TOUJEO- insulin glargine injection, solution TOUJEO MAX- insulin glargine injection, solution
TOUJEO Max by
Drug Labeling and Warnings
TOUJEO Max by is a Prescription medication manufactured, distributed, or labeled by Sanofi-Aventis U.S. LLC, Sanofi-Aventis Deutschland GmbH, Genzyme Corporation. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use TOUJEO safely and effectively. See full prescribing information for TOUJEO®.
TOUJEO (insulin glargine injection) U-300, for subcutaneous use
Initial U.S. Approval: 2015RECENT MAJOR CHANGES
INDICATIONS AND USAGE
DOSAGE AND ADMINISTRATION
- Individualize dose based on type of diabetes, metabolic needs, blood glucose monitoring results and glycemic control goal. (2.1, 2.2, 2.3)
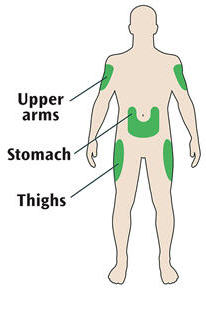
- Administer subcutaneously into the abdominal area, thigh, or deltoid once daily at any time during the day, at the same time every day. (2.1)
- Rotate injection sites to reduce risk of lipodystrophy and localized cutaneous amyloidosis. (2.1)
- Do not dilute or mix with any other insulin or solution. (2.1)
- Closely monitor glucose when changing to TOUJEO and during initial weeks thereafter. (2.4)
DOSAGE FORMS AND STRENGTHS
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- Never share a TOUJEO SoloStar or TOUJEO Max SoloStar single-patient-use prefilled pen between patients, even if the needle is changed. (5.1)
- Hyperglycemia or hypoglycemia with changes in insulin regimen: Make changes to a patient's insulin regimen (e.g., insulin strength, manufacturer, type, injection site, or method of administration) under close medical supervision with increased frequency of blood glucose monitoring. (5.2)
- Hypoglycemia: May be life-threatening. Increase frequency of glucose monitoring with changes to: insulin dosage, coadministered glucose-lowering medications, meal pattern, physical activity, and in patients with renal impairment or hepatic impairment or hypoglycemia unawareness. (5.3, 6.1)
- Medication errors: Accidental mix-ups between insulin products can occur. Instruct patients to check insulin labels before injection. (5.4)
- Hypersensitivity reactions: Severe, life-threatening, generalized allergy, including anaphylaxis, can occur. Discontinue TOUJEO, monitor and treat if indicated. (5.5, 6.1)
- Hypokalemia: May be life-threatening. Monitor potassium levels in patients at risk of hypokalemia and treat if indicated. (5.6)
- Fluid retention and heart failure with concomitant use of Thiazolidinediones (TZDs): Observe for signs and symptoms of heart failure; consider dosage reduction or discontinuation if heart failure occurs. (5.7)
ADVERSE REACTIONS
Adverse reactions commonly associated with TOUJEO (≥5%) are:
- Hypoglycemia, allergic reactions, injection site reaction, lipodystrophy, pruritus, rash, edema, and weight gain. (6.1, 6.2)
To report SUSPECTED ADVERSE REACTIONS, contact sanofi-aventis at 1-800-633-1610 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 12/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Important Administration Instructions
2.2 General Dosing Instructions
2.3 Starting Dose in Insulin-Naive Pediatric and Adult Patients
2.4 Starting Dose in Pediatric and Adult Patients with Either Type 1 or Type 2 Diabetes Already on Insulin Therapy
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Never Share a TOUJEO SoloStar or TOUJEO Max SoloStar Pen Between Patients
5.2 Hyperglycemia or Hypoglycemia with Changes in Insulin Regimen
5.3 Hypoglycemia
5.4 Medication Errors
5.5 Hypersensitivity and Allergic Reactions
5.6 Hypokalemia
5.7 Fluid Retention and Heart Failure with Concomitant Use of PPAR-gamma Agonists
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Immunogenicity
6.3 Postmarketing Experience
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Hepatic Impairment
8.7 Renal Impairment
8.8 Obesity
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Overview of Clinical Studies
14.2 Clinical Study in Adult and Pediatric Patients with Type 1 Diabetes
14.3 Clinical Studies in Adult Patients with Type 2 Diabetes
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
16.2 Storage
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 Important Administration Instructions
- Always check insulin labels before administration [see Warnings and Precautions (5.4)].
- Visually inspect the TOUJEO solution for particulate matter and discoloration prior to administration and only use if the solution is clear and colorless with no visible particles.
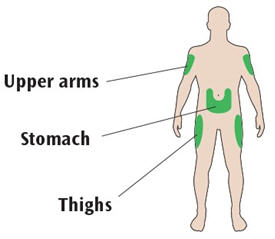
- Inject TOUJEO subcutaneously into the abdominal area, thigh, or deltoid.
- Rotate injection sites within the same region from one injection to the next to reduce the risk of lipodystrophy and localized cutaneous amyloidosis. Do not inject into areas of lipodystrophy or localized cutaneous amyloidosis [see Warnings and Precautions (5.2), Adverse Reactions (6)].
- Use TOUJEO with caution in patients with visual impairment who may rely on audible clicks to dial their dose.
- Do not administer TOUJEO intravenously or in an insulin pump.
- Do not dilute or mix TOUJEO with any other insulin products or solutions.
- Never transfer TOUJEO from the cartridges of the TOUJEO SoloStar or TOUJEO Max SoloStar prefilled pen into a syringe for administration [see Warnings and Precautions (5.4)].
2.2 General Dosing Instructions
- TOUJEO is available in 2 single-patient-use prefilled pens:
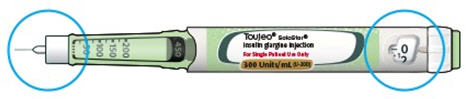
- TOUJEO SoloStar contains 450 units of TOUJEO U-300. It delivers doses in 1 unit increments and can deliver up to 80 units in a single injection.
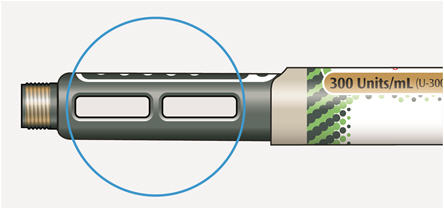
- TOUJEO Max SoloStar contains 900 units of TOUJEO U-300. It delivers doses in 2 unit increments and can deliver up to 160 units in a single injection. It is recommended for patients requiring at least 20 units per day.
- When changing between TOUJEO SoloStar and TOUJEO Max SoloStar, if the patient's previous dose was an odd number, the dose should be increased or decreased by 1 unit.
- The dose counter of the TOUJEO SoloStar or TOUJEO Max SoloStar prefilled pen shows the number of units of TOUJEO to be injected and no conversion is required.
- Inject TOUJEO subcutaneously once a day at the same time of day.
- During changes to a patient's insulin regimen, increase the frequency of blood glucose monitoring [see Warnings and Precautions (5.2)].
- Individualize and titrate the dosage of TOUJEO based on the individual's metabolic needs, blood glucose monitoring results, and glycemic control goal.
- Titrate the dose of TOUJEO no more frequently than every 3 to 4 days.
- Dosage adjustments may be needed with changes in physical activity, changes in meal patterns (i.e., macronutrient content or timing of food intake), changes in renal or hepatic function or during acute illness to minimize the risk of hypoglycemia or hyperglycemia [see Warnings and Precautions (5.2) and Use in Specific Populations (8.6, 8.7)].
2.3 Starting Dose in Insulin-Naive Pediatric and Adult Patients
Type 1 Diabetes
- The recommended starting dose of TOUJEO in insulin-naive patients with type 1 diabetes is approximately one-third to one-half of the total daily insulin dose. The remainder of the total daily insulin dose should be given as a short-acting insulin and divided between each daily meal. As a general rule, 0.2 to 0.4 units of insulin per kilogram of body weight can be used to calculate the initial total daily insulin dose in insulin-naive patients with type 1 diabetes.
- The maximum glucose lowering effect of a dose of TOUJEO may take five days to fully manifest and the first TOUJEO dose may be insufficient to cover metabolic needs in the first 24 hours of use [see Clinical Pharmacology (12.2)]. When initiating TOUJEO, monitor glucose daily.
2.4 Starting Dose in Pediatric and Adult Patients with Either Type 1 or Type 2 Diabetes Already on Insulin Therapy
- For patients currently on once-daily long or intermediate-acting insulin, start TOUJEO at the same unit dose as the once-daily long-acting insulin dose. For patients controlled on LANTUS (insulin glargine, 100 units/mL), expect that a higher daily dose of TOUJEO will be needed to maintain the same level of glycemic control [see Clinical Pharmacology (12.2) and Clinical Studies (14.1)].
- For patients currently on twice-daily long or intermediate-acting insulin, start TOUJEO at 80% of the total daily NPH or insulin detemir twice-daily dosage.
- When changing patients to TOUJEO, monitor glucose frequently in the first weeks of therapy [see Warnings and Precautions (5.2) and Clinical Pharmacology (12.2)].
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
TOUJEO is contraindicated:
- During episodes of hypoglycemia [see Warnings and Precautions (5.3)].
- In patients with hypersensitivity to insulin glargine or one of its excipients [see Warnings and Precautions (5.5)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Never Share a TOUJEO SoloStar or TOUJEO Max SoloStar Pen Between Patients
TOUJEO SoloStar or TOUJEO Max SoloStar single-patient-use prefilled pens must never be shared between patients, even if the needle is changed. Pen sharing poses a risk for transmission of blood-borne pathogens.
5.2 Hyperglycemia or Hypoglycemia with Changes in Insulin Regimen
Changes in Insulin Regimen Including Changes to Administration Site
Changes in an insulin regimen (e.g., insulin strength, manufacturer, type, injection site, or method of administration) may affect glycemic control and predispose to hypoglycemia [see Warnings and Precautions (5.3)] or hyperglycemia. Repeated insulin injections into areas of lipodystrophy or localized cutaneous amyloidosis have been reported to result in hyperglycemia, and a sudden change in the injection site (to unaffected area) has been reported to result in hypoglycemia [see Adverse Reactions (6)].
Make any changes to a patient's insulin regimen under close medical supervision with increased frequency of blood glucose monitoring. Advise patients who have repeatedly injected into areas of lipodystrophy or localized cutaneous amyloidosis to change the injection site to unaffected areas and closely monitor for hypoglycemia. For patients with type 2 diabetes, dosage adjustments of concomitant oral antidiabetic products may be needed.
Changing to TOUJEO from other Insulins
On a unit-to-unit basis, TOUJEO has a lower glucose lowering effect than LANTUS [see Clinical Pharmacology (12.2)]. In clinical trials, patients who changed to TOUJEO from other basal insulins experienced higher average fasting plasma glucose levels in the first weeks of therapy compared to patients who were changed to LANTUS. Higher doses of TOUJEO were required to achieve similar levels of glucose control compared to LANTUS in clinical trials [see Clinical Studies (14.1)].
The onset of action of TOUJEO develops over 6 hours following an injection. In type 1 diabetes patients treated with IV insulin, consider the longer onset of action of TOUJEO before stopping IV insulin. The full glucose lowering effect may not be apparent for at least 5 days [see Dosage and Administration (2.2) and Clinical Pharmacology (12.2)].
To minimize the risk of hyperglycemia when initiating TOUJEO monitor glucose daily, titrate TOUJEO as described in this prescribing information, and adjust coadministered glucose-lowering therapies per standard of care [see Dosage and Administration (2.2, 2.3)].
5.3 Hypoglycemia
Hypoglycemia is the most common adverse reaction associated with insulin, including TOUJEO. Severe hypoglycemia can cause seizures, may be life-threatening, or cause death. Hypoglycemia can impair concentration ability and reaction time; this may place an individual and others at risk in situations where these abilities are important (e.g., driving, or operating other machinery). Hypoglycemia can happen suddenly and symptoms may differ in each individual and change over time in the same individual. Symptomatic awareness of hypoglycemia may be less pronounced in patients with longstanding diabetes, in patients with diabetic nerve disease, in patients using medications that block the sympathetic nervous system (e.g., beta-blockers) [see Drug Interactions (7)], or in patients who experience recurrent hypoglycemia.
Risk Factors for Hypoglycemia
The timing of hypoglycemia usually reflects the time-action profile of the administered insulin formulation. As with all insulin preparations, the glucose lowering effect time course of TOUJEO may vary in different individuals or at different times in the same individual and depends on many conditions, including the area of injection as well as the injection site blood supply and temperature [see Clinical Pharmacology (12.2)]. Other factors which may increase the risk of hypoglycemia include changes in meal pattern (e.g., macronutrient content or timing of meals), changes in level of physical activity, or changes to coadministered medication [see Drug Interactions (7)]. Patients with renal or hepatic impairment may be at higher risk of hypoglycemia [see Use in Specific Populations (8.6, 8.7)].
Risk Mitigation Strategies for Hypoglycemia
Patients and caregivers must be educated to recognize and manage hypoglycemia. Self-monitoring of blood glucose plays an essential role in the prevention and management of hypoglycemia. In patients at higher risk for hypoglycemia and patients who have reduced symptomatic awareness of hypoglycemia, increased frequency of blood glucose monitoring is recommended. To minimize the risk of hypoglycemia, do not administer TOUJEO intravenously, intramuscularly or in an insulin pump, or dilute or mix TOUJEO with any other insulin products or solutions.
5.4 Medication Errors
Accidental mix-ups between basal insulin products and other insulins, particularly rapid-acting insulins, have been reported. To avoid medication errors between TOUJEO and other insulins, instruct patients to always check the insulin label before each injection.
To avoid dosing errors and potential overdose, never use a syringe to remove TOUJEO from the TOUJEO SoloStar or TOUJEO Max SoloStar prefilled pen into a syringe [see Dosage and Administration (2.4) and Warnings and Precautions (5.3)].
5.5 Hypersensitivity and Allergic Reactions
Severe, life-threatening, generalized allergy, including anaphylaxis, can occur with insulin products, including TOUJEO. If hypersensitivity reactions occur, discontinue TOUJEO; treat per standard of care and monitor until symptoms and signs resolve [see Adverse Reactions (6)]. TOUJEO is contraindicated in patients who have had hypersensitivity reactions to insulin glargine or other of the excipients [see Contraindications (4)].
5.6 Hypokalemia
All insulin products, including TOUJEO, cause a shift in potassium from the extracellular to intracellular space, possibly leading to hypokalemia. Untreated hypokalemia may cause respiratory paralysis, ventricular arrhythmia, and death. Monitor potassium levels in patients at risk for hypokalemia, if indicated (e.g., patients using potassium-lowering medications, patients taking medications sensitive to serum potassium concentrations).
5.7 Fluid Retention and Heart Failure with Concomitant Use of PPAR-gamma Agonists
Thiazolidinediones (TZDs), which are peroxisome proliferator-activated receptor (PPAR)-gamma agonists, can cause dose-related fluid retention, particularly when used in combination with insulin. Fluid retention may lead to or exacerbate heart failure. Patients treated with insulin, including TOUJEO, and a PPAR-gamma agonist should be observed for signs and symptoms of heart failure. If heart failure develops, it should be managed according to current standards of care, and discontinuation or dose reduction of the PPAR-gamma agonist must be considered.
-
6 ADVERSE REACTIONS
The following adverse reactions are discussed elsewhere:
- Hypoglycemia [see Warnings and Precautions (5.3)]
- Medication errors [see Warnings and Precautions (5.4)]
- Hypersensitivity and allergic reactions [see Warnings and Precautions (5.5)]
- Hypokalemia [see Warnings and Precautions (5.6)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug, and may not reflect the rates actually observed in clinical practice.
