DICLOFENAC EPOLAMINE system
diclofenac epolamine by
Drug Labeling and Warnings
diclofenac epolamine by is a Prescription medication manufactured, distributed, or labeled by Teva Pharmaceuticals USA Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% safely and effectively. See full prescribing information for DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3%.
DICLOFENAC EPOLAMINE TOPICAL SYSTEM
Initial U.S. Approval: 1988WARNING: RISK OF SERIOUS CARDIOVASCULAR and GASTROINTESTINAL EVENTS
See full prescribing information for complete boxed warning.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) cause an increased risk of serious cardiovascular thrombotic events, including myocardial infarction and stroke, which can be fatal. This risk may occur early in treatment and may increase with duration of use (5.1)
- DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% is contraindicated in the setting of coronary artery bypass graft (CABG) surgery (4, 5.1)
- NSAIDs cause an increased risk of serious gastrointestinal (GI) adverse events including bleeding, ulceration, and perforation of the stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Elderly patients and patients with a prior history of peptic ulcer disease and/or GI bleeding are at greater risk for serious GI events (5.2)
RECENT MAJOR CHANGES
Indications and Usage 03/2019 INDICATIONS AND USAGE
- DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% is a nonsteroidal anti-inflammatory drug (NSAID), and is indicated for the topical treatment of acute pain due to minor strains, sprains, and contusions in adults and pediatric patients 6 years and older. (1)
DOSAGE AND ADMINISTRATION
- Use the lowest effective dosage for shortest duration consist with the individual patient treatment goals (2.1)
- The recommended dose of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% for adults and pediatric patients 6 years and older is one (1) topical system to the most painful area twice a day. (2)
- DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% should not be applied to damaged or non-intact skin. (2)
DOSAGE FORMS AND STRENGTHS
DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3%, for topical use. Each individual topical system is debossed. (3)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- Hepatotoxicity: Inform patients of warning signs and symptoms of hepatotoxicity. Discontinue if abnormal liver tests persist or worsen or if clinical signs and symptoms of liver disease develop (5.3)
- Hypertension: Patients taking some antihypertensive medications may have impaired response to these therapies when taking NSAIDs. Monitor blood pressure (5.4, 7)
- Heart Failure and Edema: Avoid use of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% in patients with severe heart failure unless benefits are expected to outweigh risk of worsening heart failure (5.5)
- Renal Toxicity: Monitor renal function in patients with renal or hepatic impairment, heart failure, dehydration, or hypovolemia. Avoid use of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% in patients with advanced renal disease unless benefits are expected to outweigh risk of worsening renal function (5.6)
- Anaphylactic Reactions: Seek emergency help if an anaphylactic reaction occurs (5.7)
- Exacerbation of Asthma Related to Aspirin Sensitivity: DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% is contraindicated in patients with aspirin-sensitive asthma. Monitor patients with preexisting asthma (without aspirin sensitivity) (5.8)
- Serious Skin Reactions: Discontinue DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% at first appearance of skin rash or other signs of hypersensitivity (5.9)
- Premature Closure of Fetal Ductus Arteriosus: Avoid use in pregnant women starting at 30 weeks of gestation (5.10, 8.1)
- Hematologic Toxicity: Monitor hemoglobin or hematocrit in patients with any signs or symptoms of anemia (5.11, 7)
ADVERSE REACTIONS
The most common adverse reactions in DICLOFENAC EPOLAMINE TOPICAL SYSTEM and placebo-treated adult patients were pruritus (5% and 8%, respectively) and nausea (3% and 2%, respectively) (6.1). The most common adverse reactions in DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% treated pediatric patients were headache (9%) and application site pruritus (7%) (6.1).
To report SUSPECTED ADVERSE REACTIONS, contact Teva Pharmaceuticals USA, Inc.at 1-866-832-8537 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
- Drugs that Interfere with Hemostasis (e.g. warfarin, aspirin, SSRIs/SNRIs): Monitor patients for bleeding who are concomitantly using DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% with drugs that interfere with hemostasis. Concomitant use of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% and analgesic doses of aspirin is not generally recommended (7)
- ACE Inhibitors, Angiotensin Receptor Blockers (ARB), or Beta-Blockers: Concomitant use with DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% may diminish the antihypertensive effect of these drugs. Monitor blood pressure (7)
- ACE Inhibitors and ARBs: Concomitant use with DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% in elderly, volume depleted, or those with renal impairment may result in deterioration of renal function. In such high risk patients, monitor for signs of worsening renal function (7)
- Diuretics: NSAIDs can reduce natriuretic effect of furosemide and thiazide diuretics. Monitor patients to assure diuretic efficacy including antihypertensive effects (7)
- Digoxin: Concomitant use with DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% may increase serum concentration and prolong half-life of digoxin. Monitor serum digoxin levels (7)
USE IN SPECIFIC POPULATIONS
- Pregnancy: Use of NSAIDs during the third trimester of pregnancy increases the risk of premature closure of the fetal ductus arteriosus. Avoid use of NSAIDs in pregnant women starting at 30 weeks of gestation (5.10, 8.1)
- Infertility: NSAIDs are associated with reversible infertility. Consider withdrawal of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% in women who have difficulties conceiving (8.3)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 5/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: RISK OF SERIOUS CARDIOVASCULAR and GASTROINTESTINAL EVENTS
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 General Dosing Instructions
2.2 Special Precautions
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Cardiovascular Thrombotic Events
5.2 Gastrointestinal Bleeding, Ulceration, and Perforation
5.3 Hepatotoxicity
5.4 Hypertension
5.5 Heart Failure and Edema
5.6 Renal Toxicity and Hyperkalemia
5.7 Anaphylactic Reactions
5.8 Exacerbation of Asthma Related to Aspirin Sensitivity
5.9 Serious Skin Reactions
5.10 Premature Closure of Fetal Ductus Arteriosus
5.11 Hematologic Toxicity
5.12 Masking of Inflammation and Fever
5.13 Laboratory Monitoring
5.14 Accidental Exposure in Children
5.15 Eye Exposure
5.16 Oral Nonsteroidal Anti-inflammatory Drugs
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Strains, Sprains, and Contusions
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: RISK OF SERIOUS CARDIOVASCULAR and GASTROINTESTINAL EVENTS
Cardiovascular Thrombotic Events
- Nonsteroidal anti-inflammatory drugs (NSAIDs) cause an increased risk of serious cardiovascular thrombotic events, including myocardial infarction and stroke, which can be fatal. This risk may occur early in treatment and may increase with duration of use [see Warnings and Precautions (5.1)].
- DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% is contraindicated in the setting of coronary artery bypass graft (CABG) surgery [see Contraindications (4) and Warnings and Precautions (5.1)].
Gastrointestinal Bleeding, Ulceration, and Perforation
- NSAIDs cause an increased risk of serious gastrointestinal (GI) adverse events including bleeding, ulceration, and perforation of the stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Elderly patients and patients with a prior history of peptic ulcer disease and/or GI bleeding are at greater risk for serious GI events [see Warnings and Precautions (5.2)].
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 General Dosing Instructions
Use the lowest effective dosage for the shortest duration consistent with individual patient treatment goals [see Warnings and Precautions (5)].
The recommended dose of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% is one (1) topical system to the most painful area twice a day both in adults and pediatric patients 6 years of age and older.
2.2 Special Precautions
- Inform patients that, if DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% begins to peel-off, the edges of the topical system may be taped down. If problems with adhesion persist, patients may overlay the topical system with a mesh netting sleeve, where appropriate (e.g. to secure topical systems applied to ankles, knees, or elbows). The mesh netting sleeve (e.g. Curad® Hold Tite™, Surgilast® Tubular Elastic Dressing) must allow air to pass through and not be occlusive (non-breathable).
