CEFAZOLIN- cefazolin sodium injection, solution
Cefazolin by
Drug Labeling and Warnings
Cefazolin by is a Prescription medication manufactured, distributed, or labeled by Baxter Healthcare Corporation. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use CEFAZOLIN injection safely and effectively. See full prescribing information for CEFAZOLIN injection.
CEFAZOLIN injection, for intravenous use
Initial U.S. Approval: 1973INDICATIONS AND USAGE
Cefazolin injection is a cephalosporin antibacterial indicated for preoperative prophylaxis. (1.1)
Limitations of Use: Use an alternative cefazolin product when lengthy surgical procedures require supplemental doses and when postoperative dosing is required. (1.2)
To reduce the development of drug-resistant bacteria and maintain the effectiveness of Cefazolin injection and other antibacterial drugs, Cefazolin injection should be used only to prevent infections that are proven or strongly suspected to be caused by bacteria. (1.3)
DOSAGE AND ADMINISTRATION
DOSAGE FORMS AND STRENGTHS
Injection: 2 g of cefazolin per 100 mL in a single-dose GALAXY Container. (3)
CONTRAINDICATIONS
Hypersensitivity to cefazolin or other cephalosporin antibacterial drugs, penicillins, or other beta-lactam drugs. (4.1)
WARNINGS AND PRECAUTIONS
- Hypersensitivity reactions: Cross-hypersensitivity may occur in up to 10% of patients with a history of penicillin allergy. If an allergic reaction occurs, discontinue the drug. (5.1)
- Clostridium difficile-associated diarrhea (CDAD): May range from mild diarrhea to fatal colitis. Evaluate if diarrhea occurs. (5.2)
ADVERSE REACTIONS
Most common adverse reactions with cefazolin are nausea, vomiting, diarrhea, and allergic reactions (anaphylaxis, urticaria, skin rash). (6)
To report SUSPECTED ADVERSE REACTIONS, contact Baxter Healthcare at 1-866-888-2472 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
Probenecid: The renal excretion of cefazolin is inhibited by probenecid. Co-administration of probenecid with cefazolin is not recommended. (7)
USE IN SPECIFIC POPULATIONS
Pediatric use: The safety and effectiveness of Cefazolin injection in pediatric patients have not been established. (8.4)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 10/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
1.1 Preoperative Prophylaxis
1.2 Limitations of Use
1.3 Usage
2 DOSAGE AND ADMINISTRATION
2.1 Preoperative Prophylactic Use in Adults
2.2 Patients with Renal Impairment
2.3 Important Administration Instructions
2.4 Directions for Use of Cefazolin Injection
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
4.1 Hypersensitivity to Cefazolin or the Cephalosporin Class of Antibacterial Drugs, Penicillins, or Other Beta-lactams
5 WARNINGS AND PRECAUTIONS
5.1 Hypersensitivity Reactions to Cefazolin, Cephalosporins, Penicillins, or Other Beta-lactams
5.2 Clostridium difficile-associated Diarrhea
5.3 Hypersensitivity to Dextrose-containing Products
5.4 Risk of Development of Drug-resistant Bacteria
5.5 Drug and Laboratory Test Interactions
5.6 Potential Risk in Patients with Overt or Known Subclinical Diabetes Mellitus or Carbohydrate Intolerance
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Cephalosporin Adverse Reactions
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Labor and Delivery
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Patients with Renal Impairment
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
12.4 Microbiology
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
15 REFERENCES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
1.1 Preoperative Prophylaxis
Cefazolin injection is indicated for preoperative prophylaxis. The prophylactic administration of cefazolin preoperatively may reduce the incidence of certain postoperative infections in patients undergoing surgical procedures which are classified as contaminated or potentially contaminated (e.g., vaginal hysterectomy, and cholecystectomy in high-risk patients such as those older than 70 years, with acute cholecystitis, obstructive jaundice, or common duct bile stones).
The preoperative use of cefazolin may also be effective in surgical patients in whom infection at the operative site would present a serious risk.
If there are signs of infection, specimens for cultures should be obtained for the identification of the causative organism so that appropriate therapy may be instituted.
