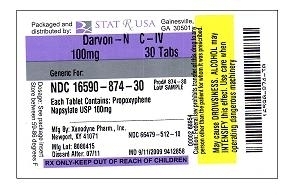
DARVON-N- propoxyphene napsylate tablet, film coated
Darvon-N by
Drug Labeling and Warnings
Darvon-N by is a Prescription medication manufactured, distributed, or labeled by Stat Rx USA. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
DESCRIPTION
DESCRIPTION
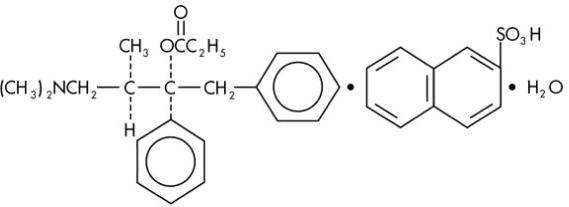
Darvon-N contains propoxyphene napsylate, USP which is an odorless, white crystalline powder with a bitter taste. It is very slightly soluble in water and soluble in methanol, ethanol, chloroform, and acetone. Chemically, it is (αS,1R)-α-[2-(Dimethylamino)-1-methylethyl]-α-phenylphenethyl propionate compound with 2-naphthalenesulfonic acid (1:1) monohydrate, which can be represented by the accompanying structural formula. Its molecular weight is 565.72
Propoxyphene napsylate differs from propoxyphene hydrochloride in that it allows more stable liquid dosage forms and tablet formulations. Because of differences in molecular weight, a dose of 100 mg (176.8 μmol) of propoxyphene napsylate is required to supply an amount of propoxyphene equivalent to that present in 65 mg (172.9 μmol) of propoxyphene hydrochloride.
Each tablet of Darvon-N contains 100 mg (176.8 μmol) propoxyphene napsylate. The tablet also contains cellulose, cornstarch, iron oxides, lactose, magnesium stearate, silicon dioxide, stearic acid, and titanium dioxide.
-
CLINICAL PHARMACOLOGY
CLINICAL PHARMACOLOGY Pharmacology
Propoxyphene is a centrally acting opiate analgesic. In vitro studies demonstrated propoxyphene and the metabolite norpropoxyphene inhibit sodium channels (local anesthetic effect) with norpropoxyphene being approximately 2-fold more potent than propoxyphene and propoxyphene approximately 10-fold more potent than lidocaine. Propoxyphene and norpropoxyphene inhibit the voltage-gated potassium current carried by cardiac rapidly activating delayed rectifier (hERG) channels with approximately equal potency. It is unclear if the effects on ion channels occur within therapeutic dose range.
Pharmacokinetics AbsorptionPeak plasma concentrations of propoxyphene are reached in 2 to 2.5 h. After a 65-mg oral dose of propoxyphene hydrochloride, peak plasma levels of 0.05 to 0.1 μg/mL for propoxyphene and 0.1 to 0.2 μg/mL for norpropoxyphene (major metabolite) are achieved. Repeated doses of propoxyphene at 6 h intervals lead to increasing plasma concentrations, with a plateau after the ninth dose at 48 h. Propoxyphene has a half-life of 6 to 12 h, whereas that of norpropoxyphene is 30 to 36 h.
DistributionPropoxyphene is about 80% bound to proteins and has a large volume of distribution, 16 L/kg.
MetabolismPropoxyphene undergoes extensive first-pass metabolism by intestinal and hepatic enzymes. The major route of metabolism is cytochrome CYP3A4 mediated N-demethylation to norpropoxyphene, which is excreted by the kidneys. Ring hydroxylation and glucuronide formation are minor metabolic pathways.
ExcretionIn 48 h, approximately 20 to 25% of the administered dose of propoxyphene is excreted via the urine, most of which is free or conjugated norpropoxyphene. The renal clearance rate of propoxyphene is 2.6 L/min.
SPECIAL POPULATIONS Geriatric PatientsAfter oral administration of propoxyphene in elderly patients (70-78 years), much longer half-lives of propoxyphene and norpropoxyphene have been reported (propropoxyphene 13 to 35 h, norpropoxyphene 22 to 41 h). In addition, the AUC was an average of 3-fold higher and the Cmax was an average of 2.5-fold higher in the elderly when compared to a younger (20-28 years) population. Longer dosage intervals may be considered in the elderly because the metabolism of propoxyphene may be reduced in this patient population. After multiple oral doses of propoxyphene in elderly patients (70-78 years), the Cmax of the metabolite (norpropoxyphene) was increased 5-fold.
Pediatric PatientsPropoxyphene has not been studied in pediatric patients.
Hepatic ImpairmentNo formal pharmacokinetic study of propoxyphene has been conducted in patients with mild, moderate or severe hepatic impairment.
