ATELVIA- risedronate sodium tablet, delayed release
Atelvia by
Drug Labeling and Warnings
Atelvia by is a Prescription medication manufactured, distributed, or labeled by Allergan, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use ATELVIA safely and effectively. See full prescribing information for ATELVIA.
ATELVIA® (risedronate sodium) delayed-release tablets
Initial U.S. Approval: 1998
INDICATIONS AND USAGE
DOSAGE AND ADMINISTRATION
One 35 mg delayed-release tablet once-a-week (2.1)
Instruct patients to:
DOSAGE FORMS AND STRENGTHS
Delayed-release tablets: 35 mg (3)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
-
Products Containing Same Active Ingredient: Patients receiving Actonel should not be treated with Atelvia (5.1)
-
Upper Gastrointestinal Adverse Reactions can occur. Instruct patients to follow dosing instructions. Discontinue use if new or worsening symptoms occur (5.2)
-
Hypocalcemia may worsen and must be corrected prior to use (5.3)
-
Osteonecrosis of the Jaw has been reported (5.4)
-
Severe Bone, Joint, Muscle Pain may occur. Discontinue use if severe symptoms develop (5.5, 6.2)
- Atypical Femur Fractures have been reported. Patients with new thigh or groin pain should be evaluated to rule out a femoral fracture (5.6)
ADVERSE REACTIONS
Most common adverse reactions (greater than 5%) include: diarrhea, influenza, arthralgia, back pain, and abdominal pain (6.1)
Hypersensitivity reactions (angioedema, generalized rash, bullous skin reactions, Stevens-Johnson syndrome, and toxic epidermal necrolysis), and eye inflammation (iritis, uveitis) have been reported rarely (6.2)
To report SUSPECTED ADVERSE REACTIONS, contact ALLERGAN USA, Inc at 1-800-678-1605 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.DRUG INTERACTIONS
USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 4/2015
-
Products Containing Same Active Ingredient: Patients receiving Actonel should not be treated with Atelvia (5.1)
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
1.1 Postmenopausal Osteoporosis
1.2 Important Limitations of Use
2 DOSAGE AND ADMINISTRATION
2.1 Treatment of Postmenopausal Osteoporosis
2.2 Important Administration Instructions
2.3 Recommendations for Calcium and Vitamin D Supplementation
2.4 Administration Instructions for Missed Doses
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Drug Products with the Same Active Ingredient
5.2 Upper Gastrointestinal Adverse Reactions
5.3 Mineral Metabolism
5.4 Jaw Osteonecrosis
5.5 Musculoskeletal Pain
5.6 Atypical Subtrochanteric and Diaphyseal Femoral Fractures
5.7 Renal Impairment
5.8 Laboratory Test Interactions
6 ADVERSE REACTIONS
6.1 Clinical Studies Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Calcium Supplements/Antacids
7.2 Histamine 2 (H2) Blockers and Proton Pump Inhibitors (PPIs)
7.3 Hormone Therapy
7.4 Aspirin/Nonsteroidal Anti-Inflammatory Drugs
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
13.2 Animal Toxicology and/or Pharmacology
14 CLINICAL STUDIES
14.1 Treatment of Osteoporosis in Postmenopausal Women
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1
INDICATIONS AND USAGE
1.1 Postmenopausal Osteoporosis
Atelvia is indicated for the treatment of osteoporosis in postmenopausal women. In postmenopausal women, risedronate sodium has been shown to reduce the incidence of vertebral fractures and a composite endpoint of nonvertebral osteoporosis-related fractures [see Clinical Studies (14.1)].
1.2 Important Limitations of Use
The optimal duration of use has not been determined. The safety and effectiveness of Atelvia for the treatment of osteoporosis are based on clinical data of one year duration. All patients on bisphosphonate therapy should have the need for continued therapy re-evaluated on a periodic basis. Patients at low-risk for fracture should be considered for drug discontinuation after 3 to 5 years of use. Patients who discontinue therapy should have their risk for fracture re-evaluated periodically.
-
2
DOSAGE AND ADMINISTRATION
2.1 Treatment of Postmenopausal Osteoporosis
[see Indications and Usage (1.1)]
The recommended regimen is:
- one 35 mg delayed-release tablet orally, taken once-a-week
2.2 Important Administration Instructions
Instruct patients to do the following:
- Take Atelvia in the morning immediately following breakfast. Atelvia should be taken immediately following breakfast and not under fasting conditions because of a higher risk of abdominal pain if taken before breakfast when fasting.
- Swallow Atelvia whole while in an upright position and with at least 4 ounces of plain water to facilitate delivery to the stomach. Avoid lying down for 30 minutes after taking the medication [see Warnings and Precautions (5.2)].
- Do not chew, cut, or crush Atelvia tablets.
2.3 Recommendations for Calcium and Vitamin D Supplementation
Instruct patients to take supplemental calcium and vitamin D if dietary intake is inadequate [see Warnings and Precautions (5.3)] and to take calcium supplements, antacids, magnesium-based supplements or laxatives, and iron preparations at a different time of the day as they interfere with the absorption of Atelvia.
- 3 DOSAGE FORMS AND STRENGTHS
-
4
CONTRAINDICATIONS
Atelvia is contraindicated in patients with the following conditions:
Abnormalities of the esophagus which delay esophageal emptying such as stricture or achalasia [see Warnings and Precautions (5.2)]
Inability to stand or sit upright for at least 30 minutes [see Dosage and Administration (2), Warnings and Precautions (5.2)]
Hypocalcemia [see Warnings and Precautions (5.3)]
Known hypersensitivity to any component of this product. Angioedema, generalized rash, bullous skin reactions, Stevens-Johnson syndrome and toxic epidermal necrolysis , have been reported [see Adverse Reactions (6.2)]
-
5
WARNINGS AND PRECAUTIONS
5.1 Drug Products with the Same Active Ingredient
Atelvia contains the same active ingredient found in Actonel®. A patient being treated with Actonel should not receive Atelvia.
5.2 Upper Gastrointestinal Adverse Reactions
Atelvia, like other bisphosphonates administered orally, may cause local irritation of the upper gastrointestinal mucosa. Because of these possible irritant effects and a potential for worsening of the underlying disease, caution should be used when Atelvia is given to patients with active upper gastrointestinal problems (such as known Barrett’s esophagus, dysphagia, other esophageal diseases, gastritis, duodenitis or ulcers) [see Contraindications (4), Adverse Reactions (6.1), Information for Patients (17)].
Esophageal adverse experiences, such as esophagitis, esophageal ulcers and esophageal erosions, occasionally with bleeding and rarely followed by esophageal stricture or perforation, have been reported in patients receiving treatment with oral bisphosphonates. In some cases, these have been severe and required hospitalization. Physicians should therefore be alert to any signs or symptoms signaling a possible esophageal reaction and patients should be instructed to discontinue Atelvia and seek medical attention if they develop dysphagia, odynophagia, retrosternal pain or new or worsening heartburn.
The risk of severe esophageal adverse experiences appears to be greater in patients who lie down after taking oral bisphosphonates and/or who fail to swallow it with the recommended 4 ounces of water, and/or who continue to take oral bisphosphonates after developing symptoms suggestive of esophageal irritation. Therefore, it is very important that the full dosing instructions are provided to, and understood by, the patient [see Dosage and Administration (2)]. In patients who cannot comply with dosing instructions due to mental disability, therapy with Atelvia should be used under appropriate supervision.
There have been post-marketing reports of gastric and duodenal ulcers with oral bisphosphonate use, some severe and with complications, although no increased risk was observed in controlled clinical trials.
