DANZITEN- nilotinib tablet
DANZITEN by
Drug Labeling and Warnings
DANZITEN by is a Prescription medication manufactured, distributed, or labeled by Azurity Pharmaceuticals, Inc., Catalent Pharma Solutions, LLC. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use DANZITEN safely and effectively. See full prescribing information for DANZITEN.
DANZITEN (nilotinib) tablets, for oral use
Initial U.S. Approval: 2007
WARNING: QT PROLONGATION and SUDDEN DEATHS
See full prescribing information for complete boxed warning.
Nilotinib prolongs the QT interval. Prior to DANZITEN administration and periodically, monitor for hypokalemia or hypomagnesemia and correct deficiencies. (5.3) Obtain ECGs to monitor the QTc at baseline, seven days after initiation, and periodically thereafter, and following any dose adjustments. (5.3, 5.4, 5.8, 5.12)
Sudden deaths have been reported in patients receiving nilotinib. (5.4) Do not administer DANZITEN to patients with hypokalemia, hypomagnesemia, or long QT syndrome. (4, 5.3)
Avoid use of concomitant drugs known to prolong the QT interval and strong CYP3A4 inhibitors. (7.1, 7.2)INDICATIONS AND USAGE
DANZITEN is a kinase inhibitor indicated for the treatment of:
Adult patients with newly diagnosed Philadelphia chromosome positive chronic myeloid leukemia (Ph+ CML) in chronic phase. (1.1)
Adult patients with chronic phase (CP) and accelerated phase (AP) Ph+ CML resistant to or intolerant to prior therapy that included imatinib. (1.2)DOSAGE AND ADMINISTRATION
To avoid medication errors and overdosage or under dosage, note that DANZITEN may have different strengths and dosages than other nilotinib products and may not be substitutable with other nilotinib products on a milligram per milligram basis. (2.1)
Recommended Adult Dose:
Newly diagnosed Ph+ CML-CP: 142 mg orally twice daily.
Resistant or intolerant Ph+ CML-CP and CML-AP: 190 mg orally twice daily. (2.2)
See Dosage and Administration for full dosing instructions and dose- reduction instructions for toxicity. (2.4, 2.5, 2.6, 2.7, 2.8, 2.9)
Reduce starting dose in patients with baseline hepatic impairment. (2.8)
Eligible newly diagnosed adult patients with Ph+ CML-CP who have received DANZITEN for a minimum of 3 years and have achieved a sustained molecular response (MR4.5) and patients with Ph+ CML-CP resistant or intolerant to imatinib who have received DANZITEN for at least 3 years and have achieved a sustained molecular response (MR4.5) may be considered for treatment discontinuation. (2.3, 2.4, 5.16)
DOSAGE FORMS AND STRENGTHS
Tablets: 71 mg, and 95 mg (3)
CONTRAINDICATIONS
DANZITEN is contraindicated in patients with hypokalemia, hypomagnesemia, or long QT syndrome. (4)
WARNINGS AND PRECAUTIONS
Substitution with Other Nilotinib Products and Risk of Medication Errors: DANZITEN (nilotinib) tablets may not be substitutable with other nilotinib products, including other nilotinib tablets, on a milligram per milligram basis. Confirm that the intended nilotinib product is being prescribed and dispensed. (5.1)
Myelosuppression: Monitor complete blood count (CBC) during therapy and manage by treatment interruption or dose reduction. (5.2)
Cardiac and Arterial Vascular Occlusive Events: Evaluate cardiovascular status, monitor and manage cardiovascular risk factors during DANZITEN therapy. (5.5)
Pancreatitis and Elevated Serum Lipase: Monitor serum lipase; if elevations are accompanied by abdominal symptoms, interrupt doses and consider appropriate diagnostics to exclude pancreatitis. (5.6)
Hepatotoxicity: Monitor hepatic function tests monthly or as clinically indicated. (5.7)
Electrolyte Abnormalities: DANZITEN can cause hypophosphatemia, hypokalemia, hyperkalemia, hypocalcemia, and hyponatremia. Correct electrolyte abnormalities prior to initiating DANZITEN and monitor periodically during therapy. (5.8)
Tumor Lysis Syndrome: Maintain adequate hydration and correct uric acid levels prior to initiating therapy with DANZITEN. (5.9)
Hemorrhage: Hemorrhage from any site may occur. Advise patients to report signs and symptoms of bleeding and medically manage as needed. (5.10)
Fluid Retention: Monitor patients for unexpected rapid weight gain, swelling, and shortness of breath. Manage medically. (5.13)
Effects on Growth and Development in Pediatric Patients: Growth retardation has been reported in pediatric patients treated with nilotinib. Monitor growth and development in pediatric patients. (5.14)
Embryo-Fetal Toxicity: Can cause fetal harm. Advise females of reproductive potential of potential risk to a fetus and to use effective contraception. (5.15, 8.1,8.3)
Treatment Discontinuation: Patients must have typical BCR-ABL transcripts. An FDA-authorized test with a detection limit below MR4.5 must be used to determine eligibility for discontinuation. Patients must be frequently monitored by the FDA authorized test to detect possible loss of remission. (5.16)ADVERSE REACTIONS
The most commonly reported non-hematologic adverse reactions (≥ 20%) in adult patients are nausea, rash, headache, fatigue, pruritus, vomiting, diarrhea, cough, constipation, arthralgia, nasopharyngitis, pyrexia, and night sweats. Hematologic adverse drug reactions include myelosuppression: thrombocytopenia, neutropenia, and anemia. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Azurity Pharmaceuticals, Inc., at 1-800-461-7449 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.DRUG INTERACTIONS
Strong CYP3A Inhibitors: Avoid concomitant use with DANZITEN or reduce DANZITEN dose if concomitant use cannot be avoided. (7.1)
Strong CYP3A Inducers: Avoid concomitant use with DANZITEN. (7.1)
Proton Pump Inhibitors: Use short-acting antacids or H2 blockers as an alternative to proton pump inhibitors. (7.1)USE IN SPECIFIC POPULATIONS
Lactation: Advise women not to breastfeed. (8.2)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 11/2024
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: QT PROLONGATION and SUDDEN DEATHS
1 INDICATIONS AND USAGE
1.1 Adult Patients with Newly Diagnosed Ph+ CML-CP
1.2 Adult Patients with Resistant or Intolerant Ph+ CML-CP and CML-AP
2 DOSAGE AND ADMINISTRATION
2.1 Important Use and Administration Instructions
2.2 Recommended Dosage and Administration
2.3 Discontinuation of Treatment After a Sustained Molecular Response (MR4.5) on DANZITEN
2.4 Reinitiation of Treatment in Patients Who Lose Molecular Response After Discontinuation of Therapy with DANZITEN
2.5 Dosage Modification for QT Interval Prolongation
2.6 Dosage Modifications for Myelosuppression
2.7 Dosage Modifications for Selected Non-Hematologic Laboratory Abnormalities and Other Toxicities
2.8 Recommended DANZITEN Dosage in Patients with Hepatic Impairment
2.9 Dosage Modification for Strong CYP3A4 Inhibitors
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Substitution with Other Nilotinib Products and Risk of Medication Errors
5.2 Myelosuppression
5.3 QT Prolongation
5.4 Sudden Deaths
5.5 Cardiac and Arterial Vascular Occlusive Events
5.6 Pancreatitis and Elevated Serum Lipase
5.7 Hepatotoxicity
5.8 Electrolyte Abnormalities
5.9 Tumor Lysis Syndrome
5.10 Hemorrhage
5.11 Total Gastrectomy
5.12 Monitoring Laboratory Tests
5.13 Fluid Retention
5.14 Effects on Growth and Development
5.15 Embryo-Fetal Toxicity
5.16 Monitoring of BCR-ABL Transcript Levels
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Effect of Other Drugs on DANZITEN
7.2 Drugs that Prolong the QT Interval
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Cardiac Disorders
8.7 Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
12.5 Pharmacogenomics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Adult Newly Diagnosed Ph+ CML-CP
14.2 Adult Patients with Resistant or Intolerant Ph+ CML-CP and CML-AP
14.3 Treatment Discontinuation in Newly Diagnosed Ph+ CML-CP Patients Who Have Achieved a Sustained Molecular Response (MR4.5)
14.4 Treatment Discontinuation in Ph+ CML-CP Patients Who Have Achieved a Sustained Molecular Response (MR4.5) on DANZITEN Following Prior Imatinib Therapy
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: QT PROLONGATION and SUDDEN DEATHS
Nilotinib prolongs the QT interval. Prior to DANZITEN administration and periodically, monitor for hypokalemia or hypomagnesemia and correct deficiencies [see Warnings and Precautions (5.3)]. Obtain ECGs to monitor the QTc at baseline, seven days after initiation, and periodically thereafter, and following any dose adjustments [see Warnings and Precautions (5.3, 5.4, 5.8, 5.12)].
Sudden deaths have been reported in patients receiving nilotinib [see Warnings and Precautions (5.4)]. Do not administer DANZITEN tablets to patients with hypokalemia, hypomagnesemia, or long QT syndrome [see Contraindications (4), Warnings and Precautions (5.3)].
Avoid use of concomitant drugs known to prolong the QT interval and strong CYP3A4 inhibitors [see Drug Interactions (7.1, 7.2)]. -
1 INDICATIONS AND USAGE
1.1 Adult Patients with Newly Diagnosed Ph+ CML-CP
DANZITEN is indicated for the treatment of adult patients with newly diagnosed Philadelphia chromosome positive chronic myeloid leukemia (Ph+ CML) in chronic phase.
Additional pediatric use information is approved for Novartis Pharmaceuticals Corporation’s Tasigna® (nilotinib) capsules. However, due to Novartis Pharmaceuticals Corporation’s marketing exclusivity rights, this drug product is not labeled with that pediatric information.1.2 Adult Patients with Resistant or Intolerant Ph+ CML-CP and CML-AP
DANZITEN is indicated for the treatment of adult patients with chronic phase and accelerated phase Philadelphia chromosome positive chronic myelogenous leukemia (Ph+ CML) resistant or intolerant to prior therapy that included imatinib.
Additional pediatric use information is approved for Novartis Pharmaceuticals Corporation’s Tasigna® (nilotinib) capsules. However, due to Novartis Pharmaceuticals Corporation’s marketing exclusivity rights, this drug product is not labeled with that pediatric information. -
2 DOSAGE AND ADMINISTRATION
2.1 Important Use and Administration Instructions
Nilotinib is available in different formulations, dosage forms, and strengths that are approved with different indications and recommended dosages.
DANZITEN may not be substitutable with other nilotinib products on a milligram per milligram basis; to avoid medication errors, including overdosage or underdosage, when using DANZITEN ensure that the recommended dosage of DANZITEN (not the recommended dosage of other nilotinib products) is prescribed [see Dosage and Administration (2.2) and Warnings and Precautions (5.1)].
When switching between DANZITEN (nilotinib) tablets and Tasigna (nilotinib) capsules, use the dosage conversion table [see Dosage and Administration (2.2)].2.2 Recommended Dosage and Administration
Dosage in Adult Patients with Newly Diagnosed Ph+ CML-CP
The recommended dosage of DANZITEN is 142 mg orally twice daily at approximately 12-hour intervals with or without food [see Clinical Pharmacology (12.3)].
Dosage in Adult Patients with Resistant or Intolerant Ph+ CML-CP and CML-AP
The recommended dosage of DANZITEN is 190 mg orally twice daily at approximately 12-hour intervals with or without food [see Clinical Pharmacology (12.3)].
Additional Administration Instructions
Advise patients to swallow the tablets whole with water and not to cut, crush, or chew the tablets [see Boxed Warning]. If a dose of DANZITEN is missed, the patient should take the next scheduled dose at its regular time. The patient should not take two doses at the same time.
Switching Instructions
Use Table 1 when switching between DANZITEN and Tasigna based on dosage equivalence.
Table 1 Recommendations for Switching between DANZITEN and Tasigna
Approved Indications
DANZITEN dosage
Tasigna dosage
Newly diagnosed Ph+ CML-CP
142 mg orally twice daily
300 mg orally twice daily
Resistant or intolerant Ph+ CML-CP and CML-AP
190 mg orally twice daily
400 mg orally twice daily
Optional Concomitant Therapy
DANZITEN may be given in combination with hematopoietic growth factors, such as erythropoietin or G-CSF if clinically indicated. DANZITEN may be given with hydroxyurea or anagrelide if clinically indicated.
Additional pediatric use information is approved for Novartis Pharmaceuticals Corporation’s Tasigna (nilotinib) capsules. However, due to Novartis Pharmaceuticals Corporation’s marketing exclusivity rights, this drug product is not labeled with that pediatric information.2.3 Discontinuation of Treatment After a Sustained Molecular Response (MR4.5) on DANZITEN
Patient Selection
Eligibility for Discontinuation of Treatment
Ph+ CML-CP patients with typical BCR-ABL transcripts, who have been taking DANZITEN for a minimum of 3 years and have achieved a sustained molecular response (MR4.5, corresponding to = BCR-ABL/ABL ≤ 0.0032% IS), may be eligible for treatment discontinuation [see Clinical Studies (14.3, 14.4)]. Information on FDA authorized tests for the detection and quantitation of BCR-ABL transcripts to determine eligibility for treatment discontinuation is available at http://www.fda.gov/CompanionDiagnostics.
Patients with typical BCR-ABL transcripts (e13a2/b2a2 or e14a2/b3a2), who achieve the sustained MR4.5 criteria, are eligible for discontinuation of DANZITEN. Patients must continue to be monitored for possible loss of molecular remission after treatment discontinuation. Use the same FDA-authorized test to consistently monitor molecular response levels while on and off treatment.
Consider discontinuation in patients with newly diagnosed Ph+ CML-CP who have:
been treated with DANZITEN for at least 3 years
maintained a molecular response of at least MR4.0 (corresponding to = BCR-ABL/ABL ≤ 0.01% IS) for one year prior to discontinuation of therapy
achieved an MR4.5 for the last assessment taken immediately prior to discontinuation of therapy
been confirmed to express the typical BCR-ABL transcripts (e13a2/b2a2 or e14a2/b3a2)
no history of accelerated phase or blast crisis
no history of prior attempts of treatment-free remission discontinuation that resulted in relapse.
Consider discontinuation in patients with Ph+ CML-CP that are resistant or intolerant to imatinib who have achieved a sustained molecular response (MR4.5) on DANZITEN who have:
been treated with DANZITEN for a minimum of 3 years
been treated with imatinib only prior to treatment with DANZITEN
achieved a molecular response of MR4.5 (corresponding to = BCR-ABL/ABL ≤ 0.0032% IS)
sustained an MR4.5 for a minimum of one year immediately prior to discontinuation of therapy
been confirmed to express the typical BCR-ABL transcripts (e13a2/b2a2 or e14a2/b3a2)
no history of accelerated phase or blast crisis
no history of prior attempts of treatment-free remission discontinuation that resulted in relapse.
Monitor BCR-ABL transcript levels and complete blood count (CBC) with differential in patients who have discontinued DANZITEN therapy monthly for one year, then every 6 weeks for the second year, and every 12 weeks thereafter [see Warnings and Precautions (5.16)].
