HYDROXYPROGESTERONE CAPROATE injection
HYDROXYPROGESTERONE CAPROATE by
Drug Labeling and Warnings
HYDROXYPROGESTERONE CAPROATE by is a Prescription medication manufactured, distributed, or labeled by AuroMedics Pharma LLC, EUGIA Pharma Specialities Limited. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use HYDROXYPROGESTERONE CAPROATE INJECTION safely and effectively. See full prescribing information for HYDROXYPROGESTERONE CAPROATE INJECTION.
HYDROXYPROGESTERONE CAPROATE injection, for intramuscular use.
Initial U.S. Approval: 1956RECENT MAJOR CHANGES
INDICATIONS AND USAGE
Hydroxyprogesterone caproate injection is a progestin indicated to reduce the risk of preterm birth in women with a singleton pregnancy who have a history of singleton spontaneous preterm birth (1). The effectiveness of hydroxyprogesterone caproate injection is based on improvement in the proportion of women who delivered < 37 weeks of gestation (14). There are no controlled trials demonstrating a direct clinical benefit, such as improvement in neonatal mortality and morbidity.
Limitation of use: Hydroxyprogesterone caproate injection is not intended for use in women with multiple gestations or other risk factors for preterm birth. (1)DOSAGE AND ADMINISTRATION
- Hydroxyprogesterone caproate injection (Multi-dose vials): Administer intramuscularly at a dose of 250 mg (1 mL) once weekly in the upper outer quadrant of the gluteus maximus (2.1)
- Begin treatment between 16 weeks, 0 days and 20 weeks, 6 days of gestation (2.1)
- Continue administration once weekly until week 37 (through 36 weeks, 6 days) of gestation or delivery, whichever occurs first (2.1)
DOSAGE FORMS AND STRENGTHS
5 mL multi-dose vial for intramuscular use contains 1,250 mg of hydroxyprogesterone caproate (250 mg/mL). (3)
CONTRAINDICATIONS
- Current or history of thrombosis or thromboembolic disorders (4)
- Known or suspected breast cancer, other hormone-sensitive cancer, or history of these conditions (4)
- Undiagnosed abnormal vaginal bleeding unrelated to pregnancy (4)
- Cholestatic jaundice of pregnancy (4)
- Liver tumors, benign or malignant, or active liver disease (4)
- Uncontrolled hypertension (4)
WARNINGS AND PRECAUTIONS
- Thromboembolic disorders: Discontinue if thrombosis or thromboembolism occurs (5.1)
- Allergic reactions: Consider discontinuing if allergic reactions occur (5.2)
- Decreased glucose tolerance: Monitor prediabetic and diabetic women receiving hydroxyprogesterone caproate (5.3)
- Fluid retention: Monitor women with conditions that may be affected by fluid retention, such as preeclampsia, epilepsy, cardiac or renal dysfunction (5.4)
- Depression: Monitor women with a history of clinical depression; discontinue hydroxyprogesterone caproate if depression recurs (5.5)
ADVERSE REACTIONS
In a study where the hydroxyprogesterone caproate intramuscular injection was compared with placebo, the most common adverse reactions reported with hydroxyprogesterone caproate intramuscular injection (reported incidence in ≥ 2% of subjects and higher than in the control group) were: injection site reactions (pain [35%], swelling [17%], pruritus [6%], nodule [5%]), urticaria (12%), pruritus (8%), nausea (6%), and diarrhea (2%). (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact AuroMedics Pharma LLC at 1-866-850-2876 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 3/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Dosing
2.2 Preparation and Administration
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Thromboembolic Disorders
5.2 Allergic Reactions
5.3 Decrease in Glucose Tolerance
5.4 Fluid Retention
5.5 Depression
5.6 Jaundice
5.7 Hypertension
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.6 Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Clinical Trial to Evaluate Reduction of Risk of Preterm Birth
14.2 Infant Follow-Up Safety Study
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
Hydroxyprogesterone caproate injection is a progestin indicated to reduce the risk of preterm birth in women with a singleton pregnancy who have a history of singleton spontaneous preterm birth. The effectiveness of hydroxyprogesterone caproate injection is based on improvement in the proportion of women who delivered < 37 weeks of gestation. There are no controlled trials demonstrating a direct clinical benefit, such as improvement in neonatal mortality and morbidity.
Limitation of use: While there are many risk factors for preterm birth, safety and efficacy of hydroxyprogesterone caproate injection has been demonstrated only in women with a prior spontaneous singleton preterm birth. It is not intended for use in women with multiple gestations or other risk factors for preterm birth. -
2 DOSAGE AND ADMINISTRATION
2.1 Dosing
- Hydroxyprogesterone caproate injection (Multi-dose vials): Administer intramuscularly at a dose of 250 mg (1 mL) once weekly (every 7 days) in the upper outer quadrant of the gluteus maximus by a healthcare provider
- Begin treatment between 16 weeks, 0 days and 20 weeks, 6 days of gestation
- Continue administration once weekly until week 37 (through 36 weeks, 6 days) of gestation or delivery, whichever occurs first
2.2 Preparation and Administration
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. Hydroxyprogesterone caproate injection is a clear pale yellow to yellow color oily solution. The solution must be clear at the time of use; replace vial if visible particles or crystals are present.
