Nitisinone by Eton Pharmaceuticals, Inc. / Zenara Pharma Private Limited / Sionc Pharmaceuticals Pvt. Ltd / Teena Biolabs Private Limited / Energon Labs Private Limited / Choksi Laboratorties Limited NITISINONE capsule
Nitisinone by
Drug Labeling and Warnings
Nitisinone by is a Prescription medication manufactured, distributed, or labeled by Eton Pharmaceuticals, Inc., Zenara Pharma Private Limited , Sionc Pharmaceuticals Pvt. Ltd, Teena Biolabs Private Limited, Energon Labs Private Limited, Choksi Laboratorties Limited. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
HIGHLIGHTS OF PRESCRIBING INFORMATION These highlights do not include all the information needed to use NITISINONE CAPSULES safely and effectively. See full prescribing information for NITISINONE CAPSULES. NITISINONE Capsules, for oral use Initial U.S. Approval: 2002
INDICATIONS AND USAGE
DOSAGE AND ADMINISTRATION
Recommended Dosage (2.1): (2)
- The recommended starting dosage is 0.5 mg/kg orally twice
daily. (2)
- In patients 5 years of age and older who have undetectable
serum and urine succinylacetone concentrations after a (2)
minimum of 4 weeks on a stable dosage of nitisinone, the total (2)
daily dose may be given once daily. (2)
- Titrate the dosage based on biochemical and/or clinical
response, as described in the full prescribing information. (2)
- The maximum total daily dosage is 2 mg/kg orally.
(2)
Administration Instructions (2.2): (2)
- Maintain dietary restriction of tyrosine and phenylalanine
- Take Nitisinone Capsules at least one hour before, or two
hours after a meal (2)
- For patients who have difficulties swallowing capsules, the
capsules may be opened and the contents suspended in a small (2)
amount of water, formula, or apple sauce immediately before (2)
use. (2)
DOSAGE FORMS AND STRENGTHS
- Capsules: 2 mg, 5 mg, 10 mg, 20 mg.
CONTRAINDICATIONS
None (4)
WARNINGS AND PRECAUTIONS
Elevated Plasma Tyrosine Levels, Ocular Symptoms, (5)
Developmental Delay and Hyperkeratotic Plaques: Inadequate (5)
restriction of tyrosine and phenylalanine intake can lead to (5)
elevations in plasma tyrosine, which at levels above 500 (5)
micromol/L can result in symptoms, intellectual disability and (5)
developmental delay or painful hyperkeratotic plaques on the soles (5)
and palms; do not adjust Nitisinone Capsules dosage in order to (5)
lower the plasma tyrosine concentration. Obtain slit-lamp (5)
examination prior to treatment, regularly during treatment; (5)
(5)
- Reexamine patients if symptoms develop or tyrosine levels
are > 500 micromol/L. Assess plasma tyrosine levels in (5)
patients with an abrupt change in neurologic status. (5.1) (5)
- Leukopenia and Severe Thrombocytopenia: Monitor platelet
and white blood cell counts. (5.2) (5)
ADVERSE REACTIONS
Most common adverse reactions (>1%) are elevated tyrosine levels, (6)
thrombocytopenia, leukopenia, conjunctivitis, corneal opacity, (6)
keratitis, photophobia, eye pain, blepharitis, cataracts, (6)
granulocytopenia, epistaxis, pruritus, exfoliative dermatitis, dry (6)
skin, maculopapular rash and alopecia. (6.1) (6)
(6)
To report SUSPECTED ADVERSE REACTIONS, contact (6)
Eton Pharmaceuticals, Inc., at 1-855-224-0233 or FDA at (6)
1-800-FDA-1088 or www.fda.gov/medwatch. (6)
DRUG INTERACTIONS
- CYP2C9 Substrates: Increased systemic exposure of these
co-administered drugs; reduce the dosage. Additional (7)
dosage adjustments may be needed to maintain (7)
therapeutic drug concentrations for narrow therapeutic index (7)
drugs. (7)
- OAT1/OAT3 Substrates: Increased systemic exposure of these
co-administered drugs; monitor for potential adverse reactions. (7)
(7)
(7)
See 17 for PATIENT COUNSELING INFORMATION and (7)
FDA approved patient labeling. (7)
(7)
Revised 02/2024 (7)
Revised: 2/2024
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
HIGHLIGHTS OF PRESCRIBING INFORMATION These highlights do not include all the information needed to use NITISINONE CAPSULES safely and effectively. See full prescribing information for NITISINONE CAPSULES. NITISINONE Capsules, for oral use Initial U.S. Approval: 2002
1. INDICATIONS AND USAGE2. DOSAGE AND ADMINISTRATION
2.1 Dosage
2.2 Administration Instructions
3. DOSAGE FORMS AND STRENGTHS
4. CONTRAINDICATION
5. WARNINGS AND PRECAUTIONS
5.1. Elevated Plasma Tyrosine Levels, Ocular Symptoms, Developmental Delay and Hyperkeratotic Plaques
5.2. Leukopenia and Severe Thrombocytopenia
6. ADVERSE REACTIONS
6.1 Clinical Trials Experience
7. DRUG INTERACTIONS
8. USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
10. OVERDOSAGE
11. DESCRIPTION
12. CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13. NONCLINICAL TOXICOLOGY
13.1. Carcinogenesis, Mutagenesis, Impairment of Fertility
14. CLINICAL STUDIES
16. HOW SUPPLIED/STORAGE AND HANDLING
- * Sections or subsections omitted from the full prescribing information are not listed.
- HIGHLIGHTS OF PRESCRIBING INFORMATION These highlights do not include all the information needed to use NITISINONE CAPSULES safely and effectively. See full prescribing information for NITISINONE CAPSULES. NITISINONE Capsules, for oral use Initial U.S. Approval: 2002 1. INDICATIONS AND USAGE
-
2. DOSAGE AND ADMINISTRATION
2.1 Dosage
Starting Dosage
The recommended starting dosage of Nitisinone Capsules is 0.5 mg/kg administered orally
twice daily.
Maintenance Regimen
In patients 5 years of age and older who have undetectable serum and urine succinylacetone
concentrations after a minimum of 4 weeks on a stable dosage of nitisinone, the total daily
dose of Nitisinone Capsules may be given once daily (e.g., 1 to 2 mg/kg once daily) [see
Clinical Pharmacology (12.2)].
Dosage Titration
Titrate the dosage in each individual patient based on biochemical and/or clinical response.
- Monitor plasma and/or urine succinylacetone concentrations, liver function
parameters and alpha-fetoprotein levels.
- If succinylacetone is still detectable in blood or urine 4 weeks after the start of
nitisinone treatment, increase the nitisinone dosage to 0.75 mg/kg twice daily. A
maximum total daily dosage of 2 mg/kg may be needed based on the evaluation of
all biochemical parameters.
- If the biochemical response is satisfactory (undetectable blood and/or urine
succinylacetone), the dosage should be adjusted only according to body weight gain
and not according to plasma tyrosine levels.
- During initiation of therapy, when switching from twice daily to once daily dosing,
or if there is a deterioration in the patient’s condition, it may be necessary to follow
all available biochemical parameters more closely (i.e. plasma and/or urine
succinylacetone, urine 5- aminolevulinate (ALA) and erythrocyte porphobilinogen
(PBG)-synthase activity).