- Do not apply DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% to non-intact or damaged skin resulting from any etiology e.g. exudative dermatitis, eczema, infected lesion, burns or wounds.
- Do not wear a DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% when bathing or showering.
- Wash your hands after applying, handling or removing the topical system.
- Avoid eye contact.
- Do not use combination therapy with DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% and an oral NSAID unless the benefit outweighs the risk and conduct periodic laboratory evaluations.
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% is contraindicated in the following patients:
- Known hypersensitivity (e.g., anaphylactic reactions and serious skin reactions) to diclofenac or any components of the drug product [see Warnings and Precautions (5.7, 5.9)]
- History of asthma, urticaria, or other allergic-type reactions after taking aspirin or other NSAIDs. Severe, sometimes fatal, anaphylactic reactions to NSAIDs have been reported in such patients [see Warnings and Precautions (5.7, 5.8)]
- In the setting of coronary artery bypass graft (CABG) surgery [see Warnings and Precautions (5.1)]
- DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% is contraindicated for use on non-intact or damaged skin resulting from any etiology, including exudative dermatitis, eczema, infection lesions, burns or wounds.
-
5 WARNINGS AND PRECAUTIONS
5.1 Cardiovascular Thrombotic Events
Clinical trials of several COX-2 selective and nonselective NSAIDs of up to three years duration have shown an increased risk of serious cardiovascular (CV) thrombotic events, including myocardial infarction (MI) and stroke, which can be fatal. Based on available data, it is unclear that the risk for CV thrombotic events is similar for all NSAIDs. The relative increase in serious CV thrombotic events over baseline conferred by NSAID use appears to be similar in those with and without known CV disease or risk factors for CV disease. However, patients with known CV disease or risk factors had a higher absolute incidence of excess serious CV thrombotic events, due to their increased baseline rate. Some observational studies found that this increased risk of serious CV thrombotic events began as early as the first weeks of treatment. The increase in CV thrombotic risk has been observed most consistently at higher doses.
To minimize the potential risk for an adverse CV event in NSAID-treated patients, use the lowest effective dose for the shortest duration possible. Physicians and patients should remain alert for the development of such events, throughout the entire treatment course, even in the absence of previous CV symptoms. Patients should be informed about the symptoms of serious CV events and the steps to take if they occur.
There is no consistent evidence that concurrent use of aspirin mitigates the increased risk of serious CV thrombotic events associated with NSAID use. The concurrent use of aspirin and an NSAID, such as diclofenac, increases the risk of serious gastrointestinal (GI) events [see Warnings and Precautions (5.2)].
Status Post Coronary Artery Bypass Graft (CABG) Surgery
Two large, controlled clinical trials of a COX-2 selective NSAID for the treatment of pain in the first 10–14 days following CABG surgery found an increased incidence of myocardial infarction and stroke. NSAIDs are contraindicated in the setting of CABG [see Contraindications (4)].
Post-MI Patients
Observational studies conducted in the Danish National Registry have demonstrated that patients treated with NSAIDs in the post-MI period were at increased risk of reinfarction, CV-related death, and all-cause mortality beginning in the first week of treatment. In this same cohort, the incidence of death in the first year post-MI was 20 per 100 person years in NSAID-treated patients compared to 12 per 100 person years in non-NSAID exposed patients. Although the absolute rate of death declined somewhat after the first year post-MI, the increased relative risk of death in NSAID users persisted over at least the next four years of follow-up.
Avoid the use of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% in patients with a recent MI unless the benefits are expected to outweigh the risk of recurrent CV thrombotic events. If DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% is used in patients with a recent MI, monitor patients for signs of cardiac ischemia.
5.2 Gastrointestinal Bleeding, Ulceration, and Perforation
NSAIDs, including diclofenac, cause serious gastrointestinal (GI) adverse events including inflammation, bleeding, ulceration, and perforation of the esophagus, stomach, small intestine, or large intestine, which can be fatal. These serious adverse events can occur at any time, with or without warning symptoms, in patients treated with NSAIDs.
Only one in five patients who develop a serious upper GI adverse event on NSAID therapy is symptomatic. Upper GI ulcers, gross bleeding, or perforation caused by NSAIDs occurred in approximately 1% of patients treated for 3-6 months, and in about 2%-4% of patients treated for one year. However, even short-term NSAID therapy is not without risk.
Risk Factors for GI Bleeding, Ulceration, and Perforation
Patients with a prior history of peptic ulcer disease and/or GI bleeding who used NSAIDs had a greater than 10-fold increased risk for developing a GI bleed compared to patients without these risk factors. Other factors that increase the risk of GI bleeding in patients treated with NSAIDs include longer duration of NSAID therapy; concomitant use of oral corticosteroids, aspirin, anticoagulants, or selective serotonin reuptake inhibitors (SSRIs); smoking; use of alcohol; older age; and poor general health status. Most postmarketing reports of fatal GI events occurred in elderly or debilitated patients. Additionally, patients with advanced liver disease and/or coagulopathy are at increased risk for GI bleeding.
Strategies to Minimize the GI Risks in NSAID-Treated Patients:
- Use the lowest effective dosage for the shortest possible duration.
- Avoid administration of more than one NSAID at a time.
- Avoid use in patients at higher risk unless benefits are expected to outweigh the increased risk of bleeding. For such patients, as well as those with active GI bleeding, consider alternate therapies other than NSAIDs.
- Remain alert for signs and symptoms of GI ulceration and bleeding during NSAID therapy.
- If a serious GI adverse event is suspected, promptly initiate evaluation and treatment, and discontinue DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% until a serious GI adverse event is ruled out.
- In the setting of concomitant use of low-dose aspirin for cardiac prophylaxis, monitor patients more closely for evidence of GI bleeding [see Drug Interactions (7)].
5.3 Hepatotoxicity
In clinical trials of oral diclofenac containing products, meaningful elevations (i.e., more than 3 times the ULN) of AST (SGOT) were observed in about 2% of approximately 5,700 patients at some time during diclofenac treatment (ALT was not measured in all studies).
In a large open-label, controlled trial of 3,700 patients treated with oral diclofenac sodium for 2-6 months, patients were monitored first at 8 weeks and 1,200 patients were monitored again at 24 weeks. Meaningful elevations of ALT and/or AST occurred in about 4% of the 3,700 patients and included marked elevations (greater than 8 times the ULN) in about 1% of the 3,700 patients. In that open-label study, a higher incidence of borderline (less than 3 times the ULN), moderate (3-8 times the ULN), and marked (greater than 8 times the ULN) elevations of ALT or AST was observed in patients receiving diclofenac when compared to other NSAIDs. Elevations in transaminases were seen more frequently in patients with osteoarthritis than in those with rheumatoid arthritis.
Almost all meaningful elevations in transaminases were detected before patients became symptomatic. Abnormal tests occurred during the first 2 months of therapy with diclofenac in 42 of the 51 patients in all trials who developed marked transaminase elevations.
In postmarketing reports, cases of drug-induced hepatotoxicity have been reported in the first month, and in some cases, the first 2 months of therapy, but can occur at any time during treatment with diclofenac. Postmarketing surveillance has reported cases of severe hepatic reactions, including liver necrosis, jaundice, fulminant hepatitis with and without jaundice, and liver failure. Some of these reported cases resulted in fatalities or liver transplantation.
In a European retrospective population-based, case-controlled study, 10 cases of diclofenac associated drug-induced liver injury with current use compared with non-use of diclofenac were associated with a statistically significant 4-fold adjusted odds ratio of liver injury. In this particular study, based on an overall number of 10 cases of liver injury associated with diclofenac, the adjusted odds ratio increased further with female gender, doses of 150 mg or more, and duration of use for more than 90 days.
