, the recommended dose of Evomela is 16 mg/m2 administered as a single intravenous infusion over 15-20 minutes at 2-week intervals for 4 doses, then, after adequate recovery from toxicity, at 4-week intervals. (2.2)
DOSAGE FORMS AND STRENGTHS
For Injection: 50 mg per vial, lyophilized powder in a single-dose vial for reconstitution. (3)
CONTRAINDICATIONS
- History of serious allergic reaction to melphalan
WARNINGS AND PRECAUTIONS
- Gastrointestinal toxicity: Nausea, vomiting, diarrhea or oral mucositis may occur; provide supportive care using antiemetic and antidiarrheal medications as needed. (2.1, 5.2)
- Embryo-fetal toxicity: Can cause fetal harm. Advise of potential risk to fetus and to avoid pregnancy. (5.6, 8.1, 8.3)
- Infertility: Melphalan may cause ovarian function suppression or testicular suppression. (5.7)
ADVERSE REACTIONS
Most common adverse reactions observed in at least 50% of patients treated with Evomela are neutrophil count decreased, white blood cell count decreased, lymphocyte count decreased, platelet count decreased, diarrhea, nausea, fatigue, hypokalemia, anemia, and vomiting. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Spectrum Pharmaceuticals, Inc. at 1-888-292-9617 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch
USE IN SPECIFIC POPULATIONS
- Nursing mothers: Advise women against breastfeeding while being treated with Evomela. (8.3)
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 9/2017
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: SEVERE BONE MARROW SUPPRESSION, HYPERSENSITIVITY, and LEUKEMOGENICITY
1 INDICATIONS AND USAGE
1.1 Multiple Myeloma-Conditioning Treatment
1.2 Multiple Myeloma-Palliative Treatment
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage for Conditioning Treatment
2.2 Recommended Dosage for Palliative Treatment
2.3 Dose Modification for Renal Impairment
2.4 Preparation and Administration
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Bone Marrow Suppression
5.2 Gastrointestinal Toxicity
5.3 Hepatotoxicity
5.4 Hypersensitivity
5.5 Secondary Malignancies
5.6 Embryo-Fetal Toxicity
5.7 Infertility
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Patients with Renal Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14. CLINICAL STUDIES
14.1 Myeloablative Conditioning in Patients with Multiple Myeloma Undergoing ASCT
14.2 Palliative Treatment of Patients with Multiple Myeloma
15 REFERENCES
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
16.2 Storage and Handling
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: SEVERE BONE MARROW SUPPRESSION, HYPERSENSITIVITY, and LEUKEMOGENICITY
- Severe bone marrow suppression with resulting infection or bleeding may occur. Controlled trials comparing intravenous (IV) melphalan to oral melphalan have shown more myelosuppression with the IV formulation. Monitor hematologic laboratory parameters. [see Warnings and Precautions (5.1)]
- Hypersensitivity reactions, including anaphylaxis, have occurred in approximately 2% of patients who received the IV formulation of melphalan. Discontinue treatment with Evomela for serious hypersensitivity reactions. [see Warnings and Precautions (5.4)]
- Melphalan produces chromosomal aberrations in vitro and in vivo. Evomela should be considered potentially leukemogenic in humans. [see Warnings and Precautions (5.5)]
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage for Conditioning Treatment
The recommended dose of Evomela for conditioning treatment is 100 mg/m2/day administered over 30 minutes by intravenous infusion for 2 consecutive days (Day -3 and Day -2) prior to autologous stem cell transplantation (ASCT, Day 0). For patients who weigh more than 130% of their ideal body weight, body surface area should be calculated based on adjusted ideal body weight.
Administer prophylactic antiemetics [see Warnings and Precautions (5.2)].
2.2 Recommended Dosage for Palliative Treatment
The recommended dose of Evomela for palliative treatment is 16 mg/m2 administered as a single intravenous infusion over 15-20 minutes at 2-week intervals for 4 doses, then, after adequate recovery from toxicity, at 4‑week intervals.
Administer prophylactic anti-emetics [see Warnings and Precautions (5.2).
2.3 Dose Modification for Renal Impairment
For Conditioning Treatment: No dose adjustment is necessary.
For Palliative Treatment: Dosage reduction of up to 50% should be considered in patients with renal impairment (BUN ≥30 mg/dL) [see Use in Specific Populations (8.6)].
2.4 Preparation and Administration
Evomela is a cytotoxic drug. Follow applicable special handling and disposal procedures1.
Evomela is light sensitive. Retain in original carton until use.
Do not mix Evomela with other melphalan hydrochloride for injection drug products.
Reconstitution and Infusion Instructions:
- 1. Use normal saline solution (0.9% Sodium Chloride Injection, USP) (8.6 mL as directed) to reconstitute Evomela and make a 50 mg/10 mL (5 mg/ mL) nominal concentration of melphalan.
