ESTERIFIED ESTROGENS AND METHYLTESTOSTERONE tablet
Esterified Estrogens and Methyltestosterone by
Drug Labeling and Warnings
Esterified Estrogens and Methyltestosterone by is a Prescription medication manufactured, distributed, or labeled by ANI Pharmaceuticals, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
BOXED WARNING
(What is this?)
ESTROGENS INCREASE THE RISK OF ENDOMETRIAL CANCER
Close clinical surveillance of all women taking estrogens is important. Adequate diagnostic measures, including endometrial sampling when indicated, should be undertaken to rule out malignancy in all cases of undiagnosed persistent or recurring abnormal vaginal bleeding. There is no evidence that the use of "natural" estrogens results in a different endometrial risk profile than synthetic estrogens at equivalent estrogen doses. (See WARNINGS, Malignant Neoplasms, Endometrial Cancer.)
CARDIOVASCULAR AND OTHER RISKS
Estrogens with or without progestins should not be used for the prevention of cardiovascular disease. (See WARNINGS, Cardiovascular Disorders.)
The Women's Health Initiative (WHI) study reported increased risks of myocardial infarction, stroke, invasive breast cancer, pulmonary emboli, and deep vein thrombosis in postmenopausal women (50 to 79 years of age) during 5 years of treatment with oral conjugated estrogens (CE 0.625 mg) combined with medroxyprogesterone acetate (MPA 2.5 mg) relative to placebo. (See CLINICAL PHARMACOLOGY, Clinical Studies.)
The Women's Health Initiative Memory Study (WHIMS), a substudy of WHI, reported increased risk of developing probable dementia in postmenopausal women 65 years of age or older during 4 years of treatment with oral conjugated estrogens plus medroxyprogesterone acetate relative to placebo. It is unknown whether this finding applies to younger postmenopausal women or to women taking estrogen alone therapy. (See CLINICAL PHARMACOLOGY, Clinical Studies.)
Other doses of oral conjugated estrogens with medroxyprogesterone acetate, and other combinations and dosage forms of estrogens and progestins were not studied in the WHI clinical trials and, in the absence of comparable data, these risks should be assumed to be similar. Because of these risks, estrogens with or without progestins should be prescribed at the lowest effective doses and for the shortest duration consistent with treatment goals and risks for the individual woman.
-
DESCRIPTION
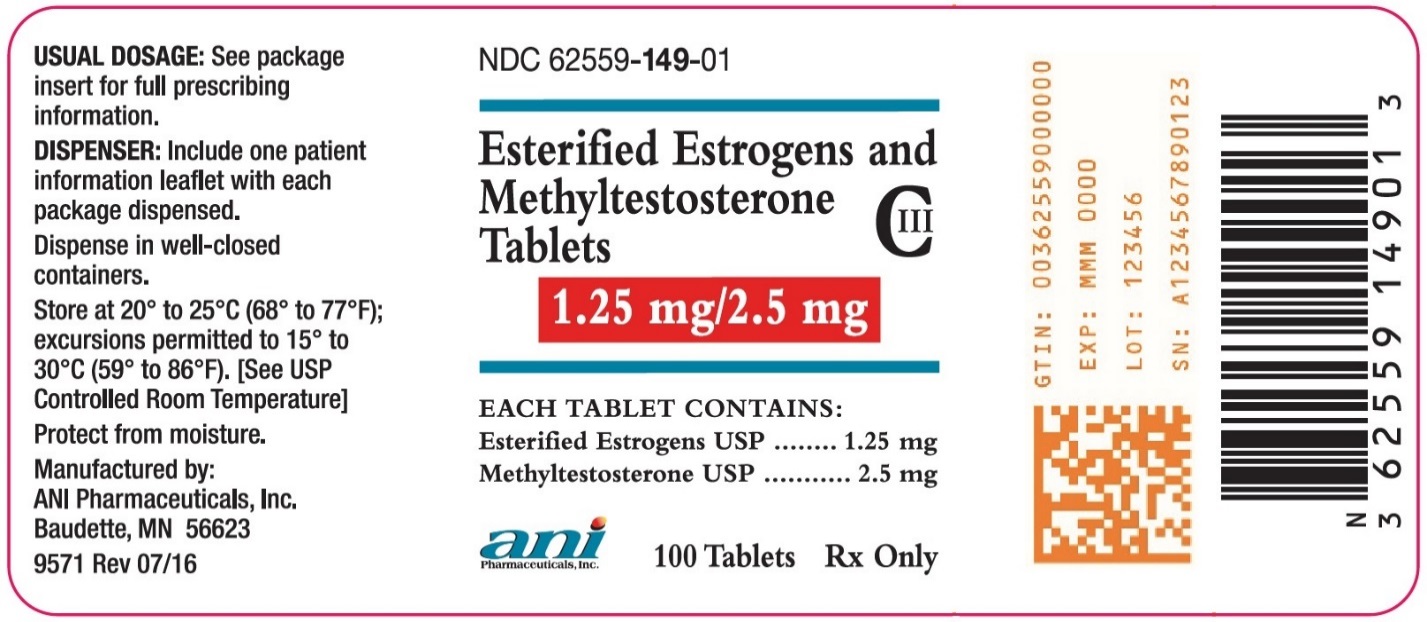
Esterified Estrogens and Methyltestosterone Tablets: Each dark green, capsule shaped, sugar-coated oral tablet imprinted with “1490” contains: 1.25 mg of Esterified Estrogens, USP and 2.5 mg of Methyltestosterone, USP.
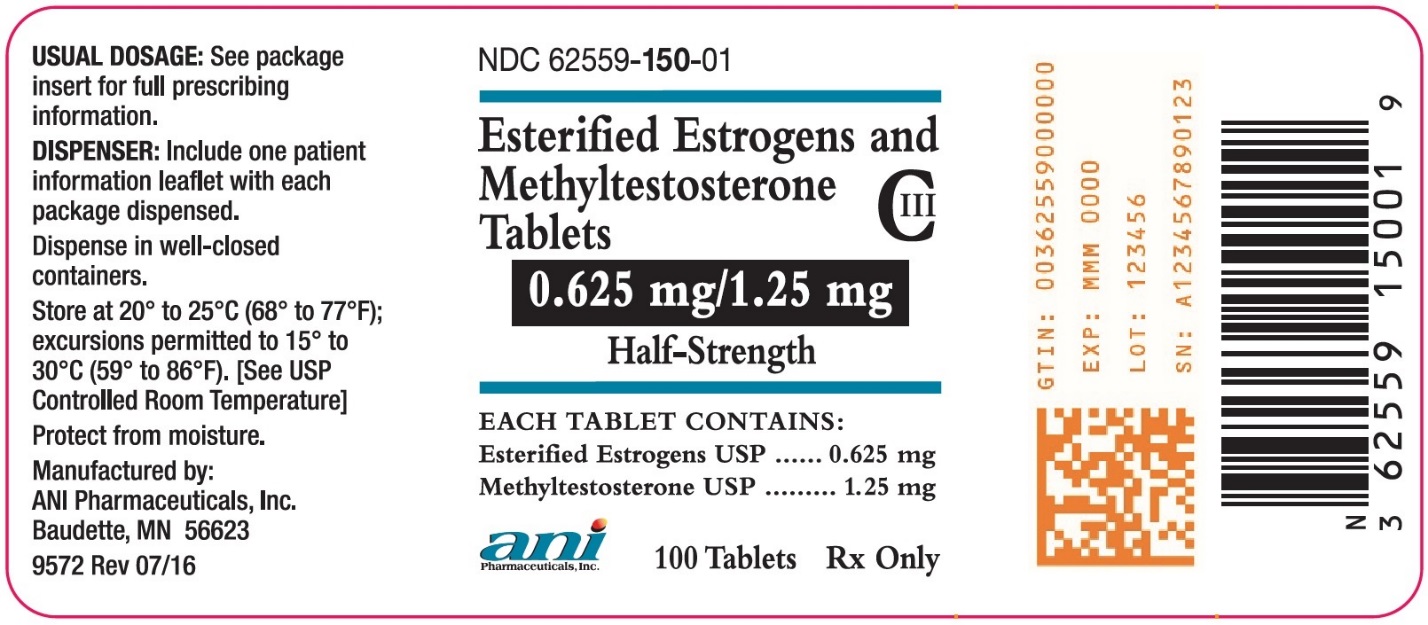
Esterified Estrogens and Methyltestosterone Half-Strength Tablets: Each light green, capsule shaped, sugar-coated oral tablet imprinted with “1507” contains: 0.625 mg of Esterified Estrogens, USP and 1.25 mg of Methyltestosterone, USP.
