REBIF- interferon beta-1a kit REBIF REBIDOSE- interferon beta-1a kit REBIF- interferon beta-1a injection, solution REBIF- interferon beta-1a injection, solution REBIF REBIDOSE- interferon beta-1a injection, solution
REBIF REBIDOSE by
Drug Labeling and Warnings
REBIF REBIDOSE by is a Prescription medication manufactured, distributed, or labeled by EMD Serono, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use REBIF safely and effectively. See full prescribing information for REBIF.
REBIF (interferon beta-1a), for subcutaneous injection
Initial U.S. Approval: 1996RECENT MAJOR CHANGES
Indications and Usage (1) 07/2019 INDICATIONS AND USAGE
Rebif is an interferon beta indicated for the treatment of relapsing forms of multiple sclerosis (MS), to include clinically isolated syndrome, relapsing-remitting disease, and active secondary progressive disease, in adults. (1)
DOSAGE AND ADMINISTRATION
- For subcutaneous injection only (2.1)
- The recommended dose is either 22 mcg or 44 mcg injected subcutaneously three times per week (2.1)
- Titration: Generally, the starting dose should be 20% of the prescribed dose three times per week, and increased over a 4 week period to the targeted recommended dose of either 22 mcg or 44 mcg injected subcutaneously three times per week (2.1)
- Analgesics and/or antipyretics on treatment days may help ameliorate flu-like symptoms (2.3)
DOSAGE FORMS AND STRENGTHS
CONTRAINDICATIONS
- History of hypersensitivity to natural or recombinant interferon beta, human albumin, or any other component of the formulation (4)
WARNINGS AND PRECAUTIONS
- Depression and Suicide: Advise patients to immediately report any symptoms of depression and/or suicidal ideation; consider discontinuation of REBIF if depression occurs (5.1)
- Hepatic injury: Monitor liver function tests; monitor patients for signs and symptoms of hepatic injury; consider discontinuing REBIF if hepatic injury occurs (5.2)
- Anaphylaxis and Other Allergic Reactions: Discontinue REBIF if anaphylaxis occurs (5.3)
- Injection Site Reactions including Necrosis: Do not administer REBIF into affected area until fully healed; if multiple lesions occur, discontinue REBIF until healing of skin lesions (5.4)
- Decreased Peripheral Blood Counts: Monitor complete blood counts (5.5)
- Thrombotic Microangiopathy: Cases of thrombotic microangiopathy have been reported. Discontinue REBIF if clinical symptoms and laboratory findings consistent with TMA occur (5.6).
- Seizures: Monitor for seizures when administering REBIF to patients, particularly those with pre-existing seizure disorders (5.7)
ADVERSE REACTIONS
The most common adverse reactions in controlled clinical trials were injection site disorders, influenza-like symptoms, abdominal pain, depression, elevation of liver enzymes and hematologic abnormalities (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact EMD Serono at 1-800-283-8088 ext. 5563 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 7/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Dosing Information
2.2 Important Administration Instructions
2.3 Premedication for Flu-like Symptoms
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Depression and Suicide
5.2 Hepatic Injury
5.3 Anaphylaxis and Other Allergic Reactions
5.4 Injection Site Reactions including Necrosis
5.5 Decreased Peripheral Blood Counts
5.6 Thrombotic Microangiopathy
5.7 Seizures
5.8 Laboratory Tests
6 ADVERSE REACTIONS
6.1 Clinical Trial Experience
6.2 Immunogenicity
6.3 Postmarketing Experience
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 Dosing Information
The recommended dose of REBIF is either 22 mcg or 44 mcg injected subcutaneously three times per week. REBIF should be administered, if possible, at the same time (preferably in the late afternoon or evening) on the same three days (e.g., Monday, Wednesday, and Friday) at least 48 hours apart each week.
Generally, patients should be started at 20% of the prescribed dose three times per week and increased over a 4-week period to the targeted dose, either 22 mcg three times per week (see Table 1) or 44 mcg three times per week (see Table 2). Patients prescribed a targeted dose of 22 mcg three times per week should use the prefilled syringes for titration.
A Titration Pack containing 6 doses of 8.8 mcg (0.2 mL) and 6 doses of 22 mcg (0.5 mL) is available for use during the titration period in both REBIF prefilled syringes and REBIF Rebidose autoinjectors.
Table 1: Titration Schedule for a 22 mcg Prescribed Dose* Week of Use Dose Syringe to Use Amount of syringe - * Use only prefilled syringes, not autoinjectors, to titrate to the 22 mcg Prescribed Dose
Week 1 Titration 4.4 mcg 8.8 mcg syringe Use half of syringe Week 2 Titration 4.4 mcg 8.8 mcg syringe Use half of syringe Week 3 Titration 11 mcg 22 mcg syringe Use half of syringe Week 4 Titration 11 mcg 22 mcg syringe Use half of syringe Week 5 and after 22 mcg 22 mcg syringe or autoinjector Use full syringe or autoinjector Table 2: Titration Schedule for a 44 mcg Prescribed Dose* Week of Use Dose Syringe or Autoinjector to Use Amount of syringe or autoinjector - * Prefilled syringes or autoinjectors can be used to titrate to the 44 mcg Prescribed Dose
Week 1 Titration 8.8 mcg 8.8 mcg syringe or autoinjector Use full syringe or autoinjector Week 2 Titration 8.8 mcg 8.8 mcg syringe or autoinjector Use full syringe or autoinjector Week 3 Titration 22 mcg 22 mcg syringe or autoinjector Use full syringe or autoinjector Week 4 Titration 22 mcg 22 mcg syringe or autoinjector Use full syringe or autoinjector Week 5 and after 44 mcg 44 mcg syringe or autoinjector Use full syringe or autoinjector Decreased peripheral blood counts or elevated liver function tests may necessitate dose reduction or discontinuation of REBIF administration until toxicity is resolved [see Warnings and Precautions (5.2, 5.5) and Adverse Reactions (6)].
2.2 Important Administration Instructions
REBIF is intended for use under the guidance and supervision of a physician. It is recommended that physicians or qualified medical personnel train patients in the proper technique for self-administering subcutaneous injections using the prefilled syringe or injection device approved for use with REBIF. Injection depth of the REBIF Rebidose autoinjector is fixed at 8 mm; the health care provider should determine the injection technique.
The initial injection should be performed under the supervision of an appropriately qualified health care provider.
Appropriate instruction for self-injection or injection by another person should be provided to the patient or their caregiver, including careful review of the REBIF Medication Guide and the REBIF Rebidose autoinjector Instructions for Use that accompanies the product. Users should demonstrate competency in all aspects of the injection prior to independent use. If a patient is to self-administer REBIF, the physical and cognitive ability of that patient to self-administer and properly dispose of prefilled syringes or the REBIF Rebidose autoinjectors should be assessed. Patients with severe neurological deficits should not self-administer injections without assistance from a trained caregiver.
Advise patients and caregivers to:
- visually inspect REBIF for particulate matter and discoloration prior to administration
- use aseptic technique when administering REBIF
- rotate site of injection with each dose to minimize the likelihood of severe injection site reactions or necrosis [see Warnings and Precautions, (5.4)]
- use a puncture-resistant container for safe disposal of used needles, prefilled syringes and REBIF Rebidose autoinjectors
- do not re-use needles, syringes or REBIF Rebidose autoinjectors
-
3 DOSAGE FORMS AND STRENGTHS
- Injection: 8.8 mcg per 0.2 mL in a graduated, single-dose REBIF prefilled syringe
- Injection: 22 mcg per 0.5 mL in a graduated, single-dose REBIF prefilled syringe
- Injection: 44 mcg per 0.5 mL in a graduated, single-dose REBIF prefilled syringe
- Injection: 8.8 mcg per 0.2 mL in a single-dose prefilled REBIF Rebidose autoinjector
- Injection: 22 mcg per 0.5 mL in a single-dose prefilled REBIF Rebidose autoinjector
- Injection: 44 mcg per 0.5 mL in a single-dose prefilled REBIF Rebidose autoinjector
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Depression and Suicide
REBIF (interferon beta-1a) should be used with caution in patients with depression, a condition that is common in people with multiple sclerosis. Depression, suicidal ideation, and suicide attempts have been reported to occur with increased frequency in patients receiving interferon compounds, including REBIF. In addition, there have been postmarketing reports of suicide in patients treated with REBIF. Patients should be advised to report immediately any symptoms of depression and/or suicidal ideation to the prescribing physician. If a patient develops depression, cessation of treatment with REBIF should be considered.
5.2 Hepatic Injury
Severe liver injury, including some cases of hepatic failure requiring liver transplantation, has been reported rarely in patients taking REBIF. Symptoms of liver dysfunction began from one to six months following the initiation of REBIF. If jaundice or other symptoms of liver dysfunction appear, treatment with REBIF should be discontinued immediately due to the potential for rapid progression to liver failure.
Asymptomatic elevation of hepatic transaminases (particularly SGPT) is common with interferon therapy [see Adverse Reactions (6.1)]. REBIF should be initiated with caution in patients with active liver disease, alcohol abuse, increased serum SGPT (> 2.5 times ULN), or a history of significant liver disease. Also, the potential risk of REBIF used in combination with known hepatotoxic products should be considered prior to REBIF administration, or when adding new agents to the regimen of patients already on REBIF. Reduction of REBIF dose should be considered if SGPT rises above 5 times the upper limit of normal. The dose may be gradually re-escalated when enzyme levels have normalized [see Warnings and Precautions (5.8); and Dosage and Administration (2.1)].