The data in Table 1 reflect the exposure of 304 patients with type 1 diabetes to TOUJEO with mean exposure duration of 23 weeks. The type 1 diabetes population had the following characteristics: Mean age was 46 years and mean duration of diabetes was 21 years. Fifty-five percent were male, 86% were Caucasian, 5% were Black or African American, and 5% were Hispanic. At baseline, the mean eGFR was 82 mL/min/1.73 m2 and 35% of patients had eGFR ≥90 mL/min/1.73 m2. The mean BMI was 28 kg/m2. HbA1c at baseline was greater or equal to 8% in 58% of patients.
The data in Table 2 reflect the exposure of 1242 patients with type 2 diabetes to TOUJEO with mean exposure duration of 25 weeks. The type 2 diabetes population had the following characteristics: Mean age was 59 years and mean duration of diabetes was 13 years. Fifty-three percent were male, 88% were Caucasian, 7% were Black or African American, and 17% were Hispanic. At baseline, mean eGFR was 79 mL/min/1.73 m2 and 27% of patients had an eGFR ≥90 mL/min/1.73 m2. The mean BMI was 35 kg/m2. HbA1c at baseline was greater or equal to 8% in 66% of patients.
TOUJEO was studied in 233 pediatric patients (6–17 years of age) with type 1 diabetes for a mean duration of 26 weeks [See Clinical Studies (14.1)].
Common adverse reactions (occurring ≥5%) in TOUJEO-treated subjects during clinical trials in adult patients with type 1 diabetes mellitus and type 2 diabetes mellitus are listed in Table 1 and Table 2, respectively. Common adverse reactions for TOUJEO-treated pediatric subjects with type 1 diabetes mellitus were similar to the adverse reactions listed in Table 1. Hypoglycemia is discussed in a dedicated subsection below.
Table 1: Adverse Reactions in Two Pooled Clinical Trials of 26 Weeks and 16 Weeks Duration in Adults with Type 1 Diabetes (with incidence ≥5%) TOUJEO + Mealtime Insulin*, %
(n=304)- * "mealtime insulin" refers to insulin glulisine, insulin lispro, or insulin aspart.
Nasopharyngitis 12.8 Upper respiratory tract infection 9.5 Table 2: Adverse Reactions in Three Pooled Clinical Trials of 26 Weeks Duration in Adults with Type 2 Diabetes (with incidence ≥5%) TOUJEO*, %
(n=1242)- * one of the trials in type 2 diabetes included mealtime insulin.
Nasopharyngitis 7.1 Upper respiratory tract infection 5.7 Hypoglycemia
Hypoglycemia is the most commonly observed adverse reaction in patients using insulin, including TOUJEO [see Warnings and Precautions (5.3)]. The rates of reported hypoglycemia depend on the definition of hypoglycemia used, diabetes type, insulin dose, intensity of glucose control, background therapies, and other intrinsic and extrinsic patient factors. For these reasons, comparing rates of hypoglycemia in clinical trials for TOUJEO with the incidence of hypoglycemia for other products may be misleading and also may not be representative of hypoglycemia rates that will occur in clinical practice.
In the TOUJEO adult program, severe hypoglycemia was defined as an event requiring assistance of another person to administer a resuscitative action. In the pediatric program, severe hypoglycemia was defined as an event with semiconsciousness, unconsciousness, coma and/or convulsions in a patient who had altered mental status and could not assist in his own care, and who may have required glucagon or intravenous glucose.
The incidence of severe hypoglycemia in adult patients with type 1 diabetes receiving TOUJEO as part of a multiple daily injection regimen was 6.6% at 26 weeks. The incidence of hypoglycemia with a glucose level less than 54 mg/dL with or without symptoms was 77.7% at 26 weeks.
The incidence of severe hypoglycemia in pediatric patients with type 1 diabetes receiving TOUJEO as part of a multiple daily injection regimen was 6% at 26 weeks and the incidence of hypoglycemia accompanied by a self-monitored or plasma glucose value less than 54 mg/dL regardless of symptoms was 80.3%.
The incidence of severe hypoglycemia in adult patients with type 2 diabetes was 5% at 26 weeks in patients receiving TOUJEO as part of a multiple daily injection regimen, and 1.0% and 0.9% respectively at 26 weeks in the two studies where patients received TOUJEO as part of a basal-insulin only regimen. The incidence of hypoglycemia accompanied by a self-monitored or plasma glucose value less than 54 mg/dL regardless of symptoms in patients with type 2 diabetes receiving TOUJEO ranged from 9% to 44.6% at 26 weeks and the highest risk was again seen in patients receiving TOUJEO as part of a multiple daily injection regimen.
Insulin Initiation and Intensification of Glucose Control
Intensification or rapid improvement in glucose control has been associated with a transitory, reversible ophthalmologic refraction disorder, worsening of diabetic retinopathy, and acute painful peripheral neuropathy. However, long-term glycemic control decreases the risk of diabetic retinopathy and neuropathy.
Peripheral Edema
Insulin, including TOUJEO, may cause sodium retention and edema, particularly if previously poor metabolic control is improved by intensified insulin therapy.
Lipodystrophy
Long-term use of insulin, including TOUJEO, can cause lipoatrophy (depression in the skin) or lipohypertrophy (enlargement or thickening of tissue) in some patients and may affect insulin absorption [see Dosage and Administration (2.1)].
Weight Gain
Weight gain has occurred with some insulin therapies including TOUJEO and has been attributed to the anabolic effects of insulin and the decrease in glucosuria.
Allergic Reactions
Some patients taking insulin therapy, including TOUJEO have experienced erythema, local edema, and pruritus at the site of injection. These conditions were usually self-limiting.
Severe cases of generalized allergy (anaphylaxis) have been reported [see Warnings and Precautions (5.5)].
Cardiovascular Safety
No clinical studies to establish the cardiovascular safety of TOUJEO have been conducted. A cardiovascular outcomes trial, ORIGIN, has been conducted with LANTUS. It is unknown whether the results of ORIGIN can be applied to TOUJEO.
The Outcome Reduction with Initial Glargine Intervention trial (i.e., ORIGIN) was an open-label, randomized, 12,537 patient study that compared LANTUS to standard care on the time to first occurrence of a major adverse cardiovascular event (MACE). MACE was defined as the composite of CV death, nonfatal myocardial infarction and nonfatal stroke. The incidence of MACE was similar between LANTUS and standard care in ORIGIN (Hazard Ratio [95% CI] for MACE; 1.02 [0.94, 1.11]).
In the ORIGIN trial, the overall incidence of cancer (all types combined) (Hazard Ratio [95% CI]; 0.99 [0.88, 1.11]) or death from cancer (Hazard Ratio [95% CI]; 0.94 [0.77, 1.15]) was also similar between treatment groups.
6.2 Immunogenicity
As with all therapeutic proteins, there is potential for immunogenicity.
In a 6-month study of type 1 diabetes patients, 79% of patients who received TOUJEO once daily were positive for anti-insulin antibodies (AIA) at least once during the study, including 62% that were positive at baseline and 44% of patients who developed antidrug antibody (i.e., anti-insulin glargine antibody [ADA]) during the study. Eighty percent of the AIA-positive patients on TOUJEO with antibody test at baseline remained AIA positive at month 6.
In two 6-month studies in type 2 diabetes patients, 25% of patients who received TOUJEO once daily were positive for AIA at least once during the study, including 42% who were positive at baseline and 20% of patients who developed ADA during the study. Ninety percent of the AIA-positive patients on TOUJEO with antibody test at baseline, remained AIA positive at month 6.
The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay and may be influenced by several factors such as: assay methodology, sample handling, timing of sample collection, concomitant medication, and underlying disease. For these reasons, comparison of the incidence of antibodies to TOUJEO with the incidence of antibodies in other studies or to other products may be misleading.
6.3 Postmarketing Experience
The following additional adverse reactions have been identified during postapproval use of TOUJEO. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Localized cutaneous amyloidosis at the injection site has occurred. Hyperglycemia has been reported with repeated insulin injections into areas of localized cutaneous amyloidosis; hypoglycemia has been reported with a sudden change to an unaffected injection site.
-
7 DRUG INTERACTIONS
Table 3 includes clinically significant drug interactions with TOUJEO.
Table 3: Clinically Significant Drug Interactions with TOUJEO Drugs That May Increase the Risk of Hypoglycemia Drugs: Antidiabetic agents, ACE inhibitors, angiotensin II receptor blocking agents, disopyramide, fibrates, fluoxetine, monoamine oxidase inhibitors, pentoxifylline, pramlintide, salicylates, somatostatin analogs (e.g., octreotide), and sulfonamide antibiotics, GLP-1 receptor agonists, DPP-4 inhibitors, and SGLT-2 inhibitors. Intervention: Dose reductions and increased frequency of glucose monitoring may be required when TOUJEO is coadministered with these drugs. Drugs That May Decrease the Blood Glucose Lowering Effect of TOUJEO Drugs: Atypical antipsychotics (e.g., olanzapine and clozapine), corticosteroids, danazol, diuretics, estrogens, glucagon, isoniazid, niacin, oral contraceptives, phenothiazines, progestogens (e.g., in oral contraceptives), protease inhibitors, somatropin, sympathomimetic agents (e.g., albuterol, epinephrine, terbutaline), and thyroid hormones. Intervention: Dose increases and increased frequency of glucose monitoring may be required when TOUJEO is coadministered with these drugs. Drugs That May Increase or Decrease the Blood Glucose Lowering Effect of TOUJEO Drugs: Alcohol, beta-blockers, clonidine, and lithium salts. Pentamidine may cause hypoglycemia, which may sometimes be followed by hyperglycemia. Intervention: Dose adjustment and increased frequency of glucose monitoring may be required when TOUJEO is coadministered with these drugs. Drugs That May Blunt Signs and Symptoms of Hypoglycemia Drugs: Beta-blockers, clonidine, guanethidine, and reserpine. Intervention: Increased frequency of glucose monitoring may be required when TOUJEO is coadministered with these drugs. -
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Published studies with use of insulin glargine during pregnancy have not reported a clear association with insulin glargine and adverse developmental outcomes [see Data]. There are risks to the mother and fetus associated with poorly controlled diabetes in pregnancy [see Clinical Considerations].
Rats and rabbits were exposed to insulin glargine in animal reproduction studies during organogenesis, respectively 50 times and 10 times the human subcutaneous dose of 0.2 unit/kg/day. Overall, the effects of insulin glargine did not generally differ from those observed with regular human insulin [see Data].
The estimated background risk of major birth defects is 6% to 10% in women with pregestational diabetes with an HbA1c >7 and has been reported to be as high as 20% to 25% in women with a HbA1c >10. The estimated background risk of miscarriage for the indicated population is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Clinical Considerations
Disease-associated maternal and/or embryo/fetal risk
Poorly controlled diabetes in pregnancy increases the maternal risk for diabetic ketoacidosis, preeclampsia, spontaneous abortions, preterm delivery, and delivery complications. Poorly controlled diabetes increases the fetal risk for major birth defects, stillbirth, and macrosomia-related morbidity.
Data
Human data
Published data do not report a clear association with insulin glargine and major birth defects, miscarriage, or adverse maternal or fetal outcomes when insulin glargine is used during pregnancy. However, these studies cannot definitely establish the absence of any risk because of methodological limitations including small sample size and some lacking comparator groups.
Animal data
Subcutaneous reproduction and teratology studies have been performed with insulin glargine and regular human insulin in rats and Himalayan rabbits. Insulin glargine was given to female rats before mating, during mating, and throughout pregnancy at doses up to 0.36 mg/kg/day, which is approximately 50 times the recommended human subcutaneous starting dose of 0.2 Units/kg/day (0.007 mg/kg/day). In rabbits, doses of 0.072 mg/kg/day, which is approximately 10 times the recommended human subcutaneous starting dose of 0.2 Units/kg/day (0.007 mg/kg/day), were administered during organogenesis. The effects of insulin glargine did not generally differ from those observed with regular human insulin in rats or rabbits. However, in rabbits, five fetuses from two litters of the high-dose group exhibited dilation of the cerebral ventricles. Fertility and early embryonic development appeared normal.
8.2 Lactation
Risk Summary
There are either no or only limited data on the presence of insulin glargine in human milk, the effects on breastfed infant, or the effects on milk production. Endogenous insulin is present in human milk. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for TOUJEO, and any potential adverse effects on the breastfed child from TOUJEO or from the underlying maternal condition.
8.4 Pediatric Use
The safety and effectiveness of TOUJEO to improve glycemic control in type 1 and type 2 diabetes mellitus have been established in pediatric patients 6 years of age and older.
The use of TOUJEO for this indication is supported by evidence from an adequate and well-controlled study in 463 pediatric patients 6 to 17 years of age with type 1 diabetes mellitus [see Clinical Studies (14.2)] and from studies in adults with diabetes mellitus [see Clinical Pharmacology (12.3), Clinical Studies (14.3)].
The safety and effectiveness of TOUJEO have not been established in pediatric patients less than 6 years of age.
8.5 Geriatric Use
In controlled clinical studies, 30 of 304 (9.8%) TOUJEO-treated patients with type 1 diabetes and 327 of 1242 (26.3%) TOUJEO-treated patients with type 2 diabetes were ≥65 years of age, among them 2.0% of the patients with type 1 and 3.0% of the patients with type 2 diabetes were ≥75 years of age. No overall differences in effectiveness and safety were observed in the subgroup analyses across the age groups.
Nevertheless, caution should be exercised when TOUJEO is administered to geriatric patients. In elderly patients with diabetes, the initial dosing, dose increments, and maintenance dosage should be conservative to avoid hypoglycemia [see Warnings and Precautions (5.3), Adverse Reactions (6), and Clinical Studies (14)].
8.6 Hepatic Impairment
The effect of hepatic impairment on the pharmacokinetics of TOUJEO has not been studied. Frequent glucose monitoring and dose adjustment may be necessary for TOUJEO in patients with hepatic impairment [see Warnings and Precautions (5.3)].
8.7 Renal Impairment
The effect of renal impairment on the pharmacokinetics of TOUJEO has not been studied. Some studies with human insulin have shown increased circulating levels of insulin in patients with renal failure. Frequent glucose monitoring and dose adjustment may be necessary for TOUJEO in patients with renal impairment [see Warnings and Precautions (5.3)].
-
10 OVERDOSAGE
Excess insulin administration may cause hypoglycemia and hypokalemia [see Warnings and Precautions (5.3, 5.6)]. Mild episodes of hypoglycemia can be treated with oral glucose. Adjustments in drug dosage, meal patterns, or physical activity level may be needed. More severe episodes of hypoglycemia with coma, seizure, or neurologic impairment may be treated with intramuscular/subcutaneous glucagon or concentrated intravenous glucose. Sustained carbohydrate intake and observation may be necessary because hypoglycemia may recur after apparent clinical recovery. Hypokalemia must be corrected appropriately.
-
11 DESCRIPTION
TOUJEO (insulin glargine injection) is a long-acting insulin supplied as a sterile solution for subcutaneous injection containing 300 units/mL of insulin glargine.
Insulin glargine is a human insulin analog produced by recombinant DNA technology utilizing a nonpathogenic laboratory strain of Escherichia coli (K12) as the production organism. Insulin glargine differs from human insulin in that the amino acid asparagine at position A21 is replaced by glycine and two arginines remain at the C-terminus of the B-chain. Chemically, insulin glargine is 21A-Gly-31B-32B-Di-Arg-human insulin and has the empirical formula C267H404N72O78S6 and a molecular weight of 6063. Insulin glargine has the following structural formula:

