OXACILLIN injection, powder, for solution
Oxacillin by
Drug Labeling and Warnings
Oxacillin by is a Prescription medication manufactured, distributed, or labeled by Mitim S.r.l., Wockhardt Limited. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
- SPL UNCLASSIFIED SECTION
-
DESCRIPTION
Oxacillin for injection, USP is a sterile product for intramuscular or intravenous administration. Oxacillin for injection, USP contains oxacillin sodium, a semisynthetic penicillin derived from the penicillin nucleus, 6-aminopenicillanic acid. It is resistant to inactivation by the enzyme penicillinase (beta-lactamase). Each vial contains oxacillin sodium monohydrate equivalent to 1 gram or 2 grams of oxacillin. The sodium content is 64 mg (2.8 mEq) per gram of oxacillin. The product is buffered with 21 mg dibasic sodium phosphate per gram of oxacillin. Oxacillin for injection, USP is white to off white powder and gives a clear solution upon reconstitution.
OXACILLIN SODIUM
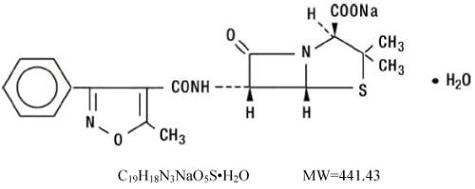
The chemical name of oxacillin sodium is 4-Thia-1-azabicyclo [3.2.0]heptane-2-carboxylic acid, 3,3-dimethyl-6-[[(5-methyl-3-phenyl-4-isoxazolyl) carbonyl] amino]-7-oxo-, monosodium salt, monohydrate, [2S(2α,5α,6β)]. It is resistant to inactivation by the enzyme penicillinase (beta-lactamase). The molecular formula of oxacillin sodium is C19H18N3NaO5SH2O. The molecular weight is 441.43.
-
CLINICAL PHARMACOLOGY
Intravenous administration provides peak serum levels approximately 5 minutes after the injection is completed. Slow I.V. administration of 500 mg gives a peak serum level of 43 mcg/mL after 5 minutes with a half-life of 20 to 30 minutes.
Oxacillin sodium, with normal doses, has insignificant concentrations in the cerebrospinal and ascitic fluids. It is found in therapeutic concentrations in the pleural, bile, and amniotic fluids.
Oxacillin sodium is rapidly excreted as unchanged drug in the urine by glomerular filtration and active tubular secretion. The elimination half-life for oxacillin is about 0.5 hours. Nonrenal elimination includes hepatic inactivation and excretion in bile.
Oxacillin sodium binds to serum protein, mainly albumin. The degree of protein binding reported varies with the method of study and the investigator, but generally has been found to be 94.2 ± 2.1%.
Probenecid blocks the renal tubular secretion of penicillins. Therefore, the concurrent administration of probenecid prolongs the elimination of oxacillin and, consequently, increases the serum concentration.
Intramuscular injections give peak serum levels 30 minutes after injection. A 250 mg dose gives a level of 5.3 mcg/mL while a 500 mg dose peaks at 10.9 mcg/mL. Intravenous injection gives a peak about 5 minutes after the injection is completed. Slow IV dosing with 500 mg gives a 5 minute peak of 43 mcg/mL with a half-life of 20 to 30 minutes.
Microbiology
Penicillinase-resistant penicillins exert a bactericidal action against penicillin susceptible microorganisms during the state of active multiplication. All penicillins inhibit the biosynthesis of the bacterial cell wall.
Mechanism of Resistance
Resistance to penicillins may be mediated by destruction of the beta-lactam ring by a beta-lactamase, altered affinity of penicillin for target, or decreased penetration of the antibiotic to reach the target site.
Cross Resistance
Resistance to oxacillin (or cefoxitin) implies resistance to all other beta-lactam agents, except newer agents with activity against methicillin-resistant Staphylococcus aureus.
