CLOZAPINE tablet, orally disintegrating
Clozapine by
Drug Labeling and Warnings
Clozapine by is a Prescription medication manufactured, distributed, or labeled by Aurobindo Pharma Limited, APL HEALTHCARE LIMITED. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use CLOZAPINE ORALLY DISINTEGRATING TABLETS safely and effectively. See full prescribing information for CLOZAPINE ORALLY DISINTEGRATING TABLETS.
CLOZAPINE orally disintegrating tablets, for oral use
Initial U.S. Approval: 1989
WARNING: SEVERE NEUTROPENIA; ORTHOSTATIC HYPOTENSION, BRADYCARDIA, AND SYNCOPE; SEIZURE; MYOCARDITIS, PERICARDITIS, AND CARDIOMYOPATHY;
INCREASED MORTALITY IN ELDERLY PATIENTS WITH DEMENTIA-RELATED PSYCHOSIS
See full prescribing information for complete boxed warning.
- Severe Neutropenia: Clozapine has caused severe neutropenia, which is associated with an increased risk of serious and fatal infections. Prior to initiating Clozapine Orally Disintegrating Tablets (Clozapine ODT) treatment, obtain baseline ANC(s). Clozapine ODT initiation is not recommended in patients with a baseline ANC less than 1500/μL (less than 1000/μL for those with Benign Ethnic Neutropenia (also known as Duffy-null associated neutrophil count)). See recommendations for dosage modifications based on ANC levels during Clozapine ODT treatment (2.1, 2.3, 2.4, 5.1).
- Orthostatic Hypotension, Bradycardia, and Syncope: Risk is dose-related. Starting dose is 12.5 mg. Titrate gradually and use divided dosages. (2.2, 5.2)
- Seizure: Risk is dose-related. Titrate gradually and use divided doses. Use with caution in patients with history of seizure or risk factors for seizure. (5.4)
- Myocarditis, Pericarditis, Cardiomyopathy and Mitral Valve Incompetence: Can be fatal. Discontinue and obtain cardiac evaluation if findings suggest these cardiac reactions. (5.5)
- Increased Mortality in Elderly Patients with Dementia-Related Psychosis: Clozapine ODT is not approved for this condition. (5.6)
INDICATIONS AND USAGE
Clozapine orally disintegrating tablets (Clozapine ODT) is an atypical antipsychotic indicated for:
- Treatment of severely ill patients with schizophrenia who fail to respond adequately to standard antipsychotic treatment. Because of the risks of severe neutropenia and of seizure associated with its use, Clozapine ODT should be used only in patients who have failed to respond adequately to standard antipsychotic treatment (1.1)
- Reducing the risk of recurrent suicidal behavior in patients with schizophrenia or schizoaffective disorder who are judged to be at chronic risk for re-experiencing suicidal behavior (1.2)
DOSAGE AND ADMINISTRATION
- Recommended starting oral dosage is 12.5 mg once daily or twice daily. (2.2)
- If well-tolerated, increase the total daily dosage in increments of 25 mg to 50 mg per day at target dosage of 150 mg to 225 mg twice per day by the end of two weeks (2.2)
- Subsequently may increase the dosage in increments up to 100 mg, once or twice weekly. (2.2)
- Maximum daily dosage is 450 mg twice daily. (2.2)
- Administer with or without food. Clozapine ODT may be allowed to disintegrate or chewed, and may be taken with or without water. See additional administration instructions in full prescribing information (2.2).
- See dosage modification based on ANC results (2.3, 2.4)
- See recommendations for discontinuing Clozapine ODT treatment (2.5), restarting Clozapine ODT after interrupting dosing (2.6), dosage modifications for drug interactions (2.7), dosage recommendations in patients with renal or hepatic impairment and CYP2D6 poor metabolizers (2.8) in the full prescribing information.
- Tablets rapidly disintegrate after placement in the mouth and may be chewed if desired. No water is needed (2.3).
DOSAGE FORMS AND STRENGTHS
Orally disintegrating tablets: 12.5 mg, 25 mg, 100 mg, 150 mg and 200 mg (3)
CONTRAINDICATIONS
Known hypersensitivity to clozapine or any other component of Clozapine ODT (4)
WARNINGS AND PRECAUTIONS
- Severe neutropenia: See Boxed Warning (5.1)
- Gastrointestinal Hypomotility with Severe Complications: Severe gastrointestinal adverse reactions have occurred with the use of clozapine. If constipation is identified, close monitoring and prompt treatment is advised. (5.7)
- Eosinophilia: Assess for organ involvement (e.g., myocarditis, pancreatitis, hepatitis, colitis, nephritis). Discontinue if these occur. (5.8)
- QT Interval Prolongation: Can be fatal. Consider additional risk factors for prolonged QT interval (disorders and drugs). (5.9)
-
Metabolic Changes: Atypical antipsychotic drugs have been associated with metabolic changes that may increase cardiovascular/cerebrovascular risk. These metabolic changes include (5.10):
- Hyperglycemia and Diabetes Mellitus: Monitor for symptoms of hyperglycemia including polydipsia, polyuria, polyphagia, and weakness. Monitor glucose regularly in patients with diabetes or at risk for diabetes.
- Dyslipidemia: Undesirable alterations in lipids have occurred in patients treated with atypical antipsychotics.
- Weight Gain: Significant weight gain has occurred. Monitor weight gain.
- Neuroleptic Malignant Syndrome (NMS): Immediately discontinue and monitor closely. Assess for co-morbid conditions. (5.11)
- Hepatotoxicity: Can be fatal. Monitor for hepatotoxicity. Discontinue treatment if hepatitis or transaminase elevations combined with other symptoms occur (5.12).
- Fever: Evaluate for infection and for neutropenia, NMS. (5.14)
- Pulmonary Embolism (PE): Consider PE if respiratory distress, chest pain, or deep-vein thrombosis occurs. (5.15)
- Anticholinergic Toxicity: When possible, avoid use with other anticholinergic drugs and use with caution in patients with a current diagnosis or prior history of constipation, urinary retention, clinically significant prostatic hypertrophy, or other conditions in which anticholinergic effects can lead to significant adverse reactions. (5.15, 7.1)
- Interference with Cognitive and Motor Performance: Advise caution when operating machinery, including automobiles. (5.16)
ADVERSE REACTIONS
Most common adverse reactions (≥5%) were: CNS reactions (sedation, dizziness/vertigo, headache, and tremor); cardiovascular reactions (tachycardia, hypotension, and syncope); autonomic nervous system reactions (hypersalivation, sweating, dry mouth, and visual disturbances); gastrointestinal reactions (constipation and nausea); and fever. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Aurobindo Pharma USA, Inc. at 1-866-850-2876 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
-
Concomitant use of Strong CYP1A2 Inhibitors: Reduce Clozapine ODT dose to one third when coadministered with strong CYP1A2 inhibitors (e.g., fluvoxamine, ciprofloxacin, enoxacin). (2.7, 7.1)
-
Concomitant use of Strong CYP3A4 Inducers is not recommended. (2.7, 7.1)
-
Discontinuation of CYP1A2 or CYP3A4 Inducers: Consider reducing Clozapine ODT dose when CYP1A2 (e.g., tobacco smoke) or CYP3A4 inducers (e.g., carbamazepine) are discontinued. (2.7, 7.1)
-
Anticholinergic drugs: Concomitant use may increase the risk for anticholinergic toxicity. (5.7, 5.15, 7.1)
USE IN SPECIFIC POPULATIONS
Lactaton: Infants exposed to Clozapine ODT through breast milk should be monitored for excess sedation and neutropenia (8.2)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 6/2025
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: SEVERE NEUTROPENIA; ORTHOSTATIC HYPOTENSION, BRADYCARDIA, AND SYNCOPE; SEIZURE; MYOCARDITIS, PERICARDITIS, AND CARDIOMYOPATHY; INCREASED MORTALITY IN ELDERLY PATIENTS WITH DEMENTIA-RELATED PSYCHOSIS
1 INDICATIONS AND USAGE
1.1 Treatment-resistant Schizophrenia
1.2 Reduction in the Risk of Recurrent Suicidal Behavior in Schizophrenia or Schizoaffective Disorder
2 DOSAGE AND ADMINISTRATION
2.1 Absolute Neutrophil Count Testing Prior to Clozapine ODT Initiation
2.2 Recommended Dosage and Administration
2.3 Dosage Modifications Based on ANC Results
2.4 Dosage Modifications Based on ANC Results for Patients with Benign Ethnic Neutropenia
2.5 Discontinuation of Clozapine ODT Treatment
2.6 Restarting Clozapine ODT Treatment After Interrupting Clozapine ODT
2.7 Dosage Modifications for Drug Interactions
2.8 Dosage Recommendations in Patients with Renal or Hepatic Impairment, or CYP2D6 Poor Metabolizers
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Severe Neutropenia
5.2 Orthostatic Hypotension, Bradycardia, and Syncope
5.3 Falls
5.4 Seizures
5.5 Myocarditis, Pericarditis, Cardiomyopathy and Mitral Valve Incompetence
5.6 Increased Mortality in Elderly Patients with Dementia-Related Psychosis
5.7 Gastrointestinal Hypomotility with Severe Complications
5.8 Eosinophilia
5.9 QT Interval Prolongation
5.10 Metabolic Changes
5.11 Neuroleptic Malignant Syndrome
5.12 Hepatotoxicity
5.13 Fever
5.14 Pulmonary Embolism
5.15 Anticholinergic Toxicity
5.16 Interference with Cognitive and Motor Performance
5.17 Tardive Dyskinesia
5.18 Patients with Phenylketonuria
5.19 Cerebrovascular Adverse Reactions
5.20 Recurrence of Psychosis and Cholinergic Rebound after Abrupt Discontinuation of Clozapine ODT
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Potential for Other Drugs to Affect Clozapine ODT
7.2 Potential for Clozapine ODT to Affect Other Drugs
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Patients with Renal or Hepatic Impairment
8.7 CYP2D6 Poor Metabolizers
10 OVERDOSAGE
10.1 Overdosage Experience
10.2 Management of Overdosage
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Treatment-Resistant Schizophrenia
14.2 Recurrent Suicidal Behavior in Schizophrenia or Schizoaffective Disorder
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
16.2 Storage and Handling
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: SEVERE NEUTROPENIA; ORTHOSTATIC HYPOTENSION, BRADYCARDIA, AND SYNCOPE; SEIZURE; MYOCARDITIS, PERICARDITIS, AND CARDIOMYOPATHY; INCREASED MORTALITY IN ELDERLY PATIENTS WITH DEMENTIA-RELATED PSYCHOSIS
Severe Neutropenia
Clozapine Orally Disintegrating Tablets (Clozapine ODT) has caused severe neutropenia which is associated with an increased risk of serious and potentially fatal infections. Prior to initiating Clozapine ODT treatment, obtain baseline ANC(s). Clozapine ODT initiation is not recommended in patients with a baseline ANC less than 1500/μL (less than 1000/μL for those with Benign Ethnic Neutropenia (also known as Duffy-null associated neutrophil count)). See recommendations for dosage modifications based on ANC levels during Clozapine ODT treatment [see Dosage and Administration (2.4, 2.5)]. Consider a hematology consultation before initiating Clozapine ODT or during Clozapine ODT treatment [see Warnings and Precautions (5.1)].
Orthostatic Hypotension, Bradycardia, Syncope
Orthostatic hypotension, bradycardia, syncope, and cardiac arrest have occurred with clozapine treatment. The risk is highest during the initial titration period, particularly with rapid dose escalation. These reactions can occur with the first dose, with doses as low as 12.5 mg per day, or when restarting patients who have had even a brief interruption in treatment with Clozapine ODT. Initiate treatment at 12.5 mg once or twice daily; titrate slowly; and use divided dosages to minimize risk. Use Clozapine ODT cautiously in patients with cardiovascular or cerebrovascular disease or conditions predisposing to hypotension (e.g., dehydration, use of antihypertensive medications) [see Dosage and Administration (2.3, and 2.6), Warnings and Precautions (5.2)].
Seizures
Seizures have occurred with clozapine treatment. The risk is dose-related. Initiate treatment at 12.5 mg, titrate gradually, and use divided dosing. Use caution when administering Clozapine ODT to patients with a history of seizures or other predisposing risk factors for seizure (CNS pathology, medications that lower the seizure threshold, alcohol abuse). Caution patients about engaging in any activity where sudden loss of consciousness could cause serious risk to themselves or others [see Dosage and Administration (2.3), Warnings and Precautions (5.4)].
Myocarditis, Pericarditis, Cardiomyopathy and Mitral Valve Incompetence
Fatal myocarditis and cardiomyopathy have occurred with clozapine treatment. Discontinue Clozapine ODT and obtain a cardiac evaluation upon suspicion of these reactions. Generally, patients with clozapine-related myocarditis or cardiomyopathy should not be rechallenged with Clozapine ODT. Consider the possibility of myocarditis, pericarditis, or cardiomyopathy if chest pain, tachycardia, palpitations, dyspnea, fever, flu-like symptoms, hypotension, or ECG changes occur [see Warnings and Precautions (5.5)].
Increased Mortality in Elderly Patients with Dementia-Related Psychosis
Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Clozapine ODT is not approved for use in patients with dementia-related psychosis [see Warnings and Precautions (5.6)].
-
1 INDICATIONS AND USAGE
1.1 Treatment-resistant Schizophrenia
Clozapine Orally Disintegrating Tablets (Clozapine ODT) are indicated for the treatment of severely ill patients with schizophrenia who fail to respond adequately to standard antipsychotic treatment. Because of the risks of severe neutropenia and of seizure associated with their use, Clozapine ODT should be used only in patients who have failed to respond adequately to standard antipsychotic treatment [see Warnings and Precautions (5.1, 5.4)].
The effectiveness of Clozapine ODT in treatment-resistant schizophrenia was demonstrated in a 6-week, randomized, double-blind, active-controlled study comparing Clozapine ODT and chlorpromazine in patients who had failed other antipsychotics [see Clinical Studies (14.1)].
1.2 Reduction in the Risk of Recurrent Suicidal Behavior in Schizophrenia or Schizoaffective Disorder
Clozapine ODT is indicated for reducing the risk of recurrent suicidal behavior in patients with schizophrenia or schizoaffective disorder who are judged to be at chronic risk for re-experiencing suicidal behavior, based on history and recent clinical state. Suicidal behavior refers to actions by a patient that put him/herself at risk for death.
The effectiveness of Clozapine ODT in reducing the risk of recurrent suicidal behavior was demonstrated over a two-year treatment period in the InterSePT™ trial [see Clinical Studies (14.2)].
-
2 DOSAGE AND ADMINISTRATION
2.1 Absolute Neutrophil Count Testing Prior to Clozapine ODT Initiation
Prior to initiating Clozapine ODT treatment, obtain a baseline absolute neutrophil count (ANC). Clozapine ODT initiation is not recommended in patients with an ANC less than 1500/μL [see Warnings and Precautions (5.1)].
For patients with documented Benign Ethnic Neutropenia (BEN) (also known as Duffy-null associated neutrophil count)), obtain at least two baseline ANC levels. Clozapine ODT initiation is not recommended in patients with BEN with an ANC less than 1000/μL [see Warnings and Precautions (5.1)].
For dosage modifications based on ANC results, see Dosage and Administration (2.4, 2.5).
2.2 Recommended Dosage and Administration
Recommended Dosage
To reduce the risk of orthostatic hypotension, bradycardia, and syncope, the recommended starting dosage is much lower than the target dosage [see Warnings and Precautions (5.3)].
The recommended starting oral dosage of Clozapine ODT is 12.5 mg once or twice daily. If well-tolerated, increase the total daily dose in increments of 25 mg to 50 mg per day to achieve a target dosage of 150 mg to 225 mg twice per day by the end of two weeks. Subsequently, may increase the dosage in increments of up to 100 mg once weekly or twice weekly. The maximum recommended Clozapine ODT oral dosage is 450 mg twice daily.