Upon the loss of MR4.0 (corresponding to = BCR-ABL/ABL ≤ 0.01% IS) during the treatment-free phase, monitor BCR-ABL transcript levels every 2 weeks until BCR-ABL levels remain lower than major molecular response [(MMR), corresponding to MR3.0 or = BCR-ABL/ABL ≤ 0.1% IS] for 4 consecutive measurements. The patient can then proceed to the original monitoring schedule.2.4 Reinitiation of Treatment in Patients Who Lose Molecular Response After Discontinuation of Therapy with DANZITEN
Newly diagnosed patients who lose MMR must reinitiate treatment within 4 weeks at the dose level prior to discontinuation of therapy [see Warnings and Precautions (5.16)]. Patients who reinitiate DANZITEN therapy should have their BCR-ABL transcript levels monitored monthly until major molecular response is re-established and every 12 weeks thereafter.
Patients resistant or intolerant to prior treatment that included imatinib with confirmed loss of MR4.0 (2 consecutive measures separated by at least 4 weeks showing loss of MR4.0) or loss of MMR must reinitiate treatment within 4 weeks at the dose level prior to discontinuation of therapy [see Warnings and Precautions (5.16)]. Patients who reinitiate DANZITEN therapy should have their BCR-ABL transcript levels monitored monthly until previous major molecular response or MR4.0 is re-established and every 12 weeks thereafter.2.5 Dosage Modification for QT Interval Prolongation
See Table 2 for dose adjustments for QT interval prolongation [see Warnings and Precautions (5.3) and Clinical Pharmacology (12.2)].
Table 2. Dosage Adjustments for Adult Patients with QT Prolongation
Degree of QTc Prolongation Dosage Adjustment ECGs with a QTc greater than 480 msec 1. Withhold DANZITEN, and perform an analysis of serum potassium and magnesium, and if below lower limit of normal, correct with supplements to within normal limits. Concomitant medication usage must be reviewed.
2. Resume within 2 weeks at prior dose if QTcF returns to less than 450 msec and to within 20 msec of baseline.
3. If QTcF is between 450 msec and 480 msec after 2 weeks, reduce the dose to 190 mg once daily in adults.
4. Discontinue DANZITEN if, following dose-reduction to 190 mg once daily in adults, QTcF returns to greater than 480 msec.
5. An ECG should be repeated approximately 7 days after any dose adjustment.Abbreviation: ECG, electrocardiogram. Additional pediatric use information is approved for Novartis Pharmaceuticals Corporation’s Tasigna® (nilotinib) capsules. However, due to Novartis Pharmaceuticals Corporation’s marketing exclusivity rights, this drug product is not labeled with that pediatric information.
2.6 Dosage Modifications for Myelosuppression
Withhold or reduce DANZITEN dosage for hematological toxicities (neutropenia, thrombocytopenia) that are not related to underlying leukemia (Table 3) [see Warnings and Precautions (5.2)].
Table 3. Dosage Adjustments for Neutropenia and Thrombocytopenia
Diagnosis Degree of Myelosuppression Dosage Adjustment Adult patients with:
Newly diagnosed Ph+ CML in chronic phase at 142 mg twice daily
Resistant or intolerant Ph+ CML in chronic phase or accelerated phase at 190 mg twice dailyANC less than 1 x 109/L and/or platelet counts less than 50 x 109/L 1. Stop DANZITEN and monitor blood counts.
2. Resume within 2 weeks at prior dose if ANC greater than 1 x 109/L and platelets greater than 50 x 109/L.
3. If blood counts remain low for greater than 2 weeks, reduce the dose to 190 mg once daily.Abbreviations: ANC, absolute neutrophil count; Ph+ CML, Philadelphia chromosome positive chronic myeloid leukemia. Additional pediatric use information is approved for Novartis Pharmaceuticals Corporation’s Tasigna® (nilotinib) capsules. However, due to Novartis Pharmaceuticals Corporation’s marketing exclusivity rights, this drug product is not labeled with that pediatric information.
2.7 Dosage Modifications for Selected Non-Hematologic Laboratory Abnormalities and Other Toxicities
See Table 4 for dosage adjustments for elevations of lipase, amylase, bilirubin, and/or hepatic transaminases. [see Warnings and Precautions (5.6, 5.7) and Adverse Reactions (6.1)].
Table 4. Dosage Adjustments for Selected Non-Hematologic Laboratory AbnormalitiesDegree of Non- Hematologic Laboratory Abnormality Dosage Adjustment Elevated serum lipase or amylase greater than or equal to Grade 3 Adult patients:
1. Withhold DANZITEN and monitor serum lipase or amylase.
2. Resume treatment at 190 mg once daily if serum lipase or amylase returns to less than or equal to Grade 1.Elevated bilirubin greater than or equal to Grade 3 in adult patients Adult patients:
1. Withhold DANZITEN and monitor bilirubin.
2. Resume treatment at 190 mg once daily if bilirubin returns to less than or equal to Grade 1.Elevated hepatic transaminases greater than or equal to Grade 3 Adult patients:
1. Withhold DANZITEN and monitor hepatic transaminases.
2. Resume treatment at 190 mg once daily if hepatic transaminases return to less than or equal to Grade 1.If clinically significant moderate or severe non-hematologic toxicity develops (including medically severe fluid retention), see Table 5 for dosage adjustments [see Adverse Reactions (6.1)].
Table 5. Dosage Adjustments for Other Non-Hematologic Toxicities
Degree of “Other Non-Hematologic Toxicity” Dosage Adjustment Other clinically moderate or severe non- hematologic toxicity Adult patients:
1. Withhold DANZITEN until toxicity has resolved.
2. Resume treatment at 190 mg once daily if previous dose was 142 mg twice daily in adult patients newly diagnosed with CML-CP or 190 mg twice daily in adult patients with resistant or intolerant CML-CP and CML-AP.
3. Discontinue treatment if the prior dose was 190 mg once daily in adult patients
4. If clinically appropriate, consider re-escalation of the dose to 142 mg (newly diagnosed Ph+ CML-CP) or 190 mg (resistant or intolerant Ph+ CML-CP and CML- AP) twice daily.Abbreviations: CML-AP, chronic myeloid leukemia-accelerated phase; CML-CP, chronic myeloid leukemia-chronic phase; Ph+, Philadelphia chromosome positive. Additional pediatric use information is approved for Novartis Pharmaceuticals Corporation’s Tasigna® (nilotinib) capsules. However, due to Novartis Pharmaceuticals Corporation’s marketing exclusivity rights, this drug product is not labeled with that pediatric information.
2.8 Recommended DANZITEN Dosage in Patients with Hepatic Impairment
If possible, consider alternative therapies. If DANZITEN must be administered to patients with hepatic impairment, the recommended DANZITEN dosage is provided in Table 6. [see Use in Specific Populations (8.7)]
Table 6. Recommended DANZITEN Dosage in Patients with Hepatic Impairment
Diagnosis Degree of Hepatic Impairment DANZITEN Dosage Newly diagnosed Ph+ CML in chronic phase Mild (Child-Pugh A), Moderate (Child-Pugh B), or Severe (Child- Pugh C) Reduce DANZITEN dosage to 95 mg twice daily. Increase DANZITEN dosage to 142 mg twice daily based on tolerability. Resistant or intolerant Ph+ CML in chronic phase or accelerated phase Mild or Moderate Reduce DANZITEN dosage to 142 mg twice daily. Increase DANZITEN dosage to 190 mg twice daily based on tolerability. Severe Reduce DANZITEN dosage to 95 mg twice daily. Increase DANZITEN dosage to 142 mg twice daily and then to 190 mg twice daily based on tolerability. 2.9 Dosage Modification for Strong CYP3A4 Inhibitors
Avoid the concomitant use of strong CYP3A4 inhibitors. Should treatment with any of these agents be required, interrupt therapy with DANZITEN.
If concomitant use is required, reduce DANZITEN dosage to 142 mg once daily in patients with resistant or intolerant Ph+ CML or to 95 mg once daily in patients with newly diagnosed Ph+ CML-CP. If the strong inhibitor is discontinued, allow a washout period of 5 half-lives before adjusting DANZITEN dose upward to the indicated dose. For patients who cannot avoid use of strong CYP3A4 inhibitors, monitor closely for prolongation of the QT interval [see Boxed Warning, Warnings and Precautions (5.3), Drug Interactions (7.1, 7.2), Clinical Pharmacology (12.3)]. - 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
DANZITEN is contraindicated in patients with hypokalemia, hypomagnesemia, or long QT syndrome [see Boxed Warning and Warnings and Precautions (5.3)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Substitution with Other Nilotinib Products and Risk of Medication Errors
Nilotinib is available in different formulations, recommended dosages, and tablet strengths, and for different indications. DANZITEN (nilotinib) tablets may not be substitutable with other nilotinib products, including other nilotinib tablets, on a milligram per milligram basis. When switching patients between other nilotinib products and DANZITEN (nilotinib) tablets, a dose conversion may be required [see Dosage and Administration (2.1 and 2.2)]. Substitution of DANZITEN (nilotinib) tablets for another nilotinib product to achieve the same daily nilotinib dosage on a milligram per milligram basis may result in a clinically significant:
Increase in nilotinib exposure which may increase the risk of nilotinib-associated adverse reactions.
Decrease in nilotinib exposure which may reduce DANZITEN effectiveness.
Confirm that the intended nilotinib product is being prescribed and dispensed.5.2 Myelosuppression
Treatment with DANZITEN can cause Grade 3/4 thrombocytopenia, neutropenia, and anemia. Perform CBCs every 2 weeks for the first 2 months and then monthly thereafter, or as clinically indicated. Myelosuppression was generally reversible and usually managed by withholding DANZITEN temporarily or dose reduction [see Dosage and Administration (2.6)].
5.3 QT Prolongation
Nilotinib has been shown to prolong cardiac ventricular repolarization as measured by the QT interval on the surface electrocardiogram (ECG) in a concentration-dependent manner [see Adverse Reactions (6.1), Clinical Pharmacology (12.2)]. Prolongation of the QT interval can result in a type of ventricular tachycardia called torsade de pointes, which may result in syncope, seizure, and/or death. Electrocardiograms should be performed at baseline, 7 days after initiation of DANZITEN, and periodically as clinically indicated and following dose adjustments [see Dosage and Administration (2.5) and Warnings and Precautions (5.12)].
DANZITEN should not be used in patients who have hypokalemia, hypomagnesemia, or long QT syndrome. Before initiating DANZITEN and periodically, test electrolyte, calcium, and magnesium blood levels. Hypokalemia or hypomagnesemia must be corrected prior to initiating DANZITEN and these electrolytes should be monitored periodically during therapy [see Warnings and Precautions (5.12)].
Significant prolongation of the QT interval may occur when DANZITEN is inappropriately taken with strong CYP3A4 inhibitors and/or medicinal products with a known potential to prolong QT. Therefore, avoid concomitant DANZITEN use with strong CYP3A4 inhibitors and/or medicinal products with a known potential to prolong QT [see Dosage and Administration (2.9), Drug Interactions (7.1, 7.2)]. The presence of hypokalemia and hypomagnesemia may further prolong the QT interval [see Warnings and Precautions (5.8, 5.12)].5.4 Sudden Deaths
Sudden deaths have been reported in 0.3% of patients with CML treated with nilotinib in clinical studies of 5661 patients. The relative early occurrence of some of these deaths relative to the initiation of nilotinib suggests the possibility that ventricular repolarization abnormalities may have contributed to their occurrence.
5.5 Cardiac and Arterial Vascular Occlusive Events
Cardiovascular events, including arterial vascular occlusive events, were reported in a randomized, clinical trial in newly diagnosed CML patients and observed in the postmarketing reports of patients receiving nilotinib therapy [see Adverse Reactions (6.1)]. With a median time on therapy of 60 months in the clinical trial, cardiovascular events, including arterial vascular occlusive events, occurred in 9% and 15% of patients receiving nilotinib dosages equivalent to DANZITEN 142 mg and 190 mg twice daily, respectively, and in 3.2% in the imatinib arm. These included cases of cardiovascular events, including ischemic heart disease-related cardiac events (5% and 9% in the nilotinib dosages equivalent to DANZITEN 142 mg and 190 mg twice daily, respectively and 2.5% in the imatinib arm), peripheral arterial occlusive disease (3.6% and 2.9% in the nilotinib dosages equivalent to DANZITEN 142 mg and 190 mg twice daily, respectively and 0% in the imatinib arm), and ischemic cerebrovascular events (1.4% and 3.2% in the nilotinib dosages equivalent to DANZITEN 142 mg and 190 mg twice daily, respectively and 0.7% in the imatinib arm). If acute signs or symptoms of cardiovascular events occur, advise patients to seek immediate medical attention. The cardiovascular status of patients should be evaluated, and cardiovascular risk factors should be monitored and actively managed during DANZITEN therapy according to standard guidelines [see Dosage and Administration (2.5)].
5.6 Pancreatitis and Elevated Serum Lipase
Nilotinib can cause increases in serum lipase [see Adverse Reactions (6.1)]. Patients with a previous history of pancreatitis may be at greater risk of elevated serum lipase. If lipase elevations are accompanied by abdominal symptoms, interrupt dosing and consider appropriate diagnostics to exclude pancreatitis [see Dosage and Administration (2.7)]. Test serum lipase levels monthly or as clinically indicated.
5.7 Hepatotoxicity
Nilotinib may result in hepatotoxicity as measured by elevations in bilirubin, aspartate aminotransferase (AST), alanine aminotransferase (ALT), and alkaline phosphatase. Grade 3-4 elevations of bilirubin, AST, and ALT were reported in adult patients. Grade 3-4 elevations of bilirubin, AST, and ALT were reported at a higher frequency in pediatric than in adult patients. Monitor hepatic function tests monthly or as clinically indicated [see Warnings and Precautions (5.12)] and following dose adjustments. [see Dosage and Administration (2.8)].
5.8 Electrolyte Abnormalities
The use of nilotinib can cause hypophosphatemia, hypokalemia, hyperkalemia, hypocalcemia, and hyponatremia. Correct electrolyte abnormalities prior to initiating DANZITEN and during therapy. Monitor these electrolytes periodically during therapy [see Warnings and Precautions (5.12)].
5.9 Tumor Lysis Syndrome
Tumor lysis syndrome (TLS) cases have been reported in nilotinib treated patients with resistant or intolerant CML. Malignant disease progression, high white blood cell (WBC) counts and/or dehydration were present in the majority of these cases. Due to potential for TLS, maintain adequate hydration and correct uric acid levels prior to initiating therapy with DANZITEN.
5.10 Hemorrhage
Serious hemorrhagic events, including fatal events, have occurred in patients with CML treated with nilotinib. In a randomized trial in patients with newly diagnosed Ph+ CML in chronic phase comparing nilotinib and imatinib, Grade 3 or 4 hemorrhage occurred in 1.1% of patients in the nilotinib dosage equivalent to DANZITEN 142 mg twice daily arm, in 1.8% of patients in the nilotinib dosage equivalent to DANZITEN 190 mg twice daily arm, and 0.4% of patients in the imatinib arm. GI hemorrhage occurred in 2.9% and 5% of patients in the nilotinib dosage equivalent DANZITEN 142 mg and 190 mg twice daily arms and in 1.4% of patients in the imatinib arm, respectively. Grade 3 or 4 events occurred in 0.7% and 1.4% of patients in the nilotinib dosage equivalent to DANZITEN 142 mg and 190 mg twice daily arms, respectively, and in no patients in the imatinib arm. Monitor for signs and symptoms of bleeding and medically manage as needed.
