ENOXAPARIN SODIUM injection
Enoxaparin Sodium by
Drug Labeling and Warnings
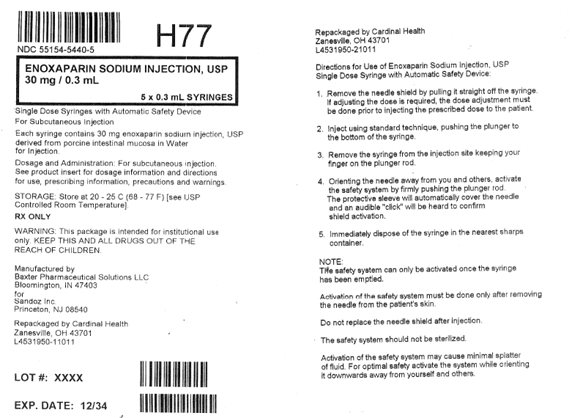
Enoxaparin Sodium by is a Prescription medication manufactured, distributed, or labeled by Cardinal Health. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use ENOXAPARIN SODIUM safely and effectively. See full prescribing information for ENOXAPARIN SODIUM.
ENOXAPARIN SODIUM injection, USP for subcutaneous and intravenous use
Initial U.S. Approval: 1993WARNING: SPINAL/EPIDURAL HEMATOMAS
See full prescribing information for complete boxed warning.
Epidural or spinal hematomas may occur in patients who are anticoagulated with low molecular weight heparins (LMWH) or heparinoids and are receiving neuraxial anesthesia or undergoing spinal puncture. These hematomas may result in long-term or permanent paralysis. Consider these risks when scheduling patients for spinal procedures. Factors that can increase the risk of developing epidural or spinal hematomas in these patients include:
- Use of indwelling epidural catheters
- Concomitant use of other drugs that affect hemostasis, such as non-steroidal anti-inflammatory drugs (NSAIDs), platelet inhibitors, and other anticoagulants
- A history of traumatic or repeated epidural or spinal punctures
- A history of spinal deformity or spinal surgery
- Optimal timing between the administration of enoxaparin sodium injection and neuraxial procedures is not known.
Monitor patients frequently for signs and symptoms of neurological impairment. If neurological compromise is noted, urgent treatment is necessary. (5.1),(7)
INDICATIONS AND USAGE
Enoxaparin sodium injection, USP is a low molecular weight heparin [LMWH] indicated for:
- Prophylaxis of deep vein thrombosis (DVT) in abdominal surgery, hip replacement surgery, knee replacement surgery, or medical patients with severely restricted mobility during acute illness (1.1)
- Inpatient treatment of acute DVT with or without pulmonary embolism (1.2)
- Outpatient treatment of acute DVT without pulmonary embolism. (1.2)
- Prophylaxis of ischemic complications of unstable angina and non-Q-wave myocardial infarction [MI] (1.3)
- Treatment of acute ST-segment elevation myocardial infarction [STEMI] managed medically or with subsequent percutaneous coronary intervention [PCI] (1.4)
DOSAGE AND ADMINISTRATION
See full prescribing information for dosing and administration information. (2)
DOSAGE FORMS AND STRENGTHS
CONTRAINDICATIONS
- Active major bleeding (4)
- History of heparin-induced thrombocytopenia (HIT) within the past 100 days or in the presence of circulating antibodies (4)
- Hypersensitivity to enoxaparin sodium (4)
- Hypersensitivity to heparin or pork products (4)
- Hypersensitivity to benzyl alcohol [for multiple-dose formulation only] (4)
WARNINGS AND PRECAUTIONS
- Increased Risk of Hemorrhage: Monitor for signs of bleeding. (5.1) , 5.2, 5.3)
- Risk of Heparin-Induced Thrombocytopenia with or without Thrombosis. (5.4)
- Thrombocytopenia: Monitor platelet count closely (5.5)
- Interchangeability with other heparins: Do not exchange with heparin or other LMWHs (5.6)
- Increased Risk of Thrombosis in Pregnant Women with Mechanical Prosthetic Heart Valves: Women and their fetuses may be at increased risk. Monitor more frequently and adjust dosage as needed. (5.7)
ADVERSE REACTIONS
Most common adverse reactions (>1%) were bleeding, anemia, thrombocytopenia, elevation of serum aminotransferase, diarrhea, nausea, ecchymosis, fever, edema, peripheral edema, dyspnea, confusion, and injection site pain. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Sandoz Inc. at 1-800-525-8747 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch
DRUG INTERACTIONS
USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 6/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: SPINAL/EPIDURAL HEMATOMAS
1 INDICATIONS AND USAGE
1.1 Prophylaxis of Deep Vein Thrombosis
1.2 Treatment of Acute Deep Vein Thrombosis
1.3 Prophylaxis of Ischemic Complications of Unstable Angina and Non-Q-Wave Myocardial Infarction
1.4 Treatment of Acute ST-Segment Elevation Myocardial Infarction
2 DOSAGE AND ADMINISTRATION
2.1 Pretreatment Evaluation
2.2 Adult Dosage
2.3 Dose Reduction for Patients with Severe Renal Impairment
2.4 Recommended Dosage for Geriatric Patients with Acute ST-Segment Elevation Myocardial Infarction
2.5 Administration
2.6 Monitoring for Safety
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Increased Risk of Hemorrhage
5.2 Increased Risk of Bleeding following Percutaneous Coronary Revascularization Procedures
5.3 Increased Risk of Bleeding in Patients with Concomitant Medical Conditions
5.4 Risk of Heparin-Induced Thrombocytopenia with or without Thrombosis
5.5 Thrombocytopenia
5.6 Interchangeability with Other Heparins
5.7 Increased Risk of Thrombosis in Pregnant Women with Mechanical Prosthetic Heart Valves
5.8 Risk of Serious Adverse Reactions in Infants due to Benzyl Alcohol Preservative
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Patients with Mechanical Prosthetic Heart Valves
8.7 Renal Impairment
8.8 Low-Weight Patients
8.9 Obese Patients
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
13.2 Animal Toxicology and/or Pharmacology
13.3 Reproductive and Developmental Toxicology
14 CLINICAL STUDIES
14.1 Prophylaxis of Deep Vein Thrombosis Following Abdominal Surgery in Patients at Risk for Thromboembolic Complications
14.2 Prophylaxis of Deep Vein Thrombosis Following Hip or Knee Replacement Surgery
14.3 Prophylaxis of Deep Vein Thrombosis in Medical Patients with Severely Restricted Mobility During Acute Illness
14.4 Treatment of Deep Vein Thrombosis with or without Pulmonary Embolism
14.5 Prophylaxis of Ischemic Complications in Unstable Angina and Non-Q-Wave Myocardial Infarction
14.6 Treatment of Acute ST-Segment Elevation Myocardial Infarction
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: SPINAL/EPIDURAL HEMATOMAS
Epidural or spinal hematomas may occur in patients who are anticoagulated with low molecular weight heparins (LMWH) or heparinoids and are receiving neuraxial anesthesia or undergoing spinal puncture. These hematomas may result in long-term or permanent paralysis. Consider these risks when scheduling patients for spinal procedures. Factors that can increase the risk of developing epidural or spinal hematomas in these patients include:
Use of indwelling epidural catheters
Concomitant use of other drugs that affect hemostasis, such as non-steroidal anti-inflammatory drugs (NSAIDs), platelet inhibitors, and other anticoagulants
A history of traumatic or repeated epidural or spinal punctures
A history of spinal deformity or spinal surgery
Optimal timing between the administration of enoxaparin sodium injection and neuraxial procedures is not known.
Monitor patients frequently for signs and symptoms of neurological impairment. If neurological compromise is noted, urgent treatment is necessary.
Consider the benefits and risks before neuraxial intervention in patients anticoagulated or to be anticoagulated for thromboprophylaxis [see Warnings and Precautions (5.1) and Drug Interactions (7)].
-
1 INDICATIONS AND USAGE
1.1 Prophylaxis of Deep Vein Thrombosis
Enoxaparin sodium injection, USP is indicated for the prophylaxis of deep vein thrombosis (DVT), which may lead to pulmonary embolism (PE):
- in patients undergoing abdominal surgery who are at risk for thromboembolic complications [see Clinical Studies (14.1)].
- in patients undergoing hip replacement surgery, during and following hospitalization.
- in patients undergoing knee replacement surgery.
- in medical patients who are at risk for thromboembolic complications due to severely restricted mobility during acute illness.
1.2 Treatment of Acute Deep Vein Thrombosis
Enoxaparin sodium injection, USP is indicated for:
- the inpatient treatment of acute deep vein thrombosis with or without pulmonary embolism, when administered in conjunction with warfarin sodium.
- the outpatient treatment of acute deep vein thrombosis without pulmonary embolism when administered in conjunction with warfarin sodium.
1.3 Prophylaxis of Ischemic Complications of Unstable Angina and Non-Q-Wave Myocardial Infarction
Enoxaparin sodium injection, USP is indicated for the prophylaxis of ischemic complications of unstable angina and non-Q-wave myocardial infarction, when concurrently administered with aspirin.
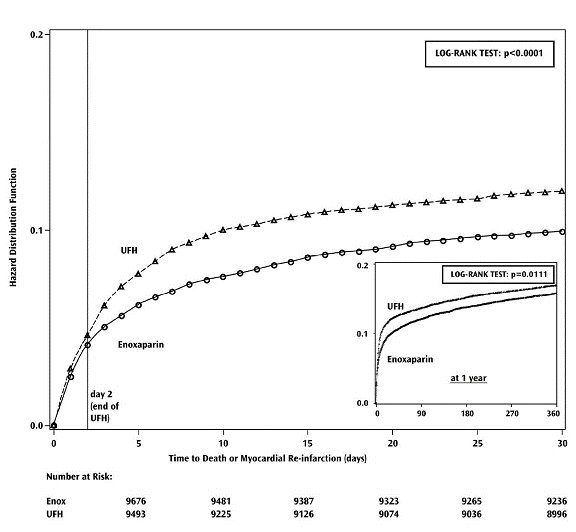
1.4 Treatment of Acute ST-Segment Elevation Myocardial Infarction
Enoxaparin sodium injection, USP, when administered concurrently with aspirin, has been shown to reduce the rate of the combined endpoint of recurrent myocardial infarction or death in patients with acute ST-segment elevation myocardial infarction (STEMI) receiving thrombolysis and being managed medically or with percutaneous coronary intervention (PCI).
-
2 DOSAGE AND ADMINISTRATION
2.1 Pretreatment Evaluation
Evaluate all patients for a bleeding disorder before starting enoxaparin sodium injection treatment, unless treatment is urgently needed.
2.2 Adult Dosage
Abdominal Surgery
The recommended dose of enoxaparin sodium injection is 40 mg by subcutaneous injection once a day (with the initial dose given 2 hours prior to surgery) in patients undergoing abdominal surgery who are at risk for thromboembolic complications. The usual duration of administration is 7 to 10 days [see Clinical Studies (14.1)].
Hip or Knee Replacement Surgery
The recommended dose of enoxaparin sodium injection is 30 mg every 12 hours administered by subcutaneous injection in patients undergoing hip or knee replacement surgery. Administer the initial dose 12 to 24 hours after surgery, provided that hemostasis has been established. The usual duration of administration is 7 to 10 days [see Clinical Studies (14.2)].
A dose of enoxaparin sodium injection of 40 mg once a day subcutaneously may be considered for hip replacement surgery for up to 3 weeks. Administer the initial dose 12 (±3) hours prior to surgery.
Medical Patients During Acute Illness
The recommended dose of enoxaparin sodium injection is 40 mg once a day administered by subcutaneous injection for medical patients at risk for thromboembolic complications due to severely restricted mobility during acute illness. The usual duration of administration is 6 to 11 days [see Clinical Studies (14.3)].
Treatment of Deep Vein Thrombosis With or Without Pulmonary Embolism
The recommended dose of enoxaparin sodium injection is 1 mg/kg every 12 hours administered subcutaneously in patients with acute deep vein thrombosis without pulmonary embolism, who can be treated at home in an outpatient setting.
The recommended dose of enoxaparin sodium injection is 1 mg/kg every 12 hours administered subcutaneously or
1.5 mg/kg once a day administered subcutaneously at the same time every day for inpatient (hospital) treatment of patients with acute deep vein thrombosis with pulmonary embolism or patients with acute deep vein thrombosis without pulmonary embolism (who are not candidates for outpatient treatment).
In both outpatient and inpatient (hospital) treatments, initiate warfarin sodium therapy when appropriate (usually within 72 hours of enoxaparin sodium injection). Continue enoxaparin sodium injection for a minimum of 5 days and until a therapeutic oral anticoagulant effect has been achieved (International Normalization Ratio 2 to 3). The average duration of administration is 7 days [see Clinical Studies (14.4)].
Unstable Angina and Non-Q-Wave Myocardial Infarction
The recommended dose of enoxaparin sodium injection is 1 mg/kg administered subcutaneously every 12 hours in conjunction with oral aspirin therapy (100 to 325 mg once daily) in patients with unstable angina or non-Q-wave myocardial infarction. Treat with enoxaparin sodium injection for a minimum of 2 days and continue until clinical stabilization. The usual duration of treatment is 2 to 8 days [see Warnings and Precautions(5.2) and Clinical Studies (14.5)].
Treatment of Acute ST-Segment Elevation Myocardial Infarction
The recommended dose of enoxaparin sodium injection is a single intravenous bolus of 30 mg plus a 1 mg/kg subcutaneous dose followed by 1 mg/kg administered subcutaneously every 12 hours (maximum 100 mg for the first two doses only, followed by 1 mg/kg dosing for the remaining doses) in patients with acute ST-segment elevation myocardial infarction. Reduce the dosage in patients ≥75 years of age [see Dosage and Administration (2.4)]. Unless contraindicated, administer aspirin to all patients as soon as they are identified as having STEMI and continue dosing with 75 to 325 mg once daily.
