MORPHINE SULFATE solution
Morphine Sulfate by
Drug Labeling and Warnings
Morphine Sulfate by is a Prescription medication manufactured, distributed, or labeled by Precision Dose, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use MORPHINE SULFATE ORAL SOLUTION safely and effectively. See full prescribing information for MORPHINE SULFATE ORAL SOLUTION.
MORPHINE SULFATE oral solution, for oral use CII
Initial U.S. Approval: 1941WARNING: SERIOUS AND LIFE-THREATENING RISKS FROM USE OF MORPHINE SULFATE ORAL SOLUTION
See full prescribing information for complete boxed warning.- Ensure accuracy when prescribing, dispensing, and administering Morphine Sulfate Oral Solution. Dosing errors due to confusion between mg and mL, and other morphine sulfate oral solutions of different concentrations can result in accidental overdose and death. (2.1, 5.1)
- Morphine Sulfate Oral Solution exposes users to risks of addiction, abuse, and misuse, which can lead to overdose and death. Assess patient's risk before prescribing and reassess regularly for these behaviors and conditions. (5.2)
- Serious, life-threatening, or fatal respiratory depression may occur especially during initiation and following dosage increase. To reduce the risk of respiratory depression, proper dosing and titration of Morphine Sulfate Oral Solution are essential. (5.3)
- Accidental ingestion of Morphine Sulfate Oral Solution, especially by children, can result in a fatal overdose of morphine. (5.3)
- Concomitant use of opioids with benzodiazepines or other central nervous system (CNS) depressants, including alcohol, may result in profound sedation, respiratory depression, coma, and death. Reserve concomitant prescribing for use in patients for whom alternative treatment options are inadequate. (5.4, 7)
- If opioid use is required for an extended period of time in a pregnant woman, advise the patient of the risk of Neonatal Opioid Withdrawal Syndrome, which may be life-threatening if not recognized and treated. Ensure that management by neonatology experts will be available at delivery. (5.5)
- Healthcare providers are strongly encouraged to complete a REMS-compliant education program and to counsel patients and caregivers on serious risks, safe use, and the importance of reading the Medication Guide with each prescription. (5.6)
RECENT MAJOR CHANGES
INDICATIONS AND USAGE
Morphine Sulfate Oral Solution is an opioid agonist.
Morphine Sulfate 2 mg/mL and 4 mg/mL is indicated for the management of:- adults with acute and chronic pain severe enough to require an opioid analgesic and for which alternative treatments are inadequate. (1)
- pediatric patients 2 years of age and older with acute pain severe enough to require an opioid analgesic and for which alternative treatments are inadequate. (1)
Morphine Sulfate Oral Solution 20 mg/mL is indicated for: - the relief of acute and chronic pain in opioid-tolerant adult patients. (1)
Limitations of Use (1): Because of the risks of addiction, abuse, and misuse with opioids, which can occur at any dosage or duration (5.2), reserve Morphine Sulfate Oral Solution for use in patients for whom alternative treatment options (e.g., non-opioid analgesics or opioid combination products): - Have not been tolerated or are not expected to be tolerated
- Have not provided adequate analgesia or are not expected to provide adequate analgesia Morphine Sulfate Oral Solution should not be used for an extended period of time unless the pain remains severe enough to require an opioid analgesic and for which alternative treatment options continue to be inadequate.
DOSAGE AND ADMINISTRATION
- Morphine Sulfate Oral Solution 20 mg/mL is only for opioid-tolerant adult patients . (2.1)
- Morphine Sulfate Oral Solution should be prescribed only by healthcare professionals who are knowledgeable about the use of opioids and how to mitigate the associated risks. (2.2)
- Use the lowest effective dosage for the shortest duration of time consistent with individual patient treatment goals. Reserve titration to higher doses of Morphine Sulfate Oral Solution for patients in whom lower doses are insufficiently effective and in whom the expected benefits of using a higher dose opioid clearly outweigh the substantial risks. (2.2, 5)
- Many acute pain conditions (e.g., the pain that occurs with a number of surgical procedures or acute musculoskeletal injuries) require no more than a few days of an opioid analgesic. Clinical guidelines on opioid prescribing for some acute pain conditions are available. (2.2)
- Initiate the dosing regimen for each patient individually, taking into account the patient's underlying cause and severity of pain, prior analgesic treatment and response, and risk factors for addiction, abuse, and misuse. (2.2, 5.2)
- Respiratory depression can occur at any time during opioid therapy, especially when initiating and following dosage increases with Morphine Sulfate Oral Solution. Consider this risk when selecting an initial dose and when making dose adjustments. (2.1, 5.3)
- Discuss availability of naloxone with the patient and caregiver and assess each patient's need for access to naloxone, both when initiating and renewing treatment with Morphine Sulfate Oral Solution. Consider prescribing naloxone based on the patient's risk factors for overdose. (2.3, 5.2, 5.3, 5.4)
- Adults : Initiate treatment with Morphine Sulfate Oral Solution 10 to 20 mg every 4 hours as needed for pain, and at the lowest dose necessary to achieve adequate analgesia. Titrate the dose based upon the individual patient's response to their initial dose of Morphine Sulfate Oral Solution. (2.4, 2.5)
- Pediatric Patients 2 Years of Age and Older : Initiate treatment with Morphine Oral Solution 2 mg/mL or 4 mg/mL at a dose of 0.15 mg/kg to 0.3 mg/kg every 4 hours as needed for pain, and at the lowest dose necessary to achieve adequate analgesia. Do not exceed 20 mg as an initial dose in pediatrics. See Full Prescribing Information for complete information on pediatric dosing. (2.3)
- Do not abruptly discontinue Morphine Sulfate Oral Solution in a physically dependent patient because rapid discontinuation of opioid analgesics has resulted in serious withdrawal symptoms, uncontrolled pain, and suicide. (2.6, 5.15)
DOSAGE FORMS AND STRENGTHS
Oral Solution:
- 10 mg per 5 mL (2 mg/mL)
- 20 mg per 5 mL (4 mg/mL)
- 100 mg per 5 mL (20 mg/mL) (only for opioid-tolerant adults) (3)
CONTRAINDICATIONS
- Significant respiratory depression. (4)
- Acute or severe bronchial asthma in an unmonitored setting or in absence of resuscitative equipment. (4)
- Concurrent use of monoamine oxidase inhibitors (MAOIs) or use of MAOIs within the last 14 days. (4)
- Known or suspected gastrointestinal obstruction, including paralytic ileus. (4)
- Hypersensitivity to morphine. (4)
WARNINGS AND PRECAUTIONS
- Opioid-Induced Hyperalgesia and Allodynia: Opioid-Induced Hyperalgesia (OIH) occurs when an opioid analgesic paradoxically causes an increase in pain, or an increase in sensitivity to pain. If OIH is suspected, carefully consider appropriately decreasing the dose of the current opioid analgesic or opioid rotation. (5.7)
- Life-Threatening Respiratory Depression in Patients with Chronic Pulmonary Disease or in Elderly, Cachectic, or Debilitated Patients: Regularly evaluate closely, particularly during initiation and titration. (5.8)
- Adrenal Insufficiency: If diagnosed, treat with physiologic replacement of corticosteroids, and wean patient off of the opioid. (5.10)
- Severe Hypotension: Regularly evaluate during dosage initiation and titration. Avoid use of Morphine Sulfate Oral Solution in patients with circulatory shock. (5.11)
- Risks of Use in Patients with Increased Intracranial Pressure, Brain Tumors, Head Injury, or Impaired Consciousness: Monitor for sedation and respiratory depression. Avoid use of Morphine Sulfate Oral Solution in patients with impaired consciousness or coma. (5.12)
ADVERSE REACTIONS
Most common adverse reactions on initiation of therapy are:
- Adults: constipation, nausea, somnolence, lightheadedness, dizziness, sedation, vomiting, sweating. (6)
- Pediatrics 2 years of age and older (≥5%): nausea, vomiting, constipation, decreased oxygen saturation, and flatulence. (6)
To report SUSPECTED ADVERSE REACTIONS, contact Precision Dose, Inc. at 1-800-397-9228 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
- Serotonergic Drugs: Concomitant use may result in serotonin syndrome. Discontinue Morphine Sulfate Oral Solution if serotonin syndrome is suspected. (7)
- Mixed Agonist/Antagonist and Partial Agonist Opioid Analgesics: Avoid use with Morphine Sulfate Oral Solution because they may reduce analgesic effect of Morphine Sulfate Oral Solution or precipitate withdrawal symptoms. (7)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 4/2024
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: SERIOUS AND LIFE-THREATENING RISKS FROM USE OF MORPHINE SULFATE ORAL SOLUTION
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Dosage and Administration Overview
2.2 Important Dosage and Administration Instructions
2.3 Patient Access to Naloxone for the Emergency Treatment of Opioid Overdose
2.4 Initial Dosage
2.5 Titration and Maintenance of Therapy
2.6 Safe Reduction or Discontinuation of Morphine Sulfate Oral Solution
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Risk of Accidental Overdose and Death due to Medication Errors
5.2 Addiction, Abuse, and Misuse
5.3 Life-Threatening Respiratory Depression
5.4 Risks from Concomitant Use with Benzodiazepines or Other CNS Depressants
5.5 Neonatal Opioid Withdrawal Syndrome
5.6 Opioid Analgesic Risk Evaluation and Mitigation Strategy (REMS)
5.7 Opioid-Induced Hyperalgesia and Allodynia
5.8 Life-Threatening Respiratory Depression in Patients with Chronic Pulmonary Disease or in Elderly, Cachectic, or Debilitated Patients
5.9 Interaction with Monoamine Oxidase Inhibitors
5.10 Adrenal Insufficiency
5.11 Severe Hypotension
5.12 Risks of Use in Patients with Increased Intracranial Pressure, Brain Tumors, Head Injury, or Impaired Consciousness
5.13 Risks of Use in Patients with Gastrointestinal Conditions
5.14 Increased Risk of Seizures in Patients with Seizure Disorders
5.15 Withdrawal
5.16 Risks of Driving and Operating Machinery
6 ADVERSE REACTIONS
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Hepatic Impairment
8.7 Renal Impairment
9 DRUG ABUSE AND DEPENDENCE
9.1 Controlled Substance
9.2 Abuse
9.3 Dependence
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: SERIOUS AND LIFE-THREATENING RISKS FROM USE OF MORPHINE SULFATE ORAL SOLUTION
Risk of Medication Errors
Ensure accuracy when prescribing, dispensing, and administering Morphine Sulfate Oral Solution. Dosing errors due to confusion between mg and mL, and other morphine sulfate oral solutions of different concentrations can result in accidental overdose and death [see Dosage and Administration (2.1), Warnings and Precautions (5.1)].Addiction, Abuse, and Misuse
Because the use of Morphine Sulfate Oral Solution exposes patients and other users to the risks of opioid addiction, abuse, and misuse, which can lead to overdose and death, assess each patient's risk prior to prescribing and reassess all patients regularly for the development of these behaviors and conditions [see Warnings and Precautions (5.2)].Life-Threatening Respiratory Depression
Serious, life-threatening, or fatal respiratory depression may occur with use of Morphine Sulfate Oral Solution, especially during initiation or following a dosage increase. To reduce the risk of respiratory depression, proper dosing and titration of Morphine Sulfate Oral Solution are essential [see Warnings and Precautions (5.3)].Accidental Ingestion
Accidental ingestion of even one dose of Morphine Sulfate Oral Solution, especially by children, can result in a fatal overdose of morphine [see Warnings and Precautions (5.3)].Risks From Concomitant Use With Benzodiazepines Or Other CNS Depressants
Concomitant use of opioids with benzodiazepines or other central nervous system (CNS) depressants, including alcohol, may result in profound sedation, respiratory depression, coma, and death. Reserve concomitant prescribing of Morphine Sulfate Oral Solution and benzodiazepines or other CNS depressants for use in patients for whom alternative treatment options are inadequate [see Warnings and Precautions (5.4), Drug Interactions (7)].Neonatal Opioid Withdrawal Syndrome (NOWS)
If opioid use is required for an extended period of time in a pregnant woman, advise the patient of the risk of NOWS, which may be life-threating if not recognized and treated. Ensure that management by neonatology experts will be available at delivery [see Warnings and Precautions (5.5)]Opioid Analgesic Risk Evaluation and Mitigation Strategy (REMS)
Healthcare providers are strongly encouraged to complete a REMS-compliant education program and to counsel patients and caregivers on serious risks, safe use, and the importance of reading the Medication Guide with each prescription [see Warnings and Precautions (5.6)]. -
1 INDICATIONS AND USAGE
Morphine Sulfate Oral Solution 2 mg/mL and 4 mg/mL is indicated for the management of:
- adults with acute and chronic pain severe enough to require an opioid analgesic and for which alternative treatments are inadequate.
