MORPHINE SULFATE solution
Morphine Sulfate by
Drug Labeling and Warnings
Morphine Sulfate by is a Prescription medication manufactured, distributed, or labeled by Safecor Health, LLC, MALLINCKRODT INC, MALLINCKRODT, INC.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use Morphine Sulfate Oral Solution safely and effectively. See full prescribing information for Morphine Sulfate Oral Solution.
Morphine Sulfate Oral Solution, CII
Initial U.S. Approval: 1941
WARNING: RISK OF MEDICATION ERRORS
See full prescribing information for complete boxed warning
Morphine sulfate oral solution is available in the 100 mg per 5 mL
(20 mg/mL) concentration and is indicated
for use in opioid-tolerant patients only.
Take care to avoid dosing errors due to confusion between
between different concentrations and between mg and mL, which
could result in accidental overdose and death. (5.1)
Keep morphine sulfate oral solution out of the reach of children.INDICATIONS AND USAGE
- Morphine sulfate is an opioid agonist indicated for the relief of moderate to severe acute and chronic pain where an opioid analgesic is appropriate. (1)
- Morphine sulfate oral solution 100 mg per 5 mL (20 mg/mL) is indicated for the relief of moderate to severe acute and chronic pain in opioid-tolerant patients. (1)
DOSAGE AND ADMINISTRATION
- Morphine sulfate oral solution: 10 to 20 mg every 4 hours as needed. (2.2)
DOSAGE FORMS AND STRENGTHS
- Morphine sulfate oral solution: For the 100 mg per 5 mL (20 mg/mL) strength, each mL contains 20 mg of morphine sulfate. (3)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- Risk of Medication Errors: Use caution when prescribing, dispensing, and administering to avoid dosing errors due to confusion between different concentrations and between mg and mL, which could result in accidental overdose and death. (5.1)
- Respiratory depression: Increased risk in elderly, debilitated patients, those suffering from conditions accompanied by hypoxia, hypercapnia, or upper airway obstruction. (5.2)
- Controlled substance: Morphine sulfate is a Schedule II controlled substance with an abuse liability similar to other opioids. (5.3)
- CNS effects: Additive CNS depressive effects when used in conjunction with alcohol, other opioids, or illicit drugs. (5.4)
- Elevation of intracranial pressure: May be markedly exaggerated in the presence of head injury, other intracranial lesions. (5.5)
- Hypotensive effect: Increased risk with compromised ability to maintain blood pressure. (5.6)
- Prolonged gastric obstruction: In patients with gastrointestinal obstruction, especially paralytic ileus. (5.7)
- Sphincter of Oddi spasm and diminished biliary/pancreatic secretions. Increased risk with biliary tract disease. (5.8)
- Special Risk Groups: Use with caution and in reduced dosages in patients with severe renal or hepatic impairment, Addison’s disease, hypothyroidism, prostatic hypertrophy, or urethral stricture, elderly, CNS depression, toxic psychosis, acute alcoholism and delirium tremens, may aggravate or induce seizures. (5.9)
- Impaired mental/physical abilities: Caution must be used with potentially hazardous activities. (5.10)
ADVERSE REACTIONS
- Most common adverse reactions seen on initiation of therapy are: constipation, nausea, somnolence, lightheadedness, dizziness, sedation, vomiting, and sweating. (6)
To report SUSPECTED ADVERSE REACTIONS, contact Mallinckrodt at 1-800-778-7898 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch
DRUG INTERACTIONS
- CNS depressants: Increased risk of respiratory depression, hypotension, profound sedation, or coma. Use with caution in reduced dosages. (7.1)
- Muscle relaxants: Enhance the neuromuscular blocking action of skeletal muscle relaxants and produce an increased degree of respiratory depression. (7.2)
- Mixed agonist/antagonist opioid analgesics (i.e. pentazocine, nalbuphine, and butorphanol): May reduce the analgesic effect and/or may precipitate withdrawal symptoms. (7.3)
- Cimetidine: Precipitates apnea, confusion and muscle twitching. (7.4)
- Monoamine oxidase inhibitors (MAOIs): Potentiate the action of morphine sulfate. Morphine sulfate should not be used in patients taking MAOIs or within 14 days of stopping such treatment. (7.5)
USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 1/2013
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: RISK OF MEDICATION ERRORS
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Individualization of Dosage
2.2 Initiation of Therapy in Opioid-Naïve Patients
2.3 Conversion to Oral Morphine Sulfate
2.4 Maintenance of Therapy
2.5 Cessation of Therapy
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Risk of Medication Errors
5.2 Respiratory Depression
5.3 Misuse, Abuse and Diversion of Opioids
5.4 Interactions with Alcohol and Drugs of Abuse
5.5 Use in Head Injury and Increased Intracranial Pressure
5.6 Hypotensive Effects
5.7 Gastrointestinal Effects
5.8 Use in Pancreatic/Biliary Tract Disease
5.9 Special Risk Groups
5.10 Driving and Operating Machinery
6 ADVERSE REACTIONS
7 DRUG INTERACTIONS
7.1 CNS Depressants
7.2 Muscle Relaxants
7.3 Mixed Agonist/Antagonist Opioid Analgesics
7.4 Cimetidine
7.5 Monoamine Oxidase Inhibitors (MAOIs)
7.6 Anticholinergics
7.7 P-Glycoprotein (PGP) Inhibitors
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Labor and Delivery
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Neonatal Withdrawal Syndrome
8.7 Gender
8.8 Hepatic Impairment
8.9 Renal Impairment
9 DRUG ABUSE AND DEPENDENCE
9.1 Controlled Substance
9.2 Abuse
9.3 Dependence
10 OVERDOSAGE
10.1 Symptoms
10.2 Treatment
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
16 HOW SUPPLIED/STORAGE AND HANDLING
Information for Patients and Caregivers
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: RISK OF MEDICATION ERRORS
Morphine sulfate oral solution is available in the 100 mg per 5 mL
(20 mg/mL) concentration and is indicated for use in opioid-tolerant patients only.
Take care when prescribing and administering morphine sulfate oral solution to avoid dosing errors due to confusion between different concentrations and between mg and mL, which could result in accidental overdose and death. Take care to ensure the proper dose is communicated and dispensed.
Keep morphine sulfate oral solution out of the reach of children. In case of accidental ingestion, seek emergency medical help immediately. -
1 INDICATIONS AND USAGE
Morphine sulfate oral solution 100 mg per 5 mL (20 mg/mL) is an opioid analgesic indicated for the relief of moderate to severe acute and chronic pain in opioid-tolerant patients.
Morphine sulfate oral solution 100 mg per 5 mL (20 mg/mL) may cause fatal respiratory depression when administered to patients not previously exposed to opioids. Patients considered to be opioid tolerant are those who are taking at least 60 mg oral morphine per day, or at least 30 mg of oral oxycodone per day, or at least 12 mg hydromorphone per day, or an equianalgesic dose of another opioid, for a week or longer. -
2 DOSAGE AND ADMINISTRATION
Morphine sulfate oral solution is available in one concentration: 100 mg per 5 mL (20 mg/mL).
Take care when prescribing and administering morphine sulfate oral solution to avoid dosing errors due to confusion between different concentrations and between mg and mL, which could result in accidental overdose and death. Take care to ensure the proper dose is communicated and dispensed. When writing prescriptions, include both the total dose in mg and the total dose in volume. Always use the enclosed calibrated oral syringe when administering morphine sulfate oral solution 100 mg per 5 mL
(20 mg/mL) to ensure the dose is measured and administered accurately.Selection of patients for treatment with morphine sulfate should be governed by the same principles that apply to the use of similar opioid analgesics. Individualize treatment in every case, using non-opioid analgesics, opioids on an as needed basis and/or combination products, and chronic opioid therapy in a progressive plan of pain management such as outlined by the World Health Organization, the Agency for Healthcare Research and Quality, and the American Pain Society.