5.3 Mineral Metabolism
Hypocalcemia has been reported in patients taking Atelvia. Treat hypocalcemia and other disturbances of bone and mineral metabolism should be effectively treated before starting Atelvia therapy. Instruct patients to take supplemental calcium and vitamin D if their dietary intake is inadequate. Adequate intake of calcium and vitamin D is important in all patients [see Contraindications (4), Adverse Reactions (6.1), Information for Patients (17)].
5.4 Jaw Osteonecrosis
Osteonecrosis of the jaw (ONJ), which can occur spontaneously, is generally associated with tooth extraction and/or local infection with delayed healing, and has been reported in patients taking bisphosphonates, including risedronate. Known risk factors for osteonecrosis of the jaw include invasive dental procedures (for example, tooth extraction, dental implants, boney surgery), diagnosis of cancer, concomitant therapies (for example, chemotherapy, corticosteroids, angiogenesis inhibitors), poor oral hygiene, and co-morbid disorders (for example, periodontal and/or other pre-existing dental disease, anemia, coagulopathy, infection, ill-fitting dentures). The risk of ONJ may increase with duration of exposure to bisphosphonates.
For patients requiring invasive dental procedures, discontinuation of bisphosphonate treatment may reduce the risk for ONJ. Clinical judgment of the treating physician and/or oral surgeon should guide the management plan of each patient based on individual benefit/risk assessment.
Patients who develop ONJ while on bisphosphonate therapy should receive care by an oral surgeon. In these patients, extensive dental surgery to treat ONJ may exacerbate the condition. Discontinuation of bisphosphonate therapy should be considered based on individual benefit/risk assessment [see Adverse Reactions (6.2)].
5.5 Musculoskeletal Pain
In postmarketing experience, there have been reports of severe and occasionally incapacitating bone, joint, and/or muscle pain in patients taking bisphosphonates [see Adverse Reactions (6.2)]. The time to onset of symptoms varied from one day to several months after starting the drug. Most patients had relief of symptoms after stopping medication. A subset had recurrence of symptoms when rechallenged with the same drug or another bisphosphonate. Consider discontinuing use if severe symptoms develop.
5.6 Atypical Subtrochanteric and Diaphyseal Femoral Fractures
Atypical, low-energy, or low trauma fractures of the femoral shaft have been reported in bisphosphonate-treated patients. These fractures can occur anywhere in the femoral shaft from just below the lesser trochanter to above the supracondylar flare and are traverse or short oblique in orientation without evidence of comminution. Causality has not been established as these fractures also occur in osteoporotic patients who have not been treated with bisphosphonates.
Atypical femur fractures most commonly occur with minimal or no trauma to the affected area. They may be bilateral and many patients report prodromal pain in the affected area, usually presenting as dull, aching thigh pain, weeks to months before a complete fracture occurs. A number of reports note that patients were also receiving treatment with glucocorticoids (for example, prednisone) at the time of fracture.
Any patient with a history of bisphosphonate exposure who presents with thigh or groin pain should be suspected of having an atypical fracture and should be evaluated to rule out an incomplete femur fracture. Patients presenting with an atypical fracture should also be assessed for symptoms and signs of fracture in the contralateral limb. Interruption of bisphosphonate therapy should be considered, pending a risk/benefit assessment, on an individual basis.
-
6
ADVERSE REACTIONS
6.1 Clinical Studies Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Treatment of Postmenopausal Osteoporosis
Once-a-Week Dosing with Atelvia (risedronate sodium) delayed-release tablets
The safety of Atelvia 35 mg once-a-week in the treatment of postmenopausal osteoporosis was assessed in a 1-year, double-blind, multicenter study comparing Atelvia 35 mg once-a-week to risedronate sodium immediate-release 5 mg daily in postmenopausal women 50 years of age or older. Atelvia was administered either at least 30 minutes before (N = 308) or immediately following (N = 307) breakfast, and risedronate sodium immediate-release 5 mg daily (N = 307) was administered at least 30 minutes before breakfast. Patients with pre-existing gastrointestinal disease and concomitant use of non-steroidal anti-inflammatory drugs, proton pump inhibitors, and H2 antagonists were included in this clinical trial. All women received daily supplementation with 1000 mg of elemental calcium plus 800 to 1000 international units vitamin D. As treatment with Atelvia resulted in a significantly higher incidence of abdominal pain when administered before breakfast under fasting conditions, safety results that follow refer only to Atelvia 35 mg once-a-week immediately following breakfast and risedronate sodium immediate-release 5 mg daily.
The incidence of all-cause mortality was 0.0% in the Atelvia 35 mg once-a-week group and 0.3% in the risedronate sodium immediate-release 5 mg daily group. The incidence of serious adverse reactions was 6.5% in the Atelvia 35 mg once-a-week group and 7.2% in the risedronate sodium immediate-release 5 mg daily group. The percentage of patients who withdrew from the study due to adverse reactions was 9.1% in the Atelvia 35 mg once-a-week group and 8.1% in the risedronate sodium immediate-release 5 mg daily group. The overall safety and tolerability profiles of the two dosing regimens were similar. Table 1 lists adverse reactions reported in greater than or equal to 2% of patients. Adverse reactions are shown without attribution of causality.
Table 1 Adverse Reactions Occurring at a Frequency of greater than or equal to 2% in Either Treatment Group 35 mg
Atelvia5 mg
Risedronate sodium
Immediate- releaseWeekly Daily System Organ Class N = 307 N = 307 Preferred Term % % Gastrointestinal disorders Diarrhea 8.8 4.9 Abdominal pain 5.2 2.9 Constipation 4.9 2.9 Vomiting 4.9 1.6 Dyspepsia 3.9 3.9 Nausea 3.6 3.9 Abdominal pain upper 2.9 2.3 Infections and infestations Influenza 7.2 6.2 Bronchitis 3.9 4.2 Upper respiratory tract infection 3.6 2.6 Musculoskeletal and connective tissue disorders Arthralgia 6.8 7.8 Back pain 6.8 5.9 Pain in extremity 3.9 2.3 Musculoskeletal pain 2.0 1.6 Muscle spasms 1.0 2.3 Nervous system disorders Dizziness 2.6 3.3 Headache 2.6 4.9 Acute Phase Reactions: Symptoms consistent with acute phase reaction have been reported with bisphosphonate use. The overall incidence of acute phase reaction was 2.3% in the Atelvia 35 mg once-a-week group and 1.3% in the risedronate sodium immediate-release 5 mg daily group. These incidence rates are based on reporting of one or more pre-specified acute phase reaction-like symptoms within 3 days of the first dose and for a duration of 7 days or less.
Gastrointestinal Adverse Reactions: Adverse reactions related to the upper gastrointestinal tract occurred in 16% of subjects treated with Atelvia 35 mg once-a-week and 15% of subjects treated with risedronate sodium immediate-release 5 mg daily. The incidence of upper gastrointestinal tract adverse reactions in the Atelvia 35 mg once-a-week and risedronate sodium immediate-release 5 mg daily groups were: abdominal pain (5.2% versus 2.9%), dyspepsia (3.9% versus 3.9%), upper abdominal pain (2.9% versus 2.3%), gastritis (1.0% versus 1.0%), and gastroesophageal reflux disease (1.0% versus 1.6%). Study discontinuation due to abdominal pain occurred in 1.3% of the Atelvia 35 mg once-a-week group and 0.7% of the risedronate sodium immediate-release 5 mg daily group.
Musculoskeletal Adverse Reactions: Selected musculoskeletal adverse reactions were reported in 16% of subjects treated with Atelvia 35 mg once-a-week and 15% of subjects treated with risedronate sodium immediate-release 5 mg daily. The incidence of musculoskeletal adverse reactions in the Atelvia 35 mg once-a-week and risedronate sodium immediate-release 5 mg daily groups were: arthralgia (6.8% versus 7.8%), back pain (6.8% versus 5.9%), musculoskeletal pain (2.0% versus 1.6%), and myalgia (1.3% versus 1.0%).
