JAVYGTOR- sapropterin dihydrochloride tablet
JAVYGTOR by
Drug Labeling and Warnings
JAVYGTOR by is a Prescription medication manufactured, distributed, or labeled by Dr. Reddys Laboratories Inc, Dr. Reddys Laboratories Limited (SEZ UNIT). Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use JAVYGTOR safely and effectively. See full prescribing information for JAVYGTOR.
JAVYGTORTM (sapropterin dihydrochloride) tablets, for oral use.
Initial U.S. Approval: 2007INDICATIONS AND USAGE
JAVYGTOR (sapropterin dihydrochloride) is a phenylalanine hydroxylase activator indicated to reduce blood phenylalanine (Phe) levels in adult and pediatric patients one month of age and older with hyperphenylalaninemia (HPA) due to tetrahydrobiopterin- (BH4-) responsive Phenylketonuria (PKU). JAVYGTOR is to be used in conjunction with a Phe-restricted diet. (1)
DOSAGE AND ADMINISTRATION
All patients with PKU who are being treated with JAVYGTOR (sapropterin dihydrochloride) should also be treated with a Phe-restricted diet, including dietary protein and Phe restriction. (2.1)
Starting dosage:
Pediatric patients 1 month to 6 years: The recommended starting dose of JAVYGTOR is 10 mg/kg administered orally once daily. (2.2)
Patients 7 years and older: The recommended starting dose of JAVYGTOR is 10 to 20 mg/kg administered orally once daily. (2.2)
Dosage Adjustment:
Doses of JAVYGTOR tablets may be adjusted in the range of 5 to 20 mg/kg taken once daily. (2.2)
Monitor blood Phe regularly, especially in pediatric patients. (2.2, 5.3)
Preparation and Administration
See the full prescribing information for preparation and administration instructions. (2.3)
DOSAGE FORMS AND STRENGTHS
Tablets: 100 mg sapropterin dihydrochloride. (3)
CONTRAINDICATIONS
None (4).
WARNINGS AND PRECAUTIONS
Hypersensitivity reactions including anaphylaxis: JAVYGTOR (sapropterin dihydrochloride) is not recommended in patients with a history of anaphylaxis to sapropterin dihydrochloride; discontinue treatment in patients who experience anaphylaxis and initate appropriate medical treatment. Continue dietary Phe restrictions. (5.1)
Upper Gastrointestinal Mucosal Inflammation: Monitor patients for signs and symptoms of these conditions including esophagitis and gastritis. (5.2)
Hypophenylalaninemia: Pediatric patients younger than 7 years treated with JAVYGTOR doses of 20 mg/kg per day are at increased risk for low levels of blood Phe compared with patients 7 years and older. (5.3)
Monitoring Blood Phe Levels During Treatment: Ensure adequate blood Phe control and nutritional balance during treatment with JAVYGTOR. Frequent blood monitoring is recommended, especially in pediatric patients. (5.4, 2.1).
Lack of Biochemical Response to JAVYGTOR Treatment: Response to JAVYGTOR treatment cannot be pre-determined by laboratory (e.g., molecular) testing and can only be determined by a therapeutic trial of JAVYGTOR. (5.5, 2.1)
Interaction with Levodopa: Seizures, over-stimulation or irritability may occur; monitor patients for a change in neurologic status. (5.6, 7)
Hyperactivity: Monitor patients for hyperactivity. (5.7)
ADVERSE REACTIONS
Most common adverse reactions ( ≥4%) are: headache, rhinorrhea, pharyngolaryngeal pain, diarrhea, vomiting, cough, and nasal congestion (6.1).
To report SUSPECTED ADVERSE REACTIONS, contact Dr. Reddy’s Laboratories, Inc. at 1-888-375-3784 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
Inhibitors of Folate Synthesis (e.g., methotrexate, valproic acid, phenobarbital, trimethoprim): Can decrease endogenous BH4 levels; monitor blood Phe levels more frequently and adjust JAVYGTOR dosage as needed. (7)
Drugs Affecting Nitric Oxide-Mediated Vasorelaxation (e.g., PDE-5 inhibitors): Potential for vasorelaxation; monitor blood pressure. (7)
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 10/2024
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Recommendations Prior to JAVYGTOR Treatment
2.2 Recommended Dosage andAdministration
2.3 Preparation and Administration Instructions
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Hypersensitivity Reactions Including Anaphylaxis
5.2 Upper Gastrointestinal Mucosal Inflammation
5.3 Hypophenylalaninemia
5.4 Monitoring Blood Phe Levels During Treatment
5.5 Lack of Biochemical Response to JAVYGTOR
5.6 Interaction with Levodopa
5.7 Hyperactivity
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment Of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
JAVYGTOR (sapropterin dihydrochloride) is indicated to reduce blood phenylalanine (Phe) levels in adult and pediatric patients one month of age and older with hyperphenylalaninemia (HPA) due to tetrahydrobiopterin-(BH4-) responsive Phenylketonuria (PKU). JAVYGTOR is to be used in conjunction with a Phe-restricted diet.
-
2 DOSAGE AND ADMINISTRATION
2.1 Recommendations Prior to JAVYGTOR Treatment
Treatment with JAVYGTOR should be directed by physicians knowledgeable in the management of PKU.
All patients with PKU who are being treated with JAVYGTOR should also be treated with a Phe-restricted diet, including dietary protein and Phe restriction.
2.2 Recommended Dosage andAdministration
The recommended starting dosage of JAVYGTOR is:
Pediatric Patients 1 month to 6 years: 10 mg/kg (actual body weight) administered orally once daily.
Patients 7 years and older: 10 to 20 mg/kg (actual body weight) administered orally once daily.
Administer JAVYGTOR with a meal, preferably at the same time each day [see ClinicalPharmacology (12.3)].
A missed dose should be administered as soon as possible, but two doses should not be administered on the same day.
Evaluation Period
Existing dietary protein and Phe intake should not be modified during the evaluation period.
If a 10 mg/kg per day starting dose is used, then response to therapy is determined by change in blood Phe following treatment with JAVYGTOR at 10 mg/kg per day for a period of up to 1 month. Blood Phe levels should be checked after 1 week of JAVYGTOR treatment and periodically for up to a month. If blood Phe does not decrease from baseline at 10 mg/kg per day, the dose may be increased to 20 mg/kg per day. Patients whose blood Phe does not decrease after 1 month of treatment at 20 mg/kg per day do not show a biochemical response and treatment with JAVYGTOR should be discontinued in these patients.
If a 20 mg/kg per day starting dose is used, then response to therapy is determined by change in blood Phe following treatment with JAVYGTOR at 20 mg/kg per day for a period of 1 month. Blood Phe levels should be checked after 1 week of JAVYGTOR treatment and periodically during the first month. Treatment should be discontinued in patients who do not show a biochemical response (blood Phe does not decrease) after 1 month of treatment at 20 mg/kg per day [see Warnings and Precautions (5.4)].
