FLUPHENAZINE HYDROCHLORIDE- fluphenazine hydrochloride injection, solution
Fluphenazine Hydrochloride by
Drug Labeling and Warnings
Fluphenazine Hydrochloride by is a Prescription medication manufactured, distributed, or labeled by Fresenius Kabi USA, LLC. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
BOXED WARNING
(What is this?)
WARNING
Increased Mortality in Elderly Patients with Dementia-Related Psychosis –
Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Analyses of seventeen placebo-controlled trials (modal duration of 10 weeks), largely in patients taking atypical antipsychotic drugs, revealed a risk of death in drug-treated patients of between 1.6 to 1.7 times the risk of death in placebo-treated patients. Over the course of a typical 10-week controlled trial, the rate of death in drug-treated patients was about 4.5%, compared to a rate of about 2.6% in the placebo group. Although the causes of death were varied, most of the deaths appeared to be either cardiovascular (e.g., heart failure, sudden death) or infectious (e.g., pneumonia) in nature. Observational studies suggest that, similar to atypical, antipsychotic drugs, treatment with conventional antipsychotic drugs may increase mortality. The extent to which the findings of increased mortality in observational studies may be attributed to the antipsychotic drug as opposed to some characteristic(s) of the patients is not clear. Fluphenazine Hydrochloride Injection, USP is not approved for the treatment of patients with dementia-related psychosis (see WARNINGS).
-
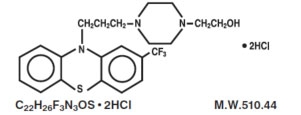
DESCRIPTION:
Fluphenazine Hydrochloride Injection, USP is a sterile, nonpyrogenic solution of fluphenazine hydrochloride in Water for Injection, for intramuscular use for the management of schizophrenia. Fluphenazine hydrochloride is a trifluoromethyl phenothiazine derivative and the chemical name is 1-Piperazineethanol, 4-[3-[2-(trifluoromethyl)-10H-phenothiazin-10-yl] propyl]-,dihydrochloride and has the following structural formula:
Each mL contains: Fluphenazine hydrochloride 2.5 mg; sodium chloride 9 mg to render the solution isotonic; methylparaben 1 mg and propylparaben 0.1 mg as preservatives; Water for Injection q.s. Hydrochloric acid and/or sodium hydroxide may have been added for pH adjustment (4.8 to 5.2).
- CLINICAL PHARMACOLOGY:
- INDICATIONS AND USAGE:
-
CONTRAINDICATIONS:
Phenothiazines are contraindicated in patients with suspected or established subcortical brain damage, in patients receiving large doses of hypnotics and in comatose or severely depressed states. The presence of blood dyscrasia or liver damage precludes the use of fluphenazine hydrochloride. Fluphenazine hydrochloride is contraindicated in patients who have shown hypersensitivity to fluphenazine; cross-sensitivity to phenothiazine derivatives may occur.
-
WARNINGS:
Increased Mortality in Elderly Patients with Dementia-Related Psychosis
Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Fluphenazine Hydrochloride Injection, USP is not approved for the treatment of patients with dementia-related psychosis (see BOXED WARNING).
Tardive Dyskinesia
Tardive dyskinesia, a syndrome consisting of potentially irreversible, involuntary, dyskinetic movements may develop in patients treated with neuroleptic (antipsychotic) drugs. Although the prevalence of the syndrome appears to be highest among the elderly, especially elderly women, it is impossible to rely upon prevalence estimates to predict, at the inception of neuroleptic treatment, which patients are likely to develop the syndrome. Whether neuroleptic drug products differ in their potential to cause tardive dyskinesia is unknown.
Both the risk of developing the syndrome and the likelihood that it will become irreversible are believed to increase as the duration of treatment and the total cumulative dose of neuroleptic drugs administered to the patient increase. However, the syndrome can develop, although much less commonly, after relatively brief treatment periods at low doses.
There is no known treatment for established cases of tardive dyskinesia, although the syndrome may remit, partially or completely, if neuroleptic treatment is withdrawn. Neuroleptic treatment, itself, however, may suppress (or partially suppress) the signs and symptoms of the syndrome and thereby may possibly mask the underlying disease process. The effect that symptomatic suppression has upon the long-term course of the syndrome is unknown.