Laboratory Test Findings:
Parathyroid hormone: The effect of Atelvia 35 mg once-a-week and risedronate sodium immediate-release 5 mg daily on parathyroid hormone was evaluated in postmenopausal women with osteoporosis. At week 52, in subjects with normal levels at baseline, PTH levels greater than 65 pg/mL (upper limit of normal) were noted in 9% of subjects receiving Atelvia 35 mg once-a-week and 8% of subjects receiving risedronate sodium immediate-release 5 mg daily. In subjects with normal levels at baseline, PTH levels greater than 97 pg/mL (1.5 times the upper limit of normal) were seen in 2% of subjects receiving Atelvia 35 mg once-a-week and no subjects receiving risedronate sodium immediate-release 5 mg daily. There were no clinically significant differences between treatment groups for levels of calcium, phosphorus and magnesium.
Daily Dosing with risedronate sodium immediate-release 5 mg tablets
The safety of risedronate sodium immediate-release 5 mg once daily in the treatment of postmenopausal osteoporosis was assessed in four randomized, double-blind, placebo-controlled multinational trials of 3232 women aged 38 to 85 years with postmenopausal osteoporosis. The duration of the trials was up to three years, with 1619 patients exposed to placebo and 1613 patients exposed to risedronate sodium immediate-release 5 mg daily. Patients with pre-existing gastrointestinal disease and concomitant use of non-steroidal anti-inflammatory drugs, proton pump inhibitors (PPIs), and H2 antagonists were included in these clinical trials. All women received 1000 mg of elemental calcium plus vitamin D supplementation up to 500 international units per day if their 25-hydroxyvitamin D3 level was below normal at baseline.
The incidence of all-cause mortality was 2.0% in the placebo group and 1.7% in the risedronate sodium immediate-release 5 mg daily group. The incidence of serious adverse reactions was 24.6% in the placebo group and 27.2% in the risedronate sodium immediate-release 5 mg daily group. The percentage of patients who withdrew from the study due to adverse reactions was 15.6% in the placebo group and 14.8% in the risedronate sodium immediate-release 5 mg daily group. The most common adverse reactions reported in greater than 10% of subjects were: back pain, arthralgia, abdominal pain and dyspepsia.
Gastrointestinal Adverse Reactions: The incidence of adverse reactions in the placebo and risedronate sodium immediate-release 5 mg daily groups were: abdominal pain (9.9% versus 12.2%), diarrhea (10.0% versus 10.8%), dyspepsia (10.6% versus 10.8%), and gastritis (2.3% versus 2.7%). Duodenitis and glossitis have been reported uncommonly in the risedronate sodium immediate-release 5 mg daily group (0.1% to 1%). In patients with active upper gastrointestinal disease at baseline, the incidence of upper gastrointestinal adverse reactions was similar between the placebo and risedronate sodium immediate-release 5 mg daily groups.
Musculoskeletal Adverse Reactions: The incidence of adverse reactions in the placebo and risedronate sodium immediate-release 5 mg daily groups were: back pain (26.1% versus 28.0%), arthralgia (22.1% versus 23.7%), myalgia (6.2% versus 6.7%), and bone pain (4.8% versus 5.3%).
Laboratory Test Findings: Throughout the Phase 3 studies, transient decreases from baseline in serum calcium (less than 1%) and serum phosphate (less than 3%) and compensatory increases in serum PTH levels (less than 30%) were observed within 6 months in patients in osteoporosis clinical trials treated with risedronate sodium immediate-release 5 mg daily. There were no significant differences in serum calcium, phosphate, or PTH levels between placebo and risedronate sodium immediate-release 5 mg daily at 3 years. Serum calcium levels below 8 mg/dL were observed in 18 patients, 9 (0.5%) in each treatment arm (placebo and risedronate sodium immediate-release 5 mg daily). Serum phosphorus levels below 2 mg/dL were observed in 14 patients, 3 (0.2%) treated with placebo and 11 (0.6%) treated with risedronate sodium immediate-release 5 mg daily. There have been rare reports (less than 0.1%) of abnormal liver function tests.
Endoscopic Findings: In the risedronate sodium immediate-release 5 mg daily clinical trials, endoscopic evaluation was encouraged in any patient with moderate-to-severe gastrointestinal complaints, while maintaining the blind. Endoscopies were performed on equal numbers of patients between the placebo and treated groups [75 (14.5%) placebo; 75 (11.9%) risedronate sodium immediate-release 5 mg daily]. Clinically important findings (perforations, ulcers, or bleeding) among this symptomatic population were similar between groups (51% placebo; 39% risedronate sodium immediate-release 5 mg daily).
6.2 Postmarketing Experience
The following adverse reactions have been reported with the use of Atelvia. Because these adverse reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Hypersensitivity Reactions
Hypersensitivity and skin reactions have been reported, including angioedema, generalized rash, bullous skin reactions, Stevens-Johnson syndrome and toxic epidermal necrolysis.
Gastrointestinal Adverse Reactions
Reactions involving upper gastrointestinal irritation, such as esophagitis and esophageal or gastric ulcers, have been reported [see Warnings and Precautions (5.2)].
Musculoskeletal Pain
Bone, joint, or muscle pain, described as severe or incapacitating, have been reported rarely [see Warnings and Precautions (5.5)].
Eye Inflammation
Reactions of eye inflammation including iritis and uveitis have been reported rarely.
Jaw Osteonecrosis
Osteonecrosis of the jaw has been reported rarely [see Warnings and Precautions (5.4)].
Pulmonary
Asthma exacerbations
-
7
DRUG INTERACTIONS
Risedronate is not metabolized and does not induce or inhibit hepatic microsomal drug-metabolizing enzymes (for example, Cytochrome P450).
7.1 Calcium Supplements/Antacids
When Atelvia was administered following breakfast, the co-administration of a tablet containing 600 mg of elemental calcium and 400 international units vitamin D reduced risedronate bioavailability by approximately 38% [see Clinical Pharmacology (12.3)]. Calcium supplements, antacids, magnesium-based supplements or laxatives, and iron preparations interfere with the absorption of Atelvia and should not be taken together.
7.2 Histamine 2 (H2) Blockers and Proton Pump Inhibitors (PPIs)
Drugs that raise stomach pH (for example, PPIs or H2 blockers) may cause faster drug release from enteric coated (delayed-release) drug products such as Atelvia. Co-administration of Atelvia with the PPI, esomeprazole, increased risedronate bioavailability. The maximum plasma concentration (Cmax) and the area under the plasma concentration (AUC) were increased by 60 percent and 22 percent, respectively.
Concomitant administration of Atelvia and H2 blockers or PPIs is not recommended.
7.3 Hormone Therapy
Concomitant use of Atelvia with estrogens and estrogen agonist/antagonists has not been studied.
7.4 Aspirin/Nonsteroidal Anti-Inflammatory Drugs
In the Phase 3 study comparing Atelvia 35 mg once-a-week immediately following breakfast and risedronate sodium 5 mg daily, 18% of NSAID users (any use) in both groups developed upper gastrointestinal adverse reactions. Among non-users, 13% of patients taking Atelvia 35 mg once-a-week immediately following breakfast developed upper gastrointestinal adverse reactions, compared to 12% taking risedronate sodium 5 mg daily.
-
8
USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category C: There are no adequate and well-controlled studies of Atelvia in pregnant women. Atelvia should be used during pregnancy only if the potential benefit justifies the potential risk to the mother and fetus.