When administered in conjunction with a thrombolytic (fibrin-specific or non-fibrin specific), administer enoxaparin sodium injection between 15 minutes before and 30 minutes after the start of fibrinolytic therapy. The usual duration of enoxaparin sodium injection therapy is 8 days or until hospital discharge.
For patients managed with percutaneous coronary intervention (PCI), if the last enoxaparin sodium injection subcutaneous administration was given less than 8 hours before balloon inflation, no additional dosing is needed. If the last enoxaparin sodium injection subcutaneous administration was given more than 8 hours before balloon inflation, administer an intravenous bolus of 0.3 mg/kg of enoxaparin sodium injection [see Warnings and Precautions (5.2)].
2.3 Dose Reduction for Patients with Severe Renal Impairment
The recommended prophylaxis and treatment dosage regimens for patients with severe renal impairment (creatinine clearance <30 mL/min) are described in Table 1[see Use in Specific Populations (8.7) and Clinical Pharmacology (12.3)].
Table 1 Dosage Regimens for Patients with Severe Renal Impairment
(creatinine clearance <30mL/minute)Indication Dosage Regimen Prophylaxis in abdominal surgery
30 mg administered subcutaneously once daily
Prophylaxis in hip or knee replacement surgery
30 mg administered subcutaneously once daily
Prophylaxis in medical patients during acute illness
30 mg administered subcutaneously once daily
Inpatient treatment of acute deep vein thrombosis with or without pulmonary embolism, when administered in conjunction with warfarin sodium
1 mg/kg administered subcutaneously once daily
Outpatient treatment of acute deep vein thrombosis without pulmonary embolism, when administered in conjunction with warfarin sodium
1 mg/kg administered subcutaneously once daily
Prophylaxis of ischemic complications of unstable angina and non-Q-wave myocardial infarction, when concurrently administered with aspirin
1 mg/kg administered subcutaneously once daily
Treatment of acute ST-segment elevation myocardial infarction in patients <75 years of age, when administered in conjunction with aspirin
30 mg single intravenous bolus plus a 1 mg/kg subcutaneous dose followed by 1 mg/kg administered subcutaneously once daily.
Treatment of acute ST-segment elevation myocardial infarction in geriatric patients ≥75 years of age, when administered in conjunction with aspirin
1 mg/kg administered subcutaneously once daily (no initial bolus)
Although no dose adjustment is recommended in patients with creatinine clearance 30 to 50 mL/min and creatinine clearance 50 to 80 mL/min, observe these patients frequently for signs and symptoms of bleeding.
2.4 Recommended Dosage for Geriatric Patients with Acute ST-Segment Elevation Myocardial Infarction
For treatment of acute ST-segment elevation myocardial infarction in geriatric patients ≥75 years of age, do not use an initial intravenous bolus. Initiate dosing with 0.75 mg/kg subcutaneously every 12 hours (maximum 75 mg for the first two doses only, followed by 0.75 mg/kg dosing for the remaining doses) [see Use in Specific Populations (8.5) and Clinical Pharmacology (12.3)].
No dose adjustment is necessary for other indications in geriatric patients unless kidney function is impaired [see Dosage and Administration (2.2)].
2.5 Administration
Do not administer enoxaparin sodium injection by intramuscular injection.
Administer enoxaparin sodium injection by intravenous or subcutaneous injection only.
Enoxaparin sodium injection is a clear, colorless to pale yellow sterile solution, and as with other parenteral drug products, should be inspected visually for particulate matter and discoloration prior to administration.
Use a tuberculin syringe or equivalent when using enoxaparin sodium injection multiple-dose vials to assure withdrawal of the appropriate volume of drug.
Patients may self-inject by the subcutaneous route of administration only after their physicians determine that it is appropriate and with medical follow-up, as necessary. Provide proper training in subcutaneous injection technique before allowing self-injection (with or without the assistance of an injection device).
Subcutaneous Injection Technique
- Position patients in a supine position for enoxaparin sodium administration by deep subcutaneous injection.
- Do not expel the air bubble from the prefilled syringes before the injection, to avoid the loss of drug.
- Alternate injection sites between the left and right anterolateral and left and right posterolateral abdominal wall.
- Introduce the whole length of the needle into a skin fold held between the thumb and forefinger; hold the skin fold throughout the injection. To minimize bruising, do not rub the injection site after completion of the injection
Enoxaparin sodium injection prefilled syringes and graduated prefilled syringes are for single, one-time use only and are available with a system that shields the needle after injection.
Remove the prefilled syringe from the blister packaging by peeling at the arrow as directed on the blister. Do not remove by pulling on the plunger as this may damage the syringe.
- 1.
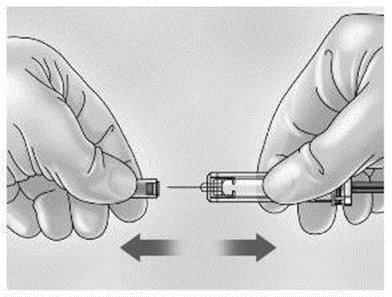
Remove the needle shield by pulling it straight off the syringe (see Figure A). If less than the full syringe volume is needed to administer the prescribed dose, eject syringe contents until the prescribed dose is left in the syringe.
Figure A
- 2.
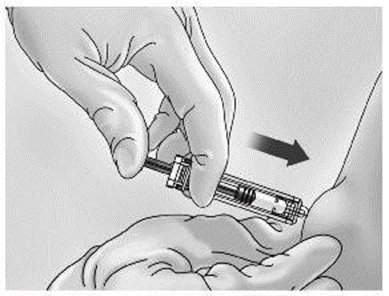
Inject using standard technique, pushing the plunger to the bottom of the syringe (see Figure B).
Figure B
- 3.
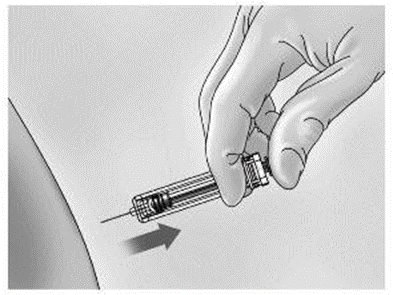
Remove the syringe from the injection site keeping your finger on the plunger rod (see Figure C).
Figure C
- 4.
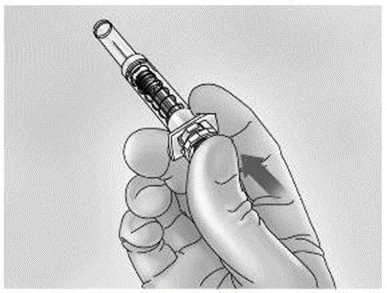
Orient the needle away from you and others, and activate the safety system by firmly pushing the plunger rod. The protective sleeve will automatically cover the needle and an audible “click” will be heard to confirm shield activation (see Figure D).
Figure D
- 5.
Immediately dispose of the syringe in the nearest sharps container (see Figure E).
Figure E
NOTE:
- The safety system can only be activated once the syringe has been emptied.
- Activation of the safety system must be done only after removing the needle from the patient’s skin.
- Do not replace the needle shield after injection.
- The safety system should not be sterilized.
Activation of the safety system may cause minimal splatter of fluid. For optimal safety, activate the system while orienting it downwards away from yourself and others.
Intravenous (Bolus) Injection Technique
Use the multiple-dose vial for intravenous injections. Administer enoxaparin sodium injection through an intravenous line. Do not mix or coadminister enoxaparin sodium injection with other medications. Flush the intravenous access device with a sufficient volume of saline or dextrose solution prior to and following the intravenous bolus administration of enoxaparin sodium injection, to prevent mixing of drugs. Enoxaparin sodium injection is compatible with normal saline solution (0.9%) or 5% dextrose in water.
2.6 Monitoring for Safety
During therapy monitor complete blood counts including platelets and stool occult blood.
Assess for signs and symptoms of bleeding.
In patients with renal impairment anti-Factor Xa levels may be used to monitor the anticoagulant effects of enoxaparin sodium injection.
If during enoxaparin sodium therapy abnormal coagulation parameters or bleeding should occur, anti-Factor Xa levels may be used to monitor the anticoagulant effects of enoxaparin sodium injection [see Clinical Pharmacology (12.3)].
Prothrombin Time (PT) and Activated Partial Thromboplastin Time (aPTT) are not adequate for monitoring the anticoagulant effects of enoxaparin sodium injection.
-
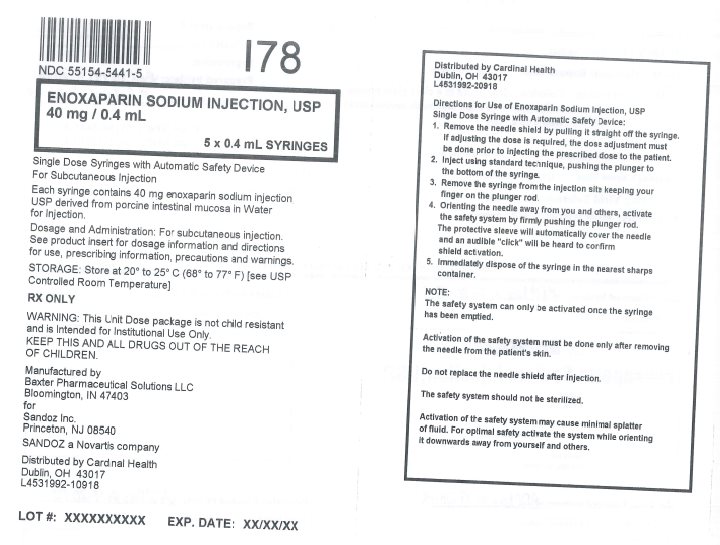
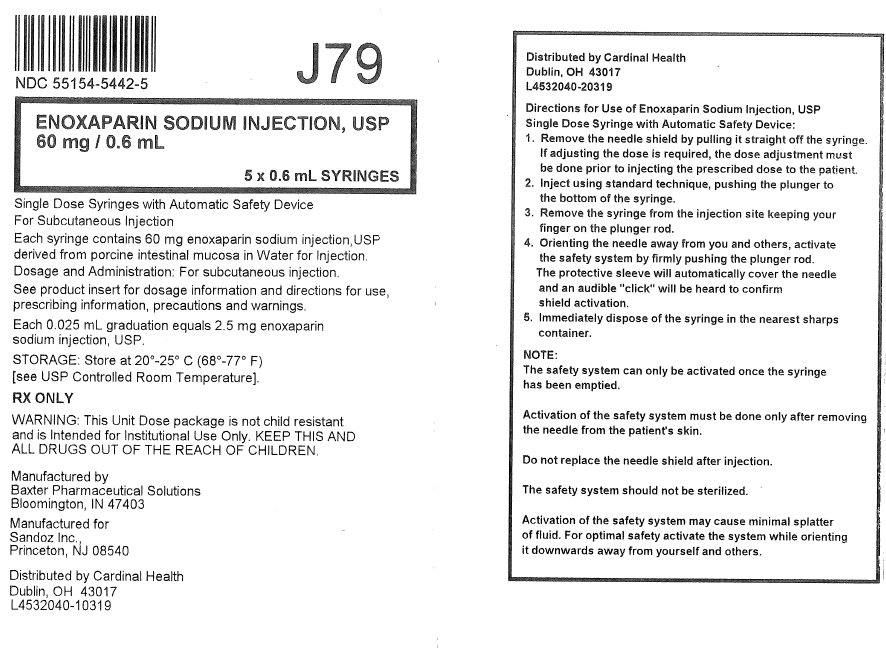
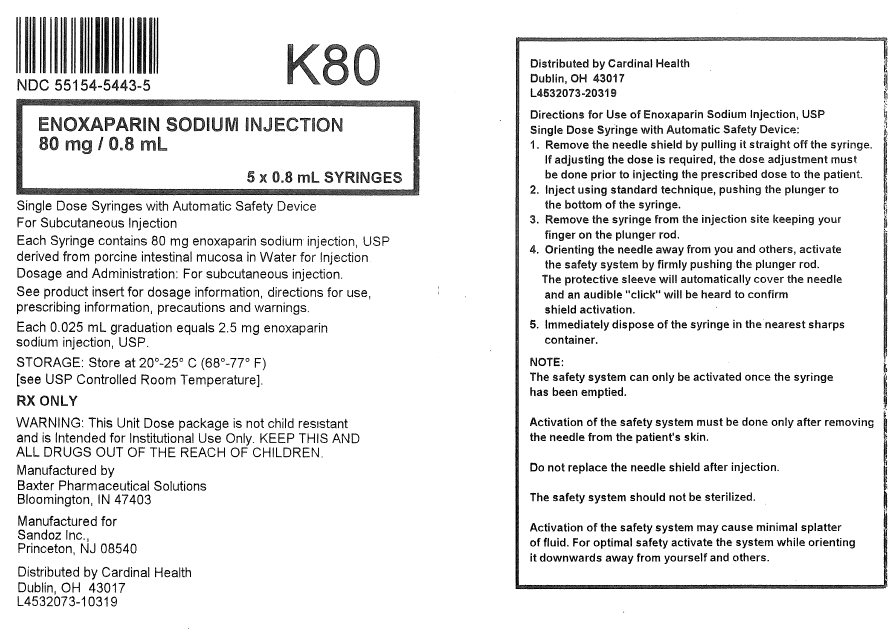
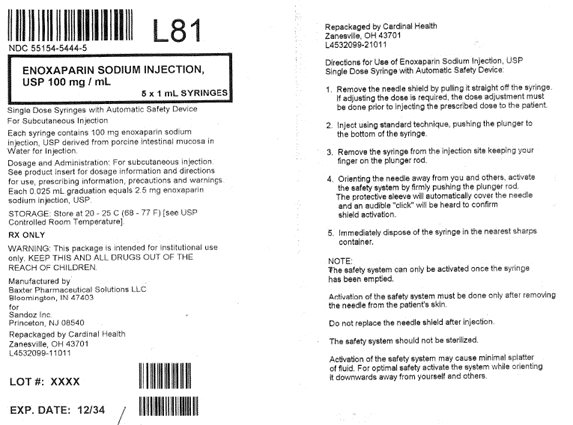
3 DOSAGE FORMS AND STRENGTHS
Enoxaparin sodium injection is available in two concentrations:
100 mg/mL Concentration
-Prefilled Syringes
30 mg / 0.3 mL, 40 mg / 0.4 mL
-Graduated Prefilled Syringes
60 mg / 0.6 mL, 80 mg / 0.8 mL, 100 mg / mL
-Multiple-Dose Vials
300 mg/3 mL
150 mg/mL Concentration
-Graduated Prefilled Syringes
120 mg / 0.8 mL, 150 mg / mL
-
4 CONTRAINDICATIONS
Enoxaparin sodium injection is contraindicated in patients with:
- Active major bleeding.