- Maintain plasma tyrosine levels below 500 micromol/L by dietary restriction of
tyrosine and phenylalanine intake [see Warnings and Precautions (5.1)]. In patients
who develop plasma tyrosine levels above 500 micromol/L, assess dietary tyrosine
and phenylalanine intake. Do not adjust the Nitisinone Capsules dosage in order to
lower the plasma tyrosine concentration.
2.2 Administration Instructions
Administration of Nitisinone Capsules
- Maintain dietary restriction of tyrosine and phenylalanine when taking Nitisinone
Capsules.
- Capsules: Take at least one hour before, or two hours after a meal [see Clinical
Pharmacology (12.3)]. For patients who have difficulty swallowing the capsules, the
capsules may be opened and the contents suspended in a small amount of water,
formula or apple sauce immediately before use.
-
3. DOSAGE FORMS AND STRENGTHS
Capsules:
- 2 mg: Size “3” hard gelatin capsules with white opaque cap imprinted with “NIT2” in
black, and white opaque body imprinted ‘ZN11’ in black, filled with white to off-white
powder.
- 5 mg: Size “3” hard gelatin capsules with white opaque cap imprinted with “NIT5” in
black, and white opaque body imprinted ‘ZN12’ in black, filled with white to off-white
powder.
- 10 mg: Size “3” hard gelatin capsules with white opaque cap imprinted with “NIT10”
in black, and white opaque body imprinted ‘ZN13’ in black, filled with white to
off-white powder.
- 20 mg: Size “3” hard gelatin capsules with white opaque cap imprinted with “NIT20”
in black, and white opaque body imprinted ‘ZN14’ in black, filled with white to
off-white powder.
- 4. CONTRAINDICATION
-
5. WARNINGS AND PRECAUTIONS
5.1. Elevated Plasma Tyrosine Levels, Ocular Symptoms, Developmental Delay and Hyperkeratotic Plaques
Nitisinone is an inhibitor of 4-hydroxyphenyl-pyruvate dioxygenase, an enzyme in the
tyrosine metabolic pathway [see Clinical Pharmacology (12.1)]. Therefore, treatment with
nitisinone may cause an increase in plasma tyrosine levels in patients with HT-1. Maintain
concomitant reduction in dietary tyrosine and phenylalanine while on nitisinone treatment.
Do not adjust nitisinone dosage in order to lower the plasma tyrosine concentration. Maintain
plasma tyrosine levels below 500 micromol/L. Inadequate restriction of tyrosine and
phenylalanine intake can lead to elevations in plasma tyrosine levels and levels greater than
500 micromol/L may lead to the following:
- Ocular signs and symptoms including corneal ulcers, corneal opacities, keratitis,
conjunctivitis, eye pain, and photophobia have been reported in patients treated with
nitisinone [see Adverse Reactions (6.1)]. In a clinical study in a non HT-1 population
without dietary restriction and reported tyrosine levels >500 micromol/l both
symptomatic and asymptomatic keratopathies have been observed. Therefore, perform
a baseline ophthalmologic examination including slit-lamp examination prior to
initiating nitisinone treatment and regularly thereafter. Patients who develop
photophobia, eye pain, or signs of inflammation such as redness, swelling, or burning
of the eyes or tyrosine levels are > 500 micromol/L during treatment with Nitisinone
Capsules should undergo slit- lamp reexamination and immediate measurement of the
plasma tyrosine concentration.
- Variable degrees of intellectual disability and developmental delay. In patients treated
with nitisinone who exhibit an abrupt change in neurologic status, perform a clinical
laboratory assessment including plasma tyrosine levels.
- Painful hyperkeratotic plaques on the soles and palms
In patients with HT-1 treated with dietary restrictions and nitisinone who develop elevated
plasma tyrosine levels, assess dietary tyrosine and phenylalanine intake.
5.2. Leukopenia and Severe Thrombocytopenia
In clinical trials, patients treated with nitisinone and dietary restriction developed transient
leukopenia (3%), thrombocytopenia (3%), or both (1.5%) [see Adverse Reactions (6.1)]. No
patients developed infections or bleeding as a result of the episodes of leukopenia and
thrombocytopenia. Monitor platelet and white blood cell counts during nitisinone therapy.
-
6. ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates
observed in the clinical trials of a drug cannot be directly compared to rates in the clinical
trials of another drug and may not reflect the rates observed in clinical practice.
Nitisinone was studied in one open-label, uncontrolled study of 207 patients with HT-1, ages
0 to 22 years at enrollment (median age 9 months), who were diagnosed with HT-1 by the
presence of succinylacetone in the urine or plasma. The starting dose of nitisinone was 0.3 to
0.5 mg/kg twice daily, and the dose was increased in some patients to 1 mg/kg twice daily
based on weight, biochemical, and enzyme markers. The recommended starting dosage of
nitisinone is 0.5 mg/kg twice daily [see Dosage and Administration (2.1)]. Median duration
of treatment was 22 months (range 0.1 to 80 months).
The most serious adverse reactions reported during nitisinone treatment were
thrombocytopenia, leukopenia, porphyria, and ocular/visual complaints associated with
elevated tyrosine levels [see Warnings and Precautions (5.1, 5.2)]. Fourteen patients
experienced ocular/visual events. The duration of the symptoms varied from 5 daysto 2 years.
Six patients had thrombocytopenia, three of which had platelet counts 30,000/microL or
lower. In 4 patients with thrombocytopenia, platelet counts gradually returned to normal
(duration up to 47 days) without change in nitisinone dose. No patients developed infections
or bleeding as a result of the episodes of leukopenia and thrombocytopenia.
Patients with HT- 1 are at increased risk of developing porphyric crises, hepatic neoplasms,
and liver failure requiring liver transplantation. These complications of HT- 1 were observed
in patients treated with nitisinone for a median of 22 months during the clinical trial (liver
transplantation 13%, liver failure 7%, malignant hepatic neoplasms 5%, benign hepatic
neoplasms 3%, porphyria 1%).
The most common adverse reactions reported in the clinical trial are summarized in Table 1.
Table 1: Most Common Adverse Reactions in Patients with HT-1 Treated with Nitisinone*
Elevated tyrosine levels >10% Leukopenia 3% Thrombocytopenia 3% Conjunctivitis 2% Corneal opacity 2% Keratitis 2% Photophobia 2% Eye pain 1% Blepharitis 1% Cataracts 1% Granulocytopenia 1% Epistaxis 1% Pruritus 1% Exfoliate dermatitis 1% Dry skin 1% Maculopapular rash 1% Alopecia 1% *reported in at least 1% of patients
Adverse reactions reported in less than 1% of the patients, included death, seizure, brain
tumor, encephalopathy, hyperkinesia, cyanosis, abdominal pain, diarrhea, enanthema,
gastrointestinal hemorrhage, melena, elevated hepatic enzymes, liver enlargement,
hypoglycemia, septicemia, and bronchitis.
-
7. DRUG INTERACTIONS
Nitisinone is a moderate CYP2C9 inhibitor, a weak CYP2E1 inducer and an inhibitor of
OAT1/OAT3. Table 2 includes drugs with clinically important drug interactions when
administered concomitantly with nitisinone and instructions for preventing or managing
them.
