TERRELL- isoflurane liquid
Terrell by
Drug Labeling and Warnings
Terrell by is a Prescription medication manufactured, distributed, or labeled by Piramal Critical Care Inc, Piramal Pharma Limited. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
DESCRIPTION
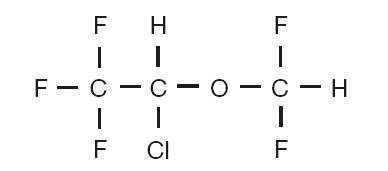
Isoflurane, USP, a nonflammable liquid administered by vaporizing, is a general inhalation anesthetic drug. It is 1-chloro-2,2,2-trifluoroethyl difluoromethyl ether, and its structural formula is:
Some physical constants are:
Molecular weight 184.5
Boiling point at 760 mm Hg 48.5°C (uncorr.)
Refractive index n20D 1.2990-1.3005
Specific gravity 25°/25°C 1.496
Vapor pressure in mm Hg** 20°C 238
25°C 295
30°C 367
35°C 450
**Equation for vapor pressure calculation:
log10Pvap = A + B where A = 8.056
T B = -1664.58
T = °C + 273.16 (Kelvin)
Partition coefficients at 37°C:
Water/gas 0.61
Blood/gas 1.43
Oil/gas 90.8
Partition coefficients at 25°C rubber and plastic
Conductive rubber/gas 62.0
Butyl rubber/gas 75.0
Polyvinyl chloride/gas 110.0
Polyethylene/gas ~2.0
Polyurethane/gas ~1.4
Polyolefin/gas ~1.1
Butyl acetate/gas ~2.5
Purity by gas chromatography >99.9%
Lower limit of flammability in oxygen None
or nitrous oxide at 9 joules/sec. and 23°C
Lower limit of flammability in oxygen Greater than useful
or nitrous oxide at 900 joules/sec. and 23°C concentration in anesthesia.
Isoflurane is a clear, colorless, stable liquid containing no additives or chemical stabilizers. Isoflurane has a mildly pungent, musty, ethereal odor. Samples stored in indirect sunlight in clear, colorless glass for five years, as well as samples directly exposed for 30 hours to a 2 amp, 115 volt, 60 cycle long wave U.V. light were unchanged in composition as determined by gas chromatography. Isoflurane in one normal sodium methoxide-methanol solution, a strong base, for over six months consumed essentially no alkali, indicative of strong base stability. Isoflurane does not decompose in the presence of soda lime (at normal operating temperatures), and does not attack aluminum, tin, brass, iron or copper.
-
CLINICAL PHARMACOLOGY
Isoflurane, USP is an inhalation anesthetic. The MAC (minimum alveolar concentration) in man is as follows:
Age 100% Oxygen 70% N 2026±4 1.28 0.56
44±7 1.15 0.50
64±5 1.05 0.37
Induction of and recovery from isoflurane anesthesia are rapid. Isoflurane has a mild pungency, which limits the rate of induction, although excessive salivation or tracheobronchial secretions do not appear to be stimulated. Pharyngeal and laryngeal reflexes are readily obtunded. The level of anesthesia may be changed rapidly with isoflurane. Isoflurane is a profound respiratory depressant. RESPIRATION MUST BE MONITORED CLOSELY AND SUPPORTED WHEN NECESSARY. As anesthetic dose is increased, tidal volume decreases and respiratory rate is unchanged. This depression is partially reversed by surgical stimulation, even at deeper levels of anesthesia. Isoflurane evokes a sigh response reminiscent of that seen with diethyl ether and enflurane, although the frequency is less than with enflurane.
Blood pressure decreases with induction of anesthesia but returns toward normal with surgical stimulation. Progressive increases in depth of anesthesia produce corresponding decreases in blood pressure. Nitrous oxide diminishes the inspiratory concentration of isoflurane required to reach a desired level of anesthesia and may reduce the arterial hypotension seen with isoflurane alone. Heart rhythm is remarkably stable. With controlled ventilation and normal PaCO 2, cardiac output is maintained despite increasing depth of anesthesia, primarily through an increase in heart rate, which compensates for a reduction in stroke volume. The hypercapnia, which attends spontaneous ventilation during isoflurane anesthesia further increases heart rate and raises cardiac output above awake levels. Isoflurane does not sensitize the myocardium to exogenously administered epinephrine in the dog. Limited data indicate that subcutaneous injection of 0.25 mg of epinephrine (50 mL of 1:200,000 solution) does not produce an increase in ventricular arrhythmias in patients anesthetized with isoflurane.
