Ifosfamide by Hikma Pharmaceuticals USA Inc. IFOSFAMIDE injection
Ifosfamide by
Drug Labeling and Warnings
Ifosfamide by is a Prescription medication manufactured, distributed, or labeled by Hikma Pharmaceuticals USA Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use IFOSFAMIDE INJECTION safely and effectively. See full prescribing information for IFOSFAMIDE INJECTION.
IFOSFAMIDE injection, intravenous use
Initial U.S. Approval: 1988WARNING: MYELOSUPPRESSION, NEUROTOXICITY, and UROTOXICITY
See full prescribing information for complete boxed warning
Myelosuppression can be severe and lead to fatal infections (5.1)
CNS toxicities can be severe and result in encephalopathy and death (5.2)
Nephrotoxicity can be severe and result in renal failure. Hemorrhagic cystitis can be severe. (5.3)
INDICATIONS AND USAGE
Ifosfamide Injection is an alkylating drug indicated for use in combination with certain other approved antineoplastic agents for third-line chemotherapy of germ cell testicular cancer. It should be used in combination with mesna for prophylaxis of hemorrhagic cystitis. (1)
DOSAGE AND ADMINISTRATION
Dosage and duration of treatment and/or treatment intervals depend on the scheme of combination therapy, the patient’s general state of health and organ function, and the results of laboratory monitoring. (2)
Ifosfamide injection should be administered as a slow intravenous infusion lasting a minimum of 30 minutes at a dose of 1.2 grams per m2 per day for 5 consecutive days. (2)
Treatment is repeated every 3 weeks or after recovery from hematologic toxicity. (2)
To prevent bladder toxicity, ifosfamide injection should be given with extensive hydration consisting of at least 2 liters of oral or intravenous fl uid per day. (2, 5.3 )
Mesna should be used to reduce the incidence of hemorrhagic cystitis. (2)
DOSAGE FORMS AND STRENGTHS
Single dose vials: 1 g/20 mL, 3 g/60 mL (3) (3)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
Myelosuppression: Can be severe and lead to fatal infections. Monitor blood counts prior to and at intervals after treatment. (5.1)
Neurotoxicity: Severe and fatal neurotoxicity can occur. Carefully monitor the patient for CNS toxicity and other neurotoxic effects. Discontinue therapy should encephalopathy develop. (5.2)
Urotoxicity: Severe nephrotoxicity with renal failure and death can occur. Monitor for nephrotoxicity with serum and urine chemistries. Mesna should be used to reduce hemorrhagic cystitis. (5.3)
Cardiotoxicity: Arrhythmias, other ECG changes, and cardiomyopathy can occur and result in death. Use with caution in patients with cardiac risk factors and in patients with preexisting cardiac disease. The risk of cardiotoxicity is dose dependent. (5.4)
Pulmonary toxicity: Interstitial pneumonitis, pulmonary fi brosis, and other forms of pulmonary toxicity with fatal outcomes can occur. Monitor for signs and symptoms of pulmonary toxicity and treat as clinically indicated (5.5)
Secondary malignancies as late sequelae have occurred. (5.6)
Pregnancy: Can cause fetal harm. Women should not become pregnant and men should not father a child during therapy. (5.8)
Anaphylactic/anaphylactoid reactions have been reported. (5.10)
ADVERSE REACTIONS
In clinical trials of ifosfamide monotherapy, the most common (≥ 10%) adverse reactions were alopecia, nausea/vomiting, leukopenia, anemia, CNS toxicity, hematuria, and infection. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact West-Ward Pharmaceuticals Corp. at 1-877-845-0689, or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 10/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: MYELOSUPPRESSION, NEUROTOXICITY, and UROTOXICITY
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Myelosuppression, Immunosuppression, and Infections
5.2 Central Nervous System Toxicity, Neurotoxicity
5.3 Renal and Urothelial Toxicity and Effects
5.4 Cardiotoxicity
5.5 Pulmonary Toxicity
5.6 Secondary Malignancies
5.7 Veno-occlusive Liver Disease
5.8 Pregnancy
5.9 Effects on Fertility
5.10 Anaphylactic/Anaphylactoid Reactions and Cross-sensitivity
5.11 Impairment of Wound Healing
5.12 Nursing
6 ADVERSE REACTIONS
6.1 Adverse Reactions from Clinical Trials
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Inducers of CYP3A4
7.2 Inhibitors of CYP3A4
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Use in Patients with Renal Impairment
8.7 Use in Patients with Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
15 REFERENCES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: MYELOSUPPRESSION, NEUROTOXICITY, and UROTOXICITY
WARNING: MYELOSUPPRESSION, NEUROTOXICITY, AND UROTOXICITY
Myelosuppression can be severe and lead to fatal infections. Monitor blood counts prior to and at intervals after each treatment cycle. CNS toxicities can be severe and result in encephalopathy and death. Monitor for CNS toxicity and discontinue treatment for encephalopathy. Nephrotoxicity can be severe and result in renal failure. Hemorrhagic cystitis can be severe and can be reduced by the prophylactic use of mesna. [see Warnings and Precautions (5.1 to 5.3) ]
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
Ifosfamide Injection should be administered intravenously at a dose of 1.2 grams per m2 per day for 5 consecutive days. Treatment is repeated every 3 weeks or after recovery from hematologic toxicity.
In order to prevent bladder toxicity, ifosfamide injection should be given with extensive hydration consisting of at least 2 liters of oral or intravenous fluid per day. Mesna should be used to reduce the incidence of hemorrhagic cystitis. Ifosfamide injection should be administered as a slow intravenous infusion lasting a minimum of 30 minutes. Studies of ifosfamide injection in patients with hepatic or renal impairment have not been conducted [see Use in Specifi c Populations (8.6 , 8.7 )].