Given these considerations, neuroleptics should be prescribed in a manner that is most likely to minimize the occurrence of tardive dyskinesia. Chronic neuroleptic treatment should generally be reserved for patients who suffer from a chronic illness that 1) is known to respond to neuroleptic drugs and 2) for whom alternative, equally effective, but potentially less harmful treatments are not available or appropriate. In patients who do require chronic treatment, the smallest dose and the shortest duration of treatment producing a satisfactory clinical response should be sought. The need for continued treatment should be reassessed periodically.
If signs and symptoms of tardive dyskinesia appear in a patient on neuroleptics, drug discontinuation should be considered. However, some patients may require treatment despite the presence of the syndrome.
(For further information about the description of tardive dyskinesia and its clinical detection, please refer to the sections on PRECAUTIONS, Information for Patients and ADVERSE REACTIONS, Tardive Dyskinesia).
The use of this drug may impair the mental and physical abilities required for driving a car or operating heavy machinery.
Potentiation of the effects of alcohol may occur with the use of this drug.
Since there is no adequate experience in children who have received this drug, safety and efficacy in children have not been established.
Neuroleptic Malignant Syndrome (NMS)
A potentially fatal symptom complex sometimes referred to as Neuroleptic Malignant Syndrome (NMS) has been reported in association with antipsychotic drugs. Clinical manifestations of NMS are hyperpyrexia, muscle rigidity, altered mental status and evidence of autonomic instability (irregular pulse or blood pressure, tachycardia, diaphoresis and cardiac dysrhythmias).
The diagnostic evaluation of patients with this syndrome is complicated. In arriving at a diagnosis, it is important to identify cases where the clinical presentation includes both serious medical illness (e.g., pneumonia, systemic infection, etc.) and untreated or inadequately treated extrapyramidal signs and symptoms (EPS). Other important considerations in the differential diagnosis include central anticholinergic toxicity, heat stroke, drug fever and primary central nervous system (CNS) pathology.
The management of NMS should include 1) immediate discontinuation of antipsychotic drugs and other drugs not essential to concurrent therapy, 2) intensive symptomatic treatment and medical monitoring and 3) treatment of any concomitant serious medical problems for which specific treatments are available. There is no general agreement about specific pharmacological treatment regimens for uncomplicated NMS.
If a patient requires antipsychotic drug treatment after recovery from NMS, the potential reintroduction of drug therapy should be carefully considered. The patient should be carefully monitored, since recurrences of NMS have been reported.
Falls
Fluphenazine Hydrochloride Injection, USP may cause somnolence, postural hypotension, motor and sensory instability, which may lead to falls and, consequently, fractures or other injuries. For patients with diseases, conditions, or medications that could exacerbate these effects, complete fall risk assessments when initiating antipsychotic treatment and recurrently for patients on long-term antipsychotic therapy.
-
PRECAUTIONS:
General
Because of the possibility of cross-sensitivity, fluphenazine hydrochloride should be used cautiously in patients who have developed cholestatic jaundice, dermatoses or other allergic reactions to phenothiazine derivatives.
Psychotic patients on large doses of a phenothiazine drug who are undergoing surgery should be watched carefully for possible hypotensive phenomena. Moreover, it should be remembered that reduced amounts of anesthetics or CNS depressants may be necessary.
The effects of atropine may be potentiated in some patients receiving fluphenazine because of added anticholinergic effects.
Fluphenazine hydrochloride should be used cautiously in patients exposed to extreme heat or phosphorus insecticides; in patients with a history of convulsive disorders, since grand mal convulsions have been known to occur and in patients with special medical disorders, such as mitral insufficiency or other cardiovascular diseases and pheochromocytoma.
The possibility of liver damage, pigmentary retinopathy, lenticular and corneal deposits and development of irreversible dyskinesia should be remembered when patients are on prolonged therapy.