Susceptibility Test Methods
When available, the clinical microbiology laboratory should provide of in vitro susceptibility test results for antimicrobial drugs used in local hospitals and practice areas to the physician as periodic reports that describe the susceptibility profile of nosocomial and community-acquired pathogens. These reports should aid the physician in selecting the most effective antibacterial drug for treatment.
Dilution techniques
Quantitative methods are used to determine antimicrobial minimum inhibitory concentrations (MICs). These MICs provide estimates of the susceptibility of bacteria to antimicrobial compounds. The MICs should be determined using a standardized test method1,2 (broth and/or agar). The MIC values should be interpreted according to the criteria in Table 1.
Diffusion techniques
Quantitative methods that require measurement of zone diameters can also provide reproducible estimates of the susceptibility of bacteria to antimicrobial compounds. The zone size should be determined using a standardized method.2,3. It has been determined that the most accurate method to test the susceptibility of microorganisms to penicillinase resistant penicillins, including oxacillin, by disk diffusion is achieved using disks impregnated with 30 mcg cefoxitin. Interpretation involves correlation of the diameter obtained with the cefoxitin disk test with the MIC for oxacillin.2 Reports from the laboratory providing results of the standard single-disk susceptibility test with a 30 microgram cefoxitin disk should be interpreted according to the following criteria in Table 1.
Table 1: Susceptibility Test Interpretive Criteria For Oxacillin S=susceptible, I=intermediate, R-resistant
a In most staphylococcal isolates, oxacillin resistance is mediated by mecA, encoding the penicillin binding protein 2a (PBP2a, also called PBP2'). Isolates that test positive for mecA or PBP2a should be reported as oxacillin resistant.2
b Cefoxitin is used as a surrogate for oxacillin; report oxacillin susceptible or resistant based on the cefoxitin result.2
c If both cefoxitin and oxacillin are tested against S. aureus or S. lugdenensis , and either result is resistant, the organism should be reported as oxacillin resistant.2
d Oxacillin MIC interpretive criteria may overcall resistance for some coagulase-negative staphylococci (CoNS), because some non-S. epidermidis strains for which the oxacillin MICs are 0.5 to 2 mcg/ml lack mecA . For serious infections with CoNS other than S. epidermidis , testing for mecA or for PBP 2a or with cefoxitin disk diffusion may be appropriate for strains for which the oxacillin MICs are 0.5 to 2 mcg/mL.2
Pathogen
Anti-microbial
Disk
Disk Diffusion
Zone Diameter
Minimum Inhibitory
Agent
Content
(mm)a
Concentrations (mcg/mL)
S
I
R
S
I
R
Staphylococcus
aureus and
Oxacillin
-
-
-
-
≤2
(oxacillin)
-
≥4
(oxacillin)
S. lugdenensisc
30 mcg
cefoxitinb
≥22
-
≤21
≤4
(cefoxitin)
-
≥8
(cefoxitin)
Coagulase-negative
Oxacillind
-
-
-
-
≤0.25
-
≥0.5
Staphylococci except
S. lugdenensis
30 mcg
cefoxitinb
≥25
-
≤24
-
-
-
A report of "Susceptible" indicates that the antimicrobial is likely to inhibit the growth of the pathogen if the antimicrobial compound reaches the concentrations at the infection site necessary to inhibit growth of the pathogen. A report of "Intermediate" indicates that the result should be considered equivocal, and if the microorganism is not fully susceptible to alternative, clinically feasible drugs, the test should be repeated. This category implies possible clinical applicability in body sites where the drug is physiologically concentrated. This category also provides a buffer zone that prevents small uncontrolled technical factors from causing major discrepancies in interpretation. A report of "Resistant" indicates that the antimicrobial is not likely to inhibit growth of the pathogen if the antimicrobial compound reaches the concentrations usually achievable at the infection site; other therapy should be selected.