Specific instructions for administration by dosage form:
Hydroxyprogesterone caproate injection multi-dose vials (intramuscular use only)
Hydroxyprogesterone caproate injection multi-dose vials are only for intramuscular injection with a syringe into the upper outer quadrant of the gluteus maximus, rotating the injection site to the alternate side from the previous week, using the following preparation and administration procedure:- Clean the vial top with an alcohol swab before use.
- Draw up 1 mL of drug into a 3 mL syringe with an 18 gauge needle.
- Change the needle to a 21 gauge 1½ inch needle.
- After preparing the skin, inject in the upper outer quadrant of the gluteus maximus. The solution is viscous and oily. Slow injection (over one minute or longer) is recommended.
- Applying pressure to the injection site may minimize bruising and swelling.
If the 5 mL multi-dose vial is used, discard any unused product 5 weeks after first use.
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
Do not use hydroxyprogesterone caproate in women with any of the following conditions:
- Current or history of thrombosis or thromboembolic disorders
- Known or suspected breast cancer, other hormone-sensitive cancer, or history of these conditions
- Undiagnosed abnormal vaginal bleeding unrelated to pregnancy
- Cholestatic jaundice of pregnancy
- Liver tumors, benign or malignant, or active liver disease
- Uncontrolled hypertension
-
5 WARNINGS AND PRECAUTIONS
5.1 Thromboembolic Disorders
Discontinue hydroxyprogesterone caproate if an arterial or deep venous thrombotic or thromboembolic event occurs.
5.2 Allergic Reactions
Allergic reactions, including urticaria, pruritus and angioedema, have been reported with use of hydroxyprogesterone caproate or with other products containing castor oil. Consider discontinuing the drug if such reactions occur.
5.3 Decrease in Glucose Tolerance
A decrease in glucose tolerance has been observed in some patients on progestin treatment. The mechanism of this decrease is not known. Carefully monitor prediabetic and diabetic women while they are receiving hydroxyprogesterone caproate.
5.4 Fluid Retention
Because progestational drugs may cause some degree of fluid retention, carefully monitor women with conditions that might be influenced by this effect (e.g., preeclampsia, epilepsy, migraine, asthma, cardiac or renal dysfunction).
5.5 Depression
Monitor women who have a history of clinical depression and discontinue hydroxyprogesterone caproate if clinical depression recurs.
-
6 ADVERSE REACTIONS
For the most serious adverse reactions to the use of progestins, see Warnings and Precautions (5).
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to the rates in the clinical trials of another drug and may not reflect the rates observed in practice.
In a vehicle (placebo)-controlled clinical trial of 463 pregnant women at risk for spontaneous preterm delivery based on obstetrical history, 310 received 250 mg of hydroxyprogesterone caproate and 153 received a vehicle formulation containing no drug by a weekly intramuscular injection beginning at 16 to 20 weeks of gestation and continuing until 37 weeks of gestation or delivery, whichever occurred first. [See Clinical Studies (14.1).]
Certain pregnancy-related fetal and maternal complications or events were numerically increased in the hydroxyprogesterone caproate-treated subjects as compared to control subjects, including miscarriage and stillbirth, admission for preterm labor, preeclampsia or gestational hypertension, gestational diabetes, and oligohydramnios (Tables 1 and 2).
Table 1 Selected Fetal Complications 1 N = Total number of subjects enrolled prior to 20 weeks 0 days
2 N = Total number of subjects at risk ≥ 20 weeksPregnancy Complication
Hydroxyprogesterone Caproate
n/N
Control
n/N
Miscarriage (< 20 weeks)1
5/209
0/107
Stillbirth (≥ 20 weeks)2
6/305
2/153
Table 2 Selected Maternal Complications 1 Other than delivery admission.
Pregnancy Complication
Hydroxyprogesterone Caproate
N=310
%
Control
N=153
%
Admission for preterm labor1
16.0
13.8
Preeclampsia or gestational hypertension
8.8
4.6
Gestational diabetes
5.6
4.6
Oligohydramnios
3.6
1.3
Common Adverse Reactions:
The most common adverse reaction with intramuscular injection was injection site pain, which was reported after at least one injection by 34.8% of the hydroxyprogesterone caproate group and 32.7% of the control group. Table 3 lists adverse reactions that occurred in ≥ 2% of subjects and at a higher rate in the hydroxyprogesterone caproate group than in the control group.