Dosage Adjustment
Once responsiveness to JAVYGTOR has been established, the dosage may be adjusted within the range of 5 to 20 mg/kg per day according to biochemical response to therapy (blood Phe). Periodic blood Phe monitoring is recommended to assess blood Phe control, especially in pediatric patients [see Warnings and Precautions (5.3)].
2.3 Preparation and Administration Instructions
JAVYGTOR(sapropterin dihydrochloride) Tablets
- JAVYGTOR tablets may be swallowed either as whole tablets or dissolved in 120 to 240 mL of water or apple juice and taken orally within 15 minutes of dissolution.
- It may take a few minutes for the tablets to dissolve.
- To make the tablets dissolve faster, tablets may be stirred or crushed.
- The tablets may not dissolve completely. Patients may see small pieces floating on top of the water or apple juice. This is normal and safe for patients to swallow.
- If after drinking the medicine patients still see pieces of the tablet in the container, more water or apple juice can be added to make sure all of the medicine is consumed.
- JAVYGTOR tablets may also be crushed and then mixed in a small amount of soft foods such as apple sauce or pudding.
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Hypersensitivity Reactions Including Anaphylaxis
JAVYGTOR is not recommended in patients with a history of anaphylaxis to sapropterin dihydrochloride. Hypersensitivity reactions, including anaphylaxis and rash, have occurred [see Adverse Reactions (6.2)]. Signs of anaphylaxis include wheezing, dyspnea, coughing, hypotension, flushing, nausea, and rash. Discontinue treatment with JAVYGTOR in patients who experience anaphylaxis and initiate appropriate medical treatment. Continue dietary protein and Phe restriction in patients who experience anaphylaxis.
5.2 Upper Gastrointestinal Mucosal Inflammation
Gastrointestinal (GI) adverse reactions suggestive of upper GI mucosal inflammation have been reported with sapropterin dihydrochloride. Serious adverse reactions included esophagitis and gastritis [see Adverse Reactions (6.2)]. If left untreated, these could lead to severe sequelae including esophageal stricture, esophageal ulcer, gastric ulcer, and bleeding and such complications have been reported in patients receiving JAVYGTOR tablets. Monitor patients for signs and symptoms of upper GI mucosal inflammation.
5.3 Hypophenylalaninemia
In clinical trials of sapropterin dihydrochloride, some PKU patients experienced hypophenylalaninemia (low blood Phe) during treatment with sapropterin dihydrochloride. In a clinical study of pediatric patients younger than 7 years old treated with sapropterin dihydrochloride 20 mg/kg per day, the incidence of hypophenylalaninemia was higher than in clinical trials of older patients [see Adverse Reactions (6.1)].
5.4 Monitoring Blood Phe Levels During Treatment
Prolonged elevations of blood Phe levels in patients with PKU can result in severe neurologic damage, including severe intellectual disability, developmental delay, microcephaly, delayed speech, seizures, and behavioral abnormalities. Conversely, prolonged levels of blood Phe that are too low have been associated with catabolism and endogenous protein breakdown, which has been associated with adverse developmental outcomes. Active management of dietary Phe intake while taking JAVYGTOR tablets are required to ensure adequate Phe control and nutritional balance. Monitor blood Phe levels during treatment to ensure adequate blood Phe level control. Frequent blood monitoring is recommended in the pediatric population [see Dosage and Administration (2.2)].
5.5 Lack of Biochemical Response to JAVYGTOR
Some patients with PKU do not show biochemical response (reduction in blood Phe) with treatment with JAVYGTOR. In two clinical trials at a sapropterin dihydrochloride dose of 20 mg/kg per day, 56% to 75% of pediatric PKU patients showed a biochemical response to sapropterin dihydrochloride, and in one clinical trial at a dose of 10 mg/kg per day, 20% of adult and pediatric PKU patients showed a biochemical response to sapropterin dihydrochloride [see Clinical Studies (14)].
Biochemical response to JAVYGTOR treatment cannot generally be pre-determined by laboratory testing (e.g., molecular testing), and should be determined through a therapeutic trial (evaluation) of sapropterin dihydrochloride response [see Dosage and Administration (2.2)].
5.6 Interaction with Levodopa
In a 10-year post-marketing safety surveillance program for a non-PKU indication using another sapropterin product, 3 patients with underlying neurological disorders experienced seizures, exacerbation of seizures, over-stimulation, and irritability during co-administration of levodopa and sapropterin. Monitor patients who are receiving levodopa for changes in neurological status during treatment with sapropterin dihydrochloride [see Drug Interactions (7)].
5.7 Hyperactivity
In the sapropterin dihydrochloride post-marketing safety surveillance program, 2 patients with PKU experienced hyperactivity when treated with sapropterin dihydrochloride [see Adverse Reactions (6.2)]. Monitor patients for hyperactivity.
-
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to the rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
PKU Clinical Studies
The safety of sapropterin dihydrochloride was evaluated in 7 clinical studies in patients with PKU (aged 1 month to 50 years) [see Clinical Studies (14)] .
In Studies1 to 4 (controlled and uncontrolled studies), 579 patients with PKU aged 4 to 49 years received sapropterin dihydrochloride in doses ranging from 5 to 20 mg/kg per day for lengths of treatment ranging from 1 to 164 weeks. The patient population was evenly distributed in gender, and approximately 95% of patients were Caucasian. The most common adverse reactions (≥4% of patients) were headache, rhinorrhea, pharyngolaryngeal pain, diarrhea, vomiting, cough, and nasal congestion.
The data described in Table 3 reflect exposure of 74 patients with PKU to sapropterin dihydrochloride at doses of 10 to 20 mg/kg per day for 6 to 10 weeks in two double-blind, placebo-controlled clinical trials (Studies 2 and 4).
Table 3 enumerates adverse reactions occurring in at least 4% of patients treated with sapropterin dihydrochloride in the double-blind, placebo-controlled clinical trials described above.
Table 3: Summary of Adverse Reactions Occurring in ≥4% of Patients in Placebo-Controlled Clinical Studies with Sapropterin Dihydrochloride
MedDRA Preferred Term Treatment
Placebo
(N=59)Sapropterin
Dihydrochloride
(N = 74)
No. Patients (%)No. Patients (%) Headache 11 (15) 8 (14) Rhinorrhea 8 (11) 0 Pharyngolaryngeal pain 7(10) 1 (2) Diarrhea 6 (8) 3 (5) Vomiting 6 (8) 4 (7) Cough 5 (7) 3 (5) Nasal congestion 3 (4) 0 In open-label, uncontrolled clinical trials (Studies 1 and 3) all patients received sapropterin dihydrochloride in doses of 5 to 20 mg/kg per day, and adverse reactions were similar in type and frequency to those reported in the double-blind, placebo-controlled clinical trials [see Clinical Studies (14)] .