Neuroleptic drugs elevate prolactin levels; the elevation persists during chronic administration. Tissue culture experiments indicate that approximately one-third of human breast cancers are prolactin dependent in vitro, a factor of potential importance if the prescription of these drugs is contemplated in a patient with a previously detected breast cancer. Although disturbances such as galactorrhea, amenorrhea, gynecomastia and impotence have been reported, the clinical significance of elevated serum prolactin levels is unknown for most patients. An increase in mammary neoplasms has been found in rodents after chronic administration of neuroleptic drugs. Neither clinical studies nor epidemiologic studies conducted to date, however, have shown an association between chronic administration of these drugs and mammary tumorigenesis; the available evidence is considered too limited to be conclusive at this time.
Information for Patients
Given the likelihood that some patients exposed chronically to neuroleptics will develop tardive dyskinesia, it is advised that all patients in whom chronic use is contemplated be given, if possible, full information about this risk. The decision to inform patients and/or their guardians must obviously take into account the clinical circumstances and the competency of the patient to understand the information provided.
Pregnancy
Non-teratogenic Effects
Neonates exposed to antipsychotic drugs, during the third trimester of pregnancy are at risk for extrapyramidal and/or withdrawal symptoms following delivery. There have been reports of agitation, hypertonia, hypotonia, tremor, somnolence, respiratory distress and feeding disorder in these neonates. These complications have varied in severity; while in some cases symptoms have been self-limited, in other cases neonates have required intensive care unit support and prolonged hospitalization.
Fluphenazine Hydrochloride should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Leukopenia, Neutropenia and Agranulocytosis
In clinical trial and postmarketing experience, events of leukopenia/neutropenia and agranulocytosis have been reported temporally related to antipsychotic agents.
Possible risk factors for leukopenia/neutropenia include pre-existing low white blood cell count (WBC) and history of drug induced leukopenia/neutropenia. Patients with a pre-existing low WBC or a history of drug induced leukopenia/neutropenia should have their complete blood count (CBC) monitored frequently during the first few months of therapy and should discontinue Fluphenazine Hydrochloride Injection, USP at the first sign of a decline in WBC in the absence of other causative factors.
Patients with neutropenia should be carefully monitored for fever or other symptoms or signs of infection and treated promptly if such symptoms or signs occur. Patients with severe neutropenia (absolute neutrophil count <1000 mm 3) should discontinue Fluphenazine Hydrochloride Injection, USP and have their WBC followed until recovery.
Abrupt Withdrawal
In general, phenothiazines do not produce psychic dependence; however, gastritis, nausea and vomiting, dizziness and tremulousness have been reported following abrupt cessation of high dose therapy. Reports suggest that these symptoms can be reduced if concomitant antiparkinsonian agents are continued for several weeks after the phenothiazine is withdrawn.
Facilities should be available for periodic checking of hepatic function, renal function and the blood picture. Renal function of patients on long-term therapy should be monitored; if blood urea nitrogen (BUN) becomes abnormal, treatment should be discontinued.
As with any phenothiazine, the physician should be alert to the possible development of ‘‘silent pneumonias’’ in patients under treatment with fluphenazine hydrochloride.
-
ADVERSE REACTIONS:
Central Nervous System
The side effects most frequently reported with phenothiazine compounds are extrapyramidal symptoms including pseudoparkinsonism, dystonia, dyskinesia, akathisia, oculogyric crises, opisthotonos and hyperreflexia. Most often these extrapyramidal symptoms are reversible; however, they may be persistent (see below). With any given phenothiazine derivative, the incidence and severity of such reactions depend more on individual patient sensitivity than on other factors, but dosage level and patient age are also determinants.
Extrapyramidal reactions may be alarming, and the patient should be forewarned and reassured. These reactions can usually be controlled by administration of antiparkinsonian drugs such as Benztropine Mesylate or Intravenous Caffeine and Sodium Benzoate Injection, and by subsequent reductions in dosage.
Dystonia
Class effect: Symptoms of dystonia, prolonged abnormal contractions of muscle groups, may occur in susceptible individuals during the first few days of treatment. Dystonic symptoms include: spasm of the neck muscles, sometimes progressing to tightness of the throat, swallowing difficulty, difficulty breathing, and/or protrusion of the tongue. While these symptoms can occur at low doses, they occur more frequently and with greater severity with high potency and at higher doses of first generation antipsychotic drugs. An elevated risk of acute dystonia is observed in males and younger age groups.
