CLEOCIN- clindamycin phosphate suppository
Cleocin by
Drug Labeling and Warnings
Cleocin by is a Prescription medication manufactured, distributed, or labeled by U.S. Pharmaceuticals, Pharmacia and Upjohn Company LLC. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
- SPL UNCLASSIFIED SECTION
-
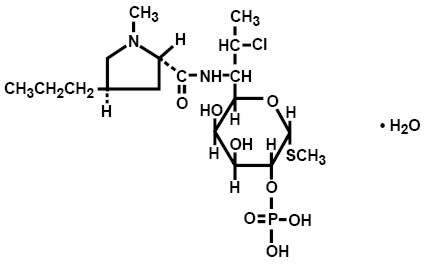
DESCRIPTION
Clindamycin phosphate is a water-soluble ester of the semisynthetic antibiotic produced by a 7(S)-chloro-substitution of the 7(R)-hydroxyl group of the parent antibiotic lincomycin. The chemical name for clindamycin phosphate is methyl 7-chloro-6,7,8-trideoxy-6-(1-methyl-trans-4-propyl-L-2-pyrrolidinecarboxamido)-1-thio-L-threo-α-D-galacto-octopyranoside 2-(dihydrogen phosphate). The monohydrate form has a molecular weight of 522.98, and the molecular formula is C18H34ClN2O8PSH2O. The structural formula is represented below:
CLEOCIN Vaginal Ovules are semisolid, white to off-white suppositories for intravaginal administration. Each 2.5 g suppository contains clindamycin phosphate equivalent to 100 mg clindamycin in a base consisting of a mixture of glycerides of saturated fatty acids.
-
CLINICAL PHARMACOLOGY
Systemic absorption of clindamycin was estimated following a once-a-day intravaginal dose of one clindamycin phosphate vaginal suppository (equivalent to 100 mg clindamycin) administered to 11 healthy female volunteers for 3 days. Approximately 30% (range 6% to 70%) of the administered dose was absorbed systemically on day 3 of dosing based on area under the concentration-time curve (AUC). Systemic absorption was estimated using a subtherapeutic 100 mg intravenous dose of clindamycin phosphate as a comparator in the same volunteers. The mean AUC following day 3 of dosing with the suppository was 3.2 µghr/mL (range 0.42 to 11 µghr/mL). The Cmax observed on day 3 of dosing with the suppository averaged 0.27 µg/mL (range 0.03 to 0.67 µg/mL) and was observed about 5 hours after dosing (range 1 to 10 hours). In contrast, the AUC and Cmax after the single intravenous dose averaged 11 µg hr/mL (range 5.1 to 26 µghr/mL) and 3.7 µg/mL (range 2.4 to 5.0 µg/mL), respectively. The mean apparent elimination half-life after dosing with the suppository was 11 hours (range 4 to 35 hours) and is considered to be limited by the absorption rate.
The results from this study showed that systemic exposure to clindamycin (based on AUC) from the suppository was, on average, three fold lower than that from a single subtherapeutic 100 mg intravenous dose of clindamycin. In addition, the recommended daily and total doses of intravaginal clindamycin suppository are far lower than those typically administered in oral or parenteral clindamycin therapy (100 mg of clindamycin per day for 3 days equivalent to about 30 mg absorbed per day from the ovule relative to 600 to 2700 mg/day for up to 10 days or more, orally or parenterally). The overall systemic exposure to clindamycin from Cleocin Vaginal Ovules is substantially lower than the systemic exposure from therapeutic doses of oral clindamycin hydrochloride (two-fold to 20-fold lower) or parenteral clindamycin phosphate (40-fold to 50-fold lower).
-
MICROBIOLOGY
Clindamycin inhibits bacterial protein synthesis at the level of the bacterial ribosome. The antibiotic binds preferentially to the 50S ribosomal subunit and affects the process of peptide chain initiation. Although clindamycin phosphate is inactive in vitro, rapid in vivo hydrolysis converts this compound to the antibacterially active clindamycin.
Culture and sensitivity testing of bacteria are not routinely performed to establish the diagnosis of bacterial vaginosis. (See INDICATIONS AND USAGE.) Standard methodology for the susceptibility testing of the potential bacterial vaginosis pathogens, Gardnerella vaginalis, Mobiluncus spp, or Mycoplasma hominis, has not been defined. Nonetheless, clindamycin is an antimicrobial agent active in vitro against most strains of the following organisms that have been reported to be associated with bacterial vaginosis:
- Bacteroides spp
- Gardnerella vaginalis
- Mobiluncus spp
- Mycoplasma hominis
- Peptostreptococcus spp
-
INDICATIONS AND USAGE
CLEOCIN Vaginal Ovules are indicated for 3-day treatment of bacterial vaginosis in non-pregnant women. There are no adequate and well-controlled studies of CLEOCIN Vaginal Ovules in pregnant women.
