PROMETHAZINE HCL- promethazine hydrochloride injection
PROMETHAZINE HCL by
Drug Labeling and Warnings
PROMETHAZINE HCL by is a Prescription medication manufactured, distributed, or labeled by Wockhardt USA LLC., Wockhardt Limited. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
DESCRIPTION
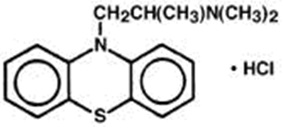
Promethazine HCl Injection USP, is a sterile, pyrogen-free solution for deep intramuscular or intravenous administration. Promethazine HCl (10H-Phenothiazine-10 ethanamine,N,N,α-trimethyl-, monohydrochloride, (±)-) is a racemic compound and has the following structural formula:
Each mL contains Promethazine HCl, either 25 mg or 50 mg with 0.1 mg edetate disodium, 0.04 mg calcium chloride, 0.5 mg sodium metabisulfite in water for injection. The pH range is 4.0 to 5.5; buffered with acetic acid-sodium acetate, and it is sealed under nitrogen.
Promethazine HCl Injection is a clear, colorless solution. The product is light sensitive. It should be inspected before use and discarded if either color or particulate is observed.
-
CLINICAL PHARMACOLOGY
Promethazine HCl is a phenothiazine derivative which possesses antihistaminic, sedative, antimotion-sickness, antiemetic, and anticholinergic effects. Promethazine is a competitive H1 receptor antagonist, but does not block the release of histamine. Structural differences from the neuroleptic phenothiazines result in its relative lack (1/10 that of chlorpromazine) of dopamine antagonist properties. Clinical effects are generally apparent within 5 minutes of an intravenous injection and within 20 minutes of an intramuscular injection. Duration of action is four to six hours, although effects may persist up to 12 hours. Promethazine HCl is metabolized in the liver, with the sulfoxides of promethazine and N-desmethylpromethazine being the predominant metabolites appearing in the urine. Following intravenous administration in healthy volunteers, the plasma half-life for promethazine has been reported to range from 9 to 16 hours. The mean plasma half-life for promethazine after intramuscular administration in healthy volunteers has been reported to be 9.8 ± 3.4 hours.
-
INDICATIONS AND USAGE
Promethazine HCl Injection is indicated for the following conditions:
- Amelioration of allergic reactions to blood or plasma.
- In anaphylaxis as an adjunct to epinephrine and other standard measures after the acute symptoms have been controlled.
- For other uncomplicated allergic conditions of the immediate type when oral therapy is impossible or contraindicated.
- For sedation and relief of apprehension and to produce light sleep from which the patient can be easily aroused.
- Active treatment of motion sickness.
- Prevention and control of nausea and vomiting associated with certain types of anesthesia and surgery.
- As an adjunct to analgesics for the control of postoperative pain.
- Preoperative, postoperative, and obstetric (during labor) sedation.
- Intravenously in special surgical situations, such as repeated bronchoscopy, ophthalmic surgery, and poor-risk patients, with reduced amounts of meperidine or other narcotic analgesic as an adjunct to anesthesia and analgesia.
-
CONTRAINDICATIONS
Promethazine HCl is contraindicated for use in pediatric patients less than two years of age.
Promethazine HCl Injection is contraindicated in comatose states and in patients who have demonstrated an idiosyncratic reaction or hypersensitivity to promethazine or other phenothiazines.
Under no circumstances should Promethazine HCl Injection be given by intra-arterial injection due to the likelihood of severe arteriospasm and the possibility of resultant gangrene (see WARNINGS-Injection Site Reactions).
Promethazine HCl Injection should not be given by the subcutaneous route; evidence of chemical irritation has been noted, and necrotic lesions have resulted following subcutaneous injection. The preferred parenteral route of administration is by deep intramuscular injection.
-
WARNINGS
WARNING: PROMETHAZINE HCl INJECTION SHOULD NOT BE USED IN PEDIATRIC PATIENTS LESS THAN 2 YEARS OF AGE BECAUSE OF THE POTENTIAL FOR FATAL RESPIRATORY DEPRESSION.