Administration Instructions
Clozapine ODT can be taken with or without food, may be allowed to disintegrate or chewed, and may be taken with or without water [see Clinical Pharmacology (12.3)].
Just prior to use, peel the foil from the blister and gently remove the orally disintegrating tablet (ODT). Do not push the ODT through the foil, because this could damage the ODT. After removing Clozapine ODT from the blister pack or bottle, immediately place in the mouth.
2.3 Dosage Modifications Based on ANC Results
Table 1 provides recommended Clozapine ODT dosage modifications based on ANC results [see Warnings and Precautions (5.1)]. For dosage modifications based on ANC results for patients with Benign Ethnic Neutropenia (BEN) (also known as Duffy-null associated neutrophil count), see Table 2 [see Dosage and Administration (2.5)].
Table 1: Clozapine ODT Dosage Modifications Based on ANC Results and Frequency of ANC Testing 1 Confirm all initial reports of ANC less than 1500/μL with a repeat ANC measurement within 24 hours Recommended Dosage Modification
Recommended Frequency of ANC Testing During Clozapine ODT Treatment
ANC Within Normal Range (≥ 1500/μL)
No dosage modification; continue treatment
- Day 1 to Month 6: Weekly
- Month 7 to Month 12: Every 2 weeks
- Month 13 and thereafter: Every month
If Clozapine ODT treatment is reinitiated after a dosage interruption (e.g., patient had neutropenia which required dosage interruption and now has a normal ANC level) for:
- < 30 days, continue the previous ANC testing frequency
- ≥ 30 days, obtain ANC tests according to the frequency for patients who initiate treatment
Mild Neutropenia (ANC between 1000 to 1499/μL)1
No dosage modification; continue treatment
- Three times weekly
- Once ANC ≥ 1500/μL, recommend returning to the patient’s last Normal Range ANC testing frequency
Moderate Neutropenia (ANC between 500 to 999/μL)1
- Interrupt treatment and recommend hematology consultation
- Resume treatment once ANC ≥1000/μL
- Daily
- Once ANC > 1000/μL, three times weekly
- Once ANC ≥ 1500/μL, test weekly for 4 weeks. If ANC ≥ 1500/μL after monitoring weekly for 4 weeks, return to the patient’s last Normal Range ANC testing frequency
Severe Neutropenia (ANC less than 500/μL)1
Discontinue treatment and recommend hematology consultation
- Daily
- Once ANC ≥ 1000/μL, three times weekly
- Once ANC ≥ 1500/μL, if the benefits outweigh the risks of restarting treatment, resume treatment and obtain ANC tests according to the frequency for patients who initiate treatment
2.4 Dosage Modifications Based on ANC Results for Patients with Benign Ethnic Neutropenia
Table 2 provides recommended Clozapine ODT dosage modifications based on ANC results for patients with Benign Ethnic Neutropenia (BEN) (also known as Duffy-null associated neutrophil count). [see Warnings and Precautions (5.1)]. For dosage modifications based on ANC results for patients without BEN, see Table 1 [see Dosage and Administration (2.4)].
Table 2: Clozapine ODT Dosage Modifications Based on ANC Results and Frequency of ANC Testing in Patients with Benign Ethnic Neutropenia1 1 Benign Ethnic Neutropenia (BEN) is also known as Duffy-null associated neutrophil count.
2 Confirm all initial reports of ANC less than 1500/μL with a repeat ANC measurement within 24 hours
Recommended Dosage
Modification
Recommended Frequency of ANC Testing During Clozapine ODT Treatment in Patients with BEN
ANC Within the Normal Range for Patients with BEN (≥ 1000/μL )
No dosage modification;
continue treatment
- Day 1 to Month 6: Weekly
- Month 7 to Month 12: Every 2 weeks
- Month 13 and thereafter: Monthly
If Clozapine ODT treatment is reinitiated after a dosage interruption (e.g., patient had neutropenia which required dosage interruption and now their ANC (≥ 1000/μL and ≥ the patient’s ANC baseline prior to treatment) for:
- < 30 days, continue previous ANC testing frequency
- ≥ 30 days, obtain ANC tests according to the frequency for patients with BEN who initiate treatment
Neutropenia in Patients with BEN (ANC level between 500 to 999/μL)2
- Recommend hematology consultation
- No dosage modification; continue treatment
- Three times weekly
- Once ANC ≥ 1000/μL and ≥ the patient’s ANC baseline, obtain ANC tests weekly for 4 weeks
- If ANC ≥1000/μL and ≥ the patient’s baseline after monitoring for 4 weeks, return to the patient’s last Normal ANC Range testing frequency for patients with BEN.
Severe Neutropenia in Patients with BEN (ANC level less than 500/μL)2
Discontinue treatment and recommend hematology consultation
- Daily
- Once ANC ≥ 500/μL, obtain ANC three times weekly
- Once ANC ≥ 1000/μL and ≥ the patient’s baseline, if the benefits outweigh the risks of restarting treatment, resume treatment and obtain ANC tests according to the frequency for patients with BEN who initiate treatment
2.5 Discontinuation of Clozapine ODT Treatment
If discontinuing Clozapine ODT in patients with:
- Moderate or severe neutropenia, see Table 1 [see Dosage and Administration (2.4)].
- Normal or mild neutropenia, reduce the dosage gradually over a period of 1 to 2 weeks, and continue monitoring ANC levels until their ANC is ≥1500/μL.
If discontinuing Clozapine ODT in patients with Benign Ethnic Neutropenia (BEN) (also known as Duffy-null associated neutrophil count) with:
- Neutropenia, see Table 2 [see Dosage and Administration (2.5)].
- ANC within their normal range of ANC reduce the dosage gradually over a period of 1 to 2 weeks.
When discontinuing Clozapine ODT, monitor patients for the symptoms related to psychotic recurrence and cholinergic rebound (e.g., profuse sweating, headache, nausea, vomiting, diarrhea).
2.6 Restarting Clozapine ODT Treatment After Interrupting Clozapine ODT
When restarting Clozapine ODT in patients who have interrupted Clozapine ODT treatment, use a lower dosage to minimize the risk of hypotension, bradycardia, and syncope [see Warnings and Precautions (5.3)].
- If one day’s dosage is missed, resume Clozapine ODT treatment at 40% to 50% of the previous dosage.
- If two days of dosing is missed, resume Clozapine ODT treatment at approximately 25% of the previous dosage.
- For longer interruptions, restart Clozapine ODT treatment with a dosage of 12.5 mg once or twice daily. If this dosage is well-tolerated, may increase the dosage to the previous dosage more quickly than recommended than for initial Clozapine ODT treatment.
2.7 Dosage Modifications for Drug Interactions
See Table 3 for recommended dosage modifications to reduce the risk of Clozapine ODT-associated adverse reactions or reduce the risk of lower effectiveness [see Drug Interactions (7)].
Table 3: Clozapine ODT Dosage Modifications for Drug Interactions Strong CYP1A2 Inhibitors
Administer one third of the Clozapine ODT dosage.
Moderate or Weak CYP1A2 Inhibitors
Consider reducing the Clozapine ODT dosage if necessary.
CYP2D6 or CYP3A4 Inhibitors
Strong CYP3A4 Inducers
Concomitant use is not recommended. However, if concomitant use is necessary, it may be necessary to increase the Clozapine ODT dosage. Monitor for decreased effectiveness.
Moderate or weak CYP1A2 or CYP3A4 Inducers
Consider increasing the Clozapine ODT dosage if necessary.
2.8 Dosage Recommendations in Patients with Renal or Hepatic Impairment, or CYP2D6 Poor Metabolizers
It may be necessary to reduce the Clozapine ODT dosage in patients with significant renal impairment or hepatic impairment, or in CYP2D6 poor metabolizers [see Use in Specific Populations (8.6, 8.7)].
- Day 1 to Month 6: Weekly
-
3 DOSAGE FORMS AND STRENGTHS
Clozapine Orally Disintegrating Tablets are available as:
12.5 mg: yellow to pale yellow color, round shaped tablet, flat faced bevelled edge debossed with “CLO” on one side and “12.5” on the other side.
25 mg: yellow to pale yellow color, round shaped tablet, flat faced bevelled edge debossed with “CLO” on one side and “25” on the other side.
100 mg: yellow to pale yellow color, round shaped tablet, flat faced bevelled edge debossed with “CLO” on one side and “100” on the other side.
150 mg: yellow to pale yellow color, round shaped tablet, flat faced bevelled edge debossed with “CLO” on one side and “150” on the other side.
200 mg: yellow to pale yellow color, round shaped tablet, flat faced bevelled edge debossed with “CLO” on one side and “200” on the other side.
-
4 CONTRAINDICATIONS
Clozapine ODT is contraindicated in patients with a history of serious hypersensitivity to clozapine (e.g., photosensitivity, vasculitis, erythema multiforme, or Stevens-Johnson syndrome) or any other component of Clozapine ODT [see Adverse Reactions (6.2)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Severe Neutropenia
Clozapine has caused severe neutropenia (absolute neutrophil count (ANC) less than 500/μL) [see Adverse Reactions (6.1, 6.2)] and is associated with an increased risk of serious and potentially fatal infections. Severe neutropenia occurred in a small percentage of clozapine-treated patients. The risk of severe neutropenia appears greatest during the first 18 weeks of Clozapine ODT treatment. The mechanism by which Clozapine ODT causes neutropenia is unknown. Neutropenia is not dose-dependent.
Consider a hematology consultation before initiating Clozapine ODT treatment or during treatment.
ANC Monitoring and Dosage Modifications
Prior to initiating Clozapine ODT treatment, obtain a baseline ANC. Clozapine ODT initiation is not recommended in patients with a baseline ANC less than 1500/μL. Throughout VERZACLOZ treatment, regularly monitor ANC. Table 1 provides recommendations for dosage modifications (dosage interruption and treatment discontinuation), based on ANC levels, during Clozapine ODT treatment and frequency of ANC monitoring [see Dosage and Administration (2.4)].
ANC Monitoring and Dosage Modification in Patients with Benign Ethnic Neutropenia
Patients with Benign Ethnic Neutropenia (BEN) (also known as Duffy-null associated neutrophil count) generally have lower baseline neutrophil counts but they are not at higher risk for developing infections, and they are not at increased risk for developing Clozapine ODT-induced neutropenia.
For patients with documented BEN, obtain at least two baseline ANC levels prior to Clozapine ODT initiation. Clozapine ODT initiation is not recommended in patients with BEN with an ANC less than 1000/μL. There are different ANC dosage modification recommendations in Clozapine ODT-treated patients with BEN due to their lower baseline ANC levels. Table 2 provides recommendations on dosage modifications (dosage interruption and treatment discontinuation), based on ANC monitoring, during Clozapine ODT treatment in patients with BEN and recommended frequency of ANC testing [see Dosage and Administration (2.5)].
Management of Clozapine ODT-Treated Patients Who Develop a Fever
For patients who develop a fever during Clozapine ODT treatment:
-
Interrupt Clozapine ODT in those who develop a temperature of 101.3 °F (38.5 °C) or greater and obtain an ANC level.
-
If the ANC is less than 1000/μL in patients without BEN, initiate appropriate workup and treatment for infection. Refer to Table 1 or Table 2 for dosage modifications based on ANC monitoring [see Dosage and Administration (2.5)].
In patients with fever and a normal neutrophil count, see Warnings and Precautions (5.11) for neuroleptic malignant syndrome and Warnings and Precautions (5.13) for fever.
Restarting Clozapine ODT in Patients Who Recovered from Severe Neutropenia
Generally, do not rechallenge patients with Clozapine ODT in those who experienced severe neutropenia. However, for some patients who had resolution of their Clozapine ODT-related severe neutropenia after stopping Clozapine ODT, the risk of schizophrenia exacerbation from not restarting Clozapine ODT treatment may be greater than the risk of neutropenia reoccurrence from restarting Clozapine ODT (e.g., patients who have no treatment options other than Clozapine ODT).
Concomitant Use of Clozapine ODT with Other Drugs Known to Cause Neutropenia
If Clozapine ODT is used concomitantly with another drug known to cause neutropenia, consider more frequently ANC monitoring than the recommendations provided in Tables 1 and 2.
5.2 Orthostatic Hypotension, Bradycardia, and Syncope
Hypotension, bradycardia, syncope, and cardiac arrest have occurred with clozapine treatment. The risk is highest during the initial titration period, particularly with rapid dose-escalation. These reactions can occur with the first dose, at doses as low as 12.5 mg. These reactions can be fatal. The syndrome is consistent with neurally mediated reflex bradycardia (NMRB).
Clozapine ODT treatment must begin at a maximum dose of 12.5 mg once daily or twice daily. The total daily dose can be increased in increments of 25 mg to 50 mg per day, if well-tolerated, to a target dose of 300 mg to 450 mg per day (administered in divided doses) by the end of 2 weeks. Subsequently, the dose can be increased weekly or twice weekly, in increments of up to 100 mg. The maximum Clozapine ODT dosage is 900 mg per day. Use cautious titration and a divided dosage schedule to minimize the risk of serious cardiovascular reactions [see Dosage and Administration (2.3)]. Consider reducing the dose if hypotension occurs. When restarting Clozapine ODT in patients who have had even a brief interruption in treatment with Clozapine ODT, the dosage must be reduced. This is necessary to minimize the risk of hypotension, bradycardia, and syncope [see Dosage and Administration (2.6)].
Use Clozapine ODT cautiously in patients with cardiovascular disease (history of myocardial infarction or ischemia, heart failure, or conduction abnormalities), cerebrovascular disease, and conditions which would predispose patients to hypotension (e.g., concomitant use of antihypertensives, dehydration and hypovolemia).
5.3 Falls
Clozapine ODT may cause somnolence, postural hypotension, and motor and sensory instability, which may lead to falls and, consequently, fractures or other injuries. For patients with diseases, conditions, or medications that could exacerbate these effects, complete fall risk assessments when initiating antipsychotic treatment and recurrently for patients on long-term antipsychotic treatment.
5.4 Seizures
Seizure has been estimated to occur in association with clozapine use at a cumulative incidence at one year of approximately 5%, based on the occurrence of one or more seizures in 61 of 1743 patients exposed to clozapine during its clinical testing prior to domestic marketing (i.e., a crude rate of 3.5%). The risk of seizure is dose-related. Initiate Clozapine ODT treatment with a low dose (12.5 mg), titrate slowly, and use divided dosing.
Use caution when administering Clozapine ODT to patients with a history of seizures or other predisposing risk factors for seizure (e.g., head trauma or other CNS pathology, use of medications that lower the seizure threshold, or alcohol abuse). Because of the substantial risk of seizure associated with Clozapine ODT use, caution patients about engaging in any activity where sudden loss of consciousness could cause serious risk to themselves or others (e.g., driving an automobile, operating complex machinery, swimming, climbing).
5.5 Myocarditis, Pericarditis, Cardiomyopathy and Mitral Valve Incompetence
Myocarditis, pericarditis, and cardiomyopathy have occurred with the use of clozapine. These reactions can be fatal. Discontinue Clozapine ODT and obtain a cardiac evaluation upon suspicion of myocarditis, pericarditis, or cardiomyopathy. Generally, patients with a history of clozapine-associated myocarditis, pericarditis or cardiomyopathy should not be rechallenged with Clozapine ODT. However, if the benefit of Clozapine ODT treatment is judged to outweigh the potential risks of recurrence, the clinician may consider rechallenge with Clozapine ODT in consultation with a cardiologist.
Consider the possibility of myocarditis or cardiomyopathy in patients receiving Clozapine ODT who present with chest pain, dyspnea, persistent tachycardia at rest, palpitations, fever, flu-like symptoms, hypotension, other signs or symptoms of heart failure, or electrocardiographic findings (low voltages, ST-T abnormalities, arrhythmias, right axis deviation, and poor R wave progression). Myocarditis and pericarditis most frequently presents within the first two months of clozapine treatment. Symptoms of cardiomyopathy generally occur later than clozapine-associated myocarditis and usually after 8 weeks of treatment. However, myocarditis, pericarditis, and cardiomyopathy can occur at any period during treatment with Clozapine ODT. In patients who are diagnosed with cardiomyopathy while taking clozapine mitral valve incompetence has been reported.