Quality Control
Standardized susceptibility test procedures require the use of laboratory controls to monitor and ensure the accuracy and precision of the supplies and reagents used in the assay, and the techniques of the individuals performing the test.1,2,3 Standard oxacillin powder should provide the following range of MIC values1 noted in Table 2. For the diffusion technique using the 30 mcg cefoxitin disk, the criteria in Table 2 should be achieved.
Table 2: Acceptable Quality Control Ranges for Susceptibility Testing ATCC = American Type Culture Collection
a Despite the lack of reliable disk diffusion interpretive criteria for S. pneumoniae with certain beta-lactams, Streptococcus pneumoniae ATCC® 49619 is the strain designated for QC of all disk diffusion tests with all Streptococcus spp.
b Deterioration of the oxacillin disk content is best assessed with QC organism S. aureus ATCC® 25923, with an acceptable zone diameter for 18 to 24.
Quality Control Organism
Minimal Inhibitory
Concentration (mcg/mL)
Disk Diffusion
Zone Diameters (mm)
Enterococcus faecalis
ATCC® 29212
8 to 32
-
Staphlococcus aureus
ATCC® 25923
-
18 to 24
Staphylococcus aureus
ATCC® 29213
0.12 to 0.5
-
Streptococcus pneumoniae
ATCC® 49619a
-
≤12b
-
INDICATIONS AND USAGE
Oxacillin is indicated in the treatment of infections caused by penicillinase producing staphylococci which have demonstrated susceptibility to the drug. Cultures and susceptibility tests should be performed initially to determine the causative organism and its susceptibility to the drug. (See CLINICAL PHARMACOLOGY: Susceptibility Test Methods).
Oxacillin may be used to initiate therapy in suspected cases of resistant staphylococcal infections prior to the availability of susceptibility test results. Oxacillin should not be used in infections caused by organisms susceptible to penicillin G. If the susceptibility tests indicate that the infection is due to an organism other than a resistant Staphylococcus, therapy should not be continued with oxacillin.
To reduce the development of drug-resistant bacteria and maintain the effectiveness of Oxacillin for Injection, USP and other antibacterial drugs, Oxacillin for Injection, USP should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
- CONTRAINDICATIONS
-
WARNINGS
Serious and occasionally fatal hypersensitivity (anaphylactic shock with collapse) reactions have occurred in patients receiving penicillin. The incidence of anaphylactic shock in all penicillin-treated patients is between 0.015 and 0.04 percent. Anaphylactic shock resulting in death has occurred in approximately 0.002 percent of the patients treated.
When oxacillin therapy is indicated, it should be initiated only after a comprehensive patient drug and allergy history has been obtained. If an allergic reaction occurs, oxacillin should be discontinued and appropriate therapy instituted.
Clostridium difficile associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents, including oxacillin for injection, USP, and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon leading to overgrowth of C. difficile.
C. difficile produces toxins A and B which contribute to the development of CDAD. Hypertoxin producing strains of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibiotic use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents.
If CDAD is suspected or confirmed, ongoing antibiotic use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibiotic treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated.
-
PRECAUTIONS
General
Oxacillin should generally not be administered to patients with a history of sensitivity to any penicillin. Penicillin should be used with caution in individuals with histories of significant allergies and/or asthma. Whenever allergic reactions occur, penicillin should be withdrawn unless, in the opinion of the physician, the condition being treated is life-threatening and amenable only to penicillin therapy. The use of antibiotics may result in overgrowth of nonsusceptible organisms. If new infections due to bacteria or fungi occur, the drug should be discontinued and appropriate measures taken.
Prescribing Oxacillin for Injection, USP in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
Laboratory Tests
Bacteriologic studies to determine the causative organisms and their susceptibility to oxacillin should be performed (See CLINICAL PHARMACOLOGY: Microbiology). In the treatment of suspected staphylococcal infections, therapy should be changed to another active agent if culture tests fail to demonstrate the presence of staphylococci.