After oral administration of propoxyphene in patients with cirrhosis, plasma concentrations of propoxyphene were considerably higher and norpropoxyphene concentrations were much lower than in control patients. This is presumably because of a decreased first-pass metabolism of orally administered propoxyphene in these patients. The AUC ratio of norpropoxyphene: propoxyphene was significantly lower in patients with cirrhosis (0.5 to 0.9) than in controls (2.5 to 4).
Renal ImpairmentNo formal pharmacokinetic study of propoxyphene has been conducted in patients with mild, moderate or severe renal impairment.
After oral administration of propoxyphene in anephric patients, the AUC and Cmax values were an average of 76% and 88% greater, respectively. Dialysis removes only insignificant amounts (8%) of administered dose of propoxyphene.
Drug InteractionsThe metabolism of propoxyphene may be altered by strong CYP3A4 inhibitors (such as ritonavir, ketoconazole, itraconazole, troleandomycin, clarithromycin, nelfinavir, nefazadone, amiodarone, amprenavir, aprepitant, diltiazem, erythromycin, fluconazole, fosamprenavir, grapefruit juice, and verapamil) leading to enhanced propoxyphene plasma levels. On the other hand, strong CYP3A4 inducers such as rifampin may lead to enhanced metabolite (norpropoxyphene) levels.
Propoxyphene is also thought to possess CYP3A4 and CYP2D6 enzyme inhibiting properties. Coadministration with a drug that is a substrate of CYP3A4 or CYP2D6, may result in higher plasma concentrations and increased pharmacologic or adverse effects of that drug.
- INDICATIONS & USAGE
-
CONTRAINDICATIONS
CONTRAINDICATIONS
Darvon-N is contraindicated in patients with known hypersensitivity to propoxyphene.
Darvon-N is contraindicated in patients with significant respiratory depression (in unmonitored settings or the absence of resuscitative equipment) and patients with acute or severe asthma or hypercarbia.
Darvon-N is contraindicated in any patient who has or is suspected of having paralytic ileus.
-
WARNINGS AND PRECAUTIONS
WARNINGS Risk of Overdose
There have been numerous cases of accidental and intentional overdose with propoxyphene products either alone or in combination with other CNS depressants, including alcohol. Fatalities within the first hour of overdosage are not uncommon. Many of the propoxyphene-related deaths have occurred in patients with previous histories of emotional disturbances or suicidal ideation/attempts and/or concomitant administration of sedatives, tranquilizers, muscle relaxants, antidepressants, or other CNS-depressant drugs. Do not prescribe propoxyphene for patients who are suicidal or have a history of suicidal ideation.
Respiratory DepressionRespiratory depression is the chief hazard from all opioid agonist preparations. Respiratory depression occurs most frequently in elderly or debilitated patients, usually following large initial doses in non-tolerant patients, or when opioids are given in conjunction with other agents that depress respiration. Darvon-N should be used with extreme caution in patients with significant chronic obstructive pulmonary disease or cor pulmonale, and in patients having substantially decreased respiratory reserve, hypoxia, hypercapnia, or pre-existing respiratory depression. In such patients, even usual therapeutic doses of Darvon-N may decrease respiratory drive to the point of apnea. In these patients alternative non-opioid analgesics should be considered, and opioids should be employed only under careful medical supervision at the lowest effective dose.
Hypotensive EffectDarvon-N, like all opioid analgesics, may cause severe hypotension in an individual whose ability to maintain blood pressure has been compromised by a depleted blood volume, or after concurrent administration with drugs such as phenothiazines or other agents which compromise vasomotor tone. Darvon-N may produce orthostatic hypotension in ambulatory patients. Darvon-N, like all opioid analgesics, should be administered with caution to patients in circulatory shock, since vasodilatation produced by the drug may further reduce cardiac output and blood pressure.
Head Injury and Increased Intracranial PressureThe respiratory depressant effects of narcotics and their capacity to elevate cerebrospinal fluid pressure may be markedly exaggerated in the presence of head injury, other intracranial lesions or a pre-existing increase in intracranial pressure. Furthermore, narcotics produce adverse reactions which may obscure the clinical course of patients with head injuries.
Drug InteractionsThe concomitant use of propoxyphene and CNS depressants, including alcohol, can result in potentially serious adverse events including death. Because of its added depressant effects, propoxyphene should be prescribed with caution for those patients whose medical condition requires the concomitant administration of sedatives, tranquilizers, muscle relaxants, antidepressants, or other CNS-depressant drugs.
Usage in Ambulatory PatientsPropoxyphene may impair the mental and/or physical abilities required for the performance of potentially hazardous tasks, such as driving a car or operating machinery. The patient should be cautioned accordingly.
Use with AlcoholPatients should be cautioned about the concomitant use of propoxyphene products and alcohol because of potentially serious CNS-additive effects of these agents that can lead to death.
-
BOXED WARNING
(What is this?)
