PREVNAR 20- pneumococcal 20-valent conjugate vaccine injection, suspension
Prevnar 20 by
Drug Labeling and Warnings
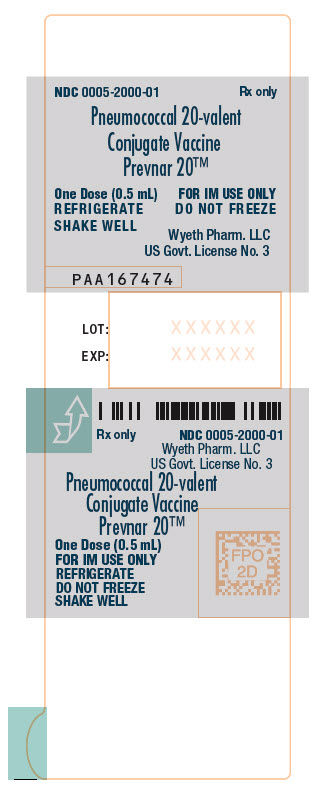
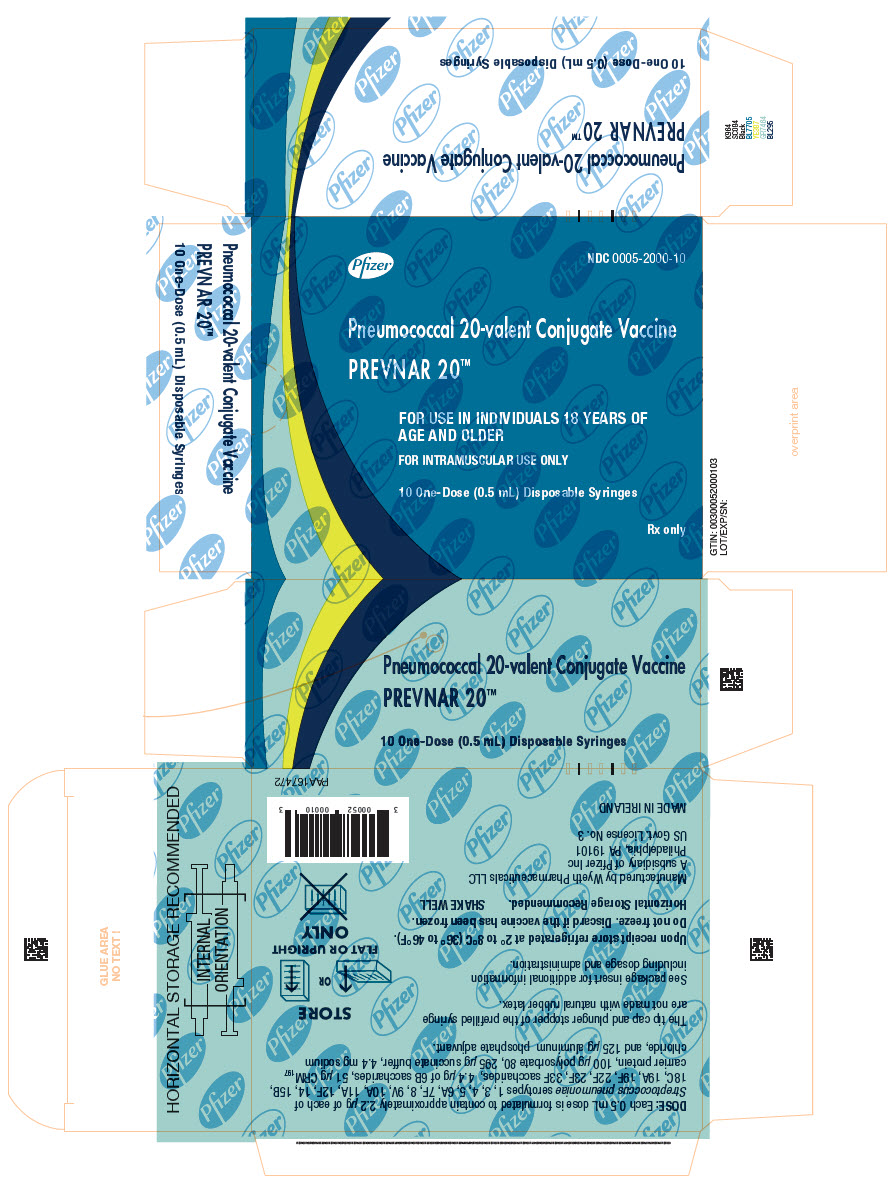
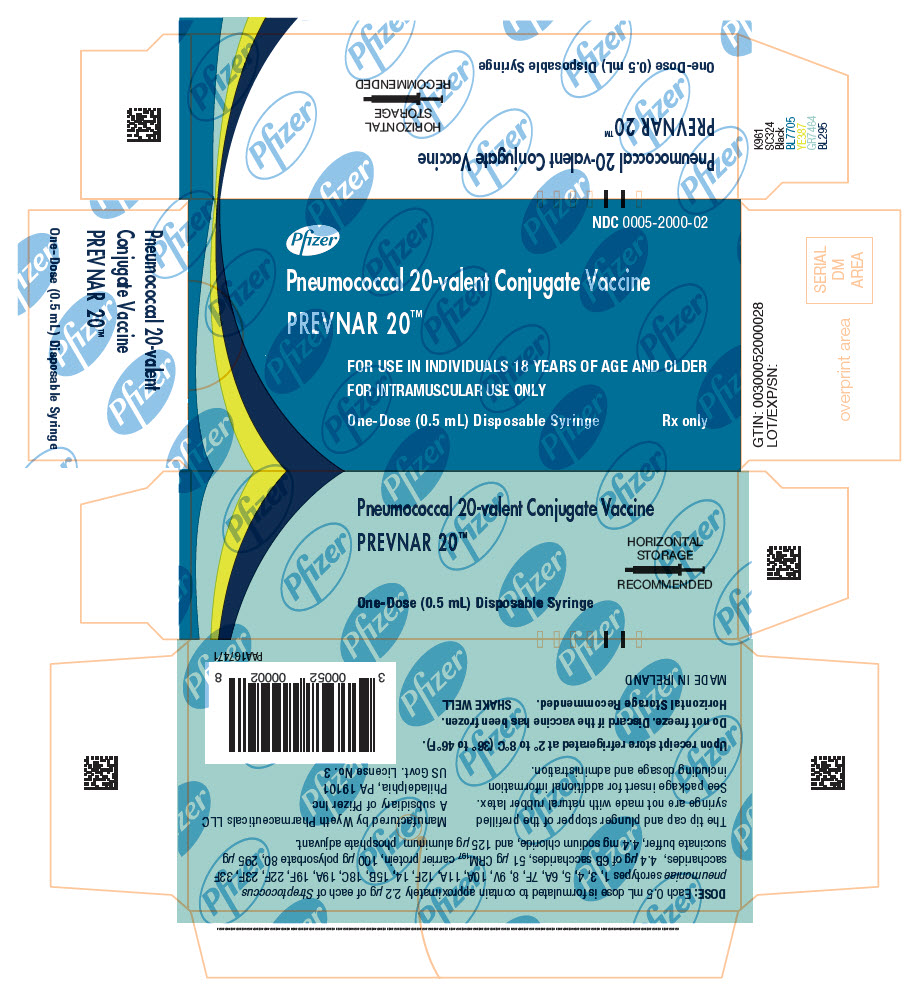
Prevnar 20 by is a Other medication manufactured, distributed, or labeled by Wyeth Pharmaceutical Division of Wyeth Holdings LLC, Pfizer Ireland Pharmaceuticals, Wyeth BioPharma Division of Wyeth Pharmaceuticals LLC, Pfizer Manufacturing Belgium NV, Pfizer Inc. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use PREVNAR 20 safely and effectively. See full prescribing information for PREVNAR 20.
PREVNAR 20® (Pneumococcal 20-valent Conjugate Vaccine), suspension for intramuscular injection
Initial U.S. Approval: 2021RECENT MAJOR CHANGES
INDICATIONS AND USAGE
Prevnar 20 is a vaccine indicated for
- active immunization for the prevention of invasive disease caused by Streptococcus pneumoniae serotypes 1, 3, 4, 5, 6A, 6B, 7F, 8, 9V, 10A, 11A, 12F, 14, 15B, 18C, 19A, 19F, 22F, 23F, and 33F in individuals 6 weeks of age and older. (1)
- active immunization for the prevention of otitis media caused by S. pneumoniae serotypes 4, 6B, 9V, 14, 18C, 19F, and 23F in individuals 6 weeks through 5 years of age. (1)
- active immunization for the prevention of pneumonia caused by S. pneumoniae serotypes 1, 3, 4, 5, 6A, 6B, 7F, 8, 9V, 10A, 11A, 12F, 14, 15B, 18C, 19A, 19F, 22F, 23F, and 33F in individuals 18 years of age and older. (1)
The indication for the prevention of pneumonia caused by S. pneumoniae serotypes 8, 10A, 11A, 12F, 15B, 22F, and 33F in individuals 18 years of age and older is approved under accelerated approval based on immune responses as measured by opsonophagocytic activity (OPA) assay. Continued approval for this indication may be contingent upon verification and description of clinical benefit in a confirmatory trial. (1)
DOSAGE AND ADMINISTRATION
DOSAGE FORMS AND STRENGTHS
0.5 mL suspension for intramuscular injection, supplied in a single-dose pre-filled syringe. (3)
CONTRAINDICATIONS
Severe allergic reaction (e.g., anaphylaxis) to any component of Prevnar 20 or to diphtheria toxoid. (4)
WARNINGS AND PRECAUTIONS
Apnea following intramuscular vaccination has been observed in some infants born prematurely. Decisions about when to administer Prevnar 20 to infants born prematurely should be based on consideration of the individual infant’s medical status, and the potential benefits and possible risks of vaccination. (5.3)
ADVERSE REACTIONS
- In individuals 2, 4, 6, and 12 through 15 months of age vaccinated with a 4‑dose schedule, the most commonly reported solicited adverse reactions >10% were irritability (>60%), pain at the injection site (>30%), drowsiness (>30%), decreased appetite and injection site redness (>20%), injection site swelling (>10%), and fever (>10%). (6.1)
- In individuals 15 months through 17 years of age vaccinated with a single dose, the most commonly reported solicited adverse reactions >10% were irritability (>60% in individuals less than 2 years of age), pain at the injection site (>50%), drowsiness (>40% in individuals less than 2 years of age), fatigue and muscle pain (>20% in individuals 2 years of age and older), decreased appetite (>20% in individuals less than 2 years of age), injection site swelling and injection site redness (>10%) and headache (>10% in individuals 5 years of age and older), and fever (>10% in individuals less than 2 years of age). (6.1)
- In individuals 18 through 59 years of age, the most commonly reported solicited adverse reactions >10% were pain at the injection site (>70%), muscle pain (>50%), fatigue (>40%), headache (>30%), and arthralgia and injection site swelling (>10%). (6.1)
- In individuals 60 years of age and older, the most commonly reported solicited adverse reactions >10% were pain at the injection site (>50%), muscle pain and fatigue (>30%), headache (>20%), and arthralgia (>10%). (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Pfizer Inc. at 1-800-438-1985 or VAERS at 1-800-822-7967 or http://vaers.hhs.gov.
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 4/2023
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Preparation
2.2 Administration
2.3 Vaccination Schedule for Individuals 6 Weeks Through 15 Months of Age
2.4 Catch-Up Vaccination Schedule for Unvaccinated Individuals 7 Months Through 17 Years of Age
2.5 Catch-Up Vaccination Schedule for Individuals Previously Vaccinated With One or More Doses of a Lower Valency Pneumococcal Conjugate Vaccine
2.6 Vaccination Schedule for Individuals 18 Years of Age and Older
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Management of Acute Allergic Reactions
5.2 Altered Immunocompetence
5.3 Apnea in Premature Infants
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience With Prevnar 13
7 DRUG INTERACTIONS
7.1 Prior Vaccination With PNEUMOVAX 23
7.2 Immunosuppressive Therapies
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Prevnar and Prevnar 13 Efficacy Data
14.2 Prevnar 20 Clinical Trials in Individuals 6 Weeks Through 15 Months of Age
14.3 Prevnar 20 Clinical Trials in Individuals 18 Years of Age and Older
14.4 Concomitant Vaccine Administration
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
Prevnar 20® is a vaccine indicated for
- active immunization for the prevention of invasive disease caused by Streptococcus pneumoniae serotypes 1, 3, 4, 5, 6A, 6B, 7F, 8, 9V, 10A, 11A, 12F, 14, 15B, 18C, 19A, 19F, 22F, 23F, and 33F in individuals 6 weeks of age and older.
- active immunization for the prevention of otitis media caused by S. pneumoniae serotypes 4, 6B, 9V, 14, 18C, 19F, and 23F in individuals 6 weeks through 5 years of age.
- active immunization for the prevention of pneumonia caused by S. pneumoniae serotypes 1, 3, 4, 5, 6A, 6B, 7F, 8, 9V, 10A, 11A, 12F, 14, 15B, 18C, 19A, 19F, 22F, 23F, and 33F in individuals 18 years of age and older.
The indication for the prevention of pneumonia caused by S. pneumoniae serotypes 8, 10A, 11A, 12F, 15B, 22F, and 33F in individuals 18 years of age and older is approved under accelerated approval based on immune responses as measured by opsonophagocytic activity (OPA) assay [see Clinical Studies (14.2)]. Continued approval for this indication may be contingent upon verification and description of clinical benefit in a confirmatory trial.
-
2 DOSAGE AND ADMINISTRATION
For intramuscular administration only.
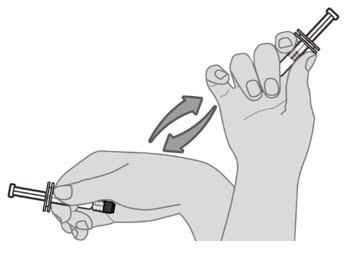
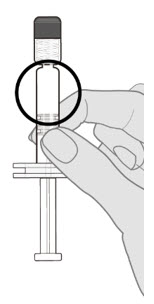
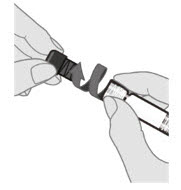
2.1 Preparation
Do not mix Prevnar 20 with other vaccines/products in the same syringe.
2.2 Administration
For intramuscular injection only.
Each 0.5-mL dose is to be injected intramuscularly using a sterile needle attached to the supplied pre-filled syringe.