NOTE: For purposes of this indication, a clinical diagnosis of bacterial vaginosis is usually defined by the presence of a homogeneous vaginal discharge that (a) has a pH of greater than 4.5, (b) emits a "fishy" amine odor when mixed with a 10% KOH solution, and (c) contains clue cells on microscopic examination. Gram's stain results consistent with a diagnosis of bacterial vaginosis include (a) markedly reduced or absent Lactobacillus morphology, (b) predominance of Gardnerella morphotype, and (c) absent or few white blood cells.
Other pathogens commonly associated with vulvovaginitis, eg, Trichomonas vaginalis, Chlamydia trachomatis, Neisseria gonorrhoeae, Candida albicans, and herpes simplex virus, should be ruled out.
-
CONTRAINDICATIONS
CLEOCIN Vaginal Ovules are contraindicated in individuals with a history of hypersensitivity to clindamycin, lincomycin, or any of the components of this vaginal suppository. CLEOCIN Vaginal Ovules are also contraindicated in individuals with a history of regional enteritis, ulcerative colitis, or a history of "antibiotic-associated" colitis.
-
WARNINGS
Pseudomembranous colitis has been reported with nearly all antibacterial agents, including clindamycin, and may range in severity from mild to life-threatening. Orally and parenterally administered clindamycin has been associated with severe colitis, which may end fatally. Diarrhea, bloody diarrhea, and colitis (including pseudomembranous colitis) have been reported with the use of orally and parenterally administered clindamycin, as well as with topical (dermal) formulations of clindamycin. Therefore, it is important to consider this diagnosis in patients who present with diarrhea subsequent to the administration of CLEOCIN Vaginal Ovules, because approximately 30% of the clindamycin dose is systemically absorbed from the vagina.
Treatment with antibacterial agents alters the normal flora of the colon and may permit overgrowth of clostridia. Studies indicate that a toxin produced by Clostridium difficile is a primary cause of "antibiotic-associated" colitis.
After the diagnosis of pseudomembranous colitis has been established, therapeutic measures should be initiated. Mild cases of pseudomembranous colitis usually respond to discontinuation of the drug alone. In moderate to severe cases, consideration should be given to management with fluids and electrolytes, protein supplementation, and treatment with an antibacterial drug clinically effective against Clostridium difficile colitis.
Onset of pseudomembranous colitis symptoms may occur during or after antimicrobial treatment.
-
PRECAUTIONS
General
The use of CLEOCIN Vaginal Ovules may result in the overgrowth of nonsusceptible organisms in the vagina. In clinical studies using CLEOCIN Vaginal Ovules, treatment-related moniliasis was reported in 2.7% and vaginitis in 3.6% of 589 nonpregnant women. Moniliasis, as reported here, includes the terms: vaginal or nonvaginal moniliasis and fungal infection. Vaginitis includes the terms: vulvovaginal disorder, vaginal discharge, and vaginitis/vaginal infection.
Information for the Patient
The patient should be instructed not to engage in vaginal intercourse or use other vaginal products (such as tampons or douches) during treatment with this product.
The patient should also be advised that these suppositories use an oleaginous base that may weaken latex or rubber products such as condoms or vaginal contraceptive diaphragms. Therefore, the use of such products within 72 hours following treatment with CLEOCIN Vaginal Ovules is not recommended.
Drug Interactions
Systemic clindamycin has been shown to have neuromuscular blocking properties that may enhance the action of other neuromuscular blocking agents. Therefore, it should be used with caution in patients receiving such agents.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term studies in animals have not been performed with clindamycin to evaluate carcinogenic potential. Genotoxicity tests performed included a rat micronucleus test and an Ames test. Both tests were negative. Fertility studies in rats treated orally with up to 300 mg/kg/day (31 times the human exposure based on mg/m2) revealed no effects on fertility or mating ability.
Pregnancy
Teratogenic effects
Pregnancy Category B
In clinical trials with pregnant women, the systemic administration of clindamycin during the second and third trimesters, has not been associated with an increased frequency of congenital abnormalities.
Clindamycin vaginal ovules should be used during the first trimester of pregnancy only if clearly needed and the benefits outweigh the risks. There are no adequate and well-controlled studies of CLEOCIN Vaginal Ovules in pregnant women during the first trimester of pregnancy.