Bisphosphonates are incorporated into the bone matrix, from which they are gradually released over periods of weeks to years. The amount of bisphosphonate incorporation into adult bone, and hence, the amount available for release back into the systemic circulation, is directly related to the dose and duration of bisphosphonate use. There are no data on fetal risk in humans. However, there is a theoretical risk of fetal harm, predominantly skeletal, if a woman becomes pregnant after completing a course of bisphosphonate therapy. The impact of variables such as time between cessation of bisphosphonate therapy to conception, the particular bisphosphonate used, and the route of administration (intravenous versus oral) on this risk has not been studied.
In animal studies, pregnant rats received risedronate sodium during organogenesis at doses 1 to 26 times the human Paget’s disease dose of 30 mg/day. Survival of neonates was decreased in rats treated during gestation with oral doses approximately 5 times the human dose and body weight was decreased in neonates from dams treated with approximately 26 times the human dose. The number of fetuses exhibiting incomplete ossification of sternebrae or skull from dams treated with approximately 2.5 times the human dose was significantly increased compared to controls. Both incomplete ossification and unossified sternebrae were increased in rats treated with oral doses approximately 5 times the human dose. A low incidence of cleft palate was observed in fetuses from female rats treated with oral doses approximately equal to the human dose. The relevance of this finding to human use of Atelvia is unclear.
No significant fetal ossification effects were seen in rabbits treated with oral doses approximately 7 times the human dose (the highest dose tested). However, 1 of 14 litters were aborted and 1 of 14 litters were delivered prematurely.
Similar to other bisphosphonates, treatment during mating and gestation with doses of risedronate sodium approximately the same as the human Paget’s disease dose of 30 mg/day resulted in periparturient hypocalcemia and mortality in pregnant rats allowed to deliver.
Dosing multiples provided above are based on the recommended human Paget’s disease dose of 30 mg/day and normalized using body surface area (mg/m2). Actual animal doses were 3.2, 7.1 and 16 mg/kg/day in the rat and 10 mg/kg/day in the rabbit.
8.3 Nursing Mothers
Risedronate was detected in feeding pups exposed to lactating rats for a 24-hour period post-dosing, indicating a small degree of lacteal transfer. It is not known whether Atelvia is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from Atelvia, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
8.4 Pediatric Use
Atelvia is not indicated for use in pediatric patients.
The safety and effectiveness of risedronate sodium immediate-release was assessed in a one-year, randomized, double-blind, placebo-controlled study of 143 pediatric patients (94 received risedronate) with osteogenesis imperfecta (OI). The enrolled population was predominantly patients with mild OI (85% Type-I), aged 4 to less than 16 years, 50% male and 82% Caucasian, with a mean lumbar spine BMD Z-score of -2.08 (2.08 standard deviations below the mean for age-matched controls). Patients received either a 2.5 mg (less than or equal to 30 kg body weight) or 5 mg (greater than 30 kg body weight) daily oral dose. After one year, an increase in lumbar spine BMD in the risedronate sodium immediate-release group compared to the placebo group was observed. However, treatment with risedronate sodium immediate-release did not result in a reduction in the risk of fracture in pediatric patients with OI. In risedronate sodium immediate-release treated subjects, no mineralization defects were noted in paired bone biopsy specimens obtained at baseline and month 12.
The overall safety profile of risedronate in OI patients treated for up to 12 months was generally similar to that of adults with osteoporosis. However, there was an increased incidence of vomiting compared to placebo. In this study, vomiting was observed in 15% of children treated with risedronate sodium immediate-release and 6% of patients treated with placebo. Other adverse reactions reported in greater than or equal to 10% of patients treated with risedronate sodium immediate-release and with a higher frequency than placebo were: pain in the extremity (21% with risedronate sodium immediate-release versus 16% with placebo), headache (20% versus 8%), back pain (17% versus 10%), pain (15% versus 10%), upper abdominal pain (11% versus 8%), and bone pain (10% versus 4%).
8.5 Geriatric Use
Of the patients receiving Atelvia in postmenopausal osteoporosis studies, 59% were 65 and over, while 13% were 75 and over. No overall differences in safety or effectiveness were observed between these patients and younger patients, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
-
10
OVERDOSAGE
Decreases in serum calcium and phosphorus following substantial overdose may be expected in some patients. Signs and symptoms of hypocalcemia may also occur in some of these patients. While milk or antacids containing calcium may be given to bind risedronate sodium immediate- release and reduce absorption of the drug, the impact of this intervention for Atelvia delayed-release tablets has not been evaluated.
In cases of substantial overdose, gastric lavage may be considered to remove unabsorbed drug. Standard procedures that are effective for treating hypocalcemia, including the administration of calcium intravenously, would be expected to restore physiologic amounts of ionized calcium and to relieve signs and symptoms of hypocalcemia.
Lethality after single oral doses of risedronate was seen in female rats at 903 mg/kg and male rats at 1703 mg/kg. The minimum lethal dose in mice and rabbits was 4000 mg/kg and 1000 mg/kg, respectively. These values represent 320 to 620 times the human Paget’s disease dose of 30 mg/day based on surface area (mg/m2).
-
11
DESCRIPTION
Atelvia (risedronate sodium) delayed-release tablets contain a pH-sensitive enteric coating and a chelating agent (EDTA).
Risedronate is a pyridinyl bisphosphonate that inhibits osteoclast-mediated bone resorption and modulates bone metabolism. Each Atelvia tablet for oral administration contains the equivalent of 35 mg of anhydrous risedronate sodium in the form of the hemi-pentahydrate with small amounts of monohydrate. The empirical formula for risedronate sodium hemi-pentahydrate is C7H10NO7P2Na 2.5 H2O. The chemical name of risedronate sodium is [1-hydroxy-2-(3-pyridinyl)ethylidene]bis[phosphonic acid] monosodium salt. The chemical structure of risedronate sodium hemi-pentahydrate is the following:
![The chemical structure for Risedronate is a pyridinyl bisphosphonate that inhibits osteoclast-mediated bone resorption and modulates bone metabolism. Each Atelvia tablet for oral administration contains the equivalent of 35 mg of anhydrous risedronate sodium in the form of the hemi-pentahydrate with small amounts of monohydrate. The empirical formula for risedronate sodium hemi-pentahydrate is C7H10NO7P2Na 2.5 H2O. The chemical name of risedronate sodium is [1-hydroxy-2-(3-pyridinyl)ethylidene]bis[phosphonic acid] monosodium salt.](https://fda.report/DailyMed/c8b9ab88-1a26-46c3-80ec-4eaa45202021/atelvia-01.jpg)
Molecular Weight:
Anhydrous: 305.10
Hemi-pentahydrate: 350.13
Risedronate sodium is a fine, white to off-white, odorless, crystalline powder. It is soluble in water and in aqueous solutions, and essentially insoluble in common organic solvents.
Inactive Ingredients
Edetate disodium, ferric oxide yellow, magnesium stearate, methacrylic acid copolymer, polysorbate 80, silicified microcrystalline cellulose (ProSolv SMCC90), simethicone, sodium starch glycolate, stearic acid, talc, and triethyl citrate.
-
12
CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Risedronate has an affinity for hydroxyapatite crystals in bone and acts as an antiresorptive agent. At the cellular level, risedronate inhibits osteoclasts. The osteoclasts adhere normally to the bone surface, but show evidence of reduced active resorption (for example, lack of ruffled border). Histomorphometry in rats, dogs, and minipigs showed that risedronate treatment reduces bone turnover (activation frequency, that is, the rate at which bone remodeling sites are activated) and bone resorption at remodeling sites.