2.3 Vaccination Schedule for Individuals 6 Weeks Through 15 Months of Age
Administer Prevnar 20 as a 4-dose series at 2, 4, 6, and 12 through 15 months of age (and at least 2 months after the third dose). The first dose may be given as early as 6 weeks of age.
2.4 Catch-Up Vaccination Schedule for Unvaccinated Individuals 7 Months Through 17 Years of Age
Individuals 7 months through 17 years of age who have never received a pneumococcal conjugate vaccine may receive Prevnar 20 according to the schedule in Table 1:
Table 1. Catch-Up Vaccination Schedule for Individuals Initiating Vaccination at 7 Months Through 17 Years of Age* - * The vaccination schedule is based on the catch-up schedule for Prevnar 13 (Pneumococcal 13-valent Conjugate Vaccine [Diphtheria CRM197 Protein]).
- † The first 2 doses at least 4 weeks apart; third dose after the one-year birthday, separated from the second dose by at least 2 months.
- ‡ Two doses at least 2 months apart.
Age at First Dose
Total Number of 0.5-mL Doses
7 through 11 months of age
3†
12 through 23 months of age
2‡
24 months of age and above
1
2.5 Catch-Up Vaccination Schedule for Individuals Previously Vaccinated With One or More Doses of a Lower Valency Pneumococcal Conjugate Vaccine
Administer a single dose of Prevnar 20 to individuals 15 months through 17 years of age previously vaccinated with one or more doses of a lower valency pneumococcal conjugate vaccine. The dose of Prevnar 20 should be administered at least 8 weeks after the last dose of the lower valency pneumococcal conjugate vaccine.
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
Do not administer Prevnar 20 to individuals with a severe allergic reaction (e.g., anaphylaxis) to any component of Prevnar 20 or to diphtheria toxoid [see Description (11)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Management of Acute Allergic Reactions
Appropriate medical treatment and supervision used to manage immediate allergic reactions must be immediately available should an acute anaphylactic reaction occur following administration of Prevnar 20.
5.2 Altered Immunocompetence
Safety and immunogenicity data on Prevnar 20 are not available for individuals in immunocompromised groups and vaccination should be considered on an individual basis.
Based on experience with pneumococcal vaccines, individuals with altered immunocompetence may have reduced immune responses to Prevnar 20.
5.3 Apnea in Premature Infants
Apnea following intramuscular vaccination has been observed in some infants born prematurely. Decisions about when to administer Prevnar 20 to infants born prematurely should be based on consideration of the individual infant’s medical status and the potential benefits and possible risks of vaccination.
-
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a vaccine cannot be directly compared to rates in the clinical trials of another vaccine and may not reflect the rates observed in practice.
In individuals 2, 4, 6, and 12 through 15 months of age vaccinated with a 4-dose schedule, the most commonly reported solicited adverse reactions >10% were irritability (>60%), pain at the injection site (>30%), drowsiness (>30%), decreased appetite and injection site redness (>20%), injection site swelling (>10%), and fever (>10%).
In individuals 15 months through 17 years of age vaccinated with a single dose, the most commonly reported solicited adverse reactions >10% were irritability (>60% in individuals less than 2 years of age), pain at the injection site (>50%), drowsiness (>40% in individuals less than 2 years of age), fatigue and muscle pain (>20% in individuals 2 years of age and older), decreased appetite (>20% in individuals less than 2 years of age), injection site swelling and injection site redness (>10%), headache (>10% in individuals 5 years of age and older), and fever (>10% in individuals less than 2 years of age).
In individuals 18 through 59 years of age, the most commonly reported solicited adverse reactions >10% were pain at the injection site (>70%), muscle pain (>50%), fatigue (>40%), headache (>30%), and arthralgia and injection site swelling (>10%).
In individuals 60 years of age and older, the most commonly reported solicited adverse reactions >10% were pain at the injection site (>50%), muscle pain and fatigue (>30%), headache (>20%), and arthralgia (>10%).
Clinical Trial Experience in Individuals 6 Weeks Through 17 Years of Age
The safety of Prevnar 20 in individuals from 6 weeks through 17 years of age was evaluated in 3 randomized, double-blind, active-controlled, clinical trials and one single-arm clinical trial. Across the 4 pediatric trials (Studies 8, 9, 10, and 11; NCT04382326, NCT04379713, NCT03512288, and NCT04642079, respectively) conducted in the Americas and Europe, 3063 participants received at least one dose of Prevnar 20, and 1720 participants received at least one dose of Prevnar 13.
Safety Assessment in Individuals Receiving a 4-Dose Series (Studies 8 through 10)
The safety of Prevnar 20 was assessed in 3 randomized, double-blind, active-controlled, clinical trials in participants (Studies 8, 9, and 10). Globally, 2232 participants who received at least one dose of a 4-dose series of Prevnar 20 and 1717 participants who received at least one dose of a 4-dose series of Prevnar 13 were included in the safety analysis. In the United States (US) (including the US territory of Puerto Rico [PR]), 1567 participants received at least one dose of a 4-dose series of Prevnar 20 and 1376 participants received at least one dose of a 4-dose series of Prevnar 13. Study 8 was a double-blind, active-controlled trial of safety and immunogenicity in participants randomized 1:1 to receive a 4-dose series of either Prevnar 20 (N=1001) or Prevnar 13 (N=990) at 2, 4, 6, and 12 through 15 months of age, conducted in the US and PR. Study 9 was a double-blind trial of tolerability and safety in participants randomized 2:1 to receive a 4-dose series of either Prevnar 20 (N=1000) or Prevnar 13 (N=503) at 2, 4, 6, and 12 through 15 months of age, conducted in countries in Europe, South America, and North America, including the US and PR. Study 10 was a double-blind, active-controlled multicenter trial of safety and immunogenicity in participants randomized 1:1 to receive a 4-dose series of either Prevnar 20 (N=231) or Prevnar 13 (N=227) at 2, 4, 6, and 12 months of age, conducted in the US.
Across the 3 infant trials, there were similar percentages of male (51.7% and 50.1%) and female (48.3% and 49.9%) participants among the Prevnar 20 and Prevnar 13 recipients respectively. Participant age at the first dose (median age: 64.0 days, range: 42 to 98 days; median age: 64.0 days, range 43 to 97 days) and last dose (median age: 372.0 days, range 365 to 460 days; median age: 372.0 days, range 366 to 455 days) in the Prevnar 20 and Prevnar 13 groups, respectively, was similar. The racial and ethnic distribution of the US/PR infant safety population was as follows: 73.8% of Prevnar 20 recipients were White, 12.1% Black, 1.9% Asian, and 7.5% multi-racial; 29.7% were Hispanic) with similar distribution among Prevnar 13 recipients. In the multi-country infant trial, Study 9, the participants were predominantly White (87.4%). This study also included 111 late preterm infants (>34 to <37 weeks gestational age) among the total study population 77 were in the Prevnar 20 group, and 34 in the Prevnar 13 group.
In Study 8, Pediarix [Diphtheria and Tetanus Toxoids and Acellular Pertussis Adsorbed, Hepatitis B (Recombinant) and Inactivated Poliovirus Vaccine Combined] (DTaP-HBV-IPV) and Hiberix [(Haemophilus influenzae type b Conjugate vaccine) [Hib] (Tetanus Toxoid conjugate)] were administered concomitantly with Prevnar 20 or Prevnar 13 at 2, 4, and 6 months of age; M-M-R II [Measles, Mumps, and Rubella Virus Vaccine Live] (MMR) and VARIVAX [Varicella virus vaccine live] were administered concomitantly with Prevnar 20 or Prevnar 13 at 12 through 15 months of age. In Study 10, Pediarix was administered concomitantly with Prevnar 20 or Prevnar 13 at 2, 4, and 6 months of age. In Studies 8 and 10, influenza and rotavirus vaccines were also permitted to be co-administered with Prevnar 20 or Prevnar 13 according to recommendations. The proportion of participants receiving a concomitant influenza vaccine and the proportions of participants receiving a concomitant rotavirus vaccine were similar across the two study groups in Studies 8 and 10. In Study 8, 65.8% to 87.3% of participants received a rotavirus vaccine with each of the first 3 doses of Prevnar 20; 11.7% and 10.1% of participants received an influenza vaccine with Dose 3 and Dose 4 of Prevnar 20, respectively. In Study 10, 65.3% to 94.8% of participants received a rotavirus vaccine with each of the first 3 doses of Prevnar 20; 21.4% of participants received an influenza vaccine with Dose 3 of Prevnar 20. In Study 9, US-licensed or non-US licensed routine pediatric vaccines were permitted to be given during the study, including with Prevnar 20 or Prevnar 13, according to local or national recommendations.
Across the infant trials, solicited local and systemic adverse reactions were recorded daily by parents/guardians using an electronic diary for 7 consecutive days following each vaccination. Adverse events (AEs) were reported from administration of the first dose until one month after the third dose, and from the fourth dose through one month after the fourth dose. Serious adverse events (SAEs) and newly diagnosed chronic medical conditions (NDCMCs) were reported from administration of the first dose through 6 months after the last dose.
Solicited Adverse Events in Individuals Receiving a 4-Dose Series (Study 8)
The percentage of participants in Study 8 with solicited local and systemic adverse reactions that occurred within 7 days following vaccination are shown in Tables 2 and 3. The median day of onset for local and systemic reactions was between Day 1 and Day 2 (Day 1 was the day of vaccination), and reactions resolved with a median duration between 1 to 2 (local reactions) or 3 days (systemic reactions).
Table 2. Percentage of Participants at 2, 4, 6, and 12 Through 15 Month of Age With Solicited Local Adverse Reactions Within 7 Days After Each Vaccination – Study 8* Note: Local reactions were collected in the e-diary from Day 1 through Day 7 after each dose. If a severe reaction was identified by the investigator as a Grade 4 reaction at a follow-up assessment, it was also reported as an adverse reaction. - * Study 8 was conducted in the United States and the territory of Puerto Rico (NCT04382326).
- † N = number of participants with any e-diary data reported after the specified dose. This value is the denominator for the percentage calculations.
- ‡ Mild: hurts if gently touched; moderate: hurts if gently touched with crying; severe: causes limitation of limb movement.
- § Any includes all participants who reported a reaction as mild, moderate, or severe during Day 1 to Day 7 after vaccination
- ¶ Mild: >0.0 to 2.0 cm; moderate: >2.0 to 7.0 cm; severe: >7.0 cm.
- # Any local reaction includes all participants who reported any injection site reaction (pain, swelling, or redness) as mild, moderate, or severe during Day 1 to Day 7 after vaccination.
Dose 1
Dose 2
Dose 3
Dose 4
Vaccine Group
Prevnar 20
(N†=993)
%
Prevnar 13
(N†=974)
%
Prevnar 20
(N†=940)
%
Prevnar 13
(N†=924)
%
Prevnar 20
(N†=914)
%
Prevnar 13
(N†=901)
%
Prevnar 20
(N†=826)
%
Prevnar 13
(N†=815)
%
Local Reaction
Pain at injection site‡
Any§
49.1
45.3
44.0
41.7
38.6
39.0
35.7
35.8
Mild
30.6
30.4
29.3
27.7
25.7
25.5
24.1
27.1
Moderate
18.4
14.9
14.8
14.0
12.9
13.4
11.3
8.7
Severe
0.1
0
0
0
0
0
0.4
0
Redness¶
Any§
25.5
24.6
23.2
26.4
25.4
27.2
23.5
26.6
Mild
21.5
22.3
21.2
23.1
21.1
23.5
19.6
22.0
Moderate
4.0
2.4
2.0
3.4
4.3
3.7
3.9
4.7
Severe
0
0
0
0
0
0
0
0
Swelling¶
Any§
16.4
18.8
15.5
17.3
17.1
17.6
14.9
17.3
Mild
11.5
14.7
11.5
13.5
12.5
13.8
10.7
13.6
Moderate
4.8
4.1
4.0
3.8
4.6
3.8
4.2
3.7
Severe
0.1
0
0
0
0
0.1
0
0
Any local reaction#
59.8
56.5
53.1
52.7
50.8
49.1
44.8
45.9
Table 3. Percentage of Participants at 2, 4, 6, and 12 Through 15 Months of Age With Solicited Systemic Adverse Reactions Within 7 Days After Each Vaccination – Study 8* Note: Systemic reactions and use of antipyretic/pain medication were collected in the e-diary from Day 1 through Day 7 after each dose. If a severe reaction was identified by the investigator as a Grade 4 reaction at a follow-up assessment, it was also reported as an adverse reaction. - * Study 8 was conducted in the United States and the territory of Puerto Rico (NCT04382326).
- † N = number of participants with any e-diary data reported after the specified dose. This value is the denominator for the percentage calculations.
- ‡ Mild: easily consolable; moderate: requiring increased attention; severe: inconsolable; crying cannot be comforted.
- § Any includes all participants who reported a reaction as mild, moderate, or severe during Day 1 to Day 7 after vaccination
- ¶ Mild: increased or prolonged sleeping bouts; moderate: slightly subdued interfering with daily activity; severe: disabling not interested in usual daily activity.
- # Mild: decreased interest in eating; moderate: decreased oral intake; severe: refusal to feed.
- Þ Any systemic reaction: includes all participants who reported any fever ≥38.0°C or any other systemic reaction (irritability, drowsiness or decreased appetite) as mild, moderate, or severe during Day 1 to Day 7 after vaccination. The route of temperature measurement was to be rectal.
- ß Severity was not collected for use of antipyretic or pain medication. The numbers listed reflect yes responses (i.e., number of events reported).