5.3 Anaphylaxis and Other Allergic Reactions
Anaphylaxis has been reported as a rare complication of REBIF use. Other allergic reactions have included skin rash and urticaria, and have ranged from mild to severe without a clear relationship to dose or duration of exposure. Several allergic reactions, some severe, have occurred after prolonged use. Discontinue REBIF if anaphylaxis occurs.
5.4 Injection Site Reactions including Necrosis
In controlled clinical trials, injection site reactions occurred more frequently in REBIF-treated patients (92% in the 44 mcg group and 89% in the 22 mcg group) than in placebo-treated patients (39%) and at a higher frequency in REBIF treated patients (83%) than in AVONEX-treated patients (28%). Injection site necrosis also occurred more frequently in REBIF-treated patients (3% in the 44 mcg group and 1% in the 22 mcg group) than in placebo-treated patients (0) during the two years of therapy. All events resolved with conservative management.
Injection site reactions including injection site pain, erythema, edema, cellulitis, abscess, and necrosis have been reported in the postmarketing setting. Some occurred more than 2 years after initiation of REBIF. Necrosis occurred at single and at multiple injection sites. Some cases of injection site necrosis required treatment with intravenous antibiotics and surgical intervention (debridement and skin grafting).
Patient understanding and use of aseptic self-injection techniques and procedures should be periodically evaluated, particularly if injection site necrosis has occurred. Patients should be advised of the importance of rotating sites of injection with each dose and not reusing syringes. Patients should be advised against injecting an area which is inflamed, edematous, erythematous, ecchymotic, or has any other signs of infection. These signs should be reported to a healthcare professional immediately.
5.5 Decreased Peripheral Blood Counts
Decreased peripheral blood counts in all cell lines, including pancytopenia, have been reported in REBIF-treated patients. In controlled clinical trials, leukopenia occurred at a higher frequency in REBIF-treated patients (36% in 44 mcg group and 28% in 22 mcg group) than in placebo-treated patients (14%) and at a higher frequency in REBIF-treated patients (6%) compared to the AVONEX-treated patients (<1%). Thrombocytopenia and anemia occurred more frequently in 44 mcg REBIF-treated patients (8% and 5%, respectively) than in placebo-treated patients (2% and 3%, respectively). In a pooled analysis of 7 placebo controlled trials with REBIF doses of 22 mcg or 44 mcg, the rate of pancytopenia (in subjects with normal baseline values who developed laboratory values less than the lower limit of normal for all 3 hematology parameters simultaneously) was higher in the total REBIF group (5.5 per 1000 subject-year) than in the placebo group (1.2 per 1000 subject-year). Patients should be monitored for symptoms or signs of decreased blood counts. Monitoring of complete blood and differential white blood cell counts is also recommended [see Dosage and Administration (2.1) and Warnings and Precautions (5.8)].
5.6 Thrombotic Microangiopathy
Cases of thrombotic microangiopathy (TMA), including thrombotic thrombocytopenic purpura and hemolytic uremic syndrome, some fatal, have been reported with interferon beta products, including REBIF. Cases have been reported several weeks to years after starting interferon beta products. Discontinue REBIF if clinical symptoms and laboratory findings consistent with TMA occur, and manage as clinically indicated.
5.7 Seizures
Caution should be exercised when administering REBIF to patients with pre-existing seizure disorders. Seizures have been temporally associated with the use of beta interferons, including REBIF, in clinical trials and in postmarketing reports.
5.8 Laboratory Tests
In addition to those laboratory tests normally required for monitoring patients with multiple sclerosis, blood cell counts and liver function tests are recommended at regular intervals (1, 3, and 6 months) following introduction of REBIF therapy and then periodically thereafter in the absence of clinical symptoms. Patients with myelosuppression may require more intensive monitoring of complete blood cell counts, with differential and platelet counts [see Dosage and Administration (2.1) and Warnings and Precautions (5.5)]. New or worsening thyroid abnormalities have developed in some patients treated with REBIF. Thyroid function tests are recommended every 6 months in patients with a history of thyroid dysfunction or as clinically indicated.
-
6 ADVERSE REACTIONS
The following adverse reactions are discussed in more detail in the Warnings and Precautions section of the label:
- Depression and Suicide [see Warnings and Precautions (5.1)]
- Hepatic Injury [see Warnings and Precautions (5.2)]
- Anaphylaxis and Other Allergic Reactions [see Warnings and Precautions (5.3)]
- Injection Site Reactions including Necrosis [see Warnings and Precautions (5.4)]
- Decreased Peripheral Blood Counts [see Warnings and Precautions (5.5)]
- Thrombotic Microangiopathy [see Warnings and Precautions (5.6) ]
- Seizures [see Warnings and Precautions (5.7)]
- Laboratory Tests [see Warnings and Precautions (5.8)]
6.1 Clinical Trial Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of REBIF cannot be directly compared to rates in the clinical trials of other drugs and may not reflect the rates observed in practice.
A total of 712 patients with relapsing-remitting multiple sclerosis (RRMS) in two controlled clinical trials took REBIF (22 mcg or 44 mcg given three times per week) [see Clinical Studies (14)]. Ages ranged from 18 to 55 years. Nearly three-fourths of the patients were female, and more than 90% were Caucasian, largely reflecting the general demographics of the population of patients with multiple sclerosis.
The most commonly reported adverse reactions were injection site disorders, influenza-like symptoms (headache, fatigue, fever, rigors, chest pain, back pain, myalgia), abdominal pain, depression, elevation of liver enzymes and hematologic abnormalities. The most frequently reported adverse reactions resulting in clinical intervention (e.g., discontinuation of REBIF, adjustment in dosage, or the need for concomitant medication to treat an adverse reaction were injection site disorders, influenza-like symptoms, depression, and elevation of liver enzymes [see Warnings and Precautions (5)].
Study 1 was a 2-year placebo-controlled study in RRMS patients treated with REBIF 22 mcg (n=189), 44 mcg (n=184), or placebo (n=187). Table 3 enumerates adverse reactions and laboratory abnormalities that occurred at an incidence that was at least 2% more in either REBIF-treated group than was observed in the placebo group.
Table 3. Adverse Reactions and Laboratory Abnormalities in Study 1 Body System Placebo tiw
(n=187)REBIF 22 mcg tiw
(n=189)REBIF 44 mcg tiw
(n=184)Preferred Term % % % BODY AS A WHOLE Influenza-like symptoms 51 56 59 Headache 63 65 70 Fatigue 36 33 41 Fever 16 25 28 Rigors 5 6 13 Chest pain 5 6 8 Malaise 1 4 5 INJECTION SITE DISORDERS Injection Site Reaction 39 89 92 Injection Site Necrosis 0 1 3 NERVOUS SYSTEM DISORDERS Hypertonia 5 7 6 Coordination Abnormal 2 5 4 Convulsions 2 5 4 Somnolence 1 4 5 ENDOCRINE DISORDERS Thyroid Disorder 3 4 6 GASTROINTESTINAL SYSTEM DISORDERS Abdominal Pain 17 22 20 Dry Mouth 1 1 5 LIVER AND BILIARY SYSTEM DISORDERS SGPT Increased 4 20 27 SGOT Increased 4 10 17 Bilirubinemia 1 3 2 MUSCULO-SKELETAL SYSTEM DISORDERS Myalgia 20 25 25 Back Pain 20 23 25 Skeletal Pain 10 15 10 HEMATOLOGIC DISORDERS Leukopenia 14 28 36 Lymphadenopathy 8 11 12 Thrombocytopenia 2 2 8 Anemia 3 3 5 SKIN DISORDERS Rash Erythematous 3 7 5 Rash Maculo-Papular 2 5 4 Hyperhidrosis 2 4 4 URINARY SYSTEM DISORDERS Micturition Frequency 4 2 7 Urinary Incontinence 2 4 2 VISION DISORDERS Vision Abnormal 7 7 13 Xerophthalmia 0 3 1 Adverse reactions in Study 2, a 1-year active-controlled (vs. interferon beta-1a, 30 mcg once weekly intramuscular injection, n=338) study including 339 patients with MS treated with REBIF were generally similar to those in Study 1, taking into account the disparity in study durations.
6.2 Immunogenicity
Anaphylaxis and other allergic reactions have been observed with the use of REBIF [see Warnings and Precautions (5.3)]. As with all therapeutic proteins, there is a potential for immunogenicity. In Study 1, the presence of neutralizing antibodies (NAb) to REBIF was determined by collecting and analyzing serum pre-study and at 6 month time intervals during the 2 years of the clinical trial. Serum NAb were detected in 59/189 (31%) and 45/184 (24%) of REBIF-treated patients at the 22 mcg and 44 mcg three times per week doses, respectively, at one or more times during the study. The data reflect the percentage of patients whose test results were considered positive for antibodies to REBIF using an antiviral cytopathic effect assay, and are highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of NAb positivity in an assay may be influenced by several factors including sample handling, timing of sample collection, concomitant medications and underlying disease. For these reasons, comparison of the incidence of antibodies to REBIF with the incidence of antibodies to other products may be misleading.
6.3 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of REBIF. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Autoimmune Disorders: Drug-induced lupus erythematosus, autoimmune hepatitis
Eye Disorders: Retinal vascular disorders (i.e. retinopathy, cotton wool spots or obstruction of retinal artery or vein)
Skin and Subcutaneous Tissue Disorders: Erythema multiforme, Stevens-Johnson syndrome
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category C
There are no adequate and well-controlled studies in pregnant women. REBIF should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
In a study in pregnant cynomolgus monkeys, interferon beta was administered daily (intramuscular doses approximately 1, 2, and 7 times the maximum recommended cumulative weekly human dose, based on body surface area) either throughout the period of organogenesis or later in pregnancy (gestation day 90 to term). No adverse effects on embryofetal development were observed; however, the possibility of adverse effects cannot be ruled out because of the small number of animals tested (six per dose group at each developmental period).