In Study 5, 65 pediatric patients with PKU aged 1 month to 6 years received sapropterin dihydrochloride 20 mg/kg per day for 6 months. Adverse reactions in these patients were similar in frequency and type as those seen in other sapropterin dihydrochloride clinical trials except for an increased incidence of low Phe levels. Twenty-five percent (16 out of 65) of patients developed Phe levels below normal for age [see Warnings and Precautions (5.3), Use in Specific Populations (8.4), and Clinical Studies (14)].
In Study 6, a long term, open-label, extension study of 111 patients aged 4 to 50 years, receiving sapropterin dihydrochloride in doses of ranging from 5 to 20 mg/kg per day, adverse reactions were similar in type and frequency to those reported in the previous clinical studies. Fifty-five patients received sapropterin dihydrochloride both as dissolved and intact tablets. There were no notable differences in the incidence or severity of adverse reactions between the two methods of administration. The mean (± SD) exposure to sapropterin for the entire study population was 659 ± 221 days (maximum 953 days).
In Study 7, 27 pediatric patients with PKU aged 0 to 4 years received sapropterin dihydrochloride 10 mg/kg per day or 20 mg/kg per day. Adverse reactions were similar in type and frequency to those observed in other clinical trials, with the addition of rhinitis, which was reported in 2 subjects (7.4%).
Safety Experience From Clinical Studies for Non-PKU Indications
Approximately 800 healthy subjects and patients with disorders other than PKU, some of whom had underlying neurologic disorders or cardiovascular disease, have been administered a different formulation of the same active ingredient (sapropterin) in approximately 19 controlled and uncontrolled clinical trials. In these clinical trials, subjects were administered sapropterin at doses ranging from 1 to 100 mg/kg per day for lengths of exposure from 1 day to 2 years. Serious and severe adverse reactions (regardless of causality) during sapropterin administration were seizures, exacerbation of seizures [see Warnings and Precautions (5.3)], dizziness, gastrointestinal bleeding, post-procedural bleeding, headache, irritability, myocardial infarction, overstimulation, and respiratory failure. Common adverse reactions were headache, peripheral edema, arthralgia, polyuria, agitation, dizziness, nausea, pharyngitis, abdominal pain, upper abdominal pain, and upper respiratory tract infection.
6.2 Postmarketing Experience
The following adverse reactions have been reported during post-approval use of sapropterin dihydrochloride. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Hypersensitivity reactions including anaphylaxis and rash: Most hypersensitivity reactions occurred within several days of initiating treatment [see Warnings and Precautions (5.1)].
Gastrointestinal reactions: esophagitis, gastritis, oropharyngeal pain, pharyngitis, esophageal pain, abdominal pain, dyspepsia, nausea, and vomiting [see Warnings and Precautions (5.2)].
Hyperactivity: Two cases have been reported. In one case, the patient received an accidental overdosage of sapropterin dihydrochloride [see Warnings and Precautions (5.6), Overdosage (10)].
-
7 DRUG INTERACTIONS
Table 4 includes drugs with clinically important drug interactions when administered with sapropterin dihydrochloride and instructions for preventing or managing them.
Table 4: Clinically Relevant Drug Interactions
Levodopa Clinical Impact Sapropterin dihydrochloride may increase the availability of tyrosine, a precursor of levodopa. Neurologic events were reported post-marketing in patients receiving sapropterin and levodopa concomitantly for a non-PKU indication [see Warnings and Precautions (5.5)] Intervention Monitor patients for a change in neurologic status. Inhibitors of Folate Synthesis (e.g., methotrexate, valproic acid, phenobarbital, trimethoprim) Clinical Impact In vitro and in vivo nonclinical data suggest that drugs that inhibit folate synthesis may decrease the bioavailability of endogenous BH4 by inhibiting the enzyme dihydrofolate reductase, which is involved in the recycling (regeneration) of BH4. This reduction in net BH4 levels may increase Phe levels. Intervention Consider monitoring blood Phe levels more frequently during concomitant administration. An increased dosage of sapropterin dihydrochloride may be necessary to achieve a biochemical response. Drugs Affecting Nitric Oxide-Mediated Vasorelaxation (e.g., PDE-5 inhibitors such as sildenafil, vardenafil, or tadalafil) Clinical Impact Both sapropterin dihydrochloride and PDE-5 inhibitors may induce vasorelaxation. A reduction in blood pressure could occur; however, the combined use of these medications has not been evaluated in humans. Intervention Monitor blood pressure. -
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Available data from pregnancy safety studies, pharmacovigilance, and published case reportswith sapropterin use during pregnancy have not identified a drug-associated risk of major birthdefects, miscarriage, or adverse maternal or fetal outcomes (see Data). Uncontrolled bloodphenylalanine concentrations before and during pregnancy are associated with an increased riskof adverse pregnancy outcomes and fetal adverse effects (see Clinical Considerations).
An embryo-fetal development study with sapropterin dihydrochloride in rats using oral doses up to 3 times the maximum recommended human dose (MRHD) given during the period of organogenesis showed no effects. In a rabbit study using oral administration of sapropterin dihydrochloride during the period of organogenesis, a rare defect, holoprosencephaly, was noted at 10 times the MRHD.
All pregnancies have a background risk of major birth defects, pregnancy loss, or other adverse pregnancy outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively. The estimated background risk of major birth defects and miscarriage in pregnant women with PKU who maintain blood phenylalanine concentrations greater than 600 micromol/L during pregnancy is greater than the corresponding background risk for pregnant women without PKU.
Clinical Considerations
Disease-associated maternal and/or embryofetal risk
Uncontrolled blood phenylalanine concentrations before and during pregnancy are associated with an increased risk of adverse pregnancy outcomes and fetal adverse effects. To reduce the risk of hyperphenylalaninemia-induced fetal adverse effects, blood phenylalanine concentrations should be maintained between 120 and 360 micromol/L during pregnancy and during the 3 months before conception [see Dosage and Administration (2.2)].
Data
Human Data
Uncontrolled Maternal PKU
Available data from the Maternal Phenylketonuria Collaborative Study on 468 pregnancies and 331 live births in PKU-affected women demonstrated that uncontrolled Phe levels above 600 micromol/L are associated with a very high incidence of neurological, cardiac, facial dysmorphism, and growth anomalies. Control of blood phenylalanine during pregnancy is essential to reduce the incidence of Phe-induced teratogenic effects.
Pregnancy Registry Data
Available data from pregnancy sub-registries within the Phenylketonuria Developmental Outcomes and Safety (PKUDOS) Registry and the Sapropterin Dihydrochloride Adult Maternal Pediatric European Registry (KAMPER) have identified 72 live births (79 pregnancies) in women with PKU exposed to sapropterin during pregnancy. Three birth defects were reported, including one case each of microcephaly, cleft palate, and tongue tie. The two major birth defects (microcephaly and cleft palate) were associated with Phe levels greater than 360 micromol/L during pregnancy.