- History of immune-mediated heparin-induced thrombocytopenia (HIT) within the past 100 days or in the presence of circulating antibodies [see Warnings and Precautions (5.4)].
- Known hypersensitivity to enoxaparin sodium (e.g., pruritus, urticaria, anaphylactic/anaphylactoid reactions) [see Adverse Reactions (6.2)].
- Known hypersensitivity to heparin or pork products.
- Known hypersensitivity to benzyl alcohol (which is in only the multiple-dose formulation of enoxaparin sodium injection) [see Warnings and Precautions (5.8)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Increased Risk of Hemorrhage
Cases of epidural or spinal hemorrhage and subsequent hematomas have been reported with the use of enoxaparin sodium injection and epidural or spinal anesthesia/analgesia or spinal puncture procedures, resulting in long-term or permanent paralysis. The risk of these events is higher with the use of postoperative indwelling epidural catheters, with the concomitant use of additional drugs affecting hemostasis such as NSAIDs, with traumatic or repeated epidural or spinal puncture, or in patients with a history of spinal surgery or spinal deformity [see Boxed Warning, Adverse Reactions (6.2) and Drug Interactions (7)].
To reduce the potential risk of bleeding associated with the concurrent use of enoxaparin sodium and epidural or spinal anesthesia/analgesia or spinal puncture, consider the pharmacokinetic profile of enoxaparin [see Clinical Pharmacology (12.3)]. Placement or removal of an epidural catheter or lumbar puncture is best performed when the anticoagulant effect of enoxaparin is low; however, the exact timing to reach a sufficiently low anticoagulant effect in each patient is not known.
Placement or removal of a catheter should be delayed for at least 12 hours after administration of lower doses (30 mg once or twice daily or 40 mg once daily) of enoxaparin sodium injection, and at least 24 hours after the administration of higher doses (0.75 mg/kg twice daily, 1 mg/kg twice daily, or 1.5 mg/kg once daily) of enoxaparin sodium injection. Anti-Xa levels are still detectable at these time points, and these delays are not a guarantee that neuraxial hematoma will be avoided. Patients receiving the 0.75 mg/kg twice daily dose or the 1 mg/kg twice daily dose should not receive the second enoxaparin dose in the twice daily regimen to allow a longer delay before catheter placement or removal. Likewise, although a specific recommendation for timing of a subsequent enoxaparin sodium injection dose after catheter removal cannot be made, consider delaying this next dose for at least four hours, based on a benefit-risk assessment considering both the risk for thrombosis and the risk for bleeding in the context of the procedure and patient risk factors. For patients with creatinine clearance <30mL/minute, additional considerations are necessary because elimination of enoxaparin is more prolonged; consider doubling the timing of removal of a catheter, at least 24 hours for the lower prescribed dose of enoxaparin sodium injection (30 mg once daily) and at least 48 hours for the higher dose (1 mg/kg/day) [see Clinical Pharmacology (12.3)].
Should the physician decide to administer anticoagulation in the context of epidural or spinal anesthesia/analgesia or lumbar puncture, frequent monitoring must be exercised to detect any signs and symptoms of neurological impairment such as midline back pain, sensory and motor deficits (numbness or weakness in lower limbs), and bowel and/or bladder dysfunction. Instruct patients to report immediately if they experience any of the above signs or symptoms. If signs or symptoms of spinal hematoma are suspected, initiate urgent diagnosis and treatment including consideration for spinal cord decompression even though such treatment may not prevent or reverse neurological sequelae.
Use enoxaparin sodium injection with extreme caution in conditions with increased risk of hemorrhage, such as bacterial endocarditis, congenital or acquired bleeding disorders, active ulcerative and angiodysplastic gastrointestinal disease, hemorrhagic stroke, or shortly after brain, spinal, or ophthalmological surgery, or in patients treated concomitantly with platelet inhibitors.
Major hemorrhages including retroperitoneal and intracranial bleeding have been reported. Some of these cases have been fatal.
Bleeding can occur at any site during therapy with enoxaparin sodium injection. An unexplained fall in hematocrit or blood pressure should lead to a search for a bleeding site.
5.2 Increased Risk of Bleeding following Percutaneous Coronary Revascularization Procedures
To minimize the risk of bleeding following the vascular instrumentation during the treatment of unstable angina, non-Q-wave myocardial infarction, and acute ST-segment elevation myocardial infarction, adhere precisely to the intervals recommended between enoxaparin sodium injection doses. It is important to achieve hemostasis at the puncture site after PCI. In case a closure device is used, the sheath can be removed immediately. If a manual compression method is used, sheath should be removed 6 hours after the last intravenous/subcutaneous enoxaparin sodium injection. If the treatment with enoxaparin sodium is to be continued, the next scheduled dose should be given no sooner than 6 to 8 hours after sheath removal. The site of the procedure should be observed for signs of bleeding or hematoma formation [see Dosage and Administration (2.1)].
5.3 Increased Risk of Bleeding in Patients with Concomitant Medical Conditions
Enoxaparin sodium injection should be used with care in patients with a bleeding diathesis, uncontrolled arterial hypertension or a history of recent gastrointestinal ulceration, diabetic retinopathy, renal dysfunction and hemorrhage.
5.4 Risk of Heparin-Induced Thrombocytopenia with or without Thrombosis
Enoxaparin sodium injection may cause Heparin-Induced Thrombocytopenia (HIT) or Heparin-Induced Thrombocytopenia with Thrombosis (HITTS). HITTS may lead to organ infarction, limb ischemia, or death. Monitor thrombocytopenia of any degree closely.
Use of enoxaparin sodium injection in patients with a history of immune-mediated HIT within the past 100 days or in the presence of circulating antibodies is contraindicated [see Contraindications (4)]. Circulating antibodies may persist for several years.
Only use enoxaparin sodium injection in patients with a history of HIT if more than 100 days have elapsed since the prior HIT episode and no circulating antibodies are present. Because HIT may still occur in these circumstances, the decision to use enoxaparin sodium injection in such a case must be made only after a careful benefit-risk assessment and after non-heparin alternative treatments are considered.
5.5 Thrombocytopenia
Thrombocytopenia can occur with the administration of enoxaparin sodium injection.
Moderate thrombocytopenia (platelet counts between 100,000/mm3 and 50,000/mm3) occurred at a rate of 1.3% in patients given enoxaparin sodium injection, 1.2% in patients given heparin, and 0.7% in patients given placebo in clinical trials.
Platelet counts less than 50,000/mm3 occurred at a rate of 0.1% in patients given enoxaparin sodium injection, in 0.2% of patients given heparin, and 0.4% of patients given placebo in the same trials.
Thrombocytopenia of any degree should be monitored closely. If the platelet count falls below 100,000/mm3, enoxaparin sodium injection should be discontinued.
5.6 Interchangeability with Other Heparins
Enoxaparin sodium injection cannot be used interchangeably (unit for unit) with heparin or other low molecular weight heparins as they differ in manufacturing process, molecular weight distribution, anti-Xa and anti-IIa activities, units, and dosage. Each of these medicines has its own instructions for use.
5.7 Increased Risk of Thrombosis in Pregnant Women with Mechanical Prosthetic Heart Valves
Use of enoxaparin sodium injection for thromboprophylaxis in pregnant women with mechanical prosthetic heart valves may result in valve thrombosis. In a clinical study of pregnant women with mechanical prosthetic heart valves given enoxaparin (1 mg/kg twice daily) to reduce the risk of thromboembolism, 2 of 8 women developed clots resulting in blockage of the valve and leading to maternal and fetal death. No patients in the heparin/warfarin group (0 of 4 women) died. There also have been isolated postmarketing reports of valve thrombosis in pregnant women with mechanical prosthetic heart valves while receiving enoxaparin for thromboprophylaxis. Women with mechanical prosthetic heart valves may be at higher risk for thromboembolism during pregnancy and, when pregnant, have a higher rate of fetal loss from stillbirth, spontaneous abortion, and premature delivery. Therefore, frequent monitoring of peak and trough anti-Factor Xa levels, and adjusting of dosage may be needed [see Use in Specific Populations (8.6)].
5.8 Risk of Serious Adverse Reactions in Infants due to Benzyl Alcohol Preservative
Enoxaparin sodium injection multiple-dose vials are not approved for use in neonates or infants.
Serious and fatal adverse reactions including “gasping syndrome” can occur in neonates and low birth weight infants treated with benzyl alcohol-preserved drugs, including enoxaparin sodium injection multiple-dose vials. The “gasping syndrome” is characterized by central nervous system depression, metabolic acidosis, and gasping respirations. The minimum amount of benzyl alcohol at which serious adverse reactions may occur is not known (enoxaparin sodium injection multiple-dose vials contain 15 mg of benzyl alcohol per mL) [see Use in Specific Populations (8.4)].
Because benzyl alcohol may cross the placenta, if anticoagulation with enoxaparin sodium injection is needed during pregnancy, use the preservative-free formulations where possible [see Use in Specific Populations (8.1)].
-
6 ADVERSE REACTIONS
The following serious adverse reactions are also discussed in other sections of the labeling:
- Spinal/epidural hematomas [see Boxed Warning and Warnings and Precautions (5.1)]
- Increased Risk of Hemorrhage [see Warnings and Precautions (5.1)]
- Thrombocytopenia [see Warnings and Precautions (5.5)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
During clinical development for the approved indications, 15,918 patients were exposed to enoxaparin sodium. These included 1,228 for prophylaxis of deep vein thrombosis following abdominal surgery in patients at risk for thromboembolic complications, 1,368 for prophylaxis of deep vein thrombosis following hip or knee replacement surgery, 711 for prophylaxis of deep vein thrombosis in medical patients with severely restricted mobility during acute illness, 1,578 for prophylaxis of ischemic complications in unstable angina and non-Q-wave myocardial infarction, 10,176 for treatment of acute ST-elevation myocardial infarction, and 857 for treatment of deep vein thrombosis with or without pulmonary embolism. Enoxaparin sodium doses in the clinical trials for prophylaxis of deep vein thrombosis following abdominal or hip or knee replacement surgery or in medical patients with severely restricted mobility during acute illness ranged from 40 mg subcutaneously once daily to 30 mg subcutaneously twice daily. In the clinical studies for prophylaxis of ischemic complications of unstable angina and non-Q-wave myocardial infarction doses were 1 mg/kg every 12 hours and in the clinical studies for treatment of acute ST-segment elevation myocardial infarction enoxaparin sodium doses were a 30 mg intravenous bolus followed by 1 mg/kg every 12 hours subcutaneously.
Hemorrhage
The following rates of major bleeding events have been reported during clinical trials with enoxaparin sodium injection (seeTables 2to7).
Table 2 Major Bleeding Episodes Following Abdominal and Colorectal Surgery* Dosing Regimen
IndicationsEnoxaparin Sodium
Injection
40 mg daily subcutaneously
Heparin
5000 U q8hsubcutaneously- * Bleeding complications were considered major: (1) if the hemorrhage caused a significant clinical event, or (2) if accompanied by a hemoglobin decrease ≥2 g/dL or transfusion of 2 or more units of blood products. Retroperitoneal, intraocular, and intracranial hemorrhages were always considered major.
Abdominal Surgery
n = 555
23 (4%)n = 560
16 (3%)Colorectal Surgery
n = 673
28 (4%)n = 674
21 (3%)Table 3 Major Bleeding Episodes Following Hip or Knee Replacement Surgery* Dosing Regimen
IndicationsEnoxaparin Sodium Injection
40 mg dailysubcutaneouslyEnoxaparin Sodium Injection
30 mg q12h subcutaneously
Heparin
15,000 U/24hsubcutaneously- * Bleeding complications were considered major: (1) if the hemorrhage caused a significant clinical event, or (2) if accompanied by a hemoglobin decrease ≥2 g/dL or transfusion of 2 or more units of blood products. Retroperitoneal and intracranial hemorrhages were always considered major. In the knee replacement surgery trials, intraocular hemorrhages were also considered major hemorrhages.
- † Enoxaparin sodium injection 30 mg every 12 hours subcutaneously initiated 12 to 24 hours after surgery and continued for up to 14 days after surgery.
- ‡ Enoxaparin sodium injection 40 mg subcutaneously once a day initiated up to 12 hours prior to surgery and continued for up to 7 days after surgery.
- § Enoxaparin sodium injection 40 mg subcutaneously once a day for up to 21 days after discharge.
Hip Replacement Surgery Without Extended Prophylaxis†
n = 786
31 (4%)n = 541
32 (6%)Hip Replacement Surgery
With Extended ProphylaxisPeri-operative Period‡
n = 288
4 (2%)Extended Prophylaxis
Period§n = 221
0 (0%)Knee Replacement Surgery
Without Extended
Prophylaxis†n = 294
3 (1%)n = 225
3 (1%)NOTE: At no time point were the 40 mg once a day pre-operative and the 30 mg every 12 hours postoperative hip replacement surgery prophylactic regimens compared in clinical trials.
Injection site hematomas during the extended prophylaxis period after hip replacement surgery occurred in 9% of the enoxaparin sodium injection patients versus 1.8% of the placebo patients.