Preparation for Intravenous Administration/Stability
Solutions of ifosfamide injection may be diluted further to achieve concentrations of 0.6 to 20 mg/mL in the following fluids:
5% Dextrose Injection
0.9% Sodium Chloride Injection
Lactated Ringer’s Injections
Sterile Water for Injection
Because essentially identical stability results were obtained for Sterile Water admixtures as for the other admixtures (5% Dextrose Injection, 0.9% Sodium Chloride Injection, and Lactated Ringer’s Injection), the use of large volume parenteral glass bottles, Viaflex bags or PAB™ bags that contain intermediate concentrations or mixtures of excipients (e.g., 2.5% Dextrose Injection, 0.45% Sodium Chloride Injection, or 5% Dextrose and 0.9% Sodium Chloride Injection) is also acceptable.
Further diluted solutions of ifosfamide injection should be refrigerated and used within 24 hours. Benzyl alcohol-containing solutions can reduce the stability of ifosfamide injection.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Myelosuppression, Immunosuppression, and Infections
Treatment with ifosfamide may cause myelosuppression and significant suppression of immune responses, which can lead to severe infections. Fatal outcomes of ifosfamide-associated myelosuppression have been reported. Ifosfamide-induced myelosuppression can cause leukopenia, neutropenia, thrombocytopenia (associated with a higher risk of bleeding events), and anemia. The nadir of the leukocyte count tends to be reached approximately during the second week after administration. When ifosfamide is given in combination with other chemotherapeutic/hematotoxic agents and/or radiation therapy, severe myelosuppression is frequently observed. The risk of myelosuppression is dose-dependent and is increased with administration of a single high dose compared with fractionated administration. The risk of myelosuppression is also increased in patients with reduced renal function.
Severe immunosuppression has led to serious, sometimes fatal, infections. Sepsis and septic shock also have been reported. Infections reported with ifosfamide include pneumonias, as well as other bacterial, fungal, viral, and parasitic infections. Latent infections can be reactivated. In patients treated with ifosfamide, reactivation has been reported for various viral infections. Infections must be treated appropriately. Antimicrobial prophylaxis may be indicated in certain cases of neutropenia at the discretion of the managing physician. In case of neutropenic fever, antibiotics and/or antimycotics must be given. Close hematologic monitoring is recommended. White blood cell (WBC) count, platelet count and hemoglobin should be obtained prior to each administration and at appropriate intervals after administration. Unless clinically essential, ifosfamide should not be given to patients with a WBC count below 2000/μL and/or a platelet count below 50,000/μL.
Ifosfamide should be given cautiously, if at all, to patients with presence of an infection, severe immunosuppression or compromised bone marrow reserve, as indicated by leukopenia, granulocytopenia, extensive bone marrow metastases, prior radiation therapy, or prior therapy with other cytotoxic agents.
5.2 Central Nervous System Toxicity, Neurotoxicity
Administration of ifosfamide can cause CNS toxicity and other neurotoxic effects. The risk of CNS toxicity and other neurotoxic effects necessitates careful monitoring of the patient. Neurologic manifestations consisting of somnolence, confusion, hallucinations, blurred vision, psychotic behavior, extrapyramidal symptoms, urinary incontinence, seizures, and in some instances, coma, have been reported following ifosfamide therapy. There have also been reports of peripheral neuropathy associated with ifosfamide use.
Ifosfamide neurotoxicity may manifest within a few hours to a few days after fi rst administration and in most cases resolves within 48 to 72 hours of ifosfamide discontinuation. Symptoms may persist for longer periods of time. Supportive therapy should be maintained until their complete resolution. Occasionally, recovery has been incomplete. Fatal outcomes of CNS toxicity have been reported. Recurrence of CNS toxicity after several uneventful treatment courses has been reported. If encephalopathy develops, administration of ifosfamide should be discontinued.
Due to the potential for additive effects, drugs acting on the CNS (such as antiemetics, sedatives, narcotics, or antihistamines) must be used with particular caution or, if necessary, be discontinued in case of ifosfamide-induced encephalopathy.
Manifestations of CNS toxicity may impair a patient’s ability to operate an automobile or other heavy machinery.
5.3 Renal and Urothelial Toxicity and Effects
Ifosfamide is both nephrotoxic and urotoxic. Glomerular and tubular kidney function must be evaluated before commencement of therapy as well as during and after treatment. Monitor urinary sediment regularly for the presence of erythrocytes and other signs of uro/nephrotoxicity. Monitor serum and urine chemistries, including phosphorus and potassium regularly. Administer appropriate replacement therapy as indicated. Renal parenchymal and tubular necrosis have been reported in patients treated with ifosfamide. Acute tubular necrosis, acute renal failure, and chronic renal failure secondary to ifosfamide therapy have been reported, and fatal outcome from nephrotoxicity has been documented.
Disorders of renal function, (glomerular and tubular) following ifosfamide administration are very common. Manifestations include a decrease in glomerular filtration rate, increased serum creatinine, proteinuria, enzymuria, cylindruria, aminoaciduria, phosphaturia, and glycosuria as well as tubular acidosis. Fanconi syndrome, renal rickets, and growth retardation in children as well as osteomalacia in adults also have been reported. Development of a syndrome resembling SIADH (syndrome of inappropriate antidiuretic hormone secretion) has been reported with ifosfamide.
Tubular damage may become apparent during therapy, months or even years after cessation of treatment. Glomerular or tubular dysfunction may resolve with time, remain stable, or progress over a period of months or years, even after completion of ifosfamide treatment.
The risk and expected benefits of ifosfamide therapy should be carefully weighed when considering the use of ifosfamide in patients with preexisting renal impairment or reduced nephron reserve.
Urotoxic side effects, especially hemorrhagic cystitis, have been very commonly associated with the use of ifosfamide. These urotoxic effects can be reduced by prophylactic use of mesna.
Hemorrhagic cystitis requiring blood transfusion has been reported with ifosfamide. The risk of hemorrhagic cystitis is dose-dependent and increased with administration of single high doses compared to fractionated administration. Hemorrhagic cystitis after a single dose of ifosfamide has been reported. Past or concomitant radiation of the bladder or busulfan treatment may increase the risk for hemorrhagic cystitis.
Before starting treatment, it is necessary to exclude or correct any urinary tract obstructions [see Contraindications(4)].