2.1 Individualization of Dosage
As with any opioid drug product, adjust the dosing regimen for each patient individually, taking into account the patient’s prior analgesic treatment experience. In the selection of the initial dose of morphine sulfate, give attention to the following:
- the total daily dose, potency and specific characteristics of the opioid the patient has been taking previously;
- the reliability of the relative potency estimate used to calculate the equivalent morphine sulfate dose needed;
- the patient’s degree of opioid tolerance;
- the general condition and medical status of the patient;
- concurrent medications;
- the type and severity of the patient’s pain;
- risk factors for abuse, addiction or diversion, including a prior history of abuse, addiction or diversion.
The following dosing recommendations, therefore, can only be considered suggested approaches to what is actually a series of clinical decisions over time in the management of the pain of each individual patient.
Continual reevaluation of the patient receiving morphine sulfate is important, with special attention to the maintenance of pain control and the relative incidence of side effects associated with therapy. During chronic therapy, especially for non-cancer-related pain, periodically reassess the continued need for the use of opioid analgesics.
During periods of changing analgesic requirements, including initial titration, frequent contact is recommended between physician, other members of the healthcare team, the patient, and the caregiver/family.2.2 Initiation of Therapy in Opioid-Naïve Patients
Start patients who have not been receiving opioid analgesics on morphine sulfate in the following dosing range using morphine sulfate oral solution,
10 mg per 5 mL or 20 mg per 5 mL strengths:
Morphine sulfate oral solution: 10 to 20 mg every 4 hours as needed for pain.
Titrate the dose based upon the individual patient’s response to their initial dose of morphine sulfate. Adjust the dose to an acceptable level of analgesia taking into account the improvement in pain intensity and the tolerability of the morphine by the patient.
The 100 mg per 5 mL (20 mg/mL) oral solution formulation is for use in opioid-tolerant patients only who have already been receiving opioid therapy. Use this strength only for patients that have already been titrated to a stable analgesic regimen using lower strengths of morphine sulfate and who can benefit from use of a smaller volume of oral solution.2.3 Conversion to Oral Morphine Sulfate
There is inter-patient variability in the potency of opioid drugs and opioid formulations. Therefore, a conservative approach is advised when determining the total daily dose of morphine sulfate. It is better to underestimate a patient’s 24-hour oral morphine sulfate dose and make available rescue medication than to overestimate the 24-hour oral morphine sulfate dose and manage an adverse experience of overdose.
Consider the following general points regarding opioid conversions.
Conversion from Parenteral Morphine to Oral Morphine Sulfate
For conversion from parenteral to oral morphine sulfate, anywhere from 3 to 6 mg of oral morphine sulfate may be required to provide pain relief equivalent to 1 mg of parenteral morphine.Conversion from Parenteral Oral Non-Morphine Opioids to Oral Morphine Sulfate
In converting patients from other opioids to morphine sulfate, close observation and adjustment of dosage based upon the patient’s response to morphine sulfate is imperative. Physicians and other healthcare professionals are advised to refer to published relative potency information, keeping in mind that conversion ratios are only approximate.Conversion from Controlled-Release Oral Morphine to Oral Morphine Sulfate
For a given dose, the same total amount of morphine sulfate is available from morphine sulfate oral solution, morphine sulfate tablets, and controlled-release and extended-release morphine capsules. The extended duration of release of morphine sulfate from controlled-release tablets or extended-release tablets results in reduced maximum and increased minimum plasma morphine sulfate concentrations than with shorter acting morphine sulfate products. Conversion from oral solution or immediate-release tablets to the same total daily dose of controlled-release tablets or extended-release tablets could lead to excessive sedation at peak serum levels. Therefore, dosage adjustment with close observation is necessary.2.4 Maintenance of Therapy
Continual reevaluation of the patient receiving morphine sulfate is important, with special attention to the maintenance of pain control and the relative incidence of side effects associated with therapy. If the level of pain increases, effort should be made to identify the source of increased pain, while adjusting the dose as described above to decrease the level of pain. During chronic therapy, especially for non-cancer-related pain (or pain associated with other terminal illnesses), periodically reassess the continued need for the use of opioid analgesics.
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
Morphine sulfate is contraindicated in patients with known hypersensitivity to morphine, morphine salts, or any components of the product.
Morphine sulfate is contraindicated in patients with respiratory depression in the absence of resuscitative equipment.
Morphine sulfate is contraindicated in patients with acute or severe bronchial asthma or hypercarbia.
Morphine sulfate is contraindicated in any patient who has or is suspected of having paralytic ileus. -
5 WARNINGS AND PRECAUTIONS
5.1 Risk of Medication Errors
Morphine sulfate oral solution is available in the 100 mg per 5 mL (20 mg/mL) concentration. Use caution when prescribing, dispensing, and administering morphine sulfate oral solution to avoid dosing errors due to confusion between different concentrations and between mg and mL, which could result in accidental overdose and death. Use caution to ensure the dose is communicated clearly and dispensed accurately.
5.2 Respiratory Depression
Respiratory depression is the primary risk of morphine sulfate. Respiratory depression occurs more frequently in elderly or debilitated patients and in those suffering from conditions accompanied by hypoxia, hypercapnia, or upper airway obstruction, in whom even moderate therapeutic doses may significantly decrease pulmonary ventilation.
Use morphine sulfate with extreme caution in patients with chronic obstructive pulmonary disease or cor pulmonale and in patients having a substantially decreased respiratory reserve (e.g., severe kyphoscoliosis), hypoxia, hypercapnia, or preexisting respiratory depression. In such patients, even usual therapeutic doses of morphine sulfate may increase airway resistance and decrease respiratory drive to the point of apnea. Consider alternative non-opioid analgesics, and use morphine sulfate only under careful medical supervision at the lowest effective dose in such patients.
Morphine sulfate oral solution 100 mg per 5 mL (20 mg/mL) is for use in opioid-tolerant patients only. Administration of this formulation may cause fatal respiratory depression when administered to patients who are not tolerant to the respiratory depressant effects of opioids.5.3 Misuse, Abuse and Diversion of Opioids
Morphine sulfate is an opioid agonist and a Schedule II controlled substance. Such drugs are sought by drug abusers and people with addiction disorders. Diversion of Schedule II products is an act subject to criminal penalty.
Morphine sulfate can be abused in a manner similar to other opioid agonists, legal or illicit. This should be considered when prescribing or dispensing morphine sulfate in situations where the physician or pharmacist is concerned about an increased risk of misuse, abuse, or diversion. Morphine sulfate may be abused by inhaling or injecting the product. These practices pose a significant risk to the abuser that could result in overdose and death [see Drug Abuse and Dependence (9)].
Concerns about abuse, addiction, and diversion should not prevent the proper management of pain. Healthcare professionals should contact their State Professional Licensing Board or State Controlled Substances Authority for information on how to prevent and detect abuse or diversion of this product.5.4 Interactions with Alcohol and Drugs of Abuse
Morphine sulfate may be expected to have additive effects when used in conjunction with alcohol, other opioids, or illicit drugs that cause central nervous system depression because respiratory depression, hypotension, profound sedation, coma or death may result.