BOXED WARNING
WARNINGS
There have been numerous cases of accidental and intentional overdose with propoxyphene products either alone or in combination with other CNS depressants, including alcohol. Fatalities within the first hour of overdosage are not uncommon. Many of the propoxyphene-related deaths have occurred in patients with previous histories of emotional disturbance or suicidal ideation/attempts and /or concomitant administration of sedatives, tranquilizers, muscle relaxants, antidepressants, or other CNS-depressant drugs. Do not prescribe propoxyphene for patients who are suicidal or have a history of suicidal ideation.
The metabolism of propoxyphene may be altered by strong CYP3A4 inhibitors (such as ritonavir, ketoconazole, itraconazole, troleandomycin, clarithromycin, nelfinavir, nefazadone, amiodarone, amprenavir, aprepitant, diltiazem, erthromycin, fulconazole, fosamprenavir, grapefruit juice, and verapamil) leading to enhanced propoxyphene plasma levels. Patients receiving propoxyphene and any CYP3A4 inhibitor should be carefully monitored for an extended period of time and dosage adjustments should be made if warranted (see Clinical Pharmacology - Drug Interactions, Warnings, Precautions and Dosage and Administration for further information.)
-
PRECAUTIONS
PRECAUTIONS Tolerance and Physical Dependence
Tolerance is the need for increasing doses of opioids to maintain a defined effect such as analgesia (in the absence of disease progression or other external factors). Physical dependence is manifested by withdrawal symptoms after abrupt discontinuation of a drug or upon administration of an antagonist. Physical dependence and tolerance are not unusual during chronic opioid therapy.
The opioid abstinence or withdrawal syndrome is characterized by some or all of the following: restlessness, lacrimation, rhinorrhea, yawning, perspiration, chills, myalgia, and mydriasis. Other symptoms also may develop, including: irritability, anxiety, backache, joint pain, weakness, abdominal cramps, insomnia, nausea, anorexia, vomiting, diarrhea, or increased blood pressure, respiratory rate, or heart rate. In general, opioids should not be abruptly discontinued (see Dosage and Administration: Cessation of Therapy).
If Darvon-N is abruptly discontinued in a physically dependent patient, an abstinence syndrome may occur (see Drug Abuse and Dependance). If signs and symptoms of withdrawal occur, patients should be treated by reinstitution of opioid therapy followed by gradual tapered dose reduction of Darvon-N combined with symptomatic support (see Dosage and Administration: Cessation of Therapy).
Use in Pancreatic/Biliary Tract DiseaseDarvon-N may cause spasm of the sphincter of Oddi and should be used with caution in patients with biliary tract disease, including acute pancreatitis. Opioids like Darvon-N may cause increases in the serum amylase level.
Hepatic or Renal ImpairmentInsufficient information exists to make appropriate dosing recommendations regarding the use of either propoxyphene in patients with hepatic or renal impairment as a function of degree of impairment. Higher plasma concentrations and/or delayed elimination may occur in case of impaired hepatic function and/or impaired renal function (see Clinical Pharmacology). If the drug is used in these patients, it should be used with caution because of the hepatic metabolism and renal excretion of propoxyphene metabolites.
Information for Patients/Caregivers- Patients should be advised to report pain and adverse experiences occurring during therapy. Individualization of dosage is essential to make optimal use of this medication.
- Patients should be advised not to adjust the dose of Darvon-N without consulting the prescribing professional.
- Patients should be advised that Darvon-N may impair mental and/or physical ability required for the performance of potentially hazardous tasks (e.g., driving, operating heavy machinery).
- Patients should not combine Darvon-N with central nervous system depressants (e.g., sleep aids, tranquilizers) except by the orders of the prescribing physician, because additive effects may occur.
- Patients should be instructed not to consume alcoholic beverages, including prescription and over-the-counter medications that contain alcohol, while using Darvon-N because of risk of serious adverse events including death.
- Women of childbearing potential who become, or are planning to become, pregnant should be advised to consult their physician regarding the effects of analgesics and other drug use during pregnancy on themselves and their unborn child.
- Patients should be advised that Darvon-N is a potential drug of abuse. They should protect it from theft, and it should never be given to anyone other than the individual for whom it was prescribed.
- Patients should be advised that if they have been receiving treatment with Darvon-N for more than a few weeks and cessation of therapy is indicated, it may be appropriate to taper the Darvon-N dose, rather than abruptly discontinue it, due to the risk of precipitating withdrawal symptoms. Their physician can provide a dose schedule to accomplish a gradual discontinuation of the medication.
Propoxyphene is metabolized mainly via the human cytochrome P450 3A4 isoenzyme system (CYP3A4), therefore potential interactions may occur when propoxyphene is administered concurrently with agents that affect CYP3A4 activity.