12.2 Pharmacodynamics
Risedronate treatment decreases the elevated rate of bone turnover that is typically seen in postmenopausal osteoporosis. In clinical trials, administration of risedronate sodium immediate- release to postmenopausal women resulted in decreases in biochemical markers of bone turnover, including urinary deoxypyridinoline/creatinine and urinary collagen cross-linked N-telopeptide (markers of bone resorption) and serum bone-specific alkaline phosphatase (a marker of bone formation). At the 5 mg daily dose, decreases in deoxypyridinoline/creatinine were evident within 14 days of treatment. Changes in bone formation markers were observed later than changes in resorption markers, as expected, due to the coupled nature of bone resorption and bone formation; decreases in bone-specific alkaline phosphatase of about 20% were evident within 3 months of treatment. Bone turnover markers reached a nadir of about 40% below baseline values by the sixth month of treatment and remained stable with continued treatment for up to 3 years. Bone turnover is decreased as early as 14 days and maximally within about 6 months of treatment, with achievement of a new steady-state that more nearly approximates the rate of bone turnover seen in premenopausal women. In a 1-year study comparing Atelvia 35 mg weekly taken immediately after breakfast versus risedronate sodium immediate-release 5 mg daily oral dosing regimens in postmenopausal women, mean decreases from baseline at 1 year in urinary collagen cross-linked N-telopeptide were 47% in the Atelvia 35 mg once-a-week following breakfast group and 42% in the risedronate sodium immediate-release 5 mg daily group. In addition, serum bone-specific alkaline phosphatase at 1 year was reduced by 33% in the Atelvia 35 mg once-a-week following breakfast group and 32% in the risedronate sodium immediate-release 5 mg daily group.
12.3 Pharmacokinetics
Absorption
The mean absolute oral bioavailability of the 30 mg risedronate sodium immediate-release tablet taken 4 hours prior to a meal is 0.63% (90% confidence interval [CI]: 0.54% to 0.75%) and is similar to an oral solution. The time to peak concentration (Tmax) for Atelvia tablet is approximately 3 hours when administered in the morning 4 hours prior to a meal.
Food Effect
In a crossover pharmacokinetic study, the bioavailability of Atelvia 35 mg delayed-release tablets decreased by approximately 30% when administered immediately after a high-fat breakfast compared to administration in the morning 4 hours before a meal.
The bioavailability of the 35 mg Atelvia tablet administered after a high-fat breakfast was similar to risedronate sodium 35 mg immediate-release tablet dosed 4 hours before a meal in one study and was approximately 2- to 4-fold greater than the immediate-release 35 mg tablet administered 30 minutes prior to a high-fat breakfast.
In a separate study, Atelvia administered after dinner exhibited approximately 87% increase in risedronate exposure compared to administration following a breakfast. The safety and efficacy of dosing Atelvia after dinner has not been evaluated [see Dosage and Administration (2)].
Distribution
The mean steady-state volume of distribution for risedronate is 13.8 L/kg in humans. Human plasma protein binding of drug is about 24%. Preclinical studies in rats and dogs dosed intravenously with single doses of [14C] risedronate indicate that approximately 60% of the dose is distributed to bone. The remainder of the dose is excreted in the urine. After multiple oral dosing in rats, the uptake of risedronate in soft tissues was in the range of 0.001% to 0.01%.
Metabolism
There is no evidence of systemic metabolism of risedronate.
Excretion
In young healthy subjects, approximately half of the absorbed dose of risedronate was excreted in urine within 24 hours, and 85% of an intravenous dose was recovered in the urine over 28 days. Based on simultaneous modeling of serum and urine data for the risedronate sodium immediate-release tablets, mean renal clearance was 105 mL/min (CV = 34%) and mean total clearance was 122 mL/min (CV = 19%), with the difference primarily reflecting nonrenal clearance or clearance due to adsorption to bone. The renal clearance is not concentration dependent, and there is a linear relationship between renal clearance and creatinine clearance. Unabsorbed drug is eliminated unchanged in feces. In osteopenic postmenopausal women, the terminal exponential half-life was 561 hours, mean renal clearance was 52 mL/min (CV = 25%), and mean total clearance was 73 mL/min (CV = 15%).
Specific Populations
Pediatric: Atelvia is not indicated for use in pediatric patients [see Pediatric Use (8.4)].
Geriatric: Effect of age on bioavailability of Atelvia has not been evaluated. Based on data from risedronate immediate-release tablet, bioavailability and disposition of risedronate are similar in elderly (greater than 60 years of age) and younger subjects. No dosage adjustment is necessary.
Race: Pharmacokinetic differences due to race have not been studied. The clinical trial of Atelvia was conducted mostly in Caucasians.
Renal Impairment: Risedronate is excreted unchanged primarily via the kidney. As compared to persons with normal renal function, the renal clearance of risedronate was decreased by about 70% in patients with creatinine clearance of approximately 30 mL/min. Atelvia is not recommended for use in patients with severe renal impairment (creatinine clearance less than 30 mL/min). No dosage adjustment is necessary in patients with a creatinine clearance greater than or equal to 30 mL/min.
Hepatic Impairment: No studies have been performed to assess risedronate’s safety or efficacy in patients with hepatic impairment. Risedronate is not metabolized in rat, dog, and human liver preparations. Insignificant amounts (less than 0.1% of intravenous dose) of drug are excreted in the bile in rats. Therefore, dosage adjustment is unlikely to be needed in patients with hepatic impairment.
Drug Interactions: Risedronate is not metabolized and does not induce or inhibit hepatic microsomal drug-metabolizing enzymes (for example, Cytochrome P450).
Calcium supplement: A Phase 1 single-dose, cross-over study in 101 postmenopausal women evaluated the relative bioavailability of Atelvia 35 mg delayed-release tablets taken after breakfast and following a 600 mg elemental calcium/400 international units vitamin D supplement, compared to Atelvia alone taken after breakfast without calcium or vitamin D supplementation. The addition of the calcium/vitamin D supplement following the meal resulted in an approximate 38% reduction in the amount of risedronate absorbed [see Drug Interactions (7)].
Proton Pump Inhibitors: A Phase 1, 2-period, cross-over study in 60 healthy postmenopausal female subjects evaluated the relative bioavailability of a single dose Atelvia 35 mg delayed-release tablet taken after breakfast following 6 days of esomeprazole magnesium delayed release 40 mg capsules. On Day 6, esomeprazole 40 mg capsule was administered with 240 mL water one hour before breakfast and Atelvia 35 mg tablet was administered with 240 mL water within 10 minutes after a standard breakfast. The Cmax and AUCinf of risedronate were increased by 60 percent and 22 percent, respectively, in presence of esomeprazole.
-
13
NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
In a 104-week carcinogenicity study, rats were administered daily oral doses up to approximately 8 times the human Paget’s disease dose of 30 mg/day. There were no significant drug-induced tumor findings in male or female rats. The high dose male group was terminated early in the study (Week 93) due to excessive toxicity, and data from this group were not included in the statistical evaluation of the study results. In an 80-week carcinogenicity study, mice were administered daily oral doses approximately 6.5 times the human dose. There were no significant drug-induced tumor findings in male or female mice.
Mutagenesis
Risedronate did not exhibit genetic toxicity in the following assays: In vitro bacterial mutagenesis in Salmonella and E. coli (Ames assay), mammalian cell mutagenesis in CHO/HGPRT assay, unscheduled DNA synthesis in rat hepatocytes and an assessment of chromosomal aberrations in vivo in rat bone marrow. Risedronate was positive in a chromosomal aberration assay in CHO cells at highly cytotoxic concentrations (greater than 675 mcg/mL, survival of 6% to 7%). When the assay was repeated at doses exhibiting appropriate cell survival (29%), there was no evidence of chromosomal damage.