- The reconstituted Evomela drug product is stable for 24 hours at refrigerated temperature (5oC) without any precipitation due to the high solubility.
- The reconstituted Evomela drug product is stable for 1 hour at room temperature.
- 2. Calculate the required volume of Evomela needed for a patient’s dose and withdraw that volume from the vial(s).
- 3. Add the required volume of Evomela to the appropriate volume of 0.9% Sodium Chloride Injection, USP to a final concentration of 0.45 mg/mL.
- The Evomela admixture solution is stable for 4 hours at room temperature in addition to the 1 hour following reconstitution.
- 4. Infuse over 30 minutes via an injection port or central venous catheter.
- Evomela may cause local tissue damage should extravasation occur. Do not administer by direct injection into a peripheral vein. Administer Evomela by injecting slowly into a fast-running IV infusion via a central venous access line.
- Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Bone Marrow Suppression
For patients receiving Evomela as part of a conditioning regimen, myeloablation occurs in all patients. Do not begin the conditioning regimen if a stem cell product is not available for rescue. Monitor complete blood counts, provide supportive care for infections, anemia and thrombocytopenia until there is adequate hematopoietic recovery.
For patients receiving Evomela as palliative treatment, if the bone marrow has been compromised by prior irradiation, prior chemotherapy or is recovering from chemotherapy, the risk of severe myelosuppression with Evomela is increased. Perform periodic complete blood counts during the course of treatment with Evomela. Provide supportive care for infections, bleeding, and symptomatic anemia [see Adverse Reactions (6.1)].
5.2 Gastrointestinal Toxicity
For patients receiving Evomela as part of a conditioning regimen, nausea, vomiting, mucositis, and diarrhea may occur in over 50% of patients. Use prophylactic antiemetic medication. Provide supportive care for nausea, vomiting, diarrhea, and mucositis. The frequency of grade 3/4 mucositis in clinical studies was 13%. Provide nutritional support and analgesics for patients with severe mucositis. [see Dosage and Administration (2.1) and Adverse Reactions (6.1)].
For patients receiving Evomela as palliative treatment, nausea and vomiting, diarrhea, and oral ulceration may occur. Use prophylactic antiemetics. Provide supportive care for nausea, vomiting, diarrhea and mucositis.
5.3 Hepatotoxicity
Hepatic disorders ranging from abnormal liver function tests to clinical manifestations such as hepatitis and jaundice have been reported after treatment with melphalan. Hepatic veno-occlusive disease has also been reported. Monitor liver chemistries.
5.4 Hypersensitivity
Acute hypersensitivity reactions, including anaphylaxis, have occurred in approximately 2% of patients who received an intravenous formulation of melphalan. Symptoms may include urticaria, pruritus, edema, and skin rashes and, in some patients, tachycardia, bronchospasm, dyspnea, and hypotension. Discontinue treatment with Evomela for serious hypersensitivity reactions.
5.5 Secondary Malignancies
Melphalan has been shown to cause chromatid or chromosome damage in humans. Secondary malignancies such as myeloproliferative syndrome or acute leukemia have been reported in multiple myeloma patients treated with melphalan-containing chemotherapy regimens. The potential benefit of Evomela therapy must be considered against the possible risk of the induction of a secondary malignancy.
5.6 Embryo-Fetal Toxicity
Based on its mechanism of action, Evomela can cause fetal harm when administered to a pregnant woman. Melphalan is genotoxic, targets actively dividing cells, and was embryolethal and teratogenic in rats. Advise females of reproductive potential to avoid pregnancy during and after treatment with Evomela. If this drug is used during pregnancy or if the patient becomes pregnant while taking this drug, advise the patient of potential risk to the fetus [see Use in Specific Populations (8.1, 8.3)].
5.7 Infertility
Melphalan-based chemotherapy regimens have been reported to cause suppression of ovarian function in premenopausal women, resulting in persistent amenorrhea in approximately 9% of patients. Reversible or irreversible testicular suppression has also been reported [see Use in Specific Populations (8.3)].
-
6 ADVERSE REACTIONS
The following serious adverse reactions are described in more detail in other sections of the prescribing information.
6.1 Clinical Trials Experience
Because clinical studies are conducted under widely varying conditions, adverse reaction rates observed in the clinical studies of Evomela may not reflect the rates observed in practice.
The most common adverse reactions observed in at least 50% of patients with multiple myeloma treated with Evomela were neutrophil count decreased, white blood cell count decreased, lymphocyte count decreased, platelet count decreased, diarrhea, nausea, fatigue, hypokalemia, anemia, and vomiting.
