OXCARBAZEPINE suspension
Oxcarbazepine by
Drug Labeling and Warnings
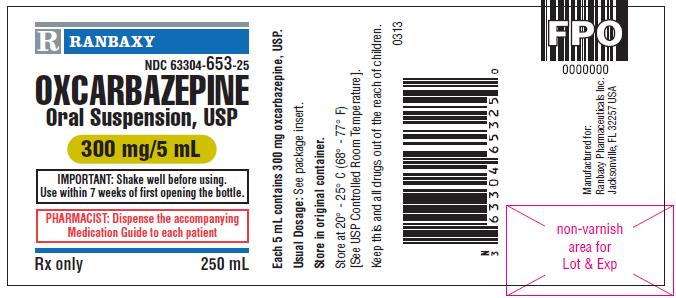
Oxcarbazepine by is a Prescription medication manufactured, distributed, or labeled by Ranbaxy Pharmaceuticals Inc., DPT Laboratories Ltd. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use oxcarbazepine oral suspension, USP safely and effectively. See full prescribing information for oxcarbazepine oral suspension, USP.
Oxcarbazepine oral suspension, USP for oral administration
Initial U.S. Approval: 2000RECENT MAJOR CHANGES
Warnings and Precautions (5.4) 06/2014
INDICATIONS AND USAGE
Oxcarbazepine oral suspension, USP is an antiepileptic drug indicated for: (1)
-
Adults:
- Monotherapy or adjunctive therapy in the treatment of partial seizures
-
Children:
- Monotherapy in the treatment of partial seizures in children 4 to 16 years
- Adjunctive therapy in the treatment of partial seizures in children 2 to 16 years (1)
DOSAGE AND ADMINISTRATION
ADULTS: initiated with a dose of 600 mg/day, given in twice-a-day regimen (2)
- Adjunctive Therapy: Maximum increment of 600 mg/day at approximately weekly intervals. The recommended daily dose is 1200 mg/day (2.1)
- Conversion to Monotherapy: Concomitant AEDs should be completely withdrawn over 3 to 6 weeks, while maximum dose of oxcarbazepine should be reached in about 2 to 4 weeks. Maximum increment of 600 mg/day at approximately weekly intervals to a recommended daily dose of 2400 mg/day (2.2)
- Initiation of Monotherapy: Increments of 300 mg/day every third day to a dose of 1200 mg/day. (2.3)
CHILDREN: initiation with 8 to 10 mg/kg/day, given in twice-a-day regimen. For patients aged 2 to < 4 years and under 20 kg, a starting dose of 16 to 20 mg/kg/day may be considered. Recommended daily dose is dependent upon patient weight (2)
- Adjunctive Patients (Aged 2 to 16 Years): For patients aged 4 to 16 years, target maintenance dose should be achieved over 2 weeks (2.4). For patients aged 2 to < 4 years, maximum maintenance dose should be achieved over 2 to 4 weeks and should not to exceed 60 mg/kg/day (2.4)
- Conversion to Monotherapy for Patients (Aged 4 to 16 Years)
Maximum increment of 10 mg/kg/day at weekly intervals, concomitant antiepileptic drugs can be completely withdrawn over 3 to 6 weeks (2.5) (2)
- Initiation of Monotherapy for Patients (Aged 4 to 16 Years)
Increments of 5 mg/kg/day every third day (2.6) (2)
DOSAGE FORMS AND STRENGTHS
- Oral suspension a 300 mg/5 mL (60 mg/mL) (3)
CONTRAINDICATIONS
- Oxcarbazepine oral suspension should not be used in patients with a known hypersensitivity to oxcarbazepine or to any of its components (4)
WARNINGS AND PRECAUTIONS
- Hyponatremia (5.1)
- Anaphylactic Reactions and Angioedema (5.2)
- Patients with a Past History of Hypersensitivity Reaction to Carbamazepine (5.3)
- Serious Dermatological Reactions (5.4)
- Suicidal Behavior and Ideation (5.5)
- Withdrawal of AEDs (5.6)
- Cognitive/Neuropsychiatric Adverse Events (5.7)
- Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS)/Multi-Organ Hypersensitivity (5.8)
- Hematologic Events (5.9)
- Seizure Control During Pregnancy (5.10)
- Laboratory Tests (5.11)
ADVERSE REACTIONS
The most commonly observed (≥ 5%) adverse experiences were: dizziness, somnolence, diplopia, fatigue, nausea, vomiting, ataxia, abnormal vision, abdominal pain, tremor, dyspepsia, abnormal gait, and in pediatric patients < 4 years old, also infections and infestations. (6.1) (6)
To report SUSPECTED ADVERSE REACTIONS, contact Ranbaxy Pharmaceuticals Inc. at 1-888-Ranbaxy (726-2299) or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. (6)
DRUG INTERACTIONS
- Phenytoin: Increased phenytoin levels. Reduced dose of phenytoin may be required. (7.1)
- Carbamazepine: Decreased plasma levels of MHD (the active metabolite). Dose adjustments may be necessary. (7.1)
- Phenobarbital: Decreased plasma levels of MHD. Dose adjustments may be necessary. (7.1)
- Oral Contraceptive: Patients should be advised that oxcarbazepine may decrease the effectiveness of hormonal contraceptives. (7.2)
USE IN SPECIFIC POPULATIONS
- Pregnancy: Plasma levels of MHD may be decreased. Monitor patients. Based on animal data, may cause fetal harm. To enroll in the North American Antiepileptic Drug Pregnancy Registry call (888) 233-2334 (toll free). (8.1)
- In patients with a creatinine clearance < 30 mL/min, oxcarbazepine should be started at one-half the usual starting dose and increased slowly (2, 8.6, 12.3)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 2/2015
-
Adults:
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Adjunctive Therapy for Adults
2.2 Conversion to Monotherapy for Adults
2.3 Initiation of Monotherapy for Adults
2.4 Adjunctive Therapy for Pediatric Patients (Aged 2 to 16 Years)
2.5 Conversion to Monotherapy for Pediatric Patients (Aged 4 to 16 Years)
2.6 Initiation of Monotherapy for Pediatric Patients (Aged 4 to 16 Years)
2.7 Patients with Hepatic Impairment
2.8 Patients with Renal Impairment
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Hyponatremia
5.2 Anaphylactic Reactions and Angioedema
5.3 Patients with a Past History of Hypersensitivity Reaction to Carbamazepine
5.4 Serious Dermatological Reactions
5.5 Suicidal Behavior and Ideation
5.6 Withdrawal of AEDs
5.7 Cognitive/Neuropsychiatric Adverse Events
5.8 Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS)/Multi-Organ Hypersensitivity
5.9 Hematologic Events
5.10 Seizure Control During Pregnancy
5.11 Laboratory Tests
6 ADVERSE REACTIONS
6.1 Clinical Studies Experience
6.2 Postmarketing and Other Experience
7 DRUG INTERACTIONS
7.1 Antiepileptic Drugs
7.2 Hormonal Contraceptives
7.3 Calcium Antagonists
7.4 Other Drug Interactions
7.5 Drug/Laboratory Test Interactions
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Labor and Delivery
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
9 DRUG ABUSE AND DEPENDENCE
9.2 Abuse
9.3 Dependence
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
12.6 Special Populations
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Oxcarbazepine Monotherapy Trials
14.2 Oxcarbazepine Adjunctive Therapy Trials
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
Oxcarbazepine oral suspension, USP is indicated for use as monotherapy or adjunctive therapy in the treatment of partial seizures in adults and as monotherapy in the treatment of partial seizures in children aged 4 years and above with epilepsy, and as adjunctive therapy in children aged 2 years and above with partial seizures.
-
2 DOSAGE AND ADMINISTRATION
All dosing should be given in a twice-a-day regimen. Oxcarbazepine oral suspension and oxcarbazepine film-coated tablets may be interchanged at equal doses.
Oxcarbazepine oral suspension should be kept out of the reach and sight of children.
Before using oxcarbazepine oral suspension, shake the bottle well and prepare the dose immediately afterwards. The prescribed amount of oral suspension should be withdrawn from the bottle using the oral dosing syringe supplied. Oxcarbazepine oral suspension can be mixed in a small glass of water just prior to administration or, alternatively, may be swallowed directly from the syringe. After each use, close the bottle and rinse the syringe with warm water and allow it to dry thoroughly.
Oxcarbazepine oral suspension can be taken with or without food [ see Clinical Pharmacology (12.3)].
2.1 Adjunctive Therapy for Adults
Treatment with oxcarbazepine should be initiated with a dose of 600 mg/day, given in a twice-a-day regimen. If clinically indicated, the dose may be increased by a maximum of 600 mg/day at approximately weekly intervals; the recommended daily dose is 1200 mg/day. Daily doses above 1200 mg/day show somewhat greater effectiveness in controlled trials, but most patients were not able to tolerate the 2400 mg/day dose, primarily because of CNS effects. It is recommended that the patient be observed closely and plasma levels of the concomitant AEDs be monitored during the period of oxcarbazepine titration, as these plasma levels may be altered, especially at oxcarbazepine doses greater than 1200 mg/day [ see Drug Interactions (7.1)].
2.2 Conversion to Monotherapy for Adults
Patients receiving concomitant AEDs may be converted to monotherapy by initiating treatment with oxcarbazepine at 600 mg/day (given in a twice-a-day regimen) while simultaneously initiating the reduction of the dose of the concomitant AEDs. The concomitant AEDs should be completely withdrawn over 3 to 6 weeks, while the maximum dose of oxcarbazepine should be reached in about 2 to 4 weeks. Oxcarbazepine may be increased as clinically indicated by a maximum increment of 600 mg/day at approximately weekly intervals to achieve the recommended daily dose of 2400 mg/day. A daily dose of 1200 mg/day has been shown in one study to be effective in patients in whom monotherapy has been initiated with oxcarbazepine. Patients should be observed closely during this transition phase.
2.3 Initiation of Monotherapy for Adults
Patients not currently being treated with AEDs may have monotherapy initiated with oxcarbazepine. In these patients, oxcarbazepine should be initiated at a dose of 600 mg/day (given in a twice-a-day regimen); the dose should be increased by 300 mg/day every third day to a dose of 1200 mg/day. Controlled trials in these patients examined the effectiveness of a 1200 mg/day dose; a dose of 2400 mg/day has been shown to be effective in patients converted from other AEDs to oxcarbazepine monotherapy (see above).
2.4 Adjunctive Therapy for Pediatric Patients (Aged 2 to 16 Years)
In pediatric patients aged 4 to 16 years, treatment should be initiated at a daily dose of 8 to 10 mg/kg generally not to exceed 600 mg/day, given in a twice-a-day regimen. The target maintenance dose of oxcarbazepine should be achieved over two weeks, and is dependent upon patient weight, according to the following chart:
20 to 29 kg - 900 mg/day
29.1 to 39 kg - 1200 mg/day
> 39 kg - 1800 mg/day
In the clinical trial, in which the intention was to reach these target doses, the median daily dose was 31 mg/kg with a range of 6 to 51 mg/kg.