5.11 Total Gastrectomy
Since the exposure of nilotinib is reduced in patients with total gastrectomy, perform more frequent monitoring of these patients. Consider dose increase or alternative therapy in patients with total gastrectomy [see Clinical Pharmacology (12.3)].
5.12 Monitoring Laboratory Tests
Complete blood counts should be performed every 2 weeks for the first 2 months and then monthly thereafter. Perform chemistry panels, including electrolytes, calcium, magnesium, liver enzymes, lipid profile, and glucose prior to therapy and periodically. Electrocardiograms should be obtained at baseline, 7 days after initiation and periodically thereafter, as well as following dose adjustments [see Warnings and Precautions (5.3)]. Monitor lipid profiles and glucose periodically during the first year of DANZITEN therapy and at least yearly during chronic therapy. Should treatment with any HMG-CoA reductase inhibitor (a lipid lowering agent) be needed to treat lipid elevations, evaluate the potential for a drug-drug interaction before initiating therapy as certain HMG-CoA reductase inhibitors are metabolized by the CYP3A4 pathway [see Drug Interactions (7.1)]. Assess glucose levels before initiating treatment with DANZITEN and monitor during treatment as clinically indicated. If test results warrant therapy, physicians should follow their local standards of practice and treatment guidelines.
5.13 Fluid Retention
In the randomized trial in patients with newly diagnosed Ph+ CML in chronic phase, severe (Grade 3 or 4) fluid retention occurred in 3.9% and 2.9% of patients receiving the nilotinib dosage equivalent to DANZITEN 142 mg and 190 mg twice daily, respectively, and in 2.5% of patients receiving imatinib. Effusions (including pleural effusion, pericardial effusion, ascites) or pulmonary edema, were observed in 2.2% and 1.1% of patients receiving the nilotinib dosage equivalent to the recommended dosage of DANZITEN 142 mg twice daily and 190 mg twice daily, respectively, and in 2.1% of patients receiving imatinib. Effusions were severe (Grade 3 or 4) in 0.7% and 0.4% of patients receiving the nilotinib dosage equivalent to the recommended dosage of DANZITEN 142 mg and 190 mg twice daily, respectively, and in no patients receiving imatinib. Similar events were also observed in postmarketing reports. Monitor patients for signs of severe fluid retention (e.g., unexpected rapid weight gain or swelling) and for symptoms of respiratory or cardiac compromise (e.g., shortness of breath) during DANZITEN treatment; evaluate etiology and treat patients accordingly.
5.14 Effects on Growth and Development
Growth retardation has been reported in pediatric patients with Ph+ CML in chronic phase treated with nilotinib. Growth deceleration was more pronounced in children who were less than age 12 at baseline. Monitor growth and development in pediatric patients receiving nilotinib treatment.
Additional pediatric use information is approved for Novartis Pharmaceuticals Corporation’s Tasigna® (nilotinib) capsules. However, due to Novartis Pharmaceuticals Corporation’s marketing exclusivity rights, this drug product is not labeled with that pediatric information.5.15 Embryo-Fetal Toxicity
Based on findings from animal studies and its mechanism of action, DANZITEN can cause fetal harm when administered to a pregnant woman. In animal reproduction studies, administration of nilotinib to pregnant rats and rabbits during organogenesis caused adverse developmental outcomes, including embryo-fetal lethality/fetal effects (small renal papilla, fetal edema, and skeletal variations) in rats and increased resorptions of fetuses and fetal skeletal variations in rabbits at maternal area under the curve (AUCs) approximately 2 and 0.5 times, respectively, the AUC in patients receiving the recommended dose.
Advise pregnant women of the potential risk to a fetus. Advise females of reproductive potential to use effective contraception during treatment and for 14 days after the last dose [see Use in Specific Populations (8.1, 8.3), Clinical Pharmacology (12.1)].5.16 Monitoring of BCR-ABL Transcript Levels
Monitoring of BCR-ABL Transcript Levels in Patients Who Discontinued Nilotinib
Monitor BCR-ABL transcript levels in patients eligible for treatment discontinuation using an FDA authorized test validated to measure molecular response levels with a sensitivity of at least MR4.5 (BCR-ABL/ABL ≤ 0.0032% IS). In patients who discontinue DANZITEN therapy, assess BCR-ABL transcript levels monthly for one year, then every 6 weeks for the second year, and every 12 weeks thereafter during treatment discontinuation [see Clinical Studies (14.3,14.4), Dosage and Administration (2.3)].
Newly diagnosed patients must reinitiate DANZITEN therapy within 4 weeks of a loss of major molecular response [(MMR), corresponding to MR3.0 or = BCR-ABL/ABL ≤ 0.1% IS].
Patients resistant or intolerant to prior treatment which included imatinib must reinitiate DANZITEN therapy within 4 weeks of a loss of MMR or confirmed loss of MR4.0 (two consecutive measures separated by at least 4 weeks showing loss of MR4.0, corresponding to = BCR-ABL/ABL ≤ 0.01% IS).
For patients who fail to achieve MMR after three months of treatment reinitiation, BCR-ABL kinase domain mutation testing should be performed.
Monitoring of BCR-ABL Transcript Levels in Patients Who Have Reinitiated Therapy After Loss of Molecular Response
Monitor CBC and BCR-ABL transcripts in patients who reinitiate treatment with DANZITEN due to loss of molecular response quantitation every 4 weeks until a major molecular response is re-established, then every 12 weeks [see Dosage and Administration (2.4)]. -
6 ADVERSE REACTIONS
The following clinically significant adverse reactions can occur with DANZITEN and are discussed in greater detail in other sections of labeling:
Myelosuppression [see Warnings and Precautions (5.2)]
QT Prolongation [see Boxed Warning, Warnings and Precautions (5.3)]
Sudden Deaths [see Boxed Warning, Warnings and Precautions (5.4)]
Cardiac and Arterial Vascular Occlusive Events [see Warnings and Precautions (5.5)]
Pancreatitis and Elevated Serum Lipase [see Warnings and Precautions (5.6)]
Hepatotoxicity [see Warnings and Precautions (5.7)]
Electrolyte Abnormalities [see Boxed Warning, Warnings and Precautions (5.8)]
Hemorrhage [see Warnings and Precautions (5.10)]
Fluid Retention [see Warnings and Precautions (5.13)]6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The safety of DANZITEN (nilotinib) tablets has been established from adequate and well-controlled studies of Tasigna® (nilotinib) capsules, which has different recommended dosages than DANZITEN, in adult patients with newly diagnosed Philadelphia chromosome positive chronic myeloid leukemia (Ph+ CML) in chronic phase (CP) and adult patients with CP and accelerated phase (AP) Ph+ CML resistant to or intolerant to prior therapy that included imatinib [see Clinical Studies (14)]. Below is a display of the adverse reactions of Tasigna® (nilotinib) capsules in these adequate and well-controlled studies.
In Adult Patients With Newly Diagnosed Ph+ CML-CP
The data below reflect exposure to nilotinib from a randomized trial in patients with newly diagnosed Ph+ CML in chronic phase treated at the equivalent recommended dosage of DANZITEN 142 mg twice daily (n = 279). The median time on treatment at the equivalent recommended dosage of DANZITEN 142 mg twice daily group was 61 months (range, 0.1 to 71 months).
The most common (greater than 10%) non-hematologic adverse drug reactions were rash, pruritus, headache, nausea, fatigue, alopecia, myalgia, and upper abdominal pain. Constipation, diarrhea, dry skin, muscle spasms, arthralgia, abdominal pain, peripheral edema, vomiting, and asthenia were observed less commonly (less than or equal to 10% and greater than 5%).
Increase in QTcF greater than 60 msec from baseline was observed in 1 patient (0.4%) at the equivalent recommended dosage of DANZITEN 142 mg twice daily treatment group. No patient had an absolute QTcF of greater than 500 msec while on study drug.
The most common hematologic adverse drug reactions (all Grades) were myelosuppression, including: thrombocytopenia (18%), neutropenia (15%), and anemia (8%). See Table 10 for Grade 3/4 laboratory abnormalities.
Discontinuation due to adverse reactions, regardless of relationship to study drug, was observed in 10% of patients.
In Adult Patients With Resistant or Intolerant Ph+ CML-CP and CML-AP
In the single-arm, open-label multicenter clinical trial, a total of 458 patients with Ph+ CML-CP and CML-AP resistant to or intolerant to at least one prior therapy, including imatinib were treated (CML-CP = 321; CML-AP = 137) at the equivalent recommended dosage of DANZITEN 190 mg twice daily.
The median duration of exposure in days for CML-CP and CML-AP patients is 561 (range, 1 to 1096) and 264 (range, 2 to 1160), respectively.
The median cumulative duration in days of dose interruptions for the CML-CP patients was 20 (range, 1 to 345), and the median duration in days of dose interruptions for the CML-AP patients was 23 (range, 1 to 234).
In patients with CML-CP, the most commonly reported non-hematologic adverse drug reactions (greater than or equal to 10%) were rash, pruritus, nausea, fatigue, headache, constipation, diarrhea, vomiting, and myalgia. The common serious drug-related adverse reactions (greater than or equal to 1% and less than 10%) were thrombocytopenia, neutropenia, and anemia.
In patients with CML-AP, the most commonly reported non-hematologic adverse drug reactions (greater than or equal to 10%) were rash, pruritus and fatigue. The common serious adverse drug reactions (greater than or equal to 1% and less than 10%) were thrombocytopenia, neutropenia, febrile neutropenia, pneumonia, leukopenia, intracranial hemorrhage, elevated lipase, and pyrexia.
Sudden deaths and QT prolongation were reported. The maximum mean QTcF change from baseline at steady- state was 10 msec. Increase in QTcF greater than 60 msec from baseline was observed in 4.1% of the patients and QTcF of greater than 500 msec was observed in 4 patients (less than 1%) [see Boxed Warning, Warnings and Precautions (5.3, 5.4), Clinical Pharmacology (12.2)].
Discontinuation due to adverse drug reactions was observed in 16% of CML-CP and 10% of CML-AP patients.
Most Frequently Reported Adverse Reactions
Tables 7 and 8 show the percentage of adult patients experiencing non-hematologic adverse reactions (excluding laboratory abnormalities) regardless of relationship to study drug. Adverse reactions reported in greater than 10% of adult patients who received at least 1 dose of Nilotinib are listed.
Table 7. Most Frequently Reported Non-Hematologic Adverse Reactions (Regardless of Relationship to Study Drug) in Adult Patients With Newly Diagnosed Ph+ CML-CP (≥ 10% in nilotinib 300 mg twice daily* or imatinib 400 mg once daily groups) 60-Month Analysisa
Patients With Newly Diagnosed Ph+ CML-CP
nilotinib
300 mg
Twice Daily*
imatinib 400 mg
Once Daily
nilotinib
300 mg
Twice Daily*
imatinib 400 mg
Once Daily
N = 279
N = 280
N = 279
N = 280
Body System and Adverse Reaction
All Grades (%)
CTC Gradesb 3/4 (%)
Skin and subcutaneous tissue disorders
Rash
38
19
< 1
2
Pruritus
21
7
< 1
0
Alopecia
13
7
0
0
Dry skin
12
6
0
0
Gastrointestinal disorders
Nausea
22
41
2
2
Constipation
20
8
< 1
0
Diarrhea
19
46
1
4
Vomiting
15
27
< 1
< 1
Abdominal pain upper
18
14
1
< 1
Abdominal pain
15
12
2
0
Dyspepsia
10
12
0
0
Nervous system disorders
Headache
32
23
3
< 1
Dizziness
12
11
< 1
< 1
General disorders and administration-site conditions
Fatigue
23
20
1
1
Pyrexia
14
13
< 1
0
Asthenia
14
12
< 1
0
Peripheral edema
9
20
< 1
0
Face edema
< 1
14
0
< 1
Musculoskeletal and connective tissue disorders
Myalgia
19
19
< 1
< 1
Arthralgia
22
17
< 1
< 1
Muscle spasms
12
34
0
1
Pain in extremity
15
16
< 1
< 1
Back pain
19
17
1
1
Respiratory, thoracic, and mediastinal disorders
Cough
17
13
0
0
Oropharyngeal pain
12
6
0
0
Dyspnea
11
6
2
< 1
Infections and infestations
Nasopharyngitis
27
21
0
0
Upper respiratory tract infection
17
14
< 1
0
Influenza
13
9
0
0
Gastroenteritis
7
10
0
< 1
Eye disorders
Eyelid edema
1
19
0
< 1
Periorbital edema
< 1
15
0
0
Psychiatric disorders
Insomnia
11
9
0
0
Vascular disorder
Hypertension
10
4
1
< 1
Abbreviations: CML-CP, chronic myeloid leukemia-chronic phase; Ph+, Philadelphia chromosome positive.
aExcluding laboratory abnormalities.
bNCI Common Terminology Criteria (CTC) for Adverse Events, version 3.0.
*Equivalent to the recommended dosage of DANZITEN 142 mg twice daily.
Table 8. Most Frequently Reported Non-Hematologic Adverse Reactions in Adult Patients with Resistant or Intolerant Ph+ CML Receiving Nilotinib 400 mg Twice Daily* (regardless of relationship to study drug) (≥ 10% in any group) 24-Month Analysisa
Body System and Adverse Reaction
CML-CP
CML-AP
N = 321
N = 137
All Grades (%)
CTC Gradesb 3/4 (%)
All Grades (%)
CTC Gradesb 3/4 (%)
Skin and subcutaneous tissue disorders
Rash
36
2
29
0
Pruritus
32
< 1
20
0
Night sweat
12
< 1
27
0
Alopecia
11
0
12
0
Gastrointestinal disorders
Nausea
37
1
22
< 1
Constipation
26
< 1
19
0
Diarrhea
28
3
24
2
Vomiting
29
< 1
13
0
Abdominal pain
15
2
16
3
Abdominal pain upper
14
< 1
12
< 1
Dyspepsia
10
< 1
4
0
Nervous system disorders
Headache
35
2
20
1
General disorders and administration-site conditions
Fatigue
32
3
23
< 1
Pyrexia
22
< 1
28
2
Asthenia
16
0
14
1
Peripheral edema
15
< 1
12
0
Musculoskeletal and connective tissue disorders
Myalgia
19
2
16
< 1
Arthralgia
26
2
16
0
Muscle spasms
13
< 1
15
0
Bone pain
14
< 1
15
2
Pain in extremity
20
2
18
1
Back pain
17
2
15
< 1
Musculoskeletal pain
11
< 1
12
1
Respiratory, thoracic, and mediastinal disorders
Cough
27
< 1
18
0
Dyspnea
15
2
9
2
Oropharyngeal pain
11
0
7
0
Infections and infestations
Nasopharyngitis
24
< 1
15
0
Upper respiratory tract infection
12
0
10
0
Metabolism and nutrition disorders
Decreased appetitec
15
< 1
17
< 1
Psychiatric disorders
Insomnia
12
1
7
0
Vascular disorders
Hypertension
10
2
11
< 1
Abbreviations: CML-AP, chronic myeloid leukemia-accelerated phase; CML-CP, chronic myeloid leukemia-chronic phase; Ph+, Philadelphia chromosome positive.
aExcluding laboratory abnormalities.
bNCI Common Terminology Criteria for Adverse Events, version 3.0.
cAlso includes preferred term anorexia.