Each milliliter of TOUJEO contains 300 units (10.91 mg) insulin glargine dissolved in a clear aqueous fluid.
The 1.5 mL TOUJEO SoloStar prefilled pen presentation contains the following inactive ingredients per mL: 90 mcg zinc, 2.7 mg m-cresol, 20 mg glycerol 85%, and water for injection.
The 3 mL TOUJEO Max SoloStar prefilled pen presentation contains the following inactive ingredients per mL: 90 mcg zinc, 2.7 mg m-cresol, 20 mg glycerol 85%, and water for injection.
The pH is adjusted by addition of aqueous solutions of hydrochloric acid and sodium hydroxide. TOUJEO has a pH of approximately 4. At pH 4, insulin glargine is completely soluble. After injection into the subcutaneous tissue, the acidic solution is neutralized, leading to formation of a precipitate from which small amounts of insulin glargine are slowly released.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The primary activity of insulin, including insulin glargine, is regulation of glucose metabolism. Insulin and its analogs lower blood glucose by stimulating peripheral glucose uptake, especially by skeletal muscle and fat, and by inhibiting hepatic glucose production. Insulin inhibits lipolysis and proteolysis, and enhances protein synthesis.
12.2 Pharmacodynamics
Onset of Action
The pharmacodynamic profiles for TOUJEO given subcutaneously as a single dose of 0.4, 0.6, or 0.9 U/kg in a euglycemic clamp study in patients with type 1 diabetes showed that on average, the onset of action develops over 6 hours post dose for all three single doses of TOUJEO.
Single-Dose Pharmacodynamics
The pharmacodynamics for single 0.4, 0.6, and 0.9 U/kg doses of TOUJEO in 24 patients with type 1 diabetes mellitus was evaluated in a euglycemic clamp study. On a unit-to-unit basis, TOUJEO had a lower maximum (GIRmax) and 24-hour glucose lowering effect (GIR-AUC0–24) compared to LANTUS. The overall glucose lowering effect of TOUJEO 0.4 U/kg was 12% of the glucose lowering effect of an equivalent dose of LANTUS. Glucose lowering at least 30% of the effect of a single 0.4 U/kg dose of LANTUS was not observed until the single dose of TOUJEO exceeded 0.6 U/kg.
Multiple Once-Daily Dose Pharmacodynamics
The pharmacodynamics of TOUJEO after 8 days of daily injection was evaluated in 30 patients with type 1 diabetes. At steady state, the 24-hour glucose lowering effect (GIR-AUC0–24) of TOUJEO 0.4 U/kg was approximately 27% lower with a different distribution profile than that of an equivalent dose of LANTUS [see Dosage and Administration (2), Warnings and Precautions (5.2), and Clinical Pharmacology (12.3)]. The glucose lowering effect of a TOUJEO dose increased with each daily administration.
The pharmacodynamic profile for TOUJEO given subcutaneously as multiple once-daily subcutaneous injections of 0.4 U/kg in a euglycemic clamp study in patients with type 1 diabetes is shown in Figure 1.
Figure 1: Glucose Infusion Rate in Patients with Type 1 Diabetes in Multiple-Dose Administration of TOUJEO
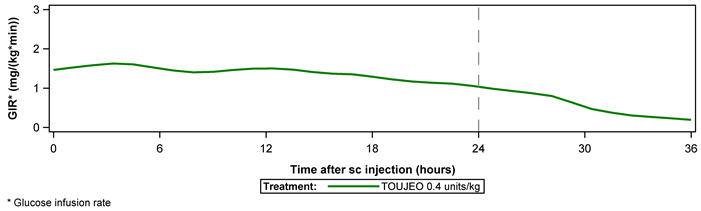
Glucose infusion rate: determined as amount of glucose infused to maintain constant plasma glucose levels.
12.3 Pharmacokinetics
Absorption and Bioavailability
The pharmacokinetic profiles for single 0.4, 0.6, and 0.9 U/kg doses of TOUJEO in 24 patients with type 1 diabetes mellitus was evaluated in a euglycemic clamp study. The median time to maximum serum insulin concentration was 12 (8–14), 12 (12–18), and 16 (12–20) hours, respectively. Mean serum insulin concentrations declined to the lower limit of quantitation of 5.02 µU/mL by 16, 28, and beyond 36 hours, respectively.
Steady-state insulin concentrations are reached by at least 5 days of once-daily subcutaneous administration of 0.4 U/kg to 0.6 U/kg doses of TOUJEO over 8 days in patients with type 1 diabetes mellitus.
After subcutaneous injection of TOUJEO, the intra-subject variability, defined as the coefficient of variation for the insulin exposure during 24 hours, was 21.0% at steady state.
Elimination
After subcutaneous injection of TOUJEO in diabetic patients, insulin glargine is metabolized at the carboxyl terminus of the B-chain with formation of two active metabolites M1 (21A-Gly-insulin) and M2 (21A-Gly-des-30B-Thr-insulin). The in vitro activity of M1 and M2 were similar to that of human insulin.
Specific Populations
Pediatrics
Population pharmacokinetic analysis was conducted for TOUJEO based on concentration data of its main metabolite M1 using data from 75 pediatric patients (6 to <18 years of age) with type 1 diabetes. The findings with regard to the effect of body weight on systemic exposure of M1 are generally consistent with findings in adults.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
In mice and rats, standard two-year carcinogenicity studies with insulin glargine were performed at doses up to 0.455 mg/kg, which was for the rat approximately 65 times the recommended human subcutaneous starting dose of 0.2 Units/kg/day (0.007 mg/kg/day). The findings in female mice were not conclusive due to excessive mortality in all dose groups during the study. Histiocytomas were found at injection sites in male rats (statistically significant) and male mice (not statistically significant) in acid vehicle containing groups. These tumors were not found in female animals, in saline control, or insulin comparator groups using a different vehicle. The relevance of these findings to humans is unknown.
Insulin glargine was not mutagenic in tests for detection of gene mutations in bacteria and mammalian cells (Ames and HGPRT test) and in tests for detection of chromosomal aberrations (cytogenetics in vitro in V79 cells and in vivo in Chinese hamsters).
In a combined fertility and prenatal and postnatal study in male and female rats at subcutaneous doses up to 0.36 mg/kg/day, which was approximately 50 times the recommended human subcutaneous starting dose of 0.2 Units/kg/day (0.007 mg/kg/day), maternal toxicity due to dose-dependent hypoglycemia, including some deaths, was observed. Consequently, a reduction of the rearing rate occurred in the high-dose group only. Similar effects were observed with NPH insulin.
-
14 CLINICAL STUDIES
14.1 Overview of Clinical Studies
The safety and effectiveness of TOUJEO given once daily was compared to that of once-daily LANTUS in 26-week, open-label, randomized, active-control, parallel studies of 546 adult patients and 463 pediatric patients with type 1 diabetes mellitus and 2,474 patients with type 2 diabetes mellitus (Tables 4 and 5). At trial end, the reduction in glycated hemoglobin (HbA1c) and fasting plasma glucose with TOUJEO titrated to goal was similar to that with LANTUS titrated to goal. At the end of the trial, depending on the patient population and concomitant therapy, patients were receiving a higher dose of TOUJEO than LANTUS.
14.2 Clinical Study in Adult and Pediatric Patients with Type 1 Diabetes
Type 1 Diabetes – Adult
In an open-label, controlled study (Study A), patients with type 1 diabetes (n=546), were randomized to basal-bolus treatment with TOUJEO or LANTUS and treated for 26 weeks. TOUJEO and LANTUS were administered once daily in the morning (time period covering from pre-breakfast until pre-lunch) or in the evening (time period defined as prior to the evening meal until at bedtime). A mealtime insulin analogue was administered before each meal. Mean age was 47.3 years and mean duration of diabetes was 21 years. Fifty-seven percent were male, 85.1% were Caucasian, 4.7% Black or African American, and 4.7% were Hispanic; 32.2% of patients had GFR >90 mL/min/1.73 m2. The mean BMI was approximately 27.6 kg/m2. At week 26, treatment with TOUJEO provided a mean reduction in HbA1c that met the prespecified noninferiority margin of 0.4% (Table 4). Patients treated with TOUJEO used 17.5% more basal insulin than patients treated with LANTUS. There were no clinically important differences in glycemic control when TOUJEO was administered once daily in the morning or in the evening. There were no clinically important differences in body weight between treatment groups.
Table 4: Type 1 Diabetes Mellitus – Adult Patients (TOUJEO plus mealtime insulin versus LANTUS plus mealtime insulin) TOUJEO + Mealtime Insulin* LANTUS + Mealtime Insulin* - * "mealtime insulin" refers to insulin glulisine, insulin lispro or insulin aspart.
- † mITT: Modified intention-to-treat population.
- ‡ Treatment difference: TOUJEO – LANTUS.
Treatment duration 26 weeks Treatment in combination with Fast-acting insulin analogue Number of subjects treated (mITT†) 273 273 HbA1c (%) Baseline mean 8.13 8.12 Adjusted mean change from baseline -0.40 -0.44 Adjusted mean difference‡
[95% Confidence Interval]0.04
[-0.10 to 0.18]Fasting Plasma Glucose mg/dL Baseline mean 186 199 Adjusted mean change from baseline -17 -20 Adjusted mean difference‡
[95% Confidence Interval]3
[-10 to 16]Type 1 Diabetes – Pediatric
The efficacy of TOUJEO was evaluated in a 26-week, randomized, open-label, multicenter trial (Study B) in 463 pediatric patients with type 1 diabetes mellitus. Patients were randomized to basal-bolus treatment with TOUJEO or LANTUS and treated for 26 weeks. TOUJEO and LANTUS were administered once daily in the morning or in the evening. A mealtime insulin analogue was administered before each meal.
The mean age of the trial population was 12.9 years; 30.9% were <12 years of age, 69.1% were ages ≥12 years of age. The mean duration of diabetes was 5.7 years. Of the 463 pediatric patients, 51.2% were male, 92.1% were White, 3.1% were Black or African American, and 30.2% were Hispanic. The mean baseline BMI percentile was 68.32.
At week 26, the difference in HbA1c reduction from baseline between TOUJEO and LANTUS was 0.02% with a 95% confidence interval (-0.16%; 0.20%) and met the prespecified noninferiority margin (0.3%). The results are presented in Table 5.
Table 5: Type 1 Diabetes Mellitus – Pediatric Patients at 26 weeks (TOUJEO plus mealtime insulin versus LANTUS plus mealtime insulin) TOUJEO
+ Mealtime Insulin*LANTUS
+ Mealtime Insulin*- * "mealtime insulin" refers to insulin glulisine, insulin lispro or insulin aspart.
- † ITT: Intention-to-treat: all randomized subjects.
- ‡ At week 26, change in HbA1c was missing for 3.9% and 4.3% of subjects, and change in FPG was missing for 12.4% and 12.2% of subjects, in TOUJEO and LANTUS respectively. Missing values were imputed with return-to-baseline method for subjects who permanently discontinued the treatment.
- § Treatment difference: TOUJEO – LANTUS.
Number of subjects (ITT†) 233 230 HbA1c (%)‡ Baseline mean 8.65 8.61 Adjusted Mean change from baseline -0.386 -0.404 Adjusted Mean difference§
[95% Confidence Interval]0.018
[-0.159, 0.195]Fasting Plasma Glucose (mg/dL)‡ Baseline mean 202.70 204.51 Adjusted Mean change from baseline -10.447 -10.633 Adjusted Mean difference§
[95% Confidence Interval]0.185
[-18.131, 18.501]14.3 Clinical Studies in Adult Patients with Type 2 Diabetes
In a 26-week open-label, controlled study (study C, n=804), adults with type 2 diabetes were randomized to once-daily treatment in the evening with either TOUJEO or LANTUS. Short-acting mealtime insulin analogues with or without metformin were also administered. The average age was 60 years. The majority of patients were White (92.3%) and 52.9% were male; 20.3% of patients had GFR >90 mL/min/1.73 m2. The mean BMI was approximately 36.6 kg/m2. At week 26, treatment with TOUJEO provided a mean reduction in HbA1c that met the prespecified noninferiority margin of 0.4% compared to LANTUS (Table 6). Patients treated with TOUJEO used 11% more basal insulin than patients treated with LANTUS. There were no clinically important differences in body weight between treatment groups.
In two open-label, controlled studies (n=1670), adults with type 2 diabetes mellitus were randomized to either TOUJEO or LANTUS once daily for 26 weeks as part of a regimen of combination therapy with noninsulin antidiabetic drugs. At the time of randomization, 808 patients were treated with basal insulin for more than 6 months (study D) and 862 patients were insulin-naive (study E).
In Study D, the average age was 58.2 years. The majority of patients were White (93.8%) and 45.9% were male; 32.8% of patients had GFR >90 mL/min/1.73 m2. The mean BMI was approximately 34.8 kg/m2. At week 26, treatment with TOUJEO provided a mean reduction in HbA1c that met the prespecified noninferiority margin of 0.4% compared to LANTUS (Table 6). Patients treated with TOUJEO used 12% more basal insulin than patients treated with LANTUS. There were no clinically important differences in body weight between treatment groups.
In Study E, the average age was 57.7 years. The majority of patients were White (78%) and 57.7% were male; 29% of patients had GFR >90 mL/min/1.73 m2. The mean BMI was approximately 33 kg/m2. At week 26, treatment with TOUJEO provided a mean reduction in HbA1c that met the prespecified noninferiority margin compared to LANTUS (Table 6). Patients treated with TOUJEO used 15% more basal insulin than patients treated with LANTUS. There were no clinically important differences in body weight between treatment groups.
Table 6: Type 2 Diabetes Mellitus – Adult Study C Study D Study E Treatment duration 26 weeks 26 weeks 26 weeks Treatment in combination with Mealtime insulin analog ± metformin Noninsulin antidiabetic drugs TOUJEO LANTUS TOUJEO LANTUS TOUJEO LANTUS - * m-ITT population: Modified intention-to-treat population.
- † Treatment difference: TOUJEO – LANTUS.
Number of patients treated* 404 400 403 405 432 430 HbA1c (%) Baseline mean 8.13 8.14 8.27 8.22 8.49 8.58 Adjusted mean change from baseline -0.90 -0.87 -0.73 -0.70 -1.42 -1.46 Adjusted mean difference† -0.03 -0.03 0.04 [95% Confidence interval] [-0.14 to 0.08] [-0.17 to 0.10] [-0.09 to 0.17] Fasting Plasma Glucose (mg/dL) Baseline mean 157 160 149 142 179 184 Adjusted mean change from baseline -29 -30 -18 -22 -61 -68 Adjusted mean difference† 0.8 3 7 [95% Confidence interval] [-5 to 7] [-3 to 9] [2 to 12] -
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
TOUJEO is supplied as a clear and colorless solution containing 300 units per mL (U-300) of insulin glargine and is available in 2 single-patient-use prefilled pen presentations:
TOUJEO Total volume Concentration Total units available in presentation Max dose per injection Dose increment NDC number Package size SoloStar single-patient-use prefilled pen 1.5 mL 300 units/mL 450 units 80 units 1 unit 0024-5869-03 3 pens/pack Max SoloStar single-patient-use prefilled pen 3 mL 300 units/mL 900 units 160 units 2 units 0024-5871-02 2 pens/pack Needles are not included in the packs of TOUJEO SoloStar or TOUJEO Max SoloStar single-patient-use prefilled pen.