POSTMARKETING CASES OF RESPIRATORY DEPRESSION , INCLUDING FATALITIES , HAVE BEEN REPORTED WITH USE OF PROMETHAZINE HCl INJECTION IN PEDIATRIC PATIENTS LESS THAN 2 YEARS OF AGE. A WIDE RANGE OF WEIGHT-BASED DOSES OF PROMETHAZINE HCl INJECTION HAVE RESULTED IN RESPIRATORY DEPRESSION IN THESE PATIENTS.
CAUTION SHOULD BE EXERCISED WHEN ADMINISTERING PROMETHAZINE HCl INJECTION TO PEDIATRIC PATIENTS 2 YEARS OF AGE AND OLDER. IT IS RECOMMENDED THAT THE LOWEST EFFECTIVE DOSE OF PROMETHAZINE HCl INJECTION BE USED IN PEDIATRIC PATIENTS 2 YEARS OF AGE AND OLDER AND CONCOMITANT ADMINISTRATION OF OTHER DRUGS WITH RESPIRATORY DEPRESSANT EFFECTS BE AVOIDED.
Sulfite Sensitivity
Promethazine HCl Injection contains sodium metabisulfite, a sulfite that may cause allergic-type reactions, including anaphylactic symptoms and life-threatening or less severe asthma episodes, in certain susceptible people. The overall prevalence of sulfite sensitivity in the general population is unknown and probably low. Sulfite sensitivity is seen more frequently in asthmatic than in nonasthmatic people.
CNS Depression
Promethazine HCl Injection may impair the mental and/or physical abilities required for the performance of potentially hazardous tasks, such as driving a vehicle or operating machinery. The impairment may be amplified by concomitant use of other central-nervous-system depressants such as alcohol, sedative/hypnotics (including barbiturates), general anesthetics, narcotics, narcotic analgesics,tricyclic antidepressants, and tranquilizers; therefore such agents should either be eliminated or given in reduced dosage in the presence of promethazine HCl (see PRECAUTIONS-Information for Patients and Drug Interactions).
Respiratory Depression
Promethazine HCl Injection may lead to potentially fatal respiratory depression.
Use of Promethazine HCl Injection in patients with compromised respiratory function (e.g. COPD, sleep apnea) should be avoided.
Lower Seizure Threshold
Promethazine HCl Injection may lower seizure threshold and should be used with caution in persons with seizure disorders or in persons who are using concomitant medications, such as narcotics or local anesthetics, which may also affect seizure threshold.
Bone-Marrow Depression
Promethazine HCl Injection should be used with caution in patients with bone-marrow depression. Leukopenia and agranulocytosis have been reported, usually when promethazine HCl has been used in association with other known marrow-toxic agents.
Neuroleptic Malignant Syndrome
A potentially fatal symptom complex sometimes referred to as Neuroleptic Malignant Syndrome (NMS) has been reported in association with promethazine HCl alone or in combination with antipsychotic drugs. Clinical manifestations of NMS are hyperpyrexia, muscle rigidity, altered mental status and evidence of autonomic instability (irregular pulse or blood pressure, tachycardia, diaphoresis and cardiac dysrhythmias).
The diagnostic evaluation of patients with this syndrome is complicated. In arriving at a diagnosis, it is important to identify cases where the clinical presentation includes both serious medical illness (e.g., pneumonia, systemic infection, etc.) and untreated or inadequately treated extrapyramidal signs and symptoms (EPS). Other important considerations in the differential diagnosis include central anticholinergic toxicity, heat stroke, drug fever and primary central nervous system (CNS) pathology.
The management of NMS should include 1) immediate discontinuation of promethazine HCl, antipsychotic drugs, if any, and other drugs not essential to concurrent therapy, 2) intensive symptomatic treatment and medical monitoring, and 3) treatment of any concomitant serious medical problems for which specific treatments are available. There is no general agreement about specific pharmacological treatment regimens for uncomplicated NMS.