In pediatric patients aged 2 to < 4 years, treatment should also be initiated at a daily dose of 8 to 10 mg/kg generally not to exceed 600 mg/day, given in a twice-a-day regimen. For patients under 20 kg, a starting dose of 16 to 20 mg/kg may be considered [ see Clinical Pharmacology (12.3)]. The maximum maintenance dose of oxcarbazepine should be achieved over 2 to 4 weeks and should not exceed 60 mg/kg/day in a twice-a-day regimen.
In the clinical trial in pediatric patients (2 to 4 years of age) in which the intention was to reach the target dose of 60 mg/kg/day, 50% of patients reached a final dose of at least 55 mg/kg/day.
Under adjunctive therapy (with and without enzyme-inducing AEDs), when normalized by body weight, apparent clearance (L/hr/kg) decreased when age increased such that children 2 to < 4 years of age may require up to twice the oxcarbazepine dose per body weight compared to adults; and children 4 to ≤ 12 years of age may require a 50% higher oxcarbazepine dose per body weight compared to adults.
2.5 Conversion to Monotherapy for Pediatric Patients (Aged 4 to 16 Years)
Patients receiving concomitant antiepileptic drugs may be converted to monotherapy by initiating treatment with oxcarbazepine at approximately 8 to 10 mg/kg/day given in a twice-a-day regimen, while simultaneously initiating the reduction of the dose of the concomitant antiepileptic drugs. The concomitant antiepileptic drugs can be completely withdrawn over 3 to 6 weeks while oxcarbazepine may be increased as clinically indicated by a maximum increment of 10 mg/kg/day at approximately weekly intervals to achieve the recommended daily dose. Patients should be observed closely during this transition phase.
The recommended total daily dose of oxcarbazepine is shown in the table below.
2.6 Initiation of Monotherapy for Pediatric Patients (Aged 4 to 16 Years)
Patients not currently being treated with antiepileptic drugs may have monotherapy initiated with oxcarbazepine. In these patients, oxcarbazepine should be initiated at a dose of 8 to 10 mg/kg/day given in a twice-a-day regimen. The dose should be increased by 5 mg/kg/day every third day to the recommended daily dose shown in the table below.
Table 1 Range of Maintenance Doses of Oxcarbazepine for Children by Weight During Monotherapy From To Weight in kg Dose (mg/day) Dose (mg/day) 20
600
900
25
900
1200
30
900
1200
35
900
1500
40
900
1500
45
1200
1500
50
1200
1800
55
1200
1800
60
1200
2100
65
1200
2100
70
1500
2100
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Hyponatremia
Clinically significant hyponatremia (sodium < 125 mmol/L) can develop during oxcarbazepine use. In the 14 controlled epilepsy studies 2.5% of oxcarbazepine-treated patients (38/1,524) had a sodium of less than 125 mmol/L at some point during treatment, compared to no such patients assigned placebo or active control (carbamazepine and phenobarbital for adjunctive and monotherapy substitution studies, and phenytoin and valproate for the monotherapy initiation studies). Clinically significant hyponatremia generally occurred during the first three months of treatment with oxcarbazepine, although there were patients who first developed a serum sodium < 125 mmol/L more than one year after initiation of therapy. Most patients who developed hyponatremia were asymptomatic but patients in the clinical trials were frequently monitored and some had their oxcarbazepine dose reduced, discontinued, or had their fluid intake restricted for hyponatremia. Whether or not these maneuvers prevented the occurrence of more severe events is unknown. Cases of symptomatic hyponatremia have been reported during postmarketing use. In clinical trials, patients whose treatment with oxcarbazepine was discontinued due to hyponatremia generally experienced normalization of serum sodium within a few days without additional treatment.
Measurement of serum sodium levels should be considered for patients during maintenance treatment with oxcarbazepine, particularly if the patient is receiving other medications known to decrease serum sodium levels (for example, drugs associated with inappropriate ADH secretion) or if symptoms possibly indicating hyponatremia develop (e.g., nausea, malaise, headache, lethargy, confusion, obtundation, or increase in seizure frequency or severity).
5.2 Anaphylactic Reactions and Angioedema
Rare cases of anaphylaxis and angioedema involving the larynx, glottis, lips and eyelids have been reported in patients after taking the first or subsequent doses of oxcarbazepine. Angioedema associated with laryngeal edema can be fatal. If a patient develops any of these reactions after treatment with oxcarbazepine, the drug should be discontinued and an alternative treatment started. These patients should not be rechallenged with the drug [ see Warnings and Precautions (5.3)].
5.3 Patients with a Past History of Hypersensitivity Reaction to Carbamazepine
Patients who have had hypersensitivity reactions to carbamazepine should be informed that approximately 25% to 30% of them will experience hypersensitivity reactions with oxcarbazepine. For this reason patients should be specifically questioned about any prior experience with carbamazepine, and patients with a history of hypersensitivity reactions to carbamazepine should ordinarily be treated with oxcarbazepine only if the potential benefit justifies the potential risk. If signs or symptoms of hypersensitivity develop, oxcarbazepine should be discontinued immediately [ see Warnings and Precautions (5.2, 5.8)].
5.4 Serious Dermatological Reactions
Serious dermatological reactions, including Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN), have been reported in both children and adults in association with oxcarbazepine use. The median time of onset for reported cases was 19 days. Such serious skin reactions may be life threatening, and some patients have required hospitalization with very rare reports of fatal outcome. The median time of onset for reported cases was 19 days after treatment initiation. Recurrence of the serious skin reactions following rechallenge with oxcarbazepine has also been reported.
The reporting rate of TEN and SJS associated with oxcarbazepine use, which is generally accepted to be an underestimate due to underreporting, exceeds the background incidence rate estimates by a factor of 3- to 10-fold. Estimates of the background incidence rate for these serious skin reactions in the general population range between 0.5 to 6 cases per million-person years. Therefore, if a patient develops a skin reaction while taking oxcarbazepine, consideration should be given to discontinuing oxcarbazepine use and prescribing another antiepileptic medication.
Association with HLA-B*1502
Patients carrying the HLA-B*1502 allele may be at increased risk for SJS/TEN with oxcarbazepine treatment.
Human Leukocyte Antigen (HLA) allele B*1502 increases the risk for developing SJS/TEN in patients treated with carbamazepine. The chemical structure of oxcarbazepine is similar to that of carbamazepine. Available clinical evidence, and data from nonclinical studies showing a direct interaction between oxcarbazepine and HLA-B*1502 protein, suggest that the HLA-B*1502 allele may also increase the risk for SJS/TEN with oxcarbazepine.
The frequency of HLA-B*1502 allele ranges from 2 to 12% in Han Chinese populations, is about 8% in Thai populations, and above 15% in the Philippines and in some Malaysian populations. Allele frequencies up to about 2% and 6% have been reported in Korea and India, respectively. The frequency of the HLA-B*1502 allele is negligible in people from European descent, several African populations, indigenous peoples of the Americas, Hispanic populations, and in Japanese (< 1%).
Testing for the presence of the HLA-B*1502 allele should be considered in patients with ancestry in genetically at-risk populations, prior to initiating treatment with oxcarbazepine. The use of oxcarbazepine should be avoided in patients positive for HLA-B*1502 unless the benefits clearly outweigh the risks. Consideration should also be given to avoid the use of other drugs associated with SJS/TEN in HLA-B*1502 positive patients, when alternative therapies are otherwise equally acceptable. Screening is not generally recommended in patients from populations in which the prevalence of HLAB*1502 is low, or in current oxcarbazepine users, as the risk of SJS/TEN is largely confined to the first few months of therapy, regardless of HLA B*1502 status.
The use of HLA-B*1502 genotyping has important limitations and must never substitute for appropriate clinical vigilance and patient management. The role of other possible factors in the development of, and morbidity from, SJS/TEN, such as antiepileptic drug (AED) dose, compliance, concomitant medications, comorbidities, and the level of dermatologic monitoring have not been well characterized.
5.5 Suicidal Behavior and Ideation
Antiepileptic drugs (AEDs), including oxcarbazepine, increase the risk of suicidal thoughts or behavior in patients taking these drugs for any indication. Patients treated with any AED for any indication should be monitored for the emergence or worsening of depression, suicidal thoughts or behavior, and/or any unusual changes in mood or behavior.
Pooled analyses of 199 placebo-controlled clinical trials (mono- and adjunctive therapy) of 11 different AEDs showed that patients randomized to one of the AEDs had approximately twice the risk (adjusted Relative Risk 1.8, 95% CI:1.2, 2.7) of suicidal thinking or behavior compared to patients randomized to placebo. In these trials, which had a median treatment duration of 12 weeks, the estimated incidence rate of suicidal behavior or ideation among 27,863 AED-treated patients was 0.43%, compared to 0.24% among 16,029 placebo-treated patients, representing an increase of approximately one case of suicidal thinking or behavior for every 530 patients treated. There were four suicides in drug-treated patients in the trials and none in placebo-treated patients, but the number is too small to allow any conclusion about drug effect on suicide.
The increased risk of suicidal thoughts or behavior with AEDs was observed as early as one week after starting drug treatment with AEDs and persisted for the duration of treatment assessed. Because most trials included in the analysis did not extend beyond 24 weeks, the risk of suicidal thoughts or behavior beyond 24 weeks could not be assessed.
The risk of suicidal thoughts or behavior was generally consistent among drugs in the data analyzed. The finding of increased risk with AEDs of varying mechanisms of action and across a range of indications suggests that the risk applies to all AEDs used for any indication. The risk did not vary substantially by age (5 to 100 years) in the clinical trials analyzed. Table 2 shows absolute and relative risk by indication for all evaluated AEDs.
Table 2 Risk by Indication for Antiepileptic Drugs in the Pooled Analysis Indication
Placebo Patients with Events Per 1,000 Patients
Patients with Events Per 1,000 Patients
Relative Risk: Incidence of Events in Drug Patients/Incidence in Placebo Patients
Risk Difference: Additional Drug Patients with Events Per 1,000 Patients
Epilepsy
1
3.4
3.5
2.4
Psychiatric
5.7
8.5
1.5
2.9
Other
1
1.8
1.9
0.9
Total
2.4
4.3
1.8
1.9
The relative risk for suicidal thoughts or behavior was higher in clinical trials for epilepsy than in clinical trials for psychiatric or other conditions, but the absolute risk differences were similar for the epilepsy and psychiatric indications.
Anyone considering prescribing oxcarbazepine or any other AED must balance the risk of suicidal thoughts or behavior with the risk of untreated illness. Epilepsy and many other illnesses for which AEDs are prescribed are themselves associated with morbidity and mortality and an increased risk of suicidal thoughts and behavior. Should suicidal thoughts and behavior emerge during treatment, the prescriber needs to consider whether the emergence of these symptoms in any given patient may be related to the illness being treated.
Patients, their caregivers, and families should be informed that AEDs increase the risk of suicidal thoughts and behavior and should be advised of the need to be alert for the emergence or worsening of the signs and symptoms of depression, any unusual changes in mood or behavior, or the emergence of suicidal thoughts, behavior, or thoughts about self-harm. Behaviors of concern should be reported immediately to healthcare providers.
5.6 Withdrawal of AEDs
As with all antiepileptic drugs, oxcarbazepine should be withdrawn gradually to minimize the potential of increased seizure frequency.