During or immediately after administration, adequate amounts of fluid should be ingested or infused to force dieresis in order to reduce the risk of urinary tract toxicity. Obtain a urinalysis prior to each dose of ifosfamide. If microscopic hematuria (greater than 10 RBCs per high power field) is present, then subsequent administration should be withheld until complete resolution. Further administration of ifosfamide should be given with vigorous oral or parenteral hydration.
Ifosfamide should be used with caution, if at all, in patients with active urinary tract infections.
5.4 Cardiotoxicity
Manifestations of cardiotoxicity reported with ifosfamide treatment include:
- Supraventricular or ventricular arrhythmias, including atrial/supraventricular tachycardia, atrial fibrillation, pulseless ventricular tachycardia
- Decreased QRS voltage and ST-segment or T-wave changes
- Toxic cardiomyopathy leading to heart failure with congestion and hypotension
- Pericardial effusion, fibrinous pericarditis, and epicardial fibrosis
Fatal outcome of ifosfamide-associated cardiotoxicity has been reported.
The risk of developing cardiotoxic effects is dose-dependent. It is increased in patients with prior or concomitant treatment with other cardiotoxic agents or radiation of the cardiac region and, possibly, renal impairment.
Particular caution should be exercised when ifosfamide is used in patients with risk factors for cardiotoxicity and in patients with preexisting cardiac disease.
5.5 Pulmonary Toxicity
Interstitial pneumonitis, pulmonary fibrosis, and other forms of pulmonary toxicity have been reported with ifosfamide treatment. Pulmonary toxicity leading to respiratory failure as well as fatal outcome has also been reported. Monitor for signs and symptoms of pulmonary toxicity and treat as clinically indicated.
5.6 Secondary Malignancies
Treatment with ifosfamide involves the risk of secondary tumors and their precursors as late sequelae. The risk of myelodysplastic alterations, some progressing to acute leukemias, is increased. Other malignancies reported after use of ifosfamide or regimens with ifosfamide include lymphoma, thyroid cancer, and sarcomas.
The secondary malignancy may develop several years after chemotherapy has been discontinued.
5.7 Veno-occlusive Liver Disease
Veno-occlusive liver disease has been reported with chemotherapy that included ifosfamide.
5.8 Pregnancy
Ifosfamide can cause fetal harm when administered to a pregnant woman. Fetal growth retardation and neonatal anemia have been reported following exposure to ifosfamide-containing chemotherapy regimens during pregnancy. Ifosfamide is genotoxic and mutagenic in male and female germ cells. Embryotoxic and teratogenic effects have been observed in mice, rats and rabbits at doses 0.05 to 0.075 times the human dose.
Women should not become pregnant and men should not father a child during therapy with ifosfamide. Further, men should not father a child for up to 6 months after the end of therapy. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug or after treatment, the patient should be apprised of the potential hazard to a fetus [see Use in Specific Populations (8.1) ].
5.9 Effects on Fertility
Ifosfamide interferes with oogenesis and spermatogenesis. Amenorrhea, azoospermia, and sterility in both sexes have been reported. Development of sterility appears to depend on the dose of ifosfamide, duration of therapy, and state of gonadal function at the time of treatment. Sterility may be irreversible in some patients.
Female Patients
Amenorrhea has been reported in patients treated with ifosfamide. The risk of permanent chemotherapy-induced amenorrhea increases with age. Pediatric patients treated with ifosfamide during prepubescence subsequently may not conceive and those who retain ovarian function after completing treatment are at increased risk of developing premature menopause.
Male Patients
Men treated with ifosfamide may develop oligospermia or azoospermia. Pediatric patients treated with ifosfamide during prepubescence might not develop secondary sexual characteristics normally, but may have oligospermia or azoospermia. Azoospermia may be reversible in some patients, though the reversibility may not occur for several years after cessation of therapy. Sexual function and libido are generally unimpaired in these patients. Some degree of testicular atrophy may occur. Patients treated with ifosfamide have subsequently fathered children.
5.10 Anaphylactic/Anaphylactoid Reactions and Cross-sensitivity
Anaphylactic/anaphylactoid reactions have been reported in association with ifosfamide. Cross-sensitivity between oxazaphosphorine cytotoxic agents has been reported.
5.12 Nursing
Ifosfamide is excreted in breast milk. Women must not breastfeed during treatment with ifosfamide [see Use in Specific Populations (8.3) ].
-
6 ADVERSE REACTIONS
6.1 Adverse Reactions from Clinical Trials
Because clinical trials are conducted from widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice. The adverse reactions and frequencies below are based on 30 publications describing clinical experience with fractionated administration of ifosfamide as monotherapy with a total dose of 4 to 12 g/m2 per course.
System Organ Class (SOC) Adverse Reaction Percentage (Ratio) INFECTIONS AND INFESTATIONS Infection 9.9%
(112/1128)BLOOD AND LYMPHATIC SYSTEM DISORDERS Leukopenia1 (any) Leukopenia
<1 x 103/µL43.5%
(267/614)Thrombocytopenia2 (any) Thrombocytopenia
50 x 103/µL4.8%
(35/729)Anemia3 37.9%
(202/533)METABOLISM AND NUTRITION DISORDERS Anorexia 1.1%
(15/1317)NERVOUS SYSTEM DISORDERS Central nervous system toxicity4,5 15.4%
(154/1001)Peripheral neuropathy 0.4%
(5/1317)CARDIAC DISORDERS Cardiotoxicity6 0.5%
(7/1317)VASCULAR DISORDERS Hypotention7 0.3%
(4/1317)GASTROINTESTINAL DISORDERS Nausea/Vomiting 46.8%
(443/964)Diarrhea 0.7%
(9/1317)Stomatitis 0.3%
(4/1317)HEPATOBILIARY DISORDERS Hepatotoxicity8 1.8%
(22/1190)SKIN AND SUBCUTANEOUS TISSUES DISORDERS Alopecia 89.6%
(540/603)Dermatitis 0.08%
(1/1317)Papular rash 0.08%
(1/1317)RENAL AND URINARY DISORDERS Hemorrhagic cystitis9 Hematuria - without mesna 44.1%
(282/640)- with mesna 21.3%
(33/155)Macrohematuria - without mesna 11.1%
(66/594)- with mesna 5.2%
(5/97)Renal dysfunction10 -- Renal structural damage -- GENERAL DISORDERS AND ADMINISTRATIVE SITE CONDITIONS Phlebitis11 2.8%
(37/1317)Neutropenic fever12 1%
(13/1317)Fatigue 0.3%
(4/1317)Malaise Unable to calculate 1 The following adverse reaction terms have been reported for leukopenia: neutropenia, granulocytopenia, lymphopenia, and pancytopenia. For neutropenic fever, see below.