- pediatric patients 2 years of age and older with acute pain severe enough to require an opioid analgesic and for which alternative treatments are inadequate.
Morphine Sulfate Oral Solution 20 mg/mL is indicated for the relief of acute and chronic pain in opioid-tolerant adult patients.
Limitations of Use: Because of the risks of addiction, abuse, and misuse with opioids, which can occur at any dosage or duration [see Warnings and Precautions (5.2)] , reserve Morphine Sulfate Oral Solution for use in patients for whom alternative treatment options (e.g., non-opioid analgesics or opioid combination products):
- Have not been tolerated or are not expected to be tolerated,
- Have not provided adequate analgesia or are not expected to provide adequate analgesia.
Morphine Sulfate Oral Solution should not be used for an extended period of time unless the pain remains severe enough to require an opioid analgesic and for which alternative treatment options continue to be inadequate.
-
2 DOSAGE AND ADMINISTRATION
2.1 Dosage and Administration Overview
Morphine Sulfate Oral Solution is available in three concentrations: 2 mg/mL, 4 mg/mL, and 20 mg/mL [see Dosage Forms and Strengths (3)].
- Morphine Sulfate Oral Solution 2 mg/mL and 4 mg/mL is indicated for use in adults and pediatric patients 2 years of age and older.
- Strongly advise patients and caregivers to always use a graduated oral syringe with metric units of measurement (i.e., mL) when administering Morphine Sulfate Oral Solution 2 mg/mL and 4 mg/mL to correctly measure the prescribed amount of medication.
- Morphine Sulfate Oral Solution 20 mg/mL is only indicated for use in opioid-tolerant adult patients who have already been receiving opioid therapy. This concentration is to be used only in adult patients who have already been titrated to a stable analgesic regimen using lower concentrations of morphine sulfate and who can benefit from use of a higher concentration (smaller volume) of oral solution.
- Adult patients considered to be opioid tolerant are those who are receiving, for one week or longer, at least 60 mg oral morphine per day, 25 mcg transdermal fentanyl per hour, 30 mg oral oxycodone per day, 8 mg oral hydromorphone per day, 25 mg oral oxymorphone per day, 60 mg oral hydrocodone per day, or an equianalgesic dose of another opioid.
- Ensure accuracy when prescribing, dispensing, and administering Morphine Sulfate Oral Solution to avoid dosing errors due to confusion between mg and mL, and with other morphine solutions of different concentrations, which could result in accidental overdose and death. Ensure the proper dose is communicated and dispensed.
2.2 Important Dosage and Administration Instructions
Ensure accuracy when prescribing, dispensing, and administering Morphine Sulfate Oral Solution to avoid dosing errors due to confusion between mg and mL, and with other morphine sulfate oral solutions of different concentrations, which could result in accidental overdose and death. Ensure the proper dose is communicated and dispensed.
- Morphine Sulfate Oral Solution should be prescribed only by healthcare professionals who are knowledgeable about the use of opioids and how to mitigate the associated risks.
- Use the lowest effective dosage for the shortest duration of time consistent with individual patient treatment goals [see Warnings and Precautions (5)]. Because the risk of overdose increases as opioid doses increase, reserve titration to higher doses of Morphine Sulfate Oral Solution for patients in whom lower doses are insufficiently effective and in whom the expected benefits of using a higher dose opioid clearly outweigh the substantial risks.
- Many acute pain conditions (e.g., the pain that occurs with a number of surgical procedures or acute musculoskeletal injuries) require no more than a few days of an opioid analgesic. Clinical guidelines on opioid prescribing for some acute pain conditions are available.
- There is variability in the opioid analgesic dose and duration needed to adequately manage pain due both to the cause of pain and to individual patient factors. Initiate the dosing regimen for each patient individually, taking into account the patient's underlying cause and severity of pain, prior analgesic treatment and response, and risk factors for addiction, abuse, and misuse [see Warnings and Precautions (5.1)].
- Respiratory depression can occur at any time during opioid therapy, especially when initiating and following dosage increases with Morphine Sulfate Oral Solution. Consider this risk when selecting an initial dose and when making dose adjustments [see Warnings and Precautions (5)].
- Initiate the dosing regimen for each patient individually, taking into account the patient's severity of pain, patient response, prior analgesic treatment experience, and risk factors for addiction, abuse, and misuse [see Warnings and Precautions (5.2)].
2.3 Patient Access to Naloxone for the Emergency Treatment of Opioid Overdose
Discuss the availability of naloxone for the emergency treatment of opioid overdose with the patient and caregiver and assess the potential need for access to naloxone, both when initiating and renewing treatment with Morphine Sulfate Oral Solution [see Warnings and Precautions (5.3)].
Inform patients and caregivers about the various ways to obtain naloxone as permitted by individual state naloxone dispensing and prescribing requirements or guidelines (e.g., by prescription, directly from a pharmacist, or as part of a community-based program).
Consider prescribing naloxone, based on the patient's risk factors for overdose, such as concomitant use of CNS depressants, a history of opioid use disorder, or prior opioid overdose. The presence of risk factors for overdose should not prevent the proper management of pain in any given patient [see Warnings and Precautions (5.2, 5.3, 5.4)].
Consider prescribing naloxone if the patient has household members (including children) or other close contacts at risk for accidental ingestion or overdose.
2.4 Initial Dosage
Initiating Treatment with Morphine Sulfate Oral Solution: Adults: Initiate treatment with Morphine Sulfate Oral Solution 2 mg/ mL and 4 mg/mL in adults in a dosing range of 10 mg to 20 mg every 4 hours as needed for pain, and at the lowest dose necessary to achieve adequate analgesia. Titrate the dose based upon the individual patient's response to their initial dose of Morphine Sulfate Oral Solution.
Do not initiate treatment with Morphine Sulfate Oral Solution 20 mg/mL) in adult patients who are opioid naïve or in pediatric patients. The recommended dosage to initiate treatment with Morphine Sulfate Oral Solution 20 mg/mL in opioid tolerant adults is 10 mg to 20 mg every 4 hours as needed for pain.
Pediatric Patients 2 Years of Age and Older: Only use Morphine Sulfate Oral Solution 2 mg/mL and 4 mg/mL in pediatric patients. Initiate treatment in pediatric patients with a dosing range of 0.15 mg/kg to 0.3 mg/kg every 4 hours as needed for pain, and at the lowest dose necessary to achieve adequate analgesia. Titrate the dose based upon the individual patient's response to their initial dose of Morphine Sulfate Oral Solution. Do not exceed 20 mg as an initial dose.
To ensure doses can be accurately measured, calculate the starting dose for pediatric patients by following the steps below:
- Multiply the patient's actual body weight by a value based on the recommended dosage range 0.15 mg/kg to 0.3 mg/kg.
- For example: 11.4 kg × 0.15 mg/kg = 1.71 mg
- Convert the calculated dose (mg) to volume (mL) based on the desired morphine sulfate concentration.
(Only use Morphine Sulfate Oral Solution 2 mg/mL or 4 mg/mL in pediatric patients)- 1.71 mg ÷ 2 mg/mL = 0.855 mL
- Round calculated volume (mL), if necessary.
- For volumes less than 1 mL, round to the nearest 0.1 mL
- For volumes greater than 1 mL, round to the nearest 0.2 mL
- Calculate the final dose (mg): Multiply the rounded dose volume from step 3 by the morphine sulfate concentration used in step 2.
- For example: 0.9 mL × 2 mg/mL = 1.8 mg
- Include both the calculated dose in mg and the calculated dose in volume on the prescription.
- For example: for the 11.4 kg patient used in this example, the calculated dose in mg (1.8 mg) and the calculated dose in volume (0.9 mL) would be included on the prescription. Ensure the concentration of the product to be dispensed is included on the prescription. In this example, the prescription would indicate the 2 mg/mL product be dispensed.
- Conversion from Parenteral Morphine to Morphine Sulfate Oral Solution: For conversion from parenteral morphine to
- Morphine Sulfate Oral Solution, anywhere from 3 to 6 mg of oral morphine sulfate may be required to provide pain relief equivalent to 1 mg of parenteral morphine.
- Conversion from Other Opioids to Morphine Sulfate Oral Solution: There is inter-patient variability in the potency of opioid drugs and opioid formulations. Therefore, a conservative approach is advised when determining the total daily dosage of Morphine Sulfate Oral Solution. It is safer to underestimate a patient's 24-hour Morphine Sulfate Oral Solution dosage than to overestimate the 24-hour Morphine Sulfate Oral Solution dosage and manage an adverse reaction due to overdose. Initiate treatment in adults a dosage range of 10 to 20 mg every 4 hours as needed for pain, and at the lowest dose necessary to achieve adequate analgesia. Titrate the dose based upon the individual patient's response to their initial dose of Morphine Sulfate Oral Solution.
- Conversion from Morphine Sulfate Oral Solution to Extended-Release Morphine: For a given dose, the same total amount of morphine sulfate is available from Morphine Sulfate Oral Solution and extended-release morphine formulations. The extended duration of release of morphine sulfate from extended-release formulations results in reduced maximum and increased minimum plasma morphine sulfate concentrations than with shorter acting morphine sulfate products. Conversion from Morphine Sulfate Oral Solution to the same total daily dose of an extended-release formulation could lead to excessive sedation at peak serum levels. Therefore, conversion to extended-release morphine formulations may lead to increased risk of excessive sedation and respiratory depression.
2.5 Titration and Maintenance of Therapy
Individually titrate Morphine Sulfate Oral Solution to a dose that provides adequate analgesia and minimizes adverse reactions. Continually reevaluate patients receiving Morphine Sulfate Oral Solution to assess the maintenance of pain control, signs and symptoms of opioid withdrawal, and other adverse reactions, as well as to reassess for the development of addiction, abuse, or misuse [see Warnings and Precautions (5.2, 5.15)]. Frequent communication is important among the prescriber, other members of the healthcare team, the patient, and the caregiver/family during periods of changing analgesic requirements, including initial titration.
If the level of pain increases after dosage stabilization, attempt to identify the source of increased pain before increasing the Morphine Sulfate Oral Solution dosage. If after increasing the dosage, unacceptable opioid-related adverse reactions are observed (including an increase in pain after a dosage increase), consider reducing the dosage [see Warnings and Precautions (5)]. Adjust the dosage to obtain an appropriate balance between management of pain and opioid-related adverse reactions.
2.6 Safe Reduction or Discontinuation of Morphine Sulfate Oral Solution
Do not abruptly discontinue Morphine Sulfate Oral Solution in patients who may be physically dependent on opioids. Rapid discontinuation of opioid analgesics in patients who are physically dependent on opioids has resulted in serious withdrawal symptoms, uncontrolled pain, and suicide. Rapid discontinuation has also been associated with attempts to find other sources of opioid analgesics, which may be confused with drug-seeking for abuse. Patients may also attempt to treat their pain or withdrawal symptoms with illicit opioids, such as heroin, and other substances.
When a decision has been made to decrease the dose or discontinue therapy in an opioid-dependent patient taking Morphine Sulfate Oral Solution, there are a variety of factors that should be considered, including the total daily dose of opioid (including Morphine Sulfate Oral Solution) the patient has been taking, the duration of treatment, the type of pain being treated, and the physical and psychological attributes of the patient. It is important to ensure ongoing care of the patient and to agree on an appropriate tapering schedule and follow-up plan so that patient and provider goals and expectations are clear and realistic. When opioid analgesics are being discontinued due to a suspected substance use disorder, evaluate and treat the patient, or refer for evaluation and treatment of the substance use disorder. Treatment should include evidence-based approaches, such as medication assisted treatment of opioid use disorder. Complex patients with co-morbid pain and substance use disorders may benefit from referral to a specialist.
There are no standard opioid tapering schedules that are suitable for all patients. Good clinical practice dictates a patientspecific plan to taper the dose of the opioid gradually. For patients on Morphine Sulfate Oral Solution who are physically opioiddependent, initiate the taper by a small enough increment (e.g., no greater than 10% to 25% of the total daily dose) to avoid withdrawal symptoms, and proceed with dose-lowering at an interval of every 2 to 4 weeks. Patients who have been taking opioids for briefer periods of time may tolerate a more rapid taper.