5.5 Use in Head Injury and Increased Intracranial Pressure
In the presence of head injury, intracranial lesions or a preexisting increase in intracranial pressure, the possible respiratory depressant effects of morphine sulfate and its potential to elevate cerebrospinal fluid pressure (resulting from vasodilation following CO2 retention) may be markedly exaggerated. Furthermore, morphine sulfate can produce effects on pupillary response and consciousness, which may obscure neurologic signs of further increases in intracranial pressure in patients with head injuries.
5.6 Hypotensive Effects
Morphine sulfate may cause severe hypotension in an individual whose ability to maintain blood pressure has already been compromised by a depleted blood volume or concurrent administration of drugs such as phenothiazines or general anesthetics. Morphine sulfate may produce orthostatic hypotension and syncope in ambulatory patients.
Administer morphine sulfate with caution to patients in circulatory shock, as vasodilation produced by the drug may further reduce cardiac output and blood pressure.5.7 Gastrointestinal Effects
Do not administer morphine sulfate to patients with gastrointestinal obstruction, especially paralytic ileus because morphine sulfate diminishes propulsive peristaltic waves in the gastrointestinal tract and may prolong the obstruction.
The administration of morphine sulfate may obscure the diagnosis or clinical course in patients with acute abdominal condition.5.8 Use in Pancreatic/Biliary Tract Disease
Use morphine sulfate with caution in patients with biliary tract disease, including acute pancreatitis, as morphine sulfate may cause spasm of the sphincter of Oddi and diminish biliary and pancreatic secretions.
5.9 Special Risk Groups
Use morphine sulfate with caution and in reduced dosages in patients with severe renal or hepatic impairment, Addison’s disease, hypothyroidism, prostatic hypertrophy, or urethral stricture, and in elderly or debilitated patients [see Use in Specific Populations (8.5)].
Exercise caution in the administration of morphine sulfate to patients with CNS depression, toxic psychosis, acute alcoholism and delirium tremens.
All opioids may aggravate convulsions in patients with convulsive disorders, and all opioids may induce or aggravate seizures in some clinical settings.
Keep morphine sulfate oral solution out of the reach of children. In case of accidental ingestion, seek emergency medical help immediately.5.10 Driving and Operating Machinery
Caution patients that morphine sulfate could impair the mental and/or physical abilities needed to perform potentially hazardous activities such as driving a car or operating machinery.
Caution patients about the potential combined effects of morphine sulfate with other CNS depressants, including other opioids, phenothiazines, sedative/hypnotics and alcohol [see Drug Interactions (7)]. -
6 ADVERSE REACTIONS
Serious adverse reactions associated with morphine sulfate use include: respiratory depression, apnea, and to a lesser degree, circulatory depression, respiratory arrest, shock and cardiac arrest.
The common adverse reactions seen on initiation of therapy with morphine sulfate are dose-dependent and are typical opioid-related side effects. The most frequent of these include constipation, nausea, and somnolence. Other commonly observed adverse reactions include: lightheadedness, dizziness, sedation, vomiting, and sweating. The frequency of these events depends upon several factors including clinical setting, the patient’s level of opioid tolerance, and host factors specific to the individual. Anticipate and manage these events as part of opioid analgesia therapy.
Other less frequently observed adverse reactions expected from opioid analgesics, including morphine sulfate include:
Body as a Whole: malaise, withdrawal syndrome
Cardiovascular System: bradycardia, hypertension, hypotension, palpitations, syncope, tachycardia
Digestive System: anorexia, biliary pain, dyspepsia, dysphagia, gastroenteritis, abnormal liver function tests, rectal disorder, thirst
Endocrine: hypogonadism
Hemic and Lymphatic System: anemia, thrombocytopenia
Metabolic and Nutritional Disorders: edema, weight loss
Musculoskeletal: skeletal muscle rigidity, decreased bone mineral density
Nervous System: abnormal dreams, abnormal gait, agitation, amnesia, anxiety, ataxia, confusion, convulsions, coma, delirium, depression, dry mouth, euphoria, hallucinations, lethargy, nervousness, abnormal thinking, tremor, vasodilation, vertigo, headache
Respiratory System: hiccup, hypoventilation, voice alteration
Skin and Appendages: dry skin, urticaria, pruritus
Special Senses: amblyopia, eye pain, taste perversion
Urogenital System: abnormal ejaculation, dysuria, impotence, decreased libido, oliguria, urinary retention or hesitancy, antidiuretic effect, amenorrhea -
7 DRUG INTERACTIONS
7.1 CNS Depressants
Other central nervous system (CNS) depressants including sedatives, hypnotics, general anesthetics, antiemetics, phenothiazines, or other tranquilizers or alcohol increases the risk of respiratory depression, hypotension, profound sedation, or coma. Use morphine sulfate with caution and in reduced dosages in patients taking these agents.
7.2 Muscle Relaxants
Morphine sulfate may enhance the neuromuscular blocking action of skeletal muscle relaxants and produce an increased degree of respiratory depression.
7.3 Mixed Agonist/Antagonist Opioid Analgesics
Do not administer mixed agonist/antagonist analgesics (i.e., pentazocine, nalbuphine, and butorphanol) to patients who have received or are receiving a course of therapy with a pure opioid agonist analgesic such as morphine sulfate. In these patients, mixed agonist/antagonist analgesics may reduce the analgesic effect and/or may precipitate withdrawal symptoms.
7.4 Cimetidine
Concomitant administration of morphine sulfate and cimetidine has been reported to precipitate apnea, confusion, and muscle twitching in an isolated report. Monitor patients for increased respiratory and CNS depression when receiving cimetidine concomitantly with morphine sulfate.
7.5 Monoamine Oxidase Inhibitors (MAOIs)
MAOIs markedly potentiate the action of morphine sulfate. Allow at least 14 days after stopping treatment with MAOIs before initiating treatment with morphine sulfate.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Teratogenic Effects - Pregnancy Category C: No formal studies to assess the teratogenic effects of morphine in animals have been conducted. It is also not known whether morphine can cause fetal harm when administered to a pregnant woman or can affect reproductive capacity. Morphine should be given to a pregnant woman only if clearly needed.
In humans, the frequency of congenital anomalies has been reported to be no greater than expected among the children of 70 women who were treated with morphine during the first four months of pregnancy or in 448 women treated with morphine anytime during pregnancy. Furthermore, no malformations were observed in the infant of a woman who attempted suicide by taking an overdose of morphine and other medication during the first trimester of pregnancy.
Several literature reports indicate that morphine administered subcutaneously during the early gestational period in mice and hamsters produced neurological, soft tissue and skeletal abnormalities. With one exception, the effects that have been reported were following doses that were maternally toxic and the abnormalities noted were characteristic of those observed when maternal toxicity is present. In one study, following subcutaneous infusion of doses greater than or equal to 0.15 mg/kg to mice, exencephaly, hydronephrosis, intestinal hemorrhage, split supraoccipital, malformed sternebrae, and malformed xiphoid were noted in the absence of maternal toxicity. In the hamster, morphine sulfate given subcutaneously on gestation day 8 produced exencephaly and cranioschisis. In rats treated with subcutaneous infusions of morphine during the period of organogenesis, no teratogenicity was observed. No maternal toxicity was observed in this study, however, increased mortality and growth retardation were seen in the offspring. In two studies performed in the rabbit, no evidence of teratogenicity was reported at subcutaneous doses up to 100 mg/kg.Nonteratogenic Effects
Controlled studies of chronic in utero morphine exposure in pregnant women have not been conducted. Infants born to mothers who have taken opioids chronically may exhibit withdrawal symptoms, reversible reduction in brain volume, small size, decreased ventilatory response to CO2 and increased risk of sudden infant death syndrome. Morphine sulfate should be used by a pregnant woman only if the need for opioid analgesia clearly outweighs the potential risks to the fetus.