Table 2: Clinically Relevant Interactions Affecting Co-Administered Drugs
Sensitive CYP2C9 Substrates (e.g., celecoxib, tolbutamide) or CYP2C9 Substrates with a Narrow Therapeutic Index (e.g., phenytoin, warfarin)
Clinical Impact Increased exposure of the co-administered drugs metabolized by CYP2C9 [see Clinical Pharmacology (12.3)]. Intervention Reduce the dosage of the co-administered drugs metabolized by CYP2C9 drug by half. Additional dosage adjustments may be needed to maintain therapeutic drug concentrations for narrow therapeutic index drugs. See prescribing information for those drugs. OAT1/OAT3 Substrates (e.g., adefovir, ganciclovir, methotrexate)
Clinical Impact Increased exposure of the interacting drug [see Clinical Pharmacology (12.3)]. Intervention Monitor for potential adverse reactions related to the co-administered drug. -
8. USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Limited available data with nitisinone use in pregnant women are not sufficient to determine
a drug-associated risk of adverse developmental outcomes. Animal reproduction studies have
been conducted for nitisinone. In these studies, nitisinone was administered to mice and
rabbits during organogenesis with oral doses of nitisinone up to 20 and 8 times respectively,
the recommended initial dose of 1 mg/kg/day. In mice, nitisinone caused incomplete skeletal
ossification of fetal bones and decreased pup survival at doses 0.4 times the recommended
initial dose and increased gestational length at doses 4 times the recommended initial dose.
In rabbits, nitisinone caused maternal toxicity and incomplete skeletal ossification of fetal
bones at doses 1.6 times the recommended initial dose [see Data].
The background risk of major birth defects and miscarriage for the indicated population are
unknown. In the U.S. general population, the estimated background risk of major birth defects
and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Data
Animal Data
Reproduction studies have been performed in mice at oral doses of about 0.4, 4 and 20 times
the recommended initial dose (1 mg/kg/day) and in rabbits at oral doses of about 1.6, 4 and 8
times the recommended initial dose based on the body surface area. In mice, nitisinone has
been shown to cause incomplete skeletal ossification of fetal bones at 0.4, 4 and 20 times the
recommended initial dose, increased gestational length at 4 and 20 times the recommended
initial dose, and decreased pup survival at 0.4 times the recommended initial dose based on
the body surface area. In rabbits, nitisinone caused incomplete skeletal ossification of fetal
bones at 1.6, 4 and 8 times the recommended initial dose based on the body surface area.
8.2 Lactation
Risk Summary
There are no data on the presence of nitisinone in human milk, the effects on the breastfed
infant, or the effects on milk production. Data suggest that nitisinone is present in rat milk
due to findings of ocular toxicity and lower body weight seen in drug naive nursing rat pups.
The development and health benefits of breastfeeding should be considered along with the
mother’s clinical need for nitisinone and any potential adverse effects on the breastfed infant
from nitisinone or from the underlying maternal condition.
8.4 Pediatric Use
The safety and effectiveness of nitisinone have been established in pediatric patients for the
treatment of HT-1 in combination with dietary restriction of tyrosine and phenylalanine. Use
of nitisinone in pediatric patients is supported by evidence from one open-label, uncontrolled
clinical study conducted in 207 patients with HT-1 ages 0 to 22 years (median age 9 months)
[ see Clinical Studies (14)].
8.5 Geriatric Use
Clinical studies of nitisinone did not include any subjects aged 65 and over. No
pharmacokinetic studies of nitisinone have been performed in geriatric patients. In general,
dose selection for an elderly patient should be cautious reflecting the greater frequency of
decreased hepatic, renal, or cardiac function, and concomitant disease or other drug therapy
in this patient population.
-
10. OVERDOSAGE
Accidental ingestion of nitisinone by individuals eating normal diets not restricted in tyrosine
and phenylalanine will result in elevated tyrosine levels. In healthy subjects given a single 1
mg/kg dose of nitisinone, the plasma tyrosine level reached a maximum of 1200 micromol/L
at 48 to 120 hours after dosing. After a washout period of 14 days, the mean value of plasma
tyrosine was still 808 micromol/L. Fasted follow-up samples obtained from volunteers
several weeks later showed tyrosine values back to normal. There were no reports of changes
in vital signs or laboratory data of any clinical significance. One patient reported sensitivity
to sunlight. Hyper- tyrosinemia has been reported with nitisinone treatment [ see Warnings
and Precautions (5.1)].
-
11. DESCRIPTION
Nitisinone capsules contain nitisinone, which is a 4-hydroxyphenyl-pyruvate dioxygenase
inhibitor indicated as an adjunct to dietary restriction of tyrosine and phenylalanine in the
treatment of hereditary tyrosinemia type 1 (HT-1).
Nitisinone occurs as white to yellowish-white, crystalline powder. It is Freely soluble in
Acetone, Ethyl acetate and Methylene chloride. Sparingly soluble in absolute alcohol and
practically insoluble in water Chemically, nitisinone is 2-(2-nitro-4-trifluoromethylbenzoyl)-
1,3-cyclohexanedione, and the structural formula is:
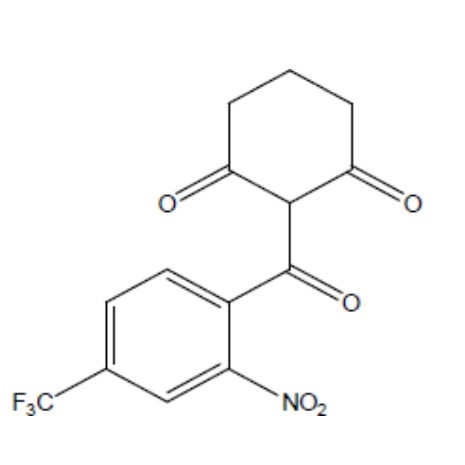
Figure 1. The molecular formula is C14H10F3NO5 with a relative mass of 329.23
Capsules: Hard, white-opaque capsule, 2 mg, 5 mg, 10 mg, and 20 mg strengths of nitisinone,
intended for oral administration. Each capsule contains 2 mg, 5 mg, 10 mg, or 20 mg
nitisinone, anhydrous lactose and stearic acid. The capsule shell contains gelatin and titanium
dioxide, and the imprinting ink contains black iron oxide, propylene glycol, potassium
hydroxide, shellac, and strong ammonia solution.
-
12. CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Nitisinone is a competitive inhibitor of 4-hydroxyphenyl-pyruvate dioxygenase, an enzyme
upstream of fumarylacetoacetate hydrolase (FAH) in the tyrosine catabolic pathway. By
inhibiting the normal catabolism of tyrosine in patients with HT-1, nitisinone prevents the
accumulation of the catabolic intermediates maleylacetoacetate and fumarylacetoacetate. In
patients with HT-1, these catabolic intermediates are converted to the toxic metabolites
succinylacetone and succinylacetoacetate, which are responsible for the observed liver and
kidney toxicity. Succinylacetone can also inhibit the porphyrin synthesis pathway leading to
the accumulation of 5- aminolevulinate, a neurotoxin responsible for the porphyric crises
characteristic of HT-1.
12.2 Pharmacodynamics
In a clinical study, patients with HT-1 were diagnosed by the presence of succinylacetone in
urine or plasma and treated with nitisinone [ see Clinical Studies (14)]. In all 186 patients
whose urine succinylacetone was measured, the urinary succinylacetone concentration
decreased to less than 1 mmol/mol creatinine, the lower limit of quantitation. The median
time to normalization of urine succinylacetone was 0.3 months. The probability of recurrence
of abnormal values of urine succinylacetone was 1% at a nitisinone concentration of 37
micromol/L (95% confidence interval: 23, 51 micromol/L). In 87% (150/172) of patients
whose plasma succinylacetone was measured, the plasma succinylacetone concentration
decreased to less than 0.1 micromol/L, the lower limit of quantitation. The median time to
normalization of plasma succinylacetone was 3.9 months.