5.7 Cognitive/Neuropsychiatric Adverse Events
Use of oxcarbazepine has been associated with central nervous system-related adverse events. The most significant of these can be classified into three general categories: 1) cognitive symptoms including psychomotor slowing, difficulty with concentration, and speech or language problems, 2) somnolence or fatigue, and 3) coordination abnormalities, including ataxia and gait disturbances.
Adult Patients
In one large, fixed-dose study, oxcarbazepine was added to existing AED therapy (up to three concomitant AEDs). By protocol, the dosage of the concomitant AEDs could not be reduced as oxcarbazepine was added, reduction in oxcarbazepine dosage was not allowed if intolerance developed, and patients were discontinued if unable to tolerate their highest target maintenance doses. In this trial, 65% of patients were discontinued because they could not tolerate the 2400 mg/day dose of oxcarbazepine on top of existing AEDs. The adverse events seen in this study were primarily CNS related and the risk for discontinuation was dose related.
In this trial, 7.1% of oxcarbazepine-treated patients and 4% of placebo-treated patients experienced a cognitive adverse event. The risk of discontinuation for these events was about 6.5 times greater on oxcarbazepine than on placebo. In addition, 26% of oxcarbazepine-treated patients and 12% of placebo-treated patients experienced somnolence. The risk of discontinuation for somnolence was about 10 times greater on oxcarbazepine than on placebo. Finally, 28.7% of oxcarbazepine-treated patients and 6.4% of placebo-treated patients experienced ataxia or gait disturbances. The risk for discontinuation for these events was about seven times greater on oxcarbazepine than on placebo.
In a single placebo-controlled monotherapy trial evaluating 2400 mg/day of oxcarbazepine, no patients in either treatment group discontinued double-blind treatment because of cognitive adverse events, somnolence, ataxia, or gait disturbance.
In the two dose-controlled conversion to monotherapy trials comparing 2400 mg/day and 300 mg/day oxcarbazepine, 1.1% of patients in the 2400 mg/day group discontinued double-blind treatment because of somnolence or cognitive adverse events compared to 0% in the 300 mg/day group. In these trials, no patients discontinued because of ataxia or gait disturbances in either treatment group.
Pediatric Patients
A study was conducted in pediatric patients (3 to 17 years old) with inadequately controlled partial seizures in which oxcarbazepine was added to existing AED therapy (up to two concomitant AEDs). By protocol, the dosage of concomitant AEDs could not be reduced as oxcarbazepine was added. Oxcarbazepine was titrated to reach a target dose ranging from 30 mg/kg to 46 mg/kg (based on a patient’s body weight with fixed doses for predefined weight ranges).
Cognitive adverse events occurred in 5.8% of oxcarbazepine-treated patients (the single most common event being concentration impairment, 4 of 138 patients) and in 3.1% of patients treated with placebo. In addition, 34.8% of oxcarbazepine-treated patients and 14% of placebo-treated patients experienced somnolence. (No patient discontinued due to a cognitive adverse event or somnolence.). Finally, 23.2% of oxcarbazepine-treated patients and 7% of placebo-treated patients experienced ataxia or gait disturbances. Two (1.4%) oxcarbazepine-treated patients and 1 (0.8%) placebo-treated patient discontinued due to ataxia or gait disturbances.
5.8 Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS)/Multi-Organ Hypersensitivity
Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS), also known as multi-organ hypersensitivity, has occurred with Trileptal. Some of these events have been fatal or life-threatening. DRESS typically, although not exclusively, presents with fever, rash, and/or lymphadenopathy, in association with other organ system involvement, such as hepatitis, nephritis, hematologic abnormalities, myocarditis, or myositis, sometimes resembling an acute viral infection. Eosinophilia is often present. This disorder is variable in its expression, and other organ systems not noted here may be involved. It is important to note that early manifestations of hypersensitivity (e.g., fever, lymphadenopathy) may be present even though rash is not evident. If such signs or symptoms are present, the patient should be evaluated immediately. Oxcarbazepine should be discontinued if an alternative etiology for the signs or symptoms cannot be established. Although there are no case reports to indicate cross sensitivity with other drugs that produce this syndrome, the experience amongst drugs associated with DRESS/multi-organ hypersensitivity would indicate this to be a possibility [ see Warnings and Precautions (5.3)].
5.9 Hematologic Events
Rare reports of pancytopenia, agranulocytosis, and leukopenia have been seen in patients treated with oxcarbazepine during postmarketing experience. Discontinuation of the drug should be considered if any evidence of these hematologic events develop.
5.10 Seizure Control During Pregnancy
Due to physiological changes during pregnancy, plasma levels of the active metabolite of oxcarbazepine, the 10-monohydroxy derivative (MHD), may gradually decrease throughout pregnancy. It is recommended that patients be monitored carefully during pregnancy. Close monitoring should continue through the postpartum period because MHD levels may return after delivery.
5.11 Laboratory Tests
Serum sodium levels below 125 mmol/L have been observed in patients treated with oxcarbazepine [ see Warnings and Precautions (5.1)]. Experience from clinical trials indicates that serum sodium levels return toward normal when the oxcarbazepine dosage is reduced or discontinued, or when the patient was treated conservatively (e.g., fluid restriction).
Laboratory data from clinical trials suggest that oxcarbazepine use was associated with decreases in T 4, without changes in T3 or TSH.
-
6 ADVERSE REACTIONS
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
6.1 Clinical Studies Experience
Most Common Adverse Reactions in All Clinical Studies
Adjunctive Therapy/Monotherapy in Adults Previously Treated with other AEDs: The most commonly observed (≥ 5%) adverse reactions seen in association with oxcarbazepine and substantially more frequent than in placebo-treated patients were: dizziness, somnolence, diplopia, fatigue, nausea, vomiting, ataxia, abnormal vision, abdominal pain, tremor, dyspepsia, abnormal gait.
Approximately 23% of these 1,537 adult patients discontinued treatment because of an adverse experience. The adverse reactions most commonly associated with discontinuation were: dizziness (6.4%), diplopia (5.9%), ataxia (5.2%), vomiting (5.1%), nausea (4.9%), somnolence (3.8%), headache (2.9%), fatigue (2.1%), abnormal vision (2.1%), tremor (1.8%), abnormal gait (1.7%), rash (1.4%), hyponatremia (1%).
Monotherapy in Adults Not Previously Treated with other AEDs: The most commonly observed (≥ 5%) adverse reactions seen in association with oxcarbazepine in these patients were similar to those in previously treated patients.
Approximately 9% of these 295 adult patients discontinued treatment because of an adverse experience. The adverse reactions most commonly associated with discontinuation were: dizziness (1.7%), nausea (1.7%), rash (1.7%), headache (1.4%).
Adjunctive Therapy/Monotherapy in Pediatric Patients 4 Years Old and Above Previously Treated with other AEDs: The most commonly observed (≥ 5%) adverse reactions seen in association with oxcarbazepine in these patients were similar to those seen in adults.
Approximately 11% of these 456 pediatric patients discontinued treatment because of an adverse experience. The adverse reactions most commonly associated with discontinuation were: somnolence (2.4%), vomiting (2%), ataxia (1.8%), diplopia (1.3%), dizziness (1.3%), fatigue (1.1%), nystagmus (1.1%).
Monotherapy in Pediatric Patients 4 Years Old and Above Not Previously Treated with other AEDs: The most commonly observed (≥ 5%) adverse reactions seen in association with oxcarbazepine in these patients were similar to those in adults.
Approximately 9.2% of 152 pediatric patients discontinued treatment because of an adverse experience. The adverse reactions most commonly associated (≥ 1%) with discontinuation were rash (5.3%) and maculopapular rash (1.3%).
Adjunctive Therapy/Monotherapy in Pediatric Patients 1 Month to < 4 Years Old Previously Treated or Not Previously Treated with other AEDs: The most commonly observed (≥ 5%) adverse reactions seen in association with oxcarbazepine in these patients were similar to those seen in older children and adults except for infections and infestations which were more frequently seen in these younger children.
Approximately 11% of these 241 pediatric patients discontinued treatment because of an adverse experience. The adverse reaction most commonly associated with discontinuation were: convulsions (3.7%), status epilepticus (1.2%), and ataxia (1.2%).
Incidence in Controlled Clinical Studies: The prescriber should be aware that the figures in Tables 3, 4, 5 and 6 cannot be used to predict the frequency of adverse reactions in the course of usual medical practice where patient characteristics and other factors may differ from those prevailing during clinical studies. Similarly, the cited frequencies cannot be directly compared with figures obtained from other clinical investigations involving different treatments, uses, or investigators. An inspection of these frequencies, however, does provide the prescriber with one basis to estimate the relative contribution of drug and nondrug factors to the adverse event incidences in the population studied.
Controlled Clinical Studies of Adjunctive Therapy/Monotherapy in Adults Previously Treated with other AEDs: Table 3 lists treatment-emergent signs and symptoms that occurred in at least 2% of adult patients with epilepsy treated with oxcarbazepine or placebo as adjunctive treatment and were numerically more common in the patients treated with any dose of oxcarbazepine. Table 4 lists treatment-emergent signs and symptoms in patients converted from other AEDs to either high dose oxcarbazepine or low dose (300 mg) oxcarbazepine. Note that in some of these monotherapy studies patients who dropped out during a preliminary tolerability phase are not included in the tables.