Esterified Estrogens
Esterified Estrogens, USP is a mixture of the sodium salts of the sulfate esters of the estrogenic substances, principally estrone, that are of the type excreted by pregnant mares. Esterified Estrogens contain not less than 75.0 percent and not more than 85.0 percent of sodium estrone sulfate, and not less than 6.0 percent and not more than 15.0 percent of sodium equilin sulfate, in such proportion that the total of these two components is not less than 90.0 percent.
Methyltestosterone
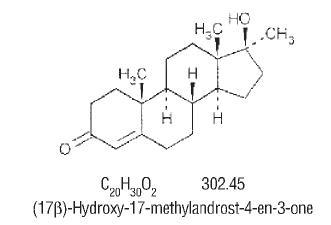
Methyltestosterone, USP is an androgen. Androgens are derivatives of cyclopentano-perhydrophenanthrene. Endogenous androgens are C-19 steroids with a side chain at C-17, and with two angular methyl groups. Testosterone is the primary endogenous androgen. Fluoxymesterone and methyltestosterone are synthetic derivatives of testosterone.
Methyltestosterone is a white to light yellow crystalline substance that is virtually insoluble in water but soluble in organic solvents. It is stable in air but decomposes in light.
Methyltestosterone structural formula:
Esterified Estrogens and Methyltestosterone Full and Half-Strength Tablets contain the following inactive ingredients: acacia, calcium carbonate, carnauba wax, citric acid, colloidal silicon dioxide, di-acetylated monoglycerides, gelatin, lactose, magnesium stearate, methylparaben, microcrystalline cellulose, pharmaceutical glaze, povidone, propylene glycol, propylparaben, shellac glaze, sodium benzoate, sodium bicarbonate, sorbic acid, starch, sucrose, talc, titanium dioxide, tromethamol, FD&C Blue No. 1 Aluminum Lake, and D&C Yellow No. 10 Aluminum Lake.
Esterified Estrogens and Methyltestosterone Tablets also contain: FD&C Yellow No. 6 Aluminum Lake.
Esterified Estrogens and Methyltestosterone Half-Strength Tablets also contain: FD&C Blue No. 2 Aluminum Lake and Iron Oxide Black.
-
CLINICAL PHARMACOLOGY
Estrogens:
Endogenous estrogens are largely responsible for the development and maintenance of the female reproductive system and secondary sexual characteristics. Although circulating estrogens exist in a dynamic equilibrium of metabolic interconversions, estradiol is the principal intracellular human estrogen and is substantially more potent than its metabolites, estrone and estriol at the receptor level.
The primary source of estrogen in normally cycling adult women is the ovarian follicle, which secretes 70 to 500 mcg of estradiol daily, depending on the phase of the menstrual cycle. After menopause, most endogenous estrogen is produced by conversion of androstenedione, secreted by the adrenal cortex, to estrone by peripheral tissues. Thus, estrone and the sulfate conjugated form, estrone sulfate, are the most abundant circulating estrogens in postmenopausal women.
Estrogens act through binding to nuclear receptors in estrogen-responsive tissues. To date, two estrogen receptors have been identified. These vary in proportion from tissue to tissue.
Circulating estrogens modulate the pituitary secretion of the gonadotropins, luteinizing hormone (LH) and follicle stimulating hormone (FSH), through a negative feedback mechanism. Estrogens act to reduce the elevated levels of these hormones seen in postmenopausal women.
Estrogen Pharmacokinetics
Distribution
The distribution of exogenous estrogens is similar to that of endogenous estrogens. Estrogens are widely distributed in the body and are generally found in higher concentrations in the sex hormone target organs. Estrogens circulate in the blood largely bound to sex hormone binding globulin (SHBG) and albumin.Metabolism
Exogenous estrogens are metabolized in the same manner as endogenous estrogens. Circulating estrogens exist in a dynamic equilibrium of metabolic interconversions. These transformations take place mainly in the liver. Estradiol is converted reversibly to estrone, and both can be converted to estriol, which is the major urinary metabolite. Estrogens also undergo enterohepatic recirculation via sulfate and glucuronide conjugation in the liver, biliary secretion of conjugates into the intestine, and hydrolysis in the gut followed by reabsorption. In postmenopausal women, a significant proportion of the circulating estrogens exist as sulfate conjugates, especially estrone sulfate, which serves as a circulating reservoir for the formation of more active estrogens.Excretion
Estradiol, estrone and estriol are excreted in the urine along with glucuronide and sulfate conjugates.Drug Interactions
In vitro and in vivo studies have shown that estrogens are metabolized partially by cytochrome P450 3A4 (CYP3A4). Therefore, inducers or inhibitors of CYP3A4 may affect estrogen drug metabolism. Inducers of CYP3A4 such as St. John’s Wort preparations (Hypericum perforatum), phenobarbital, carbamazepine, and rifampin may reduce plasma concentrations of estrogens, possibly resulting in a decrease in therapeutic effects and/or changes in the uterine bleeding profile. Inhibitors of CYP3A4 such as erythromycin, clarithromycin, ketoconazole, itraconazole, ritonavir and grapefruit juice may increase plasma concentrations of estrogens and may result in side effects.Clinical Studies
Women’s Health Initiative Studies
The Women’s Health Initiative (WHI) enrolled a total of 27,000 predominantly healthy postmenopausal women to assess the risks and benefits of either the use of oral 0.625 mg conjugated estrogens (CE) per day alone or the use of oral 0.625 mg conjugated estrogens plus 2.5 mg medroxyprogesterone acetate (MPA) per day compared to placebo in the prevention of certain chronic diseases. The primary endpoint was the incidence of coronary heart disease (CHD) (nonfatal myocardial infarction and CHD death), with invasive breast cancer as the primary adverse outcome studied. A “global index” included the earliest occurrence of CHD, invasive breast cancer, stroke, pulmonary embolism (PE), endometrial cancer, colorectal cancer, hip fracture, or death due to other cause. The study did not evaluate the effects of CE or CE/MPA on menopausal symptoms.The CE-only substudy has concluded. The impact of those results are under review. The CE/MPA substudy was stopped early because, according to the predefined stopping rule, the increased risk of breast cancer and cardiovascular events exceeded the specified benefits included in the "global index." Results of the CE/MPA substudy, which included 16,608 women (average age of 63 years, range 50 to 79; 83.9% White, 6.5% Black, 5.5% Hispanic), after an average follow-up of 5.2 years are presented in Table 1 below.
TABLE 1 Relative and Absolute Risk Seen in the CE/MPA Substudy of WHI a Eventc Relative Risk CE/MPA versus Placebo at 5.2 Years (95% CI*) Placebo
n = 8102
CE/MPA
n = 8506
Absolute Risk
per 10,000 Women-years
a adapted from JAMA, 2002; 288:321-333
b includes metastatic and non-metastatic breast cancer with the exception of in situ breast cancer
c a subset of the events was combined in a “global index”, defined as the earliest occurrence of CHD events, invasive breast cancer, stroke, pulmonary embolism, endometrial cancer, colorectal cancer, hip fracture, or death due to other causes
d not included in the Global Index
* nominal confidence intervals unadjusted or multiple looks and multiple comparisonsCHD events
1.29 (1.02 – 1.63)
30
37
Non-fatalMI
1.32 (1.02 – 1.72)
23
30
CHD death
1.18 (0.70 – 1.97)
6
7
Invasive breast cancer b
1.26 (1.00 – 1.59)
30
38
Stroke
1.41 (1.07 – 1.85)
21
29
Pulmonary embolism
2.13 (1.39 – 3.25)
8
16
Colorectal cancer
0.63 (0.43 – 0.92)
16
10
Endometrial cancer
0.83 (0.47 – 1.47)
6
5
Hip fracture
0.66 (0.45 – 0.98)
15
10
Death due to causes other than the events above
0.92 (0.74 – 1.14)
40
37
Global Indexc
1.15 (1.03 – 1.28)
151
170
Deep vein thrombosisd
2.07 (1.49 – 2.87)
13
26
Vetebral fracturesd
0.66 (0.44 – 0.98)
15
9
Other osteoporotic fracturesd
0.77 (0.69 – 0.86)
170
131
For those outcomes included in the "global index," the absolute excess risks per 10,000 women-years in the group treated with CE/MPA were 7 more CHD events, 8 more strokes, 8 more PEs, and 8 more invasive breast cancers, while the absolute risk reductions per 10,000 women-years were 6 fewer colorectal cancers and 5 fewer hip fractures. The absolute excess risk of events included in the "global index" was 19 per 10,000 women-years. There was no difference between the groups in terms of all-cause mortality. (See BOXED WARNINGS, WARNINGS and PRECAUTIONS.)