Muscle relaxation is often adequate for intra-abdominal operations at normal levels of anesthesia. Complete muscle paralysis can be attained with small doses of muscle relaxants. ALL COMMONLY USED MUSCLE RELAXANTS ARE MARKEDLY POTENTIATED WITH ISOFLURANE, THE EFFECT BEING MOST PROFOUND WITH THE NONDEPOLARIZING TYPE. Neostigmine reverses the effect of nondepolarizing muscle relaxants in the presence of isoflurane. All commonly used muscle relaxants are compatible with isoflurane.
Isoflurane can produce coronary vasodilation at the arteriolar level in selected animal models 1,2; the drug is probably also a coronary dilator in humans. Isoflurane, like some other coronary arteriolar dilators, has been shown to divert blood from collateral dependent myocardium to normally perfused areas in an animal model (“coronary steal”) 3.
Clinical studies to date evaluating myocardial ischemia, infarction and death as outcome parameters have not established that the coronary arteriolar dilation property of isoflurane is associated with coronary steal or myocardial ischemia in patients with coronary artery disease 4,5,6,7.
Pharmacokinetics
Isoflurane undergoes minimal biotransformation in man. In the postanesthesia period, only 0.17% of the isoflurane taken up can be recovered as urinary metabolites.
- INDICATIONS & USAGE
- CONTRAINDICATIONS
-
WARNINGS
Perioperative Hyperkalemia
Use of inhaled anesthetic agents has been associated with rare increases in serum potassium levels that have resulted in cardiac arrhythmias and death in pediatric patients during the postoperative period. Patients with latent as well as overt neuromuscular disease, particularly Duchenne muscular dystrophy, appear to be most vulnerable.
Concomitant use of succinylcholine has been associated with most, but not all, of these cases. These patients also experienced significant elevations in serum creatinine kinase levels and, in some cases, changes in urine consistent with myoglobinuria. Despite the similarity in presentation to malignant hyperthermia, none of these patients exhibited signs or symptoms of muscle rigidity or hypermetabolic state. Early and aggressive intervention to treat the hyperkalemia and resistant arrhythmias is recommended, as is subsequent evaluation for latent neuromuscular disease.
Malignant Hyperthermia
In susceptible individuals, isoflurane anesthesia may trigger a skeletal muscle hypermetabolic state leading to high oxygen demand and the clinical syndrome known as malignant hyperthermia. The syndrome includes nonspecific features such as muscle rigidity, tachycardia, tachypnea, cyanosis, arrhythmias, and unstable blood pressure. (It should also be noted that many of these nonspecific signs may appear with light anesthesia, acute hypoxia, etc.) An increase in overall metabolism may be reflected in an elevated temperature, (which may rise rapidly early or late in the case, but usually is not the first sign of augmented metabolism) and an increased usage of the CO 2 absorption system (hot canister). PaO 2 and pH may decrease, and hyperkalemia and a base deficit may appear. Treatment includes discontinuance of triggering agents (e.g., isoflurane), administration of intravenous dantrolene sodium, and application of supportive therapy.
Such therapy includes vigorous efforts to restore body temperature to normal, respiratory and circulatory support as indicated, and management of electrolyte-fluid-acid-base derangements. (Consult prescribing information for dantrolene sodium intravenous for additional information on patient management). Renal failure may appear later, and urine flow should be sustained if possible.
Since levels of anesthesia may be altered easily and rapidly, only vaporizers producing predictable concentrations should be used. Hypotension and respiratory depression increase as anesthesia is deepened. Increased blood loss comparable to that seen with halothane has been observed in patients undergoing abortions.
Isoflurane, USP markedly increases cerebral blood flow at deeper levels of anesthesia. There may be a transient rise in cerebral spinal fluid pressure, which is fully reversible with hyperventilation.
-
PRECAUTIONS
General Precautions
As with any potent general anesthetic, Isoflurane, USP should only be administered in an adequately equipped anesthetizing environment by those who are familiar with the pharmacology of the drug and qualified by training and experience to manage the anesthetized patient.
Regardless of the anesthetics employed, maintenance of normal hemodynamics is important to the avoidance of myocardial ischemia in patients with coronary artery disease 4,5,6,7.