1.2 Limitations of Use
Use an alternative cefazolin product when lengthy surgical procedures require supplemental doses and when postoperative dosing is required.
1.3 Usage
To reduce the development of drug-resistant bacteria and maintain the effectiveness of Cefazolin injection and other antibacterial drugs, Cefazolin injection should be used only to prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
-
2 DOSAGE AND ADMINISTRATION
2.1 Preoperative Prophylactic Use in Adults
- Only use Cefazolin injection in patients who require the entire 2 gram dose and not any fraction of it.
- Administer the entire 2 gram dose intravenously 1/2 hour to 1 hour prior to the start of surgery.
- It is important that the preoperative dose be given just prior (1/2 hour to 1 hour) to the start of surgery so that adequate antibacterial concentrations are present in the serum and tissues at the time of initial surgical incision.
2.2 Patients with Renal Impairment
Use Cefazolin injection only in patients whose creatinine clearance is greater than or equal to 35 mL/min and require the entire 2 gram dose and not any fraction of it.
2.3 Important Administration Instructions
- This premixed solution is for intravenous use only.
- Administer Cefazolin injection intravenously over approximately 30 minutes.
- Do not use plastic containers in series connections. Such use would result in air embolism due to residual air being drawn from the primary container before administration of the fluid from the secondary container is complete. If administration is controlled by a pumping device, care must be taken to discontinue pumping action before the container runs dry or air embolism may result.
- Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration. Use only if solution is clear and container and seals are intact.
- Do not introduce additives into the GALAXY Container.
2.4 Directions for Use of Cefazolin Injection
- Thawing of Plastic Container
- Thaw frozen container at room temperature (25°C/ 77°F) or under refrigeration (5°C/41°F). Product should not be thawed by immersion in water baths or by microwave irradiation. Do not force thaw.
- No further dilution is necessary.
- Check for minute leaks by squeezing container firmly. If leaks are detected, discard solution as sterility may be impaired.
- Do not add supplementary medication.
- The container should be visually inspected. If the outlet port protector is damaged, detached, or not present, discard container as solution path sterility may be impaired. Components of the solution may precipitate in the frozen state and will dissolve upon reaching room temperature with little or no agitation. Potency is not affected. Agitate after solution has reached room temperature. If after visual inspection the solution remains cloudy or if an insoluble precipitate is noted or if any seals are not intact, the container should be discarded.
- The thawed solution is stable for 30 days under refrigeration (5°C/41°F) or 48 hours at 25°C/77°F. Do not refreeze thawed antibacterial drugs.
- Preparation for Administration
- Suspend container from support.
- Remove protector from outlet port at bottom of container.
- Attach Intravenous administration set to outlet port. Refer to the manufacturer’s instructions accompanying the administration set for complete directions.
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
4.1 Hypersensitivity to Cefazolin or the Cephalosporin Class of Antibacterial Drugs, Penicillins, or Other Beta-lactams
Cefazolin injection is contraindicated in patients who have a history of immediate hypersensitivity reactions (e.g., anaphylaxis, serious skin reactions) to cefazolin or the cephalosporin antibacterial drugs, penicillins, or other beta-lactams [see Warnings and Precautions (5.1)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Hypersensitivity Reactions to Cefazolin, Cephalosporins, Penicillins, or Other Beta-lactams
Serious and occasionally fatal hypersensitivity (anaphylactic) reactions have been reported in patients receiving beta-lactam antibacterial drugs. Before therapy with Cefazolin injection is instituted, careful inquiry should be made to determine whether the patient has had previous immediate hypersensitivity reactions to cefazolin, cephalosporins, penicillins, or carbapenems. Maintain clinical supervision if this product is to be given to penicillin-sensitive patients because cross-hypersensitivity among beta-lactam antibacterial drugs has been clearly documented and may occur in up to 10% of patients with a history of penicillin allergy. If an allergic reaction to Cefazolin injection occurs, discontinue the drug.
5.2 Clostridium difficile-associated Diarrhea
Clostridium difficile-associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents, including cefazolin, and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon leading to overgrowth of C. difficile.