Animal Data
No effects on embryo-fetal development were observed in a reproduction study in rats using oral doses of up to 400 mg/kg per day sapropterin dihydrochloride (about 3 times the MRHD of 20 mg/kg per day, based on body surface area) administered during the period of organogenesis. However, in a rabbit reproduction study, oral administration of a maximum dose of 600 mg/kg per day (about 10 times the MRHD, based on body surface area) during the period of organogenesis was associated with a non-statistically significant increase in the incidence of holoprosencephaly in two high dose-treated litters (4 fetuses), compared to one control-treated litter (1 fetus).
8.2 Lactation
Risk Summary
There are insufficient data to assess the presence of sapropterin in human milk and no data on the effects on milk production. In postmarketing pregnancy registries, 13 infants were exposed to sapropterin through breastfeeding. No lactation-related safety concerns were reported in infants of mothers nursing during maternal treatment with sapropterin dihydrochloride. There are no data on the effects on milk production. Sapropterin is present in the milk of lactating rats following intravenous administration, but not following oral administration.
The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for sapropterin dihydrochloride and any potential adverse effects on the breastfed child from sapropterin dihydrochloride or from the underlying maternal condition.
8.4 Pediatric Use
Pediatric patients with PKU, ages 1 month to 16 years, have been treated with sapropterin dihydrochloride in clinical trials [see Clinical Studies (14)].
The efficacy and safety of sapropterin dihydrochloride have not been established in neonates. The safety of sapropterin dihydrochloride has been established in children younger than 4 years in trials of 6 months duration and in children 4 years and older in trials of up to 3 years in length[see Adverse Reactions (6.1)].
In children aged 1 month and older, the efficacy of sapropterin dihydrochloride has been demonstrated in trials of 6 weeks or less in duration [see Clinical Studies (14)] .
In a multicenter, open-label, single arm study, 57 patients aged 1 month to 6 years who were defined as sapropterin dihydrochloride responders after 4 weeks of sapropterin dihydrochloride treatment and Phe dietary restriction were treated for 6 months with sapropterin dihydrochloride at 20 mg/kg per day. The effectiveness of sapropterin dihydrochloride alone on reduction of blood Phe levels beyond 4 weeks could not be determined due to concurrent changes in dietary Phe intake during the study. Mean (±SD) blood Phe values over time for patients aged 1 month to <2 years and 2 to <7 years are shown in Figure 1.
Figure 1: Mean Blood Phe Level Over Time by Age (years) (N=57)
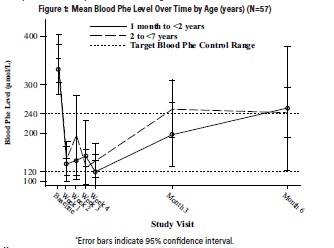
-
10 OVERDOSAGE
Two unintentional overdosages with sapropterin dihydrochloride have been reported. One adult patient in a sapropterin dihydrochloride clinical trial received a single sapropterin dihydrochloride dose of 4,500 mg (36 mg/kg) instead of 2,600 mg (20 mg/kg). The patient reported mild headache and mild dizziness immediately after taking the dose; both symptoms resolved within 1 hour with no treatment intervention. There were no associated laboratory test abnormalities. The patient suspended therapy for 24 hours and then restarted sapropterin dihydrochloride with no reports of abnormal signs or symptoms. In postmarketing, one pediatric patient received sapropterin dihydrochloride doses of 45 mg/kg per day instead of 20 mg/kg per day. The patient reported hyperactivity that began at an unspecified time after overdosage and resolved after the sapropterin dihydrochloride dose was reduced to 20 mg/kg per day.
In a clinical study to evaluate the effects of sapropterin dihydrochloride on cardiac repolarization, a single supra-therapeutic dose of 100 mg/kg (5 times the maximum recommended dose) was administered to 54 healthy adults. No serious adverse reactions were reported during the study. The only adverse reactions reported in more than 1 subject who received the supra-therapeutic dose were upper abdominal pain (6%) and dizziness (4%). A dose-dependent shortening of the QT interval was observed [see Clinical Pharmacology (12.2)].
Patients should be advised to notify their physicians in cases of overdosage.
-
11 DESCRIPTION
JAVYGTOR (sapropterin dihydrochloride) is an orally administered Phenylalanine Hydroxylase activator (or PAH activator). Sapropterin dihydrochloride, the active pharmaceutical ingredient in JAVYGTOR, is a synthetic preparation of the dihydrochloride salt of naturally occurring tetrahydrobiopterin (BH4). Sapropterin dihydrochloride is a white crystalline powder.
The chemical name of sapropterin dihydrochloride is (6R)-2-amino-6-[(1R,2S)-1,2- dihydroxypropyl]-5,6,7,8-tetrahydro-4(1H)-pteridinone dihydrochloride and the molecular formula is C9H15N5O3·2HCl with a molecular weight of 314.17.
Sapropterin dihydrochloride has the following structural formula:
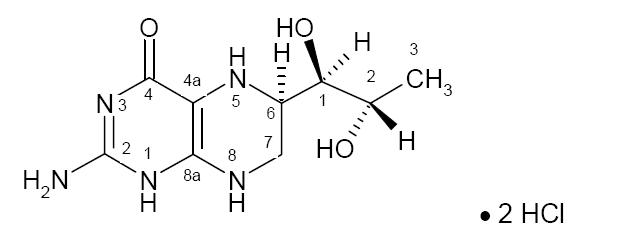
JAVYGTOR is supplied as tablets contains 100 mg of sapropterin dihydrochloride (equivalent to 76.8 mg of sapropterin base).
Tablets are off-white to light yellow, mottled, round uncoated tablet debossed with ‘|’ on one side and plain on other side. Each tablet contains the following inactive ingredients: ascorbic acid, colloidal silicon dioxide, crospovidone, low substituted hydroxypropyl cellulose, mannitol, riboflavin and sodium stearyl fumarate.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Sapropterin dihydrochloride is a synthetic form of BH4, the cofactor for the enzyme phenylalanine hydroxylase (PAH). PAH hydroxylates Phe through an oxidative reaction to form tyrosine. In patients with PKU, PAH activity is absent or deficient. Treatment with BH4 can activate residual PAH enzyme activity, improve the normal oxidative metabolism of Phe, and decrease Phe levels in some patients.
12.2 Pharmacodynamics
In PKU patients who are responsive to BH4 treatment, blood Phe levels decrease within 24 hours after a single administration of sapropterin dihydrochloride, although maximal effect on Phe level may take up to a month, depending on the patient. A single daily dose of sapropterin dihydrochloride is adequate to maintain stable blood Phe levels over a 24-hour period. Twelve patients with blood Phe levels ranging from 516 to 986 micromol/L (mean 747 ± 153 micromol/L) were assessed with 24-hour blood Phe level monitoring following a daily morning dose of 10 mg/kg per day. The blood Phe level remained stable during a 24-hour observation period. No substantial increases in blood Phe levels were observed following food intake throughout the 24-hour period.