Physicians should measure transaminases at baseline and periodically in patients receiving long-term therapy with diclofenac, because severe hepatotoxicity may develop without a prodrome of distinguishing symptoms. The optimum times for making the first and subsequent transaminase measurements are not known. Based on clinical trial data and postmarketing experiences, transaminases should be monitored within 4 to 8 weeks after initiating treatment with diclofenac. However, severe hepatic reactions can occur at any time during treatment with diclofenac.
If abnormal liver tests persist or worsen, if clinical signs and/or symptoms consistent with liver disease develop, or if systemic manifestations occur (e.g., eosinophilia, rash, abdominal pain, diarrhea, dark urine, etc.), DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% should be discontinued immediately.
Inform patients of the warning signs and symptoms of hepatotoxicity (e.g., nausea, fatigue, lethargy, diarrhea, pruritus, jaundice, right upper quadrant tenderness, and "flu-like" symptoms). If clinical signs and symptoms consistent with liver disease develop, or if systemic manifestations occur (e.g., eosinophilia, rash, etc.), discontinue DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% immediately, and perform a clinical evaluation of the patient.
To minimize the potential risk for an adverse liver related event in patients treated with DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3%, use the lowest effective dose for the shortest duration possible. Exercise caution when prescribing DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% with concomitant drugs that are known to be potentially hepatotoxic (e.g., acetaminophen, antibiotics, antiepileptics).
5.4 Hypertension
NSAIDs, including DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3%, can lead to new onset of hypertension or worsening of preexisting hypertension, either of which may contribute to the increased incidence of CV events. Patients taking angiotensin converting enzyme (ACE) inhibitors, thiazide diuretics, or loop diuretics may have impaired response to these therapies when taking NSAIDs [see Drug Interactions (7)].
Monitor blood pressure (BP) during the initiation of NSAID treatment and throughout the course of therapy.
5.5 Heart Failure and Edema
The Coxib and traditional NSAID Trialists' Collaboration meta-analysis of randomized controlled trials demonstrated an approximately two-fold increase in hospitalizations for heart failure in COX-2 selective-treated patients and nonselective NSAID-treated patients compared to placebo-treated patients. In a Danish National Registry study of patients with heart failure, NSAID use increased the risk of MI, hospitalization for heart failure, and death.
Additionally, fluid retention and edema have been observed in some patients treated with NSAIDs. Use of diclofenac may blunt the CV effects of several therapeutic agents used to treat these medical conditions (e.g., diuretics, ACE inhibitors, or angiotensin receptor blockers [ARBs]) [see Drug Interactions (7)].
Avoid the use of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% in patients with severe heart failure unless the benefits are expected to outweigh the risk of worsening heart failure. If DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% is used in patients with severe heart failure, monitor patients for signs of worsening heart failure.
5.6 Renal Toxicity and Hyperkalemia
Renal Toxicity
Long-term administration of NSAIDs has resulted in renal papillary necrosis and other renal injury.
Renal toxicity has also been seen in patients in whom renal prostaglandins have a compensatory role in the maintenance of renal perfusion. In these patients, administration of an NSAID may cause a dose-dependent reduction in prostaglandin formation and, secondarily, in renal blood flow, which may precipitate overt renal decompensation. Patients at greatest risk of this reaction are those with impaired renal function, dehydration, hypovolemia, heart failure, liver dysfunction, those taking diuretics and ACE inhibitors or ARBs, and the elderly. Discontinuation of NSAID therapy is usually followed by recovery to the pretreatment state.
No information is available from controlled clinical studies regarding the use of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% in patients with advanced renal disease. The renal effects of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% may hasten the progression of renal dysfunction in patients with pre-existing renal disease.
Correct volume status in dehydrated or hypovolemic patients prior to initiating DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3%. Monitor renal function in patients with renal or hepatic impairment, heart failure, dehydration, or hypovolemia during use of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% [see Drug Interactions (7)]. Avoid the use of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% in patients with advanced renal disease unless the benefits are expected to outweigh the risk of worsening renal function. If DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% is used in patients with advanced renal disease, monitor patients for signs of worsening renal function.
5.7 Anaphylactic Reactions
Diclofenac has been associated with anaphylactic reactions in patients with and without known hypersensitivity to diclofenac and in patients with aspirin-sensitive asthma [see Contraindications (4) and Warnings and Precautions (5.8)]. Seek emergency help if an anaphylactic reaction occurs.
5.8 Exacerbation of Asthma Related to Aspirin Sensitivity
A subpopulation of patients with asthma may have aspirin-sensitive asthma which may include chronic rhinosinusitis complicated by nasal polyps; severe, potentially fatal bronchospasm; and/or intolerance to aspirin and other NSAIDs. Because cross-reactivity between aspirin and other NSAIDs has been reported in such aspirin-sensitive patients, DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% is contraindicated in patients with this form of aspirin sensitivity [see Contraindications (4)]. When DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% is used in patients with preexisting asthma (without known aspirin sensitivity), monitor patients for changes in the signs and symptoms of asthma.
5.9 Serious Skin Reactions
NSAIDs, including diclofenac, can cause serious skin adverse reactions such as exfoliative dermatitis, Stevens-Johnson Syndrome (SJS), and toxic epidermal necrolysis (TEN), which can be fatal. These serious events may occur without warning. Inform patients about the signs and symptoms of serious skin reactions, and to discontinue the use of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% at the first appearance of skin rash or any other sign of hypersensitivity. DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% is contraindicated in patients with previous serious skin reactions to NSAIDs [see Contraindications (4)].
5.10 Premature Closure of Fetal Ductus Arteriosus
Diclofenac may cause premature closure of the fetal ductus arteriosus. Avoid use of NSAIDs, including DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3%, in pregnant women starting at 30 weeks of gestation (third trimester) [see Use in Specific Populations (8.1)].
5.11 Hematologic Toxicity
Anemia has occurred in NSAID-treated patients. This may be due to occult or gross blood loss, fluid retention, or an incompletely described effect on erythropoiesis. If a patient treated with DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% has any signs or symptoms of anemia, monitor hemoglobin or hematocrit.
NSAIDs, including DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3%, may increase the risk of bleeding events. Co-morbid conditions such as coagulation disorders, concomitant use of warfarin, other anticoagulants, antiplatelet agents (e.g., aspirin), serotonin reuptake inhibitors (SSRIs) and serotonin norepinephrine reuptake inhibitors (SNRIs) may increase this risk. Monitor these patients for signs of bleeding [see Drug Interactions (7)].
5.12 Masking of Inflammation and Fever
The pharmacological activity of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% in reducing inflammation, and possibly fever, may diminish the utility of diagnostic signs in detecting infections.
5.13 Laboratory Monitoring
Because serious GI bleeding, hepatotoxicity, and renal injury can occur without warning symptoms or signs, consider monitoring patients on long-term NSAID treatment with a CBC and a chemistry profile periodically [see Warnings and Precautions (5.2, 5.3, 5.6)].
5.14 Accidental Exposure in Children
Even a used DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% contains a large amount of diclofenac epolamine (as much as 170 mg). The potential therefore exists for a small child or pet to suffer serious adverse effects from chewing or ingesting a new or used DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3%. It is important for patients to store and dispose of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% out of the reach of children and pets.
5.15 Eye Exposure
Avoid contact of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% with eyes and mucosa. Advise patients that if eye contact occurs, immediately wash out the eye with water or saline and consult a physician if irritation persists for more than an hour.