Periodic assessment of organ system function including renal, hepatic, and hematopoietic should be made during prolonged therapy with oxacillin.
Blood cultures, white blood cell, and differential cell counts should be obtained prior to initiation of therapy and at least weekly during therapy with oxacillin.
Periodic urinalysis, blood urea nitrogen, and creatinine determinations should be performed during therapy with oxacillin and dosage alterations should be considered if these values become elevated. If any impairment of renal function is suspected or known to exist, a reduction in the total dosage should be considered and blood levels monitored to avoid possible neurotoxic reactions.
AST (SGOT) and ALT (SGPT) values should be obtained periodically during therapy to monitor for possible liver function abnormalities.
Drug Interactions
Tetracycline, a bacteriostatic antibiotic, may antagonize the bactericidal effect of penicillin and concurrent use of these drugs should be avoided.
Oxacillin blood levels may be increased and prolonged by concurrent administration of probenecid which blocks the renal tubular secretion of penicillins. Probenecid decreases the apparent volume of distribution and slows the rate of excretion by competitively inhibiting renal tubular secretion of penicillins.
Oxacillin-probenecid therapy should be limited to those infections where very high serum levels of oxacillin are necessary.
Carcinogenesis, Mutagenesis, Impairment of Fertility
No long-term animal studies have been conducted with these drugs. Studies on reproduction (nafcillin) in rats and rabbits reveal no fetal or maternal abnormalities before conception and continuously through weaning (one generation).
Pregnancy
Pregnancy Category B
Reproduction studies performed in the mouse, rat, and rabbit have revealed no evidence of impaired fertility or harm to the fetus due to the penicillinase-resistant penicillins. Human experience with the penicillins during pregnancy has not shown any positive evidence of adverse effects on the fetus. There are, however, no adequate or well-controlled studies in pregnant women showing conclusively that harmful effects of these drugs on the fetus can be excluded. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed.
Nursing Mothers
Penicillins are excreted in human milk. Caution should be exercised when penicillins are administered to a nursing woman.
Pediatric Use
Because of incompletely developed renal function in pediatric patients, oxacillin may not be completely excreted, with abnormally high blood levels resulting. Frequent blood levels are advisable in this group with dosage adjustments when necessary. All pediatric patients treated with penicillins should be monitored closely for clinical and laboratory evidence of toxic or adverse effects. Safety and effectiveness in pediatric patients have not been established.
Geriatric Use
Clinical studies of oxacillin for injection did not include sufficient number of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
This drug is known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function.
Oxacillin for Injection contains 64 mg (2.8 mEq) of sodium per gram of oxacillin. At the usual recommended doses, patients would receive between 64 and 384 mg/day (2.8 and 16.7 mEq) of sodium. The geriatric population may respond with a blunted natriuresis to salt loading. This may be clinically important with regard to such diseases as congestive heart failure.
Information for Patients
Patients should be counseled that antibacterial drugs including Oxacillin for Injection, USP should only be used to treat bacterial infections. They do not treat viral infections (e.g., the common cold). When Oxacillin for Injection, USP is prescribed to treat a bacterial infection, patients should be told that although it is common to feel better early in the course of therapy, the medication should be taken exactly as directed. Skipping doses or not completing the full course of therapy may: (1) decrease the effectiveness of the immediate treatment, and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by Oxacillin for Injection, USP or other antibacterial drugs in the future.
Diarrhea is a common problem caused by antibiotics which usually ends when the antibiotic is discontinued. Sometimes after starting treatment with antibiotics, patients can develop watery and bloody stools (with or without stomach cramps and fever) even as late as two or more months after having taken the last dose of the antibiotic. If this occurs, patients should contact their physician as soon as possible.