Impairment of Fertility
In female rats, ovulation was inhibited at an oral dose approximately 5 times the human dose. Decreased implantation was noted in female rats treated with doses approximately 2.5 times the human dose. In male rats, testicular and epididymal atrophy and inflammation were noted at approximately 13 times the human dose. Testicular atrophy was also noted in male rats after 13 weeks of treatment at oral doses approximately 5 times the human dose. There was moderate-to-severe spermatid maturation block after 13 weeks in male dogs at an oral dose approximately 8 times the human dose. These findings tended to increase in severity with increased dose and exposure time.
Dosing multiples provided above are based on the recommended human Paget’s disease dose of 30 mg/day and normalized using body surface area (mg/m2). Actual doses were 24 mg/kg/day in rats, 32 mg/kg/day in mice, and 8, 16 and 40 mg/kg/day in dogs.
13.2 Animal Toxicology and/or Pharmacology
Risedronate demonstrated potent anti-osteoclast, antiresorptive activity in ovariectomized rats and minipigs. Bone mass and biomechanical strength were increased dose-dependently at daily oral doses up to 4 and 25 times the recommended human dose of 5 mg/day for rats and minipigs, respectively. Risedronate treatment maintained the positive correlation between BMD and bone strength and did not have a negative effect on bone structure or mineralization. In intact dogs, risedronate induced positive bone balance at the level of the bone remodeling unit at oral doses ranging from 0.5 to 1.5 times the human dose of 5 mg/day.
In dogs treated with an oral dose approximately 5 times the human dose of 5 mg/day, risedronate caused a delay in fracture healing of the radius. The observed delay in fracture healing is similar to other bisphosphonates. This effect did not occur at a dose approximately 0.5 times the human daily dose.
The Schenk rat assay, based on histologic examination of the epiphyses of growing rats after drug treatment, demonstrated that risedronate did not interfere with bone mineralization even at the highest dose tested, which was approximately 3500 times the lowest antiresorptive dose in this model (1.5 mcg/kg/day) and approximately 800 times the human dose of 5 mg/day. This indicates that Atelvia administered at the therapeutic dose is unlikely to induce osteomalacia.
Dosing multiples provided above are based on the recommended human osteoporosis dose of 5 mg/day and normalized using body surface area (mg/m2).
-
14
CLINICAL STUDIES
14.1 Treatment of Osteoporosis in Postmenopausal Women
The efficacy of Atelvia 35 mg once-a-week in the treatment of postmenopausal osteoporosis was demonstrated in a randomized, double-blind, active-control trial of approximately 900 subjects. All patients in this study received supplemental calcium (1000 mg/day) and vitamin D (800 to 1000 international units/day). The primary efficacy endpoint was percent change in lumbar spine bone mineral density at 1 year.
Atelvia 35 mg once-a-week administered after breakfast was shown to be non-inferior to risedronate sodium immediate-release 5 mg daily. Table 2 presents the primary efficacy analysis, percent change in lumbar spine BMD, in the intent-to-treat population with last observation carried forward (LOCF).
Table 2 Lumbar Spine BMD - Percent Change from Baseline at Endpoint[a] Risedronate sodium immediate-release
5 mg DailyAtelvia
35 mg Once-a-Week
Following Breakfast
N = 307 N = 307 Primary Efficacy (LOCF) n 270 261 LS Mean (95% CI) 3.1* (2.7, 3.5) 3.3* (2.9, 3.7) LS Mean Difference[b] (95% CI) -0.2 (-0.8, 0.3) N = number of intent-to-treat patients within specified treatment; n = number of patients with values at the visit.
*Indicates a statistically significant difference from baseline determined from 95% CI unadjusted for multiple comparisons.
LS = Least Squares
[a] at 1 year LOCF
[b] LS Mean Difference is 5 mg daily minus 35 mg weekly treatment.Fracture efficacy with risedronate sodium immediate-release 5 mg daily
The fracture efficacy of risedronate sodium immediate-release 5 mg daily in the treatment of postmenopausal osteoporosis was demonstrated in 2 large, randomized, placebo-controlled, double-blind studies that enrolled a total of almost 4000 postmenopausal women under similar protocols. The Multinational study (VERT MN) (risedronate sodium immediate-release 5 mg daily, N = 408) was conducted primarily in Europe and Australia; a second study was conducted in North America (VERT NA) (risedronate sodium immediate-release 5 mg daily, N = 821). Patients were selected on the basis of radiographic evidence of previous vertebral fracture, and therefore, had established disease. The average number of prevalent vertebral fractures per patient at study entry was 4 in VERT MN, and 2.5 in VERT NA, with a broad range of baseline BMD levels. All patients in these studies received supplemental calcium 1000 mg/day. Patients with low 25-hydroxyvitamin D3 levels (approximately 40 nmol/L or less) also received 500 international units/day supplemental vitamin D.
Effect on Vertebral Fractures
Fractures of previously undeformed vertebrae (new fractures) and worsening of pre-existing vertebral fractures were diagnosed radiographically; some of these fractures were also associated with symptoms (that is, clinical fractures). Spinal radiographs were scheduled annually and prospectively planned analyses were based on the time to a patient’s first diagnosed fracture. The primary endpoint for these studies was the incidence of new and worsening vertebral fractures across the period of 0 to 3 years. Risedronate sodium immediate-release 5 mg daily significantly reduced the incidence of new and worsening vertebral fractures and of new vertebral fractures in both VERT NA and VERT MN at all time points (Table 3). The reduction in risk seen in the subgroup of patients who had 2 or more vertebral fractures at study entry was similar to that seen in the overall study population.
Table 3 The Effect of Risedronate sodium 5 mg Immediate-Release Daily on the Risk of Vertebral Fractures Proportion of Patients
with Fracture (%)a
VERT NAPlacebo
N = 678Risedronate sodium
5 mg
N = 696Absolute Risk
Reduction (%)Relative Risk
Reduction (%)New and Worsening 0 to 1 Year 7.2 3.9 3.3 49 0 to 2 Years 12.8 8.0 4.8 42 0 to 3 Years 18.5 13.9 4.6 33 New 0 to 1 Year 6.4 2.4 4.0 65 0 to 2 Years 11.7 5.8 5.9 55 0 to 3 Years 16.3 11.3 5.0 41
VERT MNPlacebo
N = 346Risedronate sodium
5 mg
N = 344Absolute Risk
Reduction (%)Relative Risk
Reduction (%)New and Worsening 0 to 1 Year 15.3 8.2 7.1 50 0 to 2 Years 28.3 13.9 14.4 56 0 to 3 Years 34.0 21.8 12.2 46 New 0 to 1 Year 13.3 5.6 7.7 61 0 to 2 Years 24.7 11.6 13.1 59 0 to 3 Years 29.0 18.1 10.9 49 aCalculated by Kaplan-Meier methodology. Effect on Osteoporosis-Related Nonvertebral Fractures
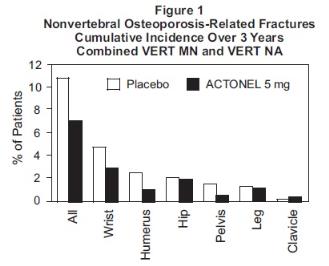
In VERT MN and VERT NA, a prospectively planned efficacy endpoint was defined consisting of all radiographically confirmed fractures of skeletal sites accepted as associated with osteoporosis. Fractures at these sites were collectively referred to as osteoporosis-related nonvertebral fractures. Risedronate sodium immediate-release 5 mg daily significantly reduced the incidence of nonvertebral osteoporosis-related fractures over 3 years in VERT NA (8% versus 5%; relative risk reduction 39%) and reduced the fracture incidence in VERT MN from 16% to 11%. There was a significant reduction from 11% to 7% when the studies were combined, with a corresponding 36% reduction in relative risk. Figure 1 shows the overall results as well as the results at the individual skeletal sites for the combined studies.