Women’s Health Initiative Memory Study
The Women's Health Initiative Memory Study (WHIMS), a substudy of WHI, enrolled 4,532 predominantly healthy postmenopausal women 65 years of age and older (47% were age 65 to 69 years, 35% were 70 to 74 years, and 18% were 75 years of age and older) to evaluate the effects of CE/MPA (0.625 mg conjugated estrogens plus 2.5 mg medroxyprogesterone acetate) on the incidence of probable dementia (primary outcome) compared with placebo.After an average follow-up of 4 years, 40 women in the estrogen/progestin group (45 per 10,000 women-years) and 21 in the placebo group (22 per 10,000 women-years) were diagnosed with probable dementia. The relative risk of probable dementia in the hormone therapy group was 2.05 (95% CI, 1.21 to 3.48) compared to placebo. Differences between groups became apparent in the first year of treatment. It is unknown whether these findings apply to younger postmenopausal women. (See BOXED WARNINGS and WARNINGS, Dementia.)
Androgens:
Endogenous androgens are responsible for the normal growth and development of the male sex organs and for maintenance of secondary sex characteristics. These effects include the growth and maturation of prostate, seminal vesicles, penis, and scrotum; the development of male hair distribution, such as beard, pubic, chest, and axillary hair, laryngeal enlargement, vocal cord thickening, alterations in body musculature, and fat distribution. Drugs in this class also cause retention of nitrogen, sodium, potassium, phosphorus, and decreased urinary excretion of calcium. Androgens have been reported to increase protein anabolism and decrease protein catabolism. Nitrogen balance is improved only when there is sufficient intake of calories and protein. Androgens are responsible for the growth spurt of adolescence and for the eventual termination of linear growth which is brought about by fusion of the epiphyseal growth centers. In children, exogenous androgens accelerate linear growth rates, but may cause a disproportionate advancement in bone maturation. Use over long periods may result in fusion of the epiphyseal growth centers and termination of growth process. Androgens have been reported to stimulate the production of red blood cells by enhancing the production of erythropoietic stimulating factor.
Androgen Pharmacokinetics
Testosterone given orally is metabolized by the gut and 44 percent is cleared by the liver in the first pass. Oral doses as high as 400 mg per day are needed to achieve clinically effective blood levels for full replacement therapy. The synthetic androgens (methyltestosterone and fluoxymesterone) are less extensively metabolized by the liver and have longer half-lives. They are more suitable than testosterone for oral administration.Testosterone in plasma is 98 percent bound to a specific testosterone-estradiol binding globulin, and about 2 percent is free. Generally, the amount of this sex-hormone binding globulin in the plasma will determine the distribution of testosterone between free and bound forms, and the free testosterone concentration will determine its half-life.
About 90 percent of a dose of testosterone is excreted in the urine as glucuronic and sulfuric acid conjugates of testosterone and its metabolites; about 6 percent of a dose is excreted in the feces, mostly in the unconjugated form. Inactivation of testosterone occurs primarily in the liver. Testosterone is metabolized to various 17-keto steroids through two different pathways. There are considerable variations of the half-life of testosterone as reported in the literature, ranging from 10 to 100 minutes.
In many tissues the activity of testosterone appears to depend on reduction to dihydrotestosterone, which binds to cytosol receptor proteins. The steroid-receptor complex is transported to the nucleus where it initiates transcription events and cellular changes related to androgen action.
-
INDICATIONS AND USAGE
Esterified Estrogens and Methyltestosterone Full and Half-Strength Tablets are indicated in the:
- Treatment of moderate to severe vasomotor symptoms associated with the menopause in those patients not improved by estrogens alone. (There is no evidence that estrogens are effective for nervous symptoms or depression without associated vasomotor symptoms, and they should not be used to treat such conditions.)
- Esterified Estrogens and Methyltestosterone Full and Half-Strength Tablets have not been shown to be effective for any purpose during pregnancy and its use may cause severe harm to the fetus.
-
CONTRAINDICATIONS
Esterified Estrogens and Methyltestosterone Full and Half-Strength Tablets should not be used in women with any of the following conditions:
- 1. Undiagnosed abnormal genital bleeding.
- 2. Known, suspected, or history of cancer of the breast.
- 3. Known or suspected estrogen-dependent neoplasia.
- 4. Active deep vein thrombosis, pulmonary embolism or history of these conditions.
- 5. Active or recent (e.g., within the past year) arterial thromboembolic disease (e.g., stroke, myocardial infarction).
- 6. Liver dysfunction or disease.
- 7. Esterified Estrogens and Methyltestosterone Full and Half-Strength Tablets should not be used in patients with known hypersensitivity to its ingredients.
- 8. Known or suspected pregnancy. There is no indication for Esterified Estrogens and Methyltestosterone Full and Half-Strength Tablets in pregnancy. There appears to be little or no increased risk of birth defects in children born to women who have used estrogens and progestins from oral contraceptives inadvertently during early pregnancy. (See PRECAUTIONS.)
Methyltestosterone should not be used in:
- 1. The presence of severe liver damage.
- 2. Pregnancy and in breast-feeding mothers because of the possibility of masculinization of the female fetus or breast-fed infant.
-
WARNINGS
See BOXED WARNINGS
Warnings Associated with Estrogens
Cardiovascular Disorders
Estrogen and estrogen/progestin therapy has been associated with an increased risk of cardiovascular events such as myocardial infarction and stroke, as well as venous thrombosis and pulmonary embolism (venous thromboembolism or VTE). Should any of these occur or be suspected, estrogens should be discontinued immediately.
Risk factors for arterial vascular disease (e.g., hypertension, diabetes mellitus, tobacco use, hypercholesterolemia, and obesity) and/or venous thromboembolism (e.g., personal history or family history of VTE, obesity, and systemic lupus erythematosus) should be managed appropriately.
Coronary Heart Disease and Stroke: In the Women's Health Initiative (WHI) study, an increase in the number of myocardial infarctions and strokes was observed in women receiving CE compared to placebo. The CE-only substudy has concluded. The impact of those results are under review. (See CLINICAL PHARMACOLOGY, Clinical Studies.)
In the CE/MPA substudy of WHI, an increased risk of coronary heart disease (CHD) events (defined as nonfatal myocardial infarction and CHD death) was observed in women receiving CE/MPA compared to women receiving placebo (37 versus 30 per 10,000 women-years). The increase in risk was observed in year 1 and persisted.
In the same substudy of WHI, an increased risk of stroke was observed in women receiving CE/MPA compared to women receiving placebo (29 versus 21 per 10,000 women-years). The increase in risk was observed after the first year and persisted.
In postmenopausal women with documented heart disease (n = 2,763, average age 66.7 years) a controlled clinical trial of secondary prevention of cardiovascular disease (Heart and Estrogen/Progestin Replacement Study; HERS) treatment with CE/MPA (0.625 mg/2.5 mg per day) demonstrated no cardiovascular benefit. During an average follow-up of 4.1 years, treatment with CE/MPA did not reduce the overall rate of CHD events in postmenopausal women with established coronary heart disease. There were more CHD events in the CE/MPA-treated group than in the placebo group in year 1, but not during the subsequent years. Two thousand three hundred and twenty one women from the original HERS trial agreed to participate in an open-label extension of HERS, HERS II. Average follow-up in HERS II was an additional 2.7 years, for a total of 6.8 years overall. Rates of CHD events were comparable among women in the CE/MPA group and the placebo group in HERS, HERS II, and overall.