Dose 1
Dose 2
Dose 3
Dose 4
Vaccine Group
Prevnar 20
(N†=993)
%
Prevnar 13
(N†=974)
%
Prevnar 20
(N†=940)
%
Prevnar 13
(N†=924)
%
Prevnar 20
(N†=914)
%
Prevnar 13
(N†=901)
%
Prevnar 20
(N†=826)
%
Prevnar 13
(N†=815)
%
Systemic Events
Irritability‡
Any§
70.9
71.7
71.6
68.8
64.4
63.0
61.0
61.1
Mild
23.4
21.6
22.9
21.2
25.2
21.6
23.4
21.8
Moderate
43.0
46.2
44.7
43.4
37.5
39.2
35.0
37.9
Severe
4.5
3.9
4.0
4.2
1.8
2.2
2.7
1.3
Drowsiness¶
Any§
67.2
66.0
54.7
55.6
44.1
44.1
39.5
39.5
Mild
50.2
49.3
37.0
36.9
31.1
30.1
27.8
28.2
Moderate
16.1
15.6
16.9
17.9
12.5
13.1
11.0
10.7
Severe
0.9
1.1
0.7
0.9
0.5
0.9
0.6
0.6
Decreased Appetite#
Any§
24.4
23.9
26.4
23.5
20.6
22.4
24.8
25.2
Mild
14.5
16.1
16.4
15.3
13.5
13.9
15.9
16.1
Moderate
9.7
7.5
9.8
7.7
6.7
8.2
8.6
8.3
Severe
0.2
0.3
0.2
0.5
0.4
0.3
0.4
0.7
FeverÞ
≥38.0℃
10.3
7.5
17.3
16.3
12.6
13.7
14.5
14.0
≥38.0℃ to 38.4°C
7.3
6.3
10.9
10.0
7.7
7.9
6.5
7.7
>38.4℃ to 38.9°C
2.2
0.9
4.0
4.2
3.4
3.9
5.1
3.2
38.9℃ to 40.0°C
0.7
0.3
2.2
2.2
1.4
1.9
2.7
2.9
>40.0°C
0.1
0
0.2
0
0.1
0
0.2
0.1
Any systemic reactionÞ
85.9
84.5
82.0
80.5
74.0
72.6
70.8
71.2
Use of antipyretic or painß
35.1
33.8
40.7
41.0
36.3
36.1
37.5
36.7
Unsolicited Serious and Non-Serious Adverse Events in Individuals Receiving a 4-Dose Series (Studies 8 through 10)
Globally, across the 3 infant trials, the proportion of participants reporting 1 or more SAEs within 6 months after the fourth dose of Prevnar 20 was 4.5% (101 of 2232 participants). This was similar to the proportion of participants with SAEs after vaccination with Prevnar 13 3.7% (64 of 1717 participants). The proportions of SAEs observed from the first dose to 1 month after the third dose were 1.1% and 1.2% for Prevnar 20 and Prevnar 13, and from the fourth dose to 1 month after the fourth dose were 0.7% and 0.5% respectively. Participants in these studies may have received other US-licensed (Studies 8, 9, and 10) or non-US-licensed concomitant (Study 9) vaccines according to their local recommended schedule. In the Prevnar 20 group, two febrile seizures considered possibly related to vaccination with Prevnar 20 were reported. One case was serious and occurred 14 days after the fourth dose given with MMR and varicella vaccine. One case was non-serious and occurred 7 days after the fourth dose of Prevnar 20 in an individual with diagnosis of COVID-19 infection.
One participant experienced isolated injection site hypersensitivity (redness) within approximately 30 minutes of Prevnar 20 after each of the first 3 doses resolving on the same day, this was not observed after the fourth dose.
There were no notable patterns or imbalances between vaccine groups for specific categories of SAEs that would suggest a causal relationship to Prevnar 20.
Safety Assessment in Individuals 15 Months Through 17 Years of Age Receiving Catch-Up Vaccination (Study 11)
The safety of Prevnar 20 in individuals (15 months through 17 years of age) was assessed in a single-arm trial of safety and immunogenicity of a single dose of Prevnar 20 conducted in the United States (Study 11) (NCT 04642079). A total of 831 participants received a single dose of Prevnar 20 among the 4 age groups (≥15 to <24 months, ≥2 to <5 years, ≥5 to <10 years, and ≥10 to <18 years). Participants <5 years of age were eligible if they had received at least 3 prior doses of Prevnar 13. Routine pediatric vaccines including DTaP vaccines, Hib, hepatitis A, and influenza vaccines were permitted to be co-administered with Prevnar 20, if not feasible to separate from Prevnar 20 by 14 days. There were similar percentages of male and female participants, with the exception of a higher percentage of male than female participants (approximately 56% males) in the age groups ≥15 months to <24 months of age and ≥10 to <18 years of age. Participants were predominantly White (80.1% to 86.6%), with nearly all the other participants being Black or African American (8.3% to 12.4%) and multiracial (2.5% to 6.0%); 15.4% to 21.0% were Hispanic.
The safety assessment was consistent with that used in studies 8 through 10, with the exception of that age-applicable systemic adverse reactions were recorded. The types of solicited systemic events collected in the participants ≥15 months to <2 years of age were consistent with those collected in participants 6 weeks through 15 months of age (i.e., irritability, decreased appetite, drowsiness/increased sleep and fever), while the solicited systemic events in participants ≥2 years of age required verbal communication by the participant (i.e., fatigue, headache, muscle pain, joint pain and fever).
Solicited Adverse Reactions in Individuals 15 Months Through 17 Years of Age Receiving Catch-Up Vaccination (Study 11)
After a single dose of Prevnar 20, most local and systemic adverse reaction in individuals 15 months through 17 years of age were mild or moderate in severity and resolved within 1 to 2 days. The most frequently reported local reaction was pain at injection site (52.5%, 66.0%, 82.9%, 82.0% in individuals ≥15 months to <24 months, ≥2 to <5 years, ≥5 to <10 years, and ≥10 to <18 years respectively), followed by redness and swelling. Most local reactions were mild or moderate in severity.
The most frequently reported solicited systemic reactions in individuals ≥15 months to <2 years of age were irritability (61.8%), followed by drowsiness and increased sleep (41.7%), and decreased appetite (25.0%). Fever ≥38.0°C was reported by 11.8% of individuals; fever >38.4°C was reported infrequently.
The most frequently reported systemic events in participants ≥2 to <18 years of age varied by age group. Fatigue was most frequently reported in individuals ≥2 to <5 years of age, and muscle pain was most frequently reported in participants ≥5 to <10 years and ≥10 to <18 years of age. Fever was reported infrequently (in ≤3.3% of individuals ≥2 to <5 years of age and only 1 participant, 0.5% ≥5 to <10 years of age).
Serious Adverse Events in Individuals 15 Months Through 17 Years of Age (Study 11)
In Study 11, five participants reported SAEs within 6 months after vaccination (2 participants [1.0%] ≥15 to <24 months of age and 3 participants [1.5%] ≥10 to <18 years of age). One participant (0.5%) ≥15 to <24 months of age reported an SAE within 1 month after vaccination. No SAEs were considered related to the vaccination.
Unsolicited Adverse Reactions Following the Use of Prevnar and Prevnar 13
Events observed in clinical trials with Prevnar (Pneumococcal 7-valent Conjugate Vaccine [Diphtheria CRM197 Protein]) or Prevnar 13 in individuals 6 weeks through 15 months of age are relevant to Prevnar 20 since the vaccines are manufactured and formulated similarly and contain 7 and 13 of the same polysaccharide conjugates, respectively.
Reactions occurring in greater than 1% of infants and toddlers following administration of Prevnar 13: diarrhea, vomiting, and rash.
Reactions occurring in less than 1% of infants and toddlers following administration of Prevnar 13: crying, hypersensitivity reaction (including face edema, dyspnea, and bronchospasm), seizures (including febrile seizures), and urticaria or urticaria-like rash.
Among 6,839 participants who received at least 1 dose of Prevnar 13 in clinical trials conducted globally, there was 1 hypotonic-hyporesponsive episode adverse reaction reported (0.015%). Among 4,204 participants who received at least 1 dose of Prevnar in clinical trials conducted globally, there were 3 hypotonic-hyporesponsive episode adverse reactions reported (0.071%). All 4 events occurred in a single clinical trial in Brazil in which participants received whole cell pertussis vaccine at the same time as Prevnar 13 or Prevnar.
Clinical Trials Experience With Prevnar 20 in Individuals 18 Years of Age and Older
The safety of a single dose of Prevnar 20 in individuals 18 years of age and older was evaluated in 6 randomized, active-controlled, multicenter clinical trials and one open-label, multicenter clinical trial. All of the trials were conducted in the United States and 2 of the trials also enrolled participants (N=172) in Sweden. Across the 7 trials, 6343 individuals received Prevnar 20 and 2496 received active control vaccine.
Safety Assessments in Pneumococcal Vaccine Naïve Participants 18 Years of Age and Older (Studies 1 through 5)
The safety of Prevnar 20 in individuals 18 years of age and older with no history of pneumococcal vaccination was evaluated in 5 studies (Studies 1–5). In the main cohort of Study 1 (NCT03760146) and in Study 2 (NCT03313037), participants ≥60 years of age and participants 60 through 64 years of age, respectively, received a single dose of Prevnar 20 followed 1 month later with administration of saline placebo or received a single dose of Prevnar 13 followed 1 month later with a dose of PNEUMOVAX® 23 (PPSV23). The 2 other cohorts of Study 1, participants 50 through 59 years of age and participants 18 through 49 years of age, received a single vaccination with Prevnar 20 or Prevnar 13. In Study 3 (NCT03828617), participants 18 through 49 years of age received a single vaccination with Prevnar 20 or Prevnar 13. In Studies 4 (NCT02955160) and 5 (NCT03642847), which were smaller studies conducted early in the clinical development of Prevnar 20, participants 18 through 49 years of age received a single dose of Prevnar 20 or an active control (Tdap or Prevnar 13).
Safety Assessments in Participants ≥65 Years of Age (Pneumococcal Vaccine Naïve or Previously Immunized with a Pneumococcal Vaccine) (Studies 6 and 7)
The safety of Prevnar 20 in individuals 65 years of age and older with pneumococcal vaccination given as routine care prior to enrollment was assessed in Study 6 (NCT03835975). Participants were enrolled into 1 of 3 cohorts based on their prior pneumococcal vaccination history (PPSV23 only ≥1 to ≤5 years prior to enrollment, Prevnar 13 only ≥6 months prior to enrollment, or Prevnar 13 followed by PPSV23 [with PPSV23 given ≥1 year prior to enrollment]). Participants in 2 of the cohorts received a single vaccination with Prevnar 20 or control pneumococcal vaccine (Prevnar 13), and the other cohort received a single vaccination with Prevnar 20. only.
The safety of Prevnar 20 in individuals 65 years of age and older when coadministered with Influenza Vaccine, Adjuvanted (Fluad Quadrivalent) was assessed in Study 7 (NCT 04526574). Randomization was stratified by prior pneumococcal vaccine status (no previous pneumococcal vaccine, receipt of at least 1 dose of PPSV23 only, receipt of at least 1 dose of Prevnar 13 only, or receipt of at least 1 dose each of PPSV23 and Prevnar 13). Participants were randomized in a 1:1 ratio to receive Prevnar 20 concomitantly administered with Fluad Quadrivalent (Group 1) or Fluad Quadrivalent followed approximately one month later by Prevnar 20 (Group 2).
Demographics of Trial Participants 18 Years of Age and Older (Studies 1, 3, 6 and 7)
In the three main trials (Studies 1, 3, and 6), participants were predominantly female (52.0% to 65.9%) across groups defined by age and prior pneumococcal vaccination status within the Prevnar 20 and control vaccine groups. Across all 3 trials combined, 59.8% of participants were 60 years of age and older, 6.9% were 50 through 59 years of age, and 33.3% were 18 through 49 years of age. In Studies 1 and 3, participants were 80.7% White, 14.2% Black, 2.1% Asian, and 10.3% Hispanic. In Study 6, participants were predominantly White (92.4%). Participants were primarily from the United States; however a portion of participants 65 years of age and older were enrolled from Sweden in Study 1 (5.7% of participants 60 years of age and older in that study) and also in Study 6 (35.5% of participants with prior PPSV23 only). In Study 7, 54.7% of participants were female. The mean age of participants was 72 years (range 65–103 years). Participants were 90.6% White, 6.9% Black, 1.2% Asian, and 9.4% Hispanic.
In the three main trials, participants with pre-existing underlying diseases were enrolled if the medical condition was stable (did not require a significant change in therapy in the 6 weeks before receipt of study vaccine or any hospitalization for worsening disease within 12 weeks before receipt of study vaccine). In Study 1, approximately one-third of all participants had risk factors that placed them at increased risk for serious pneumococcal disease, including smoking (12.9%), stable medical conditions of chronic cardiovascular disease (5.5%), chronic pulmonary disease including asthma (8.7%), chronic liver disease (0.4%), and diabetes mellitus (13.9%).
Safety Monitoring
Solicited adverse reactions for Prevnar 20 in the three main trials and Study 7 were monitored in participants recording daily into an electronic diary their local adverse reactions for 10 consecutive days and systemic reactions for 7 consecutive days following vaccination. Across all trials, serious and nonserious adverse events were collected for 1 month after each vaccination. Safety follow-up of SAEs continued through 6 months after vaccination with Prevnar 20 or Prevnar 13 (or other appropriate control vaccine), as applicable. Newly diagnosed chronic medical conditions occurring within 6 months after vaccination were also collected via telephone contact.
Serious Adverse Events in Participants 18 Years of Age and Older (Studies 1 through 6)
Across studies 1 through 6, performed in individuals of all ages, naïve to and with prior pneumococcal vaccination, the proportion of participants reporting 1 or more SAEs within 6 months after vaccination with Prevnar 20 was 1.5% (67 of 4552 participants). This was similar to the proportion of participants with SAEs after vaccination with Prevnar 13 or other applicable control vaccine (1.8%, 44 of 2496). The proportions of participants with SAEs occurring within 1 month after vaccination with Prevnar 20 or with Prevnar 13 or other applicable control vaccine were both 0.4% (19 of 4552 participants and 11 of 2496 participants, respectively). There were no notable patterns or imbalances between vaccine groups for specific categories of serious adverse events that would suggest a causal relationship to Prevnar 20.
Solicited Adverse Reactions in Participants 18 Years of Age and Older (Studies 1 and 6)
The frequency and severity of the local adverse reactions (redness, swelling, and pain at the injection site) prompted daily in the 10 days after Prevnar 20 vaccination in individuals naïve to pneumococcal vaccination (Study 1) and in individuals with prior pneumococcal vaccination (Study 6) are shown in Table 4 and Table 5, respectively. The frequency and severity of the systemic adverse reactions (fever, fatigue, headache, muscle pain, and joint pain) prompted daily in the 7 days after Prevnar 20 vaccination in individuals naïve to pneumococcal vaccination (Study 1) and in individuals with prior pneumococcal vaccination (Study 6) are shown in Table 6 and Table 7, respectively.
Table 4. Percentage of Participants With Solicited Local Adverse Reactions, by Maximum Severity, Within 10 Days After Vaccination in Pneumococcal Vaccine-Naïve Individuals - Study 1* - * Study 1 was conducted in the United States and in Sweden (NCT03760146).