2 Thrombocytopenia may also be complicated by bleeding. Bleeding with fatal outcome has been reported.
3 Includes cases reported as anemia and decrease in hemoglobin/hematocrit.
4 Encephalopathy with coma and death has been reported.
5 Central nervous system toxicity was reported to be manifested by the following signs and symptoms: Abnormal behavior, Affect lability Aggression, Agitation, Anxiety, Aphasia, Asthenia, Ataxia, Cerebellar syndrome, Cerebral function defi ciency, Cognitive disorder, Coma, Confusional state, Convulsions, Cranial nerve dysfunction, Depressed state of consciousness, Depression, Disorientation, Dizziness, Electroencephalogram abnormal, Encephalopathy, Flat affect. Hallucinations, Headache, Ideation, Lethargy, Memory impairment, Mood change, Motor dysfunction, Muscle spasms, Myoclonus, Progressive loss of brainstem reflexes, Psychotic reaction, Restlessness, Somnolence, Tremor, Urinary incontinence.
6 Cardiotoxicity was reported as congestive heart failure, tachycardia, pulmonary edema. Fatal outcome has been reported.
7 Hypotension leading to shock and fatal outcome has been reported.
8 Hepatotoxicity was reported as increases in liver enzymes, i.e., serum alanine aminotransferase, serum aspartate aminotransferase, alkaline phosphatase, gamma-glutamyltransferase and lactate dehydrogenase, increased bilirubin, jaundice, hepatorenal syndrome.
9 Reported symptoms of hemorrhagic cystitis included dysuria and pollakiuria. See also Post-marketing Adverse Reactions (6.2).
10 Renal dysfunction was reported to be manifested as: Renal failure (including acute renal failure, irreversible renal failure; fatal outcomes have been reported), Serum creatinine increased, BUN increased, Creatinine clearance decreased, Metabolic acidosis, Anuria, Oliguria, Glycosuria, Hyponatremia, Uremia, Creatinine clearance increased. Renal structural damage was reported to be manifested as: Acute tubular necrosis, renal parenchymal damage, Enzymuria, Cylindruria, Proteinuria.
11 Includes cases reported as phlebitis and irritation of the venous walls.
12 Includes cases reported as granulocytopenic fever.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of Ifosfamide injection. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
INFECTIONS AND INFESTATIONS:
The following manifestations have been associated with myelosuppression and immunosuppression caused by ifosfamide: increased risk for and severity of infections†, pneumonias†, sepsis and septic shock (including fatal outcomes), as well as reactivation of latent infections, including viral hepatitis†, Pneumocystis jiroveci†, herpes zoster, Strongyloides, progressive multifocal leukoencephalopathy†, and other viral and fungal infections.
† Severe immunosuppression has led to serious, sometimes fatal, infections.
NEOPLASMS, BENIGN AND MALIGNANT AND UNSPECIFIED (INCL. CYSTS AND POLYPS):
As treatment-related secondary malignancy*, Acute leukemia* (Acute myeloid leukemia)*, Acute promyelocytic leukemia*, Acute lymphocytic leukemia*, Myelodysplastic syndrome, Lymphoma (Non-Hodgkin’s lymphoma), Sarcomas*, Renal cell carcinoma, Thyroid cancer
BLOOD AND LYMPHATIC SYSTEM DISORDERS:
Hematotoxicity*, Myelosuppression manifested as Bone marrow failure, Agranulocytosis; Febrile bone marrow aplasia; Disseminated intravascular coagulation, Hemolytic uremic syndrome, Hemolytic anemia, Neonatal anemia, Methemoglobinemia
IMMUNE SYSTEM DISORDERS:
Angioedema*, Anaphylactic reaction, Immunosuppression, Urticaria, Hypersensitivity reaction
ENDOCRINE DISORDERS:
Syndrome of inappropriate antidiuretic hormone secretion (SIADH)
METABOLISM AND NUTRITION DISORDERS:
Tumor lysis syndrome, Metabolic acidosis, Hypokalemia, Hypocalcemia, Hypophosphatemia, Hyperglycemia, Polydipsia
PSYCHIATRIC DISORDERS:
Panic attack, Catatonia, Mania, Paranoia, Delusion, Delirium, Bradyphrenia, Mutism, Mental status change, Echolalia, Logorrhea, Perseveration, Amnesia
NERVOUS SYSTEM DISORDERS:
Convulsion*, Status epilepticus (convulsive and nonconvulsive), reversible posterior leukoencephalopathy syndrome, Leukoencephalopathy, Extrapyramidal disorder, Asterixis, Movement disorder, Polyneuropathy, Dysesthesia, Hypothesia, Paresthesia, Neuralgia, Gait disturbance, Fecal incontinence, Dysarthria
Ifosfamide has been reintroduced after neurotoxicity. While some patients did not experience neurotoxicity, others had recurrent, including fatal, events.