Large doses of estrogen (5 mg conjugated estrogens per day), comparable to those used to treat cancer of the prostate and breast, have been shown in a large prospective clinical trial in men to increase the risks of nonfatal myocardial infarction, pulmonary embolism, and thrombophlebitis.
Venous Thromboembolism (VTE.): In the Women's Health Initiative (WHI) study, an increase in VTE was observed in women receiving CE compared to placebo. The CE-only substudy has concluded. The impact of those results are under review. (See CLINICAL PHARMACOLOGY, Clinical Studies.)
In the CE/MPA substudy of WHI, a 2-fold greater rate of VTE, including deep venous thrombosis and pulmonary embolism, was observed in women receiving CE/MPA compared to women receiving placebo. The rate of VTE was 34 per 10,000 women-years in the CE/MPA group compared to 16 per 10,000 women-years in the placebo group. The increase in VTE risk was observed during the first year and persisted.
If feasible, estrogens should be discontinued at least 4 to 6 weeks before surgery of the type associated with an increased risk of thromboembolism, or during periods of prolonged immobilization.
Malignant Neoplasms
Endometrial Cancer: The use of unopposed estrogens in women with intact uteri has been associated with an increased risk of endometrial cancer. The reported endometrial cancer risk among unopposed estrogen users is about 2- to 12-fold greater than in non-users, and appears dependent on duration of treatment and on estrogen dose. Most studies show no significant increased risk associated with use of estrogens for less than one year. The greatest risk appears associated with prolonged use, with increased risks of 15- to 24-fold for 5 to 10 years or more and this risk has been shown to persist for at least 8 to 15 years after estrogen therapy is discontinued.
Clinical surveillance of all women taking estrogen/progestin combinations is important. Adequate diagnostic measures, including endometrial sampling when indicated, should be undertaken to rule out malignancy in all cases of undiagnosed persistent or recurring abnormal vaginal bleeding. There is no evidence that the use of natural estrogens results in a different endometrial risk profile than synthetic estrogens of equivalent estrogen dose. Adding a progestin to estrogen therapy has been shown to reduce the risk of endometrial hyperplasia, which may be a precursor to endometrial cancer.
Breast Cancer: The use of estrogens and progestins by postmenopausal women has been reported to increase the risk of breast cancer. The most important randomized clinical trial providing information about this issue is the Women's Health Initiative (WHI) substudy of CE/MPA. (See CLINICAL PHARMACOLOGY, Clinical Studies.) The results from observational studies are generally consistent with those of the WHI clinical trial and report no significant variation in the risk of breast cancer among different estrogens or progestins, doses, or routes of administration.
The CE/MPA substudy of WHI reported an increased risk of breast cancer in women who took CE/MPA for a mean follow-up of 5.6 years. Observational studies have also reported an increased risk for estrogen/progestin combination therapy, and a smaller increased risk for estrogen alone therapy, after several years of use. In the WHI trial and from observational studies, the excess risk increased with duration of use. From observational studies, the risk appeared to return to baseline in about five years after stopping treatment. In addition, observational studies suggest that the risk of breast cancer was greater, and became apparent earlier, with estrogen/progestin combination therapy as compared to estrogen alone therapy.
In the CE/MPA substudy, 26% of the women reported prior use of estrogen alone and/or estrogen/progestin combination hormone therapy. After a mean follow-up of 5.6 years during the clinical trial, the overall relative risk of invasive breast cancer was 1.24 (95% confidence interval 1.01-1.54), and the overall absolute risk was 41 versus 33 cases per 10,000 women-years, for CE/MPA compared with placebo. Among women who reported prior use of hormone therapy, the relative risk of invasive breast cancer was 1.86, and the absolute risk was 46 versus 25 cases per 10,000 women-years, for CE/MPA compared with placebo. Among women who reported no prior use of hormone therapy, the relative risk of invasive breast cancer was 1.09, and the absolute risk was 40 versus 36 cases per 10,000 women-years for CE/MPA compared with placebo. In the same substudy, invasive breast cancers were larger and diagnosed at a more advanced stage in the CE/MPA group compared with the placebo group. Metastatic disease was rare with no apparent difference between the two groups. Other prognostic factors such as histologic subtype, grade and hormone receptor status did not differ between the groups.
The use of estrogen plus progestin has been reported to result in an increase in abnormal mammograms requiring further evaluation. All women should receive yearly breast examinations by a healthcare provider and perform monthly breast self-examinations. In addition, mammography examinations should be scheduled based on patient age, risk factors, and prior mammogram results.
Dementia
In the Women's Health Initiative Memory Study (WHIMS), 4,532 generally healthy postmenopausal women 65 years of age and older were studied, of whom 35% were 70 to 74 years of age and 18% were 75 or older. After an average follow-up of 4 years, 40 women being treated with CE/MPA (1.8%, n = 2,229) and 21 women in the placebo group (0.9%, n = 2,303) received diagnoses of probable dementia. The relative risk for CE/MPA versus placebo was 2.05 (95% confidence interval 1.21 – 3.48), and was similar for women with and without histories of menopausal hormone use before WHIMS. The absolute risk of probable dementia for CE/MPA versus placebo was 45 versus 22 cases per 10,000 women-years, and the absolute excess risk for CE/MPA was 23 cases per 10,000 women-years. It is unknown whether these findings apply to younger postmenopausal women. (See CLINICAL PHARMACOLOGY, Clinical Studies and PRECAUTIONS, Geriatric Use.)
The estrogen alone substudy of the Women's Health Initiative Memory Study has concluded. It is unknown whether these findings apply to estrogen alone.
Gallbladder Disease
A 2- to 4-fold increase in the risk of gallbladder disease requiring surgery in postmenopausal women receiving estrogens has been reported.
Glucose Tolerance
A worsening of glucose tolerance has been observed in a significant percentage of patients on estrogen-containing oral contraceptives. For this reason, diabetic patients should be carefully observed while receiving estrogens.
Hypercalcemia
Estrogen administration may lead to severe hypercalcemia in patients with breast cancer and bone metastases. If hypercalcemia occurs, use of the drug should be stopped and appropriate measures taken to reduce the serum calcium level.
Visual Abnormalities
Retinal vascular thrombosis has been reported in patients receiving estrogens. Discontinue medication pending examination if there is sudden partial or complete loss of vision, or a sudden onset of proptosis, diplopia, or migraine. If examination reveals papilledema or retinal vascular lesions, estrogens should be permanently discontinued.
Warnings Associated with Methyltestosterone
In patients with breast cancer, androgen therapy may cause hypercalcemia by stimulating osteolysis. In this case the drug should be discontinued.
Prolonged use of high doses of androgens has been associated with the development of peliosis hepatis and hepatic neoplasms including hepatocellular carcinoma. [See PRECAUTIONS – Carcinogenesis (Androgens)] Peliosis hepatis can be a life-threatening or fatal complication.
Cholestatic hepatitis and jaundice occur with 17-alpha-alkylandrogens at a relatively low dose. If cholestatic hepatitis with jaundice appears or if liver function tests become abnormal, the androgen should be discontinued and the etiology should be determined. Drug-induced jaundice is reversible when the medication is discontinued.
Edema with or without heart failure may be a serious complication in patients with preexisting cardiac, renal, or hepatic disease. In addition to discontinuation of the drug, diuretic therapy may be required.
-
PRECAUTIONS
General Precautions Associated with Estrogens
Addition of a progestin when a woman has not had a hysterectomy: Studies of the addition of a progestin for 10 or more days of a cycle of estrogen administration, or daily with estrogen in a continuous regimen, have reported a lowered incidence of endometrial hyperplasia than would be induced by estrogen treatment alone. Endometrial hyperplasia may be a precursor to endometrial cancer.