5.6 Increased Mortality in Elderly Patients with Dementia-Related Psychosis
Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Analyses of 17 placebo-controlled trials (modal duration of 10 weeks), largely in patients taking atypical antipsychotic drugs, revealed a risk of death in drug-treated patients of between 1.6 to 1.7 times the risk of death in placebo-treated patients. Over the course of a typical 10-week controlled trial, the rate of death in drug-treated patients was about 4.5%, compared to a rate of about 2.6% in the placebo group. Although the causes of death were varied, most of the deaths appeared to be either cardiovascular (e.g., heart failure, sudden death) or infectious (e.g., pneumonia) in nature. Observational studies suggest that, similar to atypical antipsychotic drugs, treatment with conventional antipsychotic drugs may increase mortality in this population. The extent to which the findings of increased mortality in observational studies may be attributed to the antipsychotic drug as opposed to some characteristic(s) of the patients is not clear. Clozapine ODT is not approved for the treatment of patients with dementia-related psychosis [see Boxed Warning].
5.7 Gastrointestinal Hypomotility with Severe Complications
Severe gastrointestinal adverse reactions have occurred with the use of clozapine, primarily due to its potent anticholinergic effects and resulting gastrointestinal hypomotility. In post marketing experience, reported effects range from constipation to paralytic ileus. Increased frequency of constipation and delayed diagnosis and treatment increased the risk of severe complications of gastrointestinal hypomotility, which can result in fecal impaction, megacolon, and intestinal obstruction, ischemia, infarction, perforation, ulceration, or necrosis [see Adverse Reactions (6.2)]. These reactions have resulted in hospitalization, surgery, and death. The risk for severe adverse reactions is further increased with anticholinergic medications (and other medications that decrease gastrointestinal peristalsis); therefore, concomitant use should be avoided when possible [see Warnings and Precautions (5.15), Drug Interactions (7.1)].
Prior to initiating Clozapine ODT, screen for constipation and treat as necessary. Subjective symptoms of constipation may not accurately reflect the degree of gastrointestinal hypomotility in Clozapine ODT-treated patients. Therefore, reassess bowel function frequently with careful attention to any changes in the frequency or character of bowel movements, as well as signs and symptoms of complications of hypomotility (e.g., nausea, vomiting, abdominal distension, abdominal pain). If constipation or gastrointestinal hypomotility are identified, monitor closely and treat promptly with appropriate laxatives, as necessary, to prevent severe complications. Consider prophylactic laxatives in high risk patients.
5.8 Eosinophilia
Eosinophilia, defined as a blood eosinophil count of greater than 700/µL, has occurred with clozapine treatment. In clinical trials, approximately 1% of patients developed eosinophilia. Clozapine-related eosinophilia usually occurs during the first month of treatment. In some patients, it has been associated with myocarditis, pancreatitis, hepatitis, colitis, and nephritis. Such organ involvement could be consistent with a drug reaction with eosinophilia and systemic symptoms syndrome (DRESS), also known as drug induced hypersensitivity syndrome (DIHS). If eosinophilia develops during Clozapine ODT treatment, evaluate promptly for signs and symptoms of systemic reactions, such as rash or other allergic symptoms, myocarditis, or other organ-specific disease associated with eosinophilia. If clozapine-related systemic disease is suspected, discontinue Clozapine ODT immediately.
If a cause of eosinophilia unrelated to Clozapine ODT is identified (e.g., asthma, allergies, collagen vascular disease, parasitic infections, and specific neoplasms), treat the underlying cause and continue Clozapine ODT.
Clozapine-related eosinophilia has also occurred in the absence of organ involvement and can resolve without intervention. There are reports of successful rechallenge after discontinuation of Clozapine ODT, without recurrence of eosinophilia. In the absence of organ involvement, continue Clozapine ODT under careful monitoring. If the total eosinophil count continues to increase over several weeks in the absence of systemic disease, the decision to interrupt Clozapine ODT therapy and rechallenge after the eosinophil count decreases should be based on the overall clinical assessment, in consultation with an internist or hematologist.
5.9 QT Interval Prolongation
QT prolongation, Torsades de Pointes and other life-threatening ventricular arrhythmias, cardiac arrest, and sudden death have occurred with clozapine treatment. When prescribing Clozapine ODT, consider the presence of additional risk factors for QT prolongation and serious cardiovascular reactions. Conditions that increase these risks include the following: history of QT prolongation, long QT syndrome, family history of long QT syndrome or sudden cardiac death, significant cardiac arrhythmia, recent myocardial infarction, uncompensated heart failure, treatment with other medications that cause QT prolongation, treatment with medications that inhibit the metabolism of clozapine, and electrolyte abnormalities.
Prior to initiating treatment with Clozapine ODT, perform a careful physical examination, medical history, and concomitant medication history. Consider obtaining a baseline ECG and serum chemistry panel. Correct electrolyte abnormalities. Discontinue Clozapine ODT if the QTc interval exceeds 500 msec. If patients experience symptoms consistent with Torsades de Pointes or other arrhythmias (e.g., syncope, presyncope, dizziness, or palpitations), obtain a cardiac evaluation and discontinue Clozapine ODT.
Use caution when administering concomitant medications that prolong the QT interval or inhibit the metabolism of clozapine. Drugs that cause QT prolongation include: specific antipsychotics (e.g., ziprasidone, iloperidone, chlorpromazine, thioridazine, mesoridazine, droperidol, pimozide), specific antibiotics (e.g., erythromycin, gatifloxacin, moxifloxacin, sparfloxacin), Class 1A antiarrhythmic medications (e.g., quinidine, procainamide) or Class III antiarrhythmics (e.g., amiodarone, sotalol), and others (e.g., pentamidine, levomethadyl acetate, methadone, halofantrine, mefloquine, dolasetron mesylate, probucol or tacrolimus). Clozapine is primarily metabolized by CYP isoenzymes 1A2, 2D6, and 3A4. Concomitant treatment with inhibitors of these enzymes can increase the concentration of clozapine [see Drug Interactions (7.1) and Clinical Pharmacology (12.3)].
Hypokalemia and hypomagnesemia increase the risk of QT prolongation. Hypokalemia can result from diuretic therapy, diarrhea, and other causes. Use caution when treating patients at risk for significant electrolyte disturbance, particularly hypokalemia. Obtain baseline measurements of serum potassium and magnesium levels, and periodically monitor electrolytes. Correct electrolyte abnormalities before initiating treatment with Clozapine ODT.
5.10 Metabolic Changes
Atypical antipsychotic drugs, including clozapine have been associated with metabolic changes that can increase cardiovascular and cerebrovascular risk. These metabolic changes include hyperglycemia, dyslipidemia, and body weight gain. While atypical antipsychotic drugs may produce some metabolic changes, each drug in the class has its own specific risk profile.
Hyperglycemia and Diabetes Mellitus
Hyperglycemia, in some cases extreme and associated with ketoacidosis or hyperosmolar coma or death, has been reported in patients treated with atypical antipsychotics including clozapine. Assessment of the relationship between atypical antipsychotic use and glucose abnormalities is complicated by the possibility of an increased background risk of diabetes mellitus in patients with schizophrenia and the increasing incidence of diabetes mellitus in the general population. Given these confounders, the relationship between atypical antipsychotic use and hyperglycemia-related adverse reactions is not completely understood. However, epidemiological studies suggest an increased risk of treatment-emergent, hyperglycemia-related adverse reactions in patients treated with the atypical antipsychotics. Precise risk estimates for hyperglycemia-related adverse reactions in patients treated with atypical antipsychotics are not available.
Patients with an established diagnosis of diabetes mellitus who are started on Clozapine ODT should be monitored regularly for worsening of glucose control. Patients with risk factors for diabetes mellitus (e.g., obesity, family history of diabetes) who are starting treatment with atypical antipsychotics should undergo fasting blood glucose testing at the beginning of treatment and periodically during treatment. Any patient treated with atypical antipsychotics should be monitored for symptoms of hyperglycemia including polydipsia, polyuria, polyphagia, and weakness. Patients who develop symptoms of hyperglycemia during treatment with atypical antipsychotics should undergo fasting blood glucose testing. In some cases, hyperglycemia has resolved when the atypical antipsychotic was discontinued; however, some patients required continuation of anti-diabetic treatment despite discontinuation of the suspect drug.
In a pooled data analysis of 8 studies in adult subjects with schizophrenia, the mean changes in fasting glucose concentration in the clozapine and chlorpromazine groups were +11 mg/dL and +4 mg/dL respectively. A higher proportion of the clozapine group demonstrated categorical increases from baseline in fasting glucose concentrations, compared to the chlorpromazine group (Table 4). The clozapine doses were 100 to 900 mg per day (mean modal dose: 512 mg per day). The maximum chlorpromazine dose was 1800 mg per day (mean modal dose: 1029 mg per day). The median duration of exposure was 42 days for clozapine and chlorpromazine.
Table 4: Categorical Changes in Fasting Glucose Level in Studies in Adult Subjects with Schizophrenia Laboratory Parameter
Category Change
(at least once) from Baseline
Treatment Arm
N
n (%)
Fasting Glucose
Normal
(<100 mg/dL)
to
High (≥126 mg/dL)
Clozapine
198
53 (27)
Chlorpromazine
135
14 (10)
Borderline
(100 to 125 mg/dL)
to
High (≥126 mg/dL)
Clozapine
57
24 (42)
Chlorpromazine
43
12 (28)
Dyslipidemia
Undesirable alterations in lipids have occurred in patients treated with atypical antipsychotics, including clozapine. Clinical monitoring, including baseline and periodic follow-up lipid evaluations in patients using Clozapine ODT, is recommended.
In a pooled data analysis of 10 studies in adult subjects with schizophrenia, clozapine treatment was associated with increases in serum total cholesterol. No data were collected on LDL and HDL cholesterol. The mean increase in total cholesterol was 13 mg/dL in the clozapine group and 15 mg/dL in the chlorpromazine group. In a pooled data analysis of 2 studies in adult subjects with schizophrenia, clozapine treatment was associated with increases in fasting serum triglyceride. The mean increase in fasting triglyceride was 71 mg/dL (54%) in the clozapine group and 39 mg/dL (35%) in the chlorpromazine group (Table 5). In addition, clozapine treatment was associated with categorical increases in serum total cholesterol and triglyceride, as illustrated in Table 6. The proportion of patients with categorical increases in total cholesterol or fasting triglyceride increased with the duration of exposure. The median duration of clozapine and chlorpromazine exposure was 45 days and 38 days, respectively. The clozapine dose range was 100 mg to 900 mg daily; the maximum chlorpromazine dose was 1800 mg daily.
Table 5: Mean Changes in Total Cholesterol and Triglyceride Concentration in Studies in Adult Subjects with Schizophrenia Treatment Arm
Baseline Total Cholesterol Concentration (mg/dL)
Change from Baseline mg/dL (%)
Clozapine (N=334)
184
+13 (7)
Chlorpromazine (N=185)
182
+15 (8)
Baseline Triglyceride
Concentration (mg/dL)
Change from Baseline
mg/dL (%)
Clozapine (N=6)
130
+71 (54)
Chlorpromazine (N=7)
110
+39 (35)
Table 6: Categorical Changes in Lipid Concentrations in Studies in Adult Subjects with Schizophrenia Laboratory Parameter
Category Change (at least once) from Baseline
Treatment Arm
N
n (%)
Total Cholesterol (random or fasting)
Increase by ≥40 mg/dL
Clozapine
334
111 (33)
Chlorpromazine
185
46 (25)
Normal (<200 mg/dL) to High (≥240 mg/dL)
Clozapine
222
18 (8)
Chlorpromazine
132
3 (2)
Borderline (200 to 239 mg/dL)
to High (≥240 mg/dL)
Clozapine
79
30 (38)
Chlorpromazine
34
14 (41)
Triglycerides
(fasting)
Increase by ≥50 mg/dL
Clozapine
6
3 (50)
Chlorpromazine
7
3 (43)
Normal (<150 mg/dL) to High (≥200 mg/dL)
Clozapine
4
0 (0)
Chlorpromazine
6
2 (33)
Borderline (≥150 mg/dL and <200 mg/dL) to High (≥200 mg/dL)
Clozapine
1
1 (100)
Chlorpromazine
1
0 (0)
Weight Gain
Weight gain has occurred with the use of antipsychotics, including clozapine. Monitor weight during treatment with Clozapine ODT. Table 7 summarizes the data on weight gain by the duration of exposure pooled from 11 studies with clozapine and active comparators. The median duration of exposure was 609, 728, and 42 days, in the clozapine, olanzapine, and chlorpromazine group, respectively.
Table 7: Mean Change in Body Weight (kg) by Duration of Exposure from Studies in Adult Subjects with Schizophrenia Metabolic Parameter
Exposure Duration
Clozapine (N=669)
Olanzapine (N=442)
Chlorpromazine (N=155)
n
Mean
n
Mean
n
Mean
Weight change from baseline
2 weeks (Day 11 to 17)
6
+0.9
3
+0.7
2
-0.5
4 weeks (Day 21 to 35)
23
+0.7
8
+0.8
17
+0.6
8 weeks (Day 49 to 63)
12
+1.9
13
+1.8
16
+0.9
12 weeks (Day 70 to 98)
17
+2.8
5
+3.1
0
0
24 weeks
(Day 154 to 182)
42
-0.6
12
+5.7
0
0
48 weeks
(Day 322 to 350)
3
+3.7
3
+13.7
0
0
Table 8 summarizes pooled data from 11 studies in adult subjects with schizophrenia demonstrating weight gain ≥7% of body weight relative to baseline. The median duration of exposure was 609, 728, and 42 days, in the clozapine, olanzapine, and chlorpromazine group, respectively.
Table 8: Proportion of Adult Subjects in Schizophrenia Studies with Weight Gain ≥7% Relative to Baseline Body Weight Weight Change
Clozapine
Olanzapine
Chlorpromazine
N
669
442
155
≥7% (inclusive)
236 (35%)
203 (46%)
13 (8%)
5.11 Neuroleptic Malignant Syndrome
Antipsychotic drugs including Clozapine ODT can cause a potentially fatal symptom complex referred to as Neuroleptic Malignant Syndrome (NMS). Clinical manifestations of NMS include hyperpyrexia, muscle rigidity, altered mental status, and autonomic instability (irregular pulse or blood pressure, tachycardia, diaphoresis, and cardiac dysrhythmias). Associated findings can include elevated creatine phosphokinase (CPK), myoglobinuria, rhabdomyolysis, and acute renal failure.
The diagnostic evaluation of patients with this syndrome is complicated. It is important to consider the presence of other serious medical conditions (e.g., severe neutropenia, infection, heat stroke, primary CNS pathology, central anticholinergic toxicity, extrapyramidal symptoms, and drug fever).
The management of NMS should include (1) immediate discontinuation of antipsychotic drugs and other drugs not essential to concurrent therapy, (2) intensive symptomatic treatment and medical monitoring, and (3) treatment of co-morbid medical conditions. There is no general agreement about specific pharmacological treatments for NMS.
If a patient requires antipsychotic drug treatment after recovery from NMS, the potential reintroduction of drug therapy should be carefully considered. NMS can recur. Monitor closely if restarting treatment with antipsychotics.
NMS has occurred with clozapine monotherapy and with concomitant CNS-active medications, including lithium.
5.12 Hepatotoxicity
Severe, life threatening, and in some cases fatal hepatotoxicity including hepatic failure, hepatic necrosis, and hepatitis have been reported in patients treated with clozapine [see Adverse Reactions (6.2)]. Monitor for the appearance of signs and symptoms of hepatotoxicity such as fatigue, malaise, anorexia, nausea, jaundice, bilirubinemia, coagulopathy, and hepatic encephalopathy. Perform serum tests for liver injury and consider permanently discontinuing treatment if hepatitis or transaminase elevations combined with other systemic symptoms are due to Clozapine ODT.