Table 3 Treatment-Emergent Adverse Event Incidence in a Controlled Clinical Study of Adjunctive Therapy in Adults (Events in at Least 2% of Patients Treated with 2400 mg/day of Oxcarbazepine and Numerically More Frequent than in the Placebo Group) Oxcarbazepine Dosage (mg/day) Body System/
Adverse EventOXC 600
N = 163
%OXC 1200
N = 171
%OXC 2400
N = 126
%Placebo
N = 166
%Body as a Whole
Fatigue
15
12
15
7
Asthenia
6
3
6
5
Edema Legs
2
1
2
1
Weight Increase
1
2
2
1
Feeling Abnormal
0
1
2
0
Cardiovascular System
Hypotension
0
1
2
0
Digestive System
Nausea
15
25
29
10
Vomiting
13
25
36
5
Pain Abdominal
10
13
11
5
Diarrhea
5
6
7
6
Dyspepsia
5
5
6
2
Constipation
2
2
6
4
Gastritis
2
1
2
1
Metabolic and Nutritional Disorders
Hyponatremia
3
1
2
1
Musculoskeletal System
Muscle Weakness
1
2
2
0
Sprains and Strains
0
2
2
1
Nervous System
Headache
32
28
26
23
Dizziness
26
32
49
13
Somnolence
20
28
36
12
Ataxia
9
17
31
5
Nystagmus
7
20
26
5
Gait Abnormal
5
10
17
1
Insomnia
4
2
3
1
Tremor
3
8
16
5
Nervousness
2
4
2
1
Agitation
1
1
2
1
Coordination Abnormal
1
3
2
1
EEG Abnormal
0
0
2
0
Speech Disorder
1
1
3
0
Confusion
1
1
2
1
Cranial Injury NOS
1
0
2
1
Dysmetria
1
2
3
0
Thinking Abnormal
0
2
4
0
Respiratory System
Rhinitis
2
4
5
4
Skin and Appendages
Acne
1
2
2
0
Special Senses
Diplopia
14
30
40
5
Vertigo
6
12
15
2
Vision Abnormal
6
14
13
4
Accommodation Abnormal
0
0
2
0
Table 4 Treatment-Emergent Adverse Event Incidence in Controlled Clinical Studies of Monotherapy in Adults Previously Treated with Other AEDs (Events in at Least 2% of Patients Treated with 2400 mg/day of Oxcarbazepine and Numerically More Frequent than in the Low Dose Control Group) Oxcarbazepine Dosage (mg/day) Body System/
Adverse Event2400
N = 86
%300
N = 86
%Body as a Whole
Fatigue
21
5
Fever
3
0
Allergy
2
0
Edema Generalized
2
1
Pain Chest
2
0
Digestive System
Nausea
22
7
Vomiting
15
5
Diarrhea
7
5
Dyspepsia
6
1
Anorexia
5
3
Pain Abdominal
5
3
Mouth Dry
3
0
Hemorrhage Rectum
2
0
Toothache
2
1
Hemic and Lymphatic System
Lymphadenopathy
2
0
Infections and Infestations
Infection Viral
7
5
Infection
2
0
Metabolic and Nutritional Disorders
Hyponatremia
5
0
Thirst
2
0
Nervous System
Headache
31
15
Dizziness
28
8
Somnolence
19
5
Anxiety
7
5
Ataxia
7
1
Confusion
7
0
Nervousness
7
0
Insomnia
6
3
Tremor
6
3
Amnesia
5
1
Convulsions Aggravated
5
2
Emotional Lability
3
2
Hypoesthesia
3
1
Coordination Abnormal
2
1
Nystagmus
2
0
Speech Disorder
2
0
Respiratory System
Upper Respiratory Tract Infection
10
5
Coughing
5
0
Bronchitis
3
0
Pharyngitis
3
0
Skin and Appendages
Hot Flushes
2
1
Purpura
2
0
Special Senses
Vision Abnormal
14
2
Diplopia
12
1
Taste Perversion
5
0
Vertigo
3
0
Earache
2
1
Ear Infection NOS
2
0
Urogenital and Reproductive System
Urinary Tract Infection
5
1
Micturition Frequency
2
1
Vaginitis
2
0
Controlled Clinical Study of Monotherapy in Adults Not Previously Treated with other AEDs: Table 5 lists treatment-emergent signs and symptoms in a controlled clinical study of monotherapy in adults not previously treated with other AEDs that occurred in at least 2% of adult patients with epilepsy treated with oxcarbazepine or placebo and were numerically more common in the patients treated with oxcarbazepine.
Table 5 Treatment-Emergent Adverse Event Incidence in a Controlled Clinical Study of Monotherapy in Adults Not Previously Treated with Other AEDs (Events in at Least 2% of Patients Treated with Oxcarbazepine and Numerically More Frequent than in the Placebo Group) Body System/
Adverse EventOxcarbazepine
N = 55
%Placebo
N = 49
%Body as a Whole
Falling Down NOS
4
0
Digestive System
Nausea
16
12
Diarrhea
7
2
Vomiting
7
6
Constipation
5
0
Dyspepsia
5
4
Musculoskeletal System
Pain Back
4
2
Nervous System
Dizziness
22
6
Headache
13
10
Ataxia
5
0
Nervousness
5
2
Amnesia
4
2
Coordination Abnormal
4
2
Tremor
4
0
Respiratory System
Upper Respiratory Tract Infection
7
0
Epistaxis
4
0
Infection Chest
4
0
Sinusitis
4
2
Skin and Appendages
Rash
4
2
Special Senses
Vision Abnormal
4
0
Controlled Clinical Studies of Adjunctive Therapy/Monotherapy in Pediatric Patients Previously Treated with other AEDs: Table 6 lists treatment-emergent signs and symptoms that occurred in at least 2% of pediatric patients with epilepsy treated with oxcarbazepine or placebo as adjunctive treatment and were numerically more common in the patients treated with oxcarbazepine.
Table 6 Treatment-Emergent Adverse Event Incidence in Controlled Clinical Studies of Adjunctive Therapy/Monotherapy in Pediatric Patients Previously Treated with Other AEDs (Events in at Least 2% of Patients Treated with Oxcarbazepine and Numerically More Frequent than in the Placebo Group) Body System/
Adverse EventOxcarbazepine
N = 171
%Placebo
N = 139
%Body as a Whole
Fatigue
13
9
Allergy
2
0
Asthenia
2
1
Digestive System
Vomiting
33
14
Nausea
19
5
Constipation
4
1
Dyspepsia
2
0
Nervous System
Headache
31
19
Somnolence
31
13
Dizziness
28
8
Ataxia
13
4
Nystagmus
9
1
Emotional Lability
8
4
Gait Abnormal
8
3
Tremor
6
4
Speech Disorder
3
1
Concentration Impaired
2
1
Convulsions
2
1
Muscle Contractions Involuntary
2
1
Respiratory System
Rhinitis
10
9
Pneumonia
2
1
Skin and Appendages
Bruising
4
2
Sweating Increased
3
0
Special Senses
Diplopia
17
1
Vision Abnormal
13
1
Vertigo
2
0
Other Events Observed in Association with the Administration of Oxcarbazepine
In the paragraphs that follow, the adverse events, other than those in the preceding tables or text, that occurred in a total of 565 children and 1,574 adults exposed to oxcarbazepine and that are reasonably likely to be related to drug use are presented. Events common in the population, events reflecting chronic illness and events likely to reflect concomitant illness are omitted particularly if minor. They are listed in order of decreasing frequency. Because the reports cite events observed in open label and uncontrolled trials, the role of oxcarbazepine in their causation cannot be reliably determined.
Body as a Whole: fever, malaise, pain chest precordial, rigors, weight decrease.
Cardiovascular System: bradycardia, cardiac failure, cerebral hemorrhage, hypertension, hypotension postural, palpitation, syncope, tachycardia.
Digestive System: appetite increased, blood in stool, cholelithiasis, colitis, duodenal ulcer, dysphagia, enteritis, eructation, esophagitis, flatulence, gastric ulcer, gingival bleeding, gum hyperplasia, hematemesis, hemorrhage rectum, hemorrhoids, hiccup, mouth dry, pain biliary, pain right hypochondrium, retching, sialoadenitis, stomatitis, stomatitis ulcerative.
Hematologic and Lymphatic System: thrombocytopenia.
Laboratory Abnormality: gamma-GT increased, hyperglycemia, hypocalcemia, hypoglycemia, hypokalemia, liver enzymes elevated, serum transaminase increased.
Musculoskeletal System: hypertonia muscle.
Nervous System: aggressive reaction, amnesia, anguish, anxiety, apathy, aphasia, aura, convulsions aggravated, delirium, delusion, depressed level of consciousness, dysphonia, dystonia, emotional lability, euphoria, extrapyramidal disorder, feeling drunk, hemiplegia, hyperkinesia, hyperreflexia, hypoesthesia, hypokinesia, hyporeflexia, hypotonia, hysteria, libido decreased, libido increased, manic reaction, migraine, muscle contractions involuntary, nervousness, neuralgia, oculogyric crisis, panic disorder, paralysis, paroniria, personality disorder, psychosis, ptosis, stupor, tetany.
Respiratory System: asthma, dyspnea, epistaxis, laryngismus, pleurisy.
Skin and Appendages: acne, alopecia, angioedema, bruising, dermatitis contact, eczema, facial rash, flushing, folliculitis, heat rash, hot flushes, photosensitivity reaction, pruritus genital, psoriasis, purpura, rash erythematous, rash maculopapular, vitiligo, urticaria.
Special Senses: accommodation abnormal, cataract, conjunctival hemorrhage, edema eye, hemianopia, mydriasis, otitis externa, photophobia, scotoma, taste perversion, tinnitus, xerophthalmia.
Surgical and Medical Procedures: procedure dental oral, procedure female reproductive, procedure musculoskeletal, procedure skin.
Urogenital and Reproductive System: dysuria, hematuria, intermenstrual bleeding, leukorrhea, menorrhagia, micturition frequency, pain renal, pain urinary tract, polyuria, priapism, renal calculus.
Other: Systemic lupus erythematosus.
6.2 Postmarketing and Other Experience
The following adverse events not seen in controlled clinical trials have been observed in named patient programs or postmarketing experience. Because these reactions are reported voluntarily from a population of uncertain size, it is not possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Anaphylaxis: [see Warnings and Precautions (5.2)]
Digestive System: pancreatitis and/or lipase and/or amylase increase
Hematologic and Lymphatic Systems: aplastic anemia [see Warnings and Precautions (5.9)]
Metabolism: hypothyroidism
Skin and subcutaneous tissue disorders: erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis [see Warnings and Precautions (5.4)] , Acute Generalized Exanthematous Pustulosis (AGEP)
Musculoskeletal, connective tissue and bone disorders: There have been reports of decreased bone mineral density, osteoporosis and fractures in patients on long-term therapy with oxcarbazepine.
-
7 DRUG INTERACTIONS
Oxcarbazepine can inhibit CYP2C19 and induce CYP3A4/5 with potentially important effects on plasma concentrations of other drugs. The inhibition of CYP2C19 by oxcarbazepine and MHD can cause increased plasma concentrations of drugs that are substrates of CYP2C19. Oxcarbazepine and MHD induce a subgroup of the cytochrome P450 3A family (CYP3A4 and CYP3A5) responsible for the metabolism of dihydropyridine calcium antagonists, oral contraceptives and cyclosporine resulting in a lower plasma concentration of these drugs. [ see Clinical Pharmacology (12.3)]
In addition, several AEDs that are cytochrome P450 inducers can decrease plasma concentrations of oxcarbazepine and MHD. No autoinduction has been observed with oxcarbazepine.
7.1 Antiepileptic Drugs
Potential interactions between oxcarbazepine and other AEDs were assessed in clinical studies. The effect of these interactions on mean AUCs and C min are summarized in Table 7.
Table 7 Summary of AED Interactions with Oxcarbazepine 1 nc denotes a mean change of less than 10% 2 Pediatrics 3 Mean increase in adults at high oxcarbazepine doses AED Coadministered
Dose of AED (mg/day)
Oxcarbazepine
Dose (mg/day)Influence of Oxcarbazepineon AED Concentration (Mean Change, 90% Confidence Interval)
Influence of AED on MHD Concentration (Mean Change, 90% Confidence Interval)
Carbamazepine
400 to 2000
900
nc1
40% decrease [CI: 17% decrease, 57% decrease]
Phenobarbital
100 to 150
600 to 1800
14% increase [CI: 2% increase, 24% increase]
25% decrease [CI: 12% decrease, 51% decrease]
Phenytoin
250 to 500
600 to 1800 > 1200 to 2400
nc1,2 up to 40% increase3 [CI: 12% increase, 60% increase]
30% decrease [CI: 3% decrease, 48% decrease]
Valproic acid
400 to 2800
600 to 1800
nc1
18% decrease [CI: 13% decrease, 40% decrease]
In vivo, the plasma levels of phenytoin increased by up to 40% when oxcarbazepine was given at doses above 1200 mg/day. Therefore, when using doses of oxcarbazepine greater than 1200 mg/day during adjunctive therapy, a decrease in the dose of phenytoin may be required. The increase of phenobarbital level, however, is small (15%) when given with oxcarbazepine.
Strong inducers of cytochrome P450 enzymes (i.e., carbamazepine, phenytoin and phenobarbital) have been shown to decrease the plasma levels of MHD (29% to 40%).