There are, however, possible risks that may be associated with the use of progestins with estrogens compared to estrogen-alone regimens. These include a possible increased risk of breast cancer.
Elevated blood pressure: In a small number of case reports, substantial increases in blood pressure have been attributed to idiosyncratic reactions to estrogens. In a large, randomized, placebo-controlled clinical trial, a generalized effect of estrogens on blood pressure was not seen. Blood pressure should be monitored at regular intervals with estrogen use.
Hypertriglyceridemia: In patients with pre-existing hypertriglyceridemia, estrogen therapy may be associated with elevations of plasma triglycerides leading to pancreatitis and other complications.
Impaired liver function and past history of cholestatic jaundice: Estrogens may be poorly metabolized in patients with impaired liver function. For patients with a history of cholestatic jaundice associated with past estrogen use or with pregnancy, caution should be exercised and in the case of recurrence, medication should be discontinued.
Hypothyroidism: Estrogen administration leads to increased thyroid-binding globulin (TBG) levels. Patients with normal thyroid function can compensate for the increased TBG by making more thyroid hormone, thus maintaining free T4 and T3 serum concentrations in the normal range. Patients dependent on thyroid hormone replacement therapy who are also receiving estrogens may require increased doses of their thyroid replacement therapy. These patients should have their thyroid function monitored in order to maintain their free thyroid hormone levels in an acceptable range.
Fluid retention: Because estrogens may cause some degree of fluid retention, patients with conditions that might be influenced by this factor, such as a cardiac or renal dysfunction, warrant careful observation when estrogens are prescribed.
Hypocalcemia: Estrogens should be used with caution in individuals with severe hypocalcemia.
Ovarian cancer: The CE/MPA substudy of WHI reported that estrogen plus progestin increased the risk of ovarian cancer. After an average follow-up of 5.6 years, the relative risk for ovarian cancer for CE/MPA versus placebo was 1.58 (95% confidence interval 0.77 – 3.24) but was not statistically significant. The absolute risk for CE/MPA versus placebo was 4.2 versus 2.7 cases per 10,000 women-years. In some epidemiologic studies, the use of estrogen alone, in particular for 10 or more years, has been associated with an increased risk of ovarian cancer. Other epidemiologic studies have not found these associations.
Exacerbation of endometriosis: Endometriosis may be exacerbated with administration of estrogens. A few cases of malignant transformation of residual endometrial implants have been reported in women treated post-hysterectomy with estrogen alone therapy. For patients known to have residual endometriosis post-hysterectomy, the addition of progestin should be considered.
Exacerbation of other conditions: Estrogens may cause an exacerbation of asthma, diabetes mellitus, epilepsy, migraine or porphyria, systemic lupus erythematosus, and hepatic hemangiomas and should be used with caution in women with these conditions.
General Precautions Associated with Methyltestosterone
- 1. Women should be observed for signs of virilization (deepening of the voice, hirsutism, acne, clitoromegaly, and menstrual irregularities). Discontinuation of drug therapy at the time of evidence of mild virilism is necessary to prevent irreversible virilization. Such virilization is usual following androgen use at high doses.
- 2. Prolonged dosage of androgen may result in sodium and fluid retention. This may present a problem, especially in patients with compromised cardiac reserve or renal disease.
- 3. Hypersensitivity may occur rarely.
- 4. Protein-bound iodine (PBI) may be decreased in patients taking androgens.
- 5. Hypercalcemia may occur. If this does occur, the drug should be discontinued.
Patient Information (Estrogens)
Physicians are advised to discuss the PATIENT INFORMATION leaflet with patients for whom they prescribe Esterified Estrogens and Methyltestosterone Full and Half-Strength Tablets.
Patient Information (Androgens)
The physician should instruct patients to report any of the following side effects of androgens:
Women: Hoarseness, acne, changes in menstrual periods, or more hair on the face.
All Patients: Any nausea, vomiting, changes in skin color or ankle swelling.Laboratory Tests (Estrogens)
Estrogen administration should be initiated at the lowest dose approved for the indication and then guided by clinical response rather than by serum hormone levels (e.g., estradiol, FSH).
Laboratory Tests (Androgens)
- 1. Women with disseminated breast carcinoma should have frequent determination of urine and serum calcium levels during the course of androgen therapy. (See WARNINGS.)
- 2. Because of the hepatotoxicity associated with the use of 17-alpha-alkylated androgens, liver function tests should be obtained periodically.
- 3. Hemoglobin and hematocrit should be checked periodically for polycythemia in patients who are receiving high doses of androgens.
Drug/Laboratory Test Interactions (Estrogens)
- 1. Accelerated prothrombin time, partial thromboplastin time, and platelet aggregation time; increased platelet count; increased factors II, VII antigen, VIII antigen, VIII coagulant activity, IX, X, XII, VII-X complex, II-VII-X complex, and beta-thromboglobulin; decreased levels of antifactor Xa and antithrombin III, decreased antithrombin III activity; increased levels of fibrinogen and fibrinogen activity; increased plasminogen antigen and activity.
- 2. Increased thyroid-binding globulin (TBG) levels leading to increased circulating total thyroid hormone levels as measured by protein-bound iodine (PBI), T4 levels (by column or by radioimmunoassay) or T3 levels by radioimmunoassay. T3 resin uptake is decreased, reflecting the elevated TBG. Free T4 and free T3 concentrations are unaltered. Patients on thyroid replacement therapy may require higher doses of thyroid hormone.
- 3. Other binding proteins may be elevated in serum (i.e., corticosteroid binding globulin (CBG), sex hormone binding globulin (SHBG)) leading to increased total circulating corticosteroids and sex steroids, respectively. Free hormone concentrations may be decreased. Other plasma proteins may be increased (angiotensinogen/renin substrate, alpha-1-antitrypsin, ceruloplasmin).
- 4. Increased plasma HDL and HDL2 cholesterol subfraction concentrations, reduced LDL cholesterol concentration, increased triglycerides levels.
- 5. Impaired glucose tolerance.
- 6. Reduced response to metyrapone test.
Drug Interactions (Androgens)
Anticoagulants: C-17 substituted derivatives of testosterone, such as methandrostenolone, have been reported to decrease the anticoagulant requirements of patients receiving oral anticoagulants. Patients receiving oral anticoagulant therapy require close monitoring, especially when androgens are started or stopped.
Oxyphenbutazone: Concurrent administration of oxyphenbutazone and androgens may result in elevated serum levels of oxyphenbutazone.
Insulin: In diabetic patients, the metabolic effects of androgens may decrease blood glucose and insulin requirements.
Drug/Laboratory Test Interferences (Androgens)
Androgens may decrease levels of thyroxine-binding globulin, resulting in decreased T4 serum levels and increased resin uptake of T3 and T4. Free thyroid hormone levels remain unchanged, however, and there is no clinical evidence of thyroid dysfunction.
Carcinogenesis, Mutagenesis, Impairment of Fertility (Estrogens)
Long-term continuous administration of estrogen, with and without progestin, in women with and without a uterus, has shown an increased risk of endometrial cancer, breast cancer, and ovarian cancer. (See BOXED WARNINGS, WARNINGS and PRECAUTIONS.)
Long-term continuous administration of natural and synthetic estrogens in certain animal species increases the frequency of carcinomas of the breast, uterus, cervix, vagina, testis, and liver.
Carcinogenesis (Androgens)
Animal Data: Testosterone has been tested by subcutaneous injection and implantation in mice and rats. The implant induced cervical-uterine tumors in mice, which metastasized in some cases. There is suggestive evidence that injection of testosterone into some strains of female mice increases their susceptibility to hepatoma. Testosterone is also known to increase the number of tumors and decrease the degree of differentiation of chemically induced carcinomas of the liver in rats.
Human Data: There are rare reports of hepatocellular carcinoma in patients receiving long-term therapy with androgens in high doses. Withdrawal of the drugs did not lead to regression of the tumors in all cases.
Geriatric patients treated with androgens may be at increased risk for the development of prostatic hypertrophy and prostatic carcinoma.
Pregnancy (Estrogens)
Esterified Estrogens and Methyltestosterone Tablets and Esterified Estrogens and Methyltestosterone Half-Strength Tablets should not be used during pregnancy. (See CONTRAINDICATIONS.)