The metabolism of propoxyphene may be altered by strong CYP3A4 inhibitors (such as ritonavir, ketoconazole, itraconazole, troleandomycin, clarithromycin, nelfinavir, nefazadone, amiodarone, amprenavir, aprepitant, diltiazem, erythromycin, fluconazole, fosamprenavir, grapefruit juice, and verapamil) leading to enhanced propoxyphene plasma levels. Coadministration with agents that induce CYP3A4 activity may reduce the efficacy of propoxyphene. Strong CYP3A4 inducers such as rifampin may lead to enhanced metabolite (norpropoxyphene) levels.
Propoxyphene is also thought to possess CYP3A4 and CYP2D6 enzyme inhibiting properties and coadministration with drugs that rely on either of these enzymes for metabolism may result in increased pharmacologic or adverse effects of that drug. Severe neurologic signs, including coma, have occurred with concurrent use of carbamazepine (metabolized by CYP3A4).
Increased risk of bleeding has been observed with warfarin-like agents when given along with propoxyphene; however, the mechanistic basis of this interaction is unknown.
CNS DepressantsPatients receiving narcotic analgesics, general anesthetics, phenothiazines, other tranquilizers, sedative-hypnotics or other CNS depressants (including alcohol) concomitantly with propoxyphene may exhibit an additive CNS depression. Interactive effects resulting in respiratory depression, hypotension, profound sedation, or coma may result if these drugs are taken in combination with the usual dosage of Darvon-N. When such combined therapy is contemplated, the dose of one or both agents should be reduced.
Mixed Agonist/Antagonist Opioid AnalgesicsAgonist/antagonist analgesics (i.e., pentazocine, nalbuphine, butorphanol and buprenorphine) should be administered with caution to patients who have received or are receiving a course of therapy with a pure opioid agonist analgesic such as Darvon-N. In this situation, mixed agonist/antagonist analgesics may reduce the analgesic effect of Darvon-N and/or may precipitate withdrawal symptoms in these patients.
Monoamine Oxidase Inhibitors (MAOIs)MAOIs have been reported to intensify the effects of at least one opioid drug causing anxiety, confusion and significant depression of respiration or coma. The use of Darvon-N is not recommended for patients taking MAOIs or within 14 days of stopping such treatment.
Carcinogenesis, Mutagenesis, Impairment of FertilityThe mutagenic and carcinogenic potential of propoxyphene has not been evaluated.
In animal studies there was no effect of propoxyphene on mating behavior, fertility, duration of gestation, or parturition when rats were fed propoxyphene as a component of their daily diet at estimated daily propoxyphene intake up to 8-fold greater than the maximum human equivalent dose (HED) based on body surface area comparison. At this highest dose, fetal weight and survival on postnatal day 4 was reduced.
Pregnancy Risk summary Pregnancy category C.There are no adequate and well-controlled studies of propoxyphene in pregnant women. While there are limited data in the published literature, adequate animal reproduction studies have not been conducted with propoxyphene. Therefore, it is not known whether propoxyphene can affect reproduction or cause fetal harm when administered to a pregnant woman. Propoxyphene should be given to a pregnant woman only if clearly needed.
Clinical considerationsPropoxyphene and its major metabolite, norpropoxyphene, cross the human placenta. Neonates whose mothers have taken opiates chronically may exhibit respiratory depression or withdrawal symptoms.
DataIn published animal reproduction studies, no teratogenic effects occurred in offspring born to pregnant rats or rabbits that received propoxyphene during organogenesis. Pregnant animals received propoxyphene doses approximately 10-fold (rats) and 4-fold (rabbits) the maximum recommended human dose (based on mg/m2 body surface area comparison).
Nursing MothersPropoxyphene, norpropoxyphene (major metabolite), are excreted in human milk. Published studies of nursing mothers using propoxyphene detected no adverse effects in nursing infants. Based on a study of six mother-infant pairs, an exclusively breastfed infant receives approximately 2% of the maternal weight-adjusted dose. Norpropoxyphene is renally excreted and renal clearance is lower in neonates than in adults. Therefore, it is possible that prolonged maternal propoxyphene use could result in norpropoxyphene accumulation in a breastfed infant. Watch breastfeeding infants for signs of sedation including poor feeding, somnolence, or respiratory depression. Caution should be exercised when Darvon-N is administered to a nursing woman.
Pediatric PatientsSafety and effectiveness in pediatric patients have not been established.
Elderly PatientsClinical studies of Darvon-N did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. However, postmarketing reports suggest that patients over the age of 65 may be more susceptible to CNS-related side effects. Therefore, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy. Decreased total daily dosage should be considered (see Dosage and Administration).
-
ADVERSE REACTIONS
ADVERSE REACTIONS
In hospitalized patients, the most frequently reported were dizziness, sedation, nausea, and vomiting. Other adverse reactions include constipation, abdominal pain, skin rashes, lightheadedness, headache, weakness, euphoria, dysphoria, hallucinations, and minor visual disturbances.