Since recurrences of NMS have been reported with phenothiazines, the reintroduction of promethazine HCl should be carefully considered.
Use in Pediatric Patients
PROMETHAZINE HCl INJECTION IS CONTRAINDICATED FOR USE IN PEDIATRIC PATIENTS LESS THAN TWO YEARS OF AGE.
CAUTION SHOULD BE EXERCISE WHEN ADMINISTERING PROMETHAZINE HCl INJECTION TO PEDIATRIC PATIENTS 2 YEARS OF AGE AND OLDER BECAUSE OF THE POTENTIAL FOR FATAL RESPIRATORY DEPRESSION. RESPIRATORY DEPRESSION AND APNEA, SOMETIMES ASSOCIATED WITH DEATH, ARE STRONLGY ASSOCIATED WITH PROMETHAZINE PRODUCTS AND NOT FIRMLY WIEGHT-RELATED, WHICH MIGHT OTHERWISE PERMIT SAFE ADMINISTRATION OF INDIVIDUALIZED DOSING. CONCOMITANT ADMINISTRATION OF PROMETHAZINE PRODUCTS WITH OTHER RESPIRATORY DEPRESSANTS HAS AN ASSOCIATION WITH RESPIRATORY DEPRESSION, AND SOMETIMES DEATH, IN PEDIATRIC PATIENTS.
ANTIEMETICS ARE NOT RECOMMENDED FOR TREATMENT OF UNCOMPLICATED VOMITING IN PEDIATRIC PATIENTS, AND THEIR USE SHOULD BE LIMITED TO PROLONGED VOMITING OF KNOWN ETIOLOGY. THE EXTRAPYRAMIDAL SYMPTOMS WHICH CAN OCCUR SECONDARY TO PROMETHAZINE HCl INJECTION ADMINISTRATION MAY BE CONFUSED WITH THE CNS SIGNS OF UNDIAGNOSED PRIMARY DISEASE, E.G., ENCEPHALOPATHY OR REYE'S SYNDROME. THE USE OF PROMETHAZINE HCl INJECTION SHOULD BE AVOIDED IN PEDIATRIC PATIENTS WHOSE SIGNS AND SYMPTOMS MAY SUGGEST REYE'S SYNDROME OR OTHER HEPATIC DISEASES.
Excessively large dosages of antihistamines, including Promethazine HCl Injection, in pediatric patients may cause sudden death (see OVERDOSAGE). Hallucinations and convulsions have occurred with therapeutic doses and overdoses of Promethazine HCl in pediatric patients. In pediatric patients who are acutely ill associated with dehydration, there is an increased susceptibility to dystonias with the use of Promethazine HCl Injection.
Injection Site Reactions
Promethazine HCl Injection can cause severe chemical irritation and damage to tissues, regardless of the route of administration. Irritation and damage can also result from perivascular extravasation, unintentional intra-arterial injection, and intraneuronal or perineuronal infiltration.
Signs, symptoms, and manifestations of severe tissue irritation include burning, pain, erythema, swelling, severe spasm of distal vessels, thrombophlebitis, venous thrombosis, phlebitis, abscesses, tissue necrosis, and gangrene. Administration of Promethazine HCl Injection has resulted in nerve damage ranging from temporary sensory loss to palsies and paralysis. Injection into or near a nerve may result in permanent tissue damage. In some cases, surgical intervention (including fasciotomy, skin graft, and/or amputation) may be required (see ADVERSE REACTIONS).