8.3 Nursing Mothers
It is not known whether REBIF is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when REBIF is administered to a nursing woman.
8.5 Geriatric Use
Clinical studies of REBIF did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently than younger subjects. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal or cardiac function, and of concomitant disease or other drug therapy.
-
11 DESCRIPTION
REBIF (interferon beta-1a) is a purified 166 amino acid glycoprotein with a molecular weight of approximately 22,500 daltons. It is produced by recombinant DNA technology using genetically engineered Chinese Hamster Ovary cells into which the human interferon beta gene has been introduced. The amino acid sequence of REBIF is identical to that of natural fibroblast derived human interferon beta. Natural interferon beta and interferon beta-1a (REBIF) are glycosylated with each containing a single N-linked complex carbohydrate moiety.
Using a reference standard calibrated against the World Health Organization natural interferon beta standard (Second International Standard for Interferon, Human Fibroblast GB 23 902 531), REBIF has a specific activity of approximately 270 million international units (MIU) of antiviral activity per mg of interferon beta-1a determined specifically by an in vitro cytopathic effect bioassay using WISH cells and Vesicular Stomatitis virus. REBIF 8.8 mcg, 22 mcg and 44 mcg contains approximately 2.4 million international units, 6 million international units or 12 million international units, respectively, of antiviral activity using this method.
REBIF (interferon beta-1a) is formulated as a sterile solution in a prefilled syringe or REBIF Rebidose autoinjector intended for subcutaneous (sc) injection. Each 0.5 mL (0.5 cc) of REBIF contains either 22 mcg or 44 mcg of interferon beta-1a, 2 mg or 4 mg albumin (human), 27.3 mg mannitol, 0.4 mg sodium acetate, and water for injection. Each 0.2 mL (0.2 cc) of REBIF contains 8.8 mcg of interferon beta-1a, 0.8 mg albumin (human), 10.9 mg mannitol, 0.16 mg sodium acetate, and water for injection.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The mechanism(s) by which REBIF (interferon beta-1a) exerts its therapeutic effects in patients with multiple sclerosis is unknown.
12.2 Pharmacodynamics
The relationships between serum interferon beta-1a levels and measurable pharmacodynamic activities to the mechanism(s) by which REBIF exerts its effects in multiple sclerosis are unknown. No gender-related effects on pharmacodynamic parameters have been observed.
12.3 Pharmacokinetics
The pharmacokinetics of REBIF (interferon beta-1a) in people with multiple sclerosis have not been evaluated. In healthy subjects, a single subcutaneous (sc) injection of 60 mcg of REBIF (liquid formulation) resulted in a peak serum concentration (Cmax) of 5.1 ± 1.7 IU/mL (mean ± SD), with a median time of peak serum concentration (Tmax) of 16 hours. The serum elimination half-life (t1/2) was 69 ± 37 hours, and the area under the serum concentration versus time curve (AUC) from zero to 96 hours was 294 ± 81 IU h/mL. Following every other day sc injections in healthy subjects, an increase in AUC of approximately 240% was observed, suggesting that accumulation of interferon beta-1a occurs after repeat administration. Total clearance is approximately 33-55 L/hour. There have been no observed gender-related effects on pharmacokinetic parameters. Pharmacokinetics of REBIF in pediatric and geriatric patients or patients with renal or hepatic insufficiency have not been established.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Mutagenesis: Interferon beta was negative in an in vitro bacterial reverse mutation (Ames) assay and an in vitro cytogenetic assay in human lymphocytes in the presence and absence of metabolic activation.
Impairment of Fertility: In studies in normally cycling female cynomolgus monkeys given daily subcutaneous injections of interferon beta for six months at doses of up to 9 times the recommended weekly human dose (based on body surface area), no effects were observed on either menstrual cycling or serum estradiol levels. In male monkeys, the same doses of interferon beta had no demonstrable adverse effects on sperm count, motility, morphology, or function.
-
14 CLINICAL STUDIES
Two multicenter studies evaluated the safety and efficacy of REBIF in patients with relapsing-remitting multiple sclerosis.
Study 1 was a randomized, double-blind, placebo controlled study in patients with multiple sclerosis for at least one year, Kurtzke Expanded Disability Status Scale (EDSS) scores ranging from 0 to 5, and at least 2 acute exacerbations in the previous 2 years. Patients with chronic progressive forms of multiple sclerosis were excluded from the study. Patients received subcutaneous injections of either placebo (n = 187), REBIF 22 mcg (n = 189), or REBIF 44 mcg (n = 184) administered three times per week for two years. Doses of study agents were progressively increased to their target doses during the first 4 to 8 weeks for each patient in the study [see Dosage and Administration (2.1)].
The primary efficacy endpoint was the number of clinical exacerbations. Numerous secondary efficacy endpoints were also evaluated and included exacerbation-related parameters, effects of treatment on progression of disability and magnetic resonance imaging (MRI)-related parameters. Progression of disability was defined as an increase in the EDSS score of at least one point sustained for at least 3 months. Neurological examinations were completed every 3 months, during suspected exacerbations, and coincident with MRI scans. All patients underwent proton density T2-weighted (PD/T2) MRI scans at baseline and every 6 months. A subset of 198 patients underwent PD/T2 and T1-weighted gadolinium-enhanced (Gd)-MRI scans monthly for the first 9 months. Of the 560 patients enrolled, 533 (95%) provided 2 years of data and 502 (90%) received 2 years of study agent.
Study results are shown in Table 4 and Figure 1. REBIF at doses of 22 mcg and 44 mcg administered three times per week significantly reduced the number of exacerbations per patient as compared to placebo. Differences between the 22 mcg and 44 mcg groups were not significant (p >0.05).
Table 4: Clinical and MRI Endpoints from Study 1 - * Intent-to-treat analysis
- † Poisson regression model adjusted for center and time on study
- ‡ p<0.001 compared to placebo
- § p<0.0001 compared to placebo
- ¶ Logistic regression adjusted for center. Patients lost to follow-up prior to an exacerbation were excluded from this analysis. (Analysis included 185, 183, and 184 patients for three times per week placebo, 22 mcg REBIF, and 44 mcg REBIF, respectively).
- # p<0.05 compared to placebo
- Þ Cox proportional hazard model adjusted for center
- ß ANOVA on ranks adjusted for center. Patients with missing scans were excluded from this analysis.
Placebo REBIF 22 mcg REBIF
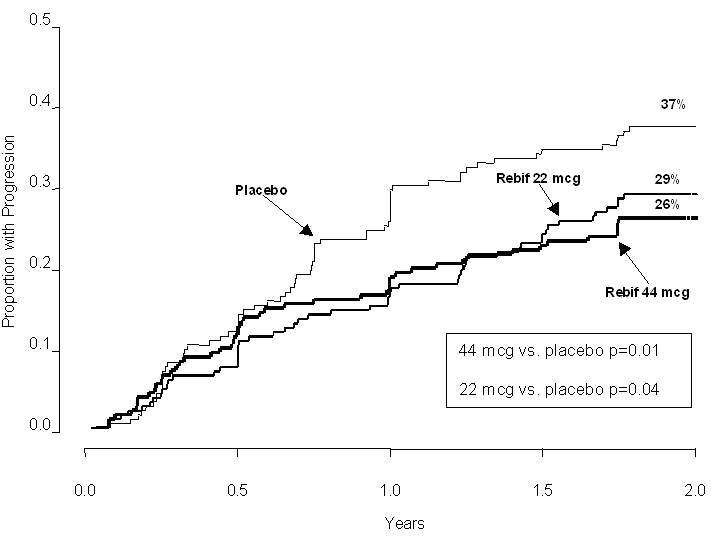
44 mcgn = 187 n = 189 n = 184 Exacerbation-related Mean number of exacerbations per patient over 2 years*,† 2.56 1.82‡ 1.73§ (Percent reduction) (29%) (32%) Percent (%) of patients exacerbation-free at 2 years¶ 15% 25%# 32%§ Median time to first exacerbation (months)*,Þ 4.5 7.6‡ 9.6§ MRI n = 172 n = 171 n = 171 Median percent (%) change of MRI PD-T2 lesion area at 2 yearsß 11.0% -1.2%§ -3.8%§ Median number of active lesions per patient per scan (PD/T2; 6 monthly)ß 2.25 0.75§ 0.5§ The time to onset of progression in disability sustained for three months was significantly longer in patients treated with REBIF than in placebo-treated patients. The Kaplan-Meier estimates of the proportions of patients with sustained disability are depicted in Figure 1.
Figure 1: Proportions of Patients with Sustained Disability Progression
Study 2 was a randomized, open-label, evaluator-blinded, active comparator study. Patients with relapsing-remitting multiple sclerosis with EDSS scores ranging from 0 to 5.5, and at least 2 exacerbations in the previous 2 years were eligible for inclusion. Patients with chronic progressive forms of multiple sclerosis were excluded from the study. Patients were randomized to treatment with three times per week subcutaneous injections of REBIF 44 mcg (n=339) or once weekly intramuscular injections of 30 mcg AVONEX (n=338). Study duration was 48 weeks.