C. difficile produces toxins A and B, which contribute to the development of CDAD. Hypertoxin-producing isolates of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibacterial drug use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents.
If CDAD is suspected or confirmed, ongoing antibacterial drug use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibacterial drug treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated.
5.3 Hypersensitivity to Dextrose-containing Products
Hypersensitivity reactions, including anaphylaxis, have been reported with administration of dextrose-containing products. These reactions have been reported in patients receiving high concentrations of dextrose (i.e. 50% dextrose).1 The reactions have also been reported when corn-derived dextrose solutions were administered to patients with or without a history of hypersensitivity to corn products.2
5.4 Risk of Development of Drug-resistant Bacteria
Prescribing Cefazolin injection in the absence of proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
As with other antimicrobials, prolonged use of Cefazolin injection may result in overgrowth of nonsusceptible microorganisms. Repeated evaluation of the patient's condition is essential. Should superinfection occur during therapy, appropriate measures should be taken.
5.5 Drug and Laboratory Test Interactions
Urinary Glucose
The administration of cefazolin may result in a false-positive reaction with glucose in the urine when using CLINITEST tablets. It is recommended that glucose tests based on enzymatic glucose oxidase reactions (e.g., CLINISTIX strips) be used.
Coombs’ Test
Positive direct Coombs' tests have been reported during treatment with cefazolin. In hematologic studies or in transfusion cross-matching procedures when antiglobulin tests are performed on the minor side or in Coombs' testing of newborns whose mothers have received cephalosporin antibacterial drugs before parturition, it should be recognized that a positive Coombs' test may be due to the drug.
5.6 Potential Risk in Patients with Overt or Known Subclinical Diabetes Mellitus or Carbohydrate Intolerance
As with other dextrose-containing solutions, maintain clinical supervision when prescribing Cefazolin injection to patients with overt or known subclinical diabetes mellitus or carbohydrate intolerance for any reason.
-
6 ADVERSE REACTIONS
The following serious adverse reactions to cefazolin are described below and elsewhere in the labeling:
- Hypersensitivity reactions [see Warnings and Precautions (5.1)]
- Clostridium difficile-associated diarrhea [see Warnings and Precautions (5.2)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The following adverse reactions were reported from clinical trials:
Gastrointestinal: Diarrhea, oral candidiasis, mouth ulcers, vomiting, nausea, stomach cramps, epigastric pain, heartburn, flatus, anorexia and pseudomembranous colitis. Onset of pseudomembranous colitis symptoms may occur during or after antibacterial treatment [see Warnings and Precautions (5.2)].
Allergic: Anaphylaxis, eosinophilia, urticaria, itching, drug fever, skin rash, Stevens-Johnson syndrome.
Hematologic: Neutropenia, leukopenia, thrombocytopenia, thrombocythemia.
Hepatic: Transient rise in alanine aminotransferase (ALT), aspartate aminotransferase (AST), hepatitis and alkaline phosphatase levels has been observed.
Renal: Increased BUN and creatinine levels, renal failure
Local Reactions: Phlebitis injection
Other Reactions: Pruritus (including genital, vulvar and anal pruritus, genital moniliasis, and vaginitis). Dizziness, fainting, lightheadedness, confusion, weakness, tiredness, hypotension, somnolence and headache.
6.2 Cephalosporin Adverse Reactions
In addition to the adverse reactions listed above that have been observed in patients treated with cefazolin, the following adverse reactions and altered laboratory tests have been reported for cephalosporin antibacterial drugs: Stevens-Johnson syndrome, erythema multiforme, toxic epidermal necrolysis, renal impairment, toxic nephropathy, aplastic anemia, hemolytic anemia, hemorrhage, hepatic impairment including cholestasis, and pancytopenia.
- 7 DRUG INTERACTIONS
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Reproduction studies have been performed in rats, mice and rabbits at doses of 2000, 4000 and 240 mg/kg/day or 1-3 times the maximum recommended human dose (based on body surface area). There was no evidence of impaired fertility or harm to the fetus due to cefazolin.