Inadvertent Intra-Arterial Injection
Due to the close proximity of arteries and veins in the areas most commonly used for intravenous injection, extreme care should be exercised to avoid perivascular extravasation or unintentional intra-arterial injection. Reports compatible with unintentional intra-arterial injection of Promethazine HCl Injection, usually in conjunction with other drugs intended for intravenous use, suggest that pain, severe chemical irritation, severe spasm of distal vessels, and resultant gangrene requiring amputation are likely under such circumstances. Intravenous injection was intended in all the cases reported but perivascular extravasation or arterial placement of the needle is now suspect. There is no proven successful management of unintentional intra-arterial injection or perivascular extravasation after it occurs. Sympathetic block and heparinization have been employed during the acute management of unintentional intra-arterial injection, because of the results of animal experiments with other known arteriolar irritants. Aspiration of dark blood does not preclude intra-arterial needle placement, because blood is discolored upon contact with Promethazine HCl Injection. Use of syringes with rigid plungers or of small-bore needles might obscure typical arterial backflow if this is relied upon alone.
When used intravenously, Promethazine HCl Injection should be given in a concentration no greater than 25 mg per mL and at a rate not to exceed 25 mg per minute. When administering any irritant drug intravenously, it is usually preferable to inject it through the tubing of an intravenous infusion set that is known to be functioning satisfactorily. In the event that a patient complains of pain during intended intravenous injection of Promethazine HCl Injection, the injection should be stopped immediately to provide for evaluation of possible arterial placement or perivascular extravasation.
-
PRECAUTIONS
General
Drugs having anticholinergic properties should be used with caution in patients with narrow-angle glaucoma, prostatic hypertrophy, stenosing peptic ulcer, pyloroduodenal obstruction, and bladder-neck obstruction.
Promethazine HCl Injection should be used cautiously in persons with cardiovascular disease or impairment of liver function.
Information for Patients
Promethazine HCl Injection may cause marked drowsiness or impair the mental or physical abilities required for the performance of potentially hazardous tasks, such as driving a vehicle or operating machinery. The use of alcohol, sedative/hypnotics (including barbiturates), general anesthetics, narcotics, narcotic analgesics, tricyclic antidepressants, and tranquilizers with Promethazine HCl Injection may enhance impairment (see WARNINGS-CNS Depression and PRECAUTIONS-Drug Interactions). Pediatric patients should be supervised to avoid potential harm in bike riding or in other hazardous activities.
Patients should be advised to report any involuntary muscle movements.
Persistent or worsening pain or burning at the injection site should be reported immediately.
Avoid prolonged exposure to the sun.
Drug Interactions
Promethazine HCl Injection may increase, prolong, or intensify the sedative action of central-nervous-system depressants, such as alcohol, sedative/hypnotics (including barbiturates), general anesthetics, narcotics, narcotic analgesics, tricyclic antidepressants, and tranquilizers; therefore, such agents should be avoided or administered in reduced dosage to patients receiving promethazine HCl. When given concomitantly with Promethazine HCl Injection, the dose of barbiturates should be reduced by at least one-half, and the dose of narcotics should be reduced by one-quarter to one-half. Dosage must be individualized. Excessive amounts of Promethazine HCl Injection relative to a narcotic may lead to restlessness and motor hyperactivity in the patient with pain; these symptoms usually disappear with adequate control of the pain.
Epinephrine
Because of the potential for Promethazine HCl to reverse epinephrine's vasopressor effect, epinephrine should NOT be used to treat hypotension associated with Promethazine HCl Injection overdose.
Anticholinergics
Concomitant use of other agents with anticholinergic properties should be undertaken with caution.
Monoamine Oxidase Inhibitors (MAOI)
Drug interactions, including an increased incidence of extrapyramidal effects, have been reported when some MAOI and phenothiazines are used concomitantly. This possibility should be considered with Promethazine HCl Injection.
Drug/Laboratory Test Interactions
The following laboratory tests may be affected in patients who are receiving therapy with Promethazine HCl Injection:
Pregnancy Tests
Diagnostic pregnancy tests based on immunological reactions between HCG and anti-HCG may result in false-negative or false-positive interpretations.
Glucose Tolerance Test
An increase in blood glucose has been reported in patients receiving promethazine HCl.
Carcinogenesis, Mutagenesis and Impairment of Fertility
Long-term animal studies have not been performed to assess the carcinogenic potential of Promethazine HCl Injection, nor are there other animal or human data concerning carcinogenicity, mutagenicity, or impairment of fertility. Promethazine HCl Injection was nonmutagenic in the Salmonella test system of Ames.