*Equivalent to the recommended dosage of DANZITEN 190 mg twice daily.
Laboratory Abnormalities
Table 9 shows the percentage of adult patients experiencing treatment-emergent Grade 3/4 laboratory abnormalities in patients who received at least one dose of nilotinib.
Table 9. Percent Incidence of Clinically Relevant Grade 3/4* Laboratory Abnormalities
Patient Population
Newly Diagnosed Adult Ph+ CML-CP
Resistant or Intolerant Adult Ph+
CML-CP
CML-AP
nilotinib 300 mga
imatinib 400 mg
nilotinib 400 mgb
nilotinib 400 mgb
Twice Daily
Once Daily
Twice Daily
Twice Daily
N = 279
N = 280
N = 321
N = 137
(%)
(%)
(%)
(%)
Hematologic Parameters
Thrombocytopenia
10
9
301
423
Neutropenia
12
22
312
424
Anemia
4
6
11
27
Biochemistry Parameters
Elevated lipase
9
4
18
18
Hyperglycemia
7
< 1
12
6
Hypophosphatemia
8
10
17
15
Elevated bilirubin (total)
4
< 1
7
9
Elevated SGPT (ALT)
4
3
4
4
Hyperkalemia
2
1
6
4
Hyponatremia
1
< 1
7
7
Hypokalemia
< 1
2
2
9
Elevated SGOT (AST)
1
1
3
2
Decreased albumin
0
< 1
4
3
Hypocalcemia
< 1
< 1
2
5
Elevated alkaline phosphatase
0
< 1
< 1
1
Elevated creatinine
0
< 1
< 1
< 1
Abbreviations: ALT alanine aminotransferase; AST, aspartate aminotransferase; CML-AP, chronic myeloid leukemia-accelerated phase; CML-CP, chronic myeloid leukemia-chronic phase; Ph+, Philadelphia chromosome positive.
*NCI Common Terminology Criteria for Adverse Events, version 3.0.
1CML-CP: Thrombocytopenia: 12% were Grade 3, 18% were Grade 4.
2CML-CP: Neutropenia: 16% were Grade 3, 15% were Grade 4.
3CML-AP: Thrombocytopenia: 11% were Grade 3, 32% were Grade 4.
4CML-AP: Neutropenia: 16% were Grade 3, 26% were Grade 4.
a Equivalent to the recommended dosage of DANZITEN 142 mg twice daily.
b Equivalent to the recommended dosage of DANZITEN 190 mg twice daily.
Elevated total cholesterol (all Grades) occurred in 28% (equivalent recommended dosage of DANZITEN 142 mg twice daily) and 4% (imatinib). Elevated triglycerides (all Grades) occurred in 12% and 8% of patients in the nilotinib and imatinib arms, respectively. Hyperglycemia (all Grades) occurred in 50% and 31% of patients in the nilotinib and imatinib arms, respectively.
Most common biochemistry laboratory abnormalities (all Grades) were alanine aminotransferase increased (72%), blood bilirubin increased (59%), aspartate aminotransferase increased (47%), lipase increased (28%), blood glucose increased (50%), blood cholesterol increased (28%), and blood triglyceride increased (12%).
Treatment Discontinuation in Patients With Ph+ CML-CP Who Have Achieved a Sustained Molecular Response (MR4.5)
In eligible patients who discontinued nilotinib therapy after attaining a sustained molecular response (MR4.5), musculoskeletal symptoms (e.g., myalgia, pain in extremity, arthralgia, bone pain, spinal pain, or musculoskeletal pain), were reported more frequently than before treatment discontinuation in the first year, as noted in Table 9. The rate of new musculoskeletal symptoms generally decreased in the second year after treatment discontinuation.
In the newly diagnosed population in whom musculoskeletal symptoms occurred at any time during the TFR phase, 23/53 (43%) had not resolved by the TFR end date or data cut-off date. In the population previously treated with imatinib in whom musculoskeletal events occurred at any time during the TFR phase, 32/57 (56%) had not resolved by the data cut-off date.
The rate of musculoskeletal symptoms decreased in patients who entered the nilotinib treatment reinitiation (NTRI) phase, at 11/88 (13%) in the newly diagnosed population and 14/56 (25%) in the population previously treated with imatinib. Other adverse reactions observed in the nilotinib re-treatment phase were similar to those observed during nilotinib use in patients with newly diagnosed Ph+ CML-CP and resistant or intolerant Ph+ CML-CP and CML-AP.
Table 10. Musculoskeletal Symptoms Occurring Upon Treatment Discontinuation in the Context of Treatment-Free Remission (TFR)
Entire TFR Period in all TFR Patients
By Time Interval, in Subset of Patients in TFR
Greater than 48 Weeks
Ph+ CML-
CP patients
N
Median follow-
up in
Patients with musculoskeletal
symptoms
N
Year prior to nilotinib
discontinuation
1st year after nilotinib
discontinuation
2nd year after nilotinib
discontinuation
TFR
All Grades
Grade 3/4
All Grades
Grade 3/4
All Grades
Grade 3/4
All Grades
Grade 3/4
Newly Diagnosed
190
76
weeks
28%
1%
100
17%
0%
34%
2%
9%
0%
Previously
treated with imatinib
126
99
weeks
45%
2%
73
14%
0%
48%
3%
15%
1%
Abbreviations: CML-CP, chronic myeloid leukemia-chronic phase; Ph+, Philadelphia chromosome positive ;TFR, treatment-free remission.
Additional Data from Clinical Trials
The following adverse drug reactions were reported in adult patients in the nilotinib clinical studies at the recommended doses. These adverse drug reactions are ranked under a heading of frequency, the most frequent first using the following convention: common (greater than or equal to 1% and less than 10%), uncommon (greater than or equal to 0.1% and less than 1%), and unknown frequency (single events). For laboratory abnormalities, very common events (greater than or equal to 10%), which were not included in Tables 7 and 8, are also reported. These adverse reactions are included based on clinical relevance and ranked in order of decreasing seriousness within each category, obtained from 2 clinical studies:
1. Adult patients with newly diagnosed Ph+ CML-CP 60 month analysis and,
2. Adult patients with resistant or intolerant Ph+ CML-CP and CMP-AP 24 months’ analysis.
Infections and Infestations: Common: folliculitis. Uncommon: pneumonia, bronchitis, urinary tract infection, candidiasis (including oral candidiasis). Unknown frequency: hepatitis B reactivation, sepsis, subcutaneous abscess, anal abscess, furuncle, tinea pedis.
Neoplasms Benign, Malignant, and Unspecified: Common: skin papilloma. Unknown frequency: oral papilloma, paraproteinemia.
Blood and Lymphatic System Disorders: Common: leukopenia, eosinophilia, febrile neutropenia, pancytopenia, lymphopenia. Unknown frequency: thrombocythemia, leukocytosis.
Immune System Disorders: Unknown frequency: hypersensitivity.
Endocrine Disorders: Uncommon: hyperthyroidism, hypothyroidism. Unknown frequency: hyperparathyroidism secondary, thyroiditis.
Metabolism and Nutrition Disorders: Very Common: hypophosphatemia. Common: electrolyte imbalance (including hypomagnesemia, hyperkalemia, hypokalemia, hyponatremia, hypocalcemia, hypercalcemia, hyperphosphatemia), diabetes mellitus, hyperglycemia, hypercholesterolemia, hyperlipidemia, hypertriglyceridemia. Uncommon: gout, dehydration, increased appetite. Unknown frequency: hyperuricemia, hypoglycemia.
Psychiatric Disorders: Common: depression, anxiety. Unknown frequency: disorientation, confusional state, amnesia, dysphoria.
Nervous System Disorders: Common: peripheral neuropathy, hypoesthesia, paresthesia. Uncommon: intracranial hemorrhage, ischemic stroke, transient ischemic attack, cerebral infarction, migraine, loss of consciousness (including syncope), tremor, disturbance in attention, hyperesthesia, facial paralysis. Unknown frequency: basilar artery stenosis, brain edema, optic neuritis, lethargy, dysesthesia, restless legs syndrome.
Eye Disorders: Common: eye hemorrhage, eye pruritus, conjunctivitis, dry eye (including xerophthalmia). Uncommon: vision impairment, vision blurred, visual acuity reduced, photopsia, hyperemia (scleral, conjunctival, ocular), eye irritation, conjunctival hemorrhage. Unknown frequency: papilledema, diplopia, photophobia, eye swelling, blepharitis, eye pain, chorioretinopathy, conjunctivitis allergic, ocular surface disease.
Ear and Labyrinth Disorders: Common: vertigo. Unknown frequency: hearing impaired, ear pain, tinnitus.
Cardiac Disorders: Common: angina pectoris, arrhythmia (including atrioventricular block, cardiac flutter, extrasystoles, atrial fibrillation, tachycardia, bradycardia), palpitations, electrocardiogram QT prolonged.
Uncommon: cardiac failure, myocardial infarction, coronary artery disease, cardiac murmur, coronary artery stenosis, myocardial ischemia, pericardial effusion, cyanosis. Unknown frequency: ventricular dysfunction, pericarditis, ejection fraction decrease.
Vascular Disorders: Common: flushing. Uncommon: hypertensive crisis, peripheral arterial occlusive disease, intermittent claudication, arterial stenosis limb, hematoma, arteriosclerosis. Unknown frequency: shock hemorrhagic, hypotension, thrombosis, peripheral artery stenosis.
Respiratory, Thoracic and Mediastinal Disorders: Common: dyspnea exertional, epistaxis, dysphonia. Uncommon: pulmonary edema, pleural effusion, interstitial lung disease, pleuritic pain, pleurisy, pharyngolaryngeal pain, throat irritation. Unknown frequency: pulmonary hypertension, wheezing.
Gastrointestinal Disorders: Common: pancreatitis, abdominal discomfort, abdominal distension, dysgeusia, flatulence. Uncommon: gastrointestinal hemorrhage, melena, mouth ulceration, gastroesophageal reflux, stomatitis, esophageal pain, dry mouth, gastritis, sensitivity of teeth. Unknown frequency: gastrointestinal ulcer perforation, retroperitoneal hemorrhage, hematemesis, gastric ulcer, esophagitis ulcerative, subileus, enterocolitis, hemorrhoids, hiatus hernia, rectal hemorrhage, gingivitis.
Hepatobiliary Disorders: Very common: hyperbilirubinemia. Common: hepatic function abnormal. Uncommon: hepatotoxicity, toxic hepatitis, jaundice. Unknown frequency: cholestasis, hepatomegaly.
Skin and Subcutaneous Tissue Disorders: Common: eczema, urticaria, erythema, hyperhidrosis, contusion, acne, dermatitis (including allergic, exfoliative and acneiform). Uncommon: exfoliative rash, drug eruption, pain of skin, ecchymosis. Unknown frequency: psoriasis, erythema multiforme, erythema nodosum, skin ulcer, palmar-plantar erythrodysesthesia syndrome, petechiae, photosensitivity, blister, dermal cyst, sebaceous hyperplasia, skin atrophy, skin discoloration, skin exfoliation, skin hyperpigmentation, skin hypertrophy, hyperkeratosis.
Musculoskeletal and Connective Tissue Disorders: Common: bone pain, musculoskeletal chest pain, musculoskeletal pain, back pain, neck pain, flank pain, muscular weakness. Uncommon: musculoskeletal stiffness, joint swelling. Unknown frequency: arthritis.
Renal and Urinary Disorders: Common: pollakiuria. Uncommon: dysuria, micturition urgency, nocturia. Unknown frequency: renal failure, hematuria, urinary incontinence, chromaturia.
Reproductive System and Breast Disorders: Uncommon: breast pain, gynecomastia, erectile dysfunction. Unknown frequency: breast induration, menorrhagia, nipple swelling.
General Disorders and Administration Site Conditions: Common: pyrexia, chest pain (including non-cardiac chest pain), pain, chest discomfort, malaise. Uncommon: gravitational edema, influenza-like illness, chills, feeling body temperature change (including feeling hot, feeling cold). Unknown frequency: localized edema.
Investigations: Very Common: alanine aminotransferase increased, aspartate aminotransferase increased, lipase increased, lipoprotein cholesterol (including very low density and high density) increased, total cholesterol increased, blood triglycerides increased. Common: hemoglobin decreased, blood amylase increased, gamma- glutamyltransferase increased, blood creatinine phosphokinase increased, blood alkaline phosphatase increased, weight decreased, weight increased, globulins decreased. Uncommon: blood lactate dehydrogenase increased, blood urea increased. Unknown frequency: troponin increased, blood bilirubin unconjugated increased, insulin C-peptide decreased, blood parathyroid hormone increased.
In Pediatric Patients With Newly Diagnosed Ph+ CML-CP or Resistant or Intolerant Ph+ CML-CP
In pediatric patients with Ph+ CML-CP, the most common (greater than 20%) non-hematologic adverse reactions were hyperbilirubinemia, headache, alanine aminotransferase increased, rash, pyrexia, nausea, aspartate aminotransferase increased, pain in extremity, upper respiratory tract infection, vomiting, diarrhea, and nasopharyngitis. The most common (greater than 5%) Grade 3/4 non-hematologic adverse reactions were hyperbilirubinemia, rash, alanine aminotransferase increased, and neutropenia.
Laboratory abnormalities of hyperbilirubinemia (Grade 3/4: 16%) and transaminase elevation (AST Grade 3/4: 2.9%, ALT Grade 3/4: 10%), were reported at a higher frequency than in adult patients.
The most common hematological laboratory abnormalities (greater than or equal to 30% of patients, of all Grades) were decreases in total white blood cells (54%), platelet count (44%), absolute neutrophils (44%), hemoglobin (38%), and absolute lymphocytes (36%).
Discontinuation of study treatment due to adverse reactions occurred in 15 patients (22%). The most frequent adverse reactions leading to discontinuation were hyperbilirubinemia (9%) and rash (6%).
Increase in QTcF greater than 30 msec from baseline was observed in 19 patients (28%). No patient had an absolute QTcF of greater than 500 msec or QTcF increase of greater than 60 msec from baseline.
Growth Retardation in Pediatric Population
Close monitoring of growth in pediatric patients under nilotinib treatment is recommended [see Warnings and Precautions (5.14)].
Additional pediatric use information is approved for Novartis Pharmaceuticals Corporation’s Tasigna® (nilotinib) capsules. However, due to Novartis Pharmaceuticals Corporation’s marketing exclusivity rights, this drug product is not labeled with that pediatric information.
6.2 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of nilotinib. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Blood and Lymphatic System Disorders: thrombotic microangiopathy
Nervous System Disorders: facial paralysisMusculoskeletal and Connective Tissue Disorders: osteonecrosis
-
7 DRUG INTERACTIONS
7.1 Effect of Other Drugs on DANZITEN
Strong CYP3A Inhibitors
Avoid concomitant use of strong CYP3A inhibitors with DANZITEN. If concomitant use cannot be avoided, reduce DANZITEN dose [see Dosage and Administration (2.9)].