In another study, comparing two dosing regimens, succinylacetone was measured in urine
and/or blood in 16 patients with HT-1 aged 5 years to 24 years. All study patients were on a
stable nitisinone daily dosage (0.4 mg/kg/day to 1 mg/kg/day) during both study dosing
regimens. After at least 4 weeks of twice daily dosing with nitisinone, both the urine and/or
blood succinylacetone concentrations were below the limit of quantitation for the assay.
Patients were then switched to once daily dosing with the same total daily dosage of nitisinone
and blood and/or urine succinylacetone concentrations remained undetectable when
measured following at least 4 weeks of treatment with once daily dosing.
Nitisinone inhibits catabolism of the amino acid tyrosine and can result in elevated plasma
levels of tyrosine. Therefore, treatment with nitisinone requires restriction of the dietary
intake of tyrosine and phenylalanine to prevent the toxicity associated with elevated plasma
levels of tyrosine [ see Warnings and Precautions (5.1)].
12.3 Pharmacokinetics
The single-dose pharmacokinetics of nitisinone have been studied for Nitisinone Capsules in
healthy adult subjects and the multiple-dose pharmacokinetics have been studied for
Nitisinone Capsules in healthy subjects.
Absorption
The pharmacokinetic characteristics following single oral administration of nitisinone 30 mg
under fasting conditions are shown in Table 3. The multiple-dose characteristics of nitisinone
80 mg once daily are shown in Table 4. Steady-state (SS) was reached within 14 days dosing
in all subjects.
Table 3: Nitisinone Arithmetic Mean (CV%) Pharmacokinetic Parameters in Healthy Subjects
Following a Single Oral 30 mg Dose of Nitisinone Under Fasting Conditions
Treatment Cmax (micromol/L) [range] tmax* (h) [range] AUC 0-72h (micromol·h/L) [range] Nitisinone Capsule (n=12) 10.5 (26) 3.5
[0.8-8.0]
406 (13) *presented as median [range]
Table 4: Nitisinone Arithmetic Mean (CV%) Pharmacokinetic Parameters in Healthy Subjects Following
Repeated Once Daily Administration of 80 mg Nitisinone Under Fasting Conditions.
Treatment Cmax,ss (micromol/L)
[CV%]
Cmin,ss (micromol/L)
[range]
tmax,ss* (h)
[range]
AUC 0-24h, ss
(micromol·h/L)
[range]
Nitisinone Capsule
(n=18)
120 (23) 73 (24) 4.0
[0.0 to 16.0]
2204 (18) *presented as median [range]
Food Effect: No food effect study was conducted with Nitisinone capsules.
Distribution
In vitro binding of nitisinone to human plasma proteins is greater than 95% at 50 micromolar
concentration.
Elimination
The mean terminal plasma half-life of single dose nitisinone in healthy male subjects is 54
hours. The mean (CV%) apparent plasma clearance in 18 healthy adults following multiple
once daily doses of Nitisinone 80 mg is 113 (16) mL/hr.
Metabolism:In vitro studies have shown that nitisinone is relatively stable in human liver microsomes
with minor metabolism possibly mediated by CYP3A4 enzyme.
Excretion: Renal elimination of nitisinone is of minor importance, since the mean of the fraction of
dose excreted as unchanged nitisinone in the urine (fe(%)) was 3.0% (n=3) following
multiple oral doses of 80 mg daily in healthy subjects. The estimated mean (CV%) renal
clearance of nitisinone was 0.003 L/h (25%).
Drug Interaction Studies
Nitisinone does not inhibit CYP2D6. Nitisinone is a moderate inhibitor of CYP2C9, and a
weak inducer of CYP2E1 (Table 5). Nitisinone is an inhibitor of OAT1/3 (Table 5).
Table 5: Percent Change in AUC 0-∞ and Cmax for Co-administered Drugs in the
Presence of Nitisinone in 18 Healthy Subjects
Co-administered Drug (a) Dose of Co-administered Drug (Route of Administration) Effect of Nitisinone on the Pharmacokinetics of Co-administered Drug (b)
AUC 0-∞ Cmax CYP2C9 Substrate Tolbutamide c 500 mg (oral) 131% ↑ 16% ↑ CYP2E1 Substrate Chlorzoxazone 250 mg (oral) 27% ↓ 18% ↓ OAT1/3 Substrate Furosemide 20 mg (intravenous) 72% ↑ 12% ↑ ↑ = Increased; ↓ = Decreased
(a) The interacting drug was administered alone on Day 1 and together with nitisinone on Day 17.
(b) Multiple doses of 80 mg nitisinone were administered daily alone from Day 3 to Day 16.
(c) 16 subjects in Period 2 received nitisinone and tolbutamide while 18 subjects in Period 1 received
nitisinone alone.
In Vitro Studies Where Drug Interaction Potential Was Not Further Evaluated Clinically
In vitro studies showed that nitisinone does not inhibit CYP1A2, 2C19, or 3A4. Nitisinone
does not induce CYP1A2, 2B6 or 3A4/5. Nitisinone does not inhibit P-gp, BCRP, OATP1B1,
OATP1B3 and OCT2-mediated transports at therapeutically relevant concentrations.
-
13. NONCLINICAL TOXICOLOGY
13.1. Carcinogenesis, Mutagenesis, Impairment of Fertility
The carcinogenic potential of nitisinone was assessed in a 26-week oral (gavage)
carcinogenicity study in Tg.rasH2 mice. There were no drug-related neoplastic findings in
male or female Tg.rasH2 mice at doses up to 100 mg/kg/ day nitisinone (approximately 8.1
times the recommended initial dose of 1 mg/kg/day on a body surface area basis).
Nitisinone was not genotoxic in the Ames test and the in vivo mouse liver unscheduled DNA
synthesis (UDS) test. Nitisinone was mutagenic in the mouse lymphoma cell
(L5178Y/TK+/- ) forward mutation test and in vivo mouse bone marrow micronucleus test.
In a single dose-group study in rats given 100 mg/kg (16.2 times the recommended initial
dose of 1 mg/kg/day on a body surface area basis), reduced litter size, decreased pup weight
at birth, and decreased survival of pups after birth was demonstrated.
-
14. CLINICAL STUDIES
The efficacy and safety of nitisinone in patients with HT-1 was evaluated in one open-label,
uncontrolled study of 207 patients with HT-1, ages 0 to 22 years at enrollment (median age
9 months). Patients were diagnosed with HT-1 by the presence of succinylacetone in the urine
or plasma. All patients were treated with nitisinone at a starting dose of 0.3 to 0.5 mg/kg twice
daily, and the dose was increased in some patients to 1 mg/kg twice daily based on weight,
liver and kidney function tests, platelet count, serum amino acids, urinary phenolic acid,
plasma and urine succinylacetone, erythrocyte PBG-synthase, and urine 5-ALA. The median
duration of treatment was 22 months (range less than 1 month to 80 months). Efficacy was
assessed by comparison of survival and incidence of liver transplant to historical controls.
For patients presenting with HT-1 younger than 2 months of age who were treated with
dietary restriction and nitisinone, 2- and 4-year survival probabilities were 88% and 88%,
respectively. Data from historical controls showed that patients presenting with HT-1 at
younger than 2 months of age and treated with dietary restriction alone had 2- and 4-year
survival probabilities of 29% and 29%, respectively. For patients presenting with HT-1
between 2 months and 6 months of age who were treated with dietary restriction and
nitisinone, 2- and 4-year survival probabilities were 94% and 94%, respectively. Data for
historical controls showed that patients presenting with HT-1 between 2 months and 6 months
of age treated with dietary restriction alone had 2- and 4-year survival probabilities of 74%
and 60%, respectively.