8.2 Labor and Delivery
When cefazolin has been administered prior to caesarean section, drug concentrations in cord blood have been approximately one quarter to one third of maternal drug levels. The drug appears to have no adverse effect on the fetus.
8.3 Nursing Mothers
Cefazolin is present in very low concentrations in the milk of nursing mothers. Caution should be exercised when Cefazolin injection is administered to a nursing woman.
8.4 Pediatric Use
The safety and effectiveness of Cefazolin injection in pediatric patients have not been established.
8.5 Geriatric Use
Of the 920 subjects who received cefazolin in clinical studies, 313 (34%) were 65 years and over, while 138 (15%) were 75 years and over. No overall differences in safety or effectiveness were observed between these subjects and younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
This drug is known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function [see Dosage and Administration (2.2)].
8.6 Patients with Renal Impairment
Cefazolin injection should be used only in patients whose creatinine clearance is greater than or equal to 35 mL/min and require the entire 2 gram dose and not any fraction of it. [see Dosage and Administration (2.2)].
-
11 DESCRIPTION
Cefazolin Injection is a frozen, premixed, iso-osmotic, sterile, nonpyrogenic, single-dose 100 mL solution containing 2 g Cefazolin, USP, equivalent to 2.10 g Cefazolin Sodium, USP in the GALAXY container (PL 2040 Plastic). Dextrose, USP has been added to adjust osmolality (4 g as dextrose hydrous). The approximate osmolality for Cefazolin injection is 290 mOsmol/kg.
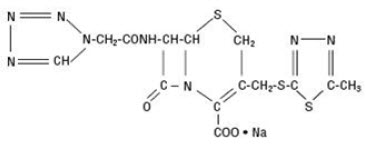
Cefazolin Sodium is a semi-synthetic cephalosporin antibacterial for parenteral administration and has the following IUPAC nomenclature: Sodium (6R,7R)-3-[[(5-methyl-1,3,4-thiadiazol-2-yl)thio]methyl]-8-oxo-7-[2-(1H-tetrazol-1-yl)acetamido]-5-thia-1-azabicyclo[4.2.0]oct‑2-ene-2-carboxylate. Its molecular formula is C14H13N8O4S3·Na and its molecular weight is 454.51 (free acid).
Cefazolin Sodium, USP has the following structural formula:
The sodium content is 48 mg/g of cefazolin sodium.
The pH of Cefazolin injection may have been adjusted with sodium bicarbonate, or sodium hydroxide/hydrochloric acid during manufacture. Water for injection, USP is added as drug vehicle. Contains no preservative. The solution is intended for intravenous use after thawing to room temperature.
This GALAXY container (PL 2040 Plastic) is fabricated from a specially designed multilayer plastic (PL 2040). Solutions are in contact with the polyethylene layer of this container and can leach out certain chemical components of the plastic in very small amounts within the expiration period. However, the suitability of the plastic has been confirmed in tests in animals according to the USP biological tests for plastic containers, as well as by tissue culture toxicity studies.
-
12 CLINICAL PHARMACOLOGY
12.2 Pharmacodynamics
The pharmacokinetic/pharmacodynamic relationship for cefazolin has not been evaluated in patients.
12.3 Pharmacokinetics
Studies have shown that following intravenous administration of cefazolin to normal volunteers, mean serum concentrations peaked at approximately 185 mcg/mL and were approximately 4 mcg/mL at 8 hours for a 1 g dose.
The serum half-life for cefazolin is approximately 1.8 hours following intravenous administration.
In a study, using normal volunteers, of constant intravenous infusion with dosages of 3.5 mg/kg for 1 hour (approximately 250 mg) and 1.5 mg/kg the next 2 hours (approximately 100 mg), cefazolin produced a steady serum concentration at the third hour of approximately 28 mcg/mL.
Plasma pharmacokinetic parameters of cefazolin in normal volunteers (N=12) following a single 15-minute intravenous infusion of 2 g of Cefazolin for injection and Dextrose injection are summarized in Table 1.