Sapropterin dihydrochloride dose-response relationship was studied in an open-label, forced titration study at doses of 5 mg/kg per day, then 20 mg/kg per day, and then 10 mg/kg per day (Study 3) [see Clinical Studies (14)]. Individual blood Phe levels were highly variable among patients. The mean blood Phe level observed at the end of each 2-week dosing period decreased as the dose of sapropterin dihydrochloride increased, demonstrating an inverse relationship between the dose of sapropterin dihydrochloride and mean blood Phe levels.
Cardiac Electrophysiology
A thorough QTc study was performed in 56 healthy adults. This randomized, placebo and active controlled crossover study was conducted to determine if a single supra-therapeutic (100 mg/kg) dose of sapropterin dihydrochloride, or a single therapeutic dose (20 mg/kg) of sapropterin dihydrochloride had an effect on cardiac repolarization. In this study, sapropterin dihydrochloride was administered after dissolving tablets in water under fed condition. This study demonstrated a dose-dependent shortening of the QT interval. The maximum placebo-subtracted mean change from baseline of the QTc interval was -3.69 and -8.32 ms (lower bound of 90% CI: -5.3 and -10.6 ms) at 20 and 100 mg/kg, respectively.
12.3 Pharmacokinetics
Studies in healthy subjects have shown comparable absorption of sapropterin when tablets are dissolved in water or orange juice and taken under fasted conditions. Administration of dissolved tablets after a high-fat/high-calorie meal resulted in mean increases in Cmax of 84% and AUC of 87% (dissolved in water). However, there was extensive variability in individual subject values for Cmax and AUC across the different modes of administration and meal conditions. In the clinical trials of sapropterin dihydrochloride, drug was administered in the morning as a dissolved tablet without regard to meals. The mean elimination half-life in PKU patients was approximately 6.7 hours (range 3.9 to 17 hours), comparable with values seen in healthy subjects (range 3 to 5.3 hours).
A study in healthy adults with 10 mg/kg of sapropterin dihydrochloride demonstrated that the absorption via intact tablet administration was 40% greater than via dissolved tablet administration under fasted conditions based on AUC0-t. The administration of intact tablets under fed conditions resulted in an approximately 43% increase in the extent of absorption compared to fasted conditions based on AUC0-t[see Dosage and Administration (2.3)].
Population pharmacokinetic analysis of sapropterin including patients from 1 month to 49 years of age showed that body weight is the only covariate substantially affecting clearance or distribution volume (see Table 5). Pharmacokinetics in patients >49 years of age have not been studied.
Table 5. Apparent Plasma Clearance by Age
Parameter 0 to <1 yr*
(N=10)1 to <6 yr*
(N=57)6 to <12 yr†
(N=23)12 to <18 yr†
(N=24)≥18 yr†
(N=42)CL/F (L/hr/kg) Mean ± SD
(Median)81.5 ± 92.4
(53.6)50.7 ± 20.1
(48.4)51.7 ± 21.9
(47.4)39.2 ± 9.3
(38.3)37.9 ± 20.2
(31.8)*Evaluated at 20 mg/kg per day dose
†Evaluated at 5, 10, or 20 mg/kg per day doses
Metabolism
Sapropterin is a synthetic form of tetrahydrobiopterin (BH4) and is expected to be metabolized and recycled by the same endogenous enzymes. In vivo endogenous BH4 is converted to quinoid dihydrobiopterin and is metabolized to dihydrobiopterin and biopterin. The enzymes dihydrofolate reductase and dihydropteridine reductase are responsible for the metabolism and recycling of BH4.
Drug Interaction Studies
Clinical Studies
In healthy subjects, administration of a single dose of sapropterin dihydrochloride at the maximum therapeutic dose of 20 mg/kg had no effect on the pharmacokinetics of a single dose of digoxin (P-gp substrate) administered concomitantly.
In vitroStudies Where Drug Interaction Potential Was Not Further Evaluated Clinically
The potential for sapropterin to induce or inhibit cytochrome P450 enzymes was evaluated in in vitro studies which showed sapropterin did not inhibit CYP 1A2, 2B6, 2C8, 2C9, 2C19, 2D6, or 3A4/5, nor induce CYP 1A2, 2B6, or 3A4/5.
In vitro sapropterin did not inhibit OAT1, OAT3, OCT2, MATE1, and MATE2-K transporters. The potential for sapropterin to inhibit OATP1B1 and OATP1B3 has not been adequately studied. In vitro, sapropterin inhibits breast cancer resistance protein (BCRP) but the potential for a clinically significant increase in systemic exposure of BCRP substrates by sapropterin dihydrochloride appears to below.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment Of Fertility
A 2-year carcinogenicity study was conducted in F-344 rats, and a 78-week carcinogenicity study was conducted in CD-1 mice. In the 104-week oral carcinogenicity study in rats, sapropterin dihydrochloride doses of 25, 80, and 250 mg/kg per day (0.2, 0.7, and 2 times the maximum recommended human dose of 20 mg/kg per day, respectively, based on body surface area) were used. In the 78-week oral carcinogenicity study in mice, sapropterin dihydrochloride doses of 25, 80, and 250 mg/kg per day (0.1, 0.3, and 2 times the recommended human dose, respectively, based on body surface area) were used. In the 2-year rat carcinogenicity study, there was a statistically significant increase in the incidence of benign adrenal pheochromocytoma in male rats treated with the 250 mg/kg per day (about 2 times the maximum recommended human dose, based on body surface area) dose, as compared to vehicle treated rats. The mouse carcinogenicity study showed no evidence of a carcinogenic effect, but the study was not ideal due to its duration of 78 instead of 104 weeks.
Sapropterin dihydrochloride was genotoxic in the in vitro Ames test at concentrations of 625 mcg (TA98) and 5,000 mcg (TA100) per plate, without metabolic activation. However, no genotoxicity was observed in the in vitro Ames test with metabolic activation. Sapropterin dihydrochloride was genotoxic in the in vitro chromosomal aberration assay in Chinese hamster lung cells at concentrations of 0.25 and 0.5 mM. Sapropterin dihydrochloride was not mutagenic in the in vivo micronucleus assay in mice at doses up to 2,000 mg/kg per day (about 8 times the maximum recommended human dose of 20 mg/kg per day, based on body surface area). Sapropterin dihydrochloride, at oral doses up to 400 mg/kg per day (about 3 times the maximum recommended human dose, based on body surface area) was found to have no effect on fertility and reproductive function of male and female rats.
-
14 CLINICAL STUDIES
The efficacy of sapropterin dihydrochloride was evaluated in five clinical studies in patients with PKU.
Study 1 was a multicenter, open-label, uncontrolled clinical trial of 489 patients with PKU, ages 8 to 48 years (mean 22 years), who had baseline blood Phe levels ≥450 micromol/L and who were not on Phe-restricted diets. All patients receivedtreatment with sapropterin dihydrochloride 10 mg/kg per day for 8 days. For the purposes of this study, response to sapropterin dihydrochloride treatment was defined as a ≥30% decrease in blood Phe from baseline. At Day 8, 96 patients (20%) were identified as responders.