Table 3 Adverse Reactions Occurring in ≥ 2% of Hydroxyprogesterone Caproate-Treated Subjects and at a Higher Rate than Control Subjects Preferred Term
Hydroxyprogesterone Caproate
N=310
%
Control
N=153
%
Injection site pain
34.8
32.7
Injection site swelling
17.1
7.8
Urticaria
12.3
11.1
Pruritus
7.7
5.9
Injection site pruritus
5.8
3.3
Nausea
5.8
4.6
Injection site nodule
4.5
2.0
Diarrhea
2.3
0.7
In the clinical trial using intramuscular injection, 2.2% of subjects receiving hydroxyprogesterone caproate were reported as discontinuing therapy due to adverse reactions compared to 2.6% of control subjects. The most common adverse reactions that led to discontinuation in both groups were urticaria and injection site pain/swelling (1% each).
Pulmonary embolus in one subject and injection site cellulitis in another subject were reported as serious adverse reactions in hydroxyprogesterone caproate-treated subjects.
6.2 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of hydroxyprogesterone caproate. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- Body as a whole: Local injection site reactions (including erythema, urticaria, rash, irritation, hypersensitivity, warmth); fatigue; fever; hot flashes/flushes
- Digestive disorders: Vomiting
- Infections: Urinary tract infection
- Nervous system disorders: Headache, dizziness
- Pregnancy, puerperium and perinatal conditions: Cervical incompetence, premature rupture of membranes
- Reproductive system and breast disorders: Cervical dilation, shortened cervix
- Respiratory disorders: Dyspnea, chest discomfort
- Skin: Rash
-
7 DRUG INTERACTIONS
In vitro drug-drug interaction studies were conducted with hydroxyprogesterone caproate. Hydroxyprogesterone caproate has minimal potential for CYP1A2, CYP2A6, and CYP2B6 related drug-drug interactions at the clinically relevant concentrations. In vitro data indicated that therapeutic concentration of hydroxyprogesterone caproate is not likely to inhibit the activity of CYP2C8, CYP2C9, CYP2C19, CYP2D6, CYP2E1, and CYP3A4 [See Clinical Pharmacology (12.3).] No in vivo drug-drug interaction studies were conducted with hydroxyprogesterone caproate.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Hydroxyprogesterone caproate is indicated to reduce the risk of preterm birth in women with a singleton pregnancy who have a history of singleton spontaneous preterm birth. Fetal, neonatal, and maternal risks are discussed throughout labeling. Data from the placebo-controlled clinical trial and the infant follow-up safety study [see Clinical Studies (14.1, 14.2)] did not show a difference in adverse developmental outcomes between children of hydroxyprogesterone caproate-treated women and children of control subjects. However, these data are insufficient to determine a drug-associated risk of adverse developmental outcomes as none of the hydroxyprogesterone caproate-treated women received the drug during the first trimester of pregnancy. In animal reproduction studies, intramuscular administration of hydroxyprogesterone caproate to pregnant rats during gestation at doses 5 times the human dose equivalent based on a 60-kg human was not associated with adverse developmental outcomes.
In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Data
Animal Data
Reproduction studies of hydroxyprogesterone caproate administered to various animal species have been reported in the literature. In nonhuman primates, embryolethality was reported in rhesus monkeys administered hydroxyprogesterone caproate up to 2.4 and 24 times the human dose equivalent, but not in cynomolgus monkeys administered hydroxyprogesterone caproate at doses up to 2.4 times the human dose equivalent, every 7 days between days 20 and 146 of gestation. There were no teratogenic effects in either strain of monkey.
Reproduction studies have been performed in mice and rats at doses up to 95 and 5, respectively, times the human dose and have revealed no evidence of impaired fertility or harm to the fetus due to hydroxyprogesterone caproate.8.2 Lactation
Risk Summary
Low levels of progestins are present in human milk with the use of progestin-containing products, including hydroxyprogesterone caproate. Published studies have reported no adverse effects of progestins on the breastfed child or on milk production.8.4 Pediatric Use
Hydroxyprogesterone caproate is not indicated for use in women under 16 years of age. Safety and effectiveness in patients less than 16 years of age have not been established. A small number of women under age 18 years were studied; safety and efficacy are expected to be the same in women aged 16 years and above as for users 18 years and older [see Clinical Studies (14)].
- 10 OVERDOSAGE
-
11 DESCRIPTION
The active pharmaceutical ingredient in hydroxyprogesterone caproate injection, USP is hydroxyprogesterone caproate, a progestin.
The chemical name for hydroxyprogesterone caproate is pregn-4-ene-3,20-dione, 17[(1-oxohexyl)oxy]. It has a molecular formula of C27H40O4 and a molecular weight of 428.60. Hydroxyprogesterone caproate, USP exists as white or creamy white, crystalline powder with a melting point of 120° to 124°C.