5.16 Oral Nonsteroidal Anti-inflammatory Drugs
Concomitant use of oral and topical NSAIDs may result in a higher rate of hemorrhage, more frequent abnormal creatinine, urea and hemoglobin. Do not use combination therapy with DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% and an oral NSAID unless the benefit outweighs the risk.
-
6 ADVERSE REACTIONS
The following adverse reactions are discussed in greater detail in other sections of the labeling:
- Cardiovascular Thrombotic Events [see Warnings and Precautions (5.1)]
- GI Bleeding, Ulceration and Perforation [see Warnings and Precautions (5.2)]
- Hepatotoxicity [see Warnings and Precautions (5.3)]
- Hypertension [see Warnings and Precautions (5.4)]
- Heart Failure and Edema [see Warnings and Precautions (5.5)]
- Renal Toxicity and Hyperkalemia [see Warnings and Precautions (5.6)]
- Anaphylactic Reactions [see Warnings and Precautions (5.7)]
- Serious Skin Reactions [see Warnings and Precautions (5.9)]
- Hematologic Toxicity [see Warnings and Precautions (5.11)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared with rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Adult Clinical Trials Experience
In controlled trials during the premarketing development of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3%, approximately 600 patients with minor sprains, strains, and contusions were treated with DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% for up to two weeks.
Adverse Events Leading to Discontinuation of Treatment
In the controlled trials, 3% of patients in both the DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% and placebo groups discontinued treatment due to an adverse event. The most common adverse events leading to discontinuation were application site reactions, occurring in 2% of both the DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% and placebo groups. Application site reactions leading to dropout included pruritus, dermatitis, and burning.
Common Adverse Events
Overall, the most common adverse events associated with DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% treatment were skin reactions at the site of treatment. Table 1 lists all adverse events, regardless of causality, occurring in ≥ 1% of patients in controlled trials of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3%. A majority of patients treated with DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% had adverse events with a maximum intensity of "mild" or "moderate."
Table 1. Common Adverse Events (by body system and preferred term) in ≥ 1% of Patients treated with DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% or Placebo* Category Diclofenac
N=572Placebo
N=564N Percent N Percent Foreign labeling describes that dermal allergic reactions may occur with DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% treatment. Additionally, the treated area may become irritated or develop itching, erythema, edema, vesicles, or abnormal sensation. - * The table lists adverse events occurring in placebo-treated patients because the placebo was comprised of the same ingredients as DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% except for diclofenac. Adverse events in the placebo group may therefore reflect effects of the non-active ingredients.
- † Includes: application site dryness, irritation, erythema, atrophy, discoloration, hyperhidriosis, and vesicles.
- ‡ Includes: gastritis, vomiting, diarrhea, constipation, upper abdominal pain, and dry mouth.
- § Includes: hypoesthesia, dizziness, and hyperkinesias.
Application Site Conditions 64 11 70 12 Pruritus 31 5 44 8 Dermatitis 9 2 3 <1 Burning 2 <1 8 1 Other† 22 4 15 3 Gastrointestinal Disorders 49 9 33 6 Nausea 17 3 11 2 Dysgeusia 10 2 3 <1 Dyspepsia 7 1 8 1 Other‡ 15 3 11 2 Nervous System Disorders 13 2 18 3 Headache 7 1 10 2 Paresthesia 6 1 8 1 Somnolence 4 1 6 1 Other§ 4 1 3 <1 Pediatric Clinical Trials Experience
In one open-label trial, 104 male and female pediatric patients 6 years and older presenting with minor strains, sprains, and contusions received DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% twice a day for as many as 16 days. The most commonly reported adverse events (incidence ≥ 2%) were headache (9%), application site pruritus (7%), nausea (3%), and dyspepsia (3%). No adverse events led to discontinuation of treatment.
-
7 DRUG INTERACTIONS
See Table 2 for clinically significant drug interactions with diclofenac.
Table 2: Clinically Significant Drug Interactions with Diclofenac Drugs That Interfere with Hemostasis Clinical Impact: - Diclofenac and anticoagulants such as warfarin have a synergistic effect on bleeding. The concomitant use of diclofenac and anticoagulants have an increased risk of serious bleeding compared to the use of either drug alone.
- Serotonin release by platelets plays an important role in hemostasis. Case-control and cohort epidemiological studies showed that concomitant use of drugs that interfere with serotonin reuptake and an NSAID may potentiate the risk of bleeding more than an NSAID alone.
Intervention: Monitor patients with concomitant use of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% with anticoagulants (e.g., warfarin), antiplatelet agents (e.g., aspirin), selective serotonin reuptake inhibitors (SSRIs), and serotonin norepinephrine reuptake inhibitors (SNRIs) for signs of bleeding [see Warnings and Precautions (5.11)]. Aspirin Clinical Impact: Controlled clinical studies showed that the concomitant use of NSAIDs and analgesic doses of aspirin does not produce any greater therapeutic effect than the use of NSAIDs alone. In a clinical study, the concomitant use of an NSAID and aspirin was associated with a significantly increased incidence of GI adverse reactions as compared to use of the NSAID alone [see Warnings and Precautions (5.2)]. Intervention: Concomitant use of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% and analgesic doses of aspirin is not generally recommended because of the increased risk of bleeding [see Warnings and Precautions (5.11)].
DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% is not a substitute for low dose aspirin for cardiovascular protection.ACE Inhibitors, Angiotensin Receptor Blockers, and Beta-Blockers Clinical Impact: - NSAIDs may diminish the antihypertensive effect of angiotensin converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), or beta-blockers (including propranolol).
- In patients who are elderly, volume-depleted (including those on diuretic therapy), or have renal impairment, co-administration of an NSAID with ACE inhibitors or ARBs may result in deterioration of renal function, including possible acute renal failure. These effects are usually reversible.
Intervention: - During concomitant use of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% and ACE-inhibitors, ARBs, or beta-blockers, monitor blood pressure to ensure that the desired blood pressure is obtained.
- During concomitant use of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% and ACE-inhibitors or ARBs in patients who are elderly, volume-depleted, or have impaired renal function, monitor for signs of worsening renal function [see Warnings and Precautions (5.6)].
- When these drugs are administered concomitantly, patients should be adequately hydrated. Assess renal function at the beginning of the concomitant treatment and periodically thereafter.
Diuretics Clinical Impact: Clinical studies, as well as post-marketing observations, showed that NSAIDs reduced the natriuretic effect of loop diuretics (e.g., furosemide) and thiazide diuretics in some patients. This effect has been attributed to the NSAID inhibition of renal prostaglandin synthesis. Intervention: During concomitant use of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% with diuretics, observe patients for signs of worsening renal function, in addition to assuring diuretic efficacy including antihypertensive effects [see Warnings and Precautions (5.6)]. Digoxin Clinical Impact: The concomitant use of diclofenac with digoxin has been reported to increase the serum concentration and prolong the half-life of digoxin. Intervention: During concomitant use of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% and digoxin, monitor serum digoxin levels. Lithium Clinical Impact: NSAIDs have produced elevations in plasma lithium levels and reductions in renal lithium clearance. The mean minimum lithium concentration increased 15%, and the renal clearance decreased by approximately 20%. This effect has been attributed to NSAID inhibition of renal prostaglandin synthesis. Intervention: During concomitant use of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% and lithium, monitor patients for signs of lithium toxicity. Methotrexate Clinical Impact: Concomitant use of NSAIDs and methotrexate may increase the risk for methotrexate toxicity (e.g., neutropenia, thrombocytopenia, renal dysfunction). Intervention: During concomitant use of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% and methotrexate, monitor patients for methotrexate toxicity. Cyclosporine Clinical Impact: Concomitant use of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% and cyclosporine may increase cyclosporine's nephrotoxicity. Intervention: During concomitant use of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% and cyclosporine, monitor patients for signs of worsening renal function. NSAIDs and Salicylates Clinical Impact: Concomitant use of diclofenac with other NSAIDs or salicylates (e.g., diflunisal, salsalate) increases the risk of GI toxicity, with little or no increase in efficacy [see Warnings and Precautions (5.2)]. Intervention: The concomitant use of diclofenac with other NSAIDs or salicylates is not recommended. Pemetrexed Clinical Impact: Concomitant use of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% and pemetrexed may increase the risk of pemetrexed-associated myelosuppression, renal, and GI toxicity (see the pemetrexed prescribing information). Intervention: During concomitant use of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% and pemetrexed, in patients with renal impairment whose creatinine clearance ranges from 45 to 79 mL/min, monitor for myelosuppression, renal and GI toxicity.