5.13 Fever
During clozapine therapy, patients have experienced transient, clozapine-related fever. The peak incidence is within the first 3 weeks of treatment. While this fever is generally benign and self- limited, it may necessitate discontinuing treatment. The fever can be associated with an increase or decrease in WBC count. Carefully evaluate patients with fever to rule out severe neutropenia or infection. [see Warnings and Precautions (5.1)]. Consider the possibility of NMS [see Warnings and Precautions (5.11)].
5.14 Pulmonary Embolism
Pulmonary embolism and deep-vein thrombosis have occurred in patients treated with clozapine. Consider the possibility of pulmonary embolism in patients who present with deep-vein thrombosis, acute dyspnea, chest pain, or with other respiratory signs and symptoms. Whether pulmonary embolus and deep vein thrombosis can be attributed to clozapine or some characteristic(s) of patients is not clear.
5.15 Anticholinergic Toxicity
Clozapine ODT has potent anticholinergic effects. Treatment with Clozapine ODT can result in CNS and peripheral anticholinergic toxicity, especially at higher dosages, or in overdose situations [see Overdosage (10)]. Use with caution in patients with a current diagnosis or prior history of constipation, urinary retention, clinically significant prostatic hypertrophy, or other conditions in which anticholinergic effects can lead to significant adverse reactions. When possible, avoid concomitant use with other anticholinergic medications because the risk for anticholinergic toxicity or severe gastrointestinal adverse reactions is increased [see Warnings and Precautions (5.7), Drug Interactions (7.1)].
5.16 Interference with Cognitive and Motor Performance
Clozapine ODT can cause sedation and impairment of cognitive and motor performance. Caution patients about operating hazardous machinery, including automobiles, until they are reasonably certain that Clozapine ODT does not affect them adversely. These reactions may be dose-related. Consider reducing the dose if they occur.
5.17 Tardive Dyskinesia
Tardive dyskinesia (TD) has occurred in patients treated with antipsychotic drugs, including clozapine. The syndrome consists of potentially irreversible, involuntary, dyskinetic movements. The risk of TD and the likelihood that it will become irreversible are believed to increase with greater durations of treatment and higher total cumulative doses. However, the syndrome can develop after relatively brief treatment periods at low doses. Prescribe Clozapine ODT in a manner that is most likely to minimize the risk of developing TD. Use the lowest effective dose and the shortest duration necessary to control symptoms. Periodically assess the need for continued treatment. Consider discontinuing treatment if TD occurs. However, some patients may require treatment with Clozapine ODT despite the presence of the syndrome.
TD may remit partially or completely if treatment is discontinued. Antipsychotic treatment, itself, may suppress (or partially suppress) the signs and symptoms, and it has the potential to mask the underlying process. The effect of symptom suppression on the long-term course of TD is unknown.
5.18 Patients with Phenylketonuria
Phenylketonuric patients should be informed that Clozapine ODT contain phenylalanine (a component of aspartame). Each 12.5 mg, orally disintegrating tablet contains 0.70 mg phenylalanine. Each 25 mg, orally disintegrating tablet contains 1.40 mg phenylalanine. Each 100 mg, orally disintegrating tablet contains 5.61 mg phenylalanine. Each 150 mg, orally disintegrating tablet contains 8.42 mg phenylalanine. Each 200 mg, orally disintegrating tablet contains 11.23 mg phenylalanine.
5.19 Cerebrovascular Adverse Reactions
In controlled trials, elderly patients with dementia-related psychosis treated with some atypical antipsychotics had an increased risk (compared to placebo) of cerebrovascular adverse reactions (e.g., stroke, transient ischemic attack), including fatalities. The mechanism for this increased risk is not known. An increased risk cannot be excluded for Clozapine ODT or other antipsychotics or other patient populations. Clozapine ODT should be used with caution in patients with risk factors for cerebrovascular adverse reactions.
5.20 Recurrence of Psychosis and Cholinergic Rebound after Abrupt Discontinuation of Clozapine ODT
If abrupt discontinuation of Clozapine ODT is necessary (because of severe neutropenia or another medical condition, for example) [see Dosage and Administration (2.4), Warnings and Precautions (5.1)], monitor carefully for the recurrence of psychotic symptoms and adverse reactions related to cholinergic rebound, such as profuse sweating, headache, nausea, vomiting, and diarrhea.
-
-
6 ADVERSE REACTIONS
The following adverse reactions are discussed in more detail in other sections of the labeling:
-
Severe Neutropenia [see Warnings and Precautions (5.1)]
-
Orthostatic Hypotension, Bradycardia, and Syncope [see Warnings and Precautions (5.2)]
-
Falls [see Warnings and Precautions (5.3)]
-
Seizures [see Warnings and Precautions (5.4)]
-
Myocarditis, Pericarditis, and Cardiomyopathy and Mitral Valve Incompetence [see Warnings and Precautions (5.5)]
-
Increased Mortality in Elderly Patients with Dementia-Related Psychosis [see Warnings and Precautions (5.6)]
-
Gastrointestinal Hypomotility with Severe Complications [see Warnings and Precautions (5.7)]
-
Eosinophilia [see Warnings and Precautions (5.8)]
-
QT Interval Prolongation [see Warnings and Precautions (5.9)]
-
Metabolic Changes (Hyperglycemia and Diabetes Mellitus, Dyslipidemia, and Weight Gain) [see Warnings and Precautions (5.10)]
-
Neuroleptic Malignant Syndrome [see Warnings and Precautions (5.11)]
-
Hepatotoxicity [see Warnings and Precautions (5.12)]
-
Fever [see Warnings and Precautions (5.13)]
-
Pulmonary Embolism [see Warnings and Precautions (5.14)]
-
Anticholinergic Toxicity [see Warnings and Precautions (5.15)]
-
Interference with Cognitive and Motor Performance [see Warnings and Precautions (5.16)]
-
Tardive Dyskinesia [see Warnings and Precautions (5.17)]
-
Patients with Phenylketonuria [see Warnings and Precautions (5.18)]
-
Cerebrovascular Adverse Reactions [see Warnings and Precautions (5.19)]
-
Recurrence of Psychosis and Cholinergic Rebound after Abrupt Discontinuation [see Warnings and Precautions (5.20)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
The most commonly reported adverse reactions (≥5%) across clozapine clinical trials were: CNS reactions, including sedation, dizziness/vertigo, headache, and tremor; cardiovascular reactions, including tachycardia, hypotension, and syncope; autonomic nervous system reactions, including hypersalivation, sweating, dry mouth, and visual disturbances; gastrointestinal reactions, including constipation and nausea; and fever. Table 9 summarizes the most commonly reported adverse reactions (≥5%) in clozapine-treated patients (compared to chlorpromazine-treated patients) in the pivotal, 6-week, controlled trial in treatment-resistant schizophrenia.
Table 9: Common Adverse Reactions (≥5%) in the 6-Week, Randomized, Chlorpromazine-Controlled Trial in Treatment-Resistant Schizophrenia Adverse Reaction
Clozapine
(N=126)
(%)
Chlorpromazine
(N=142)
(%)
Sedation
21
13
Tachycardia
17
11
Constipation
16
12
Dizziness
14
16
Hypotension
13
38
Fever (hyperthermia)
13
4
Hypersalivation
13
1
Hypertension
12
5
Headache
10
10
Nausea/vomiting
10
12
Dry mouth
5
20
Table 10 summarizes the adverse reactions reported in clozapine-treated patients at a frequency of 2% or greater across all clozapine studies (excluding the 2 year InterSePT™ Study). These rates are not adjusted for duration of exposure.
Table 10: Adverse Reactions (≥2%) Reported in Clozapine-treated Patients (N=842) Across all Clozapine Studies (excluding the 2 year InterSePT™ Study) Body System
Adverse Reaction
Clozapine
N=842
Percentage of Patients
† Rate based on population of approximately 1700 exposed during premarket clinical evaluation of clozapine. Central Nervous System
Drowsiness/Sedation
39
Dizziness/Vertigo
19
Headache
7
Tremor
6
Syncope
6
Disturbed Sleep/Nightmares
4
Restlessness
4
Hypokinesia/Akinesia
4
Agitation
4
Seizures (convulsions)
3†
Rigidity
3
Akathisia
3
Confusion
3
Fatigue
2
Insomnia
2
Cardiovascular
Tachycardia
25†
Hypotension
9
Hypertension
4
Gastrointestinal
Constipation
14
Nausea
5
Abdominal Discomfort/Heartburn
4
Nausea/Vomiting
3
Vomiting
3
Diarrhea
2
Urogenital
Urinary abnormalities
2
Autonomic Nervous System
Salivation
31
Sweating
6
Dry mouth
6
Visual disturbances
5
Skin
Rash
2
Hemic/Lymphatic
Leukopenia/Decreased WBC/Neutropenia
3
Miscellaneous
Fever
5
Weight Gain
4
Table 11 summarizes the most commonly reported adverse reactions (≥10% of the clozapine or olanzapine group) in the InterSePT™ Study. This was an adequate and well-controlled, two-year study evaluating the efficacy of clozapine relative to olanzapine in reducing the risk of suicidal behavior in patients with schizophrenia or schizoaffective disorder. The rates are not adjusted for duration of exposure.
Table 11: Incidence of Adverse Reactions in Patients Treated with Clozapine or Olanzapine in the InterSePT™ Study (≥10% in the clozapine or olanzapine group) Adverse Reactions
Clozapine
N=479
% Reporting
Olanzapine
N=477
% Reporting
Salivary hypersecretion
48%
6%
Somnolence
46%
25%
Weight increased
31%
56%
Dizziness (excluding vertigo)
27%
12%
Constipation
25%
10%
Insomnia
20%
33%
Nausea
17%
10%
Vomiting
17%
9%
Dyspepsia
14%
8%
Dystonia
Class effect: Symptoms of dystonia, prolonged abnormal contractions of muscle groups, may occur in susceptible individuals during the first few days of treatment. Dystonic symptoms include: spasm of the neck muscles, sometimes progressing to tightness of the throat, swallowing difficulty, difficulty breathing, and/or protrusion of the tongue. While these symptoms can occur at low doses, they occur more frequently and with greater severity with high potency and at higher doses of first generation antipsychotic drugs. An elevated risk of acute dystonia is observed in males and younger age groups.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of clozapine. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Central Nervous System
Delirium, EEG abnormal, myoclonus, paresthesia, possible cataplexy, status epilepticus, obsessive compulsive symptoms, and post-discontinuation cholinergic rebound adverse reactions.
Cardiovascular System
Atrial or ventricular fibrillation, ventricular tachycardia, QT interval prolongation, Torsades de Pointes, myocardial infarction, cardiac arrest, pericarditis, and periorbital edema.
Endocrine System
Pseudopheochromocytoma.
Gastrointestinal System
Acute pancreatitis, dysphagia, salivary gland swelling, megacolon, fecal incontinence, and intestinal ischemia, infarction, perforation, ulceration or necrosis.
Hepatobiliary SystemCholestasis, hepatitis, jaundice, hepatotoxicity, hepatic steatosis, hepatic necrosis, hepatic fibrosis, hepatic cirrhosis, liver injury (hepatic, cholestatic, and mixed), and liver failure.
Immune System Disorders
Angioedema, leukocytoclastic vasculitis.
Urogenital System
Acute interstitial nephritis, nocturnal enuresis, priapism, and renal failure.
Skin and Subcutaneous Tissue Disorders
Hypersensitivity reactions: photosensitivity, vasculitis, erythema multiforme, skin pigmentation disorder, and Stevens-Johnson syndrome.
Musculoskeletal System and Connective Tissue Disorders
Myasthenic syndrome, rhabdomyolysis, and systemic lupus erythematosus.
Respiratory System
Aspiration, pleural effusion, pneumonia, lower respiratory tract infection.
Hemic and Lymphatic System
Mild, moderate, or severe leukopenia, agranulocytosis, granulocytopenia, WBC decreased, deep-vein thrombosis, elevated hemoglobin/hematocrit, erythrocyte sedimentation rate (ESR) increased, sepsis, thrombocytosis, and thrombocytopenia.
Vision Disorders
Narrow-angle glaucoma.
Miscellaneous
Creatine phosphokinase elevation, hyperuricemia, hyponatremia, and weight loss.
-
-
7 DRUG INTERACTIONS
7.1 Potential for Other Drugs to Affect Clozapine ODT
Clozapine is a substrate for many cytochrome P450 isozymes, in particular CYP1A2, CYP3A4, and CYP2D6. Use caution when administering Clozapine ODT concomitantly with drugs that are inducers or inhibitors of these enzymes.
CYP1A2 Inhibitors
Concomitant use of Clozapine ODT and CYP1A2 inhibitors can increase plasma levels of clozapine, potentially resulting in adverse reactions. Reduce the Clozapine ODT dose to one third of the original dose when Clozapine ODT is coadministered with strong CYP1A2 inhibitors (e.g., fluvoxamine, ciprofloxacin, or enoxacin). The Clozapine ODT dose should be increased to the original dose when coadministration of strong CYP1A2 inhibitors is discontinued [see Dosage and Administration (2.7), Clinical Pharmacology (12.3)].
Moderate or weak CYP1A2 inhibitors include oral contraceptives and caffeine. Monitor patients closely when Clozapine ODT is coadministered with these inhibitors. Consider reducing the Clozapine ODT dosage if necessary [see Dosage and Administration (2.7)].
CYP2D6 and CYP3A4 Inhibitors
Concomitant treatment with Clozapine ODT and CYP2D6 or CYP3A4 inhibitors (e.g., cimetidine, escitalopram, erythromycin, paroxetine, bupropion, fluoxetine, quinidine, duloxetine, terbinafine, or sertraline) can increase clozapine levels and lead to adverse reactions [see Clinical Pharmacology (12.3)]. Use caution and monitor patients closely when using such inhibitors. Consider reducing the Clozapine ODT dose [see Dosage and Administration (2.7)].
CYP1A2 and CYP3A4 Inducers
Concomitant treatment with drugs that induce CYP1A2 or CYP3A4 can decrease the plasma concentration of clozapine, resulting in decreased effectiveness of Clozapine ODT. Tobacco smoke is a moderate inducer of CYP1A2. Strong CYP3A4 inducers include carbamazepine, phenytoin, St. John’s wort, and rifampin. It may be necessary to increase the Clozapine ODT dose if used concomitantly with inducers of these enzymes. However, concomitant use of Clozapine ODT and strong CYP3A4 inducers is not recommended [see Dosage and Administration (2.7)].
Consider reducing the Clozapine ODT dosage when discontinuing coadministered enzyme inducers, because discontinuation of inducers can result in increased clozapine plasma levels and an increased risk of adverse reactions [see Dosage and Administration (2.7)].
Anticholinergic Drugs
Concomitant treatment with Clozapine ODT and other drugs with anticholinergic activity (e.g., benztropine, cyclobenzaprine, diphenhydramine) can increase the risk for anticholinergic toxicity and severe gastrointestinal adverse reactions related to hypomotility. Avoid concomitant use of Clozapine ODT with anticholinergic drugs when possible [see Warnings and Precautions (5.7, 5.15)].
Drugs that Cause QT Interval Prolongation
Use caution when administering concomitant medications that prolong the QT interval or inhibit the metabolism of clozapine. Drugs that cause QT prolongation include: specific antipsychotics (e.g., ziprasidone, iloperidone, chlorpromazine, thioridazine, mesoridazine, droperidol, and pimozide), specific antibiotics (e.g., erythromycin, gatifloxacin, moxifloxacin, sparfloxacin), Class 1A antiarrhythmics (e.g., quinidine, procainamide) or Class III antiarrhythmics (e.g., amiodarone, sotalol), and others (e.g., pentamidine, levomethadyl acetate, methadone, halofantrine, mefloquine, dolasetron mesylate, probucol or tacrolimus) [see Warnings and Precautions (5.9)].