The effects of nitisinone on urine and plasma succinylacetone, porphyrin metabolism, and
urinary alpha-1-microglobulin were also assessed in this clinical study.
Porphyria-like crisis were reported in 3 patients (0.3% of cases per year) during the clinical
study. This compares to an incidence of 5 to 20% of cases per year expected as part of the
natural history of the disorder. An assessment of porphyria-like crises was performed because
these events are commonly reported in patients with HT-1 who are not treated with nitisinone.
Urinary alpha-1-microglobulin, a proposed marker of proximal tubular dysfunction, was
measured in 100 patients at baseline. The overall median pretreatment level was 4.3 grams/mol
creatinine. After one year of treatment in a subgroup of patients (N=100), overall median alpha-
1-microglobulin decreased by 1.5 grams/mol creatinine. In patients 24 months of age and
younger in whom multiple values were available (N=65), median alpha-1-microglobulin levels
decreased from 5.0 to 3.0 grams/mol creatinine (reference value for age less than or equal to
12 grams/mol creatinine). In patients older than 24 months in whom multiple values
were available (N=35), median alpha-1-microglobulin levels decreased from 2.8 to 2.0 grams/mol
creatinine (reference for age less than or equal to 6 grams/mol creatinine).
The long-term effect of nitisinone on hepatic function was not assessed.
-
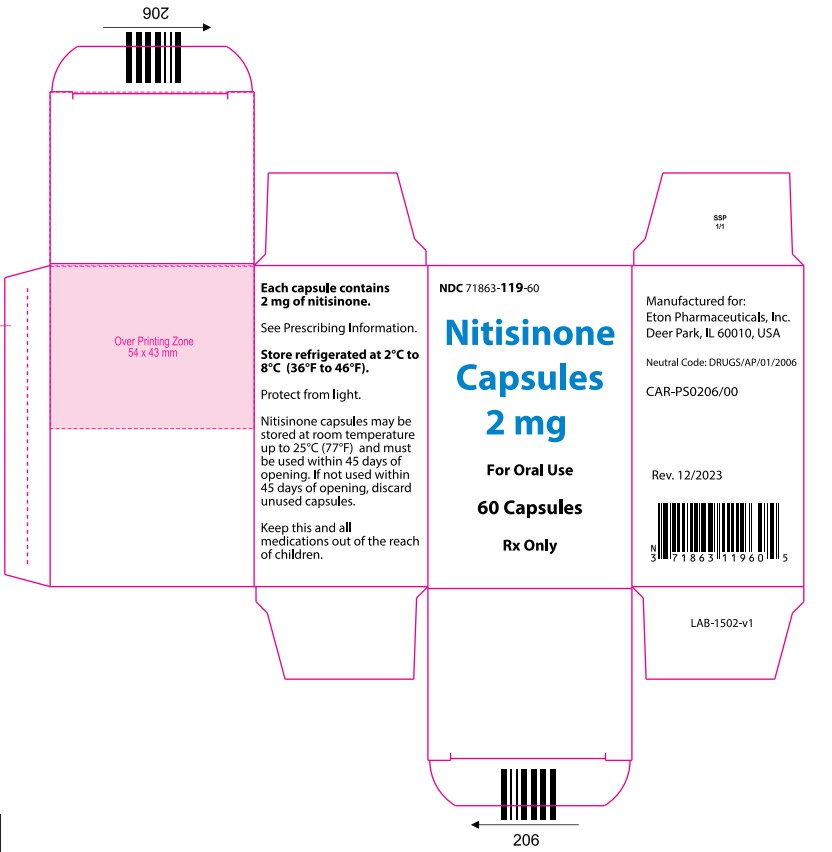
16. HOW SUPPLIED/STORAGE AND HANDLING
The capsules are packed in a high density (HD) polyethylene container fitted with 33 mm
Child-Resistant closure. Each bottle contains 60 capsules.
- 2 mg: Size “3” hard gelatin capsules with white opaque cap imprinted with “NIT2” in
black and white opaque body imprinted ‘ZN11’ in black, filled with white to off-white
powder. (NDC: 71863-119-60)
- 5 mg: Size “3” hard gelatin capsules with white opaque cap imprinted with “NIT5” in
black and white opaque body imprinted ‘ZN12’ in black, filled with white to off-white
powder. (NDC: 71863-120-60)
- 10 mg: Size “3” hard gelatin capsules with white opaque cap imprinted with “NIT10” in
black and white opaque body imprinted ‘ZN13’ in black, filled with white to off-white
powder. (NDC: 71863-121-60)
- 20 mg: Size “3” hard gelatin capsules with white opaque cap imprinted with “NIT20” in
black and white opaque body imprinted ‘ZN14’ in black, filled with white to off-white
powder. (NDC: 71863-122-60)
Store refrigerated at 2° to 8°C (36° to 46°F) “protect from light”. Alternatively,
patients/caregivers may store Nitisinone Capsules at room temperature up to 25°C (77°F) for
up to 45 days. If not used within 45 days, discard Nitisinone Capsules.
-
17. PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling.
Administration of Nitisinone Capsules
- Maintain dietary restriction of tyrosine and phenylalanine when taking nitisinone.
- Capsules: Take at least one hour before, or two hours after a meal. For patients who have
difficulty swallowing the capsules, the capsules may be opened and the contents
suspended in a small amount of water, formula or apple sauce immediately before use.
Elevated Plasma Tyrosine Levels, Ocular Symptoms, Developmental Delay
and Hyperkeratotic Plaques
- Inform patients that inadequate restriction may be associated with ocular signs and
symptoms, intellectual disability and developmental delay, and painful hyperkeratotic
plaques on the soles and palms. Advise patients and caregivers of the need to maintain
dietary restriction of tyrosine and phenylalanine and to report any unexplained ocular,
neurologic, or other symptoms promptly to their healthcare provider [ see Warnings and
Precautions (5.1)].