BD (such as BD Ultra-Fine®), Ypsomed (such as Clickfine®) or Owen Mumford (such as Unifine® Pentips®) needles‡ can be used in conjunction with TOUJEO SoloStar or TOUJEO Max SoloStar single-patient-use prefilled pen and are sold separately.
A new sterile needle must be attached before each injection. TOUJEO SoloStar or TOUJEO Max SoloStar single-patient-use prefilled pens must never be shared between patients, even if the needle is changed.
16.2 Storage
Dispense in the original sealed carton with the enclosed Instructions for Use.
TOUJEO SoloStar or TOUJEO Max SoloStar prefilled pen should not be stored in the freezer and should not be allowed to freeze. Discard TOUJEO prefilled pen if it has been frozen. Protect TOUJEO SoloStar/TOUJEO Max SoloStar from direct heat and light.
Storage conditions are summarized in the following table:
Not in-use (unopened) Refrigerated
36°F–46°F (2°C–8°C)In-use (opened)*
Room temperature only
(Do not refrigerate)
below 86°F (30°C)- * To prevent degradation, always store the prefilled pens with the cap on during in-use period.
1.5 mL TOUJEO SoloStar single-patient-use prefilled pen Until expiration date 56 days* 3 mL TOUJEO Max SoloStar single-patient-use prefilled pen Until expiration date 56 days* -
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information and Instructions for Use).
Never Share a TOUJEO SoloStar or TOUJEO Max SoloStar Pen Between Patients
Advise patients that they must never share TOUJEO SoloStar or TOUJEO Max SoloStar pen with another person even if the needle is changed. Pen sharing poses a risk for transmission of blood-borne pathogens [see Warnings and Precautions (5.1)].
Hyperglycemia or Hypoglycemia
Inform patients that hypoglycemia is the most common adverse reaction with insulin. Inform patients of the symptoms of hypoglycemia. Inform patients that the ability to concentrate and react may be impaired as a result of hypoglycemia. This may present a risk in situations where these abilities are especially important, such as driving or operating other machinery. Advise patients who have frequent hypoglycemia or reduced or absent warning signs of hypoglycemia to use caution when driving or operating machinery [see Warnings and Precautions (5.2, 5.3)].
Advise patients that changes in insulin regimen can predispose to hyperglycemia or hypoglycemia and that changes in insulin regimen should be made under close medical supervision [see Warnings and Precautions (5.2)].
Inform patients that if they change to TOUJEO from other basal insulins they may experience higher average fasting plasma glucose levels in the first weeks of therapy. Advise patients to monitor glucose daily when initiating TOUJEO [see Warnings and Precautions (5.2)].
Medication Errors
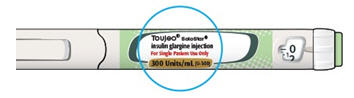
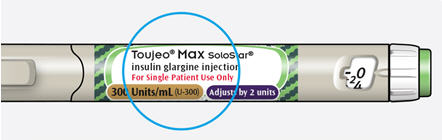
Instruct patients to always check the insulin label before each injection [see Warnings and Precautions (5.4)]. The "300 units/mL (U-300)" is highlighted in honey gold on the labels of TOUJEO and TOUJEO Max SoloStar single-patient-use prefilled pens.
Inform patients that TOUJEO (insulin glargine injection) 300 units/mL contains 3 times as much insulin in 1 mL as standard insulin (100 units/mL). To avoid dosing errors and potential overdose, instruct patients to never use a syringe to remove TOUJEO from the TOUJEO SoloStar or TOUJEO Max SoloStar single-patient-use prefilled pen [see Warnings and Precautions (5.4)].
Inform patients that the dose counter of TOUJEO SoloStar or TOUJEO Max SoloStar single-patient-use prefilled pen shows the number of units of TOUJEO to be injected and no dose recalculation is required [see Dosage and Administration (2.1, 2.4)].
Administration
TOUJEO must only be used if the solution is clear and colorless with no particles visible. Patients must be advised that TOUJEO must NOT be diluted or mixed with any other insulin or solution [see Dosage and Administration (2.4)].
-
SPL UNCLASSIFIED SECTION
sanofi-aventis U.S. LLC
Bridgewater, NJ 08807
A SANOFI COMPANY©2019 sanofi-aventis U.S. LLC
LANTUS, TOUJEO, SoloStar, and TOUJEO Max SoloStar are registered trademarks of sanofi-aventis U.S. LLC.
‡The brands listed are the registered trademarks of their respective owners and are not trademarks of sanofi-aventis U.S. LLC.
-
PATIENT PACKAGE INSERT
This Patient Information has been approved by the U.S. Food and Drug Administration. Revised: November 2019 Patient Information
TOUJEO® (Too-Jay-o)
(insulin glargine injection)
300 units/mL (U-300)
for subcutaneous useDo not share your TOUJEO SoloStar® or TOUJEO Max SoloStar® pen with other people, even if the needle has been changed. You may give other people a serious infection, or get a serious infection from them.
What is TOUJEO?
- TOUJEO is a long-acting man-made insulin used to control high blood sugar in adults and children who are 6 years of age and older with diabetes mellitus.
- TOUJEO is not for use to treat diabetic ketoacidosis.
- It is not known if TOUJEO is safe and effective in children under 6 years of age.
Who should not use TOUJEO?
Do not use TOUJEO if you:
- are having an episode of low blood sugar (hypoglycemia).
- have an allergy to insulin glargine or any of the ingredients in TOUJEO. See the end of this Patient Information leaflet for a complete list of ingredients in TOUJEO.
What should I tell my healthcare provider before using TOUJEO?
Before using TOUJEO, tell your healthcare provider about all your medical conditions, including if you:
- have liver or kidney problems.
- take other medicines, especially ones called TZDs (thiazolidinediones).
- have heart failure or other heart problems. If you have heart failure, it may get worse while you take TZDs with TOUJEO.
- are pregnant, planning to become pregnant, or are breastfeeding. It is not known if TOUJEO may harm your unborn or breastfeeding baby.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
Before you start using TOUJEO, talk to your healthcare provider about low blood sugar and how to manage it.
How should I use TOUJEO?
- TOUJEO is available in 2 single-patient-use prefilled pens: TOUJEO SoloStar and TOUJEO Max SoloStar. Your healthcare provider will tell you which TOUJEO Pen is right for you.
- Read the detailed Instructions for Use that come with your TOUJEO SoloStar or TOUJEO Max SoloStar single-patient-use prefilled pen.
- Use TOUJEO exactly as your healthcare provider tells you to. Your healthcare provider should tell you how much TOUJEO to use and when to use it.
- Know the amount of TOUJEO you use. Do not change the amount of TOUJEO you use unless your healthcare provider tells you to.
- Check your insulin label each time you give your injection to make sure you are using the correct insulin.
- Do not use a syringe to remove TOUJEO from your TOUJEO SoloStar or TOUJEO Max SoloStar single-patient-use prefilled pen. This can cause you to give yourself too much insulin. TOUJEO has 3 times as much insulin in 1 mL compared to other standard insulin pens.
- Do not re-use needles. Always use a new needle for each injection. Reusing needles increases your chance of having blocked needles, which can cause you to get the wrong dose of TOUJEO. Using a new needle for each injection also lowers your risk of getting an infection. If your needle is blocked, follow the instructions in Step 3 of the Instructions for Use.
- TOUJEO should be used 1 time each day and at the same time each day.
- TOUJEO is injected under the skin (subcutaneously) of your upper legs (thighs), upper arms, or stomach area (abdomen).
- Do not use TOUJEO in an insulin pump or inject TOUJEO into your vein (intravenously).
-
Change (rotate) your injection sites within the area you choose with each dose to reduce your risk of getting pits or thickening of the skin (lipodystrophy) and lumps in the skin (localized cutaneous amyloidosis) at the injection sites.
- Do not use the exact same spot for each injection.
- Do not inject where the skin has pits, is thickened, or has lumps.
- Do not inject where the skin is tender, bruised, scaly or hard, or into scars or damaged skin.
- Do not mix TOUJEO with any other type of insulin or liquid medicine.
- Check your blood sugar levels. Ask your healthcare provider what your blood sugar should be and when you should check your blood sugar levels.
Keep TOUJEO and all medicines out of the reach of children.
Your dose of TOUJEO may need to change because of:
- a change in level of physical activity or exercise, weight gain or loss, increased stress, illness, change in diet, or because of other medicines you take.
What should I avoid while using TOUJEO?
While using TOUJEO do not:
- drive or operate heavy machinery, until you know how TOUJEO affects you.
- drink alcohol or use over-the-counter medicines that contain alcohol.
What are the possible side effects of TOUJEO?
TOUJEO may cause serious side effects that can lead to death, including:
-
low blood sugar (hypoglycemia). Signs and symptoms that may indicate low blood sugar include:
- dizziness or light-headedness, sweating, confusion, headache, blurred vision, slurred speech, shakiness, fast heartbeat, anxiety, irritability or mood change, hunger.
-
severe allergic reaction (whole body reaction). Get medical help right away if you have any of these signs or symptoms of a severe allergic reaction:
- a rash over your whole body, trouble breathing, a fast heartbeat, or sweating
- low potassium in your blood (hypokalemia).
-
heart failure. Taking certain diabetes pills called TZDs (thiazolidinediones) with TOUJEO may cause heart failure in some people. This can happen even if you have never had heart failure or heart problems before. If you already have heart failure it may get worse while you take TZDs with TOUJEO. Your healthcare provider should monitor you closely while you are taking TZDs with TOUJEO. Tell your healthcare provider if you have any new or worse symptoms of heart failure including:
- shortness of breath, swelling of your ankles or feet, sudden weight gain.
Treatment with TZDs and TOUJEO may need to be changed or stopped by your healthcare provider if you have new or worse heart failure.
Get emergency medical help if you have:
- trouble breathing, shortness of breath, fast heartbeat, swelling of your face, tongue, or throat, sweating, extreme drowsiness, dizziness, confusion.
The most common side effects of TOUJEO include:
- low blood sugar (hypoglycemia), weight gain, itching, rash, swelling, allergic reactions, including reactions at your injection site, skin thickening or pits at the injection site (lipodystrophy).
These are not all the possible side effects of TOUJEO. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
General information about the safe and effective use of TOUJEO.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use TOUJEO for a condition for which it was not prescribed. Do not give TOUJEO to other people, even if they have the same symptoms that you have. It may harm them.
This Patient Information leaflet summarizes the most important information about TOUJEO. If you would like more information, talk with your healthcare provider. You can ask your pharmacist or healthcare provider for information about TOUJEO that is written for health professionals.
What are the ingredients in TOUJEO?
- Active ingredient: insulin glargine
- Inactive ingredients: zinc, m-cresol, glycerol, and water for injection. Hydrochloric acid and sodium hydroxide may be added to adjust the pH.
sanofi-aventis U.S. LLC, Bridgewater, NJ 08807, A SANOFI COMPANY
For more information, go to www.TOUJEO.com or call 1-800-633-1610. -
INSTRUCTIONS FOR USE
Instructions for Use
TOUJEO® SoloStar® (Too-Jay-o)
(insulin glargine injection)
1.5 mL single-patient-use prefilled penRead this first
Do not share your TOUJEO SoloStar pen with other people, even if the needle has been changed. You may give other people a serious infection, or get a serious infection from them.
TOUJEO contains 300 units/mL insulin glargine
- Do not re-use needles. If you do you might not get your dose (underdosing) or get too much (overdosing) as the needle could block.
- Do not use a syringe to remove insulin from your pen. If you do you will get too much insulin. The scale on most syringes is made for non-concentrated insulin only.
- The dose selector of your TOUJEO SoloStar pen dials by 1 unit.
People who are blind or have vision problems should not use the TOUJEO SoloStar pen without help from a person trained to use the TOUJEO SoloStar pen.
Important information
- Do not use your pen if it is damaged or if you are not sure that it is working properly.
- Always perform a safety test (see Step 3).
- Always carry a spare pen and spare needles in case they are lost or stop working.
- Change (rotate) your injection sites within the area you choose for each dose (see "Places to inject").
Learn to inject
- Talk with your healthcare provider about how to inject, before using your pen.
- Read all of these instructions before using your pen. If you do not follow all of these instructions, you may get too much or too little insulin.
Need help?
If you have any questions about your pen or about diabetes, ask your healthcare provider, go to www.Toujeo.com or call sanofi-aventis at 1-800-633-1610.
Extra items you will need:
- a new sterile needle (not included with the pen) (see Step 2).
- an alcohol swab.
- a puncture-resistant container for used needles and pens (see "Throwing your pen away").
- Inject your insulin exactly as your healthcare provider has shown you.
- Inject your insulin under the skin (subcutaneously) of your upper legs (thighs), upper arms, or stomach area (abdomen).
- Change (rotate) your injection sites within the area you choose for each dose to reduce your risk of getting pits or thickening of the skin (lipodystrophy) and lumps in the skin (localized cutaneous amyloidosis) at the injection sites.
- Do not inject where the skin has pits, is thickened, or has lumps.
- Do not inject where the skin is tender, bruised, scaly or hard, or into scars or damaged skin.
Get to know your pen
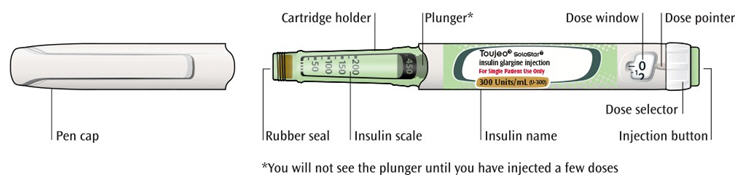
Step 1: Check your pen
Take a new pen out of the refrigerator at least 1 hour before you inject. Cold insulin is more painful to inject.
- 1A
Check the name and expiration date on the label of your pen.
-
Make sure you have the correct insulin.
-
Do not use your pen after the expiration date printed on the label.