It may be necessary to provide the patient with lower dosage strengths to accomplish a successful taper. Reassess the patient frequently to manage pain and withdrawal symptoms, should they emerge. Common withdrawal symptoms include restlessness, lacrimation, rhinorrhea, yawning, perspiration, chills, myalgia, and mydriasis. Other signs and symptoms also may develop, including irritability, anxiety, backache, joint pain, weakness, abdominal cramps, insomnia, nausea, anorexia, vomiting, diarrhea, or increased blood pressure, respiratory rate, or heart rate. If withdrawal symptoms arise, it may be necessary to pause the taper for a period of time or raise the dose of the opioid analgesic to the previous dose, and then proceed with a slower taper. In addition, evaluate patients for any changes in mood, emergence of suicidal thoughts, or use of other substances.
When managing patients taking opioid analgesics, particularly those who have been treated for an extended period of time, and/or with high doses for chronic pain, ensure that a multimodal approach to pain management, including mental health support (if needed), is in place prior to initiating an opioid analgesic taper. A multimodal approach to pain management may optimize the treatment of chronic pain, as well as assist with the successful tapering of the opioid analgesic [see Warnings and Precautions (5.15), Drug Abuse and Dependence (9.3)].
- Morphine Sulfate Oral Solution 2 mg/mL and 4 mg/mL is indicated for use in adults and pediatric patients 2 years of age and older.
-
3 DOSAGE FORMS AND STRENGTHS
Morphine Sulfate Oral Solution:
- 10 mg per 5 mL (2 mg/mL): Each 1 mL of clear, blue-green oral solution contains 2 mg of morphine sulfate, USP (equivalent to 1.5 mg morphine).
- 20 mg per 5 mL (4 mg/mL): Each 1 mL of clear, blue-green oral solution contains 4 mg of morphine sulfate, USP (equivalent to 3 mg morphine).
- 100 mg per 5 mL (20 mg/mL) (only for opioid-tolerant adults ): Each 1 mL of clear, colorless or clear, pink oral solution contains 20 mg of morphine sulfate, USP (equivalent to 15 mg morphine).
-
4 CONTRAINDICATIONS
Morphine Sulfate Oral Solution is contraindicated in patients with:
- Significant respiratory depression [see Warnings and Precautions (5.3)].
- Acute or severe bronchial asthma in an unmonitored setting or in the absence of resuscitative equipment [see Warnings and Precautions (5.8)].
- Concurrent use of monoamine oxidase inhibitors (MAOIs) or use of MAOIs within the last 14 days [see Warnings and Precautions (5.9) and Drug Interactions (7)].
- Known or suspected gastrointestinal obstruction, including paralytic ileus [see Warnings and Precautions (5.13)].
- Hypersensitivity to morphine (e.g., anaphylaxis) [see Adverse Reactions (6)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Risk of Accidental Overdose and Death due to Medication Errors
Dosing errors can result in accidental overdose and death. Avoid dosing errors that may result from confusion between mg and mL and confusion with morphine sulfate oral solutions of different concentrations, when prescribing, dispensing, and administering Morphine Sulfate Oral Solution. Ensure that the dose is communicated clearly and dispensed accurately.
5.2 Addiction, Abuse, and Misuse
Morphine Sulfate Oral Solution contains morphine, a Schedule II controlled substance. As an opioid, Morphine Sulfate Oral Solution exposes users to the risks of addiction, abuse, and misuse [see Drug Abuse and Dependence (9)].
Although the risk of addiction in any individual is unknown, it can occur in patients appropriately prescribed morphine sulfate. Addiction can occur at recommended dosages and if the drug is misused or abused.
Assess each patient's risk for opioid addiction, abuse, or misuse prior to prescribing Morphine Sulfate Oral Solution, and reassess all patients receiving Morphine Sulfate Oral Solution for the development of these behaviors and conditions. Risks are increased in patients with a personal or family history of substance abuse (including drug or alcohol abuse or addiction) or mental illness (e.g., major depression). The potential for these risks should not, however, prevent the proper management of pain in any given patient. Patients at increased risk may be prescribed opioids such as Morphine Sulfate Oral Solution but use in such patients necessitates intensive counseling about the risks and proper use of Morphine Sulfate Oral Solution along with frequent reevaluation for signs of addiction, abuse, and misuse. Consider prescribing naloxone for the emergency treatment of opioid overdose [see Dosage and Administration (2.2) and Warnings and Precautions (5.3)].
Opioids are sought for nonmedical use and are subject to diversion from legitimate prescribed use. Consider these risks when prescribing or dispensing Morphine Sulfate Oral Solution. Strategies to reduce these risks include prescribing the drug in the smallest appropriate quantity and advising the patient on careful storage of the drug during the course of treatment and on the proper disposal of unused drug. Contact local state professional licensing board or state-controlled substances authority for information on how to prevent and detect abuse or diversion of this product.
5.3 Life-Threatening Respiratory Depression
Serious, life-threatening, or fatal respiratory depression has been reported with the use of opioids, even when used as recommended. Respiratory depression, if not immediately recognized and treated, may lead to respiratory arrest and death. Management of respiratory depression may include close observation, supportive measures, and use of opioid antagonists, depending on the patient's clinical status [see Overdosage (10)]. Carbon dioxide (CO2) retention from opioid-induced respiratory depression can exacerbate the sedating effects of opioids.
While serious, life-threatening, or fatal respiratory depression can occur at any time during the use of Morphine Sulfate Oral Solution, the risk is greatest during the initiation of therapy or following a dosage increase of Morphine Sulfate Oral Solution.
To reduce the risk of respiratory depression, proper dosing and titration of Morphine Sulfate Oral Solution are essential [see Dosage and Administration (2)]. Overestimating the Morphine Sulfate Oral Solution dosage when converting patients from another opioid product can result in a fatal overdose with the first dose.
Morphine Sulfate Oral Solution 20 mg/mL is for use only in opioid-tolerant adult patients. Administration of this formulation may cause fatal respiratory depression when administered to patients who are not tolerant to the respiratory depressant effects of opioids.
Accidental ingestion of even one dose of Morphine Sulfate Oral Solution, especially by children, can result in respiratory depression and death due to an overdose of morphine.
Educate patients and caregivers on how to recognize respiratory depression and emphasize the importance of calling 911 or getting emergency medical help right away in the event of a known or suspected overdose .
Opioids can cause sleep-related breathing disorders including central sleep apnea (CSA) and sleep-related hypoxemia.
Opioid use increases the risk of CSA in a dose-dependent fashion. In patients who present with CSA, consider decreasing the opioid dosage using best practices for opioid taper [see Dosage and Administration (2.6)].
Patient Access to Naloxone for the Emergency Treatment of Opioid Overdose: Discuss the availability of naloxone for the emergency treatment of opioid overdose with the patient and caregiver and assess the potential need for access to naloxone, both when initiating and renewing treatment with Morphine Sulfate Oral Solution. Inform patients and caregivers about the various ways to obtain naloxone as permitted by individual state naloxone dispensing and prescribing requirements or guidelines (e.g., by prescription, directly from a pharmacist, or as part of a community-based program). Educate patients and caregivers on how to recognize respiratory depression and emphasize the importance of calling 911 or getting emergency medical help, even if naloxone is administered .
Consider prescribing naloxone, based on the patient's risk factors for overdose, such as concomitant use of CNS depressants, a history of opioid use disorder, or prior opioid overdose. The presence of risk factors for overdose should not prevent the proper management of pain in any given patient. Also consider prescribing naloxone if the patient has household members (including children) or other close contacts at risk for accidental ingestion or overdose. If naloxone is prescribed, educate patients and caregivers on how to treat with naloxone [see Dosage and Administration (2.3), Warnings and Precautions (5.2, 5.4), Overdosage (10)].
5.4 Risks from Concomitant Use with Benzodiazepines or Other CNS Depressants
Profound sedation, respiratory depression, coma, and death may result from the concomitant use of Morphine Sulfate Oral Solution with benzodiazepines and/or other CNS depressants, including alcohol (e.g., non-benzodiazepine sedatives/ hypnotics, anxiolytics, tranquilizers, muscle relaxants, general anesthetics, antipsychotics, other opioids). Because of these risks, reserve concomitant prescribing of these drugs for use in patients for whom alternative treatment options are inadequate.
Observational studies have demonstrated that concomitant use of opioid analgesics and benzodiazepines increases the risk of drug-related mortality compared to use of opioid analgesics alone. Because of similar pharmacological properties, it is reasonable to expect similar risk with the concomitant use of other CNS depressant drugs with opioid analgesics [see Drug Interactions (7)].
If the decision is made to prescribe a benzodiazepine or other CNS depressant concomitantly with an opioid analgesic, prescribe the lowest effective dosages and minimum durations of concomitant use. In patients already receiving an opioid analgesic, prescribe a lower initial dose of the benzodiazepine or other CNS depressant than indicated in the absence of an opioid, and titrate based on clinical response. If an opioid analgesic is initiated in a patient already taking a benzodiazepine or other CNS depressant, prescribe a lower initial dose of the opioid analgesic, and titrate based on clinical response. Inform patients and caregivers of this potential interaction and educate them on the signs and symptoms of respiratory depression (including sedation). If concomitant use is warranted, consider prescribing naloxone for the emergency treatment of opioid overdose [see Dosage and Administration (2.3), Warnings and Precautions (5.3), Overdosage (10)].
Advise both patients and caregivers about the risks of respiratory depression and sedation when Morphine Sulfate Oral Solution is used with benzodiazepines or other CNS depressants (including alcohol and illicit drugs). Advise patients not to drive or operate heavy machinery until the effects of concomitant use of the benzodiazepine or other CNS depressant have been determined. Screen patients for risk of substance use disorders, including opioid abuse and misuse, and warn them of the risk for overdose and death associated with the use of additional CNS depressants including alcohol and illicit drugs [see Drug Interactions (7)].
5.5 Neonatal Opioid Withdrawal Syndrome
Use of Morphine Sulfate Oral Solution for an extended period of time during pregnancy can result in withdrawal in the neonate. Neonatal opioid withdrawal syndrome, unlike opioid withdrawal syndrome in adults, may be life-threatening if not recognized and treated, and requires management according to protocols developed by neonatology experts. Observe newborns for signs of neonatal opioid withdrawal syndrome and manage accordingly. Advise pregnant women using opioids for an extended period of time of the risk of neonatal opioid withdrawal syndrome and ensure that appropriate treatment will be available [see Use in Specific Populations (8.1)]
5.6 Opioid Analgesic Risk Evaluation and Mitigation Strategy (REMS)
To ensure that the benefits of opioid analgesics outweigh the risks of addiction, abuse, and misuse, the Food and Drug Administration (FDA) has required a Risk Evaluation and Mitigation Strategy (REMS) for these products. Under the requirements of the REMS, drug companies with approved opioid analgesic products must make REMS-compliant education programs available to healthcare providers. Healthcare providers are strongly encouraged to do all of the following:
- Complete a REMS-compliant education program offered by an accredited provider of continuing education (CE) or another education program that includes all the elements of the FDA Education Blueprint for Health Care Providers Involved in the Management or Support of Patients with Pain.
- Discuss the safe use, serious risks, and proper storage and disposal of opioid analgesics with patients and/or their caregivers every time these medicines are prescribed. The Patient Counseling Guide (PCG) can be obtained at this link: www.fda.gov/OpioidAnalgesicREMSPCG.
- Emphasize to patients and their caregivers the importance of reading the Medication Guide that they will receive from their pharmacist every time an opioid analgesic is dispensed to them.
- Consider using other tools to improve patient, household, and community safety, such as patient-prescriber agreements that reinforce patient-prescriber responsibilities.
To obtain further information on the opioid analgesic REMS and for a list of accredited REMS CME/CE, call 1-800-503-0784, or log on to www.opioidanalgesicrems.com. The FDA Blueprint can be found at www.fda.gov/OpioidAnalgesicREMSBlueprint.
5.7 Opioid-Induced Hyperalgesia and Allodynia
Opioid-Induced Hyperalgesia (OIH) occurs when an opioid analgesic paradoxically causes an increase in pain, or an increase in sensitivity to pain. This condition differs from tolerance, which is the need for increasing doses of opioids to maintain a defined effect [see Dependence (9.3)]. Symptoms of OIH include (but may not be limited to) increased levels of pain upon opioid dosage increase, decreased levels of pain upon opioid dosage decrease, or pain from ordinarily nonpainful stimuli (allodynia). These symptoms may suggest OIH only if there is no evidence of underlying disease progression, opioid tolerance, opioid withdrawal, or addictive behavior.