Manufactured by:
M/s Zenara Pharma Private Limited
Plot No. 83/B, 84, 87 to 96, Phase III, IDA Cherlapally,
Hyderabad, Telangana State - 500051,
India (IND)
Manufactured for:
Eton Pharmaceuticals, Inc. Deer Park, IL 60010
Issued: 02/2024
-
PRINCIPAL DISPLAY PANEL
Nitisinone Capsules - NDC-71863-119-60 - 60 Capsules - 2 mg Container Label
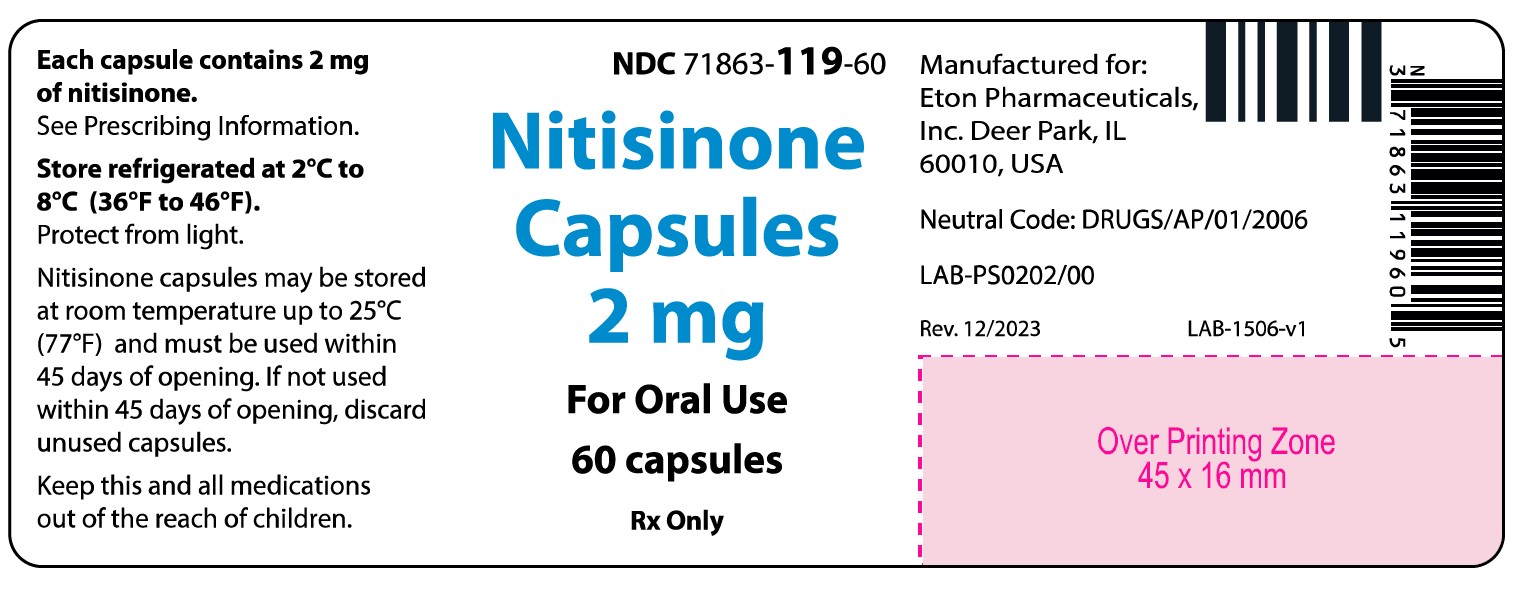
Nitisinone Capsules - NDC-71863-119-60 - 60 Capsules - 2 mg Carton Label
Nitisinone Capsules - NDC-71863-120-60 - 60 Capsules - 5 mg Container Label
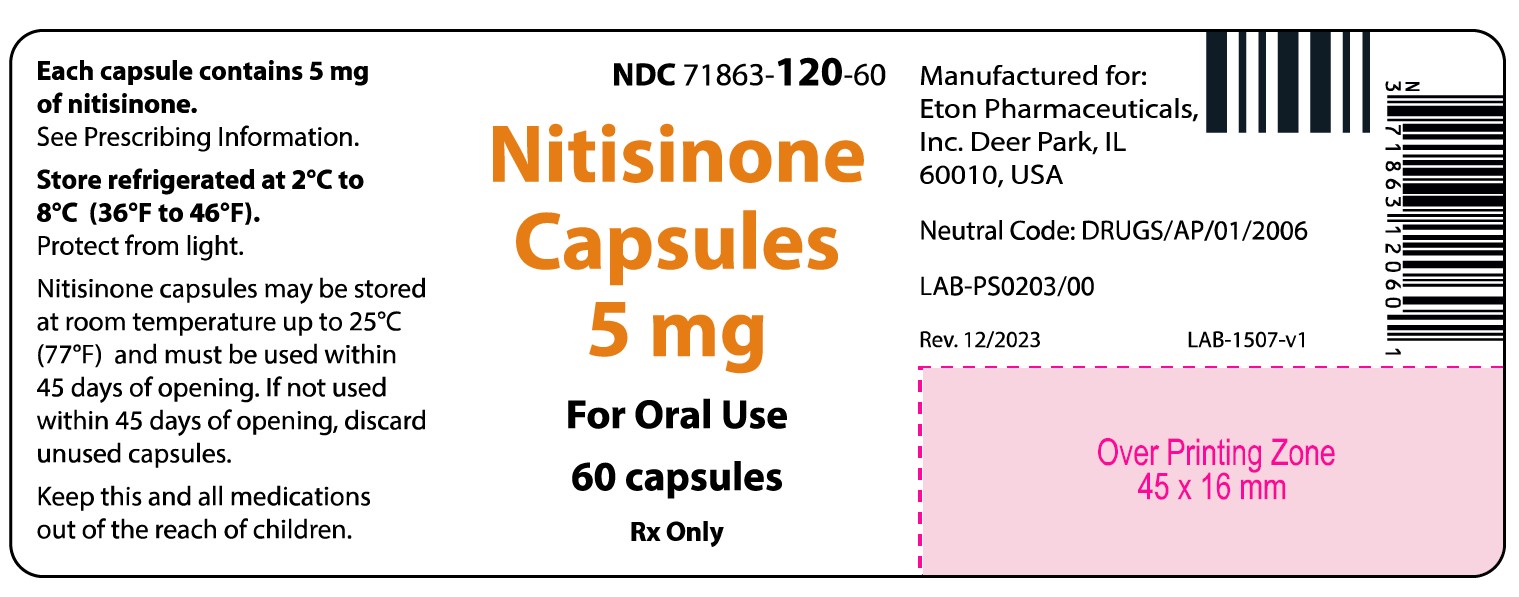
Nitisinone Capsules - NDC-71863-120-60 - 60 Capsules - 5 mg Carton Label

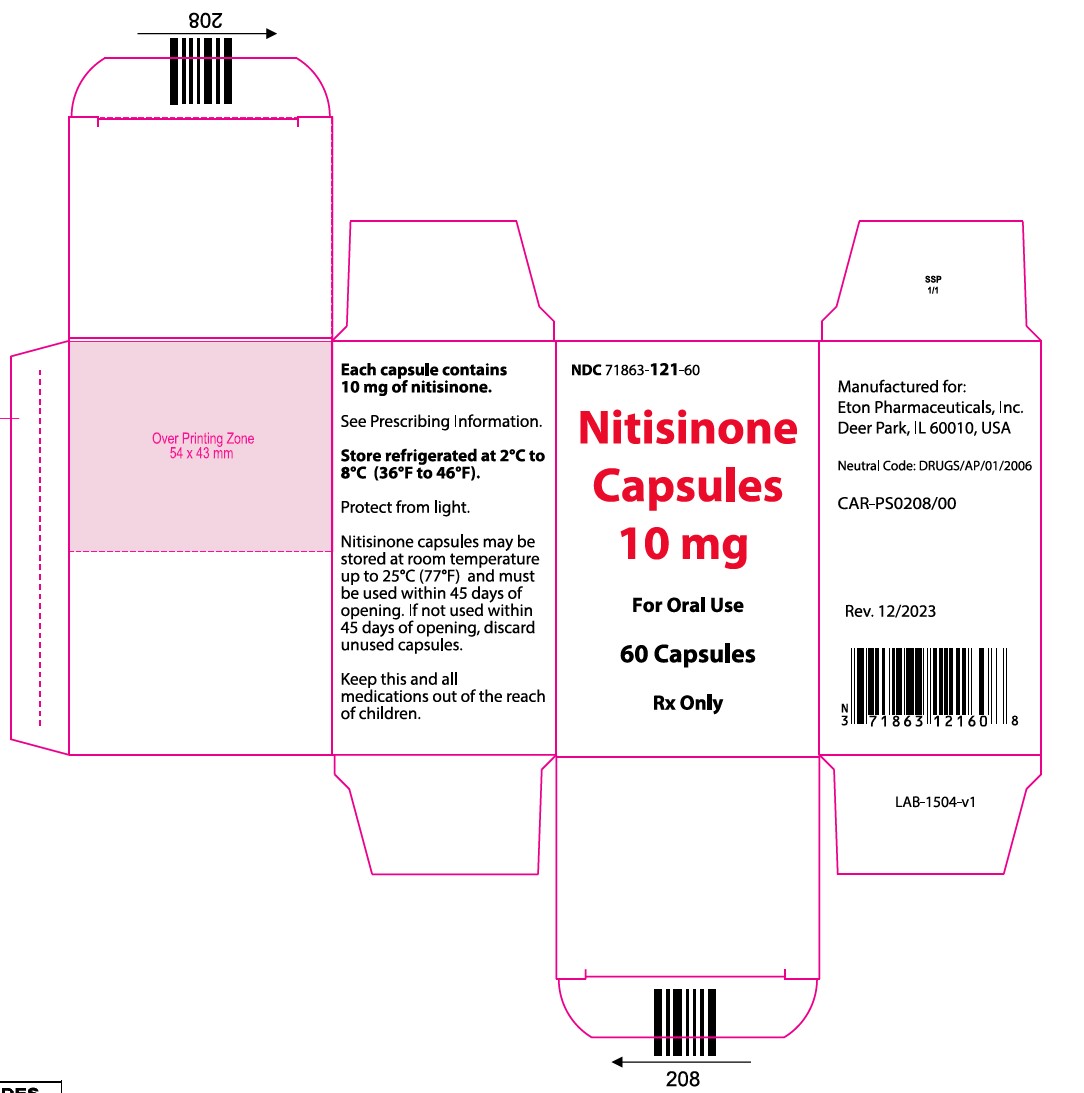
Nitisinone Capsules - NDC-71863-121-60 - 60 Capsules - 10 mg Container Label
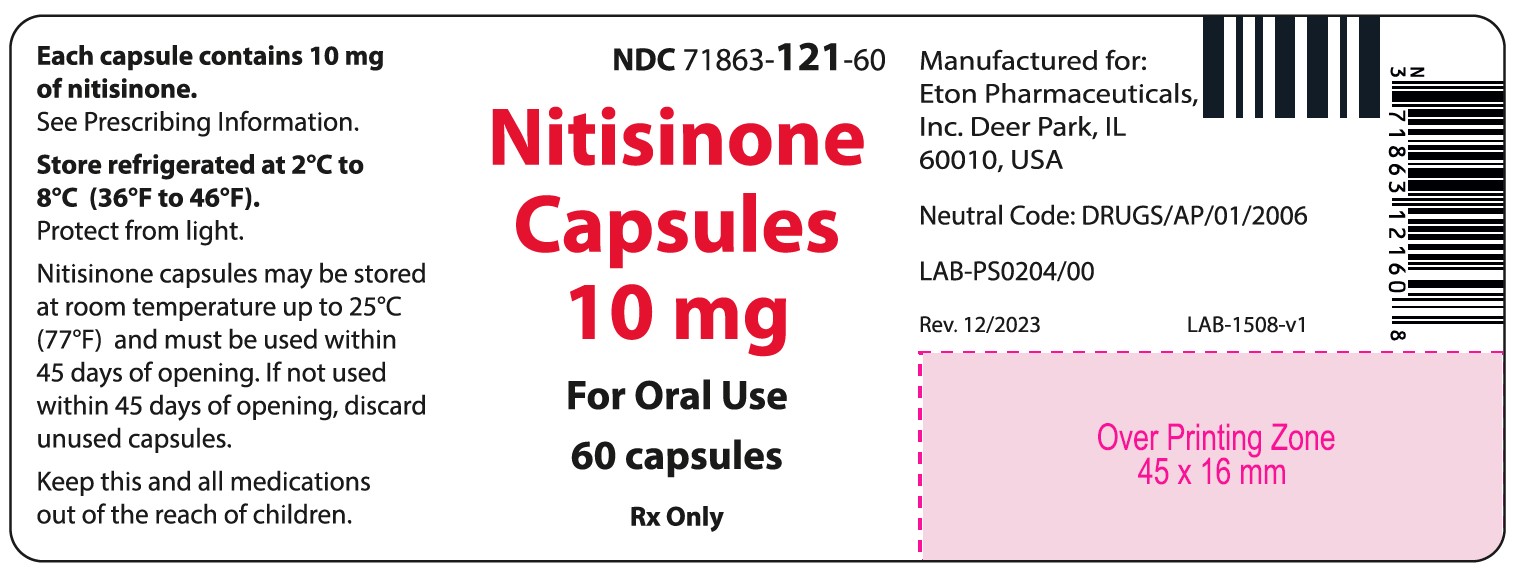
Nitisinone Capsules - NDC-71863-121-60 - 60 Capsules - 10 mg Carton Label
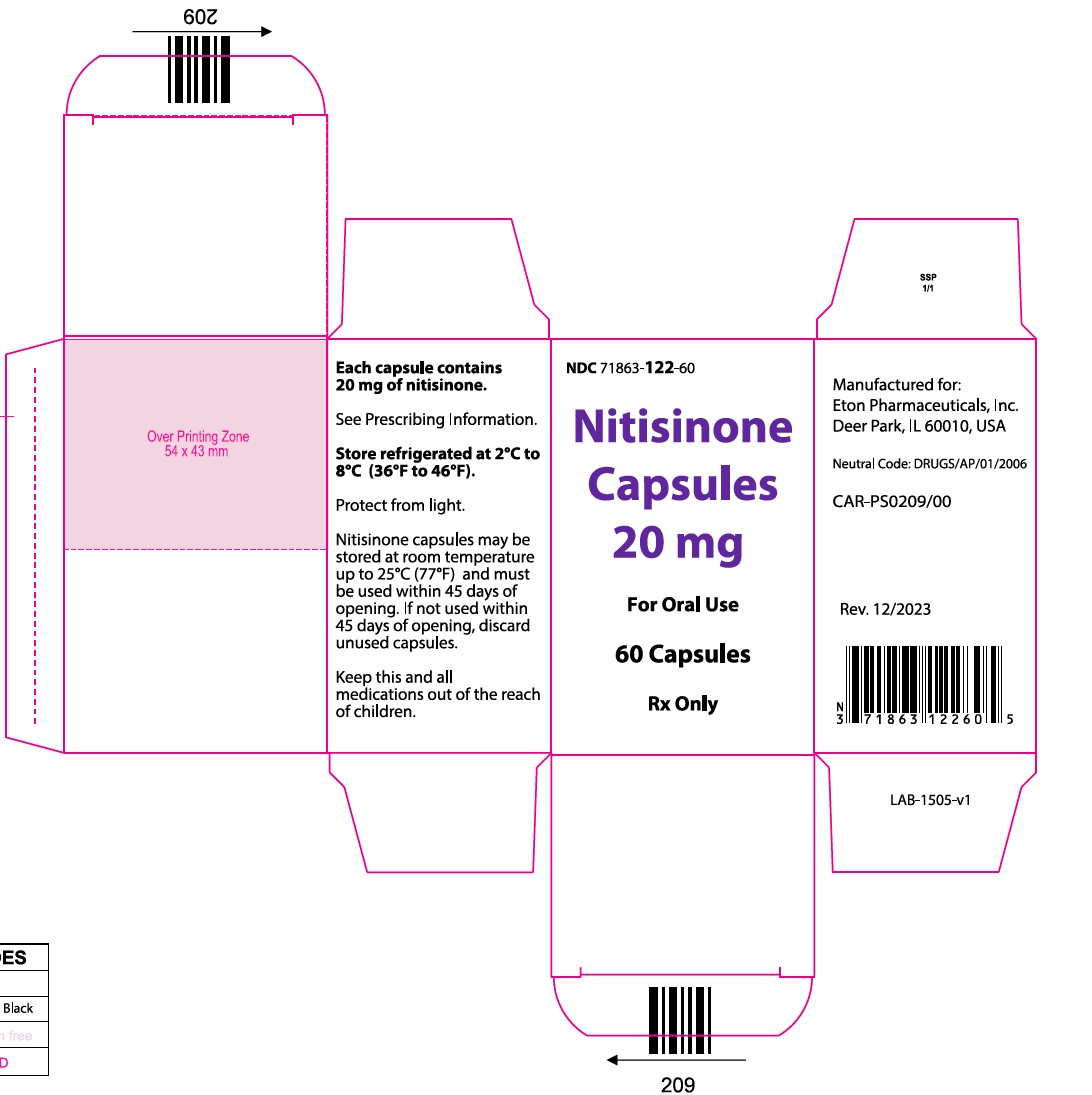
Nitisinone Capsules - NDC-71863-122-60 - 60 Capsules - 20 mg Container Label
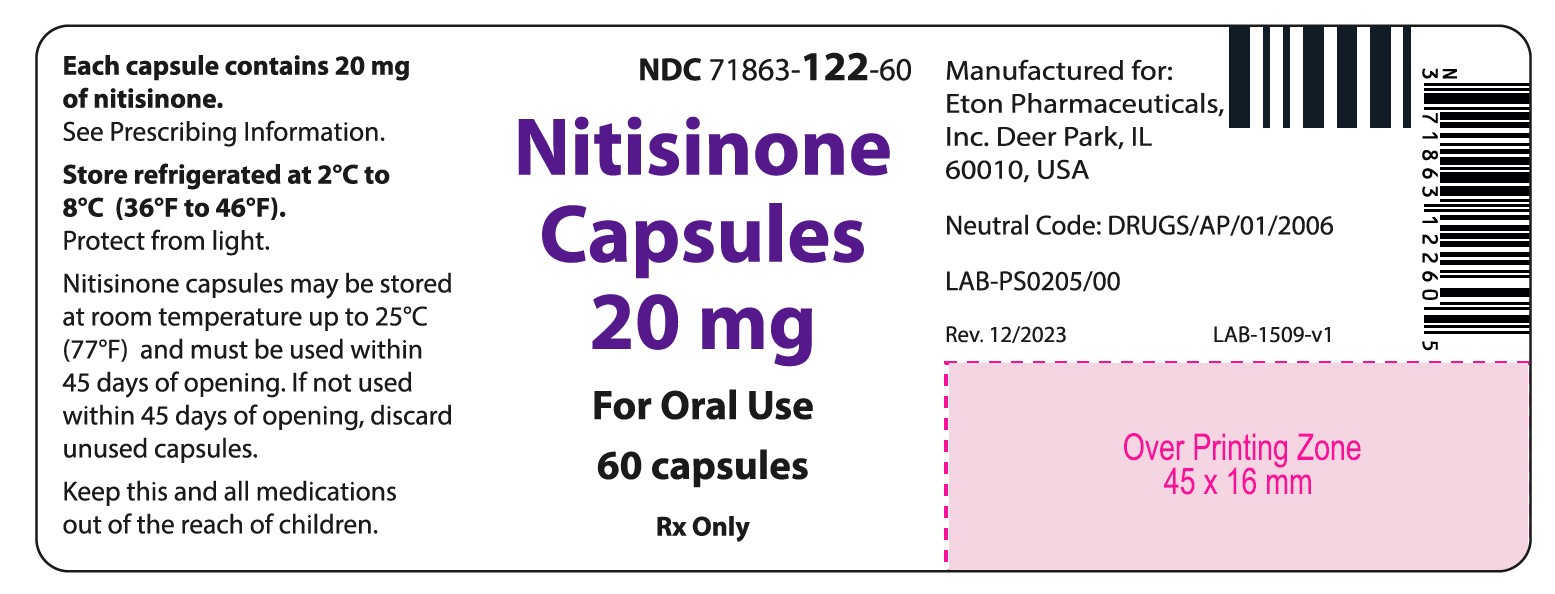
Nitisinone Capsules - NDC-71863-122-60 - 60 Capsules - 20 mg Carton Label
-
INGREDIENTS AND APPEARANCE
NITISINONE