Tardive Dyskinesia
See WARNINGS. The syndrome is characterized by involuntary choreoathetoid movements which variously involve the tongue, face, mouth, lips or jaw (e.g., protrusion of the tongue, puffing of cheeks, puckering of the mouth, chewing movements), trunk and extremities. The severity of the syndrome and the degree of impairment produced vary widely.
The syndrome may become clinically recognizable either during treatment, upon dosage reduction, or upon withdrawal of treatment. Early detection of tardive dyskinesia is important. To increase the likelihood of detecting the syndrome at the earliest possible time, the dosage of the neuroleptic drug should be reduced periodically (if clinically possible) and the patient observed for signs of the disorder. This maneuver is critical, since neuroleptic drugs may mask the signs of the syndrome.
Other Central Nervous System Effects
Occurrences of neuroleptic malignant syndrome (NMS) have been reported in patients on neuroleptic therapy (see WARNINGS, Neuroleptic Malignant Syndrome); leukocytosis, elevated CPK, liver function abnormalities and acute renal failure may also occur with NMS.
Drowsiness or lethargy, if they occur, may necessitate a reduction in dosage; the induction of a catatonic-like state has been known to occur with dosages of fluphenazine far in excess of the recommended amounts. As with other phenothiazine compounds, reactivation or aggravation of psychotic processes may be encountered.
Phenothiazine derivatives have been known to cause, in some patients, restlessness, excitement or bizarre dreams.
Autonomic Nervous System
Hypertension and fluctuation in blood pressure have been reported with fluphenazine hydrochloride.
Hypotension has rarely presented a problem with fluphenazine. However, patients with pheochromocytoma, cerebral vascular or renal insufficiency or a severe cardiac reserve deficiency such as mitral insufficiency appear to be particularly prone to hypotensive reactions with phenothiazine compounds, and should therefore be observed closely when the drug is administered. If severe hypotension should occur, supportive measures including the use of intravenous vasopressor drugs should be instituted immediately. Norepinephrine Bitartrate Injection is the most suitable drug for this purpose; epinephrine should not be used since phenothiazine derivatives have been found to reverse its action, resulting in a further lowering of blood pressure.
Autonomic reactions including nausea and loss of appetite, salivation, polyuria, perspiration, dry mouth, headache and constipation may occur. Autonomic effects can usually be controlled by reducing or temporarily discontinuing dosage.
In some patients, phenothiazine derivatives have caused blurred vision, glaucoma, bladder paralysis, fecal impaction, paralytic ileus, tachycardia or nasal congestion.
Metabolic and Endocrine
Weight change, peripheral edema, abnormal lactation, gynecomastia, menstrual irregularities, false results on pregnancy tests, impotency in men and increased libido in women have all been known to occur in some patients on phenothiazine therapy.
Allergic Reactions
Skin disorders such as itching, erythema, urticaria, seborrhea, photosensitivity, eczema and even exfoliative dermatitis have been reported with phenothiazine derivatives. The possibility of anaphylactoid reactions occurring in some patients should be borne in mind.
Hematologic
Routine blood counts are advisable during therapy since blood dyscrasias including leukopenia, agranulocytosis, thrombocytopenic or nonthrombocytopenic purpura, eosinophilia and pancytopenia have been observed with phenothiazine derivatives. Furthermore, if any soreness of the mouth, gums or throat, or any symptoms of upper respiratory infection occur and confirmatory leukocyte count indicates cellular depression, therapy should be discontinued and other appropriate measures instituted immediately.
Hepatic
Liver damage as manifested by cholestatic jaundice may be encountered, particularly during the first months of therapy; treatment should be discontinued if this occurs. An increase in cephalin flocculation, sometimes accompanied by alterations in other liver function tests, have been reported in patients receiving fluphenazine hydrochloride who have had no clinical evidence of liver damage.
Others
Sudden, unexpected and unexplained deaths have been reported in hospitalized psychotic patients receiving phenothiazines. Previous brain damage or seizures may be predisposing factors; high doses should be avoided in known seizure patients. Several patients have shown sudden flare-ups of psychotic behavior patterns shortly before death. Autopsy findings have usually revealed acute fulminating pneumonia or pneumonitis, aspiration of gastric contents or intramyocardial lesions.