Cases of OIH have been reported, both with short-term and longer-term use of opioid analgesics. Though the mechanism of OIH is not fully understood, multiple biochemical pathways have been implicated. Medical literature suggests a strong biologic plausibility between opioid analgesics and OIH and allodynia. If a patient is suspected to be experiencing OIH, carefully consider appropriately decreasing the dose of the current opioid analgesic or opioid rotation (safely switching the patient to a different opioid moiety) [see Dosage and Administration (2.6), Warnings and Precautions (5.15)].
5.8 Life-Threatening Respiratory Depression in Patients with Chronic Pulmonary Disease or in Elderly, Cachectic, or Debilitated Patients
The use of Morphine Sulfate Oral Solution in patients with acute or severe bronchial asthma in an unmonitored setting or in the absence of resuscitative equipment is contraindicated.
Patients with Chronic Pulmonary Disease: Morphine Sulfate Oral Solution-treated patients with significant chronic obstructive pulmonary disease or cor pulmonale, and those with a substantially decreased respiratory reserve, hypoxia, hypercapnia, or pre-existing respiratory depression are at increased risk of decreased respiratory drive including apnea, even at recommended dosages of Morphine Sulfate Oral Solution [see Warnings and Precautions (5.3)].
Elderly, Cachectic, or Debilitated Patients: Life-threatening respiratory depression is more likely to occur in elderly, cachectic, or debilitated patients because they may have altered pharmacokinetics or altered clearance compared to younger, healthier patients [see Warnings and Precautions (5.3)].
Regularly evaluate patients, particularly when initiating and titrating Morphine Sulfate Oral Solution and when Morphine Sulfate Oral Solution is given concomitantly with other drugs that depress respiration [see Warnings and Precautions (5.3, 5.4), Drug Interactions (7)]. Alternatively, consider the use of non-opioid analgesics in these patients.
5.9 Interaction with Monoamine Oxidase Inhibitors
Monoamine oxidase inhibitors (MAOIs) may potentiate the effects of morphine, including respiratory depression, coma, and confusion. Morphine Sulfate Oral Solution should not be used in patients taking MAOIs or within 14 days of stopping such treatment.
5.10 Adrenal Insufficiency
Cases of adrenal insufficiency have been reported with opioid use, more often following greater than one month of use. Presentation of adrenal insufficiency may include non-specific symptoms and signs including nausea, vomiting, anorexia, fatigue, weakness, dizziness, and low blood pressure. If adrenal insufficiency is suspected, confirm the diagnosis with diagnostic testing as soon as possible. If adrenal insufficiency is diagnosed, treat with physiologic replacement doses of corticosteroids. Wean the patient off of the opioid to allow adrenal function to recover and continue corticosteroid treatment until adrenal function recovers. Other opioids may be tried as some cases reported use of a different opioid without recurrence of adrenal insufficiency. The information available does not identify any particular opioids as being more likely to be associated with adrenal insufficiency.
5.11 Severe Hypotension
Morphine Sulfate Oral Solution may cause severe hypotension including orthostatic hypotension and syncope in ambulatory patients. There is increased risk in patients whose ability to maintain blood pressure has already been compromised by a reduced blood volume or concurrent administration of certain CNS depressant drugs (e.g., phenothiazines or general anesthetics) [see Drug Interactions (7)]. Regularly evaluate these patients for signs of hypotension after initiating or titrating the dosage of Morphine Sulfate Oral Solution. In patients with circulatory shock, Morphine Sulfate Oral Solution may cause vasodilation that can further reduce cardiac output and blood pressure. Avoid the use of Morphine Sulfate Oral Solution in patients with circulatory shock.
5.12 Risks of Use in Patients with Increased Intracranial Pressure, Brain Tumors, Head Injury, or Impaired Consciousness
In patients who may be susceptible to the intracranial effects of CO2 retention (e.g., those with evidence of increased intracranial pressure or brain tumors), Morphine Sulfate Oral Solution may reduce respiratory drive, and the resultant CO2 retention can further increase intracranial pressure. Monitor such patients for signs of sedation and respiratory depression, particularly when initiating therapy with Morphine Sulfate Oral Solution. Opioids may also obscure the clinical course in a patient with a head injury. Avoid the use of Morphine Sulfate Oral Solution in patients with impaired consciousness or coma.
5.13 Risks of Use in Patients with Gastrointestinal Conditions
Morphine Sulfate Oral Solution is contraindicated in patients with known or suspected gastrointestinal obstruction, including paralytic ileus.
The morphine in Morphine Sulfate Oral Solution may cause spasm of the sphincter of Oddi. Opioids may cause increases in serum amylase. Regularly evaluate patients with biliary tract disease, including acute pancreatitis, for worsening symptoms.
5.14 Increased Risk of Seizures in Patients with Seizure Disorders
The morphine in Morphine Sulfate Oral Solution may increase the frequency of seizures in patients with seizure disorders and may increase the risk of seizures occurring in other clinical settings associated with seizures. Regularly evaluate patients with a history of seizure disorders for worsened seizure control during Morphine Sulfate Oral Solution therapy.
5.15 Withdrawal
Do not abruptly discontinue Morphine Sulfate Oral Solution in a patient physically dependent on opioids. When discontinuing Morphine Sulfate Oral Solution in a physically dependent patient, gradually taper the dosage. Rapid tapering of morphine in a patient physically dependent on opioids may lead to a withdrawal syndrome and return of pain [see Dosage and Administration (2.6) and Drug Abuse and Dependence (9.3)].
Additionally, avoid the use of mixed agonist/antagonist (e.g., pentazocine, nalbuphine, and butorphanol) or partial agonist (e.g., buprenorphine) analgesics in patients who are receiving a full opioid agonist analgesic, including Morphine Sulfate Oral Solution. In these patients, mixed agonist/antagonist and partial agonist analgesics may reduce the analgesic effect and/or precipitate withdrawal symptoms [see Drug Interactions (7)].
5.16 Risks of Driving and Operating Machinery
Morphine Sulfate Oral Solution may impair the mental or physical abilities needed to perform potentially hazardous activities such as driving a car or operating machinery. Warn patients not to drive or operate dangerous machinery unless they are tolerant to the effects of Morphine Sulfate Oral Solution and know how they will react to the medication.
-
6 ADVERSE REACTIONS
The following serious adverse reactions are described, or described in greater detail, in other sections:
- Addiction, Abuse, and Misuse [see Warnings and Precautions (5.2)]
- Life-Threatening Respiratory Depression [see Warnings and Precautions (5.3)]
- Interactions with Benzodiazepine or Other CNS Depressants [see Warnings and Precautions (5.4)]
- Neonatal Opioid Withdrawal Syndrome [see Warnings and Precautions (5.5)]
- Opioid-Induced Hyperalgesia and Allodynia [see Warnings and Precautions (5.7)]
- Adrenal Insufficiency [see Warnings and Precautions (5.10)]
- Severe Hypotension [see Warnings and Precautions (5.11)]
- Gastrointestinal Adverse Reactions [see Warnings and Precautions (5.13)]
- Seizures [see Warnings and Precautions (5.14)]
- Withdrawal [see Warnings and Precautions (5.15)]
The following adverse reactions associated with the use of morphine were identified in clinical studies or postmarketing reports. Because some of these reactions were reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Serious adverse reactions associated with morphine use included: respiratory depression, apnea, and to a lesser degree, circulatory depression, respiratory arrest, shock and cardiac arrest.
The common adverse reactions seen on initiation of therapy with morphine in adults were dose-dependent and were typical opioid-related adverse reactions. The most frequent of these included constipation, nausea, and somnolence. Other commonly observed adverse reactions included: lightheadedness, dizziness, sedation, vomiting, and sweating. The frequency of these events depended upon several factors including clinical setting, the patient's level of opioid tolerance, and host factors specific to the individual.
Other less frequently observed adverse reactions from opioid analgesics, including morphine sulfate included:
Body as a Whole: malaise, withdrawal syndrome
Cardiovascular System: bradycardia, hypertension, hypotension, palpitations, syncope, tachycardia
Digestive System: anorexia, biliary pain, dyspepsia, dysphagia, gastroenteritis, abnormal liver function tests, rectal disorder, thirst
Endocrine: hypogonadism
Hemic and Lymphatic System: anemia, thrombocytopenia
Metabolic and Nutritional Disorders: edema, weight loss
Musculoskeletal: skeletal muscle rigidity, decreased bone mineral density
Nervous System: abnormal dreams, abnormal gait, agitation, amnesia, anxiety, ataxia, confusion, convulsions, coma, delirium, depression, dry mouth, euphoria, hallucinations, lethargy, nervousness, abnormal thinking, tremor, vasodilation, vertigo, headache
Skin and Appendages: dry skin, urticaria, pruritus
Special Senses: amblyopia, eye pain, taste perversion
Urogenital System: abnormal ejaculation, dysuria, impotence, decreased libido, oliguria, urinary retention or hesitancy, antidiuretic effect, amenorrhea
Serotonin Syndrome: Cases of serotonin syndrome, a potentially life-threatening condition, have been reported during concomitant use of opioids with serotonergic drugs.
Adrenal Insufficiency: Cases of adrenal insufficiency have been reported with opioid use, more often following greater than one month of use.
Anaphylaxis: Anaphylaxis has been reported with ingredients contained in Morphine Sulfate Oral Solution.
Androgen Deficiency: Cases of androgen deficiency have occurred with use of opioids for an extended period of time [see Clinical Pharmacology (12.2)].
Hyperalgesia and Allodynia: Cases of hyperalgesia and allodynia have been reported with opioid therapy of any duration [see Warnings and Precautions (5.7)].
Hypoglycemia: Cases of hypoglycemia have been reported in patients taking opioids. Most reports were in patients with at least one predisposing risk factor (e.g., diabetes).
Clinical Trial Experience in Pediatric Patients 2 Years of Age and Older: The safety of morphine sulfate was evaluated in 81 pediatric patients 2 through 17 years of age with acute pain [see Use in Specific Populations (8.4)]. The safety profile in pediatric patients is similar to adults. The most common adverse reactions reported on initiation of therapy in at least 5% of patients across all age groups were: nausea (17%), vomiting (10%), constipation (6%), decreased oxygen saturation (5%), and flatulence (5%).
-
7 DRUG INTERACTIONS
Table 1 includes clinically significant drug interactions with Morphine Sulfate Oral Solution.