The structural formula is:
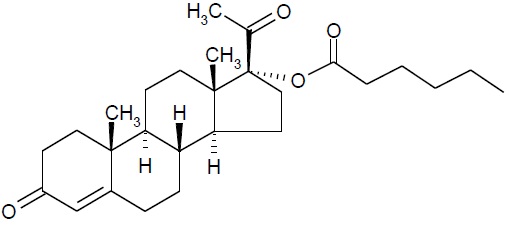
Hydroxyprogesterone caproate injection, USP is a sterile, non-pyrogenic, clear pale yellow to yellow color oily solution for intramuscular injection. Each 5 mL multi-dose vial contains hydroxyprogesterone caproate USP, 250 mg/mL (25% w/v), in castor oil USP (28.6%) and benzyl benzoate USP (46% v/v) with the preservative benzyl alcohol NF (2% v/v). -
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Hydroxyprogesterone caproate is a synthetic progestin. The mechanism by which hydroxyprogesterone caproate reduces the risk of recurrent preterm birth is not known.
12.2 Pharmacodynamics
No specific pharmacodynamic studies were conducted with hydroxyprogesterone caproate.
12.3 Pharmacokinetics
Absorption: Female patients with a singleton pregnancy received intramuscular doses of 250 mg hydroxyprogesterone caproate for the reduction of preterm birth starting between 16 weeks 0 days and 20 weeks 6 days. All patients had blood drawn daily for 7 days to evaluate pharmacokinetics.
Table 4 Summary of Mean (Standard Deviation) Pharmacokinetic Parameters for Hydroxyprogesterone Caproate Blood was drawn daily for 7 days (1) starting 24 hours after the first dose between Weeks 16 to 20 (Group 1), (2) after a dose between Weeks 24 to 28 (Group 2), or (3) after a dose between Weeks 32 to 36 (Group 3)
a Reported as median (range)
b t = 7 daysGroup (N)
Cmax (ng/mL)
Tmax (days)a
AUC(0-t)b (nghr/mL)
Group 1 (N=6)
5.0 (1.5)
5.5 (2.0 to 7.0)
571.4 (195.2)
Group 2 (N=8)
12.5 (3.9)
1.0 (0.9 to 1.9)
1269.6 (285.0)
Group 3 (N=11)
12.3 (4.9)
2.0 (1.0 to 3.0)
1268.0 (511.6)
For all three groups, peak concentration (Cmax) and area under the curve (AUC(1 to 7 days)) of the mono-hydroxylated metabolites were approximately 3 to 8-fold lower than the respective parameters for the parent drug, hydroxyprogesterone caproate. While di-hydroxylated and tri-hydroxylated metabolites were also detected in human plasma to a lesser extent, no meaningful quantitative results could be derived due to the absence of reference standards for these multiple hydroxylated metabolites. The relative activity and significance of these metabolites are not known.
The elimination half-life of hydroxyprogesterone caproate, as evaluated from 4 patients in the study who reached full-term in their pregnancies, was 16.4 (±3.6) days. The elimination half-life of the mono-hydroxylated metabolites was 19.7 (±6.2) days.
Distribution: Hydroxyprogesterone caproate binds extensively to plasma proteins including albumin and corticosteroid binding globulins.
Metabolism: In vitro studies have shown that hydroxyprogesterone caproate can be metabolized by human hepatocytes, both by phase I and phase II reactions. Hydroxyprogesterone caproate undergoes extensive reduction, hydroxylation and conjugation. The conjugated metabolites include sulfated, glucuronidated and acetylated products. In vitro data indicate that the metabolism of hydroxyprogesterone caproate is predominantly mediated by CYP3A4 and CYP3A5. The in vitro data indicate that the caproate group is retained during metabolism of hydroxyprogesterone caproate.
Excretion: Both conjugated metabolites and free steroids are excreted in the urine and feces, with the conjugated metabolites being prominent. Following intramuscular administration to pregnant women at 10 to 12 weeks gestation, approximately 50% of a dose was recovered in the feces and approximately 30% recovered in the urine.
Drug Interactions
Cytochrome P450 (CYP) enzymes: An in vitro inhibition study using human liver microsomes and CYP isoform-selective substrates indicated that hydroxyprogesterone caproate increased the metabolic rate of CYP1A2, CYP2A6, and CYP2B6 by approximately 80%, 150%, and 80%, respectively. However, in another in vitro study using human hepatocytes under conditions where the prototypical inducers or inhibitors caused the anticipated increases or decreases in CYP enzyme activities, hydroxyprogesterone caproate did not induce or inhibit CYP1A2, CYP2A6, or CYP2B6 activity. Overall, the findings indicate that hydroxyprogesterone caproate has minimal potential for CYP1A2, CYP2A6, and CYP2B6 related drug-drug interactions at the clinically relevant concentrations.