Published literature has reported that exposure to morphine during pregnancy is associated with reduction in growth and a host of behavioral abnormalities in the offspring. Morphine treatment during gestational periods of organogenesis in rats, hamsters, guinea pigs and rabbits resulted in the following treatment-related embryotoxicity and neonatal toxicity in one or more studies: decreased litter size, embryo-fetal viability, fetal and neonatal body weights, absolute brain and cerebellar weights, delayed motor and sexual maturation, and increased neonatal mortality, cyanosis and hypothermia. Decreased fertility in female offspring, and decreased plasma and testicular levels of luteinizing hormone and testosterone, decreased testes weights, seminiferous tubule shrinkage, germinal cell aplasia, and decreased spermatogenesis in male offspring were also observed. Decreased litter size and viability were observed in the offspring of male rats administered morphine (25 mg/kg, IP) for 1 day prior to mating. Behavioral abnormalities resulting from chronic morphine exposure of fetal animals included altered reflex and motor skill development, mild withdrawal, and altered responsiveness to morphine persisting into adulthood.8.2 Labor and Delivery
Opioids cross the placenta and may produce respiratory depression and psycho-physiologic effects in neonates. Morphine sulfate is not recommended for use in women during and immediately prior to labor. Occasionally, opioid analgesics may prolong labor through actions which temporarily reduce the strength, duration and frequency of uterine contractions. However this effect is not consistent and may be offset by an increased rate of cervical dilatation, which tends to shorten labor. Closely observe neonates whose mothers received opioid analgesics during labor for signs of respiratory depression. Have a specific opioid antagonist, such as naloxone, available for reversal of opioid-induced respiratory depression in the neonate.
8.3 Nursing Mothers
Low levels of morphine sulfate have been detected in maternal milk. The milk:plasma morphine AUC ratio is about 2.5:1. The amount of morphine sulfate delivered to the infant depends on the plasma concentration of the mother, the amount of milk ingested by the infant, and the extent of first-pass metabolism. Because of the potential for serious adverse reactions in nursing infants from morphine sulfate including respiratory depression, sedation and possibly withdrawal symptoms, upon cessation of morphine sulfate administration to the mother, decide whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
8.4 Pediatric Use
The safety and effectiveness and the pharmacokinetics of morphine sulfate oral solution in pediatric patients below the age of 18 have not been established.
8.5 Geriatric Use
Elderly patients (aged 65 years or older) may have increased sensitivity to morphine sulfate. In general, use caution when selecting a dose for an elderly patient, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function and of concomitant disease or other drug therapy.
8.6 Neonatal Withdrawal Syndrome
Chronic maternal use of opioids during pregnancy may cause newborns to suffer from neonatal withdrawal syndrome (NWS) following birth. Manifestations of this syndrome include irritability, hyperactivity, abnormal sleep pattern, high-pitched cry, tremor, vomiting, diarrhea, weight loss, and failure to gain weight. The time and amount of the mother’s last dose and the rate of elimination of the drug from the newborn may affect the onset, duration, and severity of the disorder. When severe symptoms occur, pharmacologic intervention may be required.
8.7 Gender
While evidence of greater post-operative morphine sulfate consumption in men compared to women is present in the literature, clinically significant differences in analgesic outcomes and pharmacokinetic parameters have not been consistently demonstrated. Some studies have shown an increased sensitivity to the adverse effects of morphine sulfate, including respiratory depression, in women compared to men.
8.8 Hepatic Impairment
Morphine sulfate pharmacokinetics have been reported to be significantly altered in patients with cirrhosis. Clearance was found to decrease with a corresponding increase in half-life. The M3G and M6G to morphine AUC ratios also decreased in these subjects, indicating diminished metabolic activity. Start these patients cautiously with lower doses of morphine sulfate and titrate slowly while carefully monitoring for side effects.
8.9 Renal Impairment
Morphine sulfate pharmacokinetics are altered in patients with renal failure. Clearance is decreased and the metabolites, M3G and M6G, may accumulate too much higher plasma levels in patients with renal failure as compared to patients with normal renal function. Start these patients cautiously with lower doses of morphine sulfate and titrate slowly while carefully monitoring for side effects.
-
9 DRUG ABUSE AND DEPENDENCE
9.1 Controlled Substance
Morphine sulfate is a mu-agonist opioid and is a Schedule II controlled substance. Morphine sulfate, like other opioids used in analgesia, can be abused and is subject to criminal diversion.
9.2 Abuse
Drug addiction is characterized by compulsive use, use for non-medical purposes, and continued use despite harm or risk of harm. Drug addiction is a treatable disease, utilizing a multidisciplinary approach, but relapse is common.
“Drug-seeking” behavior is very common in addicts and drug abusers. Drug-seeking tactics include emergency calls or visits near the end of office hours, refusal to undergo appropriate examination, testing or referral, repeated “loss” of prescriptions, tampering with prescriptions and reluctance to provide prior medical records or contact information for other treating physician(s). “Doctor shopping” to obtain additional prescriptions is common among drug abusers and people suffering from untreated addiction.
Abuse and addiction are separate and distinct from physical dependence and tolerance. Physicians should be aware that addiction may not be accompanied by concurrent tolerance and symptoms of physical dependence. The converse is also true. In addition, abuse of opioids can occur in the absence of true addiction and is characterized by misuse for non-medical purposes, often in combination with other psychoactive substances. Careful recordkeeping of prescribing information, including quantity, frequency, and renewal requests is strongly advised.
Morphine sulfate is intended for oral use only. Abuse of morphine sulfate poses a risk of overdose and death. The risk is increased with concurrent abuse of alcohol and other substances. Parenteral drug abuse is commonly associated with transmission of infectious diseases such as hepatitis and HIV.
Proper assessment of the patient, proper prescribing practices, periodic
reevaluation of therapy, and proper dispensing and storage are appropriate measures that help to limit abuse of opioid drugs.
Infants born to mothers physically dependent on opioids will also be physically dependent and may exhibit respiratory difficulties and withdrawal symptoms [see Use in Specific Populations (8.6)].9.3 Dependence
Tolerance is the need for increasing doses of opioids to maintain a defined effect such as analgesia (in the absence of disease progression or other external factors). Physical dependence is manifested by withdrawal symptoms after abrupt discontinuation of a drug or upon administration of an antagonist. Physical dependence and tolerance are not unusual during chronic opioid therapy. The opioid abstinence or withdrawal syndrome is characterized by some or all of the following: restlessness, lacrimation, rhinorrhea, yawning, perspiration, chills, myalgia, and mydriasis. Other symptoms also may develop, including irritability, anxiety, backache, joint pain, weakness, abdominal cramps, insomnia, nausea, anorexia, vomiting, diarrhea, or increased blood pressure, respiratory rate, or heart rate.
In general, taper opioids rather than abruptly discontinue [see Dosage and Administration (2.5)]. -
10 OVERDOSAGE
10.1 Symptoms
Acute overdosage with morphine sulfate is manifested by respiratory depression (a decrease in respiratory rate and/or tidal volume, Cheyne-Stokes respiration, cyanosis), extreme somnolence progressing to stupor or coma, skeletal muscle flaccidity, cold and clammy skin, constricted pupils, and, in some cases, pulmonary edema, bradycardia, hypotension, cardiac arrest and death.