Table 1: Clinically Significant Drug Interactions with Morphine Sulfate Oral Solution Benzodiazepines and Other Central Nervous System (CNS) Depressants Clinical Impact: Due to additive pharmacologic effect, the concomitant use of benzodiazepines or other CNS depressants, including alcohol, can increase the risk of hypotension, respiratory depression, profound sedation, coma, and death [see Warnings and Precautions (5.4)]. Intervention: Reserve concomitant prescribing of these drugs for use in patients for whom alternative treatment options are inadequate. Limit dosages and durations to the minimum required. Inform patients and caregivers of this potential interaction and educate them on the signs and symptoms of respiratory depression (including sedation). If concomitant use is warranted, consider prescribing naloxone for the emergency treatment of opioid overdose [see Dosage and Administration (2.3) and Warnings and Precautions (5.2, 5.3, 5.4)]. Examples: Benzodiazepines and other sedatives/hypnotics, anxiolytics, tranquilizers, muscle relaxants, general anesthetics, antipsychotics, other opioids, alcohol. Serotonergic Drugs Clinical Impact: The concomitant use of opioids with other drugs that affect the serotonergic neurotransmitter system has resulted in serotonin syndrome. Intervention: If concomitant use is warranted, frequently evaluate the patient, particularly during treatment initiation and dose adjustment. Discontinue Morphine Sulfate Oral Solution if serotonin syndrome is suspected. Examples: Selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), triptans, 5-HT3 receptor antagonists, drugs that affect the serotonin neurotransmitter system (e.g., mirtazapine, trazodone, tramadol), certain muscle relaxants (i.e., cyclobenzaprine, metaxalone), monoamine oxidase (MAO) inhibitors (those intended to treat psychiatric disorders and also others, such as linezolid and intravenous methylene blue). Monoamine Oxidase Inhibitors (MAOIs) Clinical Impact: MAOI interactions with opioids may manifest as serotonin syndrome or opioid toxicity (e.g., respiratory depression, coma) [see Warnings and Precautions (5.3, 5.9)]. Intervention: Do not use Morphine Sulfate Oral Solution in patients taking MAOIs or within 14 days of stopping such treatment. Examples: Phenelzine, tranylcypromine, linezolid. Mixed Agonist/Antagonist and Partial Agonist Opioid Analgesics Clinical Impact: May reduce the analgesic effect of Morphine Sulfate Oral Solution and/or precipitate withdrawal symptoms. Intervention: Avoid concomitant use. Examples: Butorphanol, nalbuphine, pentazocine, buprenorphine. Muscle Relaxants Clinical Impact: Morphine may enhance the neuromuscular blocking action of skeletal muscle relaxants and produce an increased degree of respiratory depression. Intervention: Because respiratory depression may be greater than otherwise expected decrease the dosage of Morphine Sulfate Oral Solution and/or the muscle relaxant as necessary. Due to the risk of respiratory depression with concomitant use of skeletal muscle relaxants and opioids, consider prescribing naloxone for the emergency treatment of opioid overdose [see Dosage and Administration (2.3) and Warnings and Precautions (5.3, 5.4)]. Examples: Cyclobenzaprine, metaxalone. Cimetidine Clinical Impact: The concomitant use of morphine and cimetidine has been reported to precipitate apnea, confusion, and muscle twitching in an isolated report. Intervention: Evaluate patients for increased respiratory and CNS depression when Morphine Sulfate Oral Solution is used concomitantly with cimetidine. Diuretics Clinical Impact: Opioids can reduce the efficacy of diuretics by inducing the release of antidiuretic hormone. Intervention: Evaluate patients for signs of diminished diuresis and/or effects on blood pressure and increase the dosage of the diuretic as needed. Anticholinergic Drugs Clinical Impact: The concomitant use of anticholinergic drugs may increase risk of urinary retention and/or severe constipation, which may lead to paralytic ileus. Intervention: Evaluate patients for signs of urinary retention or reduced gastric motility when Morphine Sulfate Oral Solution is used concomitantly with anticholinergic drugs. P-Glycoprotein (P-gp) Inhibitors Clinical Impact: The concomitant use of P-gp inhibitors can increase the exposure to morphine by two-fold and can increase the risk of hypotension, respiratory depression, profound sedation, coma, and death. Intervention: Evaluate patients for signs of respiratory depression that may be greater than otherwise expected and decrease the dosage of Morphine Sulfate Oral Solution and/or the P-gp inhibitor as necessary. Examples: Quinidine, verapamil -
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary: Use of opioid analgesics for an extended period of time during pregnancy can cause neonatal opioid withdrawal syndrome [see Warnings and Precautions (5.5)]. There are no available data with Morphine Sulfate Oral Solution in pregnant women to inform a drug-associated risk for major birth defects and miscarriage. Published studies with morphine use during pregnancy have not reported a clear association with morphine and major birth defects (see Human Data). In published animal reproduction studies, morphine administered subcutaneously during the early gestational period produced neural tube defects (i.e., exencephaly and cranioschisis) at 5 and 16 times the human daily dose of 60 mg based on body surface area (HDD) in hamsters and mice, respectively, lower fetal body weight and increased incidence of abortion at 0.4 times the HDD in the rabbit, growth retardation at 6 times the HDD in the rat, and axial skeletal fusion and cryptorchidism at 16 times the HDD in the mouse. Administration of morphine sulfate to pregnant rats during organogenesis and through lactation resulted in cyanosis, hypothermia, decreased brain weights, pup mortality, decreased pup body weights, and adverse effects on reproductive tissues at 3 to 4 times the HDD; and long-term neurochemical changes in the brain of offspring which correlate with altered behavioral responses that persist through adulthood at exposures comparable to and less than the HDD (see Animal Data). Based on animal data, advise pregnant women of the potential risk to a fetus.
The background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Clinical Considerations: Fetal/Neonatal Adverse Reactions: Use of opioid analgesics for an extended period of time during pregnancy for medical or nonmedical purposes can result in physical dependence in the neonate and neonatal opioid withdrawal syndrome shortly after birth.
Neonatal opioid withdrawal syndrome presents as irritability, hyperactivity and abnormal sleep pattern, high pitched cry, tremor, vomiting, diarrhea, and failure to gain weight. The onset, duration, and severity of neonatal opioid withdrawal syndrome vary based on the specific opioid used, duration of use, timing and amount of last maternal use, and rate of elimination of the drug by the newborn. Observe newborns for symptoms of neonatal opioid withdrawal syndrome and manage accordingly [see Warnings and Precautions (5.5)].
Labor or Delivery: Opioids cross the placenta and may produce respiratory depression and psycho-physiologic effects in neonates. An opioid antagonist, such as naloxone, must be available for reversal of opioid-induced respiratory depression in the neonate. Morphine Sulfate Oral Solution is not recommended for use in pregnant women during or immediately prior to labor, when other analgesic techniques are more appropriate. Opioid analgesics, including Morphine Sulfate Oral Solution, can prolong labor through actions which temporarily reduce the strength, duration, and frequency of uterine contractions. However, this effect is not consistent and may be offset by an increased rate of cervical dilation, which tends to shorten labor. Monitor neonates exposed to opioid analgesics during labor for signs of excess sedation and respiratory depression.
Data: Human Data: The results from a population-based prospective cohort, including 70 women exposed to morphine during the first trimester of pregnancy and 448 women exposed to morphine at any time during pregnancy, indicate no increased risk for congenital malformations. However, these studies cannot definitely establish the absence of any risk because of methodological limitations, including small sample size and non-randomized study design.
Animal Data: Formal reproductive and developmental toxicology studies for morphine have not been conducted. Exposure margins for the following published study reports are based on human daily dose of 60 mg morphine using a body surface area comparison (HDD). Neural tube defects (exencephaly and cranioschisis) were noted following subcutaneous administration of morphine sulfate (35 to 322 mg/kg) on Gestation Day 8 to pregnant hamsters (4.7 to 43.5 times the HDD). A no adverse effect level was not defined in this study and the findings cannot be clearly attributed to maternal toxicity. Neural tube defects (exencephaly), axial skeletal fusions, and cryptorchidism were reported following a single subcutaneous (SC) injection of morphine sulfate to pregnant mice (100 to 500 mg/kg) on Gestation Day 8 or 9 at 200 mg/kg or greater (16 times the HDD) and fetal resorption at 400 mg/kg or higher (32 times the HDD). No adverse effects were noted following 100 mg/kg morphine in this model (8 times the HDD). In one study, following continuous subcutaneous infusion of doses greater than or equal to 2.72 mg/kg to mice (0.2 times the HDD), exencephaly, hydronephrosis, intestinal hemorrhage, split supraoccipital, malformed sternebrae, and malformed xiphoid were noted. The effects were reduced with increasing daily dose; possibly due to rapid induction of tolerance under these infusion conditions. The clinical significance of this report is not clear.
Decreased fetal weights were observed in pregnant rats treated with 20 mg/kg/day morphine sulfate (3.2 times the HDD) from Gestation Day 7 to 9. There was no evidence of malformations despite maternal toxicity (10% mortality). In a second rat study, decreased fetal weight and increased incidences of growth retardation were noted at 35 mg/kg/day (5.7 times the HDD) and there was a reduced number of fetuses at 70 mg/kg/day (11.4 times the HDD) when pregnant rats were treated with 10, 35, or 70 mg/kg/day morphine sulfate via continuous infusion from Gestation Day 5 to 20. There was no evidence of fetal malformations or maternal toxicity.
An increased incidence of abortion was noted in a study in which pregnant rabbits were treated with 2.5 (0.8 times the HDD) to 10 mg/kg morphine sulfate via subcutaneous injection from Gestation Day 6 to 10. In a second study, decreased fetal body weights were reported following treatment of pregnant rabbits with increasing doses of morphine (10 to 50 mg/kg/day) during the pre-mating period and 50 mg/kg/day (16 times the HDD) throughout the gestation period. No overt malformations were reported in either publication; although only limited endpoints were evaluated.
In published studies in rats, exposure to morphine during gestation and/or lactation periods is associated with: decreased pup viability at 12.5 mg/kg/day or greater (2 times the HDD); decreased pup body weights at 15 mg/kg/day or greater (2.4 times the HDD); decreased litter size, decreased absolute brain and cerebellar weights, cyanosis, and hypothermia at 20 mg/kg/day (3.2 times the HDD); alteration of behavioral responses (play, social-interaction) at 1 mg/kg/day or greater (0.2 times the HDD); alteration of maternal behaviors (e.g., decreased nursing and pup retrievals) in mice at 1 mg/kg or higher (0.08 times the HDD) and rats at 1.5 mg/kg/day or higher (0.2 times the HDD); and a host of behavioral abnormalities in the offspring of rats, including altered responsiveness to opioids at 4 mg/kg/day (0.7 times the HDD) or greater.
Fetal and/or postnatal exposure to morphine in mice and rats has been shown to result in morphological changes in fetal and neonatal brain and neuronal cell loss, alteration of a number of neurotransmitter and neuromodulator systems, including opioid and non-opioid systems, and impairment in various learning and memory tests that appear to persist into adulthood. These studies were conducted with morphine treatment usually in the range of 4 to 20 mg/kg/day (0.7 to 3.2 times the HDD).
Additionally, delayed sexual maturation and decreased sexual behaviors in female offspring at 20 mg/kg/day (3.2 times the HDD), and decreased plasma and testicular levels of luteinizing hormone and testosterone, decreased testes weights, seminiferous tubule shrinkage, germinal cell aplasia, and decreased spermatogenesis in male offspring were also observed at 20 mg/kg/day (3.2 times the HDD). Decreased litter size and viability were observed in the offspring of male rats that were intraperitoneally administered morphine sulfate for 1 day prior to mating at 25 mg/kg/day (4.1 times the HDD) and mated to untreated females. Decreased viability and body weight and/or movement deficits in both first- and second-generation offspring were reported when male mice were treated for 5 days with escalating doses of 120 to 240 mg/kg/day morphine sulfate (9.7 to 19.5 times the HDD) or when female mice treated with escalating doses of 60 to 240 mg/kg/day (4.9 to 19.5 times the HDD) followed by a 5-day treatment-free recovery period prior to mating. Similar multigenerational findings were also seen in female rats pre-gestationally treated with escalating doses of 10 to 22 mg/kg/day morphine (1.6 to 3.6 times the HDD).
8.2 Lactation
Risk Summary: Morphine is present in breast milk. Published lactation studies report variable concentrations of morphine in breast milk with administration of immediate-release morphine to nursing mothers in the early postpartum period with a milk-to-plasma morphine AUC ratio of 2.5:1 measured in one lactation study. However, there is insufficient information to determine the effects of morphine on the breastfed infant and the effects of morphine on milk production.
Lactation studies have not been conducted with Morphine Sulfate Oral Solution and no information is available on the effects of the drug on the breastfed infant or the effects of the drug on milk production.
The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for Morphine Sulfate Oral Solution and any potential adverse effects on the breastfed infant from Morphine Sulfate Oral Solution or from the underlying maternal condition.
8.3 Females and Males of Reproductive Potential
Infertility: Use of opioids for an extended period of time may cause reduced fertility in females and males of reproductive potential. It is not known whether these effects on fertility are reversible [see Adverse Reactions (6) and Clinical Pharmacology (12.2)]. In published animal studies, morphine administration adversely effected fertility and reproductive endpoints in male rats and prolonged estrus cycle in female rats [see Nonclinical Toxicology (13)].
8.4 Pediatric Use
The safety and effectiveness of Morphine Sulfate Oral Solution (2 mg/mL and 4 mg/mL) have been established for the management of pediatric patients 2 to 17 years of age with acute pain severe enough to require an opioid analgesic when alternative treatments are inadequate. Use of Morphine Sulfate Oral Solution in this age group is supported by clinical evidence in adults and supportive data from an open-label, safety and pharmacokinetic study in pediatric patients 2 through 17 years of age with post-operative acute pain. Patients were excluded if they had used opioids for more than 7 days within the previous 30 days prior to surgery or had received opioids in any form in the previous 7 days prior to surgery. Initial dosing was approximately 0.15 mg/kg to 0.3 mg/kg. Pharmacokinetic modeling and simulation indicate that an initial dose of 0.3 mg/kg in pediatric patients 2 years of age and older is expected to produce a maximum systemic exposure (Cmax) similar to that achieved after single dose administration of 10 mg Morphine Sulfate Oral Solution to adults [see Clinical Pharmacology (12.3)]. Safety data were available in 81 patients who received single and multiple doses (63 patients aged 2 to 17 years received Morphine Sulfate Oral Solution; 18 patients aged 12 to 17 years received Morphine Sulfate Tablets). The median duration of treatment was 20 hours (range 4 hours to 36 hours). Opioid and non-opioid rescue analgesics were allowed. The safety profile in pediatric patients consisted primarily of opioidrelated adverse reactions and is similar to that observed in adults [see Adverse Reactions (6)].