Although this is not a general feature of fluphenazine, potentiation of CNS depressants (opiates, analgesics, antihistamines, barbiturates, alcohol) may occur.
The following adverse reactions have also occurred with phenothiazine derivatives; systemic lupus erythematosus-like syndrome; hypotension severe enough to cause fatal cardiac arrest; altered electrocardiographic and electroencephalographic tracings; altered cerebrospinal fluid proteins; cerebral edema; asthma, laryngeal edema and angioneurotic edema; with long-term use—skin pigmentation and lenticular and corneal opacities.
-
DOSAGE AND ADMINISTRATION
The average well tolerated starting dose for adult psychotic patients is 1.25 mg (0.5 mL) intramuscularly. Depending on the severity and duration of symptoms, initial total daily dosage may range from 2.5 to 10 mg and should be divided and given at six to eight hour intervals.
The smallest amount that will produce the desired results must be carefully determined for each individual, since optimal dosage levels of this potent drug vary from patient to patient. In general, the parenteral dose for fluphenazine has been found to be approximately 1/3 to 1/2 the oral dose. Treatment may be instituted with a low initial dosage, which may be increased, if necessary, until the desired clinical effects are achieved. Dosages exceeding 10 mg daily should be used with caution.
When symptoms are controlled, oral maintenance therapy can generally be instituted often with single daily doses. Continued treatment by the oral route, if possible, is needed to achieve maximum therapeutic benefits; further adjustments in dosage may be necessary during the course of therapy to meet the patient’s requirements.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
-
HOW SUPPLIED:
Product
No.
NDC
No.
28110
63323-281-10
Fluphenazine Hydrochloride Injection, USP 25 mg per 10 mL (2.5 mg per mL) flip-top vial packaged individually.
Solutions should be protected from exposure to light. Parenteral solutions may vary in color from essentially colorless to light amber. If a solution has become any darker than light amber or is discolored in any other way, it should not be used.
Store at 20° to 25°C (68° to 77°F) [see USP Controlled Room Temperature].
PROTECT FROM LIGHT.
The container closure is not made with natural rubber latex.
- SPL UNCLASSIFIED SECTION
-
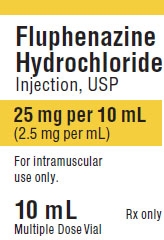
PRINCIPAL DISPLAY PANEL
PACKAGE LABEL - PRINCIPAL DISPLAY - Fluphenazine 10 mL Vial Label
Fluphenazine Hydrochloride Injection, USP
25 mg per 10 mL (2.5 mg per mL)For intramuscular use only.
10 mL Multiple Dose VialRx only
PACKAGE LABEL - PRINCIPAL DISPLAY - Fluphenazine 10 mL Vial Carton Panel
Fluphenazine Hydrochloride Injection, USP
25 mg per 10 mL (2.5 mg per mL )For intramuscular use only.
10 mL Multiple Dose VialRx only
-
INGREDIENTS AND APPEARANCE
FLUPHENAZINE HYDROCHLORIDE
fluphenazine hydrochloride injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 63323-281 Route of Administration INTRAMUSCULAR Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength FLUPHENAZINE HYDROCHLORIDE (UNII: ZOU145W1XL) (FLUPHENAZINE - UNII:S79426A41Z) FLUPHENAZINE HYDROCHLORIDE 2.5 mg in 1 mL Inactive Ingredients Ingredient Name Strength SODIUM CHLORIDE (UNII: 451W47IQ8X) 9 mg in 1 mL METHYLPARABEN (UNII: A2I8C7HI9T) 1 mg in 1 mL PROPYLPARABEN (UNII: Z8IX2SC1OH) 0.1 mg in 1 mL HYDROCHLORIC ACID (UNII: QTT17582CB) SODIUM HYDROXIDE (UNII: 55X04QC32I) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 63323-281-10 1 in 1 BOX 12/28/2010 1 10 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA089556 12/28/2010 Labeler - Fresenius Kabi USA, LLC (608775388) Establishment Name Address ID/FEI Business Operations Fresenius Kabi USA, LLC 023648251 manufacture(63323-281)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.