CLEOCIN Vaginal Cream, 2%, has been studied in pregnant women during the second trimester. In women treated for 7 days, abnormal labor was reported more frequently in patients who received CLEOCIN Vaginal Cream compared to those receiving placebo (1.1% vs. 0.5% of patients, respectively).
Reproduction studies have been performed in rats and mice using oral and parenteral doses of clindamycin up to 600 mg/kg/day (62 and 25 times, respectively, the maximum human dose based on body surface area) and have revealed no evidence of harm to the fetus due to clindamycin. Cleft palates were observed in fetuses from one mouse strain treated intraperitoneally with clindamycin at 200 mg/kg/day (about 10 times the recommended dose based on body surface area conversions). Since this effect was not observed in other mouse strains or in other species, the effect may be strain specific.
Nursing Mothers
Clindamycin has been detected in human milk after oral or parenteral administration. It is not known if clindamycin is excreted in human milk following the use of vaginally administered clindamycin phosphate.
Because of the potential for serious adverse reactions in nursing infants from clindamycin phosphate, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
The safety and efficacy of CLEOCIN Vaginal Ovules in the treatment of bacterial vaginosis in post-menarchal females have been established on the extrapolation of clinical trial data from adult women. When a post-menarchal adolescent presents to a health professional with bacterial vaginosis symptoms, a careful evaluation for sexually transmitted diseases and other risk factors for bacterial vaginosis should be considered. The safety and efficacy of CLEOCIN Vaginal Ovules in pre-menarchal females have not been established.
-
ADVERSE REACTIONS
Clinical Trials
In clinical trials, 3 (0.5%) of 589 nonpregnant women who received treatment with CLEOCIN Vaginal Ovules discontinued therapy due to drug-related adverse events. Adverse events judged to have a reasonable possibility of having been caused by clindamycin phosphate vaginal suppositories were reported for 10.5% of patients. Events reported by 1% or more of patients receiving CLEOCIN Vaginal Ovules were as follows:
Urogenital system: Vulvovaginal disorder (3.4%), vaginal pain (1.9%), and vaginal moniliasis (1.5%).
Body as a whole: Fungal infection (1.0%).
Other events reported by <1% of patients included:
Urogenital system: Menstrual disorder, dysuria, pyelonephritis, vaginal discharge, and vaginitis/vaginal infection.
Body as a whole: Abdominal cramps, localized abdominal pain, fever, flank pain, generalized pain, headache, localized edema, and moniliasis.
Digestive system: Diarrhea, nausea, and vomiting.
Skin: Nonapplication-site pruritis, rash, application-site pain, and application-site pruritis.
Other clindamycin formulations
The overall systemic exposure to clindamycin from CLEOCIN Vaginal Ovules is substantially lower than the systemic exposure from therapeutic doses of oral clindamycin hydrochloride (two-fold to 20-fold lower) or parenteral clindamycin phosphate (40-fold to 50-fold lower). (See CLINICAL PHARMACOLOGY.) Although these lower levels of exposure are less likely to produce the common reactions seen with oral or parenteral clindamycin, the possibility of these and other reactions cannot be excluded.
The following adverse reactions and altered laboratory tests have been reported with the oral or parenteral use of clindamycin and may also occur following administration of CLEOCIN Vaginal Ovules:
Gastrointestinal: Abdominal pain, esophagitis, nausea, vomiting, diarrhea, and pseudomembranous colitis. (See WARNINGS.)
Hematopoietic: Transient neutropenia (leukopenia), eosinophilia, agranulocytosis, and thrombocytopenia have been reported. No direct etiologic relationship to concurrent clindamycin therapy could be made in any of these reports.
Hypersensitivity Reactions: Maculopapular rash and urticaria have been observed during drug therapy. Generalized mild to moderate morbilliform-like skin rashes are the most frequently reported of all adverse reactions. Rare instances of erythema multiforme, some resembling Stevens-Johnson syndrome, have been associated with clindamycin. A few cases of anaphylactoid reactions have been reported. If a hypersensitivity reaction occurs, the drug should be discontinued.
Liver: Jaundice and abnormalities in liver function tests have been observed during clindamycin therapy.
Musculoskeletal: Rare instances of polyarthritis have been reported.
Renal: Although no direct relationship of clindamycin to renal damage has been established, renal dysfunction as evidenced by azotemia, oliguria, and/or proteinuria has been observed in rare instances.
There have been reports of pseudomembranous colits following the administration of clindamycin vaginal cream.
-
OVERDOSAGE
Vaginally applied clindamycin phosphate contained in CLEOCIN Vaginal Ovules could be absorbed in sufficient amounts to produce systemic effects. (See WARNINGS and ADVERSE REACTIONS.)