In vitro data indicated that therapeutic concentration of hydroxyprogesterone caproate is not likely to inhibit the activity of CYP2C8, CYP2C9, CYP2C19, CYP2D6, CYP2E1, and CYP3A4.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Hydroxyprogesterone caproate has not been adequately evaluated for carcinogenicity.
No reproductive or developmental toxicity or impaired fertility was observed in a multigenerational study in rats. Hydroxyprogesterone caproate administered intramuscularly, at gestational exposures up to 5 times the recommended human dose, had no adverse effects on the parental (F0) dams, their developing offspring (F1), or the latter offspring's ability to produce a viable, normal second (F2) generation. -
14 CLINICAL STUDIES
14.1 Clinical Trial to Evaluate Reduction of Risk of Preterm Birth
In a multicenter, randomized, double-blind, vehicle (placebo)-controlled clinical trial, the safety and effectiveness of hydroxyprogesterone caproate for the reduction of the risk of spontaneous preterm birth was studied in women with a singleton pregnancy (age 16 to 43 years) who had a documented history of singleton spontaneous preterm birth (defined as delivery at less than 37 weeks of gestation following spontaneous preterm labor or premature rupture of membranes). At the time of randomization (between 16 weeks, 0 days and 20 weeks, 6 days of gestation), an ultrasound examination had confirmed gestational age and no known fetal anomaly. Women were excluded for prior progesterone treatment or heparin therapy during the current pregnancy, a history of thromboembolic disease, or maternal/obstetrical complications (such as current or planned cerclage, hypertension requiring medication, or a seizure disorder).
A total of 463 pregnant women were randomized to receive either hydroxyprogesterone caproate (N=310) or vehicle (N=153) at a dose of 250 mg administered weekly by intramuscular injection starting between 16 weeks, 0 days and 20 weeks, 6 days of gestation, and continuing until 37 weeks of gestation or delivery. Demographics of the hydroxyprogesterone caproate-treated women were similar to those in the control group, and included: 59.0% Black, 25.5% Caucasian, 13.9% Hispanic and 0.6% Asian. The mean body mass index was 26.9 kg/m2.
The proportions of women in each treatment arm who delivered at < 37 (the primary study endpoint), < 35, and < 32 weeks of gestation are displayed in Table 5.
Table 5 Proportion of Subjects Delivering at < 37, < 35 and < 32 Weeks Gestational Age (ITT Population) 1 Four hydroxyprogesterone caproate-treated subjects were lost to follow-up. They were counted as deliveries at their gestational ages at time of last contact (184, 220, 343 and 364 weeks).
2 Adjusted for interim analysis.Delivery Outcome
Hydroxyprogesterone Caproate1
(N=310)
%
Control
(N=153)
%
Treatment difference and
95% Confidence Interval2
<37 weeks
37.1
54.9
-17.8% [-28.0%, -7.4%]
<35 weeks
21.3
30.7
-9.4% [-19.0%, -0.4%]
<32 weeks
11.9
19.6
-7.7% [-16.1%, -0.3%]
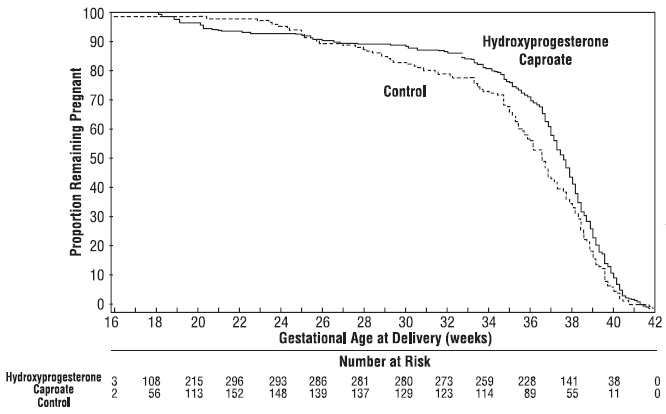
Compared to controls, treatment with hydroxyprogesterone caproate reduced the proportion of women who delivered preterm at < 37 weeks. The proportions of women delivering at < 35 and < 32 weeks also were lower among women treated with hydroxyprogesterone caproate. The upper bounds of the confidence intervals for the treatment difference at < 35 and < 32 weeks were close to zero. Inclusion of zero in a confidence interval would indicate the treatment difference is not statistically significant. Compared to the other gestational ages evaluated, the number of preterm births at < 32 weeks was limited.
After adjusting for time in the study, 7.5% of hydroxyprogesterone caproate-treated subjects delivered prior to 25 weeks compared to 4.7% of control subjects; see Figure 1.