7.2 Potential for Clozapine ODT to Affect Other Drugs
Concomitant use of Clozapine ODT with other drugs metabolized by CYP2D6 can increase levels of these CYP2D6 substrates. Use caution when coadministering Clozapine ODT with other drugs that are metabolized by CYP2D6. It may be necessary to use lower doses of such drugs than usually prescribed. Such drugs include specific antidepressants, phenothiazines, carbamazepine, and Type 1C antiarrhythmics (e.g., propafenone, flecainide, and encainide).
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to atypical antipsychotics, including CLOZARIL, during pregnancy. Healthcare providers are encouraged to advise patients to register by calling the National Pregnancy Registry for Atypical Antipsychotics at1-866-961-2388 or visiting http://womensmentalhealth.org/clinical-and-research-programs/pregnancyregistry/.
Risk Summary
Neonates exposed to antipsychotic drugs, including Clozapine ODT, during the third trimester are at risk for extrapyramidal and/or withdrawal symptoms following delivery (see Clinical Considerations). Available data from published epidemiologic studies over decades of use with clozapine during pregnancy have not established a drug-associated risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes (see Data). There are risks to the mother associated with untreated schizophrenia and with exposure to antipsychotics, including Clozapine ODT, during pregnancy (see Clinical Considerations).
In animal reproduction studies, no adverse developmental effects were observed when clozapine was administered orally to pregnant rats or rabbits during the period of organogenesis, or to pregnant rats during pregnancy and lactation, at doses up to approximately 0.4 and 0.9 times the maximum recommended human dose (MRHD) of 900 mg/day, for rats and rabbits respectively, based on mg/m2 body surface area (see Data).
The background risk of major birth defects and miscarriage for the indicated populations is unknown. All pregnancies have a background risk of birth defects, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Clinical Considerations
Disease-associated maternal and/or embryo/fetal risk
There is a risk to the mother from untreated schizophrenia, including increased risk of relapse, hospitalization, and suicide. Schizophrenia is associated with increased adverse perinatal outcomes, including preterm birth. It is not known if this is a direct result of the illness or other comorbid factors.
Fetal/Neonatal adverse reactions
Extrapyramidal and/or withdrawal symptoms, including agitation, hypertonia, hypotonia, tremor, somnolence, respiratory distress, and feeding disorder have been reported in neonates who have been exposed to antipsychotic drugs, including Clozapine ODT, during the third trimester of pregnancy. These symptoms have varied in severity. Monitor neonates for extrapyramidal and/or withdrawal symptoms and manage symptoms appropriately. Some neonates recovered within hours or days without specific treatment; others required prolonged hospitalization.
Data
Animal Data
In embryofetal developmental studies, clozapine had no effects on maternal parameters, litter sizes, or fetal parameters when administered orally to pregnant rats and rabbits during the period of organogenesis at doses up to 0.4 and 0.9 times, respectively, the MRHD of 900 mg/day on a mg/m2 body surface area basis.
In peri/postnatal developmental studies, pregnant female rats were administered clozapine over the last third of pregnancy and until day 21 postpartum. Observations were made on fetuses at birth and during the postnatal period; the offspring were allowed to reach sexual maturity and mated. Clozapine caused a decrease in maternal body weight but had no effects on litter size or body weights of either F1 or F2 generations at doses up to 0.4 times the MRHD of 900 mg/day on a mg/m2 body surface area basis.
8.2 Lactation
Risk Summary
Clozapine is present in human milk. There is one case report of sedation and a report of agranulocytosis in an infant exposed to clozapine through human milk (see Clinical Considerations). There is no information on the effects of clozapine on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for Clozapine ODT and any potential adverse effects on the breastfed child from Clozapine ODT or from the underlying maternal condition.
Clinical Considerations
Infants exposed to Clozapine ODT should be monitored for excess sedation and neutropenia.
8.4 Pediatric Use
Safety and effectiveness of clozapine in pediatric patients have not been established.
8.5 Geriatric Use
There have not been sufficient numbers of geriatric patients in clinical studies utilizing clozapine to determine whether those over 65 years of age differ from younger subjects in their response to clozapine.
Orthostatic hypotension and tachycardia can occur with Clozapine ODT treatment [see Boxed Warning and Warnings and Precautions (5.2)]. Elderly patients, particularly those with compromised cardiovascular functioning, may be more susceptible to these effects.
Elderly patients may be particularly susceptible to the anticholinergic effects of Clozapine ODT, such as urinary retention and constipation [see Warnings and Precautions (5.15)].
Carefully select Clozapine ODT doses in elderly patients, taking into consideration their greater frequency of decreased hepatic, renal, or cardiac function, as well as other concomitant disease and other drug therapy. Clinical experience suggests that the prevalence of tardive dyskinesia appears to be highest among the elderly; especially elderly women [see Warnings and Precautions (5.17)].
8.6 Patients with Renal or Hepatic Impairment
Dose reduction may be necessary in patients with significant impairment of renal or hepatic function. Clozapine concentrations may be increased in these patients, because clozapine is almost completely metabolized and then excreted [see Dosage and Administration (2.8), Clinical Pharmacology (12.3)].
8.7 CYP2D6 Poor Metabolizers
Dose reduction may be necessary in patients who are CYP2D6 poor metabolizers. Clozapine concentrations may be increased in these patients, because clozapine is almost completely metabolized and then excreted [see Dosage and Administration (2.8), Clinical Pharmacology (12.3)].
-
10 OVERDOSAGE
10.1 Overdosage Experience
The most commonly reported signs and symptoms associated with Clozapine ODT overdose are: sedation, delirium, coma, tachycardia, hypotension, respiratory depression or failure; and hypersalivation. There are reports of aspiration pneumonia, cardiac arrhythmias, and seizure. Fatal overdoses have been reported with clozapine, generally at doses above 2500 mg. There have also been reports of patients recovering from overdoses well in excess of 4 g.
10.2 Management of Overdosage
There are no specific antidotes for Clozapine ODT overdose. Establish and maintain an airway; ensure adequate oxygenation and ventilation. Monitor cardiac status and vital signs. Use general symptomatic and supportive measures. Consider the possibility of multiple-drug involvement.
Contact a Certified Poison Control Center for the most up to date information on the management of overdosage (1-800-222-1222).
-
11 DESCRIPTION
Clozapine, an atypical antipsychotic drug, is a tricyclic dibenzodiazepine derivative, 8-chloro-11-(4-methyl-1-piperazinyl)-5H-dibenzo [b,e] [1,4] diazepine.
The structural formula is:
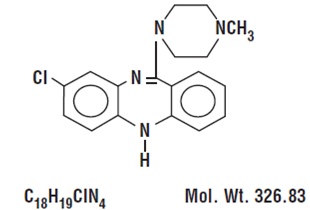
Clozapine Orally Disintegrating Tablets (referred to as Clozapine ODT) are yellow to pale yellow, and are for oral administration.
Each orally disintegrating tablet contains clozapine, USP, equivalent to 12.5 mg, 25 mg, 100 mg, 150 mg, and 200 mg.
The inactive ingredients include aspartame, crospovidone, magnesium stearate, mannitol, polyvinyl acetate, povidone, powdarome peppermint premium, silicified microcrystalline cellulose, sodium lauryl sulfate, sodium stearyl fumarate and yellow iron oxide.
Clozapine ODT contains aspartame [see Warnings and Precautions (5.18)]. Phenylalanine is a component of aspartame. Each 12.5 mg, orally disintegrating tablet contains 1.25 mg aspartame, thus, 0.70 mg phenylalanine. Each 25 mg, orally disintegrating tablet contains 2.5 mg aspartame, thus, 1.40 mg phenylalanine. Each 100 mg, orally disintegrating tablet contains 10 mg aspartame, thus, 5.61 mg phenylalanine. Each 150 mg, orally disintegrating tablet contains 15 mg aspartame, thus, 8.42 mg phenylalanine. Each 200 mg, orally disintegrating tablet contains 20 mg aspartame, thus, 11.23 mg phenylalanine.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The mechanism of action of clozapine is unknown. However, it has been proposed that the therapeutic efficacy of Clozapine ODT in schizophrenia is mediated through antagonism of the dopamine type 2 (D2) and the serotonin type 2A (5-HT2A) receptors. Clozapine also acts as an antagonist at adrenergic, cholinergic, histaminergic and other dopaminergic and serotonergic receptors.
12.2 Pharmacodynamics
Clozapine demonstrated binding affinity to the following receptors: histamine H1 (Ki 1.1 nM), adrenergic α1A (Ki 1.6 nM), serotonin 5-HT6 (Ki 4 nM), serotonin 5-HT2A (Ki 5.4 nM), muscarinic M1 (Ki 6.2 nM), serotonin 5-HT7 (Ki 6.3 nM), serotonin 5-HT2C (Ki 9.4 nM), dopamine D4 (Ki 24 nM), adrenergic α2A (Ki 90 nM), serotonin 5-HT3 (Ki 95 nM), serotonin 5-HT1A (Ki 120 nM), dopamine D2 (Ki 160 nM), dopamine D1 (Ki 270 nM), dopamine D5 (Ki 454 nM), and dopamine D3 (Ki 555 nM).
Clozapine causes little or no prolactin elevation.
Clinical electroencephalogram (EEG) studies demonstrated that clozapine increases delta and theta activity and slows dominant alpha frequencies. Enhanced synchronization occurs. Sharp wave activity and spike and wave complexes may also develop. Patients have reported an intensification of dream activity during clozapine therapy. REM sleep was found to be increased to 85% of the total sleep time. In these patients, the onset of REM sleep occurred almost immediately after falling asleep.
12.3 Pharmacokinetics
Absorption
In humans Clozapine ODT (25 mg and 100 mg) is equally bioavailable relative to a clozapine oral solution. Clozapine ODT is bioequivalent to Clozaril (clozapine) tablets. Following a dosage of 100 mg twice daily, the average steady-state peak plasma concentration was 413 ng/mL (range: 132 to 854 ng/mL), occurring at the average of 2.3 hours (range: 1 to 6 hours) after dosing. The average minimum concentration at steady-state was 168 ng/mL (range: 45 to 574 ng/mL), after 100 mg b.i.d. dosing.
A comparative bioequivalence/bioavailability study was conducted in 32 patients (with schizophrenia or schizoaffective disorder) comparing Clozapine ODT 200 mg to 2 × Clozapine ODT 100 mg (the approved reference product) under fasted conditions. The study also evaluated the effect of food and chewing on the pharmacokinetics of the 200 mg tablet. Under fasted conditions, the mean AUCss and Cmin,ss of clozapine for the 200 mg oral disintegrating tablets were equivalent to those of the 2 x 100 mg tablets. The mean Cmax,ss of clozapine for Clozapine ODT 200 mg was 85% that for 2 x 100 mg Clozapine ODT. This decrease in Cmax,ss for Clozapine ODT 200 mg is not clinically significant.
For Clozapine ODT 200 mg, food significantly increased the Cmin,ss of clozapine by 21%. However, this increase is not clinically significant. The mean AUCss and Cmax,ss of clozapine under fed conditions were equivalent to those under fasted conditions. Food delayed clozapine absorption by 1.5 hours, from a median Tmax of 2.5 hours under fasted conditions to 4 hours under fed conditions.
The mean Cmax,ss of clozapine under chewed conditions for Clozapine ODT 200 mg was about 86% that for 2 x 100 mg Clozapine ODT under non-chewed conditions, while the AUCss and Cmin,ss values were similar between the chewed and non-chewed conditions.
In a food-effect study, a single dose of Clozapine ODT 12.5 mg was administered to healthy volunteers under fasting conditions and after a high-fat meal. When Clozapine ODT were administered after a high-fat meal, the Cmax of both clozapine and its active metabolite, desmethylclozapine, were decreased by approximately 20%, compared to administration under fasting conditions, while the AUC values were unchanged. This decrease in Cmax is not clinically significant. Therefore, Clozapine ODT can be taken without regard to meals.
Distribution
Clozapine is approximately 97% bound to serum proteins. The interaction between clozapine and other highly protein-bound drugs has not been fully evaluated but may be important [see Drug Interactions (7)].
Metabolism and Excretion
Clozapine is almost completely metabolized prior to excretion, and only trace amounts of unchanged drug are detected in the urine and feces. Clozapine is a substrate for many cytochrome P450 isozymes, in particular CYP1A2, CYP2D6, and CYP3A4. Approximately 50% of the administered dose is excreted in the urine and 30% in the feces. The demethylated, hydroxylated, and N-oxide derivatives are components in both urine and feces. Pharmacological testing has shown the desmethyl metabolite (norclozapine) to have only limited activity, while the hydroxylated and N-oxide derivatives were inactive. The mean elimination half-life of clozapine after a single 75 mg dose was 8 hours (range: 4 to 12 hours), compared to a mean elimination half-life of 12 hours (range: 4 to 66 hours), after achieving steady state with 100 mg twice daily dosing.
A comparison of single-dose and multiple-dose administration of Clozapine ODT demonstrated that the elimination half-life increased significantly after multiple dosing relative to that after single-dose administration, suggesting the possibility of concentration-dependent pharmacokinetics. However, at steady state, approximately dose-proportional changes with respect to AUC (area under the curve), peak, and minimum clozapine plasma concentrations were observed after administration of 37.5, 75, and 150 mg twice daily.
Drug-Drug Interaction Studies
Fluvoxamine:
A pharmacokinetic study was conducted in 16 patients with schizophrenia who received clozapine under steady-state conditions. After coadministration of fluvoxamine for 14 days, mean trough concentrations of clozapine and its metabolites, N-desmethyl clozapine and clozapine N-oxide, were elevated about three-fold compared to baseline steady state concentrations.
Paroxetine, Fluoxetine, and Sertraline:
In a study of patients with schizophrenia (n=14) who received clozapine under steady-state conditions, coadministration of paroxetine produced only minor changes in the levels of clozapine and its metabolites. However, other published reports describe modest elevations (less than two-fold) of clozapine and metabolite concentrations when clozapine was taken with paroxetine, fluoxetine, and sertraline.
Specific Population Studies
Renal or Hepatic Impairment:
No specific pharmacokinetic studies were conducted to investigate the effects of renal or hepatic impairment on the pharmacokinetics of clozapine. Higher clozapine plasma concentrations are likely in patients with significant renal or hepatic impairment when given usual doses.
CYP2D6 Poor Metabolizers:
A subset (3% to 10%) of the population has reduced activity of CYP2D6 (CYP2D6 poor metabolizers). These individuals may develop higher than expected plasma concentrations of clozapine when given usual doses.
Patients with Pneumonia and Other Inflammatory Conditions:
Published case reports describe examples where pneumonia or other inflammatory conditions may increase clozapine concentrations. The clinical significance, the impact of treatments to modulate this inflammation, and mechanism of this potential increase in clozapine concentrations have not been fully characterized but may involve reduced cytochrome P450 1A2 activity.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
No carcinogenic potential was demonstrated in long-term studies in mice and rats at doses up to 0.3 times and 0.4 times, respectively, the maximum recommended human dose (MRHD) of 900 mg/day on a mg/m2 body surface area basis.
Mutagenesis
Clozapine was not genotoxic when tested in the following gene mutation and chromosomal aberration tests: the bacterial Ames test, the in vitro mammalian V79 in Chinese hamster cells, the in vitro unscheduled DNA synthesis in rat hepatocytes, or the in vivo micronucleus assay in mice.
Impairment of Fertility
Clozapine had no effect on any parameters of fertility, pregnancy, fetal weight, or postnatal development when administered orally to male rats 70 days before mating and to female rats for 14 days before mating at doses up to 0.4 times the MRHD of 900 mg/day on a mg/m2 body surface area basis.