EYE DISORDERS:
Visual impairment, Vision blurred, Conjunctivitis, Eye irritation
EAR AND LABYRINTH DISORDERS:
Deafness, Hypoacusis, Vertigo, Tinnitus
CARDIAC DISORDERS:
Cardiotoxicity*, Cardiac arrest*, Ventricular fi brillation*, Ventricular tachycardia*, Cardiogenic shock*, Myocardial infarction*, Cardiac failure*, Bundle branch block left, Bundle branch block right, Pericardial effusion, Myocardial hemorrhage, Angina pectoris, Left ventricular failure, Cardiomyopathy*, Congestive cardiomyopathy, Myocarditis*, Arrhythmia*, Pericarditis, Atrial fi brillation, Atrial fl utter, Bradycardia, Supraventricular extrasystoles, Premature atrial contractions, Ventricular extrasystoles, Myocardial depression, Palpitations, Ejection fraction decreased*, Electrocardiogram ST-segment abnormal, Electrocardiogram T-wave inversion, Electrocardiogram QRS complex abnormal
VASCULAR DISORDERS:
Pulmonary embolism, Deep vein thrombosis, Capillary leak syndrome, Vasculitis, Hypertension, Flushing, Blood pressure decreased
RESPIRATORY, THORACIC, AND MEDIASTINAL DISORDERS:
Respiratory failure*, Acute respiratory distress syndrome*, Pulmonary hypertension*, Interstitial lung disease* as manifested by Pulmonary fi brosis*, Alveolitis allergic, Interstitial pneumonitis, Pneumonitis*, Pulmonary edema*, Pleural effusion, Bronchospasm, Dyspnea, Hypoxia, Cough
GASTROINTESTINAL DISORDERS:
Cecitis, Colitis, Enterocolitis, Pancreatitis, Ileus, Gastrointestinal hemorrhage, Mucosal ulceration, Constipation, Abdominal pain, Salivary hypersecretion
HEPATOBILIARY DISORDERS:
Hepatic failure*, Hepatitis fulminant*, Veno-occlusive liver disease, Portal vein thrombosis, Cytolytic hepatitis, Cholestasis
SKIN AND SUBCUTANEOUS TISSUE DISORDERS:
Toxic epidermal necrolysis, Stevens-Johnson syndrome, Palmar-plantar erythrodysesthesia syndrome, Radiation recall dermatitis, Skin necrosis, Facial swelling, Petechiae, Macular rash, Rash, Pruritus, Erythema, Skin hyperpigmentation, Hyperhidrosis, nail disorder
MUSCULOSKELETAL AND CONNECTIVE TISSUE DISORDER:
Rhabdomyolysis, Osteomalacia, Rickets, Growth retardation, Myalgia, Arthralgia, Pain in extremity, Muscle twitching
RENAL AND URINARY DISORDERS:
Fanconi syndrome, Tubulointerstitial nephritis, Nephrogenic diabetes insipidus, Phosphaturia, Aminoaciduria, Polyuria, Enuresis, Feeling of residual urine Fatal outcomes from acute and chronic renal failure have been documented.
REPRODUCTIVE SYSTEM AND BREAST DISORDERS:
Infertility, Ovarian failure, Premature menopause, Amenorrhea, Ovarian disorder, Ovulation disorder, Azoospermia, Oligospermia, Impairment of spermatogenesis, Blood estrogen decreased, Blood gonadotrophin increased
CONGENITAL, FAMILIAL AND GENETIC DISORDERS:
Fetal growth retardation
GENERAL DISORDERS AND ADMINISTRATIVE SITE CONDITIONS:
Multi-organ failure*, General physical deterioration, Injection/Infusion site reactions including swelling, infl ammation, pain, erythema, tenderness, pruritus; Chest pain, Edema, Mucosal infl ammation, Pain, Pyrexia, Chills
* Including fatal outcomes
-
7 DRUG INTERACTIONS
Ifosfamide is a substrate for both CYP3A4 and CYP2B6.
7.1 Inducers of CYP3A4
CYP3A4 inducers (e.g., carbamazepine, phenytoin, fosphenytoin, phenobarbital, rifampin, St. John Wort) may increase the metabolism of ifosfamide to its active alkylating metabolites. CYP3A4 inducers may increase the formation of the neurotoxic/nephrotoxic ifosfamide metabolite, chloroacetaldehyde. Closely monitor patients taking ifosfamide with CYP3A4 inducers for toxicities and consider dose adjustment.
7.2 Inhibitors of CYP3A4
CYP3A4 inhibitors (e.g., ketoconazole, fluconazole, itraconazole, sorafenib, aprepitant, fosaprepitant, grapefruit, grapefruit juice) may decrease the metabolism of ifosfamide to its active alkylating metabolites, perhaps decreasing the effectiveness of ifosfamide treatment.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Ifosfamide can cause fetal harm when administered to a pregnant woman. Fetal growth retardation and neonatal anemia have been reported following exposure to ifosfamide-containing chemotherapy regimens during pregnancy.
Animal studies indicate that ifosfamide is capable of causing gene mutations and chromosomal damage invivo. In pregnant mice, resorptions increased and anomalies were present at day 19 after a 30 mg/m2 dose of ifosfamide was administered on day 11 of gestation. Embryo-lethal effects were observed in rats following the administration of 54 mg/m2 doses of ifosfamide from the 6th through the 15th day of gestation and embryotoxic effects were apparent after dams received 18 mg/m2 doses over the same dosing period.
Ifosfamide is embryotoxic to rabbits receiving 88 mg/m2/day doses from the 6th through the 18th day after mating. The number of anomalies was also significantly increased over the control group.
Women should not become pregnant and men should not father a child during therapy with ifosfamide. Further, men should not father a child for up to 6 months after the end of therapy. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug or after treatment, the patient should be apprised of the potential hazard to a fetus.
8.3 Nursing Mothers
Ifosfamide is excreted in breast milk. Because of the potential for serious adverse events and the tumorigenicity shown for ifosfamide in animal studies, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother. Women must not breastfeed during treatment with ifosfamide.
8.5 Geriatric Use
In general, dose selection for an elderly patient should be cautious, refl ecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
A study of patients 40 to 71 years of age indicated that elimination half-life appears to increase with advancing age [see Pharmacokinetics (12.3) ]. This apparent increase in half-life appeared to be related to increases in volume of distribution of ifosfamide with age. No signifi cant changes in total plasma clearance or renal or non-renal clearance with age were reported.
Ifosfamide and its metabolites are known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function.
8.6 Use in Patients with Renal Impairment
No formal studies were conducted in patients with renal impairment. Ifosfamide and its metabolites are known to be excreted by the kidneys and may accumulate in plasma with decreased renal function. Patients with renal impairment should be closely monitored for toxicity and dose reduction may be considered. Ifosfamide and its metabolites are dialyzable.