The primary efficacy endpoint was the proportion of patients who remained exacerbation-free at 24 weeks. The principal secondary endpoint was the mean number per patient per scan of combined unique active MRI lesions through 24 weeks, defined as any lesion that was T1 active or T2 active. Neurological examinations were performed every three months by a neurologist blinded to treatment assignment. Patient visits were conducted monthly, and mid-month telephone contacts were made to inquire about potential exacerbations. If an exacerbation was suspected, the patient was evaluated with a neurological examination. MRI scans were performed monthly and analyzed in a treatment-blinded manner.
Patients treated with REBIF 44 mcg three times per week were more likely to remain relapse-free at 24 and 48 weeks than were patients treated with AVONEX 30 mcg once per week (Table 5). This study does not support any conclusion regarding effects on the accumulation of physical disability.
Table 5: Clinical and MRI Results from Study 2 REBIF
44 mcgAVONEX
30 mcgAbsolute Difference Risk of relapse on REBIF relative to AVONEX - * Logistic regression model adjusted for treatment and center, intent to treat analysis
- † p <0.001 (REBIF compared to AVONEX)
- ‡ p = 0.009 (REBIF compared to AVONEX)
- § Nonparametric ANCOVA model adjusted for treatment and center, with baseline combined unique lesions as the single covariate
Relapses N=339 N=338 Proportion of patients relapse-free at 24 weeks* 75%† 63% 12%
(95% CI: 5%, 19%)0.68
(95% CI: 0.54, 0.86)Proportion of patients relapse-free at 48 weeks 62%‡ 52% 10%
(95% CI: 2%, 17%)0.81
(95% CI: 0.68, 0.96)MRI (through 24 weeks)
Median of the mean number of combined unique MRI lesions per patient per scan§ (25th, 75th percentiles)N=325
0.17†
(0.00, 0.67)N=325
0.33
(0.00, 1.25) -
16 HOW SUPPLIED/STORAGE AND HANDLING
REBIF is supplied as a sterile solution containing no preservative available in the following package presentations:
Prefilled Syringes:
-
REBIF (interferon beta -1a) Titration Pack, NDC: 44087-8822-1
- - Six REBIF 8.8 mcg prefilled syringes and Six REBIF 22 mcg prefilled syringes
-
REBIF (interferon beta -1a) 22 mcg Prefilled syringe
- - Twelve REBIF 22 mcg prefilled syringes, NDC: 44087-0022-3
-
REBIF (interferon beta -1a) 44 mcg Prefilled syringe
- - Twelve REBIF 44 mcg prefilled syringes, NDC: 44087-0044-3
REBIF Rebidose Autoinjectors:
-
REBIF Rebidose (interferon beta-1a) Titration Pack, NDC: 44087-0188-1
- - Six REBIF Rebidose 8.8 mcg autoinjectors with lime-green injector buttons and Six REBIF Rebidose 22 mcg with yellow injector buttons.
-
REBIF Rebidose (interferon beta-1a) 22 mcg Autoinjector
- - Twelve REBIF Rebidose 22 mcg autoinjectors with yellow injector buttons, NDC: 44087-3322-1
-
REBIF Rebidose (interferon beta-1a) 44 mcg Autoinjector
- - Twelve REBIF Rebidose 44 mcg autoinjectors with teal-green injector buttons, NDC: 44087-3344-1
REBIF should be stored refrigerated between 36°F to 46°F (2°C to 8°C). DO NOT FREEZE. If needed, REBIF may be stored between 36°F to 77°F (2°C to 25°C) for up to 30 days and away from heat and light, but refrigeration is preferred.
Do not use beyond the expiration date printed on packages. REBIF contains no preservatives. Each prefilled syringe and REBIF Rebidose autoinjector is intended for a single dose. Unused portions should be discarded.
-
REBIF (interferon beta -1a) Titration Pack, NDC: 44087-8822-1
-
17 PATIENT COUNSELING INFORMATION
See FDA-approved patient labeling (Medication Guide).
Inform patients of the availability of a Medication Guide, and instruct them to read the Medication Guide prior to taking REBIF. Instruct patients to take REBIF only as prescribed.
Depression and Suicide
Advise patients that depression, suicidal ideation, and suicide have been reported during the use of REBIF. Inform patients of the symptoms of depression and suicidal ideation and instruct patients to immediately report any of these symptoms to their healthcare provider [see Warnings and Precautions (5.1)].
Hepatic Injury
Advise patients that severe liver injury, including hepatic failure, has been reported with the use of REBIF. Educate patients about the symptoms of hepatic injury and instruct patients to report them immediately to their healthcare provider [see Warnings and Precautions (5.2)].
Anaphylaxis and Other Allergic Reactions
Advise patients of the symptoms of allergic reactions and anaphylaxis, and instruct patients to seek immediate medical attention if these symptoms occur [see Warnings and Precautions (5.3)].
Injection Site Reactions including Necrosis
Advise patients that injection site reactions occur in most patients treated with REBIF and that injection site necrosis may occur [see Warnings and Precautions (5.4)]. Instruct patients to promptly report any break in the skin, which may be associated with blue-black discoloration, swelling, or drainage of fluid from the injection site, prior to continuing their REBIF therapy.
To minimize the likelihood of injection site reactions, inform patients of the importance of rotating injection sites with each dose and the use of aseptic injection technique [see Dosage and Administration (2.2)]. Advise patients not to re-use needles or syringes and instruct patients on safe disposal procedures. Provide appropriate instruction for self-injection of REBIF and REBIF Rebidose, including careful review of the REBIF Medication Guide.
Decreased Peripheral Blood Counts
Advise patients that they may develop a lowering of their peripheral blood counts, including their white blood counts, red blood counts, and platelets, and that their blood counts will be checked during therapy with REBIF. Inform patients that they may be more likely to get infections, anemia, or be at risk for bleeding, and that they should contact their healthcare provider if they develop symptoms of these adverse reactions [see Warnings and Precautions (5.5)].
Seizures
Instruct patients to report seizures immediately to their healthcare provider [see Warnings and Precautions (5.7)].
Flu-like Symptoms
Inform patients that flu-like symptoms are common following initiation of therapy with REBIF. Advise patients that concurrent use of analgesics and/or antipyretics may help reduce flu-like symptoms on treatment days [see Dosage and Administration (2.3)].
Risk in Pregnancy
Advise patients that REBIF should not be used during pregnancy unless the potential benefit justifies the potential risk to the fetus [see Use in Specific Populations (8.1)]. Therefore, inform patients that if a pregnancy is considered, or does occur, the risks and benefits of continuing REBIF should be discussed with their healthcare provider.
- SPL UNCLASSIFIED SECTION
-
MEDICATION GUIDE
MEDICATION GUIDE
REBIF
interferon beta-1a
Injection for subcutaneous useRead this Medication Guide before you start using REBIF and each time you get a refill. There may be new information. The information does not take the place of talking with your healthcare provider about your medical condition or your treatment.
What is the most important information I should know about REBIF?
REBIF can cause serious side effects. Tell your healthcare provider right away if you have any of the symptoms listed below while taking REBIF.
- 1.
Behavioral health problems including depression and suicidal thoughts. You may have mood problems including:
- depression (feeling hopeless or feeling bad about yourself)
- thoughts of hurting yourself or suicide
- 2. Liver problems or worsening of liver problems including liver failure. Symptoms may include:
- nausea
- loss of appetite
- tiredness
- dark colored urine and pale stools
- yellowing of your skin or the white part of your eye
- bleeding more easily than normal
- confusion
- sleepiness
During your treatment with REBIF you will need to see your healthcare provider regularly and have regular blood tests to check for side effects. - 3. Serious allergic and skin reactions. Symptoms may include:
- itching
- swelling of your face, eyes, lips, tongue or throat
- trouble breathing
- anxiousness
- feeling faint
- skin rash, hives, sores in your mouth, or skin blisters and peels
- 4. Injection site problems. Symptoms at the injection site may include:
- redness
- pain
- swelling
- color changes (blue or black)
- drainage of fluid
What is REBIF?
REBIF is a prescription medicine used to treat relapsing forms of multiple sclerosis, to include clinically isolated syndrome, relapsing-remitting disease, and active secondary progressive disease, in adults. It is a form of protein called beta interferon that is produced in the body.
It is not known if REBIF is safe and effective in children.
Who should not take REBIF?
Do not take REBIF if you:
- are allergic to interferon beta, human albumin, or any of the ingredients in REBIF. See the end of this Medication Guide for a complete list of ingredients in REBIF.
What should I tell my healthcare provider before taking REBIF?
Before you take REBIF, tell your healthcare provider if have or have had any of the following conditions:
- mental illness, including depression and suicidal behavior
- liver problems
- bleeding problems or blood clots
- low blood cell counts
- seizures (epilepsy)
- thyroid problems
- drink alcohol
- you are pregnant or plan to become pregnant. (It is not known if REBIF will harm your unborn baby. Tell your healthcare provider if you become pregnant during your treatment with REBIF.)
- you are breastfeeding or plan to breastfeed. (It is not known if REBIF passes into your breast milk. You and your healthcare provider should decide if you will use REBIF or breastfeed. You should not do both.)
Tell your healthcare provider about all medicines you take, including prescription and over-the-counter medicines, vitamins and herbal supplements.
REBIF and other medicines may affect each other causing side effects.
Ask your healthcare provider or pharmacist for a list of these medicines, if you are not sure.
Know the medicines you take. Keep a list of them to show your healthcare provider and pharmacist when you get a new medicine.
How should I use REBIF?