-
14 CLINICAL STUDIES
14.1 Treatment-Resistant Schizophrenia
The efficacy of clozapine in treatment-resistant schizophrenia was established in a multicenter, randomized, double-blind, active-controlled (chlorpromazine) study in patients with a DSM-III diagnosis of schizophrenia who had inadequate responses to at least 3 different antipsychotics (from at least 2 different chemical classes) during the preceding 5 years. The antipsychotic trials must have been judged adequate; the antipsychotic dosages must have been equivalent to or greater than 1000 mg per day of chlorpromazine for a period of at least 6 weeks, each without significant reduction of symptoms. There must have been no period of good functioning within the preceding 5 years. Patients must have had a baseline score of at least 45 on the investigator- rated Brief Psychiatric Rating Scale (BPRS). On the 18-item BPRS, 1 indicates the absence of symptoms, and 7 indicates severe symptoms; the maximum potential total BPRS score is 126. At baseline, the mean BPRS score was 61. In addition, patients must have had a score of at least 4 on at least two of the following four individual BPRS items: conceptual disorganization, suspiciousness, hallucinatory behavior, and unusual thought content. Patients must have had a Clinical Global Impressions – Severity Scale score of at least 4 (moderately ill).
In the prospective, lead-in phase of the trial, all patients (N=305) initially received single-blind treatment with haloperidol (the mean dose was 61 mg per day) for 6 weeks. More than 80% of patients completed the 6-week trial. Patients with an inadequate response to haloperidol (n=268) were randomized to double-blind treatment with clozapine (N=126) or chlorpromazine (N=142). The maximum daily clozapine dose was 900 mg; the mean daily dose was >600 mg. The maximum daily chlorpromazine dose was 1800 mg; the mean daily dose was >1200 mg.
The primary endpoint was treatment response, predefined as a decrease in BPRS score of at least 20% and either (1) a CGI-S score of ≤3 (mildly ill), or (2) a BPRS score of ≤35, at the end of 6 weeks of treatment. Approximately 88% of patients from the clozapine and chlorpromazine groups completed the 6-week trial. At the end of six weeks, 30% of the clozapine group responded to treatment, and 4% of the chlorpromazine group responded to treatment. The difference was statistically significant (p<0.001). The mean change in total BPRS score was -16 and -5 in the clozapine and chlorpromazine group, respectively; the mean change in the 4 key BPRS item scores was -5 and -2 in the clozapine and chlorpromazine group, respectively; and the mean change in CGI-S score was -1.2 and -0.4, in the clozapine and chlorpromazine group, respectively. These changes in the clozapine group were statistically significantly greater than in the chlorpromazine group (p<0.001 in each analysis).
14.2 Recurrent Suicidal Behavior in Schizophrenia or Schizoaffective Disorder
The effectiveness of clozapine in reducing the risk of recurrent suicidal behavior was assessed in the International Suicide Prevention Trial (InterSePT™, a trademark of Novartis Pharmaceuticals Corporation). This was a prospective, randomized, open-label, active-controlled, multicenter, international, parallel-group comparison of clozapine (Clozaril®) versus olanzapine (Zyprexa®, a registered trademark of Eli Lilly and Company) in 956 patients with schizophrenia or schizoaffective disorder (DSM-IV) who were judged to be at risk for recurrent suicidal behavior. Only about one-fourth of these patients (27%) were considered resistant to standard antipsychotic drug treatment. To enter the trial, patients must have met one of the following criteria:
- They had attempted suicide within the three years prior to their baseline evaluation.
- They had been hospitalized to prevent a suicide attempt within the three years prior to their baseline evaluation.
- They demonstrated moderate-to-severe suicidal ideation with a depressive component within one week prior to their baseline evaluation.
- They demonstrated moderate-to-severe suicidal ideation accompanied by command hallucinations to do self-harm within one week prior to their baseline evaluation.
Dosing regimens for each treatment group were determined by individual investigators and were individualized by patient. Dosing was flexible, with a dose range of 200 to 900 mg/day for clozapine and 5 to 20 mg/day for olanzapine. For the 956 patients who received clozapine or olanzapine in this study, there was extensive use of concomitant psychotropics: 84% with antipsychotics, 65% with anxiolytics, 53% with antidepressants, and 28% with mood stabilizers. There was significantly greater use of concomitant psychotropic medications among the patients in the olanzapine group.
The primary efficacy measure was time to (1) a significant suicide attempt, including a completed suicide; (2) hospitalization due to imminent suicide risk, including increased level of surveillance for suicidality for patients already hospitalized; or (3) worsening of suicidality severity as demonstrated by “much worsening” or “very much worsening” from baseline in the Clinical Global Impression of Severity of Suicidality as assessed by the Blinded Psychiatrist (CGI-SS-BP) scale. A determination of whether or not a reported event met criterion 1 or 2 above was made by the Suicide Monitoring Board (SMB), a group of experts blinded to patient data.
A total of 980 patients were randomized to the study and 956 received study medication. Sixty-two percent of the patients were diagnosed with schizophrenia, and the remainder (38%) were diagnosed with schizoaffective disorder. Only about one-fourth of the total patient population (27%) was identified as “treatment-resistant” at baseline. There were more males than females in the study (61% of all patients were male). The mean age of patients entering the study was 37 years of age (range 18 to 69). Most patients were Caucasian (71%), 15% were Black, 1% were Asian, and 13% were classified as being of “other” races.
Patients treated with clozapine had a statistically significant longer delay in the time to recurrent suicidal behavior in comparison with olanzapine. This result should be interpreted only as evidence of the effectiveness of clozapine in delaying time to recurrent suicidal behavior and not a demonstration of the superior efficacy of clozapine over olanzapine.
The probability of experiencing (1) a significant suicide attempt, including a completed suicide, or (2) hospitalization because of imminent suicide risk, including increased level of surveillance for suicidality for patients already hospitalized, was lower for clozapine patients than for olanzapine patients at Week 104: clozapine 24% versus olanzapine 32%; 95% CI of the difference: 2%, 14% (Figure 1).
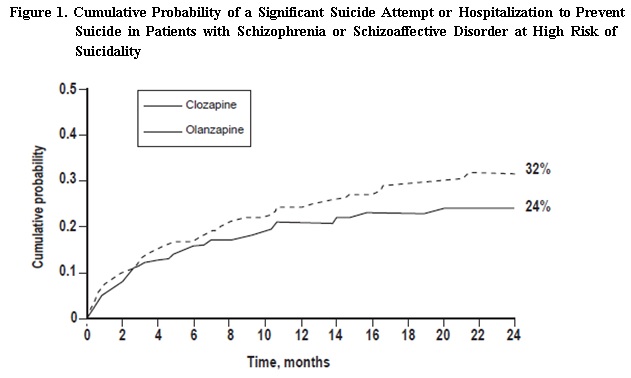
-
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
Clozapine Orally Disintegrating Tablets 12.5 mg are yellow to pale yellow color, round shaped tablet, flat faced bevelled edge debossed with “CLO” on one side and “12.5” on the other side.
Bottles of 100: 100 tablets in an HDPE bottle with child-resistant cap NDC: 59651-260-01
Clozapine Orally Disintegrating Tablets 25 mg are yellow to pale yellow color, round shaped tablet, flat faced bevelled edge debossed with “CLO” on one side and “25” on the other side.
Bottles of 100: 100 tablets in an HDPE bottle with child-resistant cap NDC: 59651-261-01
Cartons of 48 for Institutional Use Only: 8 cards, 6 non child-resistant
blisters per card NDC: 59651-261-48
Clozapine Orally Disintegrating Tablets 100 mg are yellow to pale yellow color, round shaped tablet, flat faced bevelled edge debossed with “CLO” on one side and “100” on the other side.
Bottles of 100: 100 tablets in an HDPE bottle with child-resistant cap NDC: 59651-262-01
Cartons of 48 for Institutional Use Only: 8 cards, 6 non child-resistant
blisters per card NDC: 59651-262-48
Clozapine Orally Disintegrating Tablets 150 mg are yellow to pale yellow color, round shaped tablet, flat faced bevelled edge debossed with “CLO” on one side and “150” on the other side.
Bottles of 100: 100 tablets in an HDPE bottle with child-resistant cap NDC: 59651-263-01
Cartons of 48 for Institutional Use Only: 8 cards, 6 non child-resistant
blisters per card NDC: 59651-263-48
Clozapine Orally Disintegrating Tablets 200 mg are yellow to pale yellow color, round shaped tablet, flat faced bevelled edge debossed with “CLO” on one side and “200” on the other side.
Bottles of 100: 100 tablets in an HDPE bottle with child-resistant cap NDC: 59651-264-01
Cartons of 48 for Institutional Use Only: 8 cards, 6 non child-resistant
blisters per card NDC: 59651-264-4816.2 Storage and Handling
Store Clozapine Orally Disintegrating Tablets (referred to as Clozapine ODT) at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature]. Protect from moisture.
Keep in a sealed blister until time of use. This unit-dose package is non child-resistant.
Keep Clozapine ODT in the original package until used by the patient.
Dispense in a tight, light-resistant container as defined in the USP, with a child-resistant closure (as required).
The quantity of Clozapine ODT depends on the ANC testing results [see Warnings and Precautions (5.1)]. If a patient is eligible for ANC testing:
-
Every week, then a 1-week supply of Clozapine ODT can be dispensed.
-
Every 2 weeks, then a 2-week supply of Clozapine ODT can be dispensed.
-
Every 4 weeks, then a 4-week supply of Clozapine ODT can be dispensed.
-
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide). Discuss the following issues with patients and caregivers:
Severe Neutropenia:
Instruct patients (and caregivers) [see Warnings and Precautions (5.1)]:
– About the risk of developing severe neutropenia and infection with Clozapine ODT treatment.
– To immediately report to their health care provider any symptom or sign of infection during Clozapine ODT treatment
– About the importance of having frequent ANC testing
Orthostatic Hypotension, Bradycardia, and Syncope:
Inform patients and caregivers about the risk of orthostatic hypotension and syncope, especially during the period of initial dose titration. Instruct them to strictly follow the clinician’s instructions for dosage and administration [see Dosage and Administration (2.3, 2.6)]. Advise patients to consult their clinician immediately if they feel faint, lose consciousness, or have signs or symptoms suggestive of bradycardia or arrhythmia [see Warnings and Precautions (5.2)].
Falls:
Inform patients of the risk of falls, which may lead to fractures or other injuries [see Warnings and Precautions (5.3)].
Seizures:
Inform patients and caregivers about the significant risk of seizure during Clozapine ODT treatment. Caution them about driving and any other potentially hazardous activity while taking Clozapine ODT [see Warnings and Precautions (5.4)].
Gastrointestinal Hypomotility with Severe Complications:
Educate patients and caregivers on the risks, prevention, and treatment of Clozapine ODT-induced constipation, including medications to avoid when possible (e.g., drugs with anticholinergic activity). Encourage appropriate hydration, physical activity, and fiber intake and emphasize that prompt attention and treatment to the development of constipation or other gastrointestinal symptoms is critical in preventing severe complications. Advise patients and caregivers to contact their health care provider if they experience symptoms of constipation (e.g., difficulty passing stools, incomplete passage of stool, decreased bowel movement frequency) or other symptoms associated with gastrointestinal hypomotility (e.g., nausea, abdominal distension or pain, vomiting) [see Warnings and Precautions (5.8), Drug Interactions (7.1)].
QT Interval Prolongation:
Advise patients to consult their clinician immediately if they feel faint, lose consciousness or have signs or symptoms suggestive of arrhythmia. Instruct patients to not take Clozapine ODT with other drugs that cause QT interval prolongation. Instruct patients to inform their clinicians that they are taking Clozapine ODT before any new drug [see Warnings and Precautions (5.9) and Drug Interactions (7.1)].
Metabolic Changes (hyperglycemia and diabetes mellitus, dyslipidemia, weight gain):
Educate patients and caregivers about the risk of metabolic changes and the need for specific monitoring. The risks include hyperglycemia and diabetes mellitus, dyslipidemia, weight gain, and cardiovascular reactions. Educate patients and caregivers about the symptoms of hyperglycemia (high blood sugar) and diabetes mellitus (e.g., polydipsia, polyuria, polyphagia, and weakness). Monitor all patients for these symptoms. Patients who are diagnosed with diabetes or have risk factors for diabetes (obesity, family history of diabetes) should have their fasting blood glucose monitored before beginning treatment and periodically during treatment. Patients who develop symptoms of hyperglycemia should have assessments of fasting glucose. Clinical monitoring of weight is recommended [see Warnings and Precautions (5.10)].
Patients with Phenylketonuria:
Inform patients and caregivers that Clozapine ODT contain phenylalanine (a component of aspartame) [see Warnings and Precautions (5.18)].
Interference with Cognitive and Motor Performance:
Because Clozapine ODT may have the potential to impair judgment, thinking, or motor skills, patients should be cautioned about operating hazardous machinery, including automobiles, until they are reasonably certain that Clozapine ODT therapy does not affect them adversely [see Warnings and Precautions (5.16)].
Hepatotoxicity:
Instruct patients to immediately report to their physician any symptom or sign of potential liver injury (e.g fatigue, malaise, anorexia, nausea, jaundice, bilirubinemia, coagulopathy, and hepatic encephalopathy) [see Warnings and Precautions (5.12)].
Missed Doses and Re-Initiating Treatment:
Inform patients and caregivers that if the patient misses taking Clozapine ODT for 1 day or more they should not restart their medication at the same dosage but should contact their physician for dosing instructions [see Dosage and Administration (2.5) and Warnings and Precautions (5.1, 5.2)].
Pregnancy:
Patients and caregivers should notify the clinician if the patient becomes pregnant or intends to become pregnant during therapy [see Use in Specific Populations (8.1)].
Nursing:
Advise patients and caregivers that the patient should not breast feed an infant if they are taking Clozapine ODT [see Use in Specific Populations (8.3)].
Concomitant Medication:
Advise patients to inform their healthcare provider if they are taking, or plan to take, any prescription or over-the-counter drugs; there is a potential for significant drug-drug interactions [see Dosage and Administration (2.6), Drug Interactions (7.1)].
Administration:
Patients should be advised that Clozapine ODT should remain in the original package until immediately before use [see Dosage and Administration (2.2)].
All brand names listed are the registered trademarks of their respective owners and are not trademarks of Aurobindo Pharma Limited.
Distributed by:
Aurobindo Pharma USA, Inc.
279 Princeton-Hightstown Road
East Windsor, NJ 08520
Manufactured by:
Aurobindo Pharma Limited
Hyderabad-500 032, India
Revised: 06/2025
-
MEDICATION GUIDE
MEDICATION GUIDE
Clozapine (kloe' za peen)
Orally Disintegrating Tablets,
for oral use
What is the most important information I should know about Clozapine Orally Disintegrating Tablets?
Clozapine Orally Disintegrating Tablets can cause serious side effects including:
- Severe neutropenia (low white blood cell (WBC) counts) that can lead to serious infections and death. Your healthcare provider will do WBC blood tests before starting treatment with clozapine orally disintegrating tablets and weekly for the first 6 months. After your first 6 months of treatment, your healthcare provider will determine how frequent you will have blood tests. If you have symptoms of severe neutropenia or an infection, your healthcare provider will do more frequent WBC blood test(s) to check if clozapine orally disintegrating tablets are causing your symptoms and may send you to see a blood specialist (hematologist). Tell your health care provider right away if you have any of the following symptoms or signs of neutropenia or infection:
º wounds that take a long time heal
º fever or chills
º skin, throat, vaginal, urinary tract, or lung infection
º feel extremely tired or weak
º pain or burning while peeing
º sores or ulcers inside your mouth, gums, or on your skin
º unusual vaginal discharge or itching
º sores or pain in or around your rectal area
º abdominal pain or bloating
- Orthostatic hypotension (decreased blood pressure), bradycardia (slow heart rate), or syncope (fainting) that can lead to death. You may feel lightheaded or faint when you rise too quickly from a sitting or lying position. Tell your healthcare provider right away if you feel dizzy or pass out.
- Seizures. See “What should I avoid while taking clozapine orally disintegrating tablets?”