- 1B Pull off the pen cap.
- 1C Check that the insulin is clear.
-
Do not use the pen if the insulin looks cloudy, colored or contains particles.
- 1D Wipe the rubber seal with an alcohol swab.
-
Make sure you have the correct insulin.
If you have other injector pens
- Making sure you have the correct medicine is especially important if you have other injector pens.
- Do not re-use needles. Always use a new sterile needle for each injection. This helps stop blocked needles, contamination and infection.
- Always use needles* from BD (such as BD Ultra-Fine®), Ypsomed (such as Clickfine®), or Owen Mumford (such as Unifine® Pentips®).
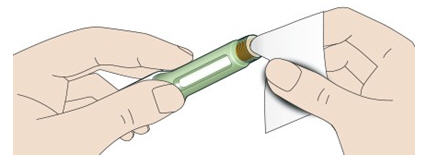
- 2A
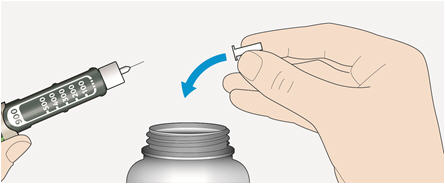
Take a new needle and peel off the protective seal.

- 2B Keep the needle straight and screw it onto the pen until fixed. Do not over-tighten.
- 2C Pull off the outer needle cap. Keep this for later.