The safety and effectiveness of Morphine Sulfate Oral Solution (2 mg/mL and 4 mg/mL) have not been established for the management of pediatric patients 2 to 17 years of age with chronic pain severe enough to require an opioid analgesic when alternative treatments are inadequate.
The safety and effectiveness of Morphine Sulfate Oral Solution (2 mg/mL and 4 mg/mL) have not been established in pediatric patients less than 2 years of age. The safety and effectiveness of Morphine Sulfate Oral Solution 20 mg/mL have not been established in pediatric patients.
8.5 Geriatric Use
Elderly patients (aged 65 years or older) may have increased sensitivity to morphine. In general, use caution when selecting a dose for an elderly patient, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function and of concomitant disease or other drug therapy. Respiratory depression is the chief risk for elderly patients treated with opioids and has occurred after large initial doses were administered to patients who were not opioid-tolerant or when opioids were co-administered with other agents that depress respiration. Titrate the dosage of Morphine Sulfate Oral Solution slowly in geriatric patients and frequently reevaluate the patient for signs of central nervous system and respiratory depression [see Warnings and Precautions (5.8)].
Morphine is known to be substantially excreted by the kidney, and the risk of adverse reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to regularly evaluate renal function.
8.6 Hepatic Impairment
Morphine pharmacokinetics have been reported to be significantly altered in patients with cirrhosis. Start these patients with a lower than usual dosage of Morphine Sulfate Oral Solution and titrate slowly while regularly evaluating for signs of respiratory depression, sedation, and hypotension [see Clinical Pharmacology (12.3)].
8.7 Renal Impairment
Morphine pharmacokinetics are altered in patients with renal failure. Start these patients with a lower than usual dosage of Morphine Sulfate Oral Solution and titrate slowly while regularly evaluating for signs of respiratory depression, sedation, and hypotension [see Clinical Pharmacology (12.3)].
-
9 DRUG ABUSE AND DEPENDENCE
9.1 Controlled Substance
Morphine Sulfate Oral Solution contains morphine, a Schedule II controlled substance.
9.2 Abuse
Morphine Sulfate Oral Solution contains morphine, a substance with a high potential for misuse and abuse, which can lead to the development of substance use disorder, including addiction [see Warnings and Precautions (5.2)].
Misuse is the intentional use, for therapeutic purposes, of a drug by an individual in a way other than prescribed by a healthcare provider or for whom it was not prescribed.
Abuse is the intentional, non-therapeutic use of a drug, even once, for its desirable psychological or physiological effects.
Drug addiction is a cluster of behavioral, cognitive, and physiological phenomena that may include a strong desire to take the drug, difficulties in controlling drug use (e.g., continuing drug use despite harmful consequences, giving a higher priority to drug use than other activities and obligations), and possible tolerance or physical dependence.
Misuse and abuse of Morphine Sulfate Oral Solution increases risk of overdose, which may lead to central nervous system and respiratory depression, hypotension, seizures, and death. The risk is increased with concurrent abuse of Morphine Sulfate Oral Solution with alcohol and/or other CNS depressants. Abuse of and addiction to opioids in some individuals may not be accompanied by concurrent tolerance and symptoms of physical dependence. In addition, abuse of opioids can occur in the absence of addiction.
All patients treated with opioids require careful and frequent reevaluation for signs of misuse, abuse, and addiction, because use of opioid analgesic products carries the risk of addiction even under appropriate medical use.
Patients at high risk of Morphine Sulfate Oral Solution abuse include those with a history of prolonged use of any opioids, including products containing morphine, those with a history of drug or alcohol abuse, or those who use Morphine Sulfate Oral Solution in combination with other abused drugs.
"Drug-seeking" behavior is very common in persons with substance use disorders. Drug-seeking tactics include emergency calls or visits near the end of office hours, refusal to undergo appropriate examination, testing, or referral, repeated "loss" of prescriptions, tampering with prescriptions, and reluctance to provide prior medical records or contact information for other treating healthcare provider(s). "Doctor shopping" (visiting multiple prescribers to obtain additional prescriptions) is common among people who abuse drugs and people with substance use disorder. Preoccupation with achieving adequate pain relief can be appropriate behavior in a patient with inadequate pain control.
Morphine Sulfate Oral Solution, like other opioids, can be diverted for nonmedical use into illicit channels of distribution. Careful record-keeping of prescribing information, including quantity, frequency, and renewal requests, as required by state and federal law, is strongly advised.
Proper assessment of the patient, proper prescribing practices, periodic reevaluation of therapy, and proper dispensing and storage are appropriate measures that help to limit abuse of opioid drugs.
Risks Specific to Abuse of Morphine Sulfate Oral Solution: Abuse of Morphine Sulfate Oral Solution poses a risk of overdose and death. The risk is increased with concurrent use of Morphine Sulfate Oral Solution with alcohol and/or other CNS depressants.
Morphine Sulfate Oral Solution is approved for oral use only.
Parenteral drug abuse is commonly associated with transmission of infectious diseases such as hepatitis and HIV.
9.3 Dependence
Both tolerance and physical dependence can develop during chronic opioid therapy.
Tolerance is a physiological state characterized by a reduced response to a drug after repeated administration (i.e., a higher dose of a drug is required to produce the same effect that was once obtained at a lower dose).
Physical dependence is a state that develops as a result of a physiological adaptation in response to repeated drug use, manifested by withdrawal signs and symptoms after abrupt discontinuation or a significant dose reduction of a drug.
Withdrawal may be precipitated through the administration of drugs with opioid antagonist activity (e.g., naloxone), mixed agonist/antagonist analgesics (e.g., pentazocine, butorphanol, nalbuphine), or partial agonists (e.g., buprenorphine). Physical dependence may not occur to a clinically significant degree until after several days to weeks of continued use.
Do not abruptly discontinue Morphine Sulfate Oral Solution in a patient physically dependent on opioids. Rapid tapering of Morphine Sulfate Oral Solution in a patient physically dependent on opioids may lead to serious withdrawal symptoms, uncontrolled pain, and suicide. Rapid discontinuation has also been associated with attempts to find other sources of opioid analgesics, which may be confused with drug-seeking for abuse.
When discontinuing Morphine Sulfate Oral Solution, gradually taper the dosage using a patient-specific plan that considers the following: the dose of Morphine Sulfate Oral Solution the patient has been taking, the duration of treatment, and the physical and psychological attributes of the patient. To improve the likelihood of a successful taper and minimize withdrawal symptoms, it is important that the opioid tapering schedule is agreed upon by the patient. In patients taking opioids for a long duration at high doses, ensure that a multimodal approach to pain management, including mental health support (if needed), is in place prior to initiating an opioid analgesic taper [see Dosage and Administration (2.6) and Warnings and Precautions (5.15)].
Infants born to mothers physically dependent on opioids will also be physically dependent and may exhibit respiratory difficulties and withdrawal signs [see Use in Specific Populations (8.1)].
-
10 OVERDOSAGE
Clinical Presentation: Acute overdose with morphine can be manifested by respiratory depression, somnolence progressing to stupor or coma, skeletal muscle flaccidity, cold and clammy skin, constricted pupils, and, in some cases, pulmonary edema, bradycardia, hypotension, hypoglycemia, partial or complete airway obstruction, atypical snoring, and death. Marked mydriasis rather than miosis may be seen with hypoxia in overdose situations [see Clinical Pharmacology (12.2)].
Treatment of Overdose: In case of overdose, priorities are the reestablishment of a patent and protected airway and institution of assisted or controlled ventilation, if needed. Employ other supportive measures (including oxygen and vasopressors) in the management of circulatory shock and pulmonary edema as indicated. Cardiac arrest or arrhythmias will require advanced life-support measures.
Opioid antagonists, such as naloxone, are specific antidotes to respiratory depression resulting from opioid overdose. For clinically significant respiratory or circulatory depression secondary to opioid overdose, administer an opioid antagonist.
Because the duration of opioid reversal is expected to be less than the duration of action of morphine in Morphine Sulfate Oral Solution, carefully monitor the patient until spontaneous respiration is reliably re-established. If the response to an opioid antagonist is suboptimal or only brief in nature, administer additional antagonist as directed by the product's prescribing information.
In an individual physically dependent on opioids, administration of the recommended usual dosage of the antagonist will precipitate an acute withdrawal syndrome. The severity of the withdrawal symptoms experienced will depend on the degree of physical dependence and the dose of the antagonist administered. If a decision is made to treat serious respiratory depression in the physically dependent patient, administration of the antagonist should be initiated with care and by titration with smaller than usual doses of the antagonist.
-
11 DESCRIPTION
Morphine Sulfate Oral Solution is an opioid agonist, available in the following concentrations for oral administration:
- 10 mg per 5 mL (2 mg/mL): Each 1 mL of oral solution contains 2 mg of morphine sulfate, USP (equivalent to 1.5 mg morphine).
- 20 mg per 5 mL (4 mg/mL): Each 1 mL of oral solution contains 4 mg of morphine sulfate, USP (equivalent to 3 mg morphine).
- 100 mg per 5 mL (20 mg/mL): Each 1 mL of oral solution contains 20 mg of morphine sulfate, USP (equivalent to 15 mg morphine).
The chemical name is 7,8-didehydro-4,5 alpha-epoxy-17 methyl-morphinan-3,6 alpha-diol sulfate (2:1) (salt) pentahydrate. The molecular weight is 758.83. Its molecular formula is (C17H21NO3)2∙H2SO4∙5H2O, and it has the following chemical structure.
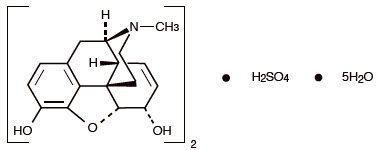
Morphine sulfate, USP is a white to off-white crystalline powder or a fine white to light yellow powder. It is soluble in water and slightly soluble in alcohol, but is practically insoluble in chloroform or ether. The octanol:water partition coefficient of morphine is 1.42 at physiologic pH and the pKa is 7.9 for the tertiary nitrogen (the majority is ionized at pH 7.4).
For the 10 mg per 5 mL (2 mg/mL) concentration: Each 5 mL of oral solution contains 10 mg of morphine sulfate, USP and the following inactive ingredients: citric acid anhydrous, disodium edetate, FD&C Green No. 3 (fast green), glycerin, sodium benzoate, sorbitol and purified water.
For the 20 mg per 5 mL (4 mg/mL) concentration: Each 5 mL of oral solution contains 20 mg of morphine sulfate, USP and the following inactive ingredients: citric acid anhydrous, disodium edetate, FD&C Green No. 3 (fast green), glycerin, methylparaben, propylparaben, sodium benzoate, sorbitol and purified water.
For the 100 mg per 5 mL (20 mg/mL) concentration (only for opioid-tolerant adults): Each 5 mL of oral solution contains 100 mg of morphine sulfate, USP and the following inactive ingredients: citric acid anhydrous, disodium edetate, glycerin, sodium benzoate, sorbitol and purified water. Additionally, the tinted solution contains D & C Red No. 33 and sucralose.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Morphine is a full opioid agonist and is relatively selective for the mu-opioid receptor, although it can bind to other opioid receptors at higher doses. The principal therapeutic action of morphine is analgesia. Like all full opioid agonists, there is no ceiling effect for analgesia with morphine. Clinically, dosage is titrated to provide adequate analgesia and may be limited by adverse reactions, including respiratory and CNS depression.
The precise mechanism of the analgesic action is unknown. However, specific CNS opioid receptors for endogenous compounds with opioid-like activity have been identified throughout the brain and spinal cord and are thought to play a role in the analgesic effects of this drug.
12.2 Pharmacodynamics
Effects on the Central Nervous System: Morphine produces respiratory depression by direct action on brain stem respiratory centers. The respiratory depression involves a reduction in the responsiveness of the brain stem respiratory centers to both increases in carbon dioxide tension and electrical stimulation.