Isoflurane, USP, like some other inhalational anesthetics, can react with desiccated carbon dioxide (CO 2) absorbents to produce carbon monoxide, which may result in elevated levels of carboxyhemoglobin in some patients. Case reports suggest that barium hydroxide lime and soda lime become desiccated when fresh gases are passed through the CO 2 absorber canister at high flow rates over many hours or days. When a clinician suspects that CO 2 absorbent may be desiccated, it should be replaced before the administration of Isoflurane, USP.
As with other halogenated anesthetic agents, Isoflurane, USP may cause sensitivity hepatitis in patients who have been sensitized by previous exposure to halogenated anesthetics (see CONTRAINDICATIONS).
Information for Patients
Isoflurane, as well as other general anesthetics, may cause a slight decrease in intellectual function for 2 or 3 days following anesthesia. As with other anesthetics, small changes in moods and symptoms may persist for up to 6 days after administration.
Laboratory Tests
Transient increases in BSP retention, blood glucose and serum creatinine with decrease in BUN, serum cholesterol and alkaline phosphatase have been observed.
Drug Interactions
Isoflurane potentiates the muscle relaxant effect of all muscle relaxants, most notably nondepolarizing muscle relaxants, and MAC (minimum alveolar concentration) is reduced by concomitant administration of N 2O. See CLINICAL PHARMACOLOGY.
Carcinogenesis & Mutagenesis & Impairment Of Fertility
Swiss ICR mice were given isoflurane to determine whether such exposure might induce neoplasia. Isoflurane was given at ½, 1/8 and 1/32 MAC for four in-utero exposures and for 24 exposures to the pups during the first nine weeks of life. The mice were killed at 15 months of age. The incidence of tumors in these mice was the same as in untreated control mice, which were given the same background gases, but not the anesthetic.
Pregnancy
Pregnancy Category C
Isoflurane has been shown to have a possible anesthetic-related fetotoxic effect in mice when given in doses 6 times the human dose. There are no adequate and well-controlled studies in pregnant women. Isoflurane should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
-
ADVERSE REACTIONS
Adverse reactions encountered in the administration of Isoflurane, USP are in general dose dependent extensions of pharmacophysiologic effects and include respiratory depression, hypotension and arrhythmias.
Shivering, nausea, vomiting and ileus have been observed in the postoperative period.
As with all other general anesthetics, transient elevations in white blood count have been observed even in the absence of surgical stress. See WARNINGS for information regarding malignant hyperthermia and elevated carboxyhemoglobin levels.
During marketing, there have been rare reports of mild, moderate and severe (some fatal) postoperative hepatic dysfunction and hepatitis.
Isoflurane USP has also been associated with perioperative hyperkalemia (see WARNINGS).
There have been rare post-marketing reports of hepatic failure and hepatic necrosis associated with the use of potent volatile anesthetic agents, including Isoflurane USP. Due to the spontaneous nature of these reports, the actual incidence and relationship of Isoflurane USP to these events cannot be established with certainty.
- OVERDOSAGE
-
DOSAGE & ADMINISTRATION
Premedication
Premedication should be selected according to the need of the individual patient, taking into account that secretions are weakly stimulated by Isoflurane, USP, and the heart rate tends to be increased. The use of anticholinergic drugs is a matter of choice.
Inspired Concentration
The concentration of isoflurane being delivered from a vaporizer during anesthesia should be known. This may be accomplished by using:
a.Vaporizers calibrated specifically for isoflurane;
b.Vaporizers from which delivered flows can be calculated, such as vaporizers delivering a saturated vapor, which is then diluted. The delivered concentration from such a vaporizer may be calculated using the formula:
% isoflurane = 100 PvFv
FT (PA PV)
Where:PA = Pressure of atmosphere
PV = Vapor pressure of isoflurane
FV = Flow of gas through vaporizer (mL/min)
FT = Total gas flow (mL/min)
Isoflurane contains no stabilizer. Nothing in the agent alters calibration or operation of these vaporizers.
Induction
Induction with isoflurane in oxygen or in combination with oxygen-nitrous oxide mixtures may produce coughing, breath holding, or laryngospasm. These difficulties may be avoided by the use of a hypnotic dose of an ultra-short-acting barbiturate. Inspired concentrations of 1.5 to 3.0% isoflurane usually produce surgical anesthesia in 7 to 10 minutes.
Maintenance
Surgical levels of anesthesia may be sustained with a 1.0 to 2.5% concentration when nitrous oxide is used concomitantly. An additional 0.5 to 1.0% may be required when isoflurane is given using oxygen alone. If added relaxation is required, supplemental doses of muscle relaxants may be used.