NSAIDs with short elimination half-lives (e.g., diclofenac, indomethacin) should be avoided for a period of two days before, the day of, and two days following administration of pemetrexed.
In the absence of data regarding potential interaction between pemetrexed and NSAIDs with longer half-lives (e.g., meloxicam, nabumetone), patients taking these NSAIDs should interrupt dosing for at least five days before, the day of, and two days following pemetrexed administration. -
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Published literature reports that use of NSAIDs, including DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3%, after 30 weeks of gestation increases the risk of premature closure of the fetal ductus arteriosus. Data from observational studies regarding potential embryofetal risks of NSAID use, including diclofenac, in women in the first or second trimester of pregnancy are inconclusive. Avoid use of NSAIDs, including DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3%, in pregnant women starting at 30 weeks of gestation (third trimester) (see Clinical Considerations and Data).
In animal reproduction studies, diclofenac epolamine administered orally to pregnant rats and rabbits during the period of organogenesis produced embryotoxicity at approximately 3 and 7 times, respectively, the topical exposure from the maximum recommended human dose (MRHD) of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3%. In rats, increased incidences of skeletal anomalies and maternal toxicity were also observed at this dose. Diclofenac epolamine administered orally to both male and female rats prior to mating and throughout the mating period, and during gestation and lactation in females produced embryotoxicity at doses approximately 3 and 7 times, respectively, the topical exposure from the MRHD (see Data).
Based on animal data, prostaglandins have been shown to have an important role in endometrial vascular permeability, blastocyst implantation, and decidualization. In animal studies, administration of prostaglandin synthesis inhibitors such as diclofenac, resulted in increased pre- and post-implantation loss.
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively.
Data
Human Data
Published literature reports that use of NSAIDS, including diclofenac, after 30 weeks of gestation may cause constriction of the patent ductus arteriosus and premature closure of the fetal ductus arteriosus.
Animal Data
Pregnant Sprague Dawley rats were administered 1, 3, or 6 mg/kg diclofenac epolamine via oral gavage daily from gestation days 6 to 15. Maternal toxicity, embryotoxicity, and increased incidence of skeletal anomalies were noted with 6 mg/kg/day diclofenac epolamine, which corresponds to 3 times the maximum recommended daily exposure in humans based on a body surface area comparison. Pregnant New Zealand White rabbits were administered 1, 3, or 6 mg/kg diclofenac epolamine via oral gavage daily from gestation days 6 to 18. No maternal toxicity was noted; however, embryotoxicity was evident at 6 mg/kg/day group which corresponds to 7 times the maximum recommended daily exposure in humans based on a body surface area comparison.
Male rats were orally administered diclofenac epolamine (1, 3, 6 mg/kg) for 60 days prior to mating and throughout the mating period, and females were given the same doses 14 days prior to mating and through mating, gestation, and lactation. Embryotoxicity was observed at 6 mg/kg diclofenac epolamine (3 times the maximum recommended daily exposure in humans based on a body surface area comparison), and was manifested as an increase in early resorptions, post-implantation losses, and a decrease in live fetuses. The number of live born and total born were also reduced as was F1 postnatal survival, but the physical and behavioral development of surviving F1 pups in all groups was the same as the deionized water control, nor was reproductive performance adversely affected despite a slight treatment-related reduction in body weight.
8.2 Lactation
Risk Summary
Data from published literature reports with oral preparations of diclofenac indicate the presence of small amounts of diclofenac in human milk (see Data). There are no data on the effects on the breastfed infant, or the effects on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% and any potential adverse effects on the breastfed infant from the DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% or from the underlying maternal condition.
Data
One woman treated orally with a diclofenac salt, 150 mg/day, had a milk diclofenac level of 100 mcg/L, equivalent to an infant dose of about 0.03 mg/kg/day. Diclofenac was not detectable in breast milk in 12 women using diclofenac (after either 100 mg/day orally for 7 days or a single 50 mg intramuscular dose administered in the immediate postpartum period). The relative bioavailability for DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% is <1% of a single 50 mg diclofenac tablet.
8.3 Females and Males of Reproductive Potential
Infertility
Females
Based on the mechanism of action, the use of prostaglandin-mediated NSAIDs, including DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% may delay or prevent rupture of ovarian follicles, which has been associated with reversible infertility in some women [see Clinical Pharmacology (12.1)]. Published animal studies have shown that administration of prostaglandin synthesis inhibitors has the potential to disrupt prostaglandin- mediated follicular rupture required for ovulation. Small studies in women treated with NSAIDs have also shown a reversible delay in ovulation. Consider withdrawal of NSAIDs, including DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3%, in women who have difficulties conceiving or who are undergoing investigation of infertility.
8.4 Pediatric Use
The safety and effectiveness of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% have been established in pediatric patients 6 years and older based on evidence from adequate and well-controlled studies with DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3 % in adults, as well as an open-label study in pediatric patients 6 years and older. The pediatric study enrolled 104 patients, 6 years of age and older with minor soft tissue injuries. One DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3 % was applied to the injury site twice daily for a maximum of 14 days or until treatment was no longer required for pain management, whichever occurred first. Based on the available data from the pediatric study, the safety profile of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3 % topical system in pediatric patients is similar to that in adults. The safety and effectiveness of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3 % has not been investigated in pediatric patients less than 6 years old. [see Clinical Trials Experience (6.1), Clinical Pharmacology (12.3)].
8.5 Geriatric Use
Elderly patients, compared to younger patients, are at greater risk for NSAID-associated serious cardiovascular, gastrointestinal, and/or renal adverse reactions. If the anticipated benefit for the elderly patient outweighs these potential risks, start dosing at the low end of the dosing range, and monitor patients for adverse effects [see Warnings and Precautions (5.1, 5.2, 5.3, 5.6, 5.13)].
Clinical studies of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients.
-
10 OVERDOSAGE
Symptoms following acute NSAID overdosages have been typically limited to lethargy, drowsiness, nausea, vomiting, and epigastric pain, which have been generally reversible with supportive care. Gastrointestinal bleeding has occurred. Hypertension, acute renal failure, respiratory depression, and coma have occurred, but were rare [see Warnings and Precautions (5.1, 5.2, 5.4, 5.6)].
Manage patients with symptomatic and supportive care following an NSAID overdosage. There are no specific antidotes. Forced diuresis, alkalinization of urine, hemodialysis, or hemoperfusion may not be useful due to high protein binding.
For additional information about overdosage treatment contact a poison control center (1-800-222-1222).
-
11 DESCRIPTION
DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% is a nonsteroidal anti-inflammatory drug, available for topical application. DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% is a 10 cm × 14 cm topical system comprised of an adhesive material containing 1.3% diclofenac epolamine which is applied to a non-woven polyester felt backing and covered with a polypropylene film release liner. The release liner is removed prior to topical application to the skin.