Pregnancy
Teratogenic Effects-Pregnancy Category C
Teratogenic effects have not been demonstrated in rat-feeding studies at doses of 6.25 and 12.5 mg/kg (approximately 2.1 and 4.2 times the maximum recommended human daily dose) of Promethazine HCl Injection. Daily doses of 25 mg/kg intraperitoneally have been found to produce fetal mortality in rats.
There are no adequate and well-controlled studies of Promethazine HCl Injection in pregnant women. Because animal reproduction studies are not always predictive of human response, Promethazine HCl Injection should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Adequate studies to determine the action of the drug on parturition, lactation and development of the animal neonate have not been conducted.
Nonteratogenic Effects
Promethazine HCl Injection administered to a pregnant woman within two weeks of delivery may inhibit platelet aggregation in the newborn.
Labor and Delivery
Promethazine HCl Injection may be used alone or as an adjunct to narcotic analgesics during labor (see DOSAGE AND ADMINISTRATION). Limited data suggest that use of Promethazine HCl Injection during labor and delivery does not have an appreciable effect on the duration of labor or delivery and does not increase the risk of need for intervention in the newborn. The effect on later growth and development of the newborn is unknown. (See also Pregnancy-Nonteratogenic Effects.)
Nursing Mothers
It is not known whether Promethazine HCl Injection is excreted in human milk. Because many drugs are excreted in human milk, and because of the potential for serious adverse reactions in nursing infants from Promethazine HCl Injection, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
PROMETHAZINE HCl IS CONTRAINDICATED FOR USE IN PEDIATRIC PATIENTS LESS THAN TWO YEARS OF AGE (see WARNINGS-Black Box Warning and Use in Pediatric Patients).
Promethazine HCl Injection should be used with caution in pediatric patients 2 years of age and older (see WARNINGS-Use in Pediatric Patients).
-
ADVERSE REACTIONS
Drowsiness is the most prominent CNS effect of this drug. Sedation, somnolence, blurred vision, dizziness, confusion, disorientation, and extrapyramidal symptoms such as oculogyric crisis, torticollis, and tongue protrusion; lassitude, tinnitus, incoordination, fatigue, euphoria, nervousness, diplopia, insomnia, tremors, convulsive seizures, excitation, catatonic-like states, hysteria. Hallucinations have also been reported.
Cardiovascular
Increased or decreased blood pressure, tachycardia, bradycardia, faintness. Thrombophlebitis, venous thrombosis, and phlebitis at the injection site have been reported and in some cases have required surgical intervention. INTRA-ARTERIAL INJECTION MAY RESULT IN GANGRENE OF THE AFFECTED EXTREMITY (see CONTRAINDICATIONS, WARNINGS-Injection Site Reactions, and DOSAGE AND ADMINISTRATION).
Dermatologic
Dermatitis, photosensitivity, urticaria.
Hematologic
Leukopenia, thrombocytopenia, thrombocytopenic purpura, agranulocytosis.
Gastrointestinal
Dry mouth, nausea, vomiting, jaundice.
Respiratory
Asthma, nasal stuffiness, respiratory depression (potentially fatal) and apnea (potentially fatal). (See WARNINGS-Respiratory Depression).
Other
Angioneurotic edema. Neuroleptic Malignant Syndrome (potentially fatal) has also been reported. (See WARNINGS-Neuroleptic Malignant Syndrome.) Administration of Promethazine HCl Injection has resulted in nerve damage ranging from temporary sensory loss to palsies and paralysis. Injection into or near a nerve may result in permanent tissue damage. Subcutaneous injection has resulted in tissue necrosis. Injection site reactions including burning, erythema, pain, and edema have been reported. Administration of Promethazine HCl Injection has resulted in abscesses and/or tissue necrosis and gangrene, regardless of the route of administration. In some cases, surgical intervention (including fasciotomy, skin graft, and/or amputation) may be required (see CONTRAINDICATIONS, WARNINGS-Injection Site Reactions, and DOSAGE AND ADMINISTRATION).