The level of blood pressure during maintenance is an inverse function of isoflurane concentration in the absence of other complicating problems. Excessive decreases may be due to depth of anesthesia and in such instances may be corrected by lightening anesthesia.
- HOW SUPPLIED
-
Safety and Handling
Occupational Caution
There is no specific work exposure limit established for Isoflurane, USP. However, the National Institute for Occupational Safety and Health Administration (NIOSH) recommends that no worker should be exposed at ceiling concentrations greater than 2 ppm of any halogenated anesthetic agent over a sampling period not to exceed one hour.
The predicted effects of acute overexposure by inhalation of Isoflurane, USP include headache, dizziness or (in extreme cases) unconsciousness. There are no documented adverse effects of chronic exposure to halogenated anesthetic vapors (Waste Anesthetic Gases or WAGs) in the workplace. Although results of some epidemiological studies suggest a link between exposure to halogenated anesthetics and increased health problems (particularly spontaneous abortion), the relationship is not conclusive. Since exposure to WAGs is one possible factor in the findings for these studies, operating room personnel, and pregnant women in particular, should minimize exposure. Precautions include adequate general ventilation in the operating room, the use of a well-designed and well-maintained scavenging system, work practices to minimize leaks and spills while the anesthetic agent is in use, and routine equipment maintenance to minimize leaks.
- Storage
- Manufactured By
-
REFERENCES
1. J.C. Sill, et al, Anesthesiology 66:273-279, 1987
2. R.F. Hickey, et al, Anesthesiology 68:21-30, 1988
3. C.W. Buffington, et al, Anesthesiology 66:280-292, 1987
4. S. Reiz, et al, Anesthesiology 59:91-97, 1983
5. S. Slogoff and A.S. Keats, Anesthesiology 70:179-188, 1989
6. K.J. Tuman, et al, Anesthesiology 70:189-198, 1989
7. D.T. Mangano, Editorial Views, Anesthesiology 70:175-178, 1989
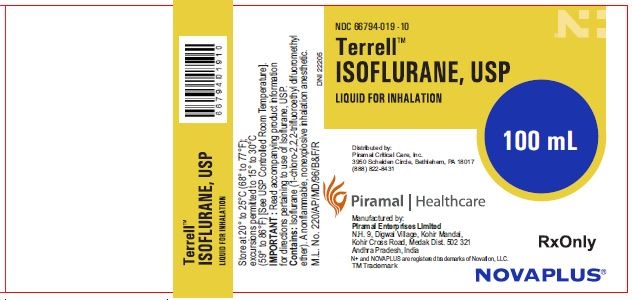
- Label 100 ml
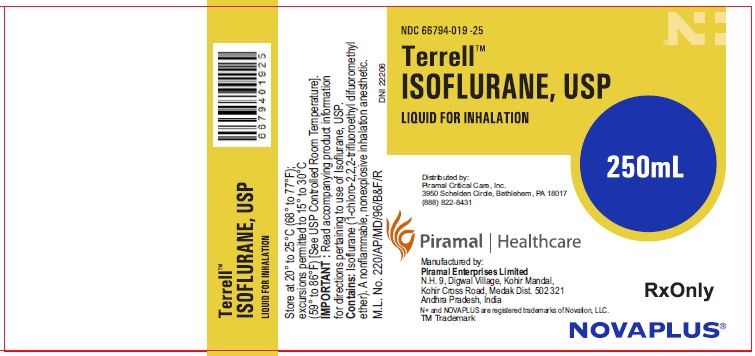
- Label 250 ml
-
INGREDIENTS AND APPEARANCE
TERRELL
isoflurane liquidProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 66794-019 Route of Administration RESPIRATORY (INHALATION) Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ISOFLURANE (UNII: CYS9AKD70P) (ISOFLURANE - UNII:CYS9AKD70P) ISOFLURANE 1 mL in 1 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 66794-019-10 100 mL in 1 BOTTLE, GLASS; Type 0: Not a Combination Product 03/21/2012 2 NDC: 66794-019-25 250 mL in 1 BOTTLE, GLASS; Type 0: Not a Combination Product 03/21/2012 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA074502 03/21/2012 Labeler - Piramal Critical Care Inc (805600439) Establishment Name Address ID/FEI Business Operations Piramal Enterprises Limited 919067108 analysis(66794-019) , api manufacture(66794-019) , manufacture(66794-019) , pack(66794-019)
Trademark Results [Terrell]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 TERRELL 86836954 5162272 Live/Registered |
Piramal Critical Care, Inc. 2015-12-02 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.