- See the Instructions for Use at the end of this Medication Guide on how to prepare and give an injection of REBIF using a prefilled syringe. For the REBIF Rebidose autoinjector, read the Instructions for Use that comes with the REBIF Rebidose autoinjector.
- Your healthcare provider should show you how to prepare and measure your dose of REBIF and how to inject your REBIF before you use it for the first time.
- REBIF is given by injection under the skin (subcutaneous injection) on the same 3 days a week, for example, Monday, Wednesday and Friday.
- Your injections should be at least 48 hours apart. Take them the same time each day.
- Inject REBIF exactly as your healthcare provider tells you.
- Your healthcare provider will tell you how much REBIF to inject, and may change the dose based on how your body responds. Do not inject more than your healthcare provider tells you to.
- Do not change your dose unless your healthcare provider tells you to.
- Change (rotate) your injection site you choose with each injection. This will help decrease the chance that you will have an injection site reaction.
- Do not inject REBIF into an area of the body where the skin is irritated, reddened, bruised, infected or scarred in any way.
- REBIF comes as a:
- prefilled syringe (REBIF)
- single-use prefilled autoinjector (REBIF Rebidose autoinjector)
What are the possible side effects of REBIF?
REBIF may cause serious side effects, including:
- See "What is the most important information I should know about REBIF?"
- Blood problems. REBIF can affect your bone marrow and cause low red and white blood cell, and platelet counts. In some people, these blood cell counts may fall to dangerously low levels. If your blood cell counts become very low, you can get infections and problems with bleeding and bruising. Your healthcare provider may ask you to have regular blood tests to check for blood problems.
- Seizures. Some people have had seizures while taking REBIF.
The most common side effects of REBIF include:
- flu-like symptoms. You may have flu-like symptoms when you first start taking REBIF. You may be able to manage these flu-like symptoms by taking over-the-counter pain and fever reducers. For many people, these symptoms lessen or go away over time. Symptoms may include:
- muscle aches
- fever
- tiredness
- chills
- stomach pain
- change in liver blood tests
Tell your healthcare provider if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of REBIF. For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.
How should I store REBIF?
- Store REBIF in the refrigerator between 36°F to 46°F (2°C to 8°C).
- Do not freeze REBIF.
- If you cannot refrigerate your REBIF, you can store your REBIF at temperatures above 36°F and below 77°˚F (2°C to 25°C) for up to 30 days.
- Keep REBIF away from heat and light.
Keep REBIF and all medicines out of the reach of children.
General information about the safe and effective use of REBIF
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use REBIF for a condition for which it was not prescribed. Do not give REBIF to other people, even if they have they have the same symptoms that you have. It may harm them.
This Medication Guide summarizes the most important information about REBIF. If you would like more information, talk with your healthcare provider. You may ask your healthcare provider or pharmacist for information about REBIF that is written for healthcare professionals.
For more information, go to www.REBIF.com or call toll-free 1-877-447-3243.
What are the ingredients in REBIF?
Active ingredient: interferon beta-1a
Inactive ingredients: albumin (human), mannitol, sodium acetate, water for injection
This Medication Guide has been approved by the U.S. Food and Drug Administration.
07/2019
- 1.
Behavioral health problems including depression and suicidal thoughts. You may have mood problems including:
-
INSTRUCTIONS FOR USE
Instructions for Use
REBIF (Re-bif)
interferon beta-1a
(in-ter-feer-on beta-one-â)
Injection for subcutaneous use
Prefilled SyringeRead and follow the Instructions for Use that come with your REBIF prefilled syringe before you start using it and each time you get a refill. Before you use a REBIF prefilled syringe for the first time, make sure your healthcare provider shows you the right way to use it.
Important: For the REBIF Rebidose autoinjector, read the Instructions for Use that come with the REBIF Rebidose autoinjector.
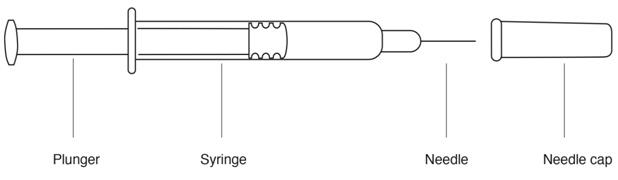
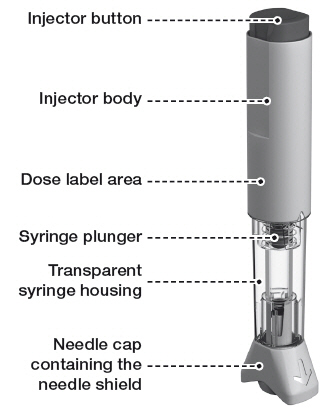
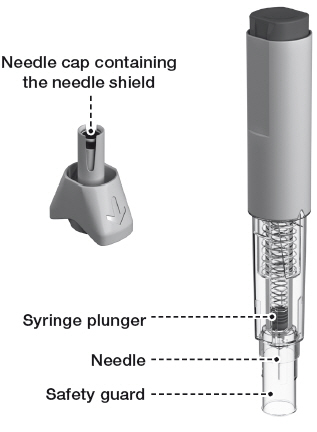
Parts of your REBIF Prefilled Syringe (See Figure A).
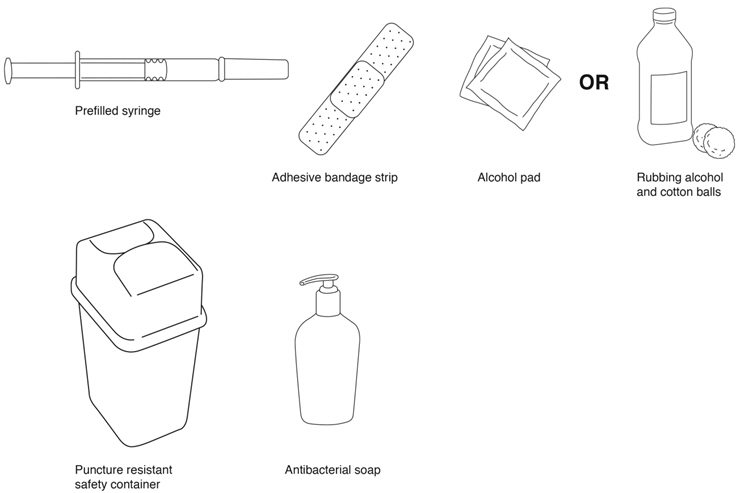
Supplies needed for a REBIF Injection (See Figure B):
- REBIF prefilled syringe
- alcohol pad or cotton balls and rubbing alcohol
- small adhesive bandage strip if desired
- puncture resistant safety container for disposal of used syringes. See "Disposing of your Needles and Syringes Section" in Step 4 of the IFU.
- antibacterial soap
- an over-the-counter pain or fever reducing medicine, if your healthcare provider has recommended that you take this before, at the same time, or after you give yourself REBIF to help decrease the fever, chills, sweating and muscle aches (flu-like symptoms) that may happen.
Titration (Dosing) Schedule
- When first starting treatment with REBIF, your healthcare provider may prescribe either the 22 mcg or 44 mcg dose of REBIF. You should gradually increase the dose over 4 weeks, starting at 20% of the prescribed dose for the first 2 weeks, half-dose for the second 2 weeks (weeks 3 and 4), and then the full dose prescribed by your healthcare provider.
If your prescribed dose is 22 mcg of REBIF, a REBIF Titration Pack containing 6 prefilled syringes with 8.8 mcg and 6 prefilled syringes with 22 mcg should be prescribed to you for use during the 4-week starting period. Table 1 explains the amount to inject using the REBIF Titration Pack syringes to gradually increase to 22 mcg.
Table 1: Titration Schedule for a 22 mcg Prescribed Dose* Week of Use Syringe to Use Amount of syringe - * Only prefilled syringes can be used to titrate to the 22 mcg Prescribed Dose
Week 1 Titration 8.8 mcg syringe Use half of syringe Week 2 Titration 8.8 mcg syringe Use half of syringe Week 3 Titration 22 mcg syringe Use half of syringe Week 4 Titration 22 mcg syringe Use half of syringe Week 5 and on 22 mcg syringe or autoinjector Use full syringe or autoinjector If your prescribed dose is 44 mcg, you may be prescribed either a REBIF Titration Pack (described above) or REBIF Rebidose Titration Pack containing 6 autoinjectors with 8.8 mcg and 6 autoinjectors with 22 mcg for use during the 4 week titration period. Table 2 explains the amount to inject using the REBIF Titration Pack or REBIF Rebidose Titration Pack to gradually increase to 44 mcg.
Table 2: Titration Schedule for a 44 mcg Prescribed Dose* Week of Use Syringe or Autoinjector to Use Amount of syringe or autoinjector - * Prefilled syringes or autoinjectors can be used to titrate to 44 mcg Prescribed Dose
Week 1 Titration 8.8 mcg syringe or autoinjector Use full syringe or autoinjector Week 2 Titration 8.8 mcg syringe or autoinjector Use full syringe or autoinjector Week 3 Titration 22 mcg syringe or autoinjector Use full syringe or autoinjector Week 4 Titration 22 mcg syringe or autoinjector Use full syringe or autoinjector Week 5 and on 44 mcg syringe or autoinjector Use full syringe or autoinjector Step 1. Preparing for your REBIF Injection
- Check the expiration date. Do not use if the medication is expired. The expiration date is printed on the syringe, plastic syringe packaging and carton.
- Remove your REBIF syringe from the refrigerator at least 30 minutes before you plan to use it so it can warm to room temperature. Do not heat or microwave the medication.