Myeloablative Conditioning in Multiple Myeloma Patients Undergoing ASCT
The safety of Evomela was evaluated in 61 patients with multiple myeloma in a single arm clinical trial in which patients were administered Evomela at a dosage of 100 mg/m2/day administered over ~30 minutes (range: 24-48 minutes) by intravenous (IV) infusion for 2 consecutive days (Day -3 and Day -2) prior to autologous stem cell transplant (ASCT, Day 0).
Table 1 summarizes the adverse reactions from the single-arm trial in patients with multiple myeloma. Severe myelosuppression is expected and these adverse reactions are not listed below.
Table 1 Non-hematologic Adverse Reactions in ≥ 25% of Patients with Multiple Myeloma Who Received Evomela Conditioning for ASCT Adverse Reactions Number (%) of Patients
(N=61)All Grades Grade 3or 4 All Adverse Reactions
61
61
Diarrhea
57 (93%)
2 (3%)
Nausea
55 (90%)
1 (2%)
Fatigue
47 (77%)
1 (2%)
Hypokalemia
45 (74%)
17 (28%)
Vomiting
39 (64%)
0 (0%)
Hypophosphatemia
30 (49%)
29 (48%)
Decreased Appetite
30 (49%)
0 (0%)
Pyrexia
29 (48%)
2 (3%)
Constipation
29 (48%)
0 (0%)
Febrile Neutropenia
25 (41%)
17 (28%)
Mucosal Inflammation
23 (38%)
6 (10%)
Dizziness
23 (38%)
0 (0%)
Edema Peripheral
20 (33%)
0 (0%)
Stomatitis
17 (28%)
3 (5%)
Abdominal Pain
17 (28%)
0 (0%)
Dysgeusia
17 (28%)
0 (0%)
Dyspepsia
16 (26%)
0 (0%)
Serious Adverse Reactions
Twelve (20%) patients experienced a treatment emergent serious adverse reaction while on study. The most common serious adverse reactions (>1 patient, 1.6%) were pyrexia, hematochezia, febrile neutropenia, and renal failure. Treatment-related serious adverse reactions reported in >1 patient were pyrexia (n=2, 3%), febrile neutropenia (n=2, 3%), and hematochezia (n=2, 3%).
Palliative Treatment of Patients with Multiple Myeloma
The safety of melphalan was evaluated in 295 patients with multiple myeloma in the randomized clinical trial. One hundred and ninety-five patients were administered IV melphalan at a dosage of 16 mg/m2 q 2 weeks x 4 (over 6 weeks) followed by the same dose every 4 weeks. One hundred patients were administered oral melphalan at a dosage of 0.15 mg/kg/day x 7 followed by 0.05 mg/kg/day when WBC counts began to rise.
Severe myelotoxicity (WBC ≤1,000 and/or platelets ≤25,000) was more common in the IV melphalan arm (28%) than in the oral melphalan arm (11%).
An association was noted between poor renal function and myelosuppression; consequently, an amendment to the protocol required a 50% reduction in IV melphalan dose if the BUN was ≥30 mg/dL. The rate of severe leukopenia in the IV arm in the patients with BUN over 30 mg/dL decreased from 50% (8/16) before protocol amendment to 11% (3/28) after the amendment.
Before the dosing amendment, there was a 10% (8/77) incidence of drug-related death in the IV arm. After the dosing amendment, this incidence was 3% (3/108). This compares to an overall 1% (1/100) incidence of drug-related death in the oral melphalan arm.
-
7 DRUG INTERACTIONS
No formal drug interaction studies have been conducted. The development of severe renal impairment has been reported in patients treated with a single dose of intravenous melphalan 140-250 mg/m2 followed by standard oral doses of cyclosporine. Intravenous melphalan may also reduce the threshold for BCNU lung toxicity. When nalidixic acid and IV melphalan are given simultaneously, the incidence of severe hemorrhagic necrotic enterocolitis has been reported to increase in pediatric patients.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Based on its mechanism of action, Evomela can cause fetal harm when administered to a pregnant woman, including teratogenicity and/or embryo-fetal lethality. Melphalan is a genotoxic drug and can cause chromatid or chromosome damage in humans [see Nonclinical Toxicology (13.1)]. In animal studies, melphalan was embryolethal and teratogenic in rats at doses below the recommended clinical doses [see Data]. Advise a pregnant woman of the potential risk to a fetus..
The background risk of major birth defects and miscarriage for the indicated populations are unknown. However, the background risk in the U.S. general population of major birth defects is 2-4% and of miscarriage is 15-20% of clinically recognized pregnancies.