- † N = number of participants with any e-diary data reported after vaccination (after Vaccination 1 [Prevnar 20 or Prevnar 13] for Study 1 participants 60 years of age and older). This value is the denominator for the percentage calculations.
- ‡ Diameters were measured in caliper units of whole numbers from 1 to 21 or 21+. One caliper unit = 0.5 cm. Measurements were rounded up to the nearest whole number. Intensity of redness and swelling were then characterized as follows: mild is >2.0 to 5.0 cm; moderate is >5.0 to 10.0 cm; severe is >10.0 cm.
- § "Any" includes all participants who reported a reaction as "mild", "moderate", or "severe" during Day 1 to Day 10 after vaccination.
- ¶ Mild = does not interfere with activity; moderate = interferes with activity; severe = prevents daily activity.
- # "Any local reaction" includes all participants who reported any injection site reaction (pain, swelling, or redness) as "mild", "moderate", or "severe" during Day 1 to Day 10 after vaccination.
18–49 Years of Age
50–59 Years of Age
≥60 Years of Age
Vaccine Group
Prevnar 20
(N†=335)
%Prevnar 13
(N†=112)
%Prevnar 20
(N†=331)
%Prevnar 13
(N†=111)
%Prevnar 20/Saline
(N†=1505)
%Prevnar 13/PPSV23
(N†=1483)
%Local Reaction
Pain at injection site‡
Any§
81.2
82.1
72.5
69.4
55.4
54.1
Mild
42.7
52.7
53.5
52.3
45.3
44.6
Moderate
38.2
28.6
17.8
16.2
9.9
9.2
Severe
0.3
0.9
1.2
0.9
0.2
0.3
Swelling¶
Any (>2.0 cm)§
11.6
12.5
8.8
10.8
7.5
8.0
Mild
7.2
8.9
5.7
7.2
4.8
4.9
Moderate
4.5
3.6
3.0
3.6
2.4
2.8
Severe
0
0
0
0
0.3
0.3
Redness¶
Any (>2.0 cm)§
9.0
9.8
8.2
5.4
7.3
6.2
Mild
3.0
5.4
5.1
2.7
3.7
3.8
Moderate
5.4
4.5
2.7
2.7
2.8
2.2
Severe
0.6
0
0.3
0
0.8
0.2
Any local reaction#
81.2
82.1
72.8
70.3
57.4
56.0
Table 5. Percentage of Participants With Solicited Local Adverse Reactions, by Maximum Severity, Within 10 Days After Vaccination in Individuals 65 Years of Age and Older With Prior Pneumococcal Vaccination – Study 6*,† - * Study 6 was conducted in the United States and in Sweden (NCT03835975)
- † Open-label administration of Prevnar 20.
- ‡ Includes participants who previously received either PPSV23 ≥1 to ≤5 years before enrollment (PPSV23), Prevnar 13 ≥6 months before enrollment (Prevnar 13), or Prevnar 13 followed by PPSV23 ≥1 year before enrollment (Prevnar 13 and PPSV23) in the study.
- § N = number of participants with any e-diary data reported after vaccination. This value is the denominator for the percentage calculations.
- ¶ Mild = does not interfere with activity; moderate = interferes with activity; severe = prevents daily activity.
- # "Any" includes all participants who reported a reaction as "mild", "moderate", or "severe" during Day 1 to Day 10 after vaccination.
- Þ Diameters were measured in caliper units of whole numbers from 1 to 21 or 21+. One caliper unit = 0.5 cm. Measurements were rounded up to the nearest whole number. Intensity of redness and swelling were then characterized as follows: mild is >2.0 to 5.0 cm; moderate is >5.0 to 10.0 cm; severe is >10.0 cm.
- ß "Any local reaction" includes all participants who reported any injection site reaction (pain, swelling, or redness) as "mild", "moderate", or "severe" during Day 1 to Day 10 after vaccination.
Prior Pneumococcal Vaccination Status‡
PPSV23
Prevnar 13
Prevnar 13 and PPSV23
Vaccine Group
Prevnar 20
(N§=253)
%Prevnar 13
(N§=121)
%Prevnar 20
(N§=245)
%PPSV23
(N§=126)
%Prevnar 20
(N§=125)
%Local Reaction
Pain at the injection site¶
Any#
50.2
43.0
61.2
56.3
52.8
Mild
45.8
38.8
54.7
40.5
47.2
Moderate
4.3
3.3
6.1
14.3
5.6
Severe
0
0.8
0.4
1.6
0
SwellingÞ
Any (>2.0 cm)#
9.9
6.6
9.4
14.3
4.0
Mild
5.1
6.6
5.7
6.3
1.6
Moderate
3.6
0
3.7
7.1
2.4
Severe
1.2
0
0
0.8
0
RednessÞ
Any (>2.0 cm)#
7.9
2.5
8.6
12.7
4.8
Mild
3.6
1.7
2.9
4.8
1.6
Moderate
3.2
0.8
5.3
7.1
3.2
Severe
1.2
0
0.4
0.8
0
Any local reactionß
53.0
43.8
64.1
57.9
54.4
Table 6. Percentage of Participants With Solicited Systemic Reactions, by Maximum Severity, Within 7 Days After Vaccination in Pneumococcal Vaccine-Naïve Individuals – Study 1* - * Study 1 was conducted in the United States and in Sweden (NCT03760146).
- † N = number of participants with any e-diary data reported after vaccination (after Vaccination 1 [Prevnar 20 or Prevnar 13] for Study 1 participants 60 years of age and older). This value is the denominator for the percentage calculations.
- ‡ Mild = does not interfere with activity; moderate = some interference with activity; severe = prevents daily activity.
- § "Any" includes all participants who reported a reaction as "mild", "moderate", or "severe" during Day 1 to Day 7 after vaccination.
- ¶ "Any systemic reaction" includes all participants who reported any fever ≥38.0°C or any other systemic reaction (fatigue, headache, joint pain, or muscle pain) as "mild", "moderate", or "severe" during Day 1 to Day 7 after vaccination.
- # Severity was not collected for use of antipyretic or pain medication. The numbers listed reflect "yes" responses (i.e., number of reactions reported).
18 through 49 Years of Age
50 through 59 Years of Age
≥60 Years of Age
Vaccine Group
Prevnar 20
(N†=335)
%Prevnar 13
(N†=112)
%Prevnar 20
(N†=331)
%Prevnar 13
(N†=111)
%Prevnar 20/Saline
(N†=1505)
%Prevnar 13/PPSV23
(N†=1483)
%Systemic Reaction
Muscle pain‡
Any§
66.6
74.1
49.8
49.5
39.1
37.3
Mild
36.4
42.0
33.8
31.5
28.9
26.8
Moderate
29.0
31.3
15.4
17.1
9.8
10.0
Severe
1.2
0.9
0.6
0.9
0.4
0.5
Fatigue‡
Any§
42.7
43.8
39.3
36.0
30.2
30.7
Mild
18.8
20.5
21.1
18.0
16.1
17.5
Moderate
22.1
19.6
17.2
15.3
12.8
11.9
Severe
1.8
3.6
0.9
2.7
1.2
1.2
Headache‡
Any§
38.8
33.9
32.3
36.0
21.5
23.3
Mild
21.5
16.1
20.5
21.6
15.5
17.0
Moderate
14.6
17.0
10.9
13.5
5.4
5.9
Severe
2.7
0.9
0.9
0.9
0.7
0.3
Joint pain‡
Any§
13.4
17.9
15.4
20.7
12.6
13.7
Mild
6.3
8.9
10.6
12.6
6.9
7.1
Moderate
7.2
8.0
4.8
7.2
5.4
6.3
Severe
0
0.9
0
0.9
0.3
0.2
Fever
≥38.0°C
1.2
1.8
1.5
0.9
0.9
0.8
≥38.0°C to 38.4°C
0.6
0
0.6
0.9
0.3
0.4
>38.4°C to 38.9°C
0.3
0
0.3
0
0.3
0.2
>38.9°C to 40.0°C
0.3
1.8
0.3
0
0
0
>40.0°C
0
0
0.3
0
0.3
0.2
Any systemic reaction¶
79.4
83.0
69.5
67.6
55.2
55.4
Use of antipyretic or pain medication#
25.7
23.2
24.5
27.9
18.5
20.4
Table 7. Percentage of Participants With Solicited Systemic Reactions, by Maximum Severity, Within 7 Days After Vaccination in Individuals 65 Years of Age and Older With Prior Pneumococcal Vaccination – Study 6*,† - * Study 6 was conducted in the United States and in Sweden (NCT03835975).
- † Open-label administration of Prevnar 20.
- ‡ Includes participants who previously received either PPSV23 ≥1 to ≤5 years before enrollment (PPSV23), Prevnar 13 ≥6 months before enrollment (Prevnar 13), or Prevnar 13 followed by PPSV23 ≥1 year before enrollment (Prevnar 13 and PPSV23) in the study.
- § N = number of participants with any e-diary data reported after vaccination. This value is the denominator for the percentage calculations.
- ¶ Mild = does not interfere with activity; moderate = interferes with activity; severe = prevents daily activity.
- # "Any" includes all participants who reported a reaction as "mild", "moderate", or "severe" during Day 1 to Day 7 after vaccination.
- Þ "Any systemic reaction" includes all participants who reported any fever ≥38.0°C or any other systemic reaction (fatigue, headache, joint pain, or muscle pain) as "mild", "moderate", or "severe" during Day 1 to Day 7 after vaccination.
- ß Severity was not collected for use of antipyretic or pain medication. The numbers listed reflect "yes" responses (i.e., number of reactions reported).
Prior Pneumococcal Vaccination Status‡
PPSV23
Prevnar 13
Prevnar 13 and PPSV23
Vaccine Group
Prevnar 20
(N§=253)
%Prevnar 13
(N§=121)
%Prevnar 20
(N§=245)
%PPSV23
(N§=126)
%Prevnar 20
(N§=125)
%Systemic Reaction
Muscle pain¶
Any#
32.0
31.4
33.9
46.0
37.6
Mild
26.1
24.0
25.3
31.7
28.0
Moderate
5.5
5.0
8.6
11.9
8.8
Severe
0.4
2.5
0
2.4
0.8
Fatigue¶
Any#
28.9
22.3
31.0
33.3
32.8
Mild
17.8
9.9
19.6
19.8
19.2
Moderate
11.1
9.9
10.2
13.5
12.0
Severe
0
2.5
1.2
0
1.6
Headache¶
Any#
17.8
18.2
13.5
21.4
19.2
Mild
12.6
12.4
9.8
20.6
12.8
Moderate
4.7
5.8
3.7
0.8
5.6
Severe
0.4
0
0
0
0.8
Joint pain¶
Any#
6.7
10.7
11.8
15.9
16.8
Mild
4.7
5.0
7.8
10.3
12.8
Moderate
2.0
5.0
4.1
5.6
4.0
Severe
0
0.8
0
0
0
Fever
≥38.0°C
0.8
0
0
1.6
0
≥38.0°C to 38.4°C
0.8
0
0
0.8
0
>38.4°C to 38.9°C
0
0
0
0.8
0
>38.9°C to 40.0°C
0
0
0
0
0
>40.0°C
0
0
0
0
0
Any systemic reactionÞ
51.8
43.8
50.2
59.5
52.8
Use of antipyretic or pain medicationß
15.8
14.9
17.1
19.8
17.6
Safety with Concomitant Vaccine Administration in Participants ≥65 years of age (Study 7)
In Study 7, the rates of local reactions at the Prevnar 20 injection site within 10 days after vaccination were similar between participants who received Prevnar 20 and Fluad Quadrivalent concomitantly (Group 1) or separately (Group 2). The rates of systemic reactions within 7 days following administration of Prevnar 20 were generally numerically higher in Group 1 compared to Group 2; however, overall, fever in both groups was uncommon (<1.5%) and other systemic reactions (fatigue, headache, muscle, or joint pain) were primarily mild to moderate (≤0.9% were severe). The proportions of participants with SAEs occurring within 1 month after vaccination with Prevnar 20 were 1.1% for Group 1 and 1.7% in Group 2. No SAEs occurring within 1 month after vaccination with Prevnar 20 were considered related to vaccination.
6.2 Postmarketing Experience With Prevnar 13
The postmarketing safety experience with Prevnar 13 in individuals 6 weeks of age and older is relevant to Prevnar 20 since the vaccines are manufactured and formulated similarly and contain 13 of the same polysaccharide conjugates. These adverse reactions are included based on one or more of the following factors: severity, frequency of reporting, or strength of evidence for a causal relationship to Prevnar 13 vaccine. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to product exposure. The following adverse reactions have been spontaneously reported during postapproval use of Prevnar 13 and may also be seen in postmarketing experience with Prevnar 20.
- Blood and lymphatic system disorders: Lymphadenopathy localized to the region of the injection site
- Cardiac disorders: Cyanosis (pediatric populations only)
- General Disorders and Administration Site Conditions: Vaccination-site dermatitis, vaccination-site pruritus, vaccination-site urticaria
- Immune System Disorders: Anaphylactic/anaphylactoid reaction, including shock
- Nervous system disorders: Hypotonia (pediatric populations only
- Respiratory: Apnea (pediatric populations only)
- Skin and Subcutaneous Tissue Disorders: Angioneurotic edema, Erythema multiforme
- Vascular disorders: Pallor (pediatric populations only)
-
7 DRUG INTERACTIONS
7.1 Prior Vaccination With PNEUMOVAX 23
In adults, receipt of PPSV23 1 to 5 years prior to Prevnar 20 resulted in diminished OPA geometric mean titers (GMTs) to Prevnar 20 compared to OPA GMTs in recipients who received Prevnar 13 at least 6 months prior to Prevnar 20, and compared to OPA GMTs in recipients who received Prevnar 13 followed by PPSV23, with the last dose of PPSV23 given at least 1 year prior to Prevnar 20 [see Clinical Studies (14.2)].
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
All pregnancies have a risk of birth defect, loss, or other adverse outcomes. In the US general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively. There are no adequate and well-controlled studies of Prevnar 20 in pregnant women. Available data on Prevnar 20 administered to pregnant women are insufficient to inform vaccine-associated risks in pregnancy.
A developmental toxicity study was performed in female rabbits administered Prevnar 20 prior to mating and during gestation. The dose was 0.5 mL at each occasion (a single human dose is 0.5 mL). This study revealed no evidence of harm to the fetus due to Prevnar 20 (see Data).