No autoinduction has been observed with oxcarbazepine.
7.2 Hormonal Contraceptives
Coadministration of oxcarbazepine with an oral contraceptive has been shown to influence the plasma concentrations of the two hormonal components, ethinylestradiol (EE) and levonorgestrel (LNG). The mean AUC values of EE were decreased by 48% [90% CI: 22 to 65] in one study and 52% [90% CI: 38 to 52] in another study. The mean AUC values of LNG were decreased by 32% [90% CI: 20 to 45] in one study and 52% [90% CI: 42 to 52] in another study. Therefore, concurrent use of oxcarbazepine with hormonal contraceptives may render these contraceptives less effective. Studies with other oral or implant contraceptives have not been conducted.
7.3 Calcium Antagonists
After repeated coadministration of oxcarbazepine, the AUC of felodipine was lowered by 28% [90% CI: 20 to 33]. Verapamil produced a decrease of 20% [90% CI: 18 to 27] of the plasma levels of MHD.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Oxcarbazepine levels may decrease during pregnancy [see Warnings and Precautions (5.10)].
Pregnancy Category C
There are no adequate and well-controlled clinical studies of oxcarbazepine in pregnant women; however, oxcarbazepine is closely related structurally to carbamazepine, which is considered to be teratogenic in humans. Given this fact, and the results of the animal studies described, it is likely that oxcarbazepine is a human teratogen. Oxcarbazepine should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Increased incidences of fetal structural abnormalities and other manifestations of developmental toxicity (embryolethality, growth retardation) were observed in the offspring of animals treated with either oxcarbazepine or its active 10-hydroxy metabolite (MHD) during pregnancy at doses similar to the maximum recommended human dose.
When pregnant rats were given oxcarbazepine (30, 300, or 1000 mg/kg) orally throughout the period of organogenesis, increased incidences of fetal malformations (craniofacial, cardiovascular, and skeletal) and variations were observed at the intermediate and high doses (approximately 1.2 and 4 times, respectively, the maximum recommended human dose [MRHD] on a mg/m 2 basis). Increased embryofetal death and decreased fetal body weights were seen at the high dose. Doses ≥ 300 mg/kg were also maternally toxic (decreased body weight gain, clinical signs), but there is no evidence to suggest that teratogenicity was secondary to the maternal effects.
In a study in which pregnant rabbits were orally administered MHD (20, 100, or 200 mg/kg) during organogenesis, embryofetal mortality was increased at the highest dose (1.5 times the MRHD on a mg/m 2 basis). This dose produced only minimal maternal toxicity.
In a study in which female rats were dosed orally with oxcarbazepine (25, 50, or 150 mg/kg) during the latter part of gestation and throughout the lactation period, a persistent reduction in body weights and altered behavior (decreased activity) were observed in offspring exposed to the highest dose (0.6 times the MRHD on a mg/m 2 basis). Oral administration of MHD (25, 75, or 250 mg/kg) to rats during gestation and lactation resulted in a persistent reduction in offspring weights at the highest dose (equivalent to the MRHD on a mg/m2 basis).
To provide information regarding the effects of in utero exposure to oxcarbazepine, physicians are advised to recommend that pregnant patients taking oxcarbazepine enroll in the NAAED Pregnancy Registry. This can be done by calling the toll free number 1-888-233-2334, and must be done by patients themselves. Information on the registry can also be found at the website http://www.aedpregnancyregistry.org/.
8.2 Labor and Delivery
The effect of oxcarbazepine on labor and delivery in humans has not been evaluated.
8.3 Nursing Mothers
Oxcarbazepine and its active metabolite (MHD) are excreted in human milk. A milk-to-plasma concentration ratio of 0.5 was found for both. Because of the potential for serious adverse reactions to oxcarbazepine in nursing infants, a decision should be made about whether to discontinue nursing or to discontinue the drug in nursing women, taking into account the importance of the drug to the mother.
8.4 Pediatric Use
Oxcarbazepine is indicated for use as adjunctive therapy for partial seizures in patients aged 2 to 16 years. Oxcarbazepine is also indicated as monotherapy for partial seizures in patients aged 4 to 16 years. Oxcarbazepine has been given to 898 patients between the ages of 1 month to 17 years in controlled clinical trials (332 treated as monotherapy) and about 677 patients between the ages of 1 month to 17 years in other trials [ see Adverse Reactions (6.1) for a description of the adverse events associated with oxcarbazepine use in this population].
8.5 Geriatric Use
There were 52 patients over age 65 in controlled clinical trials and 565 patients over the age of 65 in other trials. Following administration of single (300 mg) and multiple (600 mg/day) doses of oxcarbazepine in elderly volunteers (60 to 82 years of age), the maximum plasma concentrations and AUC values of MHD were 30% to 60% higher than in younger volunteers (18 to 32 years of age). Comparisons of creatinine clearance in young and elderly volunteers indicate that the difference was due to age-related reductions in creatinine clearance.
8.6 Renal Impairment
In renally-impaired patients (creatinine clearance < 30 mL/min), the elimination half-life of MHD is prolonged with a corresponding two-fold increase in AUC [ see Clinical Pharmacology (12.3)]. Oxcarbazepine therapy should be initiated at one-half the usual starting dose and increased, if necessary, at a slower than usual rate until the desired clinical response is achieved.
- 9 DRUG ABUSE AND DEPENDENCE
-
10 OVERDOSAGE
Human Overdose Experience
Isolated cases of overdose with oxcarbazepine have been reported. The maximum dose taken was approximately 24,000 mg. All patients recovered with symptomatic treatment.
Treatment and Management
There is no specific antidote. Symptomatic and supportive treatment should be administered as appropriate. Removal of the drug by gastric lavage and/or inactivation by administering activated charcoal should be considered.
-
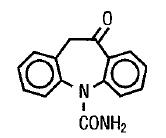
11 DESCRIPTION
Oxcarbazepine, USP is an antiepileptic drug available as a 300 mg/5 mL (60 mg/mL) oral suspension. Oxcarbazepine, USP is 10,11-Dihydro-10-oxo-5 H-dibenz[b,f]azepine-5-carboxamide, and its structural formula is
Oxcarbazepine, USP is a light orange to creamish white or off-white powder. It is soluble in acetic acid, sparingly soluble in chloroform, and practically insoluble in water. Its molecular weight is 252.27.
Oxcarbazepine oral suspension, USP contains the following inactive ingredients: artificial cherry flavor, ascorbic acid, carboxymethylcellulose sodium, colloidal silicon dioxide, copovidone, hydroxy ethylcellulose, methyl paraben, microcrystalline cellulose, non crystallizing sorbitol solution, propylene glycol, polyoxyl 8 stearate, povidone, propyl paraben, purified water, saccharin sodium, and sorbic acid.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The pharmacological activity of oxcarbazepine is primarily exerted through the 10-monohydroxy metabolite (MHD) of oxcarbazepine [see Clinical Pharmacology (12.3)]. The precise mechanism by which oxcarbazepine and MHD exert their antiseizure effect is unknown; however, in vitro electrophysiological studies indicate that they produce blockade of voltage-sensitive sodium channels, resulting in stabilization of hyperexcited neural membranes, inhibition of repetitive neuronal firing, and diminution of propagation of synaptic impulses. These actions are thought to be important in the prevention of seizure spread in the intact brain. In addition, increased potassium conductance and modulation of high-voltage activated calcium channels may contribute to the anticonvulsant effects of the drug. No significant interactions of oxcarbazepine or MHD with brain neurotransmitter or modulator receptor sites have been demonstrated.
12.2 Pharmacodynamics
Oxcarbazepine and its active metabolite (MHD) exhibit anticonvulsant properties in animal seizure models. They protected rodents against electrically induced tonic extension seizures and, to a lesser degree, chemically induced clonic seizures, and abolished or reduced the frequency of chronically recurring focal seizures in Rhesus monkeys with aluminum implants. No development of tolerance (i.e., attenuation of anticonvulsive activity) was observed in the maximal electroshock test when mice and rats were treated daily for five days and four weeks, respectively, with oxcarbazepine or MHD.
12.3 Pharmacokinetics
Following oral administration of oxcarbazepine tablets, oxcarbazepine is completely absorbed and extensively metabolized to its pharmacologically active 10-monohydroxy metabolite (MHD). In a mass balance study in people, only 2% of total radioactivity in plasma was due to unchanged oxcarbazepine, with approximately 70% present as MHD, and the remainder attributable to minor metabolites.
The half-life of the parent is about two hours, while the half-life of MHD is about nine hours, so that MHD is responsible for most antiepileptic activity.
Absorption
Based on MHD concentrations, oxcarbazepine tablets and suspension were shown to have similar bioavailability.
After single-dose administration of oxcarbazepine tablets to healthy male volunteers under fasted conditions, the median t max was 4.5 (range 3 to 13) hours. After single-dose administration of oxcarbazepine oral suspension to healthy male volunteers under fasted conditions, the median tmax was six hours.
Steady-state plasma concentrations of MHD are reached within 2 to 3 days in patients when oxcarbazepine is given twice a day. At steady state the pharmacokinetics of MHD are linear and show dose proportionality over the dose range of 300 to 2400 mg/day.
Effect of Food: Food has no effect on the rate and extent of absorption of oxcarbazepine from oxcarbazepine tablets. Although not directly studied, the oral bioavailability of the oxcarbazepine suspension is unlikely to be affected under fed conditions. Therefore, oxcarbazepine tablets and suspension can be taken with or without food.
Distribution
The apparent volume of distribution of MHD is 49L.
Approximately 40% of MHD is bound to serum proteins, predominantly to albumin. Binding is independent of the serum concentration within the therapeutically relevant range. Oxcarbazepine and MHD do not bind to alpha-1-acid glycoprotein.
Metabolism and Excretion
Oxcarbazepine is rapidly reduced by cytosolic enzymes in the liver to its 10-monohydroxy metabolite, MHD, which is primarily responsible for the pharmacological effect of oxcarbazepine. MHD is metabolized further by conjugation with glucuronic acid. Minor amounts (4% of the dose) are oxidized to the pharmacologically inactive 10,11-dihydroxy metabolite (DHD).
Oxcarbazepine is cleared from the body mostly in the form of metabolites which are predominantly excreted by the kidneys. More than 95% of the dose appears in the urine, with less than 1% as unchanged oxcarbazepine. Fecal excretion accounts for less than 4% of the administered dose. Approximately 80% of the dose is excreted in the urine either as glucuronides of MHD (49%) or as unchanged MHD (27%); the inactive DHD accounts for approximately 3% and conjugates of MHD and oxcarbazepine account for 13% of the dose.
The half-life of the parent is about two hours, while the half-life of MHD is about nine hours.
12.6 Special Populations
Hepatic Impairment
The pharmacokinetics and metabolism of oxcarbazepine and MHD were evaluated in healthy volunteers and hepatically-impaired subjects after a single 900 mg oral dose. Mild-to-moderate hepatic impairment did not affect the pharmacokinetics of oxcarbazepine and MHD. No dose adjustment for oxcarbazepine is recommended in patients with mild-to-moderate hepatic impairment. The pharmacokinetics of oxcarbazepine and MHD have not been evaluated in severe hepatic impairment and, therefore, caution should be exercised when dosing severely impaired patients [see Dosage and Administration (2.7)].