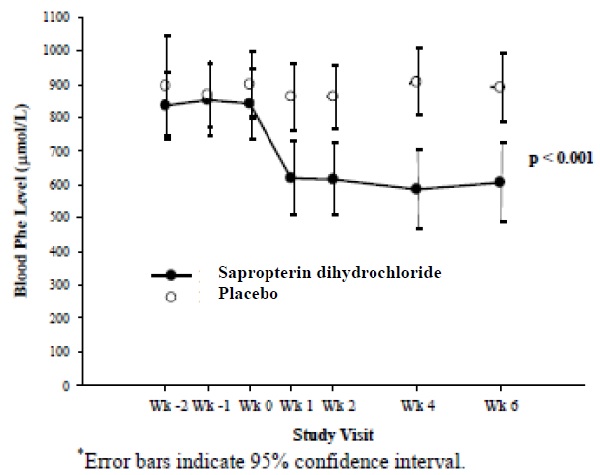
Study 2 was a multicenter, double-blind, placebo-controlled study of 88 patients with PKU who responded to sapropterin dihydrochloride in Study 1. After a washout period from Study 1, patients were randomized equally to either sapropterin dihydrochloride 10 mg/kg per day (N=41) or placebo (N=47) for 6 weeks. Efficacy was assessed by the mean change in blood Phe level from baseline to Week 6 in the sapropterin dihydrochloride-treated group as compared to the mean change in the placebo group.
The results showed that at baseline, the mean (±SD) blood Phe level was 843 (±300) micromol/L in the sapropterin dihydrochloride-treated group and 888 (±323) micromol/L in the placebo group. At Week 6, the sapropterin dihydrochloride-treated group had a mean (±SD) blood Phe level of 607 (±377) micromol/L,and the placebo group had a mean blood Phe level of 891 (±348) micromol/L. At Week 6, the sapropterin dihydrochloride- and placebo-treated groups had mean changes in blood Phe level of –239 and 6 micromol/L, respectively (mean percent changes of –29% (±32) and 3% (±33), respectively). The difference between the groups was statistically significant (p < 0.001) (Table 6).
Table 6: Blood Phe Results in Study 2
Sapropterin (N=41) Placebo (N=47) Baseline Blood Phe Level* (micromol/L) Mean (±SD) 843 (±300) 888 (±323) Percentiles (25th, 75th) 620, 990 618, 1141 Week 6 Blood Phe Level (micromol/L) Mean (±SD) 607 (±377) 891 (±348) Percentiles (25th, 75th) 307, 812 619, 1143 Mean Change in Blood Phe From Baseline to Week 6 (micromol/L) Adjusted Mean (±SE)† -239 (±38) 6 (±36) Percentiles (25th, 75th) -397, -92 -96, 93 Mean Percent Change in Blood Phe From Baseline to Week 6 Mean (±SD) -29 (±32) 3 (±33) Percentiles (25th, 75th) -61, -11 -13, 12 *The mean baseline levels shown in this table represent the mean of 3 pretreatment levels (Wk -2, Wk -1, and Wk 0). Treatment with sapropterin dihydrochloride or placebo started at Wk 0.
† p-value < 0.001, adjusted mean and standard error from an ANCOVA model with change in blood Phe level from baseline to Week 6 as the response variable, and both treatment group and baseline blood Phe level as covariates.
Change in blood Phe was noted in the sapropterin dihydrochloride-treated group at Week 1 and was sustained through Week 6 (Figure 2).
Figure 2: Mean Blood Phenylalanine (Phe) Level Over Time*
Study 3 was a multicenter, open-label, extension study in which 80 patients who responded to sapropterin dihydrochloride treatment in Study 1 and completed Study 2 underwent 6 weeks of forced dose-titration with 3 different doses of sapropterin dihydrochloride. Treatments consisted of 3 consecutive 2-week courses of sapropterin dihydrochloride at doses of 5, then 20, and then 10 mg/kg per day. Blood Phe level was monitored after 2 weeks of treatment at each dose level. At baseline, mean (±SD) blood Phe was 844 (±398) μmol/L. At the end of treatment with 5, 10, and 20 mg/kg per day, mean (±SD) blood Phe levels were 744 (±384) micromol/L, 640 (±382) micromol/L, and 581 (±399) micromol/L, respectively (Table 7).
Table 7: Blood Phe Results From Forced Dose-Titration in Study 3
Sapropterin Dihydrochloride Dose Level(mg/kg per day) No. of Patients Mean (±SD) BloodPhe Level (micromol/L) Mean Changes (±SD) inBlood Phe Level FromWeek 0 (micromol/L) Baseline(No Treatment) 80 844 (±398) — 5 80 744 (±384) -100 (±295) 10 80 640 (±382) -204 (±303) 20 80 581 (±399) -263 (±318) Study 4 was a multicenter study of 90 pediatric patients with PKU, ages 4 to 12 years, who were on Phe-restricted diets and who had blood Phe levels ≤480 micromol/L at screening. All patients were treated with open-label sapropterin dihydrochloride 20 mg/kg per day for 8 days. Response to sapropterin dihydrochloride was defined as a ≥30% decrease in blood Phe from baseline at Day 8. At Day 8, 50 patients (56%) had a ≥30% decrease in blood Phe.
Study 5 was an open label, single arm, multicenter trial in 93 pediatric patients with PKU, aged 1 month to 6 years, who had Phe levels greater than or equal to 360 micromol/L at screening. All patients were treated with sapropterin dihydrochloride at 20 mg/kg per day and maintained on a Phe-restricted diet. At Week 4, 57 patients (61%) were identified as responders (defined as ≥ 30% decreased in blood Phe from baseline) (see Use in Specific Population (8.4) Figure 1).
-
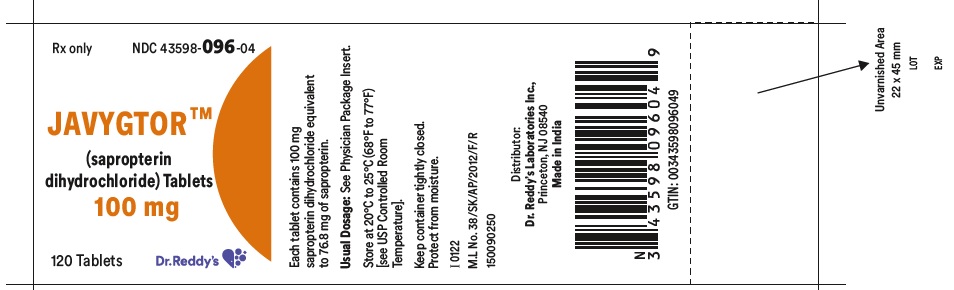
16 HOW SUPPLIED/STORAGE AND HANDLING
JAVYGTOR (sapropterin dihydrochloride) tablets 100 mg are off-white to light yellow, mottled, round uncoated tablet debossed with ‘|’ on one side and plain on other side. The tablets are supplied in bottles of 30, 120 and 500.