-
ADVERSE REACTIONS
Body as a Whole
The reported incidence of allergic reactions to penicillin ranges from 0.7 to 10 percent (see WARNINGS). Sensitization is usually the result of treatment but some individuals have had immediate reactions when first treated. In such cases, it is thought that the patients may have had prior exposure to the drug via trace amounts present in milk and vaccines.
Two types of allergic reactions to penicillins are noted clinically, immediate and delayed.
Immediate reactions usually occur within 20 minutes of administration and range in severity from urticaria and pruritus to angioneurotic edema, laryngospasm, bronchospasm, hypotension, vascular collapse, and death. Such immediate anaphylactic reactions are very rare (see WARNINGS) and usually occur after parenteral therapy but have occurred in patients receiving oral therapy. Another type of immediate reaction, an accelerated reaction, may occur between 20 minutes and 48 hours after administration and may include urticaria, pruritus, and fever. Although laryngeal edema, laryngospasm, and hypotension occasionally occur, fatality is uncommon.
Delayed allergic reactions to penicillin therapy usually occur after 48 hours and sometimes as late as 2 to 4 weeks after initiation of therapy.
Manifestations of this type of reaction include serum sickness-like symptoms (i.e, fever, malaise, urticaria, myalgia, arthralgia, abdominal pain) and various skin rashes. Nausea, vomiting, diarrhea, stomatitis, black or hairy tongue, and other symptoms of gastrointestinal irritation may occur, especially during oral penicillin therapy.
Nervous System Reactions
Neurotoxic reactions similar to those observed with penicillin G may occur with large intravenous doses of oxacillin especially with patients with renal insufficiency.
Urogenital Reactions
Renal tubular damage and interstitial nephritis have been associated with the administration of oxacillin. Manifestations of this reaction may include rash, fever, eosinophilia, hematuria, proteinuria, and renal insufficiency. Nephropathy induced by penicillins does not appear to be dose-related and is generally reversible upon prompt discontinuation of therapy.
Gastrointestinal Reactions
Pseudomembranous colitis has been reported with the use of oxacillin. The onset of pseudomembranous colitis symptoms may occur during or after antibiotic treatment (see WARNINGS).
Metabolic Reactions
Agranulocytosis, neutropenia, and bone marrow depression have been associated with the use of oxacillin. Hepatotoxicity, characterized by fever, nausea, and vomiting associated with abnormal liver function tests, mainly elevated SGOT levels, has been associated with the use of oxacillin.
To report SUSPECTED ADVERSE REACTIONS, contact FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
-
OVERDOSAGE
The signs and symptoms of oxacillin overdosage are those described in the ADVERSE REACTIONS section. If signs or symptoms occur, discontinue use of the medication, treat symptomatically, and institute appropriate supportive measures.
-
DOSAGE AND ADMINISTRATION
Bacteriologic studies to determine the causative organisms and their susceptibility to oxacillin should always be performed. Duration of therapy varies with the type of severity of infection as well as the overall condition of the patient, therefore it should be determined by the clinical and bacteriological response of the patient. In severe staphylococcal infections, therapy with oxacillin should be continued for at least 14 days. Therapy should be continued for at least 48 hours after the patient has become afebrile, asymptomatic, and cultures are negative. Treatment of endocarditis and osteomyelitis may require a longer duration of therapy.
With intravenous administration, particularly in elderly patients, care should be taken because of the possibility of thrombophlebitis.
RECOMMENDED DOSAGES FOR OXACILLIN FOR INJECTION, USP Drug
Adults
Infants and Children
<40 kg (88 lbs)
Other
Recommendations
Oxacillin
250 to 500 mg
IM or IV every
4 to 6 hours
(mild to moderate infections)
50 mg/kg/day
IM or IV in equally
divided doses every
6 hours (mild to
moderate infections)
1 gram IM or IV
every 4 to 6 hours
(severe infections)
100 mg/kg/day
IM or IV in equally divided doses every
4 to 6 hours
(severe infections)
Premature and Neonates
25 mg/kg/day
IM or IV
Directions for use
For Intramuscular Use: Use Sterile Water for Injection, USP. Add 5.4 mL to the 1 gram vial and 10.6 mL to the 2 gram vial. Shake well until a clear solution is obtained. After reconstitution, vials will contain 250 mg of active drug per 1.5 mL of solution. The reconstituted solution is stable for 3 days at 70° F or for one week under refrigeration (40° F).