Table 4 Major Bleeding Episodes in Medical Patients With Severely Restricted Mobility During Acute Illness* Dosing Regimen
IndicationEnoxaparin Sodium Injection†
20 mg dailysubcutaneouslyEnoxaparin Sodium Injection†
40 mg daily subcutaneously
Placebo†- * Bleeding complications were considered major: (1) if the hemorrhage caused a significant clinical event, (2) if the hemorrhage caused a decrease in hemoglobin of ≥2 g/dL or transfusion of 2 or more units of blood products. Retroperitoneal and intracranial hemorrhages were always considered major although none were reported during the trial.
- † The rates represent major bleeding on study medication up to 24 hours after last dose.
Medical Patients
During Acute
Illnessn = 351
1 (<1%)n = 360
3 (<1%)n = 362
2 (<1%)Table 5 Major Bleeding Episodes in Deep Vein Thrombosis with or without Pulmonary Embolism Treatment* Dosing Regimen†
IndicationEnoxaparin Sodium Injection
1.5 mg/kg dailysubcutaneouslyEnoxaparin Sodium Injection
1 mg/kg q12h subcutaneouslyHeparin
aPTT Adjusted Intravenous Therapy- * Bleeding complications were considered major: (1) if the hemorrhage caused a significant clinical event, or (2) if accompanied by a hemoglobin decrease ≥2 g/dL or transfusion of 2 or more units of blood products. Retroperitoneal, intraocular, and intracranial hemorrhages were always considered major.
- † All patients also received warfarin sodium (dose-adjusted according to PT to achieve an INR of 2.0 to 3.0) commencing within 72 hours of enoxaparin sodium injection or standard heparin therapy and continuing for up to 90 days.
Treatment of DVT and PE
n = 298
5 (2%)n = 559
9 (2%)n = 554
9 (2%)Table 6 Major Bleeding Episodes in Unstable Angina and Non-Q-Wave Myocardial Infarction Dosing Regimen
IndicationEnoxaparin Sodium Injection*
1 mg/kg q12h subcutaneouslyHeparin*
aPTT Adjusted Intravenous Therapy- * The rates represent major bleeding on study medication up to 12 hours after dose.
- † Aspirin therapy was administered concurrently (100 to 325 mg per day).
- ‡ Bleeding complications were considered major: (1) if the hemorrhage caused a significant clinical event, or (2) if accompanied by a hemoglobin decrease by ≥3 g/dL or transfusion of 2 or more units of blood products. Intraocular, retroperitoneal, and intracranial hemorrhages were always considered major.
n = 1578
17 (1%)n = 1529
18 (1%)Table 7 Major Bleeding Episodes in Acute ST-Segment Elevation Myocardial Infarction Dosing Regimen
IndicationEnoxaparin Sodium Injection*
Initial 30 mg intravenous bolus followed by 1 mg/kg q12h subcutaneouslyHeparin*
aPTT Adjusted Intravenous Therapy- * The rates represent major bleeding (including ICH) up to 30 days
- † Bleedings were considered major if the hemorrhage caused a significant clinical event associated with a hemoglobin decrease by ≥ 5 g/dL. ICH were always considered major.
Acute ST-Segment Elevation Myocardial Infarction
n = 10176
n (%)
n = 10151
n (%)
- Major bleeding (including ICH)†
211 (2.1)
138 (1.4)
- Intracranial hemorrhages (ICH)
84 (0.8)
66 (0.7)
Elevations of Serum Aminotransferases
Asymptomatic increases in aspartate (AST [SGOT]) and alanine (ALT [SGPT]) aminotransferase levels greater than three times the upper limit of normal of the laboratory reference range have been reported in up to 6.1% and 5.9% of patients, respectively, during treatment with enoxaparin sodium injection. Since aminotransferase determinations are important in the differential diagnosis of myocardial infarction, liver disease, and pulmonary emboli, elevations that might be caused by drugs like enoxaparin sodium injection should be interpreted with caution.
Local Reactions
Local irritation, pain, hematoma, ecchymosis, and erythema may follow subcutaneous injection of enoxaparin sodium injection.
Adverse Reactions in Patients Receiving Enoxaparin Sodium Injection for Prophylaxis or Treatment of DVT, PE
Other adverse reactions that were thought to be possibly or probably related to treatment with enoxaparin sodium injection, heparin, or placebo in clinical trials with patients undergoing hip or knee replacement surgery, abdominal or colorectal surgery, or treatment for DVT and that occurred at a rate of at least 2% in the enoxaparin sodium injection group, are provided below (seeTables8 to 11).
Table 8 Adverse Reactions Occurring at ≥2% Incidence in Enoxaparin Sodium Injection-Treated Patients Undergoing Abdominal or Colorectal Surgery Dosing Regimen Enoxaparin Sodium Injection
40 mg daily subcutaneously
n = 1228
%
Heparin
5000 U q8h subcutaneously
n = 1234
%Adverse Reaction Severe Total Severe Total Hemorrhage
<1
7
<1
6
Anemia
<1
3
<1
3
Ecchymosis
0
3
0
3
Table 9 Adverse Reactions Occurring at ≥2% Incidence in Enoxaparin Sodium Injection-Treated Patients Undergoing Hip or Knee Replacement Surgery Dosing Regimen
Enoxaparin Sodium Injection
40 mg daily subcutaneouslyEnoxaparin
Sodium
Injection
30 mg q12h
subcutaneously
Heparin
15,000
U/24h subcutaneously
Placebo
q12h subcutaneously
Peri-Operative
Period
n = 288*
%Extended
Prophylaxis
Period
n = 131†
%
n = 1080
%
n = 766
%
n = 115
%Adverse Reaction
Severe
Total
Severe
Total
Severe
Total
Severe
Total
Severe
Total- * Data represent enoxaparin sodium injection 40 mg subcutaneously once a day initiated up to 12 hours prior to surgery in 288 hip replacement surgery patients who received enoxaparin sodium injection peri-operatively in an unblinded fashion in one clinical trial.
- † Data represent enoxaparin sodium injection 40 mg subcutaneously once a day given in a blinded fashion as extended prophylaxis at the end of the peri-operative period in 131 of the original 288 hip replacement surgery patients for up to 21 days in one clinical trial.
Fever
0
8
0
0
<1
5
<1
4
0
3
Hemorrhage
<1
13
0
5
<1
4
1
4
0
3
Nausea
<1
3
<1
2
0
2
Anemia
0
16
0
<2
<1
2
2
5
<1
7
Edema
<1
2
<1
2
0
2
Peripheral edema
0
6
0
0
<1
3
<1
4
0
3
Table 10 Adverse Reactions Occurring at ≥2% Incidence in Enoxaparin Sodium Injection-Treated Medical Patients with Severely Restricted Mobility During Acute Illness Dosing Regimen
Adverse ReactionEnoxaparin Sodium Injection
40 mg daily subcutaneously
n = 360
%
Placebo
daily subcutaneously
n = 362
%Dyspnea
3.3
5.2
Thrombocytopenia
2.8
2.8
Confusion
2.2
1.1
Diarrhea
2.2
1.7
Nausea
2.5
1.7
Table 11 Adverse Reactions Occurring at ≥2% Incidence in Enoxaparin Sodium Injection-Treated Patients Undergoing Treatment of Deep Vein Thrombosis With or Without Pulmonary Embolism Dosing Regimen Enoxaparin Sodium Injection
1.5 mg/kg daily subcutaneously
n = 298
%Enoxaparin Sodium Injection
1 mg/kg q12h subcutaneously
n = 559
%Heparin
aPTT Adjusted Intravenous Therapy
n = 544
%Adverse Reaction Severe Total Severe Total Severe Total Injection Site Hemorrhage
0
5
0
3
<1
<1
Injection Site Pain
0
2
0
2
0
0
Hematuria
0
2
0
<1
<1
2
Adverse Events in Enoxaparin Sodium Injection-Treated Patients with Unstable Angina or Non-Q-Wave Myocardial Infarction
Non-hemorrhagic clinical events reported to be related to enoxaparin sodium injection therapy occurred at an incidence of ≤1%.
Non-major hemorrhagic events, primarily injection site ecchymosis and hematomas, were more frequently reported in patients treated with subcutaneous enoxaparin sodium injection than in patients treated with intravenous heparin.
Serious adverse events with enoxaparin sodium injection or heparin in a clinical trial in patients with unstable angina or non-Q-wave myocardial infarction that occurred at a rate of at least 0.5% in the enoxaparin sodium injection group are provided below (seeTable 12).
Table 12 Serious Adverse Events Occurring at ≥0.5% Incidence in Enoxaparin Sodium Injection-Treated Patients With Unstable Angina or Non-Q-Wave Myocardial Infarction Dosing Regimen
Adverse EventEnoxaparin Sodium Injection
1 mg/kg q12h subcutaneously
n = 1578
n (%)
Heparin
aPTT Adjusted Intravenous Therapy
n = 1529
n (%)Atrial fibrillation
11 (0.70)
3 (0.20)
Heart failure
15 (0.95)
11 (0.72)
Lung edema
11 (0.70)
11 (0.72)
Pneumonia
13 (0.82)
9 (0.59)
6.2 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of enoxaparin sodium injection. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
There have been reports of epidural or spinal hematoma formation with concurrent use of enoxaparin sodium injection and spinal/epidural anesthesia or spinal puncture. The majority of patients had a postoperative indwelling epidural catheter placed for analgesia or received additional drugs affecting hemostasis such as NSAIDs. Many of the epidural or spinal hematomas caused neurologic injury, including long-term or permanent paralysis.
Local reactions at the injection site (e.g. nodules, inflammation, oozing), systemic allergic reactions (e.g. pruritus, urticaria, anaphylactic/anaphylactoid reactions including shock), vesiculobullous rash, cases of hypersensitivity cutaneous vasculitis, purpura, skin necrosis (occurring at either the injection site or distant from the injection site), thrombocytosis, and thrombocytopenia with thrombosis [seeWarnings and Precautions (5.5)] have been reported.
Cases of hyperkalemia have been reported. Most of these reports occurred in patients who also had conditions that tend toward the development of hyperkalemia (e.g., renal dysfunction, concomitant potassium-sparing drugs, administration of potassium, hematoma in body tissues). Very rare cases of hyperlipidemia have also been reported, with one case of hyperlipidemia, with marked hypertriglyceridemia, reported in a diabetic pregnant woman; causality has not been determined.
Cases of headache, hemorrhagic anemia, eosinophilia, alopecia, hepatocellular and cholestatic liver injury have been reported. Osteoporosis has also been reported following long-term therapy.
-
7 DRUG INTERACTIONS
Whenever possible, agents which may enhance the risk of hemorrhage should be discontinued prior to initiation of enoxaparin sodium injection therapy. These agents include medications such as: anticoagulants, platelet inhibitors including acetylsalicylic acid, salicylates, NSAIDs (including ketorolac tromethamine), dipyridamole, or sulfinpyrazone. If coadministration is essential, conduct close clinical and laboratory monitoring [see Warnings and Precautions (5.1)].
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Placental transfer of enoxaparin was observed in the animal studies. Human data from a retrospective cohort study, which included 693 live births, suggest that enoxaparin does not increase the risk of major developmental abnormalities (see Data). Based on animal data, enoxaparin sodium is not predicted to increase the risk of major developmental abnormalities (see Data).
Adverse outcomes in pregnancy occur regardless of the health of the mother or the use of medications. The estimated background risk of major birth defects and miscarriage for the indicated populations is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Clinical Considerations
Pregnancy alone confers an increased risk for thromboembolism that is even higher for women with thromboembolic disease and certain high risk pregnancy conditions. While not adequately studied, pregnant women with mechanical prosthetic heart valves may be at even higher risk for thrombosis [seeWarnings and Precautions (5.7) and Use in Specific Populations (8.6)]. Pregnant women with thromboembolic disease, including those with mechanical prosthetic heart valves and those with inherited or acquired thrombophilias, have an increased risk of other maternal complications and fetal loss regardless of the type of anticoagulant used.
All patients receiving anticoagulants, including pregnant women, are at risk for bleeding. Pregnant women receiving enoxaparin sodium should be carefully monitored for evidence of bleeding or excessive anticoagulation. Consideration for use of a shorter acting anticoagulant should be specifically addressed as delivery approaches [see Boxed Warning]. Hemorrhage can occur at any site and may lead to death of mother and/or fetus. Pregnant women should be apprised of the potential hazard to the fetus and the mother if enoxaparin sodium is administered during pregnancy.
It is not known if monitoring of anti-Factor Xa activity and dose adjustment (by weight or anti-Factor Xa activity) of enoxaparin sodium injection affect the safety and the efficacy of the drug during pregnancy.
Cases of “gasping syndrome” have occurred in premature infants when large amounts of benzyl alcohol have been administered (99-405 mg/kg/day). The multiple-dose vial of enoxaparin sodium injection contains 15 mg benzyl alcohol per 1 mL as a preservative [seeWarnings and Precautions (5.8)].
Data
Human data
There are no adequate and well-controlled studies in pregnant women. A retrospective study reviewed the records of 604 women who used enoxaparin sodium during pregnancy. A total of 624 pregnancies resulted in 693 live births. There were 72 hemorrhagic events (11 serious) in 63 women. There were 14 cases of neonatal hemorrhage. Major congenital anomalies in live births occurred at rates (2.5%) similar to background rates.
There have been postmarketing reports of fetal death when pregnant women received enoxaparin sodium injection. Causality for these cases has not been determined. Insufficient data, the underlying disease, and the possibility of inadequate anticoagulation complicate the evaluation of these cases.
A clinical study using enoxaparin sodium in pregnant women with mechanical prosthetic heart valves has been conducted [seeWarnings and Precautions (5.7)].
Animal data
Teratology studies have been conducted in pregnant rats and rabbits at subcutaneous doses of enoxaparin up to 15 times the recommended human dose (by comparison with 2 mg/kg as the maximum recommended daily dose). There was no evidence of teratogenic effects or fetotoxicity due to enoxaparin. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed.