Data
Animal Data
In a developmental toxicity study, female rabbits were administered Prevnar 20 by intramuscular injection twice prior to mating (17 days and 4 days prior to mating) and twice during gestation (Gestation Days 10 and 24), 0.5 mL/rabbit/occasion (a single human dose). No adverse effects on pre-weaning development were observed. There were no vaccine-related fetal malformations or variations.
8.2 Lactation
Risk Summary
It is not known whether Prevnar 20 is excreted in human milk. Data are not available to assess the effects of Prevnar 20 on the breastfed infant or on milk production/excretion. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for Prevnar 20 and any potential adverse effects on the breastfed child from Prevnar 20 or from the underlying maternal condition. For preventive vaccines, the underlying maternal condition is susceptibility to disease prevented by the vaccine.
8.4 Pediatric Use
The safety of Prevnar 20 has been established in individuals 6 weeks through 17 years of age [see Adverse Reactions (6.1)].
The effectiveness of Prevnar 20 for the prevention of invasive disease caused by S. pneumoniae serotypes 1, 3, 4, 5, 6A, 6B, 7F, 8, 9V, 10A, 11A, 12F, 14, 15B, 18C, 19A, 19F, 22F, 23F, and 33F has been established in individuals 6 weeks through 17 years of age [see Clinical Studies (14.2)].
The effectiveness of Prevnar 20 for the prevention of otitis media caused by serotypes 4, 6B, 9V, 14, 18C, 19F, and 23F has been established in individuals 6 weeks through 5 years of age [see Clinical Studies (14.1)].
The effectiveness of Prevnar 20 in infants and children initiating vaccination at 7 months through 17 years of age and in children 15 months through 17 years of age previously vaccinated or incompletely vaccinated with a pneumococcal conjugate vaccine is supported by evidence from clinical studies in younger children who received a 4-dose series of Prevnar 20 and by evidence from clinical studies of catch-up vaccination with Prevnar 13 and Prevnar.
The effectiveness of Prevnar 20 for the prevention of pneumonia has not been established in individuals younger than 18 years of age.
The safety and effectiveness of Prevnar 20 in individuals younger than 6 weeks of age have not been established.
8.5 Geriatric Use
Of the total number of Prevnar 20 recipients 18 years of age and older evaluated for safety in the 3 main clinical trials (N=4263), 26.7% (n=1138) were 65 years of age and older and 1.7% (n=72) were 80 years of age and older [see Clinical Studies (14.2)].
Prevnar 20 recipients 70 through 79 years of age and ≥80 years of age had lower OPA GMTs for all pneumococcal serotypes compared to Prevnar 20 recipients 18 through 49 years, 50 through 59, and 60 through 64 years of age [see Clinical Studies (14.1)].
-
11 DESCRIPTION
Prevnar 20, Pneumococcal 20-valent Conjugate Vaccine is a sterile suspension of saccharides of the capsular antigens of S. pneumoniae serotypes 1, 3, 4, 5, 6A, 6B, 7F, 8, 9V, 10A, 11A, 12F, 14, 15B, 18C, 19A, 19F, 22F, 23F, and 33F, individually linked to non-toxic diphtheria CRM197 protein. Each serotype is grown in soy peptone broth. The individual polysaccharides are purified by a series of chemical and physical methods. The polysaccharides are chemically activated and then directly conjugated to the carrier protein CRM197, to form the glycoconjugate. CRM197 is a non-toxic variant of diphtheria toxin isolated from cultures of Corynebacterium diphtheriae strain C7 (β197) grown in a casamino acids and yeast extract-based medium or in a chemically-defined medium. CRM197 is purified by a series of chemical and physical methods. The individual glycoconjugates are purified by a series of chemical and physical methods and analyzed for saccharide to protein ratios, molecular size, free saccharide, and free protein.
The individual glycoconjugates are compounded to formulate Prevnar 20. Potency of the formulated vaccine is determined by quantification of each of the saccharide antigens and by the saccharide to protein ratios in the individual glycoconjugates. Each 0.5 mL dose of the vaccine is formulated to contain approximately 2.2 μg of each of S. pneumoniae serotypes 1, 3, 4, 5, 6A, 7F, 8, 9V, 10A, 11A, 12F, 14, 15B, 18C, 19A, 19F, 22F, 23F, 33F saccharides, 4.4 μg of 6B saccharides, 51 μg CRM197 carrier protein, 100 μg polysorbate 80, 295 μg succinate buffer, 4.4 mg sodium chloride, and 125 μg aluminum as aluminum phosphate adjuvant.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Protection against pneumococcal disease is conferred mainly by antibodies (immunoglobulin G [IgG] directed against capsular polysaccharides) and OPA killing of S. pneumoniae. Prevnar 20 induces IgG antibodies and OPA against the 20 vaccine serotypes.
An opsonic antibody titer or serotype-specific IgG concentration that is predictive of protection against invasive pneumococcal disease or pneumococcal pneumonia has not been established.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Prevnar 20 has not been evaluated for the potential to cause carcinogenicity, genotoxicity, or impairment of male fertility. Vaccination of female rabbits with Prevnar 20 had no effect on female fertility [see Use in Specific Populations (8.1)].
-
14 CLINICAL STUDIES
14.1 Prevnar and Prevnar 13 Efficacy Data
Efficacy and effectiveness of Prevnar and Prevnar 13 are relevant to Prevnar 20, since Prevnar, Prevnar 13 and Prevnar 20 are manufactured similarly. In addition, Prevnar and Prevnar 20 contain 7 of the same polysaccharide conjugates and Prevnar 13 and Prevnar 20 contain 13 of the same polysaccharide conjugates.
Prevnar Efficacy Data in Children
Invasive Pneumococcal Disease (IPD)
Prevnar was licensed in the United States for infants and children in 2000, following a randomized, double‑blind, clinical trial in a multiethnic population at Northern California Kaiser Permanente (NCKP) from October 1995 through August 20, 1998, in which 37,816 infants were randomized to receive either Prevnar or a control vaccine (an investigational meningococcal group C conjugate vaccine [MnCC]) at 2, 4, 6, and 12 through 15 months of age. In this study, the efficacy of Prevnar against invasive disease due to S. pneumoniae in cases accrued during this period was 100% in both the per-protocol and intent-to-treat analyses (95% confidence interval [CI]: 75.4%, 100% and 81.7%, 100%, respectively). Data accumulated through an extended follow-up period to April 20, 1999, resulted in similar efficacy estimates of 97.4% in the per-protocol analysis and 93.9% in the intent-to-treat analysis (95% CI: 82.7%, 99.9% and 79.6%, 98.5%, respectively).
Acute Otitis Media (AOM)
The efficacy of Prevnar against otitis media was assessed in 2 clinical trials: a trial in Finnish infants at the National Public Health Institute and the efficacy trial in US infants at NCKP.
The Finnish Otitis Media (FinOM) trial was a randomized, double-blind trial in which 1,662 infants were equally randomized to receive either Prevnar or a control vaccine Recombivax HB (Hepatitis B vaccine (Recombinant) [Hep B]) at 2, 4, 6, and 12 through 15 months of age. In this study, conducted between December 1995 and March 1999, parents of study participants were asked to bring their children to the study clinics if the child had respiratory infections or symptoms suggesting AOM. If AOM was diagnosed, tympanocentesis was performed, and the middle-ear fluid was cultured. If S. pneumoniae was isolated, serotyping was performed. The primary endpoint was efficacy against AOM episodes caused by vaccine serotypes in the per-protocol population.
The vaccine efficacy against AOM episodes due to vaccine serotypes assessed in the Finnish trial was 57% (95% CI: 44%, 67%) in the per-protocol population and 54% (95% CI: 41%, 64%) in the intent-to-treat population. The vaccine efficacy against AOM episodes due to vaccine-related serotypes (6A, 9N, 18B, 19A, 23A), also assessed in the Finnish trial, was 51% (95% CI: 27, 67) in the per-protocol population and 44% (95% CI: 20, 62) in the intent-to-treat population. There was a nonsignificant increase in AOM episodes caused by serotypes unrelated to the vaccine in the per-protocol population, compared to children who received the control vaccine, suggesting that children who received Prevnar appeared to be at increased risk of otitis media due to pneumococcal serotypes not represented in the vaccine. However, vaccination with Prevnar reduced pneumococcal otitis media episodes overall. In the NCKP trial, in which the endpoint was all otitis media episodes regardless of etiology, vaccine efficacy was 7% (95% CI: 4%, 10%) and 6% (95% CI: 4%, 9%), respectively, in the per-protocol and intent-to-treat analyses. Several other otitis media endpoints were also assessed in the 2 trials.
In the NCKP trial, the efficacy of Prevnar against otitis media was assessed from the beginning of the trial in October 1995 through April 1998. The otitis media analysis included 34,146 infants randomized to receive either Prevnar (N=17,070), or the control vaccine (N=17,076), at 2, 4, 6, and 12 through 15 months of age. In this trial, no routine tympanocentesis was performed, and no standard definition of otitis media was used by study physicians. The primary otitis media endpoint was efficacy against all otitis media episodes in the per‑protocol population. Recurrent AOM, defined as 3 episodes in 6 months or 4 episodes in 12 months, was reduced by 9% in both the per-protocol and intent-to-treat populations (95% CI: 3%, 15% in per-protocol and 95% CI: 4%, 14% in intent-to-treat) in the NCKP trial; a similar trend was observed in the Finnish trial. The NCKP trial also demonstrated a 20% reduction (95% CI: 2, 35) in the placement of tympanostomy tubes in the per-protocol population and a 21% reduction (95% CI: 4, 34) in the intent-to-treat population. Data from the NCKP trial accumulated through an extended follow-up period to April 20, 1999, in which a total of 37,866 children were included (18,925 in Prevnar group and 18,941 in MnCC control group), resulted in similar otitis media efficacy estimates for all endpoints.
Prevnar 13 Adult Efficacy Data
The efficacy of Prevnar 13 against vaccine-type (VT) pneumococcal community-acquired pneumonia (CAP) and IPD was assessed in a randomized, double-blind, placebo-controlled study (Community-Acquired Pneumonia Immunization Trial in Adults [CAPiTA]) conducted over ~4 years in the Netherlands. A total of 84,496 participants 65 years of age and older received a single dose of either Prevnar 13 or placebo in a 1:1 randomization; 42,240 participants were vaccinated with Prevnar 13 and 42,256 participants were vaccinated with placebo. Chronic medical conditions (asthma, diabetes, heart, liver, and/or lung diseases) were reported in 42.3% of study participants at baseline.
The primary objective was to demonstrate the efficacy of Prevnar 13 in the prevention of a first episode of confirmed VT-CAP (defined as presence of ≥2 specified clinical criteria, chest X-ray consistent with CAP as determined by a central committee of radiologists, and positive VT-specific urinary antigen detection assay [UAD] or isolation of VT S. pneumoniae from blood or other sterile site). The secondary objectives were to demonstrate the efficacy of Prevnar 13 in the prevention of a first episode of 1) confirmed nonbacteremic/noninvasive (NB/NI) VT-CAP (an episode of VT-CAP for which the blood culture result and any other sterile site culture results were negative for S. pneumoniae) and 2) VT-IPD (the presence of S. pneumoniae in a sterile site).
Surveillance for suspected pneumonia and IPD began immediately after vaccination and continued through identification of a prespecified number of cases. Participants who had a CAP or IPD episode with symptom onset less than 14 days after vaccination were excluded from all analyses.
The median duration of follow-up per participant was 3.93 years. Prevnar 13 demonstrated statistically significant vaccine efficacy (VE) in preventing first episodes of VT pneumococcal CAP, NB/NI VT pneumococcal CAP, and VT-IPD (see Table 8).
Table 8. Vaccine Efficacy for the Primary and Secondary Efficacy Endpoints – Per-Protocol Population Abbreviations: CAP = community-acquired pneumonia; CI = confidence interval; NB/NI = nonbacteremic/noninvasive; IPD = invasive pneumococcal disease; VE = vaccine efficacy; VT = vaccine-type. Vaccine Group
Prevnar 13
Placebo
N=42,240
N=42,256
Efficacy Endpoint
Total Number of Episodes
n
N
VE (%)
(95.2% CI)
Primary endpoint:
First case of confirmed VT pneumococcal CAP139
49
90
45.6
(21.8, 62.5)
Secondary endpoint:
First episode of confirmed NB/NI VT pneumococcal CAP93
33
60
45
(14.2, 65.3)
Secondary endpoint:
First episode of VT-IPD35
7
28
75
(41.1, 90.9)
14.2 Prevnar 20 Clinical Trials in Individuals 6 Weeks Through 15 Months of Age
Immunogenicity of Prevnar 20 in Individuals 6 Weeks Through 15 Months of Age
Prevnar 20 effectiveness against invasive pneumococcal disease in individuals 6 weeks through 15 months of age was demonstrated based on comparisons of serotype-specific antibody responses at 1 month after Dose 3 and 1 month after Dose 4 of Prevnar 20 to the antibody responses after vaccination with Prevnar 13.
Antibody responses elicited by Prevnar 20 and Prevnar 13 in these age groups were measured using a serotype-specific multiplex direct-binding Luminex® immunoassay (dLIA), designed to determine the concentration of serotype-specific polysaccharide-binding IgG antibodies, and OPA assays to measure serotype-specific functional OPA titers for the 20 pneumococcal serotypes of Prevnar 20. A serotype-specific IgG antibody concentration corresponding to ≥0.35 µg/mL using the World Health Organization (WHO) enzyme linked immunosorbent assay (ELISA) has been used as the threshold value for the clinical evaluation of pneumococcal conjugate vaccines when measured one month after Dose 3 of the 4-dose immunization series. The dLIA, used to measure the IgG antibody concentration, was bridged to the WHO ELISA to establish dLIA specific threshold values for each vaccine serotype that correspond to the established ≥0.35 µg/mL WHO ELISA threshold value.
In Study 8, a multicenter, randomized, active-controlled, double-blind trial, participants were randomized in a 1:1 ratio to receive Prevnar 20 (N=1004) or Prevnar 13 (N=993) in a 4-dose schedule; vaccine was administered at 2, 4, 6, and 12 through 15 months of age. Pediarix and Hiberix were administered concomitantly with each of the 3 infant doses. M-M-R II and VARIVAX were administered with the fourth dose [see Adverse Reactions (6.1) and Clinical Studies (14.3)].