For Direct Intravenous Use: Use Sterile Water for Injection, USP or Sodium Chloride Injection, USP. Add 10 mL to the 1 gram vial and 20 mL to the 2 gram vial. Withdraw the entire contents and administer slowly over a period of approximately 10 minutes.
For Administration by Intravenous Drip: Reconstitute as directed above (For Direct Intravenous Use) prior to diluting with Intravenous Solution.
STABILITY PERIODS FOR OXACILLIN FOR INJECTION, USP Concentration
mg/mL
Sterile
Water for
Injection,
USP
0.9%
Sodium
Chloride
Injection,
USP
M/6
Molar
Sodium
Lactate
Solution
5%
Dextrose
in water
5%
Dextrose
in 0.45%
Sodium
Chloride
10%
Invert
Sugar
Injection,
USP
Lactated
Ringers
Solution
ROOM TEMPERATURE (25°C)
10 to 100
4 Days
4 Days
10 to 30
24 Hrs
24 Hrs
0.5 to 2
6 Hrs
6 Hrs
6 Hrs
REFRIGERATION (4°C)
10 to 100
7 Days
7 Days
10 to 30
4 Days
4 Days
4 Days
4 Days
4 Days
FROZEN (-15°C)
50 to 100
30 Days
250/1.5 mL
30 Days
100
30 Days
10 to 100
30 Days
30 Days
30 Days
30 Days
30 Days
Stability studies on Oxacillin Sodium at concentrations of 0.5 mg/mL and 2 mg/mL in various intravenous solutions listed below indicate the drug will lose less than 10% activity at room temperature (70°F) during a 6-hour period.
IV Solution
5% Dextrose in Normal Saline
Only those solutions listed above should be used for the intravenous infusion of oxacillin sodium. The concentration of the antibiotic should fall within the range specified. The drug concentration and the rate and volume of the infusion should be adjusted so that the total dose of oxacillin is administered before the drug loses its stability in the solution in use.
If another agent is used in conjunction with oxacillin therapy, it should not be physically mixed with oxacillin but should be administered separately.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration whenever solution and container permit.
Do not add supplementary medication to oxacillin for injection, USP.
-
HOW SUPPLIED
Oxacillin for injection, USP contains oxacillin sodium equivalent to 1 or 2 grams oxacillin per vial.
NDC: 64679-698-01 1 gram vial, packaged in carton of ten vials
NDC: 64679-698-03 1 gram vial, packaged in carton of one vial
NDC: 64679-699-01 2 grams vial, packaged in carton of ten vials
NDC: 64679-699-03 2 grams vial, packaged in carton of one vial
Store dry powder at 20°-25°C (68°-77°F) [See USP Controlled Room Temperature].
-
REFERENCES
- Clinical and Laboratory Standards Institute (CLSI). Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically; Approved Standard-Tenth Edition. CLSI Document M07-A10. Clinical and Laboratory Standards Institute, 950 West Valley Road, Suite 2500, Wayne, Pennsylvania 19087, USA, 2015.
- Clinical and Laboratory Standards Institute (CLSI). Performance Standards for Antimicrobial Susceptibility Testing; Twenty-fifth Informational Supplement. CLSI Document M100-S25. Clinical and Laboratory Standards Institute, 950 West Valley Road, Suite 2500, Wayne, Pennsylvania 19087, USA, 2015.