The most frequently reported postmarketing adverse events have included completed suicide, accidental and intentional overdose, drug dependence, cardiac arrest, coma, drug ineffective, drug toxicity, nausea, respiratory arrest, cardio-respiratory arrest, death, vomiting, dizziness, convulsion, confusional state, and diarrhea.
Additional adverse experiences reported through postmarketing surveillance include:
Cardiac disorders: arrhythmia, bradycardia, cardiac/respiratory arrest, congestive arrest, congestive heart failure (CHF), tachycardia, myocardial infarction (MI)
Eye disorder: eye swelling, vision blurred
General disorder and administration site conditions: drug ineffective, drug interaction, drug tolerance, influenza type illness, drug withdrawal syndrome
Gastrointestinal disorder: gastrointestinal bleed, acute pancreatitis
Hepatobiliary disorder: hepatic steatosis, hepatomegaly, hepatocellular injury
Immune system disorder: hypersensitivity
Injury poisoning and procedural complications: drug toxicity, hip fracture, multiple drug overdose, narcotic overdose
Investigations: blood pressure decreased, heart rate elevated/abnormal
Metabolism and nutrition disorder: metabolic acidosis
Nervous system disorder: ataxia, coma, dizziness, somnolence, syncope
Psychiatric: abnormal behavior, confusional state, hallucinations, mental status change
Respiratory, thoracic, and mediastinal disorders: respiratory depression, dyspnoea
Skin and subcutaneous tissue disorder: rash, itch
Liver dysfunction has been reported in association with Darvon-N. Propoxyphene therapy has been associated with abnormal liver function tests and, more rarely, with instances of reversible jaundice (including cholestatic jaundice).
Subacute painful myopathy has been reported following chronic propoxyphene overdosage.
-
DRUG ABUSE AND DEPENDENCE
DRUG ABUSE AND DEPENDENCE Controlled Substance
Darvon-N is a Schedule IV narcotic under the U.S. Controlled Substances Act. Darvon-N can produce drug dependence of the morphine type, and therefore, has the potential for being abused. Psychic dependence, physical dependence and tolerance may develop upon repeated administration. Darvon-N should be prescribed and administered with the same degree of caution appropriate to the use of other narcotic-containing medications.
AbuseSince Darvon-N is a mu-opioid agonist, it may be subject to misuse, abuse, and addiction. Addiction to opioids prescribed for pain management has not been estimated. However, requests for opioids from opioid-addicted patients occur. As such, physicians should take appropriate care in prescribing Darvon-N.
DependenceOpioid analgesics may cause psychological and physical dependence. Physical dependence results in withdrawal symptoms in patients who abruptly discontinue the drug after long term administration. Also, symptoms of withdrawal may be precipitated through the administration of drugs with mu-opioid antagonist activity, e.g., naloxone or mixed agonist/antagonist analgesics (e.g., pentazocine, butorphanol, nalbuphine, dezocine) (see Overdosage). Physical dependence usually does not occur to a clinically significant degree, until after several weeks of continued opioid usage. Tolerance, in which increasingly larger doses are required to produce the same degree of analgesia, is initially manifested by a shortened duration of an analgesic effect and subsequently, by decreases in the intensity of analgesia.
In chronic pain patients, and in opioid-tolerant cancer patients, the administration of Darvon-N should be guided by the degree of tolerance manifested and the doses needed to adequately relieve pain.
The severity of the Darvon-N abstinence syndrome may depend on the degree of physical dependence. Withdrawal is characterized by rhinitis, myalgia, abdominal cramping, and occasional diarrhea. Most observable symptoms disappear in 5 to 14 days without treatment; however, there may be a phase of secondary or chronic abstinence which may last for 2 to 6 months characterized by insomnia, irritability, and muscular aches. The patient may be detoxified by gradual reduction of the dose. Gastrointestinal disturbances or dehydration should be treated with supportive care.
-
OVERDOSAGE
OVERDOSAGE
Overdose of Darvon-N may present with the signs and symptoms of propoxyphene overdose. Fatalities within the first hour of overdosage are not uncommon.
In all cases of suspected overdosage, call your regional Poison Control Center to obtain the most up-to-date information about the treatment of overdose. This recommendation is made because, in general, information regarding the treatment of overdosage may change more rapidly than do package inserts.
Initial consideration should be given to the management of the CNS effects of propoxyphene overdosage. Resuscitative measures should be initiated promptly.
Symptoms of Propoxyphene OverdosageThe manifestations of acute overdosage with propoxyphene are those of narcotic overdosage. The patient is usually somnolent but may be stuporous or comatose and convulsing. Respiratory depression is characteristic. The ventilatory rate and/or tidal volume is decreased, which results in cyanosis and hypoxia. Pupils, initially pinpoint, may become dilated as hypoxia increases. Cheyne-Stokes respiration and apnea may occur. Blood pressure and heart rate are usually normal initially, but blood pressure falls and cardiac performance deteriorates, which ultimately results in pulmonary edema and circulatory collapse, unless the respiratory depression is corrected and adequate ventilation is restored promptly. Cardiac arrhythmias and conduction delay may be present. A combined respiratory-metabolic acidosis occurs owing to retained CO2 (hypercapnia) and to lactic acid formed during anaerobic glycolysis. Acidosis may be severe if large amounts of salicylates have also been ingested. Death may occur.