Study 8 assessed serotype-specific IgG response rates, IgG geometric mean concentrations (GMCs) and OPA GMTs measured at one month after Dose 3 and one month after Dose 4 for all 20 serotypes contained in Prevnar 20. For each of the 13 matched serotypes, IgG response in the Prevnar 20 group were compared with the corresponding response in the Prevnar 13 group. For the 7 additional serotypes (serotypes 8, 10A, 11A, 12F, 15B, 22F, and 33F), IgG response in the Prevnar 20 group were compared with the lowest response among the 13 matched vaccine serotypes excluding serotype 3 in the Prevnar 13 group.
Pneumococcal IgG Antibody Responses Following 3 Doses of Prevnar 20
IgG antibody responses following Prevnar 20 were noninferior to those following Prevnar 13 for 8 of the 13 matched serotypes and 6 of the 7 additional serotypes, as assessed by the percentage of participants meeting the predefined serotype-specific IgG concentration one month after Dose 3, using a 10% noninferiority criterion (the lower bound of the 2-sided 95% CI for the difference in percentages [Prevnar 20 minus Prevnar 13] greater than -10%). Five of the 13 matched serotypes (serotypes 1, 3, 4, 9V and 23F) did not meet the pre-specified noninferiority criterion, as the lower bounds of the 2-sided 95% CIs for the difference in percentages (Prevnar 20 minus Prevnar 13) were -12.1%, -20.1%, -12.0%, -11.3%, and -11.4% respectively. One additional serotype (serotype 12F) also did not meet the NI criterion when compared to serotype 23F (the Prevnar 13 serotype with the lowest percentage excluding serotype 3) in the Prevnar 13 group, the lower bound of the 2-sided 95% CI for the difference in percentage (Prevnar 20 minus lowest Prevnar 13) was -41.6% (Table 9).
Additional IgG GMC data at one month after Dose 3 and OPA data at one month after Dose 3, presented in Tables 10 and 12 respectively, support the effectiveness of Prevnar 20 for each of the 6 serotypes that failed to meet the pre-specified non-inferiority criterion.
Table 9. Percentage of Participants Meeting Predefined Serotype-Specific Pneumococcal IgG Concentrations One Month After Dose 3 in Participants Vaccinated at 2, 4, and 6 Months of Age – Study 8* Abbreviation: IgG = immunoglobulin G. Note: The predefined IgG concentration was ≥0.35 µg/mL for all serotypes except for serotypes 5, 6B, 12F, and 19A which were ≥0.23 µg/mL, ≥0.10 µg/mL, ≥0.69 µg/mL and ≥0.12 µg/mL respectively. - * Study 8 was conducted in the United States and the territory of Puerto Rico (NCT04382326).
- † N = number of participants with valid assay results. These values are the denominators for the corresponding percentage calculations.
- ‡ Exact 2-sided CI, based on the Clopper and Pearson method.
- § Noninferiority for a serotype was met if the lower bound of the 2-sided CI for the percentage difference (Prevnar 20 minus Prevnar 13) >-10% (10% NI criterion) for that serotype.
- ¶ 2-Sided CI based on the Miettinen and Nurminen method for the difference in proportions, expressed as a percentage.
- # For the 7 additional serotypes, the percentage of participants with the predefined IgG concentration to serotype 23F (Prevnar 13 serotype with the lowest percentage, excluding serotype 3) in the Prevnar 13 group was used in the calculation of the percentage difference.
- Þ For the 7 additional serotypes, percentages of participants with predefined IgG concentrations to serotypes 8, 10A, 11A, 12F, 15B, 22F and 33F in the Prevnar 13 group were 1.6%, 1.2%, 1.5%, 0.1%, 2.6%, 0.9% and 1.1%, respectively.
Prevnar 20
N†=831-833
Prevnar 13
N†=801-802
Prevnar 20 minus Prevnar 13
% (95% CI‡)
% (95% CI‡)
Serotypes
1
79.8 (76.9, 82.5)
88.4 (86.0, 90.5)
-8.6 (-12.1, -5.1)
3
52.1 (48.6, 55.5)
67.6 (64.2, 70.8)
-15.5 (-20.1, -10.8)
4
79.7 (76.8, 82.4)
88.2 (85.7, 90.3)
-8.4 (-12.0, -4.9)
5
82.5 (79.7, 85.0)
86.8 (84.2, 89.1)
-4.3 (-7.8, -0.8)
6A
93.5 (91.6, 95.1)
95.9 (94.3, 97.2)
-2.4 (-4.6, -0.2)
6B
88.3 (85.9, 90.4)
92.4 (90.3, 94.1)
-4.1 (-7.0, -1.2)
7F
96.6 (95.2, 97.8)
97.6 (96.3, 98.6)
-1.0 (-2.7, 0.7)
9V
81.9 (79.1, 84.4)
89.8 (87.5, 91.8)
-7.9 (-11.3, -4.6)
14
93.4 (91.5, 95.0)
94.1 (92.3, 95.7)
-0.8 (-3.1, 1.6)
18C
92.6 (90.6, 94.2)
93.1 (91.2, 94.8)
-0.6 (-3.1, 1.9)
19A
97.1 (95.7, 98.1)
98.1 (96.9, 98.9)
-1.0 (-2.6, 0.5)
19F
96.9 (95.5, 98.0)
96.6 (95.1, 97.8)
0.2 (-1.5, 2.0)
23F
77.9 (74.9, 80.7)
85.5 (82.9, 87.9)
-7.6 (-11.4, -3.9)
Additional Serotypes#
8
96.8 (95.3, 97.9)
11.2 (8.6, 14.0)
10A
82.2 (79.5, 84.8)
-3.3 (-6.9, 0.3)
11A
92.7 (90.7, 94.4)
7.1 (4.2, 10.2)
12F
48.0 (44.6, 51.5)
-37.5 (-41.6, -33.3)
15B
98.2 (97.0, 99.0)
12.7 (10.2, 15.4)
22F
98.3 (97.2, 99.1)
12.8 (10.3, 15.5)
33F
86.7 (84.2, 88.9)
1.1 (-2.2, 4.5)
At 1 month after Dose 3, IgG GMCs in the Prevnar 20 group were noninferior to the corresponding IgG GMCs in the Prevnar 13 group for all 20 vaccine serotypes, including the 6 serotypes that missed the noninferiority criterion based on the percentage of participants meeting pre-defined IgG concentrations at one month after Dose 3. For each of the 13 matched serotypes, IgG GMCs in the Prevnar 20 group were noninferior to the corresponding IgG GMCs in the Prevnar 13 group. For each of the 7 additional serotypes, IgG GMCs in the Prevnar 20 group were noninferior to the IgG GMC for serotype 19A (the lowest result among the 13 matched vaccine serotypes excluding serotype 3) in the Prevnar 13 group (Table 10).
Table 10. Serotype-Specific Pneumococcal IgG GMCs (µg/mL) and GMC Ratios One Month After Dose 3 in Participants Vaccinated at 2, 4, 6 and 12 through 15 Months of Age – Study 8* Abbreviations: GMC = geometric mean concentration; IgG = immunoglobulin G; LLOQ = lower limit of quantitation. Note: Assay results below the LLOQ were set to 0.5 × LLOQ in the analysis. - * Study 8 was conducted in the United States and the territory of Puerto Rico (NCT04382326).
- † N = Number of participants with valid IgG concentrations.
- ‡ GMCs and 2-sided CIs were calculated by exponentiating the mean logarithm of the concentrations and the corresponding CIs (based on the Student t distribution).
- § Noninferiority for a serotype was met if the lower bound of the 2-sided CI of IgG GMC ratio (Prevnar 20/Prevnar 13) >0.5 (2-fold NI criterion) for that serotype.
- ¶ 2-Sided CIs were calculated by exponentiating the mean differences of the logarithms of the IgG concentrations (Prevnar 20 minus Prevnar 13) and the corresponding CIs (based on the Student t distribution).
- # For the 7 additional serotypes, the IgG GMC to serotype 19A (Prevnar 13 serotype with the lowest IgG GMC, excluding serotype 3) in the Prevnar 13 group was used in the calculation of the GMC ratio.
- Þ For the 7 additional serotypes, the IgG GMCs to serotypes 8, 10A, 11A, 12F, 15B, 22F and 33F in the Prevnar 13 group were 0.02 µg/mL, 0.01 µg/mL, 0.02 µg/mL, 0.01 µg/mL, 0.03 µg/mL, 0.01 µg/mL and 0.02 µg/mL, respectively.
Pneumococcal Serotype
Prevnar 20
N†=831-833
Prevnar 13
N†=801-802
Prevnar 20/Prevnar 13
Serotype
1
0.74 (0.70, 0.79)
1.14 (1.06, 1.22)
0.65 (0.59, 0.72)
3
0.36 (0.33, 0.38)
0.51 (0.48, 0.55)
0.70 (0.64, 0.76)
4
0.75 (0.70, 0.81)
1.08 (1.00, 1.17)
0.70 (0.63, 0.78)
5
0.66 (0.61, 0.71)
0.96 (0.88, 1.04)
0.69 (0.61, 0.77)
6A
1.95 (1.81, 2.10)
2.69 (2.48, 2.92)
0.72 (0.65, 0.81)
6B
0.61 (0.55, 0.68)
1.02 (0.91, 1.14)
0.60 (0.51, 0.70)
7F
1.71 (1.62, 1.81)
2.29 (2.16, 2.43)
0.75 (0.69, 0.81)
9V
0.87 (0.81, 0.93)
1.21 (1.12, 1.30)
0.72 (0.65, 0.80)
14
2.16 (2.01, 2.33)
2.72 (2.51, 2.95)
0.79 (0.71, 0.89)
18C
1.31 (1.23, 1.39)
1.71 (1.59, 1.84)
0.77 (0.70, 0.84)
19A
0.72 (0.67, 0.76)
0.91 (0.85, 0.97)
0.79 (0.72, 0.86)
19F
1.59 (1.50, 1.67)
2.00 (1.88, 2.12)
0.79 (0.73, 0.86)
23F
0.82 (0.75, 0.90)
1.25 (1.14, 1.37)
0.66 (0.58, 0.75)
Additional Serotypes#
8
1.80 (1.70, 1.91)
1.98 (1.81, 2.16)
10A
1.21 (1.09, 1.33)
1.32 (1.18, 1.49)
11A
1.39 (1.30, 1.48)
1.52 (1.39, 1.67)
12F
0.55 (0.50, 0.60)
0.60 (0.54, 0.67)
15B
4.40 (4.11, 4.71)
4.82 (4.39, 5.30)
22F
3.71 (3.45, 3.99)
4.06 (3.68, 4.48)
33F
1.49 (1.36, 1.64)
1.64 (1.46, 1.83)
Pneumococcal IgG Antibody Responses Following 4 Doses of Prevnar 20
For each of the 13 matched serotypes, IgG GMCs in the Prevnar 20 group were noninferior to the corresponding IgG GMCs in the Prevnar 13 group. For each of the 7 additional serotypes, IgG GMCs in the Prevnar 20 group were noninferior to the IgG GMC for serotype 1 (the lowest result among the 13 matched vaccine serotypes excluding serotype 3) in the Prevnar 13 group (Table 11).
Table 11. Serotype-Specific Pneumococcal IgG GMCs (µg/mL) and GMC Ratios One Month After Dose 4 in Participants Vaccinated at 2, 4, 6 and 12 through 15 Months of Age – Study 8* Prevnar 20
N†=753-755Prevnar 13
N†=744-745Prevnar 20/Prevnar 13 GMC‡ (95% CI‡) GMC‡ (95% CI‡) GMC Ratio§ (95% CI§¶) Abbreviations: GMC = geometric mean concentration; IgG = immunoglobulin G; LLOQ = lower limit of quantitation.
Note: Assay results below the LLOQ were set to 0.5 × LLOQ in the analysis.- * Study 8 was conducted in the United States and the territory of Puerto Rico (NCT04382326).
- † N = Number of participants with valid IgG concentrations.
- ‡ GMCs and 2-sided CIs were calculated by exponentiating the mean logarithm of the concentrations and the corresponding CIs (based on the Student t distribution).
- § Noninferiority for a serotype was met if the lower bound of the 2-sided CI of IgG GMC ratio (Prevnar 20/Prevnar 13) >0.5 (2-fold NI criterion) for that serotype.
- ¶ 2-Sided CIs were calculated by exponentiating the mean differences of the logarithms of the IgG concentrations (Prevnar 20 minus Prevnar 13) and the corresponding CIs (based on the Student t distribution).
- # For the 7 additional serotypes, the IgG GMC to serotype 1 (Prevnar 13 serotype with the lowest IgG GMC, excluding serotype 3) in the Prevnar 13 group was used in the calculation of the GMC ratio.
- Þ For the 7 additional serotypes, the IgG GMCs to serotypes 8, 10A, 11A, 12F, 15B, 22F and 33F in the Prevnar 13 group were 0.03 µg/mL, 0.01 µg/mL, 0.02 µg/mL, 0.01 µg/mL, 0.02 µg/mL, 0.00 µg/mL and 0.01 µg/mL, respectively.
Serotypes
1
1.47 (1.37, 1.57)
2.12 (1.97, 2.27)
0.69 (0.63, 0.76)
3
0.56 (0.53, 0.60)
0.85 (0.80, 0.90)
0.66 (0.61, 0.73)
4
3.77 (3.52, 4.04)
4.84 (4.50, 5.22)
0.78 (0.70, 0.86)
5
1.87 (1.74, 2.00)
2.51 (2.33, 2.70)
0.74 (0.67, 0.82)
6A
9.01 (8.45, 9.61)
11.69 (10.91, 12.53)
0.77 (0.70, 0.85)
6B
4.01 (3.70, 4.35)
5.74 (5.27, 6.24)
0.70 (0.62, 0.79)
7F
3.91 (3.70, 4.14)
5.18 (4.88, 5.49)
0.76 (0.70, 0.82)
9V
3.44 (3.23, 3.67)
4.30 (4.02, 4.59)
0.80 (0.73, 0.88)
14
5.68 (5.27, 6.12)
6.34 (5.88, 6.83)
0.90 (0.81, 1.00)
18C
3.46 (3.24, 3.70)
4.69 (4.34, 5.05)
0.74 (0.67, 0.82)
19A
3.53 (3.30, 3.77)
4.13 (3.84, 4.45)
0.85 (0.77, 0.94)
19F
5.01 (4.68, 5.36)
5.79 (5.36, 6.25)
0.86 (0.78, 0.96)
23F
3.95 (3.63, 4.31)
6.18 (5.66, 6.75)
0.64 (0.57, 0.72)
Additional Serotypes#
8
3.97 (3.73, 4.22)
1.87 (1.71, 2.06)
10A
6.22 (5.75, 6.72)
2.94 (2.64, 3.26)
11A
3.53 (3.31, 3.78)
1.67 (1.51, 1.84)
12F
1.85 (1.73, 1.99)
0.88 (0.79, 0.97)
15B
12.59 (11.78, 13.45)
5.95 (5.39, 6.55)
22F
10.60 (9.92, 11.33)
5.01 (4.54, 5.52)
33F
9.31 (8.71, 9.96)
4.40 (3.99, 4.85)
Opsonophagocytic Activity Responses After 3 and 4 doses of Prevnar 20
Serotype-specific OPA GMTs at 1 month after Dose 3 and 1 month after Dose 4 were descriptively evaluated in a subset of participants who had received Prevnar 20 and Prevnar 13 in Study 8 (Table 12). For serotypes 1, 3, 4, 9V, 23F and 12F, for which non-inferiority was not met 1 month after Dose 3 (for the percentage of participants meeting the pre-defined serotype-specific IgG concentration), OPA GMTs at 1 month after Dose 3 were numerically similar across groups for the 5 matched serotypes and an OPA antibody response was generated to additional serotype 12F.