Morphine causes miosis, even in total darkness. Pinpoint pupils are a sign of opioid overdose but are not pathognomonic (e.g., pontine lesions of hemorrhagic or ischemic origins may produce similar findings). Marked mydriasis rather than miosis may be seen due to hypoxia in overdose situations.
Effects on the Gastrointestinal Tract and Other Smooth Muscle: Morphine causes a reduction in motility associated with an increase in smooth muscle tone in the antrum of the stomach and duodenum. Digestion of food in the small intestine is delayed and propulsive contractions are decreased. Propulsive peristaltic waves in the colon are decreased, while tone may be increased to the point of spasm, resulting in constipation. Other opioid-induced effects may include a reduction in biliary and pancreatic secretions, spasm of sphincter of Oddi, and transient elevations in serum amylase.
Effects on the Cardiovascular System: Morphine produces peripheral vasodilation which may result in orthostatic hypotension or syncope. Manifestations of histamine release and/or peripheral vasodilation may include pruritus, flushing, red eyes, sweating, and/or orthostatic hypotension.
Effects on the Endocrine System: Opioids inhibit the secretion of adrenocorticotropic hormone (ACTH), cortisol, and luteinizing hormone (LH) in humans [see Adverse Reactions (6)]. They also stimulate prolactin, growth hormone (GH) secretion, and pancreatic secretion of insulin and glucagon.
Use of opioids for an extended period of time may influence the hypothalamic-pituitary-gonadal axis, leading to androgen deficiency that may manifest as low libido, impotence, erectile dysfunction, amenorrhea, or infertility. The causal role of opioids in the clinical syndrome of hypogonadism is unknown because the various medical, physical, lifestyle, and psychological stressors that may influence gonadal hormone levels have not been adequately controlled for in studies conducted to date [see Adverse Reactions (6)].
Effects on the Immune System: Opioids have been shown to have a variety of effects on components of the immune system in in vitro and animal models. The clinical significance of these findings is unknown. Overall, the effects of opioids appear to be modestly immunosuppressive.
Concentration–Efficacy Relationships: The minimum effective analgesic concentration will vary widely among patients, especially among patients who have been previously treated with opioid agonists. The minimum effective analgesic concentration of morphine for any individual patient may increase over time due to an increase in pain, the development of a new pain syndrome, and/or the development of analgesic tolerance [see Dosage and Administration (2.2, 2.5)].
Concentration–Adverse Reaction Relationships: There is a relationship between increasing morphine plasma concentration and increasing frequency of dose-related opioid adverse reactions such as nausea, vomiting, CNS effects, and respiratory depression. In opioid-tolerant patients, the situation may be altered by the development of tolerance to opioid-related adverse reactions [see Dosage and Administration (2.2, 2.5)].
12.3 Pharmacokinetics
Absorption: Morphine, when administered as morphine sulfate is about two-thirds absorbed from the gastrointestinal tract with the maximum analgesic effect occurring 60 minutes post-administration. The oral bioavailability of morphine sulfate is less than 40% and shows large inter-individual variability due to extensive pre-systemic metabolism.
Administration of 30 mg of Morphine Sulfate Oral Solution every six hours for 5 days resulted in a comparable 24-hour exposure (AUC). The steady-state levels were achieved within 48 hours for both tablets and solution. The mean steady state Cmax values were about 78 and 58 ng/mL for tablet and solution, respectively.
Distribution: Once absorbed, morphine sulfate is distributed to skeletal muscle, kidneys, liver, intestinal tract, lungs, spleen and brain. Although the primary site of action is the CNS, only small quantities cross the blood-brain barrier.
Morphine sulfate also crosses the placental membranes and has been found in breast milk. The volume of distribution of morphine sulfate is approximately 1 to 6 L/kg, and morphine sulfate is 20% to 35% reversibly bound to plasma proteins.
Elimination: Metabolism: The major pathway of morphine sulfate detoxification is conjugation, either with D-glucuronic acid to produce glucuronides or with sulfuric acid to produce morphine-3-etheral sulfate. While a small fraction (less than 5%) of morphine sulfate is demethylated, virtually all morphine sulfate is converted by hepatic metabolism to the 3- and 6-glucuronide metabolites (M3G and M6G; about 50% and 15%, respectively). M6G has been shown to have analgesic activity but crosses the blood-brain barrier poorly, while M3G has no significant analgesic activity.
Excretion: Most of a dose of morphine sulfate is excreted in urine as M3G and M6G, with elimination of morphine sulfate occurring primarily as renal excretion of M3G. Approximately 10% of the dose is excreted unchanged in urine. A small amount of glucuronide conjugates are excreted in bile, with minor enterohepatic recycling. Seven to 10% of administered morphine sulfate is excreted in the feces.
The mean adult plasma clearance is approximately 20 to 30 mL/min/kg. The effective terminal half-life of morphine sulfate after IV administration is reported to be approximately 2 hours. In some studies involving longer periods of plasma sampling, a longer terminal half-life of morphine sulfate of about 15 hours was reported.
Specific Populations: Pediatric Patients 2 Years of Age and Older: Morphine pharmacokinetics were analyzed in a population pharmacokinetic analysis of 66 pediatric patients aged 2 years to 17 years. Initially after dosing, the geometric mean plasma half-life of morphine was up to 1.8 hours. The geometric mean terminal elimination plasma half-life of morphine was 18.6 hours. For both the M3G metabolite and M6G metabolite, the single-dose geometric mean Cmax in pediatric patients was not greater than in adults.
Race/Ethnicity: There may be some pharmacokinetic differences associated with race. In one published study, Chinese subjects given intravenous morphine sulfate had a higher clearance when compared to Caucasian subjects (1,852 +/- 116 mL/min compared to 1,495 +/- 80 mL/min).
Sex: While evidence of greater post-operative morphine sulfate consumption in men compared to women is present in the literature, clinically significant differences in analgesic outcomes and pharmacokinetic parameters have not been consistently demonstrated. Some studies have shown an increased sensitivity to the adverse effects of morphine sulfate, including respiratory depression, in women compared to men.
Hepatic Impairment: Morphine pharmacokinetics are altered in patients with cirrhosis. Clearance was found to decrease with a corresponding increase in half-life. The M3G and M6G to morphine AUC ratios also decreased in these subjects, indicating diminished metabolic activity. Adequate studies of the pharmacokinetics of morphine in patients with severe hepatic impairment have not been conducted.
Renal Impairment: Morphine pharmacokinetics are altered in patients with renal failure. Clearance is decreased and the metabolites, M3G and M6G, may accumulate to much higher plasma levels in patients with renal failure as compared to patients with normal renal function. Adequate studies of the pharmacokinetics of morphine in patients with severe renal impairment have not been conducted.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis: Long-term studies in animals to evaluate the carcinogenic potential of morphine have not been conducted.
Mutagenesis: No formal studies to assess the mutagenic potential of morphine have been conducted. In the published literature, morphine was found to be mutagenic in vitro increasing DNA fragmentation in human T-cells. Morphine was reported to be mutagenic in the in vivo mouse micronucleus assay and positive for the induction of chromosomal aberrations in mouse spermatids and murine lymphocytes. Mechanistic studies suggest that the in vivo clastogenic effects reported with morphine in mice may be related to increases in glucocorticoid levels produced by morphine in this species. In contrast to the above positive findings, in vitro studies in the literature have also shown that morphine did not induce chromosomal aberrations in human leukocytes or translocations or lethal mutations in Drosophila.
Impairment of Fertility: No formal nonclinical studies to assess the potential of morphine to impair fertility have been conducted.
Several nonclinical studies from the literature have demonstrated adverse effects on male fertility in the rat from exposure to morphine. One study in which male rats were administered morphine sulfate subcutaneously prior to mating (up to 30 mg/kg twice daily) and during mating (20 mg/kg twice daily) with untreated females, a number of adverse reproductive effects including reduction in total pregnancies and higher incidence of pseudopregnancies at 20 mg/kg/day (3.2 times the HDD) were reported.
Studies from the literature have also reported changes in hormonal levels in male rats (i.e. testosterone, luteinizing hormone) following treatment with morphine at 10 mg/kg/day or greater (1.6 times the HDD).
Female rats that were administered morphine sulfate intraperitoneally prior to mating exhibited prolonged estrous cycles at 10 mg/kg/day (1.6 times the HDD).
Exposure of adolescent male rats to morphine has been associated with delayed sexual maturation and following mating to untreated females, smaller litters, increased pup mortality, and/or changes in reproductive endocrine status in adult male offspring have been reported (estimated 5 times the plasma levels at the HDD).
-
16 HOW SUPPLIED/STORAGE AND HANDLING
Morphine Sulfate Oral Solution:
10 mg per 5 mL (2 mg/mL) Oral Solution is supplied as a clear, blue-green solution. Each 1 mL of clear, blue-green oral solution contains 2 mg of morphine sulfate, USP (equivalent to 1.5 mg morphine).
NDC: 68094-001-62
5 mL per unit dose cup
Thirty (30) cups per shipper100 mg per 5 mL (20 mg/mL) Oral Solution (color added) (only for opioid-tolerant adults) is supplied as a clear, pink solution. Each 1 mL of clear, pink oral solution contains 20 mg of morphine sulfate, USP (equivalent to 15 mg morphine).
NDC: 68094-045-58
0.5 mL per unit dose syringe
Fifty (50) syringes per shipperNDC: 68094-056-58
0.5 mL per unit dose ENFit syringe
Fifty (50) syringes per shipperNDC: 68094-156-58
1 mL per unit dose ENFit syringe
Fifty (50) syringes per shipperNDC: 68094-256-58
0.5 mL per unit dose syringe
Fifty (50) syringes per shipperNDC: 68094-356-58
1 mL per unit dose syringe
Fifty (50) syringes per shipperNDC: 68094-456-58
0.25 mL per unit dose syringe
Fifty (50) syringes per shipperNDC: 68094-556-58
0.25 mL per unit dose ENFit syringe
Fifty (50) syringes per shipper -
17 PATIENT COUNSELING INFORMATION
Advise the patients or caregivers to read the FDA-approved patient labeling (Medication Guide and Instruction for Use).
Storage and Disposal: Because of the risks associated with accidental ingestion, misuse, and abuse, advise patients to store Morphine Sulfate Oral Solution securely, out of sight and reach of children, and in a location not accessible by others, including visitors to the home. Inform patients that leaving Morphine Sulfate Oral Solution unsecured can pose a deadly risk to others in the home [see Warnings and Precautions (5.1, 5.2, 5.3) and Drug Abuse and Dependence (9.2)].
Expired, unwanted, or unused Morphine Sulfate Oral Solution should be disposed of by flushing the unused medication down the toilet if a drug take-back option is not readily available.
Medication Errors: Morphine Sulfate Oral Solution is available in three concentrations: 2 mg/mL, 4 mg/mL, and 20 mg/mL. Inform patients and caregivers about which concentration they have been prescribed.
Addiction, Abuse, and Misuse: Inform patients that the use of Morphine Sulfate Oral Solution, even when taken as recommended, can result in addiction, abuse, and misuse, which can lead to overdose and death [see Warnings and Precautions (5.2)]. Instruct patients not to share Morphine Sulfate Oral Solution with others and to take steps to protect Morphine Sulfate Oral Solution from theft or misuse.
Life-Threatening Respiratory Depression: Inform patients of the risk of life-threatening respiratory depression, including information that the risk is greatest when starting Morphine Sulfate Oral Solution or when the dosage is increased, and that it can occur even at recommended dosages.
Educate patients and caregivers on how to recognize respiratory depression and emphasize the importance of calling 911 or getting emergency medical help right away in the event of a known or suspected overdose [see Warnings and Precautions (5.3)].
Accidental Ingestion: Inform patients that accidental ingestion, especially by children, may result in respiratory depression or death [see Warnings and Precautions (5.3)].
Interactions with Benzodiazepines and Other CNS Depressants: Inform patients and caregivers that potentially fatal additive effects may occur if Morphine Sulfate Oral Solution is used with benzodiazepines or other CNS depressants, including alcohol, and not to use these concomitantly unless supervised by a healthcare provider [see Warnings and Precautions (5.4) and Drug Interactions (7)].
Patient Access to Naloxone for the Emergency Treatment of Opioid Overdose: Discuss with the patient and caregiver the availability of naloxone for the emergency treatment of opioid overdose, both when initiating and renewing treatment with Morphine Sulfate Oral Solution. Inform patients and caregivers about the various ways to obtain naloxone as permitted by individual state naloxone dispensing and prescribing requirements or guidelines (e.g., by prescription, directly from a pharmacist, or as part of a community-based program) [see Dosage and Administration (2.3) and Warnings and Precautions (5.3)].