Histology/Histomorphometry
Bone biopsies from 110 postmenopausal women were obtained at endpoint in the VERT NA study. Patients had received placebo or daily risedronate sodium immediate-release (2.5 mg or 5 mg) for 2 to 3 years. Histologic evaluation (N = 103) showed no osteomalacia, impaired bone mineralization, or other adverse effects on bone in risedronate sodium immediate-release treated women. These findings demonstrate that bone formed during risedronate sodium immediate-release administration is of normal quality. The histomorphometric parameter mineralizing surface, an index of bone turnover, was assessed based upon baseline and post-treatment biopsy samples from 21 treated with placebo and 23 patients treated with risedronate sodium immediate-release 5 mg daily. Mineralizing surface decreased moderately in risedronate sodium immediate-release treated patients (median percent change: placebo, -21%; risedronate sodium immediate-release 5 mg daily, -74%), consistent with the known effects of treatment on bone turnover.
Effect on Height
In the two 3-year osteoporosis treatment studies, standing height was measured yearly by stadiometer. Both risedronate sodium immediate-release 5 mg daily and placebo-treated groups lost height during the studies. Patients who received risedronate sodium immediate-release 5 mg daily had a statistically significantly smaller loss of height than those who received placebo. In VERT MN, the median annual height change was -2.4 mm/yr in the placebo group compared to
-1.3 mm/yr in the risedronate sodium immediate-release 5 mg daily group. In VERT NA, the median annual height change was -1.1 mm/yr in the placebo group compared to -0.7 mm/yr in the risedronate sodium immediate-release 5 mg daily group.
Effect on Bone Mineral Density
The results of 4 randomized, placebo-controlled trials in women with postmenopausal osteoporosis (VERT MN, VERT NA, BMD MN, BMD NA) demonstrate that risedronate sodium immediate-release 5 mg daily increases BMD at the spine, hip, and wrist compared to the effects seen with placebo. Table 4 displays the significant increases in BMD seen at the lumbar spine, femoral neck, femoral trochanter, and midshaft radius in these trials compared to placebo. In both VERT studies (VERT MN and VERT NA), risedronate sodium immediate-release 5 mg daily produced increases in lumbar spine BMD that were progressive over the 3 years of treatment, and were statistically significant relative to baseline and to placebo at 6 months and at all later time points.
Table 4 Mean Percent Increase in BMD from Baseline in Patients Taking Risedronate sodium Immediate-Release 5 mg or Placebo at Endpointa VERT MNb VERT NAb BMD MNc BMD NAc Placebo
N = 3235 mg
N = 323Placebo
N = 5995 mg
N = 606Placebo
N = 1615 mg
N = 148Placebo
N = 1915 mg
N = 193Lumbar Spine 1.0 6.6 0.8 5.0 0.0 4.0 0.2 4.8 Femoral Neck -1.4 1.6 -1.0 1.4 -1.1 1.3 0.1 2.4 Femoral Trochanter -1.9 3.9 -0.5 3.0 -0.6 2.5 1.3 4.0 Midshaft Radius -1.5* 0.2* -1.2* 0.1* ND ND aThe endpoint value is the value at the study's last time point for all patients who had BMD measured at that time; otherwise the last post-baseline BMD value prior to the study's last time point is used.
bThe duration of the studies was 3 years.
cThe duration of the studies was 1.5 to 2 years.
*BMD of the midshaft radius was measured in a subset of centers in VERT MN (placebo, N = 222;
5 mg, N = 214) and VERT NA (placebo, N = 310; 5 mg, N = 306).
ND = analysis not done -
16
HOW SUPPLIED/STORAGE AND HANDLING
Atelvia® (risedronate sodium) delayed-release tablets are:
35 mg, yellow, oval-shaped, and engraved with EC 35 on one side.
NDC: 0430-0979-03 Dosepak of 4 tablets
Store at controlled room temperature 20° to 25° C (68° to 77° F) [see USP].
-
17
PATIENT COUNSELING INFORMATION
See FDA-approved patient labeling (Medication Guide)
Instruct patients to read the Medication Guide before starting therapy with Atelvia and to re-read it each time the prescription is renewed.
Instruct patients that Atelvia and Actonel contain the same active ingredient and if they are taking Actonel, they should not take Atelvia [see Warnings and Precautions (5.1)].
Instruct patients to pay particular attention to the dosing instructions as clinical benefits may be compromised by failure to take the drug according to instructions.
Instruct patients to take Atelvia in the morning, while in an upright position (sitting or standing) with at least 4 ounces of plain water immediately following breakfast. Atelvia should not be taken before breakfast.
Instruct patients to swallow Atelvia tablets whole. Patients should not chew, cut, or crush the tablet because of a potential for oropharyngeal irritation, and because the tablet coating is an important part of the delayed-release formulation. Patients should not lie down for 30 minutes after taking the medication.
Instruct patients that if they develop symptoms of esophageal disease (such as difficulty or pain upon swallowing, retrosternal pain or severe persistent or worsening heartburn) they should consult their physician before continuing Atelvia [see Warnings and Precautions (5.2)].
If a dose of Atelvia 35 mg once-a-week is missed, instruct the patient to take one tablet on the morning after they remember and return to taking one tablet once-a-week, as originally scheduled on their chosen day. Patients should not take 2 tablets on the same day.
Instruct patients to take supplemental calcium and vitamin D if dietary intake is inadequate [see Warnings and Precautions (5.3)].
Instruct patients to take calcium supplements, antacids, magnesium-based supplements or laxatives, and iron preparations at a different time of the day because they interfere with the absorption of Atelvia.
Remind patients to give all of their healthcare providers an accurate medication history. Instruct patients to tell all of their healthcare providers that they are taking Atelvia. Patients should be instructed that any time they have a medical problem they think may be from Atelvia they should talk to their doctor.
Distributed by:
Allergan USA, Inc.
Irvine CA, 92612For all medical inquiries contact:
Allergan Medical Communications
1-800-678-1605© 2018 Allergan. All rights reserved.
ATELVIA® is a registered trademark of
Allergan Pharmaceuticals International Limited.
Allergan® and its design are trademarks of Allergan, Inc.Content Updated: March 2015
73166US11
-
MEDICATION GUIDE
Medication Guide
Atelvia® (uh-TEL-v-uh)
(risedronate sodium)
delayed-release tabletsRead this Medication Guide that comes with Atelvia® before you start taking it and each time you get a refill. There may be new information. This Medication Guide does not take the place of talking with your doctor about your medical condition or your treatment. Talk to your doctor if you have any questions about Atelvia, there may be new information about it.
What is the most important information I should know about Atelvia?
Atelvia can cause serious side effects including:
- Esophagus problems
- Low calcium levels in your blood (hypocalcemia)
- Severe jaw bone problems (osteonecrosis)
- Bone, joint, or muscle pain
- Unusual thigh bone fractures
1. Esophagus problems.
Some people who take Atelvia may develop problems in the esophagus (the tube that connects the mouth and the stomach). These problems include irritation, inflammation, or ulcers of the esophagus which may sometimes bleed.
-
It is important that you take Atelvia exactly as prescribed to help lower your chance of getting esophagus problems. (See the section “How should I take Atelvia?”)
- Stop taking Atelvia and call your doctor right away if you get chest pain, new or worsening heartburn, or have trouble or pain when you swallow.