Data
Animal Data
Adequate animal studies have not been conducted with intravenous melphalan. Melphalan was embryolethal and teratogenic in rats following oral administration of 6 to 18 mg/m2/day for 10 days (0.06 to 0.18 times the highest recommended clinical dose of 100 mg/m2/day) and intraperitoneal administration of 18 mg/m2 (0.18 times the highest recommended clinical dose). Malformations resulting from melphalan administration included alterations of the brain (underdevelopment, deformation, meningocele, and encephalocele) and eye (anophthalmia and microphthalmos), reduction of the mandible and tail, and hepatocele (exomphaly).
8.2 Lactation
Risk Summary
It is not known whether melphalan is present in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from melphalan, breastfeeding is not recommended during treatment with Evomela.
8.3 Females and Males of Reproductive Potential
Contraception
Females
Evomela administration can cause fetal harm when administered to a pregnant woman. Advise females of reproductive potential to avoid pregnancy, which may include the use of effective contraception methods, during and after treatment with Evomela.
Males
Evomela administration may damage spermatozoa and testicular tissue, resulting in possible genetic fetal abnormalities. Advise males with female sexual partners of reproductive potential to use effective contraception during and after treatment with Evomela [see Nonclinical Toxicology (13.1)].
Infertility
Females
Melphalan causes suppression of ovarian function in premenopausal women, resulting in amenorrhea in a significant number of patients.
Males
Reversible and irreversible testicular suppression has been reported in male patients after administration of melphalan.
8.4 Pediatric Use
Pediatric patients were not included in clinical trials. Safety and effectiveness have not been established in pediatric patients.
8.5 Geriatric Use
Of the total number of subjects in the single-arm pivotal study of Evomela, 30% were 65 and over, but no patients were 75 and over. No overall differences in safety or effectiveness were observed between these subjects and younger subjects. A greater incidence of engraftment syndrome was observed in older patients; 7% (3 of 43) of patients younger than 65 years old versus 28% (5 of 18) of patients 65 years old and over.
8.6 Patients with Renal Impairment
For Conditioning Treatment, renal impairment is not a criterion for dose reduction or exclusion from Evomela therapy.
For Palliative Treatment, consider dose reduction for patients with renal impairment receiving Evomela. Bone marrow suppression has been observed in patients with BUN levels ≥30 mg/dL. A 50% reduction in the IV melphalan dose decreased the incidence of severe bone marrow suppression in the latter portion of this study [see Dosage and Administration (2.3)].
-
10 OVERDOSAGE
Overdoses resulting in death have been reported with melphalan. Overdoses, including doses up to 290 mg/m2, have produced the following symptoms: severe nausea and vomiting, decreased consciousness, convulsions, muscular paralysis, and cholinomimetic effects. Severe mucositis, stomatitis, colitis, diarrhea, and hemorrhage of the gastrointestinal tract occur at high doses (>100 mg/m2). Elevations in liver enzymes and veno-occlusive disease occur infrequently. Significant hyponatremia, caused by an associated inappropriate secretion of ADH syndrome, has been observed. Nephrotoxicity and adult respiratory distress syndrome have been reported rarely.
The principal toxic effect is bone marrow suppression leading to leucopenia, thrombocytopenia and anemia. Hematologic parameters should be closely followed for 3 to 6 weeks. An uncontrolled study suggests that administration of autologous bone marrow or hematopoietic growth factors (i.e., sargramostim, filgrastim) may shorten the period of pancytopenia. General supportive measures together with appropriate blood transfusions and antibiotics should be instituted as deemed necessary by the physician. This drug is not removed from plasma to any significant degree by hemodialysis or hemoperfusion. A pediatric patient survived a 254 mg/m2 overdose treated with standard supportive care.
-
11 DESCRIPTION
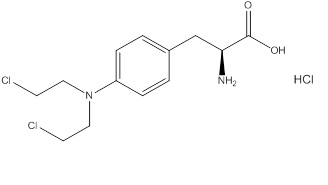
Evomela contains melphalan hydrochloride, an alkylating drug, as the active ingredient. The chemical name of melphalan hydrochloride is 4-[bis(2-chloroethyl)amino]-L-phenylalanine hydrochloride. Its molecular formula is C13H18Cl2N2O2 HCl and the molecular weight is 341.67. The structural formula is:
Melphalan hydrochloride is a white to off-white powder, with a melting range of 199°C − 201°C. It is practically insoluble in water, but freely soluble in 1 N HCl and methanol.
Evomela (melphalan) for injection is supplied as a sterile white to off-white lyophilized powder in a single-dose vial for intravenous use. Each vial contains 50 mg melphalan free base equivalent to 56 mg melphalan hydrochloride and 2700 mg Betadex Sulfobutyl Ether Sodium, NF.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Melphalan is an alkylating agent of the bischloroethylamine type. As a result, its cytotoxicity appears to be related to the extent of its interstrand cross-linking with DNA, probably by binding at the N7 position of guanine. Like other bifunctional alkylating agents, it is active against both resting and rapidly dividing tumor cells.