Morphine sulfate may cause miosis, even in total darkness. Pinpoint pupils are a sign of opioid overdose but are not pathognomonic (e.g., pontine lesions of hemorrhagic or ischemic origin may produce similar findings). Marked mydriasis rather than miosis may be seen with hypoxia in overdose situations [see Clinical Pharmacology (12)].10.2 Treatment
Give primary attention to reestablishment of a patent airway and institution of assisted or controlled ventilation. Employ supportive measures (including oxygen and vasopressors) in the management of circulatory shock and pulmonary edema accompanying overdose as indicated. Cardiac arrest or arrhythmias may require cardiac massage or defibrillation.
Naloxone is a pure opioid antagonist that is a specific antidote to respiratory depression resulting from opioid overdose. Since the duration of reversal is expected to be less than the duration of action of morphine sulfate, carefully monitor the patient until spontaneous respiration is reliably reestablished. If the response to opioid antagonists is suboptimal or only brief in nature, administer additional antagonist as directed by the manufacturer of the product.
Do not administer opioid antagonists in the absence of clinically significant respiratory or circulatory depression secondary to morphine sulfate overdose. Administer such agents cautiously to persons who are known, or suspected to be physically dependent on morphine sulfate. In such cases, an abrupt or complete reversal of opioid effects may precipitate an acute abstinence syndrome.
In an individual physically dependent on opioids, administration of the usual dose of the antagonist will precipitate an acute withdrawal syndrome. The severity of the withdrawal symptoms experienced will depend on the degree of physical dependence and the dose of the antagonist administered. Reserve use of an opioid antagonist for cases where such treatment is clearly needed. If it is necessary to treat serious respiratory depression in the physically dependent patient, initiate administration of the antagonist with care and titrate with smaller than usual doses. -
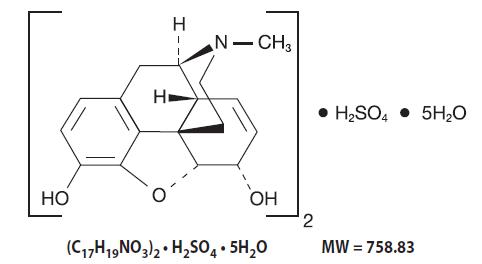
11 DESCRIPTION
Chemically, morphine sulfate is 7,8-didehydro-4,5α-epoxy-17-methylmorphinan-3,6α-diol sulfate (2:1) (salt) pentahydrate with a molecular mass of 758.83. Morphine sulfate occurs as white, feathery, silky crystals; cubical masses of crystal; or white crystalline powder. It is soluble in water and slightly soluble in alcohol, but is practically insoluble in chloroform or ether. The octanol:water partition coefficient of morphine is 1.42 at physiologic pH and the pKa is 7.9 for the tertiary nitrogen (the majority is ionized at pH 7.4).
Active Ingredient: For the 100 mg per 5 mL (20 mg/mL) strength: Each 5 mL of oral solution contains 100 mg of morphine sulfate USP.
Inactive Ingredients: anhydrous citric acid, edetate disodium, FD&C Green No. 3, glycerin, purified water, raspberry cream flavor and sodium benzoate. The pH of the solution is adjusted with diluted hydrochloric acid, as needed. -
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Morphine sulfate, an opioid agonist, is relatively selective for the mu receptor, although it can interact with other opioid receptors at higher doses. In addition to analgesia, the widely diverse effects of morphine sulfate include drowsiness, changes in mood, respiratory depression, decreased gastrointestinal motility, nausea, vomiting, and alterations of the endocrine and autonomic nervous system.
Effects on the Central Nervous System (CNS)
The principal therapeutic action of morphine sulfate is analgesia. Other therapeutic effects of morphine sulfate include anxiolysis, euphoria and feelings of relaxation. Although the precise mechanism of the analgesic action is unknown, specific CNS opiate receptors and endogenous compounds with morphine sulfate-like activity have been identified throughout the brain and spinal cord and are likely to play a role in the expression and perception of analgesic effects. In common with other opioids, morphine sulfate causes respiratory depression, in part by a direct effect on the brainstem respiratory centers. Morphine sulfate and related opioids depress the cough reflex by direct effect on the cough center in the medulla.
Morphine sulfate causes miosis, even in total darkness.
Effects on the Gastrointestinal Tract and on Other Smooth Muscle
Gastric, biliary and pancreatic secretions are decreased by morphine sulfate. Morphine sulfate causes a reduction in motility and is associated with an increase in tone in the antrum of the stomach and duodenum. Digestion of food in the small intestine is delayed and propulsive contractions are decreased. Propulsive peristaltic waves in the colon are decreased, while tone is increased to the point of spasm.
The end result may be constipation. Morphine sulfate can cause a marked increase in biliary tract pressure as a result of spasm of the sphincter of Oddi. Morphine sulfate may also cause spasm of the sphincter of the urinary bladder.
Effects on the Cardiovascular System
In therapeutic doses, morphine sulfate does not usually exert major effects on the cardiovascular system. Morphine sulfate produces peripheral vasodilation which may result in orthostatic hypotension and fainting. Release of histamine can occur, which may play a role in opioid-induced hypotension. Manifestations of histamine release and/or peripheral vasodilation may include pruritus, flushing, red eyes and sweating.
Endocrine System
Opioid agonists have been shown to have a variety of effects on the secretion of hormones. Opioids inhibit the secretion of ACTH, cortisol, and luteinizing hormone (LH) in humans. They also stimulate prolactin, growth hormone (GH) secretion, and pancreatic secretion of insulin and glucagon in humans and other species, rats and dogs. Thyroid stimulating hormone (TSH) has been shown to be both inhibited and stimulated by opioids.
Immune System
Opioids have been shown to have a variety of effects on components of the immune system in in vitro and animal models. The clinical significance of these findings is unknown.12.2 Pharmacodynamics
Morphine sulfate concentrations are not predictive of analgesic response, especially in patients previously treated with opioids. The minimum effective concentration varies widely and is influenced by a variety of factors, including the extent of previous opioid use, age and general medical condition. Effective doses in tolerant patients may be significantly higher than in opioid-naïve patients.
12.3 Pharmacokinetics
Absorption
Morphine sulfate is about two-thirds absorbed from the gastrointestinal tract with the maximum analgesic effect occurring 60 minutes postadministration. The oral bioavailability of morphine sulfate is less than 40% and shows large interindividual variability due to extensive presystemic metabolism.
Food Effects
Although the presence of a food effect was not assessed with morphine sulfate oral solution, significant food effect is not expected with a solution formulation.
Steady-State
Administration of the 30 mg morphine sulfate tablet and 30 mg of morphine sulfate oral solution every six hours for 5 days resulted in a comparable
24-hour exposure (AUC). The steady-state levels were achieved within 48 hours for both tablets and solution. The mean steady state Cmax values were about 78 and 58 ng/mL for tablet and solution, respectively.
Distribution
Once absorbed, morphine sulfate is distributed to skeletal muscle, kidneys, liver, intestinal tract, lungs, spleen and brain. Although the primary site of action is the CNS, only small quantities cross the blood-brain barrier. Morphine sulfate also crosses the placental membranes and has been found in breast milk. The volume of distribution of morphine sulfate is approximately
1 to 6 L/kg, and morphine sulfate is 20 to 35% reversibly bound to plasma proteins.