Paradoxical Reactions
Hyperexcitability and abnormal movements have been reported in patients following a single administration of Promethazine HCl Injection. Consideration should be given to the discontinuation of Promethazine HCl Injection and to the use of other drugs if these reactions occur. Respiratory depression, nightmares, delirium, and agitated behavior have also been reported in some of these patients.
-
OVERDOSAGE
Signs and symptoms of overdosage range from mild depression of the central nervous system and cardiovascular system to profound hypotension, respiratory depression, unconsciousness and sudden death. Other reported reactions include hyperreflexia, hypertonia, ataxia, athetosis, and extensor-plantar reflexes (Babinski reflex).
Stimulation may be evident, especially in pediatric patients and geriatric patients. Convulsions may rarely occur. A paradoxical-type reaction has been reported in pediatric patients receiving single doses of 75 mg to 125 mg orally, characterized by hyperexcitability and nightmares.
Atropine-like signs and symptoms-dry mouth; fixed, dilated pupils; flushing; etc., as well as gastrointestinal symptoms, may occur.
Treatment
Treatment of overdosage is essentially symptomatic and supportive. Only in cases of extreme overdosage or individual sensitivity do vital signs, including respiration, pulse, blood pressure, temperature, and EKG, need to be monitored. Attention should be given to the reestablishment of adequate respiratory exchange through provision of a patent airway and institution of assisted or controlled ventilation. Diazepam may be used to control convulsions. Acidosis and electrolyte losses should be corrected. Note that any depressant effects of Promethazine HCl Injection are not reversed by naloxone.
Avoid analeptics, which may cause convulsions. The treatment of choice for resulting hypotension is administration of intravenous fluids, accompanied by repositioning if indicated. In the event that vasopressors are considered for the management of severe hypotension which does not respond to intravenous fluids and repositioning, the administration of norepinephrine or phenylephrine should be considered. EPINEPHRINE SHOULD NOT BE USED, since its use in a patient with partial adrenergic blockade may further lower the blood pressure. Extrapyramidal reactions may be treated with anticholinergic antiparkinson agents, diphenhydramine, or barbiturates. Oxygen may also be administered. Limited experience with dialysis indicates that it is not helpful.
-
DOSAGE AND ADMINISTRATION
Promethazine HCl Injection is contraindicated for use in pediatric patients less than 2 years of age.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
Do not use Promethazine HCl Injection if solution has developed color or contains precipitate.
To avoid the possibility of physical and/or chemical incompatibility, consult specialized literature before diluting with any injectable solution or combining with any other medication. Do not use if there is a precipitate or any sign of incompatibility.
Important Notes on Administration
The preferred parenteral route of administration for Promethazine HCl Injection is by deep intramuscular injection. The proper intravenous administration of this product is well tolerated, but use of this route is not without some hazard. Not for subcutaneous administration.
UNINTENTIONAL INTRA-ARTERIAL INJECTION CAN RESULT IN GANGRENE OF THE AFFECTED EXTREMITY (see CONTRAINDICATIONS, WARNINGS-Injection Site Reactions). SUBCUTANEOUS INJECTION IS CONTRAINDICATED, AS IT MAY RESULT IN TISSUE NECROSIS (see CONTRAINDICATIONS, WARNINGS-Injection Site Reactions, and ADVERSE REACTIONS).
Injection into or near a nerve may result in permanent tissue damage (see ADVERSE REACTIONS).
When used intravenously, Promethazine HCl Injection should be given in a concentration no greater than 25 mg/mL at a rate not to exceed 25 mg per minute; it is preferable to inject through the tubing of an intravenous infusion set that is known to be functioning satisfactorily.