Table 12. Pneumococcal OPA GMTs One Month After Dose 3 and Dose 4 of a 4-Dose Series– Study 8* Abbreviations: GMT = geometric mean titer; LLOQ = lower limit of quantitation; OPA = opsonophagocytic activity. Note: Assay results below the LLOQ were set to 0.5 × LLOQ in the analysis. Note: OPA titers were determined on serum from randomly selected subsets of participants assuring equal representation of both vaccine groups. - * Study 8 was conducted in the United States and the territory of Puerto Rico (NCT04382326).
- † N = Number of participants with valid OPA titers.
- ‡ GMTs and 2-sided CIs were calculated by exponentiating the mean logarithm of the titers and the corresponding CIs (based on the Student t distribution).
Prevnar 20
N† = 85-105
After Dose 3
Prevnar 13
N† = 84-113
After Dose 3
Prevnar 20
N† = 80-99
After Dose 4
Prevnar 13
N† = 77-103
After Dose 4
Serotypes
1
26 (21, 33)
34 (27, 42)
36 (27, 48)
66 (50, 87)
3
51 (43, 61)
63 (53, 76)
62 (49, 78)
102 (86, 120)
4
339 (252, 455)
280 (207, 378)
621 (435, 887)
961 (714, 1294)
5
32 (27, 39)
39 (32, 47)
55 (45, 67)
69 (54, 87)
6A
910 (763, 1084)
936 (757, 1156)
1384 (1092, 1753)
1767(1329, 2348)
6B
318 (242, 419)
516 (409, 651)
666 (489, 906)
1211 (861, 1703)
7F
1222 (1020, 1465)
1149 (926, 1424)
2022 (1673, 2444)
2099 (1741, 2531)
9V
661 (482, 906)
594 (421, 838)
2609 (1913, 3558)
3210 (2500, 4123)
14
415 (323, 535)
420 (330, 535)
667 (523, 850)
593 (462, 761)
18C
1153 (910, 1460)
996 (754, 1317)
1973 (1472, 2643)
2425 (1914, 3072)
19A
108 (78, 149)
109 (79, 151)
844 (622, 1145)
1357 (1007, 1829)
19F
84 (67, 105)
116 (90, 149)
246 (179, 337)
373 (272, 513)
23F
255 (186, 350)
295 (215, 406)
827 (554, 1235)
1532 (1118, 2100)
Additional Serotypes
8
665 (503, 880)
18 (17, 20)
1228 (901, 1673)
26 (21, 31)
10A
2558 (1869, 3501)
37 (33, 42)
3674 (2746, 4916)
57 (44, 74)
11A
289 (212, 395)
50 (46, 55)
2728 (1975, 3768)
69 (53, 89)
12F
7677 (5952, 9901)
28 (24, 33)
9320 (7037, 12343)
31 (26, 37)
15B
1560 (1090, 2233)
18 (16, 22)
3035 (2138, 4308)
23 (17, 30)
22F
6797 (5170, 8936)
9 (9, 9)
11077 (7956, 15422)
15 (11, 20)
33F
7388 (4803, 11365)
198 (177, 220)
19216 (13193, 27990)
363 (292, 451)
14.3 Prevnar 20 Clinical Trials in Individuals 18 Years of Age and Older
Immunogenicity of Prevnar 20 in Pneumococcal Vaccine Naïve Individuals
Prevnar 20 effectiveness in adults against invasive pneumococcal disease caused by the 20 vaccine serotypes and against pneumonia caused by the 13 serotypes in Prevnar 13 was demonstrated based on comparative immunogenicity to US-licensed pneumococcal vaccines (Prevnar 13 and PPSV23). Study 1, conducted in the United States and Sweden, was designed to evaluate immunologic noninferiority of Prevnar 20 to Prevnar 13 (for the 13 original S. pneumoniae serotypes) and PPSV23 (for the 7 new S. pneumoniae serotypes) in pneumococcal vaccine naive individuals ≥60 years of age. Antibody responses elicited by Prevnar 20 and the control pneumococcal vaccines were measured by serotype-specific serum OPA assays for the 20 pneumococcal serotypes at 1-month post-vaccination. OPA assays were used to measure functional antibodies to S. pneumoniae.
Study 1 included healthy individuals and immunocompetent individuals with stable underlying conditions, including chronic cardiovascular disease, chronic pulmonary disease, renal disorders, diabetes mellitus, chronic liver disease, and medical risk conditions and behaviors (e.g., smoking) that are known to increase the risk of serious pneumococcal pneumonia and IPD. A stable medical condition was defined as a medical condition not requiring significant change in therapy in the previous 6 weeks (i.e., change to new therapy category due to worsening disease) or any hospitalization for worsening disease within 12 weeks before receipt of the study vaccine.
Comparison of Immune Responses of Prevnar 20 to Prevnar 13 and PPSV23 in Pneumococcal Vaccine Naïve Individuals ≥60 Years of Age
In a randomized, active-controlled, double-blind noninferiority clinical trial (Study 1) of Prevnar 20 in the United States and Sweden, pneumococcal vaccine -naïve individuals 18 years of age and older were enrolled into 1 of 3 cohorts based on their age at enrollment and randomized to receive either Prevnar 20 or control. Participants 60 years of age and older were randomly assigned (1:1 ratio) to Prevnar 20 followed 1 month later with saline placebo or to Prevnar 13 followed 1 month later with PPSV23.
Serotype-specific OPA GMTs were measured before the first vaccination and 1 month after each vaccination. Noninferiority of immune responses, OPA GMTs 1 month after vaccination, with Prevnar 20 to a control vaccine for a serotype was declared if the lower bound of the 2 sided 95% CI for the GMT ratio (Prevnar 20/Prevnar 13; Prevnar 20/PPSV23) for that serotype was greater than 0.5.
In individuals 60 years of age and older, immune responses to all 13 matched serotypes elicited by Prevnar 20 were noninferior to the immune responses to the serotypes elicited by Prevnar 13 one month after vaccination. Immune responses to 6 out of the 7 additional serotypes induced by Prevnar 20 were noninferior to the immune responses to these same serotypes induced by PPSV23 one month after vaccination. The response to serotype 8 missed the prespecified statistical noninferiority criterion by a small margin (the lower bound of the 2-sided 95% CI for the GMT ratio being 0.49 versus >0.50) (Table 13).
In supportive analyses, 77.8% of participants in the Prevnar 20 group achieved a ≥4-fold rise in serotype 8 OPA titers from before vaccination to 1 month post-vaccination.
Table 13. OPA GMTs 1 Month After Vaccination in Participants 60 Years of Age and Older Given Prevnar 20 Compared to Prevnar 13 for the 13 Matched Serotypes and PPSV23 for the 7 Additional Serotypes (Study 1)*,†,‡,§ Abbreviations: CI = confidence interval; GMT = geometric mean titer; LLOQ = lower limit of quantitation; N = number of participants; OPA = opsonophagocytic activity; PPSV23 = pneumococcal polysaccharide vaccine (23-valent). - * Study 1 was conducted in the United States and in Sweden (NCT03760146).
- † Noninferiority for a serotype was met if the lower bound of the 2-sided 95% CI for the GMT ratio (ratio of Prevnar 20/comparator) was greater than 0.5 (2-fold criterion for noninferiority).
- ‡ Assay results below the LLOQ were set to 0.5 × LLOQ in the analysis.
- § Evaluable immunogenicity population.
- ¶ GMTs, GMT ratios, and the associated 2-sided CIs were based on analysis of log-transformed OPA titers using a regression model with vaccine group, sex, smoking status, age at vaccination in years, and baseline log-transformed OPA titers.
Prevnar 20
(N = 1157–1430)Prevnar 13
(N = 1390–1419)PPSV23
(N = 1201–1319)Vaccine Comparison
GMT¶
GMT¶
GMT¶
Serotype
1
123
154
0.80
(0.71, 0.90)3
41
48
0.85
(0.78, 0.93)4
509
627
0.81
(0.71, 0.93)5
92
110
0.83
(0.74, 0.94)6A
889
1165
0.76
(0.66, 0.88)6B
1115
1341
0.83
(0.73, 0.95)7F
969
1129
0.86
(0.77, 0.96)9V
1456
1568
0.93
(0.82, 1.05)14
747
747
1.00
(0.89, 1.13)18C
1253
1482
0.85
(0.74, 0.97)19A
518
645
0.80
(0.71, 0.90)19F
266
333
0.80
(0.70, 0.91)23F
277
335
0.83
(0.70, 0.97)Additional Serotypes
8
466
848
0.55
(0.49, 0.62)10A
2008
1080
1.86
(1.63, 2.12)11A
4427
2535
1.75
(1.52, 2.01)12F
2539
1717
1.48
(1.27, 1.72)15B
2398
769
3.12
(2.62, 3.71)22F
3666
1846
1.99
(1.70, 2.32)33F
5126
3721
1.38
(1.21, 1.57)Immunobridging in Pneumococcal Vaccine Naïve Individuals 18 Through 59 Years of Age
In Study 1 (described above), the effectiveness of Prevnar 20 in individuals 50 through 59 years of age and in individuals 18 through 49 years of age was inferred following comparison of the immune response to each of the 20 vaccine serotypes in each of these age groups to the corresponding serotype-specific immune responses in individuals 60 through 64 years of age following Prevnar 20 (immunobridging). In Study 1, pneumococcal vaccine-naïve participants 50 through 59 years of age and 18 through 49 years of age were randomly assigned (3:1 ratio) to receive 1 vaccination with Prevnar 20 or Prevnar 13. Serotype-specific OPA GMTs were measured before vaccination and 1 month after vaccination. A comparative analysis of Prevnar 20 in the younger age group versus Prevnar 20 in individuals 60 through 64 years of age for each vaccine serotype was performed to support the indication in individuals 18 through 49 years of age and 50 through 59 years of age. Immunobridging was to be declared successful if the lower bound of the 2-sided 95% CI for the GMT ratio (Prevnar 20 in participants 18 through 49 years of age/60 through 64 years of age and in participants 50 through 59 years of age/60 through 64 years of age) for the 20 serotypes was >0.5 (2-fold). Prevnar 20 elicited serotype-specific immune responses to each of the 20 vaccine serotypes in both of the younger age groups that were within 2-fold of the corresponding serotype-specific responses in individuals 60 through 64 years of age, when measured 1 month after vaccination (Table 14).
Table 14. Comparisons of OPA GMTs 1 Month After Prevnar 20 in Participants 18 Through 49 or 50 Through 59 Years of Age to Participants 60 Through 64 Years of Age (Study 1)*,†,‡,§ Abbreviations: CI = confidence interval; GMT = geometric mean titer; LLOQ = lower limit of quantitation; N = number of participants; OPA = opsonophagocytic activity; PPSV23 = pneumococcal polysaccharide vaccine 23-valent vaccine. - * Study 1 was conducted in the United States and in Sweden (NCT03760146).
- † Immunobridging for a serotype was met if the lower bound of the 2-sided 95% CI for the GMT ratio (ratio of younger age group/60 through 64 years of age group) was greater than 0.5 (2-fold success criterion).
- ‡ Assay results below the LLOQ were set to 0.5 × LLOQ in the analysis.
- § Evaluable immunogenicity population.
- ¶ GMTs, GMT ratios, and the associated 2-sided CIs were based on analysis of log-transformed OPA titers using a regression model with age group, sex, smoking status, and baseline log-transformed OPA titers. The comparisons between individuals 18 through 49 years of age and individuals 60 through 64 years of age and between individuals 50 through 59 years of age and individuals 60 through 64 years of age were based on separate regression models.
18–49 Years
(N = 251–317)60–64 Years
(N = 765–941)18–49 Years
Relative to 60–64 Years50–59 Years
(N = 266–320)60–64 Years
(N = 765–941)50–59 Years
Relative to 60–64 YearsGMT¶
GMT¶
GMT¶
GMT¶
Serotype
1
163
132
1.23
(1.01, 1.50)136
132
1.03
(0.84, 1.26)3
42
42
1.00
(0.87, 1.16)43
41
1.06
(0.92, 1.22)4
1967
594
3.31
(2.65, 4.13)633
578
1.10
(0.87, 1.38)5
108
97
1.11
(0.91, 1.36)85
97
0.88
(0.72, 1.07)6A
3931
1023
3.84
(3.06, 4.83)1204
997
1.21
(0.95, 1.53)6B
4260
1250
3.41
(2.73, 4.26)1503
1199
1.25
(1.00, 1.56)7F
1873
1187
1.58
(1.30, 1.91)1047
1173
0.89
(0.74, 1.07)9V
6041
1727
3.50
(2.83, 4.33)1726
1688
1.02
(0.83, 1.26)14
1848
773
2.39
(1.93, 2.96)926
742
1.25
(1.01, 1.54)18C
4460
1395
3.20
(2.53, 4.04)1805
1355
1.33
(1.06, 1.68)19A
1415
611
2.31
(1.91, 2.81)618
600
1.03
(0.85, 1.25)19F
655
301
2.17
(1.76, 2.68)287
290
0.99
(0.80, 1.22)23F
1559
325
4.80
(3.65, 6.32)549
328
1.68
(1.27, 2.22)Additional Serotypes
8
867
508
1.71
(1.38, 2.12)487
502
0.97
(0.78, 1.20)10A
4157
2570
1.62
(1.31, 2.00)2520
2437
1.03
(0.84, 1.28)11A
7169
5420
1.32
(1.04, 1.68)6417
5249
1.22
(0.96, 1.56)12F
5875
3075
1.91
(1.51, 2.41)3445
3105
1.11
(0.88, 1.39)15B
4601
3019
1.52
(1.13, 2.05)3356
2874
1.17
(0.88, 1.56)22F
7568
4482
1.69
(1.30, 2.20)3808
4228
0.90
(0.69, 1.17)33F
7977
5693
1.40
(1.10, 1.79)5571
5445
1.02
(0.81, 1.30)Immunogenicity of Prevnar 20 in Individuals Previously Vaccinated With Pneumococcal Vaccine
A randomized, open-label clinical trial (Study 6) described immune responses to Prevnar 20 in individuals 65 years of age and older previously vaccinated with PPSV23 (≥1 to ≤5 years prior to enrollment), previously vaccinated with Prevnar 13 (≥6 months prior to enrollment), or previously vaccinated with Prevnar 13 followed by PPSV23 (with PPSV23 vaccination ≥1 year prior to enrollment). Participants in this clinical trial previously vaccinated with Prevnar 13 (Prevnar 13 only or followed by PPSV23) were enrolled at sites in the United States and participants previously vaccinated with PPSV23 only were also enrolled from Swedish sites (35.5% in that category). Immune responses elicited by Prevnar 20 were measured by an OPA assay.