Nilotinib is a CYP3A substrate [see Clinical Pharmacology (12.3)]. Concomitant use with a strong CYP3A inhibitor increases nilotinib exposure [see Clinical Pharmacology (12.3)], which may increase the risk of DANZITEN adverse reactions.
Strong CYP3A Inducers
Avoid concomitant use of strong CYP3A inducers with DANZITEN.
Nilotinib is a CYP3A substrate [see Clinical Pharmacology (12.3)]. Concomitant use with a strong CYP3A inducer decreases nilotinib exposure [see Clinical Pharmacology (12.3)], which may reduce DANZITEN efficacy.
Proton Pump Inhibitors
Avoid concomitant use of PPI with DANZITEN. As an alternative to PPIs, use H2 blockers approximately 10 hours before or approximately 2 hours after the dose of DANZITEN, or use antacids approximately 2 hours before or approximately 2 hours after the dose of DANZITEN.
Nilotinib displays pH-dependent aqueous solubility [see Description (11)]. Concomitant use with a proton pump inhibitor (PPI) decreases nilotinib concentrations [see Clinical Pharmacology (12.3)], which may reduce DANZITEN efficacy.7.2 Drugs that Prolong the QT Interval
Avoid coadministration of DANZITEN with agents that may prolong the QT interval, such as anti-arrhythmic drugs [see Boxed Warning, Dosage and Administration (2.5), Warnings and Precautions (5.3), Drug Interactions (7.1), Clinical Pharmacology (12.2)].
Nilotinib is associated with a clinically significant concentration-dependent QT prolongation [see Clinical Pharmacology (12.2)]. -
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Based on findings from animal studies and the mechanism of action, DANZITEN can cause fetal harm when administered to a pregnant woman [see Clinical Pharmacology (12.1)]. There are no available data in pregnant women to inform the drug-associated risk. In animal reproduction studies, administration of nilotinib to pregnant rats and rabbits during organogenesis caused adverse developmental outcomes, including embryo-fetal lethality, fetal effects, and fetal variations in rats and rabbits at maternal exposures (AUC) approximately 2 and 0.5 times, respectively, the exposures in patients at the recommended dose (see Data). Advise pregnant women of the potential risk to a fetus.
The background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies are 2%-4% and 15%-20%, respectively.
Data
Animal Data
In embryo-fetal development studies in rats and rabbits, pregnant animals received oral doses of nilotinib up to 100 mg/kg/day and 300 mg/kg/day, respectively, during the period of organogenesis.
In rats, oral administration of nilotinib produced embryo-lethality/fetal effects at doses ≥ 30 mg/kg/day. At ≥ 30 mg/kg/day, skeletal variations of incomplete ossification of the frontals and misshapen sternebra were noted, and there was an increased incidence of small renal papilla and fetal edema. At 100 mg/kg/day, nilotinib was associated with maternal toxicity (decreased gestation weight, gravid uterine weight, net weight gain, and food consumption) and resulted in a single incidence of cleft palate and two incidences of pale skin were noted in the fetuses. A single incidence of dilated ureters was noted in a fetus also displaying small renal papilla at 100 mg/kg/day. Additional variations of forepaw and hindpaw phalanx unossified, fused sternebra, bipartite sternebra ossification, and incomplete ossification of the cervical vertebra were noted at 100 mg/kg/day.
In rabbits, oral administration of nilotinib resulted in the early sacrifice of two females, maternal toxicity and increased resorption of fetuses at 300 mg/kg/day. Fetal skeletal variations (incomplete ossification of the hyoid, bent hyoid, supernumerary short detached ribs and the presence of additional ossification sites near the nasals, frontals and in the sternebral column) were also increased at this dose in the presence of maternal toxicity.
Slight maternal toxicity was evident at 100 mg/kg/day but there were no reproductive or embryo-fetal effects at this dose.
At 30 mg/kg/day in rats and 300 mg/kg/day in rabbits, the maternal systemic exposure (AUC) were 72700 ng*hr/mL and 17100 ng*hr/mL respectively, representing approximately 2 and 0.5 times the exposure in humans at the highest recommended dose 400 mg twice daily.
When pregnant rats were dosed with nilotinib during organogenesis and through lactation, the adverse effects included a longer gestational period, lower pup body weights until weaning and decreased fertility indices in the pups when they reached maturity, all at a maternal dose of 60 mg/kg (i.e., 360 mg/m2, approximately 0.7 times the clinical dose of 400 mg twice daily based on body surface area). At doses up to 20 mg/kg (i.e., 120 mg/m2, approximately 0.25 times the clinical dose of 400 mg twice daily based on body surface area) no adverse effects were seen in the maternal animals or the pups.8.2 Lactation
Risk Summary
There are no data on the presence of nilotinib or its metabolites in human milk or its effects on a breastfed child or on milk production. However, nilotinib is present in the milk of lactating rats. Because of the potential for serious adverse reactions in a breastfed child, advise women not to breastfeed during treatment with DANZITEN and for 14 days after the last dose.
Animal Data
After a single 20 mg/kg of [14C] nilotinib dose to lactating rats, the transfer of parent drug and its metabolites into milk was observed. The overall milk-to-plasma exposure ratio of total radioactivity was approximately 2, based on the AUC0-24h or AUC0-INF values. No rat metabolites of nilotinib were detected that were unique to milk.8.3 Females and Males of Reproductive Potential
Based on animal studies, DANZITEN can cause fetal harm when administered to a pregnant woman [see Use in Specific Populations (8.1)].
Pregnancy Testing
Females of reproductive potential should have a pregnancy test prior to starting treatment with DANZITEN.Contraception
Females
Advise females of reproductive potential to use effective contraception during treatment with DANZITEN and for 14 days after the last dose.
Infertility
The risk of infertility in females or males of reproductive potential has not been studied in humans. In studies in rats and rabbits, the fertility in males and females was not affected [see Nonclinical Toxicology (13.1)].8.4 Pediatric Use
The frequency, type, and severity of adverse reactions observed were generally consistent with those observed in adults, with the exception of the laboratory abnormalities of hyperbilirubinemia (Grade 3/4: 16%) and transaminase elevation (AST Grade 3/4: 2.9%, ALT Grade 3/4: 10%), which were reported at a higher frequency in pediatric patients than in adults [see Adverse Reactions (6.1)]. For pediatric growth and development, growth retardation has been reported in pediatric patients with Ph+ CML-CP treated with nilotinib [see Warnings and Precautions (5.14 and 5.12), Adverse Reactions (6.1)].
The safety and effectiveness of nilotinib in pediatric patients below the age of 1 year with newly diagnosed, or resistant or intolerant Ph+ CML in chronic phase and accelerated phase, have not been established.Additional pediatric use information is approved for Novartis Pharmaceuticals Corporation’s Tasigna® (nilotinib) capsules. However, due to Novartis Pharmaceuticals Corporation’s marketing exclusivity rights, this drug product is not labeled with that pediatric information.
8.5 Geriatric Use
In the clinical trials of nilotinib (patients with newly diagnosed Ph+ CML-CP and resistant or intolerant Ph+ CML-CP and CML-AP), approximately 12% and 30% of patients were 65 years or over respectively.
Patients with newly diagnosed Ph+ CML-CP: There was no difference in major molecular response between patients aged less than 65 years and those greater than or equal to 65 years.
Patients with resistant or intolerant CML-CP: There was no difference in major cytogenetic response rate between patients aged less than 65 years and those greater than or equal to 65 years.
Patients with resistant or intolerant CML-AP: The hematologic response rate was 44% in patients less than 65 years of age and 29% in patients greater than or equal to 65 years.
No major differences for safety were observed in patients greater than or equal to 65 years of age as compared to patients less than 65 years.8.6 Cardiac Disorders
In the clinical trials, patients with a history of uncontrolled or significant cardiovascular disease, including recent myocardial infarction, congestive heart failure, unstable angina or clinically significant bradycardia, were excluded. Caution should be exercised in patients with relevant cardiac disorders [see Boxed Warning, Warnings and Precautions (5.3)].
- 10 OVERDOSAGE
-
11 DESCRIPTION
DANZITEN (nilotinib) tablets contain nilotinib, a kinase inhibitor.
Nilotinib is present as nilotinib tartrate, with the molecular formula of C28H22F3N7O . C4H6O6 and a weight of 679.61 g/mol. Nilotinib tartrate is a white to slightly yellowish powder. The solubility of nilotinib tartrate in aqueous solutions decreases with increasing pH. The pKa1 was determined to be 3.53; pKa2 was estimated to be 1.55.
The chemical name of nilotinib tartrate is 4-methyl-N-[3-(4-methyl-1H-imidazol-1-yl)-5-(trifluoromethyl)phenyl]-3-[[4-(3-pyridinyl)-2-pyrimidinyl]amino]benzamide,(2R,3R)-2,3-dihydroxybutanedionate. Its structure is shown below:
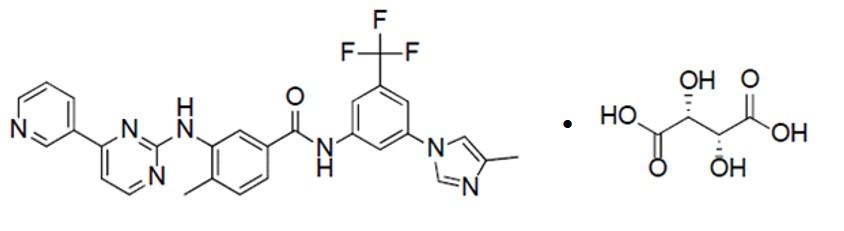
DANZITEN (nilotinib) tablets contain 71 mg or 95 mg nilotinib, equivalent to 91.14 mg, and 121.95 mg nilotinib tartrate, respectively. The inactive ingredients are: colloidal silicon dioxide, croscarmellose sodium, hypromellose acetate succinate, iron oxide red (in 71 mg strength tablets), iron oxide yellow (in 95 mg strength tablets), magnesium stearate, microcrystalline cellulose, polyethylene glycol, polyvinyl alcohol, talc, and titanium dioxide.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Nilotinib is an inhibitor of the BCR-ABL kinase. Nilotinib binds to and stabilizes the inactive conformation of the kinase domain of ABL protein. In vitro, nilotinib inhibited BCR-ABL mediated proliferation of murine leukemic cell lines and human cell lines derived from patients with Ph+ CML. Under the conditions of the assays, nilotinib was able to overcome imatinib resistance resulting from BCR-ABL kinase mutations, in 32 out of 33 mutations tested. Nilotinib inhibited the autophosphorylation of the following kinases at IC50 values as indicated: BCR-ABL (20 to 60 nM), PDGFR (69 nM), c-KIT (210 nM), CSF-1R (125 to 250 nM), and DDR1 (3.7 nM).
12.2 Pharmacodynamics
A relationship between nilotinib exposure and a greater likelihood of response and safety events, including a higher occurrence of total bilirubin elevations, was observed in clinical studies.
Nilotinib time course of pharmacodynamic response is unknown.
Cardiac Electrophysiology
Nilotinib is associated with concentration-dependent QT prolongation. At the equivalent recommended dosage of DANZITEN 190 mg twice daily given without food in healthy subjects, the maximum mean placebo-adjusted QTcF changes were 10.4 msec (90% CI: 2.85, 18.0). After a single equivalent recommended dose of DANZITEN 380 mg (two times the maximum approved recommended dose) given with a high fat meal to healthy subjects, the maximum mean placebo-adjusted QTcF changes were) 18.0 msec (90% CI: 9.65, 25.8). Peak plasma concentrations in the QT study were 26% lower than or comparable with those observed in patients enrolled in the single-arm study [see Boxed Warning, Warnings and Precautions (5.3), Adverse Reactions (6.1)]. No new significant QT findings were observed in healthy subject studies with single doses of DANZITEN given with or without food. Throughout the 14 PK studies there were no QT prolongation events associated with DANZITEN.12.3 Pharmacokinetics
Nilotinib single-dose maximum concentration (Cmax), area under the time concentration curve (AUC), predicted steady-state maximum concentration (Cmax,ss) and area under the time concentration curve (AUCss) in fasted subjects receiving the DANZITEN approved recommended dosages are presented in Tables 11 and 12.
Table 11: Nilotinib mean ±SD single-dose exposure in fasted patients receiving the DANZITEN approved recommended dosages
DANZITEN Dosage
Cmax
AUC
142 mg
849 ± 366 ng/mL
17637 ± 7744 ng*hr/mL
190 mg
811 ± 300 ng/mL
15339 ± 6935 ng*hr/mL
Abbreviations: Cmax= maximum concentration; AUC = area under the time concentration curve
Table 12: Nilotinib predicted mean ±SD steady-state exposure in fasted patients receiving the DANZITEN approved recommended dosages
DANZITEN Dosage
Cmax,ss
AUCss
142 mg twice daily
2071 ± 761 ng/mL
14525 ± 5690 ng*hr/mL
190 mg twice daily
2229 ± 790 ng/mL
15662 ± 5738 ng*hr/mL
Abbreviations: Cmax,ss= maximum concentration; AUCss = area under the time concentration curve at steady state
Absorption
The median time (range) to reach peak plasma nilotinib concentrations (Tmax) is 2.7 (1.0 to 4.7 hours) following single dose administration of DANZITEN 190 mg in fasted healthy subjects.
Effect of Food
No clinically significant differences in nilotinib exposure were observed following administration of DANZITEN 142 mg or 190 mg with a high-fat meal (800 to 1000 calories, 50% fat) or a low-fat meal (400-500 kcal, 25% fat content) compared to fasted healthy subjects.
Distribution
Serum protein binding is approximately 98% with a blood-to-serum ratio of 0.68.
Elimination
The mean elimination half-life of nilotinib is approximately 14 hours.
Metabolism
Nilotinib is primarily metabolized via CYP3A4-mediated oxidation and to a minor extent by CYP2C8.
Excretion
After a single dose of radiolabeled nilotinib, more than 90% of the administered dose was eliminated within
7 days: 93% of the dose in feces. Parent drug accounted for 69% of the dose.
Specific Populations
No clinically significant differences in the pharmacokinetic of nilotinib were observed based on age, sex, race/ethnicity, or body weight. The effect of renal impairment on nilotinib pharmacokinetics is unknown.
Additional pediatric use information is approved for Novartis Pharmaceuticals Corporation’s Tasigna® (nilotinib) capsules. However due to Novartis Pharmaceuticals Corporation’s marketing exclusivity rights, this drug product is not labeled with that pediatric information.
Patients with Hepatic Impairment
Nilotinib mean AUC increased 1.4-fold in mild (Child-Pugh class A), 1.4-fold in moderate (Child-Pugh class B), and 1.6-fold in severe (Child-Pugh class C) hepatic impairment subjects following a single equivalent recommended dose of DANZITEN 95 mg (66% of the lowest approved recommended dosage).
Drug Interaction Studies
Clinical Studies
Strong CYP3A Inhibitors: Nilotinib AUC increased by approximately 3-fold following concomitant administration of ketoconazole (strong CYP3A inhibitor) 400 mg once daily for 6 days. Nilotinib AUC increased by 1.3-fold with concomitant use with double-strength grapefruit juice.