Allergic Conditions
The average adult dose is 25 mg. This dose may be repeated within two hours if necessary, but continued therapy, if indicated, should be via the oral route as soon as existing circumstances permit. After initiation of treatment, dosage should be adjusted to the smallest amount adequate to relieve symptoms. The average adult dose for amelioration of allergic reactions to blood or plasma is 25 mg.
Sedation
In hospitalized adult patients, nighttime sedation may be achieved by a dose of 25 to 50 mg of Promethazine HCl Injection.
Nausea and Vomiting
For control of nausea and vomiting, the usual adult dose is 12.5 to 25 mg, not to be repeated more frequently than every four hours. When used for control of postoperative nausea and vomiting, the medication may be administered either intramuscularly or intravenously and dosage of analgesics and barbiturates reduced accordingly.
Antiemetics should not be used in vomiting of unknown etiology in children and adolescents (see WARNINGS–Use in Pediatric Patients).
Preoperative and Postoperative Use
As an adjunct to preoperative or postoperative medication, 25 to 50 mg of Promethazine HCl Injection in adults may be combined with appropriately reduced doses of analgesics and atropine-like drugs as desired. Dosage of concomitant analgesic or hypnotic medication should be reduced accordingly.
Promethazine HCl is contraindicated for use in pediatric patients less than two years of age.
Obstetrics
Promethazine HCl Injection in doses of 50 mg will provide sedation and relieve apprehension in the early stages of labor. When labor is definitely established, 25 to 75 mg (average dose, 50 mg) Promethazine HCl Injection may be given intramuscularly or intravenously with an appropriately reduced dose of any desired narcotic. If necessary, Promethazine HCl Injection with a reduced dose of analgesic may be repeated once or twice at four-hour intervals in the course of a normal labor. A maximum total dose of 100 mg of Promethazine HCl Injection may be administered during a 24-hour period to patients in labor.
Pediatric Patients
Promethazine HCl Injection is contraindicated for use in pediatric patients less than 2 years of age (see WARNINGS-Black Box Warning and Use in Pediatric Patients). Caution should be exercised when administering promethazine HCl to pediatric patients 2 years of age or older. It is recommended that the lowest effective dose of promethazine hydrochloride be used in pediatric patients 2 years of age and older and concomitant administration of other drugs with respiratory depressant effects be avoided (see WARNINGS-Black Box Warning and Use in Pediatric Patients).
In pediatric patients 2 years of age and older, the dosage should not exceed half that of the suggested adult dose. As an adjunct to premedication, the suggested dose is 0.5 mg per lb of body weight in combination with an appropriately reduced dose of narcotic or barbiturate and the appropriate dose of an atropine-like drug. Antiemetics should not be used in vomiting of unknown etiology in pediatric patients.
-
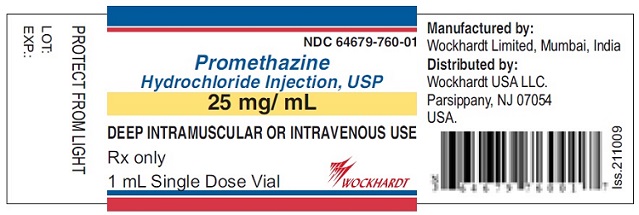
HOW SUPPLIED
Promethazine HCl Injection, USP is available as follows:
25 mg/mL