Metabolism
The major pathway of morphine sulfate detoxification is conjugation, either with D-glucuronic acid to produce glucuronides or with sulfuric acid to produce morphine-3-etheral sulfate. While a small fraction (less than 5%) of morphine sulfate is demethylated, virtually all morphine sulfate is converted by hepatic metabolism to the 3- and 6-glucuronide metabolites (M3G and M6G; about 50% and 15%, respectively). M6G has been shown to have analgesic activity but crosses the blood-brain barrier poorly, while M3G has no significant analgesic activity.
Excretion
Most of a dose of morphine sulfate is excreted in urine as M3G and M6G, with elimination of morphine sulfate occurring primarily as renal excretion of M3G. Approximately 10% of the dose is excreted unchanged in urine. A small amount of glucuronide conjugates are excreted in bile, with minor enterohepatic recycling. Seven to 10% of administered morphine sulfate is excreted in the feces.
The mean adult plasma clearance is approximately 20 to 30 mL/min/kg. The effective terminal half-life of morphine sulfate after IV administration is reported to be approximately 2 hours. In some studies involving longer periods of plasma sampling, a longer terminal half-life of morphine sulfate of about 15 hours was reported.
Race
There may be some pharmacokinetic differences associated with race. In one published study, Chinese subjects given intravenous morphine sulfate had a higher clearance when compared to Caucasian subjects (1852 ± 116 mL/min compared to 1495 ± 80 mL/min). -
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Studies in animals to evaluate the carcinogenic potential of morphine have not been conducted.
Mutagenesis
No formal studies to assess the mutagenic potential of morphine have been conducted. In the published literature, morphine was found to be mutagenic in vitro increasing DNA fragmentation in human T-cells. Morphine was reported to be mutagenic in the in vivo mouse micronucleus assay and positive for the induction of chromosomal aberrations in mouse spermatids and murine lymphocytes. Mechanistic studies suggest that the in vivo clastogenic effects reported with morphine in mice may be related to increases in glucocorticoid levels produced by morphine in this species. In contrast to the above positive findings, in vitro studies in the literature have also shown that morphine did not induce chromosomal aberrations in human leukocytes or translocations or lethal mutations in
Drosophila.
Impairment of Fertility
No formal nonclinical studies to assess the potential of morphine to impair fertility have been conducted. Several nonclinical studies from the literature have demonstrated adverse effects on male fertility in the rat from exposure to morphine. One study in which male rats were administered morphine sulfate subcutaneously prior to mating (up to 30 mg/kg twice daily) and during mating (20 mg/kg twice daily) with untreated females, a number of adverse reproductive effects including reduction in total pregnancies, higher incidence of pseudopregnancies, and reduction in implantation sites were seen. Studies from the literature have also reported changes in hormonal levels (i.e. testosterone, luteinizing hormone, serum corticosterone) following treatment with morphine. These changes may be associated with the reported effects on fertility in the rat. -
16 HOW SUPPLIED/STORAGE AND HANDLING
Morphine sulfate oral solution 100 mg per 5 mL (20 mg/mL) is available as a clear, light blue liquid with raspberry odor.
Supplied as an individual overwrapped and flagged calibrated oral syringe:
Syringes of 0.5 mL containing 0.25 mL NDC: 48433-200-47
Syringes of 1 mL containing 0.5 mL NDC: 48433-200-55
Syringes of 3 mL containing 1 mL NDC: 48433-200-01
Storage
Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
PROTECT FROM LIGHT.
All opioids are liable to diversion and misuse both by the general public and healthcare workers and should be handled accordingly. -
17 PATIENT COUNSELING INFORMATION
Information for Patients and Caregivers
Provide the following information to patients receiving morphine sulfate or their caregivers:
- Advise patients that morphine sulfate is a narcotic pain reliever, and should be taken only as directed.
- Advise patients that morphine sulfate oral solution is available in one concentration: 100 mg per 5 mL (20 mg/mL). Carefully instruct patients about which concentration they have been prescribed and how to measure and take the correct dose of morphine sulfate oral solution. Advise patients whenever the prescribed concentration is changed to avoid dosing errors which could result in accidental overdose and death.
- Advise patients to always ensure the dose is measured and administered accurately.
- The 100 mg per 5 mL (20 mg/mL) formulation is only for patients who are already receiving opioid therapy and have demonstrated opioid tolerance. Use of this formulation may cause fatal respiratory depression when administered to patients who have not had previous exposure to opioids.
- Advise patients not to adjust the dose of morphine sulfate without consulting with a physician or other healthcare professional.
- Advise patients that morphine sulfate may cause drowsiness, dizziness, or lightheadedness and may impair mental and/or physical ability required for the performance of potentially hazardous tasks (e.g., driving, operating machinery). Advise patients started on morphine sulfate or patients whose dose has been adjusted to refrain from any potentially dangerous activity until it is established that they are not adversely affected.
- Instruct patients not to combine morphine sulfate with central nervous system depressants (such as sleep aids, tranquilizers, antihistamines, general anesthetics, phenothiazines, other opioids, and monoamine oxidase [MAO] inhibitors) except by the orders of the prescribing physician, and not to combine with alcohol because dangerous additive effects may occur, resulting in serious injury or death.
- Instruct women of childbearing potential who become or are planning to become pregnant to consult a physician prior to initiating or continuing therapy with morphine sulfate.
- Advise patients that safe use in pregnancy has not been established and that prolonged use of opioid analgesics during pregnancy may cause fetal-neonatal physical dependence. Neonatal withdrawal may also occur.
- If patients have been receiving treatment with morphine sulfate for more than a few weeks and cessation of therapy is indicated, counsel them on the importance of safely tapering the dose as abrupt discontinuation of the medication could precipitate withdrawal symptoms. Provide a dose schedule to accomplish a gradual discontinuation of the medication.
- Advise patients that morphine sulfate is a potential drug of abuse. They must protect it from theft. It should never be given to anyone other than the individual for whom it was prescribed.
- Instruct patients to keep morphine sulfate in a secure place out of the reach of children. When morphine sulfate is no longer needed, the unused oral solution should be destroyed by flushing down the toilet.
- Advise patients taking morphine sulfate of the potential for severe constipation; appropriate laxatives and/or stool softeners as well as other appropriate treatments should be initiated from the onset of opioid therapy.
- Advise patients of the most common adverse events that may occur while taking morphine sulfate: constipation, nausea, somnolence, lightheadedness, dizziness, sedation, vomiting, and sweating.
-
MEDICATION GUIDE
Morphine Sulfate (mor-pheen) (CII)
Oral SolutionIMPORTANT: Keep morphine sulfate oral solution in a safe place away from children. Accidental use by a child is a medical emergency and can cause death. If a child accidentally takes morphine sulfate oral solution, get emergency help right away. Read the Medication Guide that comes with morphine sulfate oral solution before you start taking it and each time you get a new prescription. There may be new information. This Medication Guide does not take the place of talking with your healthcare provider about your medical condition or your treatment.
What is the most important information I should know about morphine sulfate oral solution?
Morphine sulfate oral solution can cause serious side effects, including death.- Take morphine sulfate oral solution exactly as prescribed by your healthcare provider. If you take the wrong dose or strength of morphine sulfate oral solution, you could overdose and die.
- It is especially important when you take morphine sulfate oral solution that you know exactly what dose and strength to take, and the right way to measure your medicine. Your healthcare provider or pharmacist should show you the right way to measure your medicine.
- Always make sure the dose is measured and administered accurately.
- The oral solution comes in several different doses (amount of medicine per mL) and strengths (number of mgs).
-
Do not take the strongest dose of morphine sulfate oral solution, 100 mg per 5 mL
(20 mg/mL) unless you are “opioid tolerant”. Opioid tolerant means that you have been regularly using morphine sulfate oral solution or another opioid medicine for your constant (around the clock) pain and your body is used to it.