Strong CYP3A Inducers: Nilotinib AUC decreased by approximately 80% following concomitant use with rifampicin (strong CYP3A inducer) 600 mg daily.
Proton Pump Inhibitors (PPIs): Nilotinib displays pH-dependent aqueous solubility [see Description (11)]. Nilotinib AUC decreased by 34% following concomitant use of multiple doses of esomeprazole (PPI) 40 mg daily.
Other Drugs: No clinically significant differences in nilotinib pharmacokinetics were observed when used concomitantly with imatinib (moderate CYP3A inhibitor), famotidine (an H2 blocker), or an antacid. No clinically significant differences in the pharmacokinetics of the following drugs were observed when used concomitantly with nilotinib; oral midazolam (CYP3A substrate), imatinib, or warfarin (CYP2C9 substrate).
In Vitro Studies Where Drug Interaction Potential was not Further Evaluated Clinically
CYP Enzymes: Nilotinib is a competitive inhibitor of CYP2C8, CYP2D6, and is an inducer of CYP2B6 and CYP2C8.
Transporter Systems: Nilotinib is an inhibitor of UGT1A1 and P-gp.12.5 Pharmacogenomics
Nilotinib can increase bilirubin levels. The (TA)7/(TA)7 genotype of UGT1A1 was associated with a statistically significant increase in the risk of hyperbilirubinemia relative to the (TA)6/(TA)6 and (TA)6/(TA)7 genotypes. However, the largest increases in bilirubin were observed in the (TA)7/(TA)7 genotype (UGT1A1*28) patients [see Warnings and Precautions (5.7)].
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
A 2-year carcinogenicity study was conducted orally in rats at nilotinib doses of 5, 15, and 40 mg/kg/day. Exposures in animals at the highest dose tested were approximately 2- to 3-fold the human exposure (based on AUC) at the nilotinib dose of 400 mg twice daily. The study was negative for carcinogenic findings. A 26-week carcinogenicity study was conducted orally in Tg.rasH2 mice, a model genetically modified to enhance susceptibility to neoplastic transformation, at nilotinib doses of 30, 100, and 300 mg/kg/day. Nilotinib induced in the skin and subcutis statistically significant increases in the incidence of papillomas in females and of papillomas and combined papillomas and carcinomas in males at 300 mg/kg/day. The no-observed-adverse- effect-level (NOAEL) for skin neoplastic lesions was 100 mg/kg/day.
Nilotinib was not mutagenic in a bacterial mutagenesis (Ames) assay, was not clastogenic in a chromosome aberration assay in human lymphocytes, did not induce DNA damage (comet assay) in L5178Y mouse lymphoma cells, nor was it clastogenic in an in vivo rat bone marrow micronucleus assay with two oral treatments at doses up to 2000 mg/kg/dose.
There were no effects on male or female rat and female rabbit mating or fertility at doses up to 180 mg/kg in rats (approximately 4- to 7-fold for males and females, respectively, the AUC in patients at the dose of 400 mg twice daily) or 300 mg/kg in rabbits (approximately one-half the AUC in patients at the dose of 400 mg twice daily). The effect of nilotinib on human fertility is unknown. In a study where male and female rats were treated with nilotinib at oral doses of 20 to 180 mg/kg/day (approximately 1- to 6.6-fold the AUC in patients at the dose of 400 mg twice daily) during the pre-mating and mating periods and then mated, and dosing of pregnant rats continued through gestation Day 6, nilotinib increased post-implantation loss and early resorption, and decreased the number of viable fetuses and litter size at all doses tested. -
14 CLINICAL STUDIES
14.1 Adult Newly Diagnosed Ph+ CML-CP
The effectiveness of 142 mg twice daily of DANZITEN (nilotinib) tablets for the treatment of adult patients with newly diagnosed Ph+ CML-CP has been established from an adequate and well-controlled study of Tasigna® (nilotinib) capsules, which has a different recommended dosage than DANZITEN. Below is a display of the results of Tasigna® (nilotinib) capsules in this adequate and well-controlled study.
The ENESTnd (Evaluating Nilotinib Efficacy and Safety in clinical Trials-Newly Diagnosed patients) study (NCT00471497) was an open-label, multicenter, randomized trial conducted to determine the efficacy of nilotinib versus imatinib in adult patients with cytogenetically confirmed newly diagnosed Ph+ CML-CP. Patients were within 6 months of diagnosis and were previously untreated for CML-CP, except hydroxyurea and/or anagrelide. Efficacy was based on a total of 846 patients: 283 patients in the imatinib 400 mg once daily group, 282 patients in the nilotinib dosage equivalent to DANZITEN 142 mg twice daily group, 281 patients in the nilotinib dosage equivalent to DANZITEN 190 mg twice daily group (an unapproved dosage regimen for this indication).
Median age was 46 years in the imatinib group and 47 years in the nilotinib group, with 12% and 13% of patients greater than or equal to 65 years of age in imatinib 400 mg once daily and nilotinib dosage equivalent to DANZITEN 142 mg twice daily treatment groups, respectively. There were slightly more male than female patients in all groups (56% and 56%, in imatinib 400 mg once daily and nilotinib dosage equivalent to DANZITEN 142 mg twice daily treatment groups). Approximately 60% of all patients were White, and 25% were Asian.
The primary data analysis was performed when all 846 patients completed 12 months of treatment (or discontinued earlier). Subsequent analyses were done when patients completed 24, 36, 48, and 60 months of treatment (or discontinued earlier). The median time on treatment was approximately 61 months in all three treatment groups.
The primary efficacy endpoint was major molecular response (MMR) at 12 months after the start of study medication. MMR was defined as less than or equal to 0.1% BCR-ABL/ABL % by international scale measured by RQ-PCR, which corresponds to a greater than or equal to 3 log reduction of BCR-ABL transcript from standardized baseline. Efficacy endpoints are summarized in Table 13.
Two patients in the nilotinib arm progressed to either accelerated phase or blast crisis (both within the first 6 months of treatment) while 12 patients on the imatinib arm progressed to either accelerated phase or blast crisis (7 patients within first 6 months, 2 patients within 6 to 12 months, 2 patients within 12 to 18 months and 1 patient within 18 to 24 months).
Table 13. Efficacy (MMR and CCyR) of Nilotinib Compared to imatinib in Adult Newly Diagnosed Ph+ CML-CP (ENESTnd)
Nilotinib 300 mg
Twice Daily*Imatinib 400 mg
Once DailyN = 282 N = 283 MMR at 12 months (95% CI) 44% (38.4, 50.3) 22% (17.6, 27.6) P-Valuea < 0.0001 CCyRb by 12 months (95% CI) 80% (75.0, 84.6) 65% (59.2, 70.6) MMR at 24 months (95% CI) 62% (55.8, 67.4) 38% (31.8, 43.4) CCyRb by 24 months (95% CI) 87% (82.4, 90.6) 77% (71.7, 81.8) Abbreviation: CI, confidence interval.
* Equivalent to DANZITEN 142 mg twice daily.
aCMH test stratified by Sokal risk group.
bCCyR: 0% Ph+ metaphases. Cytogenetic responses were based on the percentage of Ph+ metaphases among greater than or equal to 20 metaphase cells in each bone marrow sample.
By 60 months, MMR was achieved by 77% of patients on nilotinib and 60% of patients on imatinib; MR4.5 was achieved by 53.5% of patients on nilotinib and 31.4% on imatinib. Median overall survival was not reached in either arm. At the time of the 60-month final analysis, the estimated survival rate was 93.7% for patients on nilotinib and 91.7% for patients on imatinib.14.2 Adult Patients with Resistant or Intolerant Ph+ CML-CP and CML-AP
The effectiveness of 190 mg twice daily of DANZITEN (nilotinib) tablets for the treatment of adult patients with Ph+ CML- CP and Ph+ CML-AP resistant or intolerant to prior therapy that included imatinib has been established from an adequate and well-controlled study of Tasigna® (nilotinib) capsules, which has a different recommended dosage than DANZITEN. Below is a display of the results of Tasigna® (nilotinib) capsules in this adequate and well-controlled study.
Study CAMN107A2101 (referred to as Study A2101) (NCT00109707) was a single-arm, open-label, multicenter study conducted to evaluate the efficacy and safety of nilotinib (dosage equivalent to DANZITEN 190 mg twice daily) in patients with imatinib-resistant or -intolerant CML with separate cohorts for chronic and accelerated phase disease. The definition of imatinib resistance included failure to achieve a complete hematologic response (by 3 months), cytogenetic response (by 6 months) or major cytogenetic response (by 12 months) or progression of disease after a previous cytogenetic or hematologic response. Imatinib intolerance was defined as discontinuation of treatment due to toxicity and lack of a major cytogenetic response at time of study entry. At the time of data cut- off, 321 patients with CML-CP and 137 patients with CML-AP with a minimum follow-up of 24 months were enrolled. In this study, about 50% of CML-CP and CML-AP patients were males, over 90% (CML-CP) and 80% (CML-AP) were White, and approximately 30% were age 65 years or older.
Overall, 73% of patients were imatinib resistant while 27% were imatinib intolerant. The median time of prior imatinib treatment was approximately 32 (CML-CP) and 28 (CML-AP) months. Prior therapy included hydroxyurea in 85% of patients, interferon in 56% and stem cell or bone marrow transplant in 8%. The median highest prior imatinib dose was 600 mg per day for patients with CML-CP and CML-AP, and the highest prior imatinib dose was greater than or equal to 600 mg/day in 74% of all patients with 40% of patients receiving imatinib doses greater than or equal to 800 mg/day.
Median duration of nilotinib treatment was 18.4 months in patients with CML-CP and 8.7 months in patients with CML-AP.
The efficacy endpoint in CML-CP was unconfirmed major cytogenetic response (MCyR) which included complete and partial cytogenetic responses.
The efficacy endpoint in CML-AP was confirmed hematologic response (HR), defined as either a complete hematologic response (CHR) or no evidence of leukemia (NEL). The rates of response for CML-CP and CML- AP patients are reported in Table 14.
Median durations of response had not been reached at the time of data analysis.
Table 14. Efficacy of Nilotinib in Adult Resistant or Intolerant Ph+ CML-CP and CML-AP (Study A2101)
Cytogenetic Response Rate (Unconfirmed) (%)a Chronic Phase (n = 321) Major (95% CI) 51% (46%–57%) Complete (95% CI) 37% (32%–42%) Partial (95% CI) 15% (11%–19%) Accelerated Phase(n = 137) Hematologic Response Rate (Confirmed) (95% CI)b 39% (31%–48%) Complete Hematologic Response Rate (95% CI) 30% (22%–38%) No Evidence of Leukemia (95% CI) 9% (5%–16%) aCytogenetic response criteria: Complete (0% Ph+ metaphases) or partial (1% to 35%). Cytogenetic responses were based on the percentage of Ph-positive metaphases among greater than or equal to 20 metaphase cells in each bone marrow sample.
bHematologic response = CHR + NEL (all responses confirmed after 4 weeks).
CHR (CML-CP): WBC less than 10 x 109/L, platelets less than 450,000/mm3, no blasts or promyelocytes in peripheral blood, less than 5% myelocytes + metamyelocytes in bone marrow, less than 20% basophils in peripheral blood, and no extramedullary involvement. CHR (CML-AP): neutrophils greater than or equal to 1.5 x 109/L, platelets greater than or equal to 100 x 109/L, no myeloblasts in peripheral blood, myeloblasts less than 5% in bone marrow, and no extramedullary involvement.
NEL: same criteria as for CHR but neutrophils greater than or equal to 1.0 x 109/L and platelets greater than or equal to 20 x 109/L without transfusions or bleeding.
Adult Patients With Chronic Phase
The MCyR rate in 321 CML-CP patients was 51%. The median time to MCyR among responders was 2.8 months (range, 1 to 28 months). The median duration of MCyR cannot be estimated. The median duration of exposure on this single arm-trial was 18.4 months. Among the CML-CP patients who achieved MCyR, 62% of them had MCyR lasting more than 18 months. The CCyR rate was 37%.
Adult Patients With Accelerated Phase
The overall confirmed hematologic response rate in 137 patients with CML-AP was 39%. The median time to first hematologic response among responders was 1 month (range, 1 to 14 months). Among the CML-AP patients who achieved HR, 44% of them had a response lasting for more than 18 months.
After imatinib failure, 24 different BCR-ABL mutations were noted in 42% of chronic phase and 54% of accelerated phase CML patients who were evaluated for mutations.14.3 Treatment Discontinuation in Newly Diagnosed Ph+ CML-CP Patients Who Have Achieved a Sustained Molecular Response (MR4.5)
The efficacy of DANZITEN (nilotinib) tablets treatment discontinuation in adult patients with newly diagnosed Ph+ CML-CP has been established from an adequate and well-controlled study of Tasigna® (nilotinib) capsules, which has a different recommended dosage than DANZITEN. Below is a display of the results of Tasigna® (nilotinib) capsules in this adequate and well-controlled study.
The ENESTfreedom (Evaluating Nilotinib Efficacy and Safety in clinical Trials-freedom) study (NCT01784068) is an open-label, multicenter, single-arm study, where 215 adult patients with Ph+ CML-CP treated with nilotinib in first-line for ≥ 2 years who achieved MR4.5 as measured with the MolecularMD MRDx® BCR-ABL Test were enrolled to continue nilotinib treatment for an additional 52 weeks (nilotinib consolidation phase).
Of the 215 patients, 190 patients (88.4%) entered the “Treatment-Free Remission” (TFR) phase after achieving a sustained molecular response (MR4.5) during the consolidation phase, defined by the following criteria:
The 4 last quarterly assessments (taken every 12 weeks) were at least MR4 (BCR-ABL/ABL ≤ 0.01% IS), and maintained for 1 year
The last assessment being MR4.5 (BCR-ABL/ABL ≤ 0.0032% IS)
No more than two assessments falling between MR4 and MR4.5 (0.0032% IS < BCR-ABL/ABL ≤ 0.01% IS).
The median age of patients who entered the TFR phase was 55 years, 49.5% were females, and 21.1% of the patients were ≥ 65 years of age. BCR-ABL levels were monitored every 4 weeks during the first 48 weeks of the TFR phase. Monitoring frequency was intensified to every 2 weeks upon the loss of MR4.0. Biweekly monitoring ended at one of the following time points:
Loss of MMR requiring patient to reinitiate nilotinib treatment
When the BCR-ABL levels returned to a range between MR4.0 and MR4.5
When the BCR-ABL levels remained lower than MMR for 4 consecutive measurements (8 weeks from initial loss of MR4.0).
Any patient with loss of MMR during the TFR phase reinitiated nilotinib at a dosage equivalent to DANZITEN 142 mg twice daily or at a reduced dose level equivalent to DANZITEN 190 mg once daily if required from the perspective of tolerance, within 5 weeks after the collection date of the blood sample demonstrating loss of MMR. Patients who required reinitiation of nilotinib treatment were monitored for BCR-ABL levels every 4 weeks for the first 24 weeks and then every 12 weeks thereafter in patients who regained MMR.