Nursing Mothers (Estrogens)
Estrogen administration to nursing mothers has been shown to decrease the quantity and quality of the milk. Detectable amounts of estrogens have been identified in the milk of mothers receiving this drug. Caution should be exercised when Esterified Estrogens and Methyltestosterone Tablets Full and Half-Strength Tablets are administered to a nursing woman.
Nursing Mothers (Androgens)
It is not known whether androgens are excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from androgens, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
Esterified Estrogens and Methyltestosterone Tablets Full and Half-StrengthTablets are not indicated for use in children.
Geriatric Use
Clinical studies of Esterified Estrogens and Methyltestosterone Full and Half-Strength Tablets did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
In the Women's Health Initiative Memory Study, including 4,532 women 65 years of age and older, followed for an average of 4 years, 82% (n = 3,729) were 65 to 74 while 18% (n = 803) were 75 and over. Most women (80%) had no prior hormone therapy use. Women treated with conjugated estrogens plus medroxyprogesterone acetate were reported to have a two-fold increase in the risk of developing probable dementia. Alzheimer's disease was the most common classification of probable dementia in both the conjugated estrogens plus medroxyprogesterone acetate group and the placebo group. Ninety percent of the cases of probable dementia occurred in the 54% of women that were older than 70. (See WARNINGS, Dementia.)
The estrogen alone substudy of the Women's Health Initiative Memory Study has concluded. It is unknown whether these findings apply to estrogen alone.
-
ADVERSE REACTIONS
See BOXED WARNINGS, WARNINGS and PRECAUTIONS.
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. The adverse reaction information from clinical trials does, however, provide a basis for identifying the adverse events that appear to be related to drug use and for approximating rates.
Associated with Estrogens
(See WARNINGS regarding induction of neoplasia, adverse effects on the fetus, increased incidence of gallbladder disease, and adverse effects similar to those of oral contraceptives, including thromboembolism). The following additional adverse reactions have been reported with estrogen and/or progestin therapy.
Genitourinary System: Changes in vaginal bleeding pattern and abnormal withdrawal bleeding or flow; breakthrough bleeding; spotting; dysmenorrhea, increase in size of uterine leiomyomata; vaginitis, including vaginal candidiasis; change in amount of cervical secretion; changes in cervical ectropion; ovarian cancer; endometrial hyperplasia; endometrial cancer; cystitis-like syndrome.
Breasts: Tenderness; enlargement; pain, nipple discharge, galactorrhea; fibrocystic breast changes; breast cancer.
Cardiovascular: Deep and superficial venous thrombosis; pulmonary embolism; thrombophlebitis; myocardial infarction; stroke; increase in blood pressure.
Gastrointestinal: Nausea; vomiting; abdominal cramps; bloating; cholestatic jaundice; increased incidence of gallbladder disease; pancreatitis, enlargement of hepatic hemangiomas.
Skin: Chloasma or melasma that may persist when drug is discontinued; erythema multiforme; erythema nodosum; hemorrhagic eruption; loss of scalp hair; hirsutism; pruritus, rash.
Eyes: Retinal vascular thrombosis, steepening of corneal curvature, intolerance to contact lenses.
Central Nervous System: Headache, migraine, dizziness; mental depression; chorea; nervousness; mood disturbances; irritability; exacerbation of epilepsy, dementia.
Miscellaneous: Increase or decrease in weight; reduced carbohydrate tolerance; aggravation of porphyria; edema; arthralgias; leg cramps; changes in libido; urticaria, angioedema, anaphylactoid/anaphylactic reactions; hypocalcemia; exacerbation of asthma; increased triglycerides.
Associated with Methyltestosterone
Endocrine and Urogenital
Female: The most common side effects of androgen therapy are amenorrhea and other menstrual irregularities, inhibition of gonadotropin secretion, and virilization, including deepening of the voice and clitoral enlargement. The latter usually is not reversible after androgens are discontinued. When administered to a pregnant woman, androgens cause virilization of external genitalia of the female fetus.
Skin and Appendages: Hirsutism, male pattern of baldness, and acne.
Fluid and Electrolyte Disturbances: Retention of sodium, chloride, water, potassium, calcium, and inorganic phosphates.
Gastrointestinal: Nausea, cholestatic jaundice, alterations in liver function test, rarely hepatocellular neoplasms, and peliosis hepatis. (See WARNINGS.)
Hematologic: Suppression of clotting factors II, V, VII, and X, bleeding in patients on concomitant anticoagulant therapy, and polycythemia.
Central Nervous System: Increased or decreased libido, headache, anxiety, depression, and generalized paresthesia.
Metabolic: Increased serum cholesterol.
Miscellaneous: Inflammation and pain at the site of intramuscular injection or subcutaneous implantation of testosterone containing pellets, stomatitis with buccal preparations, and rarely anaphylactoid reactions.
- DRUG ABUSE AND DEPENDENCE
-
OVERDOSAGE
Serious ill effects have not been reported following acute ingestion of large doses of estrogen-containing drug products by young children. Overdosage of estrogen may cause nausea and vomiting, and withdrawal bleeding may occur in females.
There have been no reports of acute overdosage with the androgens.
-
DOSAGE AND ADMINISTRATION
When estrogen is prescribed for a postmenopausal woman with a uterus, a progestin should also be initiated to reduce the risk of endometrial cancer. A woman without a uterus does not need progestin. Use of estrogen, alone or in combination with a progestin, should be with the lowest effective dose and for the shortest duration consistent with treatment goals and risks for the individual woman. Patients should be reevaluated periodically as clinically appropriate (e.g., 3-month to 6-month intervals) to determine if treatment is still necessary. (See BOXED WARNINGS and WARNINGS.) For women who have a uterus, adequate diagnostic measures, such as endometrial sampling, when indicated, should be undertaken to rule out malignancy in cases of undiagnosed persistent or recurring abnormal vaginal bleeding.
Given cyclically for short-term use only:
For treatment of moderate to severe vasomotor symptoms associated with the menopause in patients not improved by estrogen alone.
The lowest dose that will control symptoms should be chosen and medication should be discontinued as promptly as possible.
Administration should be cyclic (e.g., three weeks on and one week off).
Attempts to discontinue or taper medication should be made at three- to six-month intervals.
Usual Dosage Range:
1 tablet of Esterified Estrogens and Methyltestosterone or 1 to 2 tablets of Esterified Estrogens and Methyltestosterone Half-Strength daily as recommended by the physician.
Treated patients with an intact uterus should be monitored closely for signs of endometrial cancer and appropriate diagnostic measures should be taken to rule out malignancy in the event of persistent or recurring abnormal vaginal bleeding.
-
HOW SUPPLIED
Esterified Estrogens and Methyltestosterone Tablets (Imprinted “1490”)
Bottles of 100 ……………………………………………………..NDC: 62559-149-01
Esterified Estrogens and Methyltestosterone Tablets (dark green, capsule shaped, sugar-coated oral tablets) contain: 1.25 mg of Esterified Estrogens, USP and 2.5 mg of Methyltestosterone, USP.
Esterified Estrogens and Methyltestosterone Half-Strength Tablets (Imprinted “1507”)
Bottles of 100 ……………………………………………………..NDC: 62559-150-01
Esterified Estrogens and Methyltestosterone Half-Strength Tablets (light green, capsule shaped, sugar-coated oral tablets) contain: 0.625 mg of Esterified Estrogens, USP and 1.25 mg of Methyltestosterone, USP.
Keep Esterified Estrogens and Methyltestosterone Tablets and Esterified Estrogens and Methyltestosterone Half-Strength Tablets out of reach of children.
Store at 20° - 25°C (68° - 77°F); excursions permitted to 15° - 30°C (59° - 86°F). [See USP Controlled Room Temperature]
† This product has not obtained FDA pre-market approval applicable for new drugs.