Bottles of 30 NDC: 43598-096-30
Bottles of 120 NDC: 43598-096-04
Bottles of 500 NDC: 43598-096-05
Storage
Store JAVYGTOR at 20°C to 25°C (68°F to 77°F) [see USP Controlled Room Temperature]. Keep container tightly closed. Protect from moisture.
-
17 PATIENT COUNSELING INFORMATION
Advise the patient or caregiver to read the FDA-approved patient labeling (Patient Information and Instructions for Use).
Hypersensitivity Reactions Including Anaphylaxis
Advise patients and caregivers to discontinue JAVYGTOR and contact the patient’s healthcare provider immediately if they experience symptoms of anaphylaxis, including (but not limited to) wheezing, dyspnea, coughing, hypotension, flushing, nausea, and rash. Continue nutritional management including dietary protein and Phe restriction [see Warnings and Precautions (5.1)].
Upper Gastrointestinal Mucosal Inflammation
Advise patients and caregivers to contact their healthcare provider if the patient experiences signs and symptoms suggestive of upper GI mucosal inflammation, including nausea, vomiting, dysphagia, dyspepsia, loss of appetite; oropharyngeal, esophageal, or upper abdominal pain [see Warnings and Precautions (5.3)].
Hypophenylalaninemia
Advise patients and caregivers that JAVYGTOR may cause hypophenylalaninemia (low blood Phe levels), especially in pediatric patients younger than 7 years of age [see Warnings and Precautions (5.3)].
Monitoring of Blood Phe Levels
Advise patients and caregivers that frequent blood Phe monitoring is important to ensure blood Phe levels are in the desirable range and that they should maintain dietary protein and Phe restriction while on JAVYGTOR [see Warnings and Precautions (5.4)].
Prolonged hyperphenylalaninemia (high blood Phe levels) in patients with PKU can result in severe neurologic damage, including intellectual disability, developmental delay, microcephaly, delayed speech,seizures, and behavioral abnormalities [see Warnings and Precautions (5.4)].
Lack of Biochemical Response to JAVYGTOR
Some patients do not show a biochemical response (blood Phe reduction) when treated with JAVYGTOR. Advise patients and caregivers to discontinue treatment with JAVYGTOR if the patient does not show an adequate biochemical response in blood Phe after one month of treatment with JAVYGTOR 20 mg/kg per day [see Dosage and Administration (2.2), Warnings and Precautions (5.4)].
Interaction with Levodopa
Advise patients and caregivers that patients with underlying neurological disorders taking JAVYGTOR in combination with levodopa may experience seizures, exacerbation of seizures, over-stimulation or irritability. Inform patients and caregivers to contact their healthcare provider if the patient has a change in neurologic status during treatment with JAVYGTOR [see Warnings and Precautions (5.5)].
Hyperactivity
Advise patients and caregivers that JAVYGTOR may cause hyperactivity and to contact their healthcare provider if the patient experiences hyperactivity, restlessness, fidgeting, or excessive talking [see Warnings and Precautions (5.6)].
Dosing and Monitoring[see Dosage and Administration (2.2)]
Advise patients and caregivers of the following:
JAVYGTOR tablets should be used in conjunction with a PKU-specific diet, including dietary protein and Phe restriction.
Dietary protein and Phe intake should not be modified during the JAVYGTOR evaluation period when assessing biochemical response.
The patient must be evaluated for changes in blood Phe after being treated with JAVYGTOR at the recommended dose(s) for age to determine if they have a biochemical response and that blood Phe levels and dietary Phe intake should be assessed frequently during the first month of JAVYGTOR treatment.
Monitoring of blood Phe levels is important during JAVYGTOR treatment.
Preparation and Administration[see Dosage and Administration (2.3)]
Advise patients and caregivers:
JAVYGTOR tablets can be swallowed whole, dissolved in water or apple juice, or crushed and mixed with a small amount of soft food such as apple sauce or pudding.
Take JAVYGTOR tablets with a meal, preferably at the same time each day.
Rx Only
Distributor:
Dr. Reddy’s Laboratories Inc.,
Princeton, NJ 08540
Made in India
Revised: 10/2024
-
PATIENT PACKAGE INSERT
PATIENT INFORMATION
JAVYGTOR™ (Jah' vig tor)
(sapropterin dihydrochloride)
TabletsWhat is JAVYGTOR?
JAVYGTOR is a prescription medicine used to lower blood levels of phenylalanine (Phe), in adults and children one month of age and older with a certain type of Phenylketonuria (PKU). JAVYGTOR is used along with a Phe-restricted diet.What should I tell my doctor before taking JAVYGTOR?
Before you take JAVYGTOR, tell your doctor about all your medical conditions, including if you
are allergic to sapropterin dihydrochloride or any of the ingredients in JAVYGTOR. See the list of ingredients in JAVYGTOR at the end of this leaflet.
have poor nutrition or have loss of appetite.
are pregnant or plan to become pregnant.
are breastfeeding or plan to breastfeed. It is not known if JAVYGTOR passes into your breast milk. Talk to your doctor about the best way to feed your baby if you take JAVYGTOR.
Tell your doctor about all the medicines you take, including prescription and over-the-counter medicines, vitamins, herbal, and dietary supplements.JAVYGTOR and other medicines may interact with each other.
Especially tell your doctor if you take:
a medicine that contains levodopa
an antifolate medicine
sildenafil (Revatio, Viagra), tadalafil (Adcirca, Cialis), vardenafil (Staxyn, Levitra)
Tell your doctor if you are not sure if your medicine is one that is listed above.
Know the medicines you take. Keep a list of them to show your doctor and pharmacist when you get a new medicine.How should I take JAVYGTOR?
- Take JAVYGTOR exactly as your doctor tells you. Your doctor should tell you how much JAVYGTOR to take and when to take them.
- Your doctor may change your dose of JAVYGTOR depending on how you respond to treatment.
- Take JAVYGTOR 1 time each day with a meal. It is best to take JAVYGTOR at the same time each day.
- JAVYGTOR comes as a tablet.
- You can swallow JAVYGTOR tablets whole or dissolve the tablets in water or apple juice. You may also crush the tablets and mix in a small amount of soft food, such as apple sauce or pudding before taking.
- See the detailed "Instructions for Use" that comes with JAVYGTOR for information about the correct way to dissolve and take a dose of JAVYGTOR.
- It is not possible to know if JAVYGTOR will work for you until you start taking JAVYGTOR tablets. Your doctor will check your blood Phe levels when you start taking JAVYGTOR to see if the medicine is working. During treatment with JAVYGTOR:
- Any change you make to your diet may affect your blood Phe level. Follow your doctor’s instructions carefully and do not make any changes to your dietary Phe intake without first talking with your doctor. Even if you take JAVYGTOR, if your Phe blood levels are not well controlled, you can develop severe neurologic problems.
- Your doctor should continue to monitor your blood Phe levels often during your treatment with JAVYGTOR, to make sure that your blood Phe levels are not too high or too low.