Figure 1 Proportion of Women Remaining Pregnant as a Function of Gestational Age
The rates of fetal losses and neonatal deaths in each treatment arm are displayed in Table 6. Due to the higher rate of miscarriages and stillbirths in the hydroxyprogesterone caproate arm, there was no overall survival difference demonstrated in this clinical trial.Table 6 Fetal Losses and Neonatal Deaths A Four of the 310 hydroxyprogesterone caproate-treated subjects were lost to follow-up and stillbirth or neonatal status could not be determined
B Percentages are based on the number of enrolled subjects and not adjusted for time on drug
C Percentage adjusted for the number of at risk subjects (n=209 for hydroxyprogesterone caproate, n=107 for control) enrolled at <20 weeks gestation.Complication
Hydroxyprogesterone
Caproate
N=306A
n (%)B
Control
N=153
n (%)B
Miscarriages <20 weeks gestationC
5 (2.4)
0
Stillbirth
6 (2.0)
2 (1.3)
Antepartum stillbirth
5 (1.6)
1 (0.6)
Intrapartum stillbirth
1 (0.3)
1 (0.6)
Neonatal deaths
8 (2.6)
9 (5.9)
Total Deaths
19 (6.2)
11 (7.2)
A composite neonatal morbidity/mortality index evaluated adverse outcomes in live births. It was based on the number of neonates who died or experienced respiratory distress syndrome, bronchopulmonary dysplasia, grade 3 or 4 intraventricular hemorrhage, proven sepsis, or necrotizing enterocolitis. Although the proportion of neonates who experienced 1 or more events was numerically lower in the hydroxyprogesterone caproate arm (11.9% vs. 17.2%), the number of adverse outcomes was limited and the difference between arms was not statistically significant.
14.2 Infant Follow-Up Safety Study
Infants born to women enrolled in this study, and who survived to be discharged from the nursery, were eligible for participation in a follow-up safety study. Of 348 eligible offspring, 79.9% enrolled: 194 children of hydroxyprogesterone caproate-treated women and 84 children of control subjects. The primary endpoint was the score on the Ages & Stages Questionnaire (ASQ), which evaluates communication, gross motor, fine motor, problem solving, and personal/social parameters. The proportion of children whose scores met the screening threshold for developmental delay in each developmental domain was similar for each treatment group.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
Hydroxyprogesterone caproate injection, multi-dose vials (for intramuscular injection)
Hydroxyprogesterone caproate injection, USP is a sterile, non-pyrogenic, clear pale yellow to yellow color oily solution and is supplied as 5 mL of a sterile solution in a multi-dose glass vial.
Each 5 mL vial contains hydroxyprogesterone caproate USP, 250 mg/mL (25% w/v), in castor oil USP (28.6% v/v) and benzyl benzoate USP (46% v/v) with the preservative benzyl alcohol NF (2% v/v).
1,250 mg per 5 mL (250 mg / mL):
5 mL Multidose Vial
Packaged Individually NDC: 55150-310-01
Store at 20° to 25°C (68° to 77°F). Do not refrigerate or freeze.
Use multi-dose vials within 5 weeks after first use.
Caution: Protect vial from light. Store vial in its box. Store upright.
The vial stopper is not made with natural rubber latex.
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information).
Counsel patients that hydroxyprogesterone caproate injections may cause pain, soreness, swelling, itching or bruising. Inform the patient to contact her physician if she notices increased discomfort over time, oozing of blood or fluid, or inflammatory reactions at the injection site [see Adverse Reactions (6.1)].
Distributed by:
AuroMedics Pharma LLC
279 Princeton-Hightstown Rd.
E. Windsor, NJ 08520
Manufactured by:
Eugia Pharma Specialities Limited
Medchal-Malkajgiri District – 500101
India -
PATIENT INFORMATION
Hydroxyprogesterone Caproate
(hye drox'' ee proe jes' ter one kap' roe ate)
Injection
vial for intramuscular use
Read this Patient Information leaflet before you receive hydroxyprogesterone caproate injection. There may be new information. This information does not take the place of talking to your healthcare provider about your medical condition or treatment.
What is hydroxyprogesterone caproate injection?
Hydroxyprogesterone caproate injection is a prescription hormone medicine (progestin) used in women who are pregnant and who have delivered a baby too early (preterm) in the past. Hydroxyprogesterone caproate injection is used in these women to help lower the risk of having a preterm baby again. It is not known if hydroxyprogesterone caproate injection reduces the number of babies who are born with serious medical conditions or die shortly after birth. Hydroxyprogesterone caproate injection is for women who:
- Are pregnant with one baby.
- Have had a preterm delivery of one baby in the past.
Hydroxyprogesterone caproate injection is not intended for use to stop active preterm labor.
It is not known if hydroxyprogesterone caproate injection is safe and effective in women who have other risk factors for preterm birth.
Hydroxyprogesterone caproate injection is not for use in women under 16 years of age.
Who should not receive hydroxyprogesterone caproate injection?