8.2 Lactation
Risk Summary
It is unknown whether enoxaparin sodium is excreted in human milk. In lactating rats, the passage of enoxaparin or its metabolites in the milk is very limited. There is no information available on the effect of enoxaparin or its metabolites on the breastfed child, or on the milk production. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for enoxaparin sodium injection and any potential adverse effects on the breastfed child from enoxaparin sodium injection or from the underlying maternal condition.
8.4 Pediatric Use
Safety and effectiveness of enoxaparin sodium injection in pediatric patients have not been established.
Enoxaparin sodium injection is not approved for use in neonates or infants.
Serious adverse reactions including fatal reactions and the “gasping syndrome” occurred in premature neonates and low birth weight infants in the neonatal intensive care unit who received drugs containing benzyl alcohol as a preservative. In these cases, benzyl alcohol dosages of 99 to 234 mg/kg/day produced high levels of benzyl alcohol and its metabolites in the blood and urine (blood levels of benzyl alcohol were 0.61 to 1.378 mmol/L). Additional adverse reactions included gradual neurological deterioration, seizures, intracranial hemorrhage, hematologic abnormalities, skin breakdown, hepatic and renal failure, hypotension, bradycardia, and cardiovascular collapse. Preterm, low-birth weight infants may be more likely to develop these reactions because they may be less able to metabolize benzyl alcohol. The minimum amount of benzyl alcohol at which serious adverse reactions may occur is not known.
Enoxaparin sodium injection multiple-dose vials contain 15 mg/mL of benzyl alcohol (at the dose of 1.5 mg/kg twice a day, benzyl alcohol exposure in patients is 0.45 mg/kg daily) [see Warnings and Precautions (5.8)].
8.5 Geriatric Use
Prevention of Deep Vein Thrombosis in Hip, Knee and Abdominal Surgery; Treatment of Deep Vein Thrombosis, Prevention of Ischemic Complications of Unstable Angina and Non-Q-Wave Myocardial Infarction
Over 2800 patients, 65 years and older, have received enoxaparin sodium injection in clinical trials. The efficacy of enoxaparin sodium injection in the geriatric (≥65 years) was similar to that seen in younger patients (<65 years). The incidence of bleeding complications was similar between geriatric and younger patients when 30 mg every 12 hours or 40 mg once a day doses of enoxaparin sodium injection were employed. The incidence of bleeding complications was higher in geriatric patients as compared to younger patients when enoxaparin sodium injection was administered at doses of 1.5 mg/kg once a day or 1 mg/kg every 12 hours. The risk of enoxaparin sodium injection -associated bleeding increased with age. Serious adverse events increased with age for patients receiving enoxaparin sodium injection. Other clinical experience (including postmarketing surveillance and literature reports) has not revealed additional differences in the safety of enoxaparin sodium injection between geriatric and younger patients. Careful attention to dosing intervals and concomitant medications (especially antiplatelet medications) is advised. Enoxaparin sodium injection should be used with care in geriatric patients who may show delayed elimination of enoxaparin. Monitoring of geriatric patients with low body weight (<45 kg) and those predisposed to decreased renal function should be considered [seeWarnings and Precautions (2.6) and Clinical Pharmacology (12.3)].
Treatment of Acute ST-Segment Elevation Myocardial Infarction
In the clinical study for treatment of acute ST-segment elevation myocardial infarction, there was no evidence of difference in efficacy between patients ≥75 years of age (n = 1241) and patients less than 75 years of age (n = 9015). Patients ≥75 years of age did not receive a 30 mg intravenous bolus prior to the normal dosage regimen and had their subcutaneous dose adjusted to 0.75 mg/kg every 12 hours [seeDosage and Administration (2.4)]. The incidence of bleeding complications was higher in patients ≥65 years of age as compared to younger patients (<65 years).
8.6 Patients with Mechanical Prosthetic Heart Valves
The use of enoxaparin sodium injection has not been adequately studied for thromboprophylaxis in patients with mechanical prosthetic heart valves and has not been adequately studied for long-term use in this patient population. Isolated cases of prosthetic heart valve thrombosis have been reported in patients with mechanical prosthetic heart valves who have received enoxaparin sodium for thromboprophylaxis. Some of these cases were pregnant women in whom thrombosis led to maternal and fetal deaths. Insufficient data, the underlying disease and the possibility of inadequate anticoagulation complicate the evaluation of these cases. Pregnant women with mechanical prosthetic heart valves may be at higher risk for thromboembolism [see Warnings and Precautions (5.7)].
8.7 Renal Impairment
In patients with renal impairment, there is an increase in exposure of enoxaparin sodium. All such patients should be observed carefully for signs and symptoms of bleeding. Because exposure of enoxaparin sodium is significantly increased in patients with severe renal impairment (creatinine clearance <30 mL/min), a dosage adjustment is recommended for therapeutic and prophylactic dosage ranges. No dosage adjustment is recommended in patients with creatinine clearance 30 to<50 mL/min and creatinine clearance 50 to80 mL/min [see Dosage and Administration (2.3) and Clinical Pharmacology (12.3)]. In patients with renal failure, treatment with enoxaparin sodium has been associated with the development of hyperkalemia [see Adverse Reactions (6.2)].
8.8 Low-Weight Patients
An increase in exposure of enoxaparin sodium with prophylactic dosages (non-weight adjusted) has been observed in low-weight women (<45 kg) and low-weight men (<57 kg). Observe low-weight patients frequently for signs and symptoms of bleeding [see Clinical Pharmacology (12.3)].
8.9 Obese Patients
Obese patients are at higher risk for thromboembolism. The safety and efficacy of prophylactic doses of enoxaparin sodium injection in obese patients (BMI >30 kg/m2) has not been fully determined and there is no consensus for dose adjustment. Observe these patients carefully for signs and symptoms of thromboembolism.
-
10 OVERDOSAGE
Accidental overdosage following administration of enoxaparin sodium injection may lead to hemorrhagic complications. Injected enoxaparin sodium may be largely neutralized by the slow intravenous injection of protamine sulfate (1% solution). The dose of protamine sulfate should be equal to the dose of enoxaparin sodium injected: 1 mg protamine sulfate should be administered to neutralize 1 mg enoxaparin sodium injection, if enoxaparin sodium was administered in the previous 8 hours. An infusion of 0.5 mg protamine per 1 mg of enoxaparin sodium may be administered if enoxaparin sodium was administered greater than 8 hours previous to the protamine administration, or if it has been determined that a second dose of protamine is required. The second infusion of 0.5 mg protamine sulfate per 1 mg of enoxaparin sodium injection may be administered if the aPTT measured 2 to 4 hours after the first infusion remains prolonged.
If at least 12 hours have elapsed since the last enoxaparin sodium injection, protamine administration may not be required; however, even with higher doses of protamine, the aPTT may remain more prolonged than following administration of heparin. In all cases, the anti-Factor Xa activity is never completely neutralized (maximum about 60%). Particular care should be taken to avoid overdosage with protamine sulfate. Administration of protamine sulfate can cause severe hypotensive and anaphylactoid reactions. Because fatal reactions, often resembling anaphylaxis, have been reported with protamine sulfate, it should be given only when resuscitation techniques and treatment of anaphylactic shock are readily available. For additional information consult the labeling of protamine sulfate injection products.
-
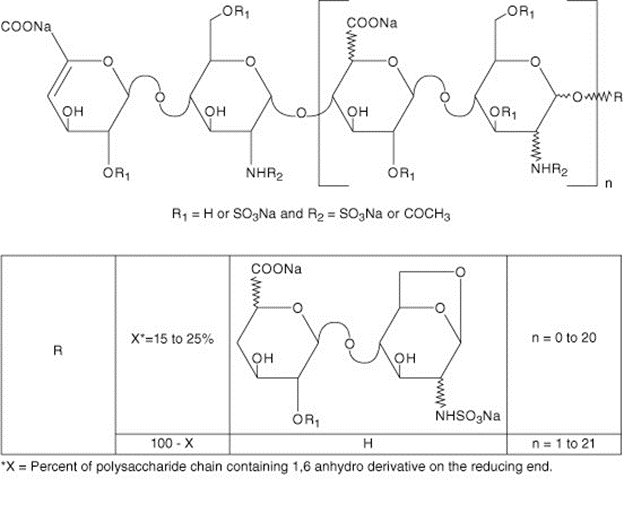
11 DESCRIPTION
Enoxaparin sodium injection, USP is a sterile aqueous solution containing enoxaparin sodium, a low molecular weight heparin. The pH of the injection is 5.5 to 7.5.
Enoxaparin sodium is obtained by alkaline depolymerization of heparin benzyl ester derived from porcine intestinal mucosa. Its structure is characterized by a 2-O-sulfo-4-enepyranosuronic acid group at the non-reducing end and a 2-N,6-O-disulfo-D-glucosamine at the reducing end of the chain. About 20% (ranging between 15% and 25%) of the enoxaparin structure contains a 1,6 anhydro derivative on the reducing end of the polysaccharide chain. The drug substance is the sodium salt. The average molecular weight is about 4500 daltons. The molecular weight distribution is:
<2000 daltons
≤20%
2000 to 8000 daltons
≥68%
>8000 daltons
≤18%
STRUCTURAL FORMULA
Enoxaparin Sodium Injection, USP 100 mg/mL Concentration contains 10 mg enoxaparin sodium (approximate anti-Factor Xa activity of 1000 IU [with reference to the W.H.O. First International Low Molecular Weight Heparin Reference Standard]) per 0.1 mL Water for Injection.
Enoxaparin Sodium Injection, USP 150 mg/mL Concentration contains 15 mg enoxaparin sodium (approximate anti-Factor Xa activity of 1500 IU [with reference to the W.H.O. First International Low Molecular Weight Heparin Reference Standard]) per 0.1 mL Water for Injection.
The enoxaparin sodium injection, USP prefilled syringes and graduated prefilled syringes are preservative-free and intended for use only as a single-dose injection. The multiple-dose vial contains 15 mg benzyl alcohol per 1 mL as a preservative [see Dosage and Administration (2) and How Supplied/Storage and Handling (16)].
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Enoxaparin is a low molecular weight heparin which has antithrombotic properties.
12.2 Pharmacodynamics
In humans, enoxaparin given at a dose of 1.5 mg/kg subcutaneously is characterized by a higher ratio of anti-Factor Xa to anti-Factor IIa activity (mean ± SD, 14.0 ± 3.1) (based on areas under anti-Factor activity versus time curves) compared to the ratios observed for heparin (mean±SD, 1.22 ± 0.13). Increases of up to 1.8 times the control values were seen in the thrombin time (TT) and the activated partial thromboplastin time (aPTT). Enoxaparin at a 1 mg/kg dose (100 mg / mL concentration), administered subcutaneously every 12 hours to patients in a large clinical trial resulted in aPTT values of 45 seconds or less in the majority of patients (n = 1607). A 30 mg intravenous bolus immediately followed by a 1 mg/kg subcutaneous administration resulted in aPTT postinjection values of 50 seconds. The average aPTT prolongation value on Day 1 was about 16% higher than on Day 4.
12.3 Pharmacokinetics
Absorption
Pharmacokinetic trials were conducted using the 100 mg/mL formulation. Maximum anti-Factor Xa and anti-thrombin (anti-Factor IIa) activities occur 3 to 5 hours after subcutaneous injection of enoxaparin. Mean peak anti-Factor Xa activity was 0.16 IU/mL (1.58 mcg/mL) and 0.38 IU/mL (3.83 mcg/mL) after the 20 mg and the 40 mg clinically tested subcutaneous doses, respectively. Mean (n = 46) peak anti-Factor Xa activity was 1.1 IU/mL at steady state in patients with unstable angina receiving 1 mg/kg subcutaneously every 12 hours for 14 days. Mean absolute bioavailability of enoxaparin, after 1.5 mg/kg given subcutaneously, based on anti-Factor Xa activity is approximately 100% in healthy subjects.
A 30 mg intravenous bolus immediately followed by 1 mg/kg subcutaneously every 12 hours provided initial peak anti-Factor Xa levels of 1.16 IU/mL (n=16) and average exposure corresponding to 84% of steady-state levels. Steady state is achieved on the second day of treatment.
Enoxaparin pharmacokinetics appears to be linear over the recommended dosage ranges [seeDosage and Administration (2)]. After repeated subcutaneous administration of 40 mg once daily and 1.5 mg/kg once-daily regimens in healthy volunteers, the steady state is reached on day 2 with an average exposure ratio about 15% higher than after a single dose. Steady-state enoxaparin activity levels are well predicted by single-dose pharmacokinetics. After repeated subcutaneous administration of the 1 mg/kg twice-daily regimen, the steady state is reached from day 4 with mean exposure about 65% higher than after a single dose and mean peak and trough levels of about 1.2 and 0.52 IU/mL, respectively. Based on enoxaparin sodium pharmacokinetics, this difference in steady state is expected and within the therapeutic range.
Although not studied clinically, the 150 mg/mL concentration of enoxaparin sodium is projected to result in anticoagulant activities similar to those of 100 mg/mL and 200 mg/mL concentrations at the same enoxaparin dose. When a daily 1.5 mg/kg subcutaneous injection of enoxaparin sodium was given to 25 healthy male and female subjects using a 100 mg/mL or a 200 mg/mL concentration the following pharmacokinetic profiles were obtained (seeTable 13):
Table 13 Pharmacokinetic Parameters* After 5 Days of 1.5 mg/kg Subcutaneous Once Daily Doses of Enoxaparin Sodium Using 100 mg/mL or 200 mg/mL Concentrations Concentration Anti-Xa Anti-IIa Heptest aPTT - * Means ± SD at Day 5 and 90% Confidence Interval (CI) of the ratio
- † Median (range)
Amax
(IU/mL or
Δ sec)100 mg/mL
1.37
(±0.23)0.23
(±0.05)105
(±17)19
(±5)200 mg/mL
1.45
(±0.22)0.26
(±0.05)111
(±17)22
(±7)90% CI
102%-110%
102%-111%
tmax† (h)
100 mg/mL
3
(2-6)4
(2-5)2.5
(2-4.5)3
(2-4.5)200 mg/mL
3.5
(2-6)4.5
(2.5-6)3.3
(2-5)3
(2-5)AUC (ss)
(h*IU/mL
or h* Δ sec)100 mg/mL
14.26
(±2.93)1.54
(±0.61)1321
(±219)200 mg/mL
15.43
(±2.96)1.77
(±0.67)1401
(±227)90% CI
105%-112%
103%-109%
Elimination
Following intravenous dosing, the total body clearance of enoxaparin is 26 mL/min. After intravenous dosing of enoxaparin labeled with the gamma-emitter, 99mTc, 40% of radioactivity and 8 to 20% of anti-Factor Xa activity were recovered in urine in 24 hours. Elimination half-life based on anti-Factor Xa activity was 4.5 hours after a single subcutaneous dose to about 7 hours after repeated dosing. Significant anti-Factor Xa activity persists in plasma for about 12 hours following a 40 mg subcutaneous once a day dose.