Table 1: Mean (Standard Deviation) Plasma Pharmacokinetic Parameters of Cefazolin in Normal Volunteers - * Tmax reported as median (range)
N
Cmax
(mcg/mL)
Tmax*
(h)
AUCo-inf
(mcg*h/mL)t1/2
(h)
CL
(L/h)
Vz
(L)
Single 2 g Dose as a 15-Minute IV Infusion
12
280.9
(45.9)0.25
(0.25-0.33)509.9
(89.3)2.01
(0.28)4.03
(0.68)11.50
(1.53)N= number of subjects observed; Cmax = maximum plasma concentration; Tmax = time to maximum plasma concentration; AUC0‑inf = area under the plasma concentration-time curve extrapolated to infinity; t1/2 = apparent plasma terminal elimination half-life; CL = total clearance; Vz = volume of distribution
Studies in patients hospitalized with infections indicate that cefazolin produces mean peak serum concentrations approximately equivalent to those seen in normal volunteers.
Distribution
Bile concentrations in patients without obstructive biliary disease can reach or exceed serum concentrations by up to five times; however, in patients with obstructive biliary disease, bile concentrations of cefazolin are considerably lower than serum concentrations (less than 1.0 mcg/mL).
In synovial fluid, the cefazolin concentration becomes comparable to that reached in serum at about 4 hours after drug administration.
Studies of cord blood show prompt transfer of cefazolin across the placenta. Cefazolin is present in very low concentrations in the milk of nursing mothers.
Excretion
Cefazolin is excreted unchanged in the urine. In the first 6 hours approximately 60% of the drug is excreted in the urine and this increases to 70% to 80% within 24 hours.
12.4 Microbiology
Mechanism of Action
Cefazolin is a bactericidal agent that acts by inhibition of bacterial cell wall synthesis.
Resistance
Predominant mechanisms of bacterial resistance to cephalosporins include the presence of extended-spectrum beta-lactamases and enzymatic hydrolysis.
Antimicrobial Activity
Cefazolin has been shown to be active against most isolates of the following microorganisms:
Gram-positive Bacteria
Staphylococcus aureus (methicillin-susceptible isolates only)
Streptococcus agalactiae
Streptococcus pyogenesGram-negative Bacteria
Escherichia coli
Proteus mirabilisMost isolates of indole positive Proteus (Proteus vulgaris), Enterobacter spp., Morganella morganii, Providencia rettgeri, Serratia spp., and Pseudomonas spp. are resistant to cefazolin.
- 13 NONCLINICAL TOXICOLOGY
- 15 REFERENCES
-
16 HOW SUPPLIED/STORAGE AND HANDLING
- Cefazolin injection is supplied as a premixed frozen iso-osmotic solution in 100 mL single-dose GALAXY plastic containers as follows:
Code
Product Description
NDC Number
2G3508
2 g cefazolin in 100 mL
Supplied as 12 bags per carton
NDC: 0338-3508-41
Store in a freezer capable of maintaining a temperature of -20°C/-4°F or below [see Dosage and Administration (2.3)].
Handle frozen product containers with care. Product containers may be fragile in the frozen state.
-
17 PATIENT COUNSELING INFORMATION
- Advise patients that allergic reactions, including serious allergic reactions could occur and that serious reactions require immediate treatment and discontinuation of Cefazolin injection.
- Advise patients to report to their health care provider any previous allergic reactions to cefazolin, cephalosporins, penicillins, or other similar antibacterial drugs.
- Advise patients that diarrhea is a common problem caused by antibacterial drugs, which usually ends when the antibacterial drug is discontinued. Sometimes after starting treatment with antibacterial drugs, patients can develop watery and bloody stools (with or without stomach cramps and fever) even as late as two or more months after having taken the last dose of the antibacterial drug. If this occurs, advise patients to contact a physician as soon as possible.
- Inform patients that antibacterial drugs, including Cefazolin injection, should only be used to prevent bacterial infections. They do not treat viral infections (e.g., the common cold).