12.2 Pharmacodynamics
Cardiac Electrophysiology
Pharmacokinetic-pharmacodynamic analysis showed that Evomela administration increased heart rate-corrected QT interval. The mean change from baseline for QTcF at the mean Cmax of 4701 ng/mL was 8.0 msec. Patients treated with 200 mg/m2 Evomela showed an increase of heart rate (mean change of 7.5 bpm from baseline).
12.3 Pharmacokinetics
Following injection, drug plasma concentrations declined rapidly in a biexponential manner with distribution phase and terminal elimination phase half-lives of approximately 10 and 75 minutes, respectively. Estimates of average total body clearance (CL) varied among studies, but typical values of approximately 7 to 9 mL/min/kg (250 to 325 mL/min/m2) were observed. One study reported that on repeat dosing of 0.5 mg/kg every 6 weeks, the clearance of melphalan decreased from 8.1 mL/min/kg after the first course, to 5.5 mL/min/kg after the third course, but did not decrease appreciably after the third course. Mean (±SD) peak melphalan plasma concentrations in myeloma patients given IV melphalan at doses of 10 or 20 mg/m2 were 1.2 ± 0.4 and 2.8 ± 1.9 mcg/mL, respectively.
Distribution
The steady-state volume of distribution of melphalan is 0.5 L/kg. Melphalan penetrates into cerebrospinal fluid (CSF). Average melphalan binding to plasma proteins ranges from approximately 50% to 90%. Serum albumin is the major binding protein, accounting for approximately 40% to 60% of the plasma protein binding, while α1-acid glycoprotein accounts for about 20% of the plasma protein binding. Approximately 30% of melphalan is (covalently) irreversibly bound to plasma proteins.
Elimination
Metabolism
Melphalan is eliminated from plasma primarily by chemical hydrolysis to inactive monohydroxymelphalan and dihydroxymelphalan.
Excretion
The contribution of renal excretion to melphalan clearance appears to be low (mean values of amount of melphalan excreted in urine range from 5.8-21.3%).
Specific Populations
Patient Body Weight
A typical patient with an ideal body weight (IBW) of 45 kg has a 28% decrease in clearance relative to a patient with IBW of 70 kg, while a patient with an IBW of 100 kg has a 31% increase in clearance as compared to a patient with an IBW of 70 kg.
Renal Impairment
A decrease in estimated creatinine CL from 100 mL/min to 30 mL/min results in 28.2% reduction in CL for a typical person with an IBW of 70 kg.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Adequate and well-controlled carcinogenicity studies have not been conducted in animals. However, intraperitoneal (IP) administration of melphalan in rats (5.4 to 10.8 mg/m2) and in mice (2.25 to 4.5 mg/m2) 3 times per week for 6 months followed by 12 months post-dose observation produced peritoneal sarcomas and lung tumors, respectively.
Intramuscular administration of melphalan at 6 and 60 mg/m2 produced structural aberrations of the chromatid and chromosomes in bone marrow cells of Wistar rats.
-
14. CLINICAL STUDIES
14.1 Myeloablative Conditioning in Patients with Multiple Myeloma Undergoing ASCT
An open-label, single-arm, non-randomized trial of Evomela was conducted at 5 US centers. The 61 patients enrolled had symptomatic multiple myeloma, and had at least 2 × 106 CD34+ cells/kg cryopreserved stem cells available. The median age was 62 years (range 32 to 73); 57% male, 80% white, 18% black, 2% Asian. Evomela was administered at 100 mg/m2/day over 30 minutes by IV infusion for two consecutive days (Day -3 and Day -2) prior to ASCT (Day 0).
The objective of the trial was to determine the overall safety and toxicity profile of 200 mg/m2 of Evomela in patients with multiple myeloma undergoing ASCT. [See Adverse Reactions (6.1)] The efficacy was evaluated by the International Myeloma Working Group response criteria comparing the disease response immediately prior to the ASCT procedure to the disease response assessed 90 to 100 days post-transplant. In addition, successful myeloablation, and time to engraftment were evaluated.
The overall response rate (partial response or better) improved from 79% (48 of 61) prior to the ASCT procedure to 95% (58 of 61) at 90 to 100 days post-transplant. There was also an increase in the number of patients with a stringent complete response from 0 patients prior to the ASCT procedure to 16% (10 of 61) at 90 to 100 days post-transplant.
Myeloablation and engraftment were evaluated by complete blood cell count tests daily until neutrophil and platelet engraftment, and then weekly until Day 30, and at Day 60 and Day 90-100. Myeloablation was defined as any of the following: absolute neutrophil count (ANC) < 500/mm3, absolute lymphocyte count < 100/mm3, or platelet count < 20,000/mm3). Neutrophil engraftment was defined as ANC > 500/mm3 ×3 consecutive daily assessments. Platelet engraftment was defined as untransfused platelet counts > 20,000/mm3 ×3 consecutive daily assessments. Nonengraftment was defined as failure to reach an ANC > 500/mm3 ×3 consecutive daily assessments by Day 90-100.