Treatment of Propoxyphene OverdosageAttention should be directed first to establishing a patent airway and to restoring ventilation. Mechanically assisted ventilation, with or without oxygen, may be required, and positive pressure respiration may be desirable if pulmonary edema is present. The opioid antagonist naloxone will markedly reduce the degree of respiratory depression, and should be administered promptly, preferably intravenously. The duration of action of the antagonist may be brief. If no response is observed after 10 mg of naloxone have been administered, the diagnosis of propoxyphene toxicity should be questioned.
In addition to the use of an opioid antagonist, the patient may require careful titration with an anticonvulsant to control convulsions. Activated charcoal can adsorb a significant amount of ingested propoxyphene. Dialysis is of little value in poisoning due to propoxyphene. Efforts should be made to determine whether other agents, such as alcohol, barbiturates, tranquilizers, or other CNS depressants, were also ingested, since these increase CNS depression as well as cause specific toxic effects or death.
-
DOSAGE & ADMINISTRATION
DOSAGE AND ADMINISTRATION
Darvon-N is intended for the management of mild to moderate pain. The dose should be individually adjusted according to severity of pain, patient response and patient size.
Darvon-N is given orally. The usual dosage is one 100 mg propoxyphene napsylate tablet every 4 hours as needed for pain. The maximum dose of Darvon-N is 6 tablets per day. Do not exceed the maximum daily dose.
Patients receiving propoxyphene and any CYP3A4 inhibitor should be carefully monitored for an extended period of time and dosage adjustments should be made if warranted.
Consideration should be given to a reduced total daily dosage in elderly patients and in patients with hepatic or renal impairment.
Cessation of TherapyFor patients who used Darvon-N on a regular basis for a period of time, when therapy with Darvon-N is no longer needed for the treatment of their pain, it may be useful to gradually discontinue the Darvon-N over time to prevent the development of an opioid abstinence syndrome (narcotic withdrawal). In general, therapy can be decreased by 25% to 50% per day with careful monitoring for signs and symptoms of withdrawal (see Drug Abuse and Dependence for description of the signs and symptoms of withdrawal). If the patient develops these signs or symptoms, the dose should be raised to the previous level and titrated down more slowly, either by increasing the interval between decreases, decreasing the amount of change in dose, or both.
-
HOW SUPPLIED
HOW SUPPLIED
Darvon-N Tablets are available in:
The 100 mg tablets are buff colored, elliptical shaped, film coated, and imprinted with the script “DARVON-N 100” on one side of the tablet, using edible black ink. They are available as follows:
Bottles of 100 NDC: 66479-512-10 Store at 25°C (77°F); excursions are permitted to 15°- 30°C (59°- 86°F) [see USP Controlled Room Temperature].
Inform patients of the availability of a Medication Guide for Darvon/Darvon-N that accompanies each prescription dispensed. Instruct patients to read the Darvon/Darvon-N Medication Guide prior to using Darvon.
Darvon, Darvon-N, Darvocet, and Darvocet-N are registered trademarks of
Xanodyne Pharmaceuticals, Inc.
© 2009 Xanodyne Pharmaceuticals, Inc.
Marketed by:
Xanodyne Pharmaceuticals, Inc.
Newport, KY
41071PI-512-A
REV. 09-2009 -
MEDICATION GUIDE
MEDICATION GUIDE
DARVON-N® [dar-von-N] (C-IV)
(propoxyphene napsylate)
Tablets
DARVON® [dar-von](C-IV)
(propoxyphene hydrochloride capsules)
Puvules®
Read this Medication Guide before you start taking Darvon-N or Darvon, and each time you get a refill. There may be new information. This information does not take the place of talking to your doctor about your medical condition or your treatment.
What is the most important information I should know about Darvon-N and Darvon?
Darvon-N and Darvon, and other medicines that contain propoxyphene can cause serious side effects, including:
Overdoses by accident or on purpose (intentional overdose). Overdoses with Darvon-N and Darvon may happen when it is taken by itself, or with alcohol or other medicines that can also decrease your breathing and make you very sleepy.
-
Death can happen within 1 hour of taking an overdose of Darvon-N or Darvon.
Many of the deaths that happen in people who take Darvon-N and Darvon happen in those who:
- have emotional problems
- have thoughts of suicide or attempted suicide, or
- also take antidepressants, sedatives, tranquilizers, muscle relaxants, or other medicines that affect your breathing and make you very sleepy. You should not use any of these medicines with Darvon-N or Darvon without talking to your doctor.