- Clinical and Laboratory Standards Institute (CLSI). Performance Standards for Antimicrobial Disk Susceptibility Tests; Approved Standard Twelfth Edition. CLSI Document M02-A12. Clinical and Laboratory Standards Institute, 950 West Valley Road, Suite 2500, Wayne, Pennsylvania 19087, USA, 2015.
-
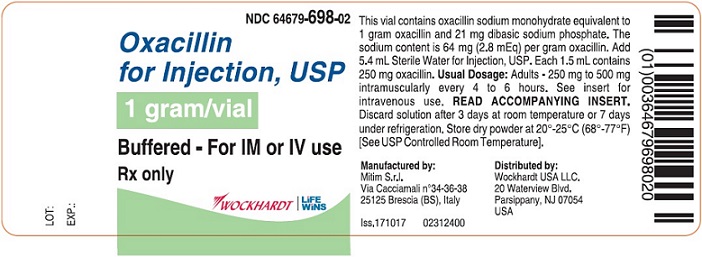
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
GENERIC: Oxacillin Sodium
DOSAGE: Injection
ADMINSTRATION: Intramuscular, Intravenous
NDC: 64679-698-02
STRENGTH: 1 gram/vial
QTY: 1 gram vial label
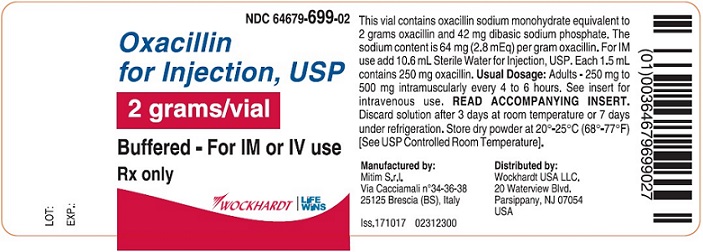
GENERIC: Oxacillin Sodium
DOSAGE: Injection
ADMINSTRATION: Intramuscular, Intravenous
NDC: 64679-699-02
STRENGTH: 2 grams/vial
QTY: 2 grams vial label
-
INGREDIENTS AND APPEARANCE
OXACILLIN
oxacillin injection, powder, for solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 22607-698 Route of Administration INTRAMUSCULAR, INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength OXACILLIN SODIUM (UNII: G0V6C994Q5) (OXACILLIN - UNII:UH95VD7V76) OXACILLIN 1 g in 20 mL Inactive Ingredients Ingredient Name Strength SODIUM PHOSPHATE, DIBASIC (UNII: GR686LBA74) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 22607-698-01 10 in 1 VIAL 07/31/2017 1 NDC: 22607-698-02 20 mL in 1 VIAL; Type 0: Not a Combination Product 2 NDC: 22607-698-03 1 in 1 CARTON 07/31/2017 2 NDC: 22607-698-02 20 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA207147 07/31/2017 OXACILLIN
oxacillin injection, powder, for solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 22607-699 Route of Administration INTRAMUSCULAR, INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength OXACILLIN SODIUM (UNII: G0V6C994Q5) (OXACILLIN - UNII:UH95VD7V76) OXACILLIN 2 g in 20 mL Inactive Ingredients Ingredient Name Strength SODIUM PHOSPHATE, DIBASIC (UNII: GR686LBA74) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 22607-699-01 10 in 1 CARTON 07/31/2017 1 NDC: 22607-699-02 20 mL in 1 VIAL; Type 0: Not a Combination Product 2 NDC: 22607-699-03 1 in 1 CARTON 07/31/2017 2 NDC: 22607-699-02 20 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA207147 07/31/2017 Labeler - Mitim S.r.l. (438137085) Registrant - Wockhardt Limited (650069115) Establishment Name Address ID/FEI Business Operations Mitim S.r.l. 438137085 ANALYSIS(22607-698, 22607-699) , LABEL(22607-698, 22607-699) , MANUFACTURE(22607-698, 22607-699) , PACK(22607-698, 22607-699)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.