Renal Impairment
There is a linear correlation between creatinine clearance and the renal clearance of MHD. When oxcarbazepine is administered as a single 300 mg dose in renally-impaired patients (creatinine clearance < 30 mL/min), the elimination half-life of MHD is prolonged to 19 hours, with a two-fold increase in AUC. Dose adjustment for oxcarbazepine is recommended in these patients [ see Use in Specific Populations (8.6) and see Dosage and Administration (2.8)].
Pediatrics
Weight-adjusted MHD clearance decreases as age and weight increases, approaching that of adults. The mean weight-adjusted clearance in children 2 years to < 4 years of age is approximately 80% higher on average than that of adults.
Therefore, MHD exposure in these children is expected to be about one-half that of adults when treated with a similar weight-adjusted dose. The mean weight-adjusted clearance in children 4 to 12 years of age is approximately 40% higher on average than that of adults. Therefore, MHD exposure in these children is expected to be about three-quarters that of adults when treated with a similar weight-adjusted dose. As weight increases, for patients 13 years of age and above, the weight-adjusted MHD clearance is expected to reach that of adults.
Pregnancy
Due to physiological changes during pregnancy, MHD plasma levels may gradually decrease throughout pregnancy [ see Use in Specific Populations (8.1)]
Geriatrics
Following administration of single (300 mg) and multiple (600 mg/day) doses of oxcarbazepine to elderly volunteers (60 to 82 years of age), the maximum plasma concentrations and AUC values of MHD were 30% to 60% higher than in younger volunteers (18 to 32 years of age). Comparisons of creatinine clearance in young and elderly volunteers indicate that the difference was due to age-related reductions in creatinine clearance.
Gender
No gender-related pharmacokinetic differences have been observed in children, adults, or the elderly.
Race
No specific studies have been conducted to assess what effect, if any, race may have on the disposition of oxcarbazepine.
Drug Interactions:
In Vitro
Oxcarbazepine can inhibit CYP2C19 and induce CYP3A4/5 with potentially important effects on plasma concentrations of other drugs. In addition, several AEDs that are cytochrome P450 inducers can decrease plasma concentrations of oxcarbazepine and MHD.
Oxcarbazepine was evaluated in human liver microsomes to determine its capacity to inhibit the major cytochrome P450 enzymes responsible for the metabolism of other drugs. Results demonstrate that oxcarbazepine and its pharmacologically active 10-monohydroxy metabolite (MHD) have little or no capacity to function as inhibitors for most of the human cytochrome P450 enzymes evaluated (CYP1A2, CYP2A6, CYP2C9, CYP2D6, CYP2E1, CYP4A9 and CYP4A11) with the exception of CYP2C19 and CYP3A4/5. Although inhibition of CYP3A4/5 by oxcarbazepine and MHD did occur at high concentrations, it is not likely to be of clinical significance. The inhibition of CYP2C19 by oxcarbazepine and MHD, is clinically relevant.
In vitro, the UDP-glucuronyl transferase level was increased, indicating induction of this enzyme. Increases of 22% with MHD and 47% with oxcarbazepine were observed. As MHD, the predominant plasma substrate, is only a weak inducer of UDP-glucuronyl transferase, it is unlikely to have an effect on drugs that are mainly eliminated by conjugation through UDP-glucuronyl transferase (e.g., valproic acid, lamotrigine).
In addition, oxcarbazepine and MHD induce a subgroup of the cytochrome P450 3A family (CYP3A4 and CYP3A5) responsible for the metabolism of dihydropyridine calcium antagonists, oral contraceptives and cyclosporine resulting in a lower plasma concentration of these drugs.
As binding of MHD to plasma proteins is low (40%), clinically significant interactions with other drugs through competition for protein binding sites are unlikely.
In Vivo
For in vivo drug interactions [see Drug Interactions (7)].
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
In two-year carcinogenicity studies, oxcarbazepine was administered in the diet at doses of up to 100 mg/kg/day to mice and by gavage at doses of up to 250 mg/kg/day to rats, and the pharmacologically active 10-hydroxy metabolite (MHD) was administered orally at doses of up to 600 mg/kg/day to rats. In mice, a dose-related increase in the incidence of hepatocellular adenomas was observed at oxcarbazepine doses ≥ 70 mg/kg/day or approximately 0.1 times the maximum recommended human dose (MRHD) on a mg/m 2 basis. In rats, the incidence of hepatocellular carcinomas was increased in females treated with oxcarbazepine at doses ≥ 25 mg/kg/day (0.1 times the MRHD on a mg/m2 basis), and incidences of hepatocellular adenomas and/or carcinomas were increased in males and females treated with MHD at doses of 600 mg/kg/day (2.4 times the MRHD on a mg/m2 basis) and ≥ 250 mg/kg/day (equivalent to the MRHD on a mg/m2 basis), respectively. There was an increase in the incidence of benign testicular interstitial cell tumors in rats at 250 mg oxcarbazepine/kg/day and at ≥ 250 mg MHD/kg/day, and an increase in the incidence of granular cell tumors in the cervix and vagina in rats at 600 mg MHD/kg/day.
Mutagenesis
Oxcarbazepine increased mutation frequencies in the Ames test in vitro in the absence of metabolic activation in one of five bacterial strains. Both oxcarbazepine and MHD produced increases in chromosomal aberrations and polyploidy in the Chinese hamster ovary assay in vitro in the absence of metabolic activation. MHD was negative in the Ames test, and no mutagenic or clastogenic activity was found with either oxcarbazepine or MHD in V79 Chinese hamster cells in vitro. Oxcarbazepine and MHD were both negative for clastogenic or aneugenic effects (micronucleus formation) in an in vivo rat bone marrow assay.
Impairment of Fertility
In a fertility study in which rats were administered MHD (50, 150, or 450 mg/kg) orally prior to and during mating and early gestation, estrous cyclicity was disrupted and numbers of corpora lutea, implantations, and live embryos were reduced in females receiving the highest dose (approximately two times the MRHD on a mg/m 2 basis).
-
14 CLINICAL STUDIES
The effectiveness of oxcarbazepine as adjunctive and monotherapy for partial seizures in adults, and as adjunctive therapy in children aged 2 to 16 years was established in seven multicenter, randomized, controlled trials.
The effectiveness of oxcarbazepine as monotherapy for partial seizures in children aged 4 to 16 years was determined from data obtained in the studies described, as well as by pharmacokinetic/pharmacodynamic considerations.
14.1 Oxcarbazepine Monotherapy Trials
Four randomized, controlled, double-blind, multicenter trials, conducted in a predominately adult population, demonstrated the efficacy of oxcarbazepine as monotherapy. Two trials compared oxcarbazepine to placebo and two trials used a randomized withdrawal design to compare a high dose (2400 mg) with a low dose (300 mg) of oxcarbazepine, after substituting oxcarbazepine 2400 mg/day for one or more antiepileptic drugs (AEDs). All doses were administered on a twice-a-day schedule. A fifth randomized, controlled, rater-blind, multicenter study, conducted in a pediatric population, failed to demonstrate a statistically significant difference between low and high dose oxcarbazepine treatment groups.
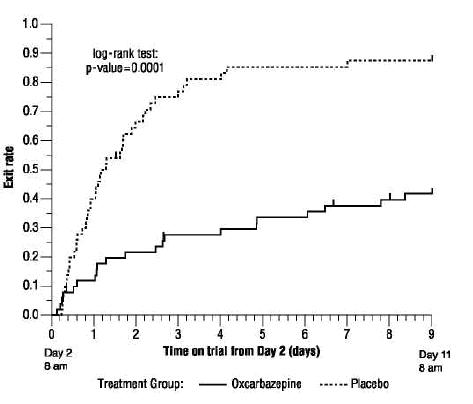
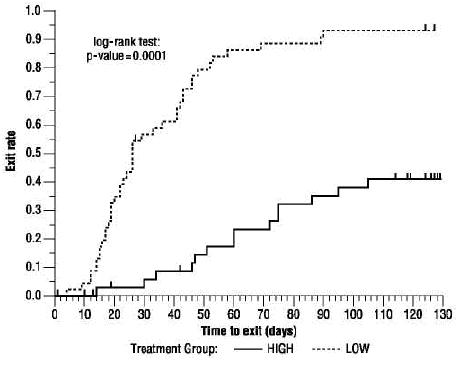
One placebo-controlled trial was conducted in 102 patients (11 to 62 years of age) with refractory partial seizures who had completed an inpatient evaluation for epilepsy surgery. Patients had been withdrawn from all AEDs and were required to have 2 to 10 partial seizures within 48 hours prior to randomization. Patients were randomized to receive either placebo or oxcarbazepine given as 1500 mg/day on Day 1 and 2400 mg/day thereafter for an additional nine days, or until one of the following three exit criteria occurred: 1) the occurrence of a fourth partial seizure, excluding Day 1, 2) two new-onset secondarily generalized seizures, where such seizures were not seen in the one-year period prior to randomization, or 3) occurrence of serial seizures or status epilepticus. The primary measure of effectiveness was a between-group comparison of the time to meet exit criteria. There was a statistically significant difference in favor of oxcarbazepine (see Figure 1), p = 0.0001.
Figure 1 Kaplan-Meier Estimates of Exit Rate by Treatment Group
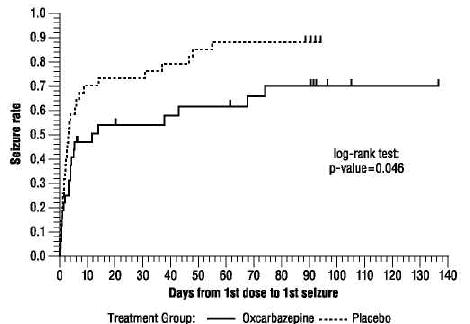
The second placebo-controlled trial was conducted in 67 untreated patients (8 to 69 years of age) with newly-diagnosed and recent-onset partial seizures. Patients were randomized to placebo or oxcarbazepine, initiated at 300 mg twice a day and titrated to 1200 mg/day (given as 600 mg twice a day) in six days, followed by maintenance treatment for 84 days. The primary measure of effectiveness was a between-group comparison of the time to first seizure. The difference between the two treatments was statistically significant in favor of oxcarbazepine (see Figure 2), p = 0.046.
Figure 2 Kaplan-Meier Estimates of First Seizure Event Rate by Treatment Group
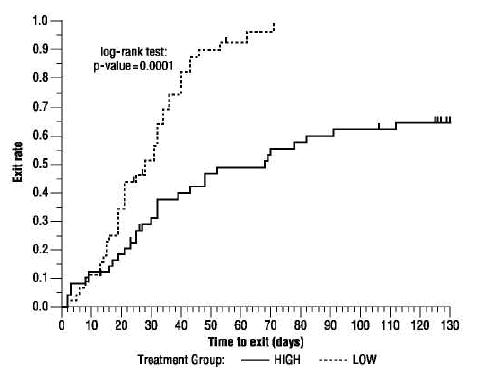
A third trial substituted oxcarbazepine monotherapy at 2400 mg/day for carbamazepine in 143 patients (12 to 65 years of age) whose partial seizures were inadequately controlled on carbamazepine (CBZ) monotherapy at a stable dose of 800 to 1600 mg/day, and maintained this oxcarbazepine dose for 56 days (baseline phase). Patients who were able to tolerate titration of oxcarbazepine to 2400 mg/day during simultaneous carbamazepine withdrawal were randomly assigned to either 300 mg/day of oxcarbazepine or 2400 mg/day oxcarbazepine. Patients were observed for 126 days or until one of the following four exit criteria occurred: 1) a doubling of the 28-day seizure frequency compared to baseline, 2) a two-fold increase in the highest consecutive two-day seizure frequency during baseline, 3) a single generalized seizure if none had occurred during baseline, or 4) a prolonged generalized seizure. The primary measure of effectiveness was a between-group comparison of the time to meet exit criteria. The difference between the curves was statistically significant in favor of the oxcarbazepine 2400 mg/day group (see Figure 3), p = 0.0001.