- 2D Pull off the inner needle cap and throw away.

- 2B Keep the needle straight and screw it onto the pen until fixed. Do not over-tighten.
Handling needles
- Be careful when you are handling needles to help prevent accidental needle-stick injury. You may give other people a serious infection, or get a serious infection from them.
Always do a safety test before each injection to:
- check your pen and the needle to make sure they are working properly.
- make sure that you get the correct insulin dose.
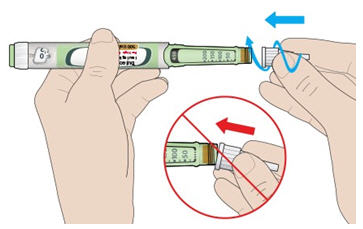
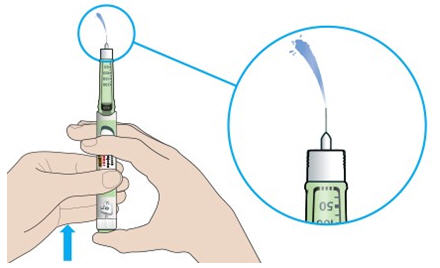
If the pen is new, you must perform safety tests before you use the pen for the first time until you see insulin coming out of the needle tip. If you see insulin coming out of the needle tip, the pen is ready to use. If you do not see insulin coming out before taking your dose, you could get an underdose or no insulin at all. This could cause high blood sugar.
- 3A
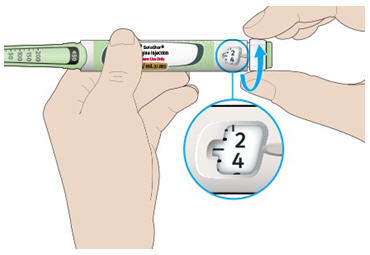
Select 3 units by turning the dose selector until the dose pointer is at the mark between 2 and 4.
- 3B Press the injection button all the way in.
- When insulin comes out of the needle tip, your pen is working correctly.
- 3B Press the injection button all the way in.
If no insulin appears:
- You may need to repeat this step up to 3 times before seeing insulin.
- If no insulin comes out after the third time, the needle may be blocked. If this happens:
- Do not use your pen if there is still no insulin coming out of the needle tip. Use a new pen.
- Do not use a syringe to remove insulin from your pen.
If you see air bubbles
- You may see air bubbles in the insulin. This is normal, they will not harm you.
Step 4: Select the dose
- Do not select a dose or press the injection button without a needle attached. This may damage your pen.
- TOUJEO SoloStar is made to deliver the number of insulin units that your healthcare provider prescribed. You do not need to do any dose calculations.
- The dose selector of your TOUJEO SoloStar pen dials by 1 unit.
- 4A
Make sure a needle is attached and the dose is set to '0'.
- 4B Turn the dose selector until the dose pointer lines up with your dose.
- Set the dose by turning the dose selector to a line in the dose window. Each line equals 1 unit.
- The dose selector clicks as you turn it.
- Always check the number in the dose window to make sure you dialed the correct dose.
- Do not dial your dose by counting the clicks. You may dial the wrong dose. This may lead to you getting too much insulin or not enough insulin.
- If you turn past your dose, you can turn back down.
- If there are not enough units left in your pen for your dose, the dose selector will stop at the number of units left.
- If you cannot select your full prescribed dose, split the dose into 2 injections or use a new pen. If you use a new pen, perform a safety test (see Step 3).
- 4B Turn the dose selector until the dose pointer lines up with your dose.
How to read the dose window
The dose selector dials by 1 unit.
Even numbers are shown in line with the dose pointer:

30 units selected
Odd numbers are shown as a line between even numbers:

29 units selected
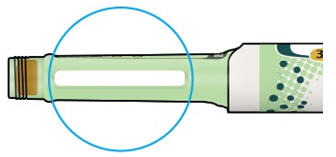
Units of insulin in your pen
- Your pen contains a total of 450 units of insulin. You can select doses from 1 to 80 units. Each pen contains more than 1 dose.
- You can see roughly how many units of insulin are left by looking at where the plunger is on the insulin scale.
Step 5: Inject your dose
If you find it hard to press the injection button in, do not force it as this may break your pen. See the section below for help.
- 5A
Choose a place to inject as shown in the picture labeled "Places to inject."
- The site you choose for the injection should be clean and dry.
- If your skin is dirty, clean it as instructed by your healthcare provider.
- 5B Push the needle into your skin as shown by your healthcare provider.
-
Do not touch the injection button yet.
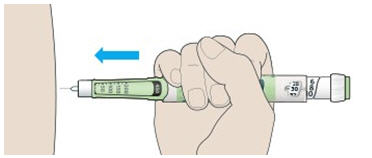
- 5C Place your thumb on the injection button. Then press all the way in and hold.
-
Do not press at an angle. Your thumb could block the dose selector from turning.
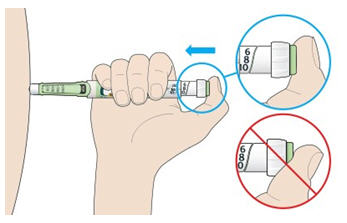
- 5D Keep the injection button held in and when you see "0" in the dose window, slowly count to 5.
- This will make sure you get your full dose.
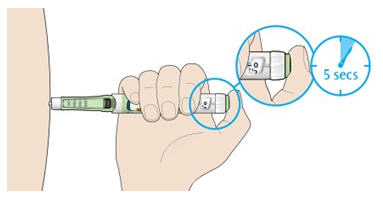
- 5E After holding and slowly counting to 5, release the injection button. Then remove the needle from your skin.
If you find it hard to press the button in:
- Change the needle (see Step 6 and Step 2) then do a safety test (see Step 3).
- If you still find it hard to press in, get a new pen.
- Do not use a syringe to remove insulin from your pen.
- Take care when handling needles to prevent needle injury and cross-infection.
- Do not put the inner needle cap back on.
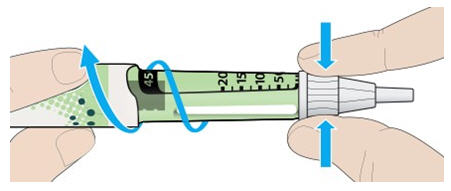
- 6A
Grip the widest part of the outer needle cap. Keep the needle straight and guide it into the outer needle cap.
Then push firmly on.- The needle can puncture the cap if it is recapped at an angle.