Efficacy was based on the 96-week analysis data cut-off date, by which time, 91 patients (47.9%) discontinued from the TFR phase due to loss of MMR, and 1 (0.5%), 1 (0.5%), 1 (0.5%) and 3 patients (1.6%) due to death from unknown cause, physician decision, lost to follow-up and subject decision, respectively. Among the 91 patients who discontinued the TFR phase due to loss of MMR, 88 patients restarted nilotinib treatment and 3 patients permanently discontinued from the study.
By the 96-week data cut-off of the 88 patients who restarted treatment due to loss of MMR in the TFR phase, 87 patients (98.9%) patients regained MMR (one patient discontinued study permanently due to subject decision after 7.1 weeks of retreatment without regaining MMR) and 81 patients (92.0%) regained MR4.5 by the time of the cut-off date. The cumulative rate of MMR and MR4.5 regained at 24 weeks since treatment reinitiation was 97.7% (86/88 patients) and 86.4% (76/88 patients), respectively.
Table 15. Efficacy Results for ENESTfreedom
Patients Who Entered the Treatment Free Remission (TFR) Phase (Full Analysis Set, N = 190) Patients in TFR phase1 at the specified time point Loss of MMR2 by the specified time point % 95% CI % 24 weeks 62.1 (54.8, 69.0) 35.8 48 weeks 51.6 (44.2, 58.9) 45.8 96 weeks 48.9 (41.6, 56.3) 47.9 Abbreviation: CI, confidence interval.
1Patients in MMR at the specified time point in the TFR phase.
2Based on the time to event (loss of MMR) data during the TFR phase.
Among the 190 patients in the TFR phase, 98 patients had a treatment-free survival (TFS) event (defined as discontinuation from TFR phase due to any reason, loss of MMR, death due to any cause, progression to AP/BC up to the end of TFR phase, or reinitiation of treatment due to any cause in the study) by the 96-week cut-off date.Figure 1. Kaplan-Meier Estimate of Treatment-Free Survival After Start of TFR (Full Analysis Set ENESTfreedom)
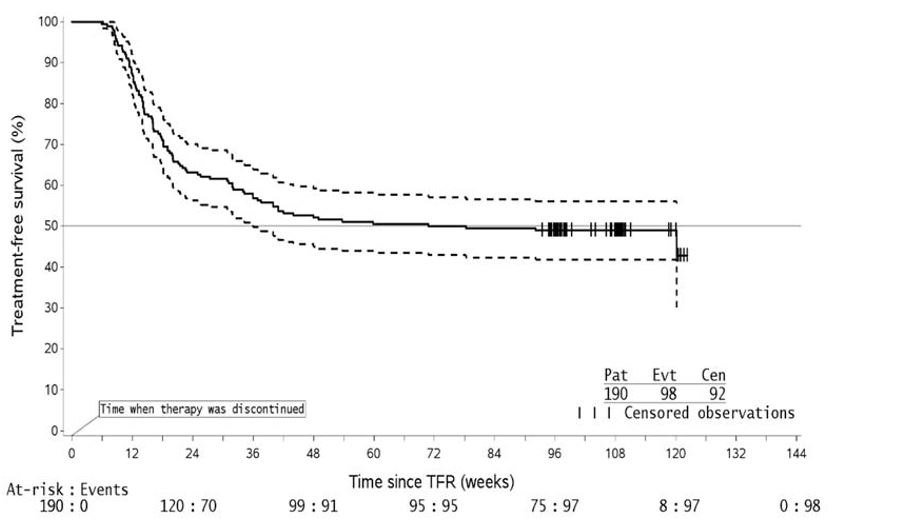
1. For a given time point, the points on the dashed curves represent the 95% confidence limits for the associated KM estimate on the solid curve.
2. By the time of the 96-week data cut-off date, one single patient lost MMR at Week 120, at the time when only 8 patients were considered at risk. This explains the artificial drop at the end of the curve.14.4 Treatment Discontinuation in Ph+ CML-CP Patients Who Have Achieved a Sustained Molecular Response (MR4.5) on DANZITEN Following Prior Imatinib Therapy
The efficacy of DANZITEN (nilotinib) tablets treatment discontinuation in adult patients with Ph+ CML-CP following prior imatinib has been established from an adequate and well-controlled study of Tasigna® (nilotinib) capsules. Below is a display of the results of Tasigna® (nilotinib) capsules in this adequate and well-controlled study.
The ENESTop (Evaluating Nilotinib Efficacy and Safety in clinical Trials-STop) study (NCT01698905) is an open-label, multicenter, single-arm study, where 163 adult patients with Ph+ CML-CP taking tyrosine kinase inhibitors (TKIs) for ≥ 3 years (imatinib as initial TKI therapy for more than 4 weeks without documented MR4.5 on imatinib at the time of switch to nilotinib, then switched to nilotinib for at least 2 years), and who achieved MR4.5 on nilotinib treatment as measured with the MolecularMD MRDx® BCR-ABL Test were enrolled to continue nilotinib treatment for an additional 52 weeks (nilotinib consolidation phase). Of the 163 patients, 126 patients (77.3%) entered the TFR phase after achieving a sustained molecular response (MR4.5) during the consolidation phase, defined by the following criterion:
The 4 last quarterly assessments (taken every 12 weeks) showed no confirmed loss of MR4.5 (BCR- ABL/ABL ≤ 0.0032% IS) during 1 year.
The median age of patients who entered the TFR phase was 56 years, 55.6% were females, and 27.8% of the patients were ≥ 65 years of age. The median actual dose intensity during the 52-week nilotinib consolidation phase was 771.8 mg/day with 52.4%, 29.4%, 0.8%, 16.7%, and 0.8% of patients receiving a daily nilotinib dosage equivalent to DANZITEN 380 mg, 284 mg, 213 mg, 190 mg and 142 mg just before entry into the TFR phase, respectively.
Patients who entered the TFR phase but experienced two consecutive measurements of BCR-ABL/ABL > 0.01% IS were considered having a confirmed loss of MR4.0, triggering reinitiation of nilotinib treatment. Patients with loss of MMR in the TFR phase immediately restarted nilotinib treatment without confirmation. All patients who restarted nilotinib therapy had BCR-ABL transcript levels monitored every 4 weeks for the first 24 weeks, then once every 12 weeks.
Efficacy was based on the 96-week analysis data cut-off date, by which time, 61 patients (48.4%) had discontinued from the TFR phase: 58 patients (46.0%) due to loss of MMR or confirmed loss of MR4.0, 2 patients (1.6%) due to subject/guardian decision and one patient (0.8%) due to pregnancy. Among the 58 patients who discontinued from the TFR phase due to confirmed loss of MR4.0 or loss of MMR, 56 patients restarted Nilotinib therapy and 2 patients permanently discontinued from the study.
By the 96-week data cut-off, of the 56 patients who restarted nilotinib treatment due to confirmed loss of MR4.0 or loss of MMR in the TFR phase, 52 patients (92.9%) regained MR4.0 and MR4.5; 4 patients (7.1%) did not regain MR4.0 by the time of the cut-off date. The cumulative rate of MR4 and MR4.5 regained by 48-weeks since treatment reinitiation, was 92.9% (52/56 patients) and 91.1% (51/56 patients), respectively.
Table 16. Efficacy Results for ENESTop
Patients Who Entered the Treatment Free Remission (TFR) Phase (Full Analysis Set, N = 126)
Patients in TFR phase1 at the specified time point
Loss of MMR or confirmed loss of MR42 by the specified time point
%
95% CI
%
24 weeks
60.3
(51.2, 68.9)
38.9
48 weeks
57.9
(48.8, 66.7)
41.3
96 weeks
53.2
(44.1, 62.1)
43.7
Abbreviation: CI, confidence interval.
1Patients without loss of MMR or confirmed loss of MR4 by specified time point of TFR phase.
2Based on the time to event (loss of MMR or confirmed loss of MR4) data during the TFR phase.
Among the 126 patients in the TFR phase, 61 patients (48.4%) had a treatment-free survival (TFS) event (defined as discontinuation from TFR phase due to any reason, loss of MMR, confirmed loss of MR4, death due to any cause, progression to AP/BC up to the end of TFR phase, or reinitiation of treatment due to any cause in the study) on or before the 96-month cut-off date.
Figure 2: Kaplan-Meier Estimate of Treatment-Free Survival after Start of TFR (Full Analysis Set ENESTop)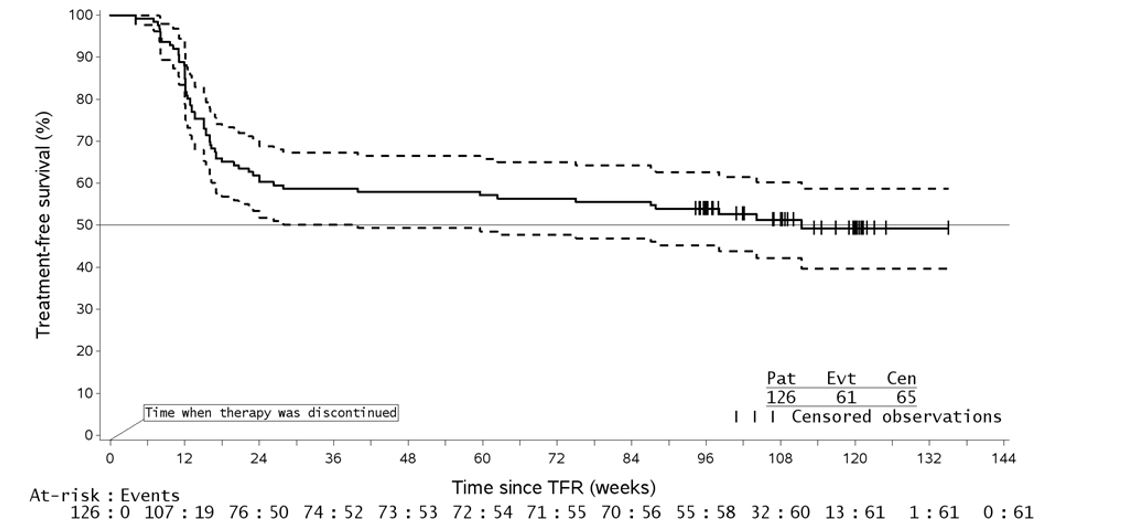
1. For a given time point, the points on the dashed curves represent the 95% confidence limits for the associated KM estimate on the solid curve.
Additional pediatric use information is approved for Novartis Pharmaceuticals Corporation’s Tasigna® (nilotinib) capsules. However, due to Novartis Pharmaceuticals Corporation’s marketing exclusivity rights, this drug product is not labeled with that pediatric information.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
DANZITEN (nilotinib) 71 mg tablets are pink, coated, oblong tablets, debossed with “N5” on one side and plain on other side. DANZITEN (nilotinib) 95 mg tablets are yellow, coated, oblong tablets, debossed with “N2” on one side and plain on other side. DANZITEN (nilotinib) 71 mg and 95 mg tablets are supplied in blister packs.
71 mg
Outer Carton containing 4 inner carton packs (4x28)...............................NDC: 24338-154-01
Inner carton containing 2 blister packs (2x14)..........................................NDC: 24338-154-02
Blisters of 14 tablets (1x14)......................................................................NDC: 24338-154-03
95 mg
Outer Carton containing 4 inner carton packs (4x28)...............................NDC: 24338-155-01
Inner carton containing 2 blister packs (2x14)..........................................NDC: 24338-155-02
Blisters of 14 tablets (1x14)......................................................................NDC: 24338-155-03
Store at 20°C to 25°C (68°F to 77°F); excursions permitted between 15°C and 30°C (59°F and 86°F) [see USP Controlled Room Temperature].
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
Taking DANZITEN
Advise patients that DANZITEN may not be substitutable, on a milligram per milligram basis, with other nilotinib products. Advise patients to take DANZITEN exactly as prescribed [see Warnings and Precautions (5.1)].
Advise patients to take DANZITEN doses twice daily approximately 12 hours apart. Advise patients to swallow the tablets whole with water and not to cut, crush, or chew the tablets.
Advise patients to take DANZITEN with or without food. Patients should not consume grapefruit products and other foods that are known to inhibit CYP3A4 at any time during DANZITEN treatment [see Dosage and Administration (2.2), Drug Interactions (7.1)].
If the patient misses a dose of DANZITEN, the patient should take the next scheduled dose at its regular time. The patient should not take two doses at the same time.
Compliance
Advise patients of the following:
Continue taking DANZITEN every day for as long as their doctor tells them.
This is a long-term treatment.
Do not change dose or stop taking DANZITEN without first consulting their doctor.Myelosuppression
Advise patients that treatment with nilotinib can cause serious thrombocytopenia, neutropenia, and anemia. Advise patients to seek immediate medical attention if symptoms suggestive of low blood counts occur, such as fever, chills or other signs of infection, unexplained bleeding or bruising, or unexplained weakness or shortness of breath [see Warnings and Precautions (5.2)].
QT Prolongation
Advise patients that nilotinib can cause possibly life-threatening, abnormal heartbeat. Advise patients to seek immediate medical attention if symptoms of abnormal heartbeat occur, such as feeling light-headed, faint or experiencing an irregular heartbeat [see Warnings and Precautions (5.3)].
Cardiac and Arterial Vascular Occlusive Events
Advise patients that cardiovascular events (including ischemic heart disease, peripheral arterial occlusive disease, and ischemic cerebrovascular events) have been reported. Advise patients to seek immediate medical attention if any symptoms suggestive of a cardiovascular event occur, such as chest or leg pain, numbness or weakness, or problems walking or speaking occur suddenly [see Warnings and Precautions (5.5)].
Pancreatitis and Elevated Serum Lipase
Advise patients that nilotinib can increase the risk of pancreatitis and that patients with a previous history of pancreatitis may be at greater risk. Advise patients to seek immediate medical attention if symptoms suggestive of pancreatitis occur, such as sudden stomach area pain with accompanying nausea and vomiting [see Warnings and Precautions (5.6)].
Hepatotoxicity
Advise patients that nilotinib can increase the risk of hepatotoxicity and that patients with previous history of liver diseases may be at risk. Advise patients to seek immediate medical attention if any symptoms suggestive of hepatotoxicity occur, such as stomach pain, yellow skin and eyes, and dark-colored urine [see Warnings and Precautions (5.7)].
Tumor Lysis Syndrome
Advise patients that nilotinib can cause TLS and to seek immediate medical attention if any symptoms suggestive of TLS occur, such as an abnormal heartbeat or less urine production [see Warnings and Precautions (5.9)].
Hemorrhage
Advise patients that serious hemorrhagic events, including fatal events, have occurred in patients with CML treated with nilotinib. Advise patients to seek immediate medical attention if symptoms suggestive of hemorrhage occur, such as uncontrolled bleeding, changes in eyesight, unconsciousness, or sudden headache or sudden confusion in surroundings [see Warnings and Precautions (5.10)].
Fluid Retention
Advise patients that nilotinib can cause fluid retention and to seek immediate medical attention if any symptoms suggestive of fluid retention, such as shortness of breath, rapid weight gain, or swelling occur [see Warnings and Precautions (5.13)].
Effects on Growth and Development in Pediatric Patients
Inform pediatric patients and their caregivers of the possibility of developing growth abnormalities. Growth retardation has been reported in pediatric patients treated with nilotinib. Therefore, monitor growth and development in pediatric patients [see Warnings and Precautions (5.14)].