-
10 OVERDOSAGE
No specific antidote for ifosfamide is known.
Patients who receive an overdose should be closely monitored for the development of toxicities. Serious consequences of overdosage include manifestations of dose-dependent toxicities such as CNS toxicity, nephrotoxicity, myelosuppression, and mucositis [see Warnings and Precautions (5)].
Management of overdosage would include general supportive measures to sustain the patient through any period of toxicity that might occur, including appropriate state-of-the-art treatment for any concurrent infection, myelosuppression, or other toxicity. Ifosfamide as well as ifosfamide metabolites are dialyzable.
Cystitis prophylaxis with mesna may be helpful in preventing or limiting urotoxic effects with overdose.
-
11 DESCRIPTION
Ifosfamide injection is presented in sterile, single-dose vials for administration by intravenous infusion. Each mL contains ifosfamide, 50 mg, monobasic sodium phosphate monohydrate, 1.035 mg, dibasic sodium phosphate, 3.55 mg and water for injection, q.s.. Ifosfamide is a chemotherapeutic agent chemically related to the nitrogen mustards and a synthetic analog cyclophosphamide. Ifosfamide is 3-(2-ChloroethyI)-2-[(2-chloroethyl) amino]tetrahydro-2H-1,3,2- oxazaphosphorine 2-oxide.
Its structural formula is:
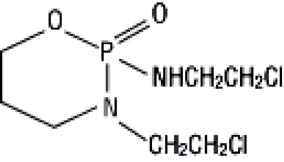
C7H15Cl2N2O2P
M. W. = 261.09
Ifosfamide is a white crystalline powder that is soluble in water.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Ifosfamide is a prodrug that requires metabolic activation by hepatic cytochrome P450 isoenzymes to exert its cytotoxic activity. Activation occurs by hydroxylation at the ring carbon atom forming the unstable intermediate 4-hydroxyifosfamide and its ring-opened aldo tautomer, which decomposes to yield the cytotoxic and urotoxic compound acrolein and an alkylating isophosphoramide mustard as well as multiple other nontoxic products. The exact mechanism of action of ifosfamide has not been determined, but its cytotoxic action is primarily through DNA crosslinks caused by alkylation by the isophosphoramide mustard at guanine N-7 positions. The formation of inter- and intra-strand cross-links in the DNA results in cell death.
12.3 Pharmacokinetics
concentrations decay biphasically and the mean terminal elimination half-life is about 15 hours. At doses of 1.6 to 2.4 g/m2/day, the plasma decay is monoexponential and the terminal elimination half-life is about 7 hours.
Ifosfamide exhibits time-dependent pharmacokinetics in humans. Following intravenous administration of 1.5 g/m2 over 0.5 hour once daily for 5 days to 15 patients with neoplastic disease, a decrease in the median elimination half-life from 7.2 hours on Day 1 to 4.6 hours on Day 5 occurred with a concomitant increase in the median clearance from 66 mL/min on Day 1 to 115 mL/min on Day 5. There was no significant change in the volume of distribution on Day 5 compared with Day 1.
Distribution
Ifosfamide volume of distribution (Vd) approximates the total body water volume, suggesting that distribution takes place with minimal tissue binding. Following intravenous administration of 1.5 g/m2 over 0.5 hour once daily for 5 days to 15 patients with neoplastic disease, the median Vd of ifosfamide was 0.64 L/kg on Day 1 and 0.72 L/kg on Day 5. Ifosfamide shows little plasma protein binding. Ifosfamide and its active metabolites are extensively bound by red blood cells. Ifosfamide is not a substrate for P-glycoprotein.
Metabolism
Ifosfamide is extensively metabolized in humans through two metabolic pathways: ring oxidation (“activation”) to form the active metabolite, 4-hydroxy-ifosfamide and side-chain oxidation to form the inactive metabolites, 3-dechloro-ethylifosfamide or 2-dechloroethylifosfamide with liberation of the toxic metabolite, chloroacetaldehyde.
Small quantities (nmol/mL) of ifosfamide mustard and 4-hydroxyifosfamide are detectable in human plasma. Metabolism of ifosfamide is required for the generation of the biologically active species and while metabolism is extensive, it is also quite variable among patients.
Excretion
After administration of doses of 5 g/m2 of 14C-labeled ifosfamide, from 70% to 86% of the dosed radioactivity was recovered in urine as metabolites, with about 61% of the dose excreted as parent compound. At doses of 1.6 to 2.4 g/m2 only 12% to 18% of the dose was excreted in the urine as unchanged drug within 72 hours.
Two different dechloroethylated derivatives of ifosfamide, 4-carboxyifosfamide, thiodiacetic acid and cysteine conjugates of chloroacetic acid have been identifi ed as the major urinary metabolites of ifosfamide in humans and only small amounts of 4-hydroxyifosfamide and acrolein are present.
Pediatrics
Population PK analysis was performed on plasma data from 32 pediatric patients various malignant diseases aged between 1 and 18 years. Patients received a total of 45 courses of ifosfamide at doses of 1.2, 2 and 3 g/m2 given intravenously over 1 or 3 hours on 1, 2, or 3 days. The mean ± standard error population estimates for the initial clearance and volume of distribution of ifosfamide were 2.4±0.33 L/h/m2 and 21±1.6 L/m2with an interindividual variability of 43% and 32%, respectively.
Effect of Age
A study of 20 patients between 40 to 71 years of age receiving 1.5 g/m2 of ifosfamide daily for 3 or 5 days indicated that elimination half-life appears to increase with age. The elimination half-life increase appeared to be related to the increase in ifosfamide volume of distribution with age. No significant changes in total plasma clearance or renal clearance with age were reported.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Ifosfamide has been shown to be carcinogenic in rats when administered by intraperitoneal injection at 6 mg/kg (37 mg/m2, or about 3% of the daily human dose on a mg/m2 basis) 3 times a week for 52 weeks. Female rats had a signifi cantly higher incidence of uterine leiomyosarcomas and mammary fibroadenomas than vehicle controls.