- If you have a fever, or if you are sick, your blood Phe level may go up. Tell your doctor as soon as possible so they can change your dose of JAVYGTOR to help keep your blood Phe levels in the desired range.
- If you forget to take your dose of JAVYGTOR, take it as soon as you remember that day. Do not take 2 doses in a day.
- If you take too much JAVYGTOR, call your doctor for advice.
What are the possible side effects of JAVYGTOR?
JAVYGTOR can cause serious side effects, including:
-
Severe allergic reactions. Stop taking JAVYGTOR and get medical help right away if you develop any of these symptoms of a severe allergic reaction:
- wheezing or trouble breathing
- coughing
- feeling lightheaded or you faint
- flushing
- nausea
- rash
- wheezing or trouble breathing
-
Inflammation of the lining of the stomach (gastritis) or esophagus (esophagitis). Gastritis or esophagitis can happen with JAVYGTOR and may be severe. Call your doctor right away if you have any of these signs or symptoms:
- severe upper stomach-area (abdominal) discomfort or pain, nausea and vomiting
- blood in your vomit or stool
- black, tarry stools
- difficulty swallowing
- loss of appetite
- pain in the throat
- Phe levels that are too low. Some children under the age of 7 years who take high doses of JAVYGTOR each day may experience low Phe levels.
-
Too much or constant activity (hyperactivity) can happen with JAVYGTOR. Tell your doctor if you have any signs of hyperactivity, including:
- fidgeting or moving around too much
- talking too much
- fidgeting or moving around too much
headache
runny nose and nasal congestion
sore throat
diarrhea
vomiting
cough
Tell your doctor if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of JAVYGTOR. For more information, ask your doctor or pharmacist. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.How should I store JAVYGTOR?
Store JAVYGTOR at room temperature between 20°C to 25°C (68°F to 77°F).
Keep JAVYGTOR in the original bottle with the cap closed tightly.
Protect from moisture.
Keep JAVYGTOR and all medicines out of the reach of children.General information about the safe and effective use of JAVYGTOR
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use JAVYGTOR for a condition for which it was not prescribed. Do not give JAVYGTOR to other people, even if they have the same symptoms you have. It may harm them. You can ask your pharmacist or doctor for information about JAVYGTOR that is written for health professionals.What are the ingredients in JAVYGTOR tablets?
Active Ingredient: sapropterin dihydrochloride.
Inactive Ingredients: ascorbic acid, colloidal silicon dioxide, crospovidone, low substituted hydroxypropyl cellulose, mannitol, riboflavin and sodium stearyl fumarate.For more information, call 1-888-375-3784.
This Patient Information has been approved by the U.S. Food and Drug Administration.
To reorder additional Patient Information Sheets contact Dr. Reddy’s Customer Service at 1-866-733-3952.
Rx Only
Distributor:
Dr. Reddy’s Laboratories Inc.,
Princeton, NJ 08540
Made in India
Revised: 10/2024
-
SPL UNCLASSIFIED SECTION
Instructions for Use
JAVYGTOR™ (Jah' vig tor)
(sapropterin dihydrochloride)TabletsRead this Instructions for Use before you start taking JAVYGTOR and each time you refill your prescription. There may be new information. This information does not take the place of talking with your healthcare provider about your treatment. Talk to your doctor if you have any questions about the right dose of JAVYGTOR to take or how to mix it.
Important information:
JAVYGTOR comes as a tablet.
Take JAVYGTOR exactly as your doctor tells you. Your doctor should tell you how much JAVYGTOR to take and when to take it.
Your doctor may change your dose of JAVYGTOR depending on how you respond to treatment, or based on your baby’s weight.
Take JAVYGTOR 1 time each day with a meal. It is best to take JAVYGTOR at the same time each day.
Instructions for taking JAVYGTOR tablets:
JAVYGTOR tablets can be swallowed whole or dissolved in water or apple juice. You may also crush the tablets and mix in a small amount of soft food, such as apple sauce or pudding.
To dissolve JAVYGTOR tablets:
Mix JAVYGTOR tablets in 4 ounces to 8 ounces (½ cup to 1 cup) of water or apple juice. It may take a few minutes for the tablets to dissolve. To make the tablets dissolve faster, you can stir or crush them.
The tablets may not dissolve completely. You may see small pieces floating on top of the water or apple juice. This is normal and safe for you to swallow.
Drink within 15 minutes.
After drinking your medicine, if you still see small pieces of the tablet, add more water or apple juice and drink to make sure that you take all of your medicine.
How should I store JAVYGTOR (sapropterin dihydrochloride) tablets?
Store JAVYGTOR tablets at room temperature between 20°C to 25°C (68°F to 77°F).
Keep JAVYGTOR tablets in the original bottle with the cap closed tightly.
Protect from moisture.
Keep JAVYGTOR and all medicines out of the reach of children.
This Instructions for Use has been approved by the U.S. Food and Drug Administration.
Rx Only
Distributor:
Dr. Reddy’s Laboratories Inc.,
Princeton, NJ 08540
Made in India
Revised: 10/2024
- PACKAGE LABEL PRINCIPAL DISPLAY PANEL SECTION
-
INGREDIENTS AND APPEARANCE
JAVYGTOR
sapropterin dihydrochloride tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 43598-096 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength SAPROPTERIN DIHYDROCHLORIDE (UNII: RG277LF5B3) (SAPROPTERIN - UNII:EGX657432I) SAPROPTERIN DIHYDROCHLORIDE 100 mg Inactive Ingredients Ingredient Name Strength ASCORBIC ACID (UNII: PQ6CK8PD0R) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) CROSPOVIDONE (UNII: 2S7830E561) HYDROXYPROPYL CELLULOSE, LOW SUBSTITUTED (UNII: 2165RE0K14) MANNITOL (UNII: 3OWL53L36A) RIBOFLAVIN (UNII: TLM2976OFR) SODIUM STEARYL FUMARATE (UNII: 7CV7WJK4UI) Product Characteristics Color WHITE (off white to light yellow) Score no score Shape ROUND Size 9mm Flavor Imprint Code l Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 43598-096-30 30 in 1 BOTTLE; Type 0: Not a Combination Product 10/03/2022 2 NDC: 43598-096-04 120 in 1 BOTTLE; Type 0: Not a Combination Product 10/03/2022 3 NDC: 43598-096-05 500 in 1 BOTTLE; Type 0: Not a Combination Product 10/03/2022 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA207685 10/03/2022 Labeler - Dr. Reddys Laboratories Inc (802315887) Establishment Name Address ID/FEI Business Operations Dr. Reddys Laboratories Limited (SEZ UNIT) 860037244 analysis(43598-096) , manufacture(43598-096)
Trademark Results [JAVYGTOR]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 JAVYGTOR 97711360 not registered Live/Pending |
Cycle Pharmaceuticals Ltd. 2022-12-09 |
 JAVYGTOR 97434525 not registered Live/Pending |
Cycle Pharmaceuticals Ltd 2022-05-30 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.