nitisinone capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 71863-119 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength NITISINONE (UNII: K5BN214699) (NITISINONE - UNII:K5BN214699) NITISINONE 2 mg Inactive Ingredients Ingredient Name Strength STEARIC ACID (UNII: 4ELV7Z65AP) ANHYDROUS LACTOSE (UNII: 3SY5LH9PMK) Product Characteristics Color white (White opaque cap filled with white to off-white powder) Score no score Shape CAPSULE Size 3mm Flavor Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 71863-119-60 1 in 1 CARTON 01/15/2024 1 60 in 1 BOTTLE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA216201 01/15/2024 NITISINONE
nitisinone capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 71863-120 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength NITISINONE (UNII: K5BN214699) (NITISINONE - UNII:K5BN214699) NITISINONE 5 mg Inactive Ingredients Ingredient Name Strength ANHYDROUS LACTOSE (UNII: 3SY5LH9PMK) STEARIC ACID (UNII: 4ELV7Z65AP) Product Characteristics Color white (white opaque cap filled with white to off-white powder) Score no score Shape CAPSULE Size 3mm Flavor Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 71863-120-60 1 in 1 CARTON 01/15/2024 1 60 in 1 BOTTLE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA216201 01/15/2024 NITISINONE
nitisinone capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 71863-122 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength NITISINONE (UNII: K5BN214699) (NITISINONE - UNII:K5BN214699) NITISINONE 20 mg Inactive Ingredients Ingredient Name Strength ANHYDROUS LACTOSE (UNII: 3SY5LH9PMK) STEARIC ACID (UNII: 4ELV7Z65AP) Product Characteristics Color white (White opaque cap filled with white to off-white powder) Score no score Shape CAPSULE Size 3mm Flavor Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 71863-122-60 1 in 1 CARTON 01/15/2024 1 60 in 1 BOTTLE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA216201 01/15/2024 NITISINONE
nitisinone capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 71863-121 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength NITISINONE (UNII: K5BN214699) (NITISINONE - UNII:K5BN214699) NITISINONE 10 mg Inactive Ingredients Ingredient Name Strength STEARIC ACID (UNII: 4ELV7Z65AP) ANHYDROUS LACTOSE (UNII: 3SY5LH9PMK) Product Characteristics Color white (White opaque cap filled with white to off-white powder) Score no score Shape CAPSULE Size 3mm Flavor Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 71863-121-60 1 in 1 CARTON 01/15/2024 1 60 in 1 BOTTLE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA216201 01/15/2024 Labeler - Eton Pharmaceuticals, Inc. (080870465) Registrant - Eton Pharmaceuticals, Inc. (080870465)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.