2. Low calcium levels in your blood (hypocalcemia).
Atelvia may lower the calcium levels in your blood. If you have low blood calcium before you start taking Atelvia, it may get worse during treatment. Your low blood calcium must be treated before you take Atelvia. Most people with low blood calcium levels do not have symptoms, but some people may have symptoms. Call your doctor right away if you have symptoms of low blood calcium such as:
- Spasms, twitches, or cramps in your muscles
- Numbness or tingling in your fingers, toes, or around your mouth
Your doctor may prescribe calcium and vitamin D to help prevent low calcium levels in your blood, while you are taking Atelvia. Take calcium and vitamin D as your doctor tells you to.
3. Severe jaw bone problems (osteonecrosis).
Severe jaw bone problems may happen when you take Atelvia. Your doctor should examine your mouth before you start Atelvia. Your doctor may tell you to see your dentist before you start Atelvia. It is important for you to practice good mouth care during treatment with Atelvia.
4. Bone, joint, or muscle pain.
Some people who take Atelvia develop severe bone, joint, or muscle pain.
5. Unusual thigh bone fractures.
Some people have developed unusual fractures in their thigh bone. Symptoms of a fracture may include new or unusual pain in your hip, groin, or thigh.
Call your doctor right away if you have any of these side effects.
What is Atelvia?
Atelvia is a prescription medicine used to treat osteoporosis in women after menopause.
It is not known how long Atelvia works for the treatment and prevention of osteoporosis. You should see your doctor regularly to determine if Atelvia is still right for you.
Atelvia is not for use in children.
Who should not take Atelvia?
Do not take Atelvia if you:
- Have certain problems with your esophagus, the tube that connects your mouth and stomach
- Cannot sit or stand up for at least 30 minutes
- Have low blood calcium (hypocalcemia)
- Are allergic to any of the other ingredients in Atelvia. See the end of this leaflet for a complete list of ingredients in Atelvia.
What should I tell my healthcare provider before taking Atelvia?
Before you take Atelvia, tell your healthcare provider if you:
- Have problems swallowing
- Have stomach or digestive problems
- Have low blood calcium
- Plan to have dental surgery or teeth removed
- Have kidney problems
- Have been told you have trouble absorbing mineral in your stomach or intestines (malabsorption syndrome)
- Are pregnant or plan to become pregnant. It is not known if Atelvia can harm your unborn baby.
- Are breastfeeding or plan to breastfeed. It is not known if Atelvia passes into your breast milk and may harm your baby. You and your doctor should decide if you will take Atelvia or breastfeed. You should not do both.
Tell your doctor about all the medicines you take, including prescription and non-prescription medicines, vitamins and herbal supplements. Certain medicines may affect how Atelvia works.
Especially tell your doctor if you take:
- Actonel® or other medicines to treat osteoporosis
- calcium supplements
- antacids
- laxatives
- iron supplements
Ask your doctor or pharmacist for a list of these medications, if you are not sure.
Know the medicines you take. Keep a list of them to show your doctor and pharmacist when you get a new medicine.
How should I take Atelvia?
- Take Atelvia exactly as your doctor tells you.
- Take Atelvia 1 time a week right after breakfast. Choose a day of the week to take Atelvia that best fits your schedule.
- Take Atelvia with at least 4 ounces (about 1-half cup) of plain water.
- Swallow Atelvia tablets whole. Do not chew, cut, or crush Atelvia tablets before swallowing. If you cannot swallow Atelvia tablets whole, tell your doctor. You may need a different medicine.
After swallowing Atelvia wait at least 30 minutes:
- Before you lie down. You may sit, stand or walk, and do normal activities like reading.
- Before you take other medicines, including antacids, calcium, and other supplements and vitamins.
Do not lie down for at least 30 minutes after you take Atelvia.
If you miss your weekly Atelvia dose, take Atelvia the morning after you remember then return to your normal schedule. Do not take 2 doses at the same time.
You should take calcium and vitamin D as directed by your doctor.
If you take too much Atelvia, call your doctor. Do not try to vomit. Do not lie down.
What are the possible side effects of Atelvia?
Atelvia may cause serious side effects:
- See “What is the most important information I should know about Atelvia”.
The most common side effects of Atelvia include:
- diarrhea
- flu-like symptoms
- muscle pain
- back and joint pain
- upset stomach
- stomach area (abdominal) pain
You may get allergic reactions, such as hives, swelling of your face, lips, tongue, or throat.
Tell your doctor if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of Atelvia. For more information, ask your doctor or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store Atelvia?
- Store Atelvia between 68° F to 77° F (20° C to 25° C).
Keep Atelvia and all medicines out of the reach of children.
General information about the safe and effective use of Atelvia
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information Leaflet. Do not use Atelvia for a condition for which it was not prescribed. Do not give Atelvia to other people, even if they have the same symptoms you have. It may harm them.
This Medication Guide summarizes the most important information about Atelvia. If you would like more information, talk with your doctor. You can ask your pharmacist or doctor for information about Atelvia that is written for health professionals.
For more information, go to www.Atelvia.com or call 1-800-678-1605.
What are the ingredients in Atelvia?
Active ingredient: risedronate sodium
Inactive ingredients: Edetate disodium, ferric oxide yellow, magnesium stearate, methacrylic acid copolymer, polysorbate 80, silicified microcrystalline cellulose (ProSolv SMCC90), simethicone, sodium starch glycolate, stearic acid, talc, and triethyl citrate.
This Medication Guide has been approved by the U.S. Food and Drug Administration.
Distributed by:
Allergan USA, Inc.
Irvine, CA, 92612For all medical inquiries contact:
Allergan Medical Communications
1-800-678-1605© 2018 Allergan. All rights reserved.
ATELVIA® is a registered trademark of
Allergan Pharmaceuticals International Limited.
Allergan® and its design are trademarks of Allergan, Inc.
Content Updated: March 2015
73166US11
- Esophagus problems
-
PRINCIPAL DISPLAY PANEL
PRINCIPAL DISPLAY PANEL
NDC: 0430-0979-03
Atelvia 35 mg
(risedronate sodium) delayed-release tablets
Once-a-Week
4 tablets
Rx Only
-
INGREDIENTS AND APPEARANCE
ATELVIA
risedronate sodium tablet, delayed releaseProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0430-0979 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength RISEDRONATE SODIUM HEMI-PENTAHYDRATE (UNII: HU2YAQ274O) (RISEDRONIC ACID - UNII:KM2Z91756Z) RISEDRONATE SODIUM ANHYDROUS 30.1 mg RISEDRONATE SODIUM MONOHYDRATE (UNII: F67L43UT5C) (RISEDRONIC ACID - UNII:KM2Z91756Z) RISEDRONATE SODIUM ANHYDROUS 4.9 mg Inactive Ingredients Ingredient Name Strength EDETATE DISODIUM (UNII: 7FLD91C86K) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) MAGNESIUM STEARATE (UNII: 70097M6I30) METHACRYLIC ACID - ETHYL ACRYLATE COPOLYMER (1:1) TYPE A (UNII: NX76LV5T8J) POLYSORBATE 80 (UNII: 6OZP39ZG8H) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) SODIUM STARCH GLYCOLATE TYPE A POTATO (UNII: 5856J3G2A2) STEARIC ACID (UNII: 4ELV7Z65AP) TALC (UNII: 7SEV7J4R1U) TRIETHYL CITRATE (UNII: 8Z96QXD6UM) Product Characteristics Color YELLOW Score no score Shape OVAL Size 12mm Flavor Imprint Code EC;35 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0430-0979-03 4 in 1 DOSE PACK; Type 0: Not a Combination Product 12/01/2010 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA022560 12/01/2010 Labeler - Allergan, Inc. (144796497)
Trademark Results [Atelvia]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 ATELVIA 85001017 3946064 Live/Registered |
ALLERGAN PHARMACEUTICALS INTERNATIONAL LIMITED 2010-03-29 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.