-
PATIENT INFORMATION
WHAT YOU SHOULD KNOW ABOUT ESTROGENS
Esterified Estrogens and Methyltestosterone Tablets, 1.25 mg/2.5 mg † and Esterified Estrogens and Methyltestosterone Tablets, 0.625 mg/1.25 mg (Half-Strength) †CIII
Rx Only
Read this PATIENT INFORMATION before you start taking Esterified Estrogens and Methyltestosterone Full and Half-Strength Tablets and read what you get each time you refill Esterified Estrogens and Methyltestosterone Full and Half-Strength Tablets. There may be new information. This information does not take the place of talking to your healthcare provider about your medical condition or your treatment.
WHAT IS THE MOST IMPORTANT INFORMATION I SHOULD KNOW ABOUT ESTERIFIED ESTROGENS AND METHYLTESTOSTERONE TABLETS AND ESTERIFIED ESTROGENS AND METHYLTESTOSTERONE HALF-STRENGTH TABLETS (A COMBINATION OF ESTROGEN AND ANDROGEN HORMONES)?
-
Estrogens increase the chances of getting cancer of the uterus.
Report any unusual vaginal bleeding right away while you are taking estrogens. Vaginal bleeding after menopause may be a warning sign of cancer of the uterus (womb). Your healthcare provider should check any unusual vaginal bleeding to find out the cause. -
Do not use estrogens with or without progestins to prevent heart disease, heart attacks, or strokes.
Using estrogens with or without progestins may increase your chances of getting heart attacks, strokes, breast cancer, and blood clots. Using estrogens with progestins may increase your risk of dementia. You and your healthcare provider should talk regularly about whether you still need treatment with Esterified Estrogens and Methyltestosterone Full and Half-Strength Tablets.
What are Esterified Estrogens and Methyltestosterone Tablets and Esterified Estrogens and Methyltestosterone Half-Strength Tablets?
Esterified Estrogens and Methyltestosterone Full and Half-Strength Tablets are medicines that contain estrogen and androgen hormones.
What are Esterified Estrogens and Methyltestosterone Tablets and Esterified Estrogens and Methyltestosterone Half-Strength Tablets used for?
Esterified Estrogens and Methyltestosterone Full and Half-Strength Tablets are used after menopause to:
-
reduce moderate to severe hot flashes. Estrogens are hormones made by a woman's ovaries. The ovaries normally stop making estrogens when a woman is between 45 to 55 years old. This drop in body estrogen levels causes the "change of life" or menopause (the end of monthly menstrual periods). Sometimes, both ovaries are removed during an operation before natural menopause takes place. The sudden drop in estrogen levels causes "surgical menopause."
When the estrogen levels begin dropping, some women develop very uncomfortable symptoms, such as feelings of warmth in the face, neck, and chest, or sudden strong feelings of heat and sweating ("hot flashes" or "hot flushes"). In some women, the symptoms are mild, and they will not need estrogens. In other women, symptoms can be more severe. You and your healthcare provider should talk regularly about whether you still need treatment with Esterified Estrogens and Methyltestosterone Full and Half-Strength Tablets - treat moderate to severe dryness, itching, and burning in and around the vagina. You and your healthcare provider should talk regularly about whether you still need treatment with Esterified Estrogens and Methyltestosterone Full and Half-Strength Tablets to control these problems. If you use Esterified Estrogens and Methyltestosterone Full and Half-Strength Tablets only to treat your dryness, itching, and burning in and around your vagina, talk with your healthcare provider about whether a topical vaginal product would be better for you.
Who should not take Esterified Estrogens and Methyltestosterone Tablets and Esterified Estrogens and Methyltestosterone Half-Strength Tablets?
Do not start taking Esterified Estrogens and Methyltestosterone Full and Half-Strength Tablets if you:
- have unusual vaginal bleeding.
- currently have or have had certain cancers. Estrogens may increase the chances of getting certain types of cancers, including cancer of the breast or uterus. If you have or had cancer, talk with your healthcare provider about whether you should take Esterified Estrogens and Methyltestosterone Full and Half-Strength Tablets.
- had a stroke or heart attack in the past year.
- currently have or have had blood clots.
- currently have or have had liver problems.
- are allergic to Esterified Estrogens and Methyltestosterone Tablets and Esterified Estrogens and Methyltestosterone Half-Strength Tablets or any of their ingredients. See the end of this leaflet for a list of ingredients in Esterified Estrogens and Methyltestosterone Full and Half-Strength Tablets.
- think you may be pregnant.
Tell your healthcare provider:
- if you are breastfeeding. The hormones in Esterified Estrogens and Methyltestosterone Full and Half-Strength Tablets can pass into your milk.
- about all of your medical problems. Your healthcare provider may need to check you more carefully if you have certain conditions, such as asthma (wheezing), epilepsy (seizures), migraine, endometriosis, lupus, problems with your heart, liver, thyroid, kidneys, or have high calcium levels in your blood.
- about all the medicines you take. This includes prescription and nonprescription medicines, vitamins, and herbal supplements. Some medicines may affect how Esterified Estrogens and Methyltestosterone Full and Half-Strength Tablets work. Esterified Estrogens and Methyltestosterone Full and Half-Strength Tablets may also affect how your other medicines work.
- if you are going to have surgery or will be on bed rest. You may need to stop taking estrogens.
How should I take Esterified Estrogens and Methyltestosterone Tablets and Esterified Estrogens and Methyltestosterone Half-Strength Tablets?
Estrogens should be used at the lowest dose possible for your treatment only as long as needed. The lowest effective dose of Esterified Estrogens and Methyltestosterone Full and Half-Strength Tablets has not been determined. You and your healthcare provider should talk regularly (for example, every 3 to 6 months) about the dose you are taking and whether you still need treatment with Esterified Estrogens and Methyltestosterone Full and Half-Strength Tablets
What are the possible side effects of estrogens?
Less common but serious side effects include:
- Breast cancer
- Cancer of the uterus
- Stroke
- Heart attack
- Blood clots
- Dementia
- Gallbladder disease
- Ovarian cancer
These are some of the warning signs of serious side effects:
- Breast lumps
- Unusual vaginal bleeding
- Dizziness and faintness
- Changes in speech
- Severe headaches
- Chest pain
- Shortness of breath
- Pains in your legs
- Changes in vision
- Vomiting
Call your healthcare provider right away if you get any of these warning signs, or any other unusual symptom that concerns you.
Common side effects include:
- Headache
- Breast pain
- Irregular vaginal bleeding or spotting
- Stomach/abdominal cramps, bloating
- Nausea and vomiting
- Hair loss
Other side effects include:
- High blood pressure
- Liver problems
- High blood sugar
- Fluid retention
- Enlargement of benign tumors of the uterus ("fibroids")
- Vaginal yeast infection
These are not all the possible side effects of Esterified Estrogens and Methyltestosterone Full and Half-Strength Tablets. For more information, ask your healthcare provider or pharmacist.
What can I do to lower my chance of a serious side effect with Esterified Estrogens and Methyltestosterone Tablets and Esterified Estrogens and Methyltestosterone Half-Strength Tablets?
- Talk with your healthcare provider regularly about whether you should continue taking Esterified Estrogens and Methyltestosterone Full and Half-Strength Tablets.
- If you have a uterus, talk to your healthcare provider about whether the addition of a progestin is right for you.
- See your healthcare provider right away if you get vaginal bleeding while taking Esterified Estrogens and Methyltestosterone Full and Half-Strength Tablets.
- Have a breast exam and mammogram (breast X-ray) every year unless your healthcare provider tells you something else. If members of your family have had breast cancer or if you have ever had breast lumps or an abnormal mammogram, you may need to have breast exams more often.
- If you have high blood pressure, high cholesterol (fat in the blood), diabetes, are overweight, or if you use tobacco, you may have higher chances for getting heart disease. Ask your healthcare provider for ways to lower your chances for getting heart disease.
General information about safe and effective use of Esterified Estrogens and Methyltestosterone Tablets and Esterified Estrogens and Methyltestosterone Half-Strength Tablets
Medicines are sometimes prescribed for conditions that are not mentioned in patient information leaflets. Do not take Esterified Estrogens and Methyltestosterone Full and Half-Strength Tablets for conditions for which it was not prescribed. Do not give Esterified Estrogens and Methyltestosterone Full and Half-Strength Tablets to other people, even if they have the same symptoms you have. It may harm them.