Myeloablation, neutrophil engraftment and platelet engraftment were achieved by all 61 patients. Myeloablation occurred on ASCT Day 5 (range ASCT days -1 to 6) with the median time to myeloablation from dosing of 8 days. The median time to neutrophil engraftment was 12 days (range ASCT days 10 to 16). The median time to platelet engraftment was 13 days (range ASCT days 10 to 28).
14.2 Palliative Treatment of Patients with Multiple Myeloma
A randomized trial compared prednisone plus IV melphalan to prednisone plus oral melphalan in the treatment of multiple myeloma. As discussed below, Overall Response Rates at Week 22 were comparable; however, because of changes in trial design, conclusions as to the relative activity of the 2 formulations after Week 22 are impossible to make.
Both arms received oral prednisone starting at 0.8 mg/kg/day with doses tapered over 6 weeks. Melphalan doses in each arm were:
- Arm 1: Oral melphalan 0.15 mg/kg/day x 7 followed by 0.05 mg/kg/day when WBC began to rise.
- Arm 2: IV melphalan 16 mg/m2 q 2 weeks x 4 (over 6 weeks) followed by the same dose every 4 weeks.
One hundred seven patients were randomized to the oral melphalan arm and 203 patients to the IV melphalan arm. More patients had a poor-risk classification (58% versus 44%) and high tumor load (51% versus 34%) on the oral arm compared to the IV arm (P<0.04). Response rates at Week 22 are shown in the following table:
Table 2 Response Rates at Week 22 for Patients with Multiple Myeloma Who Received Oral or IV Melphalan with Prednisone Initial Arm
Evaluable Patients
Responders n (%)
P
Oral melphalan
100
44 (44%)
P>0.2
IV melphalan
195
74 (38%)
Because of changes in protocol design after Week 22, other efficacy parameters such as Response Duration and Survival could not be compared.
- 15 REFERENCES
-
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
Evomela is supplied in a single carton containing one (1) vial. Each 50 mg vial contains a white to off-white lyophilized powder in single-dose vial for reconstitution (after reconstitution the solution is clear and coloress to light yellow). Each vial contains 50 mg melphalan free base equivalent to 56 mg melphalan hydrochloride.
NDC: 68152-109-00: Individual carton of Evomela 20 mL single-dose vial containing 50 mg melphalan free base.
16.2 Storage and Handling
Store Evomela at room temperature 25°C (77°F). Temperature excursions are permitted between 15-30°C (59-86°F). [see USP Controlled Room Temperature]
Evomela is light sensitive. Retain in original carton until use.
Melphalan is a cytotoxic drug. Follow special handling and disposal procedure [see References (15)].
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information).
Advise patients or their caregivers of the following:
Low Blood Cell Counts
- To report any signs or symptoms of thrombocytopenia, leukopenia (neutropenia and lymphopenia), and anemia. Inform patients of the need for routine blood counts [see Warnings and Precautions (5.1)].
Mucositis
- Inform patients of the signs and symptoms of mucositis. Instruct patients on ways to reduce the risk of its development, and on ways to maintain nutrition and control discomfort if it occurs [see Warnings and Precautions (5.2)].
Nausea, Vomiting and Diarrhea
- To report symptoms of nausea, vomiting and diarrhea, so that appropriate antiemetic and/or antidiarrheal medications can be administered [see Warnings and Precautions (5.2)].
Allergic Reactions
- To immediately report symptoms of hypersensitivity reactions including changes involving the skin, breathing or heart rate, so that antihistamine or corticosteroid therapy can be administered [see Warnings and Precautions (5.4)].
Secondary cancers
- To understand the potential long-term risks related to secondary malignancy [see Warnings and Precautions (5.5 )].
Birth Defects
- Advise pregnant women of the potential risk to a fetus [see Warnings and Precautions (5.6) and Use in Specific Populations (8.1)].
- Advise females of reproductive potential to avoid pregnancy, which may include use of effective contraception during and after treatment with Evomela. Advise females to contact their healthcare provider if they become pregnant, or if pregnancy is suspected, while taking Evomela [see Warnings and Precautions (5.6) and Use in Specific Populations (8.1, 8.3)].
- Inform both females and males of reproductive potential about the risk for infertility [see Warnings and Precautions (5.7) and Use in Specific Populations (8.3)].
- Advise women that breastfeeding is not recommended during treatment with Evomela [see Use in Specific Populations (8.2)].
- Advise males with female sexual partners of reproductive potential that they should use effective contraception during and after treatment with Evomela [see Use in Specific Populations (8.3)].