1 mL fill in a 2 mL vial (Box of 25 Vials) (NDC: 64679-760-01)
1 mL fill in a 2 mL vial (Carton Mono) (NDC: 64679-760-02)
1 mL fill in a 2 mL vial (Box of 5 Vials) (NDC: 64679-760-03)
1 mL fill in a 2 mL vial (Box of 10 Vials) (NDC: 64679-760-04)
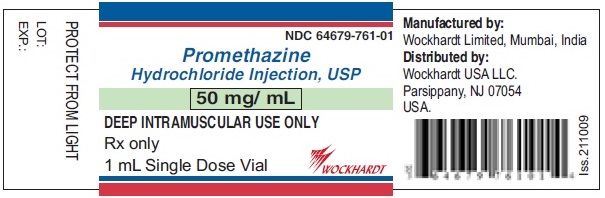
50 mg/mL
1 mL fill in a 2 mL vial (Box of 25 Vials) (NDC: 64679-761-01)
1 mL fill in a 2 mL vial (Carton Mono) (NDC: 64679-761-04)
1 mL fill in a 2 mL vial (Box of 5 Vials) (NDC: 64679-761-02)
1 mL fill in a 2 mL vial (Box of 10 Vials) (NDC: 64679-761-03)
- STORAGE AND HANDLING
- PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
PROMETHAZINE HCL
promethazine hydrochloride injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 64679-760 Route of Administration INTRAMUSCULAR, INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength PROMETHAZINE HYDROCHLORIDE (UNII: R61ZEH7I1I) (PROMETHAZINE - UNII:FF28EJQ494) PROMETHAZINE HYDROCHLORIDE 25 mg in 1 mL Inactive Ingredients Ingredient Name Strength ACETIC ACID (UNII: Q40Q9N063P) CALCIUM CHLORIDE (UNII: M4I0D6VV5M) 0.04 mg in 1 mL EDETATE DISODIUM (UNII: 7FLD91C86K) 0.1 mg in 1 mL SODIUM ACETATE (UNII: 4550K0SC9B) SODIUM METABISULFITE (UNII: 4VON5FNS3C) 0.5 mg in 1 mL WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 64679-760-01 25 in 1 CARTON 12/23/2009 1 1 mL in 1 VIAL, SINGLE-DOSE; Type 0: Not a Combination Product 2 NDC: 64679-760-04 10 in 1 CARTON 12/23/2009 2 1 mL in 1 VIAL, SINGLE-DOSE; Type 0: Not a Combination Product 3 NDC: 64679-760-03 5 in 1 CARTON 12/23/2009 3 1 mL in 1 VIAL, SINGLE-DOSE; Type 0: Not a Combination Product 4 NDC: 64679-760-02 1 in 1 CARTON 12/23/2009 4 1 mL in 1 VIAL, SINGLE-DOSE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA040785 12/23/2009 PROMETHAZINE HCL
promethazine hydrochloride injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 64679-761 Route of Administration INTRAMUSCULAR, INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength PROMETHAZINE HYDROCHLORIDE (UNII: R61ZEH7I1I) (PROMETHAZINE - UNII:FF28EJQ494) PROMETHAZINE HYDROCHLORIDE 50 mg in 1 mL Inactive Ingredients Ingredient Name Strength ACETIC ACID (UNII: Q40Q9N063P) CALCIUM CHLORIDE (UNII: M4I0D6VV5M) 0.04 mg in 1 mL EDETATE DISODIUM (UNII: 7FLD91C86K) 0.1 mg in 1 mL SODIUM ACETATE (UNII: 4550K0SC9B) SODIUM METABISULFITE (UNII: 4VON5FNS3C) 0.5 mg in 1 mL WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 64679-761-01 25 in 1 CARTON 12/23/2009 1 1 mL in 1 VIAL, SINGLE-DOSE; Type 0: Not a Combination Product 2 NDC: 64679-761-03 10 in 1 CARTON 12/23/2009 2 1 mL in 1 VIAL, SINGLE-DOSE; Type 0: Not a Combination Product 3 NDC: 64679-761-02 5 in 1 CARTON 12/23/2009 3 1 mL in 1 VIAL, SINGLE-DOSE; Type 0: Not a Combination Product 4 NDC: 64679-761-04 1 in 1 CARTON 12/23/2009 4 1 mL in 1 VIAL, SINGLE-DOSE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA040785 12/23/2009 Labeler - Wockhardt USA LLC. (170508365) Registrant - Wockhardt Limited (650069115) Establishment Name Address ID/FEI Business Operations Wockhardt Limited 676257570 ANALYSIS(64679-760, 64679-761) , LABEL(64679-760, 64679-761) , MANUFACTURE(64679-760, 64679-761) , PACK(64679-760, 64679-761)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.