- Be sure that the dose, either, 8.8 mcg, 22 mcg or 44 mcg, described on the carton is the same as the dose prescribed by your healthcare provider.
- Remove the REBIF syringe from the plastic packaging. Keep the needle capped.
- Look at the contents of the syringe carefully. The liquid should be clear to slightly yellow. Do not use if the liquid is cloudy, discolored or contains particles. Use a different syringe.
Step 2. Choose and Prepare your Injection Site
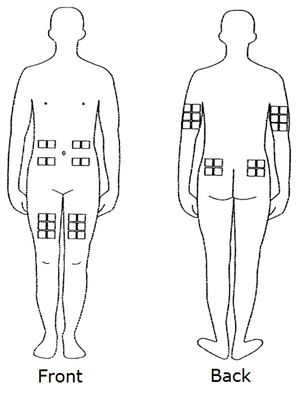
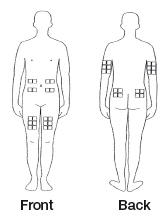
- The best sites for giving yourself an injection are those areas with a layer of fat between the skin and muscle, like your thigh, the outer surface of your upper arm, your stomach or buttocks.
- Do not use the area near your waistline or within 2 inches of your navel. If you are very thin, use only the thigh or outer surface of the arm for injection.
- Use a different site each time you inject such as the thigh, hip, stomach or upper arm (See Figure C).
- Do not inject REBIF into an area of your body where the skin is irritated, reddened, bruised, infected or abnormal in any way.
- Wash your hands thoroughly with antibacterial soap before preparing to inject the medicine.
- Clean the injection site with an alcohol pad or cotton ball with rubbing alcohol using a circular motion. To avoid stinging, you should let your skin dry before you inject REBIF.
Step 3. Inject your REBIF
- Remove the needle cap from the syringe needle.
- If your healthcare provider has told you to use less than the full 0.5 mL dose, slowly push the plunger in until the amount of medicine left in the syringe is the amount healthcare provider told you to use.
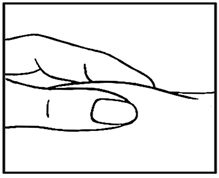
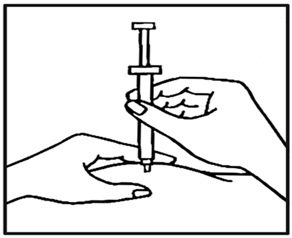
- Use your thumb and forefinger to pinch a pad of skin surrounding the cleaned injection site (See Figure D). Hold the syringe like a pencil with your other hand.
- While still pinching the skin, quickly insert the needle like a dart at about a 90 degree angle (just under the skin) into the pad of tissue as shown (See Figure E).
- After the needle is in, remove the hand that you used to pinch your skin and inject the medicine using a slow, steady push on the plunger until all the medicine is injected and the syringe is empty (See Figure F).
- Withdraw the needle and apply gentle pressure to the injection site with a dry cotton ball or sterile gauze. Applying a cold compress or ice pack to the injection site after injection may help reduce local skin reactions.
- Put a small adhesive bandage strip over the injection site, if desired.
- Keep a record of the date and location of each injection.
- After 2 hours, check the injection site for redness, swelling, or tenderness. If you have a skin reaction and it does not clear up in a few days, call your healthcare provider.
Step 4. Disposing of your Needles and Syringes
- Put your used needles, syringes, and autoinjectors, including REBIF, in an FDA-cleared sharps container right away after use. Do not throw away (dispose of) any syringes or autoinjectors in your household trash.
If you do not have an FDA-cleared sharps disposal container, you may use a household container that is:- made of a heavy-duty plastic,
- closed with a tight-fitting, puncture-resistant lid,
- upright and stable during use,
- leak-resistant, and
- properly labeled to warn of hazardous waste inside the container.
- When your sharps disposal container is almost full, you will need to follow your community guidelines for the right way to dispose of your sharps disposal container. There may be state or local laws about how you should throw away used autoinjectors and syringe needles. For more information about safe sharps disposal, and for specific information about sharps disposal in the state that you live in, go to the FDA's website at: http://www.fda.gov/safesharpsdisposal.
- Do not dispose of your used sharps disposal container in your household trash unless your community guidelines permit this. Do not recycle your used sharps disposal container.
Manufactured by:
EMD Serono, Inc.
Rockland, MA 02370
U.S. License 1773Marketed by:
EMD Serono, Inc.
Rockland, MA 02370Revised 11/2015
-
INSTRUCTIONS FOR USE
Rebif® Rebidose®
Instructions For Use

Exclusively for use with
Rebif®
(interferon beta-1a)
subcutaneous injectionWelcome
This guide contains information on how to use Rebif® Rebidose®, a pre-assembled, single-use autoinjector that administers one dose of Rebif® (interferon beta-1a) for the treatment of relapsing forms of multiple sclerosis.
Please read these instructions carefully before you start using the Rebif® Rebidose® and remember, you must have received the appropriate training before injecting.
If at any time, you have questions or concerns, please contact your health care provider or call MS LifeLines at 1-877-447-3243.
Rx Only
Contents Rebif® Rebidose® features 4  Warnings
Warnings6 Important Information 8 How Supplied 10 Titration 12 Choosing an injection site 13 Step 1: Prepare for your injection 14 Examine syringe and expiration date 15 Step 2: Administer your injection 18 Step 3: Finish your injection 20 Disposal 22 Storage 25 Travel 26 Notes 27 Rebif® Rebidose® features
Before injection:
After injection:
 Warnings
Warnings
- Always use the injection technique advised by your health care provider and contact them with any questions you might have.
- Always keep the Rebidose® autoinjector out of the reach of children.
-
Do not share the Rebidose® with anyone. Doing so may result in injury, including the transmission of infectious blood-borne diseases. Adhere to strict safety and antiseptic precautions at all times.
- - Do not insert your fingers into the opening of the safety guard.
- - Do not try to re-use a Rebidose® single-use autoinjector that has already been used.
- - Adhere to proper disposal procedures to avoid a needle stick injury.
- Check the expiration date on the Rebidose® autoinjector label and its carton. If the medication has expired, Do not use it.
- Examine the contents of the syringe carefully through the transparent housing. The liquid should be clear or slightly yellow. Inspect for cracks or breakage in the syringe or other parts. Do not use Rebidose® if it is cracked or broken or if the liquid is cloudy, discolored or contains particles.
- If the Rebidose® has been dropped more than 3 feet, or if it looks damaged for any reason, Do not use it. Instead, dispose of it in an acceptable biohazard (sharps) container and use a new Rebidose® autoinjector.
- Contact your health care provider about any damaged Rebidose® autoinjector.
Important Information
- Store your Rebidose® autoinjectors in a refrigerator until ready for use.
- If you or someone around you is injured by the needle, contact your health care provider immediately and dispose of the Rebidose® in an acceptable biohazard (sharps) container.
- Injecting Rebif® the medicine in the Rebidose® autoinjector may cause skin reactions including soreness, redness, pain, bruising, or swelling. Tell your health care provider about any skin reactions that become swollen, painful, or look infected and do not heal within a few days.
- Use a different site each time you inject. Do not inject Rebif® where your skin is irritated, reddened, bruised, infected or abnormal in any way.
- The Rebidose® autoinjector contains a glass syringe. In very rare cases, the syringe may break during the injection. If this happens, immediately dispose of any broken glass and the damaged Rebidose® autoinjector in the biohazard (sharps) container, taking necessary precautions to avoid injury. Contact your health care provider or MS LifeLines at 1-877-447-3243 immediately.
How Supplied
Rebidose® is available in 3 dose sizes. Check that the dose of Rebif® is the one prescribed for you by looking at the Rebidose® carton and at the dose label on the Rebidose® autoinjector.
Rebidose® autoinjectors are supplied in these 3 packaging presentations:
- Titration Pack
- 6 Rebif® 8.8 mcg Rebidose® autoinjectors with a lime green injector button.
- 6 Rebif® 22 mcg Rebidose® autoinjectors with a yellow injector button.
- 12 Rebif® 22 mcg Rebidose® autoinjectors with a yellow injector button.
- 12 Rebif® 44 mcg Rebidose® autoinjectors with a teal green injector button.

Titration
At the beginning of Rebif® treatment, your health care provider may prescribe a titration phase to gradually increase to the intended dosage.
The Rebif® Titration Pack contains six 8.8 mcg Rebidose® autoinjectors with a lime green injector button and six 22 mcg Rebidose® autoinjectors with a yellow injector button.
The titration period lasts 4 weeks and during this time, you will administer 12 injections:
- Weeks 1 and 2: Use one 8.8 mcg autoinjector three times a week, at least 48 hours apart.
- Weeks 3 and 4: Use one 22 mcg autoinjector three times a week, at least 48 hours apart.
Your health care provider may provide a different dose and schedule.
Choosing an injection site
The best sites for giving a subcutaneous injection are those areas with a layer of fat between the skin and muscle. These include the thigh, the outer surface of the upper arm, the stomach and the buttocks. Do not use the area near your waistline or within 2 inches of your navel.
Only choose one site for injection. Use a different site each time you inject.
- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - -
 Caution
Caution
Do not inject Rebif® where your skin is irritated, reddened, bruised, infected or abnormal in any way.
- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - -
Step 1: Prepare for your injection
1.1) Before you begin, you may find injecting more comfortable if you allow time for the Rebif® to warm up to room temperature before injecting. Therefore, it is recommended that you remove the Rebidose® autoinjector from the refrigerator at least 30 minutes prior to use.
- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - -
 Caution
Caution
Do not heat or microwave a Rebidose® autoinjector.
- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - -
1.2) Put all of the items listed below within easy reach on a table or other stable surface:
- 1 Rebidose® autoinjector containing Rebif®
- Alcohol wipes/swabs or cotton balls and rubbing alcohol
- Small adhesive bandage strip (if needed)
- A biohazard (sharps) container (see Disposal section on page 22)
1.3) Wash your hands thoroughly with antibacterial soap.
1.4) Open the tray over a table or soft surface by peeling back the plastic covering and remove 1 Rebidose® autoinjector. Do not remove the needle cap until you are ready to inject because the autoinjector could roll off the table and become unsterile.
1.5) Check the expiration date on the Rebidose® autoinjector label and its carton. If the medication has expired, do not use it.
1.6) Examine the contents of the syringe carefully through the transparent housing. The liquid should be clear or slightly yellow.
1.7) Inspect for cracks or breakage in the syringe or other parts. Do not use Rebidose® if it is cracked or broken or if the liquid is cloudy, discolored or contains particles.
1.8) Use an alcohol wipe to clean the injection site. Let your skin dry to prevent stinging during injection.
1.9) Hold the Rebidose® by the injector body (fig a ) and pull off the needle cap.
1.10) Look inside the needle cap to make sure you see a black needle shield inside the cap (fig b ).
1.11) Dispose of the needle cap and proceed to the injection step without delay.
 Warning
Warning
If the Rebidose® has been dropped more than 3 feet, or if it looks damaged for any reason, do not use it. Instead, dispose of it in an acceptable biohazard (sharps) container and use a new Rebidose® autoinjector.
Step 2: Administer your injection
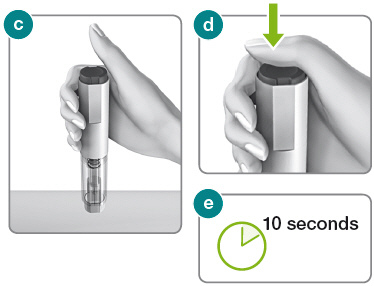
2.1) Hold the Rebidose® autoinjector in your palm with your thumb above the injector button.
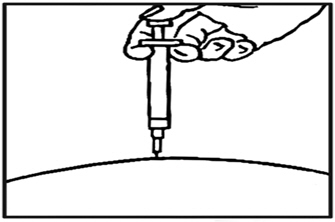
2.2) Place the Rebidose® upright with the needle end flat against your skin at a 90° angle. Push the Rebidose® against your skin until you feel resistance; this action unlocks the injector button (fig c ).
2.3) Keep the Rebidose® pressed firmly against the skin and use your thumb to push the injector button (fig d ). You will hear a click, which means the injection has begun.
2.4) Keep the Rebidose® pressed firmly against your skin for at least 10 seconds while the medication is dispensed (fig e ).
If you have any problems, contact MS LifeLines at 1-877-447-3243.
 Caution
Caution
If the injection does not start, release the injector button and make sure that the Rebidose® is still pressed firmly against your skin. Then push firmly on the injector button, listening for the click that indicates the start of the injection.
- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - -
Step 3: Finish your injection
3.1) Before lifting the Rebidose® from your skin, make sure that the syringe plunger has moved to the bottom and that the entire dose has been injected (fig f ).
3.2) Lift the Rebidose® from the injection site. The safety guard slides down and locks into place to protect you from the needle (fig g ). If any liquid is left in the syringe or if you have any other problems, contact your health care provider or MS LifeLines at 1-877-447-3243.
Do not try to put the needle cap on the used Rebidose® autoinjector. It is no longer needed.
3.3) If desired, use a small adhesive bandage to cover the injection site.

1) Put your used Rebidose® autoinjectors in a FDA-cleared sharps disposal container right away after use (fig h ). Do not throw them away (dispose of) in your household trash.

2) If you do not have a FDA-cleared sharps disposal container, you may use a household container that is:
- - made of a heavy-duty plastic;
- - can be closed with a tight-fitting, puncture-resistant lid, without sharps being able to come out;
- - upright and stable during use;
- - leak-resistant; and
- - properly labeled to warn of hazardous waste inside the container.
3) When your sharps disposal container is almost full, you will need to follow your community guidelines for the correct way to dispose of it. There may be state or local laws about how you should throw away used needles and syringes. For more information about safe sharps disposal in the state that you live in, go to the FDA's website at: http://www.fda.gov/safesharpsdisposal
4) Do not dispose of your used sharps disposal container in your household trash unless your community guidelines permit this. Do not recycle your used sharps disposal container.
- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - -
 Caution
Caution
Always keep the biohazard (sharps) container out of the sight and reach of children.
- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - -
 Warning
Warning
- Do not insert your fingers into the opening of the safety guard.
- Do not try to re-use a Rebidose® single-use autoinjector that has already been used.
- Adhere to proper disposal procedures to avoid a needle stick injury.
Storage
- Each Rebidose® autoinjector contains a single dose of Rebif®.
- Store Rebidose® autoinjectors in the refrigerator between 36°F and 46°F (2°C to 8°C). Do not freeze. If a refrigerator is not available, Rebidose® may be stored between 36˚F and 77˚F (2˚C to 25˚C) for up to 30 days away from heat and light.
- Do not put them in or near the freezer compartment. Do not inject Rebif® that you know or suspect has been frozen.
- Keep the Rebidose® in its packaging and only open one when you need it. Refer to the Rebif® drug package insert and medication guide for specific storage guidelines.
Travel
- When you travel, take 3 Rebidose® autoinjectors with you for each week of your trip. Take some extra in case you are away for longer than expected.
- Remember to pack an empty biohazard (sharps) container for proper disposal.
- When traveling by air, always carry Rebidose® autoinjectors in your hand luggage because the aircraft luggage compartment can be very cold and the Rebif® could freeze.
- It is safe to pass Rebidose® autoinjectors through x-ray machines, but you may need a note from your health care provider to allow you to carry them aboard an airplane.
- Prior to traveling, always check with your airline and your health care provider about bringing injectable medication with you.
Notes
You may find it helpful to record information about your 3 weekly injections (Inj.) to discuss with your health care provider.
Week 1 Inj. Site Date& Time Site Reaction Inj. 1 Yes No Inj. 2 Yes No Inj. 3 Yes No Week 2 Inj. Site Date& Time Site Reaction Inj. 1 Yes No Inj. 2 Yes No Inj. 3 Yes No Week 3 Inj. Site Date& Time Site Reaction Inj. 1 Yes No Inj. 2 Yes No Inj. 3 Yes No Week 4 Inj. Site Date& Time Site Reaction Inj. 1 Yes No Inj. 2 Yes No Inj. 3 Yes No - SPL UNCLASSIFIED SECTION
-
PRINCIPAL DISPLAY PANEL - Kit Carton - 8822
Rebif® Titration Pack
(interferon beta-1a)NDC: 44087-8822-1
8.8 mcg/0.2 mL
22 mcg/0.5 mLFor subcutaneous injection
Rx Only
Medication Guide for patients enclosed6 Single-use 8.8 mcg/0.2 mL prefilled syringes
6 Single-use 22 mcg/0.5 mL prefilled syringesEMD
Serono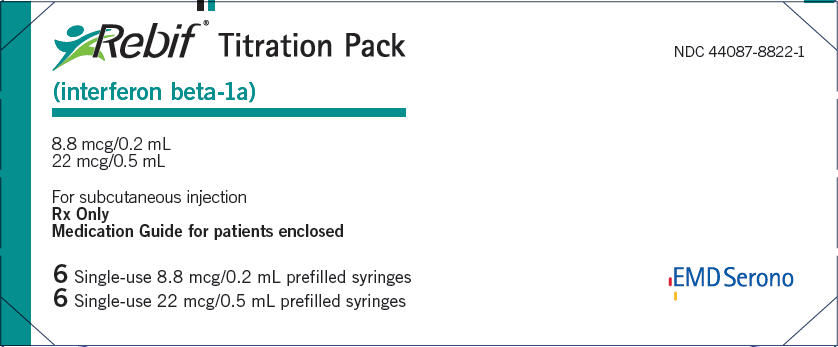
-
PRINCIPAL DISPLAY PANEL - Kit Carton - 0188
Rebif® Rebidose®
(interferon beta-1a)
InjectionNDC: 44087-0188-1
6 single-use 8.8 mcg / 0.2 mL autoinjectors