Hydroxyprogesterone caproate injection should not be used if you have:
- blood clots or other blood clotting problems now or in the past
- breast cancer or other hormone-sensitive cancers now or in the past
- unusual vaginal bleeding not related to your current pregnancy
- yellowing of your skin due to liver problems during your pregnancy
- liver problems, including liver tumors
- high blood pressure that is not controlled
What should I tell my healthcare provider before receiving hydroxyprogesterone caproate injection?
Before you receive hydroxyprogesterone caproate injection, tell your healthcare provider about all of your medical conditions, including if you have:
- a history of allergic reaction to hydroxyprogesterone caproate, castor oil, or any of the other ingredients in hydroxyprogesterone caproate injection, USP. See the end of this Patient Information leaflet for a complete list of ingredients in hydroxyprogesterone caproate injection, USP.
- diabetes or pre-diabetes.
- epilepsy (seizures).
- migraine headaches.
- asthma.
- heart problems.
- kidney problems.
- depression.
- high blood pressure.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
Hydroxyprogesterone caproate injection may affect the way other medicines work, and other medicines may affect how hydroxyprogesterone caproate injection works.
Know the medicines you take. Keep a list of them to show your healthcare provider and pharmacist when you get a new medicine.
How should I receive hydroxyprogesterone caproate injection?
- Do not give yourself hydroxyprogesterone caproate injections. A healthcare provider will give you the hydroxyprogesterone caproate injection 1 time each week (every 7 days) in the upper outer area of the buttocks as an injection into the muscle (intramuscular).
- You will start receiving hydroxyprogesterone caproate injections anytime from 16 weeks and 0 days of your pregnancy, up to 20 weeks and 6 days of your pregnancy.
- You will continue to receive hydroxyprogesterone caproate injections 1 time each week until week 37 (through 36 weeks and 6 days) of your pregnancy or when your baby is delivered, whichever comes first.
What are the possible side effects of hydroxyprogesterone caproate injection?
Hydroxyprogesterone caproate injection may cause serious side effects, including:
-
Blood clots. Symptoms of a blood clot may include:
- leg swelling
- redness in your leg
- a spot on your leg that is warm to the touch
- leg pain that gets worse when you bend your foot
Call your healthcare provider right away if you get any of the symptoms above during treatment with hydroxyprogesterone caproate injection.
- Allergic reactions. Symptoms of an allergic reaction may include:
- hives
- itching
- swelling of the face
Call your healthcare provider right away if you get any of the symptoms above during treatment with hydroxyprogesterone caproate injection.
- Decrease in glucose (blood sugar) tolerance. Your healthcare provider will need to monitor your blood sugar while taking hydroxyprogesterone caproate injection if you have diabetes or pre-diabetes.
- Your body may hold too much fluid (fluid retention).
- Depression.
- Yellowing of your skin and the whites of your eyes (jaundice).
- High blood pressure.
The most common side effects of hydroxyprogesterone caproate injection include:
- pain, swelling, itching or a hard bump at the injection site
- hives
- itching
- nausea
- diarrhea
Call your healthcare provider if you have the following at your injection site:
- increased pain over time
- oozing of blood or fluid
- swelling
Other side effects that may happen more often in women who receive hydroxyprogesterone caproate injection include:
- Miscarriage (pregnancy loss before 20 weeks of pregnancy)
- Stillbirth (fetal death occurring during or after the 20th week of pregnancy)
- Hospital admission for preterm labor
- Preeclampsia (high blood pressure and too much protein in your urine)
- Gestational hypertension (high blood pressure caused by pregnancy)
- Gestational diabetes
- Oligohydramnios (low amniotic fluid levels)
Tell your healthcare provider if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of hydroxyprogesterone caproate injection. For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store hydroxyprogesterone caproate injection?
Hydroxyprogesterone caproate injection vial for intramuscular use:
- Store the vial at room temperature between 68°F to 77°F (20°C to 25°C).
- Do not refrigerate or freeze.
- Protect the vial from light.
- Store the vial in its box in an upright position.
Keep hydroxyprogesterone caproate injection and all medicines out of the reach of children.
General information about the safe and effective use of hydroxyprogesterone caproate injection.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use hydroxyprogesterone caproate injection for a condition for which it was not prescribed. Do not give hydroxyprogesterone caproate injection to other people, even if they have the same symptoms you have. It may harm them.
This leaflet summarizes the most important information about hydroxyprogesterone caproate injection. If you would like more information, talk with your healthcare provider. You can ask your healthcare provider or pharmacist for information about hydroxyprogesterone caproate injection that is written for health professionals.
What are the ingredients in hydroxyprogesterone caproate injection?
Active ingredient: hydroxyprogesterone caproate
Inactive ingredients: castor oil and benzyl benzoate. 5 mL multi-dose vials also contain benzyl alcohol (a preservative).
Distributed by:
AuroMedics Pharma LLC
279 Princeton-Hightstown Rd.
E. Windsor, NJ 08520
Manufactured by:
Eugia Pharma Specialities Limited
Medchal-Malkajgiri District - 500101
India
For more information, go to www.auromedics.com or call AuroMedics Customer Service at the toll-free number 1-888-238-7880.