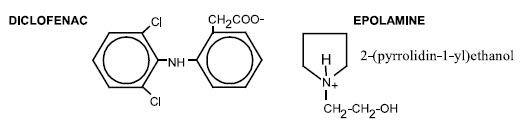
The chemical name of diclofenac epolamine is 2-[(2,6-dichlorophenyl) amino]benzeneacetic acid, (2-(pyrrolidin-1-yl) ethanol salt, with a molecular formula of C20H24Cl2N2O3, and molecular weight 411.3, an n-octanol/water partition coefficient of 8 at pH 8.5, and the following chemical structure:
Each adhesive topical system contains 180 mg of diclofenac epolamine (13 mg per gram adhesive) in an aqueous base. It also contains the following inactive ingredients: butylene glycol, carboxymethylcellulose sodium, dihydroxyaluminum aminoacetate, edetate disodium, fragrance (Dalin PH), gelatin, kaolin, methylparaben, polysorbate 80, povidone, propylene glycol, propylparaben, sodium polyacrylate, sorbitol solution, tartaric acid, titanium dioxide, and purified water.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Diclofenac has analgesic, anti-inflammatory, and antipyretic properties.
The mechanism of action of diclofenac, like that of other NSAIDs, is not completely understood but involves inhibition of cyclooxygenase (COX-1 and COX-2).
Diclofenac is a potent inhibitor of prostaglandin synthesis in vitro. Diclofenac concentrations reached during therapy have produced in vivo effects. Prostaglandins sensitize afferent nerves and potentiate the action of bradykinin in inducing pain in animal models. Prostaglandins are mediators of inflammation. Because diclofenac is an inhibitor of prostaglandin synthesis, its mode of action may be due to a decrease of prostaglandins in peripheral tissues.
12.2 Pharmacodynamics
DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% applied to intact skin provides local analgesia by releasing diclofenac epolamine from the topical system into the skin.
12.3 Pharmacokinetics
Absorption- Adults
Following a single application of the DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% on the upper inner arm, peak plasma concentrations of diclofenac (range 0.7 – 6 ng/mL) were noted between 10 – 20 hours of application. Plasma concentrations of diclofenac in the range of 1.3 – 8.8 ng/mL were noted after five days with twice-a-day DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% application.
Systemic exposure (AUC) and maximum plasma concentrations of diclofenac, after repeated dosing for four days with DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3%, were lower (<1%) than after a single oral 50-mg diclofenac sodium tablet.
The pharmacokinetics of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% has been tested in healthy volunteers at rest or undergoing moderate exercise (cycling 20 min/h for 12 h at a mean HR of 100.3 bpm). No clinically relevant differences in systemic absorption were observed, with peak plasma concentrations in the range of 2.2 – 8.1 ng/mL while resting, and 2.7 – 7.2 ng/mL during exercise.
Absorption – Pediatrics
Diclofenac plasma concentration was assessed in pediatric patients 6 years and older at a fixed time point 24-hours after the initial application and at the final visit (Day 3 – 15). The resulting average concentrations were 1.65 ng/mL and 1.80 ng/mL, respectively, both of which are similar to the values observed in adults.
Distribution
Diclofenac has a very high affinity (>99%) for human serum albumin. Diclofenac diffuses into and out of the synovial fluid. Diffusion into the joint occurs when plasma levels are higher than those in the synovial fluid, after which the process reverses, and synovial fluid levels are higher than plasma levels. It is not known whether diffusion into the joint plays a role in the effectiveness of diclofenac.
Elimination
Metabolism
Five diclofenac metabolites have been identified in human plasma and urine. The metabolites include 4'-hydroxy-, 5-hydroxy-, 3'-hydroxy-, 4',5-dihydroxy- and 3'-hydroxy-4'-methoxy diclofenac. The major diclofenac metabolite, 4'hydroxy-diclofenac, has very weak pharmacologic activity. The formation of 4'-hydroxy diclofenac is primarily mediated by CPY2C9. Both diclofenac and its oxidative metabolites undergo glucuronidation or sulfation followed by biliary excretion. Acylglucuronidation mediated by UGT2B7 and oxidation mediated by CPY2C8 may also play a role in diclofenac metabolism. CYP3A4 is responsible for the formation of minor metabolites, 5-hydroxy and 3'-hydroxy- diclofenac.
Excretion
The plasma elimination half-life of diclofenac after application of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% is approximately 12 hours. Diclofenac is eliminated through metabolism and subsequent urinary and biliary excretion of the glucuronide and the sulfate conjugates of the metabolites. Little or no free unchanged diclofenac is excreted in the urine. Approximately 65% of the dose is excreted in the urine and approximately 35% in the bile as conjugates of unchanged diclofenac plus metabolites.
Specific Populations
The pharmacokinetics of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% has not been investigated in children, patients with hepatic or renal impairment, or specific racial groups.
Drug Interaction Studies
Aspirin: When NSAIDs were administered with aspirin, the protein binding of NSAIDs were reduced, although the clearance of free NSAID was not altered. The clinical significance of this interaction is not known. See Table 1 for clinically significant drug interactions of NSAIDs with aspirin [see Drug Interactions (7)].
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Long-term studies in animals have not been performed to evaluate the carcinogenic potential of either diclofenac epolamine or DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3%.
Mutagenesis
Diclofenac epolamine is not mutagenic in Salmonella typhimurium strains, nor does it induce an increase in metabolic aberrations in cultured human lymphocytes, or the frequency of micronucleated cells in the bone marrow micronucleus test performed in rats.
Impairment of Fertility
Male and female Sprague Dawley rats were administered 1, 3, or 6 mg/kg/day diclofenac epolamine via oral gavage (males treated for 60 days prior to conception and during mating period, females treated for 14 days prior to mating through day 19 of gestation). Diclofenac epolamine treatment with 6 mg/kg/day resulted in increased early resorptions and post-implantation losses; however, no effects on the mating and fertility indices were found. The 6 mg/kg/day dose corresponds to 3 times the maximum recommended daily exposure in humans based on a body surface area comparison.
-
14 CLINICAL STUDIES
14.1 Strains, Sprains, and Contusions
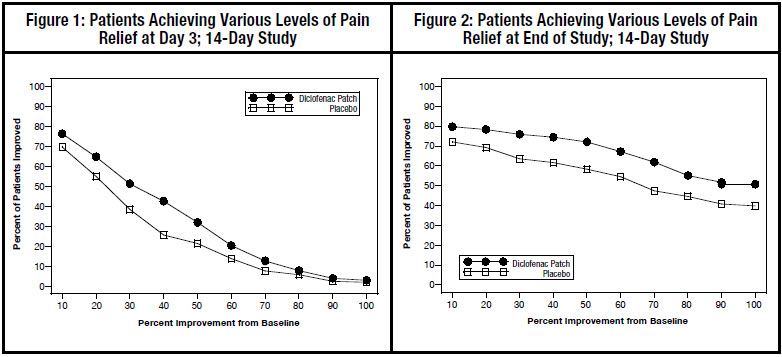
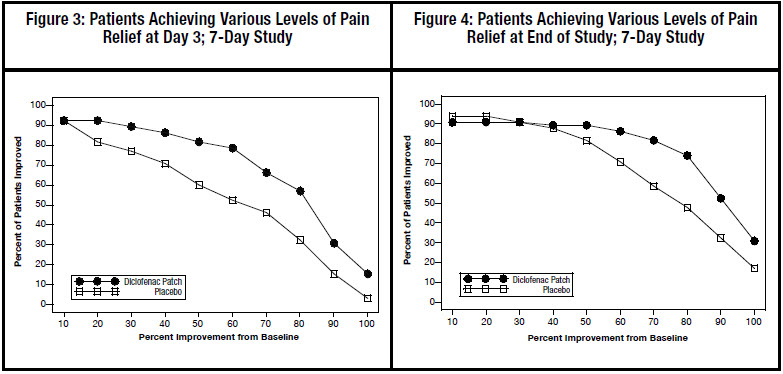
Efficacy of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% was demonstrated in two of four studies of patients with minor sprains, strains, and contusions. Patients were randomly assigned to treatment with the DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3%, or a placebo identical to the DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% minus the active ingredient. In the first of these two studies, patients with ankle sprains were treated once daily for a week. In the second study, patients with sprains, strains and contusions were treated twice daily for up to two weeks. Pain was assessed over the period of treatment. Patients treated with the DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% experienced a greater reduction in pain as compared to patients randomized to placebo as evidenced by the responder curves presented below (Figures 1-4).