6 single-use 22 mcg / 0.5 mL autoinjectorsRx only
8.8 mcg / 0.2 mL
22 mcg / 0.5 mLTitration Pack
For subcutaneous injectionAttention pharmacist:
Each patient is required to receive
the enclosed Medication GuideEMD
Serono
-
PRINCIPAL DISPLAY PANEL - 12 Syringe Carton - 0022
Rebif® 22 mcg/0.5 mL
(interferon beta-1a)NDC: 44087-0022-3
For subcutaneous injection
Rx only
Medication Guide for patients enclosed12 Single-use prefilled syringes
EMD
Serono
-
PRINCIPAL DISPLAY PANEL - 12 Syringe Carton - 0044
Rebif® 44 mcg/0.5 mL
(interferon beta-1a)NDC: 44087-0044-3
For subcutaneous injection
Rx only
Medication Guide for patients enclosed12 Single-use prefilled syringes
EMD
Serono
-
PRINCIPAL DISPLAY PANEL - 12 Autoinjector Carton - 3322
NDC: 44087-3322-1
Rebif® Rebidose®
(interferon beta-1a)
Injection12 single-use autoinjectors
22 mcg / 0.5 mL
Rx only
For subcutaneous injection
Attention pharmacist: Each patient is required
to receive the enclosed Medication GuideEMD
Serono
-
PRINCIPAL DISPLAY PANEL - 12 Autoinjector Carton - 3344
NDC: 44087-3344-1
Rebif® Rebidose®
(interferon beta-1a)
Injection12 single-use autoinjectors
44 mcg / 0.5 mL
Rx only
For subcutaneous injection
Attention pharmacist: Each patient is required
to receive the enclosed Medication GuideEMD
Serono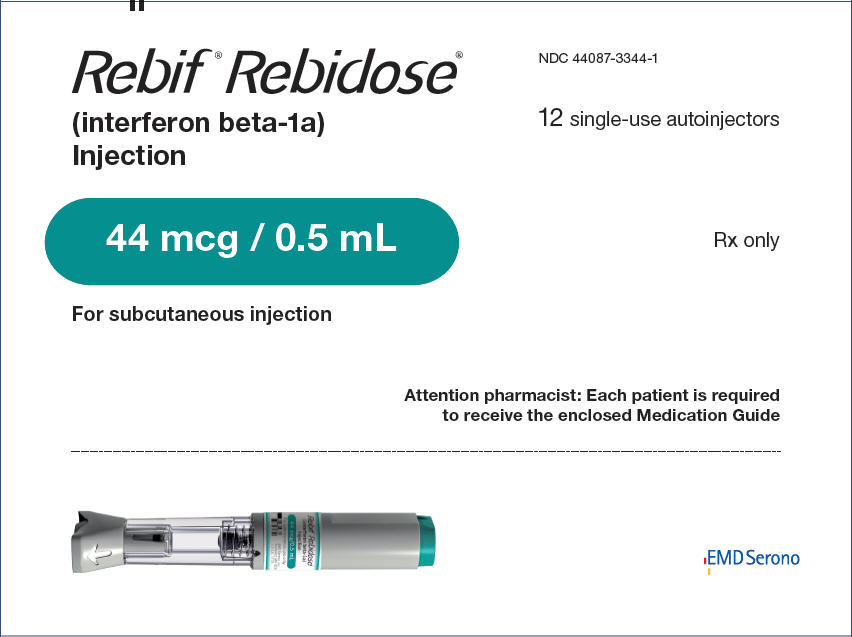
-
INGREDIENTS AND APPEARANCE
REBIF
interferon beta-1a kitProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 44087-8822 Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 44087-8822-1 1 in 1 CARTON 12/17/2004 Quantity of Parts Part # Package Quantity Total Product Quantity Part 1 6 SYRINGE, GLASS 1.2 mL Part 2 6 SYRINGE, GLASS 3 mL Part 1 of 2 REBIF
interferon beta-1a injection, solutionProduct Information Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength INTERFERON BETA-1A (UNII: XRO4566Q4R) (INTERFERON BETA-1A - UNII:XRO4566Q4R) INTERFERON BETA-1A 8.8 ug in 0.2 mL Inactive Ingredients Ingredient Name Strength MANNITOL (UNII: 3OWL53L36A) 10.9 mg in 0.2 mL ALBUMIN HUMAN (UNII: ZIF514RVZR) 0.8 mg in 0.2 mL SODIUM ACETATE (UNII: 4550K0SC9B) 0.16 mg in 0.2 mL WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 0.2 mL in 1 SYRINGE, GLASS; Type 3: Prefilled Biologic Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA103780 12/17/2004 Part 2 of 2 REBIF
interferon beta-1a injection, solutionProduct Information Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength INTERFERON BETA-1A (UNII: XRO4566Q4R) (INTERFERON BETA-1A - UNII:XRO4566Q4R) INTERFERON BETA-1A 22 ug in 0.5 mL Inactive Ingredients Ingredient Name Strength MANNITOL (UNII: 3OWL53L36A) 27.3 mg in 0.5 mL ALBUMIN HUMAN (UNII: ZIF514RVZR) 2 mg in 0.5 mL SODIUM ACETATE (UNII: 4550K0SC9B) 0.4 mg in 0.5 mL WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 0.5 mL in 1 SYRINGE, GLASS; Type 3: Prefilled Biologic Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA103780 12/17/2004 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA103780 12/17/2004 REBIF REBIDOSE
interferon beta-1a kitProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 44087-0188 Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 44087-0188-1 1 in 1 CARTON 12/21/2012 Quantity of Parts Part # Package Quantity Total Product Quantity Part 1 6 PACKAGE 1.2 mL Part 2 6 PACKAGE 3 mL Part 1 of 2 REBIF REBIDOSE
interferon beta-1a injection, solutionProduct Information Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength INTERFERON BETA-1A (UNII: XRO4566Q4R) (INTERFERON BETA-1A - UNII:XRO4566Q4R) INTERFERON BETA-1A 8.8 ug in 0.2 mL Inactive Ingredients Ingredient Name Strength MANNITOL (UNII: 3OWL53L36A) 10.9 mg in 0.2 mL ALBUMIN HUMAN (UNII: ZIF514RVZR) 0.8 mg in 0.2 mL SODIUM ACETATE (UNII: 4550K0SC9B) 0.16 mg in 0.2 mL WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 0.2 mL in 1 PACKAGE; Type 3: Prefilled Biologic Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA103780 12/21/2012 Part 2 of 2 REBIF REBIDOSE
interferon beta-1a injection, solutionProduct Information Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength INTERFERON BETA-1A (UNII: XRO4566Q4R) (INTERFERON BETA-1A - UNII:XRO4566Q4R) INTERFERON BETA-1A 22 ug in 0.5 mL Inactive Ingredients Ingredient Name Strength MANNITOL (UNII: 3OWL53L36A) 27.3 mg in 0.5 mL ALBUMIN HUMAN (UNII: ZIF514RVZR) 2 mg in 0.5 mL SODIUM ACETATE (UNII: 4550K0SC9B) 0.4 mg in 0.5 mL WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 0.5 mL in 1 PACKAGE; Type 3: Prefilled Biologic Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA103780 12/21/2012 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA103780 12/21/2012 REBIF
interferon beta-1a injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 44087-0022 Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength INTERFERON BETA-1A (UNII: XRO4566Q4R) (INTERFERON BETA-1A - UNII:XRO4566Q4R) INTERFERON BETA-1A 22 ug in 0.5 mL Inactive Ingredients Ingredient Name Strength ALBUMIN HUMAN (UNII: ZIF514RVZR) 2 mg in 0.5 mL MANNITOL (UNII: 3OWL53L36A) 27.3 mg in 0.5 mL SODIUM ACETATE (UNII: 4550K0SC9B) 0.4 mg in 0.5 mL WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 44087-0022-3 12 in 1 CARTON 03/07/2002 1 NDC: 44087-0022-9 0.5 mL in 1 SYRINGE, GLASS; Type 3: Prefilled Biologic Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA103780 03/07/2002 REBIF
interferon beta-1a injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 44087-0044 Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength INTERFERON BETA-1A (UNII: XRO4566Q4R) (INTERFERON BETA-1A - UNII:XRO4566Q4R) INTERFERON BETA-1A 44 ug in 0.5 mL Inactive Ingredients Ingredient Name Strength ALBUMIN HUMAN (UNII: ZIF514RVZR) 4 mg in 0.5 mL MANNITOL (UNII: 3OWL53L36A) 27.3 mg in 0.5 mL SODIUM ACETATE (UNII: 4550K0SC9B) 0.4 mg in 0.5 mL WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 44087-0044-3 12 in 1 CARTON 03/07/2002 1 NDC: 44087-0044-9 0.5 mL in 1 SYRINGE, GLASS; Type 3: Prefilled Biologic Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA103780 03/07/2002 REBIF REBIDOSE
interferon beta-1a injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 44087-3322 Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength INTERFERON BETA-1A (UNII: XRO4566Q4R) (INTERFERON BETA-1A - UNII:XRO4566Q4R) INTERFERON BETA-1A 22 ug in 0.5 mL Inactive Ingredients Ingredient Name Strength ALBUMIN HUMAN (UNII: ZIF514RVZR) 2 mg in 0.5 mL MANNITOL (UNII: 3OWL53L36A) 27.3 mg in 0.5 mL SODIUM ACETATE (UNII: 4550K0SC9B) 0.4 mg in 0.5 mL WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 44087-3322-1 12 in 1 CARTON 12/21/2012 1 NDC: 44087-3322-9 0.5 mL in 1 PACKAGE; Type 3: Prefilled Biologic Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA103780 12/21/2012 REBIF REBIDOSE
interferon beta-1a injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 44087-3344 Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength INTERFERON BETA-1A (UNII: XRO4566Q4R) (INTERFERON BETA-1A - UNII:XRO4566Q4R) INTERFERON BETA-1A 44 ug in 0.5 mL Inactive Ingredients Ingredient Name Strength ALBUMIN HUMAN (UNII: ZIF514RVZR) 4 mg in 0.5 mL MANNITOL (UNII: 3OWL53L36A) 27.3 mg in 0.5 mL SODIUM ACETATE (UNII: 4550K0SC9B) 0.4 mg in 0.5 mL WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 44087-3344-1 12 in 1 CARTON 12/21/2012 1 NDC: 44087-3344-9 0.5 mL in 1 PACKAGE; Type 3: Prefilled Biologic Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA103780 12/21/2012 Labeler - EMD Serono, Inc. (088514898)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.