Figure 3 Kaplan-Meier Estimates of Exit Rate by Treatment Group
Another monotherapy substitution trial was conducted in 87 patients (11 to 66 years of age) whose seizures were inadequately controlled on one or two AEDs. Patients were randomized to either oxcarbazepine 2400 mg/day or 300 mg/day and their standard AED regimen(s) were eliminated over the first six weeks of double-blind therapy. Double-blind treatment continued for another 84 days (total double-blind treatment of 126 days) or until one of the four exit criteria described for the previous study occurred. The primary measure of effectiveness was a between-group comparison of the percentage of patients meeting exit criteria. The results were statistically significant in favor of the oxcarbazepine 2400 mg/day group (14/34; 41.2%) compared to the oxcarbazepine 300 mg/day group (42/45; 93.3%) (p < 0.0001). The time to meeting one of the exit criteria was also statistically significant in favor of the oxcarbazepine 2400 mg/day group (see Figure 4), p = 0.0001.
Figure 4 Kaplan-Meier Estimates of Exit Rate by Treatment Group
A monotherapy trial was conducted in 92 pediatric patients (1 month to 16 years of age) with inadequately-controlled or new-onset partial seizures. Patients were hospitalized and randomized to either oxcarbazepine 10 mg/kg/day or were titrated up to 40 to 60 mg/kg/day within three days while withdrawing the previous AED on the second day of oxcarbazepine therapy. Seizures were recorded through continuous video-EEG monitoring from Day 3 to Day 5. Patients either completed the 5-day treatment or met one of the two exit criteria: 1) three study-specific seizures (i.e., electrographic partial seizures with a behavioral correlate), 2) a prolonged study-specific seizure. The primary measure of effectiveness was a between-group comparison of the time to meet exit criteria in which the difference between the curves was not statistically significant (p = 0.904). The majority of patients from both dose groups completed the 5-day study without exiting.
Although this study failed to demonstrate an effect of oxcarbazepine as monotherapy in pediatric patients, several design elements, including the short treatment and assessment period, the absence of a true placebo, and the likely persistence of plasma levels of previously administered AEDs during the treatment period, make the results uninterpretable. For this reason, the results do not undermine the conclusion, based on pharmacokinetic/pharmacodynamic considerations, that oxcarbazepine is effective as monotherapy in pediatric patients 4 years old and older.
14.2 Oxcarbazepine Adjunctive Therapy Trials
The effectiveness of oxcarbazepine as an adjunctive therapy for partial seizures was established in two multicenter, randomized, double-blind, placebo-controlled trials, one in 692 patients (15 to 66 years of age) and one in 264 pediatric patients (3 to 17 years of age), and in one multicenter, rater-blind, randomized, age-stratified, parallel-group study comparing two doses of oxcarbazepine in 128 pediatric patients (1 month to < 4 years of age).
Patients in the two placebo-controlled trials were on 1 to 3 concomitant AEDs. In both of the trials, patients were stabilized on optimum dosages of their concomitant AEDs during an 8-week baseline phase. Patients who experienced at least 8 (minimum of 1 to 4 per month) partial seizures during the baseline phase were randomly assigned to placebo or to a specific dose of oxcarbazepine in addition to their other AEDs.
In these studies, the dose was increased over a two-week period until either the assigned dose was reached, or intolerance prevented increases. Patients then entered a 14- (pediatrics) or 24-week (adults) maintenance period.
In the adult trial, patients received fixed doses of 600, 1200 or 2400 mg/day. In the pediatric trial, patients received maintenance doses in the range of 30 to 46 mg/kg/day, depending on baseline weight. The primary measure of effectiveness in both trials was a between-group comparison of the percentage change in partial seizure frequency in the double-blind treatment phase relative to baseline phase. This comparison was statistically significant in favor of oxcarbazepine at all doses tested in both trials (p = 0.0001 for all doses for both trials). The number of patients randomized to each dose, the median baseline seizure rate, and the median percentage seizure rate reduction for each trial are shown in Table 8. It is important to note that in the high-dose group in the study in adults, over 65% of patients discontinued treatment because of adverse events; only 46 (27%) of the patients in this group completed the 28-week study [ see Adverse Reactions (7)], an outcome not seen in the monotherapy studies.
Table 8 Summary of Percentage Change in Partial Seizure Frequency from Baseline for Placebo-Controlled Adjunctive Therapy Trials Trial Treatment Group N Baseline Median Seizure Rate* Median % Reduction 1 p = 0.0001; * = # per 28 days 1 (pediatrics)
Oxcarbazepine
136
12.5
34.81
Placebo
128
13.1
9.4
2 (adults)
Oxcarbazepine 2400 mg/day
174
10
49.91
Oxcarbazepine 1200 mg/day
177
9.8
40.21
Oxcarbazepine 600 mg/day
168
9.6
26.41
Placebo
173
8.6
7.6
Subset analyses of the antiepileptic efficacy of oxcarbazepine with regard to gender in these trials revealed no important differences in response between men and women. Because there were very few patients over the age of 65 in controlled trials, the effect of the drug in the elderly has not been adequately assessed.
The third adjunctive therapy trial enrolled 128 pediatric patients (1 month to < 4 years of age) with inadequately-controlled partial seizures on 1 to 2 concomitant AEDs. Patients who experienced at least 2 study-specific seizures (i.e., electrographic partial seizures with a behavioral correlate) during the 72-hour baseline period were randomly assigned to either oxcarbazepine 10 mg/kg/day or were titrated up to 60 mg/kg/day within 26 days. Patients were maintained on their randomized target dose for 9 days and seizures were recorded through continuous video-EEG monitoring during the last 72 hours of the maintenance period. The primary measure of effectiveness in this trial was a between-group comparison of the change in seizure frequency per 24 hours compared to the seizure frequency at baseline. For the entire group of patients enrolled, this comparison was statistically significant in favor of oxcarbazepine 60 mg/kg/day. In this study, there was no evidence that oxcarbazepine was effective in patients below the age of 2 years (N = 75).
-
16 HOW SUPPLIED/STORAGE AND HANDLING
Oxcarbazepine oral suspension, USP is an off-white to slightly yellow liquid filled in 300 mL amber glass bottle with child resistant closure containing 250 mL of oral suspension and is supplied with a 10 mL dosing syringe and press-in bottle adapter.
NDC: 63304-653-25 Bottle containing 250 mL of oral suspension
Store oxcarbazepine oral suspension, USP in the original container. Shake well before using.
Use within 7 weeks of first opening the bottle.
Store at 20° - 25° C (68° - 77° F) [See USP Controlled Room Temperature].
-
17 PATIENT COUNSELING INFORMATION
Patients and caregivers should be informed of the availability of a Medication Guide, and they should be instructed to read the Medication Guide prior to taking oxcarbazepine oral suspension, USP.
Patients should be advised that oxcarbazepine oral suspension, USP may reduce the serum sodium concentrations especially if they are taking other medications that can lower sodium. Patients should be advised to report symptoms of low sodium like nausea, tiredness, lack of energy, confusion, and more frequent or more severe seizures [ see Warnings and Precautions (5.1)].
Anaphylactic reactions and angioedema may occur during treatment with oxcarbazepine oral suspension, USP. Patients should be advised to report immediately signs and symptoms suggesting angioedema (swelling of the face, eyes, lips, tongue or difficulty in swallowing or breathing) and to stop taking the drug until they have consulted with their physician [ see Warnings and Precautions (5.2)].
Patients who have exhibited hypersensitivity reactions to carbamazepine should be informed that approximately 25% to 30% of these patients may experience hypersensitivity reactions with oxcarbazepine oral suspension, USP. Patients should be advised that if they experience a hypersensitivity reaction while taking oxcarbazepine oral suspension, USP they should consult with their physician immediately [ see Warnings and Precautions (5.3)].
Patients should be advised that serious skin reactions have been reported in association with oxcarbazepine oral suspension, USP. In the event a skin reaction should occur while taking oxcarbazepine oral suspension, USP, patients should consult with their physician immediately [ see Warnings and Precautions (5.4)].
Patients should be instructed that a fever associated with other organ system involvement (rash, lymphadenopathy, etc.) may be drug related and should be reported to the physician immediately [ see Warnings and Precautions (5.8)].
Patients should be advised that there have been rare reports of blood disorders reported in patients treated with oxcarbazepine oral suspension, USP. Patients should be instructed to immediately consult with their physician if they experience symptoms suggestive of blood disorders [ see Warnings and Precautions (5.9)].
Female patients of childbearing age should be warned that the concurrent use of oxcarbazepine oral suspension, USP with hormonal contraceptives may render this method of contraception less effective [ see Drug Interactions (7.2)]. Additional non-hormonal forms of contraception are recommended when using oxcarbazepine oral suspension, USP.
Patients, their caregivers, and families should be counseled that AEDs, including oxcarbazepine oral suspension, USP, may increase the risk of suicidal thoughts and behavior and should be advised of the need to be alert for the emergence or worsening of symptoms of depression, any unusual changes in mood or behavior, or the emergence of suicidal thoughts, behavior, or thoughts about self-harm. Behaviors of concern should be reported immediately to healthcare providers.
Caution should be exercised if alcohol is taken in combination with oxcarbazepine oral suspension, USP therapy, due to a possible additive sedative effect.
Patients should be advised that oxcarbazepine oral suspension, USP may cause dizziness and somnolence. Accordingly, patients should be advised not to drive or operate machinery until they have gained sufficient experience on oxcarbazepine oral suspension, USP to gauge whether it adversely affects their ability to drive or operate machinery.
Patients should be encouraged to enroll in the North American Antiepileptic Drug (NAAED) Pregnancy Registry if they become pregnant. This registry is collecting information about the safety of antiepileptic drugs during pregnancy. To enroll, patients can call the toll free number 1-888-233-2334 [ see Use in Specific Populations (8.1)].
-
MEDICATION GUIDE
OXCARBAZEPINE ORAL SUSPENSION, USP
Rx only
Read this Medication Guide before you start taking oxcarbazepine oral suspension, USP and each time you get a refill. There may be new information. This information does not take the place of talking to your healthcare provider about your medical condition or treatment.
What is the most important information I should know about oxcarbazepine oral suspension, USP?
Do not stop taking oxcarbazepine oral suspension, USP without first talking to your healthcare provider.
Stopping oxcarbazepine oral suspension, USP suddenly can cause serious problems.