This Patient Information has been approved by the U.S. Food and Drug Administration.
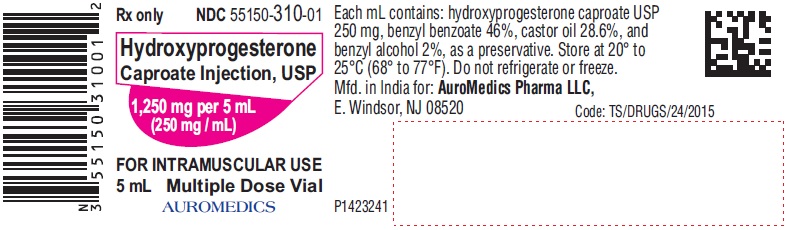
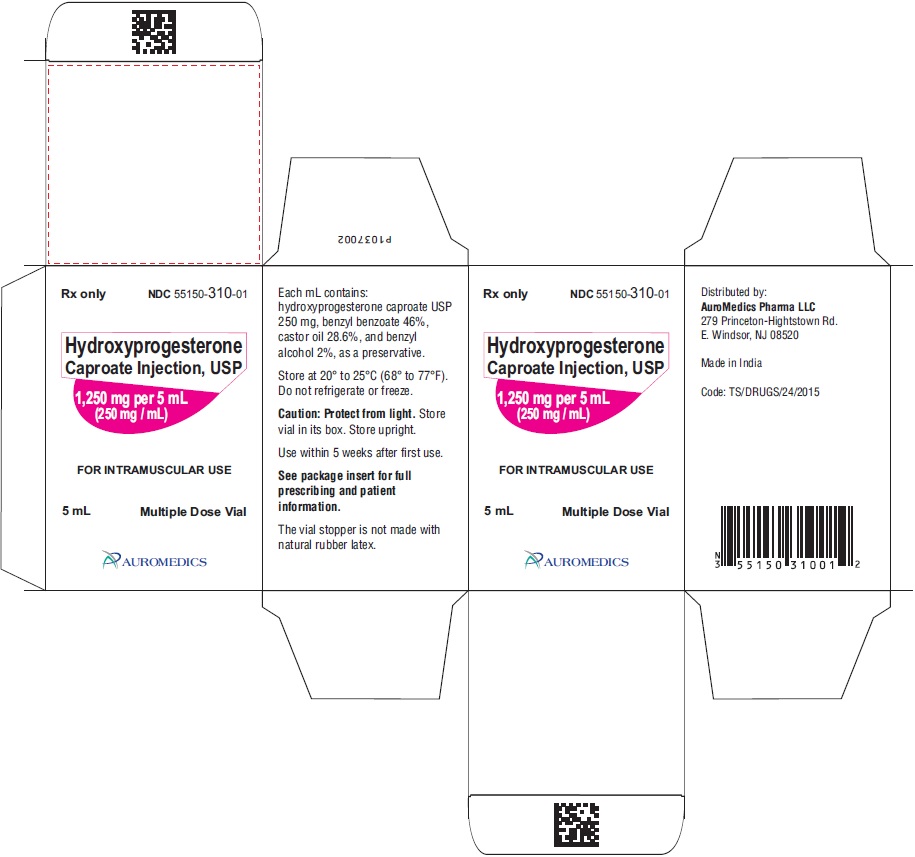
Revised: March 2019 - PACKAGE LABEL-PRINCIPAL DISPLAY PANEL - 1,250 mg per 5 mL (250 mg / mL) - Container Label
- PACKAGE LABEL-PRINCIPAL DISPLAY PANEL - 1,250 mg per 5 mL (250 mg / mL) – Container-Carton (1 vial)
-
INGREDIENTS AND APPEARANCE
HYDROXYPROGESTERONE CAPROATE
hydroxyprogesterone caproate injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 55150-310 Route of Administration INTRAMUSCULAR Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength HYDROXYPROGESTERONE CAPROATE (UNII: 276F2O42F5) (HYDROXYPROGESTERONE - UNII:21807M87J2) HYDROXYPROGESTERONE CAPROATE 1250 mg in 5 mL Inactive Ingredients Ingredient Name Strength CASTOR OIL (UNII: D5340Y2I9G) BENZYL BENZOATE (UNII: N863NB338G) BENZYL ALCOHOL (UNII: LKG8494WBH) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 55150-310-01 1 in 1 CARTON 04/16/2019 1 5 mL in 1 VIAL, MULTI-DOSE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA211070 04/16/2019 Labeler - AuroMedics Pharma LLC (968961354) Establishment Name Address ID/FEI Business Operations EUGIA Pharma Specialities Limited 872201704 ANALYSIS(55150-310) , MANUFACTURE(55150-310)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.