-
Patient Package Insert
PATIENT INFORMATION
EVOMELA (ev-ō-meh-lah)
(melphalan) for injection, for intravenous use
What is Evomela?
Evomela is a prescription medicine used in people with a type of cancer called multiple myeloma:
- before receiving a stem cell transplant (conditioning treatment)
- as a part of care to support symptom relief (palliative treatment), in people who cannot take medicine by mouth
It is not known if Evomela is safe and effective in children.
Do not receive Evomela if you are allergic to melphalan or any of the ingredients in Evomela. See the end of this leaflet for a complete list of ingredients in Evomela.
Before you receive Evomela, tell your doctor about all of your medical conditions, including if you:
- have an infection
- have had chemotherapy treatment
- have nausea, vomiting, or diarrhea
- have liver or kidney problems
-
are pregnant or plan to become pregnant. Evomela can harm your unborn baby. You should not become pregnant during and after treatment with Evomela. Tell your doctor right away if you become pregnant during treatment with Evomela.
- Females who are able to become pregnant should use effective birth control during and after treatment with Evomela. Talk with your doctor about how long to use birth control after treatment with Evomela.
- Males who have female partners who are able to become pregnant should use effective birth control during and after treatment with Evomela. Talk with your doctor about how long to use birth control after treatment with Evomela.
- are breastfeeding or plan to breastfeed. It is not known if Evomela passes into your breast milk. You should not breastfeed during treatment with Evomela.
Tell your doctor about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
How will I receive Evomela?
- Evomela is given to you into your vein through an intravenous (IV) line over 15 to 30 minutes.
- Your doctor will do blood tests before and during your treatment with Evomela.
- Your doctor may prescribe medicines to help prevent nausea.
What are the possible side effects of Evomela?
Evomela may cause serious side effects, including:
-
Low blood cell counts are common with Evomela and can be serious. Your doctor will do blood tests as needed to check your blood counts during your treatment with Evomela.
- Low platelet counts: Tell your doctor right away if you have unusual bleeding or bruising under your skin.
- Low red blood cell counts: Tell your doctor if you are feeling weak, tired, or you get tired easily, you look pale, or you feel short of breath.
- Low white blood cell counts: A low white blood cell count can cause you to get infections, which may be serious. Tell your doctor right away if you have symptoms of infection, such as fever, chills, cough, pain, or burning during urination.
- Redness and sores of the lining of the mouth, lips, throat, stomach, and genitals (mucositis). Discomfort or pain due to mucositis may happen during treatment with Evomela. Your doctor will tell you about ways to maintain nutrition and help control the discomfort from mucositis.
- Nausea, vomiting, and diarrhea are common with Evomela and can sometimes be serious. Tell your doctor if you get nausea, vomiting, or diarrhea. Your doctor may prescribe medicines to help prevent or treat these side effects.
- Liver problems. Your doctor will check you for liver problems during treatment with Evomela. Tell your doctor right away if you get any of the following signs or symptoms:
ᴼ yellowing of your skin or the whites of your eyes ᴼ severe nausea or vomiting
ᴼ pain on the right side of your stomach-area (abdomen) ᴼ dark urine (tea colored)
- Allergic reactions. Tell your doctor right away if you get any of the following signs or symptoms:
ᴼ skin reactions, including welts, rash, itching, and ᴼ feel lightheaded or dizzy
redness ᴼ blurry vision
ᴼ fast heartbeat ᴼ swelling of your face, tongue, or throat
ᴼ shortness of breath or trouble breathing
- Secondary cancers. New cancers have happened in people who have been treated with Evomela.
- Infertility. Evomela may cause fertility problems in males and females. Talk to your doctor if this is a concern for you.
The most common side effects of Evomela include tiredness and low potassium level.
These are not all the possible side effects of Evomela. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
General information about the safe and effective use of Evomela.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use Evomela for a condition for which it was not prescribed. Do not give Evomela to other people, even if they have the same symptoms that you have. It may harm them. You can ask your pharmacist or doctor for information about Evomela that is written for health professionals.
What are the ingredients in Evomela?
Active ingredient: melphalan hydrochloride
Inactive ingredient: Betadex Sulfobutyl Ether SodiumManufactured for: Spectrum Pharmaceuticals, Inc. Irvine, CA 92618
For more information, go to www.evomela.com or call 1-888-292-9617.
- This Patient Information has been approved by the U.S. Food and Drug Administration. Issued: March 2016
Manufactured for:
Spectrum Pharmaceuticals, Inc.