The mutagenic potential of ifosfamide has been documented in bacterial systems in vitro and mammalian cells in vivo. In vivo, ifosfamide has induced mutagenic effects in mice and Drosophila melanogaster germ cells, and has induced a significant increase in dominant lethal mutations in male mice as well as recessive sex-linked lethal mutations in Drosophila.
Ifosfamide was administered to male and female beagle dogs at doses of 1 or 4.64 mg/kg/day (20 or 93 mg/m2) orally 6 days a week for 26 weeks. Male dogs at 4.64 mg/kg (about 7.7% of the daily clinical dose on a mg/m2 basis) had testicular atrophy with degeneration of the seminiferous tubular epithelium. In a second study, male and female rats were given 0, 25, 50, or 100 mg/kg (0, 150, 300, or 600 mg/m2) ifosfamide intraperitoneally once every 3 weeks for 6 months. Decreased spermatogenesis was observed in most male rats given 100 mg/kg (about half the daily clinical dose on a mg/m2 basis).
-
14 CLINICAL STUDIES
Patients with refractory testicular cancer (n=59) received a combination of ifosfamide, cisplatin, and either etoposide (VePesid®) or vinblastine (VIP) as third-line therapy or later. The selection of etoposide or vinblastine (“V” in the VIP regimen) was guided by the therapeutic effect achieved with prior regimens. The contribution of ifosfamide to the VIP combination was determined in patients treated with cisplatin-etoposide prior to ifosfamide-cisplatin-etoposide or those who received cisplatin-vinblastine prior to ifosfamide-cisplatin-vinblastine.
A total of 59 patients received a third-line salvage regimen which consisted of ifosfamide 1.2 g/m2/day intravenously on days 1 to 5, cisplatin 20 mg/m2/day intravenously on days 1 to 5, and either etoposide 75 mg/m2/day intravenously on days 1 to 5 or vinblastine 0.22 mg/kg intravenously on day 1. Efficacy results with the VIP regimen were compared to data pooled from six single agent phase II trials conducted between August 1980 and October 1985 including a total of 90 patients of whom 65 were eligible as controls of this study. Twenty-three patients in the VIP regimen became free of disease with VIP alone or VIP plus surgery, whereas a single patient in the historical control group achieved complete response. The median survival time exceeded two years in the VIP group versus less than one year in the control group.
Performance status ≥ 80, embryonal carcinoma and minimal disease were favorable prognostic factors for survival. In all prognostic categories, the difference between VIP and historical controls remained highly significant.
Number. (%) of Patients p-value VIP Control Total Patients 59 (100) 65 (100) Disease-free 23 (39) 1 (2) < 0.001 Chemotherapy alone 15 (25) 1 (2) < 0.001 Chemotherapy plus surgery 8 (14) 0 Overall Response 32 (54) 2 (3) < 0.001 Time to progression (weeks) Median 19 4 < 0.001a Range 1 to 205+ 1 to 29 Disease-free interval (weeks) Median 114 29 Range 13 to 205+ -- Survival (weeks) Median 53 10 < 0.001a Range 1 to 205+ 1 to 123+ a: Gehan-Breslow and Mantel-Cox tests
In a study, 50 fully evaluable patients with germ cell testicular cancer were treated with ifosfamide in combination with cisplatin and either vinblastine or etoposide after failing (47 of 50 patients) at least two prior chemotherapy regimens consisting of cisplatin/vinblastine/bleomycin, (PVB), cisplatin/vinblastine/actinomycin D/bleomycin/cyclophosphamide, (VAB6), or the combination of cisplatin and etoposide. Patients were selected for remaining cisplatin sensitivity because they had previously responded to a cisplatin containing regimen and had not progressed while on the cisplatin containing regimen or within 3 weeks of stopping it. Patients served as their own control based on the premise that long term complete responses could not be achieved by retreatment with a regimen to which they had previously responded and subsequently relapsed.
Ten of 50 fully evaluable patients were still alive 2 to 5 years after treatment. Four of the 10 long term survivors were rendered free of cancer by surgical resection after treatment with the ifosfamide regimen; median survival for the entire group of 50 fully evaluable patients was 53 weeks.
-
15 REFERENCES
1. NIOSH Alert: Preventing occupational exposures to antineoplastic and other hazardous drugs in healthcare settings. 2004. U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, DHHS (NIOSH) Publication No. 2004-165.
2. OSHA Technical Manual, TED 1-0.15A, Section VI: Chapter 2. Controlling occupational exposure to hazardous drugs. OSHA, 1999. http://www.osha.gov/dts/osta/otm/otm_vi/otm_vi_2.html
3. American Society of Health-System Pharmacists. ASHP guidelines on handling hazardous drugs. Am JHealth-Syst Pharm. 2006; 63:1172-1193.
4. Polovich M, White JM, Kelleher LO, (eds.) 2005. Chemotherapy and biotherapy guidelines and recommendations for practice. (2nd ed.) Pittsburgh, PA: Oncology Nursing Society.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
Ifosfamide Injection is available in single-dose vials as follows:
NDC 0143-9531-01 – 1 g/20 mL Single Dose Vial of ifosfamide; individually-boxed.
NDC 0143-9530-01 – 3 g/60 mL Single Dose Vial of ifosfamide; individually-boxed.
Store in a refrigerator 2°C to 8°C (36°F to 46°F). See USP.
Exercise caution when handling ifosfamide. The handling and preparation of ifosfamide should always be in accordance with current guidelines on safe handling of cytotoxic agents. Several guidelines on this subject have been published.1-4 Skin reactions associated with accidental exposure to ifosfamide may occur. To minimize the risk of dermal exposure, always wear impervious gloves when handling vials and solutions containing ifosfamide. If ifosfamide solution contacts the skin or mucosa, immediately wash the skin thoroughly with soap and water or rinse the mucosa with copious amounts of water.
-
17 PATIENT COUNSELING INFORMATION
Myelosuppression, Immunosuppression, and Infections
- Advise patients that treatment with ifosfamide injection may cause myelosuppression which can be severe and lead to infections and fatal outcomes.