- 6B Grip and squeeze the widest part of the outer needle cap. Turn your pen several times with your other hand to remove the needle.
- Try again if the needle does not come off the first time.
- 6C Throw away the used needle in a puncture-resistant container (see "Throwing your pen away" at the end of this Instructions for Use).

- 6D Put the pen cap back on.
-
Do not put the pen back in the refrigerator.

- The needle can puncture the cap if it is recapped at an angle.
Use by
- Only use your pen for up to 56 days after its first use.
How to store your pen
Before first use
- Keep new pens in the refrigerator between 36°F and 46°F (2°C and 8°C).
- Do not freeze. Throw away your pen if it has been frozen (See "Throwing your pen away").
After first use
- Keep your pen at room temperature below 86°F (30°C).
- Protect your pen from direct heat and light.
- Do not put your pen back in the refrigerator.
- Do not store your pen with the needle attached.
- Store your pen with the pen cap on.
- Keep TOUJEO SoloStar pens and needles out of the reach of children.
How to care for your pen
Handle your pen with care
- Do not drop your pen or knock it against hard surfaces.
- If you think that your pen may be damaged, do not try to fix it. Use a new one.
Protect your pen from dust and dirt
- You can clean the outside of your pen by wiping it with a damp cloth (water only). Do not soak, wash or lubricate your pen. This may damage it.
- Put the used TOUJEO SoloStar pen in a FDA-cleared sharps disposal container right away after use.
Do not throw away (dispose of) the TOUJEO SoloStar pen in your household trash. - If you do not have a FDA-cleared sharps disposal container, you may use a household container that is:
- – made of a heavy-duty plastic,
- – can be closed with a tight-fitting, puncture-resistant lid, without sharps being able to come out,
- – upright and stable during use,
- – leak-resistant, and
- – properly labeled to warn of hazardous waste inside the container.
- When your sharps disposal container is almost full, you will need to follow your community guidelines for the right way to dispose of your sharps disposal container. There may be state or local laws about how you should throw away used needles and syringes. For more information about safe sharps disposal, and for specific information about sharps disposal in the state that you live in, go to the FDA's website at: http://www.fda.gov/safesharpsdisposal.
- Do not dispose of your used sharps disposal container in your household trash unless your community guidelines permit this. Do not recycle your used sharps disposal container.
This Instructions for Use has been approved by the U.S. Food and Drug Administration.
Revised: November 2019
sanofi-aventis U.S. LLC
Bridgewater, NJ 08807
A SANOFI COMPANY©2019 sanofi-aventis U.S. LLC
* The brands listed are the registered trademarks of their respective owners and are not trademarks of sanofi-aventis U.S. LLC.
-
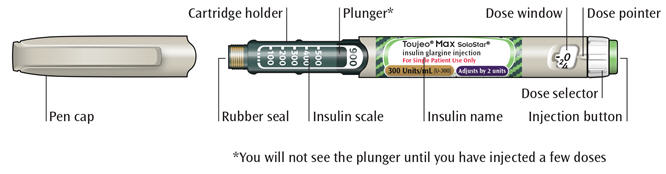
Instructions for Use
TOUJEO® Max SoloStar® (Too-Jay-o)
(insulin glargine injection)
3 mL single-patient-use prefilled penRead this first
Do not share your TOUJEO Max SoloStar pen with other people, even if the needle has been changed. You may give other people a serious infection, or get a serious infection from them.
TOUJEO contains 300 units/mL insulin glargine
- Do not re-use needles. If you do you might not get your dose (underdosing) or get too much (overdosing) as the needle could block.
- Do not use a syringe to remove insulin from your pen. If you do you will get too much insulin. The scale on most syringes is made for non-concentrated insulin only.
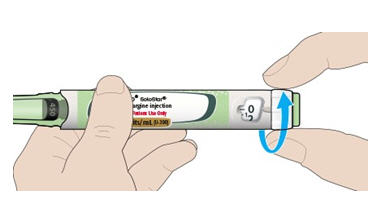
- The dose selector of your TOUJEO Max SoloStar pen dials by 2 units.
People who are blind or have vision problems should not use the TOUJEO Max SoloStar pen without help from a person trained to use the TOUJEO Max SoloStar pen.
Important information
- Do not use your pen if it is damaged or if you are not sure that it is working properly.
- Always perform a safety test (see Step 3).
- Always carry a spare pen and spare needles in case they are lost or stop working.
- Change (rotate) your injection sites within the area you choose for each dose (see "Places to inject").
Learn to inject
- Talk with your healthcare provider about how to inject, before using your pen.
- Read all of these instructions before using your pen. If you do not follow all of these instructions, you may get too much or too little insulin.
Need help?
If you have any questions about your pen or about diabetes, ask your healthcare provider, go to www.Toujeo.com or call sanofi-aventis at 1-800-633-1610.
Extra items you will need:
- a new sterile needle (not included with the pen) (see Step 2).
- an alcohol swab.
- a puncture-resistant container for used needles and pens (see "Throwing your pen away").
- Inject your insulin exactly as your healthcare provider has shown you.
- Inject your insulin under the skin (subcutaneously) of your upper legs (thighs), upper arms, or stomach area (abdomen).
- Change (rotate) your injection sites within the area you choose for each dose to reduce your risk of getting pits or thickening of the skin (lipodystrophy) and lumps in the skin (localized cutaneous amyloidosis) at the injection sites.
- Do not inject where the skin has pits, is thickened, or has lumps.
-
Do not inject where the skin is tender, bruised, scaly or hard, or into scars or damaged skin.
Get to know your pen
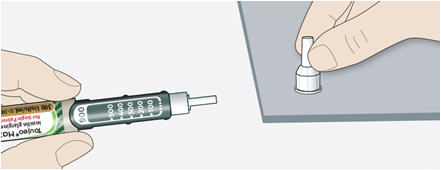
Step 1: Check your pen
Take a new pen out of the refrigerator at least 1 hour before you inject. Cold insulin is more painful to inject.
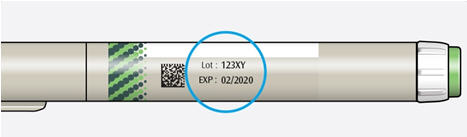
- 1A
Check the name and expiration date on the label of your pen.
-
Make sure you have the correct insulin.
-
Do not use your pen after the expiration date printed on the label.
- 1B Pull off the pen cap.
- 1C Check that the insulin is clear.
-
Do not use the pen if the insulin looks cloudy, colored or contains particles.
- 1D Wipe the rubber seal with an alcohol swab.

-
Make sure you have the correct insulin.
If you have other injector pens
- Making sure you have the correct medicine is especially important if you have other injector pens.
- Do not re-use needles. Always use a new sterile needle for each injection. This helps stop blocked needles, contamination and infection.
- Always use needles* from BD (such as BD Ultra-Fine®), Ypsomed (such as Clickfine®), or Owen Mumford (such as Unifine® Pentips®) that are 8 mm long or shorter.
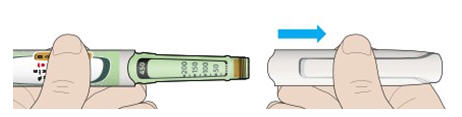
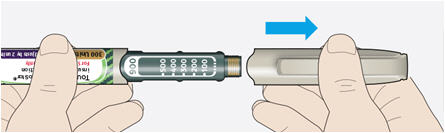
- 2A
Take a new needle and peel off the protective seal.

- 2B Keep the needle straight and screw it onto the pen until fixed. Do not over-tighten.
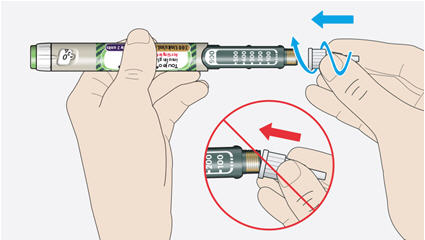
- 2C Pull off the outer needle cap. Keep this for later.
- 2D Pull off the inner needle cap and throw away.
- 2B Keep the needle straight and screw it onto the pen until fixed. Do not over-tighten.
Handling needles
- Be careful when you are handling needles to help prevent accidental needle-stick injury. You may give other people a serious infection, or get a serious infection from them.
Always do a safety test before each injection to:
- check your pen and the needle to make sure they are working properly.
- make sure that you get the correct insulin dose.
If the pen is new, you must perform safety tests before you use the pen for the first time until you see insulin coming out of the needle tip. If you see insulin coming out of the needle tip, the pen is ready to use. If you do not see insulin coming out before taking your dose, you could get an underdose or no insulin at all. This could cause high blood sugar.
- 3A
Select 4 units by turning the dose selector until the dose pointer is at the 4 mark.
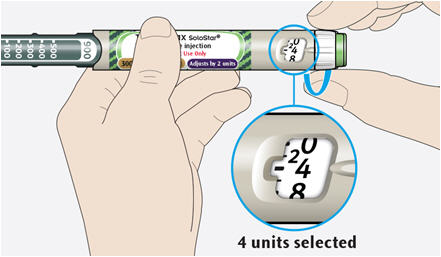
- 3B Press the injection button all the way in.
- When insulin comes out of the needle tip, your pen is working correctly.
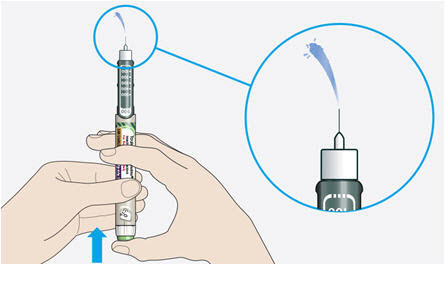
- You may need to repeat this step up to 6 times before seeing insulin.
- If no insulin comes out after the sixth time, the needle may be blocked. If this happens:
- Do not use your pen if there is still no insulin coming out of the needle tip. Use a new pen.
- Do not use a syringe to remove insulin from your pen.
- 3B Press the injection button all the way in.
If you see air bubbles
- You may see air bubbles in the insulin. This is normal, they will not harm you.
Step 4: Select the dose
- Do not select a dose or press the injection button without a needle attached. This may damage your pen.
- TOUJEO Max SoloStar is made to deliver the number of insulin units that your healthcare provider prescribed. You do not need to do any dose calculations.
- The dose selector of your TOUJEO Max SoloStar pen dials by 2 units and can only dial even doses of insulin.
- 4A
Make sure a needle is attached and the dose is set to '0'.

- 4B Turn the dose selector until the dose pointer lines up with your dose.
- Set the dose by turning the dose selector to a line in the dose window. Each line equals 2 units.
- The dose selector clicks as you turn it.
- Always check the number in the dose window to make sure you dialed the correct dose.
- Do not dial your dose by counting the clicks. You may dial the wrong dose. This may lead to you getting too much insulin or not enough insulin.
- If you turn past your dose, you can turn back down.
- If there are not enough units left in your pen for your dose, the dose selector will stop at the number of units left.
- If you cannot select your full prescribed dose, split the dose into 2 injections or use a new pen. If you use a new pen, perform a safety test (see Step 3).

- 4B Turn the dose selector until the dose pointer lines up with your dose.
How to read the dose window
The dose selector dials by 2 units.
Each line in the dose window is an even number.