Following subcutaneous dosing, the apparent clearance (CL/F) of enoxaparin is approximately 15 mL/min.
Metabolism
Enoxaparin sodium is primarily metabolized in the liver by desulfation and/or depolymerization to lower molecular weight species with much reduced biological potency. Renal clearance of active fragments represents about 10% of the administered dose and total renal excretion of active and non-active fragments 40% of the dose.
Special Populations
Gender
Apparent clearance and Amax derived from anti-Factor Xa values following single subcutaneous dosing (40 mg and 60 mg) were slightly higher in males than in females. The source of the gender difference in these parameters has not been conclusively identified; however, body weight may be a contributing factor.
Geriatric
Apparent clearance and Amax derived from anti-Factor Xa values following single and multiple subcutaneous dosing in geriatric subjects were close to those observed in young subjects. Following once a day subcutaneous dosing of 40 mg enoxaparin, the Day 10 mean area under anti-Factor Xa activity versus time curve (AUC) was approximately 15% greater than the mean Day 1 AUC value [see Dosage and Administration () and Use in Specific Populations ()].
Renal impairment
A linear relationship between anti-Factor Xa plasma clearance and creatinine clearance at steady state has been observed, which indicates decreased clearance of enoxaparin sodium in patients with reduced renal function. Anti-Factor Xa exposure represented by AUC, at steady state, is marginally increased in patients with creatinine clearance 50 to80 mL/min and patients with creatinine clearance 30 to<50 mL/min renal impairment after repeated subcutaneous 40 mg once-daily doses. In patients with severe renal impairment (creatinine clearance <30 mL/min), the AUC at steady state is significantly increased on average by 65% after repeated subcutaneous 40 mg once-daily doses [see Dosage and Administration () and Use in Specific Populations ()].
Hemodialysis
In a single study, elimination rate appeared similar but AUC was two-fold higher than control population, after a single 0.25 or 0.5 mg/kg intravenous dose.
Hepatic impairment
Studies with enoxaparin sodium in patients with hepatic impairment have not been conducted and the impact of hepatic impairment on the exposure to enoxaparin is unknown.
Weight
After repeated subcutaneous 1.5 mg/kg once-daily dosing, mean AUC of anti-Factor Xa activity is marginally higher at steady state in obese healthy volunteers (BMI 30-48 kg/m2) compared to non-obese control subjects, while Amax is not increased.
When non-weight adjusted dosing was administered, it was found after a single-subcutaneous 40 mg dose, that anti-Factor Xa exposure is 52% higher in low-weight women (<45 kg) and 27% higher in low-weight men (<57 kg) when compared to normal weight control subjects [see Use in Specific Populations ()].
Pharmacokinetic Interaction
No pharmacokinetic interaction was observed between enoxaparin sodium and thrombolytics when administered concomitantly. -
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
No long-term studies in animals have been performed to evaluate the carcinogenic potential of enoxaparin. Enoxaparin was not mutagenic in in vitro tests, including the Ames test, mouse lymphoma cell forward mutation test, and human lymphocyte chromosomal aberration test, and the in vivo rat bone marrow chromosomal aberration test. Enoxaparin was found to have no effect on fertility or reproductive performance of male and female rats at subcutaneous doses up to 20 mg/kg/day or 141 mg/m2/day. The maximum human dose in clinical trials was 2 mg/kg/day or 78 mg/m2/day (for an average body weight of 70 kg, height of 170 cm, and body surface area of 1.8 m2).
13.2 Animal Toxicology and/or Pharmacology
A single subcutaneous dose of 46.4 mg/kg enoxaparin was lethal to rats. The symptoms of acute toxicity were ataxia, decreased motility, dyspnea, cyanosis, and coma.
13.3 Reproductive and Developmental Toxicology
Teratology studies have been conducted in pregnant rats and rabbits at subcutaneous doses of enoxaparin up to 30 mg/kg/day corresponding to 211 mg/m2/day and 410 mg/m2/day in rats and rabbits respectively. There was no evidence of teratogenic effects or fetotoxicity due to enoxaparin.
-
14 CLINICAL STUDIES
14.1 Prophylaxis of Deep Vein Thrombosis Following Abdominal Surgery in Patients at Risk for Thromboembolic Complications
Abdominal surgery patients at risk include those who are over 40 years of age, obese, undergoing surgery under general anesthesia lasting longer than 30 minutes or who have additional risk factors such as malignancy or a history of deep vein thrombosis (DVT) or pulmonary embolism (PE).
In a double-blind, parallel group study of patients undergoing elective cancer surgery of the gastrointestinal, urological, or gynecological tract, a total of 1116 patients were enrolled in the study, and 1115 patients were treated. Patients ranged in age from 32 to 97 years (mean age 67 years) with 52.7% men and 47.3% women. Patients were 98% Caucasian, 1.1% Black, 0.4% Asian and 0.4% others. Enoxaparin sodium injection 40 mg subcutaneously, administered once a day, beginning 2 hours prior to surgery and continuing for a maximum of 12 days after surgery, was comparable to heparin 5000 U every 8 hours subcutaneously in reducing the risk of DVT. The efficacy data are provided below (seeTable 14).
Table 14 Efficacy of Enoxaparin Sodium Injection in the Prophylaxis of Deep Vein Thrombosis Following Abdominal Surgery Dosing Regimen
IndicationEnoxaparin Sodium
Injection
40 mg daily subcutaneously
n (%)
Heparin
5000 U q8h subcutaneously
n (%)- * VTE = Venous thromboembolic events which included DVT, PE, and death considered to be thromboembolic in origin.
- † CI = Confidence Interval
All Treated Abdominal Surgery Patients
555 (100)
560 (100)
Treatment Failures
Total VTE* (%)
56 (10.1)
(95% CI†: 8 to 13)63 (11.3)
(95% CI: 9 to 14)DVT Only (%)
54 (9.7)
(95% CI: 7 to 12)61 (10.9)
(95% CI: 8 to 13)In a second double-blind, parallel group study, enoxaparin sodium injection 40 mg subcutaneously once a day was compared to heparin 5000 U every 8 hours subcutaneously in patients undergoing colorectal surgery (one-third with cancer). A total of 1347 patients were randomized in the study and all patients were treated. Patients ranged in age from 18 to 92 years (mean age 50.1 years) with 54.2% men and 45.8% women. Treatment was initiated approximately 2 hours prior to surgery and continued for approximately 7 to 10 days after surgery. The efficacy data are provided below (seeTable 15).
Table 15 Efficacy of Enoxaparin Sodium Injection in the Prophylaxis of Deep Vein Thrombosis Following Colorectal Surgery Dosing Regimen
IndicationEnoxaparin Sodium
Injection
40 mg daily subcutaneously
n (%)
Heparin
5000 U q8h subcutaneously
n (%)- * VTE = Venous thromboembolic events which included DVT, PE, and death considered to be thromboembolic in origin.
- † CI = Confidence Interval
All Treated Colorectal
Surgery Patients673 (100)
674 (100)
Treatment Failures
Total VTE* (%)
48 (7.1)
(95% CI†: 5 to 9)45 (6.7)
(95% CI: 5 to 9)DVT Only (%)
47 (7.0)
(95% CI: 5 to 9)44 (6.5)
(95% CI: 5 to 8)14.2 Prophylaxis of Deep Vein Thrombosis Following Hip or Knee Replacement Surgery
Enoxaparin sodium injection has been shown to reduce the risk of postoperative deep vein thrombosis (DVT) following hip or knee replacement surgery.
In a double-blind study, enoxaparin sodium injection 30 mg every 12 hours subcutaneously was compared to placebo in patients with hip replacement. A total of 100 patients were randomized in the study and all patients were treated. Patients ranged in age from 41 to 84 years (mean age 67.1 years) with 45% men and 55% women. After hemostasis was established, treatment was initiated 12 to 24 hours after surgery and was continued for 10 to 14 days after surgery. The efficacy data are provided below (seeTable 16).
Table 16 Efficacy of Enoxaparin Sodium Injection in the Prophylaxis of Deep Vein Thrombosis Following Hip Replacement Surgery Dosing Regimen
IndicationEnoxaparin Sodium Injection
30 mg q12h subcutaneously
n (%)
Placebo
q12h subcutaneously
n (%)- * p value versus placebo = 0.0002
- † p value versus placebo = 0.0134
All Treated Hip Replacement Patients
50 (100)
50 (100)
Treatment Failures
Total DVT (%)
5 (10)*
23 (46)
Proximal DVT (%)
1 (2)†
11 (22)
A double-blind, multicenter study compared three dosing regimens of enoxaparin sodium injection in patients with hip replacement. A total of 572 patients were randomized in the study and 568 patients were treated. Patients ranged in age from 31 to 88 years (mean age 64.7 years) with 63% men and 37% women. Patients were 93% Caucasian, 6% Black, <1% Asian, and 1% others. Treatment was initiated within two days after surgery and was continued for 7 to 11 days after surgery. The efficacy data are provided below (seeTable 17).
Table 17 Efficacy of Enoxaparin Sodium Injection in the Prophylaxis of Deep Vein Thrombosis Following Hip Replacement Surgery Dosing Regimen
Indication10 mg daily subcutaneously
n (%)30 mg q12h subcutaneously
n (%)40 mg daily subcutaneously
n (%)- * p value versus enoxaparin sodium injection 10 mg once a day = 0.0008
- † p value versus enoxaparin sodium injection 10 mg once a day = 0.0168
All Treated Hip Replacement Patients
161 (100)
208 (100)
199 (100)
Treatment Failures
Total DVT (%)
40 (25)
22 (11)*
27 (14)
Proximal DVT (%)
17 (11)
8 (4)†
9 (5)
There was no significant difference between the 30 mg every 12 hours and 40 mg once a day regimens. In a double-blind study, enoxaparin sodium injection 30 mg every 12 hours subcutaneously was compared to placebo in patients undergoing knee replacement surgery. A total of 132 patients were randomized in the study and 131 patients were treated, of which 99 had total knee replacement and 32 had either unicompartmental knee replacement or tibial osteotomy. The 99 patients with total knee replacement ranged in age from 42 to 85 years (mean age 70.2 years) with 36.4% men and 63.6% women. After hemostasis was established, treatment was initiated 12 to 24 hours after surgery and was continued up to 15 days after surgery. The incidence of proximal and total DVT after surgery was significantly lower for enoxaparin sodium injection compared to placebo. The efficacy data are provided below (seeTable 18).
Table 18 Efficacy of Enoxaparin Sodium Injection in the Prophylaxis of Deep Vein Thrombosis Following Total Knee Replacement Surgery Dosing Regimen
IndicationEnoxaparin Sodium
Injection
30 mg q12h subcutaneously
n (%)
Placebo
q12h subcutaneously
n (%)- * p value versus placebo = 0.0001
- † CI = Confidence Interval
- ‡ p value versus placebo = 0.013
- § CL = Confidence Limit
All Treated Total Knee Replacement Patients
47 (100)
52 (100)
Treatment Failures
Total DVT (%)
32 (62)
(95% CI: 47 to 76)Proximal DVT (%)
7 (13)
(95% CI: 3 to 24)Additionally, in an open-label, parallel group, randomized clinical study, enoxaparin sodium injection 30 mg every 12 hours subcutaneously in patients undergoing elective knee replacement surgery was compared to heparin 5000 U every 8 hours subcutaneously. A total of 453 patients were randomized in the study and all were treated. Patients ranged in age from 38 to 90 years (mean age 68.5 years) with 43.7% men and 56.3% women. Patients were 92.5% Caucasian, 5.3% Black, and 0.6% others. Treatment was initiated after surgery and continued up to 14 days. The incidence of deep vein thrombosis was lower for enoxaparin sodium injection compared to heparin.
Extended Prophylaxis of Deep Vein Thrombosis Following Hip Replacement Surgery
In a study of extended prophylaxis for patients undergoing hip replacement surgery, patients were treated, while hospitalized, with enoxaparin sodium injection 40 mg subcutaneously, initiated up to 12 hours prior to surgery for the prophylaxis of postoperative DVT. At the end of the peri-operative period, all patients underwent bilateral venography. In a double-blind design, those patients with no venous thromboembolic disease were randomized to a post-discharge regimen of either enoxaparin sodium injection 40 mg (n = 90) once a day subcutaneously or to placebo (n = 89) for 3 weeks. A total of 179 patients were randomized in the double-blind phase of the study and all patients were treated. Patients ranged in age from 47 to 87 years (mean age 69.4 years) with 57% men and 43% women. In this population of patients, the incidence of DVT during extended prophylaxis was significantly lower for enoxaparin sodium injection compared to placebo. The efficacy data are provided below (seeTable 19).