- Myocarditis (heart muscle inflammation), pericarditis (inflammation of outer layer of the heart) and cardiomyopathy (heart muscle weakness) that can lead to death. Symptoms of myocarditis, pericarditis, and cardiomyopathy include:
º flu-like symptoms
º fast heartbeat or palpitations
º feel tired or faint
º shortness of breath
º swollen legs, ankles, or feet
º fever
- Increased risk of death in elderly people with dementia-related psychosis. Medicines like clozapine orally disintegrating tablets can increase the risk of death in elderly people who have lost touch with reality (psychosis) due to confusion and dementia. Clozapine orally disintegrating tablets is not for treatment of elderly people with dementia-related psychosis.
What is clozapine orally disintegrating tablets?
Clozapine orally disintegrating tablets are a prescription antipsychotic medicine used to treat people:
- Who are severely ill with schizophrenia not helped by other schizophrenia medicines
- With schizophrenia or schizoaffective disorder who have been suicidal and may be at risk of suicidal behavior again
Who should not take clozapine orally disintegrating tablets?
Do not take clozapine orally disintegrating tablets if you:
- are allergic to clozapine or any of the ingredients in clozapine orally disintegrating tablets. See the end of this Medication Guide for a complete list of ingredients in clozapine orally disintegrating tablets.
- have or have had heart problems or a family history of heart problems including heart attack, heart failure, abnormal heart rhythm or long QT syndrome, or stroke
- have or have had low or high blood pressure
- have or have had kidney or liver problems
- have or have had seizures (convulsions)
- have or have had stomach or intestinal problems including constipation, slow emptying of your stomach, or diarrhea
- have or have had low levels of potassium or magnesium in your blood
- have or have had diabetes or high blood sugar in you or your family
- have or have had high levels of total cholesterol, “bad” cholesterol (LDL-C) which causes plaque build-up in arteries, or triglycerides, or low levels of “good” cholesterol (HDL-C) which helps remove excess cholesterol from the arteries
- have increased pressure in your eyes (glaucoma), an enlarged prostate, or problems passing urine
- have or have had uncontrolled movements of your tongue, face, mouth, or jaw (tardive dyskinesia)
- smoke tobacco
- plan to stop smoking tobacco while taking clozapine orally disintegrating tablets
- use products containing caffeine
- are pregnant or plan to become pregnant. Talk to your healthcare provider if you become pregnant while taking clozapine orally disintegrating tablets.
- If you become pregnant while receiving CLOZARIL, talk to your healthcare provider about registering with the National Pregnancy Registry for Atypical Antipsychotics. You can register by calling 1-866-961-2388 or go to http://womensmentalhealth.org/clinical-and-research- programs/pregnancyregistry/
- are breast feeding or plan to breast feed. Clozapine can pass into your breast milk and may harm your baby. Talk to your healthcare provider about the best way to feed your baby if you take clozapine orally disintegrating tablets.
- Clozapine orally disintegrating tablets and other medicines may affect each other causing side effects.
- Your healthcare provider can tell you if it is safe to take clozapine orally disintegrating tablets with your other medicines. Do not start or stop any medicines while taking clozapine orally disintegrating tablets without talking to your healthcare provider first.
- Know the medicines you take. Keep a list of them to show your healthcare provider and pharmacist when you get a new medicine.
How should I take clozapine orally disintegrating tablets?
- Take clozapine orally disintegrating tablets exactly as your healthcare provider tells you to take it. Do not change your dose or stop taking clozapine orally disintegrating tablets unless your healthcare provider tells you to. Talk to your healthcare provider or pharmacist if you are not sure how to take clozapine orally disintegrating tablets.
- If you miss taking clozapine orally disintegrating tablets for 1 day or more, call your healthcare provider right away. Do not take 2 doses at the same time unless your healthcare provider tells you to.
- Take clozapine orally disintegrating tablets with or without food.
- See the detailed Instructions for Use at the end of this Medication Guide for information on how to take clozapine orally disintegrating tablets.
- If you take too much (overdose) clozapine orally disintegrating tablets, call your healthcare provider or the Poison Help line at 1-800-222-1222 or go to the nearest hospital emergency room right away.
- feeling sleepy
- fast or irregular heartbeat
- having a lot of saliva in your mouth
- confusion
- low blood pressure
- seizures
- coma
- shallow or difficult breathing
What should I avoid while taking clozapine orally disintegrating tablets?
- You should not drink alcohol while taking clozapine orally disintegrating tablets because it can increase your chances of getting serious side effects.
- Do not drive, operate machinery, swim, climb, or do dangerous activities until you know how clozapine orally disintegrating tablet affects you.
What are the possible side effects of clozapine orally disintegrating tablets?
Clozapine orally disintegrating tablets can cause serious side effects, including:
- See "What is the most important information I should know about clozapine orally disintegrating tablets?"
-
falls. Clozapine orally disintegrating tablets may make you sleepy, dizzy, may cause a decrease in your blood pressure when changing positions, and can slow your thinking and motor skills which may lead to falls that can cause fractures or other injuries.
-
slow emptying of your stomach and intestines (decreased gastric motility). Severe constipation and bowel problems can happen and can lead to hospitalization, surgery, and death. You may not feel or be aware of constipation symptoms. Your healthcare provider will examine you for possible bowel problems. Tell your healthcare provider if you get any signs and symptoms of decreased gastrointestinal motility during treatment with clozapine orally disintegrating tablets, including:
º having bowel movements less than normal
º stomach bloating or pain
º hard or dry stools
º nausea or vomiting
º difficulty passing gas
Staying well hydrated, increasing physical activity, and taking fiber during treatment with clozapine orally disintegrating tablets can help prevent constipation and other bowel problems. Your healthcare provider may prescribe medicines to prevent severe problems.
-
high count of a certain white blood cell (eosinophilia). Clozapine orally disintegrating tablets can cause a high count of eosinophils in some people and can be serious. This is a different risk than the risk of clozapine orally disintegrating tablets causing an abnormally low white blood cell count (neutropenia). Your health care provider may send you to see an internal medicine specialist (internist) or blood specialist (hematologist). Tell your healthcare provider right away if you have any of these symptoms:
º feeling very tired or weak
º coughing and wheezing
º fever
º nausea, vomiting, or diarrhea
º rash
º night sweats
º swelling
º confusion
º joint pain
º difficulty swallowing
-
serious heart rhythm problems (QTc Interval Prolongation) that can cause death. Your healthcare provider will do a physical exam and may obtain blood tests and an electrocardiogram before starting you on treatment with clozapine orally disintegrating tablets. Tell your healthcare provider right away if you have any of these symptoms:
º passing out or feeling like you will pass out
º dizziness
º feeling as if your heart is pounding or missing beats
-
problems with your metabolism such as:
- high blood sugar (hyperglycemia) or diabetes. Increases in blood sugar can happen in some people who take clozapine orally disintegrating tablets. Extremely high blood sugar can lead to coma and death. If you have diabetes or risk factors for diabetes (such as being overweight), your health care provider should check your blood sugar before you start clozapine orally disintegrating tablets and during treatment. Tell your healthcare provider if you have any of these symptoms of high blood sugar while taking clozapine orally disintegrating tablets:
º feel very hungry
º feel sick to your stomach
º need to urinate more than usual
º feel weak or tired
º feel confused, or your breath smells fruity
- increased fat levels (cholesterol and triglycerides) in your blood (dyslipidemia). Your healthcare provider should check the fat levels in your blood before you start and during treatment with clozapine orally disintegrating tablets.
- weight gain. You and your healthcare provider should check your weight regularly.
- neuroleptic malignant syndrome (NMS). NMS is a rare but serious condition that can lead to death and must be treated in a hospital. Tell your healthcare provider right away if you become severely ill and have any of these symptoms:
º confusion
º increased sweating
º stiff muscles
º changes in breathing, heartbeat, and blood pressure
- liver problems. Clozapine orally disintegrating tablets can cause serious life-threatening liver problems that can lead to death. Tell your healthcare provider right away if you have any of these symptoms:
º nausea and vomiting
º pain on the right side of your stomach (abdomen)
º loss of appetite
º yellowing of your skin or whites of your eyes
º elevated bilirubin levels
- fever. Some people may have a fever while they take clozapine orally disintegrating tablets. If you have a fever, your healthcare provider will do blood tests to check for neutropenia or an infection. Your healthcare provider may also send you to see a blood specialist (hematologist). Tell your healthcare provider if you have a fever.
- blood clot in your lung (pulmonary embolism) or in the veins of your legs (deep vein thrombosis). Get emergency help right away if you have symptoms of a blood clot including:
º swelling or pain in your leg, ankle or foot
º warm feeling in the skin of your affected leg
º changes in your skin color such as turning pale or blue
- a problem that includes dry mouth, increased sweating, increased pulse rate, constipation, and urinary retention (anticholinergic toxicity).
- problems thinking clearly and moving your body. See What should I avoid while taking clozapine orally disintegrating tablets?”
- uncontrolled movements of your tongue, face, mouth, or jaw (tardive dyskinesia). Tardive dyskinesia may not go away, even if you stop clozapine orally disintegrating tablets. Tardive dyskinesia may also start after you stop taking clozapine orally disintegrating tablets.
- stroke (cerebrovascular problems) in elderly people with dementia-related psychosis that can lead to death.
The most common side effects of clozapine orally disintegrating tablets include:
- sleepiness or drowsiness
- headache
- dizziness
- shaking movements (tremors)
- heart and blood vessel problems
- low blood pressure
- fast heartbeat
- having a lot of saliva in your mouth
- passing out (syncope)
- dry mouth
- increased sweating
- constipation and nausea
- vision problems
- fever
- These are not all the possible side effects of clozapine orally disintegrating tablets.
- Your healthcare provider may lower your dose or temporarily or permanently stop treatment with clozapine orally disintegrating tablets if you have certain symptoms or if your WBC count is low.
- Tell your healthcare provider if you have any side effect that bothers you or that does not go away.
- You may report side effects to FDA at 1-800-FDA-1088.
How should I store clozapine orally disintegrating tablets?
- Store clozapine orally disintegrating tablets at room temperature between 68°F to 77°F (20°C to 25°C).
- Keep clozapine orally disintegrating tablets in a sealed blister until time of use.
General information about the safe and effective use of clozapine orally disintegrating tablets.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use clozapine orally disintegrating tablets for a condition for which it was not prescribed. Do not give clozapine orally disintegrating tablets to other people, even if they have the same symptoms that you have. It may harm them. You can ask your healthcare provider (including pharmacist) for information about clozapine orally disintegrating tablets that is written for health professionals.
What are the ingredients in clozapine orally disintegrating tablets?
Active ingredient: clozapine
Inactive ingredients: aspartame, crospovidone, magnesium stearate, mannitol, polyvinyl acetate, povidone, powdarome peppermint premium, silicified microcrystalline cellulose, sodium lauryl sulfate, sodium stearyl fumarate and yellow iron oxide.
All brand names listed are the registered trademarks of their respective owners and are not trademarks of Aurobindo Pharma Limited.
Distributed by:
Aurobindo Pharma USA, Inc.
279 Princeton-Hightstown Road
East Windsor, NJ 08520
Manufactured by:
Aurobindo Pharma Limited
Hyderabad-500 032, India
This Medication Guide has been approved by the U.S. Food and Drug Administration.
Revised: 06/2025
-
PACKAGE LABEL-PRINCIPAL DISPLAY PANEL - 12.5 mg (100 Tablets Bottle)
NDC: 59651-260-01
Rx only
Clozapine Orally
Disintegrating Tablets
12.5 mg
Phenylketonurics: Contains
Phenylalanine, 0.70 mg per Tablet.
PHARMACIST: Dispense the Medication
Guide provided separately to each patient.
AUROBINDO 100 Tablets
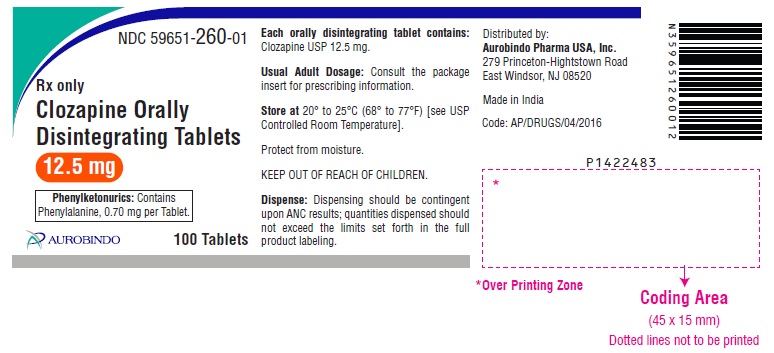
-
PACKAGE LABEL-PRINCIPAL DISPLAY PANEL - 25 mg (100 Tablets Bottle)
NDC: 59651-261-01
Rx only
Clozapine Orally
Disintegrating Tablets
25 mg
Phenylketonurics: Contains
Phenylalanine, 1.40 mg per Tablet.
PHARMACIST: Dispense the Medication
Guide provided separately to each patient.
AUROBINDO 100 Tablets
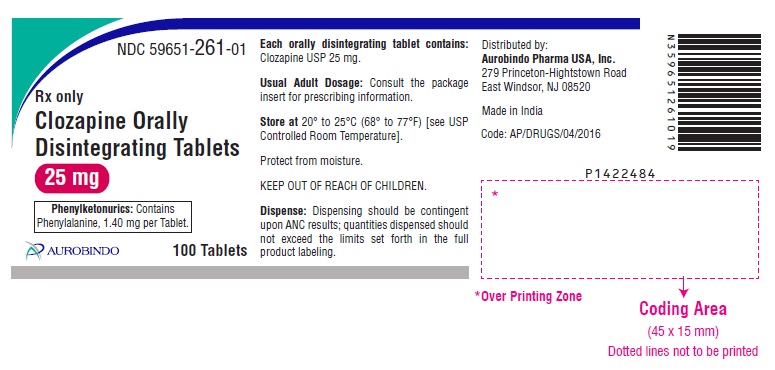
-
PACKAGE LABEL-PRINCIPAL DISPLAY PANEL - 25 mg Blister Carton 48 (8 x 6) Unit-dose Tablets
NDC: 59651-261-48
Rx only
Clozapine Orally Disintegrating Tablets
25 mg
Phenylketonurics: Contains
Phenylalanine, 1.40 mg per Tablet.
PHARMACIST: Dispense the Medication
Guide provided separately to each patient.
Non Child-Resistant
Institutional Use Only
AUROBINDO 48 (8 X 6) Unit-dose Tablets

-
PACKAGE LABEL-PRINCIPAL DISPLAY PANEL - 100 mg (100 Tablets Bottle)
NDC: 59651-262-01
Rx only
Clozapine Orally
Disintegrating Tablets
100 mg
Phenylketonurics: Contains
Phenylalanine, 5.61 mg per Tablet.
PHARMACIST: Dispense the Medication
Guide provided separately to each patient.
AUROBINDO 100 Tablets
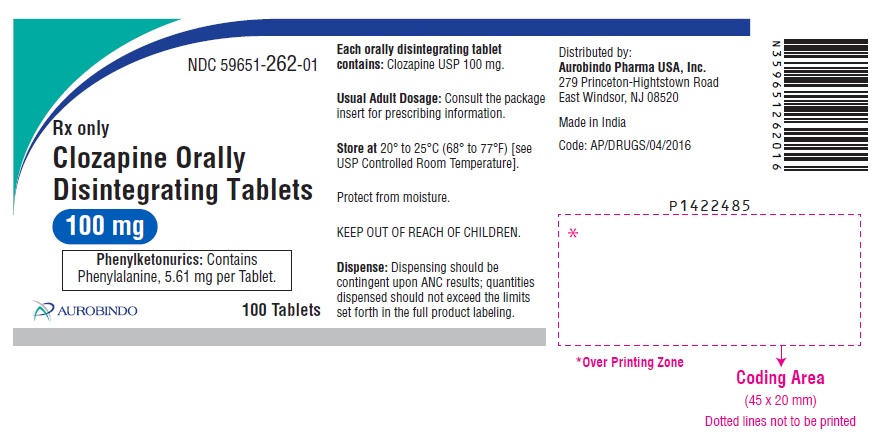
-
PACKAGE LABEL-PRINCIPAL DISPLAY PANEL - 100 mg Blister Carton 48 (8 x 6) Unit-dose Tablets
NDC: 59651-262-48
Rx only
Clozapine Orally Disintegrating Tablets
100 mg
Phenylketonurics: Contains
Phenylalanine, 5.61 mg per Tablet.