What is morphine sulfate oral solution?
Morphine sulfate oral solution is in a group of drugs called narcotic pain relievers. Morphine sulfate oral solution is only for adults who have moderate to severe pain.- Morphine sulfate oral solution is a prescription medicine that is used to manage moderate to severe pain that is expected to last a short period of time (acute), and pain that continues around-the-clock and is expected to last for a long period of time (chronic).
- Morphine sulfate oral solution is a federally controlled substance (CII) because it is a strong opioid pain medicine that can be abused by people who abuse prescription medicines or street drugs.
- Prevent theft, misuse or abuse. Keep morphine sulfate oral solution in a safe place to keep it from being stolen. Morphine sulfate oral solution can be a target for people who misuse or abuse prescription medicines or street drugs.
- Never give morphine sulfate oral solution to anyone else, even if they have the same symptoms you have. It may harm them or even cause death.
- Selling or giving away this medicine is against the law.
- It is not known if morphine sulfate oral solution is safe and effective in children under 18 years of age.
- Morphine sulfate oral solution 100 mg per 5 mL (20 mg/mL) is only for adults with moderate to severe pain who are already using an opioid narcotic pain medicine and have been using this medicine continuously for several weeks or longer.
Who should not take morphine sulfate oral solution?
Do not take morphine sulfate oral solution if you:- are allergic to morphine, morphine salts or any of the ingredients in morphine sulfate oral solution. See the end of this Medication Guide for a complete list of ingredients in morphine sulfate oral solution.
- are having an asthma attack or have severe asthma, trouble breathing, or lung problems
- have a bowel blockage called paralytic ileus
What should I tell my healthcare provider before taking morphine sulfate oral solution?
Before taking morphine sulfate oral solution, tell your healthcare provider if you:- have trouble breathing or lung problems
- have had a head injury
- have liver or kidney problems
- have had adrenal gland problems, such as Addison’s disease
- have severe scoliosis that affects your breathing
- have thyroid problems
- have problems urinating or enlargement of your prostate
- have had convulsions or seizures
- have a past or present drinking problem or alcoholism
- have severe mental problems or hallucinations (seeing or hearing things that are not really there)
- have constipation or other bowel problems
- have problems with your pancreas or gallbladder
- have past or present substance abuse or drug addiction
- plan to have surgery
- have any other medical conditions
- are pregnant or plan to become pregnant. It is not known if morphine sulfate oral solution will harm your unborn baby. Talk to your healthcare provider if you are pregnant or plan to become pregnant.
If you take morphine sulfate oral solution regularly before your baby is born, your newborn baby may have withdrawal symptoms because their body has become used to the medicine. Symptoms of withdrawal in a newborn baby may include:
- irritability
- being very active
- problems sleeping
- high pitched cry
- shaking (tremors)
- vomiting
- diarrhea or more stools than normal
- weight loss
- fever
If you take morphine sulfate oral solution right before your baby is born, your baby could have breathing problems.
- are breastfeeding or plan to breastfeed. Some morphine sulfate passes into your breast milk. A nursing baby could become very sleepy and have problems breathing or feeding well. If you stop breastfeeding, your baby may have withdrawal symptoms. See the list of withdrawal symptoms above. You and your healthcare provider should decide if you will take morphine sulfate oral solution or breastfeed.
Tell your healthcare provider about all the medicines you take, including prescription and non-prescription medicines, vitamins, and herbal supplements. Sometimes the doses of medicines that you take with morphine sulfate oral solution may need to be changed if used together. Be especially careful about taking other medicines that make you sleepy such as:
- sleeping pills
- other pain medicines
- anti-nausea medicines
- tranquilizers
- antihistamines
- anti-anxiety medicines
- antidepressants
- anticholinergic medicines
- antibiotic or antifungal medicines
- heart medicines
- anti-seizure medicines
- muscle relaxants
- Tell your healthcare provider if you take cimetidine (Tagamet®).
- Do not take morphine sulfate oral solution if you already take a monoamine oxidase inhibitor medicine (MAOI) or within 14 days after you stop taking an MAOI medicine.
- Do not take any new medicine while using morphine sulfate oral solution until you have talked with your healthcare provider or pharmacist. They will tell you if it is safe to take other medicines with morphine sulfate oral solution.
Ask your healthcare provider if you are not sure if your medicine is one listed above.
Know the medicines you take. Keep a list of them and show it to your healthcare provider and pharmacist when you get a new medicine.
How should I take morphine sulfate oral solution?
- See “What is the most important information I should know about morphine sulfate oral solution?”
- Take morphine sulfate oral solution exactly as prescribed. Do not change your dose unless your healthcare provider tells you to. Your healthcare provider may change your dose after seeing how the medicine affects you. Call your healthcare provider if your pain is not well controlled with your prescribed dose of morphine sulfate oral solution.
- You can take morphine sulfate oral solution with or without food.
- Make sure you understand exactly how to measure your dose. Always use the oral syringe provided with your morphine sulfate oral solution, 100 mg per 5 mL (20 mg/mL) to help make sure you measure the right amount. See the Instructions for Use at the end of this Medication Guide for information about how to measure your dose the right way. Ask your healthcare provider or pharmacist if you are not sure what dose of morphine sulfate oral solution you should take or if you are not sure how to use the oral syringe.
- Do not stop taking morphine sulfate oral solution suddenly. If you have been taking morphine sulfate oral solution for more than a few weeks, stopping morphine sulfate oral solution suddenly can make you sick with withdrawal symptoms (for example, nausea, vomiting, diarrhea, anxiety, and shivering). If your healthcare provider decides you no longer need morphine sulfate oral solution, ask how to slowly reduce this medicine. Do not stop taking morphine sulfate oral solution without talking to your healthcare provider.
- If you miss one dose of morphine sulfate oral solution you can take the dose when you remember it if you have pain, or you can wait for the next dose.
Talk with your healthcare provider regularly about your pain to see if you still need to take morphine sulfate oral solution.
What should I avoid while taking morphine sulfate oral solution?
- You should not drink alcohol while using morphine sulfate oral solution. Drinking alcohol with morphine sulfate oral solution may increase your risk of having dangerous side effects or death.
- Do not drive, operate heavy machinery, or do other dangerous activities, especially when you start taking morphine sulfate oral solution and when your dose is changed, until you know how morphine sulfate oral solution affects you. Morphine sulfate oral solution can make you sleepy. Ask your healthcare provider to tell you when it is okay to do these activities.
What are the possible side effects of morphine sulfate oral solution?
- See “What is the most important information I should know about morphine sulfate oral solution?”
- Morphine sulfate oral solution can cause serious breathing problems that can become life-threatening, especially if morphine sulfate oral solution is used the wrong way. Call your healthcare provider or get help right away if:
- your breathing slows down
- you have shallow breathing (little chest movement with breathing)
- you feel faint, dizzy, confused, or
- you have any other unusual symptoms
These can be symptoms that you have taken too much morphine sulfate oral solution (overdose) or the dose is too high for you. These symptoms may lead to serious problems or death if not treated right away.
- Morphine sulfate oral solution can cause your blood pressure to drop. This can make you feel dizzy if you get up too fast from sitting or lying down. Low blood pressure is also more likely to happen if you take other medicines that can also lower your blood pressure. Severe low blood pressure can happen if you lose blood or take certain other medicines.
-
There is a risk of abuse or addiction with morphine sulfate oral solution. The chance is higher if you are or have been addicted to or abused other medicines, street drugs, or alcohol, or if you have a history of mental problems.