- Inform patients of the risks associated with the use of ifosfamide injection and plan for regular blood monitoring during therapy [see Boxed Warning, Warnings and Precautions (5.1)]
- Inform patients to report fever or other symptoms of an infection [see Boxed Warning, Warnings and Precautions (5.1), Adverse Reactions (6.2)].
- Advise patients on the risks of bleeding and anemia [see Warnings and Precautions (5.1, 5.8), Adverse Reactions (6.2)], Use in Specific Populations (8.1)].
Central Nervous System Toxicity, Neurotoxicity
- Advise patients on the risk of CNS toxicity and other neurotoxic effects with fatal outcome [see Boxed Warning, Warnings and Precautions (5.2)].
Renal and Urothelial Toxicity and Effects
- Advise patients on the risk of bladder and kidney toxicity.
- Advise patients of the need to increase fluid intake and frequent voiding to prevent accumulation in the bladder [see Warnings and Precautions (5.3)].
Cardiotoxicity
- Advise patients on the risk of cardiotoxicity and fatal outcome. Advise patients to report preexisting cardiac disease and manifestations of cardiotoxicity [see Warnings and Precautions (5.4), Adverse Reactions (6.2)].
Pulmonary Toxicity
- Advise patients on the risk of pulmonary toxicity leading to respiratory failure with fatal outcome.
- Inform patients to report signs and symptoms of pulmonary toxicity [see Warnings and Precautions (5.5)].
Secondary Malignancies
- Advise patients on the risk of secondary malignancies due to therapy [see Warnings and Precautions (5.6)].
Veno-occlusive Liver Disease
- Advise patients on the risk of veno-occlusive liver disease [see Warnings and Precautions (5.7)].
Pregnancy
- Advise patients on the potential hazard to a fetus if a patient becomes pregnant or fathers a child during therapy and for up to 6 months after therapy.
- Advise patients to use effective contraception during therapy and for up to 6 months after therapy [see Warnings and Precautions (5.8), Adverse Reactions (6.2)].
Lactation
- Advise patients on the potential for serious adverse reactions and tumorigenicity when children are breastfed during therapy [see Use in Specific Populations (8.3)].
Reproductive System Disorders
- Advise patients on the risk of amenorrhea, premature menopause, and sterility [see Warnings and Precautions (5.9), Adverse Reactions (6.2)].
Skin and Subcutaneous Tissue Disorders
- Advise patients on the risk of alopecia, wound healing, and other serious skin and subcutaneous tissue disorders [see Warnings and Precautions (5.11), Adverse Reactions (6.2)].
Gastrointestinal Disorders
- Advise patients that the therapy may cause gastrointestinal disorders and alcohol may increase nausea and vomiting [see Adverse Reactions (6.2)].
- Advise patients on the risk of stomatitis and the importance of proper oral hygiene [see Adverse Reactions (6.2)].
Eye Disorders
- Advise patients on the risk of eye disorders such as visual impairment, blurred vision, and eye irritation [see Adverse Reactions (6.2)].
Ear and Labyrinth Disorders
- Advise patients on the risk of ear and labyrinth disorders such as deafness, vertigo, and tinnitus [see Adverse Reactions (6.2)].
Manufactured by:
THYMOORGAN PHARMAZIE GmbH,
Schiffgraben 23, 38690 Goslar, Germany
Distributed by:
West-Ward Pharmaceuticals
Eatontown, NJ 07724 USA
Revised: March 2019
127.207.010/02
-
PACKAGE/LABEL PRINCIPAL DISPLAY PANEL
NDC: 0143-9531-01
Rx only
IFOSFAMIDE INJECTION
1 g/20 mL
(50 mg/mL)
FOR INTRAVENOUS USE
Cytotoxic Agent
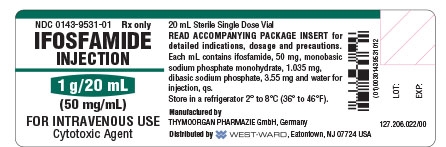
Vial label for Ifosfamide Injection 1 g/20 mL
-
PACKAGE/LABEL PRINCIPAL DISPLAY PANEL
NDC: 0143-9530-01
Rx only
IFOSFAMIDE INJECTION
3 g/60 mL
(50 mg/mL)
FOR INTRAVENOUS USE
Cytotoxic Agent
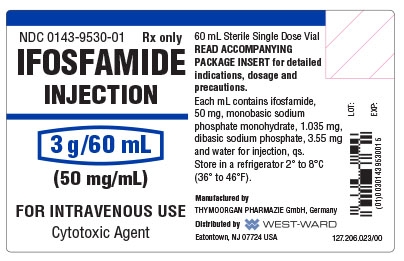
Vial label for Ifosfamide Injection 60 mL
- CARTON SERIALIZATION IMAGE
-
INGREDIENTS AND APPEARANCE
IFOSFAMIDE
ifosfamide injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0143-9531 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength IFOSFAMIDE (UNII: UM20QQM95Y) (IFOSFAMIDE - UNII:UM20QQM95Y) IFOSFAMIDE 50 mg in 1 mL Inactive Ingredients Ingredient Name Strength SODIUM PHOSPHATE, MONOBASIC, MONOHYDRATE (UNII: 593YOG76RN) 1.035 mg in 1 mL SODIUM PHOSPHATE, DIBASIC (UNII: GR686LBA74) 3.55 mg in 1 mL WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0143-9531-01 1 in 1 BOX 06/10/2017 1 20 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA076619 06/10/2017 IFOSFAMIDE
ifosfamide injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0143-9530 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength IFOSFAMIDE (UNII: UM20QQM95Y) (IFOSFAMIDE - UNII:UM20QQM95Y) IFOSFAMIDE 50 mg in 1 mL Inactive Ingredients Ingredient Name Strength SODIUM PHOSPHATE, MONOBASIC, MONOHYDRATE (UNII: 593YOG76RN) 1.035 mg in 1 mL SODIUM PHOSPHATE, DIBASIC (UNII: GR686LBA74) 3.55 mg in 1 mL WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0143-9530-01 1 in 1 BOX 06/10/2017 1 60 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA076619 06/10/2017 Labeler - Hikma Pharmaceuticals USA Inc. (001230762)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.