- SPL UNCLASSIFIED SECTION
-
PACKAGE/LABEL PRINCIPAL DISPLAY PANEL
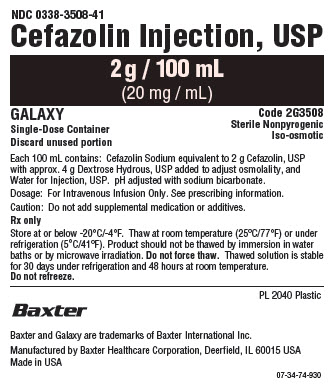
NDC: 0338-3508-41
Cefazolin Injection, USP
2g / 100 mL
(20 mg / mL)GALAXY
Single-Dose container
Discard unused portionCode 2G3508
Sterile Nonpyrogenic
Iso-osmoticEach 100 mL contains: 2g Cefazolin, USP, equivalent to 2.10g Cefazolin Sodium, USP
with approx. 4 g Dextrose Hydrous, USP added to adjust osmolality, and
Water for Injection, USP. pH may have been adjusted with sodium bicarbonate,
or sodium hydroxide/hydrochloric acid.Dosage: For Intravenous Infusion Only. See prescribing information.
Caution: Do not add supplemental medication or additives.Rx only
Store at or below -20°C/-4°F. Thaw at room temperature (25°C/77°F) or under
refrigeration (5°C/41°F). Product should not be thawed by immersion in water
baths or by microwave irradiation. Do not force thaw. Thawed solution is stable
for 30 days under refrigeration or 48 hours at room temperature.Do not refreeze.
PL 2040 Plastic
Baxter Logo
Baxter and Galaxy are trademarks of Baxter International Inc.
Manufactured by Baxter Healthcare Corporation, Deerfield, IL 60015 USA
Made in USA07-34-00-0357
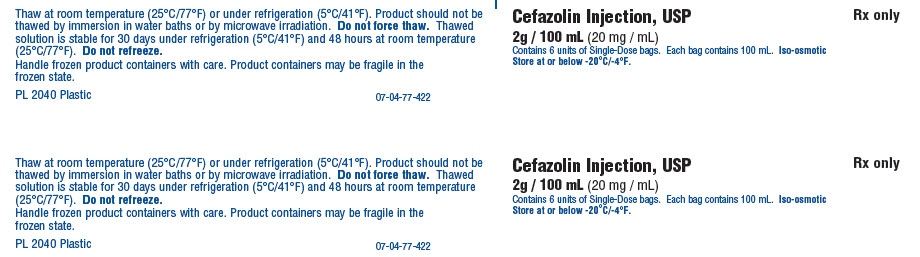
Thaw at room temperature (25°C/77°F) or under refrigeration (5°C/41°F). Product should not be
thawed by immersion in water baths or by microwave irradiation. Do not force thaw. Thawed
solution is stable for 30 days under refrigeration (5°C/41°F) or 48 hours at room temperature
(25°C/77°F). Do not refreeze.
Handle frozen product containers with care. Product containers may be fragile in the
frozen state.
PL 2040 Plastic07-04-00-0112
Cegazolin Injection, USP
2g / 100 mL (20 mg / mL)
Contains 6 units of Single-Dose bags. Each bag contains 100 mL. Iso-osmotic
Store at or below -20°C/-4°F.Rx only
Thaw at room temperature (25°C/77°F) or under refrigeration (5°C/41°F). Product should not be
thawed by immersion in water baths or by microwave irradiation. Do not force thaw. Thawed
solution is stable for 30 days under refrigeration (5°C/41°F) or 48 hours at room temperature
(25°C/77°F). Do not refreeze.
Handle frozen product containers with care. Product containers may be fragile in the
frozen state.