-
Morphine sulfate oral solution can cause physical dependence. Do not stop taking morphine sulfate or any other opioid without talking to your healthcare provider about how to slowly stop your medicine. You could become sick with uncomfortable withdrawal symptoms because your body has become used to these medicines. Physical dependence is not the same as drug addiction. Tell your healthcare provider if you have any of these symptoms of withdrawal while slowly stopping morphine sulfate oral solution:
- feel restless
- tearing eyes
- runny nose
- yawning
- sweating
- chills or hair on your arms “stand up”
- muscle aches, backache
- dilated pupils of your eyes
- feel irritable or anxious
- trouble sleeping
- increase in your blood pressure
- faster breathing, or faster heart beats
- nausea, loss of appetite, vomiting, diarrhea, stomach-area (abdominal) cramps
-
Common side effects of morphine sulfate oral solution include:
- constipation
- nausea
- sleepiness
- lightheadedness
- dizziness
- drowsiness
- vomiting
- sweating
Constipation (not often enough or hard bowel movements) is a very common side effect of pain medicines (opioids). Talk to your healthcare provider about dietary changes, and the use of laxatives (medicines to treat constipation) and stool softeners to prevent or treat constipation while taking morphine sulfate oral solution.
Tell your healthcare provider if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of morphine sulfate oral solution. For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.How should I store morphine sulfate oral solution?
- Store morphine sulfate oral solution at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
- After you stop taking morphine sulfate oral solution, flush the unused oral solution down the toilet.
- Keep morphine sulfate oral solution out of the reach of children. Accidental overdose by a child is a medical emergency and can lead to death.
General information about morphine sulfate oral solution
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use morphine sulfate oral solution for a condition for which it was not prescribed.
Do not give your morphine sulfate oral solution to other people, even if they have the same symptoms you have. Selling or giving away morphine sulfate oral solution may harm others, may cause death, and is against the law.
This Medication Guide summarizes the most important information about morphine sulfate oral solution. If you would like more information, talk with your healthcare provider. You can ask your healthcare provider or pharmacist for information about morphine sulfate oral solution that is written for healthcare professionals.
For more information about morphine sulfate oral solution, go to www.covidien.com or call Mallinckrodt at 1-800-778-7898.
What are the ingredients in morphine sulfate oral solution?
Active ingredient: morphine sulfate
Inactive ingredients: anhydrous citric acid, edetate disodium, FD&C Green No. 3, glycerin, purified water, raspberry cream flavor, and sodium benzoate. The pH of the solution is adjusted with diluted hydrochloric acid, as needed.
This Medication Guide has been approved by the U.S. Food and Drug Administration. -
INSTRUCTIONS FOR USE
Morphine Sulfate Oral Solution 100 mg per 5 mL (20 mg/mL)
Oral Syringe
Important information about measuring morphine sulfate oral solution- Take your medicine by slowly pushing the plunger of the oral syringe until the prescribed dose is administered.
Tagamet is a registered trademark of Medtech Products Inc.
Manufactured by: Mallinckrodt Inc.
Hazelwood, MO 63042 USA
Issued 07/2012
Mallinckrodt
COVIDIENTM
Repackaged by: Safecor Health -
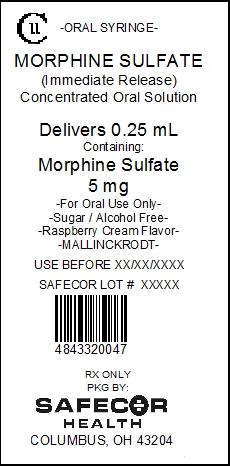
PACKAGE LABEL - PRINCIPAL DISPLAY PANEL Repackaged Oral Syringes
CII -ORAL SYRINGE-
MORPHINE SULFATE
(Immediate Release)
Concentrated Oral Solution
Delivers 0.25 mL
Containing:
Morphine Sulfate
5 mg
-For Oral Use Only-
-Sugar / Alcohol Free-
-Raspberry Cream Flavor-
-MALLINCKRODT-
USE BEFORE
SAFECOR LOT #
48433-200-47
RX ONLY
PKG BY:
SAFECOR
HEALTH
COLUMBUS, OH 43204
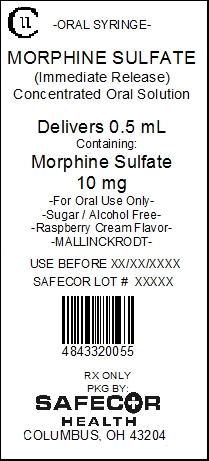
CII -ORAL SYRINGE-
MORPHINE SULFATE
(Immediate Release)
Concentrated Oral Solution
Delivers 0.5 mL
Containing:
Morphine Sulfate
10 mg
-For Oral Use Only-
-Sugar / Alcohol Free-
-Raspberry Cream Flavor-
-MALLINCKRODT-
USE BEFORE
SAFECOR LOT #
48433-200-55
RX ONLY
PKG BY:
SAFECOR
HEALTH
COLUMBUS, OH 43204
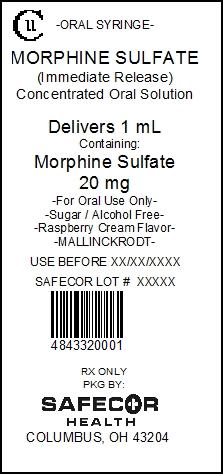
CII -ORAL SYRINGE-
MORPHINE SULFATE
(Immediate Release)
Concentrated Oral Solution
Delivers 1 mL
Containing:
Morphine Sulfate
20 mg
-For Oral Use Only-
-Sugar / Alcohol Free-
-Raspberry Cream Flavor-
-MALLINCKRODT-
USE BEFORE
SAFECOR LOT #
48433-200-01
RX ONLY
PKG BY:
SAFECOR
HEALTH
COLUMBUS, OH 43204
-
INGREDIENTS AND APPEARANCE
MORPHINE SULFATE
morphine sulfate solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 48433-200 Route of Administration ORAL DEA Schedule CII Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength MORPHINE SULFATE (UNII: X3P646A2J0) (MORPHINE - UNII:76I7G6D29C) MORPHINE SULFATE 20 mg in 1 mL Inactive Ingredients Ingredient Name Strength ANHYDROUS CITRIC ACID (UNII: XF417D3PSL) EDETATE DISODIUM (UNII: 7FLD91C86K) FD&C GREEN NO. 3 (UNII: 3P3ONR6O1S) GLYCERIN (UNII: PDC6A3C0OX) WATER (UNII: 059QF0KO0R) SODIUM BENZOATE (UNII: OJ245FE5EU) HYDROCHLORIC ACID (UNII: QTT17582CB) Product Characteristics Color BLUE (clear, light blue) Score Shape Size Flavor RASPBERRY Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 48433-200-47 0.25 mL in 1 SYRINGE; Type 0: Not a Combination Product 01/17/2013 2 NDC: 48433-200-55 0.5 mL in 1 SYRINGE; Type 0: Not a Combination Product 01/17/2013 3 NDC: 48433-200-01 1 mL in 1 SYRINGE; Type 0: Not a Combination Product 01/17/2013 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA202348 01/17/2013 Labeler - Safecor Health, LLC (828269675) Establishment Name Address ID/FEI Business Operations MALLINCKRODT INC 957414238 ANALYSIS(48433-200) , MANUFACTURE(48433-200) Establishment Name Address ID/FEI Business Operations MALLINCKRODT, INC. 163205300 API MANUFACTURE(48433-200)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.