Educate patients and caregivers on how to recognize the signs and symptoms of an overdose.
Explain to patients and caregivers that naloxone's effects are temporary, and that they must call 911 or get emergency medical help right away in all cases of known or suspected opioid overdose, even if naloxone is administered [see Overdosage (10)].
If naloxone is prescribed, also advise patients and caregivers:
- How to treat with naloxone in the event of an opioid overdose
- To tell family and friends about their naloxone and to keep it in a place where family and friends can access it in an emergency
- To read the Patient Information (or other educational material) that will come with their naloxone. Emphasize the importance of doing this before an opioid emergency happens, so the patient and caregiver will know what to do.
Hyperalgesia and Allodynia: Inform patients and caregivers not to increase opioid dosage without first consulting a clinician. Advise patients to seek medical attention if they experience symptoms of hyperalgesia, including worsening pain, increased sensitivity to pain, or new pain [see Warnings and Precautions (5.7), Adverse Reactions (6)].
Serotonin Syndrome: Inform patients that opioids could cause a rare but potentially life-threatening condition called serotonin syndrome resulting from concomitant administration of serotonergic drugs. Warn patients of the symptoms of serotonin syndrome and to seek medical attention right away if symptoms develop. Instruct patients to inform their physicians if they are taking, or plan to take serotonergic medications [see Drug Interactions (7)].
MAOI Interaction: Inform patients not to take Morphine Sulfate Oral Solution while using any drugs that inhibit monoamine oxidase. Patients should not start MAOIs while taking Morphine Sulfate Oral Solution [see Warnings and Precautions (5.9) and Drug Interactions (7)].
Important Administration Instructions
Instruct patients how to properly take Morphine Sulfate Oral Solution [see Dosage and Administration (2), Warnings and Precautions (5.1)].
- Strongly advise patients and caregivers to always use a graduated oral syringe when administering Morphine Sulfate Oral Solution to correctly measure the prescribed amount of medication [see Warnings and Precautions (5.1)].
Morphine Sulfate Oral Solution 20 mg/mL
- Inform patients that the 20 mg/mL formulation is only for adult patients who are already receiving opioid-therapy and have demonstrated opioid tolerance. Use of this formulation may cause fatal respiratory depression when administered to patients who have not had previous exposure to opioids [see Indications and Usage (1), Dosage and Administration (2.1)].
Important Discontinuation Instructions:
In order to avoid developing withdrawal symptoms, instruct patients not to discontinue Morphine Sulfate Oral Solution without first discussing a tapering plan with the prescriber [see Dosage and Administration (2.6)].
Driving or Operating Heavy Machinery: Inform patients that Morphine Sulfate Oral Solution may impair the ability to perform potentially hazardous activities such as driving a car or operating heavy machinery. Advise patients not to perform such tasks until they know how they will react to the medication [see Warnings and Precautions (5.16)].
Constipation: Advise patients of the potential for severe constipation, including management instructions and when to seek medical attention [see Adverse Reactions (6)].
Adrenal Insufficiency: Inform patients that opioids could cause adrenal insufficiency, a potentially life-threatening condition. Adrenal insufficiency may present with non-specific symptoms and signs such as nausea, vomiting, anorexia, fatigue, weakness, dizziness, and low blood pressure. Advise patients to seek medical attention if they experience a constellation of these symptoms [see Warnings and Precautions (5.10)].
Hypotension: Inform patients that Morphine Sulfate Oral Solution may cause orthostatic hypotension and syncope. Instruct patients how to recognize symptoms of low blood pressure and how to reduce the risk of serious consequences should hypotension occur (e.g., sit or lie down, carefully rise from a sitting or lying position) [see Warnings and Precautions (5.11)].
Anaphylaxis Inform patients that anaphylaxis have been reported with ingredients contained in Morphine Sulfate Oral Solution. Advise patients how to recognize such a reaction and when to seek medical attention [see Contraindications (4) and Adverse Reactions (6)].
Pregnancy: Neonatal Opioid Withdrawal Syndrome: Inform female patients of reproductive potential that use of Morphine Sulfate Oral Solution for an extended period of time during pregnancy can result in neonatal opioid withdrawal syndrome, which may be life-threatening if not recognized and treated [see Warnings and Precautions (5.5) and Use in Specific Populations (8.1)].
Embryo-Fetal Toxicity: Inform female patients of reproductive potential that Morphine Sulfate Oral Solution can cause fetal harm and to inform their healthcare provider of a known or suspected pregnancy [see Use in Specific Populations (8.1)].
Lactation: Advise nursing mothers to carefully observe infants for increased sleepiness (more than usual), breathing difficulties, or limpness. Instruct nursing mothers to seek immediate medical care if they notice these signs [see Use in Specific Populations (8.2)].
Infertility: Inform patients that use of opioids for an extended period of time may cause reduced fertility. It is not known whether these effects on fertility are reversible [see Use in Specific Populations (8.3)].
- SPL UNCLASSIFIED SECTION
-
MEDICATION GUIDE
This Medication Guide has been approved by the U.S. Food and Drug Administration LI1656 Rev. 04/24 Medication Guide
Morphine (mor-pheen) Sulfate
Oral Solution, CIIMorphine Sulfate Oral Solution is: - A strong prescription pain medicine that contains an opioid (narcotic) that is used to manage short term (acute) and long term (chronic) pain severe enough to require an opioid pain medicine, when other pain treatments such as non-opioid pain medicines do not treat your pain well enough or you cannot tolerate them.
- An opioid pain medicine that can put you at risk for overdose and death. Even if you take your dose correctly as prescribed you are at risk for opioid addiction, abuse, and misuse that can lead to death.
Important information about Morphine Sulfate Oral Solution: - Get emergency help or call 911 right away if you take too much Morphine Sulfate Oral Solution (overdose). When you first start taking Morphine Sulfate Oral Solution, when your dose is changed, or if you take too much (overdose), serious or life-threatening breathing problems that can lead to death may occur. Talk to your healthcare provider about naloxone, a medicine for the emergency treatment of an opioid overdose.
- Taking Morphine Sulfate Oral Solution with other opioid medicines, benzodiazepines, alcohol, or other central nervous system depressants (including street drugs) can cause severe drowsiness, decreased awareness, breathing problems, coma, and death.
- Never give anyone else your Morphine Sulfate Oral Solution. They could die from taking it. Selling or giving away Morphine Sulfate Oral Solution is against the law.
- Store Morphine Sulfate Oral Solution securely, out of sight and reach of children, and in a location not accessible by others, including visitors to the home.
Do not take Morphine Sulfate Oral Solution if you have: - severe asthma, trouble breathing, or other lung problems.
- a bowel blockage or have narrowing of the stomach or intestines.
- an allergy to morphine.
Before taking Morphine Sulfate Oral Solution, tell your healthcare provider if you have a history of: - head injury, seizures
- problems urinating
- abuse of street or prescription drugs, alcohol addiction, opioid overdose, or mental health problems.
- liver, kidney, thyroid problems
- pancreas or gallbladder problems
Tell your healthcare provider if you are: - noticing your pain getting worse. If your pain gets worse after you take Morphine Sulfate Oral Solution, do not take more of Morphine Sulfate Oral Solution without first talking to your healthcare provider. Talk to your healthcare provider if the pain that you have increases, if you feel more sensitive to pain, or if you have new pain after taking Morphine Sulfate Oral Solution.
- pregnant or planning to become pregnant. Use of Morphine Sulfate Oral Solution for an extended period of time during pregnancy can cause withdrawal symptoms in your newborn baby that could be life-threatening if not recognized and treated.
- breastfeeding. Morphine Sulfate Oral Solution passes into breast milk and may harm your baby. Carefully observe infants for increased sleepiness (more than usual), breathing difficulties, or limpness. Seek immediate medical care if you notice these signs.
- living in a household where there are small children or someone who has abused street or prescription drugs.
- taking prescription or over-the-counter medicines, vitamins, or herbal supplements. Taking Morphine Sulfate Oral Solution with certain other medicines can cause serious side effects that could lead to death
When taking Morphine Sulfate Oral Solution: - Take Morphine Sulfate Oral Solution exactly as prescribed by your healthcare provider. Use the lowest dose possible for the shortest time needed.
- For acute (short-term) pain, you may only need to take Morphine Sulfate Oral Solution for a few days. See disposal information at the bottom of this section for directions on how to safely throw away (dispose of) unused Morphine Sulfate Oral Solution.
- Call your healthcare provider if the dose you are taking does not control your pain.
- If you have been taking Morphine Sulfate Oral Solution regularly, do not stop taking Morphine Sulfate Oral Solution without talking to your healthcare provider.
- Dispose of expired, unwanted, or unused Morphine Sulfate Oral Solution by promptly flushing down the toilet, if a drug take-back option is not readily
- available. Visit www.fda.gov/drugdisposal for additional information on disposal of unused medicines.
While taking Morphine Sulfate Oral Solution DO NOT: - Drive or operate heavy machinery, until you know how Morphine Sulfate Oral Solution affects you. Morphine Sulfate Oral Solution can make you sleepy, dizzy, or lightheaded.
- Drink alcohol or use prescription or over-the-counter medicines that contain alcohol. Using products containing alcohol during treatment with Morphine Sulfate Oral Solution may cause you to overdose and die.
The possible side effects of Morphine Sulfate Oral Solution: - constipation, nausea, sleepiness, vomiting, tiredness, headache, dizziness, abdominal pain. Call your healthcare provider if you have any of these symptoms and they are severe.
Get emergency medical help or call 911 right away if you have: - trouble breathing, shortness of breath, fast heartbeat, chest pain, swelling of your face, tongue, or throat, extreme drowsiness, lightheadedness when changing positions, feeling faint, agitation, high body temperature, trouble walking, stiff muscles, or mental changes such as confusion.
Packaged by:
Precision Dose, Inc.
South Beloit, IL 61080
For inquiries call Precision Dose, Inc. at
1-800-397-9228 or email druginfo@precisiondose.com -
PRINCIPAL DISPLAY PANEL - 0.5 mL Syringe Label
Morphine Sulfate Oral Solution* CII
*Color Added 10 mg†/ 0.5 mL Delivers 0.5 mL
Store at 20 to 25°C (68 to77°F)
ONLY FOR USE IN ADULTS
WHO ARE OPIOID TOLERANT†Each 1 mL of oral solution contains 20 mg
Morphine Sulfate, USP equivalent to 15 mg
Morphine base.
FOR ORAL USE ONLY
Pkg: Precision Dose, Inc. S. Beloit, IL 61080
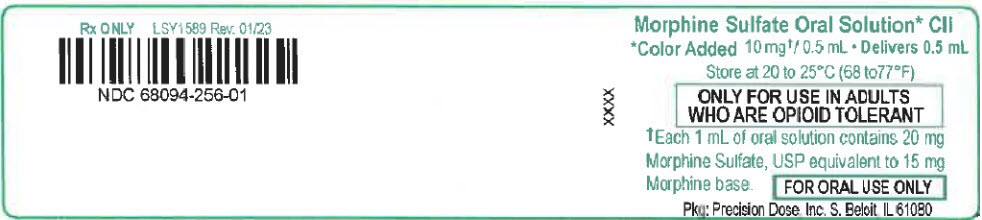
-
INGREDIENTS AND APPEARANCE
MORPHINE SULFATE
morphine sulfate solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 68094-256(NDC:0054-0517) Route of Administration ORAL DEA Schedule CII Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength Morphine Sulfate (UNII: X3P646A2J0) (Morphine - UNII:76I7G6D29C) Morphine Sulfate 100 mg in 5 mL Inactive Ingredients Ingredient Name Strength citric acid monohydrate (UNII: 2968PHW8QP) edetate disodium (UNII: 7FLD91C86K) glycerin (UNII: PDC6A3C0OX) sodium benzoate (UNII: OJ245FE5EU) sorbitol (UNII: 506T60A25R) water (UNII: 059QF0KO0R) D&C Red No. 33 (UNII: 9DBA0SBB0L) Sucralose (UNII: 96K6UQ3ZD4) Product Characteristics Color PINK (Clear) Score Shape Size Flavor Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 68094-256-58 50 in 1 CASE 08/15/2023 1 1 in 1 BAG 1 NDC: 68094-256-01 0.5 mL in 1 SYRINGE, PLASTIC; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA022195 08/15/2023 Labeler - Precision Dose, Inc. (035886746)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.