Oxcarbazepine oral suspension, USP can cause serious side effects, including:
1. Oxcarbazepine oral suspension, USP may cause the level of sodium in your blood to be low. Symptoms of low blood sodium include:
- nausea
- tiredness, lack of energy
- headache
- confusion
- more frequent or more severe seizures.
Similar symptoms that are not related to low sodium may occur from taking oxcarbazepine oral suspension, USP. You should tell your healthcare provider if you have any of these side effects and if they bother you or they do not go away.
Some other medicines can also cause low sodium in your blood. Be sure to tell your healthcare provider about all the other medicines that you are taking.
2. Oxcarbazepine oral suspension, USP may also cause allergic reactions or serious problems which may affect organs and other parts of your body like the liver or blood cells. You may or may not have a rash with these types of reactions.
Call your healthcare provider right away if you have any of the following:
- swelling of your face, eyes, lips, or tongue
- trouble swallowing or breathing
- a skin rash
- hives
- fever, swollen glands, or sore throat that do not go away or come and go
- painful sores in the mouth or around your eyes
- yellowing of your skin or eyes
- unusual bruising or bleeding
- severe fatigue or weakness
- severe muscle pain
- frequent infections or infections that do not go away
Many people who are allergic to carbamazepine are also allergic to oxcarbazepine oral suspension, USP. Tell your healthcare provider if you are allergic to carbamazepine.
3. Like other antiepileptic drugs, oxcarbazepine oral suspension, USP may cause suicidal thoughts or actions in a very small number of people, about 1 in 500.
Call a doctor right away if you have any of these symptoms, especially if they are new, worse, or worry you:
- thoughts about suicide or dying
- attempts to commit suicide
- new or worse depression
- new or worse anxiety
- feeling agitated or restless
- panic attacks
- trouble sleeping (insomnia)
- new or worse irritability
- acting aggressive, being angry, or violent
- acting on dangerous impulses
- an extreme increase in activity and talking (mania)
- other unusual changes in behavior or mood
How can I watch for early symptoms of suicidal thoughts and actions?
- Pay attention to any changes, especially sudden changes, in mood, behaviors, thoughts, or feelings.
- Keep all follow-up visits with your healthcare provider as scheduled.
Call your healthcare provider between visits as needed, especially if you are worried about symptoms.
Do not stop taking oxcarbazepine oral suspension, USP without first talking to a healthcare provider.
Stopping oxcarbazepine oral suspension, USP suddenly can cause serious problems. Stopping a seizure medicine suddenly in a patient who has epilepsy may cause seizures that will not stop (status epilepticus).
Suicidal thoughts or actions may be caused by things other than medicines. If you have suicidal thoughts or actions, your healthcare provider may check for other causes.
What is oxcarbazepine oral suspension, USP?
Oxcarbazepine oral suspension, USP is a prescription medicine used:
- alone or with other medicines to treat partial seizures in adults.
- alone to treat partial seizures in children 4 years and older.
- with other medicines to treat partial seizures in children 2 years and older.
Who should not take oxcarbazepine oral suspension, USP?
- Do not take oxcarbazepine oral suspension, USP if you are allergic to oxcarbazepine, USP or any of the other ingredients in oxcarbazepine oral suspension, USP. See the end of this leaflet for a complete list of ingredients in oxcarbazepine oral suspension, USP.
- Many people who are allergic to carbamazepine are also allergic to oxcarbazepine oral suspension, USP. Tell your healthcare provider if you are allergic to carbamazepine.
What should I tell my healthcare provider before taking oxcarbazepine oral suspension, USP?
Before taking oxcarbazepine oral suspension, USP, tell your healthcare provider about all your medical conditions, including if you:
- have or have had suicidal thoughts or actions, depression or mood problems
- have liver problems
- have kidney problems
- are allergic to carbamazepine. Many people who are allergic to carbamazepine are also allergic to oxcarbazepine oral suspension, USP.
- use birth control medicine. Oxcarbazepine oral suspension, USP may cause your birth control medicine to be less effective. Talk to your healthcare provider about the best birth control method to use.
-
are pregnant or plan to become pregnant. Oxcarbazepine oral suspension, USP may harm your unborn baby. Tell your healthcare provider right away if you become pregnant while taking oxcarbazepine oral suspension, USP. You and your healthcare provider will decide if you should take oxcarbazepine oral suspension, USP while you are pregnant.
- If you become pregnant while taking oxcarbazepine oral suspension, USP, talk to your healthcare provider about registering with the North American Antiepileptic Drug (NAAED) Pregnancy Registry. The purpose of this registry is to collect information about the safety of antiepileptic medicine during pregnancy. You can enroll in this registry by calling 1-888-233-2334.
- are breastfeeding or plan to breastfeed. Oxcarbazepine passes into breast milk. You and your healthcare provider should discuss whether you should take oxcarbazepine oral suspension, USP or breastfeed; you should not do both.
Tell your healthcare provider about all the medicines you take, including prescription and non-prescription medicines, vitamins, and herbal supplements.
Taking oxcarbazepine oral suspension, USP with certain other medicines may cause side effects or affect how well they work. Do not start or stop other medicines without talking to your healthcare provider.
Know the medicines you take. Keep a list of them and show it to your healthcare provider and pharmacist when you get a new medicine.
How should I take oxcarbazepine oral suspension, USP?
- Do not stop taking oxcarbazepine oral suspension, USP without talking to your healthcare provider. Stopping oxcarbazepine oral suspension, USP suddenly can cause serious problems, including seizures that will not stop (status epilepticus).
- Take oxcarbazepine oral suspension, USP exactly as prescribed. Your healthcare provider may change your dose. Your healthcare provider will tell you how much oxcarbazepine oral suspension, USP to take.
- Take oxcarbazepine oral suspension, USP 2 times a day.
- Take oxcarbazepine oral suspension, USP with or without food.
- Before taking oxcarbazepine oral suspension, USP shake the bottle well and use the oral dosing syringe to measure the amount of medicine needed. Oxcarbazepine oral suspension, USP can be mixed in a small glass of water, or swallowed directly from the syringe. Clean the syringe with warm water and let it dry after each use.
- If you take too much oxcarbazepine oral suspension, USP, call your healthcare provider or local Poison Control Center right away.
What should I avoid while taking oxcarbazepine oral suspension, USP?
- Do not drive, operate heavy machinery, or do other dangerous activities until you know how oxcarbazepine oral suspension, USP affects you. Oxcarbazepine oral suspension, USP may slow your thinking and motor skills.
- Do not drink alcohol or take other drugs that make you sleepy or dizzy while taking oxcarbazepine oral suspension, USP until you talk to your healthcare provider. Oxcarbazepine oral suspension, USP taken with alcohol or drugs that cause sleepiness or dizziness may make your sleepiness or dizziness worse.
What are the possible side effects of oxcarbazepine oral suspension, USP?
See “ What is the most important information I should know about oxcarbazepine oral suspension, USP?”
Oxcarbazepine oral suspension, USP may cause other serious side effects including:
- your seizures can happen more often or become worse
- trouble concentrating
- problems with your speech and language
- feeling confused
- feeling sleepy and tired
- trouble walking and with coordination
Get medical help right away if you have any of the symptoms listed above or listed in “What is the most important information I should know about oxcarbazepine oral suspension, USP?”
The most common side effects of oxcarbazepine oral suspension, USP include:
- dizziness
- sleepiness
- double vision
- tiredness
- nausea
- vomiting
- problems with vision
- stomach pain
- trembling
- upset stomach
- problems with walking and coordination (unsteadiness)
- rash
- infections (especially in children)
These are not all the possible side effects of oxcarbazepine oral suspension, USP. For more information, ask your healthcare provider or pharmacist. Tell your healthcare provider if you have any side effect that bothers you or does not go away
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store oxcarbazepine oral suspension, USP?
-
Store oxcarbazepine oral suspension, USP between 68° to 77° F (20° to 25° C).
- Keep oxcarbazepine oral suspension, USP in the original container. Use within 7 weeks of first opening the bottle. Shake well before using.
Keep oxcarbazepine oral suspension, USP and all medicines out of the reach of children.
General Information about the safe and effective use of oxcarbazepine oral suspension,USP
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use oxcarbazepine oral suspension, USP for a condition for which it was not prescribed. Do not give oxcarbazepine oral suspension, USP to other people, even if they have the same symptoms that you have. It may harm them.
This Medication Guide summarizes the most important information about oxcarbazepine oral suspension, USP. If you would like more information, talk with your healthcare provider. You can ask your pharmacist or healthcare provider for the full prescribing information about oxcarbazepine oral suspension, USP that is written for health professionals .
For more information call toll-free 1-888-Ranbaxy (726-2299).
What are the ingredients in oxcarbazepine oral suspension, USP?
Active ingredient: oxcarbazepine, USP
Inactive ingredients: artificial cherry flavor, ascorbic acid, carboxymethylcellulose sodium, colloidal silicon dioxide, copovidone, hydroxy ethylcellulose, methyl paraben, microcrystalline cellulose, non crystallizing sorbitol solution, propylene glycol, polyoxyl 8 stearate, povidone, propyl paraben, purified water, saccharin sodium, and sorbic acid.
This Medication Guide has been approved by the U.S. Food and Drug Administration.
Manufactured for:
Ranbaxy Pharmaceuticals Inc.
Jacksonville, FL 32257 USA
July 2014 FDA-08
-
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
RANBAXY
NDC: 63304-653-25
OXCARBAZEPINE Oral Suspension, USP
300 mg/5 mL
IMPORTANT: Shake well before using. Use within 7 weeks of first opening the bottle.
PHARMACIST: Dispense the accompanying Medication Guide to each patient
Rx only 250 mL
250 mL Bottle Label
250 mL Carton Label
-
INGREDIENTS AND APPEARANCE
OXCARBAZEPINE
oxcarbazepine suspensionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 63304-653 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength OXCARBAZEPINE (UNII: VZI5B1W380) (OXCARBAZEPINE - UNII:VZI5B1W380) OXCARBAZEPINE 60 mg in 1 mL Inactive Ingredients Ingredient Name Strength CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) CARBOXYMETHYLCELLULOSE SODIUM (UNII: K679OBS311) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) POVIDONES (UNII: FZ989GH94E) PEG-8 STEARATE (UNII: 2P9L47VI5E) SORBIC ACID (UNII: X045WJ989B) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) SACCHARIN SODIUM (UNII: SB8ZUX40TY) ASCORBIC ACID (UNII: PQ6CK8PD0R) METHYLPARABEN (UNII: A2I8C7HI9T) PROPYLPARABEN (UNII: Z8IX2SC1OH) WATER (UNII: 059QF0KO0R) COPOVIDONE K25-31 (UNII: D9C330MD8B) HYDROXYETHYL CELLULOSE (140 MPA.S AT 5%) (UNII: 8136Y38GY5) SORBITOL (UNII: 506T60A25R) Product Characteristics Color Score Shape Size Flavor CHERRY Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 63304-653-25 250 mL in 1 BOTTLE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA078734 12/14/2009 Labeler - Ranbaxy Pharmaceuticals Inc. (937890044) Registrant - Ranbaxy Pharmaceuticals Inc. (937890044) Establishment Name Address ID/FEI Business Operations DPT Laboratories Ltd 832224526 MANUFACTURE(63304-653)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.