Irvine, CA 92618
-
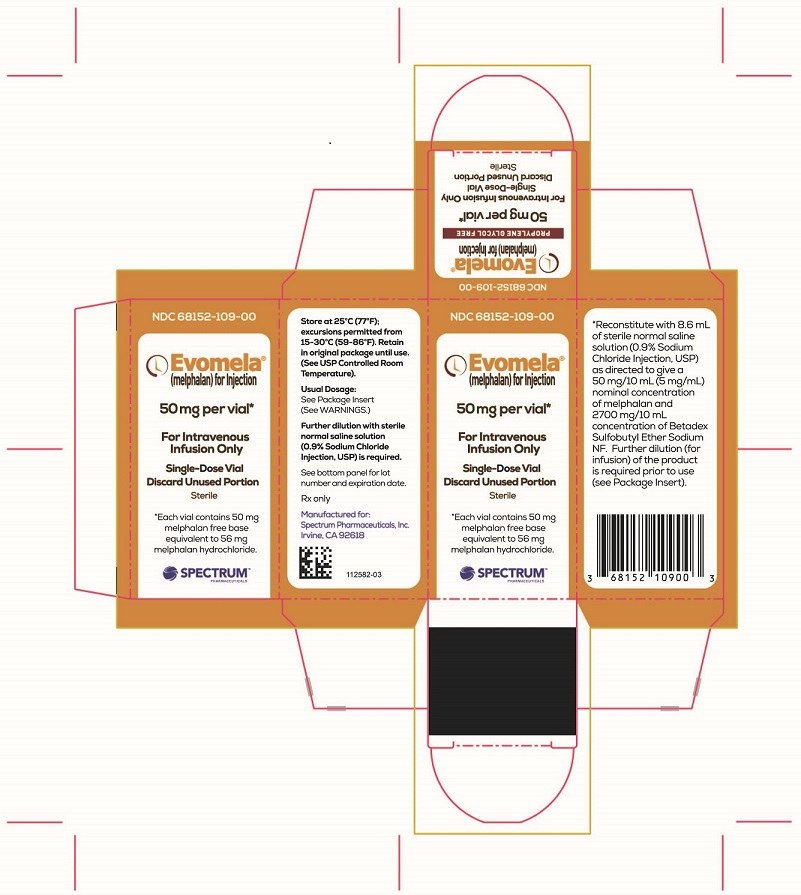
PACKAGE/LABEL PRINCIPAL DISPLAY PANEL
Evomela Carton Label
NDC: 68152-109-00
Evomela® (melphalan) for Injection
50 mg per vial*
For Intravenous Infusion Only
Single-Use Vial
Discard Unused Portion
Sterile
*Each vial contains 50 mg melphalan free base equivalent to 56 mg melphalan hydrochloride.
Spectrum Pharmaceuticals
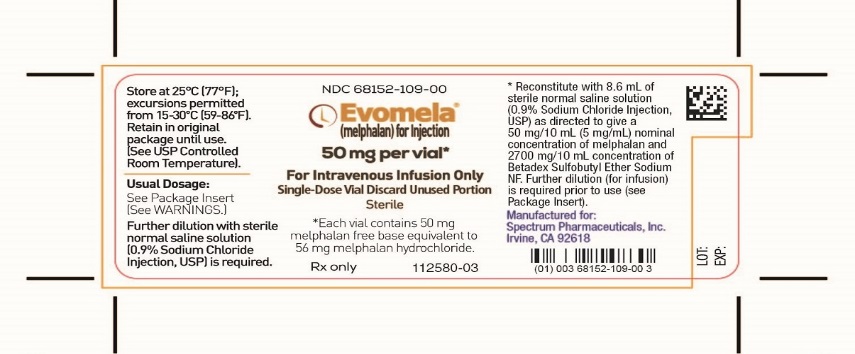
Evomela Vial Label
NDC: 68152-109-00
Evomela® (melphalan) for Injection
50 mg per vial*
For Intravenous Infusion Only
Single-Use Vial Discard Unused Portion
Sterile
*Each vial contains 50 mg melphalan free base equivalent to 56 mg melphalan hydrochloride.
Rx only
-
INGREDIENTS AND APPEARANCE
EVOMELA
melphalan injection, powder, lyophilized, for solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 68152-109 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength MELPHALAN HYDROCHLORIDE (UNII: 1VXP4V453T) (MELPHALAN - UNII:Q41OR9510P) MELPHALAN 50 mg in 10 mL Inactive Ingredients Ingredient Name Strength BETADEX SULFOBUTYL ETHER SODIUM (UNII: 2PP9364507) 2700 mg in 10 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 68152-109-00 1 in 1 CARTON 03/31/2016 1 20 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA207155 03/31/2016 Labeler - Spectrum Pharmaceuticals, Inc. (790888002)
Trademark Results [EVOMELA]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 EVOMELA 86508057 4994159 Live/Registered |
ACROTECH BIOPHARMA LLC 2015-01-20 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.