-
Before taking Darvon-N or Darvon tell your doctor if
you:
- have a lung problem, such as COPD or cor pulmonale
- have liver or kidney problems
- have problems with your pancreas or gallbladder
- have a history of head injury
- are over age 65
- have a history of drug or alcohol abuse or addiction
Take Darvon-N and Darvon exactly as prescribed. Do not change your dose or stop taking Darvon-N or Darvon without first talking to your doctor.
- If you take Darvon-N, do not take more than 6 tablets in one day.
- If you take Darvon, do not take more than 6 capsules in one day.
- Before taking Darvon-N or Darvon, tell your doctor about all the medicines you take. Darvon-N or Darvon and many other medicines may interact with each other and may cause serious side effects. Certain medicines can affect how your liver breaks down other medicines. See “What should I tell my doctor before taking Darvon-N or Darvon?”
- Do not drink grapefruit juice or eat grapefruit while you take Darvon-N or Darvon. Grapefruit juice may interact with Darvon-N or Darvon.
- Do not drink alcohol while using Darvon-N or Darvon. Using alcohol with Darvon-N or Darvon may increase your risk of having dangerous side effects.
What are Darvon-N and Darvon?
- Darvon-N and Darvon are prescription medicines used to treat mild to moderate pain.
- Darvon-N and Darvon are federally controlled substances (C-IV) because they are strong opioid pain medicines that can be abused by people who abuse prescription medicines or street drugs.
- Prevent theft, misuse or abuse. Keep Darvon-N or Darvon in a safe place to protect it from being stolen. Darvon-N and Darvon can be a target for people who misuse or abuse prescription medicines or street drugs.
- Never give Darvon-N or Darvon to anyone else, even if they have the same symptoms that you have. It may harm them or even cause death. Selling or giving away this medicine is against the law.
It is not known if Darvon-N and Darvon are safe and effective in children younger than age 18.
Who should not take Darvon-N or Darvon?
Do not take Darvon-N or Darvon if you:
- are allergic to propoxyphene. Ask your doctor if you are not sure. See the end of this Medication Guide for a list of the ingredients in Darvon-N and Darvon.
- are having an asthma attack or have severe asthma, trouble breathing, or have a lung problem
- have a bowel blockage called paralytic ileus
What should I tell my doctor before taking Darvon-N or Darvon?
Before you take Darvon-N or Darvon, tell your doctor:
- if you have any of the conditions listed in the section “What is the most important information I should know about Darvon-N and Darvon?”
- if you are allergic to propoxyphene
- if you plan to have surgery with general anesthesia
- if you are pregnant or plan to become pregnant.
- if you take Darvon-N or Darvon regularly before your baby is born, your newborn baby may have withdrawal symptoms because their body has become used to the medicine. Symptoms of withdrawal in a newborn baby may include:
- irritability
- crying more than usual)
- shaking (tremors
- jitteriness
- breathing faster than normal
- diarrhea or more stools than normal
- vomiting
- fever
- if you take Darvon-N or Darvon right before your baby is born, your baby could have breathing problems.
- if you are breast-feeding or plan to breast-feed. Some Darvon-N or Darvon passes into breast milk.
Tell your doctor about all the medicines you take, including prescription, and non-prescription medicines, vitamins, and herbal supplements. Darvon-N and Darvon interacts with many medicines and may lead to serious side effects. The doses of certain medicines may need to be changed.
Especially tell your doctor if you take:
See “What is the most important information I should know about Darvon-N and Darvon?”
- certain medicines that can affect how your liver breaks down other medicines
- a monoamine oxidase inhibitor (MAOI) medicine
- other medicines that make you sleepy, such as: other medicines for pain, including other opioid medicines, anti-depressant medicines, sleeping pills, anti-anxiety medicines, muscle relaxants, anti-nausea medicines, or tranquilizers
- a blood pressure medicine
- a blood-thinner medicine. You may have an increased risk of bleeding while also taking Darvon-N or Darvon.
Ask your doctor or pharmacist if you are not sure if your medicine is one listed above.
Know the medicines you take. Keep a list of them to show to your doctor and pharmacist when you get a new medicine.
How should I take Darvon-N or Darvon?
See “What is the most important information I should know about Darvon-N and Darvon?”
- Take Darvon-N or Darvon exactly as prescribed.
- If you take too much Darvon-N or Darvon, or take it with alcohol or other medicines, you may overdose. See “What is the most important information I should know about Darvon-N or Darvon?” You will need medical help right away if you think you have taken an overdose of Darvon-N or Darvon. A large overdose could cause you to become unconscious and die.
Signs and symptoms of an overdose of Darvon-N or Darvon include:
- you are very sleepy or do not respond to others
- confusion
- have trouble breathing or stop breathing
- changes in blood pressure and heart rate
What are the possible side effects of Darvon-N and Darvon?