-
16 HOW SUPPLIED/STORAGE AND HANDLING
- The DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% is supplied in resealable envelopes, each containing 5 topical systems (10 cm × 14 cm), with 6 envelopes per box (NDC: 0093-3727-55). Each individual topical system is embossed with " DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% TEVA 3727".
- The product is intended for topical use only.
- Keep out of reach of children and pets.
- Envelopes should be sealed at all times when not in use.
- Curad® Hold Tite™ is a trademark of Medline Industries, Inc., and Surgilast® Tubular Elastic Dressing is a trademark of Derma Sciences, Inc.
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide) that accompanies each prescription dispensed, as well as the Directions for Use on the product packaging. Inform patients, families, or their caregivers of the following information before initiating therapy with DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% and periodically during the course of ongoing therapy.
Cardiovascular Thrombotic Events
Advise patients to be alert for the symptoms of cardiovascular thrombotic events, including chest pain, shortness of breath, weakness, or slurring of speech, and to report any of these symptoms to their health care provider immediately [see Warnings and Precautions (5.1)].
Gastrointestinal Bleeding, Ulceration, and Perforation
Advise patients to report symptoms of ulcerations and bleeding, including epigastric pain, dyspepsia, melena, and hematemesis to their health care provider. In the setting of concomitant use of low-dose aspirin for cardiac prophylaxis, inform patients of the increased risk for and the signs and symptoms of GI bleeding [see Warnings and Precautions (5.2)].
Hepatotoxicity
Inform patients of the warning signs and symptoms of hepatotoxicity (e.g., nausea, fatigue, lethargy, pruritus, diarrhea, jaundice, right upper quadrant tenderness, and "flu-like" symptoms). If these occur, instruct patients to stop DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% and seek immediate medical therapy [see Warnings and Precautions (5.3)].
Heart Failure and Edema
Advise patients to be alert for the symptoms of congestive heart failure including shortness of breath, unexplained weight gain, or edema and to contact their healthcare provider if such symptoms occur [see Warnings and Precautions (5.5)].
Anaphylactic Reactions
Inform patients of the signs of an anaphylactic reaction (e.g., difficulty breathing, swelling of the face or throat). Instruct patients to seek immediate emergency help if these occur [see Contraindications (4) and Warnings and Precautions (5.7)].
Serious Skin Reactions
Advise patients to stop DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% immediately if they develop any type of rash and to contact their healthcare provider as soon as possible [see Warnings and Precautions (5.9)].
Female Fertility
Advise females of reproductive potential who desire pregnancy that NSAIDs, including DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3%, may delay or prevent rupture of ovarian follicles, which has been associated with reversible infertility in some women [see Use in Specific Populations (8.3)]
Premature Closure of the Fetal Ductus Arteriosus
Advise pregnant women to avoid use of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% and other NSAIDs starting at 30 weeks of gestation because of the risk of the premature closure of the fetal ductus arteriosus. Advise females of reproductive potential to contact their healthcare provider with a known or suspected pregnancy [see Warnings and Precautions (5.10) and Use in Specific Populations (8.1)].
Avoid Concomitant Use of NSAIDs
Inform patients that the concomitant use of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% with other NSAIDs or salicylates (e.g., diflunisal, salsalate) is not recommended due to the increased risk of gastrointestinal toxicity, and little or no increase in efficacy [see Warnings and Precautions (5.2) and Drug Interactions (7)]. Alert patients that NSAIDs may be present in "over the counter" medications for treatment of colds, fever, or insomnia.
Use of NSAIDS and Low-Dose Aspirin
Inform patients not to use low-dose aspirin concomitantly with DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% until they talk to their healthcare provider [see Drug Interactions (7)].
Eye Exposure
Instruct patients to avoid contact of DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% with the eyes and mucosa. Advise patients that if eye contact occurs, immediately wash out the eye with water or saline and consult a physician if irritation persists for more than an hour [see Warnings and Precautions (5.15)].
Special Application Instructions
- Instruct patients that, if DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% begins to peel-off, the edges of the topical system may be taped down. If problems with adhesion persist, patients may overlay the topical system with a mesh netting sleeve, where appropriate (e.g. to secure topical systems applied to ankles, knees, or elbows). The mesh netting sleeve (e.g. Curad® Hold Tite™, Surgilast® Tubular Elastic Dressing) must allow air to pass through and not be occlusive (non-breathable).
- Instruct patients not to apply DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% to non-intact or damaged skin resulting from any etiology e.g. exudative dermatitis, eczema, infected lesion, burns or wounds.
- Instruct patients not to wear a DICLOFENAC EPOLAMINE TOPICAL SYSTEM 1.3% when bathing or showering.
- Instruct patients to wash hands after applying, handling or removing the topical system.
- SPL UNCLASSIFIED SECTION
-
MEDICATION GUIDE
Medication Guide for Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
What is the most important information I should know about medicines called Nonsteroidal Anti-inflammatory Drugs (NSAIDs)?
NSAIDs can cause serious side effects, including:
-
Increased risk of a heart attack or stroke that can lead to death. This risk may happen early in treatment and may increase:
- □ with increasing doses of NSAIDs
- □ with longer use of NSAIDs
-
Increased risk of bleeding, ulcers, and tears (perforation) of the esophagus (tube leading from the mouth to the stomach), stomach and intestines:
- □ anytime during use
- □ without warning symptoms
- □ that may cause death
- □ past history of stomach ulcers, or stomach or intestinal bleeding with use of NSAIDs
- □ taking medicines called "corticosteroids", "anticoagulants", "SSRIs", or "SNRIs"
- □ increasing doses of NSAIDs
- □ longer use of NSAIDs
- □ smoking
- □ drinking alcohol
- □ older age
- □ poor health
- □ advanced liver disease
- □ bleeding problems
NSAIDs should only be used:
- □ exactly as prescribed
- □ at the lowest dose possible for your treatment
- □ for the shortest time needed
What are NSAIDs?
NSAIDs are used to treat pain and redness, swelling, and heat (inflammation) from medical conditions such as different types of arthritis, menstrual cramps, and other types of short-term pain.
Who should not take NSAIDs? Do not take NSAIDs:
- if you have had an asthma attack, hives, or other allergic reaction with aspirin or any other NSAIDs.
- right before or after heart bypass surgery.
Before taking NSAIDS, tell your healthcare provider about all of your medical conditions, including if you:
- have liver or kidney problems
- have high blood pressure
- have asthma
- are pregnant or plan to become pregnant. Talk to your healthcare provider if you are considering taking NSAIDs during pregnancy. You should not take NSAIDs after 29 weeks of pregnancy.
- are breastfeeding or plan to breast feed.