Keep Esterified Estrogens and Methyltestosterone Tablets and Esterified Estrogens and Methyltestosterone Half-Strength Tablets out of the reach of children.
This leaflet provides a summary of the most important information about Esterified Estrogens and Methyltestosterone Full and Half-Strength Tablets. If you would like more information, talk with your healthcare provider or pharmacist. You can ask for information about Esterified Estrogens and Methyltestosterone Full and Half-Strength Tablets that is written for health professionals. You can get more information by calling the toll free number 1-800-308-6755.
What are the ingredients in Esterified Estrogens and Methyltestosterone Tablets and Esterified Estrogens and Methyltestosterone Half-Strength Tablets?
Esterified Estrogens and Methyltestosterone Half-Strength Tablets is a combination of Esterified Estrogens and Methyltestosterone. Each light green, capsule shaped, sugar-coated tablet imprinted with “1507" contains the following active ingredients: 0.625 mg of Esterified Estrogens, USP and 1.25 mg of Methyltestosterone, USP.
Esterified Estrogens and Methyltestosterone Tablets is a combination of Esterified Estrogens and Methyltestosterone. Each dark green, capsule shaped, sugar-coated tablet imprinted with “1490” contains the following active ingredients: 1.25 mg of Esterified Estrogens, USP and 2.5 mg of Methyltestosterone, USP.
Esterified Estrogens and Methyltestosterone Full and Half-Strength Tablets contain the following inactive ingredients: acacia, calcium carbonate, carnauba wax, citric acid, colloidal silicon dioxide, di-acetylated monoglycerides, gelatin, lactose, magnesium stearate, methylparaben, microcrystalline cellulose, pharmaceutical glaze, povidone, propylene glycol, propylparaben, shellac glaze, sodium benzoate, sodium bicarbonate, sorbic acid, starch, sucrose, talc, titanium dioxide, tromethamol, FD&C Blue No. 1 Aluminum Lake, and D&C Yellow No. 10 Aluminum Lake.
Esterified Estrogens and Methyltestosterone Tablets also contain: FD&C Yellow No. 6 Aluminum Lake.
Esterified Estrogens and Methyltestosterone Half-Strength Tablets also contain: FD&C Blue No. 2 Aluminum Lake and Iron Oxide Black.
Store at 20° - 25°C (68° - 77°F); excursions permitted to 15° - 30°C (59° - 86°F). [See USP Controlled Room Temperature]
†This product has not obtained FDA pre-market approval applicable for new drugs.
DEA Order Form Required
Manufactured by:
ANI Pharmaceuticals, Inc.
Baudette, MN 566239574 Rev 02/13
-
Estrogens increase the chances of getting cancer of the uterus.
-
PRINCIPAL DISPLAY PANEL - 1.25 mg/2.5 mg
Esterified Estrogens and Methyltestosterone Tablets, CIII
1.25 mg/2.5 mg
NDC: 62559-149-01
Rx Only
100 Tablets
-
PRINCIPAL DISPLAY PANEL - 0.625 mg/1.25 mg
Esterified Estrogens and Methyltestosterone Tablets, CIII
0.625 mg/1.25 mg, Half-Strength
NDC: 62559-150-01
Rx Only
100 Tablets
-
INGREDIENTS AND APPEARANCE
ESTERIFIED ESTROGENS AND METHYLTESTOSTERONE
esterified estrogens and methyltestosterone tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 62559-149 Route of Administration ORAL DEA Schedule CIII Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ESTROGENS, ESTERIFIED (UNII: 3ASP8Q3768) (ESTROGENS, ESTERIFIED - UNII:3ASP8Q3768) ESTROGENS, ESTERIFIED 1.25 mg METHYLTESTOSTERONE (UNII: V9EFU16ZIF) (METHYLTESTOSTERONE - UNII:V9EFU16ZIF) METHYLTESTOSTERONE 2.5 mg Inactive Ingredients Ingredient Name Strength ACACIA (UNII: 5C5403N26O) CALCIUM CARBONATE (UNII: H0G9379FGK) CARNAUBA WAX (UNII: R12CBM0EIZ) ANHYDROUS CITRIC ACID (UNII: XF417D3PSL) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) DIACETYLATED MONOGLYCERIDES (UNII: 5Z17386USF) GELATIN, UNSPECIFIED (UNII: 2G86QN327L) ANHYDROUS LACTOSE (UNII: 3SY5LH9PMK) MAGNESIUM STEARATE (UNII: 70097M6I30) METHYLPARABEN (UNII: A2I8C7HI9T) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) POVIDONE, UNSPECIFIED (UNII: FZ989GH94E) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) PROPYLPARABEN (UNII: Z8IX2SC1OH) SHELLAC (UNII: 46N107B71O) SODIUM BENZOATE (UNII: OJ245FE5EU) SODIUM BICARBONATE (UNII: 8MDF5V39QO) SORBIC ACID (UNII: X045WJ989B) STARCH, CORN (UNII: O8232NY3SJ) SUCROSE (UNII: C151H8M554) TALC (UNII: 7SEV7J4R1U) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) TROMETHAMINE (UNII: 023C2WHX2V) FD&C BLUE NO. 1 (UNII: H3R47K3TBD) D&C YELLOW NO. 10 (UNII: 35SW5USQ3G) FD&C YELLOW NO. 6 (UNII: H77VEI93A8) Product Characteristics Color GREEN (dark green) Score no score Shape CAPSULE Size 14mm Flavor Imprint Code 1490 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 62559-149-01 100 in 1 BOTTLE; Type 0: Not a Combination Product 12/22/2010 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date Unapproved drug other 12/22/2010 ESTERIFIED ESTROGENS AND METHYLTESTOSTERONE
esterified estrogens and methyltestosterone tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 62559-150 Route of Administration ORAL DEA Schedule CIII Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ESTROGENS, ESTERIFIED (UNII: 3ASP8Q3768) (ESTROGENS, ESTERIFIED - UNII:3ASP8Q3768) ESTROGENS, ESTERIFIED 0.625 mg METHYLTESTOSTERONE (UNII: V9EFU16ZIF) (METHYLTESTOSTERONE - UNII:V9EFU16ZIF) METHYLTESTOSTERONE 1.25 mg Inactive Ingredients Ingredient Name Strength ACACIA (UNII: 5C5403N26O) CALCIUM CARBONATE (UNII: H0G9379FGK) CARNAUBA WAX (UNII: R12CBM0EIZ) ANHYDROUS CITRIC ACID (UNII: XF417D3PSL) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) DIACETYLATED MONOGLYCERIDES (UNII: 5Z17386USF) GELATIN, UNSPECIFIED (UNII: 2G86QN327L) ANHYDROUS LACTOSE (UNII: 3SY5LH9PMK) MAGNESIUM STEARATE (UNII: 70097M6I30) METHYLPARABEN (UNII: A2I8C7HI9T) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) POVIDONE, UNSPECIFIED (UNII: FZ989GH94E) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) PROPYLPARABEN (UNII: Z8IX2SC1OH) SHELLAC (UNII: 46N107B71O) SODIUM BENZOATE (UNII: OJ245FE5EU) SODIUM BICARBONATE (UNII: 8MDF5V39QO) SORBIC ACID (UNII: X045WJ989B) STARCH, CORN (UNII: O8232NY3SJ) SUCROSE (UNII: C151H8M554) TALC (UNII: 7SEV7J4R1U) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) TROMETHAMINE (UNII: 023C2WHX2V) FD&C BLUE NO. 1 (UNII: H3R47K3TBD) D&C YELLOW NO. 10 (UNII: 35SW5USQ3G) FD&C BLUE NO. 2 (UNII: L06K8R7DQK) FERROSOFERRIC OXIDE (UNII: XM0M87F357) Product Characteristics Color GREEN (light green) Score no score Shape CAPSULE Size 13mm Flavor Imprint Code 1507 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 62559-150-01 100 in 1 BOTTLE; Type 0: Not a Combination Product 12/22/2010 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date Unapproved drug other 12/22/2010 Labeler - ANI Pharmaceuticals, Inc. (145588013) Registrant - ANI Pharmaceuticals, Inc. (145588013)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.