Treatment-Free Remission (TFR)
Advise patients that frequent monitoring is required to detect possible loss of remission if TFR is attempted. Advise patients that musculoskeletal symptoms, such as muscle pain, pain in extremity, joint pain, bone pain, or spinal pain, may occur more frequently than before treatment discontinuation [see Warnings and Precautions (5.16)].
Embryo-Fetal Toxicity
Advise pregnant women of the potential risk to a fetus. Advise females of reproductive potential to inform their healthcare provider of a known or suspected pregnancy [see Warnings and Precautions (5.15), Use in Specific Populations (8.1)].
Advise females of reproductive potential to use effective contraception during treatment and for 14 days after receiving the last dose of DANZITEN [see Use in Specific Populations (8.3)].
Lactation
Advise women not to breastfeed during treatment with DANZITEN and for 14 days after the last dose [see Use in Specific Populations (8.2)].
Drug Interactions
Advise patients that DANZITEN and certain other medicines, including over the counter medications or herbal supplements (such as St. John’s Wort), can interact with each other [see Drug Interactions (7)].
Manufactured for:
Azurity Pharmaceuticals, Inc.
Woburn, MA 01801
Medication Guide
DANZITEN (dan-zi-ten)
(nilotinib)
tabletsWhat is the most important information I should know about DANZITEN?
DANZITEN can cause a possible life-threatening heart problem called QTc prolongation. QTc prolongation causes an irregular heartbeat, which may lead to sudden death.
Your healthcare provider should check the electrical activity of your heart with a test called an electrocardiogram (ECG):
before starting DANZITEN
with any dose changes
7 days after starting DANZITEN
regularly during DANZITEN treatment
You may lower your chances for having QTc prolongation with Nilotinib if you:
Do not drink grapefruit juice, eat grapefruit, or take supplements containing grapefruit extract during treatment with DANZITEN.Grapefruit products increase the amount of Nilotinib in your body.
Avoid taking other medicines or supplements with Nilotinib that can also cause QTc prolongation.
Nilotinib can interact with many medicines and supplements and increase your chance for serious and life-threatening side effects.
Do not take any other medicine during treatment with DANZITEN unless your healthcare provider tells you it is okay to do so.
For more information, see “How should I take DANZITEN?”
Call your healthcare provider right away if you feel lightheaded, faint, or have an irregular heartbeat during treatment with DANZITEN. These can be symptoms of QTc prolongation.
See “What are the possible side effects of DANZITEN? for more information about side effects.
What is DANZITEN?
DANZITEN is a prescription medicine used to treat:
adults who have been newly diagnosed with a certain type of leukemia called Philadelphia chromosome positive chronic myeloid leukemia (Ph+ CML) in chronic phase.
adults with chronic phase Ph+ CML or accelerated phase Ph+ CML who:
o are no longer benefiting from other treatments, including imatinib (Gleevec), or
o have taken other treatments, including imatinib (Gleevec), and cannot tolerate them.
It is not known if nilotinib is safe and effective in children younger than 1 year of age with newly diagnosed, resistant, or intolerant Ph+ CML in chronic phase.
The long-term effects of treating children with nilotinib for a long period of time are not known.
Who should not take DANZITEN?
Do not take if you have:
low levels of potassium or magnesium in your blood
long QTc syndromeBefore taking DANZITEN, tell your healthcare provider about all of your medical conditions, including if you:
have heart problems
have had a stroke or other problems due to decreased blood flow to the brain
have problems with decreased blood flow to your legs
have irregular heartbeat
have QTc prolongation or a family history of it
have liver problems
have had pancreatitis
have low blood levels of potassium or magnesium in your blood
have bleeding problems
had a surgical procedure involving the removal of the entire stomach (total gastrectomy)
are pregnant or plan to become pregnant. Nilotinib can harm your unborn baby. Tell your healthcare provider right away if you are pregnant, or if you become pregnant during treatment with DANZITEN.
In females who are able to become pregnant:
Your healthcare provider should do a pregnancy test before you start treatment with DANZITEN.
Use effective birth control (contraception) during treatment with DANZITEN and for 14 days after the last dose.
are breastfeeding or plan to breastfeed. It is not known if Nilotinib passes into your breast milk. Do not breastfeed during treatment and for 14 days after your last dose of DANZITEN.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins and herbal supplements.
If you need to take antacids (medicines to treat heartburn) do not take them at the same time that you take DANZITEN. If you take:
a medicine to block the amount of acid produced in the stomach (H2 blocker): Take these medicines about 10 hours before you take DANZITEN, or about 2 hours after you take DANZITEN.
an antacid that contains aluminum hydroxide, magnesium hydroxide, and simethicone to reduce the amount of acid in the stomach: Take these medicines about 2 hours before or about 2 hours after you take DANZITEN.
Nilotinib can interact with many medicines and supplements and increase your chance for serious and life-threatening side effects. See “What is the most important information I should know about DANZITEN?”How should I take DANZITEN?
Do not switch from DANZITEN to other medicines that contain nilotinib without talking to your healthcare provider. The amount of nilotinib in a dose of DANZITEN may not be the same as the amount in other medicines that contain nilotinib.
Take DANZITEN exactly as your healthcare provider tells you to take it. Do not change your dose or stop taking DANZITEN unless your healthcare provider tells you.
DANZITEN is a long-term treatment.
Take your prescribed dose of DANZITEN 2 times a day, about 12 hours apart.
Swallow DANZITEN tablets whole with water. Do not cut, crush, or chew the tablets. If you cannot swallow DANZITEN whole, tell your healthcare provider.
Take DANZITEN with or without food.
Do not drink grapefruit juice, eat grapefruit, or take supplements containing grapefruit extract at any time during treatment. See “What is the most important information I should know about DANZITEN?”
If you miss a dose, just take your next dose at your regular time. Do not take 2 doses at the same time to make up for a missed dose.
If you take too much DANZITEN, call your healthcare provider or go to the nearest hospital emergency room right away. Symptoms may include vomiting and drowsiness.
During treatment with DANZITEN your healthcare provider will do tests to check for side effects and to see how well DANZITEN is working for you. The tests will check your:
o heart
o blood cells (white blood cells, red blood cells, and platelets). Your blood cells should be checked every 2 weeks for the first 2 months and then monthly.
o electrolytes (potassium, magnesium)
o pancreas and liver function
o bone marrow samples
Your healthcare provider may change your dose. Your healthcare provider may have you stop DANZITEN for some time or lower your dose if you have side effects with it.
Your healthcare provider will monitor your CML during treatment with DANZITEN to see if you are in a remission. After at least 3 years of treatment with DANZITEN, your healthcare provider may do certain tests to determine if you continue to be in remission. Based on your test results, your healthcare provider may decide if you may be eligible to try stopping treatment with DANZITEN. This is called Treatment Free Remission (TFR).
Your healthcare provider will carefully monitor your CML during and after you stop taking DANZITEN. Based on your test results, your healthcare provider may need to re-start your DANZITEN if your CML is no longer in remission.
It is important that you are followed by your healthcare provider and undergo frequent monitoring to find out if you need to re-start your DANZITEN treatment because you are no longer in TFR. Follow your healthcare provider’s instructions about re-starting DANZITEN if you are no longer in TFR.
What are the possible side effects of DANZITEN?
DANZITEN may cause serious side effects, including:
See “What is the most important information I should know about DANZITEN?”
Low blood cell counts. Low blood cell counts (red blood cells, white blood cells, and platelets) are common with DANZITEN, but can also be severe. Your healthcare provider will check your blood counts regularly during treatment with DANZITEN. Call your healthcare provider or get medical help right away if you develop any signs or symptoms of low blood counts, including:
o fever
o chills or other signs of infection
o unexplained bleeding or bruising
o unexplained weakness
o shortness of breath
Decreased blood flow to the leg, heart, or brain. People who have recently been diagnosed with Ph+ CML and take DANZITEN may develop decreased blood flow to the leg, the heart, or brain.
Get medical help right away if you suddenly develop any of the following symptoms:
chest pain or discomfort
numbness or weakness
problems walking or speaking
leg pain
your leg feels cold
change in the skin color of your leg
Pancreas inflammation (pancreatitis). Tell your healthcare provider right away if you develop any symptoms of pancreatitis, including sudden stomach area pain with nausea and vomiting.
Liver problems.DANZITEN can increase your risk of liver problems. People who have had liver problems in the past may be at risk for getting liver problems with DANZITEN. Call your healthcare provider or get medical help right away if you develop any symptoms of liver problems, including:
stomach area (abdominal) pain yellow skin and eyes dark-colored urine
Tumor Lysis Syndrome (TLS). TLS is caused by a fast breakdown of cancer cells. Your healthcare provider may do blood tests to check you for TLS. TLS can cause you to have:
○ kidney failure and the need for dialysis treatment
○ an abnormal heartbeat
Bleeding problems. Serious bleeding problems and death have happened during treatment with DANZITEN. Tell your healthcare provider right away if you develop any signs and symptoms of bleeding during treatment with DANZITEN.
Fluid retention. Your body may hold too much fluid (fluid retention). Symptoms of fluid retention include shortness of breath, rapid weight gain, and swelling.
Abnormal growth or development in children. Effects on growth and development have happened in children with chronic phase Ph+ CML during treatment with nilotinib. Some children and adolescents may have slower than normal growth during treatment with nilotinib.
The most common side effects of DANZITEN in adults include:
nausea diarrhea
rash cough
headache constipation
tiredness muscle and joint pain
itching runny or stuffy nose, sneezing, sore throat
vomiting fever
night sweats
Side effects in adult patients attempting treatment free remission:
If you and your healthcare provider decide that you can stop taking DANZITEN and try treatment free remission (TFR), you may have more muscle and bone (musculoskeletal) symptoms than before you stopped treatment. Symptoms may include:
muscle pain bone pain
arm and leg pain spine pain
joint pain
Tell your healthcare provider if you have any side effect that bothers you or does not go away. These are not all of the possible side effects of DANZITEN.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store DANZITEN?
Store DANZITEN at room temperature between 68°F to 77°F (20°C to 25°C).
Safely throw away medicine that is out of date or no longer needed.
Keep DANZITEN and all medicines out of the reach of children.General information about the safe and effective use of DANZITEN.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use DANZITEN for a condition for which it was not prescribed. Do not give DANZITEN to other people, even if they have the same symptoms that you have. It may harm them. You can ask your pharmacist or healthcare provider for information about DANZITEN that is written for health professionals.What are the ingredients in DANZITEN?
Active ingredient: nilotinib tartrate
Inactive ingredients: colloidal silicon dioxide, croscarmellose sodium, hypromellose acetate succinate, iron oxide red (in 71 mg strength tablets), iron oxide yellow (in 95 mg strength tablets), magnesium stearate, microcrystalline cellulose, polyethylene glycol, polyvinyl alcohol, talc, and titanium dioxide.
Additional pediatric use information is approved for Novartis Pharmaceuticals Corporation’s Tasigna® (nilotinib) capsules. However, due to Novartis Pharmaceuticals Corporation’s marketing exclusivity rights, this drug product is not labeled with that pediatric information.
Manufactured for:
Azurity Pharmaceuticals, Inc.
Woburn, MA 01801
This Medication Guide has been approved by the U.S. Food and Drug Administration. Issued: 11/2024
-
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
NDC: 24338-154-01
DANZITEN (nilotinib) tablets 71 mg - Outer Carton Label
Outer Carton containing 4 inner carton packs (4x28)
71 mg per tablet

NDC: 24338-154-02
DANZITEN (nilotinib) tablets 71 mg - Inner Carton Label
Carton of 2 blister packs (2x14)
71 mg per tablet
Package Label Principal Display Panel
NDC: 24338-155-01
DANZITEN (nilotinib) tablets 95 mg - Outer Carton Label
Outer Carton containing 4 inner carton packs (4x28)
95 mg per tablet

NDC: 24338-155-02
DANZITEN (nilotinib) tablets 95 mg - Inner Carton Label
Carton of 2 blister packs (2x14)
95 mg per tablet
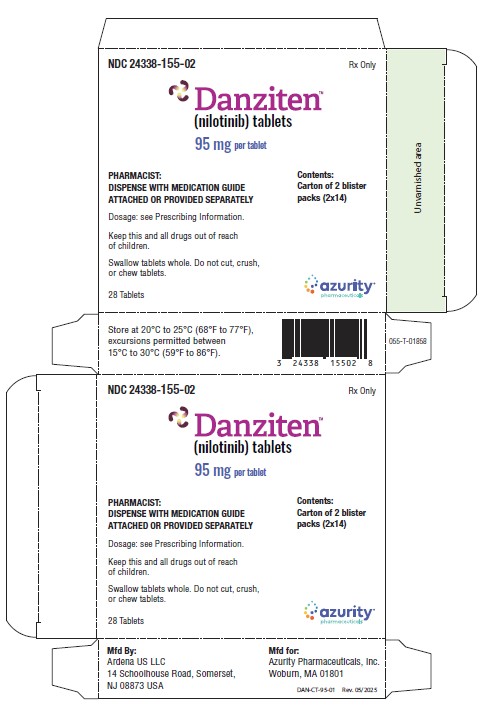
-
INGREDIENTS AND APPEARANCE
DANZITEN
nilotinib tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 24338-154 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength NILOTINIB (UNII: F41401512X) (NILOTINIB - UNII:F41401512X) NILOTINIB 71 mg Inactive Ingredients Ingredient Name Strength CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) HYPROMELLOSE ACETATE SUCCINATE 12070923 (3 MPA.S) (UNII: 36BGF0E889) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) MAGNESIUM STEARATE (UNII: 70097M6I30) POLYVINYL ALCOHOL (UNII: 532B59J990) POLYETHYLENE GLYCOL 3350 (UNII: G2M7P15E5P) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) Product Characteristics Color PINK Score no score Shape CAPSULE Size 16mm Flavor Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 24338-154-01 4 in 1 CARTON 11/30/2024 1 NDC: 24338-154-02 2 in 1 CARTON 1 NDC: 24338-154-03 14 in 1 BLISTER PACK; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA219293 11/30/2024 DANZITEN
nilotinib tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 24338-155 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength NILOTINIB (UNII: F41401512X) (NILOTINIB - UNII:F41401512X) NILOTINIB 95 mg Inactive Ingredients Ingredient Name Strength CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) HYPROMELLOSE ACETATE SUCCINATE 12070923 (3 MPA.S) (UNII: 36BGF0E889) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) MAGNESIUM STEARATE (UNII: 70097M6I30) POLYVINYL ALCOHOL (UNII: 532B59J990) POLYETHYLENE GLYCOL 3350 (UNII: G2M7P15E5P) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) Product Characteristics Color YELLOW Score no score Shape CAPSULE Size 19mm Flavor Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 24338-155-01 4 in 1 CARTON 11/30/2024 1 NDC: 24338-155-02 2 in 1 CARTON 1 NDC: 24338-155-03 14 in 1 BLISTER PACK; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA219293 11/30/2024 Labeler - Azurity Pharmaceuticals, Inc. (117505635)
Trademark Results [DANZITEN]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 DANZITEN 98354233 not registered Live/Pending |
Azurity Pharmaceuticals, Inc. 2024-01-12 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.