PL 2040 Plastic07-04-00-0112
Cegazolin Injection, USP
2g / 100 mL (20 mg / mL)
Contains 6 units of Single-Dose bags. Each bag contains 100 mL. Iso-osmotic
Store at or below -20°C/-4°F.Rx only
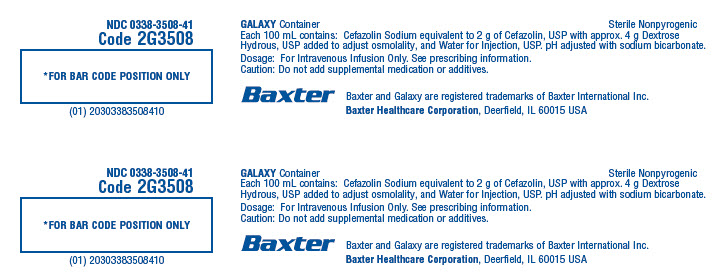
NDC: 0338-3508-41
Code 2G3508*FOR BAR CODE POSITION ONLY
(01) 20303383508410GALAXY Container
Sterile Nonpyrogenic
Each 100 mL contains: 2g Cefazolin, USP, equivalent to 2.10g Cefazolin Sodium, USP with approx. 4 g Dextrose
Hydrous, USP added to adjust osmolality, and Water for Injection, USP.
pH may have been adjusted with sodium bicarbonate, or sodium hydroxide/hydrochloric acid.
Dosage: For Intravenous Infusion Only. See prescribing information.
Caution: Do not add supplemental medication or additives.Baxter Logo
Baxter and Galaxy are registered trademarks of Baxter International Inc.
Baxter Healthcare Corporation, Deerfield, IL 60015 USANDC: 0338-3508-41
Code 2G3508*FOR BAR CODE POSITION ONLY
(01) 20303383508410GALAXY Container
Sterile Nonpyrogenic
Each 100 mL contains: Cefazolin Sodium equivalent to 2 g of Cefazolin, USP with approx. 4 g Dextrose
Hydrous, USP added to adjust osmolality, and Water for Injection, USP.
pH may have been adjusted with sodium bicarbonate, or sodium hydroxide/hydrochloric acid.
Dosage: For Intravenous Infusion Only. See prescribing information.
Caution: Do not add supplemental medication or additives.Baxter Logo
Baxter and Galaxy are registered trademarks of Baxter International Inc.
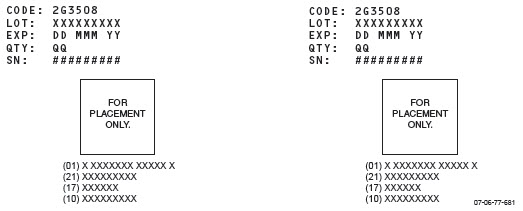
Baxter Healthcare Corporation, Deerfield, IL 60015 USACODE: 2G3508
LOT: XXXXXXXXX
EXP: DD MMM YY
QTY: QQ
SN: #########CODE: 2G3508
LOT: XXXXXXXXX
EXP: DD MMM YY
QTY: QQ
SN: #########FOR
PLACEMENT
ONLY.
(01) X XXXXXXX XXXXX X
(21) XXXXXXXXX
(17) XXXXX
(10) XXXXXXXXXFOR
PLACEMENT
ONLY.
(01) X XXXXXXX XXXXX X
(21) XXXXXXXXX
(17) XXXXX
(10) XXXXXXXXX07-06-77-681
-
INGREDIENTS AND APPEARANCE
CEFAZOLIN
cefazolin sodium injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0338-3508 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CEFAZOLIN SODIUM (UNII: P380M0454Z) (CEFAZOLIN - UNII:IHS69L0Y4T) CEFAZOLIN 2 g in 100 mL Inactive Ingredients Ingredient Name Strength ANHYDROUS DEXTROSE (UNII: 5SL0G7R0OK) 4 g in 100 mL SODIUM BICARBONATE (UNII: 8MDF5V39QO) WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0338-3508-41 12 in 1 CASE 08/07/2015 1 100 mL in 1 BAG; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA207131 08/07/2015 Labeler - Baxter Healthcare Corporation (005083209) Establishment Name Address ID/FEI Business Operations Baxter Healthcare Corporation 194684502 ANALYSIS(0338-3508) , LABEL(0338-3508) , MANUFACTURE(0338-3508) , PACK(0338-3508) , STERILIZE(0338-3508) Establishment Name Address ID/FEI Business Operations Baxter Healthcare Corporation 059140764 ANALYSIS(0338-3508)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.