Tell your healthcare provider about all of the medicines you take, including prescription or over-the-counter medicines, vitamins or herbal supplements. NSAIDs and some other medicines can interact with each other and cause serious side effects. Do not start taking any new medicine without talking to your healthcare provider first.
What are the possible side effects of NSAIDs? NSAIDs can cause serious side effects, including:
- new or worse high blood pressure
- heart failure
- liver problems including liver failure
- kidney problems including kidney failure
- low red blood cells (anemia)
- life-threatening skin reactions
- life-threatening allergic reactions
- Other side effects of NSAIDs include: stomach pain, constipation, diarrhea, gas, heartburn, nausea, vomiting, and dizziness.
Get emergency help right away if you get any of the following symptoms:
- shortness of breath or trouble breathing
- slurred speech
- chest pain
- swelling of the face or throat
- weakness in one part or side of your body
Stop taking your NSAID and call your healthcare provider right away if you get any of the following symptoms:
- nausea
- vomit blood
- more tired or weaker than usual
- there is blood in your bowel movement or it is black and sticky like tar
- diarrhea
- itching
- unusual weight gain
- your skin or eyes look yellow
- skin rash or blisters with fever
- indigestion or stomach pain
- swelling of the arms, legs, hands and feet
- flu-like symptoms
If you take too much of your NSAID, call your healthcare provider or get medical help right away. These are not all the possible side effects of NSAIDs. For more information, ask your healthcare provider or pharmacist about NSAIDs.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Other information about NSAIDs
- Aspirin is an NSAID but it does not increase the chance of a heart attack. Aspirin can cause bleeding in the brain, stomach, and intestines. Aspirin can also cause ulcers in the stomach and intestines.
- Some NSAIDs are sold in lower doses without a prescription (over-the-counter). Talk to your healthcare provider before using over-the-counter NSAIDs for more than 10 days.
General information about the safe and effective use of NSAIDs
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use NSAIDs for a condition for which it was not prescribed. Do not give NSAIDs to other people, even if they have the same symptoms that you have. It may harm them.
If you would like more information about NSAIDs, talk with your healthcare provider. You can ask your pharmacist or healthcare provider for information about NSAIDs that is written for health professionals.
Manufactured for: IBSA Institut Biochimique SA, CH-6903 Lugano, Switzerland
Distributed by:
Teva Pharmaceuticals USA, Inc., North Wales, PA 19454 (USA)
For more information call 1-866-832-8537
This Medication Guide has been approved by the U.S. Food and Drug Administration.
Revised:
May, 2019 -
Increased risk of a heart attack or stroke that can lead to death. This risk may happen early in treatment and may increase:
-
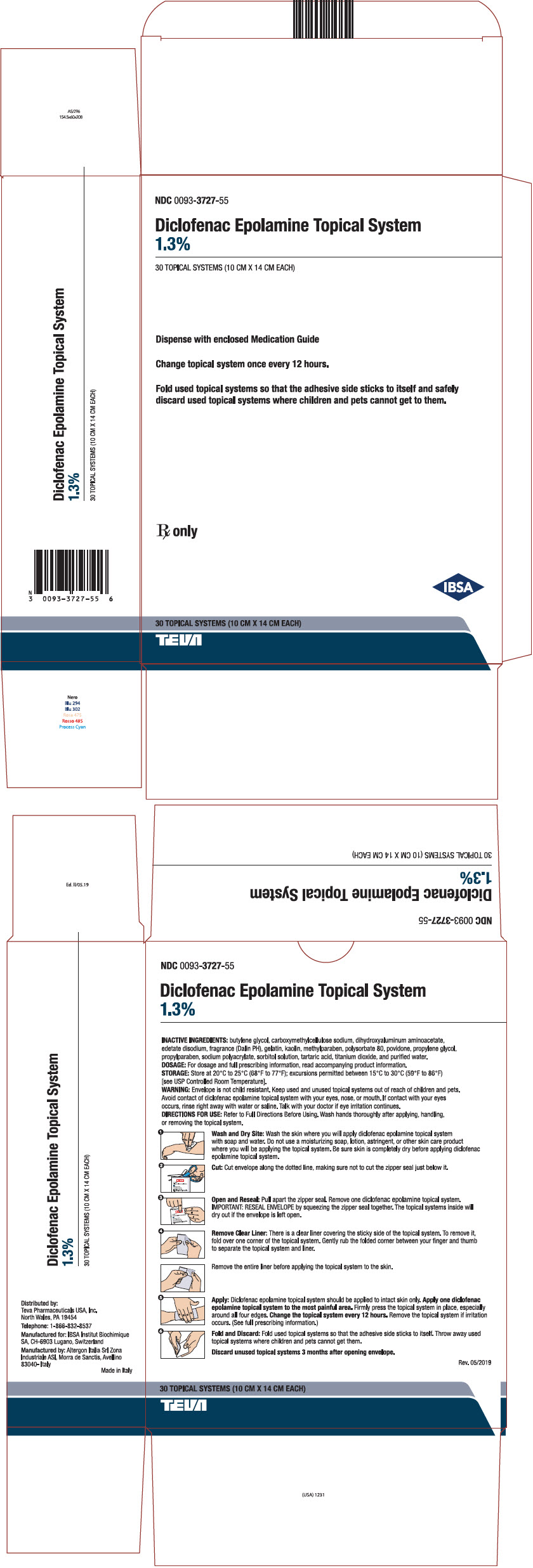
PRINCIPAL DISPLAY PANEL - 30 Topical System Pouch Carton
NDC: 0093-3727-55
Diclofenac Epolamine Topical System
1.3%30 TOPICAL SYSTEMS (10 CM X 14 CM EACH)
Dispense with enclosed Medication Guide
Change topical system once every 12 hours.
Fold used topical systems so that the adhesive side sticks to itself and safely
discard used topical systems where children and pets cannot get to them.Rx only
IBSA
30 TOPICAL SYSTEMS (10 CM X 14 CM EACH)
TEVA
-
INGREDIENTS AND APPEARANCE
DICLOFENAC EPOLAMINE
diclofenac epolamine systemProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0093-3727 Route of Administration TOPICAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength Diclofenac Epolamine (UNII: X5F8EKL9ZG) (DICLOFENAC - UNII:144O8QL0L1) Diclofenac Epolamine 0.013 g Inactive Ingredients Ingredient Name Strength Sorbitol (UNII: 506T60A25R) Butylene Glycol (UNII: 3XUS85K0RA) Dihydroxyaluminum Aminoacetate (UNII: DO250MG0W6) Edetate Disodium (UNII: 7FLD91C86K) Tartaric Acid (UNII: W4888I119H) Kaolin (UNII: 24H4NWX5CO) Methylparaben (UNII: A2I8C7HI9T) Polysorbate 80 (UNII: 6OZP39ZG8H) POVIDONE, UNSPECIFIED (UNII: FZ989GH94E) Water (UNII: 059QF0KO0R) Propylparaben (UNII: Z8IX2SC1OH) GELATIN, UNSPECIFIED (UNII: 2G86QN327L) Propylene Glycol (UNII: 6DC9Q167V3) CARBOXYMETHYLCELLULOSE SODIUM, UNSPECIFIED FORM (UNII: K679OBS311) Titanium Dioxide (UNII: 15FIX9V2JP) Product Characteristics Color WHITE Score Shape RECTANGLE Size Flavor Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0093-3727-55 6 in 1 CARTON 02/05/2019 1 NDC: 0093-3727-50 5 in 1 POUCH; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA AUTHORIZED GENERIC NDA021234 02/05/2019 Labeler - Teva Pharmaceuticals USA Inc. (001627975) Registrant - IBSA Pambio-Noranco Complex (485251214)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.