Table 19 Efficacy of Enoxaparin Sodium Injection in the Extended Prophylaxis of Deep Vein Thrombosis Following Hip Replacement Surgery Post-Discharge Dosing Regimen
Indication (Post-Discharge)Enoxaparin Sodium Injection
40 mg daily subcutaneously
n (%)
Placebo
daily subcutaneously
n (%)- * p value versus placebo = 0.008
- † CI= Confidence Interval
- ‡ p value versus placebo = 0.537
All Treated Extended Prophylaxis Patients
90 (100)
89 (100)
Treatment Failures
Total DVT (%)
18 (20)
(95% CI: 12 to 30)Proximal DVT (%)
5 (6)‡
(95% CI: 2 to 13)7 (8)
(95% CI: 3 to 16)In a second study, patients undergoing hip replacement surgery were treated, while hospitalized, with enoxaparin sodium injection 40 mg subcutaneously, initiated up to 12 hours prior to surgery. All patients were examined for clinical signs and symptoms of venous thromboembolic (VTE) disease. In a double-blind design, patients without clinical signs and symptoms of VTE disease were randomized to a post-discharge regimen of either enoxaparin sodium injection 40 mg (n = 131) once a day subcutaneously or to placebo (n = 131) for 3 weeks. A total of 262 patients were randomized in the study double-blind phase and all patients were treated. Patients ranged in age from 44 to 87 years (mean age 68.5 years) with 43.1% men and 56.9% women. Similar to the first study the incidence of DVT during extended prophylaxis was significantly lower for enoxaparin sodium injection compared to placebo, with a statistically significant difference in both total DVT (enoxaparin sodium injection 21 [16%] versus placebo 45 [34%]; p = 0.001) and proximal DVT (enoxaparin sodium injection 8 [6%] versus placebo 28 [21%]; p = <0.001).
14.3 Prophylaxis of Deep Vein Thrombosis in Medical Patients with Severely Restricted Mobility During Acute Illness
In a double blind multicenter, parallel group study, enoxaparin sodium injection 20 mg or 40 mg once a day subcutaneously was compared to placebo in the prophylaxis of deep vein thrombosis (DVT) in medical patients with severely restricted mobility during acute illness (defined as walking distance of <10 meters for ≤3 days). This study included patients with heart failure (NYHA Class III or IV); acute respiratory failure or complicated chronic respiratory insufficiency (not requiring ventilatory support): acute infection (excluding septic shock); or acute rheumatic disorder (acute lumbar or sciatic pain, vertebral compression [due to osteoporosis or tumor], acute arthritic episodes of the lower extremities). A total of 1102 patients were enrolled in the study, and 1073 patients were treated. Patients ranged in age from 40 to 97 years (mean age 73 years) with equal proportions of men and women. Treatment continued for a maximum of 14 days (median duration 7 days). When given at a dose of 40 mg once a day subcutaneously, enoxaparin sodium injection significantly reduced the incidence of DVT as compared to placebo. The efficacy data are provided below (seeTable 20).
Table 20 Efficacy of Enoxaparin Sodium Injection in the Prophylaxis of Deep Vein Thrombosis in Medical Patients with Severely Restricted Mobility During Acute Illness Dosing Regimen
IndicationEnoxaparin Sodium Injection
20 mg daily subcutaneously
n (%)Enoxaparin Sodium Injection
40 mg daily subcutaneously
n (%)
Placebo
n (%)- * Treatment failures during therapy, between Days 1 and 14.
- † VTE = Venous thromboembolic events which included DVT, PE, and death considered to be thromboembolic in origin.
- ‡ CI = Confidence Interval
All Treated Medical Patients During Acute Illness
351 (100)
360 (100)
362 (100)
Treatment Failure*
Total VTE† (%)
43 (12.3)
16 (4.4)
43 (11.9)
Total DVT (%)
43 (12.3)
(95% CI‡ 8.8 to 15.7)16 (4.4)
(95% CI‡ 2.3 to 6.6 )41 (11.3)
(95% CI‡ 8.1 to 14.6 )Proximal DVT (%)
13 (3.7)
5 (1.4)
14 (3.9)
At approximately 3 months following enrollment, the incidence of venous thromboembolism remained lower in the enoxaparin sodium injection 40 mg treatment group versus the placebo treatment group.
14.4 Treatment of Deep Vein Thrombosis with or without Pulmonary Embolism
In a multicenter, parallel group study, 900 patients with acute lower extremity deep vein thrombosis (DVT) with or without pulmonary embolism (PE) were randomized to an inpatient (hospital) treatment of either (i) enoxaparin sodium injection 1.5 mg/kg once a day subcutaneously, (ii) enoxaparin sodium injection 1 mg/kg every 12 hours subcutaneously, or (iii) heparin intravenous bolus (5000 IU) followed by a continuous infusion (administered to achieve an aPTT of 55 to 85 seconds). A total of 900 patients were randomized in the study and all patients were treated. Patients ranged in age from 18 to 92 years (mean age 60.7 years) with 54.7% men and 45.3% women. All patients also received warfarin sodium (dose adjusted according to PT to achieve an International Normalization Ratio [INR] of 2.0 to 3.0), commencing within 72 hours of initiation of enoxaparin sodium injection or standard heparin therapy, and continuing for 90 days. Enoxaparin sodium injection or standard heparin therapy was administered for a minimum of 5 days and until the targeted warfarin sodium INR was achieved. Both enoxaparin sodium injection regimens were equivalent to standard heparin therapy in reducing the risk of recurrent venous thromboembolism (DVT and/or PE). The efficacy data are provided below (seeTable 21).
Table 21 Efficacy of Enoxaparin Sodium Injection in Treatment of Deep Vein Thrombosis With or Without Pulmonary Embolism Dosing Regimen*
IndicationEnoxaparin Sodium Injection
1.5 mg/kg daily subcutaneously
n (%)Enoxaparin Sodium Injection
1 mg/kg q12h subcutaneously
n (%)Heparin
aPTT Adjusted Intravenous Therapy
n (%)- * All patients were also treated with warfarin sodium commencing within 72 hours of enoxaparin sodium injection or standard heparin therapy.
- † VTE = venous thromboembolic event (DVT and/or PE).
- ‡ The 95% Confidence Intervals for the treatment differences for total VTE were:
enoxaparin sodium injection once a day versus heparin (-3.0 to 3.5)
enoxaparin sodium injection every 12 hours versus heparin (-4.2 to 1.7).All Treated DVT Patients with or without PE
298 (100)
312 (100)
290 (100)
Patient Outcome
Total VTE† (%)
13 (4.4)‡
9 (2.9)‡
12 (4.1)
DVT Only (%)
11 (3.7)
7 (2.2)
8 (2.8)
Proximal DVT (%)
9 (3.0)
6 (1.9)
7 (2.4)
PE (%)
2 (0.7)
2 (0.6)
4 (1.4)
Similarly, in a multicenter, open-label, parallel group study, patients with acute proximal DVT were randomized to enoxaparin sodium injection or heparin. Patients who could not receive outpatient therapy were excluded from entering the study. Outpatient exclusion criteria included the following: inability to receive outpatient heparin therapy because of associated comorbid conditions or potential for non-compliance and inability to attend follow-up visits as an outpatient because of geographic inaccessibility. Eligible patients could be treated in the hospital, but ONLY enoxaparin sodium injection patients were permitted to go home on therapy (72%). A total of 501 patients were randomized in the study and all patients were treated. Patients ranged in age from 19 to 96 years (mean age 57.8 years) with 60.5% men and 39.5% women. Patients were randomized to either enoxaparin sodium injection 1 mg/kg every 12 hours subcutaneously or heparin intravenous bolus (5000 IU) followed by a continuous infusion administered to achieve an aPTT of 60 to 85 seconds (in-patient treatment). All patients also received warfarin sodium as described in the previous study. Enoxaparin sodium injection or standard heparin therapy was administered for a minimum of 5 days. Enoxaparin sodium injection was equivalent to standard heparin therapy in reducing the risk of recurrent venous thromboembolism. The efficacy data are provided below (seeTable 22).
Table 22 Efficacy of Enoxaparin Sodium Injection in Treatment of Deep Vein Thrombosis Dosing Regimen* Enoxaparin Sodium Injection
1 mg/kg q12h subcutaneouslyHeparin
aPTT Adjusted Intravenous TherapyIndication n (%) n (%) - * All patients were also treated with warfarin sodium commencing on the evening of the second day of enoxaparin sodium injection or standard heparin therapy.
- † VTE = venous thromboembolic event (deep vein thrombosis [DVT] and/or pulmonary embolism [PE]).
- ‡ The 95% Confidence Intervals for the treatment difference for total VTE was: enoxaparin sodium injection versus heparin (-5.6 to 2.7).
All Treated DVT Patients
247 (100)
254 (100)
Patient Outcome
Total VTE† (%)
13 (5.3)‡
17 (6.7)
DVT Only (%)
11 (4.5)
14 (5.5)
Proximal DVT (%)
10 (4.0)
12 (4.7)
PE (%)
2 (0.8)
3 (1.2)
14.5 Prophylaxis of Ischemic Complications in Unstable Angina and Non-Q-Wave Myocardial Infarction
In a multicenter, double-blind, parallel group study, patients who recently experienced unstable angina or non-Q-wave myocardial infarction were randomized to either enoxaparin sodium injection 1 mg/kg every 12 hours subcutaneously or heparin intravenous bolus (5000 U) followed by a continuous infusion (adjusted to achieve an aPTT of 55 to 85 seconds). A total of 3171 patients were enrolled in the study, and 3107 patients were treated. Patients ranged in age from 25 to94 years (median age 64 years), with 33.4% of patients female and 66.6% male. Race was distributed as follows: 89.8% Caucasian, 4.8% Black, 2.0% Asian, and 3.5% other. All patients were also treated with aspirin 100 to 325 mg per day. Treatment was initiated within 24 hours of the event and continued until clinical stabilization, revascularization procedures, or hospital discharge, with a maximal duration of 8 days of therapy. The combined incidence of the triple endpoint of death, myocardial infarction, or recurrent angina was lower for enoxaparin sodium injection compared with heparin therapy at 14 days after initiation of treatment. The lower incidence of the triple endpoint was sustained up to 30 days after initiation of treatment. These results were observed in an analysis of both all-randomized and all-treated patients. The efficacy data are provided below (seeTable 23).
Table 23 Efficacy of Enoxaparin Sodium Injection in the Prophylaxis of Ischemic Complications in Unstable Angina and Non-Q-Wave Myocardial Infarction (Combined Endpoint of Death, Myocardial Infarction, or Recurrent Angina) Dosing Regimen*
IndicationEnoxaparin
Sodium
Injection
1 mg/kg
q12h subcutaneous
n (%)
Heparin
aPTT
Adjusted Intravenous
Therapy
n (%)
Reduction
(%)
p Value- * All patients were also treated with aspirin 100 to 325 mg per day.
- † Evaluation time points are after initiation of treatment. Therapy continued for up to 8 days (median duration of 2.6 days).
All Treated Unstable Angina and Non-Q-Wave MI Patients
1578 (100)
1529 (100)
Time point†
48 Hours
96 (6.1)
112 (7.3)
1.2
0.120
14 Days
261 (16.5)
303 (19.8)
3.3
0.017
30 Days
313 (19.8)
358 (23.4)
3.6
0.014
The combined incidence of death or myocardial infarction at all time points was lower for enoxaparin sodium injection compared to standard heparin therapy, but did not achieve statistical significance. The efficacy data are provided below (seeTable 24).
Table 24 Efficacy of Enoxaparin Sodium Injection in the Prophylaxis of Ischemic Complications in Unstable Angina and Non-Q-Wave Myocardial Infarction (Combined Endpoint of Death or Myocardial Infarction) Dosing Regimen*
IndicationEnoxaparin
Sodium
Injection
1 mg/kg
q12h subcutaneously
n (%)
Heparin
aPTT
Adjusted Intravenous
Therapy
n (%)
Reduction
(%)
p Value- * All patients were also treated with aspirin 100 to 325 mg per day.
- † Evaluation time points are after initiation of treatment. Therapy continued for up to 8 days (median duration of 2.6 days).
All Treated Unstable Angina and Non-Q-Wave
MI Patients1578 (100)
1529 (100)
Time point†
48 Hours
16 (1.0)
20 (1.3)
0.3
0.126
14 Days
76 (4.8)
93 (6.1)
1.3
0.115
30 Days
96 (6.1)
118 (7.7)
1.6
0.069
In a survey one year following treatment, with information available for 92% of enrolled patients, the combined incidence of death, myocardial infarction, or recurrent angina remained lower for enoxaparin sodium injection versus heparin (32.0% vs 35.7%).
Urgent revascularization procedures were performed less frequently in the enoxaparin sodium injection group as compared to the heparin group, 6.3% compared to 8.2% at 30 days (p = 0.047).
14.6 Treatment of Acute ST-Segment Elevation Myocardial Infarction
In a multicenter, double-blind, double-dummy, parallel-group study, patients with acute ST-segment elevation myocardial infarction (STEMI) who were to be hospitalized within 6 hours of onset and were eligible to receive fibrinolytic therapy were randomized in a 1:1 ratio to receive either enoxaparin sodium injection or unfractionated heparin.
Study medication was initiated between 15 minutes before and 30 minutes after the initiation of fibrinolytic therapy. Unfractionated heparin was administered beginning with an intravenous bolus of 60 U/kg (maximum 4000 U) and followed with an infusion of 12 U/kg per hour (initial maximum 1000 U per hour) that was adjusted to maintain an aPTT of 1.5 to 2 times the control value. The intravenous infusion was to be given for at least 48 hours. The enoxaparin sodium dosing strategy was adjusted according to the patient’s age and renal function. For patients younger than 75 years of age, enoxaparin sodium was given as a single 30 mg intravenous bolus plus a 1 mg/kg subcutaneous dose followed by a subcutaneous injection of 1 mg/kg every 12 hours. For patients at least 75 years of age, the intravenous bolus was not given and the subcutaneous dose was reduced to 0.75 mg/kg every 12 hours. For patients with severe renal insufficiency (estimated creatinine clearance of less than 30 mL per minute), the dose was to be modified to 1 mg/kg every 24 hours. The subcutaneous injections of enoxaparin sodium were given until hospital discharge or for a maximum of eight days (whichever came first). The mean treatment duration for enoxaparin sodium was 6.6 days. The mean treatment duration of unfractionated heparin was 54 hours.