Darvon-N and Darvon can cause serious side effects, including:
See “What is the most important information I should know about Darvon-N and Darvon?”
-
Serious breathing problems that can become
life-threatening. This is especially true if you already have a serious
lung or breathing problem, or your body is not used to opioid pain medicines.
This can happen even if you take Darvon-N or Darvon exactly as prescribed by
your doctor. Call your doctor or get medical help right away if:
- your breathing slows down
- you have shallow breathing (little chest movement with breathing)
- you feel faint, dizzy, confused, or
- you have any other unusual symptoms
- Darvon-N and Darvon can cause your blood pressure to drop. This can make you feel dizzy and faint if you get up too fast from sitting or lying down. Low blood pressure is also more likely to happen if you take other medicines that can also lower your blood pressure. Severe low blood pressure can happen if you lose blood or take certain other medicines.
- Sleepiness. Darvon-N and Darvon can cause sleepiness and may affect your ability to make decisions, think clearly, or react quickly. Do not drive, operate heavy machinery, or do other dangerous activities until you know how Darvon-N or Darvon affects you.
- Darvon-N and Darvon can cause physical dependence if you take it for more than a few weeks. Do not stop taking Darvon-N or Darvon all of a sudden. You could become sick with uncomfortable withdrawal symptoms (for example, nausea, vomiting, diarrhea, anxiety, and shivering) because your body has become used to the medicine. Physical dependence is not the same as drug addiction. Your doctor can tell you more about the differences between physical dependence and drug addiction.
Tell your doctor if you have any of these withdrawal symptoms while you slowly stop taking Darvon-N or Darvon. You may need to stop Darvon-N or Darvon more slowly.
Common side effects of Darvon-N and Darvon include:
- dizziness
- feeling sleepy
- nausea and vomiting
- constipation
- stomach area (abdominal) pain
- skin rashes
- lightheadedness
- headache
- weakness
- feeling of excitement (elation) or discomfort
- seeing, hearing, or sensing things that are not really there (hallucinations)
- blurred vision
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
You may also report side effects to Xanodyne Pharmaceuticals, Inc. at 1-877-773-7793.
How should I store Darvon-N and Darvon?
- Store Darvon-N between 59°F to 86°F (15°C to 30°C).
- Store Darvon between 68°F to 77°F (20°C to 25°C).
Keep Darvon-N, Darvon and all medicines out of the reach of children.
General information about Darvon-N and Darvon
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use Darvon-N or Darvon for a purpose for which it was not prescribed. Do not give Darvon-N or Darvon to others even if they have the same symptoms you have. It may harm them and is against the law.
This Medication Guide summarizes the most important information about Darvon-N and Darvon. If you would like more information, talk with your doctor. You can ask your pharmacist or doctor for information about Darvon-N and Darvon that is written for health professionals. For more information, go to www.Xanodyne.com or call 1-877-773-7793.
What are the ingredients in Darvon-N and Darvon?
Darvon-N:
Active ingredient: propoxyphene napsylate
Inactive ingredients: cellulose, cornstarch, iron oxides, lactose, magnesium stearate, silicon dioxide, stearic acid, and titanium dioxide
Darvon:
Active ingredient: propoxyphene hydrochloride
Inactive ingredients: D and C Red No. 33, FD and C Yellow No. 6, gelatin, magnesium stearate, silicone, starch, titanium dioxide, and other inactive ingredients
Xanodyne Pharmaceuticals, Inc.
Newport, KY 41071Issued 09/2009
This Medication Guide has been approved by the U.S. Food and Drug Administration.
Darvon, Darvon-N, Darvocet-N and Darvocet are registered trademarks of Xanodyne Pharmaceuticals, Inc.
© 2009 Xanodyne Pharmaceuticals, Inc.
Marketed by:
Xanodyne Pharmaceuticals, Inc.
MG-510/512-A
Revised: 09/2009Xanodyne Pharmaceuticals, Inc.
Rev. 09/2009 -
- PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
DARVON-N
propoxyphene napsylate tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 16590-874(NDC: 66479-512) Route of Administration ORAL DEA Schedule CIV Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength propoxyphene napsylate (UNII: 38M219L1OJ) (propoxyphene - UNII:S2F83W92TK) propoxyphene napsylate 100 mg Product Characteristics Color yellow Score no score Shape OVAL Size 14mm Flavor Imprint Code DARVON;N;100 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 16590-874-30 30 in 1 BOTTLE 2 NDC: 16590-874-60 60 in 1 BOTTLE 3 NDC: 16590-874-90 90 in 1 BOTTLE Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA016862 09/25/2009 Labeler - Stat Rx USA (786036330)
Trademark Results [Darvon-N]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 DARVON-N 72403637 0952573 Dead/Cancelled |
ELI LILLY AND COMPANY 1971-09-27 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.