PHARMACIST: Dispense the Medication
Guide provided separately to each patient.
Non Child-Resistant
Institutional Use Only
AUROBINDO 48 (8 X 6) Unit-dose Tablets
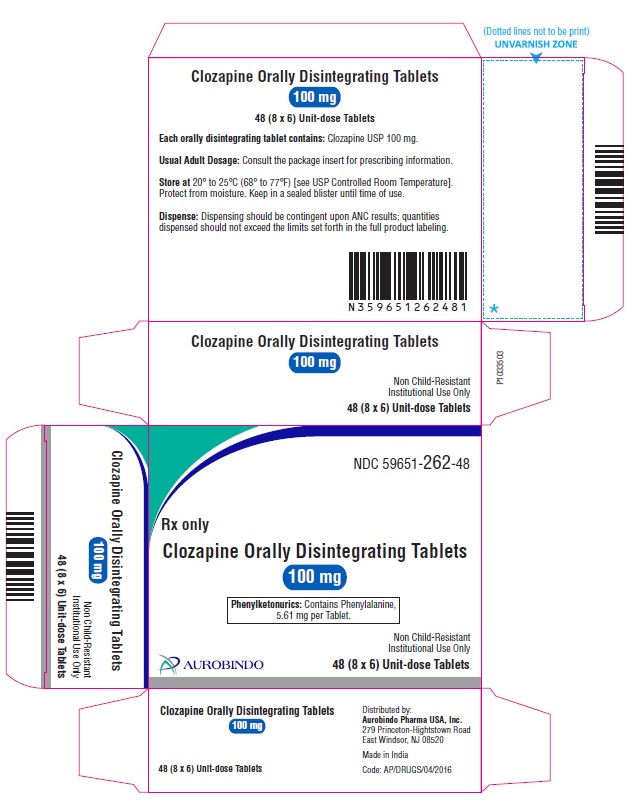
-
PACKAGE LABEL-PRINCIPAL DISPLAY PANEL - 150 mg (100 Tablets Bottle)
NDC: 59651-263-01
Rx only
Clozapine Orally
Disintegrating Tablets
150 mg
Phenylketonurics: Contains
Phenylalanine, 8.42 mg per Tablet.
PHARMACIST: Dispense the Medication
Guide provided separately to each patient.
AUROBINDO 100 Tablets
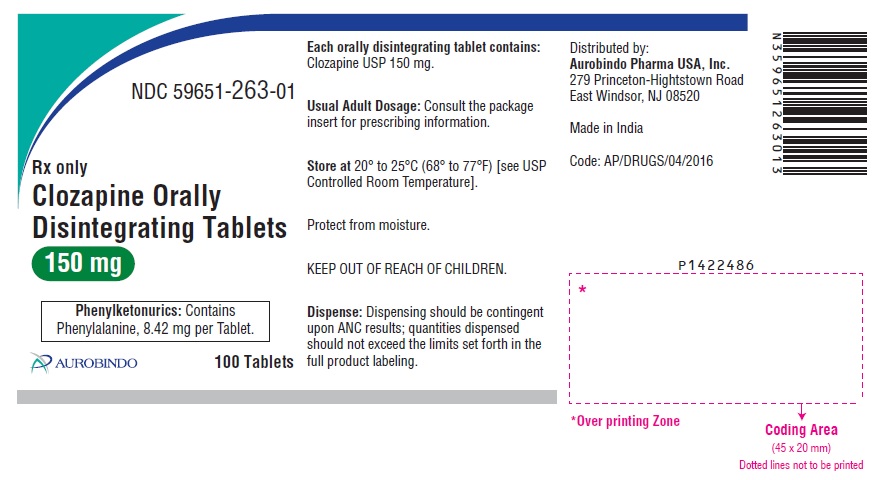
-
PACKAGE LABEL-PRINCIPAL DISPLAY PANEL - 150 mg Blister Carton 48 (8 x 6) Unit-dose Tablets
NDC: 59651-263-48
Rx only
Clozapine Orally Disintegrating Tablets
150 mg
Phenylketonurics: Contains
Phenylalanine, 8.42 mg per Tablet.
PHARMACIST: Dispense the Medication
Guide provided separately to each patient.
Non Child-Resistant
Institutional Use Only
AUROBINDO 48 (8 X 6) Unit-dose Tablets

-
PACKAGE LABEL-PRINCIPAL DISPLAY PANEL - 200 mg (100 Tablets Bottle)
NDC: 59651-264-01
Rx only
Clozapine Orally
Disintegrating Tablets
200 mg
Phenylketonurics: Contains
Phenylalanine, 11.23 mg per Tablet.
PHARMACIST: Dispense the Medication
Guide provided separately to each patient.
AUROBINDO 100 Tablets
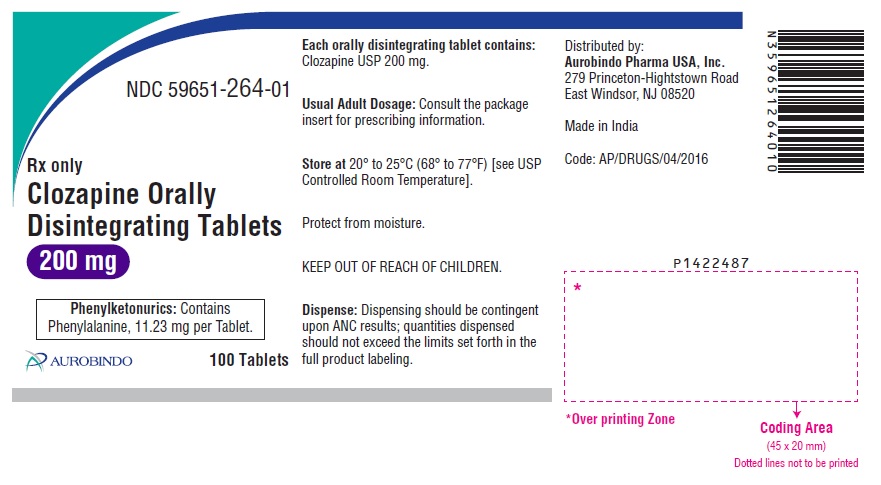
-
PACKAGE LABEL-PRINCIPAL DISPLAY PANEL - 200 mg Blister Carton 48 (8 x 6) Unit-dose Tablets
NDC: 59651-264-48
Rx only
Clozapine Orally Disintegrating Tablets
200 mg
Phenylketonurics: Contains
Phenylalanine, 11.23 mg per Tablet.
PHARMACIST: Dispense the Medication
Guide provided separately to each patient.
Non Child-Resistant
Institutional Use Only
AUROBINDO 48 (8 X 6) Unit-dose Tablets
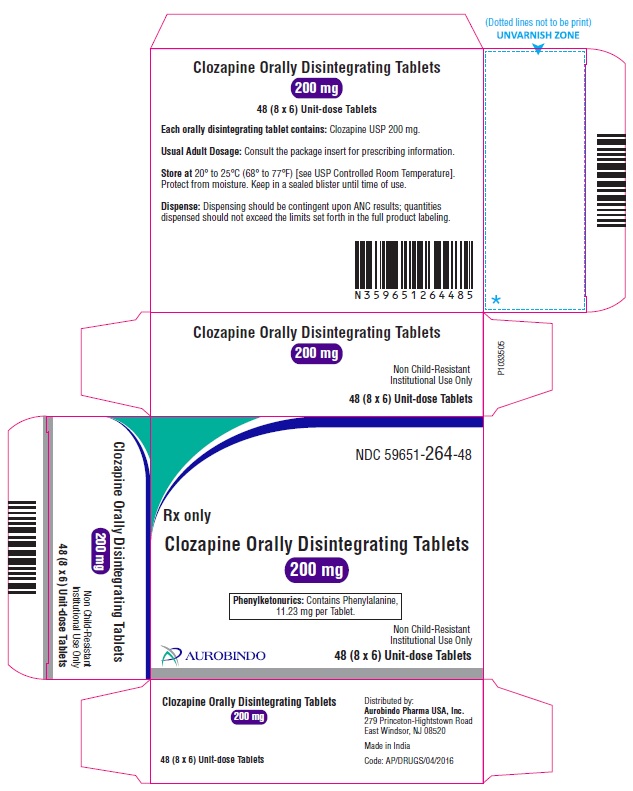
-
INGREDIENTS AND APPEARANCE
CLOZAPINE
clozapine tablet, orally disintegratingProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 59651-260 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CLOZAPINE (UNII: J60AR2IKIC) (CLOZAPINE - UNII:J60AR2IKIC) CLOZAPINE 12.5 mg Inactive Ingredients Ingredient Name Strength ASPARTAME (UNII: Z0H242BBR1) CROSPOVIDONE (35 .MU.M) (UNII: 40UAA97IT9) CROSPOVIDONE (20 .MU.M) (UNII: 6B46OH7T95) MAGNESIUM STEARATE (UNII: 70097M6I30) MANNITOL (UNII: 3OWL53L36A) POLYVINYL ACETATE (UNII: 32K497ZK2U) POVIDONE K30 (UNII: U725QWY32X) PEPPERMINT (UNII: V95R5KMY2B) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) SODIUM LAURYL SULFATE (UNII: 368GB5141J) SODIUM STEARYL FUMARATE (UNII: 7CV7WJK4UI) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) Product Characteristics Color YELLOW (Yellow to Pale Yellow) Score no score Shape ROUND (Flat Faced Bevelled Edge) Size 6mm Flavor PEPPERMINT Imprint Code CLO;12;5 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 59651-260-01 100 in 1 BOTTLE; Type 0: Not a Combination Product 12/12/2024 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA212923 12/12/2024 CLOZAPINE
clozapine tablet, orally disintegratingProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 59651-261 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CLOZAPINE (UNII: J60AR2IKIC) (CLOZAPINE - UNII:J60AR2IKIC) CLOZAPINE 25 mg Inactive Ingredients Ingredient Name Strength ASPARTAME (UNII: Z0H242BBR1) CROSPOVIDONE (35 .MU.M) (UNII: 40UAA97IT9) CROSPOVIDONE (20 .MU.M) (UNII: 6B46OH7T95) MAGNESIUM STEARATE (UNII: 70097M6I30) MANNITOL (UNII: 3OWL53L36A) POLYVINYL ACETATE (UNII: 32K497ZK2U) POVIDONE K30 (UNII: U725QWY32X) PEPPERMINT (UNII: V95R5KMY2B) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) SODIUM LAURYL SULFATE (UNII: 368GB5141J) SODIUM STEARYL FUMARATE (UNII: 7CV7WJK4UI) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) Product Characteristics Color YELLOW (Yellow to Pale Yellow) Score no score Shape ROUND (Flat Faced Bevelled Edge) Size 8mm Flavor PEPPERMINT Imprint Code CLO;25 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 59651-261-01 100 in 1 BOTTLE; Type 0: Not a Combination Product 12/12/2024 2 NDC: 59651-261-48 8 in 1 CARTON 12/12/2024 2 6 in 1 BLISTER PACK; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA212923 12/12/2024 CLOZAPINE
clozapine tablet, orally disintegratingProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 59651-262 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CLOZAPINE (UNII: J60AR2IKIC) (CLOZAPINE - UNII:J60AR2IKIC) CLOZAPINE 100 mg Inactive Ingredients Ingredient Name Strength ASPARTAME (UNII: Z0H242BBR1) CROSPOVIDONE (35 .MU.M) (UNII: 40UAA97IT9) CROSPOVIDONE (20 .MU.M) (UNII: 6B46OH7T95) MAGNESIUM STEARATE (UNII: 70097M6I30) MANNITOL (UNII: 3OWL53L36A) POLYVINYL ACETATE (UNII: 32K497ZK2U) POVIDONE K30 (UNII: U725QWY32X) PEPPERMINT (UNII: V95R5KMY2B) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) SODIUM LAURYL SULFATE (UNII: 368GB5141J) SODIUM STEARYL FUMARATE (UNII: 7CV7WJK4UI) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) Product Characteristics Color YELLOW (Yellow to Pale Yellow) Score no score Shape ROUND (Flat Faced Bevelled Edge) Size 13mm Flavor PEPPERMINT Imprint Code CLO;100 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 59651-262-01 100 in 1 BOTTLE; Type 0: Not a Combination Product 12/12/2024 2 NDC: 59651-262-48 8 in 1 CARTON 12/12/2024 2 6 in 1 BLISTER PACK; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA212923 12/12/2024 CLOZAPINE
clozapine tablet, orally disintegratingProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 59651-263 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CLOZAPINE (UNII: J60AR2IKIC) (CLOZAPINE - UNII:J60AR2IKIC) CLOZAPINE 150 mg Inactive Ingredients Ingredient Name Strength ASPARTAME (UNII: Z0H242BBR1) CROSPOVIDONE (35 .MU.M) (UNII: 40UAA97IT9) CROSPOVIDONE (20 .MU.M) (UNII: 6B46OH7T95) MAGNESIUM STEARATE (UNII: 70097M6I30) MANNITOL (UNII: 3OWL53L36A) POLYVINYL ACETATE (UNII: 32K497ZK2U) POVIDONE K30 (UNII: U725QWY32X) PEPPERMINT (UNII: V95R5KMY2B) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) SODIUM LAURYL SULFATE (UNII: 368GB5141J) SODIUM STEARYL FUMARATE (UNII: 7CV7WJK4UI) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) Product Characteristics Color YELLOW (Yellow to Pale Yellow) Score no score Shape ROUND (Flat Faced Bevelled Edge) Size 15mm Flavor PEPPERMINT Imprint Code CLO;150 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 59651-263-01 100 in 1 BOTTLE; Type 0: Not a Combination Product 12/12/2024 2 NDC: 59651-263-48 8 in 1 CARTON 12/12/2024 2 6 in 1 BLISTER PACK; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA212923 12/12/2024 CLOZAPINE
clozapine tablet, orally disintegratingProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 59651-264 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CLOZAPINE (UNII: J60AR2IKIC) (CLOZAPINE - UNII:J60AR2IKIC) CLOZAPINE 200 mg Inactive Ingredients Ingredient Name Strength ASPARTAME (UNII: Z0H242BBR1) CROSPOVIDONE (35 .MU.M) (UNII: 40UAA97IT9) CROSPOVIDONE (20 .MU.M) (UNII: 6B46OH7T95) MAGNESIUM STEARATE (UNII: 70097M6I30) MANNITOL (UNII: 3OWL53L36A) POLYVINYL ACETATE (UNII: 32K497ZK2U) POVIDONE K30 (UNII: U725QWY32X) PEPPERMINT (UNII: V95R5KMY2B) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) SODIUM LAURYL SULFATE (UNII: 368GB5141J) SODIUM STEARYL FUMARATE (UNII: 7CV7WJK4UI) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) Product Characteristics Color YELLOW (Yellow to Pale Yellow) Score no score Shape ROUND (Flat Faced Bevelled Edge) Size 16mm Flavor PEPPERMINT Imprint Code CLO;200 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 59651-264-01 100 in 1 BOTTLE; Type 0: Not a Combination Product 12/12/2024 2 NDC: 59651-264-48 8 in 1 CARTON 12/12/2024 2 6 in 1 BLISTER PACK; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA212923 12/12/2024 Labeler - Aurobindo Pharma Limited (650082092) Establishment Name Address ID/FEI Business Operations APL HEALTHCARE LIMITED 650918514 ANALYSIS(59651-260, 59651-261, 59651-262, 59651-263, 59651-264) , MANUFACTURE(59651-260, 59651-261, 59651-262, 59651-263, 59651-264)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.