60 units selected

58 units selected
Units of insulin in your pen
- Your pen contains a total of 900 units of insulin. You can select doses from 2 to 160 units. The dose is adjusted by 2 units at a time. Each pen contains more than 1 dose.
- You can see roughly how many units of insulin are left by looking at where the plunger is on the insulin scale.
Step 5: Inject your dose
If you find it hard to press the injection button in, do not force it as this may break your pen. See the section below for help.
- 5A
Choose a place to inject as shown in the picture labeled "Places to inject."
- The site you choose for the injection should be clean and dry.
- If your skin is dirty, clean it as instructed by your healthcare provider.
- 5B Push the needle into your skin as shown by your healthcare provider.
-
Do not touch the injection button yet.

- 5C Place your thumb on the injection button. Then press all the way in and hold.
-
Do not press at an angle. Your thumb could block the dose selector from turning.
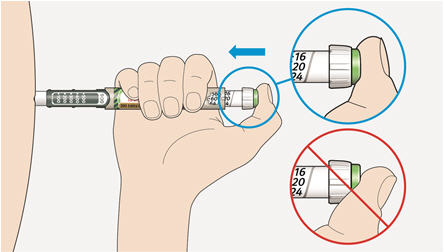
- 5D Keep the injection button held in and when you see "0" in the dose window, slowly count to 5.
- This will make sure you get your full dose.
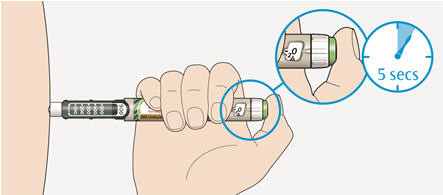
- 5E After holding and slowly counting to 5, release the injection button. Then remove the needle from your skin.
If you find it hard to press the injection button in:
- Change the needle (see Step 6 and Step 2) then do a safety test (see Step 3).
- If you still find it hard to press in, get a new pen.
- Do not use a syringe to remove insulin from your pen.
- Take care when handling needles to prevent needle injury and cross-infection.
- Do not put the inner needle cap back on.
- 6A
Grip the widest part of the outer needle cap. Keep the needle straight and guide it into the outer needle cap.
Then push firmly on.- The needle can puncture the cap if it is recapped at an angle.
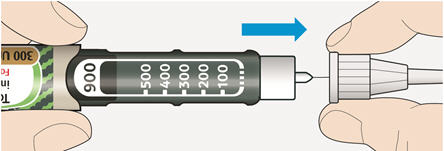
- 6B Grip and squeeze the widest part of the outer needle cap. Turn your pen several times with your other hand to remove the needle.
- Try again if the needle does not come off the first time.

- 6C Throw away the used needle in a puncture-resistant container (see "Throwing your pen away" at the end of this Instructions for Use).
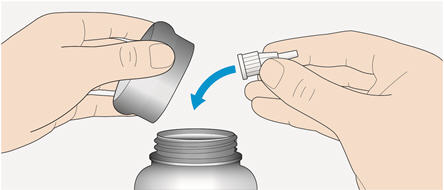
- 6D Put the pen cap back on.
-
Do not put the pen back in the refrigerator.
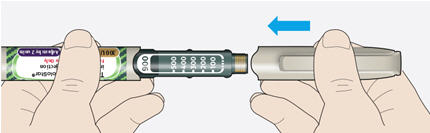
- The needle can puncture the cap if it is recapped at an angle.
Use by
- Only use your pen for up to 56 days after its first use.
How to store your pen
Before first use
- Keep new pens in the refrigerator between 36°F and 46°F (2°C and 8°C).
- Do not freeze. Throw away your pen if it has been frozen (See "Throwing your pen away").
After first use
- Keep your pen at room temperature below 86°F (30°C).
- Protect your pen from direct heat and light.
- Do not put your pen back in the refrigerator.
- Do not store your pen with the needle attached.
- Store your pen with the pen cap on.
- Keep TOUJEO Max SoloStar pens and needles out of the reach of children.
How to care for your pen
Handle your pen with care
- Do not drop your pen or knock it against hard surfaces.
- If you think that your pen may be damaged, do not try to fix it. Use a new one.
Protect your pen from dust and dirt
- You can clean the outside of your pen by wiping it with a damp cloth (water only). Do not soak, wash or lubricate your pen. This may damage it.
- Put the used TOUJEO Max SoloStar pen in a FDA-cleared sharps disposal container right away after use. Do not throw away (dispose of) the TOUJEO Max SoloStar pen in your household trash.
- If you do not have a FDA-cleared sharps disposal container, you may use a household container that is:
- – made of a heavy-duty plastic,
- – can be closed with a tight-fitting, puncture-resistant lid, without sharps being able to come out,
- – upright and stable during use,
- – leak-resistant, and
- – properly labeled to warn of hazardous waste inside the container.
- When your sharps disposal container is almost full, you will need to follow your community guidelines for the right way to dispose of your sharps disposal container. There may be state or local laws about how you should throw away used needles and syringes. For more information about safe sharps disposal, and for specific information about sharps disposal in the state that you live in, go to the FDA's website at:
http://www.fda.gov/safesharpsdisposal. - Do not dispose of your used sharps disposal container in your household trash unless your community guidelines permit this. Do not recycle your used sharps disposal container.
This Instructions for Use has been approved by the U.S. Food and Drug Administration.
Revised: November 2019
sanofi-aventis U.S. LLC
Bridgewater, NJ 08807
A SANOFI COMPANY©2019 sanofi-aventis U.S. LLC
* The brands listed are the registered trademarks of their respective owners and are not trademarks of sanofi-aventis U.S. LLC.
-
PRINCIPAL DISPLAY PANEL - 1.5 mL Pen Carton
NDC: 0024-5869-03
Rx ONLY
Toujeo® SoloStar®
insulin glargine injectionFor Single Patient Use Only
300 Units/mL (U-300)
Solution for injection in a disposable insulin delivery device
Do not remove insulin with syringe
Always use a new needle
Do not mix with other insulins
For subcutaneous Injection only
Use only if solution is clear and colorless with no particles visibleUse within 56 days after opening
*Needles not included (see back panel)
Three prefilled pens, 450 units/1.5mL each – Dispense in this sealed cartonSANOFI

-
PRINCIPAL DISPLAY PANEL - 3 mL Pen Carton
NDC: 0024-5871-02
Rx ONLY
Toujeo® Max SoloStar®
insulin glargine injectionFor Single Patient Use Only
300 Units/mL (U-300)
Adjusts by 2 unitsFor subcutaneous injection only
Solution for injection in a disposable insulin delivery device
Do not remove insulin with syringe
Always use a new needle
Do not mix with other insulins
Use only if solution is clear and colorless with no particles visible
Use within 56 days after opening
*Needles not included (see back panel)
Two prefilled pens, 900 units/3mL each – Dispense in this sealed cartonSANOFI
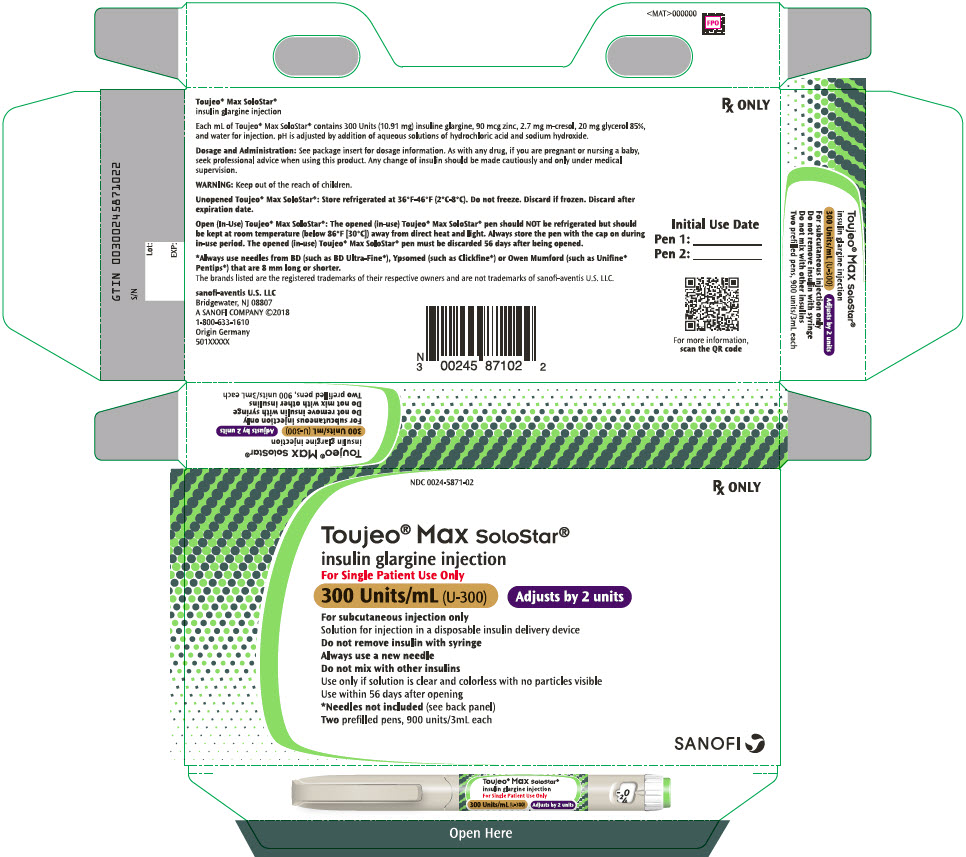
-
INGREDIENTS AND APPEARANCE
TOUJEO
insulin glargine injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0024-5869 Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength insulin glargine (UNII: 2ZM8CX04RZ) (insulin glargine - UNII:2ZM8CX04RZ) insulin glargine 300 U in 1 mL Inactive Ingredients Ingredient Name Strength zinc (UNII: J41CSQ7QDS) 90 ug in 1 mL metacresol (UNII: GGO4Y809LO) 2.7 mg in 1 mL glycerin (UNII: PDC6A3C0OX) 20 mg in 1 mL water (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0024-5869-03 3 in 1 CARTON 02/15/2015 1 NDC: 0024-5869-01 1.5 mL in 1 SYRINGE; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) 2 NDC: 0024-5869-00 1 in 1 CARTON 02/15/2015 2 1.5 mL in 1 SYRINGE; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA206538 02/15/2015 TOUJEO MAX
insulin glargine injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0024-5871 Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength insulin glargine (UNII: 2ZM8CX04RZ) (insulin glargine - UNII:2ZM8CX04RZ) insulin glargine 300 U in 1 mL Inactive Ingredients Ingredient Name Strength zinc (UNII: J41CSQ7QDS) 90 ug in 1 mL METACRESOL (UNII: GGO4Y809LO) 2.7 mg in 1 mL GLYCERIN (UNII: PDC6A3C0OX) 20 mg in 1 mL WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0024-5871-02 2 in 1 CARTON 03/26/2018 1 NDC: 0024-5871-00 3 mL in 1 SYRINGE; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) 2 NDC: 0024-5871-01 1 in 1 CARTON 03/26/2018 2 3 mL in 1 SYRINGE; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA206538 02/15/2015 Labeler - Sanofi-Aventis U.S. LLC (824676584) Establishment Name Address ID/FEI Business Operations Sanofi-Aventis Deutschland GmbH 313218430 MANUFACTURE(0024-5869, 0024-5871) , ANALYSIS(0024-5869, 0024-5871) , LABEL(0024-5869, 0024-5871) , PACK(0024-5869, 0024-5871) Establishment Name Address ID/FEI Business Operations Genzyme Corporation 050424395 LABEL(0024-5871) , PACK(0024-5871)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.