When percutaneous coronary intervention was performed during study medication period, patients received antithrombotic support with blinded study drug. For patients on enoxaparin sodium, the PCI was to be performed on enoxaparin sodium (no switch) using the regimen established in previous studies, i.e. no additional dosing, if the last subcutaneous administration was less than 8 hours before balloon inflation, intravenous bolus of 0.3 mg/kg enoxaparin sodium if the last subcutaneous administration was more than 8 hours before balloon inflation.
All patients were treated with aspirin for a minimum of 30 days. Eighty percent of patients received a fibrin-specific agent (19% tenecteplase, 5% reteplase and 55% alteplase) and 20% received streptokinase.
Among 20,479 patients in the ITT population, the mean age was 60 years, and 76% were male. Racial distribution was: 87% Caucasian, 9.8% Asian, 0.2% Black, and 2.8% other. Medical history included previous MI (13%), hypertension (44%), diabetes (15%) and angiographic evidence of CAD (5%). Concomitant medication included aspirin (95%), beta-blockers (86%), ACE inhibitors (78%), statins (70%) and clopidogrel (27%). The MI at entry was anterior in 43%, non-anterior in 56%, and both in 1%.
The primary efficacy endpoint was the composite of death from any cause or myocardial re-infarction in the first 30 days after randomization. Total follow-up was one year.
The rate of the primary efficacy endpoint (death or myocardial re-infarction) was 9.9% in the enoxaparin sodium group, and 12% in the unfractionated heparin group, a 17% reduction in the relative risk, (P=0.000003) (seeTable 25).
Table 25 Efficacy of Enoxaparin Sodium Injection in the Treatment of Acute ST-Segment Elevation Myocardial Infarction Enoxaparin Sodium (N=10,256) UFH (N=10,223)
Relative Risk (95% CI)
P ValueNote: Urgent revascularization denotes episodes of recurrent myocardial ischemia (without infarction) leading to the clinical decision to perform coronary revascularization during the same hospitalization. CI denotes confidence intervals. Outcome at 48 hours
n (%)
n (%)
Death or Myocardial Re-infarction
478 (4.7)
531 (5.2)
0.90 (0.80 to 1.01)
0.08
Death
383 (3.7)
390 (3.8)
0.98 (0.85 to 1.12)
0.76
Myocardial Re-infarction
102 (1.0)
156 (1.5)
0.65 (0.51 to 0.84)
<0.001
Urgent Revascularization
74 (0.7)
96 (0.9)
0.77 (0.57 to 1.04)
0.09
Death or Myocardial Re-infarction
or Urgent Revascularization548 (5.3)
622 (6.1)
0.88 (0.79 to 0.98)
0.02
Outcome at 8 Days
Death or Myocardial Re-infarction
740 (7.2)
954 (9.3)
0.77 (0.71 to 0.85)
<0.001
Death
559 (5.5)
605 (5.9)
0.92 (0.82 to 1.03)
0.15
Myocardial Re-infarction
204 (2.0)
379 (3.7)
0.54 (0.45 to 0.63)
<0.001
Urgent Revascularization
145 (1.4)
247 (2.4)
0.59 (0.48 to 0.72)
<0.001
Death or Myocardial Re-infarction
or Urgent Revascularization874 (8.5)
1181 (11.6)
0.74 (0.68 to 0.80)
<0.001
Outcome at 30 Days
Primary efficacy endpoint
(Death or Myocardial Re-
infarction)1017 (9.9)
1223 (12.0)
0.83 (0.77 to 0.90)
0.000003
Death
708 (6.9)
765 (7.5)
0.92 (0.84 to 1.02)
0.11
Myocardial Re-infarction
352 (3.4)
508 (5.0)
0.69 (0.60 to 0.79)
<0.001
Urgent Revascularization
213 (2.1)
286 (2.8)
0.74 (0.62 to 0.88)
<0.001
Death or Myocardial Re-infarction
or Urgent Revascularization1199 (11.7)
1479 (14.5)
0.81 (0.75 to 0.87)
<0.001
The beneficial effect of enoxaparin sodium on the primary endpoint was consistent across key subgroups including age, gender, infarct location, history of diabetes, history of prior myocardial infarction, fibrinolytic agent administered, and time to treatment with study drug (see Figure 1); however, it is necessary to interpret such subgroup analyses with caution.
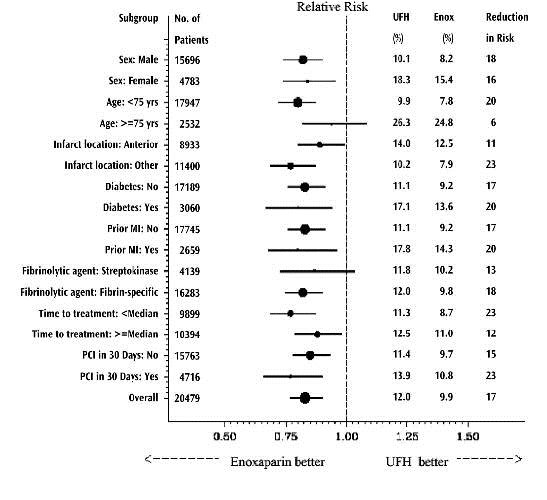
Figure 1. Relative Risks of and Absolute Event Rates for the Primary Endpoint at 30 Days in Various Subgroups*
*The primary efficacy endpoint was the composite of death from any cause or myocardial re-infarction in the first 30 days. The overall treatment effect of enoxaparin sodium as compared to the unfractionated heparin is shown at the bottom of the figure. For each subgroup, the circle is proportional to the number and represents the point estimate of the treatment effect and the horizontal lines represent the 95 % confidence intervals. Fibrin-specific fibrinolytic agents included alteplase, tenecteplase, and reteplase. Time to treatment indicates the time from the onset of symptoms to the administration of study drug (median: 3.2 hours).
The beneficial effect of enoxaparin sodium on the primary endpoint observed during the first 30 days was maintained over a 12 month follow-up period (see Figure 2).
There is a trend in favor of enoxaparin sodium during the first 48 hours, but most of the treatment difference is attributed to a step increase in the event rate in the UFH group at 48 hours (seen in Figure 2), an effect that is more striking when comparing the event rates just prior to and just subsequent to actual times of discontinuation. These results provide evidence that UFH was effective and that it would be better if used longer than 48 hours. There is a similar increase in endpoint event rate when enoxaparin sodium was discontinued, suggesting that it too was discontinued too soon in this study.
The rates of major hemorrhages (defined as requiring 5 or more units of blood for transfusion, or 15% drop in hematocrit or clinically overt bleeding, including intracranial hemorrhage) at 30 days were 2.1% in the enoxaparin sodium group and 1.4% in the unfractionated heparin group. The rates of intracranial hemorrhage at 30 days were 0.8% in the enoxaparin sodium group and 0.7% in the unfractionated heparin group. The 30-day rate of the composite endpoint of death, myocardial re-infarction or ICH (a measure of net clinical benefit) was significantly lower in the enoxaparin sodium group (10.1%) as compared to the heparin group (12.2%).
-
16 HOW SUPPLIED/STORAGE AND HANDLING
Enoxaparin sodium injection, USP is available in two concentrations (seeTables 26 and 27):
Table 26 100 mg/mL Concentration Dosage Unit / Strength* Anti-Xa Activity† Package Size
(per carton)
Label Color
NDC #- * Strength represents the number of milligrams of enoxaparin sodium in Water for Injection. Enoxaparin sodium injection, USP 30 and 40 mg prefilled syringes, and 60, 80, and 100 mg graduated prefilled syringes each contain 10 mg enoxaparin sodium per 0.1 mL Water for Injection.
- † Approximate anti-Factor Xa activity based on reference to the W.H.O. First International Low Molecular Weight Heparin Reference Standard.
- ‡ Each enoxaparin sodium injection, USP prefilled syringe is for single, one-time use only and is affixed with a 27 gauge × 1/2 inch needle.
- § Each enoxaparin sodium injection, USP multiple-dose vial contains 15 mg benzyl alcohol per 1 mL as a preservative.
Prefilled Syringes‡
30 mg / 0.3 mL
3000 IU
10 syringes
Medium Blue
0781-3133-63
40 mg / 0.4 mL
4000 IU
10 syringes
Yellow
0781-3224-64
Graduated Prefilled Syringes‡
60 mg / 0.6 mL
6000 IU
10 syringes
Orange
0781-3356-66
80 mg / 0.8 mL
8000 IU
10 syringes
Brown
0781-3428-68
100 mg / mL
10,000 IU
10 syringes
Black
0781-3500-69
Multiple-Dose Vial§
300 mg/3 mL
30,000 IU
1 vial
Red
0781-3122-93
Table 27 150 mg/mL Concentration
Dosage Unit / Strength*
Anti-Xa Activity†
Package Size
(per carton)Syringe Label Color
NDC #- * Strength represents the number of milligrams of enoxaparin sodium in Water for Injection. Enoxaparin sodium injection, USP 120 mg and 150 mg graduated prefilled syringes contain 15 mg enoxaparin sodium per 0.1 mL Water for Injection.
- † Approximate anti-Factor Xa activity based on reference to the W.H.O. First International Low Molecular Weight Heparin Reference Standard.
- ‡ Each enoxaparin sodium injection, USP graduated prefilled syringe is for single, one-time use only and is affixed with a 27 gauge × 1/2 inch needle.
Graduated Prefilled Syringes‡
120 mg / 0.8 mL
12,000 IU
10 syringes
Purple
0781-3612-68
150 mg / mL
15,000 IU
10 syringes
Navy Blue
0781-3655-69
Store at 20° to 25°C (68° to 77°F) [see USP Controlled Room Temperature].
Do not store the multiple-dose vials for more than 28 days after the first use.
-
17 PATIENT COUNSELING INFORMATION
If patients have had neuraxial anesthesia or spinal puncture, and particularly, if they are taking concomitant NSAIDs, platelet inhibitors, or other anticoagulants, advise them to watch for signs and symptoms of spinal or epidural hematoma, such as tingling, numbness (especially in the lower limbs) and muscular weakness. Instruct the patient to seek immediate medical attention if any of these symptoms occur.
Inform patients:
- of the instructions for injecting enoxaparin sodium injection if they continue enoxaparin sodium injection therapy after discharge from the hospital.
- that it may take them longer than usual to stop bleeding.
- that they may bruise and/or bleed more easily when they use enoxaparin sodium injection.
- that they should report any unusual bleeding, bruising, or signs of thrombocytopenia (such as a rash of dark red spots under the skin) to their physician [seeWarnings and Precautions (5.1, 5.5)].
- that risks are associated with the use of benzyl alcohol, a preservative in enoxaparin sodium injection multi-dose vials, in neonates, infants, and pregnant women.
- to tell their physicians and dentists they are taking enoxaparin sodium injection and/or any other product known to affect bleeding before any surgery is scheduled and before any new drug is taken [seeWarnings and Precautions (5.1, 5.3)].
- to tell their physicians and dentists of all medications they are taking, including those obtained without a prescription, such as aspirin or other NSAIDs [seeDrug Interactions (7)].
Distributed by
Sandoz Inc., Princeton, NJ 08540
Rev. January 2019
- Package/Label Display Panel
- Package/Label Display Panel
- Package/Label Display Panel
- Package/Label Display Panel
- Package/Label Display Panel
-
INGREDIENTS AND APPEARANCE
ENOXAPARIN SODIUM
enoxaparin sodium injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 55154-5440(NDC:0781-3133) Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ENOXAPARIN SODIUM (UNII: 8NZ41MIK1O) (ENOXAPARIN - UNII:E47C0NF7LV) ENOXAPARIN SODIUM 100 mg in 1 mL Inactive Ingredients Ingredient Name Strength WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 55154-5440-5 5 in 1 BAG 07/23/2010 10/31/2018 1 0.3 mL in 1 SYRINGE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA077857 07/23/2010 10/31/2018 ENOXAPARIN SODIUM
enoxaparin sodium injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 55154-5441(NDC:0781-3224) Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ENOXAPARIN SODIUM (UNII: 8NZ41MIK1O) (ENOXAPARIN - UNII:E47C0NF7LV) ENOXAPARIN SODIUM 100 mg in 1 mL Inactive Ingredients Ingredient Name Strength WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 55154-5441-5 5 in 1 BAG 07/23/2010 1 0.4 mL in 1 SYRINGE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA077857 07/23/2010 ENOXAPARIN SODIUM
enoxaparin sodium injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 55154-5442(NDC:0781-3356) Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ENOXAPARIN SODIUM (UNII: 8NZ41MIK1O) (ENOXAPARIN - UNII:E47C0NF7LV) ENOXAPARIN SODIUM 100 mg in 1 mL Inactive Ingredients Ingredient Name Strength WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 55154-5442-5 5 in 1 BAG 07/23/2010 1 0.6 mL in 1 SYRINGE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA077857 07/23/2010 ENOXAPARIN SODIUM
enoxaparin sodium injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 55154-5443(NDC:0781-3428) Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ENOXAPARIN SODIUM (UNII: 8NZ41MIK1O) (ENOXAPARIN - UNII:E47C0NF7LV) ENOXAPARIN SODIUM 100 mg in 1 mL Inactive Ingredients Ingredient Name Strength WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 55154-5443-5 5 in 1 BAG 07/23/2010 1 0.8 mL in 1 SYRINGE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA077857 07/23/2010 ENOXAPARIN SODIUM
enoxaparin sodium injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 55154-5444(NDC:0781-3500) Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ENOXAPARIN SODIUM (UNII: 8NZ41MIK1O) (ENOXAPARIN - UNII:E47C0NF7LV) ENOXAPARIN SODIUM 100 mg in 1 mL Inactive Ingredients Ingredient Name Strength WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 55154-5444-5 5 in 1 BAG 07/23/2010 06/30/2018 1 1 mL in 1 SYRINGE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA077857 07/23/2010 06/30/2018 Labeler - Cardinal Health (603638201)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.