- DOSAGE AND ADMINISTRATION
-
HOW SUPPLIED
CLEOCIN Vaginal Ovules are supplied as follows:
Carton of three suppositories with one applicator NDC: 0009-7667-01 - SPL UNCLASSIFIED SECTION
-
Cleocin® Vaginal Ovules(clindamycin phosphate vaginal suppositories)
FOR INTRAVAGINAL USE ONLY
DIRECTIONS FOR USE
How do I use CLEOCIN Vaginal Ovules?
For vaginal use only. Do not take by mouth.
Use one CLEOCIN Vaginal Ovule daily, preferably at bedtime, for 3 days in a row.
Do not use this product if the foiled pouches containing vaginal ovules are torn, opened, or incompletely sealed.
Read the full directions below before using.
Insertion with the applicator:
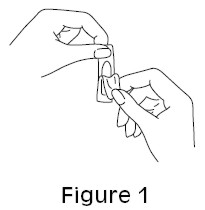
- 1. Remove the vaginal ovule from its packaging. (See Figure 1.)
- 2. Pull back the plunger about an inch and place the vaginal ovule in the wider end of the applicator barrel. (See Figure 2.)
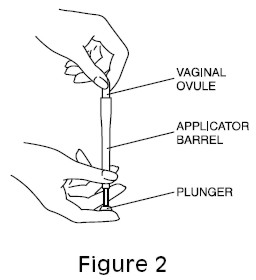
- 3. Hold the applicator as shown and gently insert the end of the applicator into the vagina as far as it will go comfortably. This can be done while lying on your back with your knees bent (as shown in Figure 3), or while standing with your feet apart and your knees bent.
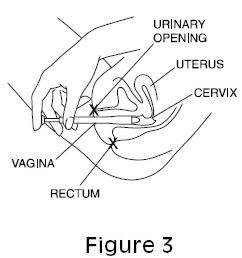
- 4. While holding the barrel of the applicator in place, push the plunger in until it stops to release the vaginal ovule. Remove the applicator from the vagina.
- 5. Clean the applicator after each use. Pull the two pieces apart and wash them with soap and warm water. Rinse well and dry. Put the two pieces back together and store in a clean, dry place.
- 6. Once inside the vagina, the ovule melts. Lie down as soon as possible. This will keep leakage to a minimum.
- 7. Repeat steps 1 through 6, before bedtime, for the next 2 days.
Insertion without the applicator:
- Remove the vaginal ovule from its packaging. (See Figure 1.)
- Holding the ovule with your thumb and a finger, insert it into the vagina.
- Using your finger, gently push the ovule into the vagina as far as it will comfortably go.
- Once inside the vagina, the ovule melts. Lie down as soon as possible. This will keep leakage to a minimum.
- Repeat steps 1 through 4, before bedtime, for the next 2 days.
STORAGE CONDITIONS:
Store at 25°C (77°F); excursions permitted to 15 – 30°C (59 – 86°F) [see USP Controlled Room Temperature]. Caution: Avoid heat over 30°C (86°F). Avoid high humidity. See end of carton for the lot number and expiration date.
LAB-0649-1.0
December 2012 - PRINCIPAL DISPLAY PANEL - 100 mg Blister Pack
-
PRINCIPAL DISPLAY PANEL - 100 mg Blister Pack Carton
PROFESSIONAL SAMPLE - NOT FOR SALE
NDC: 63539-011-01
Pfizer
Cleocin®
Vaginal Ovulesequivalent to
100 mg*
clindamycin(clindamycin phosphate
vaginal suppositories)For Intravaginal Use Only
3 Suppositories with one applicator
-
INGREDIENTS AND APPEARANCE
CLEOCIN
clindamycin phosphate suppositoryProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 63539-011 Route of Administration VAGINAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CLINDAMYCIN PHOSPHATE (UNII: EH6D7113I8) (CLINDAMYCIN - UNII:3U02EL437C) CLINDAMYCIN 100 mg Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 63539-011-01 1 in 1 CARTON 08/13/1999 1 3 in 1 BLISTER PACK; Type 1: Convenience Kit of Co-Package Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA050767 08/13/1999 Labeler - U.S. Pharmaceuticals (829076905) Establishment Name Address ID/FEI Business Operations Pharmacia and Upjohn Company LLC 618054084 ANALYSIS(63539-011) , API MANUFACTURE(63539-011) , LABEL(63539-011) , MANUFACTURE(63539-011) , PACK(63539-011)
Trademark Results [Cleocin]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 CLEOCIN 72102073 0711448 Live/Registered |
UPJOHN COMPANY, THE 1960-08-04 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.