OPA GMTs in participants who received PPSV23 1 to 5 years prior to Prevnar 20 were diminished compared to OPA GMTs in participants who received Prevnar 13 at least 6 months previously and compared to OPA GMTs in participants who received Prevnar 13 followed by PPSV23, with the last PPSV23 dose given at least 1 year prior to Prevnar 20.
14.4 Concomitant Vaccine Administration
Individuals 6 Weeks Through 15 Months of Age
In Study 8, the concomitant administration of Pediarix and Hiberix with each of the 3 infant doses of either Prevnar 20 or Prevnar 13 were evaluated 1 month after the third dose. Concomitant administration of single doses of M-M-R II and VARIVAX with the fourth dose of either Prevnar 20 or Prevnar 13 were evaluated 1 month following vaccination. There was no evidence that Prevnar 20, as compared to Prevnar 13, interfered with the antibody responses to these concomitantly administered vaccines.
Individuals 65 Years of Age and Older
Clinical Trial in Individuals to Assess Prevnar 20 Given With Influenza Vaccine, Adjuvanted (Fluad Quadrivalent)
Study 7 was a double-blind, randomized study conducted in individuals 65 years of age and older who had no history of prior pneumococcal vaccination or who had previously received PPSV23 and/or Prevnar 13 at least 6 months prior to enrollment. Study participants were randomized in a 1:1 ratio to receive Prevnar 20 concomitantly administered with Fluad Quadrivalent followed approximately one month later by placebo (Group 1, N=898) or Fluad Quadrivalent concomitantly administered with placebo followed approximately one month later by Prevnar 20 (Group 2, N=898). Pneumococcal serotype-specific OPA GMTs were evaluated 1 month after Prevnar 20 and influenza vaccine strain hemagglutinin inhibition assay (HAI) GMTs were evaluated 1 month after Fluad Quadrivalent. The noninferiority criteria for the comparisons of OPA GMTs (lower limit of the 2- sided 95% CI of the GMT ratio [Group 1/Group 2] >0.5, 2-fold noninferiority criterion) were met for all 20 pneumococcal serotypes in Prevnar 20. The noninferiority criteria for the comparisons of HAI GMTs (lower limit of the 2- sided 95% CI for the GMT ratio [Group 1/Group 2] >0.67, 1.5-fold noninferiority criterion) were also met for all 4 influenza vaccine strains.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
Pre-filled Syringe, 1 Dose (10 per package) – NDC: 0005-2000-10.
Pre-filled Syringe, 1 Dose (1 per package) – NDC: 0005-2000-02.
After shipping, Prevnar 20 may arrive at temperatures between 2 ºC to 25 ºC (36 ºF to 77 ºF).
Upon receipt, store refrigerated at 2 ºC to 8 ºC (36 ºF to 46 ºF).
Syringes should be stored in the refrigerator horizontally to minimize the resuspension time.
Do not freeze. Discard if the vaccine has been frozen.
Prevnar 20 should be administered as soon as possible after being removed from refrigeration.
Prevnar 20 can be administered provided total (cumulative multiple excursions) time out of refrigeration (at temperatures between 8 °C and 25 °C) does not exceed 96 hours. Cumulative multiple excursions between 0 °C and 2 °C are also permitted as long as the total time between 0 °C and 2 °C does not exceed 72 hours. These are not, however, recommendations for storage.
The tip cap and plunger stopper of the pre-filled syringe are not made with natural rubber latex.
-
17 PATIENT COUNSELING INFORMATION
Prior to administration of this vaccine, inform the individual of the following:
- The potential benefits and risks of immunization with Prevnar 20 [see Warnings and Precautions (5), Adverse Reactions (6)].
- Any suspected adverse reactions should be reported to their healthcare professional.
-
SPL UNCLASSIFIED SECTION
This product's labeling may have been updated. For the most recent prescribing information, please visit www.pfizer.com.
US Govt. License No. 3
LAB-1436-3.0
CPT Code 90677
-
PRINCIPAL DISPLAY PANEL - 0.5 mL Syringe Label
NDC: 0005-2000-01
Rx onlyPneumococcal 20-valent
Conjugate Vaccine
Prevnar 20®One Dose (0.5 mL)
FOR IM USE ONLY
REFRIGERATE
DO NOT FREEZE
SHAKE WELLWyeth Pharm. LLC
US Govt. License No. 3PAA201729
LOT: XXXXXX
EXP: XXXXXX
-
PRINCIPAL DISPLAY PANEL - 0.5 mL Syringe Carton - 0005-2000-10
Pfizer
NDC: 0005-2000-10Pneumococcal 20-valent Conjugate Vaccine
PREVNAR 20®
FOR INTRAMUSCULAR USE ONLY
10 One-Dose (0.5 mL) Disposable Syringes
Rx only
-
PRINCIPAL DISPLAY PANEL - 0.5 mL Syringe Carton - 0005-2000-02
Pfizer
NDC: 0005-2000-02Pneumococcal 20-valent Conjugate Vaccine
PREVNAR 20®
FOR INTRAMUSCULAR USE ONLY
One-Dose (0.5 mL) Disposable Syringe
Rx only -
INGREDIENTS AND APPEARANCE
PREVNAR 20
pneumococcal 20-valent conjugate vaccine injection, suspensionProduct Information Product Type VACCINE Item Code (Source) NDC: 0005-2000 Route of Administration INTRAMUSCULAR Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength STREPTOCOCCUS PNEUMONIAE TYPE 1 CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN (UNII: 54EC0SE5PZ) (STREPTOCOCCUS PNEUMONIAE TYPE 1 CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN - UNII:54EC0SE5PZ) STREPTOCOCCUS PNEUMONIAE TYPE 1 CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN 2.2 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 3 CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN (UNII: 2VF3V7175U) (STREPTOCOCCUS PNEUMONIAE TYPE 3 CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN - UNII:2VF3V7175U) STREPTOCOCCUS PNEUMONIAE TYPE 3 CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN 2.2 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 4 CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN (UNII: TGJ6YZC4W7) (STREPTOCOCCUS PNEUMONIAE TYPE 4 CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN - UNII:TGJ6YZC4W7) STREPTOCOCCUS PNEUMONIAE TYPE 4 CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN 2.2 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 5 CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN (UNII: 5SKG37872O) (STREPTOCOCCUS PNEUMONIAE TYPE 5 CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN - UNII:5SKG37872O) STREPTOCOCCUS PNEUMONIAE TYPE 5 CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN 2.2 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 6A CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN (UNII: Z9HK08690W) (STREPTOCOCCUS PNEUMONIAE TYPE 6A CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN - UNII:Z9HK08690W) STREPTOCOCCUS PNEUMONIAE TYPE 6A CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN 2.2 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 6B CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN (UNII: 4M543JVT7G) (STREPTOCOCCUS PNEUMONIAE TYPE 6B CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN - UNII:4M543JVT7G) STREPTOCOCCUS PNEUMONIAE TYPE 6B CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN 4.4 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 7F CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN (UNII: 0K0S2P98ZJ) (STREPTOCOCCUS PNEUMONIAE TYPE 7F CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN - UNII:0K0S2P98ZJ) STREPTOCOCCUS PNEUMONIAE TYPE 7F CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN 2.2 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 8 CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN (UNII: ADR2S9OIF2) (STREPTOCOCCUS PNEUMONIAE TYPE 8 CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN - UNII:ADR2S9OIF2) STREPTOCOCCUS PNEUMONIAE TYPE 8 CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN 2.2 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 9V CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN (UNII: 5Q768OY0GI) (STREPTOCOCCUS PNEUMONIAE TYPE 9V CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN - UNII:5Q768OY0GI) STREPTOCOCCUS PNEUMONIAE TYPE 9V CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN 2.2 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 10A CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN (UNII: N47C1SHV0F) (STREPTOCOCCUS PNEUMONIAE TYPE 10A CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN - UNII:N47C1SHV0F) STREPTOCOCCUS PNEUMONIAE TYPE 10A CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN 2.2 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 11A CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN (UNII: RDA5AKV23D) (STREPTOCOCCUS PNEUMONIAE TYPE 11A CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN - UNII:RDA5AKV23D) STREPTOCOCCUS PNEUMONIAE TYPE 11A CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN 2.2 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 12F CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN (UNII: T6O227OX7Q) (STREPTOCOCCUS PNEUMONIAE TYPE 12F CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN - UNII:T6O227OX7Q) STREPTOCOCCUS PNEUMONIAE TYPE 12F CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN 2.2 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 14 CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN (UNII: SK54I0S386) (STREPTOCOCCUS PNEUMONIAE TYPE 14 CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN - UNII:SK54I0S386) STREPTOCOCCUS PNEUMONIAE TYPE 14 CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN 2.2 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 15B CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN (UNII: H8Q6FRO6DY) (STREPTOCOCCUS PNEUMONIAE TYPE 15B CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN - UNII:H8Q6FRO6DY) STREPTOCOCCUS PNEUMONIAE TYPE 15B CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN 2.2 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 18C CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN (UNII: XK87D9J012) (STREPTOCOCCUS PNEUMONIAE TYPE 18C CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN - UNII:XK87D9J012) STREPTOCOCCUS PNEUMONIAE TYPE 18C CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN 2.2 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 19A CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN (UNII: B970MQT365) (STREPTOCOCCUS PNEUMONIAE TYPE 19A CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN - UNII:B970MQT365) STREPTOCOCCUS PNEUMONIAE TYPE 19A CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN 2.2 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 19F CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN (UNII: 2E1M7F958B) (STREPTOCOCCUS PNEUMONIAE TYPE 19F CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN - UNII:2E1M7F958B) STREPTOCOCCUS PNEUMONIAE TYPE 19F CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN 2.2 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 22F CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN (UNII: U1E9VSB2K2) (STREPTOCOCCUS PNEUMONIAE TYPE 22F CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN - UNII:U1E9VSB2K2) STREPTOCOCCUS PNEUMONIAE TYPE 22F CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN 2.2 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 23F CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN (UNII: 25N8E57V6T) (STREPTOCOCCUS PNEUMONIAE TYPE 23F CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN - UNII:25N8E57V6T) STREPTOCOCCUS PNEUMONIAE TYPE 23F CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN 2.2 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 33F CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN (UNII: 9WP2BC3I04) (STREPTOCOCCUS PNEUMONIAE TYPE 33F CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN - UNII:9WP2BC3I04) STREPTOCOCCUS PNEUMONIAE TYPE 33F CAPSULAR POLYSACCHARIDE DIPHTHERIA CRM197 PROTEIN CONJUGATE ANTIGEN 2.2 ug in 0.5 mL Inactive Ingredients Ingredient Name Strength POLYSORBATE 80 (UNII: 6OZP39ZG8H) 100 ug in 0.5 mL ALUMINUM PHOSPHATE (UNII: F92V3S521O) 125 ug in 0.5 mL CORYNEBACTERIUM DIPHTHERIAE CRM197 PROTEIN (UNII: 08VC9WC084) 51 ug in 0.5 mL SUCCINATE DIANION (UNII: AJ326AG789) 295 ug in 0.5 mL SODIUM CHLORIDE (UNII: 451W47IQ8X) 4.4 mg in 0.5 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0005-2000-10 10 in 1 CARTON 1 NDC: 0005-2000-01 0.5 mL in 1 SYRINGE; Type 3: Prefilled Biologic Delivery Device/System (syringe, patch, etc.) 2 NDC: 0005-2000-02 1 in 1 CARTON 2 NDC: 0005-2000-01 0.5 mL in 1 SYRINGE; Type 3: Prefilled Biologic Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA125731 08/10/2021 Labeler - Wyeth Pharmaceutical Division of Wyeth Holdings LLC (054065909) Establishment Name Address ID/FEI Business Operations Pfizer Ireland Pharmaceuticals Unlimited Company 985586408 ANALYSIS(0005-2000) , MANUFACTURE(0005-2000) , API MANUFACTURE(0005-2000) , PACK(0005-2000) Establishment Name Address ID/FEI Business Operations Wyeth BioPharma Division of Wyeth Pharmaceuticals LLC 174350868 ANALYSIS(0005-2000) , API MANUFACTURE(0005-2000) Establishment Name Address ID/FEI Business Operations Wyeth Pharmaceutical Division of Wyeth Holdings LLC 883534067 ANALYSIS(0005-2000) , API MANUFACTURE(0005-2000) Establishment Name Address ID/FEI Business Operations Pfizer Manufacturing Belgium NV 370156507 PACK(0005-2000) , LABEL(0005-2000) , ANALYSIS(0005-2000) , MANUFACTURE(0005-2000) Establishment Name Address ID/FEI Business Operations Pfizer Inc 004954111 API MANUFACTURE(0005-2000) , ANALYSIS(0005-2000)
Trademark Results [Prevnar 20]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 PREVNAR 20 90458834 not registered Live/Pending |
Wyeth LLC 2021-01-11 |
 PREVNAR 20 88293753 not registered Live/Pending |
WYETH LLC 2019-02-08 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.